Abstract
Summary: Francisella tularensis is a facultative intracellular gram-negative pathogen and the etiological agent of the zoonotic disease tularemia. Recent advances in the field of Francisella genetics have led to a rapid increase in both the generation and subsequent characterization of mutant strains exhibiting altered growth and/or virulence characteristics within various model systems of infection. In this review, we summarize the major properties of several Francisella species, including F. tularensis and F. novicida, and provide an up-to-date synopsis of the genes necessary for pathogenesis by these organisms and the determinants that are currently being targeted for vaccine development.
INTRODUCTION
Francisella tularensis is a gram-negative coccobacillus that has an exceedingly low infectious dose. It is a category A select agent and is one of the most infectious bacteria known. Following the terrorist attacks of 2001 and subsequent anthrax mailings in the fall of that year, there has been a renewed interest in the study of this organism. Advancements in the field of F. tularensis genetics have lead to a dramatic expansion in the generation of mutant strains of various F. tularensis subspecies. Collectively, this has led to an improved understanding of F. tularensis biology, host responses to infection, and virulence factors required for infection and/or disease elicitation. Many investigators in this field have focused on the development of a vaccine capable of protecting against the most virulent biovars of F. tularensis. Of particular interest are those providing substantive protection against type A strains delivered by the respiratory route. Here, we review the major characteristics of F. tularensis and provide an update regarding genes required for pathogenesis and determinants being targeted for vaccine development.
FRANCISELLA TULARENSIS AND TULAREMIA
Classification
Francisella tularensis is one of the most infectious and pathogenic bacteria known. It is the etiological agent of the debilitating febrile illness tularemia. The bacterium is a gram-negative, capsulated, facultative intracellular pathogen and is one of the members of the genus Francisella of the Gammaproteobacteria class. Francisella has no close pathogenic relatives but exists in a sister clade with the arthropod endosymbiont Wolbachia persica. It is also distantly related to human pathogens Coxiella burnetii and Legionella pneumophila (109). F. tularensis is commonly classified into three subspecies, F. tularensis subsp. tularensis, F. tularensis subsp. holarctica, and F. tularensis subsp. mediasiatica, based on genetic makeup, virulence, ability to produce acid from glycerol, and citrulline ureidase activity (49) (Table 1). Francisella novicida is also often considered a subspecies of F. tularensis; however, recent whole-genome single-nucleotide polymorphism analysis indicates that it is likely an independent species (104). F. tularensis subsp. tularensis and F. tularensis subsp. holarctica are the primary biovars associated with disease in humans. F. tularensis subsp. tularensis, also known as type A Francisella, is found primarily in North America and is highly virulent in humans. This subspecies is responsible for roughly 70% of Francisella disease cases in North America (186). Type A strains have an infectious dose of <10 CFU in humans (174, 175) and can lead to life-threatening illness, particularly when infection occurs via the respiratory route. Molecular subtyping techniques indicate that F. tularensis subsp. tularensis can be further divided into two genetically distinct clades (A.I and A.II) that differ with respect to disease outcome, transmission, and geographic location (59, 98, 104, 187, 194). F. tularensis subsp. holarctica, or type B strains, is found throughout much of the Northern Hemisphere and is the primary cause of tularemia in Europe (141). These organisms have an infectious dose of <103 CFU and cause a milder form of tularemia in humans. The live vaccine strain (LVS) that was developed in the former Soviet Union and gifted to the United States in the 1950s is a human-attenuated type B derivative. F. tularensis subsp. mediasiatica and F. novicida are focally distributed and are rarely associated with disease in humans. F. tularensis subsp. mediasiatica is primarily isolated to central Asian regions of the former USSR, while F. novicida is found in North America and Australia (57, 141, 147). F. novicida has been extensively studied as a model organism in the laboratory setting due to its enhanced genetic tractability relative to other subspecies and its relative avirulence in humans. All F. tularensis subspecies are highly pathogenic in animal models, particularly in rabbits and mice. F. novicida is also highly pathogenic in mice, but its virulence remains less characterized outside this model system.
TABLE 1.
Characteristics of Francisella speciesa
| Species or subspecies | LD50 (CFU) in: |
Straind | Accession no. | Length (bp) | No. of: |
||
|---|---|---|---|---|---|---|---|
| Miceb | Humansc | Genes | Pseudogenese | ||||
| F. tularensis subsp. tularensis | <10 | <10 | Schu S4 | NC 006570 | 1,892,819 | 1,852 | 201 |
| FSC198 | NC 008245 | 1,892,616 | 1,852 | 199 | |||
| WY96-3418 | NC 009257 | 1,898,476 | 1,872 | 0 | |||
| F. tularensis subsp. holarctica | <10 | <103 | LVS | NC 007880 | 1,895,994 | 2,020 | 213 |
| OSU18 | NC 008369 | 1,895,727 | 1,932 | 328 | |||
| FTNF002-00 | NC 009749 | 1,890,909 | 1,887 | 2 | |||
| F. tularensis subsp. mediasiatica | NRf | NR | FSC147 | NC 010677 | 1,893,886 | 1,750 | 297 |
| F. novicida | <10 | >103 | U112 | NC 008601 | 1,910,031 | 1,781 | 14 |
Adapted from Table 1 in reference 140 with kind permission from Springer Science + Business Media (© Springer 2005) and from reference 203 with kind permission of Wiley-Blackwell.
Doses delivered subcutaneously.
Estimated LD based on virulence in animal models and case studies.
Several additional Francisella isolates are currently being sequenced, including F. tularensis subsp. tularensis (strains MA00-2987 [NZ ABRI00000000] and FSC033 [NZ AAYE00000000]), F. tularensis subsp. holarctica (strains FSC200 [NZ AASP00000000], FSC022 [NZ AAYD00000000], and 257 [NZ AAUD00000000], and F. novicida (strains FTG [NZ ABXZ00000000], FTE [NZABSS00000000], GA99-3548 [NZ ABAH00000000], and GA99-3549 [NZ AAYF00000000]).
Refers to sequences resembling functional genes but thought to have lost protein-coding capability.
NR, doses have not been reported.
Comparative Genomics
There are currently eight completely sequenced Francisella genomes (Table 1) and an additional nine genomes for which shotgun sequencing is currently under way. Sequence analysis of F. tularensis subsp. tularensis (FSC198 [NC 008245], Schu S4 [NC 006570], and WY96-3418 [NC 009257]), F. tularensis subsp. holarctica (FTNF002-00 [NC 009749], OSU18 [NC 008369], and LVS [NC 067880]), F. tularensis subsp. mediasiatica (FSC147 [NC 010677]), and F. novicida (U112 [NC 008601]) indicates that these strains are highly similar at the genetic level. The genome of each strain is roughly 1.8 Mb, with F. novicida U112 having the largest genome at 1.91 Mb. All genomes have a G+C content of approximately 32%, with between 1,800 and 2,000 putative coding sequences depending on the subspecies and strain. Between 70 and 90% of open reading frames within these isolates are predicted to code for functional proteins. Interestingly, the more virulent subspecies, F. tularensis subsp. tularensis and F. tularensis subsp. holarctica, contain roughly 200 to 300 pseudogenes, depending on the strain, while the less pathogenic F. novicida U112 contains only 14 pseudogenes (109, 203). Additionally, nearly 30% of annotated genes within an F. tularensis isolate are characterized as hypothetical proteins with unknown function, suggesting that Francisella is likely to encode novel virulence determinants. A 30-kb region with low G+C content (27.5%) that is unique to Francisella among the 17 gammaproteobacterial genomes exists in duplicate in type A and B strains of F. tularensis but is present in single copy in F. novicida. This locus has been identified as a pathogenicity island and is required for aspects of F. tularensis survival within host cells.
Comparative genomic studies have indicated that there is a high level of nucleotide identity between and within F. tularensis subspecies, ranging from roughly 97% to 99%. Despite this, there are numerous DNA rearrangements present between subspecies, particularly between type A and type B strains, and among different type A strains (148). These rearranged sequences are flanked by repeated DNA insertion sequence elements, indicating that they likely evolved from homologous recombination events. In contrast, little genomic reorganization is observed in type B strains. Though the precise impact of these rearrangements remains unclear, it is of note that they exist primarily in the more virulent type A strains.
Comparisons of deletion events, repeat sequences, and single-nucleotide polymorphisms between sequenced Francisella genomes have provided important insights into the evolution of these organisms. The presence of conserved genomic deletion events and single-nucleotide variations in F. tularensis and F. novicida isolates suggest that these species have evolved vertically, with F. novicida being the most ancestral. Additionally, the highly virulent type A strains appeared before the less virulent type B strains (59). The reduced genomic heterogeneity of type B strains compared with type A strains and the recovery of type B strains from around the world indicate that F. tularensis subsp. holarctica has evolved recently and spread rapidly (59). The evolution of F. tularensis from a common ancestor appears to have resulted from both a loss and a gain of genetic information over time, as type A strains have undergone a reduction in their genomic content relative to F. novicida, but type B strains contain additional genomic content that is otherwise absent from their type A counterparts. These observations indicate either that rearrangements occurred in type A Francisella after type A and B strains diverged evolutionarily or that type B strains were derived from one type A strain that lost the ability to undergo such rearrangements (148).
Epidemiology of F. tularensis
Though its primary environmental niche remains unknown, F. tularensis has a broad and complex host distribution, infecting a number of wildlife species, including lagomorphs, rodents, insectivores, carnivores, ungulates, marsupials, birds, amphibians, fish, and invertebrates (14, 18, 136, 196). F. tularensis is most frequently found in rodents, hares, and rabbits; however, these are unlikely reservoirs for F. tularensis, considering that infection often leads to acute disease in these animals. It has also been suggested that protozoa may play a role as hosts in aquatic cycles, which is supported by the demonstration of F. tularensis in amoebal cysts (2, 111, 141, 202). Finally, although most arthropod vectors serve only as transient hosts, F. tularensis may be transmitted by ticks throughout their life cycle, raising the possibility that a single tick may infect multiple hosts (90, 149).
A primary route of F. tularensis transmission to humans and other animals is through arthropod vectors such as ticks, biting flies, and possibly mosquitoes. Infection by F. tularensis can also occur through direct contact with contaminated water, food supplies, or infected animals (49). F. tularensis is occasionally acquired by inhalation of organisms that have been aerosolized through disruption of contaminated materials. For these reasons, high-risk groups include hunters or trappers, who might come into contact with infected animals, and landscapers, who may encounter aerosolized organisms through mechanical disruption of contaminated soil or animal carcasses. Though F. tularensis organisms are readily aerosolized, transmission via human-to-human contact has yet to be reported.
F. tularensis-mediated disease was first recognized as a plague-like illness in rodents during an outbreak in Tulare County, CA, in 1911, resulting in the first isolation of the bacterium (70). Three years later, human disease caused by F. tularensis in two patients in Ohio who had recent contact with wild rabbits was described (215). In 1919, Edward Francis established that a number of clinical symptoms were specifically caused by “Bacterium tularense,” named for the county in which the disease was found to be endemic, and the name “tularemia” was subsequently used to describe them (68, 70). Tularemia has been referred to as “rabbit fever,” “market men's disease,” and “meat-cutter's disease,” all named for the frequent incidence of disease associated with dressing rabbits for meat. The terms “deer-fly fever” and “glandular type of tick fever” have also been used to describe tularemia in the context of symptoms arising from a tick or fly bite resulting in a noted enlargement of lymph nodes. Identification of symptoms and potential sources led to the subsequent accumulation of tularemia reports in the United States, with roughly 14,000 cases reported by 1945 (96) and a peak incidence of 2,291 cases in 1939 (60, 183). Concurrently, reports of a similar disease were emerging from Japan and Russia. Large waterborne outbreaks in the 1930s and 1940s further solidified the epidemic potential of this organism and prompted further investigation into the characteristics of F. tularensis. The largest recorded tularemia outbreak occurred via airborne transmission of the European biovar F. tularensis subsp. holarctica and involved more than 600 individuals between 1966 and 1967 in a farming area of Sweden (45). In this case, most individuals acquired tularemia while doing farm work that created aerosols, such as sorting hay.
Today, the worldwide occurrence of human tularemia is likely underestimated and underreported due to the generic nature of the disease symptoms. It is well established that natural tularemia outbreaks are typically highly localized, with areas of endemicity often encompassing only a few hundred square kilometers. Outbreaks of tularemia often occur in parallel with outbreaks in rodents, hares, rabbits, and other small mammals (196). Tularemia is known to be dispersed throughout much of the Northern Hemisphere, particularly in parts of North America, Europe, and northern Asia (57, 91). There have been reports of human tularemia in every state in the United States except Hawaii, with a localization of most cases to south-central and western states (18, 24a, 48). Overall, reported cases of tularemia have dropped from several thousand per year prior to 1950 to fewer than 200 in the 1990s (18, 24a, 48). Cases are typically sporadic or occur in small clusters during June through September, correlating with the incidence of arthropod-borne transmission (18, 48, 58). A summary of a number of tularemia reports during the 1980s in the United States revealed that 63% of infected individuals reported an attached tick, and 23% reported contact with wild rabbits (197). The most recent major incident involving F. tularensis in the United States occurred on Martha's Vineyard in 2000 and involved 15 patients with one fatality; 11 of the patients had acquired pneumonic tularemia (61). Many of those infected were landscapers, and it is speculated that lawn mowing or brush cutting was a major risk factor (61). Though less numerous, reports of tularemia continue to arise from Martha's Vineyard annually, with landscapers representing a majority of the infected. Most tularemia reports in Europe are from the northern and central countries, particularly Scandinavian countries (196). Disease in many of these countries occurs in an uneven geographical distribution, with high percentages of reports coming from localized rural regions. Furthermore, a strain similar to Francisella novicida was recently isolated from a patient in Australia, indicating that the geographic distribution of Francisella is likely more widespread than previously reported (216).
Tularemia
Tularemia is an acute febrile illness, the type and severity of which depend on the route of infection and the infecting biovar. F. tularensis can infect humans through the skin, mucous membranes, gastrointestinal tract, and respiratory tract. Major target organs include the lymph nodes, lungs, spleen, liver, and kidneys (58, 69, 116, 154, 190). Infection acquired through the skin or mucous membranes results in ulceroglandular tularemia, which comprises up to 90% of all cases (195). Ulceroglandular tularemia results from direct contact of the organism with the skin, often while handling infected animals or animal tissues or as a result of vector-borne transmission. A primary ulcer develops at the infection site, followed by painful swelling of the nearby lymph nodes. After an incubation period that can last up to 21 days, there is a rapid onset of high fever accompanied by flu-like symptoms. F. tularensis may further disseminate to and replicate in other organs in the body, particularly the lungs, liver, and spleen. Ulceroglandular tularemia has a mortality rate of less than 5% (58), though dissemination and replication within the lung may lead to a more serious respiratory disease. Inhalation of live organisms or accumulation of organisms in the lung following dissemination from other infection routes often leads to respiratory tularemia, the most severe form of the disease. Outbreaks resulting from respiratory transmission are rare but can involve a large number of cases, depending on the mechanism of dispersion. Symptoms for respiratory tularemia can be somewhat variable. While inhalation of F. tularensis subsp. holarctica results in a mild and generally non-life-threatening respiratory infection, inhalation of F. tularensis subsp. tularensis results in an acute, serious infection that presents with a high fever, chills, malaise, and cough. Organisms deposited into the lung readily spread to the draining lymph nodes and further disseminate to the liver and spleen, where severe inflammation and tissue damage can occur. Tularemia resulting from respiratory infection of type A Francisella has mortality rates approaching 30% to 60% if untreated (50, 174, 175). However, the fatality rate is reduced to less than 2% when antibiotics are administered in a timely fashion (58). Other, less common forms of the disease include oculoglandular tularemia, which results from direct contact of organisms with the eye, accounting for 1% to 4% of all cases (141). Ingestion of food or water contaminated with F. tularensis may also cause oropharyngeal and/or gastrointestinal tularemia, which is the least common form of the disease. Typhoidal tularemia is a term used to describe infection with severe systemic symptoms without regional ulcerations or swollen lymph nodes indicative of a site of inoculation (49). Though less common, these additional disease forms highlight the ability of Francisella to infect humans via multiple routes.
Potential as a Biological Weapon
F. tularensis has long been considered a potential biological weapon based on its ability to cause severe disease upon inhalation of doses as low as 10 CFU (174). The biological weapons programs in several countries, including Japan, the former Soviet Union, and the United States, developed weapons containing F. tularensis (49, 87). In the 1960s, F. tularensis was one of a number of agents stockpiled by the United States military as part of a biological weapons development program that was eventually terminated by executive order in 1970 (30). Despite efforts to disengage biological weapons programs around the world, former Soviet Union biological weapons senior scientist Ken Alibeck reported that weaponization efforts occurred in the Soviet Union well into the 1990s (3). In light of recent world events, the extreme infectivity and the ability to potentially disseminate aerosolized organisms over an urban area continue to drive concerns regarding Francisella weaponization and/or intentional release. In 1969, a report from a World Health Organization committee assessed the bioweapon threat of F. tularensis. It estimated that an aerosol release of 50 kg of F. tularensis over an urban area with a population of nearly 5 million individuals would result in 250,000 incapacitating casualties and 19,000 deaths (220a). More recently, the Centers for Disease Control and Prevention (CDC) estimated that the total base costs to society resulting from such an attack would approach $5.4 billion for every 100,000 persons exposed (102). In the event of an intentional release of F. tularensis, it is likely that prompt treatment of at-risk individuals would dramatically reduce the impact of the event.
F. TULARENSIS PATHOGENESIS
The success of Francisella as a pathogen is intimately associated with its ability to survive and replicate within a wide variety of host cell types. Upon entering a mammalian host, Francisella is known to target macrophages. However, it has become increasingly clear that these organisms can infect and survive in a number of additional cell types, including dendritic cells, neutrophils, hepatocytes, and lung epithelial cells. While the importance of these cell types to infection is not completely understood, it is well documented that Francisella replicates within mononuclear phagocytes in vivo and exhibits a disease cycle within these cells that appears to differ little between strains or subspecies.
Intracellular Life Cycle of F. tularensis in Phagocytic Cells
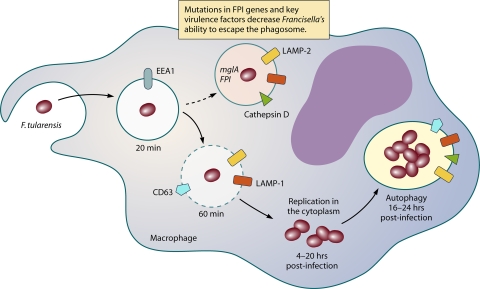
Francisella enters cells through the process of phagocytosis. It has been reported that F. tularensis may utilize an unusual mechanism involving the formation of spacious asymmetric pseudopod loops. This process, termed “looping phagocytosis” (33), involves actin rearrangement through phosphatidylinositol 3-kinase signaling and is strongly dependent on the presence of complement factor C3 and complement receptor CR3 (32, 33). Francisella may also enter cells via the mannose receptor, type I and II class A scavenge receptors, and the Fcγ receptor (11, 151, 178). Following internalization into host cells, F. tularensis is able to alter normal bactericidal processes. It prevents induction of the respiratory burst (66), limiting its exposure to superoxide or other reactive oxygen by-products. It alters phagosome maturation and as a result only transiently interacts with components of the endocytic trafficking network (Fig. 1). The organism initially resides in a membrane-bound compartment that acquires limited amounts of early endosomal and late endosomal-lysosomal markers, including EEA1, CD63, LAMP1, and LAMP2 (35). The F. tularensis-containing vacuole (FCV) fails to acquire the acid hydrolase cathepsin D and does not fuse with lysosomes (35). In addition, F. tularensis alters host cell trafficking by escaping from the phagosome and entering the host cell cytosol, where it undergoes extensive replication (27, 35, 82, 173). While the relative timing of these events appears to differ between the various Francisella species and the host cell types infected (27, 35, 82, 173), mutants that fail to prevent fusion with the lysosome and/or are unable to escape from the phagosome are highly attenuated in virulence in vitro and in vivo (19, 117, 133, 135).
FIG. 1.
Illustration of Francisella survival inside macrophages. Francisella is taken up by macrophages through looping phagocytosis (33) into an endosomal compartment that transiently acquires late endosome-associated markers (29, 32). Francisella then exits the phagosomal compartment and replicates to high numbers in the cellular cytosol. Prior to lysis of the cell, Francisella has been shown to reside in an autophagy-like compartment (27).
There are conflicting reports regarding the extent to which the FCV acidifies as it transiently interacts with components of the endocytic pathway. It also remains controversial whether exposure to acidic pH is necessary and/or sufficient for F. tularensis egress from the phagosome. Studies conducted by Clemens et al. using THP1 cells (a human macrophage-like cell line) or primary macrophages derived from peripheral blood monocytes have demonstrated that FCVs harboring LVS or type A F. tularensis become only minimally acidified (pH of 6.7) and acquire limited amounts of the proton vacuolar ATPase (34, 35). Additionally, use of the proton pump inhibitor bafilomycin A prior to infection of these macrophage types with F. tularensis strains does not alter the efficiency of F. tularensis phagosomal escape (34). In contrast, studies published by Santic et al. and Chong et al. have reported significant levels of FCV acidification and vacuolar ATPase acquisition in primary human and murine macrophages infected with F. tularensis Schu S4, LVS, and F. novicida (29, 173). Treatment of these macrophages with bafilomycin A prior to infection significantly reduced the efficiency with which these F. tularensis derivatives were able to escape from the phagosome (29, 173).
Phagosomal escape requires viable F. tularensis and occurs via an unknown mechanism that involves degradation of the surrounding lipid bilayers (27, 34, 35, 78, 173). At roughly 12 h postinfection, Francisella begins to replicate to high numbers within the host cell cyotosol, eventually leading to cell death, egress of Francisella, and presumably infection of nearby cells. Escape of F. tularensis from the phagosome and replication within the host cell cytosol is dependent on genes present in the Francisella pathogenicity island (FPI) (29, 78, 83, 110, 117, 138, 171, 173, 176). Francisella has also been shown to reside in vesicles similar to autolysosomes at ≥24 h postinfection, prior to host cell death, indicating that Francisella may reenter the endocytic pathway through host cell autophagy (27). The significance of this process for either Francisella infection or the immune response to infection remains unclear. Francisella may also exhibit an extracellular phase, as both LVS and Schu S4 have been found in the plasma following infection of mice via various inoculation routes (63). Whether this observation correlates to humans or plays a significant role in the ability of the organism to cause disease awaits further investigation.
IMMUNITY AND HOST RESPONSE TO INFECTION
Successful development of a Francisella vaccine will ultimately rely on a comprehensive understanding of the host immune response to infection. Many of the details regarding the host response to F. tularensis infection have come from studies using the less virulent F. novicida or the F. tularensis subsp. holarctica LVS, both of which are thought to differ from the more virulent type A strains in certain aspects of infection. Studies carried out with various murine infection models have shown that low doses of the attenuated LVS strain can be cleared by innate host defense mechanisms, while the fully virulent type A and B strains are able to rapidly kill mice prior to generation of a cell-mediated immune response. The precise mechanisms by which virulent strains avoid and overcome murine immune responses remain unknown. Differences in the host response to these subspecies and the route of infection highlight the complexities of this issue and suggest that the correlates of immunity need to be evaluated for each potential infection scenario.
Innate Immunity
The innate immune responses to F. tularensis infection share much in common with the responses seen with other intracellular pathogens. Francisella infection results in an early pronounced inflammatory response, with initial induction of proinflammatory and Th1-type cytokines, including interleukin-12, tumor necrosis factor alpha, and gamma interferon (IFN-γ) (38, 81, 189, 217). Tumor necrosis factor alpha and IFN-γ are essential for control of infection, as depletion of either converts typically sublethal infections into lethal ones (55, 56, 112). Macrophages, dendritic cells, and natural killer (NK) cells are likely responsible for the cytokine induction seen almost immediately postinfection (17, 118). Activation of proinflammatory cytokines in murine macrophages occurs in a Toll-like receptor 2 (TLR2)-dependent manner, indicating that TLR2-mediated signaling may be crucial for early pathogen recognition (37). IFN-γ activation of macrophages and other professional phagocytes is also particularly important for initial containment of Francisella, as these cells are a primary target of the organism for infection and replication. In addition to macrophages, neutrophils have been shown to be important in the initial control of infection, but their importance may differ with respect to the different tissues infected. In mouse infection models, depletion of neutrophils increases sensitivity to systemic infection but has little effect on respiratory infection with Francisella (41, 56, 184).
There is evidence that Francisella evades and modulates the host immune response beyond its ability to inhibit maturation of the host phagosome and escape lysosomal degradation. Francisella diminishes the capacity of macrophages to respond to engagement of TLRs with secondary stimuli such as lipopolysaccharide (LPS) (198). Similar effects have also been demonstrated in dendritic cells (81). A recent report by Bosio et al. has indicated that when delivered via the respiratory route, the type A strain Schu S4 actively suppresses early inflammatory responses in the lung (16). In particular, Schu S4 fails to activate pulmonary macrophages and dendritic cells and actively interferes with induction of proinflammatory cytokines, in part through the induction of transforming growth factor β (16). In addition, Woolard et al. have recently demonstrated that Francisella infection of bone marrow-derived macrophages results in secretion of prostaglandin E2, which inhibits interleukin-2 production and promotes a Th2-type response, a T-cell response that is ineffective against the clearing of intracellular organisms (220). This increase in prostaglandin E2 has also been confirmed in the lung in vivo (219). Finally, Francisella has been shown to infect and replicate within neutrophils and inhibit the respiratory burst, thus evading neutrophil killing mechanisms (127, 179). Though the precise contributions of these findings to infection remain unclear, it is likely that immune evasion and/or suppression is essential to the highly virulent nature of Francisella and differences between subspecies.
Adaptive Immunity
Exposure to sublethal concentrations of Francisella induces strong protective immunity against secondary exposure in humans and in experimental animal models (51, 188). Though specific antibodies are readily detectable in sera upon F. tularensis infection, their importance to immunity remains unclear. Passive antibody transfer studies carried out in animals suggest that antibodies may play a role in combating infection with lower-virulence strains while playing a lesser role against the more virulent subspecies (51, 54, 188). Although Francisella antibodies may prove beneficial in some situations, they are likely not essential. Rather, they must be coupled with an effective cellular immune response to fully control infection. Adaptive immunity to F. tularensis infection is largely dependent on T-cell-mediated immunity, particularly that mediated by CD4+ and CD8+ T cells (56). In mice, either CD4+ or CD8+ cells are able to control infection by F. novicida or LVS, while both cell types seem to be required for successful defense against the highly virulent type A strains (43, 74, 222). Similar to the case for mice, CD4+ and CD8+ T-cell responses are prominent in humans vaccinated with LVS (107, 192). The T-cell effector functions are likely very closely linked to the ability to activate macrophage intracellular killing mechanisms. Despite the known requirement of CD4+ and CD8+ T cells for resolving F. tularensis infection, little is known regarding the T-cell receptors, coreceptors, memory profiles, or major histocompatibility complex restriction of T-cell responses to infection.
Immunity to Infection by Different Routes
An effective vaccine against F. tularensis will require generation of an immune response that is protective against pulmonary infection. However, much of the work examining and characterizing the immune responses to Francisella infection have involved infection by the systemic route. Though there are many general consistencies, correlates of immunity to F. tularensis infection differ in certain aspects depending on the route of infection. A number of recent reports highlight potentially key differences in the host immune response to respiratory versus systemic infection (41). In addition to the diminished role of neutrophils and reactive nitrogen species, there exists disparity in the timing of initial host inflammation when comparing respiratory versus systemic infection. During murine infection initiated via the intradermal or subcutaneous route, there is an immediate onset of inflammation within the first 2 days postinfection that includes the rapid induction of IFN-γ (36, 54). During respiratory infection this response is delayed, not occurring until 3 to 5 days postinfection. By this time, significant bacterial burdens have begun to accumulate in the livers and spleens of infected mice, and it has been speculated that systemic disease contributes to the morbidity observed in these animals (40). The delay in inflammation onset is consistent with what has been seen in human disease (6). The precise reasons for this delay remain unclear, but it may play a contributing factor in the general difficulty in vaccinating against respiratory forms of the disease. Other recent reports also highlight potential differences in T-cell responses between respiratory and systemic infection. Woolard et al. have demonstrated that intranasal infection of mice produces much lower levels of IFN-γ-secreting T cells than systemic infection (219). Furthermore, intranasal inoculation results in a delayed accumulation of T cells in the spleen and lung, along with a significant increase in the amounts of prostaglandin E2. Collectively, these observations suggest that virulent F. tularensis subspecies alter T-cell responses to the detriment of the host (220).
Though our understanding of Francisella host/pathogen interactions is advancing, there is still a great deal that remains unclear. Of particular interest, the host immune response to infection by highly virulent type A strains has only now been investigated in any great detail. Further evaluation of the host immune response to infection, as well as identification of key Francisella virulence mediators, will be necessary to gain a more complete understanding of the interplay between Francisella and the host immune system, particularly for the development of novel prophylactic treatments.
FRANCISELLA GENETICS AND VIRULENCE FACTORS
The ability to effectively colonize or parasitize a diverse array of hosts suggests that F. tularensis is capable of adapting to a wide variety of growth environments. Despite its extreme virulence and fairly well-characterized intracellular life cycle, very little is known about the mechanisms of F. tularensis pathogenesis or the virulence factors encoded by this organism. Initial assessments of the completed genomic sequences from different F. tularensis subspecies have indicated that F. tularensis does not encode any toxins or secretion systems that are commonly present in other intracellular pathogens. In addition, F. tularensis does not encode homologs of genes that mediate phagosomal escape in other organisms, such as Listeria and Shigella. Due in large part to an increase in the development and efficiency of genetic tools, recent studies have begun to shed light on the specific virulence genes necessary for successful infection by F. tularensis.
Genetic Tools
Shuttle and integration vectors.
The field of Francisella genetics has undergone an extensive expansion over the past 10 years (71). Until recently, few vectors or selectable markers were amenable for use in Francisella, and the available methods for introducing DNA were generally inefficient. In 1994, identification of a 3,990-bp cryptic plasmid (pFNL10) from an F. novicida-like strain designated F6168 helped to usher in the first generation of useful genetic vectors for this organism (144). pFNL10 could be introduced by standard procedures and maintained in various subspecies of F. tularensis, although it was not capable of replicating in Escherichia coli and lacked any antibiotic resistance markers (144). Further modifications to pFNL10 led to the construction of second-generation vectors that carried replication origins for E. coli and selectable antibiotic resistance markers. pFNL100 included sequences from both pFNL10 and cloning vector pBR328 (143). pFNL200 was a deletion derivative of pFNL100 and expressed tetracycline and chloramphenicol resistance; however, it suffered from stability issues (143). pKK202 was a more stable derivative of pFNL200 that carried the p15A origin of replication from E. coli (139). Finally, the generation of pKK214 and its variants expanded the utility of pKK202 by incorporating a promoterless chloramphenicol acetyltransferase or green fluorescent protein reporter gene in place of the chloramphenicol acetyltransferase gene (2, 108).
More recently, Maier et al. have constructed a series of E. coli-Francisella shuttle vectors, termed pFNLTP, that are hybrids between pFNL10 and cloning vector pCR2.1-TOPO (125). These vectors can be efficiently transformed into F. tularensis subspecies by electroporation, are stably maintained even in the absence of antibiotic selection, and do not alter virulence characteristics of F. tularensis in vitro or in vivo (124, 125, 145, 146). A variety of pFNLTP1 variants have been generated, and these include derivatives that carry antibiotic resistance elements amenable for use in type A strains of F. tularensis, multiple cloning sites, reporter genes and counterselectable markers, and temperature-sensitive origins of replication (93, 125). In addition to their use as complementation and reporter gene platforms, pFNLTP1-based vectors (or vectors that have been derived from them) have been used as delivery vehicles to carry out transposon mutagenesis, targeted allelic exchange, and promoter-trap library construction (22, 125, 128).
LoVullo et al. have recently developed a series of shuttle vectors, pMP, that are based on the minimal regions of pFNL10 required for replication and regions from E. coli-mycobacterial shuttle vector pMV261 carrying the aphA1 antibiotic resistance determinant and ColE1 replication origin (121). While the original plasmid, pMP393, could be efficiently introduced by electroporation and was stable in various F. tularensis subspecies, it was frequently lost in the absence of selection (121). Second-generation variants of pMP393 have corrected maintenance issues and expanded the choice and utility of antibiotic resistance determinants for selection within F. tularensis (120). Third-generation pMP-based vectors have also been developed, in which stability has been further enhanced, useful multiple cloning sites introduced, and heterologous promoters added for gene expression studies (120). Finally, a single-copy chromosomal integration system for Francisella has been developed by that group (119). Vectors designed for this system include plasmids allowing integration at the attachment site for the Tn7 transposon (located downstream of the glmS gene) or within the blaB gene, encoding resistance to the antibiotic ampicillin (119). Development of an integration system for F. tularensis represents a major advancement for the field, as it alleviates some of the previous issues inherent with use of multicopy shuttle vectors, including lack of stability, use of heterologous antibiotic resistance determinants, and multicopy expression artifacts.
Gene disruption vectors.
Much of the lack of understanding of Francisella virulence can be directly attributed to the difficulty in generating defined genetic lesions within this family. While genetic tools and methodologies have been available for some time to disrupt genes in F. novicida, construction of mutant derivatives in the type A or B genetic background was not reported until 2004 (82). Gene disruptions in F. novicida have been generated using a variety of approaches, including allelic exchange of linear substrates (Table 2) (110). Initial efforts to disrupt genes in type A or type B strains were based largely on utilization of pUC19-derived suicide vectors (82). Optimization of these vectors, along with the development of additional vectors, has allowed the list of Francisella mutants to expand significantly (Tables 3 and 4). This list includes mutants that are defective for putative virulence factors as well as metabolic genes that may be utilized for the construction of live attenuated vaccine candidates. More recently, the TargeTron group II intron mutagenesis system has been adapted for use with various F. tularensis subspecies (162, 163). This system has proven efficient, and it is advantageous as it allows simultaneous disruption of genes that are present in more than one copy (162, 163).
TABLE 2.
F. novicida genes involved in pathogenesis
| Locus tag | Name | Function | Method(s)a | Cells/animals in which mutant strain is attenuatedb | Reference(s) |
|---|---|---|---|---|---|
| FTN_0008 | FTN_0008 | Ten-transmembrane-spanning drug/metabolite exporter protein | Tp | C57BL/6 | 106 |
| FTN_0012 | FTN_0012 | Hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_0019 | pyrB | Aspartate carbamoyltransferase | Tp | C57BL/6 | 213 |
| FTN_0020 | carB | Carbamoylphosphate synthase large chain | Tp | J774A.1, RAW, BMDM, BALB/c | 199, 213 |
| FTN_0021 | carA | Carbamoylphosphate synthase small chain | Tp | C57BL/6 | 213 |
| FTN_0023 | tmpT | Thiopurine S-methyltransferase | Tp | C57BL/6 | 106 |
| FTN_0028 | FTN_0028 | Conserved hypothetical membrane protein | Tp | C57BL/6 | 106 |
| FTN_0031 | FTN_0031 | Transcriptional regulator, LysR family | Tp | C57BL/6 | 106 |
| FTN_0035 | pyrF | Orotidine 5′-phosphate decarboxylase | Tp | C57BL/6 | 213 |
| FTN_0036 | pyrD | Diyroorotate dehydrogenase | Tp | C57BL/6 | 213 |
| FTN_0045 | FTN_0045 | Protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0055 | tyrA | Prephenate dehydrogenase | Tp | C57BL/6 | 106 |
| FTN_0090, FTN_1556, FTN_1061, FTN_0954 | acpABC, hap | Acid phosphatasesc | Ar | J774A.1, activated THP-1, BALB/c | 13, 133, 135 |
| FTN_0096 | FTN_0096 | Conserved hypothetical membrane protein | Tp | C57BL/6 | 213 |
| FTN_0097 | FTN_0097 | Aromatic amino acid transporter of the hydroxy/aromatic amino acid permease family | Tp | C57BL/6 | 213 |
| FTN_0098 | gidB | Methyltransferase, glucose-inhibited cell division protein | Tp | C57BL/6 | 213 |
| FTN_0111 | ribH | Riboflavin synthase beta-chain | Tp | C57BL/6 | 106 |
| FTN_0112 | ribA | RibA/GTP-cyclohydrolase II | Tp | C57BL/6 | 213 |
| FTN_0113 | ribB | Riboflavin synthase a-subunit 3,4-digydroxy-2-butanone 4-phosphate synthetase | Tp | C57BL/6 | 213 |
| FTN_0132 | FTN_0132 | Protein of unknown function | Tp | C57BL/6 | 106, 213 |
| FTN_0133 | FTN_0133 | RNase II family protein | Tp | C57BL/6 | 106 |
| FTN_0143 | FTN_0143 | Monovalent cation:proton antiporter | Tp | C57BL/6 | 106 |
| FTN_0169 | FTN_0169 | Conserved hypothetical membrane protein | Tp | C57BL/6 | 106 |
| FTN_0177 | purH | AICAR transformylase/IMP cyclohydrolase | Tp | J774A.1, RAW, BMDM, BALB/c | 199, 213 |
| FTN_0178 | purA | Adenylosuccinate synthetase | Ar/In | J774A.1, BALB/c | 158 |
| FTN_0196 | cyoB | Cytochrome o ubiquinol oxidase subunit I | Tp | C57BL/6 | 213 |
| FTN_0197 | cyoC | Cytochrome o ubiquinol oxidase subunit III | Tp | C57BL/6 | 213 |
| FTN_0198 | cyoD | Cytochrome o ubiquinol oxidase subunit IV | Tp | C57BL/6 | 213 |
| FTN_0199 | cyoE | Heme O synthase | Tp | C57BL/6 | 106 |
| FTN_0202 | pdxY | Pyridoxal/pyridoxine/pyridoxamine kinase | Tp | C57BL/6 | 213 |
| FTN_0205 | FTN_0205 | Conserved hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_0208 | FTN_0208 | Hypothetical membrane protein | Tp | C57BL/6 | 106 |
| FTN_0210 | FTN_0210 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_0211 | pcp | Pyrrolidone-carboxylate peptidase | Tp | C57BL/6 | 213 |
| FTN_0217 | FTN_0217 | l-Lactate dehydrogenase | Tp | C57BL/6 | 106 |
| FTN_0229 | pyrH | Uridylate kinase | Tp | C57BL/6 | 213 |
| FTN_0240 | rplD | 50S ribosomal protein L4 | Tp | C57BL/6 | 213 |
| FTN_0241 | rplW | 50S ribosomal protein L23 | Tp | C57BL/6 | 213 |
| FTN_0248 | rpsQ | 30S ribosomal protein S17 | Tp | RAW | 199 |
| FTN_0265 | rplQ | 50S ribosomal protein L17 | Tp | C57BL/6 | 213 |
| FTN_0266 | htpG | Chaperone Hsp90, heat shock protein HtpG | Tp | J774A.1, RAW, BMDM, BALB/c | 199, 213 |
| FTN_0280 | FTN_0280 | Hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_0281 | FTN_0281 | Protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0289 | FTN_0289 | ProP osmoprotectant transporter, fragment | Tp | C57BL/6 | 213 |
| FTN_0292 | FTN_0292 | Protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0295 | lpxF | Phosphatidic acid phosphatase, PAP2 superfamily | Ar | C57BL/6 | 209 |
| FTN_0296 | FTN_0296 | Amino acid transporter | Tp | C57BL/6 | 213 |
| FTN_0297 | FTN_0297 | Conserved protein of unknown function | Tp | C57BL/6 | 106, 213 |
| FTN_0298 | gplX | Fructose 1,6-bisphosphatase II | Tp | C57BL/6 | 106, 213 |
| FTN_0299 | putP | Proline:Na+ symporter | Tp | C57BL/6 | 106 |
| FTN_0300 | FTT1629c | Glycosyl transferase, group 2 | Tp | RAW | 199 |
| FTN_0302 | FTN_0302 | Hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_0326 | FTN_0326 | Conserved hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_0330c | minD | Septum formation inhibitor-activating ATPase | In | PM, BMDM, C57BL/6NCrIBR | 8 |
| FTN_0337 | fumA | Fumarate hydratase, class I | Tp | J774A.1, RAW, BMDM, BALB/c | 199 |
| FTN_0340 | FTN_0340 | Protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0344 | FTN_0344 | Aspartate:alanine exchanger family | Tp | C57BL/6 | 106 |
| FTN_0347 | fkpB | FK506 binding protein-type peptidyl-prolyl, cis-trans | Tp | C57BL/6 | 106 |
| FTN_0351 | FTN_0351 | Hypothetical protein, novel liver | Tp | C57BL/6 | 106 |
| FTN_0365 | FTN_0365 | Conserved hypothetical membrane protein | Tp | C57BL/6 | 106 |
| FTN_0393 | FTN_0393 | Conserved protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0395 | FTN_0395 | Transcriptional regulator, ArsR family | Tp | C57BL/6 | 106 |
| FTN_0397 | gpsA | Glycerol-3-phosphate-dehydrogenase | Tp | C57BL/6 | 106 |
| FTN_0400 | FTN_0400 | Protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0402 | aroC | Chorismate synthase | Tp | C57BL/6 | 106 |
| FTN_0416 | FTN_0416 | Conserved hypothetical membrane protein | Tp | C57BL/6 | 213 |
| FTN_0417 | folD | Methylene tetrahydrofolate | Tp | C57BL/6 | 106, 213 |
| FTN_0419 | purM | Phosphoribosylformylglycinamide cyclo-ligase | Tp | J774A.1, RAW, BMDM, BALB/c | 199, 213 |
| FTN_0420 | purCD | SAICAR synthetase/phosphoribosylamine-glycine ligase | Tp | J774A.1, RAW, BMDM, BALB/c | 199, 213 |
| FTN_0422 | purE | Phosphoribosylaminoimidazole carboxylase, catalytic subunit | Tp | C57BL/6 | 213 |
| FTN_0426 | FTN_0426 | Conserved protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0427 | tul4 | Lipoprotein of unknown function | Ar/In | J774A.1c | 110 |
| FTN_0429 | FTN_0429 | Hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_0430 | lpnB | Protein of unknown function | Tp | C57BL/6 | 106, 213 |
| FTN_0431 | FTN0431 | Type IV pilus glycosylation protein | Tp | C57BL/6 | 213 |
| FTN_0436 | FTN_0436 | Hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_0437 | FTN_0437 | Hydrolase, HD superfamily | Tp | C57BL/6 | 106 |
| FTN_0438 | rrmJ | 23S rRNA methylase | Tp | C57BL/6 | 106 |
| FTN_0443 | maeA | NAD-dependent malic enzyme | Tp | RAW | 199 |
| FTN_0444 | FTT0918 | Membrane protein of unknown function | Tp | C57BL/6 | 181 |
| FTN_0480 | fevR | Protein of unknown function | Ar | BMDM, C57BL/6 | 20 |
| FTN_0488 | cspC | Cold shock protein, | Tp | C57BL/6 | 106 |
| FTN_0493 | mtn | Adenosylhomocysteine nucleosidase | Tp | C57BL/6 | 213 |
| FTN_0494 | FTN_0494 | Hypothetical membrane protein | Tp | C57BL/6 | 213 |
| FTN_0494 | FTN_0494 | BNR/Asp box repeat protein | Tp | C57BL/6 | 213 |
| FTN_0503 | lolD | Lipoprotein releasing system, subunit D, ABC transporter, ATP-binding protein | Tp | C57BL/6 | 213 |
| FTN_0504 | cadA | Lysine decarboxylase, inducible | Tp | C57BL/6 | 213 |
| FTN_0505 | gcvT | Glycine cleavage complex T protein (aminomethyltransferase) | Tp | C57BL/6 | 213 |
| FTN_0506 | gcvH | Glycine cleavage system H protein | Tp | C57BL/6 | 213 |
| FTN_0507 | gcvP1 | Glycine cleavage system P protein, subunit 1 | Tp | C57BL/6 | 213 |
| FTN_0514 | pgm | Phosphoglucomutase | Tp | C57BL/6 | 213 |
| FTN_0536 | yjjK | ABC transporter, ATP binding protein | Tp | C57BL/6 | 213 |
| FTN_0537 | FTN_0537 | Proton-dependent oligopeptide | Tp | C57BL/6 | 106 |
| FTN_0544 | FTN_0544 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_0545 | flmF2 | Glycosyl transferase, group 2 | Tp | BALB/c, C57BL/6 | 101, 213 |
| FTN_0546 | flmK | Dolichyl-phosphate-mannose-protein, mannosyltransferase family protein | Tp | BALB/c, C57BL/6 | 101, 213 |
| FTN_0554 | FTN_0554 | RNA methyltransferase, | Tp | C57BL/6 | 106 |
| FTN_0559 | surA | Peptidyl-prolyl cis-trans isomerase | Tp | C57BL/6 | 213 |
| FTN_0560 | ksgA | Dimethyladenosine transferase, kasugamycin resistance | Tp | C57BL/6 | 213 |
| FTN_0571 | xasA | Amino acid-polyamine-organocation | Tp | C57BL/6 | 106, 213 |
| FTN_0578 | FTN_0578 | Major facilitator superfamily transport | Tp | C57BL/6 | 106 |
| FTN_0582 | gph | Phosphoglycolate phosphatase | Tp | C57BL/6 | 106 |
| FTN_0594 | sucC | Succinyl-coenzyme A synthetase, beta chain | Tp | RAW | 199 |
| FTN_0599 | FTN_0599 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_0609 | pnp | Polyribonucleotide nucleotidyltransferase | Tp | C57BL/6 | 106 |
| FTN_0624 | sdaC1 | Serine transporter | Tp | C57BL/6 | 213 |
| FTN_0643 | FTN_0643 | Hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_0646 | cscK | ROK family protein | Tp | C57BL/6 | 106 |
| FTN_0651 | cdd | Cytidine deaminase | Tp | C57BL/6 | 213 |
| FTN_0669 | deoD | Purine nucleoside phosphorylase | Tp | C57BL/6 | 213 |
| FTN_0678 | FTN_0678 | Drug:H+ antiporter-1 (DHA1) family | Tp | C57BL/6 | 106 |
| FTN_0689 | ppiC | Parvulin-like peptidyl-prolyl isomerase | Tp | C57BL/6 | 106 |
| FTN_0690 | deaD | DEAD box subfamily, ATP-dependent | Tp | C57BL/6 | 106 |
| FTN_0710 | FTN_0710 | Type I restriction-modification system | Tp | C57BL/6 | 106 |
| FTN_0713 | ostA2 | Organic solvent tolerance protein OstA | Tp | C57BL/6 | 106 |
| FTN_0714 | FTT0742 | Protein of unknown function | Tp | J774A.1, RAW, BMDM, BALB/c | 199 |
| FTN_0720 | FTN_0720 | Transcriptional regulator, LclR family | Tp | C57BL/6 | 106, 213 |
| FTN_0728 | FTN_0728 | Cation efflux family protein | Tp | C57BL/6 | 213 |
| FTN_0737 | potI | ATP binding cassette putrescine uptake | Tp | C57BL/6 | 106 |
| FTN_0740 | FTN_0740 | Protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0756 | fopA | OmpA family protein | Tp | RAW | 199 |
| FTN_0757 | FTN_0757 | Hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_0768 | tspO | Tryptophan-rich sensory protein | Tp | C57BL/6 | 106 |
| FTN_0787 | rep | UvrD/REP superfamily I | Tp | C57BL/6 | 106 |
| FTN_0806 | FTN_0806 | β-Glucosidase-related glycosidase | Tp | C57BL/6 | 213 |
| FTN_0810 | FTN_0810 | ROK family protein | Tp | C57BL/6 | 106 |
| FTN_0814 | bioF | 8-Amino-7-oxononanoate synthase | Tp | C57BL/6 | 213 |
| FTN_0815 | bioB | Biotin synthase | Tp | C57BL/6 | 213 |
| FTN_0816 | bioA | Oxononanoate aminotransferase | Tp | C57BL/6 | 213 |
| FTN_0817 | FTN_0817 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_0818 | FTN_0818 | Lipase/esterase | Tp | C57BL/6 | 213 |
| FTN_0821 | FTN_0821 | AMP binding family protein | Tp | C57BL/6 | 213 |
| FTN_0822 | FTN_0822 | Chorismate binding family protein | Tp | C57BL/6 | 213 |
| FTN_0823 | trpG | Anthranilate synthase component II | Tp | C57BL/6 | 213 |
| FTN_0824 | FTN_0824 | Major facilitator superfamily | Tp | C57BL/6 | 106 |
| FTN_0825 | FTN_0825 | Aldo/keto reductase family protein | Tp | C57BL/6 | 106 |
| FTN_0840 | mdaB | NADPH-quinone reductase | Tp | C57BL/6 | 106 |
| FTN_0848 | FTN_0848 | Amino acid antiporter | Tp | C57BL/6 | 213 |
| FTN_0853 | sufD | SufS activator complex, SufD subunit | Tp | C57BL/6 | 106 |
| FTN_0857 | FTN_0857 | Conserved hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_0869 | FTT0989 | Conserved protein of unknown function | Ar/In | BMDM, C57BL/6 | 21 |
| FTN_0873 | dcd | dCTP deaminase | Tp | C57BL/6 | 106 |
| FTN_0877 | cls | Cardiolipin synthetase | Tp | C57BL/6 | 106 |
| FTN_0881 | FTN_0881 | Fe2/Zn2 uptake regulator protein | Tp | C57BL/6 | 106 |
| FTN_0891 | ruvB | Holliday junction DNA helicase, subunit B | Tp | C57BL/6 | 213 |
| FTN_0918 | FTN_0918 | Conserved protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0925 | FTN_0925 | Hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_0933 | FTN_0933 | Protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_0938 | FTN_0938 | Hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_0998 | FTN_0998 | Potassium channel protein | Tp | C57BL/6 | 213 |
| FTN_1006 | FTN_1006 | Transporter-associated protein | Tp | C57BL/6 | 106 |
| FTN_1015 | FTN_1015 | Isochorismatase family protein | Tp | C57BL/6 | 106 |
| FTN_1016 | FTN_1016 | Conserved protein of unknown function | Tp | C57BL/6 | 106, 213 |
| FTN_1029 | FTN_1029 | Conserved protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_1030 | lipA | Lipoic acid synthetase | Tp | C57BL/6 | 106 |
| FTN_1038 | FTN_1038 | Conserved hypothetical membrane protein | Tp | C57BL/6 | 213 |
| FTN_1055 | lon | DNA binding, ATP dependent | Tp | C57BL/6 | 106 |
| FTN_1063 | FTN_1063 | tRNA-methylthiotransferase MiaB protein | Tp | C57BL/6 | 106 |
| FTN_1064 | phoH | PhoH-like protein | Tp | C57BL/6 | 213 |
| FTN_1066 | FTN_1066 | Metal ion transporter protein | Tp | C57BL/6 | 213 |
| FTN_1090 | FTN_1090 | Hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1098 | FTN_1098 | Conserved hypothetical membrane protein | Tp | C57BL/6 | 106 |
| FTN_1107 | metIQ | Methionine uptake transporter family | Tp | C57BL/6 | 106 |
| FTN_1111 | FTN_1111 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1112 | cphA | Cyanophycin synthetase | Tp | C57BL/6 | 213 |
| FTN_1131 | putA | Multifunctional protein, transcriptional repressor of proline utilization, proline dehydrogenase, pyrroline-5-carboxylate dehydrogenase | Tp | C57BL/6 | 213 |
| FTN_1132 | FTN_1132 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1133 | FTN_1133 | Protein of unknown function, novel lung, spleen | Tp | C57BL/6 | 106 |
| FTN_1146 | aspC2 | Aspartate aminotransferase | Tp | RAW | 199 |
| FTN_1148 | FTN_1148 | Glycoprotease family protein | Tp | C57BL/6 | 106 |
| FTN_1157 | FTN_1157 | GTP binding translational elongation | Tp | C57BL/6 | 106 |
| FTN_1165 | FTN_1165 | Predicted ATPase of the PP loop | Tp | C57BL/6 | 106 |
| FTN_1177 | sbcB | Exodeoxyribonuclease I | Tp | C57BL/6 | 106 |
| FTN_1186 | pepO | M13 family metallopeptidase | Ar/In | C57BL/6 | 21 |
| FTN_1196 | FTN_1196 | Conserved protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_1199 | FTN_1199 | Conserved protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_1200 | capC | Capsule biosynthesis protein CapC | Tp | C57BL/6 | 106 |
| FTN_1201 | capB | Capsule biosynthesis protein CapB | Tp | C57BL/6 | 213 |
| FTN_1209 | cphB | Cyanophycinase | Tp | C57BL/6 | 106, 213 |
| FTN_1211 | FTN_1211 | Haloacid dehalogenase-like hydrolase family protein | Tp | C57BL/6 | 213 |
| FTN_1212 | FTN_1212 | Glycosyltransferase group 1 family protein | Tp | C57BL/6 | 213 |
| FTN_1213 | FTN_1213 | Glycosyltransferase family protein | Tp | C57BL/6 | 213 |
| FTN_1214 | FTN_1214 | Glycosyltransferase family protein | Tp | C57BL/6 | 213 |
| FTN_1217 | FTN_1217 | ABC transporter, ATP binding and membrane protein | Tp | C57BL/6 | 213 |
| FTN_1218 | FTN_1218 | Glycosyltransferase, group 1 | Tp | C57BL/6 | 106, 213 |
| FTN_1219 | gale | UDP-glucose 4-epimerase | Tp | C57BL/6 | 213 |
| FTN_1220 | FTN_1220 | Bacterial sugar transferase family protein | Tp | C57BL/6 | 213 |
| FTN_1232 | FTN_1232 | Conserved hypothetical membrane protein | Tp | C57BL/6 | 106 |
| FTN_1241 | dedA2 | DedA family protein | Tp | RAW | 199 |
| FTN_1242 | dedA1 | DedA family protein | Tp | C57BL/6 | 213 |
| FTN_1243 | recO | RecFOR complex, RecO component | Tp | C57BL/6 | 106 |
| FTN_1254 | FTN_1254 | Hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1255 | FTN_1255 | Glycosyl transferase family 8 protein | Tp | C57BL/6 | 213 |
| FTN_1256 | FTN_1256 | Hypothetical membrane protein | Tp | C57BL/6 | 213 |
| FTN_1257 | FTN_1257 | Hypothetical membrane protein | Tp | C57BL/6 | 213 |
| FTN_1259 | glyA | Serine hydroxymethyltransferase | Tp | RAW | 199 |
| FTN_1272 | FTN_1272 | Proton-dependent oligopeptide | Tp | C57BL/6 | 106 |
| FTN_1273 | fadD1 | Acyl coenzyme A synthetase | Tp | C57BL/6 | 213 |
| FTN_1276 | emrA1 | HlyD family secretion protein | Tp | C57BL/6 | 213 |
| FTN_1277 | FTN_1277 | Outer membrane efflux protein | Tp | C57BL/6 | 213 |
| FTN_1284 | dnaK | Chaperone, heat shock protein, HSP 70 family | Tp | J774A.1, RAW, BMDM, BALB/c | 199 |
| FTN_1290 | mglA | Macrophage growth locus, protein A | Ar/In | J774A.1, Acanthamoeba castellanii, BALB/cAnNHsd, BALB/c | 110, 111, 214 |
| FTN_1292 | FTN_1292 | Solute:sodium symporter | Tp | C57BL/6 | 106 |
| FTN_1298 | FTN_1298 | GTPase of unknown function | Tp | C57BL/6 | 106 |
| FTN_1309 | pdpA | Protein of unknown function | Ar | CE, BALB/cByJ | 176, 177, 213 |
| FTN_1310 | pdpB | Protein of unknown function | Ar/In, Tp | BMDM, C57BL/6, J774A.1, RAW, BALB/c | 21, 199, 213 |
| FTN_1311 | FTN_0311 | Hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1312 | FTN_1312 | Conserved hypothetical protein | Tp | C57BL/6 | 106, 213 |
| FTN_1313 | FTN_1313 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1314 | FTN_1314 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1315 | FTN_1315 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1316 | FTN_1316 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1317 | FTN_1317 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1318 | cds2 | Hypothetical protein | Ar/In, Tp | BMDM, C57BL/6 | 21, 213 |
| FTN_1319 | FTN_1319 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1320 | FTN_1320 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1321 | iglD | Intracellular growth locus protein D | Ar/In, Tp | BALB/c, hMDMs, C57BL/6 | 106, 172, 213 |
| FTN_1322 | iglC | Intracellular growth locus, protein C | Ar/In | J774A.1, Acanthamoeba castellanii, BALB/cAnNHsd, C57BL/6 | 110, 111, 142, 213 |
| FTN_1323 | iglB | Intracellular growth locus, protein B | In | J774, BALB/c | 39, 213 |
| FTN_1324 | iglA | Intracellular growth locus protein A | Ar | J774A.1, CE | 46, 213 |
| FTN_1325c | pdpD | Protein of unknown function | Ar/In | BMDM, BALB/cByJ | 138, 213 |
| FTN_1326 | FTN_1326 | Conserved hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1333 | tktA | Transketolase I | Tp | J774A.1, RAW, BMDM, BALB/c | 199 |
| FTN_1349 | FTN_1349 | Hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_1351 | FTN_1351 | Conserved hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_1355 | FTN_1355 | Regulatory factor, Bvg | Tp | C57BL/6 | 106 |
| FTN_1357 | recB | Exodeoxyribonuclease V b-chain | Tp | C57BL/6 | 213 |
| FTN_1362 | FTN_1362 | Hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_1400 | FTN_1400 | S-Adenosylmethionine dependent | Tp | C57BL/6 | 106 |
| FTN_1403 | flmF1 | Glycosyltransferase | Tp | BALB/c, C57BL/6 | 101 |
| FTN_1415 | FTN_1415 | Thioredoxin | Tp | C57BL/6 | 106 |
| FTN_1417 | manB | Phosphomannomutase | Tp | C57BL/6 | 213 |
| FTN_1421 | wbtH | Asparagine synthase | Tp | C57BL/6 | 213 |
| FTN_1423 | wbtG | Glycosyl transferase | Tp | C57BL/6 | 213 |
| FTN_1425c-FTN_1427c | wbtDEF | LPS O-antigen biosynthetic gene cluster | Ar/In | BALB/c | 200, 213 |
| FTN_1432 | wbtA | dTDP-glucose 4,6-dehydratase | Tp | C57BL/6 | 213 |
| FTN_1439 | fadA | Acetyl coenzyme A acetyltransferase | Tp | C57BL/6 | 106 |
| FTN_1440 | FTN_1440 | Conserved hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_1444 | ocd | Ornithine cyclodeaminase, mu-crystallin homolog | Tp | RAW | 199 |
| FTN_1455 | FTN_1455 | Conserved hypothetical protein | Tp | C57BL/6 | 106 |
| FTN_1459 | FTN_1459 | Short-chain dehydrogenase | Tp | C57BL/6 | 106 |
| FTN_1464 | lepB | Signal peptidase I | Tp | C57BL/6 | 106 |
| FTN_1465 | pmrA | Two-component response regulator, orphan | Ar | J774A.1, activated THP-1, HeLa, BALB/c | 134 |
| FTN_1467 | proC | Pyrroline-5-carboxylate reductase | Tp | C57BL/6 | 106 |
| FTN_1471 | pcs | (CDP-alcohol) phosphatidyltransferase | Tp | C57BL/6 | 106 |
| FTN_1500 | FTN_1500 | Hypothetical protein | Tp | C57BL/6 | 213 |
| FTN_1501 | FTN_1501 | Na+/H+ antiporter | Tp | C57BL/6 | 213 |
| FTN_1507 | FTN_1507 | Pilus assembly protein | Tp | C57BL/6 | 106 |
| FTN_1513 | xerC | Integrase/recombinase XerC | Tp | C57BL/6 | 213 |
| FTN_1518 | relA | GTP pyrophosphokinase | Tp | C57BL/6 | 213 |
| FTN_1433 | FTN_1433 | Hypothetical membrane protein | Tp | C57BL/6 | 213 |
| FTN_1438 | fadB-acbP | Fusion product of 3-hydroxacyl-coenzyme A dehydrogenase and acyl coenzyme A binding protein | Tp | C57BL/6 | 213 |
| FTN_1470 | ispA | Geranyltransferase | Tp | C57BL/6 | 213 |
| FTN_1471 | pcs | Phosphatidylcholine synthase | Tp | C57BL/6 | 213 |
| FTN_1534 | FTN_1534 | Conserved protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_1536 | FTN_1536 | Amino acid-polyamine-organocation | Tp | C57BL/6 | 106 |
| FTN_1538 | groL | Chaperone protein, GroEL | Tp | C57BL/6 | 213 |
| FTN_1548 | FTN_1548 | Conserved hypothetical lipoprotein | Tp | C57BL/6 | 213 |
| FTN_1551 | ampD | N-Acetylmuramoyl-l-alanine amidase | Tp | C57BL/6 | 213 |
| FTN_1558 | xerD | Integrase/recombinase | Tp | C57BL/6 | 213 |
| FTN_1567 | rpoC | DNA-directed RNA polymerase, beta′ subunit/160-kDa subunit | Tp | RAW | 199 |
| FTN_1582 | FTN_1582 | Hypothetical membrane protein | Tp | C57BL/6 | 213 |
| FTN_1587 | FTN_1587 | Protein of unknown function | Tp | C57BL/6 | 106 |
| FTN_1588 | FTN_1588 | Major facilitator superfamily transport | Tp | C57BL/6 | 106 |
| FTN_1592 | oppB | Peptide/opine/nickel uptake transporter (PepT) family protein | Ar/In | C57BL/6 | 21 |
| FTN_1597 | prfC | Peptide chain release factor 3 | Tp | C57BL/6 | 213 |
| FTN_1602 | deoB | Phosphopentomutase | Tp | C57BL/6 | 213 |
| FTN_1607 | cca | tRNA nucleotidyltransferase | Tp | C57BL/6 | 213 |
| FTN_1608 | dsbB | Disulfide bond formation protein | Tp | J774A.1, RAW, BMDM, BALB/c, C57BL/6 | 199, 213 |
| FTN_1611 | FTN_1611 | Major facilitator superfamily transport | Tp | C57BL/6 | 106 |
| FTN_1617 | qseC | Sensor histidine kinase | Tp | C57BL/6 | 213 |
| FTN_1633 | apt | Adenine phosphoribosyltransferase | Tp | C57BL/6 | 213 |
| FTN_1634 | sucB | Dihydrolipoamide succinyltransferase component of 2-oxoglutarate dehydrogenase complex | Tp | C57BL/6 | 213 |
| FTN_1639 | sdhC | Succinate dehydrogenase, cytochrome b556 | Tp | C57BL/6 | 213 |
| FTN_1645 | FTN_1645 | AtpC ATP synthase, F1 sector, subunit epsilon | Tp | C57BL/6 | 106 |
| FTN_1653 | FTN_1653 | Hypothetical membrane protein | Tp | C57BL/6 | 213 |
| FTN_1654 | FTN_1654 | Transport protein | Tp | C57BL/6 | 213 |
| FTN_1655 | rluC | Ribosomal large subunit pseudouridine synthase C | Tp | C57BL/6 | 213 |
| FTN_1656 | FTN_1656 | ATPase | Tp | C57BL/6 | 213 |
| FTN_1657 | FTN_1657 | Major facilitator superfamily transport protein | Tp | C57BL/6 | 213 |
| FTN_1658 | hisS | Histidyl-tRNA synthetase | Tp | C57BL/6 | 213 |
| FTN_1659 | rbfA | Ribosome binding factor A | Tp | C57BL/6 | 213 |
| FTN_1665 | FTN_1665 | Magnesium chelatase | Tp | C57BL/6 | 106 |
| FTN_1673 | nuoH | NADPH dehydrogenase I, H subunit | Tp | C57BL/6 | 106 |
| FTN_1682 | figA (fslA) | Siderophore biosynthesis protein | Ar/In | J774A.1 | 47, 213 |
| FTN_1683 | FTN_1683 | Conserved membrane protein | Tp | C57BL/6 | 213 |
| FTN_1684 | lysA | Diaminopimelate decarboxylase | Tp | C57BL/6 | 213 |
| FTN_1686 | figE | Hypothetical membrane protein involved in siderophore uptake | Ar | BALB/c | 132 |
| FTN_1699 | purL | Phosphoribosylformylglycinamide synthase | Tp | J774A.1, RAW, BMDM, BALB/c | 199, 213 |
| FTN_1700 | purF | Amidophosphoribosyltransferase | Ar/In | J774A.1, BALB/c | 158, 213 |
| FTN_1715 | kdpD | Two-component sensor protein KdpD | Tp | C57BL/6 | 213 |
| FTN_1726 | FTN_1726 | Pyridoxal-dependent decarboxylase | Tp | C57BL/6 | 106 |
| FTN_1731 | pip | Proline iminopeptidase | Tp | C57BL/6 | 106 |
| FTN_1743 | clpB | ClpB protein | Tp | RAW | 199, 213 |
| FTN_1744 | FTN_1744 | Chitinase | Tp | C57BL/6 | 213 |
| FTN_1745 | purT | Phosphoribosylglycinamide formyltransferase 2 | Tp | C57BL/6 | 213 |
| FTN_1753 | FTN_1753 | Rieske (2Fe-2S) domain protein | Tp | C57BL/6 | 106 |
| FTN_1756 | bcp | Bacterioferritin comigratory protein | Tp | C57BL/6 | 106 |
| FTN_1760 | FTN_1760 | Zinc binding alcohol dehydrogenase | Tp | C57BL/6 | 106 |
| FTN_1778 | trpE | Anthranilate synthase component I | Tp | C57BL/6 | 106 |
Ar, allelic replacement; In, insertion; Tp, transposon insertion.
BMDM, bone marrow-derived macrophages; PM, peritoneal macrophages; CE, chicken embryos; hMDMs, human monocyte-derived macrophages; RAW, RAW264.7 murine macrophages.
Attenuated phenotype more pronounced with accumulated mutations.
TABLE 3.
F. tularensis subsp. holarctica genes involved in pathogenesis
| Locus tag | Name | Function | Method(s)a | Cells/animals in which mutant strain is attenuatedb | Reference(s) |
|---|---|---|---|---|---|
| FTL_0009 | FTT1747 | Outer membrane protein | STM | BALB/c | 191 |
| FTL_0010 | glpE | Thiosulfate sulfurtransferase | STM | BALB/c | 191 |
| FTL_0012 | recA | Recombinase A protein | STM | BALB/c | 191 |
| FTL_0028-FTL_0030 | carA, carB, pyrB | Uracil biosynthesis | Tp | MDM | 179 |
| FTL_0050 | FTT1645 | Hypothetical protein | Tp | J774A.1, BALB/c | 124 |
| FTL_0058 | FTT1688 | Aromatic amino acid transporter of the hydroxy/aromatic amino acid permease family | Tp | J774A.1 | 124 |
| FTL_0073 | FTT1676 | Membrane protein | STM | BALB/c | 191 |
| FTL_0094 | clpB | Caseinolytic protease | Ar, Tp, STM | BMM, J774A.1c, BALB/c | 124, 129, 191 |
| FTL_0111 | iglA | Intracellular growth | STM | BALB/c | 191 |
| FTL_0112 | iglB | Intracellular growth | STM | BALB/c | 191 |
| FTL_0113 | iglC | Intracellular growth | STM | BALB/c | 191 |
| FTL_0113, FTL_1159 | iglC1, iglC2 | Intracellular growth locus C | Ar | J774A.1, PM, PEC, BALB/c | 82, 117 |
| FTL_0133 | feoB | Ferrous iron transport protein | STM | BALB/c | 191 |
| FTL_0193 | cyoC | Cytochrome o-ubiquinol oxidase subunit III | STM | BALB/c | 191 |
| FTL_0257 | rpmJ | 50S ribosomal protein L36 | STM | BALB/c | 191 |
| FTL_0304 | FTT1490 | Na+/H+ antiporter | Tp | J774A.1 | 124 |
| FTL_0337 | FTT0843 | Unknown | STM | BALB/c | 191 |
| FTL_0382 | rocE | Amino acid permease | STM | BALB/c | 191 |
| FTL_0387 | aspC1 | Aspartate aminotransferase | STM | BALB/c | 191 |
| FTL_0395-FTL_0396 | purMCD | Purine biosynthesis | Ar/In, Ar | J774A.1, THP-1, PM, A549, BALB/c | 145, 146 |
| FTL_0421 | tul4 | Lipoprotein, T-cell-stimulating antigen | STM | BALB/c | 191 |
| FTL_0428 | parB | Chromosome partition protein B | STM | BALB/c | 191 |
| FTL_0430 | FTT0910 | Unknown | STM | BALB/c | 191 |
| FTL_0439 | FTT0919 | Hypothetical outer membrane protein | Tp | J774A.1, BALB/c | 124 |
| FTL_0439 | FTT0918 | Unknown | STM | BALB/c | 191 |
| FTL_0440 | FTT0920 | Transposase | STM | BALB/c | 191 |
| FTL_0456 | rpsU1 | 30S ribosomal protein S21 | STM | BALB/c | 191 |
| FTL_0483 | glgB | Glycogen branching enzyme, GlgB; polysaccharide metabolism | Tp, STM | J774A.1, BALB/c | 124, 191 |
| FTL_0485 | glgC | Glucose-1-phosphate adenylyltransferase | STM | BALB/c | 191 |
| FTL_0514 | FTT1611 | Unknown | STM | BALB/c | 191 |
| FTL_0519 | minD | Division inhibitor ATPase | STM | BALB/c | 191 |
| FTL_0520 | minC | Septum site-determining protein | STM | BALB/c | 191 |
| FTL_0525 | fumA | Fumarate hydratase | STM | BALB/c | 191 |
| FTL_0540 | lpxB | Lipid A-disaccharide synthase | STM | BALB/c | 191 |
| FTL_0544 | FTT1564 | Hypothetical protein | Tp | J774A.1, BALB/c | 191 |
| FTL_0552 | pmrA | Two-component response regulator, orphan | Ar/In | J774A.1, PM, MH-S, BALB/c, C57BL/6 | 165 |
| FTL_0584 | fadB | Acyl coenzyme A binding protein | STM | BALB/c | 191 |
| FTL_0589 | FTT1525c | Hypothetical membrane protein | STM | BALB/c | 191 |
| FTL_0592 | wbtA | dTDP-glucose 4,6-dehydratase | Ar, Tp | J774A.1, BALB/c, BALB/cByJ | 124, 160, 180, 191 |
| FTL_0594 | wbtC | UDP-glucose-4-epimerase | Tp | J774A.1 | 124 |
| FTL_0597 | wbtF | NAD-dependent epimerase, LPS modification | STM | BALB/c | 191 |
| FTL_0601 | wbtI | Sugar transaminase/perosamine synthetase | Pm | BALB/c | 115 |
| FTL_0606 | wbtM | dTDP-glucose 4,6-dehydratase | Tp | J774A.1 | 124 |
| FTL_0616 | rpoA2 | DNA-directed RNA polymerase, subunit | STM | BALB/c | 191 |
| FTL_0617 | bfr | Bacterioferritin | STM | BALB/c | 191 |
| FTL_0645 | FTT1416c | Lipoprotein | STM | BALB/c | 191 |
| FTL_0663 | FTT1400c | Unknown | STM | BALB/c | 191 |
| FTL_0706 | FTT1238c | Hypothetical membrane protein | Tp | J774A.1, BALB/c | 124 |
| FTL_0723 | FTT1221 | Unknown | STM | BALB/c | 191 |
| FTL_0766 | ggt | Gamma-glutamyltranspeptidase | Tp | J774A.1, RAW, THP-1, BMM, BALB/c | 4, 124 |
| FTL_0768 | bipA | GTP-binding translational elongation factor Tu and G family protein | STM | BALB/c | 191 |
| FTL_0789 | aspC2 | Aspartate aminotransferase, amino acid biosynthesis | Tp, STM | J774A.1, BALB/c | 124, 191 |
| FTL_0803 | FTT1152 | Unknown | STM | BALB/c | 191 |
| FTL_0837 | metIQ | d-Methionine transport protein (ABC transporter) | Tp, STM | J774A.1, BALB/c | 124, 191 |
| FTL_0838 | metN | d-Methionine transport protein (ABC transporter) | Tp | J774A.1 | 124 |
| FTL_0846 | FTT1117c | Isochorismatase hydrolase family protein | STM | BALB/c | 191 |
| FTL_0878 | FTT0610 | DNA/RNA endonuclease family | Tp | J774A.1 | 124 |
| FTL_0886 | FTT0618c | Conserved hypothetical protein YleA | Tp | J774A.1, BALB/c | 124 |
| FTL_0891 | tig | Molecular chaperone | STM | BALB/c | 191 |
| FTL_0892 | clpP | ATP-dependent Clp protease subunit P | STM | BALB/c | 191 |
| FTL_0893 | clpX | ATP-dependent Clp protease subunit X | STM | BALB/c | 191 |
| FTL_0894 | lon | ATP-dependent protease Lon | STM | BALB/c | 191 |
| FTL_0899 | hflX | Protease, GTP binding subunit | STM | BALB/c | 191 |
| FTL_0903 | hflK | Protease modulator | STM | BALB/c | 191 |
| FTL_0928 | elbB | DJ-1/PfpI family protein | STM | BALB/c | 191 |
| FTL_0950 | rplY | 50S ribosomal protein L25 | STM | BALB/c | 191 |
| FTL_0960 | sthA | Soluble pyridine nucleotide transhydrogenase | STM | BALB/c | 191 |
| FTL_1029 | pilF | Type IV pilus lipoprotein | Ar | C3H/HeN | 25 |
| FTL_1030 | rluB | Ribosomal large subunit pseudouridine synthase B | STM | BALB/c | 191 |
| FTL_1071, FTL_1478 | guaA, guaB | Guanine biosynthesis | Ar/In | J774, BALB/c | 170 |
| FTL_1075 | FTT1015 | Unknown | STM | BALB/c | 191 |
| FTL_1096 | FTT1103 | Hypothetical lipoprotein | Tp | J774A.1, BALB/c | 124, 191 |
| FTL_1096 | FTT1103 | Lipoprotein | STM | BALB/c | 191 |
| FTL_1097 | FTT1102 | Macrophage infectivity potentiator | STM | BALB/c | 191 |
| FTL_1134 | NA | Membrane protein | STM | BALB/c | 191 |
| FTL_1158, FTL_0112 | iglB | Intracellular growth locus B | Ar | J774A.1 | 19 |
| FTL_1225 | FTT0975 | Unknown | STM | BALB/c | 191 |
| FTL_1233 | FTT0968c | Amino acid antiporter | STM | BALB/c | 191 |
| FTL_1240 | aroG | Phospho-2-dehydro-3-deoxyheptonate aldolase | STM | BALB/c | 191 |
| FTL_1262 | FTT0945 | Chorismate family binding protein, aromatic amino acid and folate biosynthesis | Tp | J774A.1 | 124 |
| FTL_1266 | lipP | Lipase/esterase | STM | BALB/c | 191 |
| FTL_1273 | bioF | 8-Amino-7-oxononanoate synthase | STM | BALB/c | 191 |
| FTL_1274 | bioC | Biotin synthesis | STM | BALB/c | 191 |
| FTL_1275 | bioD | Dethiobiotin synthetase | STM | BALB/c | 191 |
| FTL_1328 | fopA | Outer membrane-associated protein | STM | BALB/c | 191 |
| FTL_1354 | FTT0759 | Membrane protein | STM | BALB/c | 191 |
| FTL_1392 | deaD | Cold shock DEAD box protein A | STM | BALB/c | 191 |
| FTL_1393 | ppiC | Peptidyl-prolyl cis-trans isomerase or parvulin | STM | BALB/c | 191 |
| FTL_1404 | rplT | 50S ribosomal protein L20 | STM | BALB/c | 191 |
| FTL_1414 | capA | Transmembrane HSP60 family protein | STM | BALB/c | 191 |
| FTL_1414-FTL_1416 | capACB | Capsule biosynthesis | Ar, Tp | J774A.1, BALB/c | 124, 191 |
| FTL_1415 | capC | Capsular polyglutamate biosynthesis protein CapC | STM | BALB/c | 191 |
| FTL_1416 | capB | Capsular polyglutamate biosynthesis protein CapB | STM | BALB/c | 191 |
| FTL_1419 | cphB | Cyanophycinase | STM | BALB/c | 191 |
| FTL_1452 | rpmA | 50S ribosomal protein L27 | STM | BALB/c | 191 |
| FTL_1458 | secA | Preprotein translocase, subunit A | STM | BALB/c | 191 |
| FTL_1461 | deoD | Purine nucleoside phosphorylase | STM | BALB/c | 191 |
| FTL_1473 | uvrA | DNA excision repair enzyme, subunit A | STM | BALB/c | 191 |
| FTL_1474 | greA | Transcription elongation factor | STM | BALB/c | 191 |
| FTL_1475 | FTT1314c | Type IV pilus fiber building block protein | STM | BALB/c | 191 |
| FTL_1504 | katG | Catalase | STM | BALB/c | 191 |
| FTL_1528 | FTT0708 | Major facilitator superfamily transport protein | STM | BALB/c | 191 |
| FTL_1542 | migR | Transcriptional regulator | Ar | MDM | 22 |
| FTL_1553 | sucC | Succinyl coenzyme A synthetase beta chain | STM | BALB/c | 191 |
| FTL_1554 | sucD | Succinyl coenzyme A synthetase alpha chain | STM | BALB/c | 191 |
| FTL_1581 | tivA | Hypothetical lipoprotein | Ar/In | CE, MDM | 93 |
| FTL_1583 | xasA | Glutamate-aminobutyric acid antiporter, XasA; amino acid transport | Tp | J774A.1 | 124 |
| FTL_1601 | yibK | tRNA/rRNA methyltransferase | STM | BALB/c | 191 |
| FTL_1622 | FTT0444 | Multidrug transporter | STM | BALB/c | 191 |
| FTL_1623 | FTT0443 | Unknown | STM | BALB/c | 191 |
| FTL_1664 | deoB | Phosphopentomutase | Ar/In | CE, MDM, DC, HEK-293 | 93 |
| FTL_1670 | dsbB | Disulfide bond formation protein, DsbB | Tp | J774A.1 | 124 |
| FTL_1672 | acrB | RND efflux pump | In, STM | BALB/c | 15, 191 |
| FTL_1678 | FTT0101 | Membrane protein | STM | BALB/c | 191 |
| FTL_1701 | gplX | Fructose-1,6-bisphosphatase | Tp, STM | J774A.1, BALB/c | 124, 191 |
| FTL_1750 | secE | Preprotein translocase, subunit E | STM | BALB/c | 191 |
| FTL_1771 | pilT | Twitching motility protein PilT | Tp | C3H/HeN | 25 |
| FTL_1793 | sodB | Fe-superoxide dismutase | Ar | BALB/c, C57BL/6, MH-S | 9 |
| FTL_1806 | FTT0053 | Major facilitator superfamily transporter | Tp | J774A.1 | 124 |
| FTL_1832 | FTT0029c | Unknown | STM | BALB/c | 191 |
| FTL_1865 | tolC | Glutamate decarboxylase | Ar | C3H/HeN | 77 |
| FTL_1867 | yegQ | Protease | STM | BALB/c | 191 |
| FTL_1912 | rpsA | 30S ribosomal protein S1 | STM | BALB/c | 191 |
| FTL_1914 | ripA | Hypothetical protein | Ar | J774A.1, TC-1, C57BL/6 | 72 |
| FTL_1936 | FTT0209c | Periplasmic solute binding family protein | STM | BALB/c | 191 |
| FTL_1947 | yjjk | ABC transporter ATP binding protein | STM | BALB/c | 191 |
| FTL_R0003 | 16S rRNA | 16S rRNA | STM | BALB/c | 191 |
| FTL_R0004 | tRNA-Ile | tRNA-isoleucine | STM | BALB/c | 191 |
| FTT0890 | pilA | Type IV pilus fiber building block protein | Recomb. | C57BL/6 | 65 |
Ar, allelic replacement; In, insertion; Tp, transposon insertion; STM, signature-tagged mutagenesis; Recomb., direct repeat-mediated deletion.
MDM, monocyte-derived macrophages; PM, peritoneal macrophages; PEC, peritoneal exudate cells; CE, chicken embryos; DC, dendritic cells.
Intermediate attenuation phenotype.
TABLE 4.
F. tularensis subsp. tularensis genes involved in pathogenesis
| Locus tag | Name | Function | Method(s)a | Cells/animals in which mutant strain is attenuatedb | Reference(s) |
|---|---|---|---|---|---|
| FTT0026c | fslE | Siderophore uptake | Tp, Ar | BALB/c | 100, 159 |
| FTT0056c | FTT0056c | Major facilitator superfamily transport protein | Tp | Hep G2 | 155 |
| FTT0069c | FTT0069 | Unannotated | Tp | BALB/c | 100 |
| FTT0107c | dsbB | Transposon mutant | Tp, Ar | C57BL/6 | 157 |
| FTT0107c | dsbB | Disulfide bond formation protein | Tp | Hep G2, J774A.1 | 155 |
| FTT0118 | prfC | Peptide chain release factor 3 | Tp | BALB/c | 100 |
| FTT0129 | FTT0129 | Major facilitator superfamily transport protein | Tp | Hep G2 | 155 |
| FTT0132 | glpA | Glycerol-3-phosphate dehydrogenase | Tp | BALB/c | 100 |
| FTT0141 | rplA | 50S ribosomal protein L1 | Tp | BALB/c | 100 |
| FTT0156 | FTT0156 | Acid phosphatase | Tp | BALB/c | 100 |
| FTT0203c | purH | Bifunctional purine biosynthesis protein | Tp | Hep G2 | 155 |
| FTT0204 | purA | Adenylosuccinate synthetase | Tp | Hep G2 | 155 |
| FTT0245 | usp | Universal stress protein | Tp | BALB/c | 100 |
| FTT0250 | ppdK | Phosphoenolpyruvate synthase/pyruvate phosphate dikinase | Tp | BALB/c | 100 |
| FTT0290 | moxR | MoxR-like ATPase | Tp | BALB/c | 100 |
| FTT0425 | asd | Aspartate semialdehyde dehydrogenase | Tp | BALB/c | 100 |
| FTT0435 | ctv | Carbon-nitrogen hydrolase | Ar | BMDM, MH-S, BALB/c | 123 |
| FTT0444 | tet | Drug:H+ antiporter-1 (DNA1) family protein | Tp | BALB/c | 100 |
| FTT0486 | mutL | DNA mismatch repair enzyme with ATPase activity | Tp | BALB/c | 100 |
| FTT0588 | aroA | 3-Phosphoshikimate I-carboxyvinyl transferase | Tp | Hep G2 | 155 |
| FTT0609 | FTT0609 | Unannotated | Tp | BALB/c | 100 |
| FTT0623 | tig | Trigger factor protein (peptidyl-prolyl cis/trans isomerase), chaperone | Tp | BALB/c | 100 |
| FTT0626 | lon | DNA binding, ATP-dependent protease LA | Tp | BALB/c | 100 |
| FTT0654 | elbB | DJ-1/PfpI family protein | Tp | BALB/c | 100 |
| FTT0687c | hslU | ATP-dependent protease HslVU, ATPase subunit | Tp | BALB/c | 100 |
| FTT0862c | htpX | Zn-dependent protease with chaperone function | Tp | BALB/c | 100 |
| FTT0876c | aroC | Chorismate synthase | Tp | BALB/c | 100 |
| FTT0891 | FTT0891 | Conserved hypothetical membrane protein | Tp | BALB/c | 100 |
| FTT0893-FTT0894 | purMCD | Purine biosynthesis | Ar | MDM, J774A.1, A549, BALB/c | 146 |
| FTT0918 | FTT0918 | Hypothetical protein | Ar | BALB/c | 204 |
| FTT1087c | rep | UvrD/REP superfamily I DNA and RNA helicases | Tp | BALB/c | 100 |
| FTT1103 | FTT1103 | Conserved hypothetical lipoprotein | Tp/Ar | Hep G2, BALB/c, C57BL/6 | 155, 157 |
| FTT1120c | tgt | Queuine tRNA-ribosyltransferase | Tp | BALB/c | 100 |
| FTT1130c | cphA | Cyanophycin synthetase | Tp | BALB/c | 100 |
| FTT1158c | pilO | Type IV pilus glycosylation protein | Tp | BALB/c | 100 |
| FTT1179 | bipA | GTP binding translational elongation, factor Tu and G family protein | Tp | BALB/c | 100 |
| FTT11802c | trpE | Anthranilate synthase component I | Tp | BALB/c | 100 |
| FTT1181c | ggt | Gamma-glutamyltranspeptidase | Ar, Tp | BALB/c, HepG2 | 100, 155 |
| FTT1234 | FTT1234 | Choloylglycine hydrolase family protein | Tp | Hep G2 | 155 |
| FTT1236 | FTT1236 | Hypothetical protein | Tp | Hep G2, J774A.1 | 155 |
| FTT1244c | yfiO | Conserved hypothetical lipoprotein | Tp | Hep G2 | 155 |
| FTT1278c | rnhB | RNase HII | Tp | BALB/c | 100 |
| FTT1310c | hflB | ATP-dependent metalloprotease | Tp | Hep G2 | 155 |
| FTT1312c | uvrA | DNA excision repair enzyme, subunit A | Tp | BALB/c | 100 |
| FTT1356, FTT1711 | idlD | Intracellular growth locus D | Ar | BALB/c | 100 |
| FTT1357c, FTT1712c | iglC2, iglC1 | Intracellular growth locus C | Ar | BALB/c | 204 |
| FTT1358, FTT1713 | iglB | Intracellular growth locus B | Ar | BALB/c | 100 |
| FTT1455 | wbtI | Sugar transamine/perosamine synthetase | Ar | BALB/c | 100 |
| FTT1455 | wbtI | LPS O-antigen synthesis | Tp | BALB/c | 100 |
| FTT1459c-FTN1461c | wbtDEF | LPS O-antigen biosynthetic cluster | Ar/In | J774A.1, BALB/c | 200 |
| FTT1490 | FTT1490 | Na+/H+ antiporter | Tp | Hep G2 | 155 |
| FTT1542c | omp26 | Protein of unknown function | Tp | BALB/c | 100 |
| FTT1561 | kdtA | 3-Deoxy-d-manno-octulosonic-acid transferase | Ar | BALB/c | 100 |
| FTT1631 | glpX | Fructose 1,6-bisphosphatase II | Ar | BALB/c | 100 |
| FTT1640c | FTT1640 | Activator of osmoprotectant transporter ProP, fragment | Tp | BALB/c | 100 |
| FTT1663 | carA | Carbamoylphosphate synthase small chain | Tp | Hep G2 | 155 |
| FTT1664 | carB | Carbamoylphosphate synthase large chain | Tp | Hep G2 | 155 |
| FTT1665 | pyrB | Aspartate carbamoyltransferase | Tp | Hep G2 | 155 |
| FTT1720c | purL | Phosphoribosylformylglycinamide synthase | Tp | BALB/c, Hep G2 | 100, 155 |
| FTT1721 | purF | Amidophosphoribosyltransferase | Tp | BALB/c, Hep G2 | 100, 155 |
| FTT1724c | tolC | Outer membrane efflux protein | Tp | BALB/c | 100 |
| FTT1744c | ipdC | Indolepyruvate decarboxylase | Tp | BALB/c | 100 |
| FTT1762c | FTT1762c | Acetyltransferase protein | Tp | Hep G2 | 155 |
| FTT1773c | trpB | Tryptophan synthase beta chain | Tp | BALB/c | 100 |
| FTT1782c | yjjK | ABC transporter ATP binding protein | Tp | BALB/c | 100 |
Ar, allelic replacement; In, insertion; Tp, transposon insertion.
BMDM, bone marrow-derived macrophages; MDM, moncyte-derived macrophages; HepG2, human hepatocellularcarcinoma cells; MH-S, murine alveolar macrophages.
The development of Francisella genetic tools has also allowed for the implementation of global mutagenesis strategies. These include transposon mutagenesis of F. novicida, the LVS, and type A strain Schu S4. In 2004, Kawula et al. described the use of Tn5 transposon-transposase complexes to create random, stable insertion mutations in the LVS chromosome (103). Another strategy, employed by Maier et al., involved the utilization of either a temperature-sensitive version of pFNLTP1 or a derivative of pFNLTP1 in which the origin of replication for Francisella had been removed as a delivery vehicle for Himar transposon mutagenesis (124, 126). This library has since been used to identify mutants of LVS defective for intracellular growth within macrophages (124). More recently, a number of negative selection strategies including transposon site hybridization and signature-tagged mutagenesis have been optimized for use with Francisella and employed to identify genes required for growth of F. novicida or LVS in mice (106, 191, 213). In 2007, Gallagher et al. completed a full-scale genomic mutagenesis of the F. novicida U112 genome in which each putative nonessential open reading frame had been interrupted, thereby contributing a comprehensive mutagenesis library available for analyses (76). In addition, a Tn5-based transposon mutagenesis system has also been developed (23). This system expands upon the utility of current transposon tools by allowing unmarking of the antibiotic resistance determinant following transposition into the genome and inclusion of promoterless lux and lacZ alleles for analyzing gene expression using reporter gene technology (23). Mutagenesis using this transposon system has allowed identification of genes from F. tularensis LVS that are required for inhibition of the respiratory burst in neutrophils and for intracellular growth or survival within this cell type (179). Additionally, this system was used to identify FevR, a novel regulator of iglB (22). Finally, useful genetic surrogates of F. novicida which lack all of the resident restriction-modification systems that otherwise act as a barrier to gene transfer have now been developed (75). Clearly, the ongoing genetic work with Francisella is rapidly expanding our understanding of Francisella pathogenesis, and it will no doubt lead to identification of key virulence mediators that can be exploited for the development of potential vaccines and therapeutics.
Virulence Factors
Developments in the field of F. tularensis genetics have played an important role in identifying the repertoire of virulence genes utilized by this organism during infection within the host. While the characterization of these determinants is still in its infancy, the large numbers of mutants that exhibit defects in virulence indicate that the pathogenic lifestyle of F. tularensis is both complex and multifaceted. Further characterization of these genes will be necessary to fully understand F. tularensis infection and the type of immunity required to control infection.
Surface structures. (i) Capsule.
F. tularensis is thought to encode a carbohydrate-rich capsule that may assist the bacterium in mediating resistance to various environmental and host-generated stresses. Capsule-negative mutants were first reported for F. tularensis LVS following mutagenesis with acridine orange (166). Mutants exhibited a rough rather than smooth colony phenotype on agar medium and failed to produce an electron-dense surface layer, which was readily observable on the wild-type parent by electron microscopy (166). Rough mutants of LVS were found to be more sensitive to killing by serum complement, and they exhibited a diminished capacity to cause disease in mice (166). Consistent with the potential importance of capsule production in virulence, removal of capsule-like material by exposure to hypertonic solutions of sodium chloride was also found to attenuate virulence of F. tularensis following infection of guinea pigs (89). A locus in Francisella (capBCA) containing genes with similarity to determinants encoding the poly-γ-d-glutamic capsule in Bacillus anthracis has recently been described (191). This locus has been shown to be essential for virulence of F. tularensis strains LVS and U112 in a murine model of tularemia using two independent negative-selection screens (191, 213). However, definitive demonstration that these determinants encode components of the capsule has not yet been realized.
(ii) LPS.
LPS is a major structural component of most gram-negative bacteria and is a predominant eptiope recognized by components of the innate immune system. LPS is comprised of a hydrophobic lipid A portion that anchors the structure to the outer membrane, an oligosaccharide core, and an O-polysaccharide chain that specifies antigenicity. Compared to other gram-negative bacteria such as E. coli, the LPS produced by F. tularensis, particularly by the more virulent subspecies including F. tularensis subsp. tularensis and F. tularensis subsp. holarctica, elicits relatively low immunobiological activity (5, 167). While the exact reasons for this are unclear, the lipid A moiety of F. tularensis differs from that present in most other organisms (131, 150, 206). In particular, lipid A from Francisella lacks the 4′-phosphate moiety commonly found on the nonreducing glucosamine dimer in E. coli LPS and is hypoacylated compared to other LPS species. Wang et al. have shown that the 4′-phosphate is removed postproduction by the lipid A 4′-phosphatase LpxF (208). Deletion of lpxF leads to decreased virulence following intradermal inoculation in the footpads of mice (209). Interestingly, the deletion of lpxF also leads to retention of the 3′-O-acyl chain on the core glucosamine, possibly further contributing to increased immunogenicity (209). Several studies have established the importance of LPS in the virulence of F. tularensis. “Rough” LPS phase derivatives of type A strain Schu S4 (i.e., the blue-to-gray color variants observed under obliquely transmitted light and first described by Eigelsbach in 1951) are less virulent and less immunogenic in mice than their “smooth” wild-type counterparts (52). A similar pattern of reduced virulence and immunogenicity in mice and guinea pigs is also observed with gray variants of F. tularensis LVS (53). More recent studies have revisited the blue-to-gray phase variation in F. tularensis and the importance of LPS in resistance to bactericidal factors made by host cells (7, 31, 44, 56, 88). Finally, other studies have described LPS biosynthetic mutants and shown them to be attenuated for virulence in vitro and/or in vivo (114, 124, 155, 191, 213).
(iii) Type IV pili.
Pili are complex filamentous bacterial surface structures that have been shown to play an important role in numerous physiological processes in bacteria, including association of organisms with host cell surfaces and protein secretion (153). Pili are comprised of a main structural pilus shaft that contains a terminal adhesin that promotes interactions with specific surface-exposed host cell determinants. Analysis of genomic sequences from various Francisella strains indicates that these organisms contain clusters of genes that share homology with type IV pilus determinants in other species, including Neisseria meningitidis and Pseudomonas aeruginosa (64, 77, 109, 223). Pili have been observed on the surface of several Francisella species following growth in laboratory medium (77, 223). Importantly, disruption of genes predicted to encode pilus biosynthetic factors abolishes expression of these structures on the bacterial surface of Francisella (25, 65). Interestingly, a subset of pilus-like genes does not appear to be directly involved in pilus production but rather is required for protein secretion (86, 223). Expression of pilus biosynthetic genes from Francisella has also been shown to functionally complement pilus-negative strains of Neisseria gonorrhoeae with deletions in the analogous determinant (164). Several lines of evidence indicate that production of pili or expression of pilus-like genes is important for virulence by Francisella. Pilus-like genes are regulated by MglA (223), a well-established virulence determinant of F. tularensis. Disruption of specific pilus-like genes also attenuates the ability of Francisella to adhere to various host cell types (25) or grow intracellularly (223). Finally, mutations in pilus-like genes alter virulence of Francisella in a mouse model of tularemia (25, 65, 86, 223).
The FPI.
An FPI of approximately 30 kb is present in duplicate in virulent F. tularensis subsp. tularensis and F. tularensis subsp. holarctica and in single copy in F. novicida. The FPI is comprised of roughly 17 open reading frames (137), a majority of which have been shown to be required for aspects of F. tularensis pathogenesis. It is currently thought that several FPI genes encode components of a secretion system, similar to the type VI system recently described in other organisms (46, 122). Genes present in the FPI are arranged into two major transcriptional units (138) and are induced during intracellular growth of F. tularensis (29, 111, 212). FPI genes have also been shown to be regulated by other environmental conditions, including iron (22, 23, 47, 105, 113, 177) and hydrogen peroxide (80), and by several regulatory factors, including MglAB (21, 46, 85, 111, 177), SspA (26), PmrA (134, 165), FevR (20), and MigR (22). One major transcriptional unit encodes genes of the intracellular growth locus (i.e., iglABCD). Mutation within any of these genes attenuates growth of Francisella in macrophages, in insect cells, and/or in mice (78, 83, 100, 110, 117, 161, 173, 207). IglA and IglB are interacting cytoplasmic proteins and have been predicted to be involved in effector protein secretion (46). iglC encodes a 23-kDa hypothetical protein. Although the exact function of this protein has not yet been defined, iglC mutants generated in F. tularensis subsp. tularensis, F. tularensis subsp. holarctica, and F. novicida are highly attenuated for growth in vitro and in vivo (12, 78, 83, 110, 111, 117, 161, 173, 191, 198, 204, 213). In particular, IglC is required for the inhibition of phagosomal maturation and/or escape from the host phagosome by F. novicida (173). Finally, iglD has been shown to be essential for intracellular replication of Francisella in human monocyte-derived macrophages as well as for intracellular replication in mice (29, 100, 171).
pdpA and pdpB represent the first two genes in the second major transcriptional unit located within the FPI. pdpA and pdpB encode hypothetical proteins that are required for virulence of F. novicida in insect cells, in chicken embryos, and/or in mice (21, 138, 161, 176, 199, 213). While little is known regarding the role of PdpB, mutants with deletions in pdpA localize with markers of lysosomes following infection into host cells (176). This phenotype is reminiscent of that observed with iglC mutants, suggesting that PdpA may be required for phagosomal maturation modification and/or escape of F. tularensis from the phagosome. Francisella PdpA contains a motif in its N-terminal region that is characteristic of proteins that interact with components of the eukaryotic ubiquitin-proteosome pathway (176). However, this protein does not contain an identifiable secretion signal, it localizes to the cytoplasm in F. novicida, and it has not been detected inside host cells following infection by the bacterium (176). Thus, the roles of PdpA and PdpB and their localization during an infection currently remain undefined.
Transcriptional regulators. (i) MglAB.
MglAB (macrophage growth locus) was first identified in a screen for suppressors of acid phosphatase expression in F. novicida (12). mglA and mglB are organized in an operon and encode proteins exhibiting homology to SspA and SspB of E. coli and Haemophilus spp. (12). SspA is an RNA polymerase-associated protein in E. coli, and it has been shown to regulate expression of numerous genes in response to stress (95, 218). Mutations in either mglA or mglB attenuate growth of F. tularensis in macrophages (12), in mosquito cells (161), in amoebas (12, 111), in fruit flies (207), and in mice (12, 111). Microarray comparisons between wild-type strains and mglA mutants indicate that MglA functions as a global transcription factor in F. tularensis, regulating expression of more than 100 genes, including those within and outside of the FPI (21). Of note, disruption of mglA attenuates the ability of Francisella to inhibit phagosome maturation and escape into the host cell cytosol, likely due to regulation of genes, including iglABCD.
(ii) SspA.
SspA is a transcription factor in the Francisella genome that exhibits high homology to MglA. In F. tularensis LVS, both SspA and MglA associate with RNA polymerase (26). Furthermore, SspA and MglA directly interact, and association of MglA with RNA polymerase requires SspA (26). Targeted gene and global gene expression studies carried out using DNA microarrays indicate that SspA and MglA coregulate the same gene set in F. tularensis, providing further evidence that these proteins likely work together in combination with RNA polymerase to regulate gene expression (26).
(iii) PmrA.
pmrA encodes an orphaned response regulator that shares homology with the Salmonella enterica serovar Typhimurium response regulator PmrA (134). Response regulators (and their cognate histidine sensor kinases) function to regulate gene expression through phosphorylation-based signal transduction cascades initiated following exposure of the histidine kinase to extracytoplasmic signals. In general, F. tularensis encodes a paucity of two-component signal transduction systems and other transcription factors relative to other organisms of similar genome size. The consequences of pmrA disruption have been examined in both F. novicida and in F. tularensis LVS (134, 165). Mutants generated in either strain background are attenuated for virulence in macrophages and in mice. In addition, pmrA mutants of F. novicida are more sensitive to antimicrobial peptides than their wild-type counterparts (134). DNA microarray studies carried out with these mutants indicate that PmrA regulates a large group of genes, including those contained within the FPI (134, 165). However, PmrA does not appear to regulate MglA or vice versa (134).
(iv) FevR.
fevR (Francisella effector of virulence regulation) encodes a hypothetical protein and was identified in a screen of genes requiring MglA/SspA for their expression (20). FevR is required for replication of F. novicida and F. tularensis LVS in murine and human macrophages (20, 22), in the human epithelial cell lines HEp-2 and A549 (22), and in mice (20). While the mechanism(s) of FevR's activity remains unclear, fevR mutants of F. tularensis LVS remain trapped within a phagosome that retains late endosomal marker LAMP-1 but not lysosomal marker cathepsin D (22). fevR mutants are also compromised in their ability to block NADPH oxidase activity following infection into neutrophils (22). Based on these and other observations not discussed here, FevR has been postulated to act in parallel with MglA/SspA in a feed-forward loop to positively regulate virulence factors essential for Francisella pathogenesis, including genes within the FPI (20). fevR expression is also positively regulated by response regulator PmrA (134). Thus, expression of this regulatory determinant is complex and is mediated by multiple input signals.
(v) MigR.
migR (macrophage intracellular growth regulator) is a newly identified regulator of virulence gene expression in F. tularensis LVS (22). Isolated in a transposon mutagenesis screen for transcriptional activators of iglB, migR encodes a hypothetical protein containing a predicted AMP binding domain (22). F. tularensis LVS migR mutants are attenuated for growth in human monocyte-derived macrophages relative to their wild-type counterparts; however, they exhibit no growth differences following infection into human epithelial cell lines, including HEp-2 and A549 pneumocytes (22). In addition to its ability to regulate the igl locus in LVS, MigR is also a positive regulator of transcription factor fevR (22). However, it remains unclear whether this regulation is direct or indirect or whether the observed regulation on igl expression occurs indirectly through FevR.
Additional virulence factors.
Apart from the genetic determinants described above, a number of other virulence factors involved in Francisella pathogenesis have also been identified (Tables 2, 3, and 4). While a comprehensive discussion of these genes is beyond the scope of this review, it is possible to make several general observations regarding genes contained within this list and phenotypes of selected mutants carrying disruptions within these genes. First, advancements in genetic tools and procedures for doing allelic replacement and transposon mutagenesis have greatly expanded the number of mutants that have been generated from type A strains of F. tularensis. While the first report of a nonspontaneous mutant of a type A strain did not occur until 2005 (204), nearly 70 Schu S4 derivatives carrying targeted or randomly generated transposon insertions have been reported to date. Second, a large percentage of the genes identified in screens for virulence factors in the various F. tularensis subspecies encode hypothetical proteins with unknown function. This suggests that many of the mechanisms utilized by this organism to infect, be maintained, and/or cause disease within its host are likely to be novel. Third, there is a high correlation between the requirement of a given gene for intracellular growth and/or survival and its requirement for F. tularensis to cause disease in vivo. While there have been exceptions to this rule, the ability of F. tularensis to infect cells, alter phagosome trafficking, egress into the host cell cytosol, and undergo extensive multiplication is an essential part of the overall life cycle of this organism. Finally, phenotypes observed following the disruption of a given gene in one Francisella species or subspecies do not necessarily correlate with the phenotype observed in another strain. This characteristic will be particularly important as more and more mutant strains are generated and target genes characterized for their potential utilization as vaccine targets.
DEVELOPING A FRANCISELLA VACCINE
Early Studies
Foshay vaccine.
As the potential for weaponization of F. tularensis has been realized for some time, efforts to develop a Francisella vaccine have been ongoing since the 1940s. Early efforts involved preparations of killed whole-cell F. tularensis. However, these materials offered limited efficacy in both human and animal studies (67). Administration of such preparations resulted in poor or incomplete protection in most cases and in adverse side effects that ultimately limited utility (205). A vaccine developed by Foshay et al. using acid extraction and preservation in phenol was less reactogenic and was used to vaccinate several thousand volunteers in Ohio between 1933 and 1941 (67). However, due to the limited sample size and inadequate reporting of infection in the general population, the effectiveness of this vaccine could not be directly determined (67). The Foshay preparation was able to protect nonhuman primates from death after challenge with 740 CFU of Schu S4, but in many cases it was unable to prevent disease symptoms (84). Further studies with mice indicated that the Foshay vaccine offered only low levels of protection against highly virulent strains (67, 99).
LVS.
The isolation of an LVS in Russia and its subsequent transfer to the United States in the 1950s constituted a significant breakthrough in vaccination against Francisella. LVS was developed by multiple passages in vitro and in vivo of a virulent F. tularensis subsp. holarctica strain (201). This strain was gifted to the United States in 1956 and was approved as an investigational new drug by the Federal Drug Administration (FDA) in the early 1960s (39a). Early evaluation of LVS as a live vaccine was performed in human volunteers by the U.S. Army in the late 1950s (174, 175). LVS was given by scarification for evaluation against subsequent subcutaneous or aerosol challenges with F. tularensis type A strain Schu S4. Vaccination with LVS protected against high-dose (1,000 CFU) subcutaneous and low-dose (10 to 100 CFU) aerosol challenge with Schu S4 but did not confer significant protection against aerosol challenge with doses approaching 1,000 CFU (174, 175). Improved efficacy of LVS was observed following vaccination of volunteers via the respiratory route; however, LVS was capable of inducing human tularemia in a subset of volunteers when given at the dose necessary to confer immunity (92). Regardless, LVS was used to vaccinate laboratory workers at the U.S. Army Medical Research Institute of Infectious Diseases (USAMRID), after which the incidence of laboratory-acquired tularemia decreased significantly. It remains unclear whether a part of this decrease may also have resulted from improved laboratory practices (24). Despite its successes, the unknown nature of its attenuation and residual virulence following vaccination by the aerosol route has limited the overall utility of LVS and resulted in its removal from the Investigational New Drug list by the FDA. Consequently, it remains unlicensed for use in the United States. Even so, LVS remains the benchmark to which other Francisella vaccine candidates are compared.
Subunit Vaccines
Efforts toward developing subunit vaccines against F. tularensis have met with limited success (Table 5). Early attempts to identify protective antigens were based on identification of immunoreactive surface-associated proteins. While these proteins were found to stimulate in vitro responses using T cells from LVS-vaccinated animals or individuals (79, 168, 185, 193), the level of in vivo protective immunity conferred by some of these immunoreactive complexes in mice was below that observed with LVS vaccination (79). Other surface-exposed antigens, including carbohydrates and LPS, have also been investigated as to their potential to stimulate an immunoreactive and/or immunoprotective response (42, 73, 74, 169, 200). While immunization with LPS has been shown to generate a protective antibody response to challenge with less virulent Francisella species or subspecies of F. tularensis, it provides only limited protection against high-dose type A challenge (42, 73, 74, 200). A number of specific immunoreactive protein and lipoprotein antigens have also been investigated, including GroEL, KatG, and Tul4. Despite their immunogenicity, evaluations of these and other protein antigens have yet to demonstrate significant protection as subunit vaccine candidates (39a, 73, 79). These results, along with the failure of the Foshay preparation years before, indicate that generation of protective immunity against F. tularensis likely requires recognition of multiple antigenic determinants capable of stimulating both humoral and cell-mediated immune responses. Consistent with this observation, administration of an LVS boost following primary vaccination with LPS provides almost complete protection in mice against 1,000 50% lethal doses (LD50s) of type A F. tularensis, a level of protection better than that seen with LVS alone (74). More recently, Huntley et al. have demonstrated that vaccination with a mixture of outer membrane preparations from LVS provides partial protection against 40 CFU of type A Schu S4 delivered via the respiratory route (94). Given these recent advances and the reduced risks associated with subunit preparations relative to other vaccination types, development of protective subunit vaccines for F. tularensis remains a plausible goal.
TABLE 5.
Francisella subunit vaccine candidates
| Antigen | Adjuvant | Dose, μg (route)a | Challenge strain | Boost | Challenge route (dose, CFU)b | Host mouse strain | Protection | Reference |
|---|---|---|---|---|---|---|---|---|
| Ethanol-inactivated LVS | Freund's adjuvant | 20 (i.p.) | Schu S4 | No | i.n. (40) | C3H/HeN | Yes | 94 |
| LPS | Freund's adjuvant | 20 (i.p.) | Schu S4 | No | i.n. (40) | C3H/HeN | No | 94 |
| Outer membrane proteins | Freund's adjuvant | 20 (i.p.) | Schu S4 | No | i.n. (40) | C3H/HeN | Yes | 94 |
| LPS | Freund's adjuvant | 50 (s.c.) | LVS | Yes | i.p. (2.5 × 106) | BALB/c | Yes | 73 |
| OMP | Freund's adjuvant | 100 | LVS | Yes | i.p. (2.5 × 106) | BALB/c | Yes | 73 |
| LPS | Bovine serum albumin | 20 (s.c.) | Type B no. 108 | No | i.d. (80) | BALB/c | Yes | 42 |
| Aerosol (30) | BALB/c | No | 42 | |||||
| Type A no. 33 | No | i.d. (60) | BALB/c | No | 42 | |||
| Aerosol (50) | BALB/c | No | 42 |
i.p., intraperitoneal; s.c., subcutaneous.
i.d., intradermal; i.n., intranasal.
Live Vaccines
The utility of live attenuated strains as vaccines has been demonstrated for a number of bacterial pathogens and has resulted in the development of commercially available vaccines for Salmonella enterica serovar Typhi (Ty21a), Vibrio cholerae (CVD 103-HgR), and Mycobacterium tuberculosis (Mycobacterium bovis BCG). A live vaccine typically contains one or more defined genetic lesions in pathways that are essential for in vivo growth of the bacterium. Vaccination with these strains is advantageous, as the organism is generally unable to survive for extended periods or at high levels within host cells but remains capable of expressing its repertoire of antigenic determinants. Conversely, an inherent caveat of working with live vaccines is that they must strike an intricate balance between attenuation and stimulation of immunity. Bacterial derivatives that are overattenuated may not prime substantive immunity. On the other hand, derivatives that are able to prime substantive immunity may retain partial virulence, undermining their use as a safe vaccination tool. Despite its limitations, the successes of LVS as a vaccine suggest that developing a rationally attenuated Francisella strain is both feasible and warranted.
F. novicida.
Many of the studies examining the initial feasibility of defined F. tularensis mutants as live attenuated vaccine candidates have been conducted using F. novicida as a surrogate organism (Table 6). Mutant derivatives examined have included those carrying gene disruptions in the FPI (iglC and pdpB), in metabolic pathways (purA, purF, carB, and fumA), in transcription factors (mglA, and pmrA), in acid phosphatases (acpABCH), in LPS biosynthesis (fmlK), in disulfide bond formation (dsbB), and in other, as-yet-uncharacterized processes. While results from these studies indicate that many of the generated mutants are able to prime robust immune responses in mice following vaccination, host responses generated to these mutants, or even to sublethal concentrations of the wild-type F. novicida parent, have led to protection only against challenge with the homologous species (Table 6). To date, no F. novicida mutants have been shown to confer adequate protective immunity against challenge with virulent type A or type B F. tularensis isolates (Table 6) (134, 158, 182). This suggests that despite the high level of genetic similarity between the Francisella species, F. novicida exhibits significant differences either in immunodominant antigens or in the profile of immunological responses that it elicits relative to the more virulent subspecies. Alternatively, the in vivo lifestyle of F. novicida may differ in some as-yet-unapparent aspect from that of its more virulent type A or type B counterparts.
TABLE 6.
Francisella live vaccine candidates
| Species or subspecies | Locus tag for attenuating mutation | Annotation | Vaccination routea (dose, CFU) | Challenge strain | Boost | Challenge route (dose, CFU) | Host mouse strain(s) | Protection | Reference |
|---|---|---|---|---|---|---|---|---|---|
| F. novicida | None (wild type) | i.d. (100) | FSC033 | No | Aerosol (10) | BALB/c | No | 182 | |
| FTN_1645 | atpC | i.n. (149) | U112 | No | i.n. (25) | C57BL/6 | Yes | 106 | |
| FTN_0178 | purA | i.p. (3.3 × 106) | U112 | No | i.p. (170) | BALB/c | No | 158 | |
| FTN_1700 | purF | i.p. (6.95 × 103) | U112 | No | i.p. (170) | BALB/c | Yes | 158 | |
| Schu S4 | No | i.p. (100) | BALB/c | No | 158 | ||||
| FTN_1465 | pmrA | i.n. (106) | Schu S4 | No | i.n. (100) | BALB/c | No | 134 | |
| U112 | No | i.n. (106) | BALB/c | Yes | 134 | ||||
| FTN_1608 | dsbB | i.n. (6 × 105) | U112 | No | i.n. (6 × 107) | BALB/c | Yes | 199 | |
| FTN_0714 | FTT0742 | i.n. (6 × 107) | U112 | No | i.n. (6 × 107) | BALB/c | Yes | 199 | |
| FTN_1310 | pdpB | i.n. (6 × 107) | U112 | No | i.n. (6 × 107) | BALB/c | Yes | 199 | |
| FTN_0337 | fumA | i.n. (6 × 105) | U112 | No | i.n. (6 × 107) | BALB/c | Yes | 199 | |
| FTN_0020 | carB | i.n. (6 × 103) | U112 | No | i.n. (8 × 105) | BALB/c | Yes | 199 | |
| FTN_1322 | iglC | i.n. (106) | U112 | No | i.n. (103) | BALB/c | Yes | 142 | |
| i.n. (104) | BALB/c | Yes | 142 | ||||||
| i.n. (105) | BALB/c | No | 142 | ||||||
| FTN_1322 | iglB | i.n. (106) | U112 | No | i.n. (103) | BALB/c | Yes | 39 | |
| LVS | No | i.n. (3 × 104) | BALB/c | Yes | 39 | ||||
| Oral (103) | Schu S4 | Yes | i.n. (52) | BALB/c | No | 39 | |||
| FTN_1290 | mglA | Aerosol (105) | U112 | No | Aerosol (35-8 × 104) | BALB/c, C57BL/6 | No | 214 | |
| FTN_0050, FTN_1556, FTN_1061, FTN_0954 | acpABCH | i.n. (103) | U112 | No | i.n. (106) | BALB/c | Yes | 135 | |
| i.n. (106) | U112 | No | i.n. (106) | BALB/c | Yes | 135 | |||
| FTN_0090, FTN_1061, FTN_0954 | acpCH or acpACH | i.n. (103) | U112 | No | i.n. (103) | BALB/c | No | 135 | |
| FTN_0546 | flmK | s.c. (400-500) | U112 | No | s.c. (660) | BALB/c, C57BL/6 | Yes | 101 | |
| Aerosol (100) | U112 | No | i.n. (50) | BALB/c | Yes | 101 | |||
| F. tularensis subsp. holarctica | None (wild type) | i.n. (200) | Schu S4 | No | i.n. (100) | BALB/c | Yes | 146 | |
| i.n. (2,000) | BALB/c | No | 146 | ||||||
| Yes | i.d. (100, 2,000) | BALB/c | Yes | 146 | |||||
| FTL_0094 | clpB | i.p. (13) | LVS | No | i.p. (1 × 104) | BALB/c | Yes | 129 | |
| i.p. (1,300) | LVS | No | i.p. (1 × 104) | BALB/c | Yes | 129 | |||
| FTL0395-FTL0396 | purMCD | i.n. (106) | Schu S4 | No | i.n. (100, 2,000) | BALB/c | No | 146 | |
| i.d. (100, 2,000) | BALB/c | No | 146 | ||||||
| Yes | i.n. (100) | BALB/c | Yes | 146 | |||||
| i.n. (2,000) | BALB/c | No | 146 | ||||||
| i.d. (100, 2,000) | BALB/c | Yes | 146 | ||||||
| FTL0552 | pmrA | i.n. (105) | Schu S4 | No | i.n. (102) | C57BL/6, BALB/c | Yes | 165 | |
| FTL0421 | lpnA | i.d. (105) | LVS | No | i.d. (107) | C3H/HeN | Yes | 62 | |
| FTL_1071 | guaA | (2.2 × 107) | LVS | No | 2.8 × 105 | BALB/c | Yes | 170 | |
| FTL_1478 | guaB | (3.6 × 107) | LVS | No | 2.8 × 105 | BALB/c | 170 | ||
| FTL_1793 | sodB | i.n. (5,000) | Schu S4 | No | i.n. (14 × 103) | C57BL/6 | Yes | 9 | |
| i.n. (500) | LVS | Yes | i.n. (1.3 × 106) | C57BL/6 | Yes | 9 | |||
| Schu S4 | Yes | i.n. (104) | C57BL/6 | No | 9 | ||||
| FTL_0592 | wbtA | i.d. (1.5 × 108) | FSC 108 | Yes | i.d. (17) | BALB/c | Yes | 180 | |
| Schu S4 | Yes | i.d. (10) | BALB/c | Yes | 180 | ||||
| F. tularensis subsp. tularensis | FTT0107c | dsbB | i.n. (6.8 × 103) | Schu S4 | No | i.n. (13-13,000) | C57BL/6 | No | 156 |
| FTT0893-FTT0894 | purMCD | i.n. (104) | Schu S4 | No | i.n. (100, 2,000) | BALB/c | No | 146 | |
| i.d. (100, 2,000) | BALB/c | Yes | 146 | ||||||
| Yes | i.n. (100) | BALB/c | Yes | 146 | |||||
| i.n. (2,000) | BALB/c | No | 146 | ||||||
| i.d. (100, 2,000) | BALB/c | Yes | 146 | ||||||
| FTT0918 | FTT0918 | i.d. (105) | FSC033 | No | i.d. (500) | BALB/c | Yes | 204 | |
| Aerosol (10) | BALB/c | Yes | 204 | ||||||
| FTT1357c, FTT1712c | iglC, iglC1 | i.d. (106-107) | FSC033 | No | i.d. (500), aerosol (10) | BALB/c | No | 204 | |
| FTT1459c-FTT1461c | wbtDEF | s.c. (105) | Schu S4 | No | s.c. (100) | BALB/c | No | 200 | |
| FTT1103 | FTT1103 | i.n. (1.6 × 108) | Schu S4 | No | i.n. (1,000) | C57BL/6, BALB/c | Yes | 157 |
i.d., intradermal; i.n., intranasal; i.p., intraperitoneal; s.c., subcutaneous.
Infection-vaccination studies with specific F. novicida mutants have also provided important insights into characteristics that will be necessary for successful F. tularensis vaccine development. Mutants unable to escape from the phagosome (i.e., iglC and mglA mutants) do not function well as live vaccine candidates even though they are extremely attenuated and can be administered at high doses in vivo (Table 6) (142, 214). This suggests that replication within the host cell cytosol is essential for priming a protective immune response against Francisella. The variable effectiveness of metabolic mutants as vaccine candidates also indicates that limited intracellular (or extracellular) replication is an important criterion for generating a protective immune response. For example, F. novicida mutants disrupted in purA, a gene involved in the early steps of purine biosynthesis, are unable to protect against homologous challenge (158). In contrast, protective immunity against homologous challenge is observed following vaccination of mice with mutants defective in a later step of the purine biosynthetic pathway (i.e., purF) (158). It is likely that differences in the ability of these mutants to persist in host tissues contribute to this phenotype.
F. tularensis subsp. holarctica.
While LVS remains problematic as a host for vaccine development for several reasons, its previous success as a live vaccine against type A F. tularensis challenge indicates that it may be a more suitable surrogate for evaluating the efficacies of specific genes as vaccine targets. In this regard, a variety of mutants have been generated in the LVS background and examined for their ability to confer protective immunity against challenge with type A or type B strains (Table 6) (10, 62, 129, 145, 146, 165, 170, 180). These have included LVS derivatives mutated in the clpB heat shock protein gene, purine biosynthetic genes purMCD and guaAB, response regulator gene pmrA, predicted lipoprotein gene lpnA, superoxide dismutase gene sodB, and LPS biosynthetic gene wbtA (Table 6). In general, results from these studies indicate that vaccination with sublethal doses of wild-type LVS or LVS-derived mutants confer high levels of protective immunity against challenge with wild-type LVS (10, 62, 129, 145, 170). Vaccination with these derivatives also provides variable protection against virulent type A or type B strains when administered by the parenteral route (146, 180) and against relatively low doses of Schu S4 delivered via the respiratory route (10, 146, 165). Not surprisingly, mice vaccinated with LVS mutants are not well protected against respiratory infection with higher doses of type A or type B F. tularensis (10, 146), and this level of protection is similar to that observed following sublethal vaccination with wild-type LVS (146).
F. tularensis subsp. tularensis.
It has been speculated that the limited protection offered by LVS or its derivatives against aerosol challenge with type A strains of F. tularensis might be related to differences in protective antigens and could be countered by vaccination with an attenuated type A strain (39a, 40, 84, 204, 221). Alternatively, the types of immune responses elicited or cell types encountered during type A pulmonary infection may be different than those generated with other subspecies. Consistent with this idea, Wu et al. have observed that boosting with sublethal doses of the type A strain NMFTA after LVS vaccination affords mice superior protection against NMFTA challenge compared to simply boosting with LVS (221). While only a limited number of F. tularensis subsp. tularensis mutants have been evaluated for their potential as live attenuated vaccine candidates (Table 3), results from these studies have indicated that it is possible to generate highly attenuated derivatives in this genetic background, including some that are able to provide low to modest levels of protection against virulent type A or type B isolates delivered by the respiratory route (146, 157, 204). However, given the highly infectious nature of type A strains of F. tularensis and the broad host range that these strains exhibit in nature, development of vaccine candidates that are safe, immunogenic, and highly protective will undoubtedly be a formidable task.
Heterologous hosts.
The inherent problems with the use of live attenuated Francisella vaccines, as well as the limitations of subunit/component vaccines, have led some groups to explore the use of heterologous bacteria to express Francisella antigens (73, 97, 186) (Table 7). Of the various outer membrane protein, lipoprotein, and virulence factor genes studied to date, only iglC expressed in a Listeria monocytogenes ΔactA mutant confers protection against challenge with type A or B F. tularensis (97).
TABLE 7.
Expression of Francisella antigens in heterologous hosts
| F. tularensis antigen(s) | Host | Attenuating mutation(s) | Vaccination routea (dose, CFU) | Challenge strain | Boost | Challenge routeb (dose, CFU) | Host mouse strain | Protection | Reference |
|---|---|---|---|---|---|---|---|---|---|
| IglC | L. monocytogenes | ΔactA | i.d. (106-107) | LVS | Yes | i.n. (4,400) | BALB/c | Yes | 97 |
| Schu S4 | Yes | Aerosol (1 [10 LD50]) | BALB/c | Yes | 97 | ||||
| KatG | L. monocytogenes | ΔactA | i.d. (106-107) | LVS | Yes | i.n. (4,400) | BALB/c | No | 97 |
| Schu S4 | Yes | Aerosol (1 [10 LD50]) | BALB/c | No | 97 | ||||
| AcpA, Bfr, DnaK, GroEL, Pld | L. monocytogenes | ΔactA | i.d. (106-107) | LVS | Yes | i.n. (4,400) | BALB/c | No | 97 |
| Tul4 | S. enterica serovar Typhimurium | Δasd, Δcya, Δcrp | i.p. (5 × 103) | LVS | No | i.v. (160-230) | BALB/cJ | No | 186 |
| FopA | S. enterica serovar Typhimurium | ΔaroA | i.v. (1 × 107) | LVS | Yes | i.p. (101-2.5 × 106) | BALB/c | No | 73 |
i.d., intradermal; i.p., intraperitoneal; i.v., intravenous.
i.n., intranasal.
Respiratory versus parenteral vaccination.
A growing body of literature indicates that pulmonary vaccination may provide optimal protection against respiratory pathogens, rather than vaccination via the typical parenteral routes (39b, 92, 221). Aerosol delivery of a tularemia vaccine may be important for the stimulation of lung-associated lymph nodes and key immune mediators present in the lung. While inoculation of vaccines via the intradermal or intramuscular route typically induces systemic immune responses, vaccination via these routes often fails to induce substantial responses in mucosal tissues such as the lungs (130). This may in part explain the fact that while offering considerable protection against subsequent parenteral Schu S4 challenge, LVS delivered by scarification confers poor protection against respiratory challenge with Schu S4. An advantage of vaccination via the respiratory route is the generation of immune responses at local as well as at distal mucosal sites, thus generating the necessary response in lymphoid organs (130). Chen et al. demonstrated that intranasal vaccination of mice with LVS confers superior protection against subsequent aerosol challenge with 10 CFU of type A F. tularensis relative to that observed following vaccination with LVS via the intradermal route (28). Importantly, immunization via this route also maintains protective efficacy against intradermal challenge (28). These results are also consistent with findings by Wu et al. demonstrating that intranasal vaccination with LVS confers superior protection against subsequent intranasal challenge with type A strain NMFTA (221). These findings and others indicate that a live attenuated Francisella strain delivered via the respiratory route may provide optimal protection against subsequent aerosol challenge.
CONCLUDING REMARKS
F. tularensis is a highly virulent pathogen with the potential to cause severe disease in humans. Very few infectious bacteria have as broad a host range and the capacity to replicate to such high numbers in a variety of host tissues. Humans can be infected via a number of routes, resulting in a variety of disease manifestations. Inhalation of as few as 10 live organisms can result in potentially lethal disease. The biological weapons programs of several countries included F. tularensis as a bioagent due to its potential to cause debilitating disease. However, since the conclusion of these weapons programs, little work has been done to understand the genetic determinants required for Francisella disease and pathogenesis. The recent influx of investigators and funding initiatives in the Francisella field has lead to a number of advancements in the study of genetics, pathogenesis, and vaccine development for this organism. Continued support of initiatives in these areas will undoubtedly continue to uncover important new aspects of the F. tularensis lifestyle and/or the mechanisms by which this organism interacts with its host. Undoubtedly, these insights will prove crucial as studies into the development of a safe and protective Francisella vaccine continue forward.
As increasing amounts of literature examining vaccination strategies against virulent F. tularensis subspecies have become available, a picture of the characteristics necessary for protective immunity is emerging. It is likely that a successful vaccine candidate will need to induce aspects of both cell-mediated and humoral immunity. Both CD4+ and CD8+ T-cell responses are necessary for clearance of highly virulent strains, and induction of such responses is essential to generate F. tularensis immunity. Despite efforts to identify key antigenic mediators, it is evident that live attenuated vaccines may offer the best protection, as has been demonstrated in mouse infection models. Vaccination with attenuated derivatives of type A F. tularensis strains appears thus far to offer no significant advantage over vaccination with LVS, indicating that work toward developing a live attenuated vaccine candidate based on utilization of a type B background may be more suitable. Regardless of the subspecies utilized, it may be necessary to disrupt bacterial determinants involved in initial suppression of the host immune response. Particularly during respiratory infection, F. tularensis uses a number of strategies to limit the host response, allowing for significant bacterial proliferation and dissemination early after infection. It is likely no coincidence that respiratory tularemia is the most difficult disease manifestation to prevent with vaccination. Identification and elimination of F. tularensis immunosuppressive mediators in already-attenuated strains may also be a plausible strategy that leads to a safer and less reactogenic vaccine. Finally, the route of vaccination needs to be considered when developing vaccine candidates, as evidence indicates that respiratory vaccination may provide better protection against aerosol challenge. Despite difficulties in vaccinating against highly virulent F. tularensis strains, the multitude of vaccine candidates emerging as a result of recent advancements in F. tularensis genetics continues to yield important information regarding the elements necessary to elicit immunity against this highly virulent pathogen.
ADDENDUM IN PROOF
Presently, the genome for Francisella tularensis subsp. holarctica strain URFT1 (NZABAZ00000000) is undergoing shotgun sequencing.
Acknowledgments
We thank members of the Zahrt laboratory and Dara Frank for useful discussions and collaborations. We apologize to any of our colleagues whose contributions to the field of Francisella research have been overlooked or we have been unable to cite.
Work on Francisella is sponsored by the Center of Biopreparedness and Infectious Disease at the Medical College of Wisconsin; the NIH/NIAID Regional Center of Excellence for Bio-defense and Emerging Infectious Diseases Research (RCE) Program, Region V “Great Lakes” RCE (NIH award 1-U54-AI-057153); and the National Institutes of Health and Infectious Diseases (RO1-AI-06344).
Biography
 Thomas C. Zahrt is an Associate Professor in the Department of Microbiology and Molecular Genetics and the Center for Biopreparedness and Infectious Diseases at the Medical College of Wisconsin. He received his B.A. from Kalamazoo College and his Ph.D. from the University of Illinois in Urbana-Champaign, and he conducted postdoctoral work at the University of Michigan Medical School in the laboratory of Dr. Vojo Deretic. Dr. Zahrt's interests include the study of intracellular bacterial pathogens and the regulatory factors utilized by these organisms to adapt within the host. In particular, Dr. Zahrt studies Mycobacterium tuberculosis and the importance of two-component signal transduction systems in the establishment and maintenance of this organism and in its reactivation from long-term persistent infection. Dr. Zahrt also studies Francisella tularensis pathogenesis, including the genetic programs necessary for growth and/or survival within tissues of the host, including macrophages and lung pneumocytes.
Thomas C. Zahrt is an Associate Professor in the Department of Microbiology and Molecular Genetics and the Center for Biopreparedness and Infectious Diseases at the Medical College of Wisconsin. He received his B.A. from Kalamazoo College and his Ph.D. from the University of Illinois in Urbana-Champaign, and he conducted postdoctoral work at the University of Michigan Medical School in the laboratory of Dr. Vojo Deretic. Dr. Zahrt's interests include the study of intracellular bacterial pathogens and the regulatory factors utilized by these organisms to adapt within the host. In particular, Dr. Zahrt studies Mycobacterium tuberculosis and the importance of two-component signal transduction systems in the establishment and maintenance of this organism and in its reactivation from long-term persistent infection. Dr. Zahrt also studies Francisella tularensis pathogenesis, including the genetic programs necessary for growth and/or survival within tissues of the host, including macrophages and lung pneumocytes.
 Roger Pechous obtained a B.S. in Biology from the University of Illinois at Champaign-Urbana and an M.S. in Biological Sciences from Illinois State University, analyzing the response of Staphylococcus aureus to antibiotic challenge in the laboratory of Dr. Radheshyam Jayaswal. He then obtained his Ph.D. in Microbiology and Molecular Genetics at the Medical College of Wisconsin in the laboratory of Dr. Thomas Zahrt, where he developed new genetic tools for Francisella tularensis and utilized these tools to generate live attenuated vaccine candidates and identify potential virulence determinants using in vivo expression technology. Dr. Pechous is currently a Postdoctoral Research Associate in the laboratory of Dr. Bill Goldman at the University of North Carolina at Chapel Hill, where he is studying the pathogenesis of primary pneumonic plague.
Roger Pechous obtained a B.S. in Biology from the University of Illinois at Champaign-Urbana and an M.S. in Biological Sciences from Illinois State University, analyzing the response of Staphylococcus aureus to antibiotic challenge in the laboratory of Dr. Radheshyam Jayaswal. He then obtained his Ph.D. in Microbiology and Molecular Genetics at the Medical College of Wisconsin in the laboratory of Dr. Thomas Zahrt, where he developed new genetic tools for Francisella tularensis and utilized these tools to generate live attenuated vaccine candidates and identify potential virulence determinants using in vivo expression technology. Dr. Pechous is currently a Postdoctoral Research Associate in the laboratory of Dr. Bill Goldman at the University of North Carolina at Chapel Hill, where he is studying the pathogenesis of primary pneumonic plague.
 Travis McCarthy became interested in microbe/host interactions as an undergraduate student at Wartburg College. He earned his Ph.D. from the University of Iowa in the laboratory of Dr. Larry Schlesinger, where he studied the involvement of mycobacterial phosphomannomutases in surface-associated mannoglycoconjugate biosynthesis and the importance of these molecules in interactions with host macrophage receptors. Dr. McCarthy is currently a postdoctoral fellow at the Medical College of Wisconsin in the laboratory of Dr. Thomas Zahrt, where he is studying genetic programs utilized by Francisella tularensis to grow and/or survive inside macrophages and mice.
Travis McCarthy became interested in microbe/host interactions as an undergraduate student at Wartburg College. He earned his Ph.D. from the University of Iowa in the laboratory of Dr. Larry Schlesinger, where he studied the involvement of mycobacterial phosphomannomutases in surface-associated mannoglycoconjugate biosynthesis and the importance of these molecules in interactions with host macrophage receptors. Dr. McCarthy is currently a postdoctoral fellow at the Medical College of Wisconsin in the laboratory of Dr. Thomas Zahrt, where he is studying genetic programs utilized by Francisella tularensis to grow and/or survive inside macrophages and mice.
REFERENCES
- 1.Reference deleted.
- 2.Abd, H., T. Johansson, I. Golovliov, G. Sandstrom, and M. Forsman. 2003. Survival and growth of Francisella tularensis in Acanthamoeba castellanii. Appl. Environ. Microbiol. 69:600-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alibek, K. 1999. Biohazard. Random House, New York, NY.
- 4.Alkhuder, K., K. L. Meibom, I. Dubail, M. Dupuis, and A. Charbit. 2009. Glutathione provides a source of cysteine essential for intracellular multiplication of Francisella tularensis. PLoS Pathog 5:e1000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ancuta, P., T. Pedron, R. Girard, G. Sandstrom, and R. Chaby. 1996. Inability of the Francisella tularensis lipopolysaccharide to mimic or to antagonize the induction of cell activation by endotoxins. Infect. Immun. 64:2041-2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andersson, H., B. Hartmanova, R. Kuolee, P. Ryden, W. Conlan, W. Chen, and A. Sjostedt. 2006. Transcriptional profiling of host responses in mouse lungs following aerosol infection with type A Francisella tularensis. J. Med. Microbiol. 55:263-271. [DOI] [PubMed] [Google Scholar]
- 7.Anthony, L. D., R. D. Burke, and F. E. Nano. 1991. Growth of Francisella spp. in rodent macrophages. Infect. Immun. 59:3291-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anthony, L. S., S. C. Cowley, K. E. Mdluli, and F. E. Nano. 1994. Isolation of a Francisella tularensis mutant that is sensitive to serum and oxidative killing and is avirulent in mice: correlation with the loss of MinD homologue expression. FEMS Microbiol. Lett. 124:157-165. [DOI] [PubMed] [Google Scholar]
- 9.Bakshi, C. S., M. Malik, M. Mahawar, G. S. Kirimanjeswara, K. R. Hazlett, L. E. Palmer, M. B. Furie, R. Singh, J. A. Melendez, T. J. Sellati, and D. W. Metzger. 2008. An improved vaccine for prevention of respiratory tularemia caused by Francisella tularensis SchuS4 strain. Vaccine 26:5276-5288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bakshi, C. S., M. Malik, K. Regan, J. A. Melendez, D. W. Metzger, V. M. Pavlov, and T. J. Sellati. 2006. Superoxide dismutase B gene (sodB)-deficient mutants of Francisella tularensis demonstrate hypersensitivity to oxidative stress and attenuated virulence. J. Bacteriol. 188:6443-6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balagopal, A., A. S. MacFarlane, N. Mohapatra, S. Soni, J. S. Gunn, and L. S. Schlesinger. 2006. Characterization of the receptor-ligand pathways important for entry and survival of Francisella tularensis in human macrophages. Infect. Immun. 74:5114-5125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baron, G. S., and F. E. Nano. 1998. MglA and MglB are required for the intramacrophage growth of Francisella novicida. Mol. Microbiol. 29:247-259. [DOI] [PubMed] [Google Scholar]
- 13.Baron, G. S., T. J. Reilly, and F. E. Nano. 1999. The respiratory burst-inhibiting acid phosphatase AcpA is not essential for the intramacrophage growth or virulence of Francisella novicida. FEMS Microbiol. Lett. 176:85-90. [DOI] [PubMed] [Google Scholar]
- 14.Berdal, B. P., R. Mehl, N. K. Meidell, A. M. Lorentzen-Styr, and O. Scheel. 1996. Field investigations of tularemia in Norway. FEMS Immunol. Med. Microbiol. 13:191-195. [DOI] [PubMed] [Google Scholar]
- 15.Bina, X. R., C. L. Lavine, M. A. Miller, and J. E. Bina. 2008. The AcrAB RND efflux system from the live vaccine strain of Francisella tularensis is a multiple drug efflux system that is required for virulence in mice. FEMS Microbiol. Lett. 279:226-233. [DOI] [PubMed] [Google Scholar]
- 16.Bosio, C. M., H. Bielefeldt-Ohmann, and J. T. Belisle. 2007. Active suppression of the pulmonary immune response by Francisella tularensis Schu4. J. Immunol. 178:4538-4547. [DOI] [PubMed] [Google Scholar]
- 17.Bosio, C. M., and S. W. Dow. 2005. Francisella tularensis induces aberrant activation of pulmonary dendritic cells. J. Immunol. 175:6792-6801. [DOI] [PubMed] [Google Scholar]
- 18.Boyce, J. M. 1975. Recent trends in the epidemiology of tularemia in the United States. J. Infect. Dis. 131:197-199. [DOI] [PubMed] [Google Scholar]
- 19.Broms, J. E., M. Lavander, and A. Sjostedt. 2009. A conserved alpha-helix essential for a type VI secretion-like system of Francisella tularensis. J. Bacteriol. 191:2431-2446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brotcke, A., and D. M. Monack. 2008. Identification of fevR, a novel regulator of virulence gene expression in Francisella novicida. Infect. Immun. 76:3473-3480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brotcke, A., D. S. Weiss, C. C. Kim, P. Chain, S. Malfatti, E. Garcia, and D. M. Monack. 2006. Identification of MglA-regulated genes reveals novel virulence factors in Francisella tularensis. Infect. Immun. 74:6642-6655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buchan, B. W., R. L. McCaffrey, S. R. Lindemann, L. A. Allen, and B. D. Jones. 2009. Identification of migR, a regulatory element of the Francisella tularensis live vaccine strain iglABCD virulence operon required for normal replication and trafficking in macrophages. Infect. Immun. 77:2517-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buchan, B. W., M. K. McLendon, and B. D. Jones. 2008. Identification of differentially regulated Francisella tularensis genes by use of a newly developed Tn5-based transposon delivery system. Appl. Environ. Microbiol. 74:2637-2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burke, D. S. 1977. Immunization against tularemia: analysis of the effectiveness of live Francisella tularensis vaccine in prevention of laboratory-acquired tularemia. J. Infect. Dis. 135:55-60. [DOI] [PubMed] [Google Scholar]
- 24a.Centers for Disease Control and Prevention. 1998. Summary of notifiable diseases, United States, 1997. MMWR Morb. Mortal. Wkly. Rep. 46:71-80. [PubMed] [Google Scholar]
- 25.Chakraborty, S., M. Monfett, T. M. Maier, J. L. Benach, D. W. Frank, and D. G. Thanassi. 2008. Type IV pili in Francisella tularensis: roles of pilF and pilT in fiber assembly, host cell adherence, and virulence. Infect. Immun. 76:2852-2861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Charity, J. C., M. M. Costante-Hamm, E. L. Balon, D. H. Boyd, E. J. Rubin, and S. L. Dove. 2007. Twin RNA polymerase-associated proteins control virulence gene expression in Francisella tularensis. PLoS Pathog. 3:e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Checroun, C., T. D. Wehrly, E. R. Fischer, S. F. Hayes, and J. Celli. 2006. Autophagy-mediated reentry of Francisella tularensis into the endocytic compartment after cytoplasmic replication. Proc. Natl. Acad. Sci. USA 103:14578-14583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen, W., R. Kuolee, J. W. Austin, H. Shen, Y. Che, and J. W. Conlan. 2005. Low dose aerosol infection of mice with virulent type A Francisella tularensis induces severe thymus atrophy and CD4+CD8+ thymocyte depletion. Microb. Pathog. 39:189-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chong, A., T. D. Wehrly, V. Nair, E. R. Fischer, J. R. Barker, K. E. Klose, and J. Celli. 2008. The early phagosomal stage of Francisella tularensis determines optimal phagosomal escape and Francisella pathogenicity island protein expression. Infect. Immun. 76:5488-5499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Christopher, G. W., T. J. Cieslak, J. A. Pavlin, and E. M. Eitzen, Jr. 1997. Biological warfare. A historical perspective. JAMA 278:412-417. [PubMed] [Google Scholar]
- 31.Clay, C. D., S. Soni, J. S. Gunn, and L. S. Schlesinger. 2008. Evasion of complement-mediated lysis and complement C3 deposition are regulated by Francisella tularensis lipopolysaccharide O antigen. J. Immunol. 181:5568-5578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clemens, D. L., and M. A. Horwitz. 2007. Uptake and intracellular fate of Francisella tularensis in human macrophages. Ann. N. Y. Acad. Sci. 1105:160-186. [DOI] [PubMed] [Google Scholar]
- 33.Clemens, D. L., B. Y. Lee, and M. A. Horwitz. 2005. Francisella tularensis enters macrophages via a novel process involving pseudopod loops. Infect. Immun. 73:5892-5902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clemens, D. L., B. Y. Lee, and M. A. Horwitz. 2009. Francisella tularensis phagosomal escape does not require acidification of the phagosome. Infect. Immun. 77:1757-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clemens, D. L., B. Y. Lee, and M. A. Horwitz. 2004. Virulent and avirulent strains of Francisella tularensis prevent acidification and maturation of their phagosomes and escape into the cytoplasm in human macrophages. Infect. Immun. 72:3204-3217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cole, L. E., K. L. Elkins, S. M. Michalek, N. Qureshi, L. J. Eaton, P. Rallabhandi, N. Cuesta, and S. N. Vogel. 2006. Immunologic consequences of Francisella tularensis live vaccine strain infection: role of the innate immune response in infection and immunity. J. Immunol. 176:6888-6899. [DOI] [PubMed] [Google Scholar]
- 37.Cole, L. E., K. A. Shirey, E. Barry, A. Santiago, P. Rallabhandi, K. L. Elkins, A. C. Puche, S. M. Michalek, and S. N. Vogel. 2007. Toll-like receptor 2-mediated signaling requirements for Francisella tularensis live vaccine strain infection of murine macrophages. Infect. Immun. 75:4127-4137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Collazo, C. M., A. Sher, A. I. Meierovics, and K. L. Elkins. 2006. Myeloid differentiation factor-88 (MyD88) is essential for control of primary in vivo Francisella tularensis LVS infection, but not for control of intra-macrophage bacterial replication. Microbes Infect. 8:779-790. [DOI] [PubMed] [Google Scholar]
- 39.Cong, Y., J. J. Yu, M. N. Guentzel, M. T. Berton, J. Seshu, K. E. Klose, and B. P. Arulanandam. 2009. Vaccination with a defined Francisella tularensis subsp. novicida pathogenicity island mutant (DeltaiglB) induces protective immunity against homotypic and heterotypic challenge. Vaccine 27:5554-5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39a.Conlan, J. W., and P. C. Oyston. 2007. Vaccines against Francisella tularensis. Ann. N. Y. Acad. Sci. 1105:325-350. [DOI] [PubMed] [Google Scholar]
- 39b.Conlan, J. W., H. Shen, R. Kuolee, X. Zhao, and W. Chen. 2005. Aerosol-, but not intradermal-immunization with the live vaccine strain of Francisella tularensis protects mice against subsequent aerosol challenge with a highly virulent type A strain of the pathogen by an alphabeta T cell- and interferon gamma-dependent mechanism. Vaccine 23:2477-2485. [DOI] [PubMed] [Google Scholar]
- 40.Conlan, J. W., W. Chen, H. Shen, A. Webb, and R. KuoLee. 2003. Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: bacteriologic and histopathologic studies. Microb. Pathog. 34:239-248. [DOI] [PubMed] [Google Scholar]
- 41.Conlan, J. W., R. KuoLee, H. Shen, and A. Webb. 2002. Different host defences are required to protect mice from primary systemic vs pulmonary infection with the facultative intracellular bacterial pathogen, Francisella tularensis LVS. Microb. Pathog. 32:127-134. [DOI] [PubMed] [Google Scholar]
- 42.Conlan, J. W., H. Shen, A. Webb, and M. B. Perry. 2002. Mice vaccinated with the O-antigen of Francisella tularensis LVS lipopolysaccharide conjugated to bovine serum albumin develop varying degrees of protective immunity against systemic or aerosol challenge with virulent type A and type B strains of the pathogen. Vaccine 20:3465-3471. [DOI] [PubMed] [Google Scholar]
- 43.Conlan, J. W., A. Sjostedt, and R. J. North. 1994. CD4+ and CD8+ T-cell-dependent and -independent host defense mechanisms can operate to control and resolve primary and secondary Francisella tularensis LVS infection in mice. Infect. Immun. 62:5603-5607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cowley, S. C., S. V. Myltseva, and F. E. Nano. 1996. Phase variation in Francisella tularensis affecting intracellular growth, lipopolysaccharide antigenicity and nitric oxide production. Mol. Microbiol. 20:867-874. [DOI] [PubMed] [Google Scholar]
- 45.Dahlstrand, S., O. Ringertz, and B. Zetterberg. 1971. Airborne tularemia in Sweden. Scand. J. Infect. Dis. 3:7-16. [DOI] [PubMed] [Google Scholar]
- 46.de Bruin, O. M., J. S. Ludu, and F. E. Nano. 2007. The Francisella pathogenicity island protein IglA localizes to the bacterial cytoplasm and is needed for intracellular growth. BMC Microbiol. 7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Deng, K., R. J. Blick, W. Liu, and E. J. Hansen. 2006. Identification of Francisella tularensis genes affected by iron limitation. Infect. Immun. 74:4224-4236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dennis, D. T. 1998. Tularemia, p. 354-357. In R. B. Wallace (ed.), Maxcy-Rosenau-Last public health and preventive medicine, 14th ed. Appleton & Lange, Stamford, CT.
- 49.Dennis, D. T., T. V. Inglesby, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, A. M. Friedlander, J. Hauer, M. Layton, S. R. Lillibridge, J. E. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2763-2773. [DOI] [PubMed] [Google Scholar]
- 50.Dienst, F. T., Jr. 1963. Tularemia: a perusal of three hundred thirty-nine cases. J. Louisiana State Med. Soc. 115:114-127. [PubMed] [Google Scholar]
- 51.Drabick, J. J., R. B. Narayanan, J. C. Williams, J. W. Leduc, and C. A. Nacy. 1994. Passive protection of mice against lethal Francisella tularensis (live tularemia vaccine strain) infection by the sera of human recipients of the live tularemia vaccine. Am. J. Med. Sci. 308:83-87. [DOI] [PubMed] [Google Scholar]
- 52.Eigelsbach, H. T., W. Braun, and R. D. Herring. 1951. Studies on the variation of Bacterium tularense. J. Bacteriol. 61:557-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eigelsbach, H. T., and C. M. Downs. 1961. Prophylactic effectiveness of live and killed tularemia vaccines. I. Production of vaccine and evaluation in the white mouse and guinea pig. J. Immunol. 87:415-425. [PubMed] [Google Scholar]
- 54.Elkins, K. L., S. C. Cowley, and C. M. Bosio. 2007. Innate and adaptive immunity to Francisella. Ann. N. Y. Acad. Sci. 1105:284-324. [DOI] [PubMed] [Google Scholar]
- 55.Elkins, K. L., T. Rhinehart-Jones, C. A. Nacy, R. K. Winegar, and A. H. Fortier. 1993. T-cell-independent resistance to infection and generation of immunity to Francisella tularensis. Infect. Immun. 61:823-829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Elkins, K. L., T. R. Rhinehart-Jones, S. J. Culkin, D. Yee, and R. K. Winegar. 1996. Minimal requirements for murine resistance to infection with Francisella tularensis LVS. Infect. Immun. 64:3288-3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ellis, J., P. C. Oyston, M. Green, and R. W. Titball. 2002. Tularemia. Clin. Microbiol. Rev. 15:631-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Evans, M. E., D. W. Gregory, W. Schaffner, and Z. A. McGee. 1985. Tularemia: a 30-year experience with 88 cases. Medicine 64:251-269. [PubMed] [Google Scholar]
- 59.Farlow, J., D. M. Wagner, M. Dukerich, M. Stanley, M. Chu, K. Kubota, J. Petersen, and P. Keim. 2005. Francisella tularensis in the United States. Emerg. Infect. Dis. 11:1835-1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Feldman, K. A. 2003. Tularemia. J. Am. Vet. Med. Assoc. 222:725-730. [DOI] [PubMed] [Google Scholar]
- 61.Feldman, K. A., R. E. Enscore, S. L. Lathrop, B. T. Matyas, M. McGuill, M. E. Schriefer, D. Stiles-Enos, D. T. Dennis, L. R. Petersen, and E. B. Hayes. 2001. An outbreak of primary pneumonic tularemia on Martha's Vineyard. N. Engl. J. Med. 345:1601-1606. [DOI] [PubMed] [Google Scholar]
- 62.Forestal, C. A., H. Gil, M. Monfett, C. E. Noah, G. J. Platz, D. G. Thanassi, J. L. Benach, and M. B. Furie. 2008. A conserved and immunodominant lipoprotein of Francisella tularensis is proinflammatory but not essential for virulence. Microb. Pathog. 44:512-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Forestal, C. A., M. Malik, S. V. Catlett, A. G. Savitt, J. L. Benach, T. J. Sellati, and M. B. Furie. 2007. Francisella tularensis has a significant extracellular phase in infected mice. J. Infect. Dis. 196:134-137. [DOI] [PubMed] [Google Scholar]
- 64.Forsberg, A., and T. Guina. 2007. Type II secretion and type IV pili of Francisella. Ann. N. Y. Acad. Sci. 1105:187-201. [DOI] [PubMed] [Google Scholar]
- 65.Forslund, A. L., K. Kuoppa, K. Svensson, E. Salomonsson, A. Johansson, M. Bystrom, P. C. Oyston, S. L. Michell, R. W. Titball, L. Noppa, E. Frithz-Lindsten, M. Forsman, and A. Forsberg. 2006. Direct repeat-mediated deletion of a type IV pilin gene results in major virulence attenuation of Francisella tularensis. Mol. Microbiol. 59:1818-1830. [DOI] [PubMed] [Google Scholar]
- 66.Fortier, A. H., S. J. Green, T. Polsinelli, T. R. Jones, R. M. Crawford, D. A. Leiby, K. L. Elkins, M. S. Meltzer, and C. A. Nacy. 1994. Life and death of an intracellular pathogen: Francisella tularensis and the macrophage. Immunol. Ser. 60:349-361. [PubMed] [Google Scholar]
- 67.Foshay, L., W. H. Hesselbrock, H. J. Wittenberg, and A. H. Rodenberg. 1942. Vaccine prophylaxis against tularemia in man. Am. J. Public Health Nations Health 32:1131-1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Francis, E. 1921. The occurence of tularaemia in man. Public Health Rep. 36:1731-1738.19314784 [Google Scholar]
- 69.Francis, E. 1928. A summary of present knowledge of tularemia. Medicine 7:411-432. [Google Scholar]
- 70.Francis, E. 1925. Tularemia. JAMA 84:1243-1250. [Google Scholar]
- 71.Frank, D. W., and T. C. Zahrt. 2007. Genetics and genetic manipulation in Francisella tularensis. Ann. N. Y. Acad. Sci. 1105:67-97. [DOI] [PubMed] [Google Scholar]
- 72.Fuller, J. R., R. R. Craven, J. D. Hall, T. M. Kijek, S. Taft-Benz, and T. H. Kawula. 2008. RipA, a cytoplasmic membrane protein conserved among Francisella species is required for intracellular survival. Infect. Immun. 76:4934-4943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fulop, M., R. Manchee, and R. Titball. 1995. Role of lipopolysaccharide and a major outer membrane protein from Francisella tularensis in the induction of immunity against tularemia. Vaccine 13:1220-1225. [DOI] [PubMed] [Google Scholar]
- 74.Fulop, M., P. Mastroeni, M. Green, and R. W. Titball. 2001. Role of antibody to lipopolysaccharide in protection against low- and high-virulence strains of Francisella tularensis. Vaccine 19:4465-4472. [DOI] [PubMed] [Google Scholar]
- 75.Gallagher, L. A., M. McKevitt, E. R. Ramage, and C. Manoil. 2008. Genetic dissection of the Francisella novicida restriction barrier. J. Bacteriol. 190:7830-7837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gallagher, L. A., E. Ramage, M. A. Jacobs, R. Kaul, M. Brittnacher, and C. Manoil. 2007. A comprehensive transposon mutant library of Francisella novicida, a bioweapon surrogate. Proc. Natl. Acad. Sci. USA 104:1009-1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gil, H., G. J. Platz, C. A. Forestal, M. Monfett, C. S. Bakshi, T. J. Sellati, M. B. Furie, J. L. Benach, and D. G. Thanassi. 2006. Deletion of TolC orthologs in Francisella tularensis identifies roles in multidrug resistance and virulence. Proc. Natl. Acad. Sci. USA 103:12897-12902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Golovliov, I., V. Baranov, Z. Krocova, H. Kovarova, and A. Sjostedt. 2003. An attenuated strain of the facultative intracellular bacterium Francisella tularensis can escape the phagosome of monocytic cells. Infect. Immun. 71:5940-5950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Golovliov, I., M. Ericsson, L. Akerblom, G. Sandstrom, A. Tarnvik, and A. Sjostedt. 1995. Adjuvanticity of ISCOMs incorporating a T cell-reactive lipoprotein of the facultative intracellular pathogen Francisella tularensis. Vaccine 13:261-267. [DOI] [PubMed] [Google Scholar]
- 80.Golovliov, I., M. Ericsson, G. Sandstrom, A. Tarnvik, and A. Sjostedt. 1997. Identification of proteins of Francisella tularensis induced during growth in macrophages and cloning of the gene encoding a prominently induced 23-kilodalton protein. Infect. Immun. 65:2183-2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Golovliov, I., G. Sandstrom, M. Ericsson, A. Sjostedt, and A. Tarnvik. 1995. Cytokine expression in the liver during the early phase of murine tularemia. Infect. Immun. 63:534-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Golovliov, I., A. Sjostedt, A. Mokrievich, and V. Pavlov. 2003. A method for allelic replacement in Francisella tularensis. FEMS Microbiol. Lett. 222:273-280. [DOI] [PubMed] [Google Scholar]
- 83.Gray, C. G., S. C. Cowley, K. K. Cheung, and F. E. Nano. 2002. The identification of five genetic loci of Francisella novicida associated with intracellular growth. FEMS Microbiol. Lett. 215:53-56. [DOI] [PubMed] [Google Scholar]
- 84.Griffin, K. F., P. C. Oyston, and R. W. Titball. 2007. Francisella tularensis vaccines. FEMS Immunol. Med. Microbiol. 49:315-323. [DOI] [PubMed] [Google Scholar]
- 85.Guina, T., D. Radulovic, A. J. Bahrami, D. L. Bolton, L. Rohmer, K. A. Jones-Isaac, J. Chen, L. A. Gallagher, B. Gallis, S. Ryu, G. K. Taylor, M. J. Brittnacher, C. Manoil, and D. R. Goodlett. 2007. MglA regulates Francisella tularensis subsp. novicida (Francisella novicida) response to starvation and oxidative stress. J. Bacteriol. 189:6580-6586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hager, A. J., D. L. Bolton, M. R. Pelletier, M. J. Brittnacher, L. A. Gallagher, R. Kaul, S. J. Skerrett, S. I. Miller, and T. Guina. 2006. Type IV pili-mediated secretion modulates Francisella virulence. Mol. Microbiol. 62:227-237. [DOI] [PubMed] [Google Scholar]
- 87.Harris, S. 1992. Japanese biological warfare research on humans: a case study of microbiology and ethics. Ann. N. Y. Acad. Sci. 666:21-52. [DOI] [PubMed] [Google Scholar]
- 88.Hartley, G., R. Taylor, J. Prior, S. Newstead, P. G. Hitchen, H. R. Morris, A. Dell, and R. W. Titball. 2006. Grey variants of the live vaccine strain of Francisella tularensis lack lipopolysaccharide O-antigen, show reduced ability to survive in macrophages and do not induce protective immunity in mice. Vaccine 24:989-996. [DOI] [PubMed] [Google Scholar]
- 89.Hood, A. M. 1977. Virulence factors of Francisella tularensis. J. Hyg. (London) 79:47-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hopla, C. E. 1955. The multiplication of tularemia organisms in the lone star tick. Am. J. Hyg. 61:371-380. [DOI] [PubMed] [Google Scholar]
- 91.Hopla, C. E., and A. K. Hopla. 1994. Tularemia, p. 113-126. In G. W. Beran and J. H. Steele (ed.), Handbook of zoonosis, 2nd ed. CRC Press, Boca Raton, FL.
- 92.Hornick, R. B., and H. T. Eigelsbach. 1966. Aerogenic immunization of man with live tularemia vaccine. Bacteriol. Rev. 30:532-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Horzempa, J., D. M. Tarwacki, P. E. Carlson, Jr., C. M. Robinson, and G. J. Nau. 2008. Characterization and application of a glucose-repressible promoter in Francisella tularensis. Appl. Environ. Microbiol. 74:2161-2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Huntley, J. F., P. G. Conley, D. A. Rasko, K. E. Hagman, M. A. Apicella, and M. V. Norgard. 2008. Native outer membrane proteins protect mice against pulmonary challenge with virulent type A Francisella tularensis. Infect. Immun. 76:3664-3671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ishihama, A., and T. Saitoh. 1979. Subunits of RNA polymerase in function and structure. IX. Regulation of RNA polymerase activity by stringent starvation protein (SSP). J. Mol. Biol. 129:517-530. [DOI] [PubMed] [Google Scholar]
- 96.Jellison, W. L. 1950. Tularemia; geographical distribution of deerfly fever and the biting fly, Chrysops discalis Williston. Public Health Rep. 65:1321-1329. [PubMed] [Google Scholar]
- 97.Jia, Q., B. Y. Lee, D. L. Clemens, R. A. Bowen, and M. A. Horwitz. 2009. Recombinant attenuated Listeria monocytogenes vaccine expressing Francisella tularensis IglC induces protection in mice against aerosolized type A F. tularensis. Vaccine 27:1216-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Johansson, A., J. Farlow, P. Larsson, M. Dukerich, E. Chambers, M. Bystrom, J. Fox, M. Chu, M. Forsman, A. Sjostedt, and P. Keim. 2004. Worldwide genetic relationships among Francisella tularensis isolates determined by multiple-locus variable-number tandem repeat analysis. J. Bacteriol. 186:5808-5818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kadull, P. J., H. R. Reames, L. L. Coriell, and L. Foshay. 1950. Studies on tularemia. V. Immunization of man. J. Immunol. 65:425-435. [PubMed] [Google Scholar]
- 100.Kadzhaev, K., C. Zingmark, I. Golovliov, M. Bolanowski, H. Shen, W. Conlan, and A. Sjostedt. 2009. Identification of genes contributing to the virulence of Francisella tularensis SCHU S4 in a mouse intradermal infection model. PLoS One 4:e5463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kanistanon, D., A. M. Hajjar, M. R. Pelletier, L. A. Gallagher, T. Kalhorn, S. A. Shaffer, D. R. Goodlett, L. Rohmer, M. J. Brittnacher, S. J. Skerrett, and R. K. Ernst. 2008. A Francisella mutant in lipid A carbohydrate modification elicits protective immunity. PLoS Pathog. 4:e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kaufmann, A. F., M. I. Meltzer, and G. P. Schmid. 1997. The economic impact of a bioterrorist attack: are prevention and postattack intervention programs justifiable? Emerg. Infect. Dis. 3:83-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kawula, T. H., J. D. Hall, J. R. Fuller, and R. R. Craven. 2004. Use of transposon-transposase complexes to create stable insertion mutant strains of Francisella tularensis LVS. Appl. Environ. Microbiol. 70:6901-6904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Keim, P., A. Johansson, and D. M. Wagner. 2007. Molecular epidemiology, evolution, and ecology of Francisella. Ann. N. Y. Acad. Sci. 1105:30-66. [DOI] [PubMed] [Google Scholar]
- 105.Kiss, K., W. Liu, J. F. Huntley, M. V. Norgard, and E. J. Hansen. 2008. Characterization of fig operon mutants of Francisella novicida U112. FEMS Microbiol. Lett. 285:270-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kraemer, P. S., A. Mitchell, M. R. Pelletier, L. A. Gallagher, M. Wasnick, L. Rohmer, M. J. Brittnacher, C. Manoil, S. J. Skerett, and N. R. Salama. 2009. Genome-wide screen in Francisella novicida for genes required for pulmonary and systemic infection in mice. Infect. Immun. 77:232-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kroca, M., A. Tarnvik, and A. Sjostedt. 2000. The proportion of circulating gammadelta T cells increases after the first week of onset of tularaemia and remains elevated for more than a year. Clin. Exp. Immunol. 120:280-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kuoppa, K., A. Forsberg, and A. Norqvist. 2001. Construction of a reporter plasmid for screening in vivo promoter activity in Francisella tularensis. FEMS Microbiol. Lett. 205:77-81. [DOI] [PubMed] [Google Scholar]
- 109.Larsson, P., P. C. Oyston, P. Chain, M. C. Chu, M. Duffield, H. H. Fuxelius, E. Garcia, G. Halltorp, D. Johansson, K. E. Isherwood, P. D. Karp, E. Larsson, Y. Liu, S. Michell, J. Prior, R. Prior, S. Malfatti, A. Sjostedt, K. Svensson, N. Thompson, L. Vergez, J. K. Wagg, B. W. Wren, L. E. Lindler, S. G. Andersson, M. Forsman, and R. W. Titball. 2005. The complete genome sequence of Francisella tularensis, the causative agent of tularemia. Nat. Genet. 37:153-159. [DOI] [PubMed] [Google Scholar]
- 110.Lauriano, C. M., J. R. Barker, F. E. Nano, B. P. Arulanandam, and K. E. Klose. 2003. Allelic exchange in Francisella tularensis using PCR products. FEMS Microbiol. Lett. 229:195-202. [DOI] [PubMed] [Google Scholar]
- 111.Lauriano, C. M., J. R. Barker, S. S. Yoon, F. E. Nano, B. P. Arulanandam, D. J. Hassett, and K. E. Klose. 2004. MglA regulates transcription of virulence factors necessary for Francisella tularensis intraamoebae and intramacrophage survival. Proc. Natl. Acad. Sci. USA 101:4246-4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Leiby, D. A., A. H. Fortier, R. M. Crawford, R. D. Schreiber, and C. A. Nacy. 1992. In vivo modulation of the murine immune response to Francisella tularensis LVS by administration of anticytokine antibodies. Infect. Immun. 60:84-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lenco, J., M. Hubalek, P. Larsson, A. Fucikova, M. Brychta, A. Macela, and J. Stulik. 2007. Proteomics analysis of the Francisella tularensis LVS response to iron restriction: induction of the F. tularensis pathogenicity island proteins IglABC. FEMS Microbiol. Lett. 269:11-21. [DOI] [PubMed] [Google Scholar]
- 114.Li, H., S. Nookala, X. R. Bina, J. E. Bina, and F. Re. 2006. Innate immune response to Francisella tularensis is mediated by TLR2 and caspase-1 activation. J. Leukoc. Biol. 80:766-773. [DOI] [PubMed] [Google Scholar]
- 115.Li, J., C. Ryder, M. Mandal, F. Ahmed, P. Azadi, D. S. Snyder, R. D. Pechous, T. Zahrt, and T. J. Inzana. 2007. Attenuation and protective efficacy of an O-antigen-deficient mutant of Francisella tularensis LVS. Microbiology 153:3141-3153. [DOI] [PubMed] [Google Scholar]
- 116.Lillie, R. D., and E. I. Francis. 1937. The pathology of tularemia in man (Homo sapiens). NIH Bull. 167:1-81. [Google Scholar]
- 117.Lindgren, H., I. Golovliov, V. Baranov, R. K. Ernst, M. Telepnev, and A. Sjostedt. 2004. Factors affecting the escape of Francisella tularensis from the phagolysosome. J. Med. Microbiol. 53:953-958. [DOI] [PubMed] [Google Scholar]
- 118.Lopez, M. C., N. S. Duckett, S. D. Baron, and D. W. Metzger. 2004. Early activation of NK cells after lung infection with the intracellular bacterium, Francisella tularensis LVS. Cell. Immunol. 232:75-85. [DOI] [PubMed] [Google Scholar]
- 119.LoVullo, E. D., C. R. Molins-Schneekloth, H. P. Schweizer, and M. S. Pavelka, Jr. 2009. Single-copy chromosomal integration systems for Francisella tularensis. Microbiology 155:1152-1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.LoVullo, E. D., L. A. Sherrill, and M. S. Pavelka, Jr. 2009. Improved shuttle vectors for Francisella tularensis genetics. FEMS Microbiol. Lett. 291:95-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.LoVullo, E. D., L. A. Sherrill, L. L. Perez, and M. S. Pavelka, Jr. 2006. Genetic tools for highly pathogenic Francisella tularensis subsp. tularensis. Microbiology 152:3425-3435. [DOI] [PubMed] [Google Scholar]
- 122.Ludu, J. S., O. M. de Bruin, B. N. Duplantis, C. L. Schmerk, A. Y. Chou, K. L. Elkins, and F. E. Nano. 2008. The Francisella pathogenicity island protein PdpD is required for full virulence and associates with homologues of the type VI secretion system. J. Bacteriol. 190:4584-4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mahawar, M., G. S. Kirimanjeswara, D. W. Metzger, and C. S. Bakshi. 2009. Contribution of citrulline ureidase to Francisella tularensis strain Schu S4 pathogenesis. J. Bacteriol. 191:4798-4806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Maier, T. M., M. S. Casey, R. H. Becker, C. W. Dorsey, E. M. Glass, N. Maltsev, T. C. Zahrt, and D. W. Frank. 2007. Identification of Francisella tularensis Himar1-based transposon mutants defective for replication in macrophages. Infect. Immun. 75:5376-5389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Maier, T. M., A. Havig, M. Casey, F. E. Nano, D. W. Frank, and T. C. Zahrt. 2004. Construction and characterization of a highly efficient Francisella shuttle plasmid. Appl. Environ. Microbiol. 70:7511-7519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Maier, T. M., R. Pechous, M. Casey, T. C. Zahrt, and D. W. Frank. 2006. In vivo Himar1-based transposon mutagenesis of Francisella tularensis. Appl. Environ. Microbiol. 72:1878-1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.McCaffrey, R. L., and L. A. Allen. 2006. Francisella tularensis LVS evades killing by human neutrophils via inhibition of the respiratory burst and phagosome escape. J. Leukoc. Biol. 80:1224-1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.McLendon, M. K., B. Schilling, J. R. Hunt, M. A. Apicella, and B. W. Gibson. 2007. Identification of LpxL, a late acyltransferase of Francisella tularensis. Infect. Immun. 75:5518-5531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Meibom, K. L., I. Dubail, M. Dupuis, M. Barel, J. Lenco, J. Stulik, I. Golovliov, A. Sjostedt, and A. Charbit. 2008. The heat-shock protein ClpB of Francisella tularensis is involved in stress tolerance and is required for multiplication in target organs of infected mice. Mol. Microbiol. 67:1384-1401. [DOI] [PubMed] [Google Scholar]
- 130.Metzger, D. W., C. S. Bakshi, and G. Kirimanjeswara. 2007. Mucosal immunopathogenesis of Francisella tularensis. Ann. N. Y. Acad. Sci. 1105:266-283. [DOI] [PubMed] [Google Scholar]
- 131.Miller, S. I., R. K. Ernst, and M. W. Bader. 2005. LPS, TLR4 and infectious disease diversity. Nat. Rev. Microbiol. 3:36-46. [DOI] [PubMed] [Google Scholar]
- 132.Milne, T. S., S. L. Michell, H. Diaper, P. Wikstrom, K. Svensson, P. C. Oyston, and R. W. Titball. 2007. A 55 kDa hypothetical membrane protein is an iron-regulated virulence factor of Francisella tularensis subsp. novicida U112. J. Med. Microbiol. 56:1268-1276. [DOI] [PubMed] [Google Scholar]
- 133.Mohapatra, N. P., A. Balagopal, S. Soni, L. S. Schlesinger, and J. S. Gunn. 2007. AcpA is a Francisella acid phosphatase that affects intramacrophage survival and virulence. Infect. Immun. 75:390-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mohapatra, N. P., S. Soni, B. L. Bell, R. Warren, R. K. Ernst, A. Muszynski, R. W. Carlson, and J. S. Gunn. 2007. Identification of an orphan response regulator required for the virulence of Francisella spp. and transcription of pathogenicity island genes. Infect. Immun. 75:3305-3314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mohapatra, N. P., S. Soni, T. J. Reilly, J. Liu, K. E. Klose, and J. S. Gunn. 2008. Combined deletion of four Francisella novicida acid phosphatases attenuates virulence and macrophage vacuolar escape. Infect. Immun. 76:3690-3699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Morner, T. 1992. The ecology of tularaemia. Rev. Sci. Tech. 11:1123-1130. [PubMed] [Google Scholar]
- 137.Nano, F. E., and C. Schmerk. 2007. The Francisella pathogenicity island. Ann. N. Y. Acad. Sci. 1105:122-137. [DOI] [PubMed] [Google Scholar]
- 138.Nano, F. E., N. Zhang, S. C. Cowley, K. E. Klose, K. K. Cheung, M. J. Roberts, J. S. Ludu, G. W. Letendre, A. I. Meierovics, G. Stephens, and K. L. Elkins. 2004. A Francisella tularensis pathogenicity island required for intramacrophage growth. J. Bacteriol. 186:6430-6436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Norqvist, A., K. Kuoppa, and G. Sandstrom. 1996. Construction of a shuttle vector for use in Francisella tularensis. FEMS Immunol. Med. Microbiol. 13:257-260. [DOI] [PubMed] [Google Scholar]
- 140.Oyston, P. C., and J. E. Quarry. 2005. Tularemia vaccine: past, present and future. Antonie van Leeuwenhoek 87:277-281. [DOI] [PubMed] [Google Scholar]
- 141.Oyston, P. C., A. Sjostedt, and R. W. Titball. 2004. Tularaemia: bioterrorism defence renews interest in Francisella tularensis. Nat. Rev. Microbiol. 2:967-978. [DOI] [PubMed] [Google Scholar]
- 142.Pammit, M. A., E. K. Raulie, C. M. Lauriano, K. E. Klose, and B. P. Arulanandam. 2006. Intranasal vaccination with a defined attenuated Francisella novicida strain induces gamma interferon-dependent antibody-mediated protection against tularemia. Infect. Immun. 74:2063-2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Pavlov, V. M., A. N. Mokrievich, and K. Volkovoy. 1996. Cryptic plasmid pFNL10 from Francisella novicida-like F6168: the base of plasmid vectors for Francisella tularensis. FEMS Immunol. Med. Microbiol. 13:253-256. [DOI] [PubMed] [Google Scholar]
- 144.Pavlov, V. M., I. V. Rodionova, A. N. Mokrievich, and I. S. Meshcheriakova. 1994. Isolation and molecular-genetic characteristic of a cryptic plasmid from the Francisella novicida like F6168 strain. Mol. Gen. Mikrobiol Virusol. 3:39-40. [PubMed] [Google Scholar]
- 145.Pechous, R., J. Celli, R. Penoske, S. F. Hayes, D. W. Frank, and T. C. Zahrt. 2006. Construction and characterization of an attenuated purine auxotroph in a Francisella tularensis live vaccine strain. Infect. Immun. 74:4452-4461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Pechous, R. D., T. R. McCarthy, N. P. Mohapatra, S. Soni, R. M. Penoske, N. H. Salzman, D. W. Frank, J. S. Gunn, and T. C. Zahrt. 2008. A Francisella tularensis Schu S4 purine auxotroph is highly attenuated in mice but offers limited protection against homologous intranasal challenge. PLoS One 3:e2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Petersen, J. M., and M. E. Schriefer. 2005. Tularemia: emergence/re-emergence. Vet. Res. 36:455-467. [DOI] [PubMed] [Google Scholar]
- 148.Petrosino, J. F., Q. Xiang, S. E. Karpathy, H. Jiang, S. Yerrapragada, Y. Liu, J. Gioia, L. Hemphill, A. Gonzalez, T. M. Raghavan, A. Uzman, G. E. Fox, S. Highlander, M. Reichard, R. J. Morton, K. D. Clinkenbeard, and G. M. Weinstock. 2006. Chromosome rearrangement and diversification of Francisella tularensis revealed by the type B (OSU18) genome sequence. J. Bacteriol. 188:6977-6985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Petrov, V. G. 1960. Experimental study of Dermacentor marginatus Sulz. and Rhipicephalus rossicus Jak. et K. Jak. ticks as vectors of tularemia. J. Parasitol. 46:877-884. [PubMed] [Google Scholar]
- 150.Phillips, N. J., B. Schilling, M. K. McLendon, M. A. Apicella, and B. W. Gibson. 2004. Novel modification of lipid A of Francisella tularensis. Infect. Immun. 72:5340-5348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Pierini, L. M. 2006. Uptake of serum-opsonized Francisella tularensis by macrophages can be mediated by class A scavenger receptors. Cell. Microbiol. 8:1361-1370. [DOI] [PubMed] [Google Scholar]
- 152.Reference deleted.
- 153.Proft, T., and E. N. Baker. 2009. Pili in Gram-negative and Gram-positive bacteria—structure, assembly and their role in disease. Cell Mol. Life Sci. 66:613-635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Pullen, R. L., and B. M. Stuart. 1945. Tularemia: analysis of 225 cases. JAMA 129:495-500. [Google Scholar]
- 155.Qin, A., and B. J. Mann. 2006. Identification of transposon insertion mutants of Francisella tularensis tularensis strain Schu S4 deficient in intracellular replication in the hepatic cell line HepG2. BMC Microbiol. 6:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Qin, A., D. W. Scott, and B. J. Mann. 2008. Francisella tularensis subsp. tularensis Schu S4 disulfide bond formation protein B, but not an RND-type efflux pump, is required for virulence. Infect. Immun. 76:3086-3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Qin, A., D. W. Scott, J. A. Thompson, and B. J. Mann. 2009. Identification of an essential Francisella tularensis subsp. tularensis virulence factor. Infect. Immun. 77:152-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Quarry, J. E., K. E. Isherwood, S. L. Michell, H. Diaper, R. W. Titball, and P. C. Oyston. 2007. A Francisella tularensis subspecies novicida purF mutant, but not a purA mutant, induces protective immunity to tularemia in mice. Vaccine 25:2011-2018. [DOI] [PubMed] [Google Scholar]
- 159.Ramakrishnan, G., A. Meeker, and B. Dragulev. 2008. fslE is necessary for siderophore-mediated iron acquisition in Francisella tularensis Schu S4. J. Bacteriol. 190:5353-5361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Raynaud, C., K. L. Meibom, M. A. Lety, I. Dubail, T. Candela, E. Frapy, and A. Charbit. 2007. Role of the wbt locus of Francisella tularensis in lipopolysaccharide O-antigen biogenesis and pathogenicity. Infect. Immun. 75:536-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Read, A., S. J. Vogl, K. Hueffer, L. A. Gallagher, and G. M. Happ. 2008. Francisella genes required for replication in mosquito cells. J. Med. Entomol. 45:1108-1116. [DOI] [PubMed] [Google Scholar]
- 162.Rodriguez, S. A., G. Davis, and K. E. Klose. 2009. Targeted gene disruption in Francisella tularensis by group II introns. Methods 49:270-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Rodriguez, S. A., J. J. Yu, G. Davis, B. P. Arulanandam, and K. E. Klose. 2008. Targeted inactivation of Francisella tularensis genes by group II introns. Appl. Environ. Microbiol. 74:2619-2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Salomonsson, E. M., A. Forsberg, N. Roos, C. Holz, B. Maier, M. Koomey, and H. C. Winther-Larsen. 2009. Functional analyses of pilin-like proteins from Francisella species: complementation of type IV pilus phenotypes in Neisseria gonorrhoeae. Microbiology 155:2546-2559. [DOI] [PubMed] [Google Scholar]
- 165.Sammons-Jackson, W. L., K. McClelland, J. N. Manch-Citron, D. W. Metzger, C. S. Bakshi, E. Garcia, A. Rasley, and B. E. Anderson. 2008. Generation and characterization of an attenuated mutant in a response regulator gene of Francisella tularensis live vaccine strain (LVS). DNA Cell Biol. 27:387-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sandstrom, G., S. Lofgren, and A. Tarnvik. 1988. A capsule-deficient mutant of Francisella tularensis LVS exhibits enhanced sensitivity to killing by serum but diminished sensitivity to killing by polymorphonuclear leukocytes. Infect. Immun. 56:1194-1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Sandstrom, G., A. Sjostedt, T. Johansson, K. Kuoppa, and J. C. Williams. 1992. Immunogenicity and toxicity of lipopolysaccharide from Francisella tularensis LVS. FEMS Microbiol. Immunol. 5:201-210. [DOI] [PubMed] [Google Scholar]
- 168.Sandstrom, G., A. Tarnvik, and H. Wolf-Watz. 1987. Immunospecific T-lymphocyte stimulation by membrane proteins from Francisella tularensis. J. Clin. Microbiol. 25:641-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sandstrom, G., A. Tarnvik, H. Wolf-Watz, and S. Lofgren. 1984. Antigen from Francisella tularensis: nonidentity between determinants participating in cell-mediated and humoral reactions. Infect. Immun. 45:101-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Santiago, A. E., L. E. Cole, A. Franco, S. N. Vogel, M. M. Levine, and E. M. Barry. 2009. Characterization of rationally attenuated Francisella tularensis vaccine strains that harbor deletions in the guaA and guaB genes. Vaccine 27:2426-2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Santic, M., R. Asare, I. Skrobonja, S. Jones, and Y. Abu Kwaik. 2008. Acquisition of the vacuolar ATPase proton pump and phagosome acidification are essential for escape of Francisella tularensis into the macrophage cytosol. Infect. Immun. 76:2671-2677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Santic, M., M. Molmeret, J. R. Barker, K. E. Klose, A. Dekanic, M. Doric, and Y. Abu Kwaik. 2007. A Francisella tularensis pathogenicity island protein essential for bacterial proliferation within the host cell cytosol. Cell. Microbiol. 9:2391-2403. [DOI] [PubMed] [Google Scholar]
- 173.Santic, M., M. Molmeret, K. E. Klose, S. Jones, and Y. A. Kwaik. 2005. The Francisella tularensis pathogenicity island protein IglC and its regulator MglA are essential for modulating phagosome biogenesis and subsequent bacterial escape into the cytoplasm. Cell. Microbiol. 7:969-979. [DOI] [PubMed] [Google Scholar]
- 174.Saslaw, S., H. T. Eigelsbach, J. A. Prior, H. E. Wilson, and S. Carhart. 1961. Tularemia vaccine study. II. Respiratory challenge. Arch. Intern. Med. 107:702-714. [DOI] [PubMed] [Google Scholar]
- 175.Saslaw, S., H. T. Eigelsbach, H. E. Wilson, J. A. Prior, and S. Carhart. 1961. Tularemia vaccine study. I. Intracutaneous challenge. Arch. Intern. Med. 107:689-701. [DOI] [PubMed] [Google Scholar]
- 176.Schmerk, C. L., B. N. Duplantis, P. L. Howard, and F. E. Nano. 2009. A Francisella novicida pdpA mutant exhibits limited intracellular replication and remains associated with the lysosomal marker LAMP-1. Microbiology 155:1498-1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Schmerk, C. L., B. N. Duplantis, D. Wang, R. D. Burke, A. Y. Chou, K. L. Elkins, J. S. Ludu, and F. E. Nano. 2009. Characterization of the pathogenicity island protein PdpA and its role in the virulence of Francisella novicida. Microbiology 155:1489-1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Schulert, G. S., and L. A. Allen. 2006. Differential infection of mononuclear phagocytes by Francisella tularensis: role of the macrophage mannose receptor. J. Leukoc. Biol. 80:563-571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Schulert, G. S., R. L. McCaffrey, B. W. Buchan, S. R. Lindemann, C. Hollenback, B. D. Jones, and L. A. Allen. 2009. Francisella tularensis genes required for inhibition of the neutrophil respiratory burst and intramacrophage growth identified by random transposon mutagenesis of strain LVS. Infect. Immun. 77:1324-1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sebastian, S., S. T. Dillon, J. G. Lynch, L. T. Blalock, E. Balon, K. T. Lee, L. E. Comstock, J. W. Conlan, E. J. Rubin, A. O. Tzianabos, and D. L. Kasper. 2007. A defined O-antigen polysaccharide mutant of Francisella tularensis live vaccine strain has attenuated virulence while retaining its protective capacity. Infect. Immun. 75:2591-2602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Sharma, J., Q. Li, B. B. Mishra, C. Pena, and J. M. Teale. 2009. Lethal pulmonary infection with Francisella novicida is associated with severe sepsis. J. Leukoc. Biol. 86:491-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Shen, H., W. Chen, and J. W. Conlan. 2004. Mice sublethally infected with Francisella novicida U112 develop only marginal protective immunity against systemic or aerosol challenge with virulent type A or B strains of F. tularensis. Microb. Pathog. 37:107-110. [DOI] [PubMed] [Google Scholar]
- 183.Sjostedt, A. 2007. Tularemia: history, epidemiology, pathogen physiology, and clinical manifestations. Ann. N. Y. Acad. Sci. 1105:1-29. [DOI] [PubMed] [Google Scholar]
- 184.Sjostedt, A., J. W. Conlan, and R. J. North. 1994. Neutrophils are critical for host defense against primary infection with the facultative intracellular bacterium Francisella tularensis in mice and participate in defense against reinfection. Infect. Immun. 62:2779-2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Sjostedt, A., M. Eriksson, G. Sandstrom, and A. Tarnvik. 1992. Various membrane proteins of Francisella tularensis induce interferon-gamma production in both CD4+ and CD8+ T cells of primed humans. Immunology 76:584-592. [PMC free article] [PubMed] [Google Scholar]
- 186.Sjostedt, A., G. Sandstrom, and A. Tarnvik. 1992. Humoral and cell-mediated immunity in mice to a 17-kilodalton lipoprotein of Francisella tularensis expressed by Salmonella typhimurium. Infect. Immun. 60:2855-2862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Staples, J. E., K. A. Kubota, L. G. Chalcraft, P. S. Mead, and J. M. Petersen. 2006. Epidemiologic and molecular analysis of human tularemia, United States, 1964-2004. Emerg. Infect. Dis. 12:1113-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Stenmark, S., H. Lindgren, A. Tarnvik, and A. Sjostedt. 2003. Specific antibodies contribute to the host protection against strains of Francisella tularensis subspecies holarctica. Microb. Pathog. 35:73-80. [DOI] [PubMed] [Google Scholar]
- 189.Stenmark, S., D. Sunnemark, A. Bucht, and A. Sjostedt. 1999. Rapid local expression of interleukin-12, tumor necrosis factor alpha, and gamma interferon after cutaneous Francisella tularensis infection in tularemia-immune mice. Infect. Immun. 67:1789-1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Stuart, B. M., and R. L. Pullen. 1945. Tularemia pneumonia: review of American literature and report of 15 additional cases. Am. J. Med. Sci. 210:223-236. [Google Scholar]
- 191.Su, J., J. Yang, D. Zhao, T. H. Kawula, J. A. Banas, and J. R. Zhang. 2007. Genome-wide identification of Francisella tularensis virulence determinants. Infect. Immun. 75:3089-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Sumida, T., T. Maeda, H. Takahashi, S. Yoshida, F. Yonaha, A. Sakamoto, H. Tomioka, and T. Koike. 1992. Predominant expansion of V gamma 9/V delta 2 T cells in a tularemia patient. Infect. Immun. 60:2554-2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Surcel, H. M., M. Sarvas, I. M. Helander, and E. Herva. 1989. Membrane proteins of Francisella tularensis LVS differ in ability to induce proliferation of lymphocytes from tularemia-vaccinated individuals. Microb. Pathog. 7:411-419. [DOI] [PubMed] [Google Scholar]
- 194.Svensson, K., P. Larsson, D. Johansson, M. Bystrom, M. Forsman, and A. Johansson. 2005. Evolution of subspecies of Francisella tularensis. J. Bacteriol. 187:3903-3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Tarnvik, A., and L. Berglund. 2003. Tularaemia. Eur. Respir. J. 21:361-373. [DOI] [PubMed] [Google Scholar]
- 196.Tarnvik, A., G. Sandstrom, and A. Sjostedt. 1996. Epidemiological analysis of tularemia in Sweden 1931-1993. FEMS Immunol. Med. Microbiol. 13:201-204. [DOI] [PubMed] [Google Scholar]
- 197.Taylor, J. P., G. R. Istre, T. C. McChesney, F. T. Satalowich, R. L. Parker, and L. M. McFarland. 1991. Epidemiologic characteristics of human tularemia in the southwest-central states, 1981-1987. Am. J. Epidemiol. 133:1032-1038. [DOI] [PubMed] [Google Scholar]
- 198.Telepnev, M., I. Golovliov, T. Grundstrom, A. Tarnvik, and A. Sjostedt. 2003. Francisella tularensis inhibits Toll-like receptor-mediated activation of intracellular signalling and secretion of TNF-alpha and IL-1 from murine macrophages. Cell. Microbiol. 5:41-51. [DOI] [PubMed] [Google Scholar]
- 199.Tempel, R., X. H. Lai, L. Crosa, B. Kozlowicz, and F. Heffron. 2006. Attenuated Francisella novicida transposon mutants protect mice against wild-type challenge. Infect. Immun. 74:5095-5105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Thomas, R. M., R. W. Titball, P. C. Oyston, K. Griffin, E. Waters, P. G. Hitchen, S. L. Michell, I. D. Grice, J. C. Wilson, and J. L. Prior. 2007. The immunologically distinct O antigens from Francisella tularensis subspecies tularensis and Francisella novicida are both virulence determinants and protective antigens. Infect. Immun. 75:371-378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Tigertt, W. D. 1962. Soviet viable Pasteurella tularensis vaccines. A review of selected articles. Bacteriol. Rev. 26:354-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Titball, R. W., A. Johansson, and M. Forsman. 2003. Will the enigma of Francisella tularensis virulence soon be solved? Trends Microbiol. 11:118-123. [DOI] [PubMed] [Google Scholar]
- 203.Titball, R. W., and J. F. Petrosino. 2007. Francisella tularensis genomics and proteomics. Ann. N. Y. Acad. Sci. 1105:98-121. [DOI] [PubMed] [Google Scholar]
- 204.Twine, S., M. Bystrom, W. Chen, M. Forsman, I. Golovliov, A. Johansson, J. Kelly, H. Lindgren, K. Svensson, C. Zingmark, W. Conlan, and A. Sjostedt. 2005. A mutant of Francisella tularensis strain SCHU S4 lacking the ability to express a 58-kilodalton protein is attenuated for virulence and is an effective live vaccine. Infect. Immun. 73:8345-8352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Van Metre, T. E., Jr., and P. J. Kadull. 1959. Laboratory-acquired tularemia in vaccinated individuals: a report of 62 cases. Ann. Intern. Med. 50:621-632. [DOI] [PubMed] [Google Scholar]
- 206.Vinogradov, E., M. B. Perry, and J. W. Conlan. 2002. Structural analysis of Francisella tularensis lipopolysaccharide. Eur. J. Biochem. 269:6112-6118. [DOI] [PubMed] [Google Scholar]
- 207.Vonkavaara, M., M. V. Telepnev, P. Ryden, A. Sjostedt, and S. Stoven. 2008. Drosophila melanogaster as a model for elucidating the pathogenicity of Francisella tularensis. Cell. Microbiol. 10:1327-1338. [DOI] [PubMed] [Google Scholar]
- 208.Wang, X., S. C. McGrath, R. J. Cotter, and C. R. Raetz. 2006. Expression cloning and periplasmic orientation of the Francisella novicida lipid A 4′-phosphatase LpxF. J. Biol. Chem. 281:9321-9330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Wang, X., A. A. Ribeiro, Z. Guan, S. N. Abraham, and C. R. Raetz. 2007. Attenuated virulence of a Francisella mutant lacking the lipid A 4′-phosphatase. Proc. Natl. Acad. Sci. USA 104:4136-4141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Reference deleted.
- 211.Reference deleted.
- 212.Wehrly, T. D., A. Chong, K. Virtaneva, D. E. Sturdevant, R. Child, J. A. Edwards, D. Brouwer, V. Nair, E. R. Fischer, L. Wicke, A. J. Curda, J. J. Kupko III, C. Martens, D. D. Crane, C. M. Bosio, S. F. Porcella, and J. Celli. 2009. Intracellular biology and virulence determinants of Francisella tularensis revealed by transcriptional profiling inside macrophages. Cell. Microbiol. 11:1128-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Weiss, D. S., A. Brotcke, T. Henry, J. J. Margolis, K. Chan, and D. M. Monack. 2007. In vivo negative selection screen identifies genes required for Francisella virulence. Proc. Natl. Acad. Sci. USA 104:6037-6042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.West, T. E., M. R. Pelletier, M. C. Majure, A. Lembo, A. M. Hajjar, and S. J. Skerrett. 2008. Inhalation of Francisella novicida ΔmglA causes replicative infection that elicits innate and adaptive responses but is not protective against invasive pneumonic tularemia. Microbes Infect. 10:773-780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Wherry, W. B., and B. H. Lamb. 1914. Infection of man with Bacterium tularense. J. Infect. Dis. 15:331-340. [DOI] [PubMed] [Google Scholar]
- 216.Whipp, M. J., J. M. Davis, G. Lum, J. de Boer, Y. Zhou, S. W. Bearden, J. M. Petersen, M. C. Chu, and G. Hogg. 2003. Characterization of a novicida-like subspecies of Francisella tularensis isolated in Australia. J. Med. Microbiol. 52:839-842. [DOI] [PubMed] [Google Scholar]
- 217.Wickstrum, J. R., K. J. Hong, S. Bokhari, N. Reed, N. McWilliams, R. T. Horvat, and M. J. Parmely. 2007. Coactivating signals for the hepatic lymphocyte gamma interferon response to Francisella tularensis. Infect. Immun. 75:1335-1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Williams, M. D., T. X. Ouyang, and M. C. Flickinger. 1994. Starvation-induced expression of SspA and SspB: the effects of a null mutation in sspA on Escherichia coli protein synthesis and survival during growth and prolonged starvation. Mol. Microbiol. 11:1029-1043. [DOI] [PubMed] [Google Scholar]
- 219.Woolard, M. D., L. L. Hensley, T. H. Kawula, and J. A. Frelinger. 2008. Respiratory Francisella tularensis live vaccine strain infection induces Th17 cells and prostaglandin E2, which inhibits generation of gamma interferon-positive T cells. Infect. Immun. 76:2651-2659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Woolard, M. D., J. E. Wilson, L. L. Hensley, L. A. Jania, T. H. Kawula, J. R. Drake, and J. A. Frelinger. 2007. Francisella tularensis-infected macrophages release prostaglandin E2 that blocks T cell proliferation and promotes a Th2-like response. J. Immunol. 178:2065-2074. [DOI] [PubMed] [Google Scholar]
- 220a.World Health Organization. 1970. Health aspects of chemical and biological weapons. World Health Organization, Geneva, Switzerland.
- 221.Wu, T. H., J. A. Hutt, K. A. Garrison, L. S. Berliba, Y. Zhou, and C. R. Lyons. 2005. Intranasal vaccination induces protective immunity against intranasal infection with virulent Francisella tularensis biovar A. Infect. Immun. 73:2644-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Yee, D., T. R. Rhinehart-Jones, and K. L. Elkins. 1996. Loss of either CD4+ or CD8+ T cells does not affect the magnitude of protective immunity to an intracellular pathogen, Francisella tularensis strain LVS. J. Immunol. 157:5042-5048. [PubMed] [Google Scholar]
- 223.Zogaj, X., S. Chakraborty, J. Liu, D. G. Thanassi, and K. E. Klose. 2008. Characterization of the Francisella tularensis subsp. novicida type IV pilus. Microbiology 154:2139-2150. [DOI] [PubMed] [Google Scholar]