There is no widely accepted standard for antifungal prophylaxis in patients with hematologic malignancies. The Infectious Diseases Working Party of the German Society for Haematology and Oncology assigned a committee of hematologists and infectious disease specialists to develop the recommendations described in this Decision Making and Problem Solving article.
Keywords: invasive fungal infection, antifungal prophylaxis, itraconazole, fluconazole, posaconazole, amphotericin B, liposomal
Abstract
There is no widely accepted standard for antifungal prophylaxis in patients with hematologic malignancies. The Infectious Diseases Working Party of the German Society for Haematology and Oncology assigned a committee of hematologists and infectious disease specialists to develop recommendations. Literature data bases were systematically searched for clinical trials on antifungal prophylaxis. The studies identified were shared within the committee. Data were extracted by two of the authors (OAC and MSi). The consensus process was conducted by email communication. Finally, a review committee discussed the proposed recommendations. After consensus was established the recommendations were finalized. A total of 86 trials were identified including 16,922 patients. Only a few trials yielded significant differences in efficacy. Fluconazole 400 mg/d improved the incidence rates of invasive fungal infections and attributable mortality in allogeneic stem cell recipients. Posaconazole 600 mg/d reduced the incidence of IFI and attributable mortality in allogeneic stem cell recipients with severe graft versus host disease, and in patients with acute myelogenous leukemia or myelodysplastic syndrome additionally reduced overall mortality. Aerosolized liposomal amphotericin B reduced the incidence rate of invasive pulmonary aspergillosis. Posaconazole 600 mg/d is recommended in patients with acute myelogenous leukemia/myelodysplastic syndrome or undergoing allogeneic stem cell recipients with graft versus host disease for the prevention of invasive fungal infections and attributable mortality (Level A I). Fluconazole 400 mg/d is recommended in allogeneic stem cell recipients until development of graft versus host disease only (Level A I). Aerosolized liposomal amphotericin B is recommended during prolonged neutropenia (Level B II).
Introduction
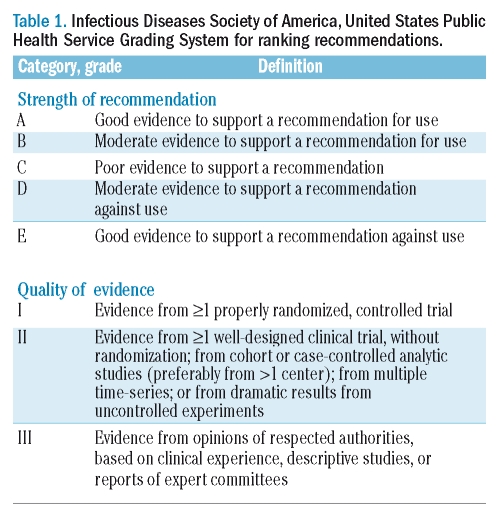
The rising incidence of invasive fungal infections, especially invasive aspergillosis, compromises therapeutic outcomes in hematologic cancer patients and in transplant recipients.1–5 The utilization of newly introduced antifungal agents clearly improved the tolerability of patients combating severe underlying diseases.6,7 Despite better outcome in primary treatment of invasive aspergillosis in comparison to conventional amphotericin B, response and survival require further improvement.8,9 Additionally, early diagnosis of invasive fungal infections is critical.10 But usually diagnosis is delayed and thus hampers further treatment outcome.11 Therefore, the prevention of invasive fungal infections upfront has become the major goal in patient care in high-risk patient populations. Since the first edition of these recommendations regarding antifungal prophylaxis, close to 20 relevant publications have been added to the field, necessitating an updated review of their impact on clinical decision making.12 On the other hand new meta-analyses on prophylaxis of invasive fungal infections have also been published, but do not differentiate between specific patient populations and risk factors.13,14 To maintain comparability with the previous recommendation, the EBM criteria proposed by the Infectious Diseases Society of America (IDSA) are again employed throughout this document (Table 1).15
Table 1.
Infectious Diseases Society of America, United States Public Health Service Grading System for ranking recommendations.
Several newly introduced antifungal agents have been utilized in prophylaxis for the first time. These and other new studies have been incorporated into this updated guideline of the Infectious Diseases Working Party (AGIHO) of the German Society for Haematology and Oncology. The aim of this review is to provide the treating physician an up-to-date tool for the daily bedside decisions on primary antifungal prophylaxis.
Objectives of antifungal prophylaxis
It is evident that the most relevant endpoint of antifungal prophylaxis is the reduction of mortality. However, death attributable to invasive fungal infection is difficult to prove and a reduction in overall mortality as a desirable endpoint of any clinical decision is difficult to achieve in the context of multiple competing illnesses in a severely immunocompromised host. Thus usually the reduction of the incidence rate of breakthrough invasive fungal infection is chosen as the primary endpoint of clinical trials. Improving rates of mucosal or other superficial infection and reducing colonization are no proper endpoints for antifungal prophylaxis with systemically active compounds.
Design and Methods
The guideline was prepared by a group of German clinicians. Systematic literature search comprised Medline, CancerLit, Embase, Cochrane Library and conference proceedings of Advances Against Aspergillosis, ASH, EBMT, ECCMID, ESMO, Focus on Fungal Infections, and ICAAC/IDSA, yielding a total of 86 clinical trials comprising 16,922 patients. Data extracted by OAC and MSi from each clinical study identified, were patient characteristics and outcomes, year published, number of patients, demographic characteristics, underlying malignancy, type of transplant, type of control group, prophylactic regimens including dosage, duration of neutropenia, isolation measures, mucositis grade, central venous catheters, duration of prophylactic treatment, adverse events, premature discontinuations, incidence and etiology of invasive and superficial fungal infections, level of certainty of diagnosis (proven, probable, possible), overall and invasive fungal infections attributable mortality. For easier comparison, this consensus paper contains comprehensive tables of the trials on antifungal prophylaxis published to date (Online Supplementary Tables S1 to S7). Trials published as abstracts only, and meta-analyses were not taken into account for the recommendations. Clean air systems are not addressed in this guideline.
Data extracted were tabulated and distributed to the committee together with a first manuscript drafted by OAC and AJU. The consensus process was performed as an email based discussion group moderated by OAC. In a second step the panelists draft was peer reviewed by the review committee of the Infectious Diseases Working Party of the German Society for Haematology and Oncology. The resulting recommendations are based on scientific publications and information published at the conferences named above. In case of a lack of uniform consensus, the vote of the majority of group members was adopted. Both committees serve as the authors of the recommendation. Since the IDSA criteria are most commonly used in infectious diseases, the ID Working Party of the DGHO decided to adopt these. Thus, meta-analyses and studies not published as a full paper are reported when considered appropriate, but do not influence the levels of evidence given.
Results
Azoles
Fluconazole (Online Supplementary Table S1) is the antifungal with the highest number of well-designed prophylaxis trials. In comparative trials oral daily doses from 50 mg up to 400 mg were given.16,17 The two most relevant trials were placebo controlled, double blinded and involved mainly allogeneic stem cell transplant recipients.16–18 Fluconazole 400 mg/d was significantly superior to placebo in both the reduction of breakthrough invasive fungal infection and the decrease of IFI attributable mortality. In a longitudinal observation survival benefit extended beyond the period of fluconazole treatment (75 days) and was accompanied by a lower incidence of intestinal graft versus host disease.19 Moreover, fluconazole has been reported to protect from cyclophosphamide toxicity.20 A particular strength of both trials was the homogeneous, strictly defined and high-risk patient population. Other trials mostly examined heterogeneous patient groups with different underlying conditions and risk groups, and subsequently failed to demonstrate an advantage over the comparator drug. A large placebo-controlled trial on fluconazole 400 mg/d resulted in a significant reduction of proven invasive candidiasis and mortality attributed to fungal infection, but the study population was too heterogeneous to lead to a clear cut recommendation for a specific patient group.21 Moreover, two more trials comparing fluconazole 400 mg/d versus placebo in non-transplant settings found no significant effect on the incidence rate of proven invasive fungal infections and mortality.22,23 Doses lower than 400 mg/d failed to show a marked benefit and have not been carried out in a placebo controlled fashion.17,24–27 Since moulds and Candida krusei, harbor intrinsic resistance to fluconazole and only dose dependent activity against Candida glabrata, breakthrough infections with these fungi have occurred.16,21,23,28,29 The clinical relevance of the development of resistance during fluconazole prophylaxis is still a matter of debate,30,31 while a general shift towards higher rates of strains exhibiting primary resistance have been clearly shown in the intensive care setting.32 The favorable safety profile and patient compliance rate of fluconazole resulted in discontinuation rates of less than 8%. There is good evidence (Level A I) that primary prophylaxis with fluconazole 400 mg/d reduces the incidence of invasive candidiasis and the mortality rate after allogeneic hematopoietic stem cell transplant. For patients with acute leukemia prophylaxis with fluconazole 400 mg/d cannot be recommended with similar strength (Level C I). Doses less than 400 mg/d have not been effective in well designed trials (Level E I).
Itraconazole (Online Supplementary Table S2) has a broader spectrum of activity than fluconazole including non-albicans Candida species and moulds. Itraconazole capsules lead to adequate plasma levels with delay, if at all, and thus are not recommended as a start-up for prophylaxis of invasive fungal infection.27,33,34 A superior bioavailability is achieved with itraconazole oral suspension. A double-blind, double dummy, placebo controlled trial comparing the suspension at a dose of 2.5 mg/kg bid plus nystatin 500.000 IU qid to nystatin alone found a more effective reduction in the rate of fatal candidemia from 2% to zero. Invasive mould infections and death due to fungal infection were not prevented.35 Lower daily doses of itraconazole oral suspension did not effectively reduce the incidence of invasive fungal infections or mortality.36 Itraconazole oral solution 2.5 mg/kg bid compared to fluconazole 400 mg/d showed no difference in the incidence rate of fungal infection or mortality in patients with hematologic malignancies.37 A randomized trial on allogeneic stem cell transplant recipients compared intravenous followed by oral itraconazole solution 400 mg/d versus fluconazole 400 mg/d given until day 100 post transplant (for treatment schedules see Online Supplementary Table S2). Itraconazole reduced proven invasive fungal infections more effectively, but failed to improve attributable mortality.38 Another controlled trial compared intravenous itraconazole 200 mg/d or oral suspension 7.5 mg/kg/d with parenteral or oral fluconazole 400 mg/d. The trial included 304 allogeneic transplant recipients. In patients on itraconazole therapy, a statistically significant reduction of breakthrough mould infection was achieved. But a reduction in the rate of proven and probable invasive fungal infections, and overall or attributable mortality, was not observed. Prophylaxis was associated with a higher rate of toxicity and gastrointestinal intolerance leading to a 36% withdrawal rate.39 Moreover the concomitant use of the chemotherapy regimen busulfan/cyclophosphamide and itraconazole resulted in a higher toxic death rate documented here for the first time.40 Clinical trial protocols thereafter did not allow for concomitant azole prophylaxis during chemotherapy with busulfan, cyclophosphamide and – for theoretical concerns of cardiotoxicity – anthracyclines. In the non-transplant setting high withdrawal rates had been previously reported with itraconazole oral solution given at doses of 2.5 mg/kg bid and 400 mg/d. These withdrawals were primarily due to gastrointestinal adverse events.26,35 While no single study demonstrated a lower rate of death attributed to invasive fungal infection, only one meta-analysis suggested that itraconazole oral suspension is effective to this regard.41 Close patient supervision and motivation appears to be warranted because of the unpleasant taste of the oral solution. Moreover, the use of itraconazole demands frequent plasma level monitoring to evaluate whether plasma concentrations of greater than 500 ng/mL are reliably reached within a few days.42 This concentration is achieved by the majority of patients after one week of prophylactic itraconazole oral solution 400 mg/d plus capsules 800 mg/d.42 Other investigators evaluated intravenous loading dose concepts.43,44 In summary, itraconazole has been shown to be effective in reducing breakthrough fungal infections in randomized trials, but did not reduce attributable or overall mortality rates. There is poor evidence for the use of itraconazole capsules alone (Level C I). For the reduction of mortality attributable to invasive fungal infections, there is poor evidence as well as for the use of itraconazole 400 mg/d oral solution (Level C I), with or without an intravenous equivalent dose loading period. Itraconazole exposure should be avoided during the chemotherapy period, especially vincristin and cyclophosphamide.
Posaconazole (Online Supplementary Table S3) has been compared to fluconazole 400 mg/d or itraconazole 400 mg/d in a randomized, open-label clinical trial in patients undergoing induction chemotherapy for acute myelogenous leukemia or myelodysplastic syndrome. At a dose of 600 mg/d posaconazole resulted in a significant reduction in proven and probable invasive fungal infections, mainly by reducing the incidence rate of aspergillosis. Attributable and overall mortality were significantly reduced as well. Safety, including the overall rate of patients with serious adverse events, was comparable between the three drugs. The only difference was a higher rate of patients on posaconazole experiencing possibly or probably related serious adverse events than patients on fluconazole or itraconazole prophylaxis. However, these events did not translate into a higher rate of study drug discontinuation.28 In addition, this study was open-labeled and evaluation of adverse events was not without possible investigator bias. In another trial, allogeneic hematopoietic stem cell recipients with severe graft versus host disease (GvHD) were randomly allocated to receive posaconazole 600 mg/d or fluconazole 400 mg/d in a double blinded fashion. Patients receiving posaconazole prophylaxis had reduced rates of proven and probable invasive fungal infections and attributable mortality. Posaconazole was found to be as safe and tolerated as fluconazole in this trial.29 Prophylaxis with posaconazole 600 mg/d is recommended during induction chemotherapy induced neutropenia in patients with AML or MDS due to its effects on the rate reduction of invasive fungal infection and death (Level A I). Posaconazole 600 mg/d is recommended in hematopoietic stem cell recipients with GvHD because of the reduction in the rates of invasive fungal infection and attributable mortality (Level A I).
Voriconazole (Online Supplementary Table S3) prophylaxis has been evaluated in a small clinical trial.45 Currently prospective clinical trials are either ongoing (clinicaltrials.gov Identifier NCT00289991;) or have recently been presented at conferences.46 As of yet no data are available from peer-reviewed publications of sufficiently powered randomized trials in this indication. In case series prolonged voriconazole exposure has been associated with a reduction of invasive aspergillosis, but an increase in breakthrough zygomycosis.47–49 To date voriconazole prophylaxis cannot be recommended (Level C II).
Ketoconazole (Online Supplementary Table S4) is used as a prophylactic option in very few centers. The majority of trials published have evaluated a daily dose of 400 mg. Virtually all of these trials are underpowered, so that a reliable conclusion is not achievable.50–58
Miconazole (Online Supplementary Table S4) did not effectively reduce the incidence rate of invasive fungal infections at a dose of 2 g/d in a small randomized placebo-controlled trial.59 Another trial evaluated miconazole inhalation, but was too small to uncover any statistically significant difference to the comparator, fluconazole 400 mg/d.60
Clotrimazole (Online Supplementary Table S4) at a dose of 20 mg/d applied together with nystatin 2 Mill IU was inferior to fluconazole 200 mg/d in a single trial evaluating the prophylactic benefit of this drug.61 In summary, there is poor evidence for the prophylactic use of ketoconazole, miconazole or clotrimazole (Level E II).
Polyenes
Amphotericin B has broad spectrum antifungal activity. It is frequently used as oral suspension at doses of 1.5 to 3 g/d. Lozenges and suspension may lower the incidence of superficial fungal infections.17,62 Prevention of invasive candidiasis was not demonstrated and reduction of aspergillosis acquired by inhalation can obviously not be expected from a non-absorbable oral drug.
Amphotericin B inhalation (Online Supplementary Table S6) in the deoxycholate formulation was considered active in reducing invasive pulmonary aspergillosis on the basis of non-comparative studies.63,64 The only large multicenter trial did not confirm these results (Level E I).65 In a non-comparative evaluation of inhalational amphotericin B lipid complex 50 mg/d and concomitant fluconazole 400 mg/d were found to be safe in allogeneic stem cell recipients.66 A placebo-controlled trial on aerosolized liposomal amphotericin B resulted in a significant reduction of invasive pulmonary aspergillosis, but did not improve survival. All patients received fluconazole at an undisclosed dose and route.67 Aerosolized liposomal amphotericin B appears to be effective, but does not prevent invasive fungal infections other than pulmonary (Level B II). Adverse events in these trials included coughing, bad taste and nausea.65–67
Polyenes have been applied intranasally, but there has never been any supporting randomized trial.
Amphotericin B deoxycholate infusion (Online Supplementary Table S5) has been evaluated in different dosages ranging from 0.1 mg/kg/d to 1.0 mg/kg/tiw. A low dose of 0.1 mg/kg/d had no benefit over placebo.68 A prospective trial of amphotericin B 0.2 mg/kg/d versus fluconazole 400 mg p.o. in allogeneic and autologous stem cell transplant recipients showed comparable efficacy, but a higher toxicity of amphotericin B.69 Amphotericin B 0.5 mg/kg three times weekly resulted in a 22% rate of serum creatinine increases above 2 mg/dL and an 11% withdrawal rate in a small trial conducted in the early 1990s.70 A historically controlled study suggested efficacy of intravenous prophylaxis with amphotericin B 1 mg/kg/q48h in reducing proven and probable invasive fungal infections. Amphotericin B had to be discontinued due to adverse events in 4% of patients only,71 and in another historically controlled trial 1 out of 10 patients withdrew from prophylaxis.72 As of today amphotericin B in a dose higher than 0.2 mg/kg/d has not been evaluated in a sufficiently powered well-designed trial. Amphotericin B deoxycholate is a toxic drug, but preventive measures such as sodium chloride loading evolved over the years.73 Other trials could not confirm that toxicity is preventable.74,75 Due to its infusion related and other toxic potential, amphotericin B deoxycholate needs an experienced team if it is ever to be considered to be used in patients. Its prophylactic use is strongly discouraged due to its toxicity profile (Level E I). The drug has now been replaced in almost all its former indications.76
Lipid-based amphotericin B formulations (Online Supplementary Table S5). Prophylactic use of liposomal amphotericin B remains attractive due to its lower toxicity. Its efficacy has been shown in a murine model.77 Liposomal amphotericin B was evaluated in a small study population at 1 mg/kg/d versus placebo, but no significant effect could be detected.78–80 A second placebo-controlled but underpowered trial also failed to disclose an advantage of liposomal amphotericin B 2 mg/kg/tiw.81 Recently a randomized clinical trial (n= 132) compared liposomal amphotericin B 50 mg q48h with no prophylaxis in a population with hematologic malignancies. In this reasonably sized and dosed study on the prophylactic properties of the drug the investigators observed a significant reduction in the rates for proven and probable invasive fungal infections as well as IFI-attributable mortality rates.82 The results contrast those of a previous placebo controlled trial evaluating a similar approach.81 A pilot trial evaluated a novel loading dose concept of liposomal amphotericin B 10 mg/kg qw; while the regimen was feasible in acute leukemia, it was associated with adverse events leading to treatment discontinuation in 6 of 8 stem cell recipients.83 Intravenous Amphotericin B Lipid Complex and Amphotericin B Colloidal Dispersion prophylaxis may be conceivable as well.84 However, neither approach has been sufficiently evaluated and cannot be recommended at present.
In conclusion, prophylaxis with topical amphotericin B is not recommended (Level E I). For aerosolized amphotericin B deoxycholate there is evidence against a recommendation (Level E I). Aerosolized liposomal amphotericin B reduces the incidence of invasive pulmonary aspergillosis, but yields no protection for extra-pulmonary infections (Level B II). Intravenous prophylaxis with amphotericin B deoxycholate is not recommended (Level E I). Liposomal amphotericin B prophylaxis at a dose of 50 mg q48h can be considered (Level C II).
Nystatin use has been criticised in a recent Cochrane review because its efficacy against invasive fungal infections has not been demonstrated.85 A trial conducted in the 1980s suggested a reduction in the colonization rate, but in the end the results were inconclusive.86
In summary, there is no evidence to support the prophylactic efficacy of nystatin (Level E II).
Echinocandins
Caspofungin (Online Supplementary Table S7) prophylaxis at a dose of 50 mg/d has been compared with intravenous itraconazole 400 mg/d in a randomized open-label study. In 192 patients with acute myelogenous leukemia, similar efficacy and safety was found in both treatments.87
Micafungin (Online Supplementary Table S7) at a dose of 50 mg/d has been compared to fluconazole 400 mg/d in a large double-blind trial on 882 patients undergoing autologous or allogeneic hematopoietic stem cell transplantation. Invasive candidiasis was effectively prevented by both regimens, and the rate of aspergillosis was lower in the micafungin group but did not reach significance in those subgroups despite the fact of successful prophylaxis in the primary composite endpoint. Unfortunately, possible invasive fungal infections were part of the primary endpoint of the trial, impairing comparability with other clinical trials.88 No significant reduction of the overall and attributable fungal mortality was detected. The study population comprised autologous and allogeneic stem cell recipients with various underlying malignant diseases and were studied only during the neutropenic phase.89 The results may be difficult to put into the context of other trials, since for the 46% autologous transplant patients, who are not at risk for invasive fungal infection, both treatment arms have to be considered experimental.88
In summary, there is limited evidence supporting the prophylactic use of micafungin (Level C I) during the neutropenic phase of hematopoietic stem cell transplantation and caspofungin use during neutropenia (Level C I).
Conclusions
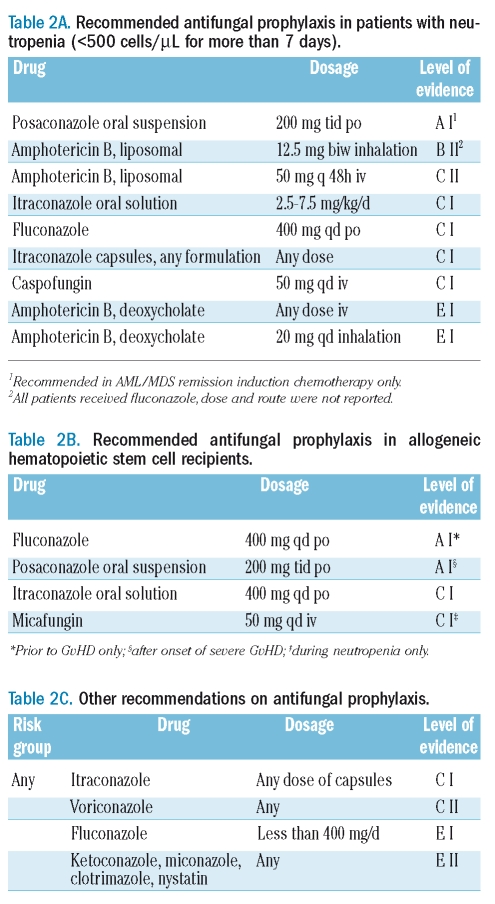
The following recommendations are summarized in Tables 2A-C. Improvement of mortality attributable to invasive fungal infection and a reduced rate of candida infections have been shown for fluconazole 400 mg/day in allogeneic transplant recipients from conditioning until day 75. Since posaconazole reduced the incidence of proven and probable invasive fungal infections and attributable mortality in allogeneic hematopoietic stem cell recipients with severe GvHD (Level A I) the recommendation of fluconazole 400 mg/day is now limited for the time from conditioning until development of severe GvHD (Level A I). Prophylactic use of posaconazole 600 mg/d demonstrated a reduction of the incidence rates of proven and probable invasive fungal infections and more importantly a reduction of attributable and overall mortality in patients with AML/MDS remission induction chemotherapy (Level A I). At present, data advocating itraconazole prophylaxis are less conclusive (Level C I). Data quality on voriconazole prophylaxis is currently inadequate, but emerging zygomycosis has been reported with its prolonged use (Level C II). Studies of the echinocandins, caspofungin and micafungin harbor limited support in prophylactic use during neutropenia (Level C I). Intravenous liposomal amphotericin B 50 mg q48h can be applied in neutropenic leukemia patients (Level C II). Aerosolized liposomal amphotericin B significantly reduced the incidence rate of invasive pulmonary aspergillosis, but was given with concomitant fluconazole (Level B II). The use of amphotericin B deoxycholate in antifungal prophylaxis is discouraged (Level E I). Despite several trials in less aggressive chemotherapy, evidence for the use of antifungal prophylaxis in these situations is poor (Level E I). Further the authors recommend not utilizing antifungal agents such as ketoconazole, miconazole and clotrimazole (Level E II).
Table 2A.
Recommended antifungal prophylaxis in patients with neutropenia (<500 cells/μL for more than 7 days).
Table 2C.
Other recommendations on antifungal prophylaxis.
Table 2B.
Recommended antifungal prophylaxis in allogeneic hematopoietic stem cell recipients.
Invasive fungal infections are an ongoing diagnostic and prognostic challenge for clinicians in the everyday care of immunocompromised patients. The principal efficacy of antifungal prophylaxis has been proven in certain high-risk patient populations but not for others. Intensive efforts need to be undertaken to decrease the incidence and attributable mortality of invasive fungal infections by targeted prophylaxis or improved diagnostic procedures.
Supplementary Material
Acknowledgments
The guideline was prepared by the Committee on Antifungal Prophylaxis of the IDWP of the DGHO: Oliver A. Cornely, Meinolf Karthaus, William Krüger, Michael Sandherr, Michal Sieniawski, and Andrew J. Ullmann. The draft version was peer reviewed by the other members of the IDWP referred to as the Review Committee: Angelika Böhme, Dieter Buchheidt, Werner Heinz, Hermann Einsele, Stefan W. Krause, Georg Maschmeyer, Olaf Penack, Jörg Ritter, Markus Ruhnke, Jörg-Janne Vehreschild, and Hans-Heinrich Wolf.
Footnotes
Authorship and Disclosures
All authors have substantially contributed to the manuscript, the discussion leading in a consensus process to this guideline, every single author can take public responsibility for the content. The authors developed the conception and design of the work, analyzed and interpreted data, drafted the article, revised it critically several times, and finally approved the version submitted. OAC is supported by the German Federal Ministry of Research and Education (BMBF grant 01KN0706) has received research grants from Astellas, Basilea, Bayer, Essex/Schering-Plough, Genzyme, Gilead, Pfizer, Merck/MSD, Optimer, and Vicuron, is a consultant to Astellas, Basilea, F2G, Gilead, Pfizer, Merck/MSD, Mölnlycke, Nektar, Essex/Schering-Plough, and Zeneus, and served at the speakers’ bureau of Astellas, Gilead, Merck/MSD, Pfizer, Essex/Schering-Plough, SpePharm, and United Medical. AB has received research grants from Astellas, Basilea, Essex/Schering-Plough, Gilead Sciences, Merck/MSD and Pfizer, and is a consultant to and served at the speakers’ bureau of Essex/Schering-Plough, Gilead Sciences, and Merck/MSD. DB has received research grants from Gilead Sciences, Merck/MSD, Pfizer, and Essex/Schering-Plough and served at the speakers’ bureau of Essex/Schering-Plough, Gilead Sciences, Merck/MSD, and Pfizer. HE is a consultant to MSD. WJH has received research grants from Astellas, Essex/Schering-Plough, Gilead Sciences, Merck/MSD, Pfizer, is a consultant to Essex/Schering-Plough, and served at the speakers’ bureau of Essex/Schering-Plough, Gilead Sciences, MSD, and Pfizer. MK is a consultant to Essex/Schering-Plough and Pfizer. SWK has received research grants from Gilead Sciences, and served at the speakers’ bureau of Merck/MSD and Pfizer. GM has received research grants from Amgen, Janssen-Cilag, Novartis, and Roche, is a consultant to Essex/Schering-Plough, Gilead Sciences, Sanofi-Aventis, Merck/MSD, Novartis, Pfizer, Riemser, and served at the speakers’ bureau of Cephalon, Gilead Sciences, Merck/MSD, and Pfizer. OP has received research grants from and served at the speakers’ bureau of Gilead Sciences. MR has received research grants from Deutsche Krebshilfe/German Cancer Aid, Pfizer, and Merck/MSD, is a consultant to Astellas, Basilea, Essex/Schering-Plough, Gilead Sciences, Janssen, Merck/MSD, Novartis, Pfizer, and Pliva, and served at the speakers’ bureau of Gilead Sciences, Merck/MSD, and Pfizer. JJV has received travel grant support from Astellas, Essex/Schering-Plough, Gilead Sciences, Merck/MSD, Pfizer and Viro-Pharma. HHW served at the speakers’ bureau of Merck/MSD. AU has received research grants from Schering-Plough, is a consultant to Astellas, Basilea, Essex/Schering-Plough, Gilead Sciences, Merck/MSD, Pfizer, and Stiefel, and served at the speakers’ bureau of Astellas, Essex/Schering-Plough, Gilead Sciences, MSD, and Pfizer. JR, MS, MSi, WK declare no conflicts.
The online version of this article contains a supplementary appendix.
References
- 1.Pfaffenbach B, Donhuijsen K, Pahnke J, Bug R, Adamek RJ, Wegener M, et al. [Systemic fungal infections in hematologic neoplasms. An autopsy study of 1,053 patients] Med Klin. 1994;89:299–304. [PubMed] [Google Scholar]
- 2.Groll AH, Shah PM, Mentzel C, Schneider M, Just-Nuebling G, Huebner K. Trends in the postmortem epidemiology of invasive fungal infections at a university hospital. J Infect. 1996;33:23–32. doi: 10.1016/s0163-4453(96)92700-0. [DOI] [PubMed] [Google Scholar]
- 3.Bodey G, Bueltmann B, Duguid W, Gibbs D, Hanak H, Hotchi M, et al. Fungal infections in cancer patients: an international autopsy survey. Eur J Clin Microbiol Infect Dis. 1992;11:99–109. doi: 10.1007/BF01967060. [DOI] [PubMed] [Google Scholar]
- 4.Rex JH, Sobel JD. Prophylactic antifungal therapy in the intensive care unit. Clin Infect Dis. 2001;32:1191–200. doi: 10.1086/319763. [DOI] [PubMed] [Google Scholar]
- 5.Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, Wenzel RP. Nosocomial bloodstream infections in United States hospitals: a three-year analysis. Clin Infect Dis. 1999;29:239–44. doi: 10.1086/520192. [DOI] [PubMed] [Google Scholar]
- 6.Ullmann AJ. Review of the safety, tolerability, and drug interactions of the new antifungal agents caspofungin and voriconazole. Curr Med Res Opin. 2003;19:263–71. doi: 10.1185/030079903125001884. [DOI] [PubMed] [Google Scholar]
- 7.Raad II, Graybill JR, Bustamante AB, Cornely OA, Gaona-Flores V, Afif C, et al. Safety of long-term oral posaconazole use in the treatment of refractory invasive fungal infections. Clin Infect Dis. 2006;42:1726–34. doi: 10.1086/504328. [DOI] [PubMed] [Google Scholar]
- 8.Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347:408–15. doi: 10.1056/NEJMoa020191. [DOI] [PubMed] [Google Scholar]
- 9.Walsh TJ, Raad I, Patterson TF, Chandrasekar P, Donowitz GR, Graybill R, et al. Treatment of invasive aspergillosis with posaconazole in patients who are refractory to or intolerant of conventional therapy: an externally controlled trial. Clin Infect Dis. 2007;44:2–12. doi: 10.1086/508774. [DOI] [PubMed] [Google Scholar]
- 10.Greene RE, Schlamm HT, Oestmann JW, Stark P, Durand C, Lortholary O, et al. Imaging findings in acute invasive pulmonary aspergillosis: clinical significance of the halo sign. Clin Infect Dis. 2007;44:373–9. doi: 10.1086/509917. [DOI] [PubMed] [Google Scholar]
- 11.von Eiff M, Roos N, Schulten R, Hesse M, Zuhlsdorf M, van de Loo J. Pulmonary aspergillosis: early diagnosis improves survival. Respiration. 1995;62:341–7. doi: 10.1159/000196477. [DOI] [PubMed] [Google Scholar]
- 12.Cornely OA, Böhme A, Buchheidt D, Glasmacher A, Kahl C, Karthaus M, et al. Prophylaxis of invasive fungal infections in patients with hematological malignancies and solid tumors. Guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO) Ann Hematol. 2003;82 (Suppl 2):S186–200. doi: 10.1007/s00277-003-0773-3. [DOI] [PubMed] [Google Scholar]
- 13.Vardakas KZ, Michalopoulos A, Falagas ME. Fluconazole versus itraconazole for antifungal prophylaxis in neutropenic patients with haematological malignancies: a meta-analysis of randomised-controlled trials. Br J Haematol. 2005;131:22–8. doi: 10.1111/j.1365-2141.2005.05727.x. [DOI] [PubMed] [Google Scholar]
- 14.Robenshtok E, Gafter-Gvili A, Goldberg E, Weinberger M, Yeshurun M, Leibovici L, et al. Antifungal prophylaxis in cancer patients after chemotherapy or hematopoietic stem-cell transplantation: systematic review and meta-analysis. J Clin Oncol. 2007;25:5471–89. doi: 10.1200/JCO.2007.12.3851. [DOI] [PubMed] [Google Scholar]
- 15.Kish MA. Guide to development of practice guidelines. Clin Infect Dis. 2001;32:851–4. doi: 10.1086/319366. [DOI] [PubMed] [Google Scholar]
- 16.Goodman JL, Winston DJ, Greenfield RA, Chandrasekar PH, Fox B, Kaizer H, et al. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med. 1992;326:845–51. doi: 10.1056/NEJM199203263261301. [DOI] [PubMed] [Google Scholar]
- 17.Philpott-Howard JN, Wade JJ, Mufti GJ, Brammer KW, Ehninger G. Randomized comparison of oral fluconazole versus oral polyenes for the prevention of fungal infection in patients at risk of neutropenia. Multicentre Study Group. J Antimicrob Chemother. 1993;31:973–84. doi: 10.1093/jac/31.6.973. [DOI] [PubMed] [Google Scholar]
- 18.Slavin MA, Osborne B, Adams R, Levenstein MJ, Schoch HG, Feldman AR, et al. Efficacy and safety of fluconazole prophylaxis for fungal infections after marrow transplantation--a prospective, randomized, double-blind study. J Infect Dis. 1995;171:1545–52. doi: 10.1093/infdis/171.6.1545. [DOI] [PubMed] [Google Scholar]
- 19.Marr KA, Seidel K, Slavin MA, Bowden RA, Schoch HG, Flowers ME, et al. Prolonged fluconazole prophylaxis is associated with persistent protection against candidiasis-related death in allogeneic marrow transplant recipients: long-term follow-up of a randomized, placebo-controlled trial. Blood. 2000;96:2055–61. [PubMed] [Google Scholar]
- 20.Upton A, McCune JS, Kirby KA, Leisenring W, McDonald G, Batchelder A, et al. Fluconazole coadministration concurrent with cyclophosphamide conditioning may reduce regimen-related toxicity postmyeloablative hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2007;13:760–4. doi: 10.1016/j.bbmt.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rotstein C, Bow EJ, Laverdiere M, Ioannou S, Carr D, Moghaddam N. Randomized placebo-controlled trial of fluconazole prophylaxis for neutropenic cancer patients: benefit based on purpose and intensity of cytotoxic therapy. The Canadian Fluconazole Prophylaxis Study Group. Clin Infect Dis. 1999;28:331–40. doi: 10.1086/515128. [DOI] [PubMed] [Google Scholar]
- 22.Schaffner A, Schaffner M. Effect of prophylactic fluconazole on the frequency of fungal infections, amphotericin B use, and health care costs in patients undergoing intensive chemotherapy for hematologic neoplasias. J Infect Dis. 1995;172:1035–41. doi: 10.1093/infdis/172.4.1035. [DOI] [PubMed] [Google Scholar]
- 23.Winston DJ, Chandrasekar PH, Lazarus HM, Goodman JL, Silber JL, Horowitz H, et al. Fluconazole prophylaxis of fungal infections in patients with acute leukemia. Results of a randomized placebo-controlled, double-blind, multicenter trial. Ann Intern Med. 1993;118:495–503. doi: 10.7326/0003-4819-118-7-199304010-00003. [DOI] [PubMed] [Google Scholar]
- 24.Young GA, Bosly A, Gibbs DL, Durrant S. A double-blind comparison of fluconazole and nystatin in the prevention of candidiasis in patients with leukaemia. Antifungal Prophylaxis Study Group. Eur J Cancer. 1999;35:1208–13. doi: 10.1016/s0959-8049(99)00102-1. [DOI] [PubMed] [Google Scholar]
- 25.Menichetti F, Del Favero A, Martino P, Bucaneve G, Micozzi A, D’Antonio D, et al. Preventing fungal infection in neutropenic patients with acute leukemia: fluconazole compared with oral amphotericin B. The GIMEMA Infection Program. Ann Intern Med. 1994;120:913–8. doi: 10.7326/0003-4819-120-11-199406010-00003. [DOI] [PubMed] [Google Scholar]
- 26.Morgenstern GR, Prentice AG, Prentice HG, Ropner JE, Schey SA, Warnock DW. A randomized controlled trial of itraconazole versus fluconazole for the prevention of fungal infections in patients with haematological malignancies. U.K. Multicentre Antifungal Prophylaxis Study Group. Br J Haematol. 1999;105:901–11. doi: 10.1046/j.1365-2141.1999.01465.x. [DOI] [PubMed] [Google Scholar]
- 27.Huijgens PC, Simoons-Smit AM, van Loenen AC, Prooy E, van Tinteren H, Ossenkoppele GJ, et al. Fluconazole versus itraconazole for the prevention of fungal infections in haemato-oncology. J Clin Pathol. 1999;52:376–80. doi: 10.1136/jcp.52.5.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cornely OA, Maertens J, Winston DJ, Perfect J, Ullmann AJ, Walsh TJ, et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007;356:348–59. doi: 10.1056/NEJMoa061094. [DOI] [PubMed] [Google Scholar]
- 29.Ullmann AJ, Lipton JH, Vesole DH, Chandrasekar P, Langston A, Tarantolo SR, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med. 2007;356:335–47. doi: 10.1056/NEJMoa061098. [DOI] [PubMed] [Google Scholar]
- 30.Abbas J, Bodey GP, Hanna HA, Mardani M, Girgawy E, Abi-Said D, et al. Candida krusei fungemia. An escalating serious infection in immunocompromised patients. Arch Intern Med. 2000;160:2659–64. doi: 10.1001/archinte.160.17.2659. [DOI] [PubMed] [Google Scholar]
- 31.Laverdiere M, Rotstein C, Bow EJ, Roberts RS, Ioannou S, Carr D, et al. Impact of fluconazole prophylaxis on fungal colonization and infection rates in neutropenic patients. The Canadian Fluconazole Study. J Antimicrob Chemother. 2000;46:1001–8. doi: 10.1093/jac/46.6.1001. [DOI] [PubMed] [Google Scholar]
- 32.Trick WE, Fridkin SK, Edwards JR, Hajjeh RA, Gaynes RP. Secular trend of hospital-acquired candidemia among intensive care unit patients in the United States during 1989–1999. Clin Infect Dis. 2002;35:627–30. doi: 10.1086/342300. [DOI] [PubMed] [Google Scholar]
- 33.Nucci M, Biasoli I, Akiti T, Silveira F, Solza C, Barreiros G, et al. A double-blind, randomized, placebo-controlled trial of itraconazole capsules as antifungal prophylaxis for neutropenic patients. Clin Infect Dis. 2000;30:300–5. doi: 10.1086/313654. [DOI] [PubMed] [Google Scholar]
- 34.Glasmacher A, Hahn C, Molitor E, Marklein G, Sauerbruch T, Schmidt-Wolf IG. Itraconazole through concentrations in antifungal prophylaxis with six different dosing regimens using hydroxypropyl-beta-cyclodextrin oral solution or coated-pellet capsules. Mycoses. 1999;42:591–600. doi: 10.1046/j.1439-0507.1999.00518.x. [DOI] [PubMed] [Google Scholar]
- 35.Menichetti F, Del Favero A, Martino P, Bucaneve G, Micozzi A, Girmenia C, et al. Itraconazole oral solution as prophylaxis for fungal infections in neutropenic patients with hematologic malignancies: a randomized, placebo-controlled, double-blind, multicenter trial. GIMEMA Infection Program. Gruppo Italiano Malattie Ematologiche dell’Adulto. Clin Infect Dis. 1999;28:250–5. doi: 10.1086/515129. [DOI] [PubMed] [Google Scholar]
- 36.Boogaerts M, Maertens J, van Hoof A, de Bock R, Fillet G, Peetermans M, et al. Itraconazole versus amphotericin B plus nystatin in the prophylaxis of fungal infections in neutropenic cancer patients. J Antimicrob Chemother. 2001;48:97–103. doi: 10.1093/jac/48.1.97. [DOI] [PubMed] [Google Scholar]
- 37.Glasmacher A, Cornely O, Ullmann AJ, Wedding U, Bodenstein H, Wandt H, et al. An open-label randomized trial comparing itraconazole oral solution with fluconazole oral solution for primary prophylaxis of fungal infections in patients with haematological malignancy and profound neutropenia. J Antimicrob Chemother. 2006;57:317–25. doi: 10.1093/jac/dki440. [DOI] [PubMed] [Google Scholar]
- 38.Winston DJ, Maziarz RT, Chandrasekar PH, Lazarus HM, Goldman M, Blumer JL, et al. Intravenous and oral itraconazole versus intravenous and oral fluconazole for long-term antifungal prophylaxis in allogeneic hematopoietic stem-cell transplant recipients. A multicenter, randomized trial. Ann Intern Med. 2003;138:705–13. doi: 10.7326/0003-4819-138-9-200305060-00006. [DOI] [PubMed] [Google Scholar]
- 39.Marr KA, Crippa F, Leisenring W, Hoyle M, Boeckh M, Balajee SA, et al. Itraconazole versus fluconazole for prevention of fungal infections in patients receiving allogeneic stem cell transplants. Blood. 2004;103:1527–33. doi: 10.1182/blood-2003-08-2644. [DOI] [PubMed] [Google Scholar]
- 40.Marr KA, Leisenring W, Crippa F, Slattery JT, Corey L, Boeckh M, et al. Cyclophosphamide metabolism is affected by azole antifungals. Blood. 2004;103:1557–9. doi: 10.1182/blood-2003-07-2512. [DOI] [PubMed] [Google Scholar]
- 41.Glasmacher A, Prentice A, Gorschluter M, Engelhart S, Hahn C, Djulbegovic B, et al. Itraconazole prevents invasive fungal infections in neutropenic patients treated for hematologic malignancies: evidence from a meta-analysis of 3,597 patients. J Clin Oncol. 2003;21:4615–26. doi: 10.1200/JCO.2003.04.052. [DOI] [PubMed] [Google Scholar]
- 42.Glasmacher A, Molitor E, Hahn C, Bomba K, Ewig S, Leutner C, et al. Antifungal prophylaxis with itraconazole in neutropenic patients with acute leukaemia. Leukemia. 1998;12:1338–43. doi: 10.1038/sj.leu.2401137. [DOI] [PubMed] [Google Scholar]
- 43.Caillot D, Bassaris H, McGeer A, Arthur C, Prentice HG, Seifert W, et al. Intravenous itraconazole followed by oral itraconazole in the treatment of invasive pulmonary aspergillosis in patients with hematologic malignancies, chronic granulomatous disease, or AIDS. Clin Infect Dis. 2001;33:e83–90. doi: 10.1086/323020. [DOI] [PubMed] [Google Scholar]
- 44.Sandherr M, Vogeser M, Hartwig C, Aulmann C, Fuhrmann S, Wondzinski L, et al. Antifungal prophylaxis with itraconazole in patients with acute leukemia and after stem cell transplantation. 46th Annual Meeting of the American Society of Hematology; 2004 December 4–7, 2004; San Diego, CA, USA. 2004. [Google Scholar]
- 45.Vehreschild JJ, Bohme A, Buchheidt D, Arenz D, Harnischmacher U, Heussel CP, et al. A double-blind trial on prophylactic voriconazole (VRC) or placebo during induction chemotherapy for acute myelogenous leukaemia (AML) J Infect. 2007;55:445–9. doi: 10.1016/j.jinf.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 46.Wingard JR, Carter SL, Walsh TJ, Kurtzberg J, Small TN, Gersten ID, et al. Results of a Randomized, Double-Blind trial of Fluconazole vs. Voriconazole for the prevention of invasive fungal infections in 600 allogeneic blood and marrow transplant patients. Blood. 2007;110 doi: 10.1182/blood-2010-02-268151. [Abstract #163] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marty FM, Cosimi LA, Baden LR. Breakthrough zygomycosis after voriconazole treatment in recipients of hematopoietic stem-cell transplants. N Engl J Med. 2004;350:950–2. doi: 10.1056/NEJM200402263500923. [DOI] [PubMed] [Google Scholar]
- 48.Glöckner A, Vehreschild JJ, Cornely OA. Zygomycosis - current epidemiological aspects. Mycoses. 2007;50 (Suppl 1):50–5. doi: 10.1111/j.1439-0507.2007.01380.x. [DOI] [PubMed] [Google Scholar]
- 49.Kontoyiannis DP, Lionakis MS, Lewis RE, Chamilos G, Healy M, Perego C, et al. Zygomycosis in a tertiary-care cancer center in the era of Aspergillus-active antifungal therapy: a case-control observational study of 27 recent cases. J Infect Dis. 2005;191:1350–9. doi: 10.1086/428780. [DOI] [PubMed] [Google Scholar]
- 50.Brincker H. Prevention of mycosis in granulocytopenic patients with prophylactic ketoconazole treatment. Mykosen. 1983;26:242–7. [PubMed] [Google Scholar]
- 51.Donnelly JP, Starke ID, Galton DA, Catovsky D, Goldman JM, Darrell JH. Oral ketoconazole and amphotericin B for the prevention of yeast colonization in patients with acute leukaemia. J Hosp Infect. 1984;5:83–91. doi: 10.1016/0195-6701(84)90105-1. [DOI] [PubMed] [Google Scholar]
- 52.Estey E, Maksymiuk A, Smith T, Fainstein V, Keating M, McCredie KB, et al. Infection prophylaxis in acute leukemia. Comparative effectiveness of sulfamethoxazole and trimethoprim, ketoconazole, and a combination of the two. Arch Intern Med. 1984;144:1562–8. doi: 10.1001/archinte.144.8.1562. [DOI] [PubMed] [Google Scholar]
- 53.Hann IM, Prentice HG, Corringham R, Blacklock HA, Keaney M, Shannon M, et al. Ketoconazole versus nystatin plus amphotericin B for fungal prophylaxis in severely immunocompromised patients. Lancet. 1982;1:826–9. doi: 10.1016/s0140-6736(82)91874-8. [DOI] [PubMed] [Google Scholar]
- 54.Hansen RM, Reinerio N, Sohnle PG, Abrams RA, Ritch PS, Libnoch JA, et al. Ketoconazole in the prevention of candidiasis in patients with cancer. A prospective, randomized, controlled, double-blind study. Arch Intern Med. 1987;147:710–2. [PubMed] [Google Scholar]
- 55.Jones PG, Kauffman CA, McAuliffe LS, Liepman MK, Bergman AG. Efficacy of ketoconazole vs nystatin in prevention of fungal infections in neutropenic patients. Arch Intern Med. 1984;144:549–51. [PubMed] [Google Scholar]
- 56.Shepp DH, Klosterman A, Siegel MS, Meyers JD. Comparative trial of ketoconazole and nystatin for prevention of fungal infection in neutropenic patients treated in a protective environment. J Infect Dis. 1985;152:1257–63. doi: 10.1093/infdis/152.6.1257. [DOI] [PubMed] [Google Scholar]
- 57.Vogler WR, Malcom LG, Winton EF. A randomized trial comparing ketoconazole and nystatin prophylactic therapy in neutropenic patients. Cancer Invest. 1987;5:267–73. [PubMed] [Google Scholar]
- 58.Palmblad J, Lonnqvist B, Carlsson B, Grimfors G, Jarnmark M, Lerner R, et al. Oral ketoconazole prophylaxis for Candida infections during induction therapy for acute leukaemia in adults: more bacteraemias. J Intern Med. 1992;231:363–70. doi: 10.1111/j.1365-2796.1992.tb00945.x. [DOI] [PubMed] [Google Scholar]
- 59.Brincker H. Prophylactic treatment with miconazole in patients highly predisposed to fungal infection. A placebo-controlled double-blind study. Acta Med Scand. 1978;204:123–8. doi: 10.1111/j.0954-6820.1978.tb08410.x. [DOI] [PubMed] [Google Scholar]
- 60.Egger T, Gratwohl A, Tichelli A, Uhr M, Stebler Gysi C, Passweg J, et al. Comparison of fluconazole with oral polyenes in the prevention of fungal infections in neutropenic patients. A prospective, randomized, single-center study. Support Care Cancer. 1995;3:139–46. doi: 10.1007/BF00365855. [DOI] [PubMed] [Google Scholar]
- 61.Ellis ME, Clink H, Ernst P, Halim MA, Padmos A, Spence D, et al. Controlled study of fluconazole in the prevention of fungal infections in neutropenic patients with haematological malignancies and bone marrow transplant recipients. Eur J Clin Microbiol Infect Dis. 1994;13:3–11. doi: 10.1007/BF02026116. [DOI] [PubMed] [Google Scholar]
- 62.Rozenberg-Arska M, Dekker AW, Branger J, Verhoef J. A randomized study to compare oral fluconazole to amphotericin B in the prevention of fungal infections in patients with acute leukaemia. J Antimicrob Chemother. 1991;27:369–76. doi: 10.1093/jac/27.3.369. [DOI] [PubMed] [Google Scholar]
- 63.Hertenstein B, Kern WV, Schmeiser T, Stefanic M, Bunjes D, Wiesneth M, et al. Low incidence of invasive fungal infections after bone marrow transplantation in patients receiving amphotericin B inhalations during neutropenia. Ann Hematol. 1994;68:21–6. doi: 10.1007/BF01695915. [DOI] [PubMed] [Google Scholar]
- 64.Erjavec Z, Woolthuis GM, de Vries-Hospers HG, Sluiter WJ, Daenen SM, de Pauw B, et al. Tolerance and efficacy of Amphotericin B inhalations for prevention of invasive pulmonary aspergillosis in haematological patients. Eur J Clin Microbiol Infect Dis. 1997;16:364–8. doi: 10.1007/BF01726364. [DOI] [PubMed] [Google Scholar]
- 65.Schwartz S, Behre G, Heinemann V, Wandt H, Schilling E, Arning M, et al. Aerosolized amphotericin B inhalations as prophylaxis of invasive aspergillus infections during prolonged neutropenia: results of a prospective randomized multicenter trial. Blood. 1999;93:3654–61. [PubMed] [Google Scholar]
- 66.Alexander BD, Dodds Ashley ES, Addison RM, Alspaugh JA, Chao NJ, Perfect JR. Non-comparative evaluation of the safety of aerosolized amphotericin B lipid complex in patients undergoing allogeneic hematopoietic stem cell transplantation. Transpl Infect Dis. 2006;8:13–20. doi: 10.1111/j.1399-3062.2006.00125.x. [DOI] [PubMed] [Google Scholar]
- 67.Rijnders BJ, Cornelissen JJ, Slobbe L, Becker MJ, Doorduijn JK, Hop WC, et al. Aerosolized liposomal amphotericin B for the prevention of invasive pulmonary aspergillosis during prolonged neutropenia: a randomized, placebo-controlled trial. Clin Infect Dis. 2008;46:1401–8. doi: 10.1086/586739. [DOI] [PubMed] [Google Scholar]
- 68.Perfect JR, Klotman ME, Gilbert CC, Crawford DD, Rosner GL, Wright KA, et al. Prophylactic intravenous amphotericin B in neutropenic autologous bone marrow transplant recipients. J Infect Dis. 1992;165:891–7. doi: 10.1093/infdis/165.5.891. [DOI] [PubMed] [Google Scholar]
- 69.Wolff SN, Fay J, Stevens D, Herzig RH, Pohlman B, Bolwell B, et al. Fluconazole vs low-dose amphotericin B for the prevention of fungal infections in patients undergoing bone marrow transplantation: a study of the North American Marrow Transplant Group. Bone Marrow Transplant. 2000;25:853–9. doi: 10.1038/sj.bmt.1702233. [DOI] [PubMed] [Google Scholar]
- 70.Bodey GP, Anaissie EJ, Elting LS, Estey E, O’Brien S, Kantarjian H. Antifungal prophylaxis during remission induction therapy for acute leukemia fluconazole versus intravenous amphotericin B. Cancer. 1994;73:2099–106. doi: 10.1002/1097-0142(19940415)73:8<2099::aid-cncr2820730814>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 71.Karthaus M, Doellmann T, Klimasch T, Elser C, Rosenthal C, Ganser A, et al. Intensive intravenous amphotericin B for prophylaxis of systemic fungal infections. Results of a prospective controlled pilot study in acute leukemia patients. Chemotherapy. 2000;46:293–302. doi: 10.1159/000007301. [DOI] [PubMed] [Google Scholar]
- 72.Böhme A, Hoelzer D. Primary antifungal prophylaxis with low-dose intravenous amphotericin B in hematological malignancies. Results of a pilot study. Onkologie. 2000;23:145–50. [Google Scholar]
- 73.Arning M, Scharf RE. Prevention of amphotericin-B-induced nephrotoxicity by loading with sodium chloride: a report of 1291 days of treatment with amphotericin B without renal failure. Klin Wochenschr. 1989;67:1020–8. doi: 10.1007/BF01727003. [DOI] [PubMed] [Google Scholar]
- 74.Bates DW, Su L, Yu DT, Chertow GM, Seger DL, Gomes DR, et al. Mortality and costs of acute renal failure associated with amphotericin B therapy. Clin Infect Dis. 2001;32:686–93. doi: 10.1086/319211. [DOI] [PubMed] [Google Scholar]
- 75.Ullmann AJ, Sanz MA, Tramarin A, Barnes RA, Wu W, Gerlach BA, et al. Prospective study of amphotericin B formulations in immunocompromised patients in 4 European countries. Clin Infect Dis. 2006;43:e29–38. doi: 10.1086/505969. [DOI] [PubMed] [Google Scholar]
- 76.Cornely OA, Vehreschild JJ, Ullmann AJ. Is there a role for polyenes in treating invasive mycoses¿. Curr Opin Infect Dis. 2006;19:565–70. doi: 10.1097/QCO.0b013e328010851d. [DOI] [PubMed] [Google Scholar]
- 77.BitMansour A, Brown JMY. Prophylactic administration of Liposomal amphotericin B is superior to treatment in a Murine Model of Invasive aspergillosis after hematopoietic cell transplantation. J Inf Dis. 2002;186:134–7. doi: 10.1086/341294. [DOI] [PubMed] [Google Scholar]
- 78.Tollemar J, Ringden O, Andersson S, Sundberg B, Ljungman P, Tyden G. Randomized double-blind study of liposomal amphotericin B (Ambisome) prophylaxis of invasive fungal infections in bone marrow transplant recipients. Bone Marrow Transplant. 1993;12:577–82. [PubMed] [Google Scholar]
- 79.Tollemar J, Ringden O, Andersson S, Sundberg B, Ljungman P, Sparrelid E, et al. Prophylactic use of liposomal amphotericin B (AmBisome) against fungal infections: a randomized trial in bone marrow transplant recipients. Transplant Proc. 1993;25:1495–7. [PubMed] [Google Scholar]
- 80.Tollemar J, Hockerstedt K, Ericzon BG, Sundberg B, Ringden O. Fungal prophylaxis with AmBisome in liver and bone marrow transplant recipients: results of two randomized double-blind studies. Transplant Proc. 1994;26:1833. [PubMed] [Google Scholar]
- 81.Kelsey SM, Goldman JM, McCann S, Newland AC, Scarffe JH, Oppenheim BA, et al. Liposomal amphotericin (AmBisome) in the prophylaxis of fungal infections in neutropenic patients: a randomised, double-blind, placebo-controlled study. Bone Marrow Transplant. 1999;23:163–8. doi: 10.1038/sj.bmt.1701543. [DOI] [PubMed] [Google Scholar]
- 82.Penack O, Schwartz S, Martus P, Reinwald M, Schmidt-Hieber M, Thiel E, et al. Low-dose liposomal amphotericin B in the prevention of invasive fungal infections in patients with prolonged neutropenia: results from a randomized, single-center trial. Ann Oncol. 2006;17:1306–12. doi: 10.1093/annonc/mdl128. [DOI] [PubMed] [Google Scholar]
- 83.Cordonnier C, Mohty M, Faucher C, Pautas C, Robin M, Vey N, et al. Safety of a weekly high dose of liposomal amphotericin B for prophylaxis of invasive fungal infection in immunocompromised patients: PROPHYSOME Study. Int J Antimicrob Agents. 2008;31:135–41. doi: 10.1016/j.ijantimicag.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 84.Timmers GJ, Zweegman S, Simoons-Smit AM, van Loenen AC, Touw D, Huijgens PC. Amphotericin B colloidal dispersion (Amphocil) vs fluconazole for the prevention of fungal infections in neutropenic patients: data of a prematurely stopped clinical trial. Bone Marrow Transplant. 2000;25:879–84. doi: 10.1038/sj.bmt.1702243. [DOI] [PubMed] [Google Scholar]
- 85.Gotzsche PC, Johansen HK. Nystatin prophylaxis and treatment in severely immunodepressed patients (Cochrane Review) Cochrane Database Syst Rev. 2002:CD002033. doi: 10.1002/14651858.CD002033. [DOI] [PubMed] [Google Scholar]
- 86.Buchanan AG, Riben PD, Rayner EN, Parker SE, Ronald AR, Louie TJ. Nystatin prophylaxis of fungal colonization and infection in granulocytopenic patients: correlation of colonization and clinical outcome. Clin Invest Med. 1985;8:139–47. [PubMed] [Google Scholar]
- 87.Mattiuzzi GN, Alvarado G, Giles FJ, Ostrosky-Zeichner L, Cortes J, O’Brien S, et al. Open-label, randomized comparison of itraconazole versus caspofungin for prophylaxis in patients with hematologic malignancies. Antimicrob Agents Chemother. 2006;50:143–7. doi: 10.1128/AAC.50.1.143-147.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cornely OA, Ullmann AJ, Karthaus M. Choosing a study population for the evaluation of antifungal prophylaxis. Clin Infect Dis. 2005;40:1699–701. doi: 10.1086/429823. [DOI] [PubMed] [Google Scholar]
- 89.van Burik JA, Ratanatharathorn V, Stepan DE, Miller CB, Lipton JH, Vesole DH, et al. Micafungin versus Fluconazole for prophylaxis against invasive fungal infections during Neutropenia in patients undergoing hematopoietic stem cell transplantation. Clin Infect Dis. 2004;39:1407–16. doi: 10.1086/422312. [DOI] [PubMed] [Google Scholar]
- 90.Chandrasekar PH, Gatny CM. Effect of fluconazole prophylaxis on fever and use of amphotericin in neutropenic cancer patients. Bone Marrow Transplantation Team. Chemotherapy. 1994;40:136–43. doi: 10.1159/000239184. [DOI] [PubMed] [Google Scholar]
- 91.MacMillan ML, Goodman JL, DeFor TE, Weisdorf DJ. Fluconazole to prevent yeast infections in bone marrow transplantation patients: a randomized trial of high versus reduced dose, and determination of the value of maintenance therapy. Am J Med. 2002;112:369–79. doi: 10.1016/s0002-9343(01)01127-5. [DOI] [PubMed] [Google Scholar]
- 92.Oren I, Rowe JM, Sprecher H, Tamir A, Benyamini N, Akria L, et al. A prospective randomized trial of itraconazole vs fluconazole for the prevention of fungal infections in patients with acute leukemia and hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2006;38:127–34. doi: 10.1038/sj.bmt.1705418. [DOI] [PubMed] [Google Scholar]
- 93.Mattiuzzi GN, Estey E, Raad I, Giles F, Cortes J, Shen Y, et al. Liposomal amphotericin B versus the combination of fluconazole and itraconazole as prophylaxis for invasive fungal infections during induction chemotherapy for patients with acute myelogenous leukemia and myelodysplastic syndrome. Cancer. 2003;97:450–6. doi: 10.1002/cncr.11094. [DOI] [PubMed] [Google Scholar]
- 94.Yamac K, Senol E, Haznedar R. Prophylactic use of fluconazole in neutropenic cancer patients. Postgrad Med J. 1995;71:284–6. doi: 10.1136/pgmj.71.835.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kern W, Behre G, Rudolf T, Kerkhoff A, Grote-Metke A, Eimermacher H, et al. Failure of fluconazole prophylaxis to reduce mortality or the requirement of systemic amphotericin B therapy during treatment for refractory acute myeloid leukemia: results of a prospective randomized phase III study. German AML Cooperative Group. Cancer. 1998;83:291–301. [PubMed] [Google Scholar]
- 96.Hashino S, Morita L, Takahata M, Onozawa M, Nakagawa M, Kawamura T, et al. Administration of micafungin as prophylactic antifungal therapy in patients undergoing allogeneic stem cell transplantation. Int J Hematol. 2008;87:91–7. doi: 10.1007/s12185-007-0011-1. [DOI] [PubMed] [Google Scholar]
- 97.Annaloro C, Oriana A, Tagliaferri E, Bertolli V, Della Volpe A, Soligo D, et al. Efficacy of different prophylactic antifungal regimens in bone marrow transplantation. Haematologica. 1995;80:512–7. [PubMed] [Google Scholar]
- 98.Ito Y, Ohyashiki K, Yoshida I, Takeuchi M, Aoyama Y, Mugitani A, et al. The prophylactic effect of itraconazole capsules and fluconazole capsules for systemic fungal infections in patients with acute myeloid eukemial and myelodysplastic syndromes: a Japanese multicenter randomized, controlled study. Int J Hematol. 2007;85:121–7. doi: 10.1532/IJH97.06079. [DOI] [PubMed] [Google Scholar]
- 99.Akiyama H, Mori S, Tanikawa S, Sakamaki H, Onozawa Y. Fluconazole versus oral amphotericin B in preventing fungal infection in chemotherapy-induced neutropenic patients with haematological malignancies. Mycoses. 1993;36:373–8. doi: 10.1111/j.1439-0507.1993.tb00725.x. [DOI] [PubMed] [Google Scholar]
- 100.Meunier F, Aoun M, Janssens M, Dekoster C, Paesmans M. Chemoprophylaxis of fungal infections in granulocytopenic patients using fluconazole vs oral amphotericin B. Drug Invest. 1991;3:258–65. [Google Scholar]
- 101.Takatsuka H, Takemoto Y, Okamoto T, Fujimori Y, Tamura S, Wada H, et al. Fluconazole versus amphotericin B for the prevention of fungal infection in neutropenic patients with hematologic malignancy. Drugs Exp Clin Res. 1999;25:193–200. [PubMed] [Google Scholar]
- 102.Ninane J. A multicentre study of fluconazole versus oral polyenes in the prevention of fungal infection in children with hematological or oncological malignancies. Multicentre Study Group. Eur J Clin Microbiol Infect Dis. 1994;13:330–7. doi: 10.1007/BF01974614. [DOI] [PubMed] [Google Scholar]
- 103.Groll AH, Just-Nuebling G, Kurz M, Mueller C, Nowak-Goettl U, Schwabe D, et al. Fluconazole versus nystatin in the prevention of candida infections in children and adolescents undergoing remission induction or consolidation chemotherapy for cancer. J Antimicrob Chemother. 1997;40:855–62. doi: 10.1093/jac/40.6.855. [DOI] [PubMed] [Google Scholar]
- 104.Alangaden G, Chandrasekar PH, Bailey E, Khaliq Y. Antifungal prophylaxis with low-dose fluconazole during bone marrow transplantation. The Bone Marrow Transplantation Team. Bone Marrow Transplant. 1994;14:919–24. [PubMed] [Google Scholar]
- 105.Brammer KW. Management of fungal infection in neutropenic patients with fluconazole. Haematology and Blood Transfusion. 1990;33:546–50. doi: 10.1007/978-3-642-74643-7_97. [DOI] [PubMed] [Google Scholar]
- 106.Finke R. Comparison of oral fluconazole and amphotericin B prophylaxis against fungal infections in the neutropenic phase of patients treated with antileukemic agents. Mycoses. 1990;33 (Suppl 1):42–54. [PubMed] [Google Scholar]
- 107.Lass-Flörl C, Gunsilius E, Gastl G, Englisch M, Koch G, Ulmer H, et al. Fungal colonization in neutropenic patients: a randomized study comparing itraconazole solution and amphotericin B solution. Ann Hematol. 2003;82:565–9. doi: 10.1007/s00277-003-0666-5. [DOI] [PubMed] [Google Scholar]
- 108.Harousseau JL, Dekker AW, Stamatoullas-Bastard A, Fassas A, Linkesch W, Gouveia J, et al. Itraconazole oral solution for primary prophylaxis of fungal infections in patients with hematological malignancy and profound neutropenia: a randomized, double-blind, double-placebo, multicenter trial comparing itraconazole and amphotericin B. Antimicrob Agents Chemother. 2000;44:1887–93. doi: 10.1128/aac.44.7.1887-1893.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kaptan K, Ural AU, Cetin T, Avcu F, Beyan C, Yalcin A. Itraconazole is not effective for the prophylaxis of fungal infections in patients with neutropenia. J Infect Chemother. 2003;9:40–5. doi: 10.1007/s10156-002-0207-5. [DOI] [PubMed] [Google Scholar]
- 110.Vreugdenhil G, Van Dijke BJ, Donnelly JP, Novakova IR, Raemaekers JM, Hoogkamp-Korstanje MA, et al. Efficacy of itraconazole in the prevention of fungal infections among neutropenic patients with hematologic malignancies and intensive chemotherapy. A double blind, placebo controlled study. Leuk Lymphoma. 1993;11:353–8. doi: 10.3109/10428199309067926. [DOI] [PubMed] [Google Scholar]
- 111.Böhme A, Just-Nübling G, Bergmann L, Shah PM, Stille W, Hoelzer D. Itraconazole for prophylaxis of systemic mycoses in neutropenic patients with haematological malignancies. J Antimicrob Chemother. 1996;38:953–61. doi: 10.1093/jac/38.6.953. [DOI] [PubMed] [Google Scholar]
- 112.Thunnissen PL, Sizoo W, Hendriks WD. Safety and efficacy of itraconazole in prevention of fungal infections in neutropenic patients. Neth J Med. 1991;39:84–91. [PubMed] [Google Scholar]
- 113.Tricot G, Joosten E, Boogaerts MA, Vande Pitte J, Cauwenbergh G. Ketoconazole vs. itraconazole for antifungal prophylaxis in patients with severe granulocytopenia: preliminary results of two nonrandomized studies. Rev Infect Dis. 1987;9 (Suppl 1):S94–9. doi: 10.1093/clinids/9.supplement_1.s94. [DOI] [PubMed] [Google Scholar]
- 114.Lamy T, Bernard M, Courtois A, Jacquelinet C, Chevrier S, Dauriac C, et al. Prophylactic use of itraconazole for the prevention of invasive pulmonary aspergillosis in high risk neutropenic patients. Leuk Lymphoma. 1998;30:163–74. doi: 10.3109/10428199809050939. [DOI] [PubMed] [Google Scholar]
- 115.Todeschini G, Murari C, Bonesi R, Pizzolo G, Amaddi G, Ambrosetti A, et al. Oral itraconazole plus nasal amphotericin B for prophylaxis of invasive aspergillosis in patients with hematological malignancies. Eur J Clin Microbiol Infect Dis. 1993;12:614–8. doi: 10.1007/BF01973640. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.