Abstract
Objective:
To investigate the interrelations of serum vitamin B12 markers with brain volumes, cerebral infarcts, and performance in different cognitive domains in a biracial population sample cross-sectionally.
Methods:
In 121 community-dwelling participants of the Chicago Health and Aging Project, serum markers of vitamin B12 status were related to summary measures of neuropsychological tests of 5 cognitive domains and brain MRI measures obtained on average 4.6 years later among 121 older adults.
Results:
Concentrations of all vitamin B12–related markers, but not serum vitamin B12 itself, were associated with global cognitive function and with total brain volume. Methylmalonate levels were associated with poorer episodic memory and perceptual speed, and cystathionine and 2-methylcitrate with poorer episodic and semantic memory. Homocysteine concentrations were associated with decreased total brain volume. The homocysteine-global cognition effect was modified and no longer statistically significant with adjustment for white matter volume or cerebral infarcts. The methylmalonate-global cognition effect was modified and no longer significant with adjustment for total brain volume.
Conclusions:
Methylmalonate, a specific marker of B12 deficiency, may affect cognition by reducing total brain volume whereas the effect of homocysteine (nonspecific to vitamin B12 deficiency) on cognitive performance may be mediated through increased white matter hyperintensity and cerebral infarcts. Vitamin B12 status may affect the brain through multiple mechanisms.
White matter hyperintensity volume (WMHV), cerebral infarcts, and total brain volume (TBV) have been related to performance in multiple cognitive domains1–4 but few reports exist in which both cognitive performance and structural brain abnormalities are examined in the context of vitamin B12 status.5,6 To date, no study has investigated these relations with vitamin B12 status among nonwhites or in populations with folic acid fortification policies such as in the United States.
In our ongoing study of the risk factors for cognitive disorders in a biracial community, the Chicago Health and Aging Project (CHAP), we reported that brain MRI measures were associated with cognitive performance, especially perceptual speed in both blacks and whites.1 Moreover, we found that serum vitamin B12 and methylmalonic acid (MMA) concentrations were associated with 6-year cognitive decline.7 However, neither performance in specific cognitive domains nor brain MRI measures were examined in relation to vitamin B12–related markers in these reports. Thus, our primary objective in this study was to examine the relations of circulating levels of vitamin B12 and related metabolites to WMHV, cerebral infarcts, and TBV among black and white CHAP participants. We sought to investigate whether these vitamin B12– related markers were associated with test scores of individual cognitive domains and whether cognitive effects associated with these vitamin B12–related metabolites, if observed, were independent of brain measures.
METHODS
Study population.
Study subjects were participants in CHAP, an ongoing, geographically defined cohort of older residents 65 years and older on the south side of Chicago. A total of 6,158 participated in the initial cycle of baseline interviews during 1993–1996 (79% participation overall; 81% among blacks, 75% among whites). In-home interviews are conducted in 3-year cycles on all participants. Stratified random samples of participants are drawn at each cycle for clinical evaluation of dementia that included neuropsychological testing, neurologic examination, and laboratory tests.8 MRI was requested of all clinically evaluated persons in cycles 3, 4, and 5. The Institutional Review Board of Rush University Medical Center approved the study; all participants gave written informed consent.
Blood drawn at each clinical evaluation cycle is routinely analyzed for measurement of serum vitamin B12 levels. In addition, we analyzed several vitamin B12 markers, including homocysteine, MMA, and other related metabolites—cystathionine, and 2-methylcitrate in stored blood of participants.
This report describes analyses relating serum vitamin B12 and B12-related metabolites to cognitive performance at cycle 2. A total of 842 persons were clinically evaluated in cycle 2. Only 682 had stored serum available for biochemical analyses of vitamin B12 markers and related metabolites, of which only 121 had MRI scans on average 4.6 years later.
Clinical assessment and cognitive measures.
Cycle 2 clinical evaluations were conducted between 1996 and 1999 in subjects' homes by a team of a neurologist, nurse clinician, neuropsychological technician, and a phlebotomist. Neuropsychological testing included a battery of 17 cognitive function tests.9 These included 1) 7 measures of episodic memory: Word List Memory, Recall, and Recognition and immediate and delayed recall of Story A from the Logical Memory and the East Boston Story; 2) 2 measures of visuospatial ability or perceptual organization: a short form of Judgment of Line Orientation and Standard Progressive Matrices; 3) 2 measures of perceptual speed: an oral version of the Symbol Digit Modalities Test and Number Comparisons; 4) 2 measures of semantic memory: a 15-item version of the Boston Naming Test, and short form of the National Adult Reading Test; and 5) 3 measures of working memory: Digit Span Forward, Digit Span Backward, and Digit Ordering. To minimize floor and ceiling effects of the individual tests, summary measures of each cognitive domain were constructed by converting raw scores on each individual test (using the mean and SD for the CHAP population at baseline) to z scores, and averaging the z scores. A measure of global cognitive function was also formed by averaging the z scores on all 17 tests.9 Diagnosis of dementia was made by an experienced neurologist and required the loss of cognitive function by neurologic assessment and impairment in 2 or more areas on the cognitive performance testing.10
Biochemical assessment of vitamin B12 status.
For the present effort, biochemical analyses were performed on nonfasting blood. Earliest samples included in these analyses were collected August 1997, the latest in November 2000; hence, sampling occurred during both the voluntary and mandatory folate fortification of the US food supply. Serum vitamin B12 was measured by competitive displacement immunoassay (Quest Laboratories, Wooddale, IL) immediately following the clinical evaluation because this measurement was part of a routine diagnostic panel. From frozen sera aliquots stored at −80°C for 7–10 years, the other vitamin B12 markers (methylmalonic acid [MMA], homocysteine, 2-methylcitric acid, and cystathionine) were measured using stable-isotope dilution and capillary gas chromatography–mass spectrometry (Metabolite Labs at the University of Colorado Health Sciences Center, Denver, CO).11,12
MRI.
See also e-Methods on the Neurology® Web site at www.neurology.org. Subjects were imaged on a General Electric 1.5-T scanner (Excite platform, version 11) and the following imaging sequences were obtained: fluid-attenuated inversion recovery: repetition time (TR)=11,000, echo time (TE) 144, inversion time (TI) 2,250, 22 cm field of view (FOV), 3 mm slice thickness, 192 × 256 acquisition matrix; spoiled gradient: TE minimum, 20 degree flip angle, 24 cm FOV, 1.5 mm slice thickness with 256 × 256 acquisition matrix; double spin echo: TR=2,100, TE=30/92, 22 cm FOV, 4 mm slice thickness, with 256/192 acquisition matrix. Axial images were angled to be parallel to the anterior and posterior commissure lines. After acquisition of the MRI scans, digital information was transferred to the laboratory of Dr. Charles DeCarli for processing and analysis.
White matter hyperintensity segmentation was performed by a 2-step process according to previously reported methods.13–15 WMHV was expressed in proportion to total cranial volume to correct for head size and log transformed to create a normal distribution (log-WMHV) for analysis as a continuous measure. TBV was computed as the ratio of total brain parenchymal volume to total cranial volume. The presence or absence of cerebral infarcts was determined manually by the operator who considered the size, location, and imaging characteristics of the lesion.16 Only lesions 3 mm or larger were considered cerebral infarcts. Repeat analysis of intrarater and interrater reliabilities of MRI measures for the purpose of this study were consistently above 0.90.17–20
Definition of covariates or mediators.
Sex and race were obtained at the time of the census and verified at the baseline population interview. Age was computed from self-reported birth date and date of the MRI evaluation. Education was computed from self-reported highest grade or years of formal education. Height, current smoking status, and lifetime daily alcohol use (drinks/day) were based on self-report during the cycle 2 population interview. Participant's weight without shoes was measured on a digital freestanding scale. From these measures, body mass index (BMI) in kg/m2 was calculated. Hypertension was defined as self-reported hypertension or measured systolic blood pressure ≥160 mm Hg or diastolic pressure ≥95 mm Hg. Participants were categorized according to the presence or absence of one or more APOE4 alleles. Serum creatinine measurements were performed by Rush University Medical Laboratories.
Statistics.
Our primary objective was to expand on our previous findings of association between levels of MMA and vitamin B12 and cognitive decline by examining the relations between these serum markers of vitamin B12 status to brain MRI measures. In addition, we sought to explore the relations of serum vitamin B12 markers with different cognitive domain scores.7 In separate models, we used multiple linear regression (SAS/STAT software version 9.2) to regress either brain volume or cognitive score outcome measures on each vitamin B12 marker. Logistic regression models were used to examine the associations of vitamin B12 markers on the presence or absence of infarcts. For primary analyses all models were controlled for age, sex, education, race, serum creatinine concentrations, and time elapsed between blood sampling and MRI evaluation (MRI lag) and the MRI instrument. Because homocysteine and MMA are elevated when there is renal failure,12 serum creatinine level was included in all models to account for possible confounding.
In secondary analyses, because of the small sample size we examined confounding by other factors by including them one at a time in the primary model. Among these factors were APOE4, dementia diagnosis, hypertension, BMI, smoking status, and lifetime alcohol intake. We examined possible interactions by age, sex, race, APOE4, dementia, and hypertension with the inclusion of multiplicative terms for each vitamin B12–related marker and the effect modifier in the primary model. To examine potential mediation effects on observed associations of vitamin B12 markers with cognitive function, we added a term for each MRI measure to each primary model, noting differences in the effect estimates and p values with and without terms in the model.
RESULTS
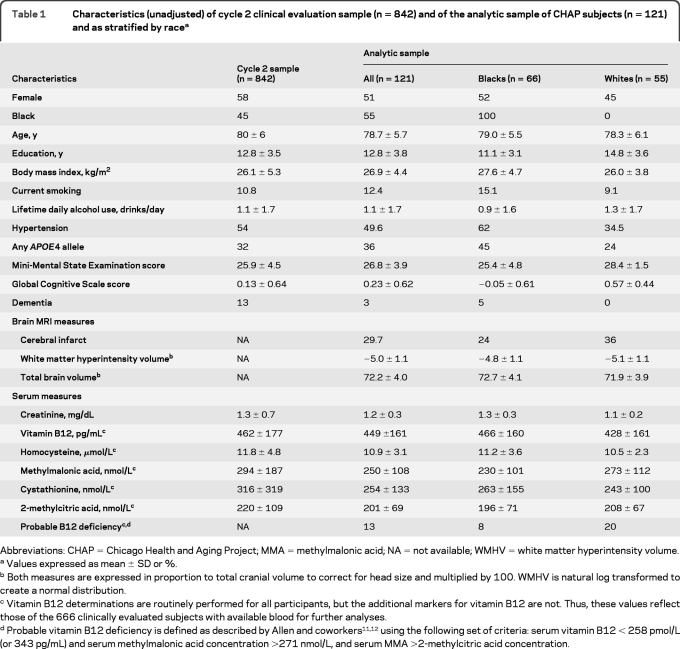
At cycle 2 (baseline for our analyses) half of the analytic sample was female (51%) and 45% was white (table 1). Global cognitive scores ranged from −2.18 to 1.42 with a mean of 0.23. Risk factors and comorbidities were similar between the full and analyzed samples except that the analytic sample had fewer female participants, more black participants, and only 2.5% of the analytic sample had clinical dementia vs 13% of the full cycle 2 sample. Elevated homocysteine concentrations (>14 μmol/L) were observed in 17.5% of the sample and 15.2% had elevated MMA concentrations (>271 nmol/L) (table 1). Serum homocysteine and MMA concentrations were correlated (r=0.55, p < 0.0001).
Table 1.
Characteristics (unadjusted) of cycle 2 clinical evaluation sample (n=842) and of the analytic sample of CHAP subjects (n=121) and as stratified by racea
Abbreviations: CHAP=Chicago Health and Aging Project; MMA=methylmalonic acid; NA=not available; WMHV=white matter hyperintensity volume.
Values expressed as mean ± SD or %.
Both measures are expressed in proportion to total cranial volume to correct for head size and multiplied by 100. WMHV is natural log transformed to create a normal distribution.
Vitamin B12 determinations are routinely performed for all participants, but the additional markers for vitamin B12 are not. Thus, these values reflect those of the 666 clinically evaluated subjects with available blood for further analyses.
B12 markers and cognitive function.
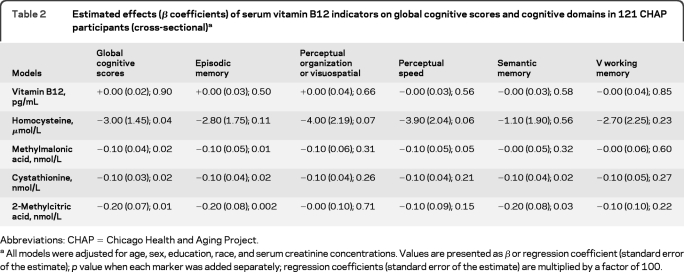
First, we examined the relations of the vitamin B12 markers with scores for global cognitive function and with each of the 5 cognitive domains (table 2). Each of the vitamin B12–related markers, but not vitamin B12 itself, was associated with global cognitive scores in separate models adjusted for age, sex, education, race, and serum creatinine concentrations. For example, for each 1 μmol/L increase in homocysteine concentration, global cognitive score decreased by 0.03 standardized units (p=0.04). The relations of the different B12 markers to scores of the individual cognitive domains, however, were not consistent. Serum homocysteine concentration was not associated with any of the individual cognitive domains although scores for perceptual organization and perceptual speed had marginal associations. Serum concentrations of MMA, cystathionine, and 2-methylcitrate were each associated with episodic memory scores: the higher the concentrations of these markers, the lower the scores. Higher MMA concentrations were also associated with reduced perceptual speed, and higher cystathionine and 2-methylcitrate concentrations were each associated with poorer semantic memory. These associations remained in analyses that adjusted individually for BMI, smoking status, lifetime alcohol intake, hypertension, dementia, or APOE4 (data not shown). In further analyses, there was no evidence for effect modification by these factors.
Table 2.
Estimated effects (β coefficients) of serum vitamin B12 indicators on global cognitive scores and cognitive domains in 121 CHAP participants (cross-sectional)a
Abbreviations: CHAP=Chicago Health and Aging Project.
All models were adjusted for age, sex, education, race, and serum creatinine concentrations. Values are presented as β or regression coefficient (standard error of the estimate); p value when each marker was added separately; regression coefficients (standard error of the estimate) are multiplied by a factor of 100.
B12 markers and brain MRI measures.
Similar to our findings for cognitive function, vitamin B12 levels were not associated with any of the MRI measures in models adjusted for age, sex, race, education, and serum creatinine (table 3). Homocysteine concentration was the only vitamin B12 indicator that was associated with WMHV; WMHV increased by 0.103 units per μmol/L increase in homocysteine concentration. Higher levels of each of the B12-related markers (that is, serum homocysteine, MMA, cystathionine, and 2-methylcitrate concentrations) were significantly associated with decreased TBV.
Table 3.
Effects of serum vitamin B12 indicators on MRI measures: White matter hyperintensity volume, cerebral infarcts, and total brain volume of 121 CHAP participantsa
Abbreviation: CHAP=Chicago Health and Aging Project.
All models were adjusted for age, sex, education, race, MRI instrument, and time elapsed between blood sampling and MRI evaluation, and serum creatinine concentrations.
Values are presented as β or regression coefficient (standard error of the estimate); p value when each marker was added separately; regression coefficients (standard error of the estimate) are multiplied by a factor of 100.
Values are presented as odds ratios (95% confidence intervals); p value.
We also examined whether these associations were modified by level of age, sex, race, education, APOE4, or dementia. The only evidence of effect modification was stronger adverse effects on TBV by cystathionine among persons with the APOE4 allele (pinteraction=0.02). The influence of hypertension on the association between homocysteine and TBV was marginal (pinteraction=0.069).
Investigation of potential mechanisms.
We explored potential underlying mechanisms for the associations between the vitamin B12 markers and cognitive function by adding covariates for the individual MRI measures into these models. The association of homocysteine and global cognitive performance was attenuated (β=−0.024, p=0.08) when we adjusted for WMHV. Adjustment for cerebral infarcts also attenuated the homocysteine association to a similar extent (β=−0.024, p=0.08), though when we adjusted for TBV, we observed no marked attenuation (β=−0.029, p=0.04). Associations between global cognitive function and each of MMA, cystathionine, and 2-methylcitric acid were attenuated and no longer statistically significant with adjustment for TBV (for MMA, β=−0.001, p=0.14). Both TBV and WMHV accounted for the associations between B12 markers and episodic memory (for MMA, β=−0.001; p value=0.10). Adjustment for any of the MRI measures attenuated the observed associations between perceptual speed and MMA (for example with WMHV, β=−0.001; p value=0.16). In contrast, the association noted for semantic memory and cystathionine was not markedly attenuated when TBV was entered into the model (β=−0.03, p=0.048).
DISCUSSION
This report describes the associations of serum vitamin B12 and vitamin B12–related metabolites to cognitive performance at cycle 2 and to MRI measurements on average 4.6 years later. Associations are observed for concentrations of vitamin B12 and related markers that are considered reflective of adequate vitamin status.
The finding of associations between several of the vitamin B12 markers and global cognitive scores is consistent with our previous report of 516 CHAP subjects7 as well as that of others,21–25 but not all.26 Associations between brain MRI measures (in particular, TBV and WMHV) and global cognition as well as performance in multiple domains have been reported previously by our group, but not in relation to vitamin B12 status.1 In the present report, we did not observe associations between the vitamin B12 markers and cerebral infarcts. This observation is in contrast to reports by other groups who have described a greater number of infarcts and more WMH burden with higher homocysteine concentrations.27–29 Absence of an association in our study may be due to the few subjects. The observation of effect modification by APOE4 on the association of cystathionine and TBV is consistent with evidence that the genotype and low B vitamin status confers greater vulnerability to cognitive deficits.30
In the present study, the potential mediation of MRI measures on the relation of vitamin B12– related markers to cognition has been investigated. Serum homocysteine levels were associated with cognitive performance which was independent of TBV. Others have noted a relationship between homocysteine and cognition31,32 but not simultaneously with brain MRI measures. In a British cohort where mandatory folate fortification is in place, a comprehensive set of vitamin B12 markers were examined in association with brain atrophy over 5 years in 107 older adults. After adjustment for confounders, neither homocysteine nor MMA was predictive of brain atrophy, though vitamin B12 and its carrier, holotranscobalamin, were.6 In the VITACOG trial, treatment with a supplement containing vitamin B6, vitamin B12, and folate for 2 years reduced homocysteine levels and slowed brain atrophy in British adults with mild cognitive impairment, but concomitant changes in cognitive scores were not reported.33 Associations between several vitamin B12 indicators and white matter lesions and with cognitive function were reported in the Rotterdam Scan Study but potential mediation effects were not examined.26 Our data suggest that both vascular and nonvascular mechanisms play a role in vitamin B12 status. The vascular mechanism is consistent with the attenuation of the relation between homocysteine and cognitive performance when cerebral infarcts were entered in the model. For the nonvascular contribution, small differences in vitamin B12 markers may alter the integrity of white matter, specifically by modifying the extent of myelin damage. Areas of demyelination on brain MRI have been described in vitamin B12–deficient patients or in those with diseases that affect vitamin B12 metabolism.33–35
Thus, our findings lend support for the contention that poor vitamin B12 status is a risk factor for brain atrophy and possibly WMHV which in turn may contribute to cognitive impairment. The single MRI measure in the present study prevents direct investigation of whether poor vitamin B12 status results in cognitive decline by promoting faster rates of total brain atrophy or demyelination in selected white matter areas. On the basis of repeated MRI scans, brain atrophy associated with cognitive decline appears to be a slow process; brain atrophy rates among adults aged 70 years or more ranged from 0.7% to 1.1% per year.6,33
A distinct contribution made by our group is a comprehensive study of the metabolic indicators of vitamin B12 status and the possible role it has on both cognitive performance and brain measures. Both homocysteine and MMA accumulate when insufficient vitamin B12 is available as a cofactor for 2 separate reactions; cystathionine and 2-methylcitric acid also accumulate.11,12 Folate and vitamin B6 status may also contribute to elevated cystathionine and 2-methylcitric acid, however. Only MMA accumulates specifically in response to low vitamin B12 status. A limitation to this study is the absence of serum folate and vitamin B6 determinations. Strengths of this study include a sensitive imaging method to assess WMHV and TBV at the same MRI facility, a well-characterized biracial cohort of older adults, and use of validated measures of cognitive function.
Marginal vitamin B12 status in older age36 is frequently missed by measurement of serum vitamin B12 levels alone. Our findings suggest that MMA, the specific marker of B12 deficiency, may affect cognition by reducing TBV whereas the effect of homocysteine on cognition may be mediated through increased WMHV and cerebral infarcts. Vitamin B12 status as reflected by functional markers such as homocysteine and MMA concentrations and the relations to brain changes on MRI and cognitive testing deserves further examination.
Supplementary Material
GLOSSARY
- BMI
body mass index
- CHAP
Chicago Health and Aging Project
- FOV
field of view
- MMA
methylmalonic acid
- TBV
total brain volume
- TE
echo time
- TI
inversion time
- TR
repetition time
- WMHV
white matter hyperintensity volume
Footnotes
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
Dr. Tangney: draft/revise manuscript, study concept or design, analysis or interpretation of data, acquisition of data, statistical analysis. Dr. Aggarwal: draft/revise manuscript, study concept or design, analysis or interpretation of data, contribution of patients/tools, acquisition of data, study coordination. H. Li: analysis or interpretation of data, acquisition of data, statistical analysis. Dr. Wilson: draft/revise manuscript, contribution of patients/tools. Dr. DeCarli: draft/revise manuscript, analysis or interpretation of data, contribution of patients/tools, acquisition of data. Dr. Evans: draft/revise manuscript, analysis or interpretation of data, contribution of patients/tools, acquisition of data, obtaining funding. Dr. Morris: draft/revise manuscript, study concept or design, analysis or interpretation of data, contribution of patients/tools, acquisition of data, statistical analysis, obtaining funding.
DISCLOSURE
Dr. Tangney receives research support from the NIH/NIA. Dr. Aggarwal has served on a scientific advisory board for Pfizer Inc and receives research support from the NIH and the Alzheimer's Association. H. Li reports no disclosures. Dr. Wilson serves on editorial advisory boards for Aging, Neuropsychology, and Cognition and Psychology and Aging; serves as a consultant for Pain Therapeutics, Inc.; and receives research support from the NIH/NIA. Dr. DeCarli serves as Editor-in-Chief for Alzheimer Disease and Associated Disorders; serves as a consultant for Bayer Schering Pharma and Avanir Pharmaceuticals; and receives research support from the NIH (NIA, NHLBI). Dr. Evans has served on a data monitoring committee for Eli Lily and Company; and receives research support from the NIH. Dr. Morris has received research support from the US Department of Health and Human Services, the NIH/NIA, the Abbott Fund, and the Sprague Institute.
REFERENCES
- 1. Aggarwal NT, Wilson RS, Bienias JL, et al. The association of magnetic resonance imaging measures with cognitive function in a biracial population sample. Arch Neurol 2010;67:475–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gunning-Dixon FM, Raz N. Neuroanatomical correlates of selected executive functions in middle-aged and older adults: a prospective MRI study. Neuropsychologia 2003;41:1929–1941 [DOI] [PubMed] [Google Scholar]
- 3. Verdelho A, Madureira S, Moleiro C, et al. White matter changes and diabetes predict cognitive decline in the elderly: the LADIS study. Neurology 2010;75:160–167 [DOI] [PubMed] [Google Scholar]
- 4. Smith EE, Egorova S, Blacker D, et al. Magnetic resonance imaging white matter hyperintensities and brain volume in the prediction of mild cognitive impairment and dementia. Arch Neurol 2008;65:94–100 [DOI] [PubMed] [Google Scholar]
- 5. De Lau LM, Refsum H, Smith AD, Johnston C, Breteler MM. Plasma folate concentration and cognitive performance: Rotterdam Scan study. Am J Clin Nutr 2007;86:728–734 [DOI] [PubMed] [Google Scholar]
- 6. Vogiatzoglou A, Refsum H, Johnston C, et al. Vitamin B12 status and rate of brain volume loss in community-dwelling elderly. Neurology 2008;71:826–832 [DOI] [PubMed] [Google Scholar]
- 7. Tangney CC, Tang Y, Evans DA, Morris MC. Biochemical indicators of vitamin B12 and folate insufficiency and cognitive decline. Neurology 2009;72:361–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bienias JL, Beckett LA, Bennett DA, Wilson RS, Evans DA. Design of the Chicago Health and Aging Project (CHAP). J Alzheimer Dis 2003;5:349–355 [DOI] [PubMed] [Google Scholar]
- 9. Wilson RS, Aggarwal NT, Barnes LL, Bienias JL, Mendes de Leon CF, Evans DA. Biracial population study of mortality in mild cognitive impairment and Alzheimer disease. Arch Neurol 2009;66:767–772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bennett DA, Schneider JA, Aggarwal NT, et al. Decision rules guiding the clinical diagnosis of Alzheimer's disease in two community-based cohort studies compared to standard practice in a clinic-based cohort study. Neuroepidemiology 2006;27:169–176 [DOI] [PubMed] [Google Scholar]
- 11. Allen RH, Stabler SP, Savage DG, Lindenbaum J. Metabolic abnormalities in cobalamin (vitamin B12) and folate deficiency. FASEB J 1993;7:1344–1353 [DOI] [PubMed] [Google Scholar]
- 12. Allen RH, Stabler SP, Savage DG, Lindenbaum J. Elevation of 2-methylcitric acid I and II levels in serum, urine, and cerebrospinal fluid of patients with cobalamin deficiency. Metabolism 1993;42:978–988 [DOI] [PubMed] [Google Scholar]
- 13. DeCarli C, Maisog J, Murphy DG, Teichberg D, Rapoport SI, Horwitz B. Method for quantification of brain, ventricular, and subarachnoid CSF volumes from MR images. J Comput Assist Tomogr 1992;16:274–284 [DOI] [PubMed] [Google Scholar]
- 14. DeCarli C, Murphy DG, Teichberg D, Campbell G, Sobering GS. Local histogram correction of MRI spatially dependent image pixel intensity nonuniformity. J Magn Reson Imaging 1996;6:519–528 [DOI] [PubMed] [Google Scholar]
- 15. DeCarli C, Fletcher E, Ramey V, Harvey D, Jagust WJ. Anatomical mapping of white matter hyperintensities (WMH): exploring the relationships between periventricular WMH, deep WMH, and total WMH burden. Stroke 2005;36:50–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. DeCarli C, Reed T, Miller BL, Wolf PA, Swan GE, Carmelli D. Impact of apolipoprotein E epsilon4 and vascular disease on brain morphology in men from the NHLBI twin study. Stroke 1999;30:1548–1553 [DOI] [PubMed] [Google Scholar]
- 17. Murphy DG, DeCarli C, Schapiro MB, Rapoport SI, Horwitz B. Age-related differences in volumes of subcortical nuclei, brain matter, and cerebrospinal fluid in healthy men as measured with magnetic resonance imaging. Arch Neurol 1992;49:839–845 [DOI] [PubMed] [Google Scholar]
- 18. DeCarli C, Murphy DG, Gillette JA, et al. Lack of age-related differences in temporal lobe volume of very healthy adults. AJNR Am J Neuroradiol 1994;15:689–696 [PMC free article] [PubMed] [Google Scholar]
- 19. DeCarli C, Massaro J, Harvey D, et al. Measures of brain morphology and infarction in the Framingham heart study: establishing what is normal. Neurobiol Aging 2005;26:491–510 [DOI] [PubMed] [Google Scholar]
- 20. Murphy DG, DeCarli C, McIntosh AR, et al. Sex differences in human brain morphometry and metabolism: an in vivo quantitative magnetic resonance imaging and positron emission tomography study on the effect of aging. Arch Gen Psychiatry 1996;53:585–594 [DOI] [PubMed] [Google Scholar]
- 21. Clarke R, Birks J, Nexo E, et al. Low vitamin B-12 status and risk of cognitive decline in older adults. Am J Clin Nutr 2007;86:1384–1391 [DOI] [PubMed] [Google Scholar]
- 22. Hin H, Clarke R, Sherliker P, et al. Clinical relevance of low serum vitamin B12 concentrations in older people: the Banbury B12 study. Age Ageing 2006;35:416–422 [DOI] [PubMed] [Google Scholar]
- 23. Dufouil C, Alperovitch A, Ducros V, Tzourio C. Homocysteine, white matter hyperintensities, and cognition in healthy elderly people. Ann Neurol 2003;53:214–221 [DOI] [PubMed] [Google Scholar]
- 24. Haan MN, Miller JW, Aiello AE, et al. Homocysteine, B vitamins, and the incidence of dementia and cognitive impairment: results from the Sacramento Area Latino Study on Aging. Am J Clin Nutr 2007;85:511–517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tucker KL, Qiao N, Scott T, Rosenberg I, Spiro A., III High homocysteine and low B vitamins predict cognitive decline in aging men: The Veterans Affairs Normative Aging study. Am J Clin Nutr 2005;82:627–635 [DOI] [PubMed] [Google Scholar]
- 26. De Lau LM, Smith AD, Refsum H, Johnston C, Breteler MM. Plasma vitamin B12 status and cerebral white-matter lesions. J Neurol Neurosurg Psychiatry 2009;80:149–157 [DOI] [PubMed] [Google Scholar]
- 27. Tseng Y, Chang Y, Liu J, Su C, Lai S, Lan M. Association of plasma homocysteine concentration with cerebral white matter hyperintensity on magnetic resonance images in stroke patients. J Neurol Sci 2009;284:36–39 [DOI] [PubMed] [Google Scholar]
- 28. Wright CB, Paik MC, Brown TR, et al. Total homocysteine is associated with white matter hyperintensity volume: The Northern Manhattan Study. Stroke 2005;36:1207–1211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vermeer SE, van Dijk EJ, Koudstaal PJ, et al. Homocysteine, silent brain infarcts, and white matter lesions: The Rotterdam Scan Study. Ann Neurol 2002;51:285–289 [DOI] [PubMed] [Google Scholar]
- 30. Bunce D, Kivipelto M, Wahlin A. Apolipoprotein E, B vitamins, and cognitive function in older adults. J Gerontol Psychol Sci 2005;60B:P41–P48 [DOI] [PubMed] [Google Scholar]
- 31. Wright CB, Lee H-L, Paik MC, et al. Total homocysteine and cognition in a tri-ethnic cohort: The Northern Manhattan Study. Neurology 2004;63:254–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Seshadri S, Beiser A, Selhub J, et al. Plasma homocysteine as a risk factor for dementia and Alzheimer's disease. N Engl J Med 2002;346:476–483 [DOI] [PubMed] [Google Scholar]
- 33. Smith AD, Smith SM, De Jager CA, et al. Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: a randomized clinical trial. PLoS One 2010;5:e12244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stojsavljovic N, Levic Z, Drulovic J, et al. A 44-month clinical brain MRI follow-up in a patient with B12 deficiency. Neurology 1997;49:878–891 [DOI] [PubMed] [Google Scholar]
- 35. Scalabrino G. Cobalamin (vitamin B12) in subacute combined degeneration and beyond: traditional interpretations and novel theories. Exp Neurol 2005;192:463–479 [DOI] [PubMed] [Google Scholar]
- 36. Allen LH. How common is vitamin B-12 deficiency? Am J Clin Nutr 2009;89:693S–696S [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.