Abstract
The use of Bacillus anthracis as a biological weapon in 2001 heightened awareness of the need for validated methods for the inactivation of B. anthracis spores. This study determined the gamma irradiation dose for inactivating virulent B. anthracis spores in suspension and its effects on real-time PCR and antigen detection assays. Strains representing eight genetic groups of B. anthracis were exposed to gamma radiation, and it was found that subjecting spores at a concentration of 107 CFU/ml to a dose of 2.5 × 106 rads resulted in a 6-log-unit reduction of spore viability. TaqMan real-time PCR analysis of untreated versus irradiated Ames strain (K1694) spores showed that treatment significantly enhanced the detection of B. anthracis chromosomal DNA targets but had no significant effect on the ability to detect targets on the pXO1 and pXO2 plasmids of B. anthracis. When analyzed by an enzyme-linked immunosorbent assay (ELISA), irradiation affected the detection of B. anthracis spores in a direct ELISA but had no effect on the limit of detection in a sandwich ELISA. The results of this study showed that gamma irradiation-inactivated spores can be tested by real-time PCR or sandwich ELISA without decreasing the sensitivity of either type of assay. Furthermore, the results suggest that clinical and public health laboratories which test specimens for B. anthracis could potentially incorporate gamma irradiation into sample processing protocols without compromising the sensitivity of the B. anthracis assays.
Bacillus anthracis is a gram-positive, nonmotile, nonhemolytic, spore-forming bacterium closely related to two motile, hemolytic Bacillus species, B. cereus and B. thuringiensis (12). The virulence of B. anthracis is associated with the presence of two plasmids, pXO1 and pXO2, and strains lacking either plasmid are avirulent or exhibit attenuated virulence (27, 28, 39). The pXO1 plasmid (174 kbp) contains the lef, pagA, and cya genes, which encode the lethal factor, protective antigen, and edema factor proteins, respectively (4, 32, 34, 42). These proteins interact to produce the two anthrax toxins, lethal toxin and edema toxin. The pXO2 plasmid (95 kbp) contains the capA, capB, and capC genes, which are responsible for capsule biosynthesis (10, 26, 40). Although the presence of these plasmids is associated with virulence, their presence alone cannot be used to classify B. anthracis isolates. Early attempts at molecular characterization of B. anthracis strains showed a lack of diversity, but recently, variable-number tandem repeat analysis and the use of single-nucleotide polymorphism markers have been successfully used to genotype isolates (11, 20-22, 30, 41).
B. anthracis is the causative agent of anthrax, a serious disease of animals and humans. It is regarded as one of the most effective potential biological weapons because of the ability of its spores to persist in the environment for long periods of time as well as the potential for large-scale dissemination of spores (18, 35). Animals typically become infected by direct contact with soil containing spores. Infection in humans usually occurs via one of three routes of exposure to spores: cutaneous, gastrointestinal, and inhalational. Inhalational anthrax is associated with a high fatality rate. Intentional release of B. anthracis spores has the potential to result in mass casualties (35). Because of the potential use of B. anthracis as an agent of bioterrorism, several groups have developed and evaluated rapid diagnostic assays for the detection of B. anthracis in clinical and environmental samples (1, 3, 15, 33, 37).
Prior to 2001, human cases of inhalational anthrax in the United States were associated with occupational exposure or close contact with animals or contaminated animal products. However, in October 2001, the Ames strain of B. anthracis was used in the first confirmed bioterrorism-related outbreak of inhalational and cutaneous anthrax (14, 19). During the 2001 anthrax outbreak investigation, a joint effort between many agencies, including the Centers for Disease Control and Prevention and laboratories of the Laboratory Response Network (LRN) (23), the Department of Defense, and laboratories at the Naval Medical Research Center and U.S. Army Medical Research Institute of Infectious Diseases, Department of Energy, and the National Institutes of Health, resulted in the testing of large numbers of clinical and environmental specimens for B. anthracis (13, 15, 17, 24). This increased number of diagnostic specimens elevated the risk of exposure to B. anthracis spores for laboratory personnel and workers handling pre- and postremediation samples.
Many studies have revealed that irradiation is a powerful process for inactivating various types of microorganisms and that bacterial spores are generally the most resistant (36). A review of B. anthracis spore inactivation methods by Spotts Whitney et al. (38) listed gamma irradiation as a method for inactivating B. anthracis spores. Horne et al. (16) described the use of gamma radiation for inactivation of virulent B. anthracis spores and found that a dose of 1.5 × 106 rads was required to inactivate live spores at a concentration of 106 spores/ml. A more recent study conducted by Dang et al. (7) reported that 2.0 × 106 to 2.24 × 106 rads was sufficient to inactivate B. anthracis spores at a concentration of 108 CFU/ml, but the study used only avirulent strains missing one of the two virulence plasmids. In addition, the study (7) reported that irradiation decreased the sensitivity of real-time PCR and antigen detection by enzyme-linked immunosorbent assay (ELISA) with monoclonal antibodies (MAbs) and polyclonal antibodies (PAbs).
The purposes of this study were to determine the gamma radiation dose for inactivating virulent B. anthracis spores in suspension and to characterize the effects of gamma irradiation on the limit of detection for real-time PCR and antigen detection assays. Experiments were carried out using virulent strains representing eight genetic groups of B. anthracis, while testing employed a validated real-time PCR assay currently used by LRN laboratories (15) and three ELISAs.
MATERIALS AND METHODS
Biosafety procedures.
All procedures involving the use of live B. anthracis spores were performed in a biosafety level 3 laboratory. Culturing and manipulation of live spores were conducted in a class II type A2 biological safety cabinet (NuAire, Plymouth, MN). Additional biosafety level 3 precautions included the use of a powered air-purifying respirator and protective laboratory clothing.
Bacillus strains used in this study.
B. anthracis spore suspensions originated from stock preparations maintained in the Bioterrorism Rapid Response and Advanced Technology Laboratory, Division of Bioterrorism Preparedness and Response, Centers for Disease Control and Prevention. Eight B. anthracis strains were selected representing eight of the genetic groups first described by Keim et al. (22) (Table 1). Two additional control strains, B. cereus ATCC 14579 and B. thuringiensis ATCC 35646, were also used.
TABLE 1.
B. anthracis strains used in this studyb
| Strain IDa | Genotype | Genetic cluster and group |
|---|---|---|
| K1340 | 15 | A1.a |
| K9002 | 23 | A1.b |
| K5135 | 29 | A2 |
| K2484 | 38 | A3.a |
| K1694 (Ames) | 62 | A3.b |
| K4596 (Vollum) | 77 | A4 |
| K2762 | 80 | B2 |
| K2478 | 85 | B1 |
Strain identification (ID) assigned by the Special Pathogens Laboratory, Department of Pathobiological Sciences, Louisiana State University.
Data taken from Keim et al. (22).
Spore preparation.
Stock preparations of B. anthracis were streaked for isolation onto duplicate Trypticase soy agar plates containing 5% (vol/vol) sheep blood (TSAB) (BD Diagnostic Systems, Sparks, MD) and incubated for 24 h at 37°C. Isolated colonies were transferred to 5 ml of sterile phosphate-buffered saline (PBS) (0.1 M, pH 7.4) using sterile inoculating loops. Sporulation of B. anthracis was induced by growth on soil extraction agar (416.66 g of dried garden soil, 5.0 g of peptone, 3.0 g of beef extract, and 15.0 g of Bacto agar, all per liter) (6). Quadruplicate 200-μl aliquots of B. anthracis were spread onto soil extraction agar plates and incubated for 48 to 96 h at 37°C. The plates were monitored daily for spore formation by malachite green staining and light microscopy using a model VHX-600 digital light microscope (Keyence Corp., Woodcliff Lake, NJ), until ≥90% of the material observed was free spores. Cultures were harvested using sterile disposable spreaders and suspended into 5 ml sterile deionized water. Vegetative cells were removed by treatment with 50 mg/ml aqueous lysozyme (Sigma, St. Louis, MO) or by washing three times with cold, sterile deionized water (7). Harvested spore suspensions were viewed microscopically as described above to ensure that vegetative cells had been removed. To reduce clumping, spore suspensions were centrifuged at 10,000 × g for 15 min, resuspended in 2.5% (wt/vol) aqueous Pluronic F-68 (Sigma, St. Louis, MO), and vortexed for 2 min at high speed. Tenfold serial dilutions in PBS were performed, and triplicate 100-μl aliquots were spread onto TSAB plates. Colonies were enumerated after incubation for 24 h at 37°C. Spore suspensions were stored at 4°C.
Irradiation and viability testing.
B. anthracis spore suspensions were centrifuged at 10,000 × g for 15 min and resuspended in cold, sterile deionized water. Dilutions of spore suspensions ranging from 107 to 101 CFU/ml were subjected to irradiation. Duplicate 1-ml aliquots in 2-ml screw-cap polypropylene tubes (Fisher Scientific, Pittsburgh, PA) were gamma irradiated on ice at doses of 0.5 × 106, 1.0 × 106, 1.5 × 106, 2.0 × 106, 2.5 × 106, and 3.0 × 106 rads, corresponding to 18, 36, 54, 71, 90, and 107 min, respectively, in a GammaCell 220 Excel cobalt (60Co) irradiator (MDS Nordion, Ottawa, Ontario, Canada). For viability testing, a 100-μl aliquot of irradiated spores, plus a nonirradiated control aliquot for each strain, was spread onto TSAB plates, and plates were incubated for 48 h at 37°C. A separate 100-μl aliquot of each irradiated sample and nonirradiated control was also used to inoculate 3-ml Trypticase soy broth (BD Diagnostic Systems, Sparks, MD), and cultures were incubated for 48 h at 37°C with shaking at 300 rpm. Viability was determined by direct observation of plates for colonies and liquid cultures for turbidity. Staining and microscopy were performed as described above to compare untreated versus irradiated spores.
Irradiation kill curves were generated to determine the efficiency of inactivation for each treatment dose. Immediately following exposure to gamma radiation, spore suspensions were placed on ice, and serial tenfold dilutions were performed in PBS. Dilutions were spread onto triplicate TSAB plates, and the plates were incubated for 24 h at 37°C. Colonies were enumerated, and the percentage of survivors was calculated for each treatment dose.
Real-time PCR analysis.
The LRN real-time PCR reagents for B. anthracis (15) were used to determine the effects of gamma irradiation on nucleic acid detection. The PCR reagents consist of three primer/probe sets, BA1, BA2, and BA3, which target the pXO2 plasmid, pXO1 plasmid, and chromosome of B. anthracis, respectively, and were evaluated and validated previously (15). It has been demonstrated that B. anthracis DNA is present on the surfaces of spores (7); therefore, a known number of spores were added to the PCR mixtures. PCRs were carried out in triplicate 25-μl volumes. Each contained 1× PCR master mix (LightCycler FastStart DNA master hybridization probes [Roche Molecular Biochemicals, Indianapolis, IN]), 500 nΜ each PCR primer, 100 nM each TaqMan probe, 5 mM total MgCl2) and 10 μl of either spore suspensions, negative controls B. cereus and B. thuringiensis, or water in the case of the no-template controls. Real-time PCR was performed using the MiniOpticon real-time PCR detection system (Bio-Rad, Hercules, CA) with a thermocycling protocol of 10 min at 95°C, followed by 45 cycles, with 1 cycle consisting of 10 s at 95°C and 30 s at 60°C. Data collection and analysis were performed using the MJ OpticonMonitor analysis software version 3.1.
To determine the limit of detection for gamma-irradiated B. anthracis spores, a stock preparation of live strain K1694 (Ames) spores was diluted in cold, sterile, deionized water and adjusted to concentrations ranging from 107 to 101 CFU/ml. Each dilution was exposed to 2.5 × 106 rads of gamma radiation on ice as described above. Real-time PCR was performed in triplicate on untreated and gamma-irradiated spore dilutions and controls as described above, using the BA1, BA2, and BA3 primer/probe sets. To compare the detection levels of B. anthracis chromosomal DNA for each of the eight strains, spores at a concentration of 107 CFU/ml were exposed to gamma radiation on ice as described above. Real-time PCR was performed in triplicate on untreated and irradiated spores and controls using the BA3 primer/probe set as described above.
Preparation of spores for ELISA.
B. anthracis Ames strain and strain K4596 (Vollum) spore suspensions were adjusted to concentrations ranging from 107 to 101 CFU/ml in sterile deionized water and exposed to 2.5 × 106 rads of gamma radiation as described above. For a negative control for ELISA experiments, B. cereus spores were adjusted to a concentration of 107 CFU/ml in sterile deionized water and exposed to gamma radiation on ice as described above. Untreated and irradiated spores were then centrifuged at 10,000 × g for 15 min, resuspended in 1 ml PBS, and stored at 4°C.
Direct ELISA using a MAb.
A 100-μl volume of untreated and irradiated B. anthracis Ames strain, Vollum strain, and B. cereus spores at a concentration of 107 CFU/ml in PBS was added to each well (triplicate wells) on Immulon 2HB microtiter plates (Thermo, Milford, MA). The microtiter plates were incubated overnight at 4°C and then were washed once with wash buffer (PBS [pH 7.4], 0.1% Tween 20) using a model 1575 ImmunoWash microplate washer (Bio-Rad, Hercules, CA). Mouse anti-B. anthracis MAb (Naval Medical Research Center, Silver Spring, MD) was conjugated with horseradish peroxidase (HRP) using the E-Z Link maleimide-activated peroxidase kit (Pierce, Rockford, IL). The HRP-conjugated MAb was adjusted to a concentration of 5.0 μg/ml in dilution buffer (PBS [pH 7.4], 5% dry skim milk), and 100 μl was added to each well on microtiter plates. The plates were incubated for 1.5 h at 37°C and washed six times with wash buffer. For detection of the MAb, 100 μl of 3,3′,5,5′-tetramethylbenzidine (TMB) substrate (Sigma, St. Louis, MO) was added to each well. The plates were then incubated for 15 min at room temperature, and the reactions were stopped using an equal volume of 1 N hydrochloric acid. The plates were read at 450 nm using a model 680 microplate reader (Bio-Rad, Hercules, CA). The reactive cutoff for ELISA was defined as the mean absorbance for background wells plus three times the standard deviation.
Indirect ELISA using a PAb.
A 100-μl volume of untreated and irradiated B. anthracis Ames strain, Vollum strain, and B. cereus spores was added to each well (triplicate wells) at a concentration of 107 CFU/ml in PBS, and the plates were incubated overnight at 4°C. The plates were washed once as described above. Affinity-purified goat antianthrax PAb (Naval Medical Research Center, Silver Spring, MD) was adjusted to a concentration of 5.0 μg/ml in dilution buffer, and 100 μl was added to each well. The plates were incubated for 1.5 h at 37°C and then washed six times with wash buffer. A secondary HRP-conjugated anti-goat immunoglobulin G (Sigma, St. Louis, MO) was diluted 1:2,000 in dilution buffer, and 100 μl was added to each well. The plates were then incubated for 1.5 h at 37°C and washed six times with wash buffer. TMB substrate addition, plate reading, and cutoff calculations were carried out as described above.
Sandwich ELISA.
The sandwich format ELISA used the PAb employed in the indirect ELISA as a capture antibody and the MAb from the direct ELISA as a detection antibody. The PAb was diluted to a concentration of 5.0 μg/ml in PBS, 100 μl was added to each well on the microtiter plates, and the plates were incubated overnight at 4°C. The plates were washed once as described above, and 100 μl of untreated and irradiated B. anthracis Ames strain, Vollum strain, and B. cereus spores was added to each well (triplicate wells) at a concentration of 107 CFU/ml in PBS. The plates were incubated for 1.5 h at 37°C and washed six times with wash buffer. The HRP-conjugated MAb was used as the detection antibody at a concentration of 5.0 μg/ml in dilution buffer, 100 μl was added to each well, and the plates were incubated for 1.5 h at 37°C and washed six times with wash buffer. TMB substrate addition, plate reading, and cutoff calculations were carried out as described above.
Sandwich ELISA was also used to determine the limit of detection for untreated versus irradiated B. anthracis spores. The PAb was added to microtiter plate wells as described above, and the plates were incubated overnight at 4°C. The plates were then washed once with wash buffer, and 100 μl of untreated and irradiated B. anthracis Ames strain spores at concentrations ranging from 107 to 101 CFU/ml in PBS was added to each well (triplicate wells) on microtiter plates. Incubations, washes, TMB substrate addition, plate reading, and cutoff calculations were carried out as described above.
Statistical analysis.
To determine whether irradiation significantly affected the level of detection of B. anthracis spores by real-time PCR, the cross-threshold (cycle threshold) (CT) values for untreated versus irradiated spores were compared using a paired t test (two tailed). To determine whether irradiation significantly affected the level of detection of B. anthracis spores by ELISA, the absorbance at 450 nm minus the background was calculated, and the data for untreated versus irradiated spores were compared using a paired t test (two tailed).
RESULTS
Inactivation of live B. anthracis spores by gamma radiation.
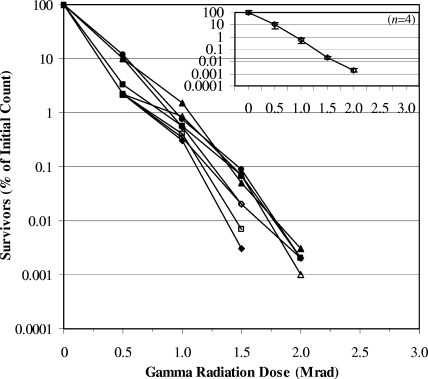
Microscopic observation of malachite green-stained spore preparations revealed no difference in spore morphology between those that were treated with lysozyme and those that were washed with sterile deionized water. Compared to nonirradiated spores, some gamma-irradiated spores appeared to be irregularly shaped. Culture of irradiated and nonirradiated spores revealed that 2.5 × 106 rads of gamma radiation resulted in a 6-log-unit reduction in viability, which was sufficient to completely inactivate live B. anthracis spores at a concentration of 107 CFU/ml (Fig. 1) when 0.1-ml aliquots were tested. Of the eight B. anthracis strains tested, K1340, K4596, and K2478 were the most sensitive to gamma radiation, as there was no growth observed 48 h following exposure to 2.0 × 106 rads. For the five strains that were more resistant to gamma radiation, K9002, K5135, K2484, K1694, and K2762, >99.9% were inactivated at this dose. For all strains tested, 1.5 × 106 rads of gamma radiation was sufficient to inactivate >99% of spores. Since 2.5 × 106 rads of gamma radiation was sufficient to inactivate 99.999% of the spores of all strains of B. anthracis tested, this treatment dose was used for all subsequent experiments in this study.
FIG. 1.
Gamma radiation inactivation curves for the spores of eight strains of B. anthracis. Spores of B. anthracis strains K1340 (♦), K9002 (▪), K5135 (▴), K2484 (•), K1694 (Ames) (⋄), K4596 (Vollum) (□), K2762 (▵), and K2478 (○) were exposed to six doses of gamma radiation, and the results were plotted as the percentage of survivors versus the gamma radiation dose. The inset depicts intrastrain variability in susceptibility to irradiation for one representative strain (K1694 [Ames]).
Real-time PCR analysis of untreated versus irradiated B. anthracis spores.
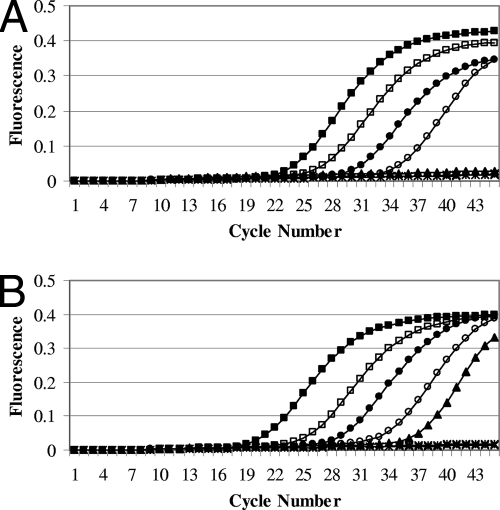
Untreated and gamma-irradiated B. anthracis Ames strain spores at concentrations ranging from 107 to 101 CFU/ml were assayed using the chromosome-specific primer/probe set, and the data were plotted as the mean relative fluorescence of triplicate wells versus the cycle number (Fig. 2). Irradiation resulted in a 1-log-unit increase in detection of B. anthracis chromosomal DNA by real-time PCR. The limit of detection for untreated Ames strain spores using the BA3 primer/probe set was 104 CFU/ml (100 CFU) (Fig. 2A), whereas the limit of detection for irradiated spores was 103 CFU/ml (10 CFU) (Fig. 2B).
FIG. 2.
Results of TaqMan real-time PCR analysis targeting the chromosome of B. anthracis. Serial tenfold dilutions of strain K1694 (Ames) spores were performed, and spores were exposed to 2.5 × 106 rads of gamma radiation. Untreated (A) and irradiated (B) spores at concentrations ranging from 107 to 101 CFU/ml (105 CFU [▪], 104 CFU [□], 103 CFU [•], 102 CFU [○], 10 CFU [▴], 1 CFU [*], and 0 CFU [x]) were detected by real-time PCR. The results were plotted as the average relative fluorescence of triplicate wells versus the cycle number.
Overall, irradiation increased the sensitivity of the assay to B. anthracis chromosomal DNA by real-time PCR. The data in Table 2 show the average CT values of triplicate wells for eight B. anthracis strains at a concentration of 107 CFU/ml using the BA3 primer/probe set. For each strain, irradiation resulted in a decrease of 2 or greater in CT values, and the difference in CT values for untreated versus irradiated spores was found to be significant (P = 0.001). The mean CT value for the untreated spores of all strains was 23.4 compared to 19.1 for irradiated spores. Neither one of the negative controls, B. cereus or B. thuringiensis, was detected at a concentration of 107 CFU/ml (data not shown).
TABLE 2.
Real-time PCR analysis of live versus gamma-irradiated B. anthracis spores using the BA3 chromosomal primer/probe set
| Strain IDa | Avg CT (mean ± SD)b
|
|
|---|---|---|
| Live spores | Irradiated spores | |
| K1340 | 21.1 ± 0.57 | 18.3 ± 0.53 |
| K9002 | 22.3 ± 0.22 | 18.9 ± 0.21 |
| K5135 | 24.9 ± 0.21 | 19.1 ± 0.31 |
| K2484 | 25.3 ± 0.33 | 19.4 ± 0.51 |
| K1694 (Ames) | 24.3 ± 0.54 | 19.9 ± 0.30 |
| K4596 (Vollum) | 25.5 ± 0.34 | 19.0 ± 0.30 |
| K2762 | 22.0 ± 0.57 | 18.7 ± 0.48 |
| K2478 | 21.6 ± 0.39 | 19.3 ± 0.27 |
ID, identification.
The differences in CT values for live (untreated) versus irradiated spores were found to be significant by paired t test (two tailed) (P = 0.001; n = 24).
In contrast, irradiation did not change the detection level for the pXO1 and pXO2 plasmids of B. anthracis by real-time PCR. Table 3 shows the average CT values for untreated versus irradiated Ames strain spores at concentrations ranging from 107 to 101 CFU/ml using the chromosome and pXO1 and pXO2 plasmids as targets. The difference in CT values for untreated versus irradiated spores was not significant for either plasmid target (Table 3). The average CT value for untreated spores at 107 CFU/ml using the pXO1-specific primer/probe set was 20.9 compared to 21.0 for irradiated spores. The limit of detection for the pXO1 plasmids of both untreated and irradiated spores was 104 CFU/ml (100 CFU), and the average CT values at this concentration were 32.7 and 32.8, respectively. Similarly, average CT values for untreated versus irradiated spores were comparable using the pXO2-specific primer/probe set. The limit of detection for the pXO2 plasmid was also 104 CFU/ml (100 CFU) for both untreated and irradiated spores. The average CT value for untreated spores at 107 CFU/ml was 21.7 compared to 21.9 for irradiated spores, and the average for untreated spores at the lower limit was 32.2 compared to 32.4 for irradiated spores. One or two out of three replicates at 103 CFU/ml (10 CFU) were positive for both plasmid targets of live and irradiated spores; however, average CT values were calculated only for those samples in which all three replicates produced a positive result. Neither one of the negative controls, B. cereus or B. thuringiensis, was detected using the BA1 and BA2 primer/probe sets (data not shown).
TABLE 3.
Real-time PCR analysis of live versus gamma-irradiated B. anthracis Ames strain spores using the chromosome and pXO1 and pXO2 plasmids as targets
| Concn (CFU/ml) | Avg CT (mean ± SD)a
|
|||||
|---|---|---|---|---|---|---|
| Chromosomeb
|
pXO1c
|
pXO2d
|
||||
| Live spores | Irradiated spores | Live spores | Irradiated spores | Live spores | Irradiated spores | |
| 107 | 23.3 ± 0.29 | 20.3 ± 0.17 | 20.9 ± 0.26 | 21.0 ± 0.18 | 21.7 ± 0.32 | 21.9 ± 0.16 |
| 106 | 26.6 ± 0.11 | 22.7 ± 0.16 | 23.0 ± 0.21 | 23.2 ± 0.27 | 24.8 ± 0.35 | 24.7 ± 0.31 |
| 105 | 29.4 ± 0.76 | 24.9 ± 0.27 | 26.5 ± 0.21 | 27.1 ± 0.33 | 27.3 ± 0.36 | 28.9 ± 0.81 |
| 104 | 36.0 ± 0.31 | 27.4 ± 0.24 | 32.7 ± 0.56 | 32.8 ± 0.76 | 32.2 ± 0.57 | 32.4 ± 0.52 |
| 103 | ND | 35.4 ± 0.34 | ++ | ++ | ++ | + |
Live versus gamma-irradiated B. anthracis Ames strain spores were analyzed by real-time PCR using the chromosome and pXO1 and pXO2 plasmids as targets. Mean CT values were determined only for those samples for which all three replicates produced a positive result. The CT values were not determined for 102 and 10 spore concentrations because none of the three replicates produced a positive result. Symbols: +, one out of three replicates produced a positive result; ++, two out of three replicates produced a positive result. ND, not detected.
Differences in the CT values for live (untreated) versus irradiated spores were found to be significant by paired t test (two tailed) (P < 0.05; n = 12).
Differences in the CT values for live (untreated) versus irradiated spores were not significant by paired t test (two tailed) (P = 0.09; n = 12).
Differences in the CT values for live (untreated) versus irradiated spores were not significant by paired t test (two tailed) (P = 0.34; n = 12).
Detection of untreated versus irradiated B. anthracis spores by ELISA.
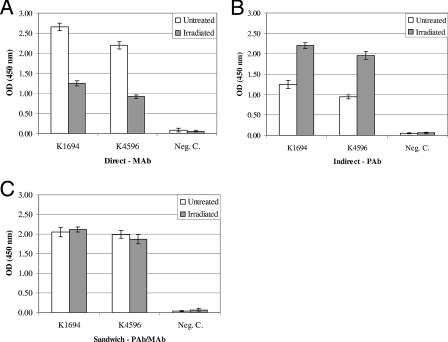
Irradiation of B. anthracis spores resulted in differential reactivity of the MAb and PAb by ELISA. Figure 3 shows the mean absorbance of triplicate wells for untreated versus irradiated B. anthracis spores by direct, indirect, and sandwich ELISAs. Irradiation decreased the detection level of Ames and Vollum strain spores by direct ELISA with the MAb (Fig. 3A). Compared to untreated spores, a 53% decrease in signal was observed for irradiated Ames strain spores and a 58.2% decrease in signal was observed for irradiated Vollum strain spores. The MAb did not detect B. cereus spores. In contrast, irradiation enhanced the detection level of B. anthracis Ames and Vollum strain spores by indirect ELISA with the PAb (Fig. 3B). Compared to untreated spores, a 76% increase in signal was observed for irradiated Ames strain spores and a 109% increase in signal was observed for irradiated Vollum strain spores. The PAb did not detect B. cereus spores. Irradiation had no effect on the detection level of B. anthracis spores when the PAb was used for capture and the MAb was used for detection (Fig. 3C). The sandwich ELISA did not detect B. cereus spores.
FIG. 3.
ELISA analysis of untreated versus gamma-irradiated B. anthracis spores. Untreated and irradiated B. anthracis strain K1694 (Ames) and K4596 (Vollum) spores and negative-control (Neg. C.) B. cereus spores at a concentration of 107 CFU/ml were detected by using mouse anti-B. anthracis MAb in a direct ELISA (A), goat anti-B. anthracis PAb by an indirect ELISA (B), and the PAb as the capture antibody and the MAb as the detection antibody by a sandwich ELISA (C). The results were plotted as the mean optical density (OD) or absorbance of triplicate wells at 450 nm minus the background ± standard error of the mean (error bars).
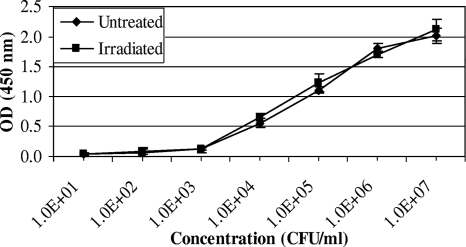
Sandwich ELISA was used to determine the limit of detection for untreated versus irradiated B. anthracis spores, since irradiation did not affect the level of detection in this format. Figure 4 shows the mean absorbance of triplicate wells for untreated versus irradiated Ames strain spores at concentrations ranging from 107 to 101 CFU/ml. Irradiation had no significant effect on the level of detection of B. anthracis spores (P = 0.56). At each concentration, the average ELISA signal for irradiated spores was comparable to that of the untreated spores, and the limit of detection for both untreated and irradiated B. anthracis spores was 104 CFU/ml (1,000 CFU).
FIG. 4.
Sandwich ELISA detection of untreated versus gamma-irradiated B. anthracis spores. Untreated and irradiated B. anthracis strain K1694 (Ames) spores at concentrations ranging from 101 to 107 CFU/ml were detected by sandwich ELISA using the PAb for capture and the MAb for detection. The results were plotted as the mean optical density (OD) or absorbance of triplicate wells at 450 nm minus the background ± standard error of the mean (error bars). The differences between untreated versus irradiated spores were not found to be significant using a paired t test (two tailed) (P = 0.56; n = 21).
DISCUSSION
This study is the first to report the gamma radiation dose for inactivating live virulent spores representing eight described genetic groups of B. anthracis (22). A dose of 2.5 × 106 rads inactivated spores at a concentration of 107 CFU/ml, though some strains were inactivated by 2.0 × 106 rads. It is important to emphasize that although the 2.5 × 106 rad dose killed 100% of spores in 0.1-ml aliquots testing viability, as used in this study, it is possible that larger sample volumes containing 107 CFU/ml spores may require longer periods of irradiation to achieve complete inactivation. Also, B. anthracis spores at concentrations greater than 107 CFU/ml may require a higher gamma radiation dose to kill 100% of spores.
Horne et al. (16) described differences in resistance to gamma irradiation among B. anthracis strains in a dry goat hair matrix to a range of radiation doses and reported an inactivation dose of 1.5 × 106 rads. There are several important differences in study procedures which may have contributed to the difference in reported inactivation doses. Horne et al. (16) used dried spore preparations, whereas this study used aqueous spore suspensions, which are the processed sample type most likely to be tested in clinical and diagnostic laboratories that test large numbers of specimens for B. anthracis (8). Additionally, Horne et al. (16) carried out irradiation dose experiments at room temperature, and studies have shown that the chamber equilibrium temperature will rise during the irradiation process when using a GammaCell 220 Excel cobalt (60Co) irradiator (K. P. J. O'Hara, MDS Nordion, personal communication). In this study, spore suspensions were kept on ice during exposure to minimize any possible contribution of heat to the inactivation process. Finally, the study (16) was conducted before the development of molecular subtyping methods that can distinguish B. anthracis isolates. This study used eight genetically distinct strains of B. anthracis, including virulent Ames strain spores in every experiment.
Dang et al. (7) used aqueous spore suspensions to evaluate spore inactivation methods but reported that a lower dose (60 min, 2.0 × 106 to 2.24 × 106 rads) was sufficient to kill 100% of spores at 108 CFU/ml (the study used a dose range of 2.5 × 106 to 2.8 × 106 rads as a safety measure). There are important differences in study design which may have contributed to the difference in reported inactivation doses. Dang et al. (7) used two avirulent strains of B. anthracis, whereas this study included eight virulent strains. The increased number of samples used in this study would be more likely to demonstrate differences in susceptibility to gamma irradiation.
Real-time PCR assays, which include targets for the plasmids of B. anthracis, allow for a high level of specificity and identify virulent strains (1, 9, 37). In this study, the chromosome was also targeted to provide results when testing plasmid-cured and avirulent strains of B. anthracis, as well as fully virulent strains. Additionally, the use of multiple targets decreases the rate of false-positive and false-negative results. All three targets of the assay used in this study have been used for the confirmatory identification of virulent strains of B. anthracis, and the assay was successfully used by LRN laboratories to test both clinical and environmental samples during the 2001 anthrax attack investigation (15). This study showed that irradiation increased the detection level of B. anthracis chromosomal DNA by real-time PCR (Fig. 2 and Table 2). A possible explanation for this effect is damage to B. anthracis spores during gamma irradiation, allowing increased access to target chromosomal DNA. This explanation is consistent with a study conducted by Phillips et al. (31), which reported that gamma irradiation resulted in structural damage of B. anthracis spores. In contrast, irradiation did not significantly affect detection of the pXO1 and pXO2 plasmids of B. anthracis by real-time PCR. These results conflict with those of a previous report that showed decreased detection of the pXO1 and pXO2 plasmids of irradiated spores (7). A possible explanation for the difference is that Dang et al. (7) used avirulent strains lacking one of the two virulence plasmids. It has been reported that virulence in B. anthracis is associated not only with the presence of the pXO1 and pXO2 plasmids but also to the copy number of the plasmid and that copy numbers may differ among virulent strains of B. anthracis (5). Therefore, it is plausible that avirulent strains used in the study (7) may differ in plasmid copy number from the fully virulent strains of B. anthracis used in this study, which may affect detection levels by real-time PCR and which further emphasizes the need for including a chromosomal target when testing specimens for B. anthracis. Another possible explanation for the difference is that Dang et al. (7) did not specify the temperature at which irradiation procedures were carried out, but one can presume that they were conducted at ambient temperature, which would not have excluded the possible effects of heat on DNA present on the outside of spores.
It has been reported that gamma irradiation of B. anthracis spores may affect epitopes recognized by MAbs and PAbs (7, 31). The results of this study are consistent with this observation, as the detection level of irradiated spores was decreased when the MAb was used and enhanced when the PAb was used. However, it is important to emphasize that the reactivity of antibodies to irradiated spores is very likely to depend upon how specific epitopes are affected by irradiation, particularly in the case of MAbs. Dang et al. (7) reported that spore inactivation methods can affect the sensitivity of antibody-based assays but did not evaluate the effects of irradiation on the sensitivity of sandwich ELISA. This study showed that irradiation of virulent spores affects the level of detection by direct and indirect ELISAs but does not significantly affect the sensitivity by sandwich ELISAs (Fig. 3 and 4). Sandwich ELISAs have been used for the detection of Bacillus spores in food and environmental samples and have been shown to be superior to direct ELISA when used with gamma-irradiated antigens of other microorganisms (2, 29). Additionally, the sandwich ELISA format has recently been used for the development of rapid multiplex detection of other pathogenic bacteria (25). Therefore, it is recommended that the sandwich ELISA format, as described in this study, be used for the detection of gamma-irradiated B. anthracis spores, though we acknowledge that assay performance is dependent on the specificity and quality of the antibodies used.
This study determined the gamma irradiation dose for inactivating live virulent spores (2.5 × 106 rads) and showed differences in resistance among B. anthracis strains. A 6-log-unit reduction of viable spores was observed for B. anthracis spores at a concentration of 107 CFU/ml, though higher concentrations will likely require higher doses of gamma radiation. The results showed that gamma irradiation may be used to inactivate live B. anthracis spores without significantly affecting the sensitivity of real-time PCR and sandwich ELISAs. This study proposes the use of gamma irradiation as a method to inactivate B. anthracis spores in specimens prior to testing. The mechanism by which gamma irradiation induces changes in the structural components of B. anthracis spores is a topic for future research.
Acknowledgments
We gratefully acknowledge Nancy McKinney for assistance with the preparation of B. anthracis spore stocks. Many people at CDC have contributed to this study. We acknowledge J. Todd Parker and William Morrill for the evaluation of B. anthracis antibodies used in this study. We thank John Hart for the conjugation of antibodies used in this study. We thank Stephen Morse, Harvey Holmes, Alex Hoffmaster, Robin Broeker, Eduardo Gomez-Saladin, John Kools, and Heather Stang for their critical review of the manuscript. We acknowledge Charles Rose for assistance with statistical analysis and Justin Schrager and Benjamin Moser for assistance with data compilation and literature searches.
B. anthracis is a select agent, and its possession, use, and transfer are regulated by the U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, and the U.S. Department of Agriculture, Animal and Plant Health Inspection Service. The select agent regulations have mandatory reporting requirements for identification of select agents in diagnostic specimens.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the funding agency.
Footnotes
Published ahead of print on 30 May 2008.
REFERENCES
- 1.Bell, C. A., J. R. Uhl, T. L. Hadfield, J. C. David, R. F. Meyer, T. F. Smith, and F. R. Cockerill III. 2002. Detection of Bacillus anthracis DNA by LightCycler PCR. J. Clin. Microbiol. 40:2897-2902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blake, M. R., and B. C. Weimer. 1997. Immunomagnetic detection of Bacillus stearothermophilus spores in food and environmental samples. Appl. Environ. Microbiol. 63:1643-1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bode, E., W. Hurtle, and D. Norwood. 2004. Real-time PCR assay for a unique chromosomal sequence of Bacillus anthracis. J. Clin. Microbiol. 42:5825-5831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bragg, T. S., and D. L. Robertson. 1989. Nucleotide sequence and analysis of the lethal factor gene (lef) from Bacillus anthracis. Gene 81:45-54. [DOI] [PubMed] [Google Scholar]
- 5.Coker, P. R., K. L. Smith, P. F. Fellows, G. Rybachuck, K. G. Kousoulas, and M. E. Hugh-Jones. 2003. Bacillus anthracis virulence in guinea pigs vaccinated with anthrax vaccine adsorbed is linked to plasmid quantities and clonality. J. Clin. Microbiol. 41:1212-1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cowan, S. T., and K. K. Steel. 1974. Cowen & Steele's manual for the identification of medical bacteria, 2nd ed. Cambridge University Press, London, United Kingdom.
- 7.Dang, J. L., K. Heroux, J. Kearney, A. Arasteh, M. Gostomski, and P. A. Emanuel. 2001. Bacillus spore inactivation methods affect detection assays. Appl. Environ. Microbiol. 67:3665-3670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drago, L., A. Lombardi, E. D. Vecchi, and M. R. Gismondo. 2002. Real-time PCR assay for rapid detection of Bacillus anthracis spores in clinical samples. J. Clin. Microbiol. 40:4399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ellerbrok, H., H. Nattermann, M. Ozel, L. Beutin, B. Appel, and G. Pauli. 2002. Rapid and sensitive identification of pathogenic and apathogenic Bacillus anthracis by real-time PCR. FEMS Microbiol. Lett. 214:51-59. [DOI] [PubMed] [Google Scholar]
- 10.Green, B., L. Battisti, T. Koehler, C. Thorne, and B. Ivins. 1985. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 49:291-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrell, L. J., G. L. Andersen, and K. H. Wilson. 1995. Genetic variability of Bacillus anthracis and related species. J. Clin. Microbiol. 33:1847-1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Helgason, E., O. A. Okstad, D. A. Caugant, H. A. Johansen, A. Fouet, M. Mock, I. Hegna, and A.-B. Kolsto. 2000. Bacillus anthracis, Bacillus cereus, and Bacillus thuringiensis—one species on the basis of genetic evidence. Appl. Environ. Microbiol. 66:2627-2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heller, M. B., M. L. Bunning, M. E. France, D. M. Niemeyer, L. Peruski, T. Naimi, P. M. Talboy, P. H. Murray, H. W. Pietz, J. Kornblum, W. Oleszko, S. T. Beatrice, Joint Microbiological Rapid Response Team, and New York City Anthrax Investigation Working Group. 2002. Laboratory response to anthrax bioterrorism, New York City, 2001. Emerg. Infect. Dis. 8:1096-1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmaster, A. R., C. C. Fitzgerald, E. Ribot, L. W. Mayer, and T. Popovic. 2002. Molecular subtyping of Bacillus anthracis and the 2001 bioterrorism-associated anthrax outbreak, United States. Emerg. Infect. Dis. 8:1111-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoffmaster, A. R., R. F. Meyer, M. D. Bowen, C. K. Marston, R. S. Weyant, K. Thurman, S. L. Messenger, E. E. Minor, J. M. Winchell, M. V. Rassmussen, B. R. Newton, J. T. Parker, W. E. Morrill, N. McKinney, G. A. Barnett, J. J. Sejvar, J. A. Jernigan, B. A. Perkins, and T. Popovic. 2002. Evaluation and validation of a real-time polymerase chain reaction assay for rapid identification of Bacillus anthracis. Emerg. Infect. Dis. 8:1178-1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horne, T., G. Turner, and A. Willis. 1959. Inactivation of Bacillus anthracis by G-radiation. Nature 4659:475-476. [DOI] [PubMed] [Google Scholar]
- 17.Hsu, V. P., S. L. Lukacs, T. Handzel, J. Hayslett, S. Harper, T. Hales, V. A. Semenova, S. Romero-Steiner, C. Elie, C. P. Quinn, R. Khabbaz, A. S. Khan, G. Martin, J. Eisold, A. Schuchat, and R. A. Hajjeh. 2002. Opening a Bacillus anthracis-containing envelope, Capitol Hill, Washington, D.C.: the public health response. Emerg. Infect. Dis. 8:1039-1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Inglesby, T. V., D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. M. Friedlander, J. Hauer, J. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat for the Working Group on Civilian Biodefense. 1999. Anthrax as a biological weapon: medical and public health management. JAMA 281:1735-1745. [DOI] [PubMed] [Google Scholar]
- 19.Jernigan, J. A., D. S. Stephens, D. A. Ashford, C. Omenaca, M. S. Topiel, M. Galbraith, M. Tapper, T. L. Fisk, S. Zaki, T. Popovic, R. F. Meyer, C. P. Quinn, S. A. Harper, S. K. Fridkin, J. J. Sejvar, C. W. Shepard, M. McConnell, J. Guarner, W. J. Shieh, J. M. Malecki, J. L. Gerberding, J. M. Hughes, B. A. Perkins, and members of the Anthrax Bioterrorism Investigation Team. 2001. Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Emerg. Infect. Dis. 7:933-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keim, P., A. Kalif, J. Schupp, K. Hill, S. E. Travis, K. Richmond, D. M. Adair, M. Hugh-Jones, C. R. Kuske, and P. Jackson. 1997. Molecular evolution and diversity in Bacillus anthracis as detected by amplified fragment length polymorphism markers. J. Bacteriol. 179:818-824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keim, P., A. M. Klevytska, L. B. Price, J. M. Schupp, G. Zinser, K. L. Smith, M. E. Hugh-Jones, R. Okinaka, K. K. Hill, and P. J. Jackson. 1999. Molecular diversity in Bacillus anthracis. J. Appl. Microbiol. 87:215-217. [DOI] [PubMed] [Google Scholar]
- 22.Keim, P., L. B. Price, A. M. Klevytska, K. L. Smith, J. M. Schupp, R. Okinaka, P. J. Jackson, and M. E. Hugh-Jones. 2000. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 182:2928-2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khan, A. S., S. Morse, and S. Lillibridge. 2000. Public-health preparedness for biological terrorism in the USA. Lancet 356:1179-1182. [DOI] [PubMed] [Google Scholar]
- 24.Kiratisin, P., C. D. Fukuda, A. Wong, F. Stock, J. C. Preuss, L. Ediger, T. N. Brahmbhatt, S. H. Fischer, D. P. Fedorko, F. G. Witebsky, and V. J. Gill. 2002. Large-scale screening of nasal swabs for Bacillus anthracis: descriptive summary and discussion of the National Institutes of Health's experience. J. Clin. Microbiol. 40:3012-3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Magliulo, M., P. Simoni, M. Guardigli, E. Michelini, M. Luciani, R. Lelli, and A. Roda. 2007. A rapid multiplexed chemiluminescent immunoassay for the detection of Escherichia coli O157:H7, Yersinia enterocolitica, Salmonella typhimurium, and Listeria monocytogenes pathogen bacteria. J. Agric. Food Chem. 55:4933-4939. [DOI] [PubMed] [Google Scholar]
- 26.Makino, S., I. Uchida, N. Terakado, C. Sasakawa, and M. Yoshikawa. 1989. Molecular characterization and protein analysis of the cap region, which is essential for encapsulation in Bacillus anthracis. J. Bacteriol. 171:722-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mikesell, P., B. E. Ivins, J. D. Ristroph, and T. M. Dreier. 1983. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect. Immun. 39:371-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Okinaka, R. T., K. Cloud, O. Hampton, A. R. Hoffmaster, K. K. Hill, P. Keim, T. M. Koehler, G. Lamke, S. Kumano, J. Mahillon, D. Manter, Y. Martinez, D. Ricke, R. Svensson, and P. J. Jackson. 1999. Sequence and organization of pXO1, the large Bacillus anthracis plasmid harboring the anthrax toxin genes. J. Bacteriol. 181:6509-6515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paweska, J. T., F. J. Burt, and R. Swanepoel. 2005. Validation of IgG-sandwich and IgM-capture ELISA for the detection of antibody to Rift Valley fever virus in humans. J. Virol. Methods 124:173-181. [DOI] [PubMed] [Google Scholar]
- 30.Pearson, T., J. D. Busch, J. Ravel, T. D. Read, S. D. Rhoton, J. M. U'Ren, T. S. Simonson, S. M. Kachur, R. R. Leadem, M. L. Cardon, M. N. Van Ert, L. Y. Huynh, C. M. Fraser, and P. Keim. 2004. Phylogenetic discovery bias in Bacillus anthracis using single-nucleotide polymorphisms from whole-genome sequencing. Proc. Natl. Acad. Sci. USA 101:13536-13541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Phillips, A. P., A. M. Campbell, and R. Quinn. 1988. Monoclonal antibodies against spore antigens of Bacillus anthracis. FEMS Microbiol. Immunol. 1:169-178. [DOI] [PubMed] [Google Scholar]
- 32.Price, L. B., M. Hugh-Jones, P. J. Jackson, and P. Keim. 1999. Genetic diversity in the protective antigen gene of Bacillus anthracis. J. Bacteriol. 181:2358-2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qi, Y., G. Patra, X. Liang, L. E. Williams, S. Rose, R. J. Redkar, and V. G. DelVecchio. 2001. Utilization of the rpoB gene as a specific chromosomal marker for real-time PCR detection of Bacillus anthracis. Appl. Environ. Microbiol. 67:3720-3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robertson, D. L., M. T. Tippetts, and S. H. Leppla. 1988. Nucleotide sequence of the Bacillus anthracis edema factor gene (cya): a calmodulin-dependent adenylate cyclase. Gene 73:363-371. [DOI] [PubMed] [Google Scholar]
- 35.Rotz, L. D., A. S. Khan, S. R. Lillibridge, S. M. Ostroff, and J. M. Hughes. 2002. Public health assessment of potential biological terrorism agents. Emerg. Infect. Dis. 8:225-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Russell, A. D., W. B. Hugo, and G. A. J. Ayliffe. 1999. Principles and practice of disinfection, preservation and sterilization, 3rd ed. Blackwell Science, Inc., Malden, MA.
- 37.Ryu, C., K. Lee, C. Yoo, W. K. Seong, and H. B. Oh. 2003. Sensitive and rapid quantitative detection of anthrax spores isolated from soil samples by real-time PCR. Microbiol. Immunol. 47:693-699. [DOI] [PubMed] [Google Scholar]
- 38.Spotts Whitney, E. A., M. E. Beatty, T. H. Taylor, Jr., R. Weyant, J. Sobel, M. J. Arduino, and D. A. Ashford. 2003. Inactivation of Bacillus anthracis spores. Emerg. Infect. Dis. 9:623-627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Uchida, I., K. Hashimoto, and N. Terakado. 1986. Virulence and immunogenicity in experimental animals of Bacillus anthracis strains harbouring or lacking 110 MDa and 60 MDa plasmids. J. Gen. Microbiol. 132:557-559. [DOI] [PubMed] [Google Scholar]
- 40.Uchida, I., T. Sekizaki, K. Hashimoto, and N. Terakado. 1985. Association of the encapsulation of Bacillus anthracis with a 60 megadalton plasmid. J. Gen. Microbiol. 131:363-367. [DOI] [PubMed] [Google Scholar]
- 41.Van Ert, M. N., W. R. Easterday, L. Y. Huynh, R. T. Okinaka, M. E. Hugh-Jones, J. Ravel, S. R. Zanecki, T. Pearson, T. S. Simonson, J. M. U'Ren, S. M. Kachur, R. R. Leadem-Dougherty, S. D. Rhoton, G. Zinser, J. Farlow, P. R. Coker, K. L. Smith, B. Wang, L. J. Kenefic, C. M. Fraser-Liggett, D. M. Wagner, and P. Keim. 2007. Global genetic population structure of Bacillus anthracis. PLoS One 2:e461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Welkos, S. L., J. R. Lowe, F. Eden-McCutchan, M. Vodkin, S. H. Leppla, and J. J. Schmidt. 1988. Sequence and analysis of the DNA encoding protective antigen of Bacillus anthracis. Gene 69:287-300. [DOI] [PubMed] [Google Scholar]