Abstract
Generation of induced pluripotent stem cells (iPSCs) has opened new avenues for the investigation of heart diseases, drug screening and potential autologous cardiac regeneration. However, their application is hampered by inefficient cardiac differentiation, high interline variability, and poor maturation of iPSC-derived cardiomyocytes (iPS-CMs). To identify efficient inducers for cardiac differentiation and maturation of iPSCs and elucidate the mechanisms, we systematically screened sixteen cardiomyocyte inducers on various murine (m) iPSCs and found that only ascorbic acid (AA) consistently and robustly enhanced the cardiac differentiation of eleven lines including eight without spontaneous cardiogenic potential. We then optimized the treatment conditions and demonstrated that differentiation day 2-6, a period for the specification of cardiac progenitor cells (CPCs), was a critical time for AA to take effect. This was further confirmed by the fact that AA increased the expression of cardiovascular but not mesodermal markers. Noteworthily, AA treatment led to approximately 7.3-fold (miPSCs) and 30.2-fold (human iPSCs) augment in the yield of iPS-CMs. Such effect was attributed to a specific increase in the proliferation of CPCs via the MEK-ERK1/2 pathway by through promoting collagen synthesis. In addition, AA-induced cardiomyocytes showed better sarcomeric organization and enhanced responses of action potentials and calcium transients to β-adrenergic and muscarinic stimulations. These findings demonstrate that AA is a suitable cardiomyocyte inducer for iPSCs to improve cardiac differentiation and maturation simply, universally, and efficiently. These findings also highlight the importance of stimulating CPC proliferation by manipulating extracellular microenvironment in guiding cardiac differentiation of the pluripotent stem cells.
Keywords: induced pluripotent stem cells, ascorbic acid, cardiomyocytes, cardiac progenitor cells
Introduction
Establishment of embryonic stem cell (ESC)-like cells (also know as induced pluripotent stem cells or iPSCs) by the reprogramming of adult somatic cells with a few defined transcription factors provides a fascinating route to generate patient-specific pluripotent cells as disease models and drug-testing systems 1, 2, 3. Improvement of cardiac function by the transplantation of iPSC-derived cardiomyocytes (iPS-CMs) after myocardial infarction in animal models 4 suggests a potential of using iPSCs in patient-specific cardiac regeneration 5, 6. However, to realize these application potentials, establishment of a highly efficient and easily practicable differentiation system is one of the prerequisites.
Cardiogenesis is a well-organized process tightly regulated by key developmental signals and extracellular microenvironment 7, 8. Although cardiomyocytes are successfully generated from mouse (m) 9, 10 and human (h) 11, 12 iPSCs in vitro, the cardiac differentiation efficiency remains very low 5. Several attractive approaches focusing on the manipulation of critical signaling pathways to improve the cardiac differentiation efficiency of iPSCs have been reported currently 13, 14, 15, while little is known about the contribution of manipulating extracellular microenvironments to the process of cardiac differentiation from iPSCs.
Another important obstacle hampering the utilization of iPSCs is the high interline variability in cardiac differentiation efficiency 11, 12, 16, with some of the lines even showing no cardiac differentiation properties in vitro 17. Therefore, a highly efficient and universal system must be developed to overcome or minimize such variations before the extensive use of iPSCs.
In addition, iPS-CMs have been proved to be less mature than those from ESCs or fetal hearts, reflected by the delayed development of sarcoplasmic reticulum and lower responses to β-adrenergic stimulus 18, 19. Such immaturity not only results in ineffective contractile force generation but may also lead to arrhythmia 6. Thus, it is important to develop approaches to facilitate the maturation of iPS-CMs.
ESC-derived cardiac progenitor cells (CPCs) are capable of populating multiple lineages of the heart and offer exciting alternative avenues for cardiac regeneration 20, while iPSCs are a novel source to generate individual-specific CPCs 21, 22. Although CPCs have been identified by multiple markers 20, the mechanism underlying the renewal and differentiation of CPCs is poorly understood, and proper methods to efficiently obtain and expand iPSC-derived CPCs in vitro remain challenging.
Accumulating evidences have shown that iPSCs are similar but not fully identical to ESCs and are considered a unique subtype of pluripotent cells 2, 3, 23. Previous studies on ESC differentiation have provided knowledge and methods for directing cardiac differentiation of ESCs 7, 24 and will facilitate the development of optimal approaches for the cardiac differentiation of iPSCs. However, it is unclear whether these knowledge and methods can be fully applied to iPSCs. Kattman et al. 14 developed an efficient cardiac differentiation approach recently by adjusting the levels of Activin/Nodal and BMP signaling. They found distinct responses of iPSCs to cytokine stimulation compared with ESCs. Thus, systematic and detailed analyses on iPSCs with the knowledge learned from ESC differentiation are required.
Ascorbic acid (AA) has been demonstrated to promote the cardiac differentiation of ESCs 25, 26, 27 and is applied in several reported protocols in both ESCs and iPSCs 14, 15, 28. However, the exact roles of AA in the cardiac differentiation of iPSCs and the underlying mechanism have not yet been assessed.
To identify suitable inducers for iPSC-CMs, we here systematically screened sixteen cytokines and chemical compounds reported to facilitate the cardiac differentiation of ESCs. We found that only AA robustly and reproducibly enhanced cardiac differentiation of iPSCs even in the lines without spontaneous cardiogenic potential. Optimized treatment of AA led to approximately 7.3-fold (miPSCs) and 30.2-fold (hiPSCs) increases in the relative abundance of cardiomyocytes. Moreover, the structural and functional maturation of iPS-CMs were improved by AA treatment, providing the first successful pro-maturation method that works on iPS-CMs to our knowledge. Then we analyzed the mechanisms underlining AA-promoted cardiac differentiation and showed that AA specifically enhanced the proliferation of CPCs via the MEK-ERK1/2 pathway through manipulating collagen synthesis. Furthermore, isolated CPCs expanded more rapidly in the presence of AA. Therefore, we have developed a universal, economical, and efficient system for producing CPCs and functional iPS-CMs. Our findings also provide new insight into the mechanisms of AA-promoted cardiac differentiation and collagen-enhanced CPC proliferation.
Results
AA consistently and robustly enhances cardiac diffe-rentiation of iPSCs
To understand more about the ability of cardiomyocyte inducers of ESCs in the facilitation of cardiogenesis of iPSCs, we first systematically screened 16 cytokines and chemical components that were reported to promote the cardiac differentiation of ESCs following the optimized concentration and window in six miPSC lines generated from various origins or developed by different methods (Supplementary information, Table S1). Utilizing the classical hanging drop-based embryoid body (EB) model, we identified that only AA showed consistent and robust cardiac-inducing effects among different iPSC lines, even in the lines without spontaneous cardiac differentiation potential by evaluating the profile of Ebs containing beating clusters (Supplementary information, Figure S1), a typical phenomenon for the presence of functional cardiomyocytes 29.
Characteristics of AA-induced cardiac differentiation in miPSCs
To further determine the effects of AA and dissect its mechanisms in promoting cardiomyocytes differentiation, we utilized miPSC lines IP20D-3 generated by retroviral delivery of four transcription factors, Oct4, Sox2, Klf4, and c-Myc (iPS-4F) 30 and iPS-R-B1 (without c-Myc, iPS-3F) as two representative cell lines. Undifferentiated iPSCs showed typical ESC-like morphology, high alkaline phosphatase activity, and universally expressed pluripotent markers Oct4 and SSEA1 (Supplementary information, Figure S2A). Fluorescence-activated cell sorting (FACS) analysis further confirmed that > 86% cells expressed SSEA1 (Supplementary information, Figure S2B). RT-PCR analysis detected the expressions of key endogenous pluripotent genes Oct4, Sox2, Nanog, and Rex1 in both iPSC lines but not the exogenous transgenic factors (Supplementary information, Figure S2C).
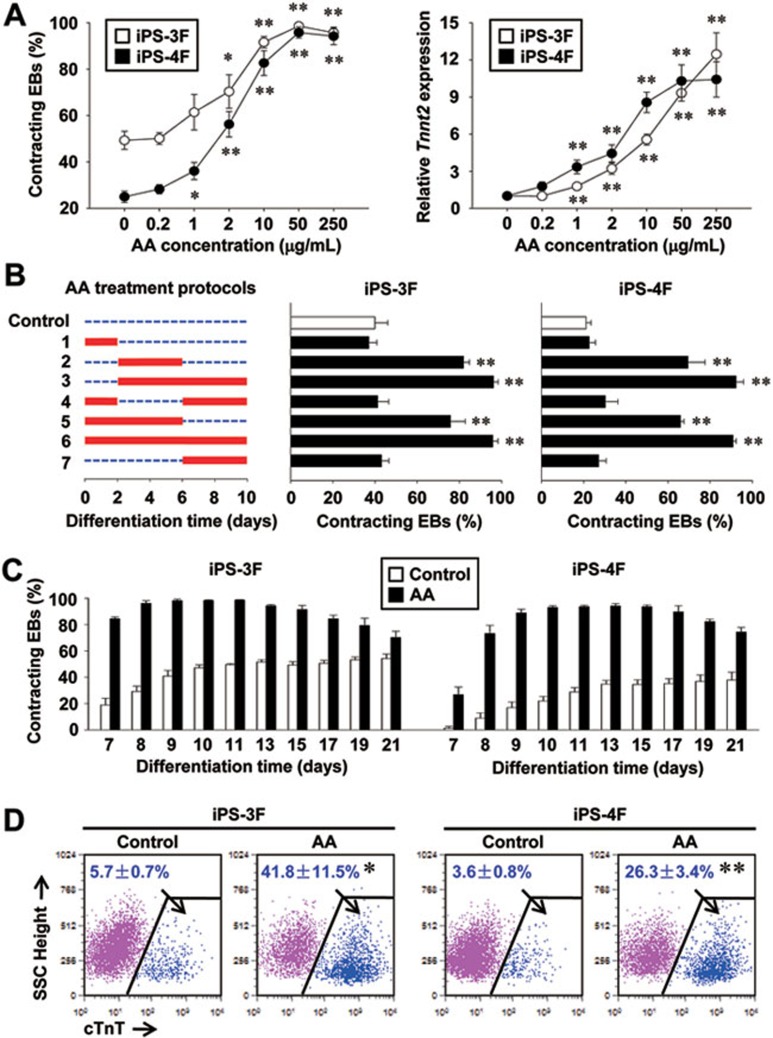
To characterize the effect of AA in the cardiogenesis of iPSCs, cells were treated with AA from 0.2 to 250 μg/ml for 10 days from the initiation of differentiation. The percentage of contracting EBs and the relative expression level of cardiac gene Tnnt2 significantly increased in a concentration-dependent manner and reached a peak around 50 μg/ml (Figure 1A). To determine the exact stage in which AA takes effect, we then systematically added AA (50 μg/ml) during early-phase (day 0-2), mid-phase (day 2-6), or late-phase (day 6-10) of iPSC differentiation (Figure 1B) both individually and throughout. AA treatment during differentiation day 2-10 significantly increased cardiac differentiation equivalent to the treatment during the entire differentiation period (Figure 1B, 3 and 6). Consistently, AA treatment during day 0-2 failed to promote cardiac differentiation of both iPSC lines (Figure 1B, 1). Moreover, AA treatment during day 0-6 or 2-6 fulfilled 76%-85% or 72%-79% of its maximal cardiac induction potential, whereas this effect was totally disappeared by withdrawal of AA during day 2-6 (Figure 1B, 2, 4 and 5). These results reveal that the mid-phase (day 2-6), a critical phase for CPC specification 20, is the most crucial period for AA to inure.
Figure 1.
AA robustly enhances cardiogenesis of 3F and 4F miPSCs. (A) Concentration-dependent relationships of AA. Data were collected at day 10. (B) Time windows for AA-promoted cardiac differentiation. Left panel, schematic diagram of the differentiation protocols; middle and right panels, corresponding efficiency in 3F and 4F lines. (C) Differentiation profile of cardiomyocytes in both iPSC lines. (D) Percentages of cTnT+ cardiomyocytes at day 15 in the total population derived from both iPSC lines with or without AA treatment. n = 3 each. Data are expressed as means ± SEM. *P < 0.05, **P < 0.01 vs control.
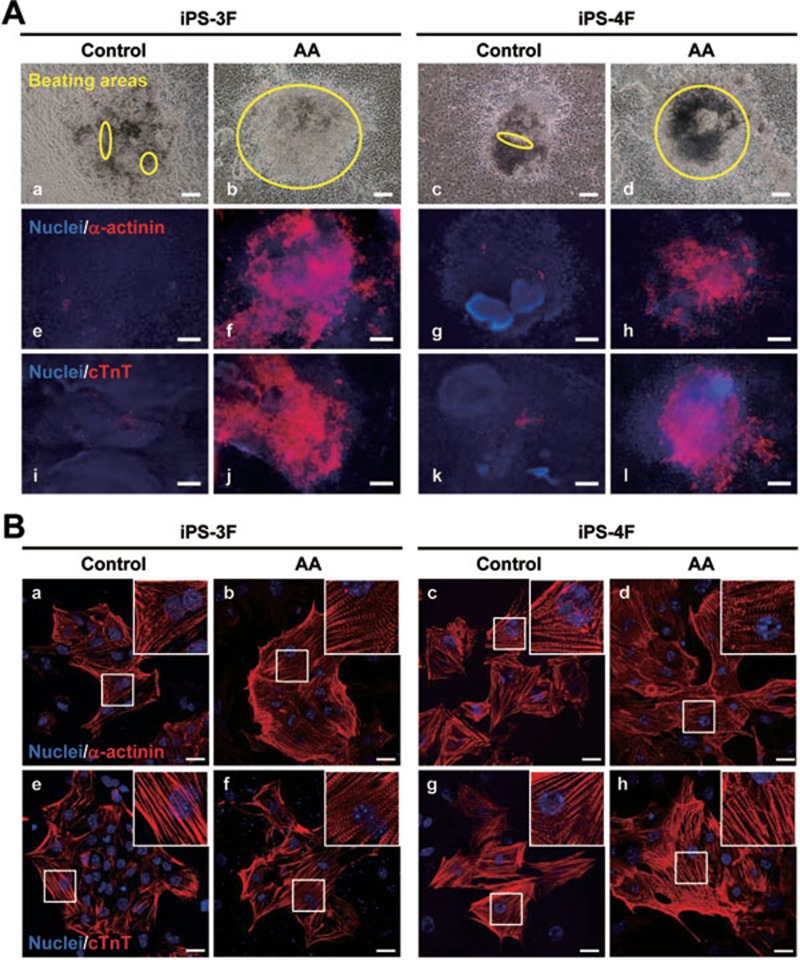
Then profiles of contracting EBs with or without AA treatment were further examined. Spontaneously beating cardiomyocytes were visible at day 7 without AA treatment and 38% (iPS-4F) to 54% (iPS-3F) of the EBs developed contracting clusters 4-5 days later and remained stable up to 21 days examined, whereas contracting EBs were robustly enhanced to 90%-100% 1-3 days after plating in AA-treated cells (Figure 1C), implying the faster development of AA-induced cardiomyocytes. An approximate 7.3-fold increase of cardiomyocyte formation in the total population of AA-treated EBs was further confirmed by intracellular staining of the cardiac isoform of Troponin T (cTnT) in FACS analysis at day 15 (Figure 1D). Consistently, larger beating areas were observed in AA-treated EBs and further consolidated by the immunostaining analysis of specific myofilamental protein markers α-actinin and cTnT (Figure 2A). AA treatment always led to a synchronous beating of the entire EB (Figure 2A and Supplementary information, Movie SI-SIV). In addition, AA-promoted cardiac differentiation was also observed in an auto-aggregated model, which allowed the scalable production of EBs, as well as in a serum-free differentiation system (Supplementary information, Figure S3).
Figure 2.
AA increases the content and improves the sarcomeric organization of iPS-CMs. (A) Representative images showing increased beating areas (a-d) and the content of α-actinin+ (e-h) or cTnT+ (i-l) cardiomyocytes in day-10 EBs treated with AA. Scale bars = 100 μm. (B) Sarcomeric structure analysis of the day-18 iPS-CMs by α-actinin and cTnT staining. The insets were magnifications of the framed areas showing more organized cross-striation alignment of sarcomeres in AA-induced iPS-CMs. Scale bars = 25 μm. Nuclei were counterstained with Hoechst33258 (blue).
Next, we examined whether AA treatment affects the sarcomeric organization of iPSC-CMs by immunostaining of α-actinin and cTnT on day-18 iPS-CMs. AA-induced cardiomyocytes showed better-organized cross-striated myofilaments compared with the control ones (Figure 2B), suggesting that the sarcomeric organization and structural maturation of iPS-CMs is enhanced by AA treatment.
AA promotes cardiovascular but not mesodermal differentiation of iPSCs
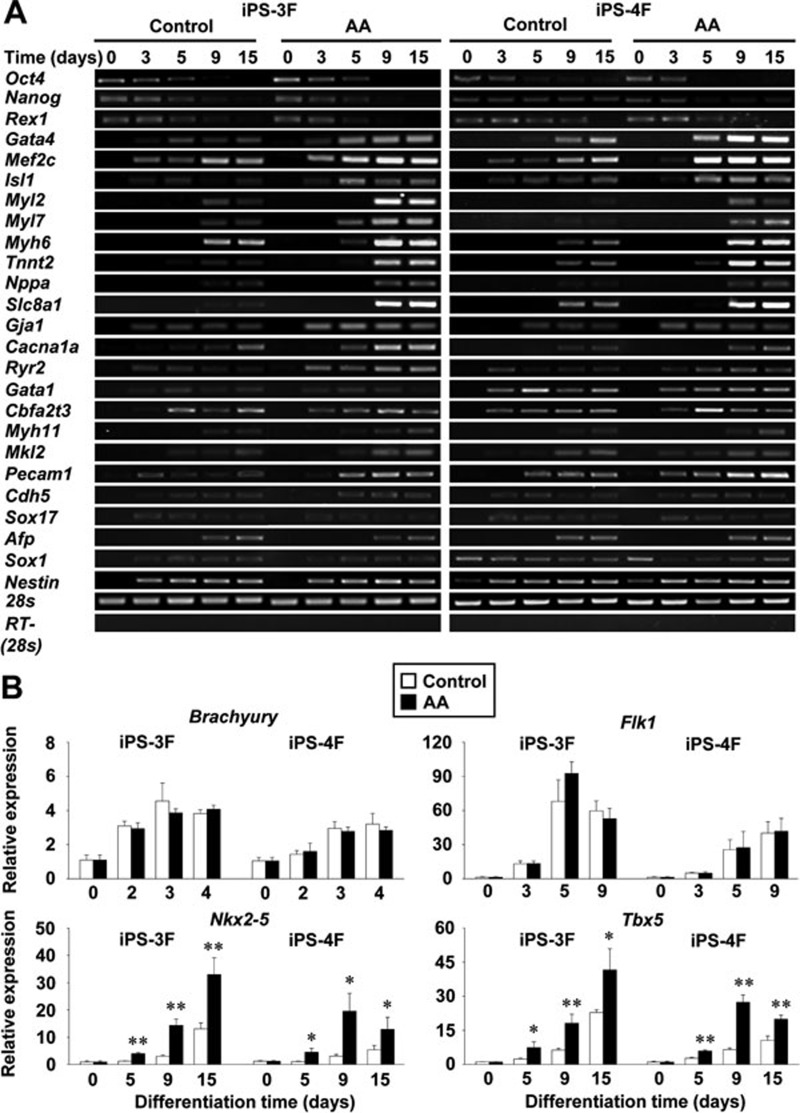
To elucidate the critical stage for AA in promoting cardiomyocyte differentiation of iPSCs, we then analyzed the expression of pluripotent, mesoderm, cardiac precursor, and cardiomyocyte genes by RT-PCR and quantitative RT-PCR (qPT-PCR). AA-treatment clearly increased the expression of cardiac transcription factors Gata4, Isl1, and Mef2c in both iPSC lines, whereas the expression of pluripotency markers Oct4, Nanog, and Rex1 decreased more rapidly with the time of iPSC differentiation (Figure 3A). The expression levels of cardiac muscle-specific genes Myl2, Myl7, Myh6, and Tnnt2 also remarkably upregulated in AA-applied cells (Figure 3A). Concomitantly, genes major encoding cardiac function regulators and calcium-handling proteins, including Nppa, Slc8a1, Gja1, Cacna1a, and Ryr2, were more intensively induced by AA treatment (Figure 3A). qRT-PCR analyses further revealed that the expression levels of mesodermal genes Brachyury and Flk1 remained unchanged in AA-treated EBs compared with the corresponding controls (P > 0.05, Figure 3B, upper panels), whereas the expression of cardiac genes, Nkx2-5 and Tbx5, was remarkably increased from differentiation day 5, a critical time point for CPC specification (Figure 3B, lower panels). In addition, AA also moderately increased the expressions of smooth-muscle markers Myh11 and Mkl2, endothelial markers Pecam1 and Cdh5, but not hematopoietic markers Gata1 and Cbfa2t3 (Figure 3A), which were further confirmed by FACS analysis of α-SMA (smooth muscle), CD31 (endothelial), and CD41 (hematopoietic, Supplementary information, Figure S4). However, the expression of endodermal (Sox17 and Afp) and ectodermal markers (Sox1 and Nestin) was not obviously affected by AA treatment (Figure 3A). Taken together with the observation of AA without effects during differentiation day 0-2 (Figure 1B), these data suggest that AA specifically increases cardiovascular but not mesoderm differentiation of iPSCs.
Figure 3.
AA increases the expression of cardiac genes. (A) RT-PCR analysis showing the particular upregulation of cardiac genes in AA-stimulated EBs compared with the untreated ones. (B) Quantitative RT-PCR analysis indicated the increased expression of cardiac progenitor but not mesodermal transcripts (n = 3). Data are expressed as means ± SEM. *P < 0.05, **P < 0.01 vs control.
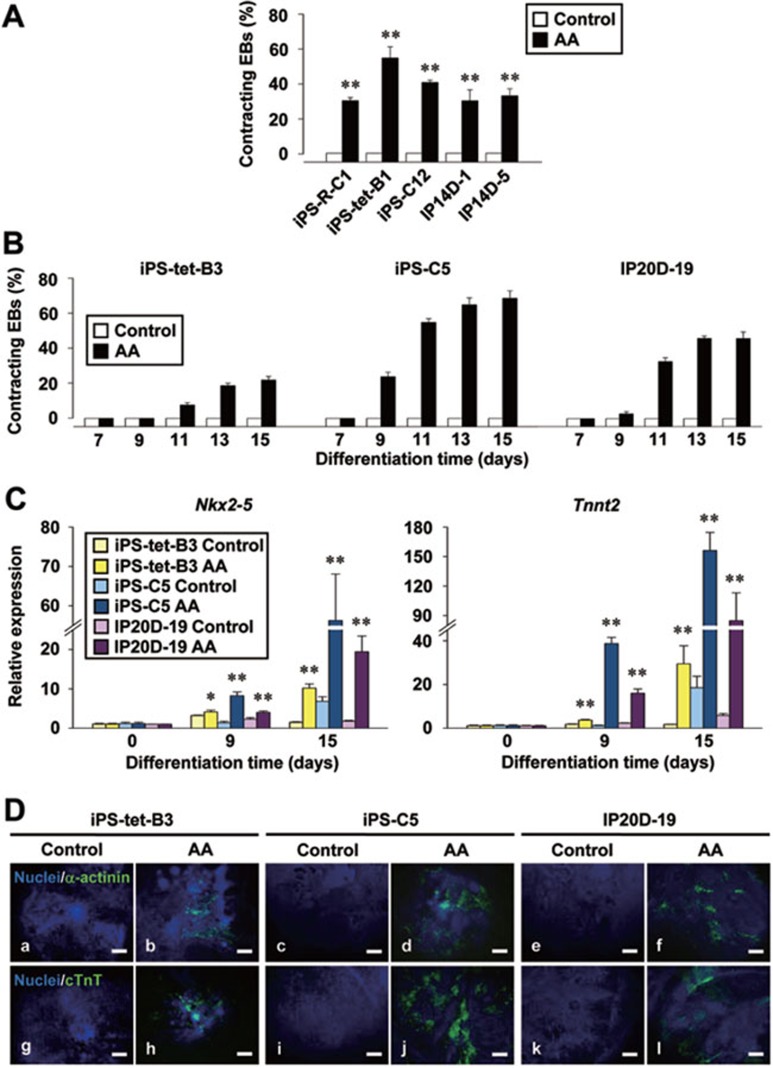
AA treatment rescues innate cardiogenic deficiency of iPSC lines
iPSC lines display a huge variation in their cardiac differentiation capacity 11, 12, 16, 17. Such phenomenon was observed in six iPSC lines used for the preliminary screening of cardiomyocyte inducers in our study and was minimized after AA treatment (Supplementary information, Figure S1), indicating that AA might overcome cell line variation in the cardiac differentiation. To confirm this, we then tested AA on five other lines generated from various origins and methods (Supplementary information, Table S1) by examining the profile of contracting EBs. AA treatment induced cardiac differentiation of all tested cell lines originally without spontaneous development of beating cardiomyocytes (Figure 4A). Further analyses were performed on three representative iPSC lines established by different laboratories 30, 31, 32. The control EBs from all three lines showed no spontaneous contractility, whereas evident beating activities were reproducibly observed in AA-treated EBs with an increasing tendency from differentiation day 9-11 (Figure 4B). Coordinately, the expression of key cardiac genes Nkx2-5 and Tnnt2 was robustly increased in AA-treated EBs during differentiation (Figure 4C) and the occurrence of α-actinin+ or cTnT+ cardiomyocytes was only detected in AA-treated EBs at day 15 from all three iPSC lines (Figure 4D). These data indicate that AA induces cardiac differentiation in iPSC lines without intrinsic cardiac potential in vitro and might be useful in overcoming cell line variation in the cardiac differentiation efficiency.
Figure 4.
Rescue of innate cardiac deficiency by AA treatment. (A) AA induced the development of contracting EBs in other 5 iPSC lines without spontaneous cardiogenic potential. Data were collected at day 10. (B) Differentiation profile of cardiomyocytes in three representative iPSC lines. (C) Quantitative RT-PCR analysis of the expression level of cardiac genes. (D) Immunostaining showing the only emergence of α-actinin+ and cTnT+ cardiomyocytes in AA-treated EBs at day 10. Scale bars = 100 μm. Nuclei were counterstained with Hoechst33258 (blue). Data are expressed as means ± SEM. *P < 0.05, **P < 0.01 vs control.
AA treatment improves maturation of iPS-CMs reflected by enhanced responses to β-adrenergic and muscarinic stimulations
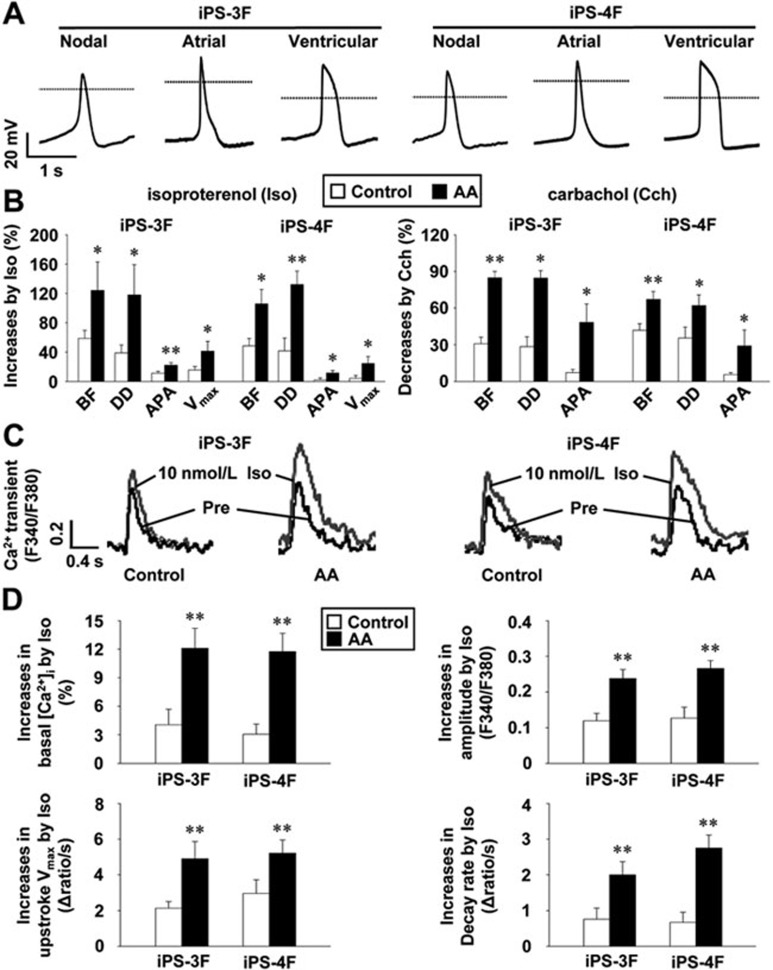
Because AA was observed to enhance the sarcomeric organization and structural maturation of iPS-CMs (Figure 2B), we then tested whether AA could improve the functional maturity of iPS-CMs by characterizing action potentials (APs) of iPS-CMs with or without AA treatment and detected their responses to β-adrenergic and muscarinic stimulations, critical signaling pathways in cardiomyocytes. iPS-CMs at differentiation day 16-18 displayed nodal-like, atrial-like, and ventricular-like APs in both control (data not shown) and AA-treated groups (Figure 5A). AA treatment did not affect the beating frequency (BF), amplitude (APA), maximum rise rate (Vmax), and rate of diastolic depolarization (DD) of APs, as well as the AP duration at 50% repolarization (APD50) in iPS-4F cells, whereas the DD was increased by AA treatment in iPS-3F cells (Supplementary information, Table S2). β-adrenergic agonist isoproterenol (Iso) at 10 nmol/l significantly increased the BF, DD, APA, and Vmax of the APs in iPS-CMs, whereas carbachol (Cch), a synthetic muscarinic agonist, showed opposite negative effects at 1 μmol/l in both cell lines. Strikingly, these responses were both much stronger in AA-applied cells (Figure 5B). In addition, AA-treated cells showed higher basal intracellular free Ca2+ concentration ([Ca2+]i), APA, upstroke Vmax, and decay rate of Ca2+ transients (Supplementary information, Figure S5A), as well as stronger responses to 10 nmol/l Iso characterized by larger increases of the Ca2+ transient parameters in both cell lines (Figure 5C and 5D), implying a larger internal store and more rapid operation of Ca2+ in these cells. This was supported by the dramatic increased expression of Ryr2, Atp2a2, Pln and Gja1 encoding crucial calcium-handling and gap junction proteins (Supplementary information, Figure S5B) and their corresponding proteins (Supplementary information, Figure S5C) in purified AA-treated day-18 iPS-CMs by tetramethylrhodamine methyl ester perchlorate (TMRM) staining 33. These data demonstrate that AA treatment improves the maturation of iPS-CMs and enhances the ability of iPS-CMs to respond to critical functional regulations.
Figure 5.
AA enhances the response of day 16-18 iPS-CMs to β-adrenergic and muscarinic stimulations. (A) Representative APs of AA-induced iPS-CMs showing characteristics of nodal-like, atrial-like, and ventricular-like APs. Dotted lines indicate 0 mV. (B) Comparison of Iso (10 nmol/l)-stimulated increases (left panel) and Cch (1 μmol/l)-induced decreases (right panel) in characteristics of APs between control and AA-applied iPS-CMs (n = 10-13). BF, beating frequency; DD, diastolic depolarization; APA, AP amplitude; Vmax, maximum rise rate. (C) Representative tracings of spontaneous rhythmic Ca2+ transients with (grey) and without (black) Iso-simulation (10 nmol/l). (D) Iso-induced increases in basal [Ca2+]i, APA, upstroke Vmax, and decay rate of Ca2+ transients in control or AA-applied iPS-CMs (n = 12-13). Data are expressed as means ± SEM. *P < 0.05, **P < 0.01 vs control.
AA-promoted cardiac differentiation through increasing collagen synthesis
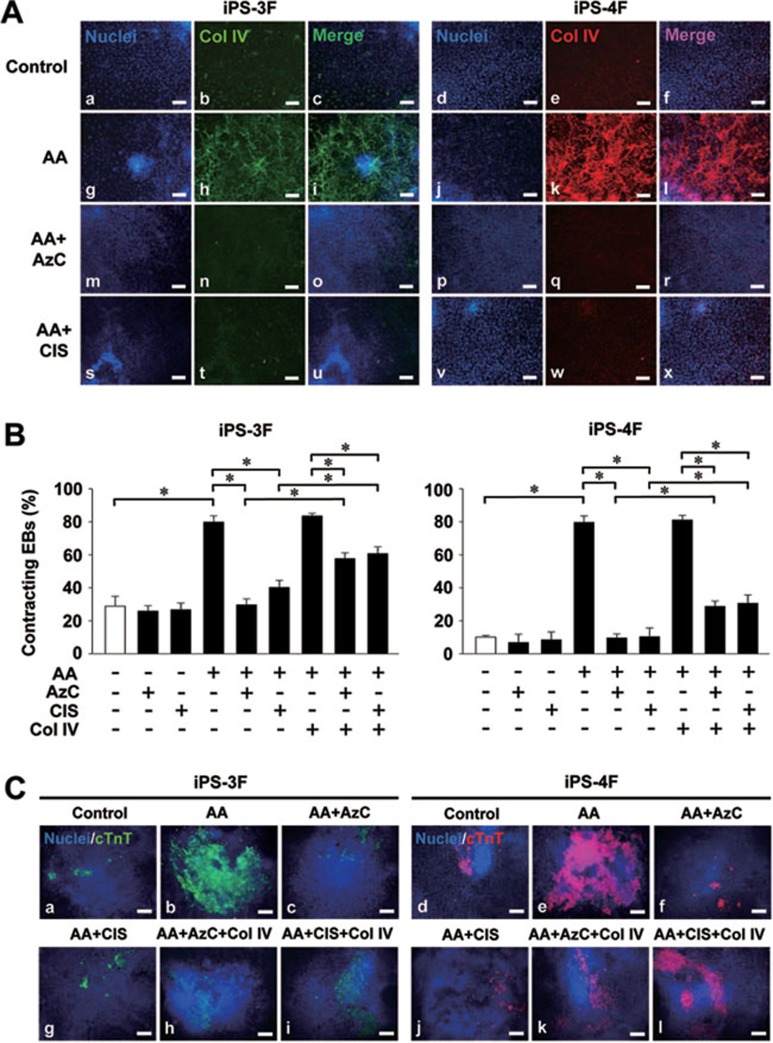
To explore the specific mechanism underlying AA-stimulated cardiac differentiation of iPSCs, we then investigated whether the cardiomyocyte-promoting effect of AA is attributed to its antioxidative property. Treatment with alternative antioxidants such as vitamin B1 (Vb1), reduced gluthatione (GMEE), and N-acetyl-L-cysteine (NAC), failed to mimic the effect of AA on the cardiac differentiation (Supplementary information, Figure S6A), suggesting that the cardiomyocyte-promoting role of AA is independent of its antioxidative property. Since collagen synthesis has been shown to be required for AA-enhanced cardiac differentiation of mESCs 25, we then analyzed the effect of AA on collagen synthesis and found significant increases in the expression of collagen genes Col1a1 and Col4a1 from differentiation day 5-15 in AA-treated iPSCs (Supplementary information, Figure S6B). Immunostaining results further confirmed the robust increased expression of type IV collagen (Col IV), which has been shown to facilitate the development of cardiovascular cells from iPSCs 10, in AA-applied EBs (Figure 6A). To further clarify the role of collagen synthesis in AA-induced cardiac differentiation of iPSCs, we stably downregulated the expression of Col I or Col IV in iPS-3F and iPS-4F lines by lentiviral delivery of small interfering RNAs (siRNAs, Supplementary information, Figure S7A). The AA-promoted cardiac differentiation was partially hampered by either downregulation of Col I or Col IV and the knockdown of both Col I and Col IV had an additive effect (Supplementary information, Figure S7B), suggesting that various types of collagens are required for AA-enhanced cardiac differentiation. We thus utilized two general collagen synthesis inhibitors, L-2-Azetidine carboxylic acid (AzC) and cis-4-hydroxy-D-proline (CIS) and found that the increased expression of Col IV and enhanced cardiomyocyte development by AA were completely abolished by AzC (50 μmol/l) and CIS (100 μmol/l) in both iPSC lines, while the blocking effects of AzC and CIS were partially rescued by directly plating the day-2 EBs onto Col IV-coated dishes (Figure 6A and 6B). These effects on cardiomyocyte formation were further confirmed by immunostaining of cTnT (Figure 6C). These data demonstrate that the collagen synthesis rather than antioxidative property of AA accounts for its promotive role in cardiac differentiation of iPSCs.
Figure 6.
AA-enhanced collagen synthesis is required for its cardiomyocyte-promoting effect. (A) Immunostaining of Col IV at day-6 EBs treated with or without AA and collagen synthesis inhibitor AzC and CIS. (B and C) Cardiomyocyte-promoting effect of AA was abolished by AzC and CIS, and could be partially rescued by Col IV. Scale bars = 100 μm. Nuclei were counterstained with Hoechst33258 (blue). Data are expressed as means ± SEM. *P < 0.01 vs corresponding values.
AA augments the cardiomyocyte population derived from iPSCs by specifically promoting the proliferation of CPCs in a collagen synthesis-dependent mechanism
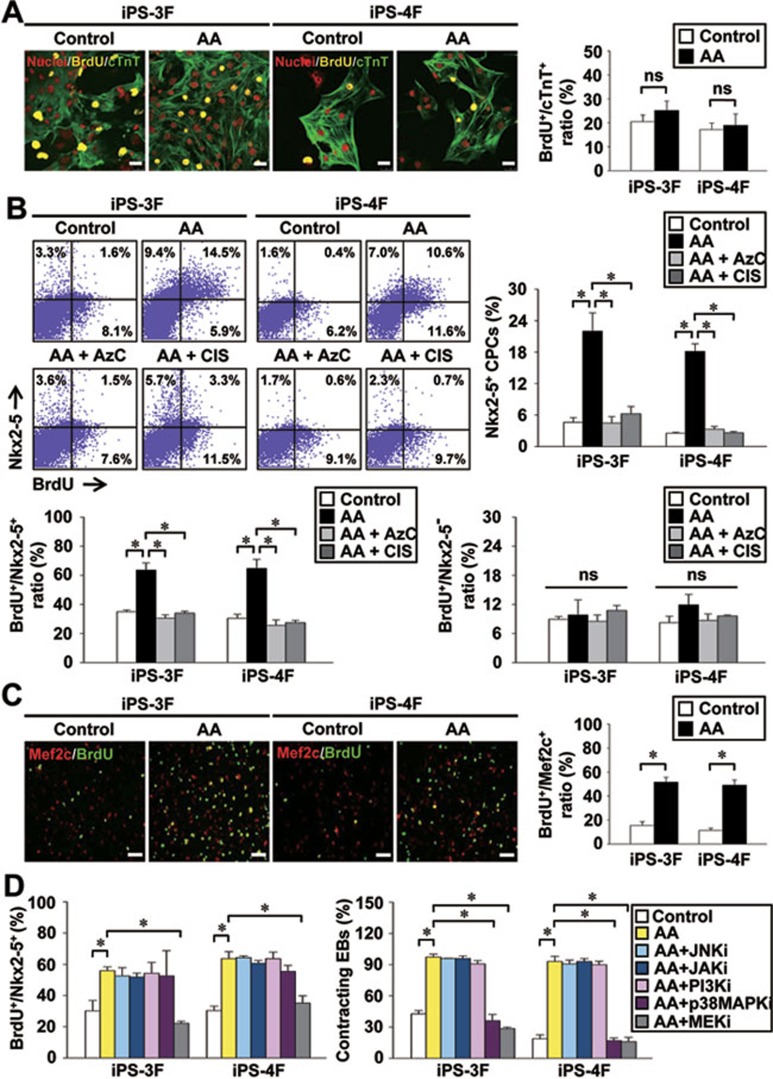
Next, we attempted to elucidate further why AA-increased collagen expression promotes cardiac differentiation of iPSCs. Collagens are indispensible components of the extracellular matrix (ECM), which plays a critical role in cardiac development and function, and have been shown to affect cell proliferation and differentiation 8. However, the effect of collagens on the proliferation and specification of CPCs is unclear. We found that day-10 iPS-CMs with double-immunostaining of BrdU and cTnT showed comparable percentages of double-positive cells between control and AA-applied groups (Figure 7A). Taken together with the observation that AA shows no cardiac-inducing effect when applied after differentiation day 6 (Figure 1B), these results suggest that AA treatment appears not to affect the proliferation of cardiomyocytes. As the most critical stage for AA to take effect is day 2-6 (Figure 1B), a crucial time for CPC specification, we then investigated the proliferation of day-5 CPCs by FACS analysis of Nkx2-5/BrdU double-staining cells. AA-treated EBs showed a markedly increased percentages of both Nkx2-5+ and proliferating BrdU+/Nkx2-5+ CPCs, while the promoting effects were fully abrogated by AzC and CIS treatment (Figure 7B). Interestingly, the ratio of BrdU+/Nkx2-5− cells was not significantly altered by AA application (Figure 7B, right lower panel), indicating that this pro-proliferation effect of AA is restricted in CPCs. As ECM may affect cell survival 8, we also examined the apoptosis status of day-5 EBs and found that AA did not affect the apoptotic index and cell viability (Supplementary information, Figure S8).
Figure 7.
AA specifically enhances the proliferation of CPCs in a collagen synthesis-dependent manner. (A) Immunostaining of cTnT and BrdU in day-10 iPS-CMs. Data were quantified from 6-8 random fields in two assays. Scale bars = 25 μm. Nuclei were counterstained with PI (red). (B) Double staining of Nkx2-5 and BrdU at day-5 (n = 3). (C) Immunostaining of Mef2c and BrdU in day-8 CPCs (3 days after sorting). Data were quantified from five random fields in two assays. Scale bars = 100 μm. (D) Effects of signal inhibitors on proliferation of Nkx2-5+ CPCs and percentage of contracting EBs (n = 3). Data are expressed as means ± SEM. *P < 0.01 vs corresponding values. ns, no significant difference.
To further assess whether this effect is directly mediated by AA or indirectly mediated by other cells, we isolated Flk1+/Cxcr4+ CPCs 34 by FACS from day-5 EBs and expanded them in the presence or absence of AA for 3 days. Schematic diagram of the strategy for analyzing the role of AA in expansion or differentiation of the CPCs was shown in Supplementary information, Figure S9A. We found that AA markedly increased the number of Mef2c+ CPCs and the level of BrdU incorporation in these cells (Figure 7C), whereas it did not affect the cardiac differentiation capacity of sorted CPCs (Supplementary information, Figure S9B). These data further prove that AA enhances cardiogenesis of iPSCs mainly through promoting the proliferation of CPCs.
AA enhances CPC proliferation via the MEK-ERK1/2 pathway
We next sought to identify signaling pathways involved in AA-mediated CPC proliferation by using specific signaling inhibitors. The AA-enhanced BrdU+/Nkx2-5+ CPC population remained unchanged when addition of JNK, JAK, PI3K, or p38MAPK inhibitor, whereas the MEK inhibitor completely abolished AA-induced increases of BrdU+/Nkx2-5+ CPCs and contracting EBs (Figure 7D), suggesting that the MEK-ERK1/2 pathway is involved in the AA-dependent CPC expansion and cardiomyocyte augmentation. This was confirmed by the strongly increased phosphorylation of ERK1/2 in AA-treated cells at differentiation day 5 and this effect was eliminated by the collagen synthesis inhibitors AzC and CIS (Supplementary information, Figure S10). Noticeably, p38MAPK inhibitor suppressed AA-enhanced cardiomyocyte differentiation, but not the proliferation of CPCs (Figure 7D), which is consistent with the observation in mESCs 35, and suggesting that the involvement of p38MAPK pathway in cardiac differentiation is independent of the proliferation of CPCs.
Taken together, these data reveal that AA-induced collagens synthesis enhances the differentiation of iPSCs into cardiomyocytes through specifically promoting the CPC proliferation via MEK-ERK1/2 pathway.
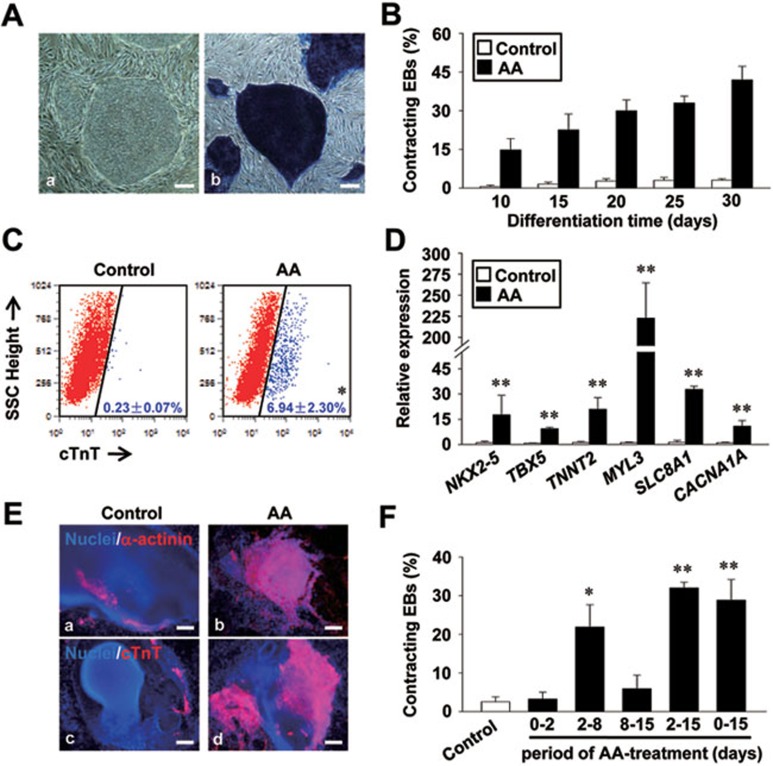
AA remarkably enhances the cardiac differentiation of hiPSCs
To further investigate whether the cardiomyocyte-promoting effect of AA is conserved in human, we examined its role on hiPSC line hAFDC-iPS-36 36. Figure 8A showed typical morphology of undifferentiated hiPSC clones. AA treatment at 50 μg/ml during day 0-30 robustly enhanced both the percentage of contracting EBs and cTnT+ cardiomyocytes in hiPSCs (Figure 8B and 8C). This effect was further confirmed by the enhanced expression of cardiac genes NKX2-5, TBX5, TNNT2, MYL3, SLC8A1, CACNA1A (Figure 8D), and myofilamental protein markers α-actinin and cTnT (Figure 8E). Optimal treatment-phase analysis also proved the CPC specification period (day 2-8) to be the most critical time-window for AA to take effect (Figure 8F). These data indicate that AA promotes cardiac differentiation in both miPSCs and hiPSCs through stimulating the proliferation of CPCs.
Figure 8.
AA promotes cardiogenesis of human iPSCs (hiPSCs). (A) Morphology (a) and alkaline phosphatase staining (b) of undifferentiated hiPSCs colonies. (B) Percentages of contracting EBs during differentiation. (C) Percentages of cTnT+ cardiomyocytes in hiPSC-derived EBs at day 30. (D, E) Quantitative RT-PCR (D) and immunostaining (E) analysis showed the remarkable increases in expression of cardiac markers following AA treatment (n = 3). (F) Time windows for AA-promoted cardiogenesis. Scale bars = 100 μm. Nuclei were counterstained with Hoechst33258 (blue). *P < 0.05, **P < 0.01 vs control.
Discussion
Our findings here extend previous knowledge of AA in promoting the cardiac differentiation of ESCs 25, 26, 27, indicating that AA is an ideal cardiomyocyte inducer of both miPSCs and hiPSCs, and reveal a novel cardiomyocyte-promoting mechanism. The important findings are that (i) only AA shows consistent cardiac-inducing capacity among different iPSC lines including those without spontaneous cardiogenic potential and remarkably enhances the cardiac differentiation of both miPSCs and hiPSCs; (ii) the cardiomyocyte-promoting effect is also seen in large-scale generated and serum-free cultivated EBs; (iii) such effect of AA is restricted to the phase of CPC specification and is attributed to the collagen synthesis-based increase of CPC proliferation via MEK-ERK1/2 pathway; (iv) AA facilitates the in vitro expansion of CPCs isolated from iPSCs; and (v) AA improves structural and functional maturation of iPS-CMs. Therefore, by using AA, a straightforward, economical, and efficient system has been successfully established from which significant amount of CPCs and functional cardiomyocytes could be produced from various iPSC lines.
Cardiomyocytes can be successfully obtained from iPSCs, however the differentiation efficiency is low and a huge interline variability is observed 11, 12, 16, 17. Moreover, the diverse levels of endogenous signaling between different iPSC lines make them difficult to be universally manipulated by exogenous cytokines 14. AA has been well documented to promote cardiac differentiation of ESCs 25, 26, 27. Here, we demonstrate, for the first time, the conclusive and universal role of AA in cardiac differentiation of iPSCs and provide novel insight into the underlying mechanism. Most of the existing cardiac differentiation protocols, especially for human ESCs, require a complicated switch of culture condition, addition of expensive cytokines and signal inhibitors at accurate timing and concentration, or co-culture with stroma cells 7. To develop an easily practicable and universal system suitable for the efficient cardiac differentiation of iPSCs, we performed single factor-based screening to make the system as simple as possible. It is noteworthy that only AA shows the uniform and robust cardiomyocyte-promoting effect among all of the iPSC lines tested, including the lines that failed to differentiate into cardiomyocytes spontaneously in our screening. With the simple supplement of AA, a relative large amount of cardiomyocytes is efficiently generated from ESCs 25, 26, 27 and iPSCs, suggesting that AA is a suitable cardiomyocyte inducer of pluripotent stem cells for both scientific and economical reasons.
The most successful cardiac differentiation approaches to date are those focusing on the induction of CPCs 28, 37. Our observations of AA is not only increasing the percentage of iPSC-derived CPCs but also specifically promotes their proliferation by manipulating the microenvironment (Figure 7), further proving the importance of manipulating CPCs in guiding efficient cardiac differentiation. ECM and MEK-ERK1/2 pathway have been shown to be involved in the proliferation of cardiomyocytes 38. Our data here, for the first time, link the ECM to the control of CPC fate and show that the MEK-ERK1/2 pathway is activated by AA by regulating collagen synthesis and plays an important role in stimulating proliferation of the CPCs derived from iPSCs. Moreover, the possibility to generate patient-specific CPCs from iPSCs offers exciting novel routes in the field of cardiac translational medicine and drug discovery. iPSC-derived multipotent CPCs, which possess better proliferation capacity and can differentiate into multiple lineages of the heart, might offer an advantage over mere cardiomyocytes, as they contribute to both muscularization and vascularization 20. However, one of the major limitations for their utilization is the difficulty in CPC expansion. Here, we provide a simple and effective method for the in vitro expansion of CPCs isolated from iPSCs by utilizing AA. This approach may facilitate the cloning of CPCs or direct transdifferentiation of somatic tissues into CPCs. Whether AA would affect the proliferation of other types of cardiovascular progenitors needs to be further examined.
We showed here that alternative antioxidants (including Vb1, GMEE and NAC) failed to mimic the cardiomyocyte-promoting role of AA in iPSCs (Supplementary information, Figure S6A). This is consistent with previous observations showing the inability of alternative antioxidative agents, such as 4,5-dihydroxy-1,3-benzene-disulfonic acid, vitamin E 26 or NAC 25, to mimic the effect of AA on the cardiac differentiation of ESCs. These observations suggest that the cardiac promoting role of AA is independent of its antioxidative property, or at least, that its antioxidative effect is insufficient to induce cardiac differentiation of the ESCs and iPSCs. Paradoxically, Crespo et al. 39 observed that antioxidants including NAC and mitoubiquinone hampered the cardiac differentiation of ESCs. Those inconsistent findings may be caused by the different cell lines and differentiation conditions, such as different batch of serum used in each study. In addition, they found that the impaired cardiac differentiation induced by antioxidants or low glucose (5 mM) culture condition, which resulted in a decrease of reactive oxygen species (ROS) production, could be rescued by AA. Thus, they attributed the cardiomyocyte-promoting effect of AA to its ability in increasing ROS level 39. However, this could be alternatively explained that this rescue effect of AA may be mediated by the increased synthesis of collagen, which has been proved critical to the cardiomyocyte-promoting role of AA in previous 25 studies as well as ours. This hypothesis is further confirmed by the fact that AA 2-phosphate (A2-P), a stable form of AA but without pro-oxidant effect 40, also robustly enhances the cardiac differentiation of ESCs 25. Moreover, we demonstrated here that the increased cardiac differentiation and proliferation of the CPCs, as well as the robust activation of MEK-ERK1/2 pathway, could be eliminated by the collagen synthesis inhibitors AzC and CIS (Figures 6, 7 and Supplementary information, Figure S10). Taken together, those data support that the collagen synthesis rather than the antioxidative property of AA accounts for its cardiac promoting role in iPSCs.
Maturation of pluripotent stem cell-derived cardiomyocytes is critical for their application in either drug screen or cell transplantation. However, iPS-CMs are not only immature compared with the ESCs- or fetal heart-derived ones, but also more resistant to maturation methods that work effectively for ESC-derived cardiomyocytes 6, 18, 19. Interestingly, AA promotes the maturation of iPS-CMs characterized by the rapid decrease of contracting EBs after differentiation day 17 (Figure 1C). This is further supported by the fact that AA-induced iPS-CMs show better sarcomeric organization (Figure 2B) and higher responses to β-adrenergic and muscarinic stimulations (Figure 5). The underlying mechanism may be related to its role in promoting accumulation of ECM proteins that have been shown to improve the maturation of ESC-derived cardiomyocytes 41. Alternatively, this effect may be related to the accelerated dynamics of cardiac differentiation or activation of particular transcriptional program and signaling pathways following AA treatment. These possibilities need to be further investigated. Taken together, our findings reveal the role of AA in promoting the maturation of iPSC-CMs and provide the first pro-maturation method that works in iPS-CMs to our knowledge.
Besides the in vitro application, AA has been reported to improve cardiomyoblast propagation and promote vascularization in bioartificial grafts in vivo 42, which can be explained by our findings that AA activates CPCs that are capable of differentiating into multiple cardiovascular cells. Thus, it is fascinating to elucidate whether AA could facilitate transplantation of iPSC-derived CPCs and has the potential to activate endogenous CPCs in vivo in the future.
In summary, our findings demonstrate that AA is a suitable cardiomyocyte inducer of iPSCs in vitro and robustly enhances the cardiac differentiation of both miPSCs and hiPSCs. Moreover, AA minimizes the interline variance in cardiogenic capacity of iPSCs and facilitates the structural and functional maturation of iPS-CMs. In addition, we have proved that AA specifically promotes the proliferation of iPSC-derived CPCs via MEK-ERK1/2 pathway by increasing the collagen synthesis, which also offers a novel method for the in vitro expansion of CPCs. The discoveries in this study are useful to fully harness the unrivaled potential of iPSCs in scientific studies, drug discovery, and toxicity testing, and patient-specific cardiac regenerative medicine.
Materials and Methods
Culture and differentiation of mouse iPSCs (miPSCs)
All miPSC lines used in this study were routinely maintained in standard ESC medium containing 15% FBS (Hyclone, Logan, UT, USA), 1 μmol/l non-essential amino acids, 1 mmol/l Glutamine, 100 μmol/l β-mercaptoethanol, 50 U/ml penicillin, and 50 mg/ml streptomycin on mitomycin-C-treated mouse embryonic fibroblast (MEF) feeder layers in the presence of leukemia inhibitory factor (Millipore, Billerica, MA, USA, 1 000 U/ml). Differentiation of the iPSCs was initiated by the classical hanging-drop method as described previously 29. The formed EBs were harvested 2 days later and then transferred into ultralow attachment plates (Corning, Canton, NY, USA) for 3 days of suspension culture. Then the EBs were seeded onto gelatin-coated plates for adhered culture and examinations. For large-scale generation of EBs, iPSCs were trypsinized and seeded onto non-attach petri dishes at a density of 105 cells/ml and the auto-aggregated EBs were plated onto gelatin-coated plates at day 5. For differentiation of the iPSCs in serum-free conditions, EBs were induced to form in medium containing 2.5% Knockout Serum Replacement (KSR, Invitrogen, Carlsbad, CA, USA) by hanging-drop method. BMP4 (R&D Systems, Minneapolis, MN, USA) was added from day 2-5 at 10 ng/ml to induce cardiomyocytes formation. All cytokines used were purchased from R&D Systems. AA (Sigma, St. Louis, MO, USA) was added during the entire differentiation period at 50 μg/ml unless otherwise indicated. Medium was renewed every 2-3 days. All cultivation medium/substances for cell cultures were from Invitrogen BRL if not indicated.
Culture and differentiation of hiPSCs
Undifferentiated hiPSCs 36 were maintained on inactivated MEFs at a density of 2 × 104 cells/cm2 in DMEM/F12 containing 20% KSR and 4 ng/ml bFGF (Sigma) as described previously 12. The hiPSCs were passaged onto a low-density MEF feeder layers (1.3 × 104 cells/cm2) and expanded for 3-4 days before differentiation. Colonies were then detached from the feeder layer by dispase (Invitrogen) and seeded onto ultralow attachment plates in hESCs culture medium without bFGF to induce EB formation. At day 2, the medium was replaced with differentiation medium containing 20% FBS (EB20) and the EBs were plated onto gelatin-coated plates at day 5. The FBS concentration was reduced to 5% (EB5) at day-10 and the medium was changed every 4-5 days. AA was added during the entire differentiation period at 50 μg/ml.
Reverse transcription (RT)-PCR and quantitative qRT-PCR
Total RNA was extracted from different samples using an RNeasy Plus Mini Kit (QIAGEN, Valencia, CA, USA) following the manufacturer's instructions and treated with DNAse I (Promega, Madison, WI, USA) for 15 min to eliminate the potential contamination of genomic DNA. cDNA was generated by reverse-transcribed total RNA (1 μg) using oligo (dT) primer and ReverTra Ace reverse transcriptase (Toyobo, Osaka, Japan). PCR was carried out using Taq DNA Polymerase (Takara, Shiga, Japan). The PCR primers are listed in Supplementary information, Table S3. m28s was used as endogenous control, and samples without reverse transcription were used as negative controls. Q-PCR was performed and analyzed by kinetic real-time PCR using the ABI PRISM 7900 system (Applied Biosystems, Foster City, CA, USA) with SYBR Green Realtime PCR Master Mix plus (Toyobo) for relative quantification of the indicated genes. The transcript of Gapdh was used for internal normalization. The qRT-PCR primers are listed in Supplementary information, Table S4.
Flow-cytometry analysis and cell sorting
Undifferentiated iPSCs or EBs were harvested and dissociated by Non-enzyme Cell Dissociation Buffer (Invitrogen). Samples were then stained for the presence of appropriate membrane markers including: SSEA1 (1:200; Millipore), PE-conjugated CD31 (1:200; eBioscience, San Diego, CA, USA), PE-conjugated CD41 (1:200; eBioscience) or isotype-matched negative control. Alexa Fluor 594 goat anti-mouse IgMs (1:1 000, Invitrogen) were used as secondary antibody to visualize SSEA1. To detect the intracellular antigen, cells were fixed and permeabilized by Foxp3 Staining Buffer Set (eBioscience), blocked by 5% FBS and incubated with primary antibody of cTnT (1:100; Abcam, La Jolla, CA, USA) and α-SMA (1:100, Sigma). Isotype-matched IgGs (BD Biosciences, Bedford, MA, USA) were used as negative control. DyLight 549-conjugated antibodies (Jackson ImmunoResearch, West Grove, PA, USA) were used as secondary antibody. Cells were then analyzed and quantified by flow cytometry (FACStar Plus Flow Cytometer, BD Biosciences).
For cell sorting, live cells were harvested and double-stained with APC-conjugated Flk1 (1:200, BD Biosciences) and PE-conjugated Cxcr4 (1:50, BD Biosciences). Flk1+/Cxcr4+ cells were then sorted by flow cytometry and plated onto gelatin-coated plates for proliferation determination. For differentiation assays, cells were seeded onto U-bottom ultralow attachment 96-well plates (Corning) at a density of 5 000 cells/well to induce the formation of reaggregates in OP9 stroma cells-conditioned medium containing 5% FBS, 100 ng/ml DKK1 (R&D Systems), and 10 ng/ml VEGF (R&D Systems). Cardiac differentiation efficiency was estimated by flow cytometry at differentiation day 15 (10 days after sorting). For cardiomyocytes purification, cells were dispersed and stained by 10 nmol/l TMRM (Invitrogen) with stirring for 30 min, then analyzed and sorted by flow cytometry 33.
Immunocytochemical staining analysis
ALP activity was analyzed by staining with an ALP substrate kit III (Vector Laboratories, Burlingame, CA, USA) according to the manufacturer's instructions. Immunostaining assays were performed according to the protocol described before 43. Briefly, cells were fixed with 4% paraformaldehyde, permeabilized in 0.3% Triton X-100 (Sigma), blocked in 10% normal goat serum (Vector Laboratories) and then incubated with primary antibodies against Oct4 (1:200), SSEA1 (1:200; Millipore), α-actinin (1:300; Sigma), cTnT (1:300; Abcam), and Col IV (1:200; Abcam) in 4 °C overnight and detected by Alexa Fluor 594 goat anti-mouse IgMs, and DyLight 488- or DyLight 549-conjugated secondary antibodies. Nuclei were stained with Hoechst33258 (Sigma) and staining with normal goat serum was used to be a negative control. A Nikon TS100 fluorescence microscope or Leica TCS SP2 confocal laser-scanning microscope was used for slide observing and image capture.
Plasmid construction and cell transfection
siRNAs constructs in the pLKO.1-Puro plasmid system for lentivirus-mediated gene knockdown were obtained from Sigma. siRNA sequence were obtained from TRC Library Database (Sigma) and listed in Supplementary information, Table S5. Viral production and infection were performed according to standard protocol. Puromycin selection was applied continuously during all subsequent cell culture including differentiation.
Proliferation and apoptosis assays
Proliferation status of the cells was determined by measuring the incorporation of BrdU. Cells were incubated with 100 μmol/l BrdU (Sigma) and BrdU labeling was detected by confocal laser scanning microscope or flow cytometry using an FITC or APC-conjugated anti-BrdU antibody (BD Biosciences), following the immunostaining protocols. Staining of samples without BrdU addition was used as negative control. Double staining of BrdU with Nkx2-5 and Mef2c was performed by Nkx2-5 (1:100; Santa Cruz Biotechnology, Santa Cruz, CA, USA) and Mef2c (1:100; Cell Signaling, Beverly, MA, USA) antibody. Signal inhibitors used in this assay were 10 μmol/l JNK inhibitor SP600125 (Calbiochem, Gibbstown, NJ, USA), 50 μmol/l JAK inhibitors AG490 (Sigma), 20 μmol/l PI3K inhibitor Wortmannin (Calbiochem), 10 μmol/l p38MAPK inhibitor SB203580 (Calbiochem), and 1 μmol/l MEK inhibitor PD0325901 (Stemgent, San Diego, CA, USA) according to previous publication 44.
To determine the apoptosis status of the cells, TUNEL staining was performed with the in situ Cell Death Detection kit (Roche, Mannheim, Germany) according to the manufacturer's instruction. Annexin V-PI double-stainings performed with PI (0.5 μg/ml) and APC-labeled Annexin V antibody (1:20; BD Biosciences) were further used to evaluate the apoptosis and necrosis levels. Cells were analyzed and quantified by flow cytometry.
Whole cell patch clamp
Whole cell patch clamps using EPC-10 amplifier (Heka Electronics, Bellmore, NY, USA) in current clamp mode were used to record APs in spontaneously beating iPS-CMs following the method described previously 43. For AP recording, the pipette electrode (2∼6 MΩ) were filled with a solution containing (mmol/l): 50 KCl, 80 K-Asparate, 5 MgCl2, 5 EGTA, 10 Hepes, 5 Na2ATP (pH 7.2 adjusted with KOH); the extracellular bathing solution containing (mmol/l): 135 NaCl, 5.4 KCl, 1.8 CaCl2, 1.0 MgCl2, 10.0 glucose and 10.0 HEPES (pH 7.4, adjusted with NaOH). The glass coverslips containing the cells were placed onto a temperature-controlled (35 °C) recording chamber and perfused continuously with extracellular solution.
Measurement of Ca2+ transients
Isolated mouse iPS-CMs were loaded with 5 μmol/l fura-2 AM and 0.45% pluronic F-127 (Molecular Probes, Eugene, OR, USA) for 10 min and washed in extracellular solution for 15 min at 35 °C room temperature. The cells were perfused continuously with extracellular solution at 35 °C. Fluorescence signals of fura-2 were detected by a Fluorescence System (IonOptix, Milton, MA). After subtraction of background fluorescence, the 340- to 380-nm fluorescence ratio (R) was recorded and analyzed by IonWizard 6.0 software (IonOptix).
Immunoblot analysis
Immunoblot analyses were performed according to the protocol described previously 45. Protein samples were size fractionated by SDS-polyacrylamide gel electrophoresis and the separated proteins were electrophoretically transferred to polyvinylindene difluoride membranes (Bio-Rad, Hercules, CA, USA). Then the membrane was incubated with primary antibodies against p-ERK1/2 (1:1 000; Santa Cruz Biotechnology), total ERK1/2 (1:1 000; Cell Signaling), RyR2 (1:1 000; Abcam), SERCA2 (1:1 000; Santa Cruz Biotechnology), Phospholamban (1:2 000; Millipore), Connexin43 (1:500; Invitrogen), and GAPDH (1:1 000; Santa Cruz Biotechnology). Horseradish peroxidase-linked anti-rabbit (1:4 000; Santa Cruz Biotechnology) or anti-mouse antibodies (1:4 000; Sigma) were used as secondary antibodies.
Statistical analysis
Data were presented as means ± SEM. Statistical significance of differences was estimated by one way ANOVA or Student's t test by SigmaStat 3.5 software (Sigma). P < 0.05 was considered significant.
Acknowledgments
This study was supported by grants from the National Basic Research Program of China (2011CB965300, 2009CB941100, 2010CB945600), the National Natural Science Foundation of China (31030050), Strategic Priority Research Program of CAS (XDA01000000), Science and Technology Committee of Shanghai Municipality (08DJ1400501), National Science and Technology Project of China (2012ZX09501-001-001), and Sanofi-Aventis Recherche & Développement-SIBS funding. We thank Dr Duanqing Pei (Guangzhou Institutes of Biomedicine and Health, China) for kindly providing the miPSC lines iPS-C5 and iPS-C12.
Footnotes
(Supplementary information is linked to the online version of the paper on the Cell Research website.)
Supplementary Material
iPSC lines used in this study
Action potential properties of iPS-CMs with or without AA-treatment
Primers used for RT-PCRs
Primers used for Q-PCRs
Target sequences of siRNAs used for specific gene knockdown experiments
Systematic screening of suitable cardiomyocyte inducers of iPSCs.
Characteristics of undifferentiated miPSCs.
AA enhances cardiac differentiation of iPSCs in auto-aggregated EBs and serum-free cultivated EBs.
AA increases the proportion of smooth muscle, endothelial but not hematopoietic progenitor cells.
Ca2+ handling properties of iPS-CMs induced with or without AA.
AA-promoted cardiogenesis is independent of its antioxidative property.
Cardiomyocyte-promoting effect of AA is partially abolished by siRNA-mediated stable silencing of type I and IV collagen (Col I and ColIV).
AA does not influence the apoptotic statues of differentiating iPSCs.
AA does not affect the differentiation potential of sorted cardiac progenitors (CPCs).
AA activates ERK signaling in a collagen synthesis-dependent manner.
A control mouse EB of iPS-3F showing the contracting area at differentiation day 10.
An ascorbic acid-treated mouse EB of iPS-3F showing the contracting area at differentiation day 10.
A control mouse EB of iPS-4F showing the contracting area at differentiation day 10.
An ascorbic acid-treated mouse EB of iPS-4F showing the contracting area at differentiation day 10.
References
- Yu J, Vodyanik MA, Smuga-Otto K, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–1920. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- Takahashi K, Tanabe K, Ohnuki M, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–872. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- Nelson TJ, Martinez-Fernandez A, Yamada S, et al. Repair of acute myocardial infarction by human stemness factors induced pluripotent stem cells. Circulation. 2009;120:408–416. doi: 10.1161/CIRCULATIONAHA.109.865154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nsair A, Maclellan WR. Induced pluripotent stem cells for regenerative cardiovascular therapies and biomedical discovery. Adv Drug Deliv Rev. 2011;63:324–330. doi: 10.1016/j.addr.2011.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong CW, Akar FG, Li RA. Translational potential of human embryonic and induced pluripotent stem cells for myocardial repair: insights from experimental models. Thromb Haemost. 2010;104:30–38. doi: 10.1160/TH10-03-0189. [DOI] [PubMed] [Google Scholar]
- Vidarsson H, Hyllner J, Sartipy P. Differentiation of human embryonic stem cells to cardiomyocytes for in vitro and in vivo applications. Stem Cell Rev. 2010;6:108–120. doi: 10.1007/s12015-010-9113-x. [DOI] [PubMed] [Google Scholar]
- Bowers SL, Banerjee I, Baudino TA. The extracellular matrix: at the center of it all. J Mol Cell Cardiol. 2010;48:474–482. doi: 10.1016/j.yjmcc.2009.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauritz C, Schwanke K, Reppel M, et al. Generation of functional murine cardiac myocytes from induced pluripotent stem cells. Circulation. 2008;118:507–517. doi: 10.1161/CIRCULATIONAHA.108.778795. [DOI] [PubMed] [Google Scholar]
- Narazaki G, Uosaki H, Teranishi M, et al. Directed and systematic differentiation of cardiovascular cells from mouse induced pluripotent stem cells. Circulation. 2008;118:498–506. doi: 10.1161/CIRCULATIONAHA.108.769562. [DOI] [PubMed] [Google Scholar]
- Zwi L, Caspi O, Arbel G, et al. Cardiomyocyte differentiation of human induced pluripotent stem cells. Circulation. 2009;120:1513–1523. doi: 10.1161/CIRCULATIONAHA.109.868885. [DOI] [PubMed] [Google Scholar]
- Zhang J, Wilson GF, Soerens AG, et al. Functional cardiomyocytes derived from human induced pluripotent stem cells. Circ Res. 2009;104:e30–e41. doi: 10.1161/CIRCRESAHA.108.192237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujiwara M, Yan P, Otsuji TG, et al. Induction and enhancement of cardiac cell differentiation from mouse and human induced pluripotent stem cells with cyclosporin-a. PLoS One. 2011;6:e16734. doi: 10.1371/journal.pone.0016734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kattman SJ, Witty AD, Gagliardi M, et al. Stage-specific optimization of activin/nodal and BMP signaling promotes cardiac differentiation of mouse and human pluripotent stem cell lines. Cell Stem Cell. 2011;8:228–240. doi: 10.1016/j.stem.2010.12.008. [DOI] [PubMed] [Google Scholar]
- Burridge PW, Thompson S, Millrod MA, et al. A universal system for highly efficient cardiac differentiation of human induced pluripotent stem cells that eliminates interline variability. PLoS One. 2011;6:e18293. doi: 10.1371/journal.pone.0018293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaichi S, Hasegawa K, Takaya T, et al. Cell line-dependent differentiation of induced pluripotent stem cells into cardiomyocytes in mice. Cardiovasc Res. 2010;88:314–323. doi: 10.1093/cvr/cvq189. [DOI] [PubMed] [Google Scholar]
- Martinez-Fernandez A, Nelson TJ, Ikeda Y, Terzic A. c-MYC independent nuclear reprogramming favors cardiogenic potential of induced pluripotent stem cells. J Cardiovasc Transl Res. 2010;3:13–23. doi: 10.1007/s12265-009-9150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xi J, Khalil M, Shishechian N, et al. Comparison of contractile behavior of native murine ventricular tissue and cardiomyocytes derived from embryonic or induced pluripotent stem cells. FASEB J. 2010;24:2739–2751. doi: 10.1096/fj.09-145177. [DOI] [PubMed] [Google Scholar]
- Kuzmenkin A, Liang H, Xu G, et al. Functional characterization of cardiomyocytes derived from murine induced pluripotent stem cells in vitro. FASEB J. 2009;23:4168–4180. doi: 10.1096/fj.08-128546. [DOI] [PubMed] [Google Scholar]
- Lam JT, Moretti A, Laugwitz KL. Multipotent progenitor cells in regenerative cardiovascular medicine. Pediatr Cardiol. 2009;30:690–698. doi: 10.1007/s00246-009-9450-1. [DOI] [PubMed] [Google Scholar]
- van Laake LW, Qian L, Cheng P, et al. Reporter-based isolation of induced pluripotent stem cell- and embryonic stem cell-derived cardiac progenitors reveals limited gene expression variance. Circ Res. 2010;107:340–347. doi: 10.1161/CIRCRESAHA.109.215434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moretti A, Bellin M, Jung CB, et al. Mouse and human induced pluripotent stem cells as a source for multipotent Isl1+ cardiovascular progenitors. FASEB J. 2010;24:700–711. doi: 10.1096/fj.09-139477. [DOI] [PubMed] [Google Scholar]
- Chin MH, Mason MJ, Xie W, et al. Induced pluripotent stem cells and embryonic stem cells are distinguished by gene expression signatures. Cell Stem Cell. 2009;5:111–123. doi: 10.1016/j.stem.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noseda M, Peterkin T, Simoes FC, Patient R, Schneider MD. Cardiopoietic factors: extracellular signals for cardiac lineage commitment. Circ Res. 2011;108:129–152. doi: 10.1161/CIRCRESAHA.110.223792. [DOI] [PubMed] [Google Scholar]
- Sato H, Takahashi M, Ise H, et al. Collagen synthesis is required for ascorbic acid-enhanced differentiation of mouse embryonic stem cells into cardiomyocytes. Biochem Biophys Res Commun. 2006;342:107–112. doi: 10.1016/j.bbrc.2006.01.116. [DOI] [PubMed] [Google Scholar]
- Takahashi T, Lord B, Schulze PC, et al. Ascorbic acid enhances differentiation of embryonic stem cells into cardiac myocytes. Circulation. 2003;107:1912–1916. doi: 10.1161/01.CIR.0000064899.53876.A3. [DOI] [PubMed] [Google Scholar]
- Chan SS, Chen JH, Hwang SM, et al. Salvianolic acid B-vitamin C synergy in cardiac differentiation from embryonic stem cells. Biochem Biophys Res Commun. 2009;387:723–728. doi: 10.1016/j.bbrc.2009.07.122. [DOI] [PubMed] [Google Scholar]
- Yang L, Soonpaa MH, Adler ED, et al. Human cardiovascular progenitor cells develop from a KDR+ embryonic-stem-cell-derived population. Nature. 2008;453:524–528. doi: 10.1038/nature06894. [DOI] [PubMed] [Google Scholar]
- Boheler KR, Czyz J, Tweedie D, et al. Differentiation of pluripotent embryonic stem cells into cardiomyocytes. Circ Res. 2002;91:189–201. doi: 10.1161/01.res.0000027865.61704.32. [DOI] [PubMed] [Google Scholar]
- Zhao XY, Li W, Lv Z, et al. iPS cells produce viable mice through tetraploid complementation. Nature. 2009;461:86–90. doi: 10.1038/nature08267. [DOI] [PubMed] [Google Scholar]
- Qin D, Gan Y, Shao K, et al. Mouse meningiocytes express Sox2 and yield high efficiency of chimeras after nuclear reprogramming with exogenous factors. J Biol Chem. 2008;283:33730–33735. doi: 10.1074/jbc.M806788200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J, Chen T, Liu X, et al. More synergetic cooperation of Yamanaka factors in induced pluripotent stem cells than in embryonic stem cells. Cell Res. 2009;19:1127–1138. doi: 10.1038/cr.2009.106. [DOI] [PubMed] [Google Scholar]
- Hattori F, Chen H, Yamashita H, et al. Nongenetic method for purifying stem cell-derived cardiomyocytes. Nat Methods. 2010;7:61–66. doi: 10.1038/nmeth.1403. [DOI] [PubMed] [Google Scholar]
- Nelson TJ, Faustino RS, Chiriac A, et al. CXCR4+/FLK-1+ biomarkers select a cardiopoietic lineage from embryonic stem cells. Stem Cells. 2008;26:1464–1473. doi: 10.1634/stemcells.2007-0808. [DOI] [PubMed] [Google Scholar]
- Aouadi M, Bost F, Caron L, et al. p38 mitogen-activated protein kinase activity commits embryonic stem cells to either neurogenesis or cardiomyogenesis. Stem Cells. 2006;24:1399–1406. doi: 10.1634/stemcells.2005-0398. [DOI] [PubMed] [Google Scholar]
- Li C, Zhou J, Shi G, et al. Pluripotency can be rapidly and efficiently induced in human amniotic fluid-derived cells. Hum Mol Genet. 2009;18:4340–4349. doi: 10.1093/hmg/ddp386. [DOI] [PubMed] [Google Scholar]
- Bu L, Jiang X, Martin-Puig S, et al. Human ISL1 heart progenitors generate diverse multipotent cardiovascular cell lineages. Nature. 2009;460:113–117. doi: 10.1038/nature08191. [DOI] [PubMed] [Google Scholar]
- Ieda M, Tsuchihashi T, Ivey KN, et al. Cardiac fibroblasts regulate myocardial proliferation through beta1 integrin signaling. Dev Cell. 2009;16:233–244. doi: 10.1016/j.devcel.2008.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespo FL, Sobrado VR, Gomez L, Cervera AM, McCreath KJ. Mitochondrial reactive oxygen species mediate cardiomyocyte formation from embryonic stem cells in high glucose. Stem Cells. 2010;28:1132–1142. doi: 10.1002/stem.441. [DOI] [PubMed] [Google Scholar]
- Duarte TL, Almeida GM, Jones GD. Investigation of the role of extracellular H2O2 and transition metal ions in the genotoxic action of ascorbic acid in cell culture models. Toxicol Lett. 2007;170:57–65. doi: 10.1016/j.toxlet.2007.02.005. [DOI] [PubMed] [Google Scholar]
- Baharvand H, Azarnia M, Parivar K, Ashtiani SK. The effect of extracellular matrix on embryonic stem cell-derived cardiomyocytes. J Mol Cell Cardiol. 2005;38:495–503. doi: 10.1016/j.yjmcc.2004.12.011. [DOI] [PubMed] [Google Scholar]
- Martinez EC, Wang J, Gan SU, et al. Ascorbic acid improves embryonic cardiomyoblast cell survival and promotes vascularization in potential myocardial grafts in vivo. Tissue Eng Part A. 2010;16:1349–1361. doi: 10.1089/ten.TEA.2009.0399. [DOI] [PubMed] [Google Scholar]
- Cao N, Liao J, Liu Z, et al. In vitro differentiation of rat embryonic stem cells into functional cardiomyocytes. Cell Res. 2011;21:1316–1331. doi: 10.1038/cr.2011.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimoji K, Yuasa S, Onizuka T, et al. G-CSF promotes the proliferation of developing cardiomyocytes in vivo and in derivation from ESCs and iPSCs. Cell Stem Cell. 2010;6:227–237. doi: 10.1016/j.stem.2010.01.002. [DOI] [PubMed] [Google Scholar]
- Liang J, Wang YJ, Tang Y, et al. Type 3 inositol 1,4,5-trisphosphate receptor negatively regulates apoptosis during mouse embryonic stem cell differentiation. Cell Death Differ. 2010;17:1141–1154. doi: 10.1038/cdd.2009.209. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
iPSC lines used in this study
Action potential properties of iPS-CMs with or without AA-treatment
Primers used for RT-PCRs
Primers used for Q-PCRs
Target sequences of siRNAs used for specific gene knockdown experiments
Systematic screening of suitable cardiomyocyte inducers of iPSCs.
Characteristics of undifferentiated miPSCs.
AA enhances cardiac differentiation of iPSCs in auto-aggregated EBs and serum-free cultivated EBs.
AA increases the proportion of smooth muscle, endothelial but not hematopoietic progenitor cells.
Ca2+ handling properties of iPS-CMs induced with or without AA.
AA-promoted cardiogenesis is independent of its antioxidative property.
Cardiomyocyte-promoting effect of AA is partially abolished by siRNA-mediated stable silencing of type I and IV collagen (Col I and ColIV).
AA does not influence the apoptotic statues of differentiating iPSCs.
AA does not affect the differentiation potential of sorted cardiac progenitors (CPCs).
AA activates ERK signaling in a collagen synthesis-dependent manner.
A control mouse EB of iPS-3F showing the contracting area at differentiation day 10.
An ascorbic acid-treated mouse EB of iPS-3F showing the contracting area at differentiation day 10.
A control mouse EB of iPS-4F showing the contracting area at differentiation day 10.
An ascorbic acid-treated mouse EB of iPS-4F showing the contracting area at differentiation day 10.