Abstract
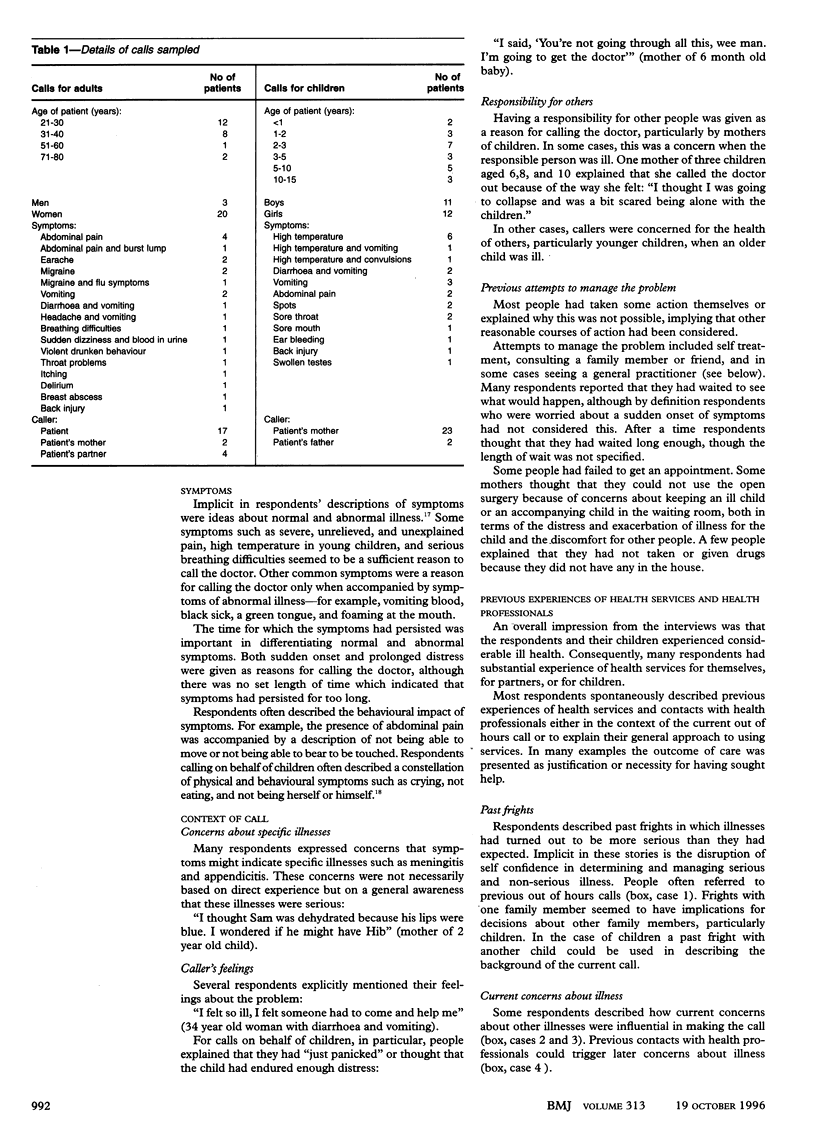
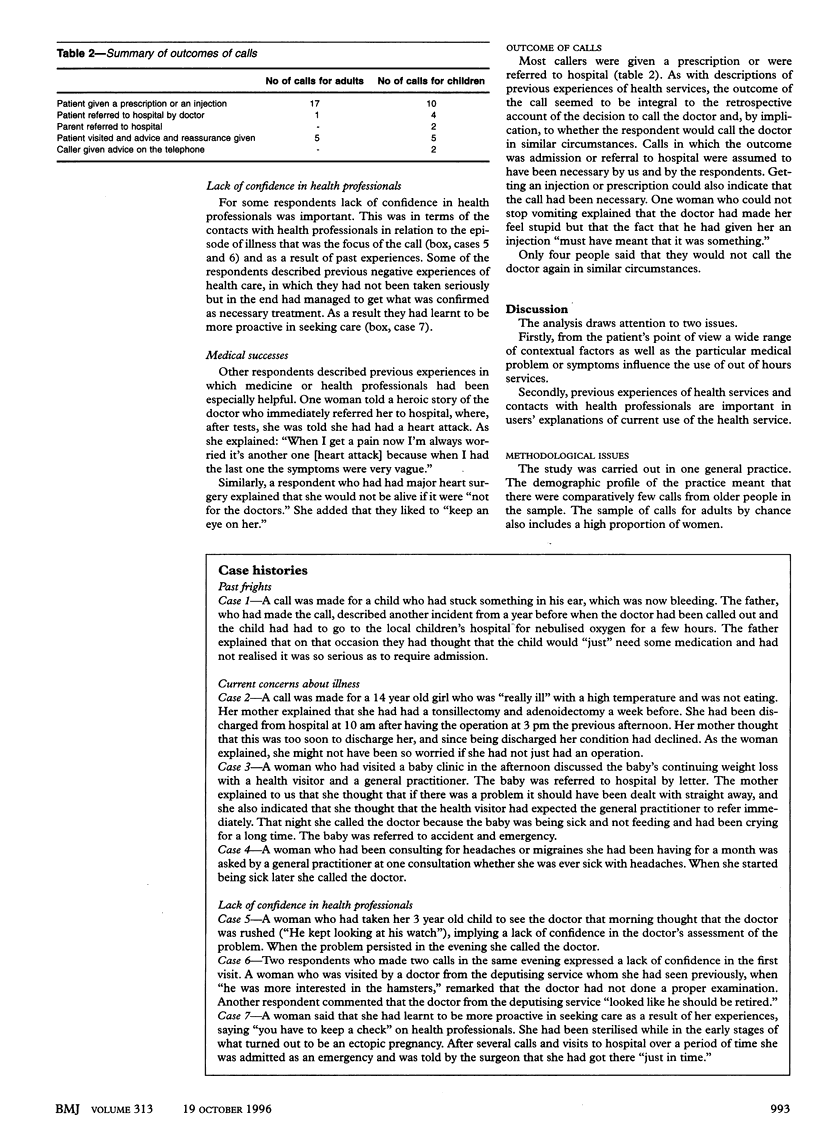
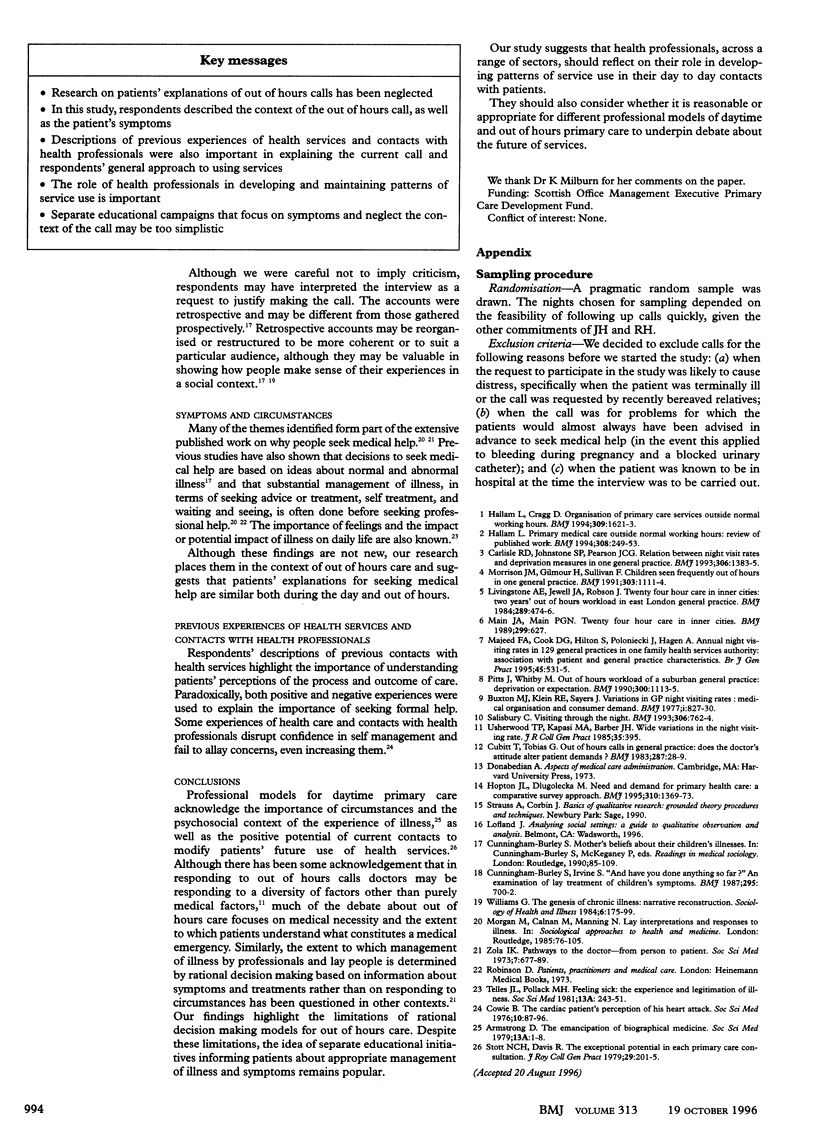
OBJECTIVE: To investigate patients' accounts of calling the doctor out of hours. DESIGN: Qualitative analysis of semi-structured interviews with two groups of patients who called their doctors out of hours from one general practice. SUBJECTS: 23 people who had called the doctor on their behalf or on behalf of another adult and 23 people who had called on behalf of a child between 6 pm and 8 am on a week day (omitting the weekend from 6 pm on Friday to 8 am on Monday). RESULTS: although respondents described symptoms as the main reason for the call, they also described a range of other factors that led to the call, including their feelings, concerns about specific illnesses, their responsibility for others, and their previous attempts to manage the problem themselves. They also described past experiences with health services that were important in explaining the current out of hours call or explaining their general approach to using services. CONCLUSIONS: The pursuit of a model of out of hours care based on medical necessity that neglects the psychosocial context of illness may not be appropriate. The importance of previous experiences of health services and contacts with health professionals in explaining current service use requires wider acknowledgement by health professionals across sectors. Separate educational programmes to encourage patients to use out of hours services more appropriately that neglect these issues may be too simplistic.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brumfitt W., Hamilton-Miller J. M., Gillespie W. A. The mysterious "urethral syndrome". BMJ. 1991 Jul 6;303(6793):1–2. doi: 10.1136/bmj.303.6793.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton M. J., Klein R. E., Sayers J. Variations in GP night visiting rates: medical organisation and consumer demand. Br Med J. 1977 Mar 26;1(6064):827–830. doi: 10.1136/bmj.1.6064.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlisle R. D., Johnstone S. P., Pearson J. C. Relation between night visit rates and deprivation measures in one general practice. BMJ. 1993 May 22;306(6889):1383–1385. doi: 10.1136/bmj.306.6889.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cubitt T., Tobias G. Out of hours calls in general practice: does the doctor's attitude alter patient demands? Br Med J (Clin Res Ed) 1983 Jul 2;287(6384):28–30. doi: 10.1136/bmj.287.6384.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham-Burley S., Irvine S. "And have you done anything so far?" An examination of lay treatment of children's symptoms. Br Med J (Clin Res Ed) 1987 Sep 19;295(6600):700–702. doi: 10.1136/bmj.295.6600.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallam L., Cragg D. Organisation of primary care services outside normal working hours. BMJ. 1994 Dec 17;309(6969):1621–1623. doi: 10.1136/bmj.309.6969.1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallam L. Primary medical care outside normal working hours: review of published work. BMJ. 1994 Jan 22;308(6923):249–253. doi: 10.1136/bmj.308.6923.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopton J. L., Dlugolecka M. Need and demand for primary health care: a comparative survey approach. BMJ. 1995 May 27;310(6991):1369–1373. doi: 10.1136/bmj.310.6991.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main J. A., Main P. G. Twenty four hour care in inner cities. BMJ. 1989 Sep 2;299(6699):627–627. doi: 10.1136/bmj.299.6699.627-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majeed F. A., Cook D. G., Hilton S., Poloniecki J., Hagen A. Annual night visiting rates in 129 general practices in one family health services authority: association with patient and general practice characteristics. Br J Gen Pract. 1995 Oct;45(399):531–535. [PMC free article] [PubMed] [Google Scholar]
- Pitts J., Whitby M. Out of hours workload of a suburban general practice: deprivation or expectation. BMJ. 1990 Apr 28;300(6732):1113–1115. doi: 10.1136/bmj.300.6732.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salisbury C. Visiting through the night. BMJ. 1993 Mar 20;306(6880):762–764. doi: 10.1136/bmj.306.6880.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheldon M. G., Harris S. J. Use of deputising services and night visit rates in general practice. Br Med J (Clin Res Ed) 1984 Aug 25;289(6443):474–476. doi: 10.1136/bmj.289.6443.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stott N. C., Davis R. H. The exceptional potential in each primary care consultation. J R Coll Gen Pract. 1979 Apr;29(201):201–205. [PMC free article] [PubMed] [Google Scholar]
- Telles J. L., Pollack M. H. Feeling sick: the experience and legitimation of illness. Soc Sci Med A. 1981 May;15(3 Pt 1):243–251. doi: 10.1016/0271-7123(81)90007-9. [DOI] [PubMed] [Google Scholar]
- Usherwood T. P., Kapasi M. A., Barber J. H. Wide variations in the night visiting rate. J R Coll Gen Pract. 1985 Aug;35(277):395–395. [PMC free article] [PubMed] [Google Scholar]
- Williams G. The genesis of chronic illness: narrative re-construction. Sociol Health Illn. 1984 Jul;6(2):175–200. doi: 10.1111/1467-9566.ep10778250. [DOI] [PubMed] [Google Scholar]
- Zola I. K. Pathways to the doctor-from person to patient. Soc Sci Med. 1973 Sep;7(9):677–689. doi: 10.1016/0037-7856(73)90002-4. [DOI] [PubMed] [Google Scholar]


