Abstract
Objective: In this article, the presentation, pathophysiology, diagnosis, treatment, and complications of lipomas of the hand are reviewed and evaluated. Methods: A thorough review of the literature is completed, and a series of 13 patients are summarized and briefly examined. Results: Lipomas may present as asymptomatic tumors or produce concerning signs and symptoms such as muscular atrophy and paralysis. Some lipomas may be identified by physical examination alone. However, magnetic resonance imaging best facilitates definitive diagnosis. Conclusions: In the absence of mechanical impairment or cosmetic concern, observation remains the clinical standard of care. When pain, compression neuropathy, disfigurement, or decreased function affect the patient, surgical resection is typically curative. Malignant transformation rarely occurs.
BACKGROUND
Lipomas present as the most common tumor in the body.1 More common in obese individuals,1,2 these benign soft tissue neoplasms typically develop in the 5th to 7th decade of life.1,3 Lipomas are rarely found in children.1,4
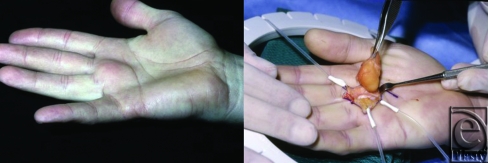
Histologically, lipomas are nearly indistinguishable from normal adipose tissue.1 Composed primarily of mature adipocytes, these lesions are uniform in shape and size and well-circumscribed. A capsule typically surrounds a soft, yellow to orange lobular mass as shown in Figure 1. Although the histological appearance resembles mature adipose tissue, lipomas are not derived from mature adipocytes but rather from mesenchymal preadipocytes.3 Indeed, some variants of lipomas contain a heterogeneous mixture of other mesenchymally derived tissues. Related benign mesenchymomas include the following: fibrolipomas, which contain abundant fibrous tissue; angiolipomas, which are composed chiefly of mature adipocytes within extensive narrow vascular channels that contain fibrin microthrombi; chondrolipomas, which contain cartilaginous and lipomatous elements; myxolipomas, in which areas of mucoid mesenchymal tissues are intermixed with mature fat; myelolipomas, which contain adipocytes and hematopoietic tissue; and ossifying lipomas, which show osseous changes without a connection to bone.
Figure 1.
A 41-year-old man presented with a 2-year history of a right palmar mass between the long and ring fingers. Dissection revealed an encapsulated and multilocular lipoma.
The etiology of a lipoma is unknown. Multiple causative factors have been proposed that include genetic,5 traumatic,6-8 and metabolic1,9-13 triggers. The leading genetic theory for lipoma formation proposes that spontaneous karyotypic anomalies lead to chromosomal fusion products which promote proliferation of adipocytes.5 Although numerous other chromosomal aberrations have been described, lipomas are most commonly associated with translocations and rearrangements of the 12q13˜q15 chromosomal region.5,14 However, not all lipomatous neoplasms exhibit abnormal karyotypes.15 As an example, lipomas have been described in association with retinoblastoma gene mutations.16
In further support of a genetic origin, approximately 5% of patients with lipomas have multifocal lesions,1,17 and many of these individuals have a positive family history.1,18 Some families demonstrate an autosomal dominant mode of inheritance consistent with familial multiple lipomatosis.19 A simple dominant pattern has also been seen in Dercum's disease (adiposis dolorosa), which is typically observed in obese, postmenopausal women in whom numerous painful lipomas occur primarily around the hips and thighs.20 Furthermore, multiple lipomatous lesions are also components of several rare congenital syndromes that include Cowden's Syndrome,21 Bannayan-Zonana Syndrome,22 and Proteus Syndrome.23
Lipoma formation following physical trauma has been reported by multiple investigators. For decades, it was speculated that lipomatous tumors that arose after trauma were not actually a proliferation of adipocytes, but rather a herniation of preexisting adipose tissue through overlying fascia.24,25 These unencapsulated lesions were termed “pseudolipomas.” Later, a competing theory proposed that growth factors, cytokines, and other inflammatory mediators released following blunt trauma to soft tissue induced preadipocyte differentiation into mature adipocytes and formed a clinically apparent mass.6,7,25 More recently, it was suggested that fat necrosis and the extravasation of blood secondary to trauma stimulated preadipocyte differentiation.8,26 Interestingly, a spontaneous elevated partial thromboplastin time has been noted in 7 of 19 patients with posttraumatic lipomas.25 A novel, although unproven, theory is that microhemorrhage and focal release of cytokines secondary to a bleeding diathesis may trigger lipomatous growth.
Lipomas have been associated with numerous pathophysiological processes. Diabetes,9 hyperlipidemia,1 mitochondrial dysfunction,10 and endocrinopathies such as nodular goiter,11 multiple endocrine neoplasia type 1,12 and Cushing's syndrome13 have been noted. A case of lipoma development in a diabetic patient treated with chlorpropamide has also been reported.27 These findings suggest a role for metabolic dysfunction in the development of lipomatous neoplasms.
LIPOMAS OF THE HAND
Lipomas were once believed to be rare in the upper extremity but are now considered common among soft tissue tumors of the hand.28 Most often found in subcutaneous fascia, lipomatous neoplasms occasionally occur in deeper layers. Development typically begins with an initial insidious growth period followed by a prolonged and latent maintenance state.17
Most often presenting as a solitary mass, hand lipomas are often asymptomatic and only come to clinical attention when they are of cosmetic concern or become large enough to create mechanical impairment. In Leffert's series of 141 lipomas of the upper extremity,29 109 tumors were asymptomatic and excised solely for aesthetic reasons. Of the 32 symptomatic lesions, 26 caused pain or tenderness, and 6 produced paresthesias or sensory deficit secondary to nerve compression. Similar symptomatic presentations have been documented extensively in the literature. Lipomas that restricted range of motion and deformed the wrist or digits,30-2 decreased grip strength,30 or caused muscle paralysis,33 polyarthritis,34 trigger finger,35,36 dysesthesias,35 muscle atrophy,33,35 and nail plate dystrophy and thinning37 have been reported.
DIAGNOSIS
History and physical examination are the foundation of diagnosis. As illustrated in Figure 2, lipomas most frequently present as a slowly enlarging, soft and mobile nontender mass. When subcutaneous, diagnosis can be made by a characteristic “doughy” feel on palpation. Application of an ice pack to the tumor to chill and harden the fat has also been used to aid in diagnosis.38
Figure 2.
A 52-year-old woman presented with a subcutaneous lipoma on the dorsum of the left hand. The mass, located between the second and third metacarpals, was mobile with respect to the overlying skin but fixed to underlying structures.
Occasionally, lipomas of the hand may be difficult to differentiate from ganglion cysts by palpation. Ganglion cysts allow passage of light on transillumination while lipomas do not.39 In patients presenting with symptoms of compression neuropathy, a positive Tinel's sign (distal paresthesia secondary to percussion over the tumor) may be helpful in confirming a lipoma as the source of nerve compression.40
When a subcutaneous tumor cannot be diagnosed by palpation, or when a lipoma develops within deeper structures where palpation is difficult, imaging may be necessary for diagnosis. On plain radiograph, lipomas appear as an area of characteristic radiolucency referred to as a “water-clear density.”29 Ultrasound examination demonstrates a homogeneous and circumscribed hyperechoic area.41,42 With computed tomography (CT), lipomas exhibit smooth edges with distinct margins,43 a uniform density comparable to normal fat,44,45 and do not enhance with intravenous contrast.46 Using magnetic resonance (MR) imaging, a homogeneous, high-intensity signal similar to subcutaneous fat may be observed.31,47
Both CT and MR imaging are reliable for localization,48 diagnosis,45,48,49 size estimation,49-51 as well as evaluation of bony involvement.34,52 Superior to plain-film radiographs, three-dimensional imaging allows for preoperative planning of approach, incision, and extent of dissection.48,53 Magnetic resonance imaging is preferable as it is both highly sensitive and specific for diagnosis.54 However, ultrasound may be used as a reasonable and cost-effective alternative if the suspicion for malignancy is low55 and the tumor is not contiguous with surrounding neurovascular or bony structures.40
TREATMENT
Small asymptomatic lesions that have been diagnosed by history and physical examination may be observed without intervention. However, surgical excision is indicated when pain, interference with hand function, compression neuropathy, or cosmetic concern are present.29,30 As demonstrated in Figure 3, the anatomical organization of the hand is complex, and a delicate dissection must be employed. The lipoma is usually surrounded by a thin, fibrous capsule, which may allow the mass to be shelled-out in toto. Marginal excision is appropriate and should result in complete resolution of symptoms over time33 that include restoration of sensation in cases of nerve compression.3,51 Rarely, in patients presenting with carpal tunnel syndrome, extensive nerve infiltration by a lipoma may not allow for tumor resection without causing permanent neurological damage. For such complex presentations, division of the flexor retinaculum without tumor excision is a good strategy for symptom relief.56
Figure 3.
A 72-year-old woman presented with a lipoma of the left hypothenar eminence. The patient complained of swelling and tenderness over the ulnar aspect of the hand with numbness and tingling in the left ring and little fingers. Intraoperatively, the tumor was found to extend into Guyon's canal and could be traced to originate from the bifurcation of the motor and sensory branches of the ulnar nerve. Two months after resection, the patient was symptom-free with full use of the hand.
Alternative methods of tumor removal such as liposuction57 and endoscopically-assisted excision58 aim to minimize scarring. In addition, mesotherapy or intralesional phosphatidylcholine59 and deoxycholate60 injections have been used to shrink small lipomas. However, surgical resection or observation without intervention remain the standard of care.
COMPLICATIONS
Lipomas rarely cause complications. However, patients with untreated compression syndromes may experience decreased neurological function and intractable neuropathic pain.40 In addition, there have been 2 unique reports of lipomas eroding into an adjacent metacarpal.29,61 Operative complications include neurovascular injury, hematoma, and hemorrhage.62 Division of nerves may produce enduring dysesthesias.63 Rarely, recurrence may be of concern and is typically associated with incomplete excision of deep, infiltrative lesions or lesions entangled within neurovascular structures.64 In patients with complicated anatomical infiltration or multilocular lesions, follow-up MR imaging to monitor for local recurrence is appropriate if symptoms develop.
MALIGNANT VARIATION
Liposarcomas present as one of the most common soft tissue sarcomas of the body1 but are uncommon in the hand.65 Like lipomas, these tumors usually present as a small, slowly enlarging painless mass, although high-grade lesions may develop rapidly.17 Histologically, there is wide variation based on subtype and tumor grade, but all liposarcomas are defined by lipoblasts—malignant cells that recapitulate differentiating preadipocytes. The etiology of a liposarcoma is unknown, but most are thought to arise de novo.1,17 Reports of malignant transformation of lipomas are rare in the literature.66-8
CT may be used to visualize liposarcomas,46,69 but MR imaging is ideal.54,70 Findings on imaging are variable and dependent on degree of differentiation, but most show irregular or thickened septa69 and enhancement with gadolinium contrast.71,72 Features such as nodular, globular, or nonfatty areas as well as decreased fat composition also suggest malignancy.49
Treatment of liposarcomas requires wide local excision and in some cases may necessitate amputation.65 Occasionally, (neo)adjuvant chemotherapy or radiotherapy are administered,73-5 especially for high-grade lesions.76 The most common complications of liposarcomas are recurrence and metastasis.
CLINICAL CASE SERIES
To illustrate the clinical presentation and management of lipomas of the hand, a series of 13 patients is briefly examined (Table 1). Seven male and 6 female patients presented at an average age of 57 years (range, 41-72). A variety of presentations were observed that included a single lesion in the left or right hand, dorsal or volar surface, and involvement of fingers or the wrist. The most common presenting symptoms were the description of a mass, swelling, pain, weakness, and decreased function. One patient complained of itching over the tumor site.
Table 1.
Lipomas of the Hand*
| Patient No. | Age | Sex | Location | Presenting Symptoms | Tissue Involvement | Tumor Size | Operative Approach | Follow-up | Recurerence | Note |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 52 | F | Dorsum of L hand, webspace of 2nd and 3rd metacarpals | N/A | Not fixed to overlying skin; fixed to extensor tendons of index and long fingers and dorsal interossei | N/A | Longitudinal incision, simple dissection, neurolysis, tenolysis, excision | 46 months | No | — |
| 2 | 50 | M | R long finger, middle phalanx, dorsal radial aspect | N/A | Extensor tendon of long finger; dorsal branch of radial digital nerve | 3.2 × 1.3 × 0.9 cm3 | Transverse oblique fusiform incision, complex dissection, neurolysis, tenolysis, excision | 108 months | No | — |
| 3 | 41 | M | R palm, between long and ring fingers | painless mass × 2 years | Radial digital nerve and artery of ring finger; ulnar digital nerve and artery of long finger | 3 × 1.5 × 1.5 cm3 | Modified Brunner incision, complex dissection, neurolysis, arteriolysis, excision | 56 months | No | Figure 1 |
| 4 | 58 | M | R index finger, proximal phalynx, radial aspect | painless mass × 2 weeks | Adherent to overlying skin; ulnar neurovascular bundle of index finger; dorsal surface of extensor tendon of index finger | 2.5 × 2.2 × 1.1 cm3 | Modified Brunner incision, complex dissection, arteriolysis, neurolysis, excision | 1 month | No | — |
| 5 | 63 | M | R palm, thenar eminence | Swelling, aching, weakness of R thumb × 2 months | Radial neurovascular bundle of thumb | 3 × 1.8 × 1.1 cm3 | Brunner incision, complex dissection, arteriolysis, neurolysis, excision | N/A | N/A | — |
| 6 | 72 | F | L palm, hypothenar eminence | Swelling, tenderness over ulnar border of L hand × 14 months | Ulnar nerve at bifurcation of motor and sensory branches; Guyon's canal | 4.5 × 2.5 × 1.2 cm3 | Resection of previous scar along ulnar border, complex dissection, neurolysis, excision | 26 months | No | History of previous attempted resection 1 month prior, Figure 3 |
| 7 | N/A | F | Dorsum of R hand, webspace of 1st and 2nd metacarpals | Large mass | Princeps pollicis artery; ulnar neurovascular bundle of thumb; radial neurovascular bundle of index finger | 6.5 × 4 × 4 cm3 | Longitudinal incision, complex dissection, arteriolysis, neurolysis, excision, placement of silastic drains × 2 | N/A | N/A | Closure with 2 silastic drains; Figure 2 |
| 8 | 58 | F | L palm, webspace of 1st and 2nd metacarpals, extending into carpal tunnel | Swelling, itching × 4 months | Radial neurovascular bundle of index finger; noninvasive pressure on ulnar nerve | 3.2 × 2.2 × 1 cm3 | Longitudinal incision on dorsum of hand + classic carpal tunnel incision, complex dissection, neurolysis, tenolysis, excision, decompression L carpal tunnel | 61 months | No | — |
| 9 | 55 | M | L forearm, deep to supinator | Unable to extend fingers or wrist × 3 months | Supinator; radial nerve | 5 × 3.5 × 2.5 cm3 | Transverse incision on dorsal wrist with exploration, curved incision on lateral aspect of elbow and forearm, complex dissection, neurolysis, excision | 12 months | No | — |
| 10 | 62 | F | Dorsum of R hand | Enlarging mass × 30 months | Superficial fascia | 2.2 × 1.1 × 0.6 cm3 | Fusiform incision, simple dissection, excision | 1 month | No | — |
| 11 | 57 | M | Distal volar aspect of L wrist | Progressively enlarging mass with discomfort × 2–3 years | Adherent to overlying skin and flexor retinaculum | 2.6 × 1.9 × 0.7 cm3 | Transverse incision, complex dissection, excision | 1 month | No | — |
| 12 | 71 | F | L thumb, proximal phalynx, palmar aspect | Pain at base of left thumb and wrist | 300° circumferential involvement of proximal phalynx; neurovascular bundle; flexor pollicis longus | 4 × 3 × 3 cm3 | Transverse incision, complex dissection, arteriolysis, neurolysis, tenolysis, excision | 3 months | No | — |
| 13 | 48 | M | R palm | Hand cramps, mass × 72 months, enlarging × 3 months | Adductor pollicis; opponens pollicis; ulnar neurovascular bundle of thumb; radial neurovascular bundle of index finger | 5.3 × 4 × 2 cm3 | Counter incisions on anterior and posterior surfaces of webspace between 1st and 2nd metacarpals extending into thenar eminence, complex dissection, extensive neurolysis, excision, placement of silastic drains × 2 | 1 month | No | Closure with 2 silastic drains |
*F, female; M, male; L, left; R, right; N/A, not availabale.
Surgical incision and approach were variable. Nearly all lipomas involved surrounding tissues such as nerves, vasculature, musculature, tendons, and skin, which illustrated the potential of these tumors to interfere with functions of the hand. As a result, most tumors required extensive dissection and lysis of adherent structures to ensure complete excision. Two of 13 cases required temporary silastic drains. The mean tumor size was 3.8 cm × 2.4 cm × 1.6 cm after fixation. Eleven of 13 patients returned for follow-up between 1 and 108 months. No recurrences were found.
SUMMARY
This article outlines the current understanding of the pathophysiology, methods of diagnosis, treatment modalities, and complications of lipomatous tumors of the hand. Lipomas remain a common benign neoplasm of the hand. Simple subcutaneous lipomas may be diagnosed by history and physical examination alone. For more complicated tumors, MR imaging is most useful for diagnosis and preoperative planning. Most lipomas are treated with surgical excision with few complications or recurrence. Malignant degeneration is rare.
Acknowledgment
The authors thank Jeremiah Redstone, MD for his assistance.
REFERENCES
- 1.Weiss SW, Goldblum JR. Benign Lipomatous Tumors. In: Enzinger FM, Weiss SW, editors. Soft Tissue Tumors. 3rd ed. St Louis, Mo: Mosby; 1995. pp. 381–430. [Google Scholar]
- 2.Froimson AI. Benign solid tumors. Hand Clin. 1987;3(2):213–7. [PubMed] [Google Scholar]
- 3.Phalen GS, Kendrick JI, Rodriguez JM. Lipomas of the upper extremity: a series of fifteen tumors in the hand and wrist and six tumors causing nerve compression. Am J Surg. 1971;121(3):298–306. doi: 10.1016/0002-9610(71)90208-x. [DOI] [PubMed] [Google Scholar]
- 4.Rydholm A, Berg NO. Size, site and clinical incidence of lipoma: factors in the differential diagnosis of lipoma and sarcoma. Acta Orthop Scand. 1983;54(6):929–34. doi: 10.3109/17453678308992936. [DOI] [PubMed] [Google Scholar]
- 5.Sandberg AA. Updates on the cytogenetics and molecular genetics of bone and soft tissue tumors: lipoma. Cancer Genet Cytogenet. 2004;150(2):93–115. doi: 10.1016/j.cancergencyto.2003.12.018. [DOI] [PubMed] [Google Scholar]
- 6.Signorini M, Campiglio GL. Posttraumatic lipomas: where do they really come from? Plast Reconstr Surg. 1998;101(3):699–705. doi: 10.1097/00006534-199803000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Aust MC, Spies M, Kall S, et al. Lipomas after blunt soft tissue trauma: are they real? Analysis of 31 cases. Br J Dermatol. 2007;157(1):92–9. doi: 10.1111/j.1365-2133.2007.07970.x. [DOI] [PubMed] [Google Scholar]
- 8.Copcu E, Sivrioglu NS. Posttraumatic lipoma: analysis of 10 cases and explanation of possible mechanisms. Dermatol Surg. 2003;29(3):215–20. doi: 10.1046/j.1524-4725.2003.29052.x. [DOI] [PubMed] [Google Scholar]
- 9.Weinberg T, Feldman M. Sr. Lipomas of the gastrointestinal tract. Am J Clin Pathol. 1955;25(3):272–81. doi: 10.1093/ajcp/25.3.272. [DOI] [PubMed] [Google Scholar]
- 10.Berkovic SF, Andermann F, Shoubridge EA, et al. Mitochondrial dysfunction in multiple symmetrical lipomatosis. Ann Neurol. 1991;29(5):566–9. doi: 10.1002/ana.410290519. [DOI] [PubMed] [Google Scholar]
- 11.Leiva SF, Navachia D, Nigro N, Ibarra R, Cresto JC. Lipoma in the thyroid? J Pediatr Endocrinol Metab. 2004;17(7):1013–5. doi: 10.1515/jpem.2004.17.7.1013. [DOI] [PubMed] [Google Scholar]
- 12.Pack S, Turner ML, Zhuang Z, et al. Cutaneous tumors in patients with multiple endocrine neoplasia type 1 show allelic deletion of the MEN1 gene. J Invest Dermatol. 1998;110(4):438–40. doi: 10.1046/j.1523-1747.1998.00140.x. [DOI] [PubMed] [Google Scholar]
- 13.Miyake O, Hara T, Matsumiya K, Oka T, Takaha M, Kurata A. [Adrenal myelolipoma associated with Cushing's syndrome: a case report] Hinyokika Kiyo. 1992;38(6):681–4. [PubMed] [Google Scholar]
- 14.Sandberg AA, Bridge JA. Tumors of Fat. The Cytogenetics of Bone and Soft Tissue Tumors. Austin: R.G. Landes Company; 1994. pp. 147–92. [Google Scholar]
- 15.Sreekantaiah C, Leong SP, Karakousis CP, et al. Cytogenetic profile of 109 lipomas. Cancer Res. 1991;51(1):422–33. [PubMed] [Google Scholar]
- 16.Genuardi M, Klutz M, Devriendt K, Caruso D, Stirpe M, Lohmann DR. Multiple lipomas linked to an RB1 gene mutation in a large pedigree with low penetrance retinoblastoma. Eur J Hum Genet. 2001;9(9):690–4. doi: 10.1038/sj.ejhg.5200694. [DOI] [PubMed] [Google Scholar]
- 17.Ragsdale BD, Dupree WB. Neoplasms of the fatty tissues. In: Bogumill GB, Fleegler EJ, editors. Tumors of the Hand and Upper Limb. New York, NY: Churchill Livingstone; 1993. [Google Scholar]
- 18.Solvonuk PF, Taylor GP, Hancock R, Wood WS, Frohlich J. Correlation of morphologic and biochemical observations in human lipomas. Lab Invest. 1984;51(4):469–74. [PubMed] [Google Scholar]
- 19.Leffell DJ, Braverman IM. Familial multiple lipomatosis: report of a case and a review of the literature. J Am Acad Dermatol. 1986;15(2, pt 1):275–9. [PubMed] [Google Scholar]
- 20.Brodovsky S, Westreich M, Leibowitz A, Schwartz Y. Adiposis dolorosa (Dercum's disease): 10-year follow-up. Ann Plast Surg. 1994;33(6):664–8. doi: 10.1097/00000637-199412000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Weary PE, Gorlin RJ, Gentry WC, Jr, Comer JE, Greer KE. Multiple hamartoma syndrome (Cowden's disease) Arch Dermatol. 1972;106(5):682–90. [PubMed] [Google Scholar]
- 22.Bannayan GA. Lipomatosis, angiomatosis, and macrencephalia. a previously undescribed congenital syndrome. Arch Pathol. 1971;92(1):1–5. [PubMed] [Google Scholar]
- 23.Clark RD, Donnai D, Rogers J, Cooper J, Baraitser M. Proteus syndrome: an expanded phenotype. Am J Med Genet. 1987;27(1):99–117. doi: 10.1002/ajmg.1320270111. [DOI] [PubMed] [Google Scholar]
- 24.Brooke RI, MacGregor AJ. Traumatic pseudolipoma of the buccal mucosa. Oral Surg Oral Med Oral Pathol. 1969;28(2):223–5. doi: 10.1016/0030-4220(69)90290-4. [DOI] [PubMed] [Google Scholar]
- 25.Aust MC, Spies M, Kall S, Jokuszies A, Gohritz A, Vogt P. Posttraumatic lipoma: fact or fiction? Skinmed. 2007;6(6):266–70. doi: 10.1111/j.1540-9740.2007.06361.x. [DOI] [PubMed] [Google Scholar]
- 26.Copcu E. Posttraumatic fingertip lipoma. Plast Reconstr Surg. 2004;114(7):1986–7. doi: 10.1097/01.prs.0000143905.98346.3d. [DOI] [PubMed] [Google Scholar]
- 27.Garfinkel HA. A massive lipoma in a patient receiving chlorpropamide therapy. Postgrad Med J. 1971;47(544):137–8. doi: 10.1136/pgmj.47.544.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Calandruccio J, Jobe M. Tumors and tumorous conditions of the hand. In: Canale ST, Beaty JH, editors. Campbell's Operative Orthopedics. Philadelphia, Pa: Mosby Elsevier; 2007. [Google Scholar]
- 29.Leffert RD. Lipomas of the upper extremity. J Bone Joint Surg Am. 1972;54(6):1262–6. [PubMed] [Google Scholar]
- 30.Oster LH, Blair WF, Steyers CM. Large lipomas in the deep palmar space. J Hand Surg Am. 1989;14(4):700–4. doi: 10.1016/0363-5023(89)90193-7. [DOI] [PubMed] [Google Scholar]
- 31.Lee YH, Jung JM, Baek GH, Chung MS. Intramuscular lipoma in thenar or hypothenar muscles. Hand Surg. 2004;9(1):49–54. doi: 10.1142/s0218810404002005. [DOI] [PubMed] [Google Scholar]
- 32.Hoehn JG, Farber HF. Massive lipoma of the palm. Ann Plast Surg. 1983;11(5):431–3. doi: 10.1097/00000637-198311000-00012. [DOI] [PubMed] [Google Scholar]
- 33.McFarland GB, Jr, Hoffer MM. Paralysis of the intrinsic muscles of the hand secondary to lipoma in Guyon's tunnel. J Bone Joint Surg Am. 1971;53(2):375–6. [PubMed] [Google Scholar]
- 34.Fernandez-Sueiro JL, Pinto JA, Blanco FJ, et al. Multiple parosteal lipoma associated to polyarthritis. Joint Bone Spine. 2006;73(2):202–4. doi: 10.1016/j.jbspin.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 35.Sonoda H, Takasita M, Taira H, Higashi T, Tsumura H. Carpal tunnel syndrome and trigger wrist caused by a lipoma arising from flexor tenosynovium: a case report. J Hand Surg Am. 2002;27(6):1056–8. doi: 10.1053/jhsu.2002.36522. [DOI] [PubMed] [Google Scholar]
- 36.Pampliega T, Arenas AJ. An unusual trigger finger. Acta Orthop Belg. 1997;63(2):132–3. [PubMed] [Google Scholar]
- 37.Bardazzi F, Savoia F, Fanti PA. Subungual lipoma. Br J Dermatol. 2003;149(2):418. doi: 10.1046/j.1365-2133.2003.05370.x. [DOI] [PubMed] [Google Scholar]
- 38.Posch JL. Tumors of the hand. J Bone Joint Surg Am. 1956;38-A(3):517–39. discussion, 539–540; passim. [PubMed] [Google Scholar]
- 39.Ingari JV, Faillace JJ. Benign tumors of fibrous tissue and adipose tissue in the hand. Hand Clin. 2004;20(3):243–8. doi: 10.1016/j.hcl.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 40.Flores LP, Carneiro JZ. Peripheral nerve compression secondary to adjacent lipomas. Surg Neurol. 2007;67(3):258–62. doi: 10.1016/j.surneu.2006.06.052. discussion 262-3. [DOI] [PubMed] [Google Scholar]
- 41.James JJ, Robin A, Wilson M, Evans AJ. The Breast. In: Adam A, Dixon AK, editors. Grainger & Allison's Diagnostic Radiology. 5th ed. Philadelphia, Pa: Elsevier; 2008. [Google Scholar]
- 42.Pant R, Poh AC, Hwang SG. An unusual case of an intramuscular lipoma of the pectoralis major muscle simulating a malignant breast mass. Ann Acad Med Singapore. 2005;34(3):275–6. [PubMed] [Google Scholar]
- 43.Weekes RG, McLeod RA, Reiman HM, Pritchard DJ. CT of soft-tissue neoplasms. AJR Am J Roentgenol. 1985;144(2):355–60. doi: 10.2214/ajr.144.2.355. [DOI] [PubMed] [Google Scholar]
- 44.Egund N, Ekelund L, Sako M, Persson B. CT of soft-tissue tumors. AJR Am J Roentgenol. 1981;137(4):725–9. doi: 10.2214/ajr.137.4.725. [DOI] [PubMed] [Google Scholar]
- 45.Halldorsdottir A, Ekelund L, Rydholm A. CT-diagnosis of lipomatous tumors of the soft tissues. Arch Orthop Trauma Surg. 1982;100(4):211–6. doi: 10.1007/BF00381659. [DOI] [PubMed] [Google Scholar]
- 46.Dooms GC, Hricak H, Sollitto RA, Higgins CB. Lipomatous tumors and tumors with fatty component: MR imaging potential and comparison of MR and CT results. Radiology. 1985;157(2):479–83. doi: 10.1148/radiology.157.2.4048459. [DOI] [PubMed] [Google Scholar]
- 47.Capelastegui A, Astigarraga E, Fernandez-Canton G, Saralegui I, Larena JA, Merino A. Masses and pseudomasses of the hand and wrist: MR findings in 134 cases. Skeletal Radiol. 1999;28(9):498–507. doi: 10.1007/s002560050553. [DOI] [PubMed] [Google Scholar]
- 48.Babins DM, Lubahn JD. Palmar lipomas associated with compression of the median nerve. J Bone Joint Surg Am. 1994;76(9):1360–2. doi: 10.2106/00004623-199409000-00010. [DOI] [PubMed] [Google Scholar]
- 49.Kransdorf MJ, Bancroft LW, Peterson JJ, Murphey MD, Foster WC, Temple HT. Imaging of fatty tumors: distinction of lipoma and well-differentiated liposarcoma. Radiology. 2002;224(1):99–104. doi: 10.1148/radiol.2241011113. [DOI] [PubMed] [Google Scholar]
- 50.Matsuyama K, Nakagawa T, Horio Y, Hongo H, Miyauchi Y, Yasue H. Thymolipoma simulating cardiomegaly: diagnostic usefulness of computed tomography. Jpn Circ J. 1986;50(9):839–42. doi: 10.1253/jcj.50.839. [DOI] [PubMed] [Google Scholar]
- 51.Bagatur AE, Yalcinkaya M. Unilateral carpal tunnel syndrome caused by an occult palmar lipoma. Orthopedics. 2009;32(10) doi: 10.3928/01477447-20090818-20. pii: orthosupersite.com/view.asp?rID=43775. doi: 10.3928/01477447-20090818-20. [DOI] [PubMed] [Google Scholar]
- 52.Brooks ML, Mayer DP, Grannick MS, Solomon MP, Rhoda CH. Parosteal lipoma of the finger: preoperative evaluation with computed tomography. Comput Med Imaging Graph. 1989;13(6):481–5. doi: 10.1016/0895-6111(89)90291-7. [DOI] [PubMed] [Google Scholar]
- 53.Boussouga M, Bousselmame N, Lazrak KH. [Thenar lipoma causing nervous compression. A case report] Chir Main. 2006;25(3-4):156–8. doi: 10.1016/j.main.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 54.Gaskin CM, Helms CA. Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol. 2004;182(3):733–9. doi: 10.2214/ajr.182.3.1820733. [DOI] [PubMed] [Google Scholar]
- 55.Hoglund M, Muren C, Brattstrom G. A statistical model for ultrasound diagnosis of soft-tissue tumours in the hand and forearm. Acta Radiol. 1997;38(3):355–8. doi: 10.1080/02841859709172082. [DOI] [PubMed] [Google Scholar]
- 56.Friedlander HL, Rosenberg NJ, Graubard DJ. Intraneural lipoma of the median nerve. Report of two cases and review of the literature. J Bone Joint Surg Am. 1969;51(2):352–62. [PubMed] [Google Scholar]
- 57.Choi CW, Kim BJ, Moon SE, Youn SW, Park KC, Huh CH. Treatment of lipomas assisted with tumescent liposuction. J Eur Acad Dermatol Venereol. 2007;21(2):243–6. doi: 10.1111/j.1468-3083.2006.02037.x. [DOI] [PubMed] [Google Scholar]
- 58.Berger A, Tanzella U. [Endoscopically-assisted lipoma removal] Langenbecks Arch Chir Suppl Kongressbd. 1998;115:1538–40. [PubMed] [Google Scholar]
- 59.Kopera D, Binder B, Toplak H. Intralesional lipolysis with phosphatidylcholine for the treatment of lipomas: pilot study. Arch Dermatol. 2006;142(3):395–6. doi: 10.1001/archderm.142.3.395. [DOI] [PubMed] [Google Scholar]
- 60.Rotunda AM, Ablon G, Kolodney MS. Lipomas treated with subcutaneous deoxycholate injections. J Am Acad Dermatol. 2005;53(6):973–8. doi: 10.1016/j.jaad.2005.07.068. [DOI] [PubMed] [Google Scholar]
- 61.Schoffl H, Hager D, Dunst KM, Huemer GM. Giant lipoma of the thenar. Wien Klin Wochenschr. 2007;119(5-6):149. doi: 10.1007/s00508-006-0750-7. [DOI] [PubMed] [Google Scholar]
- 62.Green DP, Hotchkiss RN, Pedersen WC, Wolfe SW. Green's Operative Hand Surgery. 5th ed. Philadelphia, Pa: Elsevier; 2005. [Google Scholar]
- 63.Cribb GL, Cool WP, Ford DJ, Mangham DC. Giant lipomatous tumours of the hand and forearm. J Hand Surg Br. 2005;30(5):509–12. doi: 10.1016/j.jhsb.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 64.Bancroft LW, Kransdorf MJ, Peterson JJ, O'Connor MI. Benign fatty tumors: classification, clinical course, imaging appearance, and treatment. Skeletal Radiol. 2006;35(10):719–33. doi: 10.1007/s00256-006-0189-y. [DOI] [PubMed] [Google Scholar]
- 65.Sawhney KK, McDonald JM, Jaffe HW. Liposarcoma of the hand. Am Surg. 1975;41(2):117–20. [PubMed] [Google Scholar]
- 66.Sternberg SS. Liposarcoma arising within a subcutaneous lipoma. Cancer. 1952;5(5):975–8. doi: 10.1002/1097-0142(195209)5:5<975::aid-cncr2820050513>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 67.Baer W, Schaller P, Ruf S. [Coincidence of lipoma and liposarcoma of the right hand in an 84-year-old patient: a case report] Handchir Mikrochir Plast Chir. 2001;33(5):321–5. doi: 10.1055/s-2001-17764. [DOI] [PubMed] [Google Scholar]
- 68.Sampson CC, Saunders EH, Green WE, Laurey JR. Liposarcoma developing in a lipoma. Arch Pathol. 1960;69:506–10. [PubMed] [Google Scholar]
- 69.Jelinek JS, Kransdorf MJ, Shmookler BM, Aboulafia AJ, Malawer MM. Liposarcoma of the extremities: MR and CT findings in the histologic subtypes. Radiology. 1993;186(2):455–9. doi: 10.1148/radiology.186.2.8421750. [DOI] [PubMed] [Google Scholar]
- 70.Demas BE, Heelan RT, Lane J, Marcove R, Hajdu S, Brennan MF. Soft-tissue sarcomas of the extremities: comparison of MR and CT in determining the extent of disease. AJR Am J Roentgenol. 1988;150(3):615–20. doi: 10.2214/ajr.150.3.615. [DOI] [PubMed] [Google Scholar]
- 71.Panzarella MJ, Naqvi AH, Cohen HE, Damron TA. Predictive value of gadolinium enhancement in differentiating ALT/WD liposarcomas from benign fatty tumors. Skeletal Radiol. 2005;34(5):272–8. doi: 10.1007/s00256-004-0884-5. [DOI] [PubMed] [Google Scholar]
- 72.Sung MS, Kang HS, Suh JS, et al. Myxoid liposarcoma: appearance at MR imaging with histologic correlation. Radiographics. 2000;20(4):1007–19. doi: 10.1148/radiographics.20.4.g00jl021007. [DOI] [PubMed] [Google Scholar]
- 73.Mack LA, Crowe PJ, Yang JL, et al. Preoperative chemoradiotherapy (modified Eilber protocol) provides maximum local control and minimal morbidity in patients with soft tissue sarcoma. Ann Surg Oncol. 2005;12(8):646–53. doi: 10.1245/ASO.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 74.Loubignac F, Bourtoul C, Chapel F. Myxoid liposarcoma: a rare soft-tissue tumor with a misleading benign appearance. World J Surg Oncol. 2009;7:42. doi: 10.1186/1477-7819-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schofer MD, Abu-Safieh MY, Paletta J, Fuchs-Winkelmann S, El-Zayat BF. Liposarcoma of the forearm in a man with type 1 neurofibromatosis: a case report. J Med Case Reports. 2009;3:7071. doi: 10.1186/1752-1947-3-7071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dalal KM, Antonescu CR, Singer S. Diagnosis and management of lipomatous tumors. J Surg Oncol. 15 2008;97(4):298–313. doi: 10.1002/jso.20975. [DOI] [PubMed] [Google Scholar]