Abstract
Background
We determined the rate of incarceration of inguinal hernia among infants and young children waiting for elective surgery and examined the relation to wait times. We also explored the relation between wait times and the use of emergency department services before surgery.
Methods
We used linked data from administrative databases to identify infants and children less than 2 years of age who underwent surgical repair of an inguinal hernia between Apr. 1, 2002, and Mr. 31, 2004. We determined the rate of hernia incarceration during the wait for surgery and stratified the risk by patient age and sex. We used logistic regression analysis to examine factors associated with hernia incarceration and wait times.
Results
A total of 1065 infants and children less than 2 years old underwent surgical repair of an inguinal hernia during the study period. The median wait time was 35 days (interquartile range 17–77 days). Within 30 days after diagnosis, 126 (11.8%) of the patients had at least 1 emergency department visit; 23.8% of them presented with hernia incarceration. The overall rate of hernia incarceration was 11.9%. The rate was 5.2% with a wait time of up to 14 days (median time from diagnosis to first emergency department visit), as compared with 10.1% with a wait time of up to 35 days (median wait time to surgery) (p < 0.001). Factors associated with an increased risk of incarcerated hernia were age less than 1 year (odds ratio [OR] 2.07, 95% confidence interval [CI] 1.32–3.23), female sex (OR 1.75, 95% CI 1.04–2.93) and emergency department visits (1 visit, OR 2.73, 95% 1.65–4.50; ≥ 2 visits, OR 3.77, 95% CI 1.89–7.43). Children less than 1 year old who waited longer than 14 days had a significant 2-fold risk of incarcerated hernia (OR 1.92, 95% CI 1.11–3.32).
Interpretation
A wait time for surgery of more than 14 days was associated with a doubling of the risk of hernia incarceration among infants and young children with inguinal hernia. Our data support a recommendation that inguinal hernias in this patient population be repaired within 14 days after diagnosis.
Inguinal hernias in infants and young children are a result of a failure of the processus vaginalis to close.1 Once diagnosed, an inguinal hernia should be promptly repaired on an elective basis to prevent the risk of hernia incarceration. Incarceration occurs in about 12% of infants and young children with an inguinal hernia. The incidence is highest (approaching 30%) among infants (< 1 year old).2 Boys who experience incarceration of an inguinal hernia have a 30% risk of testicular atrophy that may affect future fertility.3
Many countries are struggling with long wait times for elective surgical procedures.4–6 To date, research has been skewed toward examining wait times for surgery and other medical or diagnostic care in adults.7–10 Prolonged wait times for surgery to repair hernias have not been associated with adverse outcomes in adults,11 but the effect of prolonged wait times in children has not been well studied.1,12
We conducted this study to examine the relation between wait times for elective surgery and the risk of incarceration of inguinal hernia in infants and young children. We also explored the relation between wait times and the use of emergency department services before surgery.
Methods
Study population and data sources
We used the Ontario Discharge Abstract Database to identify infants and young children who were waiting for surgery to repair an inguinal hernia. This database is maintained by the Canadian Institute for Health Information and contains data on all hospital admissions in Ontario.
We included infants and children less than 2 years of age who had a diagnosis of inguinal hernia (International Classification of Diseases [ICD], 9th revision, code 550 or ICD, 10th revision, code K40) and a surgical procedure code for hernia repair (ICD, clinical modification, codes 53.0 to 53.9) between Apr. 1, 2002, and Mar. 31, 2004. We included only patients whose inguinal hernia was diagnosed through a physician's office. We linked the data for these children to claims data from the Ontario Health Insurance Plan database for fiscal years 2001 to 2003 to determine the date of first clinic or office visit when the hernia was diagnosed. We chose this timeframe assuming that any infant with a diagnosis of inguinal hernia during this period who was otherwise healthy would undergo surgical repair within a maximum of 2 years.
Since the Ontario Discharge Abstract Database did not allow for complete capturing of patients presenting for the first time to an emergency department, we focused on estimating the wait time from diagnosis to elective hernia repair. We excluded 4 patients who presented with a hernia that was associated with intestinal gangrene (ICD-9 code 550.0 or ICD-10 codes K40.1 and K40.4) and 20 boys with undescended testes (ICD-9 code 752.2 or ICD-10 code Q53), since these diagnoses could have an impact on the choice for timing of surgical repair. For instance, in children with a hernia associated with undescended testes, the operation is delayed to allow for a technically successful orchedopexy. The inclusion of such a child in our study cohort could confound the association of prolonged time with the examined outcomes. These exclusion criteria were decided in advance.
Definition of wait time
We defined wait time as the number of days from the clinic or office visit where the diagnosis was made to the date of the surgical repair. If a patient had more than one physician billing for a clinic visit for inguinal hernia, we used the first visit to calculate wait time.
Outcome measures
The primary outcome measure was the rate of hernia incarceration from the time of diagnosis to surgery. We examined the relation between wait times and the rate of incarceration. We also explored the relation between wait times and use of emergency department services. We used the National Ambulatory Care Reporting System to capture patients' visits to the emergency department during the wait for surgery. This national administrative database records all visits to emergency departments in Canada and the clinical reason for the visit.
Statistical analysis
We first calculated the Pearson correlation coefficient to indicate the association of hernia incarceration and wait time. We then used the life-table method to calculate the risk of incarceration by wait time while adjusting for the number of visits to the emergency department during the wait. We stratified the risk of hernia incarceration by patient age (< 1 year v. 1–2 years) and sex. We also used multivariable logistic regression models to estimate the effects of different covariates (age, sex, visits to the emergency department) influencing the risk of hernia incarceration.
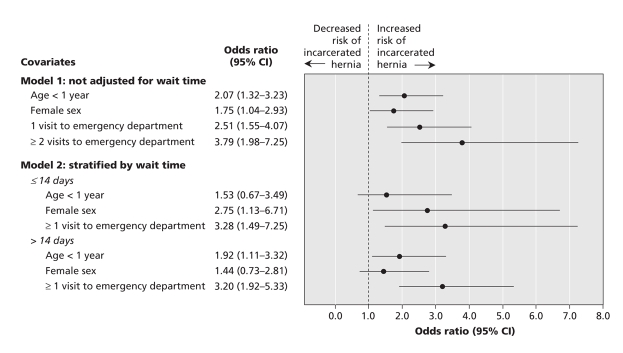
We further stratified the logistic regression models by wait time for surgery. We compared wait times of 14 days or less with those of more than 14 days (the current median time from diagnosis to emergency department visit). In the stratified logistic regression models, we dichotomized the number of visits to the emergency department (≥ 1 visit v. none). Finally, we compared the adjusted odds ratios by various logistic models in a forest plot.
The study design was approved by the Hospital for Sick Children Research Ethics Board.
Results
During fiscal years 2002 and 2003, a total of 1065 infants and children less than 2 years of age underwent surgery to repair an inguinal hernia in Ontario. The majority of the patients (943 [88.5%]) were boys (Table 1).
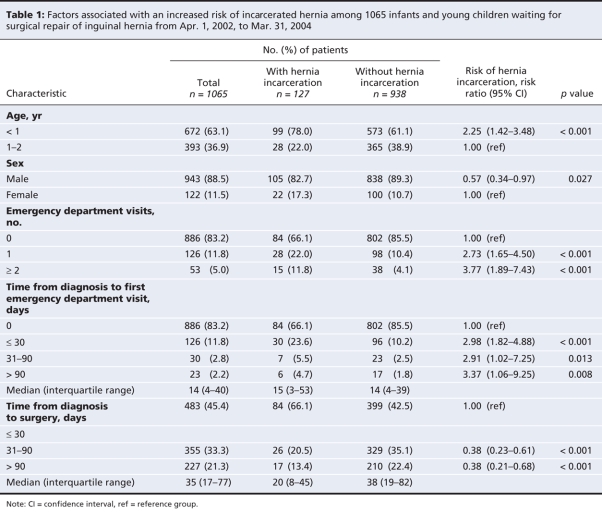
Table 1
The median wait time from diagnosis to surgery was 35 days (interquartile range 17–77 days). The overall rate of hernia incarceration was 11.9%. Longer wait times were associated with an increased rate of hernia incarceration. The rate was 5.2% with a wait time of 14 days or less (median time from diagnosis to first visit to emergency department), as compared with 10.0% with a wait time of 35 days or less (current median wait time for surgery) (p < 0.001).
The frequency of emergency department visits was also positively and significantly associated with wait times (Pearson correlation coefficient 0.23, p = 0.010). During the study period, 179 (16.8%) of the patients were taken to the emergency department at least once because of their hernia while waiting for surgery (Table 1). Within 30 days after diagnosis, 126 (11.8%) of the patients had their first visit to the emergency department; 30 (23.8%) of them presented with an incarcerated hernia. Among patients who visited the emergency department, the median time from diagnosis to first visit was 14 days (interquartial range 4–40 days). Children with an incarcerated hernia were more likely than those without an incarcerated hernia to visit the emergency department before surgery (33.8% v. 14.5%, p < 0.001).
Overall, a risk reduction of hernia incarceration of almost 50% could be achieved if the hernia were repaired within 14 days after diagnosis. This also means that, to prevent 1 unnecessary visit to the emergency department or incarceration, 21 hernias would need to be repaired no later than 14 days after diagnosis.
Patients less than 1 year old were at significantly higher risk of an incarcerated hernia than were patients 1–2 years old (odds ratio [OR] 2.07, 95% confidence interval [CI] 1.32–3.23, p < 0.001) (Figure 1 and Figure 2). Compared with boys, girls were at higher risk of an incarcerated hernia after adjustment for age (OR 1.75, 95% CI 1.04–2.93, p = 0.035) (Figure 2 and Figure 3). Use of emergency department services was also significantly associated with an increased risk of incarcerated hernia. In the stratified logistic regression analysis, children less than 1 year old had a higher but nonsignificant risk of incarcerated hernia if the surgery was conducted no later than 14 days after diagnosis (OR 1.53, 95% CI 0.67–3.49). The risk increased to 2-fold if the wait time was more than 14 days (OR 1.92, 95% CI 1.11–3.32, p = 0.020). (Figure 2).
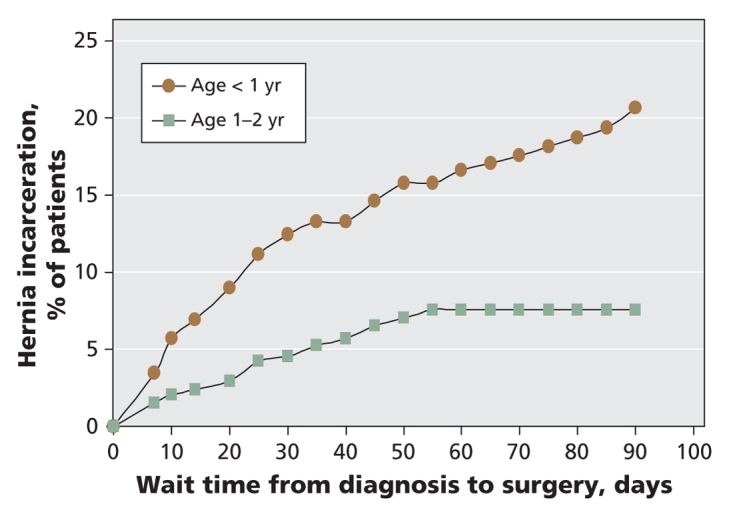
Figure 1: Risk of hernia incarceration by wait time and age group among 1065 infants and young children waiting for surgical repair of an inguinal hernia in fiscal years 2002 and 2003.
Figure 2: Effect of covariates on the probability of hernia incarceration. Variables included in the logistic regression model were children's age, sex, number of visits to the emergency department after diagnosis and wait time for surgery. In the stratified logistic regression model, the variable of visits to the emergency department was dichotomized (≥ 1 visit v. none). CI = confidence interval.
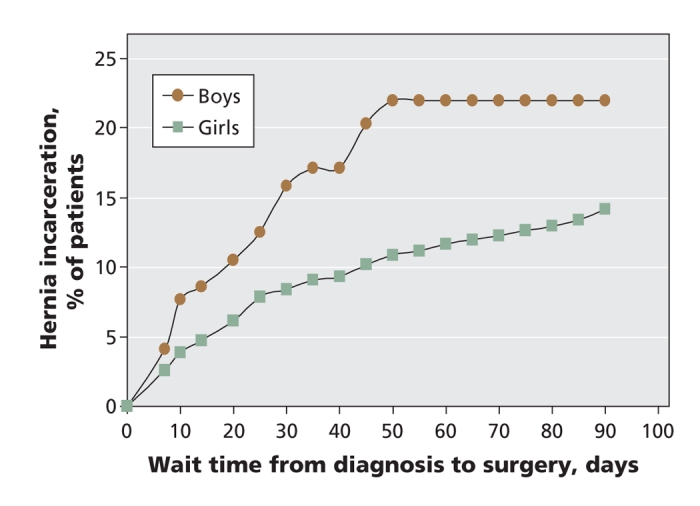
Figure 3: Risk of hernia incarceration by wait time and patient sex among 1065 infants and young children waiting for surgical repair of an inguinal hernia.
Interpretation
We observed an overall rate of hernia incarceration of 11.9% among the infants and young children with inguinal hernia in our study. A wait time for surgery of more than 14 days was associated with a doubling of the risk of incarceration. The overall rate of incarceration is comparable to those reported by others.1,12
In a retrospective report of institutional-based data, Stylianos and colleagues13 reviewed all cases of children with an incarcerated hernia who presented to an emergency department. They calculated a risk of hernia incarceration of 9% related to a mean wait time of 8 days (range 0.5–28 days).
More than 16% of our patients had 1 visit to the emergency department, and almost 5% had 2 or more visits while waiting for surgery. We also found that, by 30 days after diagnosis, 1 in 9 children had already presented to the emergency department because of their hernia. Almost one quarter of these visits were related to hernia incarceration. Emergency department visits are important indicators because they reflect use of health care resources as well as being a surrogate for parental concern and patient suffering during the wait for surgery.
The fact that inguinal hernias are not self-limiting and that there is a risk of complications dictate the need for expedient surgical repair.14 Parental anxiety while waiting for surgery is another important issue. In a survey by Miller15 of parents of children awaiting various operations, 49% of the children were waiting for repair of an inguinal hernia. Over 95% of the families in the survey suggested that the wait for surgery was emotionally stressful. Furthermore, 37% felt that waiting for surgery prohibited them from participating in their usual activities. Dissatisfaction with wait times for surgery has also been expressed by adults.16,17
Our findings have important implications for physicians and policy-makers. They point out the high risk of hernia incarceration among infants and children less than 2 years of age while waiting for surgery. The results also highlight the importance of prompt referral to a surgeon and prompt scheduling of elective surgery. That 11.8% of the patients visited an emergency department at least once also provides important information to health care practitioners about what is happening to their patients while they await surgery. That 5.0% of the cohort had 2 or more visits underscores the importance of educating parents at the time of the first medical encounter. This step may decrease underlying anxiety and result in fewer visits to the emergency department.
Health care planners and policy-makers must design strategies to decrease wait times and improve outcomes for hernia repair among infants and young children. In a recent economic analysis, Schaafsma18 discussed the importance of substituting the current “consensus” method of benchmarking an acceptable wait time — as many specialties, including our own, have done — with an evidence-based strategy. Our study provides important information for achieving such a strategy.
Limitations
Our study has a number of limitations. First, our use of administrative databases limited our ability to examine the underlying causes of prolonged wait times. However, the use of the Canadian Institute for Health Information database to study wait times for surgical procedures and treatment has been validated by others.7
Second, the use of data for fiscal years 2002 and 2003 may not reflect what is occurring currently. We chose this period, however, because it was the latest for which complete data were available from the Canadian Institute for Health Information database.
Third, we were unable to distinguish whether the prolonged wait times were due to lack of physician education or to limited resources. It is likely that both factors are important.
Finally, because of database limitations, we were unable to include children who presented to an emergency department for the first time. This could decrease our ability to capture the full magnitude of morbidities associated with the wait times for hernia repair and to comprehensively examine issues of access to care.
Conclusion
Longer wait times were associated with an increased risk of hernia incarceration and more visits to the emergency department among infants and young children waiting for surgical repair of an inguinal hernia. Waiting for surgery for more than 14 days doubled the risk for incarceration. Our data support a recommendation that all inguinal hernias in infants and young children should be repaired within 14 days after surgical consultation.
@@ See related commentary by Blair, page 983
Supplementary Material
Acknowledgments
We thank the Institute for Clinical Evaluative Sciences for the use of the Ontario health administrative databases.
Footnotes
Une version française de ce résumé est disponible à l'adresse www.cmaj.ca/cgi/content/full/179/10/1001/DC1
Funding: No external funding was received for this research.
This article has been peer reviewed.
Contributors: All of the authors contributed to the conception and design of the study, the acquisition and interpretation of the data, and the drafting and revising of the manuscript. All of the authors approved the final version of the manuscript for publication.
Mohammed Zamakhshary is supported by the King Abdullah International Medical Research Center. Teresa To is supported by the 2007 Dales Award in Medical Research awarded by the University of Toronto Life Sciences Committee. Jacob Langer is supported by the Robert M. Filler Chair in Pediatric General Surgery, The Hospital for Sick Children Research Institute.
Competing interests: None declared.
Correspondence to: Dr. Jacob C. Langer, Division of General Surgery, Rm. 1526, The Hospital for Sick Children, 555 University Ave., Toronto ON M5G 1X8; fax 416 813-7477; jacob.langer@sickkids.ca
REFERENCES
- 1.Lau ST, Lee YH, Caty MG. Current management of hernias and hydroceles. Semin Pediatr Surg 2007;16:50-7. [DOI] [PubMed]
- 2.Bronsther B, Abrams MW, Elboim C. Inguinal hernias in children — a study of 1,000 cases and a review of the literature. J Am Med Womens Assoc 1972;27:522-5. [PubMed]
- 3.Puri P, Guiney EJ, O'Donnell B. Inguinal hernia in infants: the fate of the testis following incarceration. J Pediatr Surg 1984;19:44-6. [DOI] [PubMed]
- 4.Lawrentschuk N, Hewitt P, Ritchard M. Elective laparoscopic cholecystectomy: implications of prolonged waiting times for surgery. ANZ J Surg 2003;73:890-3. [DOI] [PubMed]
- 5.Dodds W, Morgan M, Wolfe C, et al. Implementing the 2-week wait rule for cancer referral in the UK: general practitioners' views and practices. Eur J Cancer Care (Engl) 2004;13:82-7. [DOI] [PubMed]
- 6.Lofvendahl S, Eckerlund I, Hansagi H, et al. Waiting for orthopaedic surgery: factors associated with waiting times and patients' opinion. Int J Qual Health Care 2005;17:133-40. [DOI] [PubMed]
- 7.Simunovic M, Theriault ME, Paszat L, et al. Using administrative databases to measure waiting times for patients undergoing major cancer surgery in Ontario, 1993–2000. Can J Surg 2005;48:137-42. [PMC free article] [PubMed]
- 8.Bardell T, Belliveau P, Kong W, et al. Waiting times for cancer surgery in Ontario: 1984–2000. Clin Oncol (R Coll Radiol) 2006;18:401-9. [DOI] [PubMed]
- 9.Sobolev B, Mercer D, Brown P, et al. Risk of emergency admission while awaiting elective cholecystectomy. CMAJ 2003;169:662-5. [PMC free article] [PubMed]
- 10.Coyte PC, Wright JG, Hawker GA, et al. Waiting times for knee-replacement surgery in the United States and Ontario. N Engl J Med 1994;331:1068-71. [DOI] [PubMed]
- 11.Malek S, Torella F, Edwards PR: Emergency repair of groin herniae: outcome and implications for elective surgery waiting times. Int J Clin Pract 2004;58:207-9. [DOI] [PubMed]
- 12.Grosfeld JL. Current concepts in inguinal hernia in infants and children. World J Surg 1989;13:506-15. [DOI] [PubMed]
- 13.Stylianos S, Jacir NN, Harris BH. Incarceration of inguinal hernia in infants prior to elective repair. J Pediatr Surg 1993;28:582-3. [DOI] [PubMed]
- 14.Borenstein SH, To T, Wajja A, et al. Effect of subspecialty training and volume on outcome after pediatric inguinal hernia repair. J Pediatr Surg 2005;40:75-80. [DOI] [PubMed]
- 15.Miller GG. Waiting for an operation: parents' perspectives. Can J Surg 2004;47:179-81. [PMC free article] [PubMed]
- 16.Ho E, Coyte PC, Bombardier C, et al. Ontario patients' acceptance of waiting times for knee replacements. J Rheumatol 1994;21:2101-5. [PubMed]
- 17.Kee F, McDonald P, Gaffney B. Prioritising the cardiac surgery waiting list: the angina patient's perspective. Heart 1997;77:330-2. [DOI] [PMC free article] [PubMed]
- 18.Schaafsma J. Are there better ways to determine wait times? CMAJ 2006;174:1551-2. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.