Abstract
Objective
To examine the effectiveness of day hospital attendance in prolonging independent living for elderly people.
Design
Systematic review of 12 controlled clinical trials (available by January 1997) comparing day hospital care with comprehensive care (five trials), domiciliary care (four trials), or no comprehensive care (three trials).
Subjects
2867 elderly people.
Main outcome measures
Death, institutionalisation, disability, global “poor outcome,” and use of resources.
Results
Overall, there was no significant difference between day hospitals and alternative services for death, disability, or use of resources. However, compared with subjects receiving no comprehensive care, patients attending day hospitals had a lower odds of death or “poor” outcome (0.72, 95% confidence interval 0.53 to 0.99; P<0.05) and functional deterioration (0.61, 0.38 to 0.97; P<0.05). The day hospital group showed trends towards reductions in hospital bed use and placement in institutional care. Eight trials reported treatment costs, six of which reported that day hospital attendance was more expensive than other care, although only two analyses took into account cost of long term care.
Conclusions
Day hospital care seems to be an effective service for elderly people who need rehabilitation but may have no clear advantage over other comprehensive care. Methodological problems limit these conclusions, and further randomised trials are justifiable.
Key messages
The benefits of geriatric day hospital care have been controversial for many years
This systematic review of 12 randomised trials comparing a variety of day hospitals with a range of alternative services found no overall advantage for day hospital care
Day hospitals had a possible advantage over no comprehensive care in terms of death or poor outcome, disability, and use of resources
The costs of day hospital care may be partly offset by a reduced use of hospital beds and institutional care among survivors
Introduction
Geriatric day hospitals developed rapidly in the United Kingdom in the 1960s as an important component of care provision. The model has since been widely applied in several Western countries. Day hospitals provide multidisciplinary assessment and rehabilitation in an outpatient setting and have a pivotal position between hospital and home based services. Although there is considerable descriptive literature on day hospital care,1 concern has been expressed that evidence for effectiveness is equivocal and that day hospital care is expensive.2 We therefore undertook a systematic review of the randomised trials of day hospital care.
Methods
The primary question addressed was whether older patients attending a day hospital would experience better outcomes than those receiving alternative forms of care. We anticipated considerable heterogeneity in both the intervention and control services and so specified key subgroup comparisons before reviewing the trials.
Inclusion criteria
We set out to identify all relevant controlled clinical trials of geriatric day hospital care. A day hospital was defined as an outpatient facility where older patients attend for a full or near full day and receive multidisciplinary rehabilitation in a health care setting.3 Trials evaluating social day centres, other types of day hospitals such as those for patients with dementia or psychiatric conditions, and single condition day hospitals were excluded.
Search strategy
We searched for relevant published and unpublished papers up to January 1997. Our search strategy included Medline, SIGLE (System for Information on Grey Literature in Europe), BIDS (Bath Information and Data Services), CINAHL (Cumulative Index to Nursing and Allied Health), and the Cochrane Library. Key search terms included day hospital, day care, ambulatory care, and outpatient clinic. We also searched Index Medicus, British and international dissertation abstracts, conference abstracts (Society for Research in Rehabilitation, British Geriatrics Society), bibliographies of known trials, and other relevant articles and books. We publicised our work through presentations at geriatric symposia and by contacting authors of previous articles on day hospital care.
Study appraisal and extraction of data
We selected outcomes to reflect a previous definition of the purpose of day hospital care: “to facilitate and prolong independent living for the elderly in the community.”4 Thus death, the need for institutional care, disability, hospital use, and resource use were selected as quantitative outcomes. In anticipation of incomplete data we also defined a global “poor outcome” comprising death or one of the following (in order of preference): resident in institutional care, severe disability at end of follow up, or deterioration in physical function during follow up. The research reports were independently assessed by three reviewers to establish eligibility, agree subcategories for the trials based on the treatment comparison, and to extract data.
Statistical methods
When possible, studies were analysed on an intention to treat basis. Surviving authors were contacted and asked to supply additional information when necessary. Patients who were lost to follow up or for whom outcome data were not available were excluded from the initial analysis. However, they were included in “best case” (all missing data in favour of day hospital care), “neutral” (all missing data recorded at the average event rate for the trial), and “worst case” (all missing data in favour of alternative care) sensitivity analyses.
We calculated odds ratios (with 95% confidence intervals) for the dichotomous outcomes using standard methods. A fixed effects approach5 was used initially and, if substantial heterogeneity was present, we confirmed this with a random effects approach.6 Outcomes were recorded at the end of scheduled follow up.
Results
We identified 703 abstracts, of which 687 were not relevant to the review or of descriptive studies. Sixteen evaluated a service fulfilling our definition of geriatric day hospital care. This analysis includes 12 trials which recruited 2867 subjects.7–18 Of the remaining four trials, one has just completed (J Baskett, personal communication); two did not include a random or quasirandom allocation procedure,19,20 and one was excluded because day hospital attendance was only one component of a complex multiple service intervention.21 Details of randomisation procedures, treatment schedules, and numbers of patients followed up are given on the BMJ website.
Multidisciplinary outpatient rehabilitation was available at all the day hospital sites. Comparison groups comprised comprehensive elderly care (a range of inpatient, outpatient, and domiciliary geriatric medical services)9,10,12,13,15; domiciliary care (therapy provided in the patient’s home11,14,16 or day centre18); and no comprehensive elderly care (patients who were eligible for, but not referred to, existing services).7,8,17 For the trial by Gladman et al,16 only patients in the health care of the elderly strata have been included as the random treatment allocation of these patients included day hospital care.
Patient characteristics
One study was run by the Department of Veterans Affairs in the United States and was exceptional in that the sample was 96% male.15 In all trials the mean age of participants was at least 65 years and usually over 70 years. Three trials14,16,17 recruited only stroke patients, but the rest had a mixed population. Most patients had significant disability on a variety of scales.
Outcome data
Details on deaths were published, or provided on request, for all trials. Information about institutionalisation was published in only four studies7,9,13,16; additional data were provided by the authors for a further six studies.11,12,14,15,17,18 Data were also available concerning some aspect of disability (11 trials) and use of hospital beds (12 trials).
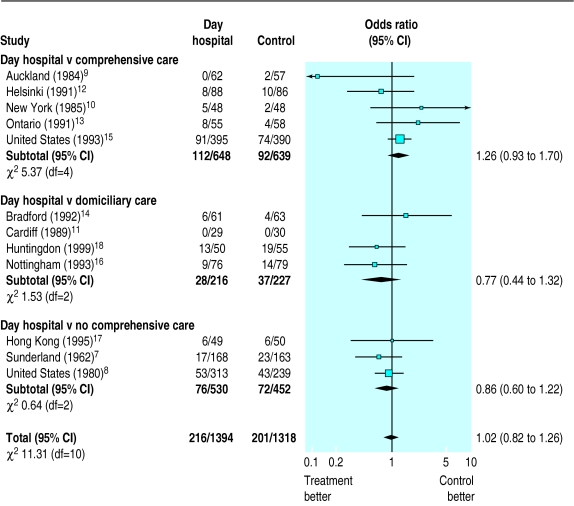
No significant differences in numbers of deaths occurred between patients attending day hospitals and those receiving any of the alternative services (fig 1). The pooled odds ratio for death was 1.02 (95% confidence interval 0.82 to1.26). There was no significant heterogeneity between the results of individual trials or categories of trials.
Figure 1.
Deaths among patients receiving day hospital care or alternative services. Odds ratios of death by end of follow up were calculated by fixed effects model. Heterogeneity between trials is presented as χ2
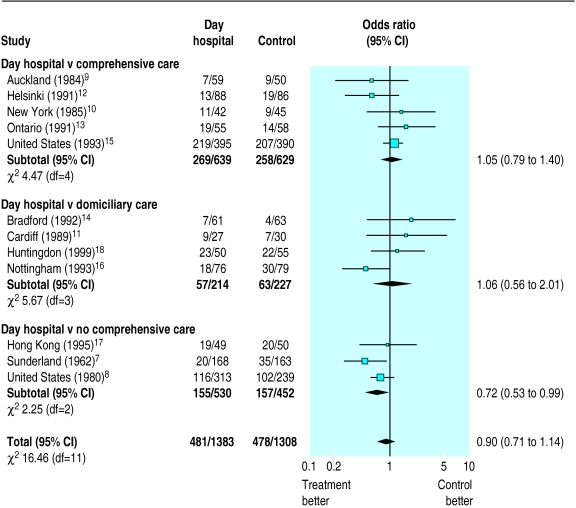
Figure 2 shows that overall there was no significant difference between day hospital and alternative forms of care in preventing death or a “poor” outcome at final follow up (odds ratio 0.90, 0.71 to 1.14; random effects model). However, patients attending day hospitals were less likely to have poor outcome than those receiving no comprehensive care (0.72, 0.53 to 0.99; P<0.05).
Figure 2.
Odds of death or poor outcome in patients receiving day hospital care or alternative services (random effects model). Heterogeneity between trials is presented as χ2
Sensitivity analyses
Sensitivity analyses indicated that excluding trials with uncertain or insecure randomisation procedures would not substantially affect our conclusions.8,10,12 Data were missing on death for 155 (6%) patients and on death or poor outcome for 174 (7%). Best case and worst case sensitivity analyses include significant benefit (P<0.001) or harm (P<0.05) from day hospital care. The most plausible (neutral) sensitivity analysis suggested no effect on death (odds ratio 1.02, P>0.05) or death and poor outcome (0.92, P>0.2).
Disability
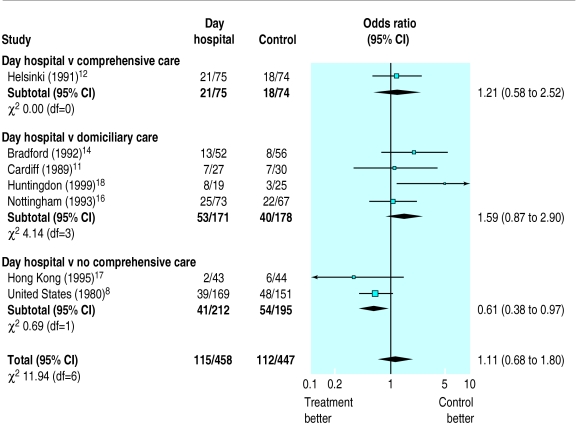
Eleven of the trials included a standardised measurement of activities of daily living,8–18 but seven different measures were used which could not be combined in a statistical summary. Seven trials8,11,12,14,16–18 provided data on 905 survivors (data missing for 65, 7%) whose disability scores were monitored during follow up (fig 3). Overall, day hospital patients had a similar chance as controls of suffering deteriorating function (1.11, 0.68 to 1.80; random effects model) but tended to have better outcomes than those receiving no comprehensive care (0.61, 0.38 to 0.97; P<0.05).
Figure 3.
Deterioration in activities of daily living among survivors allocated to day hospital care or alternative services (random effects model). Heterogeneity between trials is presented as χ2
Use of resources
Institutional care
—Eleven trials provided information about the number of patients requiring institutional care at the end of follow up. Overall, there was a trend towards fewer day hospital patients requiring long term (median follow up 12 months) institutional care than those receiving alternative services (table) and the difference was significant in comparison with no comprehensive care.
Use of hospital beds
—Average hospital bed use per patient recruited could be calculated for all the trials, but a measure of variance could not be obtained and therefore we cannot report confidence intervals. The table shows a small reduction in bed use by day hospital patients across all trials (15.0 v 16.4 days).
Costs
—Eight trials compared treatment costs, only two of which included costs of nursing home care.10,15 Six reported that day hospital care was more expensive than the comparison treatment,8,9,15,18,22,23 and two trials reported that the costs were similar.10,17
Discussion
Geriatric day hospitals have several functions, but rehabilitation has been regarded as most important1 and was the focus for this systematic review. We selected outcomes to reflect a definition of the core purpose of a geriatric day hospital.4 We used a predetermined definition of day hospital care3 and identified and categorised comparison services before collecting and analysing data. We excluded day hospitals for patients with specific conditions such as mental illness, dementia, or rheumatoid arthritis.
Limitations of the review
The main limitations of our review lie in the 30 years over which the trials were done, during which health and social care policies will inevitably have changed, and in the multinational location of the studies. Nevertheless, our data provide the best evidence available on which to judge the effectiveness of day hospitals.
A further problem is the limitations of the trials themselves, in particular the lack of statistical power resulting from small, heterogeneous trials. This raises the possibility of false positive and false negative results. Furthermore, the amount of missing outcome data adds uncertainty to most of our conclusions.
Publication bias remains a possibility, but our search strategy was extensive and included contacting authors of papers on day hospital care around the world. Many of the authors were able to provide unpublished additional information. A funnel plot analysis24 did not show any major evidence of missing data.
Findings
A big problem was that most trials compared day hospital care with an alternative “active” control. Only three trials7,8,17 used a comparison group of patients who received neither comprehensive care nor domiciliary rehabilitation. Compared with patients receiving no comprehensive care, patients attending day hospitals had less functional deterioration and institutional care and a small reduction in average hospital bed use. However, there was considerable loss to follow up in these three trials.
When day hospital services were compared with comprehensive elderly care (integrated inpatient, outpatient, and domiciliary services), the outcomes were largely similar. One interpretation is that day hospitals are comparable with an alternative service for which there is considerable evidence of effectiveness.25 However, the question arises whether day hospitals provide additional benefits when other comprehensive elderly care services are already in place. Our systematic review does not directly address this question.
We focused on a few specified outcomes, but many other important outcome domains, including patient preference and instrumental daily living activities, could not be examined as these outcomes were not widely available. It was also difficult to determine a summary statistic for disability because different measurement instruments were used and analysed in different ways. Moreover, commonly used measures of disability may be insensitive to change in the outpatient setting of a day hospital.26 This may explain why six trials reported no significant difference in disability outcome between day hospital and comparison services. Future trials should incorporate measures of intrumental activities of daily living as a more relevant and sensitive outcome.
Our analysis suggests that attending day hospital may reduce patients’ use of hospital and institutional care resources. However, costing studies need to balance any possible savings with the direct costs of day hospital care. Several studies have drawn attention to the expense of day hospital services.22,23 For six of the eight trials reporting cost information, day hospital care was more expensive than the alternative treatment.
On the whole, the trials we included took a pragmatic design approach and attempted to address a broad question of overall efficacy of day hospitals. Given the diversity of patients attending day hospitals and the corresponding diversity of interventions used, future trials need to be large multicentre trials or should examine more focused questions.
Supplementary Material
Table.
Numbers of patients receiving institutional care at the end of scheduled follow up and use of hospital beds among those allocated to day hospital or alternative services
| Institutional care
|
Bed use (days)
|
|||||
|---|---|---|---|---|---|---|
| Control group | Day hospital | Control | Odds ratio (95% CI) | Day hospital | Control | |
| Comprehensive care (5 trials) | 151/597* | 159/584 | 0.91 (0.70 to 1.19) | 20.5 | 21.4 | |
| Domiciliary care (4 trials) | 20/216 | 19/227 | 1.61 (0.30 to 8.55) | 7.7 | 11.1 | |
| No comprehensive care (3 trials) | 37/411 | 66/403 | 0.50† (0.26 to 0.96) | 11.2 | 11.7 | |
| Total | 208/1224 | 244/1214 | 0.77 (0.52 to 1.13) | 15.0 | 16.4 | |
Data not available for 1 trial.
P<0.05 (random effects model).
Acknowledgments
An expanded version of this review has been submitted for publication in the Cochrane Library.
Footnotes
Funding: NHS Executive Northern and Yorkshire Region, Stroke Association.
Competing interests: None declared.
References
- 1.Research Unit of the Royal College of Physicians and British Geriatric Society. Geriatric day hospitals: their role and guidelines for good practice. London: RCP; 1994. [Google Scholar]
- 2.National Audit Office. National health service day hospitals for elderly people in England. London: HMSO; 1994. [Google Scholar]
- 3.Siu AL, Morishita L, Blaustein J. Comprehensive geriatric assessment in a day hospital. J Am Ger Soc. 1994;42:1094–1099. doi: 10.1111/j.1532-5415.1994.tb06215.x. [DOI] [PubMed] [Google Scholar]
- 4.Donaldson C, Wright KG, Maynard AK, Hamill JD, Sutcliffe E. Day hospitals for the elderly: utilisation and performance. Community Med. 1987;9:55–61. doi: 10.1093/oxfordjournals.pubmed.a043906. [DOI] [PubMed] [Google Scholar]
- 5.Peto R. Why do we need systematic overviews of randomized trials? Stat Med. 1987;6:233–240. doi: 10.1002/sim.4780060306. [DOI] [PubMed] [Google Scholar]
- 6.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 7.Woodford-Williams E, McKeon JA, Trotter IS, Watson D, Bushby C. The day hospital in the community care of the elderly. Gerontology Clinic. 1962;4:241–256. doi: 10.1159/000244750. [DOI] [PubMed] [Google Scholar]
- 8.Weissert W, Wan T, Livieratos B, Katz S. Effects and costs of day-care services for the chronically ill: a randomized experiment. Medical Care. 1980;18:567–584. doi: 10.1097/00005650-198006000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Tucker MA, Davison JG, Ogle SJ. Day hospital rehabilitation—effectiveness and cost in the elderly: a randomised controlled trial. BMJ. 1984;289:1209–1212. doi: 10.1136/bmj.289.6453.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cummings V, Kerner JF, Arones S, Steinbock C. Day hospital service in rehabilitation medicine: an evaluation. Arch Phys Med Rehabil. 1985;66:86–91. [PubMed] [Google Scholar]
- 11.Vetter NJ, Smith A, Sastry D, Tinker G. Day hospital pilot study report. Cardiff : Department of Geriatrics, St David’s Hospital; 1989. [Google Scholar]
- 12.Pitkala K, Winell K, Tilvis RS. Effects of geriatric day hospital care for home care patients. Arch Gerontol Geriatric. 1991;suppl 2:51–54. [Google Scholar]
- 13.Eagle DJ, Guyatt GH, Patterson C, Turpie I, Sackett B, Singer J. Effectiveness of a geriatric day hospital. Can Med Assoc J. 1991;144:699–704. [PMC free article] [PubMed] [Google Scholar]
- 14.Young JB, Forster A. The Bradford community stroke trial: results at six months. BMJ. 1992;304:1085–1089. doi: 10.1136/bmj.304.6834.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Branch LG, editor. Adult day health care evaluation study. Medical Care. 1993;31(suppl):SS1–124. [PubMed] [Google Scholar]
- 16.Gladman JRF, Lincoln NB, Barer DH. A randomised controlled trial of domiciliary and hospital-based rehabilitation for stroke patients after discharge from hospital. J Neurol Neurosurg Psychiatry. 1993;56:960–966. doi: 10.1136/jnnp.56.9.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hui E, Lum CM, Woo J, Or KH, Kay RLC. Outcomes of elderly stroke patients day hospital versus conventional medical management. Stroke. 1995;26:1616–1619. doi: 10.1161/01.str.26.9.1616. [DOI] [PubMed] [Google Scholar]
- 18.Burch S, Longbottom J, McKay M, Borland C, Prevost T. A randomised controlled trial of day hospital and day centre therapy. Clin Rehab (in press). [DOI] [PubMed]
- 19.Weiler PG, Kim P, Pickard LS. Health care for elderly Americans: evaluation of an adult day health care model. Medical Care. 1976;14:700–708. doi: 10.1097/00005650-197608000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Sherwood S, Morris JN, Ruchlin HS. Alternative paths to long-term care: nursing home, geriatric day hospital, senior center, and domiciliary care options. Am J Public Health. 1986;76:38–44. doi: 10.2105/ajph.76.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Skellie FA, Mobley GM, Coan RE. Cost-effectiveness of community-based long-term care: current findings of Georgia’s alternative health services project. Am J Public Health. 1982;72:353–358. doi: 10.2105/ajph.72.4.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Young J, Forster A. Day hospital and home physiotherapy for stroke patients: a comparative cost-effectiveness study. J R Coll Phys Lond. 1993;27:252–257. [PMC free article] [PubMed] [Google Scholar]
- 23.Gladman J, Whynes D, Lincoln N. Cost comparison of domiciliary and hospital-based stroke rehabilitation. Age Ageing. 1994;23:241–245. doi: 10.1093/ageing/23.3.241. [DOI] [PubMed] [Google Scholar]
- 24.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet. 1993;342:1032–1036. doi: 10.1016/0140-6736(93)92884-v. [DOI] [PubMed] [Google Scholar]
- 26.Parker SG, Du X, Bardsley MJ, Goodfellow J, Cooper RG, Cleary R, et al. Measuring outcomes in care of the elderly. J R Coll Phys Lond. 1994;28:428–433. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.