Abstract
Two oncogenic pathways have been hypothesized for multiple myeloma (MM) and premalignant monoclonal gammopathy of undetermined significance (MGUS) tumors: a nonhyperdiploid pathway associated with a high prevalence of IgH translocations and a hyperdiploid pathway associated with multiple trisomies of 8 chromosomes. Cyclin D1, D2, or D3 expression appears to be increased and/or dysregulated in virtually all MM tumors despite their low proliferative capacity. Translocations can directly dysregulate CCND1 (11q13) or CCND3 (6p21), or MAF (16q23) or MAFB (20q11) transcription factors that target CCND2. Biallelic dysregulation of CCND1 occurs in nearly 40% of tumors, most of which are hyperdiploid. Other tumors express increased CCND2, either with or without a t(4;14) translocation. Using gene expression profiling to identify 5 recurrent translocations, specific trisomies, and expression of cyclin D genes, MM tumors can be divided into 8 TC (translocation/cyclin D) groups (11q13, 6p21, 4p16, maf, D1, D1+D2, D2, and none) that appear to be defined by early, and perhaps initiating, oncogenic events. However, despite subsequent progression events, these groups have differing gene expression profiles and also significant differences in the prevalence of bone disease, frequency at relapse, and progression to extramedullary tumor.
Introduction
A diversity of numeric and structural cytogenetic abnormalities are shared by premalignant monoclonal gammopathy of undetermined significance (MGUS) and malignant multiple myeloma (MM) tumors.1,2 The prevalence of IgH translocations is about 50%, whereas the prevalence of IgL translocations is no more than 10% to 20%. About 40% of MM tumors have Ig translocations involving 5 recurrent chromosomal partners and oncogenes: 11q13 (CCND1); 4p16 (FGFR3 and MMSET); 6p21 (CCND3); 16q23 (MAF); and 20q11 (MAFB). Recurrent translocations appear to be mediated mostly by errors in IgH switch recombination that occur during the maturation of B cells in germinal centers.3 Translocations involving 8q24 (MYC) and an Ig locus are very late progression events. Little is known about other (mostly rare) chromosomal partners (and oncogenes).
Hyperdiploid tumors, which include about 50% of MM tumors, often have multiple trisomies involving chromosomes 3, 5, 7, 9, 11, 15, 19, and 21 and a substantially lower prevalence of IgH translocations and monosomy of chromosome 13 compared with nonhyperdiploid tumors.2 Trisomies of these same chromosomes also occur in premalignant MGUS tumors. This led to the proposal that there are 2 early pathways of pathogenesis for MM: a nonhyperdiploid pathway that often involves an early, perhaps initiating, IgH translocation and a hyperdiploid pathway that facilitates transformation by a yet to be determined mechanism.4
Recently, we suggested that dysregulation of 1 of the 3 cyclin D genes is a unifying oncogenic event in MM.5 The goal of the present study is to gain a better understanding of how cyclin D dysregulation, Ig translocations, and hyperdiploidy contribute to different pathways of pathogenesis and to different phenotypic consequences for MM tumors.
Patients, materials, and methods
Samples
We studied 231 patients with newly diagnosed MM, 30 with relapsed MM, 12 with MGUS, 32 human myeloma cell lines (HMCLs), and 14 control subjects. The institutional review board of the University of Arkansas for Medical Sciences approved the research studies, and all subjects provided written informed consent in accordance with the Declaration of Helsinki. The HMCLs have been described previously.6-10
Plasma-cell isolation and gene expression profiling
Isolation of plasma cells (PCs) and profiling of RNA was performed as described.11,12 Gene expression intensity values, measured with the use of MAS software, version 5.01 (Affymetrix, Santa Clara, CA), were log transformed, normalized to the median, and analyzed using GeneSpring 7 (Silicon Genetics, Redwood City, CA).
Contamination of MM tumor and normal PC samples
Some MM samples coexpressed a number of genes characteristic of normal PCs. These included specific variable region genes from the Ig heavy and light chains, as well as IgM, IgD, IgE, and CD19, suggesting the presence of a major polyclonal PC contamination. Eight samples (P257, P377, P506, P524, P532, P551, P594, P633) had expression of these genes at levels equivalent to normal PCs and also lacked expression of genes characteristic of MMPCs. On further review, we concluded that these patients all had macrofocal disease, with no evidence of diffuse marrow involvement and a good prognosis. Contamination of purified normal PCs (typically < 1% of mononuclear cells in the bone marrow [BM]) with other cells was a more significant problem. We excluded 26 of the normal PC samples from analysis because of apparent contamination by monocyte/macrophages or by pre-B-cells.
Assignment of 261 MM tumors to 8 groups
Tumors were assigned to 8 different translocation/cyclin D (TC) groups based on the RNA expression levels of 8 genes (CCND1, CCND2, CCND3, FGFR3, MMSET, MAF, ITGB7, and CX3CR1). For each sample, the relative expression level was a fraction of the highest signal (1.0) for that gene in any of the samples analyzed (Supplemental Worksheet, Table S1; see the Supplemental Materials link at the top of the online article at the Blood website). Samples were assigned sequentially to the 8 groups in the order described. The first 4 groups were based on recurrent IgH translocations. Group 4p16 included 42 samples with FGFR3 greater than 0.3 or MMSET greater than 0.1. The maf group included 19 samples with integrin β7 (ITGB7) greater than 0.18 (and CX3CR1 > 0.02). Eleven of these samples had MAF greater than 0.27, whereas the remaining 8 samples had MAF less than 0.1; 4 (P187, P266, P504, and P563) of these latter 8 samples were confirmed to overexpress MAFB by analysis on a U133 Affymetrix chip (data not shown). Group 6p21 included 7 samples with CCND3 greater than 0.5, and group 11q13 has 40 samples with CCND1 (average of all 3 CCND1 probe sets) greater than 0.25. The remaining 4 groups were based solely on increased expression of CCND1 and/or CCND2 in tumors compared with normal bone marrow plasma cells (BMPCs; CCND1 < 0.012 and CCND2 < 0.09). For 102 tumors with CCND1 greater than 0.024 (at least twice the value of the highest normal BMPC sample), 81 samples with CCND2 less than 0.09 were assigned to the D1 group, and 21 samples with CCND2 greater than 0.09 were assigned to the D1+D2 group. For the remaining tumor samples (all with CCND1 < 0.024), 45 with CCND2 greater than 0.09 were assigned to the D2 group, and 6 with CCND2 less than 0.07 were assigned to the none group. Although assignment of most tumors is reasonably straightforward, the boundaries distinguishing the groups cannot be determined with certainty. Previously published results validate the use of expression arrays for assignment of samples to the 4p16, 6p21, and 11q13 translocation groups (Zhan et al13). Additional validation of the maf group is provided by the fact that this group forms an uninterrupted cluster by an unsupervised cluster analysis (not shown). Further validation of assignments to these 8 groups is based on conventional cytogenetic analyses for the 101 of 261 MM tumors for which abnormal tumor karyotypes were generated (Supplemental Worksheet, Table S2). Conventional cytogenetics detected a classical t(11;14) in 12 of 18 samples in the 11q13 group but in 0 of 37 samples in the D1 group and 1 of 6 samples in the D1+D2 group; sample P092 in the D1+D2 group had a t(11;14) in 27% of tumor cells despite a relative CCND1 expression level of 0.052.
An expression-based proliferation index (PI) was calculated using the median value of 12 genes associated with proliferation (TYMS, TK1, CCNB1, MKI67, KIAA101, KIAA0186, CKS1B, TOP2A, UBE2C, ZWINT, TRIP13, KIF11), scaled to the maximum value among all samples.14 In an independent data set we have found a good correlation (r = 0.73) between the expression-based PI and the plasma-cell labeling index (PCLI; data not shown).
Identifying CCND1 alleles with Hpa II polymorphism in DNA and RNA
Exon 4 sense oligonucleotides for cDNA (X59578) (CTCTGTGCCACAGATGTGAA) and genomic DNA (AP001888) (GCAGTGCAAGGCCTGAACCTGAGGAGC) were perfect matches, but antisense oligonucleotides in intron 4 (GGATTCAAGTTAGGCAAGGCTGCCTGGGACA) and exon 5 (AGCAGGGCTTCGATCTGCTCCTGGCAGGAACGGAGGCAGT) were designed to eliminate a HpaII site that in each case occurred downstream of the polymorphic HpaII site (polymorphine at nucleotide [nt] 870 in cDNA and at nt 9630 in genomic DNA). An annealing temperature of 60°C was used for each polymerase chain reaction (PCR) reaction. The HpaII-digested product was analyzed on a 4% NuSieve-0.5% standard agarose gel to distinguish the A (undigested 138-base pair (bp) genomic or 203-bp cDNA PCR product) and G (92 + 46-bp genomic or 161 + 42-bp cDNA HpaII products) alleles. For sequence analyses of the PCR products, the corresponding sense oligonucleotides were used as sequencing primers.
Results
Different patterns of cyclin D expression in MM
Cyclin D genes (D1, D2, D3) are expressed at low levels in quiescent cells but in response to growth factors they are transcriptionally up-regulated and expressed in virtually all proliferating cells.15 We analyzed the relative RNA expression of all 3 cyclin D genes in 314 samples, including normal BMPCs, plasmablasts (PBs), 231 untreated and 30 relapsed MM tumors, and a panel of HMCLs (Figure 1; Figure S1). Highly proliferative PBs have substantially increased levels of CCND2 compared with normal BMPCs that express low levels of CCND2 and CCND3 but little or no CCND1.16 We subdivided the 261 MM tumors into 8 TC groups: 4 groups based on oncogenes dysregulated by 5 recurrent Ig translocations (4p16, 11q13, 6p21, maf), and then another 4 groups based on increased expression of cyclins D1 and/or D2 compared with normal BMPCs. The expression levels of the cyclin D genes and 5 other genes were used to identify all groups (Figure 1; also see “Assignment of 261 MM tumors to 8 groups”). With the exception of tumors in the 6p21 group, MM tumors express CCND3 at a low level that is comparable to normal BMPCs. Tumors in the 11q13 group express a markedly high level of CCND1. Tumors in the maf group express the highest levels of CCND2, with one tumor (P187) also expressing a very high level of CCND1 because of a coexisting t(11;14) translocation.13 Tumors in the 4p16 group uniformly express CCND2 at higher levels than normal BMPCs. However, several tumors in the 4p16 and maf groups also express slightly increased levels of CCND1. For the 60% of tumors not having 1 of the 5 recurrent Ig translocations, nearly half (31% overall) express increased levels of CCND1 and are assigned to a D1 group. Tumors in the D1+D2 group (8% overall) express increased levels of CCND1 and CCND2, and tumors in the D2 group express increased levels of CCND2. Finally, about 2% of tumors are assigned to the none group since they do not express increased levels of cyclins D1, D2, or D3 compared with normal BMPCs. Three of 6 tumors in the none group have an expression profile indistinguishable from normal BMPCs, consistent with little or no contribution of tumor cells to the observed expression profile. Highly proliferating PBs and HMCLs express increased levels of at least one cyclin D gene and have a high expression PI (Figure 1). In contrast, normal BMPCs and most MM tumors have a low PI. Importantly, for MM tumors there appears to be no obvious correlation that relates the level of cyclin D expression with the PI.
Figure 1.
Identification of TC groups in MM by RNA expression profiling. The samples are 6 peripheral blood-generated plasmablasts and 1 reactive plasmacytosis (PB) (5), 14 bone marrow PCs (PC) from healthy volunteers, samples from newly diagnosed (231) or relapsed (30) MM, and 32 human myeloma cell lines (HMCL). In addition they are all samples from patients with newly diagnosed (231) or relapsed MM (30). Among these 261 samples there are 42 with elevated FGFR3 and/or MMSET (4p16), 19 with elevated MAF or ITGB7 and CX3CR1 as surrogates for MAFB (maf), 7 with elevated CCND3 (6p21), 40 with high CCND1 (11q13), 81 with lower levels of CCND1 (D1), 21 with lower levels of CCND1 and elevated CCND2 (D1+D2), 45 remaining patients with elevated CCND2 (D2), and 6 patients without an elevated cyclin D (none). The relative level of expression of each gene in each sample is shown. For cyclin D1 (CCND1), the expression of the long-form mRNA is in dark green and total mRNA is in light green. The fifth line shows a PI calculated from the log of the median of the normalized values for 12 genes associated with proliferation. The values for PB were extrapolated from a HuFL dataset.16 The bottom line shows a chromosome 3, 5, 7, 9, 11, 15, 19, 21 index (CI) calculated from the median of the normalized values for genes on a given chromosome. The deviation from 1 for the average of 8 chromosomes (3, 5, 7, 9, 11, 15, 19, and 21) is plotted.
Patterns of translocation and cyclin D expression in MGUS, relapsed MM, and HMCLs
Given that MGUS shares many of the genetic features of MM, including recurrent IgH translocations and the presence of multiple trisomies, we examined the expression of the same 8 genes in 12 individuals with MGUS (Figure S1). The MGUS samples fall neatly into 5 of the TC groups (maf, 1; 11q13, 3; D1, 4; D1+D2, 1; and D2, 3). Consistent with a reported lower frequency of t(4;14) in MGUS,2 and the small sample size, no examples of 4p16, 6p21, or none were identified. Similarly, relapsed MM was represented in each of the TC groups with an underrepresentation in D1 (10% vs 33%; P = .009) and overrepresentation in D1+D2 (17% vs 6%; P = .03). In contrast, no groupings in D1, D1+D2, or none were identified among the HMCLs, which instead were overrepresented in the 4p16 (31% vs 16%; P = .03) and maf (28% vs 7%; P <.001) groups.
Validation of cyclin D mRNA expression
We provide validation for the levels of cyclin D expression in 3 ways. First, we have virtually identical results for each of the cyclin D genes based on a pair-wise comparison of the same tumor samples on 3 kinds of Affymetrix chips (FL6800 with one probe set for each gene; U95A with 3 probe sets for D1, 2 probe sets each for D2 and D3; U133 Plus 2.0 with 2 probe sets for D1, 4 probe sets for D2, and one probe set for D3; data not shown). Second, we have been able to successfully identify reproducible TC groups in samples prepared and analyzed by 3 other groups of investigators (the Mayo Clinic Myeloma and Dysproteinemia Disease Oriented Group [MADDOG]; the Translational Genomics Research Institute [TGEN]; and the Eastern Cooperative Oncology Group [ECOG]; data not shown). Finally, our results for the expression of cyclin D1 RNA in MM tumors is fully in accord with the published results of Soverini et al17 and Specht et al,18 both of whom did real-time PCR for cyclin D1 RNA expression. Specifically, Specht et al18 analyzed formalin-fixed, paraffin-imbedded blocks of MM tumor cells and showed that 11 (23%) of 48 of tumors expressed high levels of cyclin D1 RNA and had t(11;14) translocations (similar to our 11q group); whereas 15 (31%) of 48 of samples expressed low to intermediate levels of cyclin D1 RNA and had polysomy of chromosome 11 in 13 of 15 samples but no translocation involving cyclin D1 (similar to our D1 and D1+D2 groups that together are found in 102/261 [39%] MM tumors).
Transdysregulation of CCND1 in D1 group
Cyclin D1 has a HpaII A>G polymorphism.19 For 26 MM tumors in the D1 group, 5 were homozygous for the A allele, 8 for the G allele, and 13 were heterozygous, a result consistent with the normal allele frequency (58% G). Seven tumors had twice as many copies of the A allele as the G allele, 4 tumors had twice as many copies of the G allele, and 2 tumors had an equal content of the 2 alleles. This result is consistent with the presence of trisomy 11 in about 90% of patients in the D1 group (see “Genetic signature of multiple trisomies in the D1 group”). It indicates that trisomy results from disomy of one parental chromosome and also that none of these tumors have additional amplification of one cyclin D allele. Importantly, all but one of 13 D1 group tumors that are heterozygous for the 2 CCND1 alleles express both alleles at a level that is similar to the gene content (Figure 2). The one exception (tumor P092) had a t(11;14) translocation detected by a conventional karyotypic analysis but was placed in the D1+D2 group instead of the 11q13 group because of the inexplicably low level of CCND1 expression. We also analyzed cDNA from 12 MM tumors in the 11q13 group. As expected, each tumor in this group expressed either the G allele (10) or the A allele (2), but none expressed both alleles despite the fact that at least 4 of these tumors contained both the A and G alleles. Unlike tumors with a t(11;14) translocation that express CCND1 from one structurally altered allele, D1 group tumors express CCND1 from both alleles.
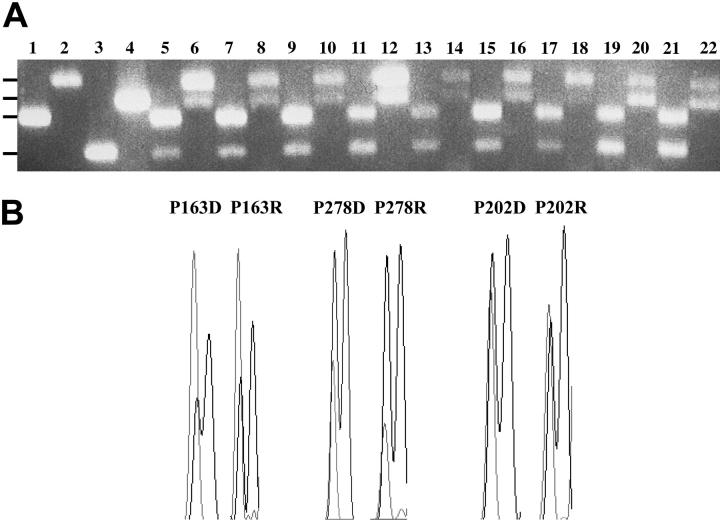
Figure 2.
Biallelic expression of CCND1 alleles in D1 group of MM tumors. Paired genomic DNA and cDNA samples were used to PCR amplify 138-bp exon 4-intron 4 or, respectively, 203-bp exon 4-exon 5 DNA fragments that include an A>G polymorphism at the ultimate exon 4 nucleotide. (A) The resultant fragments were digested with HpaII, which generates 92 + 46-bp fragments or, respectively, 161 + 42-bp fragments when a G is present at the polymorphic site. Paired HpaII-digested samples were subjected to electrophoresis on a 4% Nusieve-0.5% agarose gel. Odd lanes contain genomic fragments; subsequent even lanes contain the corresponding cDNA fragment. Lanes 1-2, homozygous A allele; lanes 3-4, homozygous G allele; lanes 5-22, 9 MM tumor samples. The positions of the 203-bp, 161-bp, 138-bp, and 92-bp fragments are indicated at the left. (B) Paired sequence tracings of genomic and cDNA fragments from representative tumors that have an excess of the A allele (dotted lines), the G allele (solid lines), or equal representation of both alleles. The polymorphic A>G nucleotide and the subsequent G nucleotide are shown. Further details in “Patients, materials, and methods.”
Genetic signature of multiple trisomies in the D1 group
Noting that the expression of many genes from chromosome 15 distinguishes the D1 group (Supplemental Worksheet, Table S3), we then determined that genes from chromosomes 3, 5, 7, 9, 11, 15, 19, and 21 were overrepresented (Figure 3A). Since these chromosomes often are trisomic in hyperdiploid MM, we suspected that this represented the gene expression signature of hyperdiploidy. In support of this conclusion, we analyzed an acute lymphoblastic leukemia (ALL) dataset20 and found that genes overexpressed in hyperdiploid ALL tumors, compared with other ALL tumors, were overrepresented on chromosomes 6, 10, 14, 18, 21, and X, the chromosomes most frequently trisomic in hyperdiploid ALL.
Figure 3.
Trisomy of chromosomes 3, 5, 7, 9, 11, 15, 19, and 21 in D1 group. (A) Chromosome localization of genes overexpressed in D1 group and in hyperdiploid ALL. For both the hyperdiploid greater than 50 subgroup of ALL and the D1 group of MM, a list of 618 (ALL) or 545 (MM) genes overexpressed within that group, compared with all other patients with ALL or MM, was generated. From these lists, the ratio of the number of observed to expected genes from each chromosome is plotted. (B) Chromosome index in ALL and MM. For each patient, a chromosome index was calculated for each chromosome using the median level of expression of the genes on that chromosome and plotted with chromosome 1 at the top, down to X at the bottom. No index was calculated for chromosome Y. For the MM samples, this chromosome index was normalized to the median value in BMPCs. A color scale on the left indicates red above 1.3, yellow for 1, and green below 0.7. Patients with MM are grouped as described in Figure 1. The patients with ALL are grouped based on the genetics as described in Yeoh et al20 (TEL, T, normal, MLL, hyperdiploid, EZA, BCR). See also Supplemental Worksheet, data for Figure 3.
To examine trisomies in individual tumors we calculated for each sample an expression-based ploidy index for each chromosome. With a trisomy, copy number changes in gene expression should result in a slightly higher median expression (see “Validation of multiple trisomy expression signature” for validation). We determined the median level of expression of genes from each chromosome for the ALL and MM tumors and plotted the results on a red-yellow-green color scale (Figure 3B). Higher median expression from the mostly even-number chromosomes in hyperdiploid ALL and from the 8 odd-number chromosomes in D1 group of MM appears as alternating red-yellow stripes on these plots. This expression signature extends into the D1+D2 group and also occurs in nearly half of tumors in the D2 group (also see chromosome expression index for 8 odd chromosomes in Figure 1). Similarly, in MGUS this profile was evident in 3 of 4 D1 tumors and in the one D1+D2 tumor (data not shown). Another striking feature of this plot is the low median expression of genes from chromosome 13, most notably in the 4p16 and maf groups. This is consistent with the very high prevalence of monosomy 13 previously reported in these groups.2,21,22 More information can be obtained when the index is divided into short and long chromosome arm indices (Figure S2). For example, it appears that increased expression from 1q is most common in the 4p16 group but also occurs with a relatively high prevalence in the D1+D2 and D2 groups and in the HMCLs.
Validation of multiple trisomy expression signature
The availability of cytogenetic analyses for 101 MM tumors (Supplemental Worksheet, Table S2) enabled a direct comparison of chromosome content and gene expression patterns. The assignment of tumors into the 8 TC groups shows a similar distribution for the 101 tumors with abnormal karyotypes compared with the full set of 261 tumors (Tables 1, 2). Fifty-six of the 101 tumors are classified as hyperdiploid based on a content of 48 to 75 chromosomes. Hyperdiploidy is strongly associated with multiple trisomies involving chromosomes 3, 5, 7, 9, 11, 15, 19, and 21, with 52 (93%) of the hyperdiploid tumors but only 1 (2%) of the nonhyperdiploid tumors having trisomies of 4 or more of these 8 chromosomes. Relaxing the stringency to trisomies of 3 or more of these chromosomes identifies the same 52 hyperdiploid tumors but identifies 3 additional nonhyperdiploid tumors The chromosome expression index showed 43 hyperdiploid and 3 nonhyperdiploid tumors with at least 4 of these 8 chromosomes having a chromosome expression index of at least 1.1; decreasing the stringency to at least 3 chromosomes identified 47 hyperdiploid and 5 nonhyperdiploid tumors. There appears to be a reasonable, albeit imperfect, concordance of karyotypic and expression analyses in determining which tumors contain extra copies of at least 3 of these 8 odd chromosomes.
Table 1.
Validation of gene expression calculated chromosome index (CI)
|
MM with abnormal karyotype
|
||||
|---|---|---|---|---|
| TC group | n | HD | T (K) | T (CI) |
| 6p21 | 2 | 1 | 0 | 0 |
| 11q13 | 18 | 2 | 0 | 0 |
| D1 | 37 | 34 | 35 | 35 |
| D1 + D2 | 6 | 4 | 4 | 5 |
| D2 | 12 | 7 | 7 | 4 |
| none | 2 | 2 | 2 | 1 |
| 4p16 | 19 | 5 | 5 | 6 |
| maf | 5 | 1 | 0 | 1 |
| Total | 101 | 56 | 53 | 52 |
HD indicates 48-75 chromosomes by karyotype; T (K), more than 4 trisomies of 8 odd chromosomes; and T (CI), more than 3 of 8 odd chromosomes have a gene expression calculated chromosome expression index of greater than 1.1. Data summarized in this table is generated from the data for individual tumor samples in the Supplemental Worksheet, Tables S1 and S2.
Table 2.
Clinical and genetic features of translocation and cyclin D (TC) molecular subgroups of multiple myeloma
|
Multiple trisomies
|
MRI positive
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| TC group | Recurrent tx | Gene(s) at breakpoint | Dysregulated D cyclin | % of untreated patients | % of 30 relapsed patients | n | %* | PI greater than 0.2, %† | n | %‡ |
| 6p21 | 6p21 | CCND3 | D3 | 3 | 3 | 7 | 29 | 14 | 5 | 100 |
| 11q13 | 11q13 | CCND1 | D1 | 16 | 17 | 40 | 0 | 18 | 27 | 94∥ |
| D1 | none | none | D1 | 34∥ | 10∥ | 81 | 93§ | 5§ | 57 | 86 |
| D1 + D2 | none | none | D1 + D2 | 6∥ | 17∥ | 21 | 86§ | 43∥ | 13 | 100∥ |
| D2 | none | none | D2 | 17 | 20 | 45 | 40 | 16 | 27 | 67 |
| none | none | none | none | 2 | 3 | 6 | 33 | 17 | 4 | 100 |
| 4p16 | 4p16 | FGFR3/MMSET | D2 | 15 | 23 | 42 | 29§ | 21 | 28 | 57∥ |
| maf | 16q23, 20q11 | MAF, MAFB | D2 | 7 | 7 | 19 | 16§ | 32 | 11 | 55∥ |
| Total | – | – | – | 100 | 100 | 261 | 50 | 17 | 172 | 79 |
– indicates not applicable.
Percentage of samples within each TC group with gene expression profiling evidence for 3 or more trisomies of chromosomes 3, 5, 7, 9, 11, 15, 19, or 21
Percentage of samples within each TC group with an expression PI greater then 0.2. There is a PI >0.2 in 67% of relapsed samples, and 10% of newly diagnosed MM (P < 10-13)
Percentage of samples within each TC group from patients with lytic lesions on MRI. In pairwise comparisons, each of groups 11q13, D1, and D1 + D2 is significantly different (P < .05) from each of groups D2, 4p16, and maf
P < .001
P < .05
A shared phenotype for the D1 and D1+D2 groups
The level of CCND1 mRNA in the group D1 and D1+D2 tumors is almost always lower than for group 11q13 tumors. In addition, there is differential expression of the alternatively polyadenylated forms of CCND1 mRNA, with group 11q13 tumors expressing mostly the 2.2-kilobase (kb) mRNA form and the group D1 and D1+D2 tumors expressing mainly the 4.5-kb mRNA form (Figure S1). Approximately 90% of tumors in the D1 or D1+D2 groups are hyperdiploid and have 3 or more trisomies that involve chromosomes 3, 5, 7, 9, 11, 15, 19, and 21 (Tables 1, 2; Figure 1). There is no predominant combination of trisomies but each of 6 chromosomes is trisomic in 80% to 90% of tumors, whereas chromosomes 7 and 21 are somewhat less often trisomic. Thus the reported association of trisomy 11 with CCND1 expression is not unique.17
Distinct gene expression profiles for the MM TC groups
We identified 576 genes that vary significantly between the 8 groups in the 261 MM tumors. A hierarchical cluster using these genes shows striking differential recurrent patterns of gene expression for many of the groups (Figure 4A). The pattern of gene expression associated with the different groups was particularly striking for the maf, 4p16, and D1 groups. Not surprisingly, a large number of genes are specifically overexpressed in the maf group, at least some of which are direct transcriptional targets of the MAF and MAFB transcription factors (Hurt et al,23 and C. Cultraro, unpublished data, November 2004). Surprisingly, a similarly large number of genes characterize the D1 group, a group that was identified solely by low expression of one gene (CCND1). Many of these genes are located on the 8 chromosomes frequently involved in trisomies. A slightly smaller number of genes characterize the 4p16 group. In contrast, most of the genes that characterize the 11q13 and 6p21 groups are shared (Figure 4B), and the gene expression pattern in these 2 groups clearly overlaps other groups. The D1+D2 group expressed a large number of genes characteristic of group D1. However this group failed to express an almost equal number of group D1 genes (eg, genes that are associated with an interferon response, such as TNFSF10, PRKR, MX1, MX2, STAT1, IF127, IRF7, IFNGR1). This group also appeared to express some genes characteristic of groups D2 and 4p16. These results suggest that apparently early genetic events (translocations and/or dysregulation of a cyclin D gene) may substantially determine the gene expression pattern despite subsequent similar progression events.
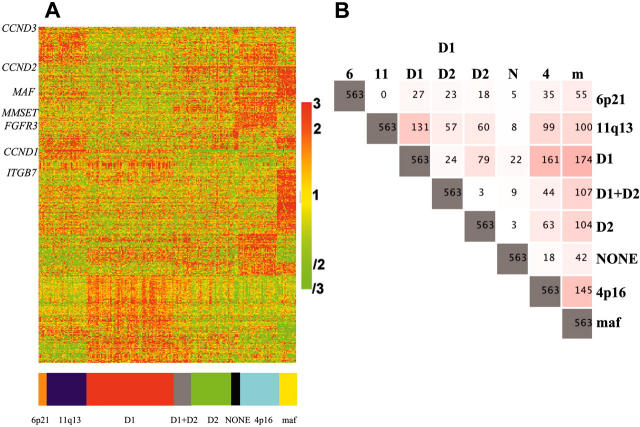
Figure 4.
Shared gene expression profiles for TC groups. (A) Two hundred thirty MM samples were categorized into the 8 TC groups. Five hundred seventy-six genes significantly different between the 8 subtypes (P < .05; Benjamin and Hochberg analysis was used to adjust for the multiple univariate hypothesis tests, with multiple testing correction) were identified. The genes were subjected to hierarchical clustering (Supplemental Worksheet, Table S2). A color code on the bottom identifies the color associated with each TC group. (B) Differences in gene expression between TC groups. A list of 576 genes that differs between the 8 TC groups with a P value less than .05 was generated, and the 13 probe sets corresponding to the genes used to assign the TC class (CCND1, CCND2, CCND3, FGFR3, MMSET, MAF, ITGB7, CX3CR1) were removed. The number of genes from this list that are statistically different (P < .05) in pair-wise comparisons between TC groups is shown, with the intensity of pink shading highlighting the more profound differences. 6 indicates 6p21; 11, 11q13; N, none; 4, 4p16; and M, maf.
Clinical correlates associated with TC groups
The most striking clinical feature of MM is lytic bone disease. We correlated the presence of lytic lesions detected on magnetic resonance imaging (MRI) in 172 untreated patients with the TC groups (Table 2).11 Whereas 79% of all patients had evidence of lytic disease, it was higher in the groups 11q13 (94%; P = .02), D1 (86%; P = .22), and D1+D2 (100%; P = .05) and significantly lower in the groups 4p16 (57%; P = .002) and maf (55%; P = .04). In individual pair-wise comparisons, each of the groups 11q13, D1, and D1+D2 had significantly (P < .05) more bone disease than each of the groups D2, 4p16, and maf.
We identified other phenotypic distinctions between the various groups. First, there is a substantial difference in the prevalence of an elevated expression PI, with a significantly low prevalence in the D1 group, a significantly increased prevalence in the maf group, and a markedly high prevalence in the D1+D2 group (Table 2). Consistent with this, the D1 group is underrepresented in the relapsed versus untreated patients (10% vs 34%; P < .01), whereas the D1+D2 group is overrepresented in the relapsed versus untreated patients (17% vs 6.5%; P = .01; Table 2). Second, the low frequency of bone disease in the maf and 4p16 groups is consistent with previous reports that these groups are overrepresented in primary plasma-cell leukemia (PCL) and in HMCLs that are derived from extramedullary tumors.5,21,24 Moreover, since hyperdiploidy associated with multiple trisomies was present in only 1 of 23 primary PCLs, it is apparent that the D1 group is underrepresented or absent both in PCL and HMCLs.5,24 Taken together these results imply a very different biology and interaction with the bone marrow microenvironment among these different genetic subgroups, with the D1 group being particularly dependent on these interactions.
Discussion
Biallelic dysregulation of CCND1 is frequent in MM but not other B-cell tumors
Cyclins D1, D2, or D3 positively interact with cyclin-dependent kinase 4 (cdk4) or cdk6 to regulate phosphorylation of retinoblastoma (RBI) thereby facilitating the G1/S cell-cycle transition.25,26 Cyclin D1 is expressed in most proliferating tissues, but there is little or no expression of CCND1 in lymphoid tissues or tumors that instead express CCND2 and/or CCND3.27,28 Exceptions include tumors with Ig translocations involving CCND1,29 hairy cell leukemias that express CCND1 without an apparent translocation,30 and a substantial fraction of MM tumors that express increased CCND1 in the absence of a t(11;14) translocation.5,17,31 We show here that nearly 40% of MM tumors biallelically express CCND1 mRNA. Therefore, a novel mechanism that biallelically dysregulates CCND1 is one of the most frequent oncogenic events in MM. Presumably, biallelic expression of CCND1 must be controlled by trans-acting factors, but analyses of the expression data have not identified obvious candidates.
Dysregulation of a cyclin D gene: a potential unifying event in pathogenesis of MM
Cyclin D is dysregulated in at least two thirds of MM tumors: IgH translocations directly dysregulate CCND1 or CCND3 in nearly 20% of tumors, or the MAF or MAFB transcription factors that target CCND2 in about 7% of tumors,23 and biallelic dysregulation of CCND1 occurs in approximately 40% of tumors. Most of the remaining tumors (4p16 and D2 groups) often express high levels of CCND2, suggesting that these tumors have dysregulated expression of CCND2 in the context of a very low proliferative index. Further support for the hypothesis that dysregulation of cyclin D is a unifying event in early pathogenesis is provided by a preliminary analysis of 12 MGUS tumors, which shows patterns of cyclin D expression that are similar to MM tumors despite an even lower ability to proliferate. The low proliferative capacity of MGUS or MM tumors that express a dysregulated cyclin D gene is consistent with the fact that a high level of expression of transgenic ccnd1 in murine B cells does not seem to perturb normal B-cell development and proliferation or lead to tumors, unless there is, for example, a cooperating myc or activated ras transgene.32,33
Two apparently different pathogenic pathways in MM
The karyotypic and gene expression data summarized here are in accord with the 2 pathways hypothesized for the early pathogenesis of MM (Figure 5). Several thoughts come to mind. First, multiple trisomies probably represent the critical feature and not hyperdiploidy per se. We cannot directly relate the multiple trisomies with biallelic expression of CCND1 since many MM tumors with multiple trisomies express CCND2 and not CCND1, whereas other tumors express low levels of CCND1 in the absence of multiple trisomies (eg, some in group 4p16). Second, the pathways partially overlap (eg, some group 4p16 tumors), which suggests that the 2 pathways sometimes can complement one another. Third, although both pathways seem to be implicated as very early events that are shared by MGUS and MM, the relative timing of IgH translocations, aneuploidy (including chromosome 13 monosomy), and cyclin D dysregulation is unclear. In fact, we presently have no mechanistic insight into the causes or consequences of numeric and structural chromosomal changes that collectively are nearly invariant in MGUS and MM. Finally, despite the perturbation of the Rb pathway by cyclin D dysregulation in virtually all MM tumors, additional components of this pathway (p18INK4c and Rb) apparently can be disrupted by late progression events that are associated with enhanced proliferation in some tumors.34-36
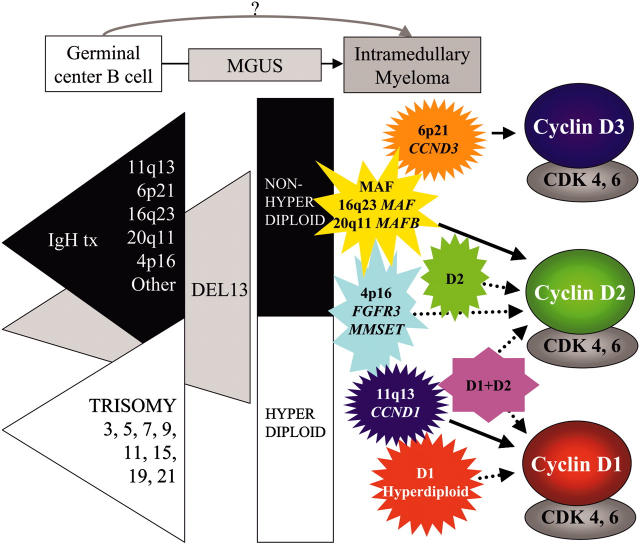
Figure 5.
Early oncogenic events in MM. The earliest oncogenic changes, which involve 3 overlapping pathways, probably occur in germinal center B cells and appear to be already present in premalignant MGUS tumors. Two partially overlapping pathways, indicated by IgH translocations (tx) and multiple trisomies, usually generate nonhyperdiploid and hyperdiploid tumors, respectively. A third pathway that leads to monosomy of chromosome 13 or deletion of 13q14 can be present in both types of tumors but occurs with a higher prevalence in nonhyperdiploid tumors, where it occurs in almost all tumors with t(4;14) and t(14;16) but infrequently in tumors with t(11;14). The essentially invariant dysregulation of a cyclin D gene appears to be associated with these early oncogenic changes. The identification of 5 recurrent IgH translocations and the dysregulated expression of a cyclin D gene by expression profiling forms the basis for assignment of MGUS and MM tumors into TC groups as depicted.
Assignment of MM tumors to TC groups
We have subdivided 231 untreated and 30 relapsed MM tumors into 7 groups (4p16, maf, 6p21, 11q13, D1, D1+D2, and D2) that have an increased expression of at least one cyclin D gene compared with normal BMPCs. An eighth none group includes 1% of MM “tumor” samples that have a polyclonal normal BMPC signature and another 1% of MM tumor samples that do not express increased levels of cyclin D1, D2, or D3 RNA. With the exception of the 4p16 group, each of the groups is characterized by the increased expression of CCND1 (11q13, D1, D1+D2 groups), CCND2 (maf, D1+D2, D2 groups), or CCND3 (6p21 group). In fact, even though we do not understand the mechanism(s) responsible, the 4p16 group invariably shows increased expression of CCND2. Although not unequivocally established, we think that the basis for assignment of tumors to the TC groups is focused primarily on very early if not initiating oncogenic events that are shared by MGUS and MM tumors, although the D1+D2 group might represent an exception.
Shared features of the D1, D1+D2, and D2 groups
The D1 and D1+D2 groups share several features, including a very high incidence of hyperdiploidy associated with specific trisomies and a shared gene expression signature. The D1+D2 group is different than the D1 group not only in the increased expression of CCND2 but also in the lack of increased expression of some genes that cluster with the D1 group and the increased expression of some genes that cluster with the D2 group (Figure 4). Excluding 5 D2 tumors that appear to be markedly contaminated with normal BMPCs (“Assignment of 261 MM tumors to 8 groups”), approximately 50% of the D2 group tumors are hyperdiploid and have the same specific trisomies. The expression patterns of the D2 tumors are not particularly distinctive but do overlap the D1+D2 tumors and, to a lesser extent, the 4p16 tumors (Figure 4). Thus the global expression phenotypes of tumors in the D2 and D1+D2 groups clearly seem to be more heterogeneous than tumors in the other groups. The paired comparison of the 8 groups (Figure 4B) suggests that the D1+D2 and D2 groups have fewer genes that distinguish them than either of these 2 groups compared with the D1 group. Finally, the D1+D2 group is strikingly different from the D1 and D2 groups since tumors in the former group more frequently have a higher PI and are more frequent at relapse than at diagnosis (Table 2). Clearly, much remains to be learned about the nature and genesis of these 3 groups.
Concluding thoughts
We think that the 8 TC groups are determined by very early if not initiating oncogenic events that result in dysregulation of 1 of the 3 cyclin D genes. Despite a variety of subsequent progression events, it seems remarkable that the ultimate tumor phenotype, as measured by global expression profiling, biology (bone disease, PI), and clinical course (relapse, progression to an extramedullary location), is significantly correlated with these groups. One might argue that some or all of these groups represent different albeit related diseases that may require different therapeutic approaches. In any case, it seems probable that a definitive molecular classification will require revision and refinement to reflect further insights as additional initiating and progression events are identified. Although it appears that the TC groups may be useful to classify tumors for therapeutic response and prognosis, it is important to recognize that there is unlikely to be a single classification system for this purpose. It seems more likely that the classification of MM tumors for prognosis will differ, depending on the availability and response to an ever-widening variety of therapeutic regimens. What will remain constant are the genetic lesions that give rise to MM and contribute to its progression. The TC groups that are based mainly on what appear to be early, perhaps initiating, pathogenic events that are shared by MGUS and MM should continue to provide a foundation for biologically and clinically relevant insights.
Supplementary Material
Acknowledgments
We wish to thank members of the Donna D. and Donald M. Lambert Laboratory of Myeloma Genetics for excellent technical assistance: Christopher Adams, Christopher Crane, Adam Hicks, Yongsheng Huang, Bob Kordsmeier, Steven McMorran, Christopher Randolph, Owen Stephens, Erming Tian, Yan Xaio, and Hongwei Xu. We also thank Myeloma Institute for Research and Therapy clinicians Elias Anaissie, Athanasios Fassas, Raymond Thertulien, Gianpaolo Talamo, Frits Van Rhee, Maurizio Zangari, and Guido Tricot.
Prepublished online as Blood First Edition Paper, March 8, 2005; DOI 10.1182/blood-2005-01-0034.
Supported in part by The Fund to Cure Myeloma (J.D.S.), National Institutes of Health (NIH) grants CA100707 (P.L.B.), CA55819 (B.B., J.D.S.), and CA97513 (J.D.S.), and the Leukemia and Lymphoma Society Specialized Center of Research (SCOR) in Myeloma (P.L.B.).
P.L.B. and W.M.K. contributed equally to this study.
The online version of the article contains a data supplement.
An Inside Blood analysis of this article appears at the front of the issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
- 1.Kuehl WM, Bergsagel PL. Multiple myeloma: evolving genetic events and host interactions. Nat Rev Cancer. 2002;2: 175-187. [DOI] [PubMed] [Google Scholar]
- 2.Fonseca R, Barlogie B, Bataille R, et al. Genetics and cytogenetics of multiple myeloma: a workshop report. Cancer Res. 2004;64: 1546-1558. [DOI] [PubMed] [Google Scholar]
- 3.Bergsagel PL, Kuehl WM. Chromosomal translocations in multiple myeloma. Oncogene. 2001;20: 5611-5622. [DOI] [PubMed] [Google Scholar]
- 4.Fonseca R, Debes-Marun CS, Picken EB, et al. The recurrent IgH translocations are highly associated with non-hyperdiploid variant multiple myeloma. Blood. 2003;102: 2562-2567. [DOI] [PubMed] [Google Scholar]
- 5.Bergsagel PL, Kuehl WM. Critical roles for immunoglobulin translocations and cyclin D dysregulation in multiple myeloma. Immunol Rev. 2003;194: 96-104. [DOI] [PubMed] [Google Scholar]
- 6.Gojo I, Zhang B, Fenton RG. The cyclin-dependent kinase inhibitor flavopiridol induces apoptosis in multiple myeloma cells through transcriptional repression and down-regulation of Mcl-1. Clin Cancer Res. 2002;8: 3527-3538. [PubMed] [Google Scholar]
- 7.Chesi M, Brents LA, Ely SA, et al. Activated fibroblast growth factor receptor 3 is an oncogene that contributes to tumor progression in multiple myeloma. Blood. 2001;97: 729-736. [DOI] [PubMed] [Google Scholar]
- 8.Otsuki T, Nakazawa N, Taniwaki M, et al. Establishment of a new human myeloma cell line, KMS-18, having t(4;14)(p16.3;q32.3) derived from a case phenotypically transformed from Ig A-lambda to BJP-lambda, and associated with hyperammonemia. Int J Oncol. 1998;12: 545-552. [DOI] [PubMed] [Google Scholar]
- 9.Hitzler JK, Martinez-Valdez H, Bergsagel DB, Minden MD, Messner HA. Role of interleukin-6 in the proliferation of human multiple myeloma cell lines OCI-My 1 to 7 established from patients with advanced stage of the disease. Blood. 1991;78: 1996-2004. [PubMed] [Google Scholar]
- 10.Zhang XG, Gaillard JP, Robillard N, et al. Reproducible obtaining of human myeloma cell lines as a model for tumor stem cell study in human multiple myeloma. Blood. 1994;83: 3654-3663. [PubMed] [Google Scholar]
- 11.Tian E, Zhan F, Walker R, et al. The role of the Wnt-signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N Engl J Med. 2003;349: 2483-2494. [DOI] [PubMed] [Google Scholar]
- 12.Zhan F, Hardin J, Kordsmeier B, et al. Global gene expression profiling of multiple myeloma, monoclonal gammopathy of undetermined significance, and normal bone marrow plasma cells. Blood. 2002;99: 1745-1757. [DOI] [PubMed] [Google Scholar]
- 13.Zhan F, Tian E, Bumm K, Smith R, Barlogie B, Shaughnessy J Jr. Gene expression profiling of human plasma cell differentiation and classification of multiple myeloma based on similarities to distinct stages of late-stage B-cell development. Blood. 2003;101: 1128-1140. [DOI] [PubMed] [Google Scholar]
- 14.Perou CM, Jeffrey SS, van de Rijn M, et al. Distinctive gene expression patterns in human mammary epithelial cells and breast cancers. Proc Natl Acad Sci U S A. 1999;96: 9212-9217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ciemerych MA, Kenney AM, Sicinska E, et al. Development of mice expressing a single D-type cyclin. Genes Dev. 2002;16: 3277-3289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tarte K, De Vos J, Thykjaer T, et al. Generation of polyclonal plasmablasts from peripheral blood B cells: a normal counterpart of malignant plasmablasts. Blood. 2002;100: 1113-1122. [PubMed] [Google Scholar]
- 17.Soverini S, Cavo M, Cellini C, et al. Cyclin D1 overexpression is a favorable prognostic variable for newly diagnosed multiple myeloma patients treated with high-dose chemotherapy and single or double autologous transplantation. Blood. 2003;102: 1588-1594. [DOI] [PubMed] [Google Scholar]
- 18.Specht K, Haralambieva E, Bink K, et al. Different mechanisms of cyclin D1 overexpression in multiple myeloma revealed by fluorescence in situ hybridization and quantitative analysis of mRNA levels. Blood. 2004;104: 1120-1126. [DOI] [PubMed] [Google Scholar]
- 19.Betticher DC, Thatcher N, Altermatt HJ, Hoban P, Ryder WD, Heighway J. Alternate splicing produces a novel cyclin D1 transcript. Oncogene. 1995;11: 1005-1011. [PubMed] [Google Scholar]
- 20.Yeoh EJ, Ross ME, Shurtleff SA, et al. Classification, subtype discovery, and prediction of outcome in pediatric acute lymphoblastic leukemia by gene expression profiling. Cancer Cell. 2002;1: 133-143. [DOI] [PubMed] [Google Scholar]
- 21.Avet-Loiseau H, Facon T, Grosbois B, et al. Oncogenesis of multiple myeloma: 14q32 and 13q chromosomal abnormalities are not randomly distributed, but correlate with natural history, immunological features, and clinical presentation. Blood. 2002;99: 2185-2191. [DOI] [PubMed] [Google Scholar]
- 22.Sawyer JR, Lukacs JL, Thomas EL, et al. Multicolour spectral karyotyping identifies new translocations and a recurring pathway for chromosome loss in multiple myeloma. Brit J Haematol. 2001;112: 167-174. [DOI] [PubMed] [Google Scholar]
- 23.Hurt EM, Wiestner A, Rosenwald A, et al. Overexpression of c-maf is a frequent oncogenic event in multiple myeloma that promotes proliferation and pathological interactions with bone marrow stroma. Cancer Cell. 2004;5: 191-199. [DOI] [PubMed] [Google Scholar]
- 24.Avet-Loiseau H, Daviet A, Brigaudeau C, et al. Cytogenetic, interphase, and multicolor fluorescence in situ hybridization analyses in primary plasma cell leukemia: a study of 40 patients at diagnosis, on behalf of the Intergroupe Francophone du Myelome and the Groupe Francais de Cytogenetique Hematologique. Blood. 2001;97: 822-825. [DOI] [PubMed] [Google Scholar]
- 25.Stacey DW. Cyclin D1 serves as a cell cycle regulatory switch in actively proliferating cells. Curr Opin Cell Biol. 2003;15: 158-163. [DOI] [PubMed] [Google Scholar]
- 26.Sherr CJ, McCormick F. The RB and p53 pathways in cancer. Cancer Cell. 2002;2: 103-112. [DOI] [PubMed] [Google Scholar]
- 27.Lam EW, Glassford J, Banerji L, Thomas NS, Sicinski P, Klaus GG. Cyclin D3 compensates for loss of cyclin D2 in mouse B-lymphocytes activated via the antigen receptor and CD40. J Biol Chem. 2000;275: 3479-3484. [DOI] [PubMed] [Google Scholar]
- 28.Sicinska E, Aifantis I, Le Cam L, et al. Requirement for cyclin D3 in lymphocyte development and T cell leukemias. Cancer Cell. 2003;4: 451-461. [DOI] [PubMed] [Google Scholar]
- 29.Rosenwald A, Wright G, Wiestner A, et al. The proliferation gene expression signature is a quantitative integrator of oncogenic events that predicts survival in mantle cell lymphoma. Cancer Cell. 2003;3: 185-197. [DOI] [PubMed] [Google Scholar]
- 30.Basso K, Liso A, Tiacci E, et al. Gene expression profiling of hairy cell leukemia reveals a phenotype related to memory B cells with altered expression of chemokine and adhesion receptors. J Exp Med. 2004;199: 59-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Specht K, Kremer M, Muller U, et al. Identification of cyclin D1 mRNA overexpression in B-cell neoplasias by real-time reverse transcription-PCR of microdissected paraffin sections. Clin Cancer Res. 2002;8: 2902-2911. [PubMed] [Google Scholar]
- 32.Lovec H, Grzeschiczek A, Kowalski MB, Moroy T. Cyclin D1/bcl-1 cooperates with myc genes in the generation of B-cell lymphoma in transgenic mice. EMBO J. 1994;13: 3487-3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bodrug SE, Warner BJ, Bath ML, Lindeman GJ, Harris AW, Adams JM. Cyclin D1 transgene impedes lymphocyte maturation and collaborates in lymphomagenesis with the myc gene. EMBO J. 1994;13: 2124-2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guillerm G, Gyan E, Wolowiec D, et al. p16(INK4a) and p15(INK4b) gene methylations in plasma cells from monoclonal gammopathy of undetermined significance. Blood. 2001;98: 244-246. [DOI] [PubMed] [Google Scholar]
- 35.Kulkarni MS, Daggett JL, Bender TP, Kuehl WM, Bergsagel PL, Williams ME. Frequent inactivation of the cyclin-dependent kinase inhibitor p18 by homozygous deletion in multiple myeloma cell lines: ectopic p18 expression inhibits growth and induces apoptosis. Leukemia. 2002;16: 127-134. [DOI] [PubMed] [Google Scholar]
- 36.Kramer A, Schultheis B, Bergmann J, et al. Alterations of the cyclin D1/pRb/p16(INK4A) pathway in multiple myeloma. Leukemia. 2002;16: 1844-1851. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.