Abstract
It has been a decade since scientists realized that microRNAs (miRNAs) are not an oddity invented by worms to regulate gene expression at post-transcriptional levels. Rather, many of these 21–22-nucleotide-short RNAs exist in invertebrates and vertebrates alike and some of them are in fact highly conserved. miRNAs are now recognized as an important class of non-coding small RNAs that inhibit gene expression by targeting mRNA stability and translation. In the last ten years, our knowledge of the miRNAs world was expanding at vertiginous speed, propelled by the development of computational engines for miRNA identification and target prediction, biochemical tools and techniques to modulate miRNA activity, and last but not least, the emergence of miRNA-centric animal models. One important conclusion that has emerged from this effort is that many microRNAs and their cognate targets are strongly implicated in cancer, either as oncogenes or tumor and metastasis suppressors. In this review we will discuss the diverse role that miRNAs play in cancer initiation and progression and also the tools with which miRNA expression could be corrected in vivo. While the idea of targeting microRNAs towards therapeutic ends is getting considerable traction, basic, translational, and clinical research done in the next few years will tell whether this promise is well-founded.
Keywords: miRNA, cancer, therapy, target prediction, chemosensitivity, adjuvant
1. Introduction
microRNAs (miRNAs or miRs) are an integral part of the RNA interference (RNAi) machinery which results in post-transcriptional gene silencing. In general, RNAi is triggered by double-stranded RNAs (dsRNAs) that are processed first into short RNA duplexes, and then into single-stranded small RNAs that will bind target cellular mRNAs or viral genomic RNAs (Fire et al. 1998). Depending on their origin, function and structure, there are three types of short RNAs that follow the RNAi pathway for gene silencing: siRNAs (small interfering RNAs), piRNAs (PiwiRNAs) and miRNAs [reviewed in (Liu & Paroo, 2010; Paroo et al. 2007; Rana, 2007)].
miRNAs were first discovered in C.elegans by the laboratories of Ambros and Ruvkun. Lin-4 was identified in 1993 (Lee et al. 1993; Wightman et al. 1993) and let-7 - in 2000 (Reinhart et al. 2000; Slack et al. 2000). A year later, the Ambros and Bartel labs demonstrated that they represent an extensive class of small RNAs (Lau et al. 2001; Lee & Ambros, 2001). Importantly, in the companion paper from the Tuschl lab the existence of many microRNAs was confirmed in vertebrates, including humans (Lagos-Quintana et al. 2001). In subsequent years, microRNAs have been shown to be involved in many biological processes: signaling, differentiation, and possibly cell fate determination, as hinted at by the existence of tissue-specific microRNAs (e.g., miR-1b-2 and miR-99b in the brain, miR-1 in the muscle, and miR-122 in the liver).
Germanely to this review, miRNAs play a role in tumor pathogenesis and progression. This is because miRNAs can regulate the expression and activity of canonical, protein-coding tumor suppressor genes and oncogenes. Furthermore, several miRNAs themselves have been reported to function as tumor suppressor (TSmiRs) or oncogenes (oncomiRs) (see section 4). In addition, miRNA expression profiling and generation of transgenic mice have been of great utility in identifying miRNAs which attenuate or enhance the development of specific types of tumors or are involved in the acquisition of invasive capabilities.
2. miRNA Biogenesis
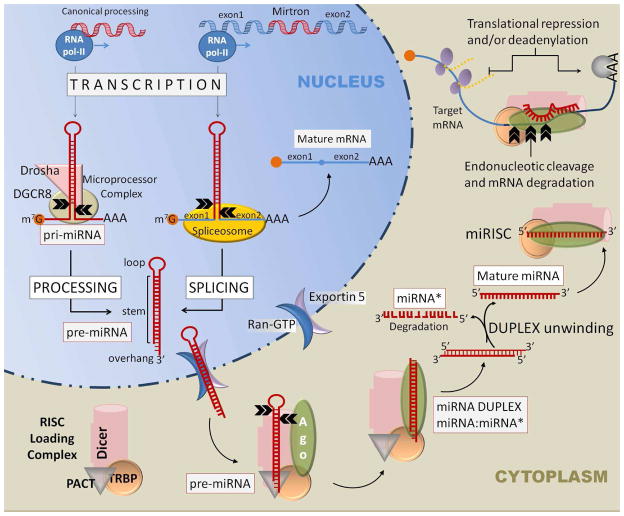
miRNA-encoding genes are localized in either intronic or exonic regions of protein-coding genes, or alternatively in intergenic regions of non-coding DNA. They are transcribed mainly by the RNA-polymerase II into primary miRNA transcripts (primiRNA). Consequently, pri-miRNAs contain cap structures as well as poly(A) tails and their synthesis is inhibited by α-amanitin (Lee et al. 2004). The initial steps of pri-miRNA processing depend on whether the miRNA gene is located within a intragenic (protein-coding) or an intergenic region (Fig. 1). miRNA encoded by intronic regions of protein-coding DNA (“mirtrons”) in flies and worms (Okamura et al. 2007; Ruby et al. 2007) as well as in mammals (Berezikov et al. 2007) skip the initial processing by Drosha (see below), but the biogenesis pathway in the cytoplasm is identical to other miRNAs processed from pri-miRNAs.
Figure 1. miRNA Biogenesis.
Canonical miRNA and mirtron processing pathways are depicted. See text for more explanations. Double black arrows indicate cleavage sites.
Approximately half of all human miRNAs are encoded by genomic clusters that are transcribed as single polycistronic units (Lee et al. 2002; Lau et al. 2001; Lagos-Quintana et al. 2001; Mourelatos et al. 2002). An extreme example of this grouping is the C19MC locus, which encodes the largest human microRNA gene cluster consisting of 40+ tandemly repeated, primate-specific pre-miRNAs (Bentwich et al. 2005). Each specific miRNA from this and other clusters will be processed individually, and mature miRNAs from the same cluster can exhibit different patterns of expression.
Pri-miRNAs then fold into imperfect hairpins, which serve as substrates for Drosha (Lee et al. 2003). A member of the RNase III family of enzymes, Drosha functions as part of a protein assembly called the microprocessor complex, which also includes the dsRNA binding protein DGCR8 (called Pasha in flies) (Denli et al. 2004; Gregory et al. 2004). Drosha and DGCR8 will cleave and transform a pri-miRNA into a pre-miRNA, a stem-loop structure of ~70 nucleotides and a two-nucleotide 3′-overhang. Generally, pre-miRNAs will be exported to the cytoplasm by Exportin-5 and Ran-GTP (Lund et al. 2004; Yi et al. 2003; Bohnsack et al. 2004). However, it is important to highlight that there are some variations in the cellular distribution of mature miRNAs and, for instance, miR-29b, miR-320 and miR-373 have been shown to function and accumulate primarily in the nuclear compartment (Liao et al. 2010; Hwang et al. 2007; Kim et al. 2008; Place et al. 2008).
Once in the cytoplasm, pre-miRNA will be cleaved for the second time, this time by Dicer, another endoribonuclease from the RNAse III family (Hutvagner et al. 2001; Grishok et al. 2001). Because Dicer is also involved in processing siRNA, it represents a common node in RNAi pathways - as discovered by the Hannon and Plasterck labs (Bernstein et al. 2001; Ketting et al. 2001)
Before Dicer can cleave pre-miRNA, it has to form a complex with TRBP (a dsRNA binding protein) (Chendrimada et al. 2005), and perhaps auxiliary, non-essential proteins such as PACT (protein activator of PKR) (Lee et al. 2006). Dicer cleaves the loop off the pre-miRNA stem-loop structure generating a 22–25 nucleotides long dsRNA also known as miRNA duplex. This duplex consists of the functional, or guide, miRNA strand and its complementary non-functional, or passenger, strand (miRNA*). In principle, both strands (miRNA and miRNA*) have the ability to be incorporated into the miRISC (miRNA-Induced Silencing Complex) and become mature miRNA - or get degraded. Thermodynamics usually is the deciding factor, and the strand with the less stable 5′ end is loaded into the RISC while the strand with more stable terminal base pairing is degraded (Schwarz et al. 2003; Khvorova et al. 2003).
In order to function, miRNA-loaded RISC complexes recruit one of the 4 Argonaute proteins (Ago1-4), with no apparent preference; however only Ago2 has endonuclease activity and can cleave target mRNA (Meister et al. 2004; Liu et al. 2004). Neither TRBP nor PACT are necessary for processing activity itself, but to the extent that they participate in the recruitment of Argonaute-2 (Ago-2) their depletion reduces the efficiency of posttranscriptional gene silencing (Lee et al. 2006; Chendrimada et al. 2005; Macrae et al. 2008).
Once the miRISC is formed, it will bind to the 3′-UTR (untranslated region) of its mRNA target. This binding occurs, most frequently (but not always) through the miRNA seed sequence, a region of 7–8 nucleotides located at the miRNA 5′-terminus (Lewis et al. 2005; Lewis et al. 2003). Generally speaking, a perfect mRNA/miRNA complementarity has destabilizing effects (Davis et al. 2005; Davis et al. 2005; Yekta et al. 2004; Shin et al. 2010). At least three independent mechanism of miRNA-mediated mRNA silencing have been described: target cleavage, translational inhibition and mRNA decay. Typically, the seed sequence extends from nucleotides 2 to 7, and when the miRNA/mRNA pairing extends to positions 10 and 11, Ago2 catalyzes the cleavage of the mRNA target (Yekta et al. 2004; Elbashir et al. 2001; Hutvagner & Zamore, 2002). Very recently, it has been shown that higher concentrations of magnesium allow for a more permissive cleavage of mRNA/miRNA duplexes, requiring less complementarity between the two molecules (Shin et al. 2010).
Once the miRISC binds the target mRNA it inhibits its translation either by a cap-dependent mechanism (Humphreys et al. 2005; Pillai et al. 2005) whereby Ago proteins prevent cap recognition by the initiation factor eIF4E (Kiriakidou et al. 2007) or by directly recruiting ribosome inhibitory proteins, like eIF6 (Chendrimada et al. 2007). This, however, is usually accompanied by mRNA deadenylation (Wu & Belasco, 2005; Giraldez et al. 2006), and consequently both protein and mRNA levels are usually affected (Baek et al. 2008; Selbach et al. 2008). Additionally, microRNAs have been reported to promote relocation of mRNAs to sites of RNA storage named P-bodies, which are devoid of ribosomes (Liu et al. 2005; Liu et al. 2005). Overall, there is no doubt that microRNAs exert profound effects on gene expression. However, identification of key target genes proved difficult and wrought with uncertainties.
3. Target Prediction and Validation
It wasn’t until 2004 that the basis of miRNA target prediction was established by Doench and Sharp, who found that the efficiency and specificity with which miRNAs repress target mRNAs are mostly determined by the free energy of binding of the first eight nucleotides in the 5′ region of a miRNA (the “seed” sequence) (Doench & Sharp, 2004). They also uncovered that one mRNA can be simultaneously inhibited by more than one miRNA species. To complicate the matters, over-expression of a certain miRNA can result in “forced” non-physiological inhibition of mRNA targets through competition with other mRNAs or miRNAs (Doench & Sharp, 2004). Subsequent work confirmed the bias towards 5′-end-driven recognition (although not necessarily nucleotides 2–8) (Miranda et al. 2006) but also the existence of non-seed-based recognition mechanisms (Tay et al. 2008; Lal et al. 2009).
There are currently several computational algorithms to predict putative targets of given miRNAs, as well as complete databases where newly discovered or putative miRNA sequences are annotated (Table 1). Prediction tools must be used cautiously and taken for what they are: predictors necessitating the use of experimental validation techniques, which can be laborious and challenging.
Table 1.
Computational tools for miRNA target prediction and miRNA databases.
Confirmation of predicted targets is generally achieved using luciferase sensor assays where the tested 3′UTR is attached to the luciferase reporter gene and then introduced into cells expressing the miRNA of interest (Doench et al. 2003; Stark et al. 2003). Simultaneously, mutated versions of the targeted 3′UTR must be included as controls to ensure that downregulation of the luciferase activity upon exposure to a certain miRNA is mediated by base-pairing between the miRNA’s seed sequence and the predicted site, and is not due to secondary indirect effects.
While luciferase sensor assays can suggest physical interaction between miRNA and mRNA, they don’t prove it directly. For this purpose, more rigorous pull-down assays can be used. In this case, a labeled miRNA is mixed with cellular extracts and immunoprecipitated with an antiserum against the labeling moiety or passed through affinity columns. Once labeled-miRNA/mRNA complexes have been isolated, cDNA is obtained using reverse transcriptase-PCR (RT-PCR) and sequenced (Hsu et al. 2009). Additionally, to assert that the mRNA/miRNA interaction results in effective gene silencing, Darnell’s lab has very recently developed a method of high-throughput sequencing (HITS) of RNAs isolated by crosslinking and immunoprecipitation (CLIP) with Ago2 antibodies. Using this Ago-HITS-CLIP assay, it is possible to detect not just the binary mRNA/miRNA complex, but the ternary (and presumably functional) miRNA/mRNA/Ago2 complex (Chi et al. 2009). This technique provides a precise map of miRNA/mRNA interactions and suggests specific sequences for targeting clinically relevant miRNA/mRNA interactions. What exactly these interactions are is still being aggressively researched, but there is a preponderance of newly emerging evidence that some microRNAs and their cognate targets are implicated in cancer.
4. miRNA and Cancer
Some initial evidence that miRNAs are linked to cancer was the transcriptional regulation of miRNAs by oncogenes and tumor suppressor genes. In parallel, more hard genetic evidence has emerged showing that miRNA genes could be amplified, deleted, or epigenetically regulated in cancer in the same way that canonical cancer genes are affected by somatic or germline mutations. Many of these putative cancer miRNAs have also been validated in mouse models. Finally, consistent overexpression/ downregulation of certain miRNAs in advanced versus early-stage cancers lead to the idea that some microRNA might confer metastatic properties and function as metastamiRs (Hurst et al. 2009)
4.a) Transcriptional deregulation of miRNAs in cancer cells
Depending on the genomic localization of the miRNA gene, it will be under the control of the host gene within which it is transcribed, or its own dedicated promoter. In the first case, the microRNA pattern of expression will parallel that of the host gene, leading to some confusion as to which of the two plays a role in cancer. This was recently highlighted in a study where intronic miR-211- and not its host gene melastatin - was found to function as a tumor suppressor in malignant melanoma (Levy et al. 2010). The analysis is somewhat simpler when a miRNA gene has its own promoter. These dedicated miRNA transcripts were shown in the last 5 years to be affected by such well-known oncogenic and tumor suppressive transcription factors such as Myc and p53.
The first evidence emerged in 2005 from the Mendell and Dang laboratories and demonstrated that Myc, via direct DNA binding, activates transcription of the miR-17~92 cluster composed of seven mature miRNAs: miR-17-5p, miR-18a, miR-19a, miR-19b-1, miR-20a and miR-92a-1 (O’Donnell et al. 2005). Subsequently, through work from Mendell’s and our own laboratories, it became apparent that Myc also down-regulates many microRNAs, by mechanisms that range from direct DNA binding/transcriptional repression (Chang et al. 2008) to the deregulation of the RNA-binding protein Lin28b (Chang et al. 2009). Importantly, down-regulation of miRNA expression by Myc not merely accompanies Myc-induced B-lymphomagenesis, but in many cases (e.g., miR- 15a/16) is required for efficient expansion of neoplastic B-cells in vivo (Chang et al. 2008; Chung et al. 2008)
On the opposite side of the cancer gene spectrum, the tumor suppressor par excellence p53 also counts miRNAs among its transcriptional targets. A very complex network of cross-regulation between p53 and miRNAs is being untangled (Fabbri et al. 2011; Neveu et al. 2010; Welch et al. 2007). Its centerpiece is miR-34a, a TSmiR (see section 4.b) which has been identified as one of the main effectors of p53-induced apoptosis and cell cycle arrest (Tarasov et al. 2007; Chang et al. 2007; Raver-Shapira et al. 2007; Bommer et al. 2007; He et al. 2007; Corney et al. 2007). This occurs via targeting of key proteins like BCL-2, CDK4, CDK6, or G1-Cyclins (Sun et al. 2008; Ji et al. 2008) and, simultaneously, via enhancing p53 activity through inhibition of the SIRT-1 deacetylase (Yamakuchi et al. 2008; Fujita et al. 2008). To make the p53/miRNA network even more intricate, miR-125b, miR-504, miR-30d and miR-25 all have been shown to directly target p53 (Le et al. 2009; Hu et al. 2010; Kumar et al. 2010).
In addition to regulation by transcription factors, epigenetic regulation by methylation of CpG island and histone modifications at miRNA regulatory regions have also been described for ~5% of all human miRNAs (Lujambio et al. 2007; Saito et al. 2006; Scott et al. 2006). Conversely, some miRNAs are known to regulate key components of the epigenetic machinery, including histone deacetylases and DNA methyltransferases (Fabbri et al. 2007; Noonan et al. 2009; Tuddenham et al. 2006; Sinkkonen et al. 2008; Benetti et al. 2008).
A good example of this complexity is the epigenetic regulation of miR-127 in bladder cancer (Saito et al. 2006). In normal cells, miR-127 is expressed as part of the miRNA cluster, but its expression is shut down in cancer cells. When bladder cancer cells are treated with a DNA demethylating agent (5-aza) and an inhibitor of histone deacetylation, 17 out of 313 human miRNAs increase their expression levels more than 3-fold. Of note, miR-127 is upregulated ~50 fold, resulting in the inhibition of the transcription factor and proto-oncogene BCL6, one of its direct targets. Interestingly, the polycistronic region encoding miR-127 also includes miR-136, miR-432 and miR-433, but miR-127 is the only member of the cluster upregulated upon inhibition of methylation and deacetylation.
4.b) Tumor Suppressor miRNAs
This category includes miRNAs whose loss promotes tumor formation. The genetic mechanisms involved in down-regulation of a TSmiR gene in cancer are the same as those described for protein-coding genes: biallelic deletion, loss of heterozygosity, somatic mutations, altered processing, or epigenetic modification. The parallelism between miR-15a/16 and Rb is the case in point.
Deletions of the chromosomal region 13q were initially described in retinoblastoma (Vogel, 1979) and later in hematological malignances (Cheng et al. 1990). Once the retinoblastoma gene was mapped to the 13q14.14 region, it was assumed that RB1 deletion is the sole cause of leukemias. However, as techniques for gene mapping were developed and refined, it became apparent that the 13q locus deleted in B-cell chronic lymphocytic leukemia (CLL) and multiple myeloma (MM) did not involve the RB1 gene (Brown et al. 1993; Migliazza et al. 2001), but instead overlapped a minimal deletion region called MDR. However, it wasn’t until 2001 that DLEU2 was identified as the putative key transcript of the MDR (Migliazza et al. 2001). One year later, DLEU2 was found to host miR-15a/16-1, whose allelic loss is responsible for CLL pathogenesis (Calin et al. 2002). Soon thereafter, the miR-15a/16-1 role as a tumor suppressor was confirmed using a megakaryocytic leukemia cell line, where its expression caused apoptosis and downregulation of BCL-2 (Cimmino et al. 2005). Furthermore, miR-15a/16 induces growth arrest in multiple myeloma cells (Roccaro et al. 2009).
Even more definitive genetic evidence of the tumor suppressive effects of miR-15a/16-1 came recently from the Dalla-Favera lab, where MDR and miR-15a/16-1 knockout mice were generated. Mice of both genotypes initially developed peripheral blood clonal lymphoproliferative disease similar to human monoclonal B cell lymphocytosis (MBL). By 18 months of age, 42% of MDR−/− and 26% or miR15a/16-1−/− mice developed MBL, CLL and non-Hodgkin lymphoma (Klein et al. 2010). The increase in B cells proliferation detected in both mouse models was due to elevated levels of cell cycle-related proteins that drive exit from quiescence. The authors demonstrated that miR-15a/16-1 target several proteins involved in the G0/G1 to S phase transition: Cyclin D3, Cyclin E, CDK6, CHK1 and MCM5. Interestingly, MDR−/− mice displayed a more aggressive phenotype, suggesting that DLEU2 itself may have important regulatory functions, besides serving as the primary transcript for miR15a/16-1. Alternatively, additional genetic elements within the MDR locus could contribute to its tumor suppressive functions.
Another TSmiR frequently lost in cancer is miR-34a located in the chromosomal region 1p36. This region is recurrently deleted in neuroblastoma, breast, hepatic, pancreatic and colon carcinomas [reviewed in (Bagchi & Mills, 2008)]. Initial evidence suggested that tumor suppressive effects of miR-34a stem from its essential role in the p53 network. As discussed above, miR-34a is transcriptionaly activated by p53 and also enhances its function by targeting the p53 deacetylase SIRT-1, thus creating a positive feed-back-loop [reviewed in (Hermeking, 2010)]. More recently, it has been shown that over-expression of miR-34a induces cell cycle arrest in glioblastoma cell lines by targeting, besides SIRT-1, multiple oncogenes such as Notch-1, Notch-2 and CDK6 (Li et al. 2009). Also, we and others have shown that miR-34a, together with miR-34b and miR34c, target Myc by recognizing one, and potentially more, non-canonical seed sequences in its 3′UTR (Christoffersen et al. 2010; Kong et al. 2008; Sotillo et al, 2011).
As mentioned above, loss of expression of a TSmiR also can be due to epigenetic modifications, such as methylation. miR-34b and miR-34c have been shown to be under epigenetic regulation in gastric carcinoma. In one study, 13 out of 13 gastric carcinoma cell lines tested showed miR-34b and miR-34c epigenetically silenced by hypermethylation of the neighboring CpG island. The same chromosomal region was not methylated in normal gastric mucosa from Helicobacter pylori-negative healthy individuals (Suzuki et al. 2010).
Methylation of miRNA-associated CpG islands is not limited to the miR-34 loci. It frequently occurs, for example, at the miR-137 promoter in colorectal carcinoma where it inversely correlates with miR-137 expression. In a set of 409 tissue samples obtained from cancer patients, 82.3% adenomas and 81.4% colorectal carcinomas showed silencing of miR-137 by methylation, versus only 14.4% of non-cancerous samples from the same patients or 4.7% of samples from healthy individuals (Balaguer et al. 2010). Other miRNAs shown to be silenced by hypermethylation in tumor samples or tumor cell lines are: miR-193-b in prostate cancer (Rauhala et al. 2010), miR-124 in cervical cancer (Wilting et al. 2010), miR-107 in pancreatic cancer (Lee et al. 2009), miR-199b-5 in medulloblastoma (Garzia et al. 2009), miR-1-1 in hepatocellular carcinoma (Datta et al. 2008) or miR-203 in Philadelphia chromosome-positive human leukemias (Bueno et al. 2008). Finally, epigenetic modifications are largely responsible for the silencing of miR-200 family members [reviewed in (Mongroo & Rustgi, 2010)], whose importance in cancer will be described below.
Many other miRNAs have been shown to inhibit tumor growth when expressed ectopically. Examples include miR-26, miR-29, miR-30, miR-145, miR-146a, miR-150, miR-181, miR-192, miR-194, miR-215 and the let-7 family of miRNAs (Chang et al. 2008; Shin et al, 2010; Chen et al. 2010; Fu et al. 2010; Pichiorri et al. 2010; Ma et al, 2010; Mott et al. 2007; Pekarsky et al. 2006; Xiong et al. 2010; Gebeshuber et al. 2009; Xu et al. 2009; Lan et al. 2011; Trang et al. 2010; Mayr et al. 2007; Lee & Dutta, 2007; Johnson et al. 2007; Chang et al. 2009; Esquela-Kerscher et al. 2008; Sachdeva et al. 2009). However, the genetic evidence for their bona fide tumor suppressor roles is still lacking. One possible exception is the let-7 family. While its members are too numerous to be eliminated by somatic or germ-line mutations, there exists indirect but intriguing evidence for tumor suppressive effects of let-7. It turns out that a single nucleotide polymorphism at the let-7-complementary site in the KRAS 3′ UTR increases the risk of developing non-small cell lung and ovarian cancers (Chin et al. 2008; Ratner et al. 2010).
4.c) Oncomirs
The term “oncomiRs” is reserved for miRNAs whose constitutive over-expression by genetic means initiates or accelerates cancer formation or progression. Although there seems to be a general trend towards down-regulation of cellular miRNAs expression throughout tumor formation (Lu et al. 2005; Kumar et al. 2007), some miRNAs follow the opposite pattern. The first identified oncomiR (oncomir-1) was the miR17~92 cluster discussed in section 4a. In addition to being a direct Myc target (O’Donnell et al. 2005), miR-17~92 acts as an oncogene in its own right, as evidenced by two key pieces of data. One is that this polycistronic gene (previously known as c13orf25) is located in the chromosomal locus 13q31-q32, which is frequently amplified in solid and hematopoietic tumors (Ota et al. 2004). Not surprisingly, Lowe’s, Hannon’s and Hammond’s labs have found that oncomir-1 accelerates Myc–induced B-cell lymphoma in the Eμ-myc mouse model (He et al. 2005). Interestingly, E2F1, an oncogenic and pro-apoptotic transcriptional target of c-Myc, was found to be repressed by miR-17-5p and miR-20a, two members of the oncomir-1 cluster (O’Donnell et al. 2005). Since then, the list of targets inhibited by oncomir-1 has grown and it now includes, among others, inhibitors of proliferation (CDKN1A) (Inomata et al. 2009; Ivanovska et al. 2008), transcription factors of the E2F family (O’Donnell et al. 2005; Sylvestre et al. 2007), regulators of angiogenesis (CTGF, Tsp1) (Dews et al. 2006; Ernst et al. 2010), various members of the TGF-β pathway such as type II TGF-β receptor and SMADs (Volinia et al. 2006; Dews et al. 2010; Mestdagh et al. 2010), and direct regulators of apoptosis (Bim, PTEN) (Olive et al. 2009; Xiao et al. 2008; Koralov et al. 2008; Mu et al. 2009). Over-expression of miR-17~92 gene has also been documented in several solid tumors of breast, lung, colon, stomach, pancreas, and prostate (Volinia et al. 2006; Petrocca et al. 2008).
Another miRNA with oncomiR aspirations is miR-21. Although there is no genetic evidence for its involvement in tumorigenesis, miR-21 over-expression is common in most cancers, its expression is linked to increased cell growth in cancer cells, and data obtained from knock-down of miR-21 in cell lines supports its role as an oncomiR [reviewed in (Selcuklu et al. 2009; O’Day & Lal, 2010; Gabriely et al. 2008)]. Consistent with this idea, among miR-21- targeted genes are several well-recognized tumor suppressors, such as PTEN, PDCD4, TPM-1, Tap63, SPRY2, and hMSH2 depending on the cell type (Meng et al. 2006; Zhu et al. 2008; Papagiannakopoulos et al. 2008; Sayed et al. 2008; Valeri et al. 2010). For example, microarray profiling performed on MCF7 cells showed that knock-down of miR-21 alters expression of 737 genes: 45% of genes were down-regulated and 55% up-regulated. As expected, the set of up-regulated genes was enriched with those with putative target sequences for miR-21 in their 3′UTRs. Of all those putative targets, the authors pinpoint the tumor suppressor Programmed Cell Death 4 (PDCD4) gene as a miR-21 target central to its oncogenic functions (Frankel et al. 2008). Not surprisingly, over-expression of miR-21 in primary breast cancer samples is associated with advance clinical stage, lymph node metastasis and poor prognosis (Yan et al. 2008),
It is important to stress that the oncogenic or tumor suppressor effects of a certain miRNA occur in the context of a given disease. For instance, in prostate cancer, knockdown of miR-21 does not affect cell proliferation or invasiveness. Nor does it modulate PTEN or Pdcd4 (Folini et al. 2010), indicating that in prostate cancer a miR-21 inhibitor has no therapeutic potential by itself. One obvious way the changing cellular context can render miRNA ineffective is by altering the repertoire of its target mRNAs. For example, we have shown that ectopic expression of miR-34a in the context of overexpressed Myc [i.e., in Burkitt’s lymphoma cells] does not enhance p53 function via down-regulation of SIRT-1. Instead, it efficiently targets Myc which sustains p53 levels via the Arf-Mdm-2 pathway. As a net result, levels of p53 in miR-34-overexpressing lymphoblasts decrease, as do p53-dependend responses (Sotillo et al, 2011).
4.d) MetastamiRs
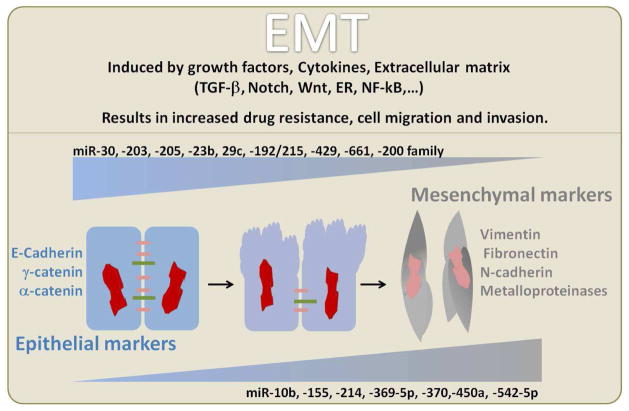
From the therapeutic point of view, the ability to prevent tumor cells dissemination outside their primary sites determines how favorable the prognosis will be. As mentioned above, miRNAs involved in the acquisition of invasive abilities are called metastamiRs. These miRNAs have been implicated in the maintenance of different components of the metastatic cascade: loss of cellular adhesion, entry into and exit from the vascular system and survival in the vascular system and at distant sites [reviewed in (Yilmaz & Christofori, 2010)]. How does this occur? At the cellular level, there is solid evidence that the epithelial-to-mesenchymal transition (EMT) tightly correlates with the invasive and metastatic phenotype (Yang et al. 2004; Thiery, 2003). During EMT, neoplastic epithelial cells lose their cell-cell adhesion and assume a mesenchymal phenotype by becoming more motile and invasive (Figure 2). EMT is a reversible process (counterbalanced by mesenchymal-to-epithelial transition) and as such, it is regulated by numerous signaling pathways, including Wnt, Notch, TGF-β and Hedgehog. These pathways in turn regulate several transcriptions factors, such as Twist, Snail and ZEB (Comijn et al. 2001; Cano et al. 2000; Thiery, 2003; Yang et al. 2004; Zhou et al. 2004; Batlle et al. 2000), which directly control cell adhesion and motility genes.
Figure 2. EMT and miRNAs.
Some of the miRNAs regulated during and implicated in EMT.
Numerous miRNAs have been shown to be positively or negatively regulated during EMT. Moreover, some of them are known to target many genes that are critical for the regulation of EMT, thus becoming desirable therapeutic targets in metastatic cancers (Zavadil et al. 2007; Wang et al. 2010). Some of these miRNAs are miR-192/215 which target E-cadherin repressors ZEB-1 and ZEB-2 (Wang et al. 2010), miR-10b which is induced by the transcription factor Twist (Ma et al. 2007), miR-9 which directly inhibits E-cadherin (Ma et al. 2010), miR-30, miR-200, and miR-382 which are regulated by the TGFβ pathway (Kriegel et al. 2010; Braun et al. 2010), miR-155 and miR-31 which regulate RhoA (O’Day & Lal, 2010; Kong et al. 2008; Valastyan et al. 2009), miR-181 which inhibits the tumor suppressor metalloprotease inhibitor 3 (TIMP3) (Wang et al. 2009), and miR-205 which targets Erb3 and VEGF-A (Wu et al. 2009). Many other examples were revealed in the recent study by (Castilla et al. 2011).
One of the better studied examples of miRNA involvement in EMT is the miR-200 family, which directly targets ZEB-1 and ZEB-2, potent repressors of E-cadherin (Park et al. 2008; Korpal et al. 2008; Bracken et al. 2008; Gregory et al. 2008). It has been shown that during EMT miR-200 is silenced by methylation of its promoter, leading to upregulation of ZEB-1 and-2, which in turn repress E-cadherin (Vrba et al. 2010; Wiklund et al. 2010). Interestingly, Zeb-1 has been shown to repress transcription of two miR-200 family members, miR-200c and miR-141, resulting in a negative feed-back loop (Burk et al. 2008).
After undergoing EMT, tumor cells still must be able to spread to distant sites, and miRNAs have been strongly implicated in the acquisition of the metastatic behavior. Valuable data explaining how this might occur were recently obtained in Massagué’s lab. This group analyzed human lung (CN34-LM1) and bone (CN34-BoM1) metastatic lesions obtained after injection of malignant cells from a metastatic breast cancer patient (CN34) into mice (Tavazoie et al. 2008). They discovered that both CN34-LM1 and CN34-BoN1 cells had lost expression of miR-355, miR-126 and miR-206, relative to parental CN34 cells. Furthermore, exogenous expression of any of the three miRNAs significantly reduced the ability of CN34-LM1 and CN34-BoM1 to metastasize to lung and bone, respectively. Interestingly, these miRNAs were suppressing metastasis by different mechanisms. While miR-126 was inhibiting cell proliferation, miR-355 and miR-206 were targeting cell migration, without affecting the overall mesenchymal phenotype as defined by vimentin expression. Inhibition of migration was due in part to the targeting by miR-355 of the transcription factor SOX4 and the extracellular matrix component tenascin C, both important mediators of metastasis in vivo.
Based on these and similar data, a concept has emerged that inhibition of oncomiRs and metastamiRs as well as restoration of TSmiRs hold considerable promise for the treatment of cancer.
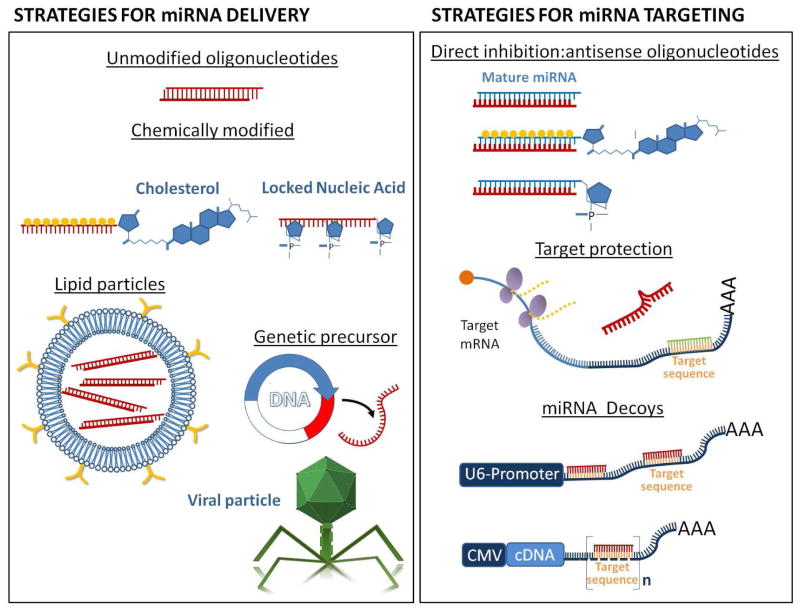
5 miRNA-Based Therapies
Given the importance of miRNAs in cancer, several strategies to manipulate miRNA activity and expression are being pursued. Due to the way miRNAs function, they can be targeted at two different levels: reducing/increasing their levels and/or interfering with the miRNA/mRNA interaction. When the levels of an active miRNA are altered, it affects all of its downstream targets, while by modulating mRNA/miRNA interaction higher degrees of specificity could be obtained. Still, the challenges are daunting. In this section we will discuss and evaluate commonly used methods to deliver microRNAs or their inhibitors in vitro and in vivo, as well as the strategies to interfere, either directly or indirectly, with miRNA function (Fig.3).
Figure 3.
Strategies for miRNA delivery and targeting.
5.a) Delivery Strategies
There are two basic ways to deliver microRNAs into target cells: either in their prêt-à-porter, already-functional version, or as genetic precursors. Both alternatives have their pros and cons, and the choice between the two is usually determined by specific experimental conditions and desired biological scenarios.
Delivery of chemically synthesized oligonucleotides
The main advantage of this method is that the compound is already functional and doesn’t need to be further processed. On the other hand, therapeutic oligonucleotides must successfully avoid degradation in the host body, penetrate tumor microenvironment, access the neoplastic compartment, negotiate the intracellular trafficking, localize at the same subcellular compartment as their intended targets, and have specific activity while avoiding off-target effects. The main challenge is that unmodified nucleotides generally have difficulty permeating through the plasma membrane, and once within the cells they are very unstable and prone to degradation. Nevertheless, these two weaknesses could be overcome. The first problem can be solved by using one of the several types of conjugation and/or encapsulation systems to enhance cellular intake and to efficiently deliver oligonucleotides inside the cells. The second solution is to engineer chemically modified oligonucleotides to prevent rapid degradation by nucleolytic enzymes.
One well-known example of these extensively engineered oligonucleotides are antagomirs (Krutzfeldt et al. 2005). Antagomirs are 21–23 long ribonucleotide chains wherein 2′-hydroxyl on the ribose is replaced with the 2′-O-methyl group. The backbone is also modified by replacing some of the phosphodiester linkages by phosphothioate ones. These two modifications greatly improve the biostability yielding oligonucleotides more resistant to degradation. To enhance cell penetration, the single-stranded modified RNA is conjugated to a molecule of cholesterol. As an additional clever trick, antagomirs sequences are not perfectly complementary to their targeted miRNA; instead they have base modifications and mispairings that inhibit cleavage by Ago proteins. This results in a near-irreversible binding between the miRNA and the antagomir, which prevents recognition by miRNA of its cognate mRNA target.
The first in vivo delivery of antagomirs was achieved by Stoffel’s group at the Rockefeller University. Via intravenous injection they successfully delivered antagomirs against miR-16, miR-122, miR-192 and miR-194 and attained long-lasting reduction of these miRNAs in several organs (Krutzfeldt et al. 2005). They further focused on inhibition of miR-122, the most abundant miRNA in the liver and a key regulator of cholesterol metabolism. Not surprisingly, Stoffel and co-authors found that cholesterol biosynthesis was affected and that mice with impaired miR-122 function had lower levels of cholesterol in plasma.
Yet for this to occur milligram amounts of antagomirs had to be delivered (80 mg per kg body weight) rising a question about the feasibility of antagomir use in human subjects – and also about possible off-target effects, especially in organs other than the liver (Morrisey, 2010). The latter problem is illustrated by studies where inhibition of cardiac hypertrophy and fibrosis had been observed in mice using a miR-21 antagomir (Thum et al. 2008) but subsequent genetic ablation of the miR-21 gene failed to elicit a similar cardiac phenotype (Patrick et al. 2010).
Another example of chemically modified oligonucleotides are Morpholinos. These are oligonucleotides which contain six-member morpholine rings in place of five-member ribose or deoxyribose residues and are fully resistant to the action of nucleases. Oligomers of 25 morpholinos units are very stable inside the cell and they do not trigger immune responses (Summerton, 1999). To enhance cellular intake, morpholinos can be covalently conjugated with cell-penetrating peptides. These conjugated morphorlinos, called PPMOs (Peptide-conjugated Phosphorodiamidate Morpholino Oligomers) have been tested in various animal models of Duchenne muscular dystrophy (DMD) [reviewed in (Moulton & Moulton, 2010)] where the antisense oligonucleotide is designed to modify the splicing of the aberrant dystrophin mRNA by skipping the mutated exon (Aartsma-Rus et al. 2004; Alter et al. 2006; McClorey et al. 2006). Furthermore, AVI-4658, a PMO-based drug that targets exon 50 and is delivered by intramuscular injection, is currently in clinical trial for systemic treatment of DMD (NCT00844597) (Kinali et al. 2009).
Locked Nucleid Acids (LNAs) are another version of chemically modified ribonucleotides. In this case, the ribose moiety has an extra bridge connecting the 2′ oxygen and 4′ carbon, resulting in a “locked” conformation. LNAs can be mixed with regular RNA and DNA nucleotides yielding more stable oligomers (Kaur et al. 2006). Currently, a LNA-based miR-122 inhibitor developed by Santaris Pharma is in phase II clinical trial for the treatment of hepatitis C (Lanford et al. 2010).
Another approach to improve cellular intake of oligonucleotides is the use of liposomal nanoparticles. Systemic delivery of miR-34a in a lipid-based vehicle by intravenous injection was enough to block proliferation of engrafted subcutaneous human lung cancer cells, inducing tumor cells death without triggering toxicity in liver, kidney or heart, as shown in a recent study from Mirna Therapeutics, Inc. Furthermore, the formulated miR- 34a didn’t trigger an immune response (Wiggins et al. 2010).
In another study, direct vaginal and intrarectal administration of siRNA delivered using liposomes (called lipoplexes) was used to target endogenous mRNAs expressed in vaginal and intrarectal mucosae, respectively. The gene silencing effects of the siRNA in the mucosae persisted for up to 7 days, although maximal inhibition was maintained over the first 4 days, with 86% reduction in expression. At day 10 after delivery, expression levels of targeted mRNA were back to normal (Zhang et al. 2006). This promising method has not yet been used to target – or enhance - miRNA expression, but there is no obvious reason why it couldn’t be applied to the microRNA field.
Delivery of genetic precursors
While chemically synthesized oligonucleotides can only provide transient overexpression, the use of genetic precursors could in principle allow for stable continuous expression of the encoded oligonucleotide. Viral and non-viral expression cassettes have been used for decades for the introduction of foreign genetic material into host cells, but there are lingering concerns about their safety and their susceptibility to elimination by the immune system. Furthermore, the designing of expression cassettes is not a straightforward process. The choice of promoter, the length of the genetic precursor and the nature of the targeted cell or tissue must be taken into consideration.
Depending on the nature of the viral vector, the delivered material will be integrated into the host DNA or remain in the episomal state [reviewed in (Verma & Weitzman, 2005)]. Retroviral and lentiviral vectors integrate their DNAs into host genomes, while adenoviral vectors replicate as autonomous units. Because the site of integration is unpredictable, there is always the risk of insertional mutagenesis and activation of proto-oncogenes. Apparently, retroviruses are more likely than lentiviruses to integrate in places that potentially cause cancer (Cattoglio et al. 2007; Montini et al. 2006; Montini et al. 2009). A classical example of unintended consequences of retroviral gene therapy is the development of T-cell lymphomas in patients with X-linked SCID. This happened as a result of retroviral transfer of the γ-chain gene into autologous bone marrow-derived CD34+ cells (Howe et al. 2008; Hacein-Bey-Abina et al. 2003; Hacein-Bey-Abina et al. 2008). In those cases, supposedly beneficial retroviral vector was found integrated next to promoter regions of one of several proto-oncogenes: LMO2, BIM1 and CCDN2, leading to their aberrant activation. This scenario could also unfold in case of microRNA-encoding retroviruses. Another drawback of retroviral vectors is that their use is limited to actively dividing target cells..
Lentiviral and adenoviral particles can in principal be used for both dividing and quiescent cells. Nevertheless, because adenoviral DNA is neither integrated nor replicated with each cell division, they are recommended mainly for stable expression in non-dividing cells, to prevent dilution of the adenoviral genomes. Another caveat of using adenoviruses is that they induce strong immunological responses, although new adenoviral species are being tested that do not unnecessarily provoke the immune system [reviewed in (Nayak & Herzog, 2010)].
The use of viral expression vectors also limits the size of the DNA that can be inserted. Thus, it is important to determine the minimal amount of genetic material required to drive expression of mature miRNA mimics or inhibitors. At first approximation, this issue was resolved in the study from Cullen’s lab where a 70-nucleotide sequence corresponding to the miR-30 precursor was cloned into a plasmid under the control of the CMV promoter (Zeng et al. 2002). This plasmid was transiently transfected into 293T cells, resulting in the production of mature miR-30. This exogenously encoded miR-30 was able to induce degradation of an artificial mRNA target in 293T, HeLa and NIH3T3 cells. In contrast when the same plasmid was engineered to encode just the mature 22-nucleotide RNA sequence, no functional miR-30 was expressed, which is consistent with our current knowledge of miRNA biogenesis. However, it remains to be determined whether clusters of microRNAs could be expressed in a way that faithfully reproduces processing of the primary transcript.
The introduction of miRNA-encoding genes into retroviral cassettes was pioneered by Bartel’s lab. Similarly to what Zeng and collaborators had observed, Bartel and coauthors established that for successful miRNA expression, they needed the entire pre-miRNA-coding DNA plus 125 nucleotides of genomic sequence flanking each side of the miRNA for proper processing and maturation (Chen et al. 2004). Armed with this knowledge, they used retroviral constructs expressing precursors of miR-181, miR-223, miR-142 or miR-30 to infect hematopoietic progenitor cells from mouse bone marrow to study the effects of ectopic expression of these miRNAs on hematopoietic lineages in vitro. They also transplanted these cells into lethally irradiated mice, resulting in reconstitution of all blood lineages but with different ratios of each depending on the manipulated miRNA (Chen et al. 2004). Subsequently, bone marrow transplantation of hematopoietic cells with manipulated miRNA levels was widely used to study the role of miRNAs in normal hematopoiesis (Starczynowski et al, 2010; O’Connell et al. 2010) and in hematological malignancies (Olive et al. 2009; Chang et al. 2008; Mu et al. 2009). The latter studies built on the original observation that bone marrow transplantation of hematopoietic progenitor cells from Eμ-myc mice overexpressing the miR17~92 cluster resulted in accelerated Myc-induced B-lymphomagenesis (He et al. 2005).
5.b) Strategies to alter miRNA function
As stated above, to rescue expression levels of a TS-miRNA, either dsRNA identical to the mature miRNA duplex (miRNA mimics) or cDNA encoding the miRNA of interest could be used. Similarly, oncomiR or metastamiR activities can be targeted by either directly inhibiting their expression using antisense oligonucleotides or by interfering with the miRNA/mRNA interaction using miRNA decoys and target protectors. All these strategies enjoyed some measure of success in the last few years, albeit in preclinical settings.
i) Delivery of miRNA mimics
In vivo small RNA delivery techniques used to be challenging but are clearly improving. In a very recent high-profile paper, Liu and coauthors observed that systemic delivery of miR-34a inhibited prostate cancer metastasis and extended survival of tumor-bearing mice, at least in part by targeting CD44 (Liu et al. 2011). The delivery was achieved using intratumoral and, notably, intravenous injection and newly emerging delivery reagents such RNALancerII (BIOO Scieintific) and siPORT™ amine (Ambion).
ii) Delivery of miRNA genetic precursors
In a study from Slack’s laboratory, adenoviral particles expressing miRNAs were delivered intranasally using a mouse model of lung cancer (Esquela-Kerscher et al. 2008). Specifically, mice with mutant K-ras were infected with an adenovirus expressing let-7a pre-miRNA (Ad-let-7) along with the β-galactosidase marker to track adenoviral expression. The authors detected β-galactosidase staining within 72 hours after intranasal infection in cells surrounding the bronchial tree, and the signal persisted in the lungs for as long as 2 weeks. What is more important is that the size of K-ras-induced lung tumors was reduced by 66–90% in mice treated with Ad-let-7.
In parallel, Mendell’s group demonstrated that systemic delivery of a miR-26a expressing adenoviral vector by intravenous injection resulted in impaired Myc-induced hepatic cancer progression by inducing tumor-specific cell cycle arrest and apoptosis (Kota et al. 2009). Undoubtedly such approaches will be rigorously tested in other pre-clinical models as well. However, their utility is probably limited to miRs with proven tumor suppressor qualities, that is to say 5 to 10 microRNAs (see above). On the other hand, inhibition of microRNA function could probably be performed on a larger repertoire, as detailed below.
iii) Antisense oligonucleotides
Cell culture experiments using antagomirs helped identified numerous miRNAs involved in tumor proliferation or resistance to drugs, as well as their cognate target genes. For instance, antagomirs against miR-221 and miR-222 impair proliferation of cancer cells lines by targeting of p27 (le Sage C. et al. 2007), while antagomirs against miR-27a and miR-451, which regulate MDR1/P-glycoprotein, increase cancer cell sensitivity to therapeutic drugs, such as vinblastine, that are pumped out by P-glycoprotein (Zhu et al. 2008).
Antagomirs are also beginning to prove their worth in xenograft models. For example, Fontana et al. showed that tumors generated from MYCN-amplified LAN-5 neuroblastoma cells completely regress in 30% of the cases upon injection of the antagomir against miR-17-5p (Fontana et al. 2008). Using a more complicated tumor progression model, the Massagué laboratory showed that poorly metastatic breast cancer cells treated with antagomir against miR-355 and reinjected into mice are more capable of colonizing lungs that control antagomir-treated cells (Tavazoie et al. 2008).
To be sure, making tumors more metastatic is not a therapeutic goal; however approaches like this are useful for determining what microRNAs drive tumor dissemination. Indeed, in a recent paper from Weinberg’s lab, systemic administration of miR-10b antagomirs to mice bearing highly metastatic breast cancer cells had no effect on primary tumors but markedly suppresses formation of lung metastases (Ma et al. 2010). This work was based on the previous identification of miR-10b as a metastamiR [(Ma et al. 2007), see above]. Likewise, the above-mentioned miR-34a delivery study was based on the initial observation that antagomirs against miR-34a, when introduced into prostate cancer cells, promoted tumor development and metastasis (Liu et al. 2011).
iv) miRNA Decoys
One notable disadvantage of antisense inhibitors is that they cannot be stably expressed or target multiple members of the same miRNA family. This lead to the idea of competitive inhibitors of miRNA function, or “sponges”, developed by Sharp’s group. Instead of inhibiting miRNAs via direct binding, sponges were designed to inhibit miRNA activity by providing target sites that will function as decoys, namely by attracting multiple miRNA family members and letting the cognate mRNA target escape inhibition (Ebert et al. 2007). An miRNA sponge consists of a strong promoter driving expression of an artificial transcript that carry numerous tandem repeats complementary to the heptameric seed sequence of an specific miRNA (or family of miRNAs.) The efficiency of a sponge depends on the affinity of its binding sites and on the miRNA:sponge ratio. It has been shown that sponges with bulged sites that are unpaired at miRNA positions 9–12 are better baits. A very recent review on sponges by Ebert and Sharp summarizes currently available miRNA sponge constructs and their applications, together with information about the composition of the expression-cassettes (Ebert & Sharp, 2010). Of note, sponge cassettes can be readily delivered by viral vectors. These viral vectors typically have 4 to 10 miRNA-targeted sites separated by several nucleotides, and they often include selection markers, such as fluorescent tags or antibiotic resistance genes. This makes possible the isolation, follow-up and subsequent analysis of sponge-expressing cells.
One recent example of the use of sponges came from Weinberg’s lab, where the researchers targeted miR-31 proving its role in the development of breast cancer metastasis (Valastyan et al. 2009). Specifically, the authors cloned a miR-31 sponge into a retroviral vector and infected non-metastatic MCF7-Ras cells. This procedure yielded a stable sponge-expressing cell line (MCF7-Ras-sp31) with 4.5-fold less miR-31 activity than control cells. When these cells were orthotopically implanted into mice, there was no difference in primary tumor growth or proliferation but MCF7-Ras-sp31cells were more invasive and metastasized to the lungs at 10-times the frequency of control cells.
A more recent example of the use of sponges helped confirm the function of miR-15/16 as tumor suppressors and validated some of their targets in multiple myeloma. Carrasco’s lab showed that in vitro transduction of MM cells with a lentiviral vector targeting the miR-15/16 seed sequence was sufficient to increase cell proliferation 1.5–2 fold and invasiveness in matrigel experiments 3-fold (Gatt et al, 2010). Not surprisingly, intravenous injection of miR-16 sponge-transduced cells into sublethally-irradiated mice accelerated disease progression and enhanced metastatic potential. The inhibition of the miR-16 family also induced an increase in cell resistance to conventional MM therapies: adriamycin and melphalan, confirming the therapeutic importance of the miR15a/16-1 cluster.
v) Target protection
Although morpholinos were initially designed to block mRNA translation (Taylor et al. 1996; Wienholds et al. 2003) they are currently being directed towards different aspects of the miRNA activity. First, they can bind directly to the miRNA functional guide strand incorporated into the miRISC complex, thus inhibiting binding to target mRNA. Second, they can bind pri-miRNA hairpin or pre-miRNA stem-loop, inhibiting processing by Drosha or Dicer, respectively. Third, morpholinos can be used as “target protectors”, designed to bind and protect the target sequence on the mRNA in such a way that the miRNA cannot access it (Choi et al. 2007). The great advantage of target protection is its specificity, leading to inhibition of miRNA activity towards a single mRNA target, while all other miRNA loss-of-function methods affect all downstream targets indiscriminately.
So far, target protectors have been used mostly in zebrafish developmental biology to elucidate the role of microRNAs in patterning and cell fate determinaiton (Choi et al. 2007; Leucht et al. 2008; Li et al. 2008; Zeng et al. 2009). Most recently, the Lodish and Lim laboratories used morpholinos against miR-125b in zebrafish to demonstrate its role in regulation of p53 in vivo (Le et al. 2009). They first showed that ectopically expressed miR-125b represses endogenous p53 expression and p53-induced apoptosis in human cells. However, the analysis of zebrafish development also allowed the authors to observe an inverse correlation between endogenous miR-125b expression and p53 activity during zebrafish embryogenesis. The injection of morpholinos (125bMO) against the mature guide strand or against the three alternative miR-125b precursors almost completely blocked the expression of mature miR-125b. By performing injections at the one-to-four-cells stage (18-14 hours post fertilization), they observed increased apoptosis in the embryonic brain, along with higher levels of p53 protein expression. Furthermore, injection of miR-125b mimics into 125bMO embryos rescued the phenotype by restoring the normal levels of p53. Finally, inhibition of p53 activation and expression either by injection of miR-125b mimics or morpholinos against p53, prevented apoptosis when embryos were γ-irradiated or treated with camptothecin. In an important follow-up study, the effects of miR-125b on p53 were reproduced in a prostate cancer xenograft model, where the levels of this microRNA correlated with neoplastic growth (Shi et al. 2011)
Also relevantly to the field of cancer therapeutics, a recent version called vivomorpholinos has been developed to be used in adult animals including vertebrates (Morcos et al. 2008). Vivo-morpholinos can be delivered systemically via intravenous injection or to specific organs by localized injection. So far, vivo-morpholinos have been successfully used in xenopus (Matsuda & Shi, 2010), newt (Maki et al. 2010), zebrafish (Carrillo et al. 2010; Guo et al. 2010), and finally mice (Parra et al, 2010; Kang et al. 2010; Azoitei et al. 2010). Although none of these studies involves targeting of miRNA activity or expression, custom-made morpholinos are now available for research purposes from Gene Tools, LLC.
6. The promise of miRNAs as Therapeutic Adjuvants
Contrary to what occurs in other genetic diseases where a single mutation is responsible for a given phenotype, most human cancers arise from several genetic mutations that accumulate over time. In fact, human tumorigenesis is a dynamic biological process where tumor cells evolve to overcome their limitations and escape therapeutic interventions (Merlo et al. 2006).
Having considered this natural selection process, it is hard to imagine cures based on inhibition or enhancement of a single miRNA, even after repeated treatments. Moreover, it has been shown that long-term exposure to short dsRNAs results in the saturation of the endogenous RNAi machinery. This saturation leads to a shortage of proteins required for the processing of miRNAs, such as exportin-5, resulting in high organ toxicity and, in some cases, death (Grimm et al. 2006).
This leads us to believe that miRNAs would have more therapeutic value as acute, rather than chronic adjuvant targets. This utility is supported by numerous studies showing that miRNAs affect sensitivity to different chemotherapeutic agents in multiple tumor types. Admittedly, most of these are in vitro gain- or loss-of-function experiments, where candidate miRNAs are first identified in tumor cell lines with different degrees of resistance to specific chemotherapeutic drugs and subsequently targeted in order to overcome drug resistance. Although the in vitro studies discussed below still await in vivo validation, the chemosensitization effects appear to be very robust.
One of the first studies linking miRNA levels and chemoresistance was performed in human cholangiocarcinoma cell lines (Meng et al. 2006). In this study, levels of expression of several miRNAs were compared in malignant and non-malignant human cholangiocytes. Not only the authors identified miR-21, miR-141 and miR-200b as highly over-expressed in malignant cells, but they also discovered that while inhibition of miR-141 primarily decreases cell growth, inhibition of miR-21 and miR-200b increase sensitivity to gemcitabine. Another example of miRNAs involvement in chemoresistance is the work by Kovalchuk and collaborators (Kovalchuk et al. 2008). First, by microarray analysis, the authors compared the miRNA profiles of MCF-7 breast adenocarcinoma cells resistant or sensitive to doxorubicin. They identified 137 differentially regulated miRNAs (75 down-regulated, 63 upregulated). Of these, miR-451 silencing was critical for the acquisition of drug resistance, due to its targeting of the P-glycoprotein (Mdr1) gene. Many more studies on the same subject came out in the last two years (Table 2).
Table 2.
miRNAs linked to chemoresistance or chemosensitivity to chemotherapeutic agents in human cancer.
| Cancer Type | miRNA | Drug | Targeted gene | Reference |
|---|---|---|---|---|
| miRNAs whose expression increased sensitivity to chemotherapeutic drugs | ||||
| Lung | miR-1 | Doxorubicine | MET, Pim-1 | (Nasser et al. 2008) |
| miR-16 | NSC236613, NSC670550 | (Blower et al. 2008) | ||
| miR-21 | NSC63878, NSC265450 | (Blower et al. 2008) | ||
| Multidrug-resistant gastric cancer | miR-15b | Vincristine, adriamycin, cisplatin, ateposide | BCL2 | (Xia et al. 2008) |
| miR-16 | ||||
| Prostate Cancer | miR-34a | Camtothecin | SIRT-1 | (Fujita et al. 2008) |
| Gastric cancer (p53mutant, high BCL2) | miR34a miR43b miR34c |
Doxorubicine, cisplatin, gemcitabine, docetaxel | Bcl-2, Notch, HMGA2 | (Ji et al. 2008) |
| Gastric cancer/Cisplatinres* | miR-200c | Cisplatin, ψ5-FU, paclitaxel, and adriamycin | E-cadherin | (Chen et al. 2010) |
| Hepatocellular carcinoma | miR-101 | Etoposide, curcumin, doxorubicine | Mcl-1 | (Su et al. 2009) |
| miR-199a-3p | Doxorubicine | mTOR, c-Met | (Fornari et al. 2010) | |
| miR-122 | Cyclin G1 | (Fornari et al. 2009) | ||
| Breast cancer/doxorubibineres | miR-451 | Doxorubicine | Mdr1 | (Kovalchuk et al. 2008) |
| Breast cancer | miR-200b | Ferritin | (Shpyleva et al, 2010) | |
| Breast cancer/VP-16res | miR-326 | Doxorubicine, VP-16 | MRP-1 | (Liang et al. 2010) |
| Glioblastoma | miR-451 | Imitanib | SMAD3, SMAD4 | (Gal et al. 2008) |
| Leukemia/doxorubicineres | miR-331-5p miR27a |
Doxorubcin | P-glycoprotein | (Feng et al. 2010) |
| Leukemia/VCR** | miR-138 | Vincristine, adriamycin, cisplatin, 5-FU | P-glycoprotein, MDR1, BCL2 | (Zhao et al. 2010) |
| Small cell lung carcinoma | miR-134 miR-379 miR-495 |
Cisplatin, Etoposide and Doxorubicin | MRP1/ABCC1 | (Guo et al. 2010) |
| miRNAs whose inhibition increased sensitivity to chemotherapeutic drugs | ||||
| Lung | Let-7i | NSC670550 | (Blower et al. 2008) | |
| miR-21 | NSC621888, NSC622700, NSC670550, NSC122750 | (Blower et al. 2008) | ||
| Ovarian Cancer | miR-214 | Cisplatin | PTEN | (Yang et al. 2006) |
| Breast Cancer | miR-221 | Tamoxifen | ER-γ | (Zhao et al. 2008) |
| miR-222 | ||||
| miR-21 | Topotecan | PTEN | (Meng et al. 2006) | |
| Neuroblastoma | miR-17-5p | Doxycline | p21, BIM | (Fontana et al. 2008) |
| Malignant Cholangiocytes | miR-21 | Gemcitabine | PTEN | (Meng et al. 2006) |
| miR-200b | ||||
| Malignant Cholangiocytes/IL6 | Let-7a | Gemcitabine, 5-FU, Campothecin | ||
| Glioblatoma | miR-21 | NSC670550, NSC122750 | (Blower et al. 2008) | |
| Burkitt’s Lymphoma | miR-34a | Bortezomib | c-Myc | (Sotillo et al, 2011) |
| Leukemia | miR-21 | Arabinosylcytosine | PDCD4 | (Li et al. 2010) |
| Pancreatic adenocarcinoma | miR-21 | 5-FU | (Hwang et al. 2010) | |
| Multiple Myeloma | miR-15a/16-1 | adriamycin and melphalan | FGFR1, PI3KCa, MDM4, VEGFa | (Gatt et al, 2010) |
| miRNAs whose inhibition decreased sensitivity to chemotherapeutic drugs | ||||
| Ovarian Cancer | miR-21 | NSC265450 | (Blower et al. 2008) | |
| Let-7i | Cisplatin | H-RAS, HMGA2 | (Yang et al. 2008) | |
| Glioblastoma | miR-21 | NSC123127 | (Blower et al. 2008) | |
| miRNAs whose expression decreased sensitivity to chemotherapeutic drugs | ||||
| HNSCC† | miR-98 | Cislatin, doxorubicine | HMGA2 | (Hebert et al. 2007) |
| SCC, HCC § | Let-7a | Doxorubicine, paclitaxel, IF-γ | RAS, HMGA2 | (Tsang & Kwok, 2008) |
| Hepatocellular carcinoma | miR-188b | Doxorubicine | metalloprotease 3 | (Wang et al. 2009) |
| Breast cancer | miR-221 miR-222 |
Tamoxifen | P27 | (Miller et al. 2008) |
res: Resistant;
VCR: Vincristine-induced multidrug resistance;
HNSCC: Head and Neck Squamous Cell Carcinoma;
SCC, HCC: Squamous cell carcinoma, Hepatocellular Carcinoma.
5-FU: 5-Fluorouracil.
We have recently shown that inhibition of miR-34a in Myc-transformed B-cells enhances apoptotic responses to the protease inhibitor bortezomib (Sotillo et al, 2011). This is because in cells with the functional Myc-Arf-Mdm2 axis miR-34a downregulates steady-state levels of p53, which is a key determinant of bortezomib sensitivity (Yu et al. 2007). In contrast, ectopic expression of miR-34a in colorectal cancer cells resistant to treatment with 5-fluorouracile (5-FU), inhibited cell proliferation but also sensitized cells to 5-FU treatment (Akao et al. 2011). Thus, once again, the involvement of microRNAs in chemoresistance is context dependent, and close attention needs to be paid to the repertoire of relevant microRNA targets in a given cancer or cell type.
7. Conclusions and Perspectives
There is no doubt that miRNAs play critical roles in cancer initiation and progression. The proof of this principle came from numerous animal models as well as human cancer genetics, in particular the studies on hematological malignancies. In these neoplasms often addicted to a single genetic lesion or pathway, manipulating microRNA levels is proving to be a viable therapeutic option, especially in light of recent advances in the field of small RNA delivery. However, there is a concern that in genetically complex solid cancers these single-pronged attacks might ultimately prove unsuccessful. Thus, the idea that targeting of microRNAs should be considered as an adjuvant therapy is getting considerable traction. Basic, translational, and clinical research done in the next few years will tell whether this promise is well-founded.
Acknowledgments
We are thankful to Dr. Michele A. Cleary (Merk & Co., Inc.) for her comments and reviewing the manuscript. Elena Sotillo is partially supported by the Alex’s Lemonade Stand Foundation. Andrei Thomas-Tikhonenko is supported by grants from the US National Institutes of Health and the Institutional Development Fund of the Children’s Hospital of Philadelphia. The authors declare that they have no competing financial interests.
Abbreviations
- Ago
Argonaute
- dsRNA
double stranded RNA
- EMT
Epithelial to Mesenchimal Transition
- mRNA
messenger RNA
- miRNA
microRNA
- RISC
RNA Induced Silencing Complex
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aartsma-Rus A, Kaman WE, Bremmer-Bout M, Janson AA, den Dunnen JT, van Ommen GJ, et al. Comparative analysis of antisense oligonucleotide analogs for targeted DMD exon 46 skipping in muscle cells. Gene Ther. 2004;11:1391–1398. doi: 10.1038/sj.gt.3302313. [DOI] [PubMed] [Google Scholar]
- Akao Y, Noguchi S, Iio A, Kojima K, Takagi T, Naoe T. Dysregulation of microRNA-34a expression causes drug-resistance to 5-FU in human colon cancer DLD-1 cells. Cancer Lett. 2011;300:197–204. doi: 10.1016/j.canlet.2010.10.006. [DOI] [PubMed] [Google Scholar]
- Alexiou P, Vergoulis T, Gleditzsch M, Prekas G, Dalamagas T, Megraw M, et al. miRGen 2.0: a database of microRNA genomic information and regulation. Nucleic Acids Res. 2010;38:137–141. doi: 10.1093/nar/gkp888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alter J, Lou F, Rabinowitz A, Yin H, Rosenfeld J, Wilton SD, et al. Systemic delivery of morpholino oligonucleotide restores dystrophin expression bodywide and improves dystrophic pathology. Nat Med. 2006;12:175–177. doi: 10.1038/nm1345. [DOI] [PubMed] [Google Scholar]
- Azoitei N, Pusapati GV, Kleger A, Moller P, Kufer R, Genze F, et al. Protein kinase D2 is a crucial regulator of tumour cell-endothelial cell communication in gastrointestinal tumours. Gut. 2010;59:1316–1330. doi: 10.1136/gut.2009.206813. [DOI] [PubMed] [Google Scholar]
- Baek D, Villen J, Shin C, Camargo FD, Gygi SP, Bartel DP. The impact of microRNAs on protein output. Nature. 2008;455:64–71. doi: 10.1038/nature07242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagchi A, Mills AA. The quest for the 1p36 tumor suppressor. Cancer Res. 2008;68:2551–6. doi: 10.1158/0008-5472.CAN-07-2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balaguer F, Link A, Lozano JJ, Cuatrecasas M, Nagasaka T, Boland CR, et al. Epigenetic silencing of miR-137 is an early event in colorectal carcinogenesis. Cancer Res. 2010;70:6609–6618. doi: 10.1158/0008-5472.CAN-10-0622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batlle E, Sancho E, Franci C, Dominguez D, Monfar M, Baulida J, et al. The transcription factor snail is a repressor of E-cadherin gene expression in epithelial tumour cells. Nat Cell Biol. 2000;2:84–89. doi: 10.1038/35000034. [DOI] [PubMed] [Google Scholar]
- Benetti R, Gonzalo S, Jaco I, Munoz P, Gonzalez S, Schoeftner S, et al. A mammalian microRNA cluster controls DNA methylation and telomere recombination via Rbl2-dependent regulation of DNA methyltransferases. Nat Struct Mol Biol. 2008;15:268–279. doi: 10.1038/nsmb.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentwich I, Avniel A, Karov Y, Aharonov R, Gilad S, Barad O, et al. Identification of hundreds of conserved and nonconserved human microRNAs. Nat Genet. 2005;37:766–770. doi: 10.1038/ng1590. [DOI] [PubMed] [Google Scholar]
- Berezikov E, Chung WJ, Willis J, Cuppen E, Lai EC. Mammalian mirtron genes. Mol Cell. 2007;28:328–336. doi: 10.1016/j.molcel.2007.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein E, Caudy AA, Hammond SM, Hannon GJ. Role for a bidentate ribonuclease in the initiation step of RNA interference. Nature. 2001;409:363–366. doi: 10.1038/35053110. [DOI] [PubMed] [Google Scholar]
- Betel D, Wilson M, Gabow A, Marks DS, Sander C. The microRNA.org resource: targets and expression. Nucleic Acids Res. 2008;36:149–153. doi: 10.1093/nar/gkm995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blower PE, Chung JH, Verducci JS, Lin S, Park JK, Dai Z, et al. MicroRNAs modulate the chemosensitivity of tumor cells. Mol Cancer Ther. 2008;7:1–9. doi: 10.1158/1535-7163.MCT-07-0573. [DOI] [PubMed] [Google Scholar]
- Bohnsack MT, Czaplinski K, Gorlich D. Exportin 5 is a RanGTP-dependent dsRNA-binding protein that mediates nuclear export of pre-miRNAs. RNA. 2004;10:185–191. doi: 10.1261/rna.5167604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bommer GT, Gerin I, Feng Y, Kaczorowski AJ, Kuick R, Love RE, et al. p53-mediated activation of miRNA34 candidate tumor-suppressor genes. Curr Biol. 2007;17:1298–1307. doi: 10.1016/j.cub.2007.06.068. [DOI] [PubMed] [Google Scholar]
- Bracken CP, Gregory PA, Kolesnikoff N, Bert AG, Wang J, Shannon MF, et al. A double-negative feedback loop between ZEB1-SIP1 and the microRNA-200 family regulates epithelial-mesenchymal transition. Cancer Res. 2008;68:7846–7854. doi: 10.1158/0008-5472.CAN-08-1942. [DOI] [PubMed] [Google Scholar]
- Braun J, Hoang-Vu C, Dralle H, Huttelmaier S. Downregulation of microRNAs directs the EMT and invasive potential of anaplastic thyroid carcinomas. Oncogene. 2010;29:4237–4244. doi: 10.1038/onc.2010.169. [DOI] [PubMed] [Google Scholar]
- Brown AG, Ross FM, Dunne EM, Steel CM, Weir-Thompson EM. Evidence for a new tumour suppressor locus (DBM) in human B-cell neoplasia telomeric to the retinoblastoma gene. Nat Genet. 1993;3:67–72. doi: 10.1038/ng0193-67. [DOI] [PubMed] [Google Scholar]
- Bueno MJ, Perez dCI, Gomez de CM, Santos J, Calin GA, Cigudosa JC, et al. Genetic and epigenetic silencing of microRNA-203 enhances ABL1 and BCR-ABL1 oncogene expression. Cancer Cell. 2008;13:496–506. doi: 10.1016/j.ccr.2008.04.018. [DOI] [PubMed] [Google Scholar]
- Burk U, Schubert J, Wellner U, Schmalhofer O, Vincan E, Spaderna S, et al. A reciprocal repression between ZEB1 and members of the miR-200 family promotes EMT and invasion in cancer cells. EMBO Rep. 2008;9:582–589. doi: 10.1038/embor.2008.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calin GA, Dumitru CD, Shimizu M, Bichi R, Zupo S, Noch E, et al. Frequent deletions and down-regulation of micro- RNA genes miR15 and miR16 at 13q14 in chronic lymphocytic leukemia. Proc Natl Acad Sci USA. 2002;99:15524–9. doi: 10.1073/pnas.242606799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano A, Perez-Moreno MA, Rodrigo I, Locascio A, Blanco MJ, del Barrio MG, et al. The transcription factor snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat Cell Biol. 2000;2:76–83. doi: 10.1038/35000025. [DOI] [PubMed] [Google Scholar]
- Carrillo M, Kim S, Rajpurohit SK, Kulkarni V, Jagadeeswaran P. Zebrafish von Willebrand factor. Blood Cells Mol Dis. 2010;9(45):326–333. doi: 10.1016/j.bcmd.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castilla MA, Moreno-Bueno G, Romero-Perez L, Van DV, Biscuola M, Lopez-Garcia MA, et al. Micro-RNA signature of the epithelial-mesenchymal transition in endometrial carcinosarcoma. J Pathol. 2011;223:72–80. doi: 10.1002/path.2802. [DOI] [PubMed] [Google Scholar]
- Cattoglio C, Facchini G, Sartori D, Antonelli A, Miccio A, Cassani B, et al. Hot spots of retroviral integration in human CD34+ hematopoietic cells. Blood. 2007;110:1770–1778. doi: 10.1182/blood-2007-01-068759. [DOI] [PubMed] [Google Scholar]
- Chang TC, Wentzel EA, Kent OA, Ramachandran K, Mullendore M, Lee KH, et al. Transactivation of miR-34a by p53 broadly influences gene expression and promotes apoptosis. Mol Cell. 2007;26:745–752. doi: 10.1016/j.molcel.2007.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang TC, Yu D, Lee YS, Wentzel EA, Arking DE, West KM, et al. Widespread microRNA repression by Myc contributes to tumorigenesis. Nat Genet. 2008;40:43–50. doi: 10.1038/ng.2007.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang TC, Zeitels LR, Hwang HW, Chivukula RR, Wentzel EA, Dews M, et al. Lin-28B transactivation is necessary for Myc-mediated let-7 repression and proliferation. Proc Natl Acad Sci U S A. 2009;106:3384–3389. doi: 10.1073/pnas.0808300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CZ, Li L, Lodish HF, Bartel DP. MicroRNAs modulate hematopoietic lineage differentiation. Science. 2004;303:83–86. doi: 10.1126/science.1091903. [DOI] [PubMed] [Google Scholar]
- Chen Y, Zuo J, Liu Y, Gao H, Liu W. Inhibitory effects of miRNA-200c on chemotherapy-resistance and cell proliferation of gastric cancer SGC7901/DDP cells. Chin J Cancer. 2010;29:1006–1011. doi: 10.5732/cjc.010.10236. [DOI] [PubMed] [Google Scholar]
- Chen Z, Zeng H, Guo Y, Liu P, Pan H, Deng A, et al. miRNA-145 inhibits non-small cell lung cancer cell proliferation by targeting c-Myc. J Exp Clin Cancer Res. 2010;29:151. doi: 10.1186/1756-9966-29-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chendrimada TP, Finn KJ, Ji X, Baillat D, Gregory RI, Liebhaber SA, et al. MicroRNA silencing through RISC recruitment of eIF6. Nature. 2007;447:823–828. doi: 10.1038/nature05841. [DOI] [PubMed] [Google Scholar]
- Chendrimada TP, Gregory RI, Kumaraswamy E, Norman J, Cooch N, Nishikura K, et al. TRBP recruits the Dicer complex to Ago2 for microRNA processing and gene silencing. Nature. 2005;436:740–744. doi: 10.1038/nature03868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng J, Scully P, Shew JY, Lee WH, Vila V, Haas M. Homozygous deletion of the retinoblastoma gene in an acute lymphoblastic leukemia (T) cell line. Blood. 1990;75:730–735. [PubMed] [Google Scholar]
- Chi SW, Zang JB, Mele A, Darnell RB. Argonaute HITS-CLIP decodes microRNA-mRNA interaction maps. Nature. 2009;460:479–486. doi: 10.1038/nature08170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin LJ, Ratner E, Leng S, Zhai R, Nallur S, Babar I, et al. A SNP in a let-7 microRNA complementary site in the KRAS 3′ untranslated region increases non-small cell lung cancer risk. Cancer Res. 2008;68:8535–8540. doi: 10.1158/0008-5472.CAN-08-2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi WY, Giraldez AJ, Schier AF. Target protectors reveal dampening and balancing of Nodal agonist and antagonist by miR-430. Science. 2007;318:271–274. doi: 10.1126/science.1147535. [DOI] [PubMed] [Google Scholar]
- Christoffersen NR, Shalgi R, Frankel LB, Leucci E, Lees M, Klausen M, et al. p53-independent upregulation of miR-34a during oncogene-induced senescence represses MYC. Cell Death Differ. 2010;17:236–245. doi: 10.1038/cdd.2009.109. [DOI] [PubMed] [Google Scholar]
- Chung EY, Dews M, Cozma D, Yu D, Wentzel EA, Chang TC, et al. c- Myb oncoprotein is an essential target of the dleu2 tumor suppressor microRNA cluster. Cancer Biol Ther. 2008;7:1758–1764. doi: 10.4161/cbt.7.11.6722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimmino A, Calin GA, Fabbri M, Iorio MV, Ferracin M, Shimizu M, et al. miR-15 and miR-16 induce apoptosis by targeting BCL2. Proc Natl Acad Sci U S A. 2005;102:13944–13949. doi: 10.1073/pnas.0506654102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comijn J, Berx G, Vermassen P, Verschueren K, van GL, Bruyneel E, et al. The two-handed E box binding zinc finger protein SIP1 downregulates E-cadherin and induces invasion. Mol Cell. 2001;7:1267–1278. doi: 10.1016/s1097-2765(01)00260-x. [DOI] [PubMed] [Google Scholar]
- Corney DC, Flesken-Nikitin A, Godwin AK, Wang W, Nikitin AY. MicroRNA-34b and MicroRNA-34c are targets of p53 and cooperate in control of cell proliferation and adhesion-independent growth. Cancer Res. 2007;67:8433–8438. doi: 10.1158/0008-5472.CAN-07-1585. [DOI] [PubMed] [Google Scholar]
- Datta J, Kutay H, Nasser MW, Nuovo GJ, Wang B, Majumder S, et al. Methylation mediated silencing of MicroRNA-1 gene and its role in hepatocellular carcinogenesis. Cancer Res. 2008;68:5049–5058. doi: 10.1158/0008-5472.CAN-07-6655. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Davis E, Caiment F, Tordoir X, Cavaille J, Ferguson-Smith A, Cockett N, et al. RNAi-mediated allelic trans-interaction at the imprinted Rtl1/Peg11 locus. Curr Biol. 2005;15:743–749. doi: 10.1016/j.cub.2005.02.060. [DOI] [PubMed] [Google Scholar]
- Denli AM, Tops BB, Plasterk RH, Ketting RF, Hannon GJ. Processing of primary microRNAs by the Microprocessor complex. Nature. 2004;432:231–235. doi: 10.1038/nature03049. [DOI] [PubMed] [Google Scholar]
- Dews M, Fox JL, Hultine S, Sundaram P, Wang W, Liu YY, et al. The myc-miR-17~92 axis blunts TGF{beta} signaling and production of multiple TGF{beta}-dependent antiangiogenic factors. Cancer Res. 2010;70:8233–8246. doi: 10.1158/0008-5472.CAN-10-2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dews M, Homayouni A, Yu D, Murphy D, Sevignani C, Wentzel E, et al. Augmentation of tumor angiogenesis by a Myc-activated microRNA cluster. Nat Genet. 2006;38:1060–1065. doi: 10.1038/ng1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doench JG, Petersen CP, Sharp PA. siRNAs can function as miRNAs. Genes Dev. 2003;17:438–442. doi: 10.1101/gad.1064703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doench JG, Sharp PA. Specificity of microRNA target selection in translational repression. Genes Dev. 2004;18:504–511. doi: 10.1101/gad.1184404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert MS, Neilson JR, Sharp PA. MicroRNA sponges: competitive inhibitors of small RNAs in mammalian cells. Nat Methods. 2007;4:721–6. doi: 10.1038/nmeth1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert MS, Sharp PA. MicroRNA sponges: progress and possibilities. RNA. 2010;16:2043–2050. doi: 10.1261/rna.2414110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbashir SM, Lendeckel W, Tuschl T. RNA interference is mediated by 21- and 22-nucleotide RNAs. Genes Dev. 2001;15:188–200. doi: 10.1101/gad.862301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst A, Campos B, Meier J, Devens F, Liesenberg F, Wolter M, et al. De-repression of CTGF via the miR-17-92 cluster upon differentiation of human glioblastoma spheroid cultures. Oncogene. 2010;29:3411–3422. doi: 10.1038/onc.2010.83. [DOI] [PubMed] [Google Scholar]
- Esquela-Kerscher A, Trang P, Wiggins JF, Patrawala L, Cheng A, Ford L, et al. The let-7 microRNA reduces tumor growth in mouse models of lung cancer. Cell Cycle. 2008;7:759–764. doi: 10.4161/cc.7.6.5834. [DOI] [PubMed] [Google Scholar]
- Fabbri M, Bottoni A, Shimizu M, Spizzo R, Nicoloso MS, Rossi S, et al. Association of a microRNA/TP53 feedback circuitry with pathogenesis and outcome of B-cell chronic lymphocytic leukemia. JAMA. 2011;305:59–67. doi: 10.1001/jama.2010.1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabbri M, Garzon R, Cimmino A, Liu Z, Zanesi N, Callegari E, et al. MicroRNA-29 family reverts aberrant methylation in lung cancer by targeting DNA methyltransferases 3A and 3B. Proc Natl Acad Sci U S A. 2007;104:15805–15810. doi: 10.1073/pnas.0707628104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng DD, Zhang H, Zhang P, Zheng YS, Zhang XJ, Han BW, et al. Down-regulated miR-331-5p and miR-27a are associated with chemotherapy resistance and relapse in leukemia. J Cell Mol Med. 2010 doi: 10.1111/j.1582-4934.2010.01213.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fire A, Xu S, Montgomery MK, Kostas SA, Driver SE, Mello CC. Potent and specific genetic interference by double-stranded RNA in Caenorhabditis elegans. Nature. 1998;391:806–811. doi: 10.1038/35888. [DOI] [PubMed] [Google Scholar]
- Folini M, Gandellini P, Longoni N, Profumo V, Callari M, Pennati M, et al. miR-21: an oncomir on strike in prostate cancer. Mol Cancer. 2010;9:12. doi: 10.1186/1476-4598-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontana L, Fiori ME, Albini S, Cifaldi L, Giovinazzi S, Forloni M, et al. Antagomir-17-5p abolishes the growth of therapy-resistant neuroblastoma through p21 and BIM. PLoS One. 2008;3:e2236. doi: 10.1371/journal.pone.0002236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fornari F, Gramantieri L, Giovannini C, Veronese A, Ferracin M, Sabbioni S, et al. MiR-122/cyclin G1 interaction modulates p53 activity and affects doxorubicin sensitivity of human hepatocarcinoma cells. Cancer Res. 2009;69:5761–5767. doi: 10.1158/0008-5472.CAN-08-4797. [DOI] [PubMed] [Google Scholar]
- Fornari F, Milazzo M, Chieco P, Negrini M, Calin GA, Grazi GL, et al. MiR-199a-3p regulates mTOR and c-Met to influence the doxorubicin sensitivity of human hepatocarcinoma cells. Cancer Res. 2010;70:5184–5193. doi: 10.1158/0008-5472.CAN-10-0145. [DOI] [PubMed] [Google Scholar]
- Frankel LB, Christoffersen NR, Jacobsen A, Lindow M, Krogh A, Lund AH. Programmed cell death 4 (PDCD4) is an important functional target of the microRNA miR-21 in breast cancer cells. J Biol Chem. 2008;283:1026–1033. doi: 10.1074/jbc.M707224200. [DOI] [PubMed] [Google Scholar]
- Fu TY, Chang CC, Lin CT, Lai CH, Peng SY, Ko YJ, et al. Let-7b-mediated suppression of basigin expression and metastasis in mouse melanoma cells. Exp Cell Res. 2010;317:445–451. doi: 10.1016/j.yexcr.2010.11.004. [DOI] [PubMed] [Google Scholar]
- Fujita Y, Kojima K, Hamada N, Ohhashi R, Akao Y, Nozawa Y, et al. Effects of miR-34a on cell growth and chemoresistance in prostate cancer PC3 cells. Biochem Biophys Res Commun. 2008;377:114–119. doi: 10.1016/j.bbrc.2008.09.086. [DOI] [PubMed] [Google Scholar]
- Gabriely G, Wurdinger T, Kesari S, Esau CC, Burchard J, Linsley PS, et al. MicroRNA 21 promotes glioma invasion by targeting matrix metalloproteinase regulators. Mol Cell Biol. 2008;28:5369–5380. doi: 10.1128/MCB.00479-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gal H, Pandi G, Kanner AA, Ram Z, Lithwick-Yanai G, Amariglio N, et al. MIR-451 and Imatinib mesylate inhibit tumor growth of Glioblastoma stem cells. Biochem Biophys Res Commun. 2008;376:86–90. doi: 10.1016/j.bbrc.2008.08.107. [DOI] [PubMed] [Google Scholar]
- Garzia L, Andolfo I, Cusanelli E, Marino N, Petrosino G, De MD, et al. MicroRNA-199b-5p impairs cancer stem cells through negative regulation of HES1 in medulloblastoma. PLoS One. 2009;4:e4998. doi: 10.1371/journal.pone.0004998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatt ME, Zhao JJ, Ebert MS, Zhang Y, Chu Z, Mani M, et al. MicroRNAs 15a/16-1 function as tumor suppressor genes in multiple myeloma. Blood. 2010 doi: 10.1182/blood-2009–11–253294. blood-2009-11-253294 [pii]; [DOI] [PubMed] [Google Scholar]
- Gebeshuber CA, Zatloukal K, Martinez J. miR-29a suppresses tristetraprolin, which is a regulator of epithelial polarity and metastasis. EMBO Rep. 2009;10:400–405. doi: 10.1038/embor.2009.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giraldez AJ, Mishima Y, Rihel J, Grocock RJ, van DS, Inoue K, et al. Zebrafish MiR-430 promotes deadenylation and clearance of maternal mRNAs. Science. 2006;312:75–79. doi: 10.1126/science.1122689. [DOI] [PubMed] [Google Scholar]
- Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G, et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol. 2008;10:593–601. doi: 10.1038/ncb1722. [DOI] [PubMed] [Google Scholar]
- Gregory RI, Yan KP, Amuthan G, Chendrimada T, Doratotaj B, Cooch N, et al. The Microprocessor complex mediates the genesis of microRNAs. Nature. 2004;432:235–240. doi: 10.1038/nature03120. [DOI] [PubMed] [Google Scholar]
- Griffiths-Jones S, Saini HK, van DS, Enright AJ. miRBase: tools for microRNA genomics. Nucleic Acids Res. 2008;36:154–158. doi: 10.1093/nar/gkm952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm D, Streetz KL, Jopling CL, Storm TA, Pandey K, Davis CR, et al. Fatality in mice due to oversaturation of cellular microRNA/short hairpin RNA pathways. Nature. 2006;441:537–541. doi: 10.1038/nature04791. [DOI] [PubMed] [Google Scholar]
- Grishok A, Pasquinelli AE, Conte D, Li N, Parrish S, Ha I, et al. Genes and mechanisms related to RNA interference regulate expression of the small temporal RNAs that control C. elegans developmental timing. Cell. 2001;106:23–34. doi: 10.1016/s0092-8674(01)00431-7. [DOI] [PubMed] [Google Scholar]
- Guo L, Liu Y, Bai Y, Sun Y, Xiao F, Guo Y. Gene expression profiling of drug-resistant small cell lung cancer cells by combining microRNA and cDNA expression analysis. Eur J Cancer. 2010;46:1692–1702. doi: 10.1016/j.ejca.2010.02.043. [DOI] [PubMed] [Google Scholar]
- Guo Y, Ma L, Cristofanilli M, Hart RP, Hao A, Schachner M. Transcription factor Sox11b is involved in spinal cord regeneration in adult zebrafish. Neuroscience. 2010;172:329–341. doi: 10.1016/j.neuroscience.2010.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacein-Bey-Abina S, Garrigue A, Wang GP, Soulier J, Lim A, Morillon E, et al. Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. J Clin Invest. 2008;118:3132–3142. doi: 10.1172/JCI35700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacein-Bey-Abina S, von KC, Schmidt M, McCormack MP, Wulffraat N, Leboulch P, et al. LMO2-associated clonal T cell proliferation in two patients after gene therapy for SCID-X1. Science. 2003;302:415–419. doi: 10.1126/science.1088547. [DOI] [PubMed] [Google Scholar]
- He L, He X, Lim LP, de SE, Xuan Z, Liang Y, et al. A microRNA component of the p53 tumour suppressor network. Nature. 2007;447:1130–1134. doi: 10.1038/nature05939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He L, Thomson JM, Hemann MT, Hernando-Monge E, Mu D, Goodson S, et al. A microRNA polycistron as a potential human oncogene. Nature. 2005;435:828–33. doi: 10.1038/nature03552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert C, Norris K, Scheper MA, Nikitakis N, Sauk JJ. High mobility group A2 is a target for miRNA-98 in head and neck squamous cell carcinoma. Mol Cancer. 2007;6:5. doi: 10.1186/1476-4598-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermeking H. The miR-34 family in cancer and apoptosis. Cell Death Differ. 2010;17:193–199. doi: 10.1038/cdd.2009.56. [DOI] [PubMed] [Google Scholar]
- Howe SJ, Mansour MR, Schwarzwaelder K, Bartholomae C, Hubank M, Kempski H, et al. Insertional mutagenesis combined with acquired somatic mutations causes leukemogenesis following gene therapy of SCID-X1 patients. J Clin Invest. 2008;118:3143–3150. doi: 10.1172/JCI35798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu PW, Huang HD, Hsu SD, Lin LZ, Tsou AP, Tseng CP, et al. miRNAMap: genomic maps of microRNA genes and their target genes in mammalian genomes. Nucleic Acids Res. 2006;34:135–139. doi: 10.1093/nar/gkj135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu RJ, Yang HJ, Tsai HJ. Labeled microRNA pull-down assay system: an experimental approach for high-throughput identification of microRNA-target mRNAs. Nucleic Acids Res. 2009;37:e77. doi: 10.1093/nar/gkp274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu W, Chan CS, Wu R, Zhang C, Sun Y, Song JS, et al. Negative regulation of tumor suppressor p53 by microRNA miR-504. Mol Cell. 2010;38:689–699. doi: 10.1016/j.molcel.2010.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys DT, Westman BJ, Martin DI, Preiss T. MicroRNAs control translation initiation by inhibiting eukaryotic initiation factor 4E/cap and poly(A) tail function. Proc Natl Acad Sci U S A. 2005;102:16961–16966. doi: 10.1073/pnas.0506482102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurst DR, Edmonds MD, Welch DR. Metastamir: the field of metastasisregulatory microRNA is spreading. Cancer Res. 2009;69:7495–7498. doi: 10.1158/0008-5472.CAN-09-2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutvagner G, McLachlan J, Pasquinelli AE, Balint E, Tuschl T, Zamore PD. A cellular function for the RNA-interference enzyme Dicer in the maturation of the let-7 small temporal RNA. Science. 2001;293:834–838. doi: 10.1126/science.1062961. [DOI] [PubMed] [Google Scholar]
- Hutvagner G, Zamore PD. A microRNA in a multiple-turnover RNAi enzyme complex. Science. 2002;297:2056–2066. doi: 10.1126/science.1073827. [DOI] [PubMed] [Google Scholar]
- Hwang HW, Wentzel EA, Mendell JT. A hexanucleotide element directs microRNA nuclear import. Science. 2007;315:97–100. doi: 10.1126/science.1136235. [DOI] [PubMed] [Google Scholar]
- Hwang JH, Voortman J, Giovannetti E, Steinberg SM, Leon LG, Kim YT, et al. Identification of microRNA-21 as a biomarker for chemoresistance and clinical outcome following adjuvant therapy in resectable pancreatic cancer. PLoS One. 2010;5:e10630. doi: 10.1371/journal.pone.0010630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inomata M, Tagawa H, Guo YM, Kameoka Y, Takahashi N, Sawada K. MicroRNA-17–92 down-regulates expression of distinct targets in different B-cell lymphoma subtypes. Blood. 2009;113:396–402. doi: 10.1182/blood-2008-07-163907. [DOI] [PubMed] [Google Scholar]
- Ivanovska I, Ball AS, Diaz RL, Magnus JF, Kibukawa M, Schelter JM, et al. MicroRNAs in the miR-106b family regulate p21/CDKN1A and promote cell cycle progression. Mol Cell Biol. 2008;28:2167–2174. doi: 10.1128/MCB.01977-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji Q, Hao X, Meng Y, Zhang M, Desano J, Fan D, et al. Restoration of tumor suppressor miR-34 inhibits human p53-mutant gastric cancer tumorspheres. BMC Cancer. 2008;8:266. doi: 10.1186/1471-2407-8-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson CD, Esquela-Kerscher A, Stefani G, Byrom M, Kelnar K, Ovcharenko D, et al. The let-7 microRNA represses cell proliferation pathways in human cells. Cancer Res. 2007;67:7713–7722. doi: 10.1158/0008-5472.CAN-07-1083. [DOI] [PubMed] [Google Scholar]
- Kang JK, Malerba A, Popplewell L, Foster K, Dickson G. Antisense-induced Myostatin Exon Skipping Leads to Muscle Hypertrophy in Mice Following Octa guanidine Morpholino Oligomer Treatment. Mol Ther. 2010;19:159–164. doi: 10.1038/mt.2010.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur H, Arora A, Wengel J, Maiti S. Thermodynamic, counterion, and hydration effects for the incorporation of locked nucleic acid nucleotides into DNA duplexes. Biochemistry. 2006;45:7347–7355. doi: 10.1021/bi060307w. [DOI] [PubMed] [Google Scholar]
- Kertesz M, Iovino N, Unnerstall U, Gaul U, Segal E. The role of site accessibility in microRNA target recognition. Nat Genet. 2007;39:1278–1284. doi: 10.1038/ng2135. [DOI] [PubMed] [Google Scholar]
- Ketting RF, Fischer SE, Bernstein E, Sijen T, Hannon GJ, Plasterk RH. Dicer functions in RNA interference and in synthesis of small RNA involved in developmental timing in C. elegans. Genes Dev. 2001;15:2654–2659. doi: 10.1101/gad.927801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khvorova A, Reynolds A, Jayasena SD. Functional siRNAs and miRNAs exhibit strand bias. Cell. 2003;115:209–216. doi: 10.1016/s0092-8674(03)00801-8. [DOI] [PubMed] [Google Scholar]
- Kim DH, Saetrom P, Snove O, Jr, Rossi JJ. MicroRNA-directed transcriptional gene silencing in mammalian cells. Proc Natl Acad Sci U S A. 2008;105:16230–16235. doi: 10.1073/pnas.0808830105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinali M, Arechavala-Gomeza V, Feng L, Cirak S, Hunt D, Adkin C, et al. Local restoration of dystrophin expression with the morpholino oligomer AVI-4658 in Duchenne muscular dystrophy: a single-blind, placebo-controlled, dose-escalation, proof-of-concept study. Lancet Neurol. 2009;8:918–928. doi: 10.1016/S1474-4422(09)70211-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiriakidou M, Tan GS, Lamprinaki S, De Planell-Saguer M, Nelson PT, Mourelatos Z. An mRNA m7G cap binding-like motif within human Ago2 represses translation. Cell. 2007;129:1141–1151. doi: 10.1016/j.cell.2007.05.016. [DOI] [PubMed] [Google Scholar]
- Klein U, Lia M, Crespo M, Siegel R, Shen Q, Mo T, et al. The DLEU2/miR-15a/16-1 cluster controls B cell proliferation and its deletion leads to chronic lymphocytic leukemia. Cancer Cell. 2010;17:28–40. doi: 10.1016/j.ccr.2009.11.019. [DOI] [PubMed] [Google Scholar]
- Kong W, Yang H, He L, Zhao JJ, Coppola D, Dalton WS, et al. MicroRNA-155 is regulated by the transforming growth factor beta/Smad pathway and contributes to epithelial cell plasticity by targeting RhoA. Mol Cell Biol. 2008;28:6773–6784. doi: 10.1128/MCB.00941-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong YW, Cannell IG, de Moor CH, Hill K, Garside PG, Hamilton TL, et al. The mechanism of micro-RNA-mediated translation repression is determined by the promoter of the target gene. Proc Natl Acad Sci U S A. 2008;105:8866–8871. doi: 10.1073/pnas.0800650105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koralov SB, Muljo SA, Galler GR, Krek A, Chakraborty T, Kanellopoulou C, et al. Dicer ablation affects antibody diversity and cell survival in the B lymphocyte lineage. Cell. 2008;132:860–874. doi: 10.1016/j.cell.2008.02.020. [DOI] [PubMed] [Google Scholar]
- Korpal M, Lee ES, Hu G, Kang Y. The miR-200 family inhibits epithelial-mesenchymal transition and cancer cell migration by direct targeting of E-cadherin transcriptional repressors ZEB1 and ZEB2. J Biol Chem. 2008;283:14910–14914. doi: 10.1074/jbc.C800074200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kota J, Chivukula RR, O’Donnell KA, Wentzel EA, Montgomery CL, Hwang HW, et al. Therapeutic microRNA delivery suppresses tumorigenesis in a murine liver cancer model. Cell. 2009;137:1005–1017. doi: 10.1016/j.cell.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovalchuk O, Filkowski J, Meservy J, Ilnytskyy Y, Tryndyak VP, Chekhun VF, et al. Involvement of microRNA-451 in resistance of the MCF-7 breast cancer cells to chemotherapeutic drug doxorubicin. Mol Cancer Ther. 2008;7:2152–2129. doi: 10.1158/1535-7163.MCT-08-0021. [DOI] [PubMed] [Google Scholar]
- Krek A, Grun D, Poy MN, Wolf R, Rosenberg L, Epstein EJ, et al. Combinatorial microRNA target predictions. Nat Genet. 2005;37:495–500. doi: 10.1038/ng1536. [DOI] [PubMed] [Google Scholar]
- Kriegel AJ, Fang Y, Liu Y, Tian Z, Mladinov D, Matus IR, et al. MicroRNA-target pairs in human renal epithelial cells treated with transforming growth factor beta 1: a novel role of miR-382. Nucleic Acids Res. 2010;38:8388–8347. doi: 10.1093/nar/gkq718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krutzfeldt J, Rajewsky N, Braich R, Rajeev KG, Tuschl T, Manoharan M, et al. Silencing of microRNAs in vivo with ‘antagomirs’. Nature. 2005;438:685–689. doi: 10.1038/nature04303. [DOI] [PubMed] [Google Scholar]
- Kumar M, Lu Z, Takwi AA, Chen W, Callander NS, Ramos KS, et al. Negative regulation of the tumor suppressor p53 gene by microRNAs. Oncogene. 2010 doi: 10.1038/onc.2010.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar MS, Lu J, Mercer KL, Golub TR, Jacks T. Impaired microRNA processing enhances cellular transformation and tumorigenesis. Nat Genet. 2007;39:673–677. doi: 10.1038/ng2003. [DOI] [PubMed] [Google Scholar]
- Lagos-Quintana M, Rauhut R, Lendeckel W, Tuschl T. Identification of novel genes coding for small expressed RNAs. Science. 2001;294:853–858. doi: 10.1126/science.1064921. [DOI] [PubMed] [Google Scholar]
- Lal A, Navarro F, Maher CA, Maliszewski LE, Yan N, O’Day E, et al. miR-24 Inhibits cell proliferation by targeting E2F2, MYC, and other cell-cycle genes via binding to “seedless” 3′UTR microRNA recognition elements. Mol Cell. 2009;35:610–625. doi: 10.1016/j.molcel.2009.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan FF, Wang H, Chen YC, Chan CY, Ng SS, Li K, et al. Hsa-let-7g inhibits proliferation of hepatocellular carcinoma cells by downregulation of c-Myc and upregulation of p16(INK4A) Int J Cancer. 2011;128:319–331. doi: 10.1002/ijc.25336. [DOI] [PubMed] [Google Scholar]
- Lanford RE, Hildebrandt-Eriksen ES, Petri A, Persson R, Lindow M, Munk ME, et al. Therapeutic silencing of microRNA-122 in primates with chronic hepatitis C virus infection. Science. 2010;327:198–201. doi: 10.1126/science.1178178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau NC, Lim LP, Weinstein EG, Bartel DP. An abundant class of tiny RNAs with probable regulatory roles in Caenorhabditis elegans. Science. 2001;294:858–862. doi: 10.1126/science.1065062. [DOI] [PubMed] [Google Scholar]
- le Sage C, Nagel R, Egan DA, Schrier M, Mesman E, Mangiola A, et al. Regulation of the p27(Kip1) tumor suppressor by miR-221 and miR-222 promotes cancer cell proliferation. EMBO J. 2007;26:3699–3708. doi: 10.1038/sj.emboj.7601790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le MT, Teh C, Shyh-Chang N, Xie H, Zhou B, Korzh V, et al. MicroRNA-125b is a novel negative regulator of p53. Genes Dev. 2009;23:862–876. doi: 10.1101/gad.1767609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KH, Lotterman C, Karikari C, Omura N, Feldmann G, Habbe N, et al. Epigenetic silencing of MicroRNA miR-107 regulates cyclin-dependent kinase 6 expression in pancreatic cancer. Pancreatology. 2009;9:293–301. doi: 10.1159/000186051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee RC, Ambros V. An extensive class of small RNAs in Caenorhabditis elegans. Science. 2001;294:862–864. doi: 10.1126/science.1065329. [DOI] [PubMed] [Google Scholar]
- Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75:843–854. doi: 10.1016/0092-8674(93)90529-y. [DOI] [PubMed] [Google Scholar]
- Lee Y, Ahn C, Han J, Choi H, Kim J, Yim J, et al. The nuclear RNase III Drosha initiates microRNA processing. Nature. 2003;425:419–419. doi: 10.1038/nature01957. [DOI] [PubMed] [Google Scholar]
- Lee Y, Hur I, Park SY, Kim YK, Suh MR, Kim VN. The role of PACT in the RNA silencing pathway. Embo J. 2006;25:522–535. doi: 10.1038/sj.emboj.7600942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y, Jeon K, Lee JT, Kim S, Kim VN. MicroRNA maturation: stepwise processing and subcellular localization. Embo J. 2002;21:4663–4670. doi: 10.1093/emboj/cdf476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y, Kim M, Han J, Yeom KH, Lee S, Baek SH, et al. MicroRNA genes are transcribed by RNA polymerase II. Embo J. 2004;23:4051–4060. doi: 10.1038/sj.emboj.7600385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee YS, Dutta A. The tumor suppressor microRNA let-7 represses the HMGA2 oncogene. Genes Dev. 2007;21:1025–1030. doi: 10.1101/gad.1540407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leucht C, Stigloher C, Wizenmann A, Klafke R, Folchert A, Bally-Cuif L. MicroRNA-9 directs late organizer activity of the midbrain-hindbrain boundary. Nat Neurosci. 2008;11:641–648. doi: 10.1038/nn.2115. [DOI] [PubMed] [Google Scholar]
- Levy C, Khaled M, Iliopoulos D, Janas MM, Schubert S, Pinner S, et al. Intronic miR-211 assumes the tumor suppressive function of its host gene in melanoma. Mol Cell. 2010;40:841–849. doi: 10.1016/j.molcel.2010.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis BP, Burge CB, Bartel DP. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell. 2005 Jan 14;120(1):15–20. doi: 10.1016/j.cell.2004.12.035. [DOI] [PubMed] [Google Scholar]
- Lewis BP, Shih IH, Jones-Rhoades MW, Bartel DP, Burge CB. Prediction of mammalian microRNA targets. Cell. 2003;115:787–798. doi: 10.1016/s0092-8674(03)01018-3. [DOI] [PubMed] [Google Scholar]
- Li N, Flynt AS, Kim HR, Solnica-Krezel L, Patton JG. Dispatched Homolog 2 is targeted by miR-214 through a combination of three weak microRNA recognition sites. Nucleic Acids Res. 2008;36:4277–4285. doi: 10.1093/nar/gkn388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Guessous F, Zhang Y, Dipierro C, Kefas B, Johnson E, et al. MicroRNA-34a inhibits glioblastoma growth by targeting multiple oncogenes. Cancer Res. 2009;69:7569–7576. doi: 10.1158/0008-5472.CAN-09-0529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Zhu X, Gu J, Hu H, Dong D, Yao J, et al. Anti-miR-21 oligonucleotide enhances chemosensitivity of leukemic HL60 cells to arabinosylcytosine by inducing apoptosis. Hematology. 2010;14:215–221. doi: 10.1179/102453310X12647083620840. [DOI] [PubMed] [Google Scholar]
- Liang Z, Wu H, Xia J, Li Y, Zhang Y, Huang K, et al. Involvement of miR-326 in chemotherapy resistance of breast cancer through modulating expression of multidrug resistance-associated protein 1. Biochem Pharmacol. 2010;79:817–824. doi: 10.1016/j.bcp.2009.10.017. [DOI] [PubMed] [Google Scholar]
- Liao JY, Ma LM, Guo YH, Zhang YC, Zhou H, Shao P, et al. Deep sequencing of human nuclear and cytoplasmic small RNAs reveals an unexpectedly complex subcellular distribution of miRNAs and tRNA 3′ trailers. PLoS One. 2010;5:e10563. doi: 10.1371/journal.pone.0010563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C, Kelnar K, Liu B, Chen X, Calhoun-Davis T, Li H, et al. The microRNA miR-34a inhibits prostate cancer stem cells and metastasis by directly repressing CD44. Nat Med. 2011;17:211–215. doi: 10.1038/nm.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Carmell MA, Rivas FV, Marsden CG, Thomson JM, Song JJ, et al. Argonaute2 is the catalytic engine of mammalian RNAi. Science. 2004;305:1437–1441. doi: 10.1126/science.1102513. [DOI] [PubMed] [Google Scholar]
- Liu J, Rivas FV, Wohlschlegel J, Yates JRI, Parker R, Hannon GJ. A role for the P-body component GW182 in microRNA function. Nat Cell Biol. 2005;7:1261–1266. doi: 10.1038/ncb1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Valencia-Sanchez MA, Hannon GJ, Parker R. MicroRNAdependent localization of targeted mRNAs to mammalian P-bodies. Nat Cell Biol. 2005;7:719–723. doi: 10.1038/ncb1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, Paroo Z. Biochemical principles of small RNA pathways. Annu Rev Biochem. 2010;79:295–319. doi: 10.1146/annurev.biochem.052208.151733. [DOI] [PubMed] [Google Scholar]
- Lu J, Getz G, Miska EA, Alvarez-Saavedra E, Lamb J, Peck D, et al. MicroRNA expression profiles classify human cancers. Nature. 2005;435:834–838. doi: 10.1038/nature03702. [DOI] [PubMed] [Google Scholar]
- Lujambio A, Ropero S, Ballestar E, Fraga MF, Cerrato C, Setien F, et al. Genetic unmasking of an epigenetically silenced microRNA in human cancer cells. Cancer Res. 2007;67:1424–1429. doi: 10.1158/0008-5472.CAN-06-4218. [DOI] [PubMed] [Google Scholar]
- Lund E, Guttinger S, Calado A, Dahlberg JE, Kutay U. Nuclear export of microRNA precursors. Science. 2004;303:95–98. doi: 10.1126/science.1090599. [DOI] [PubMed] [Google Scholar]
- Ma L, Reinhardt F, Pan E, Soutschek J, Bhat B, Marcusson EG, et al. Therapeutic silencing of miR-10b inhibits metastasis in a mouse mammary tumor model. Nat Biotechnol. 2010;28:341–347. doi: 10.1038/nbt.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L, Teruya-Feldstein J, Weinberg RA. Tumour invasion and metastasis initiated by microRNA-10b in breast cancer. Nature. 2007;449:682–688. doi: 10.1038/nature06174. [DOI] [PubMed] [Google Scholar]
- Ma L, Young J, Prabhala H, Pan E, Mestdagh P, Muth D, et al. miR-9, a MYC/MYCN-activated microRNA, regulates E-cadherin and cancer metastasis. Nat Cell Biol. 2010;12:247–256. doi: 10.1038/ncb2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma YL, Zhang P, Wang F, Moyer MP, Yang JJ, Liu ZH, et al. Human embryonic stem cells and metastatic colorectal cancer cells shared the common endogenous human microRNA-26b. J Cell Mol Med. 2010 doi: 10.1111/j.1582-4934.2010.01170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macrae IJ, Ma E, Zhou M, Robinson CV, Doudna JA. In vitro reconstitution of the human RISC-loading complex. Proc Natl Acad Sci U S A. 2008;105:512–517. doi: 10.1073/pnas.0710869105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maki N, Suetsugu-Maki R, Sano S, Nakamura K, Nishimura O, Tarui H, et al. Oocyte-type linker histone B4 is required for transdifferentiation of somatic cells in vivo. Faseb J. 2010;24:3462–3467. doi: 10.1096/fj.10-159285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maragkakis M, Alexiou P, Papadopoulos GL, Reczko M, Dalamagas T, Giannopoulos G, et al. Accurate microRNA target prediction correlates with protein repression levels. BMC Bioinformatics. 2009;10:295. doi: 10.1186/1471-2105-10-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maselli V, Di BD, Banfi S. CoGemiR: a comparative genomics microRNA database. BMC Genomics. 2008;9:457. doi: 10.1186/1471-2164-9-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuda H, Shi YB. An essential and evolutionarily conserved role of protein arginine methyltransferase 1 for adult intestinal stem cells during postembryonic development. Stem Cells. 2010;28:2073–2083. doi: 10.1002/stem.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayr C, Hemann MT, Bartel DP. Disrupting the pairing between let-7 and Hmga2 enhances oncogenic transformation. Science. 2007;315:1576–9. doi: 10.1126/science.1137999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClorey G, Moulton HM, Iversen PL, Fletcher S, Wilton SD. Antisense oligonucleotide-induced exon skipping restores dystrophin expression in vitro in a canine model of DMD. Gene Ther. 2006;13:1373–1381. doi: 10.1038/sj.gt.3302800. [DOI] [PubMed] [Google Scholar]
- Meister G, Landthaler M, Patkaniowska A, Dorsett Y, Teng G, Tuschl T. Human Argonaute2 mediates RNA cleavage targeted by miRNAs and siRNAs. Mol Cell. 2004;15:185–197. doi: 10.1016/j.molcel.2004.07.007. [DOI] [PubMed] [Google Scholar]
- Meng F, Henson R, Lang M, Wehbe H, Maheshwari S, Mendell JT, et al. Involvement of human micro-RNA in growth and response to chemotherapy in human cholangiocarcinoma cell lines. Gastroenterology. 2006;130:2113–2129. doi: 10.1053/j.gastro.2006.02.057. [DOI] [PubMed] [Google Scholar]
- Merlo LM, Pepper JW, Reid BJ, Maley CC. Cancer as an evolutionary and ecological process. Nat Rev Cancer. 2006;6:924–935. doi: 10.1038/nrc2013. [DOI] [PubMed] [Google Scholar]
- Mestdagh P, Bostrom AK, Impens F, Fredlund E, Van PG, De AP, et al. The miR-17-92 microRNA cluster regulates multiple components of the TGF-beta pathway in neuroblastoma. Mol Cell. 2010;40:762–773. doi: 10.1016/j.molcel.2010.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Migliazza A, Bosch F, Komatsu H, Cayanis E, Martinotti S, Toniato E, et al. Nucleotide sequence, transcription map, and mutation analysis of the 13q14 chromosomal region deleted in B-cell chronic lymphocytic leukemia. Blood. 2001;97:2098–2104. doi: 10.1182/blood.v97.7.2098. [DOI] [PubMed] [Google Scholar]
- Miller TE, Ghoshal K, Ramaswamy B, Roy S, Datta J, Shapiro CL, et al. MicroRNA-221/222 confers tamoxifen resistance in breast cancer by targeting p27Kip1. J Biol Chem. 2008;283:29897–29903. doi: 10.1074/jbc.M804612200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda KC, Huynh T, Tay Y, Ang YS, Tam WL, Thomson AM, et al. A pattern-based method for the identification of MicroRNA binding sites and their corresponding heteroduplexes. Cell. 2006;126:1203–1217. doi: 10.1016/j.cell.2006.07.031. [DOI] [PubMed] [Google Scholar]
- Mongroo PS, Rustgi AK. The role of the miR-200 family in epithelialmesenchymal transition. Cancer Biol Ther. 2010;10:219–222. doi: 10.4161/cbt.10.6312548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montini E, Cesana D, Schmidt M, Sanvito F, Bartholomae CC, Ranzani M, et al. The genotoxic potential of retroviral vectors is strongly modulated by vector design and integration site selection in a mouse model of HSC gene therapy. J Clin Invest. 2009;119:964–975. doi: 10.1172/JCI37630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montini E, Cesana D, Schmidt M, Sanvito F, Ponzoni M, Bartholomae C, et al. Hematopoietic stem cell gene transfer in a tumor-prone mouse model uncovers low genotoxicity of lentiviral vector integration. Nat Biotechnol. 2006;24:687–696. doi: 10.1038/nbt1216. [DOI] [PubMed] [Google Scholar]
- Morcos PA, Li Y, Jiang S. Vivo-Morpholinos: a non-peptide transporter delivers Morpholinos into a wide array of mouse tissues. Biotechniques. 2008;45:613–618. doi: 10.2144/000113005. [DOI] [PubMed] [Google Scholar]
- Morrisey EE. The magic and mystery of miR-21. J Clin Invest. 2010;120:3817–3819. doi: 10.1172/JCI44596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mott JL, Kobayashi S, Bronk SF, Gores GJ. mir-29 regulates Mcl-1 protein expression and apoptosis. Oncogene. 2007;26:6133–6140. doi: 10.1038/sj.onc.1210436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulton HM, Moulton JD. Morpholinos and their peptide conjugates: therapeutic promise and challenge for Duchenne muscular dystrophy. Biochim Biophys Acta. 2010;1798:2296–2303. doi: 10.1016/j.bbamem.2010.02.012. [DOI] [PubMed] [Google Scholar]
- Mourelatos Z, Dostie J, Paushkin S, Sharma A, Charroux B, Abel L, et al. miRNPs: a novel class of ribonucleoproteins containing numerous microRNAs. Genes Dev. 2002;16:720–728. doi: 10.1101/gad.974702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mu P, Han YC, Betel D, Yao E, Squatrito M, Ogrodowski P, et al. Genetic dissection of the miR-17~92 cluster of microRNAs in Myc-induced B-cell lymphomas. Genes Dev. 2009;23:2806–2811. doi: 10.1101/gad.1872909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasser MW, Datta J, Nuovo G, Kutay H, Motiwala T, Majumder S, et al. Down-regulation of micro-RNA-1 (miR-1) in lung cancer. Suppression of tumorigenic property of lung cancer cells and their sensitization to doxorubicin-induced apoptosis by miR-1. J Biol Chem. 2008;283:33394–33405. doi: 10.1074/jbc.M804788200. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Nayak S, Herzog RW. Progress and prospects: immune responses to viral vectors. Gene Ther. 2010;17:295–304. doi: 10.1038/gt.2009.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neveu P, Kye MJ, Qi S, Buchholz DE, Clegg DO, Sahin M, et al. MicroRNA profiling reveals two distinct p53-related human pluripotent stem cell states. Cell Stem Cell. 2010;7:671–681. doi: 10.1016/j.stem.2010.11.012. [DOI] [PubMed] [Google Scholar]
- Noonan EJ, Place RF, Pookot D, Basak S, Whitson JM, Hirata H, et al. miR-449a targets HDAC-1 and induces growth arrest in prostate cancer. Oncogene. 2009;28:1714–1724. doi: 10.1038/onc.2009.19. [DOI] [PubMed] [Google Scholar]
- O’Connell RM, Chaudhuri AA, Rao DS, Gibson WS, Balazs AB, Baltimore D. MicroRNAs enriched in hematopoietic stem cells differentially regulate long-term hematopoietic output. Proc Natl Acad Sci U S A. 2010;107:14235–14240. doi: 10.1073/pnas.1009798107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Day E, Lal A. MicroRNAs and their target gene networks in breast cancer. Breast Cancer Res. 2010;12:201. doi: 10.1186/bcr2484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell KA, Wentzel EA, Zeller KI, Dang CV, Mendell JT. c-Myc-regulated microRNAs modulate E2F1 expression. Nature. 2005;435:839–843. doi: 10.1038/nature03677. [DOI] [PubMed] [Google Scholar]
- Okamura K, Hagen JW, Duan H, Tyler DM, Lai EC. The mirtron pathway generates microRNA-class regulatory RNAs in Drosophila. Cell. 2007;130:89–100. doi: 10.1016/j.cell.2007.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olive V, Bennett MJ, Walker JC, Ma C, Jiang I, Cordon-Cardo C, et al. miR-19 is a key oncogenic component of mir-17-92. Genes Dev. 2009;23:2839–2849. doi: 10.1101/gad.1861409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ota A, Tagawa H, Karnan S, Tsuzuki S, Karpas A, Kira S, et al. Identification and characterization of a novel gene, C13orf25, as a target for 13q31-q32 amplification in malignant lymphoma. Cancer Res. 2004;64:3087–3095. doi: 10.1158/0008-5472.can-03-3773. [DOI] [PubMed] [Google Scholar]
- Papagiannakopoulos T, Shapiro A, Kosik KS. MicroRNA-21 targets a network of key tumor-suppressive pathways in glioblastoma cells. Cancer Res. 2008;68:8164–8172. doi: 10.1158/0008-5472.CAN-08-1305. [DOI] [PubMed] [Google Scholar]
- Park SM, Gaur AB, Lengyel E, Peter ME. The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev. 2008;22:894–907. doi: 10.1101/gad.1640608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paroo Z, Liu Q, Wang X. Biochemical mechanisms of the RNA-induced silencing complex. Cell Res. 2007;17:187–194. doi: 10.1038/sj.cr.7310148. [DOI] [PubMed] [Google Scholar]
- Parra MK, Gee S, Mohandas N, Conboy JG. Efficient in vivo manipulation of alternative pre-mRNA splicing events using antisense morpholinos in mice. J Biol Chem. 2010 doi: 10.1074/jbc.M110.158154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick DM, Montgomery RL, Qi X, Obad S, Kauppinen S, Hill JA, et al. Stress-dependent cardiac remodeling occurs in the absence of microRNA-21 in mice. J Clin Invest. 2010;120:3912–3916. doi: 10.1172/JCI43604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekarsky Y, Santanam U, Cimmino A, Palamarchuk A, Efanov A, Maximov V, et al. Tcl1 expression in chronic lymphocytic leukemia is regulated by miR-29 and miR-181. Cancer Res. 2006;66:11590–11593. doi: 10.1158/0008-5472.CAN-06-3613. [DOI] [PubMed] [Google Scholar]
- Petrocca F, Visone R, Onelli MR, Shah MH, Nicoloso MS, de MI, et al. E2F1-regulated microRNAs impair TGFbeta-dependent cell-cycle arrest and apoptosis in gastric cancer. Cancer Cell. 2008;13:272–286. doi: 10.1016/j.ccr.2008.02.013. [DOI] [PubMed] [Google Scholar]
- Pichiorri F, Suh SS, Rocci A, De LL, Taccioli C, Santhanam R, et al. Downregulation of p53-inducible microRNAs 192, 194, and 215 impairs the p53/MDM2 autoregulatory loop in multiple myeloma development. Cancer Cell. 2010;18:367–381. doi: 10.1016/j.ccr.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Pillai RS, Bhattacharyya SN, Artus CG, Zoller T, Cougot N, Basyuk E, et al. Inhibition of translational initiation by Let-7 MicroRNA in human cells. Science. 2005;309:1573–1576. doi: 10.1126/science.1115079. [DOI] [PubMed] [Google Scholar]
- Place RF, Li LC, Pookot D, Noonan EJ, Dahiya R. MicroRNA-373 induces expression of genes with complementary promoter sequences. Proc Natl Acad Sci U S A. 2008;105:1608–1613. doi: 10.1073/pnas.0707594105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rana TM. Illuminating the silence: understanding the structure and function of small RNAs. Nat Rev Mol Cell Biol. 2007;8:23–36. doi: 10.1038/nrm2085. [DOI] [PubMed] [Google Scholar]
- Ratner E, Lu L, Boeke M, Barnett R, Nallur S, Chin LJ, et al. A KRAS-variant in ovarian cancer acts as a genetic marker of cancer risk. Cancer Res. 2010;70:6509–6515. doi: 10.1158/0008-5472.CAN-10-0689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauhala HE, Jalava SE, Isotalo J, Bracken H, Lehmusvaara S, Tammela TL, et al. miR-193b is an epigenetically regulated putative tumor suppressor in prostate cancer. Int J Cancer. 2010;127:1363–1372. doi: 10.1002/ijc.25162. [DOI] [PubMed] [Google Scholar]
- Raver-Shapira N, Marciano E, Meiri E, Spector Y, Rosenfeld N, Moskovits N, et al. Transcriptional activation of miR-34a contributes to p53-mediated apoptosis. Mol Cell. 2007;26:731–743. doi: 10.1016/j.molcel.2007.05.017. [DOI] [PubMed] [Google Scholar]
- Reinhart BJ, Slack FJ, Basson M, Pasquinelli AE, Bettinger JC, Rougvie AE, et al. The 21-nucleotide let-7 RNA regulates developmental timing in Caenorhabditis elegans. Nature. 2000;403:901–906. doi: 10.1038/35002607. [DOI] [PubMed] [Google Scholar]
- Roccaro AM, Sacco A, Thompson B, Leleu X, Azab AK, Azab F, et al. MicroRNAs 15a and 16 regulate tumor proliferation in multiple myeloma. Blood. 2009;113:6669–6680. doi: 10.1182/blood-2009-01-198408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruby JG, Jan CH, Bartel DP. Intronic microRNA precursors that bypass Drosha processing. Nature. 2007;448:83–86. doi: 10.1038/nature05983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachdeva M, Zhu S, Wu F, Wu H, Walia V, Kumar S, et al. p53 represses c-Myc through induction of the tumor suppressor miR-145. Proc Natl Acad Sci U S A. 2009;106:3207–3212. doi: 10.1073/pnas.0808042106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito Y, Liang G, Egger G, Friedman JM, Chuang JC, Coetzee GA, et al. Specific activation of microRNA-127 with downregulation of the proto-oncogene BCL6 by chromatin-modifying drugs in human cancer cells. Cancer Cell. 2006;9:435–443. doi: 10.1016/j.ccr.2006.04.020. [DOI] [PubMed] [Google Scholar]
- Sayed D, Rane S, Lypowy J, He M, Chen IY, Vashistha H, et al. MicroRNA-21 targets Sprouty2 and promotes cellular outgrowths. Mol Biol Cell. 2008;19:3272–82. doi: 10.1091/mbc.E08-02-0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz DS, Hutvagner G, Du T, Xu Z, Aronin N, Zamore PD. Asymmetry in the assembly of the RNAi enzyme complex. Cell. 2003;115:199–208. doi: 10.1016/s0092-8674(03)00759-1. [DOI] [PubMed] [Google Scholar]
- Scott GK, Mattie MD, Berger CE, Benz SC, Benz CC. Rapid alteration of microRNA levels by histone deacetylase inhibition. Cancer Res. 2006;66:1277–1281. doi: 10.1158/0008-5472.CAN-05-3632. [DOI] [PubMed] [Google Scholar]
- Selbach M, Schwanhausser B, Thierfelder N, Fang Z, Khanin R, Rajewsky N. Widespread changes in protein synthesis induced by microRNAs. Nature. 2008;455:58–63. doi: 10.1038/nature07228. [DOI] [PubMed] [Google Scholar]
- Selcuklu SD, Donoghue MT, Spillane C. miR-21 as a key regulator of oncogenic processes. Biochem Soc Trans. 2009;37:918–925. doi: 10.1042/BST0370918. [DOI] [PubMed] [Google Scholar]
- Sethupathy P, Corda B, Hatzigeorgiou AG. TarBase: A comprehensive database of experimentally supported animal microRNA targets. RNA. 2006;12:192–197. doi: 10.1261/rna.2239606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi XB, Xue L, Ma AH, Tepper CG, Kung HJ, White RW. miR-125b promotes growth of prostate cancer xenograft tumor through targeting pro-apoptotic genes. Prostate. 2011;71:538–549. doi: 10.1002/pros.21270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin C, Nam JW, Farh KK, Chiang HR, Shkumatava A, Bartel DP. Expanding the microRNA targeting code: functional sites with centered pairing. Mol Cell. 2010;38:789–802. doi: 10.1016/j.molcel.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin KH, Bae SD, Hong HS, Kim RH, Kang MK, Park NH. miR- 181a shows tumor suppressive effect against oral squamous cell carcinoma cells by downregulating K-ras. Biochem Biophys Res Commun. 2010 doi: 10.1016/j.bbrc.2010.12.055. [DOI] [PubMed] [Google Scholar]
- Shpyleva SI, Tryndyak VP, Kovalchuk O, Starlard-Davenport A, Chekhun VF, Beland FA, et al. Role of ferritin alterations in human breast cancer cells. Breast Cancer Res Treat. 2010 doi: 10.1007/s10549-010-0849-4. [DOI] [PubMed] [Google Scholar]
- Sinkkonen L, Hugenschmidt T, Berninger P, Gaidatzis D, Mohn F, Artus-Revel CG, et al. MicroRNAs control de novo DNA methylation through regulation of transcriptional repressors in mouse embryonic stem cells. Nat Struct Mol Biol. 2008;15:259–267. doi: 10.1038/nsmb.1391. [DOI] [PubMed] [Google Scholar]
- Slack FJ, Basson M, Liu Z, Ambros V, Horvitz HR, Ruvkun G. The lin- 41 RBCC gene acts in the C. elegans heterochronic pathway between the let-7 regulatory RNA and the LIN-29 transcription factor. Mol Cell. 2000;5:659–669. doi: 10.1016/s1097-2765(00)80245-2. [DOI] [PubMed] [Google Scholar]
- Sotillo E, Laver T, Mellert H, Schelter JM, Cleary MA, McMahon S, et al. Myc overexpression brings out unexpected antiapoptotic effects of miR-34a. Oncogene. 2011 doi: 10.1038/onc.2010.634. onc2010634 [pii]; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starczynowski DT, Kuchenbauer F, Wegrzyn J, Rouhi A, Petriv O, Hansen CL, et al. MicroRNA-146a disrupts hematopoietic differentiation and survival. Exp Hematol. 2010 doi: 10.1016/j.exphem.2010.09.011. [DOI] [PubMed] [Google Scholar]
- Stark A, Brennecke J, Russell RB, Cohen SM. Identification of Drosophila MicroRNA targets. PLoS Biol. 2003;1:E60. doi: 10.1371/journal.pbio.0000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su H, Yang JR, Xu T, Huang J, Xu L, Yuan Y, et al. MicroRNA-101, down-regulated in hepatocellular carcinoma, promotes apoptosis and suppresses tumorigenicity. Cancer Res. 2009;69:1145–42. doi: 10.1158/0008-5472.CAN-08-2886. [DOI] [PubMed] [Google Scholar]
- Summerton J. Morpholino antisense oligomers: the case for an RNase H-independent structural type. Biochim Biophys Acta. 1999;1489:141–158. doi: 10.1016/s0167-4781(99)00150-5. [DOI] [PubMed] [Google Scholar]
- Sun F, Fu H, Liu Q, Tie Y, Zhu J, Xing R, et al. Downregulation of CCND1 and CDK6 by miR-34a induces cell cycle arrest. FEBS Lett. 2008;582:1564–1568. doi: 10.1016/j.febslet.2008.03.057. [DOI] [PubMed] [Google Scholar]
- Suzuki H, Yamamoto E, Nojima M, Kai M, Yamano HO, Yoshikawa K, et al. Methylation-associated silencing of microRNA-34b/c in gastric cancer and its involvement in an epigenetic field defect. Carcinogenesis. 2010;31:2066–2073. doi: 10.1093/carcin/bgq203. [DOI] [PubMed] [Google Scholar]
- Sylvestre Y, De GV, Querido E, Mukhopadhyay UK, Bourdeau V, Major F, et al. An E2F/miR-20a autoregulatory feedback loop. J Biol Chem. 2007;282:2135–2143. doi: 10.1074/jbc.M608939200. [DOI] [PubMed] [Google Scholar]
- Tarasov V, Jung P, Verdoodt B, Lodygin D, Epanchintsev A, Menssen A, et al. Differential regulation of microRNAs by p53 revealed by massively parallel sequencing: miR-34a is a p53 target that induces apoptosis and G1-arrest. Cell Cycle. 2007;6:1586–1593. doi: 10.4161/cc.6.13.4436. [DOI] [PubMed] [Google Scholar]
- Tavazoie SF, Alarcon C, Oskarsson T, Padua D, Wang Q, Bos PD, et al. Endogenous human microRNAs that suppress breast cancer metastasis. Nature. 2008;451:147–152. doi: 10.1038/nature06487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tay Y, Zhang J, Thomson AM, Lim B, Rigoutsos I. MicroRNAs to Nanog, Oct4 and Sox2 coding regions modulate embryonic stem cell differentiation. Nature. 2008;455:1124–1128. doi: 10.1038/nature07299. [DOI] [PubMed] [Google Scholar]
- Taylor MF, Paulauskis JD, Weller DD, Kobzik L. In vitro efficacy of morpholino-modified antisense oligomers directed against tumor necrosis factor-alpha mRNA. J Biol Chem. 1996;271:17445–17452. doi: 10.1074/jbc.271.29.17445. [DOI] [PubMed] [Google Scholar]
- Thiery JP. Epithelial-mesenchymal transitions in development and pathologies. Curr Opin Cell Biol. 2003 Dec;15(6):740–746. doi: 10.1016/j.ceb.2003.10.006. [DOI] [PubMed] [Google Scholar]
- Thum T, Gross C, Fiedler J, Fischer T, Kissler S, Bussen M, et al. MicroRNA-21 contributes to myocardial disease by stimulating MAP kinase signalling in fibroblasts. Nature. 2008;456:980–984. doi: 10.1038/nature07511. [DOI] [PubMed] [Google Scholar]
- Trang P, Medina PP, Wiggins JF, Ruffino L, Kelnar K, Omotola M, et al. Regression of murine lung tumors by the let-7 microRNA. Oncogene. 2010;29:1580–1587. doi: 10.1038/onc.2009.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang WP, Kwok TT. Let-7a microRNA suppresses therapeutics-induced cancer cell death by targeting caspase-3. Apoptosis. 2008;13:1215–1222. doi: 10.1007/s10495-008-0256-z. [DOI] [PubMed] [Google Scholar]
- Tuddenham L, Wheeler G, Ntounia-Fousara S, Waters J, Hajihosseini MK, Clark I, et al. The cartilage specific microRNA-140 targets histone deacetylase 4 in mouse cells. FEBS Lett. 2006;580:4214–4217. doi: 10.1016/j.febslet.2006.06.080. [DOI] [PubMed] [Google Scholar]
- Valastyan S, Reinhardt F, Benaich N, Calogrias D, Szasz AM, Wang ZC, et al. A pleiotropically acting microRNA, miR-31, inhibits breast cancer metastasis. Cell. 2009;12:1032–1046. doi: 10.1016/j.cell.2009.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Valeri N, Gasparini P, Braconi C, Paone A, Lovat F, Fabbri M, et al. MicroRNA-21 induces resistance to 5-fluorouracil by down-regulating human DNA MutS homolog 2 (hMSH2) Proc Natl Acad Sci U S A. 2010;107:21098–21103. doi: 10.1073/pnas.1015541107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma IM, Weitzman MD. Gene therapy: twenty-first century medicine. Annu Rev Biochem. 2005;74:711–738. doi: 10.1146/annurev.biochem.74.050304.091637. [DOI] [PubMed] [Google Scholar]
- Vogel F. Genetics of retinoblastoma. Hum Genet. 1979;52:1–54. doi: 10.1007/BF00284597. [DOI] [PubMed] [Google Scholar]
- Volinia S, Calin GA, Liu CG, Ambs S, Cimmino A, Petrocca F, et al. A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci U S A. 2006;103:2257–2256. doi: 10.1073/pnas.0510565103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrba L, Jensen TJ, Garbe JC, Heimark RL, Cress AE, Dickinson S, et al. Role for DNA methylation in the regulation of miR-200c and miR-141 expression in normal and cancer cells. PLoS One. 2010;5:e8697. doi: 10.1371/journal.pone.0008697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B, Herman-Edelstein M, Koh P, Burns W, Jandeleit-Dahm K, Watson A, et al. E-cadherin expression is regulated by miR-192/215 by a mechanism that is independent of the profibrotic effects of transforming growth factor-beta. Diabetes. 2010;59:1794–1802. doi: 10.2337/db09-1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B, Hsu SH, Majumder S, Kutay H, Huang W, Jacob ST, et al. TGFbeta-mediated upregulation of hepatic miR-181b promotes hepatocarcinogenesis by targeting TIMP3. Oncogene. 2009;29:1787–1797. doi: 10.1038/onc.2009.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Li Y, Ahmad A, Azmi AS, Kong D, Banerjee S, et al. Targeting miRNAs involved in cancer stem cell and EMT regulation: An emerging concept in overcoming drug resistance. Drug Resist Updat. 2010;13:109–118. doi: 10.1016/j.drup.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch C, Chen Y, Stallings RL. MicroRNA-34a functions as a potential tumor suppressor by inducing apoptosis in neuroblastoma cells. Oncogene. 2007;26:5017–5022. doi: 10.1038/sj.onc.1210293. [DOI] [PubMed] [Google Scholar]
- Wienholds E, Koudijs MJ, van Eeden FJ, Cuppen E, Plasterk RH. The microRNA-producing enzyme Dicer1 is essential for zebrafish development. Nat Genet. 2003;35:217–218. doi: 10.1038/ng1251. [DOI] [PubMed] [Google Scholar]
- Wiggins JF, Ruffino L, Kelnar K, Omotola M, Patrawala L, Brown D, et al. Development of a lung cancer therapeutic based on the tumor suppressor microRNA-34. Cancer Res. 2010;70:5923–5930. doi: 10.1158/0008-5472.CAN-10-0655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wightman B, Ha I, Ruvkun G. Posttranscriptional regulation of the heterochronic gene lin-14 by lin-4 mediates temporal pattern formation in C. elegans. Cell. 1993;75:855–862. doi: 10.1016/0092-8674(93)90530-4. [DOI] [PubMed] [Google Scholar]
- Wiklund ED, Bramsen JB, Hulf T, Dyrskjot L, Ramanathan R, Hansen TB, et al. Coordinated epigenetic repression of the miR-200 family and miR-205 in invasive bladder cancer. Int J Cancer. 2010 doi: 10.1002/ijc.25461. [DOI] [PubMed] [Google Scholar]
- Wilting SM, van Boerdonk RA, Henken FE, Meijer CJ, Diosdado B, Meijer GA, et al. Methylation-mediated silencing and tumour suppressive function of hsa-miR-124 in cervical cancer. Mol Cancer. 2010;9:167. doi: 10.1186/1476-4598-9-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu H, Zhu S, Mo YY. Suppression of cell growth and invasion by miR-205 in breast cancer. Cell Res. 2009;19:439–448. doi: 10.1038/cr.2009.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L, Belasco JG. Micro-RNA regulation of the mammalian lin-28 gene during neuronal differentiation of embryonal carcinoma cells. Mol Cell Biol. 2005;25:9198–9208. doi: 10.1128/MCB.25.21.9198-9208.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia L, Zhang D, Du R, Pan Y, Zhao L, Sun S, et al. miR-15b and miR-16 modulate multidrug resistance by targeting BCL2 in human gastric cancer cells. Int J Cancer. 2008;123:372–379. doi: 10.1002/ijc.23501. [DOI] [PubMed] [Google Scholar]
- Xiao C, Srinivasan L, Calado DP, Patterson HC, Zhang B, Wang J, et al. Lymphoproliferative disease and autoimmunity in mice with increased miR-17-92 expression in lymphocytes. Nat Immunol. 2008;9:405–414. doi: 10.1038/ni1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao F, Zuo Z, Cai G, Kang S, Gao X, Li T. miRecords: an integrated resource for microRNA-target interactions. Nucleic Acids Res. 2009;37:105–110. doi: 10.1093/nar/gkn851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong Y, Fang JH, Yun JP, Yang J, Zhang Y, Jia WH, et al. Effects of microRNA-29 on apoptosis, tumorigenicity, and prognosis of hepatocellular carcinoma. Hepatology. 2010;51:836–845. doi: 10.1002/hep.23380. [DOI] [PubMed] [Google Scholar]
- Xu H, Cheung IY, Guo HF, Cheung NK. MicroRNA miR-29 modulates expression of immunoinhibitory molecule B7-H3: potential implications for immune based therapy of human solid tumors. Cancer Res. 2009;69:6275–6281. doi: 10.1158/0008-5472.CAN-08-4517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamakuchi M, Ferlito M, Lowenstein CJ. miR-34a repression of SIRT1 regulates apoptosis. Proc Natl Acad Sci U S A. 2008;105:13421–13426. doi: 10.1073/pnas.0801613105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan LX, Huang XF, Shao Q, Huang MY, Deng L, Wu QL, et al. MicroRNA miR-21 overexpression in human breast cancer is associated with advanced clinical stage, lymph node metastasis and patient poor prognosis. RNA. 2008;14:2348–2360. doi: 10.1261/rna.1034808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Kong W, He L, Zhao JJ, O’Donnell JD, Wang J, et al. MicroRNA expression profiling in human ovarian cancer: miR-214 induces cell survival and cisplatin resistance by targeting PTEN. Cancer Res. 2006;68:425–433. doi: 10.1158/0008-5472.CAN-07-2488. [DOI] [PubMed] [Google Scholar]
- Yang J, Mani SA, Donaher JL, Ramaswamy S, Itzykson RA, Come C, et al. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell. 2004;117:927–939. doi: 10.1016/j.cell.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Yang JH, Li JH, Shao P, Zhou H, Chen YQ, Qu LH. starBase: a database for exploring microRNA-mRNA interaction maps from Argonaute CLIP-Seq and Degradome-Seq data. Nucleic Acids Res. 2010;39:202–209. doi: 10.1093/nar/gkq1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang JH, Shao P, Zhou H, Chen YQ, Qu LH. deepBase: a database for deeply annotating and mining deep sequencing data. Nucleic Acids Res. 2010;38:123–130. doi: 10.1093/nar/gkp943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang N, Kaur S, Volinia S, Greshock J, Lassus H, Hasegawa K, et al. MicroRNA microarray identifies Let-7i as a novel biomarker and therapeutic target in human epithelial ovarian cancer. Cancer Res. 2008;68:10307–10314. doi: 10.1158/0008-5472.CAN-08-1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yekta S, Shih IH, Bartel DP. MicroRNA-directed cleavage of HOXB8 mRNA. Science. 2004;304:594–596. doi: 10.1126/science.1097434. [DOI] [PubMed] [Google Scholar]
- Yi R, Qin Y, Macara IG, Cullen BR. Exportin-5 mediates the nuclear export of pre-microRNAs and short hairpin RNAs. Genes Dev. 2003;17:3011–3013. doi: 10.1101/gad.1158803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yilmaz M, Christofori G. Mechanisms of motility in metastasizing cells. Mol Cancer Res. 2010;8:629–642. doi: 10.1158/1541-7786.MCR-10-0139. [DOI] [PubMed] [Google Scholar]
- Yu D, Carroll M, Thomas-Tikhonenko A. p53 status dictates responses of B lymphomas to monotherapy with proteasome inhibitors. Blood. 2007;109:4936–4943. doi: 10.1182/blood-2006-10-050294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zavadil J, Narasimhan M, Blumenberg M, Schneider RJ. Transforming growth factor-beta and microRNA:mRNA regulatory networks in epithelial plasticity. Cells Tissues Organs. 2007;185:157–161. doi: 10.1159/000101316. [DOI] [PubMed] [Google Scholar]
- Zeng L, Carter AD, Childs SJ. miR-145 directs intestinal maturation in zebrafish. Proc Natl Acad Sci U S A. 2009;106:17993–17998. doi: 10.1073/pnas.0903693106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Y, Wagner EJ, Cullen BR. Both natural and designed micro RNAs can inhibit the expression of cognate mRNAs when expressed in human cells. Mol Cell. 2002;9:1327–1333. doi: 10.1016/s1097-2765(02)00541-5. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Cristofaro P, Silbermann R, Pusch O, Boden D, Konkin T, et al. Engineering mucosal RNA interference in vivo. Mol Ther. 2006;14:336–342. doi: 10.1016/j.ymthe.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Zhao JJ, Lin J, Yang H, Kong W, He L, Ma X, et al. MicroRNA-221/222 negatively regulates estrogen receptor alpha and is associated with tamoxifen resistance in breast cancer. J Biol Chem. 2008;283:31079–31086. doi: 10.1074/jbc.M806041200. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Zhao X, Yang L, Hu J, Ruan J. miR-138 might reverse multidrug resistance of leukemia cells. Leuk Res. 2010;34:1078–1082. doi: 10.1016/j.leukres.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Zhou BP, Deng J, Xia W, Xu J, Li YM, Gunduz M, et al. Dual regulation of Snail by GSK-3beta-mediated phosphorylation in control of epithelialmesenchymal transition. Nat Cell Biol. 2004;6:931–940. doi: 10.1038/ncb1173. [DOI] [PubMed] [Google Scholar]
- Zhu H, Wu H, Liu X, Evans BR, Medina DJ, Liu CG, et al. Role of MicroRNA miR-27a and miR-451 in the regulation of MDR1/P-glycoprotein expression in human cancer cells. Biochem Pharmacol. 2008;76:582–588. doi: 10.1016/j.bcp.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S, Wu H, Wu F, Nie D, Sheng S, Mo YY. MicroRNA-21 targets tumor suppressor genes in invasion and metastasis. Cell Res. 2008;18:350–359. doi: 10.1038/cr.2008.24. [DOI] [PubMed] [Google Scholar]