Abstract
Because T cell differentiation leads to an expanded repertoire of chemokine receptors, a subgroup of G protein-coupled receptors, we hypothesized that the repertoire of G proteins might be altered in parallel. We analyzed the abundance of mRNA and/or protein of six G protein α-subunits in human CD4+ and CD8+ T cell subsets from blood. Although most G protein α-subunits were similarly expressed in all subsets, the abundance of Gαo, a protein not previously described in hematopoietic cells, was much higher in memory versus naive cells. Consistent with these data, activation of naive CD4+ T cells in vitro significantly increased the abundance of Gαo in cells stimulated under nonpolarizing or TH17 (but not TH1 or TH2)-polarizing conditions. In functional studies, the use of a chimeric G protein α-subunit, Gαqo5, demonstrated that chemokine receptors could couple to Gαo-containing G proteins. We also found that Gαi1, another α-subunit not described previously in leukocytes, was expressed in naive T cells but virtually absent from memory subsets. Corresponding to their patterns of expression, siRNA-mediated knockdown of Gαo in memory (but not naive) and Gαi1 in naive (but not memory) CD4+ T cells inhibited chemokine-dependent migration. Moreover, although even in Gαo- and Gαi1-expressing cells mRNAs of these α-subunits were much less abundant than Gαi2 or Gαi3, knockdown of any of these subunits impaired chemokine receptor-mediated migration similarly. Together, our data reveal a change in the repertoire of Gαi/o subunits during T cell differentiation and suggest functional equivalence among Gαi/o subunits irrespective of their relative abundance.
Keywords: Cell Differentiation, G Protein-coupled Receptors (GPCR), G Proteins, Lymphocyte, Receptors
Introduction
Exposure of naive T cells to cognate antigens in the context of infection results in their rapid clonal expansion to produce large numbers of antigen-specific effector cells. After an infection has been cleared, most effector cells die, leaving behind a smaller population of long-lived memory cells that are able to mount a rapid response upon reinfection (1). Because it is often difficult to distinguish between effector and long-lived memory cells in blood or other sites by phenotypic markers alone, non-naive T cells are often described as “effector/memory” cells. Unlike naive cells, which are generally homogeneous except for their antigen receptors, the effector/memory population is highly heterogeneous. For CD4+ or helper T (TH)3 cells, separate pathways of effector/memory differentiation have been described, resulting in, for example, TH1, TH2, and TH17 cells, which can be identified by their abilities to produce the signature cytokines, interferon-γ (IFNγ), interleukin 4 (IL-4), and IL-17, respectively. For CD8+ or cytotoxic T cells, progressive differentiation results in the production of proteins such as perforin and granzymes, which enhance the ability of these cells to kill infected cells (1–3).
A more general scheme has been proposed for understanding CD4+ and CD8+ effector/memory T cell differentiation, whereby naive cells give rise first to central memory T cells (TCM), and these can in turn, either through homeostatic or antigen-driven proliferation, yield effector memory T cells (TEM) (4) (not to be confused with effector/memory cells). TCM express L-selectin (CD62L) and the chemokine receptor CCR7, which are necessary for trafficking to non-inflamed lymphoid tissues, whereas TEM lose expression of CD62L, CCR7, or both along with the ability to enter non-inflamed lymphoid organs. TEM possess the highest levels of effector functions, such as the production of effector cytokines or cytotoxicity (4). An expanded ability to migrate into tissue to combat infection is an essential component of effector/memory T cell differentiation. This latter capability is due in part to the expression of an expanded number of species of chemokine receptors (for example, from two on naïve cells, to at least 15, in various combinations, on effector/memory T cells) and is associated with an intrinsic, enhanced response to chemokines in assays in vitro (5). In humans, chemokine receptors form a group of 19 seven-transmembrane domain, G protein-coupled receptors (GPCRs), which have ligands that form a corresponding group of more than 40 chemoattractant proteins.
We hypothesized that the expanded repertoire of receptors on memory T cells might be associated with gains and/or losses of downstream effector molecules, such as the heterotrimeric G proteins, which are the proximal transducers of chemokine receptor signals. Changes in the abundance of G protein α-subunits have functional consequences for GPCR-mediated signaling. In some cellular contexts, the abundance of certain G protein α-subunits is limiting, and increased responsiveness to various ligands is achieved through the increased expression of G protein α-subunits, as well as, or in place of, increased expression of a given GPCR (6–10). Regulation can be subtle, for example the result of selectively increasing or decreasing the abundance of individual Gαi/0 family members while leaving others unchanged (7, 8), and changes in the abundance of various G proteins can result in functional differences by affecting the balance among different signaling pathways (6). Changes in the abundance of Gi-family G proteins might have particular relevance for chemokine receptor signaling, because these G proteins are critical for chemoattractant receptor signaling (11–13).
We compared naive and memory T cells for the expression of G protein α-subunits. In experiments described below, we found that effector/memory T cells from human peripheral blood, much more so than naive T cells, expressed the Gi family member Gαo, which has not been described previously in hematopoietic cells. In functional studies, we found that despite being of relatively low abundance in the effector/memory population based on mRNA expression, Gαo contributed significantly to chemokine receptor signaling in these cells. We also found that Gαi1 had a reciprocal pattern as compared with Gαo; Gαi1 was expressed and functioned with chemokine receptors in naive cells but was down-regulated after differentiation to effector/memory cells. Together, these data are the first description of the presence and function of Gαo (and Gαi1) in leukocytes and suggest that the low abundance of some Gα proteins belies their functional importance in GPCR signaling.
EXPERIMENTAL PROCEDURES
Cell Culture and Reagents
Cell culture media and salt solutions were obtained from Invitrogen, and fetal bovine serum (FBS) was purchased from Gemini Bio-Products (Woodland, CA). Ficoll-Hypaque was purchased from Amersham Pharmacia Biotech. All recombinant chemokines were purchased from Peprotech (Rocky Hill, NJ). The anti-CD3 mAb (OKT3) was obtained from Ortho Biotech (Raritan, NJ). The anti-CD28 mAb clone 9.3 was a kind gift from Carl June (University of Pennsylvania, Philadelphia). Anti-IL-4, anti-IL-12, and anti-IFNγ antibodies were obtained from BD Biosciences. rIL-2 was obtained from Hoffmann-La Roche. The cytokines IL-4, IL-12, IFNγ, and TGF-β were purchased from R&D Systems (Minneapolis, MN). Rabbit polyclonal antibodies against Gαi2 (catalogue number sc-7276), Gαi3 (sc-262), Gαo (sc-387), Gαq/11 (sc-392), Gα13 (sc-410), goat polyclonal antibody against actin (sc-1615), and anti-rabbit and anti-goat preadsorbed HRP-conjugated secondary antibodies were purchased from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA). A second rabbit polyclonal antibody against Gαo (catalogue number 3975) was purchased from Cell Signaling Technology (Danvers, MA). The metalloproteinase inhibitor TAPI-0 was obtained from Peptides International (Louisville, KY).
Plasmid DNAs
cDNA encoding human CXCR6 was amplified by polymerase chain reaction (PCR) using the previously described pCEP4:CXCR6 clone C3-9.1 as a template (14) and inserted in-frame into the pEYFP-N1 vector (Clontech Laboratories, Palo Alto, CA) to encode a CXCR6 C-terminal fusion protein with yellow fluorescent protein (YFP). DNAs were verified by sequencing. The construction of plasmids expressing G protein chimeras, in which the five C-terminal amino acid residues of Gαq were replaced with those of Gαi2 (qi5 chimera), Gαo (qo5), or Gαs (qs5), has been described previously (15, 16); these were a kind gift of Bruce M. Conklin (Gladstone Institute of Cardiovascular Disease, University of California, San Francisco). All chimeras have an internal hemagglutinin (HA) epitope, allowing for recognition by an anti-HA antibody (clone 12CA5, Roche Diagnostics). The cDNA clones for human Gαi1, Gαi2, Gαi3, GαoA, GαoB, and Gα13 in pcDNA3.1(+), were obtained from the University of Missouri cDNA Resource Center.
Purification and Sorting of Leukocyte Subsets
Elutriated lymphocytes and monocytes were obtained from healthy donors by the Department of Transfusion Medicine, Clinical Center, National Institutes of Health (Bethesda, MD), under an Institutional Review Board-approved protocol. In initial experiments, CD4+ and CD8+ T lymphocytes were isolated from elutriated lymphocytes by negative selection with either the CD4+ T cell isolation kit II or the CD8+ T cell isolation kit (Miltenyi Biotec, Auburn, CA) according to the manufacturer's instructions. These cells were further purified using CD45RA microbeads (Miltenyi Biotec) for positive and negative selection of naive and memory cells, respectively. CD45RA−CD4+ T cells (memory T cells) were further purified by incubation with CD62L microbeads for positive selection of central memory (CD62L+) and negative selection of effector memory (CD62L−) cells. For the isolation of other leukocyte subsets from elutriated cells, positive selection was performed using microbeads for the following cell type-specific markers (all from Miltenyi Biotec): CD3 (total T cells) and CD11b (monocytes). All selected leukocyte subsets were analyzed for phenotypic cell surface marker expression by antibody staining and flow cytometric analysis as described below. In later experiments (indicated in the legends to Figs. 2, 3, and 8), CD4+ and CD8+ T cell subsets were first purified by negative selection with either the RosetteSep CD4+ T cell or CD8+ T cell enrichment mixtures (StemCell Technologies, Vancouver, British Columbia, Canada) as described previously (17), and naive and effector/memory subsets were purified by sorting using a FACSAria flow cytometer (BD Biosciences) after staining with the following antibodies obtained from BD Biosciences: FITC-conjugated anti-CD8, phycoerythrin-conjugated anti-CD62L, phycoerythrin-Cy5-conjugated anti-CD3, allophycocyanin-conjugated anti-CD45RO, and allophycocyanin-Cy7-conjugated anti-CD4 as described previously (18). It is noteworthy that published experiments have demonstrated the cleavage of CD62L from the surface of lymphocytes through the activity of a zinc metalloproteinase (19, 20). In our sorting of CD8+ T cell subsets, we sometimes detected substantial amounts of CD62L mRNA in the “CD45RO−CD62L−” effector/memory population, presumably through contamination with naive cells in which CD62L had been cleaved. We found that treatment of CD8+ T cells during staining and sorting with TAPI-0 (50 μg/ml), a specific inhibitor of the zinc metalloproteinase responsible for CD62L cleavage (21), resulted in very low amounts of CD62L mRNA in the effector/memory population (data not shown). The data presented here are from experiments in which real-time RT-PCR analysis demonstrated little or no contamination of the CD8+CD62L− subsets with cells expressing mRNA for CD62L (data not shown).
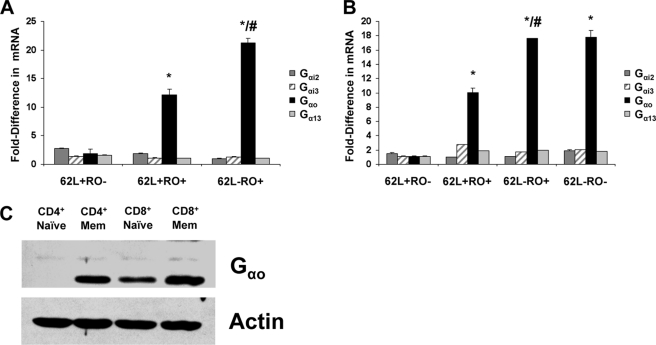
FIGURE 2.
Gαo mRNA and protein expression is highest in the most differentiated subsets of human CD4+ and CD8+ T cells. CD4+ (A) and CD8+ (B) T cells from peripheral blood were sorted into naive (CD62L+CD45RO−), TCM (CD62L+CD45RO+), and TEM (CD62L−CD45RO+; CD62L−CD45RO−) subsets as described under “Experimental Procedures.” Each subset was analyzed by semiquantitative real-time RT-PCR for mRNAs for Gαi2, Gαi3, Gαo, and Gα13. -Fold differences in the abundance of the indicated mRNAs, each normalized to that of GAPDH mRNA, between each subset of CD4+ (8) (A) or CD8+ (B) T cells were calculated for each mRNA species as described in the legend for Fig. 1. For each mRNA of interest, the lowest level of expression versus GAPDH from a single well was set at 1. Values cannot be compared between mRNA species. The data shown are the mean -fold differences ± S.E. in expression for the indicated mRNAs from assays performed in duplicate from separate donors for CD4+ and CD8+ T cells and are representative of five and three donors for CD4+ and CD8+ T cells, respectively. *, p < 0.05, when compared with mRNA in naive subsets; #, p < 0.05 when comparing mRNA content of the CD62L−CD45RO+ subset with that of the CD62L+CD45RO+ subset. C, whole-cell lysates (40 μg of protein) of purified subsets of CD4+ and CD8+ T cells, isolated as described under “Experimental Procedures,” were analyzed by Western blotting with anti-Gαo and anti-actin antibodies. Results are for naive and combined memory subsets (CD4+ Mem, CD8+ Mem) of CD4+ or CD8+ T cells. Data are from the same donor for both CD4+ and CD8+ T cell subsets and are representative of three donors.
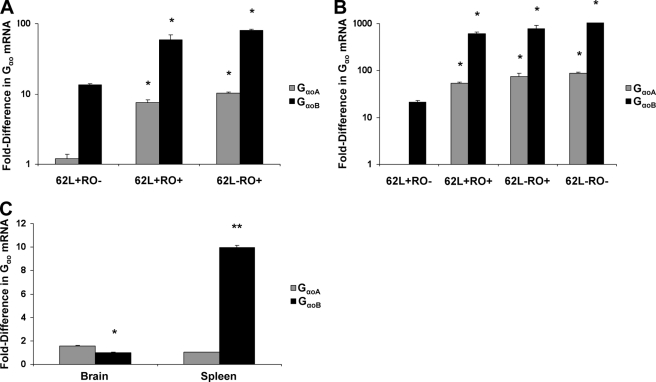
FIGURE 3.
GαoB mRNA is expressed more abundantly than GαoA mRNA in CD4+ and CD8+ T cells. CD4+ (A) and CD8+ (B) T cells from peripheral blood were sorted into naive (CD62L+CD45RO−), TCM (CD62L+CD45RO+), and TEM (CD62L−CD45RO+; CD62L−CD45RO−) subsets, and each subset was analyzed by semiquantitative real-time RT-PCR for mRNAs for GαoA and GαoB. -Fold differences in the expression of the indicated mRNAs, each normalized to GAPDH expression, for each subset of CD4+ (A) or CD8+ (B) T cells were calculated as described in the legend for Fig. 1, relative to GαoA mRNA abundance in the naive subset. Data shown in A and B are from one donor each for CD4+ and CD8+ T cells and are representative of three donors. *, p < 0.05 for abundance of each species of mRNA when compared with amounts in naive subsets. Within each CD4+ and CD8+ subset, differences between GαoA and GαoB mRNA levels were also significant. C, poly(A)+ mRNA from human brain and spleen were analyzed by semiquantitative real-time RT-PCR for the expression of mRNAs for GαoA, GαoB, and GAPDH as described earlier. Data shown are the mean -fold differences in GαoA and GαoB mRNAs in spleen relative to the amount of GαoA mRNA and in brain relative to the amount of GαoB mRNA, assayed in triplicate, from one experiment. *, p < 0.05; **, p < 0.005 when comparing GαoA and GαoB mRNA levels within each tissue.
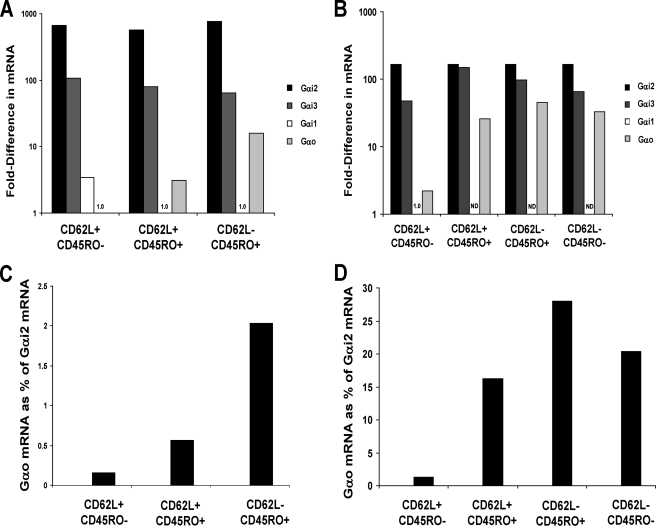
FIGURE 8.
Relative amounts of Gα subunit mRNAs. CD4+ and CD8+ T cell subsets were purified by cell sorting from peripheral blood and analyzed by semiquantitative real-time RT-PCR for the expression of mRNAs for the indicated G protein α-subunits and GAPDH for determining ΔCT values. A, -fold differences in mRNAs in CD4+ T cell subsets. Within each subset of cells, the -fold differences in expression were calculated versus the mRNA with the lowest expression (value set to 1), as shown above the positions for Gαo in the CD62L+CD45RO− cells and Gαi1 in the other subsets. B, -fold differences in mRNAs in CD8+ T cell subsets. Within the CD62L+CD45RO− subset, the -fold differences were calculated versus the mRNA for Gαi1. For the other subsets, because the mRNA for Gαi1 was not detectable (ND), the values for Gαi3 and Gαo were normalized to the value for Gαi2, which was set in each case equal to the Gαi2 value in the CD62L+CD45RO− subset. C, Gαo mRNA as a percentage of Gαi2 mRNA in CD4+ T cell subsets. D, Gαo mRNA as a percentage of Gαi2 mRNA in CD8+ T cell subsets. Data shown are for one donor and are representative of three donors for each group of CD4+ or CD8+ T cell subsets.
Flow Cytometry
For phenotypic analysis of leukocyte subsets based on the expression of cell surface markers, 100 μl of cells at 1 × 107 cells/ml in PBS, 1% FBS, 10 mm HEPES was incubated with dye-conjugated primary antibodies (1 μg) for 15 min on ice. Cells were then washed twice with PBS/FBS/HEPES and fixed in 1% paraformaldehyde. Antibody-staining data were collected on a FACSCalibur (BD Biosciences) flow cytometer. Flow cytometry data files were analyzed with FlowJo software (Tree Star Inc., San Carlos, CA).
In Vitro Activation of Naive Cord Blood CD4+ T Cells
Human cord blood was obtained from term placentas following the delivery of healthy newborns at Shady Grove Adventist Hospital (Gaithersburg, MD) as approved by that institution's review board. Naive CD4+ T cells were isolated from cord blood with the RosetteSep/human CD4+ T cell reagent (StemCell Technologies). Stimulation of the CD4+ T cells was performed as described previously (17). Cells were cultured at 1 × 106 cells/ml in 24-well plates in RPMI 1640 medium/10% FBS with gentamicin (20 μg/ml; Invitrogen) and stimulated with plate-bound anti-CD3 (OKT3, 10 μg/ml), soluble anti-CD28 (1 μg/ml), and rIL-2 (200 IU/ml). In addition, these cells were treated under one of four regimens: anti-IL-4 (0.4 μg/ml), anti-IL-12 (2 μg/ml), and anti-IFNγ (8 μg/ml) with rTGF-β (10 ng/ml) for nonpolarizing (NP) conditions; rIL-12 (2 ng/ml) and anti-IL-4 (0.4 μg/ml) for TH1-polarizing conditions; rIL-4 (4 ng/ml), anti-IL-12 (2 μg/ml), and anti-IFNγ (8 μg/ml) for TH2-polarizing conditions; and with no cytokines (other than rIL-2) and no antibodies as a control. On day 3 or 4, cells were harvested, washed, and resuspended in fresh medium at 1 × 106 cells/ml containing rIL-2 and the appropriate cytokine and antibody combinations. In some experiments, to produce TH17 cells, CD4+ T cells from cord blood were activated with anti-CD3 and anti-CD28 as above (without rIL-2) with rIL-23 (100 ng/ml), rIL-6 (20 ng/ml), rIL-1β (10 ng/ml), rTNFα (10 ng/ml), and rTGF-β (either 2 or 10 ng/ml) as well as anti-IL-4 (0.4 μg/ml), anti-IL-12 (2 μg/ml), and anti-IFNγ (8 μg/ml) antibodies.
Isolation of RNA, Synthesis of cDNA, and Semiquantitative Real-time RT-PCR
In early experiments, total cellular RNA was isolated with the TRIzol reagent (Invitrogen), and first-strand cDNA synthesis was performed with the SuperScript first-strand synthesis system for RT-PCR (Invitrogen) as described by the manufacturer. In experiments involving cells purified by cell sorting, RT-PCR was performed with the Platinum quantitative inventoried RT-PCR ThermoScript one-step system (Invitrogen) as described by the manufacturer. Inventoried primer and probe sets (FAM/MGB-labeled) for human Gαi1, Gαi2, Gαi3, Gαo, Gα13, CD3, CD62L, and GAPDH and for mouse Gαi2, Gαo, and β2-microglobulin were purchased from Applied Biosystems (Foster City, CA). Primers and probes specific for human GαoA and GαoB were designed with Primer Express v2.0 (Applied Biosystems) with probes overlapping variant-specific splice junctions. Primer/probe sequences are available upon request. Real-time PCR analysis was performed on samples in duplicate with either an ABI 7700 or 7900 sequencer system (Applied Biosystems), and data were analyzed by the 2−ΔΔCT method as described (22). Except as noted, ΔCT values for each target mRNA compared with GAPDH (or β2-microglobulin) were determined; ΔΔCT values were calculated by subtracting the highest ΔCT value from the other ΔCT values. Samples with the highest ΔCT values for a given mRNA were given the value of 1, and mRNA levels in other samples were expressed as the -fold difference in mRNA (through calculation of 2−ΔΔCT).
Cell Transfections
HEK293:hCCR6 cells (14) or HEK293T cells were harvested by trypsinization, washed, counted, and transfected with the Amaxa Nucleofector device as described by the manufacturer (Amaxa Inc., Gaithersburg, MD). Cells were resuspended at 5 × 107 cells/ml in Nucleofector solution V (Amaxa Inc.), and 100 μl of cells together with plasmid DNAs (total 5 μg) were treated according to program Q-001. Transfected cells were resuspended in 5 ml of Dulbecco's modified Eagle's medium (DMEM) containing 10% FBS and split into two wells of a 6-well plate. Transfected cells were incubated at 37 °C, 5% CO2 for 48 h before being harvested.
Knockdown of G Protein α-Subunits by Short Interfering RNA (siRNA)
SmartPool control siRNAs (catalogue number D-001810-10-0005), siRNAs specific for Gαi1 (L-010404-00-0005), Gαi2 (L-003897-00-0005), Gαi3 (L-005184-00-0005), Gαo (L-009486-00-0005), and Gαt (L-009827), and a separate custom siRNA for Gαo as described by Krumins and Gilman (23) along with a non-targeting control were obtained from Dharmacon (Lafayette, CO). Each siRNA sample was resuspended in 250 μl of buffer as per the manufacturer's instructions to give 20 μm stock solutions. Transfections were performed with the Amaxa Nucleofector device. Jurkat cells were transfected in solution V with the program S-018, whereas sorted subsets of primary CD4+ T cells were transfected with the T cell Nucleofector solution and program V-024. In all cases, cells were resuspended at 5 × 107 cells/ml in Nucleofector solution, and 100 μl of cells together with 15 or 20 μl of siRNA solution were treated with the appropriate program. Transfected cells were resuspended in 5 ml of DMEM containing 10% FBS and split into two wells of a 6-well plate. Transfected cells were incubated at 37 °C, 5% CO2 for 72 h before being harvested.
Measurement of Calcium Flux
Assays of calcium flux in transfected cells were performed on an RF-M2001 ratio fluorescence spectrometer (Photon Technology International, South Brunswick, NJ) essentially as described (24). Briefly, transfected cells were harvested by trypsinization, washed twice with PBS, and resuspended at 107cells/ml in Hanks' balanced salt solution (HBSS) containing calcium and magnesium, 10 mm HEPES, and 1% FBS (HBSS/FBS) and loaded with 2 μm fura-2 acetoxymethyl ester (Molecular Probes, Eugene, OR) for 40 min at 30 °C followed by two washes in HBSS/FBS buffer. Measurements of calcium flux were made in cuvettes containing 2 ml of cells at 0.5 × 106 cells/ml. Excitation was done alternately at 340 and 380 nm, and emission was measured at 510 nm. The integration time was 0.5 s, and the ratios of the signals obtained at each excitation wavelength were plotted as a function of time.
Chemotaxis Assays
Chemotaxis assays were performed according to standard protocols. Cultured cells were harvested, washed twice in PBS, counted, and resuspended in chemotaxis medium (RPMI 1640 containing 25 mm HEPES, pH 8, and 1% BSA) at 107 cells/ml. Chemotaxis assays were performed with Transwell plates containing 5-μm pores. Cells in 100 μl of chemotaxis medium were added to inserts that were preincubated at 37 °C for 30 min before being placed in wells that contained either medium alone or medium with 100 ng/ml CXCL12 or CCL20 and incubated for 2 h at 37 °C, 5% CO2. Cells that had migrated into the lower wells were harvested and counted with a Vi-CELL analyzer (Beckman Coulter). Dose-response experiments showed that 100 ng/ml was the optimal concentration for both CXCL12 and CCL20 in these chemotaxis assays (data not shown).
Western Blotting
For analysis of leukocyte populations for the expression of individual G protein α-subunits, total protein was measured using either the Bio-Rad assay or Pierce Coomassie Plus reagent (Pierce Biotechnology, Inc.). Cell samples containing equal amounts of protein were boiled in 2× Laemmli buffer and resolved by 10% SDS-PAGE. We used gels of both 8.6 × 6.8 cm and 16 × 16 cm. Gels were transferred to Immobilon-P PVDF membranes (Millipore Corp., Bedford, MA) overnight in the cold in a Transblot apparatus (Bio-Rad Laboratories) at 50 V in 25 mm Tris, 190 mm glycine, 20% methanol. Blots were washed in Tris-buffered saline, pH 7.4, containing 0.01% Tween-20 (TBST) and then blocked in TBST containing 2% (w/v) nonfat dry milk (Bio-Rad Laboratories) for 1 h at room temperature. All subsequent incubations and washes were done in TBST, 2% milk. Blots were incubated with the appropriate primary antibodies (at 1:200 dilution, or 1 μg/ml) for 2 h followed by two 10-min washes and then incubated in a 1:2000 dilution of the appropriate secondary antibody (HRP-conjugated goat anti-rabbit, or donkey anti-goat) for 30 min followed by two washes. For visualizing bands, blots were treated with SuperSignal West Pico chemiluminescent substrate (Pierce Biotechnology) and exposed to X-OMAT XAR film (Eastman Kodak Co.). Quantification of Western blots was performed with Adobe Photoshop (San Jose, CA) and ImageJ software (National Institutes of Health) as described previously (25).
Statistical Analysis
Unpaired, two-tail t tests were performed using InStat version 3 software from GraphPad Software Inc. (San Diego, CA). Statistical significance was indicated by a two-tailed p value of <0.05. Where multiple comparisons were required, simple one-way ANOVA was performed followed by running the Bonferroni post-hoc test.
RESULTS
Gαo Is Expressed in Human Peripheral Blood T Cells
To detect differences in the expression of G proteins between naive and effector/memory T cells, we analyzed purified human peripheral blood CD4+ T cells by Western blotting with subtype-specific antibodies against a number of G protein α-subunits. The major Gi family members found in lymphocytes, Gαi2 and Gαi3 (26, 27), were equivalently abundant in naive and memory cells, as were Gαq/11, and Gα13 (Fig. 1A). Because the Gi proteins are crucial to chemokine-induced functions in leukocytes (28), we investigated the expression of Gαo, a Gi family member for which the expression and function in leukocytes had not been described previously. (In the absence of a reliable specific antibody, we were unable to assess the expression of Gαi1 protein.) We could easily detect Gαo protein but only in effector/memory cells (Fig. 1A). Representative full-length Western blots that show molecular mass markers and positive controls can be seen in supplemental Fig. S1A. In supplemental Fig. S1B, using transfected cells, we provide additional evidence that the anti-Gαi/o antibodies recognized the appropriate proteins. We also confirmed our finding that the Gαo protein was expressed in effector/memory CD4+ T cells in separate experiments using a second commercially available anti-Gαo antibody (supplemental Fig. S2).
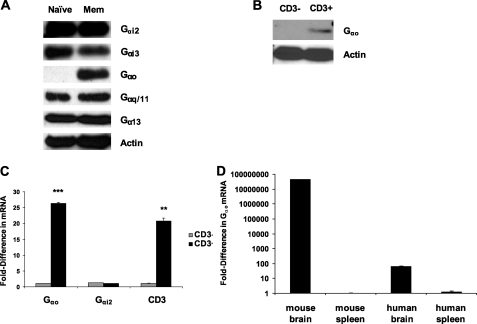
FIGURE 1.
Gαo is expressed in peripheral blood T cells, preferentially in the memory subset. A, CD4+ T cells were isolated from peripheral blood by negative selection and then further purified into naive and effector/memory subsets as described under “Experimental Procedures.” Whole-cell lysates (100 μg of protein) were analyzed by Western blotting with rabbit polyclonal anti-Gα or anti-actin antibodies as indicated. Results are for naive and effector/memory CD4+ T cells from one donor and are representative of three donors. Representative full-length Western blots that show molecular mass markers and positive controls can be seen in supplemental Fig. S1. B, CD3+ and CD3− cells were purified from peripheral blood with magnetic beads for CD3. Whole-cell lysates (100 μg of protein) were then analyzed by Western blotting with anti-Gαo and anti-actin antibodies. Results are for cells from one donor and are representative of two donors. C, CD3+ and CD3− cells were isolated as described for B, total RNA was isolated from each subset, and samples were then analyzed by semiquantitative real-time RT-PCR for the expression of mRNAs for Gαo, Gαi2, CD3, and as a control, GAPDH. The -fold differences in abundance of the indicated mRNAs, each normalized to GAPDH expression, between CD3− (gray bars) and CD3+ cells (black bars) were calculated according to the method of ΔΔCT. For each mRNA of interest, the lowest level of expression versus GAPDH from a single well for both CD3+ and CD3− samples was set at one. Values cannot be compared between mRNA species. The data shown are the mean -fold differences ± S.E. in expression for the indicated mRNAs from one donor from assays performed in duplicate and are representative of three donors, separate from those analyzed in B. **, p < 0.005; and ***, p < 0.0005, when comparing CD3− and CD3+ cells. D, poly(A)+ mRNA from mouse and human brain and spleen samples were analyzed by semiquantitative real-time RT-PCR for the expression of mRNAs for Gαo and either β2-microglobulin in the case of mouse samples or GAPDH for human samples. Data shown are the mean -fold differences ±S.E. in Gαo mRNA for each sample within each species, assayed in triplicate, from one experiment.
This finding led us to examine other leukocyte populations for the expression of Gαo. Analysis of Western blots of lysates of cells purified from peripheral blood on the basis of CD3 revealed that Gαo was found in CD3+ cells (consisting mainly of CD4+ and CD8+ α/β T cells) but not in CD3− cells (Fig. 1B). This difference was confirmed at the level of mRNA by real-time RT-PCR analysis of the same cell types, where the relative difference in the expression of Gαo mRNA between the purified CD3− and CD3+ samples was similar to that of CD3 itself (Fig. 1C). The abundance of Gαi2 mRNA was not significantly different between the groups (Fig. 1C).
The experimental advantages of using mice led us to investigate whether Gαo was found in mouse lymphocytes, where published data suggested that Gαo was not expressed (29). To compare relative levels of Gαo mRNA, we analyzed the abundance of Gαo mRNA in spleen and brain for both BALB/c mouse and human tissues. In the human samples, real-time RT-PCR analysis showed a ΔΔCT value of between 6 and 7 when comparing brain and spleen RNAs, indicating an ∼90-fold higher abundance of Gαo mRNA in brain compared with spleen (Fig. 1D). However, Gαo mRNA, although highly expressed in mouse brain, was undetectable in spleen, resulting in a ΔΔCT of at least 25 (Fig. 1D), consistent with published data from Northern blot analysis (29). Together, the data demonstrate that although Gαo can be detected in human T cells, this is not the case in mice.
Gαo Is Most Abundant in Differentiated CD4+ and CD8+ T Cells
Because we found that Gαo protein was found in CD3+ T cells and that it was more abundant in memory than in naive CD4+ T cells, we looked more carefully at Gαo mRNA and protein in specific subsets of CD4+ and CD8+ T cells, which were sorted on the basis of the surface markers CD62L and CD45RO to define naive (CD62L+CD45RO−), central memory (CD62L+CD45RO+), and effector memory (CD62L−CD45RO+; CD62L−CD45RO−) cells (5, 18). CD45RO is a protein-tyrosine phosphatase involved in T cell activation for which alternative mRNA splicing yields isoforms differentially expressed on naive cells compared with effector/memory cells (30). Substantial numbers of CD62L−CD45RO− cells are present only within the CD8+ population; we needed to use the metalloproteinase inhibitor TAPI-0 to obtain pure populations of these cells, which otherwise were contaminated with naive (CD45RO−) cells that had lost surface CD62L during processing (see “Experimental Procedures”). The three subsets of CD4+ and four subsets of CD8+ T cells were sorted by flow cytometry, and real-time RT-PCR was performed as described previously. Analysis of CD4+ T cell subsets revealed that, as before, Gαo mRNA was expressed at low abundance in naive cells (CD62L+CD45RO−) but was progressively more abundant in TCM (CD62L+CD45RO+) followed by TEM (CD62L−CD45RO+), (Fig. 2A). Moreover, none of the mRNAs for Gαi2, Gαi3, and Gα13 were significantly different in their abundance among the CD4+ T cell subsets.
A similar pattern of Gαo mRNA expression was observed when sorted subsets of CD8+ T cells were analyzed (Fig. 2B). Naive CD8+ T cells expressed the lowest amount of Gαo mRNA, whereas the most differentiated TEM (CD62L−CD45RO+/CD45RO−) generally had the highest abundance of Gαo mRNA, with no significant differences among the subsets for the other G protein α-subunits analyzed (Fig. 2B). We analyzed purified subsets of CD8+ T cells and, for the purposes of comparison, CD4+ T cells from the same donor by Western blotting. Memory cells were pooled for Western blotting because of limitations in the numbers of cells within memory subsets from individual donors. Consistent with the above patterns of Gαo mRNA expression, Gαo protein was more abundant in memory CD8+ T cells than in naive cells (Fig. 2C). Both naive and memory subsets of CD8+ T cells had higher amounts of Gαo protein than did their CD4+ T cell counterparts (Fig. 2C), although Gαo could not be detected in naive CD8+ T cells from all donors (data not shown).
GαoB mRNA Is More Abundant Than GαoA mRNA in Differentiated T Cells
Alternative splicing of Gαo mRNA gives rise to two protein isoforms, GαoA and GαoB, which differ in their C-terminal sequences. The GαoA isoform is more abundant than the GαoB isoform in mouse brain and heart (29, 31, 32). We used real-time RT-PCR to examine the relative expression of GαoA and GαoB mRNAs in T cell subsets. We first used plasmid DNAs encoding GαoA or GαoB sequences to demonstrate the specificities and equal efficiencies for the primer/probe sets that we had designed (data not shown). We then analyzed sorted subsets of CD4+ and CD8+ T cells for the expression of GαoA versus GαoB mRNAs and found that both Gαo isoforms were more highly expressed in TEM subsets compared with naive subsets (Fig. 3, A and B). Comparison of the ΔCT values revealed that, unexpectedly, GαoB mRNA was ∼12-fold more abundant than GαoA mRNA (Fig. 3, A and B). Real-time RT-PCR analysis of Gαo isoform mRNA expression in human brain revealed that, as expected, GαoA mRNA was ∼2-fold more abundant than that of GαoB (Fig. 3C). By contrast, and consistent with our data from peripheral blood lymphocytes, GαoB mRNA was ∼10-fold more abundant than GαoA mRNA in human spleen (Fig. 3C).
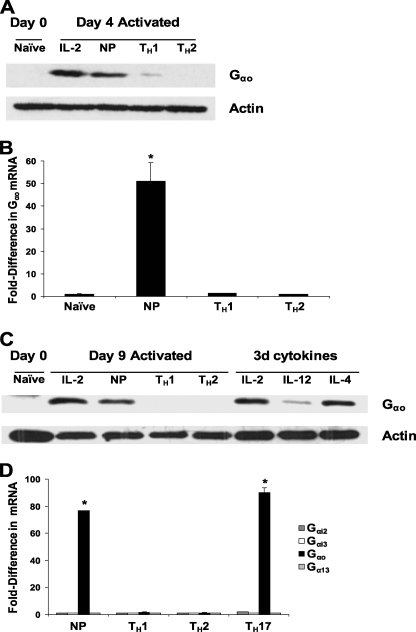
Gαo mRNA Expression Is Increased in CD4+ T Cells Activated in Vitro under Nonpolarizing or TH17-polarizing Conditions
The increased expression of Gαo mRNA in TEM compared with naive cells suggested that Gαo expression was induced during T cell activation and differentiation. We investigated this with an in vitro system for activation and differentiation of human T cells. Cord blood naive CD4+ T cells were activated in the presence of cytokines and anti-cytokine antibodies to yield TH1, TH2, or NP cells, and cells were also activated in the presence of IL-2 alone, i.e. under “neutral” conditions without other added cytokines or anti-cytokine antibodies. Consistent with our previous data from adult peripheral blood (Figs. 1A and 2C), naive CD4+ T cells from cord blood had no detectable Gαo by Western blotting (Fig. 4A). Activation of these cells for 4 days led to an increase in the abundance of Gαo protein in cells that were not polarized but not in cells activated under TH1- or TH2-polarizing conditions (Fig. 4A). Analysis of Gαo mRNA by real-time RT-PCR supported the Western blotting data (Fig. 4B). By contrast with Gαo, the amounts of mRNAs for Gαi2, Gαi3, and Gα13 were not affected by activation under these conditions (Fig. 4D).
FIGURE 4.
Gαo mRNA and protein are expressed in CD4+ T cells activated in vitro under NP or TH17-polarizing conditions. Naive CD4+ T cells were isolated from cord blood by negative selection and then activated for 6 days with anti-CD3 and anti-CD28 in the presence of rIL-2 alone (IL-2); rIL-2, rTGF-β and antibodies against IL-12, IFNγ, and IL-4 (NP); rIL-2 with rIL-12 and anti-IL-4 (TH1); or rIL-2 with rIL-4 and anti-IL-12 and anti-IFNγ (TH2) as described under “Experimental Procedures.” A, whole-cell lysates (100 μg of protein) from each condition harvested after 4 days of activation were analyzed by Western blotting with anti-Gαo and anti-actin antibodies. The data shown are from one donor and are representative of three donors. B, in separate experiments, cells were activated for 6 days, as described in A, after which each cell type was analyzed by semiquantitative real-time RT-PCR for the expression of mRNAs for Gαo and, as a control, for GAPDH, as described in the legend for Fig. 1. The data shown are the mean -fold differences ± S.E. in expression for Gαo mRNA for assays performed in duplicate for one donor and are representative of three donors. *, p < 0.05 when compared with mRNA abundance in the naive subset. C, naive CD4+ T cells were isolated from cord blood by negative selection and activated for 6 days as described in A. Subsequently, cells were cultured for an additional 3 days under NP or polarizing conditions as indicated. In addition, on day 6, cells that had been activated under NP conditions were left untreated (IL-2) or were treated with rIL-12 (IL-12) or rIL-4 (IL-4) until day 9. Whole-cell lysates (100 μg of protein) from each condition were analyzed by Western blotting with anti-Gαo and anti-actin antibodies. Results are from one donor and are representative of three donors. D, naive CD4+ T cells from cord blood were activated for 6 days with anti-CD3 and anti-CD28 under NP, TH1-, TH2-, or TH17-polarizing conditions as described under “Experimental Procedures.” -Fold differences among the samples in the expression of Gαi2, Gαi3, Gαo, and Gα13 mRNAs, normalized to GAPDH mRNA, were calculated as described in the legend for Fig. 1. For each mRNA of interest, the lowest level of expression versus GAPDH from a single well was set at 1. Values cannot be compared between mRNA species. The data shown are the mean -fold differences ± S.E. in the abundance of the indicated mRNAs assayed in duplicate for one donor and are representative of two donors. *, p < 0.05 when compared with Gαo mRNA abundance in TH2-polarized cells, which showed the lowest Gαo expression.
In an effort to examine the stability of Gαo expression in nonpolarized cells, we activated naive cord blood cells as described above, and after 6 days removed the cells from activation and cultured them for 3 days in IL-2 alone. A sample of nonpolarized cells was also moved to media with polarizing cytokines, either IL-12 or IL-4. After the 9 days, Gαo protein was still confined to the nonpolarized cells and was not detectable in cells activated initially under either TH1- or TH2-polarizing conditions (Fig. 4C, Day 9 Activated). Treatment of nonpolarized, Gαo-high cells with IL-12 for 3 days substantially decreased the abundance of Gαo, whereas treatment with IL-4 had no such effect (Fig. 4C, 3d cytokines). In investigating non-TH1 and non-TH2 subsets; we next analyzed cord blood cells cultured under conditions that have been described as driving mouse CD4+ T cells to differentiate to produce IL-17 (33). As noted above, TH17 cells are a recently recognized separate lineage of non-TH1, non-TH2 memory/effector CD4+ T cells thought to be critical in autoimmune disease (34). Cells activated under TH17 conditions showed significant induction of Gαo mRNA, comparable to that seen in the nonpolarized cells (Fig. 4D).
Chemokine Receptors CCR6, CXCR6, and CXCR4 Couple to Gαo-containing G Proteins
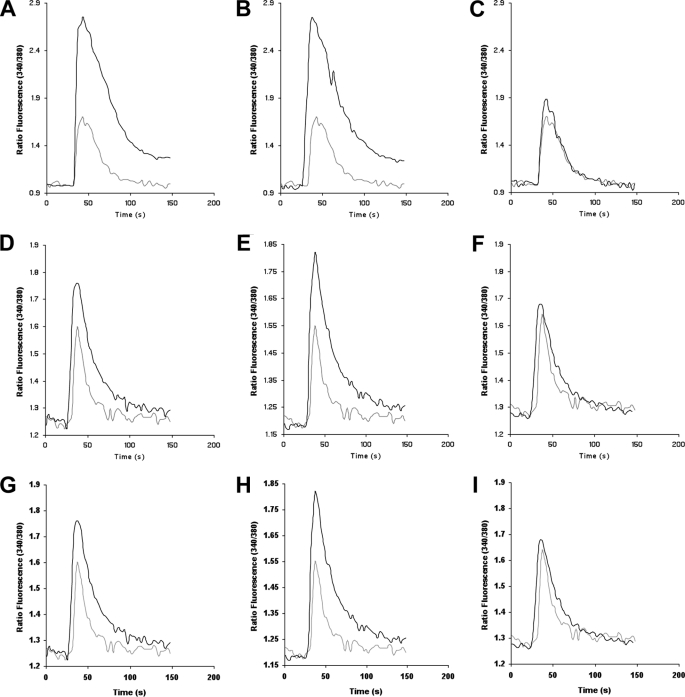
We next investigated whether the presence of Gαo in memory/effector T cells might have functional relevance for the many chemokine receptors found on these cells. We measured intracellular Ca2+ mobilization in cells transfected with plasmids encoding chimeric G protein α-subunits, in which the last five amino acid residues of Gαq have been replaced with those of Gαo, Gαi2, or Gαs to create the chimeras Gαqo5, Gαqi5 and Gαqs5, respectively (15, 16, 35). Because the last five amino acid residues of the α-subunit are critical for the coupling of a G protein to a given GPCR, Gαqo5, Gαqi5, and Gαqs5 allow GPCRs coupled to Gαo-, Gαi2-, and Gαs-containing G proteins, respectively, to activate Gαq-dependent pathways such as phospholipase Cβ-mediated intracellular Ca2+ mobilization (15, 16, 35). Because the last five amino acid residues of GαoA and GαoB are identical (29), the Gαqo5 chimera serves to analyze responses common to both isoforms.
Transfection of an HEK293 cell line stably expressing CCR6 with a plasmid encoding Gαqo5 resulted in an increase in the mobilization of intracellular Ca2+ in response to the CCR6 ligand, CCL20, when compared with cells transfected with empty vector (Fig. 5A), similar to the increase following transfection with a plasmid encoding Gαqi5 (Fig. 5B). CCR6 is a receptor found on effector/memory T cells (36) and, in particular, on all cells of the TH17 lineage (37–39). As expected, given that chemokine receptors do not couple to Gs proteins (28), transfection with Gαqs5 had no effect on Ca2+ mobilization (Fig. 5C). Western blots of cell lysates showed equivalent abundance of all three HA-tagged chimeric G proteins (data not shown). We performed similar experiments in 293T cells co-transfected with a plasmid encoding YFP-tagged CXCR6, a second chemokine receptor found on effector/memory T cells (40), and either control empty vector or plasmids encoding the chimeric G protein α-subunits as described above and treated with the CXCR6 ligand, CXCL16. As for CCR6, CXCR6 coupled to Gαqo5 (and Gαqi5)- but not Gαqs5-containing G proteins (Fig. 5, D–F). Analogous experiments were performed in transfected Jurkat T cells, a human CD4+ T cell line, in which we found that the endogenously expressed chemokine receptor CXCR4, which is expressed on both naive and memory T cells, could also couple to both Gαqi5- and Gαqo5-containing G proteins to mobilize intracellular calcium (Fig. 5, G–I). The effects of expressing Gαqo5 or Gαqi5 on signaling through CXCR6 and CXCR4 were smaller than for CCR6, possibly because co-transfections were used to express CXCR6 and because of the lower efficiency of transfection for Jurkat versus HEK293T cells.
FIGURE 5.
The human chemokine receptors, CCR6, CXCR6, and CXCR4 can couple to G proteins containing the chimeric Gαqo5. A–C, HEK293:CCR6 cells were transfected with plasmids encoding each of the chimeric G protein α-subunits, Gαqo5 (A), Gαqi5 (B), and Gαqs5 (C), and as a control, the empty vector, pcDNA3.1(+), as described under “Experimental Procedures.” D–F, in separate experiments, HEK293T cells were co-transfected with plasmids encoding CXCR6-YFP, each of the chimeric G protein α-subunits, Gαqo5 (D), Gαqi5 (E), and Gαqs5 (F), and as a control, the empty vector, pcDNA3.1(+). G–I, Jurkat T cells, which express CXCR4 endogenously, were transfected with plasmids encoding each of the chimeric G protein α-subunits, Gαqo5 (G), Gαqi5 (H), and Gαqs5 (I), and as a control, the empty vector, pcDNA3.1(+). After 48 h, cells were harvested, loaded with fura-2/AM, and assayed for intracellular calcium mobilization in response to treatment with the chemokine CCL20 (for CCR6), CXCL16 (for CXCR6), or CXCL12 (for CXCR4) at 1 μg/ml, added at ∼25 s. Fluorescence measurements were made as described under “Experimental Procedures.” Individual panels show intracellular calcium mobilization for cells transfected with a plasmid encoding the G protein chimera (black trace) compared with pcDNA3.1(+)-transfected control cells (gray trace) from one experiment each for HEK293:CCR6 cells (A–C), HEK293T cells (D–F), and Jurkat cells (G–I) and are representative of three experiments.
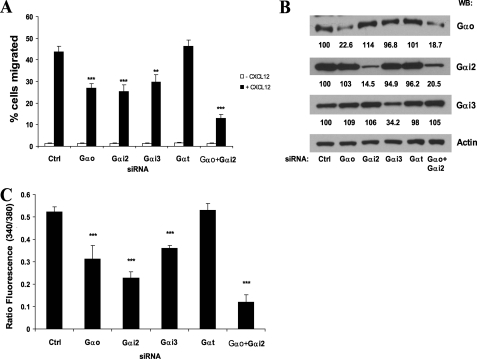
Knockdown of Gαo Inhibits CXCL12-dependent Chemotaxis and Ca2+ Flux
To determine whether the presence of Gαo in T cell subsets was physiologically relevant, we used siRNA to knock down Gαo in Jurkat cells and examined these cells for their ability to migrate or mobilize intracellular Ca2+ in response to CXCL12. Knockdown of Gαo resulted in a ∼40% decrease in the number of cells that migrated to CXCL12 compared with that of cells transfected with either control siRNA or siRNA specific for Gαt, which is not expressed in these cells (Fig. 6A). We confirmed these data by knocking down Gαo with an independent Gαo-specific siRNA (23) (supplemental Fig. S3). Surprisingly, the effect of knockdown of Gαo on chemotaxis was similar to that of knockdown of either Gαi2 or Gαi3 (Fig. 6A). Chemotaxis of cells transfected with siRNAs against both Gαo and Gαi2 was even more significantly inhibited than that of cells depleted of either protein alone. The efficiencies and specificities of these siRNAs in knocking down their targets were verified by Western blotting (Fig. 6B). We also examined the effect of knockdown of these Gαi subunits on CXCL12-dependent Ca2+ mobilization, which is a much more rapid functional response to stimulation of chemokine receptors than is chemotaxis. Knockdown of Gαo, Gαi2, or Gαi3 had similar effects on the inhibition of CXCL12-induced Ca2+ flux as compared with cells transfected with either control or Gαt-specific siRNAs (Fig. 6C). Consistent with our chemotaxis data (Fig. 6A), knockdown of both Gαo and Gαi2 had a more dramatic effect on Ca2+ flux than that observed in cells transfected with either siRNA alone (Fig. 6C).
FIGURE 6.
Knockdown of Gαo inhibits CXCL12-mediated chemotaxis and Ca2+ flux in Jurkat cells. A, Jurkat cells transfected with the indicated SmartPool siRNAs were harvested 72 h later and used in duplicate in Transwell chemotaxis assays. Data shown are the mean percentage ± S.E. of starting cells that migrated to either medium alone or CXCL12 (100 ng/ml) and are combined from six experiments. ***, p < 0.001; **, p < 0.01 when compared with CXCL12-dependent migration of cells transfected with control siRNA. B, lysates (15 μg) of the cells used in the chemotaxis assays in A were resolved by SDS-PAGE and analyzed by Western blotting (WB) for the indicated G protein α-subunits and for actin as a loading control. Data shown are from a single experiment and are representative of three experiments. Actin is shown for only one of the three blots. For each blot, bands were analyzed by densitometry; the quantitative data, normalized to actin and then to control (Ctrl), which was set to 100, are shown below each lane. C, in parallel to chemotaxis assays, siRNA-transfected cells were analyzed for their ability to mobilize intracellular Ca2+ in response to CXCL12 (1 μg/ml) as described under “Experimental Procedures.” Data shown are the mean ratio of fluorescence (340 nm:380 nm) ± S.E. from three independent experiments. ***, p < 0.001 when compared with the CXCL12-dependent Ca2+ flux of cells transfected with control siRNA.
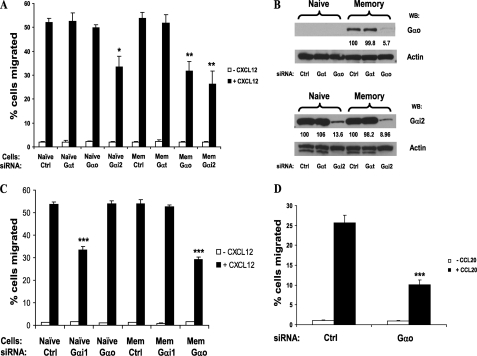
We extended our findings by examining the effect of knockdown of G protein α-subunits in primary cells. We sorted naive and memory subsets of human CD4+ T cells from peripheral blood and transfected them with the appropriate siRNAs. Transfection of naive CD4+ T cells with siRNA against Gαo had no effect on their chemotaxis to CXCL12 (Fig. 7A), consistent with their lack of expression of Gαo. However, knockdown of Gαi2 reduced CXCL12-mediated chemotaxis by ∼35% compared with that of control cells (Fig. 7A). In contrast, knockdown of Gαo in memory CD4+ T cells had a similar effect to that of Gαi2 knockdown on chemotaxis to CXCL12 (Fig. 7A). As before, the specificities of the siRNAs were verified by Western blot analysis (Fig. 7B). These data suggest that the contribution of Gαo to chemokine-dependent migration of human memory CD4+ T cells is equivalent to that of the abundant Gαi2.
FIGURE 7.
Gαo and Gαi1 contribute, respectively, to chemotaxis of effector/memory and naive CD4+ T cells. A, naive and memory CD4+ T cells purified by cell sorting from peripheral blood were transfected with the indicated SmartPool siRNAs and harvested after 72 h. Chemotaxis assays were performed as described in the legend for Fig. 6. Data shown are the mean percentage ± S.E. of starting cells that migrated to either medium alone or CXCL12 (100 ng/ml) and are combined from three experiments. *, p < 0.05 when compared with control (Ctrl) siRNA-transfected naive cells; **, p < 0.01 when compared with control siRNA-transfected memory cells. B, lysates (15 μg) of siRNA-transfected naive and memory CD4+ T cells were analyzed by Western blotting (WB) for the indicated G protein α-subunits and for actin as a loading control. Data shown are from one of two experiments. For each blot, bands were analyzed by densitometry and the quantitative data, normalized to actin and then to the matching Ctrl, which was set to 100, are shown below each lane having a detectable band. C, naive and memory CD4+ T cells were purified, transfected, and analyzed in chemotaxis assays as in A. Data shown are the mean percentage ± S.E. of starting cells that migrated to either medium alone or CXCL12 (100 ng/ml) from duplicate wells of one experiment and are representative of three experiments. ***, p < 0.001 when compared with the CXCL12-mediated migration of the matching control siRNA-transfected naive or memory cells. D, cord blood naive CD4+ T cells were cultured under TH17-polarizing conditions after which CCR6-expressing cells were purified with magnetic beads. The purified cells were transfected with the indicated siRNAs and, after 72 h, analyzed in chemotaxis assays as described in A using the CCR6 ligand, CCL20. Data shown are the mean percentage ± S.E. of starting cells that migrated to either medium alone or CCL20 (100 ng/ml) from experiments with three donors. ***, p < 0.001 when compared with the CCL20-mediated migration of the control siRNA-transfected cells.
In separate experiments to test the effect of knockdown of Gαo on primary human memory CD4+ T cells, we used siRNA specific for Gαi1 as a negative control because Gαi1 had not been previously detected in lymphocytes (26, 27). We were therefore surprised to find that knockdown of Gαi1 in purified naive CD4+ T cells led to a ∼35% decrease in CXCL12-dependent chemotaxis compared with that of control naive cells, whereas knockdown of Gαi1 in memory CD4+ T cells had no effect (Fig. 7C). In agreement with our previous data, siRNA-mediated knockdown of Gαo inhibited CXCL12-dependent chemotaxis of memory, but not naive, CD4+ T cells (Fig. 7C). Because we could not identify a Gαi1 band on Western blots of naive CD4+ T cells using commercial antibodies (data not shown), we verified the specificity of siRNA-mediated knockdown of the appropriate G protein α-subunits by real-time RT-PCR (data not shown). Together, these data suggest that, analogous to the role of Gαo in memory CD4+ T cell subsets, the minor G protein α-subunit Gαi1 makes a substantial contribution to chemotactic responses in naive CD4+ T cells.
To extend our findings for Gαo in primary cells, we cultured cord blood naive CD4+ T cells under TH17-polarizing conditions and then used magnetic beads to purify cells that expressed CCR6, which is expressed on all TH17 cells (39). Purified cells were transfected with control or Gαo-specific siRNAs and subjected to chemotaxis assays with the CCR6 ligand, CCL20. Knockdown of Gαo resulted in a ∼60% reduction in migration (Fig. 7D), indicating that in addition to coupling to CXCR4, Gαo-containing G proteins also couple to CCR6 to mediate chemotaxis in primary CD4+ T cells.
Comparative Analysis of the Expression of G Protein α-Subunit mRNAs Reveals the Enrichment of Gαo and the Decline of Gαil in Memory T Cell Subsets
To make direct comparisons among the different G protein α-subunit mRNAs by RT-PCR, we first established that the corresponding sets of primers and probes showed equal efficiencies of amplification from plasmids containing each of the Gα cDNA sequences (data not shown). We then used these sets of primers and probes to analyze samples from sorted populations of T cells. Our data are summarized in Fig. 8. Gαi2 mRNA was the most abundant G protein α-subunit mRNA in all subsets analyzed. Gαo mRNA abundance in CD4+ effector/memory cells was ∼2% of that of Gαi2 mRNA. As mentioned previously, the abundance of Gαo mRNA was generally higher in naive CD8+ T cells than in their CD4+ T cell counterparts, and similar (or sometimes higher) -fold increases in the abundance of Gαo mRNA were observed during CD8+ T cell differentiation compared with that of CD4+ T cells. These findings are reflected in Gαo mRNA being found at a higher percentage of that of Gαi2 mRNA in CD8+ T cells as compared with CD4+ T cells (Fig. 8, C and D). Of interest, Gαi1 mRNA was not detectable in most of the subsets analyzed but was expressed at low abundance in naive subsets of CD4+ and CD8+ T cells (Fig. 8, A and B), which is consistent with the effect of Gαi1-specific siRNA on the migration of naive, but not memory, CD4+ T cells (Fig. 7C). The amount of Gαi1 mRNA was substantially lower in the more differentiated cells, sometimes below the limit of detection, especially in CD8+ T cells. Despite our inability to detect Gαi1 in Western blots of T cell protein, these findings raise the interesting possibility of a reciprocal relationship between Gαo and Gαi1 mRNA expression in human T cell subsets.
DISCUSSION
As far as we are aware, ours is the first description of the expression of Gαo in hematopoietic cells and the first description of differences in the content of Gα subunits in memory cells as compared with naive T cells. We have shown that among the major subsets of leukocytes in human peripheral blood, expression of Gαo was limited to T cells, and that, in contradistinction to other Gα subunits, expression of Gαo was correlated with increasingly differentiated phenotypes, with the most dramatic increment occurring in the naive to TCM transition. Our mRNA data and knockdown experiments also suggest that expression of Gαi1 shows a reciprocal profile. Beyond the immune system, we believe that these are the first examples reported of changes in the repertoire of Gαi/o subunits as part of pathways of cellular differentiation in the adult.
Gαo is highly abundant in the central nervous system, so much so that it constitutes ∼0.5–1.0% of the plasma membrane protein of the brain (41, 42). Its expression has been reported to be restricted to the central nervous system, the endocrine system, and the heart, and Gαo cannot be detected in mouse spleen or thymus (29, 43). Two main forms of Gαo are expressed, GαoA and GαoB, resulting from alternative splicing of mRNA, which produces differences in the C-terminal third of each protein (29, 31, 32, 44). In addition, there are two further isoforms of Gαo, GαoC and GαoD, which are derived from posttranslational modifications of GαoA and GαoB, respectively (45).
Within the nervous system, Gαo activates neuronal Ca2+ and K+ channels (46–50). Mice defective in Gαo show abnormalities that include tremors, impaired olfactory behavior, and decreased survival of neurons in the basal vomeronasal organ, as well as defective ion channel regulation in the heart (43, 51–53). In contrast to Gαo, Gαi1 is more widely distributed (54), although it also has not been detected previously in mouse lymphocytes (26) or, to our knowledge, in human lymphocytes. Apparently, mice deficient in Gαi1 exhibit no abnormalities (55). Gαi2 and Gαi3 are considered the major Gαi subunits in hematopoietic and immune cells given their expression in mouse T cells (56) and the immunological, proinflammatory phenotype of Gαi2-deficient mice (57, 58).
We found that by contrast to brain (and other tissues (29)), human T cells contained more GαoB than GαoA mRNA; these are the first cells, to our knowledge, described as showing this pattern of differential splicing. We recapitulated differentiation-associated induction of Gαo in T cells by activating naive cord blood cells in vitro through the T cell receptor (TCR), and have shown that, just as for many aspects of T cell differentiation, induction of Gαo depended both on activation and on the cytokine environment. Of particular interest, we found preferential expression of Gαo under conditions inducing TH17 cells, which have recently been recognized as a separate lineage of effector/memory CD4+ T cells important for autoimmune disease (34). We have provided the first evidence that Gαo-containing G proteins can couple to chemokine receptors that are expressed on T cells, including the TH17-associated receptor, CCR6 (37–39). Finally, we have shown that siRNA-mediated depletion of Gαi1 in primary naive CD4+ T cells and of Gαo in memory CD4+ T cell subsets inhibited CXCR4-mediated migration to a similar extent to knocking down the major Gα subunit, Gαi2. These data suggest that CXCR4, and perhaps other GPCRs, switch their Gα subunit usage from Gαi1 in naive CD4+ T cells to Gαo in memory CD4+ T cell subsets and that the contribution of these Gα subunits to GPCR-mediated functions belies their relatively low abundance in these cells. The discordance between functional importance and relative abundance was also reported for Gαq as compared with Gα11 in HeLa cells (23). It is notable that in those experiments, knocking down some species of Gαi/o subunits resulted in “compensatory” increases in others (23). We did not observe such changes among the limited number of Gα proteins that we analyzed, perhaps because we harvested cells at only 3 days after transfection with siRNA and not the 5 days used in the previous study and/or because of cell type-specific differences.
We presume that Gαo and Gαi1 have roles in T cells beyond chemokine receptor signaling. One possible role for Gαo would be in signaling from GPCRs such as species of opioid, muscarinic acetylcholine (mAChR), and somatostatin receptors, which are expressed in the central nervous system, have been shown to use Gαo (59–61), and can be expressed by T cells (62–69).
The published data on downstream targets of activated Gαo raise some additional, interesting possibilities as to specific roles for Gαo in memory T cells. For example, channels with characteristics of L-type Ca2+ channels are found in T cells, and inhibitor studies have shown that these channels play a role in mediating TCR-induced lymphocyte activation and proliferation both in vitro and in vivo (70, 71). Given the documented, specific role for Gαo in regulating these channels in the heart (43), it is possible that Gαo contributes to the differences in Ca2+ signals, and other consequences of TCR activation that distinguish memory from naive T cells (72). Connections between chemokine receptors, G proteins, and the TCR are suggested by reports that CXCL12 acts as a costimulator for the activation of CD4+ T cells (73) and that CXCR4 activates ζ chain-associated protein kinase of 70 kDa (Zap70) (74) and associates directly with the TCR (75). In addition, Gαi2 mediates inhibition of TCR-induced Ca2+ signals and cytokine production (27).
Finally, Gαo is thought to mediate the activities of Wnt receptors (frizzled proteins) in mouse cells (76) and in Drosophila (77, 78), and the effectors of the Wnt pathway, β-catenin and lymphoid-enhancing factor/T cell factor proteins, are important, respectively, for thymocyte survival (79) and T cell differentiation (80). A possible role for (Gαo-mediated) Wnt signaling in the survival, proliferation, or both of memory T cells is intriguing but as yet unexplored. However, the accumulating data that chemokine receptors are involved in stimulating cell growth and proliferation (81, 82), and that GPCRs other than frizzled proteins can activate components of the Wnt pathway (83) raise the possibility that chemokine receptor signaling through Gαo to the β-catenin pathway in memory T cells could contribute to their proliferation. However, given the lack of Gαo protein in mouse lymphocytes, any of the possible roles that we have suggested for Gαo would by necessity be specific to human T cells, representing a clear difference between the immune system in humans and mice.
Supplementary Material
Acknowledgments
We are very grateful to Dr. Bruce R. Conklin, Gladstone Institute of Cardiovascular Disease, University of California, San Francisco, for providing cDNAs of chimeric G protein α-subunits and to Dr. William F. Simonds, Metabolic Diseases Branch, NIDDK, National Institutes of Health, and Dr. Paul Goldsmith, Center for Cancer Research, NCI, National Institutes of Health, for helpful discussions. We thank Calvin Eigsti, Flow Cytometry Section, Research Technology Branch, NIAID, National Institutes of Health, for help with cell sorting.
This work was supported, in whole or in part, by the National Institutes of Health NIAID Intramural Research Program.

The on-line version of this article (available at http://www.jbc.org) contains supplemental Figs. S1–S3.
- TH
- helper T (cells)
- IL
- interleukin
- TCM
- central memory T cells
- TEM
- effector memory T cells
- GPCR
- G protein-coupled receptor
- NP
- nonpolarized
- TCR
- T cell receptor
- rIL
- recombinant interleukin.
REFERENCES
- 1.Seder R. A., Ahmed R. (2003) Nat. Immunol. 4, 835–842 [DOI] [PubMed] [Google Scholar]
- 2.Berke G. (1995) Immunol. Today 16, 343–346 [DOI] [PubMed] [Google Scholar]
- 3.Harty J. T., Tvinnereim A. R., White D. W. (2000) Annu. Rev. Immunol. 18, 275–308 [DOI] [PubMed] [Google Scholar]
- 4.Sallusto F., Geginat J., Lanzavecchia A. (2004) Annu. Rev. Immunol. 22, 745–763 [DOI] [PubMed] [Google Scholar]
- 5.Rabin R. L., Park M. K., Liao F., Swofford R., Stephany D., Farber J. M. (1999) J. Immunol. 162, 3840–3850 [PubMed] [Google Scholar]
- 6.Hadcock J. R., Ros M., Watkins D. C., Malbon C. C. (1990) J. Biol. Chem. 265, 14784–14790 [PubMed] [Google Scholar]
- 7.Loganzo F., Jr., Fletcher P. W. (1992) Mol. Endocrinol. 6, 1259–1267 [DOI] [PubMed] [Google Scholar]
- 8.Loganzo F., Jr., Fletcher P. W. (1993) Mol. Endocrinol. 7, 434–440 [DOI] [PubMed] [Google Scholar]
- 9.Bahouth S. W. (1995) Biochem. J. 307, 831–841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.El Jamali A., Rachdaoui N., Dib K., Corrèze C. (1998) J. Neurochem. 71, 2271–2277 [DOI] [PubMed] [Google Scholar]
- 11.Goldman D. W., Chang F. H., Gifford L. A., Goetzl E. J., Bourne H. R. (1985) J. Exp. Med. 162, 145–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neptune E. R., Bourne H. R. (1997) Proc. Natl. Acad. Sci. U.S.A. 94, 14489–14494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neptune E. R., Iiri T., Bourne H. R. (1999) J. Biol. Chem. 274, 2824–2828 [DOI] [PubMed] [Google Scholar]
- 14.Liao F., Alderson R., Su J., Ullrich S. J., Kreider B. L., Farber J. M. (1997) Biochem. Biophys. Res. Commun. 236, 212–217 [DOI] [PubMed] [Google Scholar]
- 15.Conklin B. R., Herzmark P., Ishida S., Voyno-Yasenetskaya T. A., Sun Y., Farfel Z., Bourne H. R. (1996) Mol. Pharmacol. 50, 885–890 [PubMed] [Google Scholar]
- 16.Conklin B. R., Farfel Z., Lustig K. D., Julius D., Bourne H. R. (1993) Nature 363, 274–276 [DOI] [PubMed] [Google Scholar]
- 17.Rabin R. L., Alston M. A., Sircus J. C., Knollmann-Ritschel B., Moratz C., Ngo D., Farber J. M. (2003) J. Immunol. 171, 2812–2824 [DOI] [PubMed] [Google Scholar]
- 18.Song K., Rabin R. L., Hill B. J., De Rosa S. C., Perfetto S. P., Zhang H. H., Foley J. F., Reiner J. S., Liu J., Mattapallil J. J., Douek D. C., Roederer M., Farber J. M. (2005) Proc. Natl. Acad. Sci. U.S.A. 102, 7916–7921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hafezi-Moghadam A., Ley K. (1999) J. Exp. Med. 189, 939–948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Preece G., Murphy G., Ager A. (1996) J. Biol. Chem. 271, 11634–11640 [DOI] [PubMed] [Google Scholar]
- 21.Feehan C., Darlak K., Kahn J., Walcheck B., Spatola A. F., Kishimoto T. K. (1996) J. Biol. Chem. 271, 7019–7024 [DOI] [PubMed] [Google Scholar]
- 22.Livak K. J., Schmittgen T. D. (2001) Methods 25, 402–408 [DOI] [PubMed] [Google Scholar]
- 23.Krumins A. M., Gilman A. G. (2006) J. Biol. Chem. 281, 10250–10262 [DOI] [PubMed] [Google Scholar]
- 24.Yu C. R., Peden K. W., Zaitseva M. B., Golding H., Farber J. M. (2000) J. Immunol. 164, 1293–1305 [DOI] [PubMed] [Google Scholar]
- 25.Miller R. K., Qadota H., Stark T. J., Mercer K. B., Wortham T. S., Anyanful A., Benian G. M. (2009) Mol. Biol. Cell 20, 3608–3616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kehrl J. H. (1998) Immunity 8, 1–10 [DOI] [PubMed] [Google Scholar]
- 27.Huang T. T., Zong Y., Dalwadi H., Chung C., Miceli M. C., Spicher K., Birnbaumer L., Braun J., Aranda R. (2003) Int. Immunol. 15, 1359–1367 [DOI] [PubMed] [Google Scholar]
- 28.Murphy P. M., Baggiolini M., Charo I. F., Hébert C. A., Horuk R., Matsushima K., Miller L. H., Oppenheim J. J., Power C. A. (2000) Pharmacol. Rev. 52, 145–176 [PubMed] [Google Scholar]
- 29.Strathmann M., Wilkie T. M., Simon M. I. (1990) Proc. Natl. Acad. Sci. U.S.A. 87, 6477–6481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hermiston M. L., Xu Z., Weiss A. (2003) Annu. Rev. Immunol. 21, 107–137 [DOI] [PubMed] [Google Scholar]
- 31.Hsu W. H., Rudolph U., Sanford J., Bertrand P., Olate J., Nelson C., Moss L. G., Boyd A. E., Codina J., Birnbaumer L. (1990) J. Biol. Chem. 265, 11220–11226 [PubMed] [Google Scholar]
- 32.Murtagh J. J., Jr., Moss J., Vaughan M. (1994) Nucleic Acids Res. 22, 842–849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liang S. C., Tan X. Y., Luxenberg D. P., Karim R., Dunussi-Joannopoulos K., Collins M., Fouser L. A. (2006) J. Exp. Med. 203, 2271–2279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wynn T. A. (2005) Nat. Immunol. 6, 1069–1070 [DOI] [PubMed] [Google Scholar]
- 35.Voyno-Yasenetskaya T., Conklin B. R., Gilbert R. L., Hooley R., Bourne H. R., Barber D. L. (1994) J. Biol. Chem. 269, 4721–4724 [PubMed] [Google Scholar]
- 36.Liao F., Rabin R. L., Smith C. S., Sharma G., Nutman T. B., Farber J. M. (1999) J. Immunol. 162, 186–194 [PubMed] [Google Scholar]
- 37.Acosta-Rodriguez E. V., Rivino L., Geginat J., Jarrossay D., Gattorno M., Lanzavecchia A., Sallusto F., Napolitani G. (2007) Nat. Immunol. 8, 639–646 [DOI] [PubMed] [Google Scholar]
- 38.Annunziato F., Cosmi L., Santarlasci V., Maggi L., Liotta F., Mazzinghi B., Parente E., Filì L., Ferri S., Frosali F., Giudici F., Romagnani P., Parronchi P., Tonelli F., Maggi E., Romagnani S. (2007) J. Exp. Med. 204, 1849–1861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singh S. P., Zhang H. H., Foley J. F., Hedrick M. N., Farber J. M. (2008) J. Immunol. 180, 214–221 [DOI] [PubMed] [Google Scholar]
- 40.Kim C. H., Rott L., Kunkel E. J., Genovese M. C., Andrew D. P., Wu L., Butcher E. C. (2001) J. Clin. Invest. 108, 1331–1339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neer E. J., Lok J. M., Wolf L. G. (1984) J. Biol. Chem. 259, 14222–14229 [PubMed] [Google Scholar]
- 42.Sternweis P. C., Robishaw J. D. (1984) J. Biol. Chem. 259, 13806–13813 [PubMed] [Google Scholar]
- 43.Valenzuela D., Han X., Mende U., Fankhauser C., Mashimo H., Huang P., Pfeffer J., Neer E. J., Fishman M. C. (1997) Proc. Natl. Acad. Sci. U.S.A. 94, 1727–1732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goldsmith P., Backlund P. S., Jr., Rossiter K., Carter A., Milligan G., Unson C. G., Spiegel A. (1988) Biochemistry 27, 7085–7090 [DOI] [PubMed] [Google Scholar]
- 45.McIntire W. E., Dingus J., Schey K. L., Hildebrandt J. D. (1998) J. Biol. Chem. 273, 33135–33141 [DOI] [PubMed] [Google Scholar]
- 46.Hescheler J., Rosenthal W., Trautwein W., Schultz G. (1987) Nature 325, 445–447 [DOI] [PubMed] [Google Scholar]
- 47.Ewald D. A., Sternweis P. C., Miller R. J. (1988) Proc. Natl. Acad. Sci. U.S.A. 85, 3633–3637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harris-Warrick R. M., Hammond C., Paupardin-Tritsch D., Homburger V., Rouot B., Bockaert J., Gerschenfeld H. M. (1988) Neuron 1, 27–32 [DOI] [PubMed] [Google Scholar]
- 49.VanDongen A. M., Codina J., Olate J., Mattera R., Joho R., Birnbaumer L., Brown A. M. (1988) Science 242, 1433–1437 [DOI] [PubMed] [Google Scholar]
- 50.McFadzean I., Mullaney I., Brown D. A., Milligan G. (1989) Neuron 3, 177–182 [DOI] [PubMed] [Google Scholar]
- 51.Jiang M., Gold M. S., Boulay G., Spicher K., Peyton M., Brabet P., Srinivasan Y., Rudolph U., Ellison G., Birnbaumer L. (1998) Proc. Natl. Acad. Sci. U.S.A. 95, 3269–3274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tanaka M., Treloar H., Kalb R. G., Greer C. A., Strittmatter S. M. (1999) Proc. Natl. Acad. Sci. U.S.A. 96, 14106–14111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Luo A. H., Cannon E. H., Wekesa K. S., Lyman R. F., Vandenbergh J. G., Anholt R. R. (2002) Brain Res. 941, 62–71 [DOI] [PubMed] [Google Scholar]
- 54.Wettschureck N., Offermanns S. (2005) Physiol. Rev. 85, 1159–1204 [DOI] [PubMed] [Google Scholar]
- 55.Wettschureck N., Moers A., Offermanns S. (2004) Pharmacol. Ther. 101, 75–89 [DOI] [PubMed] [Google Scholar]
- 56.Chaffin K. E., Beals C. R., Wilkie T. M., Forbush K. A., Simon M. I., Perlmutter R. M. (1990) EMBO J. 9, 3821–3829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rudolph U., Finegold M. J., Rich S. S., Harriman G. R., Srinivasan Y., Brabet P., Boulay G., Bradley A., Birnbaumer L. (1995) Nat. Genet. 10, 143–150 [DOI] [PubMed] [Google Scholar]
- 58.He J., Gurunathan S., Iwasaki A., Ash-Shaheed B., Kelsall B. L. (2000) J. Exp. Med. 191, 1605–1610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kurose H., Katada T., Haga T., Haga K., Ichiyama A., Ui M. (1986) J. Biol. Chem. 261, 6423–6428 [PubMed] [Google Scholar]
- 60.Carter B. D., Medzihradsky F. (1993) Proc. Natl. Acad. Sci. U.S.A. 90, 4062–4066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kleuss C., Scherübl H., Hescheler J., Schultz G., Wittig B. (1993) Science 259, 832–834 [DOI] [PubMed] [Google Scholar]
- 62.Ricci A., Amenta F., Bronzetti E., Mannino F., Mariotta S., Tayebati S. K. (2002) J. Neuroimmunol. 129, 178–185 [DOI] [PubMed] [Google Scholar]
- 63.Fujino H., Kitamura Y., Yada T., Uehara T., Nomura Y. (1997) Mol. Pharmacol. 51, 1007–1014 [DOI] [PubMed] [Google Scholar]
- 64.Fujii T., Watanabe Y., Inoue T., Kawashima K. (2003) Neurochem. Res. 28, 423–429 [DOI] [PubMed] [Google Scholar]
- 65.Gavériaux C., Peluso J., Simonin F., Laforet J., Kieffer B. (1995) FEBS Lett. 369, 272–276 [DOI] [PubMed] [Google Scholar]
- 66.Li M. D., McAllen K., Sharp B. M. (1999) J. Leukoc. Biol. 65, 707–714 [DOI] [PubMed] [Google Scholar]
- 67.Miller B. (1996) J. Immunol. 157, 5324–5328 [PubMed] [Google Scholar]
- 68.Ghamrawy C. E., Rabourdin-Combe C., Krantic S. (1999) Peptides 20, 305–311 [DOI] [PubMed] [Google Scholar]
- 69.Cardoso A., el Ghamrawy C., Gautron J. P., Horvat B., Gautier N., Enjalbert A., Krantic S. (1998) J. Cell. Biochem. 68, 62–73 [DOI] [PubMed] [Google Scholar]
- 70.Gallo E. M., Canté-Barrett K., Crabtree G. R. (2006) Nat. Immunol. 7, 25–32 [DOI] [PubMed] [Google Scholar]
- 71.Kotturi M. F., Carlow D. A., Lee J. C., Ziltener H. J., Jefferies W. A. (2003) J. Biol. Chem. 278, 46949–46960 [DOI] [PubMed] [Google Scholar]
- 72.Farber D. L. (2009) Semin. Immunol. 21, 84–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nanki T., Lipsky P. E. (2000) J. Immunol. 164, 5010–5014 [DOI] [PubMed] [Google Scholar]
- 74.Ottoson N. C., Pribila J. T., Chan A. S., Shimizu Y. (2001) J. Immunol. 167, 1857–1861 [DOI] [PubMed] [Google Scholar]
- 75.Kumar A., Humphreys T. D., Kremer K. N., Bramati P. S., Bradfield L., Edgar C. E., Hedin K. E. (2006) Immunity 25, 213–224 [DOI] [PubMed] [Google Scholar]
- 76.Liu X., Liu T., Slusarski D. C., Yang-Snyder J., Malbon C. C., Moon R. T., Wang H. (1999) Proc. Natl. Acad. Sci. U.S.A. 96, 14383–14388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Katanaev V. L., Ponzielli R., Sémériva M., Tomlinson A. (2005) Cell 120, 111–122 [DOI] [PubMed] [Google Scholar]
- 78.Katanaev V. L., Tomlinson A. (2006) Proc. Natl. Acad. Sci. U.S.A. 103, 6524–6529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Xie H., Huang Z., Sadim M. S., Sun Z. (2005) J. Immunol. 175, 7981–7988 [DOI] [PubMed] [Google Scholar]
- 80.Timm A., Grosschedl R. (2005) Curr. Top. Microbiol. Immunol. 290, 225–252 [DOI] [PubMed] [Google Scholar]
- 81.Sutton A., Friand V., Brulé-Donneger S., Chaigneau T., Ziol M., Sainte-Catherine O., Poiré A., Saffar L., Kraemer M., Vassy J., Nahon P., Salzmann J. L., Gattegno L., Charnaux N. (2007) Mol. Cancer Res. 5, 21–33 [DOI] [PubMed] [Google Scholar]
- 82.Cho H. H., Kyoung K. M., Seo M. J., Kim Y. J., Bae Y. C., Jung J. S. (2006) Stem Cells Dev. 15, 853–864 [DOI] [PubMed] [Google Scholar]
- 83.Yang M., Zhong W. W., Srivastava N., Slavin A., Yang J., Hoey T., An S. (2005) Proc. Natl. Acad. Sci. U.S.A. 102, 6027–6032 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.