Abstract
Aims
Cannabis and tobacco use and misuse frequently co-occur. This review examines the epidemiological evidence supporting the lifetime co-occurrence of cannabis and tobacco use and outlines the mechanisms that link these drugs to each other. Mechanisms include (a) shared genetic factors; (b) shared environmental influences, including (c) route of administration (via smoking), (d) co-administration and (e) models of co-use. We also discuss respiratory harms associated with co-use of cannabis and tobacco, overlapping withdrawal syndromes and outline treatment implications for cooccurring use.
Methods
Selective review of published studies.
Results
Both cannabis and tobacco use and misuse are influenced by genetic factors and a proportion of these genetic factors influence both cannabis and tobacco use and misuse. Environmental factors such as availability play an important role, with economic models suggesting a complementary relationship where increases in price of one drug decrease the use of the other. Route of administration and smoking cues may contribute to their sustained use. Similar withdrawal syndromes, with many symptoms in common, may have important treatment implications. Emerging evidence suggests that dual abstinence may predict better cessation outcomes, yet empirically researched treatments tailored for co-occurring use are lacking.
Conclusion
There is accumulating evidence that some mechanisms linking cannabis and tobacco use are distinct from those contributing to co-occurring use of drugs in general. There is an urgent need for research to identify the underlying mechanisms and harness their potential etiological implications to tailor treatment options for this serious public health challenge.
Keywords: Cannabis, Tobacco, Nicotine, Marijuana, Genetics, Treatment, Policy, Co-administration
Introduction
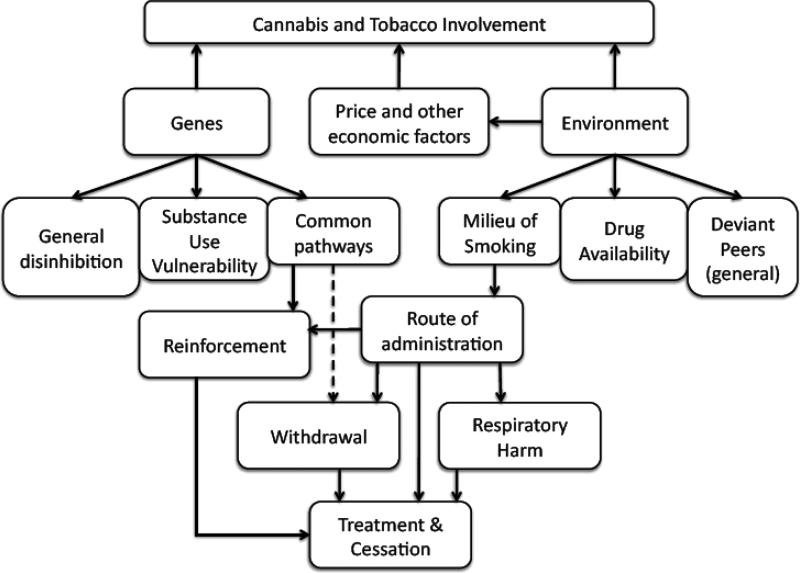
According to the CDC, tobacco kills more people worldwide than HIV, tuberculosis and malaria combined (1;2). One in 5 deaths in the U.S. are attributable to cigarette smoking (1) and over 27.4% of the U.S. population aged 12 and older reported past month use of a tobacco product, primarily cigarette smoking, in 2010 (3). Cannabis (marijuana) remains the most commonly used illicit drug in most developed nations (4). Rates in the U.S. have been stable (5) with recent trends indicating a slight increase, especially in youth (6). Compared with 2002, when 6.2% of those aged 12 and older in the U.S. reported past month cannabis use, 6.9% reported past month use in 2010 (3). In Australia, while population trends also indicate a similar increase from 9.1% in 2007 to 10.3% in 2010, recent cannabis use appears to have declined in youth since 1998 (7). Despite cross-national variations in rates of use, cannabis smoking has been and continues to be associated with adverse effects on school, employment, relationships, cognitive processing, mental health, health (primarily respiratory), and health-care utilization (8). Independently, each of these psychoactive substances is associated, to varying degrees, with considerable morbidity (9;10). However, given these associated harms, what is perhaps most alarming is that the use of cannabis and tobacco (primarily as tobacco cigarettes) frequently co-occurs across the lifespan (11;12). In this review, we discuss lifetime co-occurrence, which indicates the use and misuse of cannabis and tobacco at any point (and not necessarily at the same time). Discussion of the implications of simultaneous use (i.e. used on the same occasion) and co-administration (e.g. mulling – adding tobacco to cannabis joints, or blunts – rolling cannabis in cigar paper) is also presented. The extent of and mechanisms underlying the co-occurring use of these psychoactive substances, the consequences, and the treatment implications remain research questions of considerable interest. Figure 1 provides an overview of these various mechanisms - we discuss (a) the epidemiology of lifetime co-occurrence of cannabis and tobacco use; (b) the mechanisms underlying lifetime co-occurring use, including shared genetic and environmental factors and economic factors; (c) route of administration as a contributing factor; (d) respiratory complications associated with co-occurring use; (e) overlapping withdrawal features; and (f) treatment approaches for smokers with cannabis problems and cannabis users with nicotine dependence.
FIGURE 1.
Overview of mechanisms contributing to the lifetime co-occurrence of cannabis and tobacco use.
Epidemiology
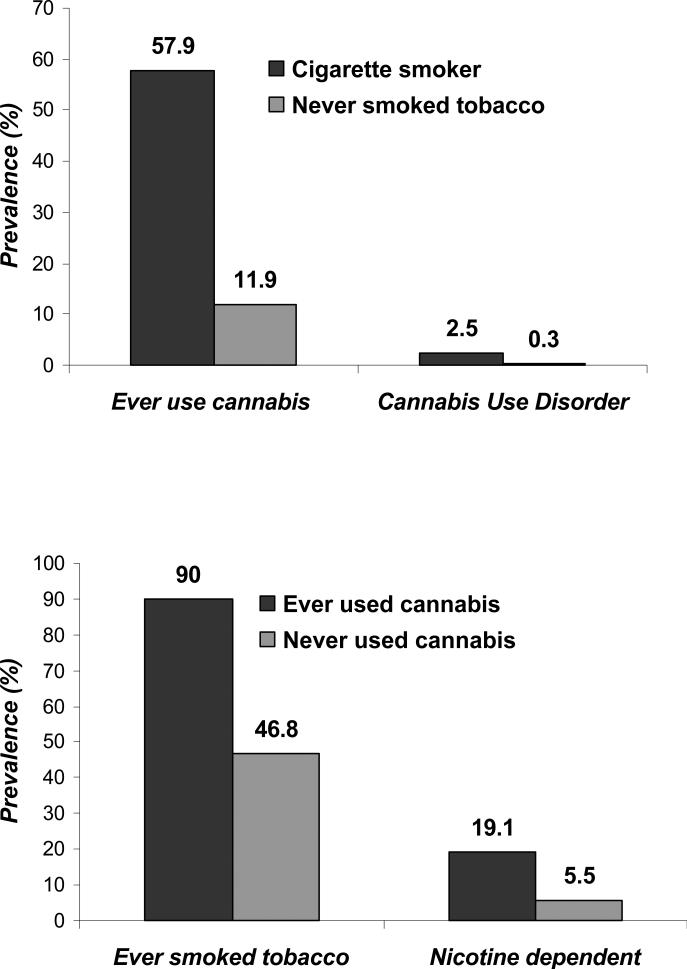
Figure 2 shows the extent of lifetime co-occurring cannabis and tobacco use in the United States, based on data collected by the National Household Survey on Drug Use and Health in 2009 (NSDUH, estimated using available data: http://www.icpsr.umich.edu/icpsrweb/SAMHDA/studies/29621). In the U.S. population aged 12 and older, lifetime prevalence of cigarette smoking was 60.6% for females and 69.3% for males. Cannabis use was reported by 37.1% of females and 46.4% of males. Importantly, 57.9% of cigarette smokers (compared with 11.9% of non smokers) reported a lifetime history of cannabis use while 90% of cannabis users (vs. 46.8% of nonusers) reported being cigarette smokers at some point during their lifetime. Similarly elevated rates of recent (not lifetime) nicotine dependence in cannabis users and cannabis use disorders in cigarette smokers are noted (Figure 2). Additionally, both disorders co-occur with 4.9% (vs. 1.2%) of those with past month nicotine dependence reporting past year cannabis use disorders and 37.5% (vs. 12.9%) of those with cannabis use disorders meeting criteria for nicotine dependence.
FIGURE 2.
Prevalence of cannabis use, cigarette smoking, cannabis use disorders (past 12 months) and nicotine dependence (based on the Fagerstrom Test of Nicotine Dependence (130)) in those aged 12 and older from the 2009 National Household Survey of Drug Use and Health (NSDUH)(5). For instance, 57.9% of cigarette smokers (including former smokers) report ever using cannabis compared with 11.9% of those who have never smoked cigarettes. Nicotine dependence based on Fagerstrom Test for Nicotine Dependence. Both cannabis use disorder (abuse/dependence) and nicotine dependence are recent.
Mechanisms of Co-Occurring Use
As indicated by Figure 2 and the literature (13), most cannabis users report a lifetime history of cigarette smoking. Cigarette smoking, however, is commonly reported in users of a variety of illicit psychoactive drugs (e.g. in NSDUH, over 90% of cocaine and methamphetamine users report cigarette smoking). Nonetheless, the co-occurring use of cannabis and tobacco may extend beyond the mechanisms underlying general co-use of substances. In the following sections, we describe evidence accumulating from the literature on the putative mechanisms connecting cannabis and tobacco use – an overview may be found in Figure 1.
Gateways and Reverse Gateways
A gateway drug is distinguished by sequence (gateway drug is used prior to other drugs), association (use of the gateway drug is associated with an increased likelihood of using other drugs) and, controversially, causation (use of the gateway drug has a causal influence on use of other drugs) (14;15). Historically, while the most frequent debate surrounds the role of cannabis as a gateway drug for other illicit psychoactive substances, cigarette smoking may serve as a gateway drug for cannabis use. For example, Yu and Williford (16), in their study of 16-24 year olds found that alcohol and cigarettes served as a gateway to cannabis use. Even in former daily smokers, risk of developing cannabis dependence is elevated (17) suggesting that tobacco exposure, particularly cigarette smoking increases the likelihood of cannabis use (18). These findings require further study, particularly to examine the potential role of confounders, such as conduct problems and other externalizing psychopathology (18).
To some extent, sequence of drug use reflects ease of access and youth may use cigarettes and tobacco prior to cannabis due to its availability. However, there is now growing support for reverse gateways (the use of cannabis prior to and increasing the risk for tobacco use) (19-21). Patton and colleagues (22) found that, while a majority of teenagers smoked cigarettes prior to experimenting with cannabis, in a subset, first use of cannabis preceded onset of cigarette smoking, representing a reversal of the conventional sequence (23;24). Whether these individuals represent a unique group or whether growing evidence for reverse gateways reflects increasing ease of access to cannabis relative to cigarettes, sale of which to minors may now be more stringently monitored, remains to be investigated.
Escalation of use in reverse gateways
While gateways and reverse gateways have traditionally referred to substance initiation, there is also overwhelming support for associations between cannabis use and escalation of tobacco involvement. In the study by Patton and colleagues (22), daily cannabis use was associated with a 3.6-fold increase in nicotine dependence. In data from the U.S., past month cannabis use was associated with a more rapid transition into daily smoking and nicotine dependence (25) (26).
Based on these epidemiological trends, there has been increasing research into the factors that contribute to co-occurring use and misuse of cannabis and tobacco. Perhaps the strongest and most consistent contributor to co-occurring cannabis and tobacco use are shared genetic influences.
Shared genetic predispositions
Individual differences in tobacco use (or, smoking initiation, heritability, h2=75%), cannabis use (h2=48%), nicotine dependence (h2=60%) and cannabis abuse/dependence (h2=50-60%) are partly attributable to genetic factors (or heritability, h2) (27;28). There is robust evidence from twin studies suggesting that these heritable influences on tobacco and cannabis use and misuse overlap with each other, with liability to use and misuse of other psychoactive substances and with a general vulnerability to externalizing behaviors.
A general liability to externalizing problems
Consistent with a problem behavior model (29), the earliest studies investigated genetic factors that also played a role in the etiology of impulsivity and conduct disorder (30). Recently, Hicks and colleagues (31) found that genetic factors for externalizing problems also influence cannabis and tobacco misuse indicating that, to some degree, the genetic underpinnings of cannabis and tobacco use are attributable to a predisposition to disinhibition.
A general propensity to drug use and misuse
Additionally, a number of twin studies find that underlying all forms of substance use behavior is a shared genetic propensity to use and misuse drugs. Examining this hypothesis, Young and colleagues (32) reported that while the genetic overlap across alcohol, tobacco and cannabis use was modest (r=0.14-0.31), shared genetic influences played a significantly more prominent role when examining alcohol, tobacco and cannabis dependence symptoms (r=0.56-0.62). Expanding this to include other substances, Kendler and colleagues (33) found that an overwhelming 83% of the genetic variance in cannabis abuse/dependence symptoms was shared with genetic influences on alcohol, nicotine, caffeine and cocaine abuse/dependence. However for nicotine dependence, these shared factors were responsible for only 37% of the genetic variance. Thus, while there is consistent support for common genetic factors influencing use and misuse of multiple substances, the extent to which these general factors impact the co-occurring use and misuse of cannabis and tobacco remains unclear.
Genetic overlap between liability to tobacco and cannabis use
A few studies have specifically interrogated the genetic overlap between cannabis and tobacco involvement. In a study of U.S. twins, (34), the high correlation between cannabis and tobacco use during adolescence was primarily attributable to shared environmental factors (e.g. at age 15, RG=0 and RSE=0.75, where RG is genetic correlation and RSE is shared environmental correlation) with the role of overlapping genetic influences becoming more prominent during late adolescence and early adulthood (e.g. at age 17-19, RG=0.75 and RSE=0.25). This high degree of genetic overlap has also been found between cannabis and regular tobacco smoking (RG=0.60-0.75) (35) and between early cannabis use and nicotine dependence (RG=0.4-0.5)(36).
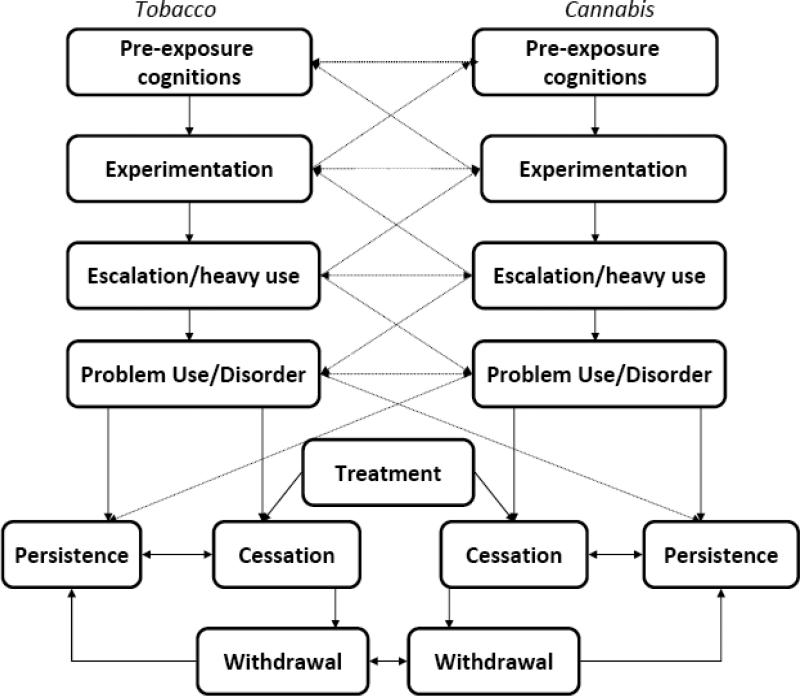
This varying degree to which shared genetic factors influence cannabis and tobacco use and misuse is partly dependent on the stage of cannabis and tobacco involvement that is under study – as shown in Figure 3. Genetic factors reflecting a predisposition to disinhibition, impulsivity, sensation-seeking and general problem behavior are more likely to contribute to early onset of cannabis and tobacco use (37;38). Maintenance of substance use followed by development of problems (e.g. cannabis abuse/dependence and nicotine dependence) is also genetically influenced, but these genes may be less related to disinhibition, and more so, to positive reinforcement and shared features of abuse/dependence (e.g. common genetic influences on cannabis and tobacco withdrawal symptoms). Two influential studies examined the impact of these potentially etiologically distinct sources of genetic overlap by examining the shared genetic influences across cannabis use, nicotine use, cannabis abuse/dependence and nicotine dependence. Importantly, these studies specified that a proportion of the genetic influences on nicotine dependence was in common with and contingent on exposure to nicotine use (39). When such a contingency was imposed on both cannabis and tobacco involvement, Neale and colleagues (40) found that, while there was considerable genetic overlap (RG=0.82) between cannabis and tobacco initiation, after accounting for this genetic overlap, the residual genetic covariance between cannabis and tobacco progression was modest (RG=0.38). In a sample of adolescent twins, after accounting for that initial genetic overlap, Huizink and colleagues (41) also found no further evidence for shared genetic influences on cannabis and tobacco progression. Both these studies concluded that shared genetic factors have the strongest influence at earlier stages of cannabis and tobacco use while genes specific to each drug are of particular importance at later stages.
FIGURE 3.
Stages of progression from drug use to drug use disorders, followed by cessation or persistence and the influential role of withdrawal and treatment on these latter stages.
Genes for cannabis and nicotine involvement
The most widely studied genetic variants for tobacco involvement are part of the cluster of genes encoding the alpha 5, alpha 3 and beta 4 subunits (CHRNA5/A3/B4) of the cholinergic nicotinic receptor (42). Specifically, rs16969968, a variant in this gene cluster that causes an amino acid coding change in the gene, has been associated with cigarettes smoked per day at p-values exceeding 10E-70 (β=1.03) (43-45). Each increasing copy of the risk allele contributed to an increase in smoking quantity of 1 cigarette per day. In addition to CHRNA5/A3/B4, genetic variants in CYP2A6, the cytochrome P450 2A6 gene, involved in the oxidation of nicotine and its metabolic product, cotinine, have also been implicated (45). Studies of cannabis involvement have seen less success. The most biologically plausible polymorphisms are in the gene encoding the cannabinoid receptor 1 (CNR1) to which endocannabinoids bind and the gene encoding fatty acid amide hydrolase (FAAH) which encodes the enzyme involved in the metabolism of cannabinoids and lipids (46). However, multiple studies have shown no relationship with these polymorphisms (47).
Which of these genes are drug-specific in their action and which genes might contribute to the genetic covariance between cannabis and tobacco involvement? It is expected that genes involved in metabolism, such as CYP2A6 (for nicotine) and FAAH (for cannabis), are highly likely to have drug-specific effects. We are unaware of any published association results for CYP2A6 and cannabis involvement or for FAAH and tobacco involvement. In contrast, given the widespread evidence for receptor cross-talk, it is intriguing to speculate that chronic use of cannabis may modify nicotinic receptor activity and vice versa. Supporting this possibility, for CNR1, Chen and colleagues (48) found multiple polymorphisms to be associated with nicotine dependence but not with smoking initiation.
Overlapping environmental factors
As with genetic influences, environmental factors influencing lifetime co-occurrence of cannabis and tobacco use may be common to a general externalizing domain, to all forms of drug use or to the co-use of cannabis and tobacco alone. Twin studies identify two sources of environmental variation and covariation in cannabis and tobacco use. The first, which is more prominent during early adolescence, includes those environmental factors that are shared by members of a twin pair – these may include familial factors (e.g. parental monitoring) that both twins are exposed to or differing environments (e.g. recreational activities) that are perceived by both twins in a similar manner. These shared environments are distinguished from the second, which is individual-specific environment (e.g. life events experienced by one twin but not the other). Individual-specific environmental exposures are uncorrelated across members of a twin pair and are found to be highly significant contributors to cannabis and tobacco use and their lifetime co-occurring use across adolescence and adulthood (34). Like genetic influences, environmental influences on cannabis and tobacco use may be broadly classified as those that impact general externalizing behaviors, those that impact all forms of drug involvement and those specifically linking cannabis and tobacco use.
Peer influences
Peer deviance is amongst the leading correlates of general externalizing psychopathology, including early onset of drug use – for instance, Lynskey and colleagues reported that vulnerability to substance use was strongly associated with self-reported affiliations with deviant peers (11). While peer affiliations are governed, in part, by the same heritable factors that influence substance use (49-51), they continue to play an environmental role in sustained drug involvement (52). While the role of peer affiliations may be viewed as tautological (i.e. we examine the characteristics of a population of drug using individuals by using population membership as a covariate), several studies report the independent effect of peers on drug use and externalizing psychopathology (53-57).
Availability, exposure opportunity and drug use
Policy oriented tobacco research indicates that a number of interventions aimed at reducing access to tobacco among youth leads to significant declines in experimentation and tobacco use (58). Such interventions include laws placing age restrictions on the purchase of tobacco products and tax-driven increases in the price (and, by implication, availability) of tobacco products. Parallel research has indicated that self-reported measures of availability and age at first opportunity to use cannabis (59;60) are strong predictors of onset of cannabis use and tobacco smokers tend to report earlier opportunities to use cannabis (61). Intriguingly, there is evidence for genetic influences on self-reported availability (62). However, whether the effects of tobacco smoking on availability of cannabis are purely environmental or include activation of genetic vulnerabilities remains unexplored.
The social milieu of smoking
Considering the conclusions from the research literatures described above it seems not unreasonable to propose that there may be aspects of the environment, including peer affiliations and access, that specifically encourage both lifetime and simultaneous use of tobacco and cannabis and that, in particular, such environments may specifically encourage smoking as a route of administration (20;63;64).
Route of Administration
An intriguing aspect of cannabis and tobacco co-use is that, for both drugs, the predominant route of administration is via inhalation. The aero-respiratory adaptations afforded by smoking one drug may facilitate the use of the other such that cigarette smokers may be more likely to continue smoking cannabis past a preliminary phase of experimentation, partly because the sensation of inhaled smoke is less unpleasant than it would be in non cigarette smokers. For instance, in a prior study of a representative U.S. sample (64), even after accounting for a lifetime history of nicotine dependence and other covariates, those using smoked forms of tobacco were more likely, compared with those using non-smoked forms, to report cannabis use and, importantly, meet criteria for cannabis use disorders. However, vanLeeuwen and colleagues (65) argue that if route of administration (i.e. smoking) were important, then early onset of tobacco use would predict the subsequent use of cannabis more strongly than early use of alcohol, which is not the case in their cohort of Dutch adolescents. We posit that route of administration may be an additional (not in lieu of) adaptive mechanism that contributes to sustained cannabis use in tobacco smokers.
If it does, how does this cross-drug adaptation occur? It is not as simple as variation in smoking topography with multiple studies failing to find any differences in inhalation patterns, lung capacity measured by breath holding, puff volume, or other characteristics (66-69) of inhaled drug use between cannabis smokers with those who smoke both cannabis and cigarettes. Smoking may serve as a cue - persistent exposure to smoking cues along with the associated pharmacological effects may well be learned, conditioned cues that can trigger use or relapse (70). There is also the possibility that cigarette smokers experience more positive subjective reactions to cannabis smoking and therefore, continue to use it. Distinct from aero-respiratory adaptation, these experiences reflect drug sensitivity, including experiences such as dizziness, giggling, a pleasurable rush or buzz and nausea (71-73), although coughing is also included. This effect may be environmental – one twin study noted that the extent to which the same genetic factors influenced subjective reactions to tobacco and cannabis was modest (74). In addition, implicit cognitive processes (i.e. an expectancy that cannabis smoking is less unpleasant, based on prior experiences with tobacco smoking) may also play a role in cross-drug adaptation. This latter hypothesis implies that, in addition to a predisposition to substance use, some individuals may have a preference for (or an absence of aversion from) smoked substances.
While it is limited, there is evidence for genetic influences on route of administration. One twin study identified variations in the extent to which heritable factors influence tobacco use by route of administration. Genetic factors explained 16% of the variance in cigarette smoking and up to 73% of the variance in dip (smokeless chewed tobacco) use while they were found to have no appreciable impact on pipe and cigar use (75). Thus, it is possible that the influence of a shared route of administration is partially governed by genetic factors.
Co-administration
Cannabis can be smoked by itself (e.g. marijuana cigarettes, or in bongs or pipes) or can be rolled with small amounts of tobacco to facilitate smoking (referred to as mulling in some countries) (20;76;77). Some studies contend that these small amounts of tobacco produce nicotine withdrawal which cannabis users stave off by sustained use of tobacco-containing cannabis preparations (78;79). Preliminary research also indicates that cannabis and tobacco are often smoked on the same occasion and that these simultaneous users are at greater risk for cannabis use disorders (80). Similar increases in cannabis involvement have been noted in those who report chasing cannabis with tobacco smoking (i.e., closely following cannabis smoking with tobacco) (81). In both those co-administering tobacco and cannabis and those smoking cigarettes and joints on the same occasion, an additional source of respiratory adaption may arise from additives in manufactured tobacco. For instance, in addition to flavorants, cigarettes typically contain compounds (e.g. salicylates) that have anti-inflammatory and anesthetic effects which may facilitate cannabis inhalation (82).
An additional form of co-administration occurs in the form of blunt smoking (83;84). Blunts are prepared by removing a majority of the tobacco from a cigar paper and rolling cannabis in it and can contain more cannabis and tobacco than other tobacco-containing cannabis preparations (85). This is consistent with the epidemiological observation of elevated rates of cannabis use disorders in blunt versus joint smokers (86). While there is a distinct ethnic sub-culture surrounding blunt usage in the U.S, Cooper and Haney (87) find that blunts produced greater increases in carbon monoxide levels and, in women, joints increased plasma tetrahydrocannabinol levels. Thus, blunt smokers may be at greater risk for the hemodynamic consequences of carbon monoxide, particularly because the relatively reduced plasma levels of tetrahydrocannabinol may delay intoxication and, consequently, prolonged blunt smoking. However, joint smokers consistently reported greater subjective liking than blunt smokers. Thus, the link between cannabis preparation and development of cannabis use disorders remains unclear.
Thus far, our discussion of the lifetime co-occurring use of cannabis and tobacco has focused on individual-specific mechanisms, both genetic and environmental. Given the strong socio-political trends that follow the use of these drugs, there is also extensive research into macro-environmental forces that may link these drugs. The next section highlights some of these economic models.
Economic factors influencing co-use
Economic models of addiction posit that examination of price elasticity – changes in patterns of use of a drug in conjunction with changes in price – can reveal important clues about the rationale for drug choice. Such studies typically classify pairs of drugs as complements (as price of one drug increases and its use correspondingly decreases, use of other drug decreases) and substitutes (as price of one drug increases, use of other drug increases). While economic studies of cannabis and cigarettes are few, there is growing support for cannabis and cigarettes serving as complements. Pacula (88) used data from the U.S. National Longitudinal Survey of Youth to report that as cigarette prices increased (and cigarette use decreased), marijuana use decreased as well, indicating complementarity. Two additional studies of U.S. data have reinforced this finding (89;90). In a similar study conducted in Australia, Cameron and Williams (91) found that a 10% monetary price increase in cannabis price resulted in a 1.32% drop in past 12 month cigarette smoking. Decriminalization had no impact on cigarette smoking nor did changes in cigarette prices influence past 12 month cannabis use.
Policy changes can exert powerful effects on expression or suppression of genetic vulnerability. For instance, Boardman and colleagues found that genetic factors played a significantly greater role in smoking cessation in those who quit after bans and restrictions on smoking had begun to be imposed. These analyses suggested that even crude indices of policy change can impact the contribution of genetic influences. In the next sections, we shift our focus from the etiology of co-occurring cannabis and tobacco involvement to a discussion of its possible consequences.
Health-related harms
The highly carcinogenic effects of nicotine and other compounds contained in cigarettes and other tobacco-related products are well recognized (92). Perhaps less well appreciated is the fact that smoked cannabis can contain more tar and polycyclic aromatic hydrocarbons than smoked tobacco (93). While its link to lung cancer is tenuous (66;94), cannabis smoking has been linked to chronic bronchitis and there is growing evidence for cannabis-related impairment of respiratory function (95). A cannabis joint can produce as much airflow obstruction as 2.5-6 tobacco cigarettes (96) and multiple population studies support the adverse respiratory effects of cannabis (97-100). Taylor and colleagues (99) found that even after adjustment for tobacco use, respiratory symptoms in young adult cannabis dependent subjects exceeded those observed in tobacco smokers smoking 1-10 cigarettes/day. Cannabis-dependent individuals experience wheezing, exercise-related shortness of breath, nocturnal wakening with chest tightness, morning sputum, coughing, chest sounds and phlegm production (100). Individuals who use both cannabis and tobacco have a markedly elevated risk of respiratory distress, compared with cannabis use or tobacco use alone (99;101). For instance, Moore and colleagues (100) found that even though those who smoked both cannabis and tobacco reported smoking as many cigarettes as those who smoked tobacco alone, there was a considerable elevation in odds of respiratory distress indicators and reduced lung functioning (101)in those who used both.
The withdrawal syndrome
Despite health-related harms, individuals continue to use cannabis and tobacco. A major barrier to successful cessation is the experience of withdrawal. Tobacco withdrawal has been well documented (102). The next iteration of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) is considering the inclusion of cannabis withdrawal as a criterion in the diagnosis of cannabis use disorders (103;104). Based on multiple clinical (105;106) and epidemiological (107;108) studies, little doubt remains in the reliability and validity of the cannabis withdrawal syndrome. However, as a majority of cannabis users also smoke tobacco, it is necessary to examine both unique and shared components of the withdrawal syndrome that emerge consequent to cessation of one or both drugs. Cannabis withdrawal is characterized by anger, aggression or irritability, nervousness or anxiety, sleep difficulties, decreased appetite or weight loss, psychomotor agitation or restlessness, depressed mood, and less commonly by physical symptoms such as stomach pain or shakes/tremors (109). Many of these withdrawal features are also noted subsequent to tobacco cessation, which has led to direct comparisons of these withdrawal syndromes (110-112). While the number of withdrawal symptoms and the symptoms themselves are equally reported across both syndromes, those experiencing cannabis withdrawal are more likely to report irritability and decreased appetite while those experiencing tobacco withdrawal are more likely to report appetite increase and craving. Importantly, the subjective experience of withdrawal severity appears comparable for both drugs, as are reports of withdrawal impeding successful cessation (112).
Concurrent cessation of tobacco and cannabis and the associated withdrawal syndrome is typically expected to be a challenging experience. In the only experimental study we know of, Vandrey and colleagues (110) found that simultaneous cessation of cannabis and tobacco, compared with withdrawal from either drug alone, was associated with greater aggression, anger and irritability, but only during day 2 of abstinence. Interestingly, comparable numbers of participants rated withdrawal associated with dual abstinence as less severe than withdrawal from either drug alone. Revisiting the role of route of administration, the authors suggest that absence of smoking cues when abstaining from both substances may reduce withdrawal severity in some individuals.
The etiology of these syndromes warrants examination, particularly from a genetic perspective. Nicotine withdrawal is heritable (113) with a proportion of these genes being distinct from those influencing other aspects of smoking. While there have been no formal tests of the univariate heritability of cannabis withdrawal, one study indicates that variance in withdrawal may be adequately captured by a factor representing general vulnerability to cannabis abuse/dependence (114). There are no studies, however, of the extent to which shared genetic influences impact tobacco and cannabis withdrawal, either the syndrome in general or individual features.
The withdrawal syndrome that emerges during simultaneous cessation has considerable implications for treatment. In the following sections, we briefly review treatment strategies and implications.
Treatment of cannabis and nicotine addiction in co-users
Published clinical trials investigating treatments for adults with cannabis use disorders suggest that approximately 50% are current tobacco smokers (115;116). For adolescents receiving treatment for cannabis, the rate of tobacco smoking appears even higher (117;118). Rates of the converse, the number of cannabis users among those seeking help with tobacco cessation is less clear, but is likely a smaller, yet substantial proportion (see Figure 1, (19)).
Tobacco Use Influences Treatment for Cannabis
Studies of teens (119;120) and adults (121) indicate that persistent tobacco use is associated with a poorer response to treatment for cannabis use disorders. For example, among teens, persistent non-tobacco smokers and those who quit tobacco use relapsed to cannabis less rapidly and showed reduced odds of relapse to cannabis compared with persistent smokers or those who initiated smoking [104]. Among adults, current tobacco smokers reported more psychosocial problems and achieved poorer cannabis abstinence outcomes than ex-smokers (121).
Cannabis Use Impacts Treatment for Tobacco
While limited, studies also suggest that cannabis use among tobacco smokers may predict poorer tobacco cessation outcomes (122-124). An epidemiological study found that cannabis use among tobacco smokers predicted persistent tobacco use 13 years later, and also was associated with a lower probability of making a tobacco quit attempt (19). In a clinical sample, cannabis use reported at baseline greatly reduced the probability of sustained tobacco abstinence at a 6-month assessment following treatment with NRT and counseling (123).
Treatment Approaches Directed at Co-Use
Multiple studies have addressed tobacco smoking in treatment-seeking alcohol or opioid-dependent patients (125;126) but research into co-treatment of cannabis and tobacco is lacking (120). Although cannabis users were included in some of these studies (e.g., (127)), few of the studies were performed in outpatient settings where most treatment for cannabis occurs, and thus, the generality of these treatments for cannabis and tobacco co-use remain unexplored. Testing tobacco cessation interventions specifically in cannabis dependent patients would seem vitally important because, as discussed above, the common route of administration and the tendency to use a mixture of cannabis and tobacco may make quitting more difficult and require tailored interventions.
Treatment Options
Briefly, alternative approaches to treating co-use of tobacco and cannabis must first determine whether to intervene on both substances simultaneously or sequentially, i.e., target one substance then the other. This issue in relation to treatment of other non-cannabis substances and tobacco has been somewhat controversial because of concern that intervening on tobacco will interfere with treatment for the other substance. However most studies suggest that simultaneous tobacco treatment does not jeopardize outcomes for treating addiction to alcohol or other illicit drugs (126). Further, as many cannabis users smoke a mixture of cannabis and tobacco or chase cannabis use with tobacco, and as conditioned cues associated with smoking both substances may trigger use of either substance, a simultaneous cessation approach with cannabis and tobacco may be most beneficial.
Specific options for treatment components to effectively address co-use of tobacco and cannabis can readily be gleaned from the extant evidence-based approaches for each individual substance. For tobacco, behavioral counseling plus medication (e.g., nicotine replacement medications, bupropion, or varenicline) is the optimal choice (128); whereas for cannabis, behavioral treatments (e.g., cognitive behavioral therapy, contingency management) are the best available option as no effective medications are yet available (129). Tailoring programs for combining these interventions have yet to be explored and tested in empirical studies.
Future directions
As is evident from this review, multiple aspects of research into the co-occurring use of cannabis and tobacco require attention. This review, in particular, highlights the importance of genetic influences on various mechanisms that contribute to and might be a consequence of co-occurring use. Despite evidence that cannabis use disorders are heritable, genetic studies have struggled to identify gene variants associated with it – studying it in the context of co-occurring smoking behaviors may facilitate these gene searches. The identification of environmental factors, including the important role of route of administration needs to be carefully examined. Importantly, these environmental factors may further modify genetic susceptibility – this requires study. Also, as shown in Figure 3, these psychoactive substances are linked at multiple stages in their progression of use – in fact, they may be irreparably coupled as early as the emergence of drug expectancies, exposure or initial reactions. Identifying the earliest stage and mechanism for their co-occurrence, following further stages of cross-drug reinforcement and delineating the genetic and environmental underpinnings of these stages will greatly facilitate prevention efforts. Finally, given these associations and overlapping withdrawal symptoms, perhaps even more than with use of alcohol or other drugs, treating tobacco at the same time as cannabis and vice versa may be beneficial to outcomes for both. Empirically based interventions have yet to address and evaluate interventions targeting both substances. Developing outpatient models that do so will likely improve public health by reducing health problems associated with continued use of either substance or their combination.
Acknowledgments
Funding: DA23668 (AA), DA15186 & DA23526 (AJB), DA18267 & DA18660 (MTL). Declaration of Interest: Dr. Agrawal receives peer-reviewed grant funding (no-cost extension) from ABMRF/The Foundation for Alcohol Research.
Reference List
- 1.Centers for Disease Control (CDC) Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses --- United States, 2000--2004. MMWR. 2008;57(45):1226–8. [PubMed] [Google Scholar]
- 2.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993 Nov 10;270(18):2207–12. [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2010 National Survey of Drug Use and Health: Summary of National Findings. SAMHSA; Rockville, MS: 2011. HHS Publication no. (SMA) 11-4658. Report No.: NSDUH series H-41. [Google Scholar]
- 4.Degenhardt L, Chiu WT, Sampson N, Kessler RC, Anthony JC, Angermeyer M, et al. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO World Mental Health Surveys. PLoS Med. 2008 Jul 1;5(7):e141. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration . Results from the 2009 National Survey of Drug Use and Health: Volume I. Summary of National Findings. Office of Applied Studies, NSDUH; Rockville, M.D.: 2010. Series H-38A, HHS Publication No. SMA 10-4856Findings. [Google Scholar]
- 6.Johnston LD, O'Malley P, Bachman JG, Schulenberg J. [11 A.D. Dec 12];Marijuana use is rising; ecstasy use is beginning to rise; and alcohol use is declining among U.S. teens. http://www monitoringthefuture org 2011 January 21; Available from: URL: http://www.monitoringthefuture.org.
- 7.Australian Institute of Health and Welfare . 2010 National Drug Strategy Household Survey Report. AIHW; Canberra: 2011. Cat no. PHE 145. Report No.: Data statistics series no. 25. [Google Scholar]
- 8.Budney AJ, Moore BA, Vandrey R. Health consequences of marijuana use. In: Brick J, editor. Medical Consequences of Drug Abuse. Haworth Press; 2008. pp. 251–82. [Google Scholar]
- 9.Centers for Disease Control (CDC) Annual smoking-attributable mortality, years of potential life lost, and economic costs-United States. MMWR. 2002;51:300–3. [PubMed] [Google Scholar]
- 10.Hall W, Pacula RL. Cannabis Use and Dependence. Cambridge University Press; Melbourne: 2003. [Google Scholar]
- 11.Lynskey MT, Fergusson DM, Horwood LJ. The origins of the correlations between tobacco, alcohol, and cannabis use during adolescence. J Child Psychol Psychiatry. 1998 Oct;39(7):995–1005. [PubMed] [Google Scholar]
- 12.Degenhardt L, Hall W, Lynskey M. Alcohol, cannabis and tobacco use among Australians: a comparison of their associations with other drug use and use disorders, affective and anxiety disorders, and psychosis. Addiction. 2001 Nov;96(11):1603–14. doi: 10.1046/j.1360-0443.2001.961116037.x. [DOI] [PubMed] [Google Scholar]
- 13.Kandel D. Stages and Pathways of Drug Involvement. Cambridge University Press; New York, NY: 2002. [Google Scholar]
- 14.Kandel D. Stages in adolescent involvement in drug use. Science. 1975;190:912–4. doi: 10.1126/science.1188374. [DOI] [PubMed] [Google Scholar]
- 15.Kandel DB. Does marijuana use cause the use of other drugs? JAMA. 2003 Jan 22;289(4):482–3. doi: 10.1001/jama.289.4.482. [DOI] [PubMed] [Google Scholar]
- 16.Yu J, Williford WR. The age of alcohol onset and alcohol, cigarette, and marijuana use patterns: an analysis of drug use progression of young adults in New York State. Int J Addict. 1992 Nov;27(11):1313–23. doi: 10.3109/10826089209047353. [DOI] [PubMed] [Google Scholar]
- 17.Patton GC, Coffey C, Carlin JB, Sawyer SM, Wakefield M. Teen smokers reach their mid twenties. J Adolesc Health. 2006 Aug;39(2):214–20. doi: 10.1016/j.jadohealth.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 18.Korhonen T, Levalahti E, Dick DM, Pulkkinen L, Rose RJ, Kaprio J, et al. Externalizing behaviors and cigarette smoking as predictors for use of illicit drugs: a longitudinal study among Finnish adolescent twins. Twin Res Hum Genet. 2010 Dec;13(6):550–8. doi: 10.1375/twin.13.6.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ford DE, Vu HT, Anthony JC. Marijuana use and cessation of tobacco smoking in adults from a community sample. Drug Alcohol Depend. 2002;67(3):243–38. doi: 10.1016/s0376-8716(02)00066-2. [DOI] [PubMed] [Google Scholar]
- 20.Amos A, Wiltshire S, Bostock Y, Haw S, McNeill A. ‘You can't go without a fag...you need it for your hash’--a qualitative exploration of smoking, cannabis and young people. Addiction. 2004 Jan;99(1):77–81. doi: 10.1111/j.1360-0443.2004.00531.x. [DOI] [PubMed] [Google Scholar]
- 21.Humfleet GL, Haas AL. Is marijuana use becoming a ‘gateway’ to nicotine dependence? Addiction. 2004 Jan;99(1):5–6. doi: 10.1111/j.1360-0443.2004.00596.x. [DOI] [PubMed] [Google Scholar]
- 22.Patton GC, Coffey C, Carlin JB, Sawyer SM, Lynskey M. Reverse gateways? Frequent cannabis use as a predictor of tobacco initiation and nicotine dependence. Addiction. 2005 Oct;100(10):1518–25. doi: 10.1111/j.1360-0443.2005.01220.x. [DOI] [PubMed] [Google Scholar]
- 23.Degenhardt L, Chiu WT, Conway K, Dierker L, Glantz M, Kalaydjian A, et al. Does the ‘gateway’ matter? Associations between the order of drug use initiation and the development of drug dependence in the National Comorbidity Study Replication. Psychol Med. 2009 Jan;39(1):157–67. doi: 10.1017/S0033291708003425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agrawal A, Scherrer JF, Lynskey M, Sartor CE, Grant JD, Haber JR, et al. Patterns of use, sequence of onsets and correlates of tobacco and cannabis. Addict Behav. 2011 doi: 10.1016/j.addbeh.2011.07.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Timberlake DS, Haberstick BC, Hopfer CJ, Bricker J, Sakai JT, Lessem JM, et al. Progression from marijuana use to daily smoking and nicotine dependence in a national sample of U.S. adolescents. Drug Alcohol Depend. 2007 May 11;88(2-3):272–81. doi: 10.1016/j.drugalcdep.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 26.Agrawal A, Madden PA, Bucholz KK, Heath AC, Lynskey MT. Transitions to regular smoking and to nicotine dependence in women using cannabis. Drug Alcohol Depend. 2008 May 1;95(1-2):107–14. doi: 10.1016/j.drugalcdep.2007.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verweij KJ, Zietsch BP, Lynskey MT, Medland SE, Neale MC, Martin NG, et al. Genetic and environmental influences on cannabis use initiation and problematic use: a meta-analysis of twin studies. Addiction. 2010 Mar;105(3):417–30. doi: 10.1111/j.1360-0443.2009.02831.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maes HH, Sullivan PF, Bulik CM, Neale MC, Prescott CA, Eaves LJ, et al. A twin study of genetic and environmental influences on tobacco initiation, regular tobacco use and nicotine dependence. Psychol Med. 2004 Oct;34(7):1251–61. doi: 10.1017/s0033291704002405. [DOI] [PubMed] [Google Scholar]
- 29.Jessor R, Jessor SL. Problem Behavior and Psychosocial Development: A Longitudinal Study. New York Academic Press; New York: 1977. [Google Scholar]
- 30.Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol. 2002 Aug;111(3):411–24. [PubMed] [Google Scholar]
- 31.Hicks BM, Schalet BD, Malone SM, Iacono WG, McGue M. Psychometric and genetic architecture of substance use disorder and behavioral disinhibition measures for gene association studies. Behav Genet. 2011 Jul;41(4):459–75. doi: 10.1007/s10519-010-9417-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Young SE, Rhee SH, Stallings MC, Corley RP, Hewitt JK. Genetic and environmental vulnerabilities underlying adolescent substance use and problem use: general or specific? Behav Genet. 2006 Jul;36(4):603–15. doi: 10.1007/s10519-006-9066-7. [DOI] [PubMed] [Google Scholar]
- 33.Kendler KS, Myers J, Prescott CA. Specificity of genetic and environmental risk factors for symptoms of cannabis, cocaine, alcohol, caffeine, and nicotine dependence 1. Arch Gen Psychiatry. 2007 Nov;64(11):1313–20. doi: 10.1001/archpsyc.64.11.1313. [DOI] [PubMed] [Google Scholar]
- 34.Kendler KS, Schmitt E, Aggen SH, Prescott CA. Genetic and environmental influences on alcohol, caffeine, cannabis, and nicotine use from early adolescence to middle adulthood. Arch Gen Psychiatry. 2008 Jun;65(6):674–82. doi: 10.1001/archpsyc.65.6.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agrawal A, Silberg JL, Lynskey MT, Maes HH, Eaves LJ. Mechanisms underlying the lifetime co-occurrence of tobacco and cannabis use in adolescent and young adult twins. Drug Alcohol Depend. 2010 Apr 1;108(1-2):49–55. doi: 10.1016/j.drugalcdep.2009.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agrawal A, Lynskey MT, Pergadia ML, Bucholz KK, Heath AC, Martin NG, et al. Early cannabis use and DSM-IV nicotine dependence: a twin study. Addiction. 2008 Nov;103(11):1896–904. doi: 10.1111/j.1360-0443.2008.02354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-use disorders: findings from the Minnesota Twin Family Study. Dev Psychopathol. 1999;11(4):869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- 38.Meyers JL, Dick DM. Genetic and environmental risk factors for adolescent-onset substance use disorders. Child Adolesc Psychiatr Clin N Am. 2010 Jul;19(3):465–77. doi: 10.1016/j.chc.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heath AC, Martin NG, Lynskey MT, Todorov AA, Madden PA. Estimating two-stage models for genetic influences on alcohol, tobacco or drug use initiation and dependence vulnerability in twin and family data. Twin Res. 2002;5(2):113–24. doi: 10.1375/1369052022983. [DOI] [PubMed] [Google Scholar]
- 40.Neale MC, Harvey E, Maes HH, Sullivan PF, Kendler KS. Extensions to the modeling of initiation and progression: applications to substance use and abuse. Behav Genet. 2006 Jul;36(4):507–24. doi: 10.1007/s10519-006-9063-x. [DOI] [PubMed] [Google Scholar]
- 41.Huizink AC, Levalahti E, Korhonen T, Dick DM, Pulkkinen L, Rose RJ, et al. Tobacco, cannabis, and other illicit drug use among finnish adolescent twins: causal relationship or correlated liabilities? J Stud Alcohol Drugs. 2010 Jan;71(1):5–14. doi: 10.15288/jsad.2010.71.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bierut LJ. Convergence of genetic findings for nicotine dependence and smoking related diseases with chromosome 15q24-25. Trends Pharmacol Sci. 2010 Jan;31(1):46–51. doi: 10.1016/j.tips.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Genome-wide meta-analyses identify multiple loci associated with smoking behavior. Nat Genet. 2010 May;42(5):441–7. doi: 10.1038/ng.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu JZ, Tozzi F, Waterworth DM, Pillai SG, Muglia P, Middleton L, et al. Meta-analysis and imputation refines the association of 15q25 with smoking quantity. Nat Genet. 2010 May;42(5):436–40. doi: 10.1038/ng.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thorgeirsson TE, Gudbjartsson DF, Surakka I, Vink JM, Amin N, Geller F, et al. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat Genet. 2010 May;42(5):448–53. doi: 10.1038/ng.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Agrawal A, Lynskey MT. Candidate genes for cannabis use disorders: findings, challenges and directions. Addiction. 2009 Apr;104(4):518–32. doi: 10.1111/j.1360-0443.2009.02504.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Agrawal A, Lynskey MT. Candidate genes for cannabis use disorders: findings, challenges and directions. Addiction. 2009 Apr;104(4):518–32. doi: 10.1111/j.1360-0443.2009.02504.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen X, Williamson VS, An SS, Hettema JM, Aggen SH, Neale MC, et al. Cannabinoid receptor 1 gene association with nicotine dependence. Arch Gen Psychiatry. 2008 Jul;65(7):816–24. doi: 10.1001/archpsyc.65.7.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kendler KS, Jacobson KC, Gardner CO, Gillespie N, Aggen SA, Prescott CA. Creating a social world: a developmental twin study of peer-group deviance. Arch Gen Psychiatry. 2007 Aug;64(8):958–65. doi: 10.1001/archpsyc.64.8.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gillespie NA, Neale MC, Jacobson K, Kendler KS. Modeling the genetic and environmental association between peer group deviance and cannabis use in male twins. Addiction. 2009 Mar;104(3):420–9. doi: 10.1111/j.1360-0443.2008.02457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Button TM, Stallings MC, Rhee SH, Corley RP, Boardman JD, Hewitt JK. Perceived peer delinquency and the genetic predisposition for substance dependence vulnerability. Drug Alcohol Depend. 2009 Feb 1;100(1-2):1–8. doi: 10.1016/j.drugalcdep.2008.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Agrawal A, Balasubramanian S, Smith EK, Madden PA, Bucholz KK, Heath AC, et al. Peer substance involvement modifies genetic influences on regular substance involvement in young women. Addiction. 2010 Jun 21; doi: 10.1111/j.1360-0443.2010.02993.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Henry KL. Low prosocial attachment, involvement with drug-using peers, and adolescent drug use: a longitudinal examination of mediational mechanisms. Psychol Addict Behav. 2008 Jun;22(2):302–8. doi: 10.1037/0893-164X.22.2.302. [DOI] [PubMed] [Google Scholar]
- 54.Creemers HE, Dijkstra JK, Vollebergh WA, Ormel J, Verhulst FC, Huizink AC. Predicting life-time and regular cannabis use during adolescence; the roles of temperament and peer substance use: the TRAILS study. Addiction. 2010 Apr;105(4):699–708. doi: 10.1111/j.1360-0443.2009.02819.x. [DOI] [PubMed] [Google Scholar]
- 55.Korhonen T, Huizink AC, Dick DM, Pulkkinen L, Rose RJ, Kaprio J. Role of individual, peer and family factors in the use of cannabis and other illicit drugs: a longitudinal analysis among Finnish adolescent twins. Drug Alcohol Depend. 2008 Sep 1;97(1-2):33–43. doi: 10.1016/j.drugalcdep.2008.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Agrawal A, Lynskey MT, Bucholz KK, Madden PA, Heath AC. Correlates of cannabis initiation in a longitudinal sample of young women: the importance of peer influences. Prev Med. 2007 Jul;45(1):31–4. doi: 10.1016/j.ypmed.2007.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guxens M, Nebot M, Ariza C, Ochoa D. Factors associated with the onset of cannabis use: a systematic review of cohort studies. Gac Sanit. 2007 May;21(3):252–60. doi: 10.1157/13106811. [DOI] [PubMed] [Google Scholar]
- 58.Wakefield M, Chaloupka F. Effectiveness of comprehensive tobacco control programmes in reducing teenage smoking in the USA. Tob Control. 2000 Jun;9(2):177–86. doi: 10.1136/tc.9.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wagner FA, Anthony JC. Into the world of illegal drug use: exposure opportunity and other mechanisms linking the use of alcohol, tobacco, marijuana, and cocaine. Am J Epidemiol. 2002 May 15;155(10):918–25. doi: 10.1093/aje/155.10.918. [DOI] [PubMed] [Google Scholar]
- 60.Wilcox HC, Wagner FA, Anthony JC. Exposure opportunity as a mechanism linking youth marijuana use to hallucinogen use. Drug Alcohol Depend. 2002 Apr 1;66(2):127–35. doi: 10.1016/s0376-8716(01)00191-0. [DOI] [PubMed] [Google Scholar]
- 61.Wagner FA, Anthony JC. Into the world of illegal drug use: exposure opportunity and other mechanisms linking the use of alcohol, tobacco, marijuana, and cocaine. Am J Epidemiol. 2002 May 15;155(10):918–25. doi: 10.1093/aje/155.10.918. [DOI] [PubMed] [Google Scholar]
- 62.Gillespie NA, Kendler KS, Prescott CA, Aggen SH, Gardner CO, Jr., Jacobson K, et al. Longitudinal modeling of genetic and environmental influences on self-reported availability of psychoactive substances: alcohol, cigarettes, marijuana, cocaine and stimulants. Psychol Med. 2007 Jul;37(7):947–59. doi: 10.1017/S0033291707009920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Highet G. The role of cannabis in supporting young people's cigarette smoking: a qualitative exploration. Health Educ Res. 2004 Dec;19(6):635–43. doi: 10.1093/her/cyg089. [DOI] [PubMed] [Google Scholar]
- 64.Agrawal A, Lynskey MT. Tobacco and cannabis co-occurrence: does route of administration matter? Drug Alcohol Depend. 2009 Jan 1;99(1-3):240–7. doi: 10.1016/j.drugalcdep.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.van Leeuwen AP, Verhulst FC, Reijneveld SA, Vollebergh WA, Ormel J, Huizink AC. Can the gateway hypothesis, the common liability model and/or, the route of administration model predict initiation of cannabis use during adolescence? A survival analysis--the TRAILS study. J Adolesc Health. 2011 Jan;48(1):73–8. doi: 10.1016/j.jadohealth.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 66.Tashkin DP. Smoked marijuana as a cause of lung injury. Monaldi Arch Chest Dis. 2005 Jun;63(2):93–100. doi: 10.4081/monaldi.2005.645. [DOI] [PubMed] [Google Scholar]
- 67.Nemeth-Coslett R, Henningfield JE, O'Keeffe MK, Griffiths RR. Effects of marijuana smoking on subjective ratings and tobacco smoking. Pharmacol Biochem Behav. 1986 Sep;25(3):659–65. doi: 10.1016/0091-3057(86)90156-5. [DOI] [PubMed] [Google Scholar]
- 68.Aung AT, Pickworth WB, Moolchan ET. History of marijuana use and tobacco smoking topography in tobacco-dependent adolescents. Addict Behav. 2004 Jun;29(4):699–706. doi: 10.1016/j.addbeh.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 69.Simmons MS, Tashkin DP. The relationship of tobacco and marijuana smoking characteristics. Life Sci. 1995;56(23-24):2185–91. doi: 10.1016/0024-3205(95)00206-l. [DOI] [PubMed] [Google Scholar]
- 70.Niaura R, Shadel WG, Abrams DB, Monti PM, Rohsenow DJ, Sirota A. Individual differences in cue reactivity among smokers trying to quit: effects of gender and cue type. Addict Behav. 1998 Mar;23(2):209–24. doi: 10.1016/s0306-4603(97)00043-9. [DOI] [PubMed] [Google Scholar]
- 71.Pomerleau OF, Pomerleau CS, Namenek RJ. Early experiences with tobacco among women smokers, ex-smokers, and never-smokers. Addiction. 1998 Apr;93(4):595–9. doi: 10.1046/j.1360-0443.1998.93459515.x. [DOI] [PubMed] [Google Scholar]
- 72.Fergusson DM, Horwood LJ, Lynskey MT, Madden PA. Early reactions to cannabis predict later dependence. Arch Gen Psychiatry. 2003 Oct;60(10):1033–9. doi: 10.1001/archpsyc.60.10.1033. [DOI] [PubMed] [Google Scholar]
- 73.Lyons MJ, Toomey R, Meyer JM, Green AI, Eisen SA, Goldberg J, et al. How do genes influence marijuana use? The role of subjective effects. Addiction. 1997 Apr;92(4):409–17. [PubMed] [Google Scholar]
- 74.Haberstick BC, Zeiger JS, Corley RP, Hopfer CJ, Stallings MC, Rhee SH, et al. Common and drug-specific genetic influences on subjective effects to alcohol, tobacco and marijuana use. Addiction. 2011 Jan;106(1):215–24. doi: 10.1111/j.1360-0443.2010.03129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schmitt JE, Prescott CA, Gardner CO, Neale MC, Kendler KS. The differential heritability of regular tobacco use based on method of administration. Twin Res Hum Genet. 2005 Feb;8(1):60–2. doi: 10.1375/1832427053435346. [DOI] [PubMed] [Google Scholar]
- 76.Akre C, Michaud PA, Berchtold A, Suris JC. Cannabis and tobacco use: where are the boundaries? A qualitative study on cannabis consumption modes among adolescents. Health Educ Res. 2010 Feb;25(1):74–82. doi: 10.1093/her/cyp027. [DOI] [PubMed] [Google Scholar]
- 77.Belanger RE, Akre C, Kuntsche E, Gmel G, Suris JC. Adding Tobacco to Cannabis--Its Frequency and Likely Implications. Nicotine Tob Res. 2011 Mar 31; doi: 10.1093/ntr/ntr043. [DOI] [PubMed] [Google Scholar]
- 78.van Beurden EK, Zask A, Passey M, Kia AM. The Mull Hypothesis: is cannabis use contributing to high tobacco use prevalence among young North Coast males? N S W Public Health Bull. 2008 Mar;19(3-4):72–4. doi: 10.1071/nb07052. [DOI] [PubMed] [Google Scholar]
- 79.Burns CB, Ivers RG, Lindorff KJ, Clough AR. Cannabis: a Trojan horse for nicotine? Aust N Z J Public Health. 2000 Dec;24(6):637. doi: 10.1111/j.1467-842x.2000.tb00533.x. [DOI] [PubMed] [Google Scholar]
- 80.Agrawal A, Lynskey MT, Madden PA, Pergadia ML, Bucholz KK, Heath AC. Simultaneous cannabis and tobacco use and cannabis-related outcomes in young women. Drug Alcohol Depend. 2009 Apr 1;101(1-2):8–12. doi: 10.1016/j.drugalcdep.2008.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ream GL, Benoit E, Johnson BD, Dunlap E. Smoking tobacco along with marijuana increases symptoms of cannabis dependence. Drug Alcohol Depend. 2008 Jun 1;95(3):199–208. doi: 10.1016/j.drugalcdep.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rabinoff M, Caskey N, Rissling A, Park C. Pharmacological and chemical effects of cigarette additives. Am J Public Health. 2007 Nov;97(11):1981–91. doi: 10.2105/AJPH.2005.078014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kelly BC. Bongs and blunts: notes from a suburban marijuana subculture. J Ethn Subst Abuse. 2005;4(3-4):81–97. doi: 10.1300/J233v04n03_04. [DOI] [PubMed] [Google Scholar]
- 84.Golub AL, Johnson BD. Cohort changes in illegal drug use among arrestees in Manhattan: from the Heroin Injection Generation to the Blunts Generation. Subst Use Misuse. 1999 Nov;34(13):1733–63. doi: 10.3109/10826089909039425. [DOI] [PubMed] [Google Scholar]
- 85.Mariani JJ, Brooks D, Haney M, Levin FR. Quantification and comparison of marijuana smoking practices: blunts, joints, and pipes. Drug Alcohol Depend. 2011 Jan 15;113(2-3):249–51. doi: 10.1016/j.drugalcdep.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Timberlake DS. A comparison of drug use and dependence between blunt smokers and other cannabis users. Subst Use Misuse. 2009;44(3):401–15. doi: 10.1080/10826080802347651. [DOI] [PubMed] [Google Scholar]
- 87.Cooper ZD, Haney M. Comparison of subjective, pharmacokinetic, and physiological effects of marijuana smoked as joints and blunts. Drug Alcohol Depend. 2009 Aug 1;103(3):107–13. doi: 10.1016/j.drugalcdep.2009.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pacula RL. Adolescent Alcohol and Marijuana Consumption: Is There Really a Gateway Effect? National Bureau of Economic Research Working Paper. 1998:6348. [Google Scholar]
- 89.Chaloupka FJ, Pacula RL, Farrelly MC, Johnston LD, O'Malley P, Bray DF. Do Higher Cigarette Prices Encourage Youth to Use Marijuana. 1998 Report No.: 6939. [Google Scholar]
- 90.Farrelly MC, Bray JW, Zarking GA, Wendling BW, Pacula RL. The Effects of Prices and Policies on the Demand for Marijuana: Evidence from the National Household Survey of Drug Abuse. 1999 Report No.: 6940. [Google Scholar]
- 91.Cameron L, Williams J. Cannabis, Alcohol and Cigarettes: Substitutes or Complements? Economic Record. 2001;77:19–34. [Google Scholar]
- 92.Mackay J, Eriksen M, Shafey O. In: The Tobacco Atlas. Nyraid Editions Limited, editor. The American Cancer Society; 2006. [Google Scholar]
- 93.Melamede R. Cannabis and tobacco smoke are not equally carcinogenic. Harm Reduct J. 2005 Oct 18;2:21. doi: 10.1186/1477-7517-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Calabria B, Degenhardt L, Hall W, Lynskey M. Does cannabis use increase the risk of death? Systematic review of epidemiological evidence on adverse effects of cannabis use. Drug Alcohol Rev. 2010 May;29(3):318–30. doi: 10.1111/j.1465-3362.2009.00149.x. [DOI] [PubMed] [Google Scholar]
- 95.Tashkin DP. Does cannabis use predispose to chronic airflow obstruction? Eur Respir J. 2010 Jan;35(1):3–5. doi: 10.1183/09031936.00109309. [DOI] [PubMed] [Google Scholar]
- 96.Aldington S, Williams M, Nowitz M, Weatherall M, Pritchard A, McNaughton A, et al. The effects of cannabis on pulmonary structure, function and symptoms. Thorax. 2007 Jul 31; doi: 10.1136/thx.2006.077081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wu TC, Tashkin DP, Djahed B, Rose JE. Pulmonary hazards of smoking marijuana as compared with tobacco. N Engl J Med. 1988 Feb 11;318(6):347–51. doi: 10.1056/NEJM198802113180603. [DOI] [PubMed] [Google Scholar]
- 98.Sherrill DL, Krzyzanowski M, Bloom JW, Lebowitz MD. Respiratory effects of non-tobacco cigarettes: a longitudinal study in general population. Int J Epidemiol. 1991 Mar;20(1):132–7. doi: 10.1093/ije/20.1.132. [DOI] [PubMed] [Google Scholar]
- 99.Taylor DR, Poulton R, Moffitt TE, Ramankutty P, Sears MR. The respiratory effects of cannabis dependence in young adults. Addiction. 2000 Nov;95(11):1669–77. doi: 10.1046/j.1360-0443.2000.951116697.x. [DOI] [PubMed] [Google Scholar]
- 100.Moore BA, Augustson EM, Moser RP, Budney AJ. Respiratory effects of marijuana and tobacco use in a U.S. sample. J Gen Intern Med. 2005 Jan;20(1):33–7. doi: 10.1111/j.1525-1497.2004.40081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Taylor DR, Fergusson DM, Milne BJ, Horwood LJ, Moffitt TE, Sears MR, et al. A longitudinal study of the effects of tobacco and cannabis exposure on lung function in young adults. Addiction. 2002 Aug;97(8):1055–61. doi: 10.1046/j.1360-0443.2002.00169.x. [DOI] [PubMed] [Google Scholar]
- 102.Hughes JR. Effects of abstinence from tobacco: etiology, animal models, epidemiology, and significance: a subjective review. Nicotine Tob Res. 2007 Mar;9(3):329–39. doi: 10.1080/14622200701188927. [DOI] [PubMed] [Google Scholar]
- 103.Budney AJ, Hughes JR. The cannabis withdrawal syndrome. Curr Opin Psychiatry. 2006 May;19(3):233–8. doi: 10.1097/01.yco.0000218592.00689.e5. [DOI] [PubMed] [Google Scholar]
- 104.Budney AJ. Are specific dependence criteria necessary for different substances: how can research on cannabis inform this issue? Addiction. 2006 Sep;101(Suppl 1):125–33. doi: 10.1111/j.1360-0443.2006.01582.x. 125-33. [DOI] [PubMed] [Google Scholar]
- 105.Budney AJ, Moore BA, Vandrey RG, Hughes JR. The time course and significance of cannabis withdrawal. J Abnorm Psychol. 2003 Aug;112(3):393–402. doi: 10.1037/0021-843x.112.3.393. [DOI] [PubMed] [Google Scholar]
- 106.Budney AJ, Hughes JR, Moore BA, Vandrey R. Review of the validity and significance of cannabis withdrawal syndrome. Am J Psychiatry. 2004 Nov;161(11):1967–77. doi: 10.1176/appi.ajp.161.11.1967. [DOI] [PubMed] [Google Scholar]
- 107.Agrawal A, Pergadia ML, Lynskey MT. Is there evidence for symptoms of cannabis withdrawal in the national epidemiologic survey of alcohol and related conditions? Am J Addict. 2008 May;17(3):199–208. doi: 10.1080/10550490802019519. [DOI] [PubMed] [Google Scholar]
- 108.Hasin DS, Keyes KM, Alderson D, Wang S, Aharonovich E, Grant BF. Cannabis withdrawal in the United States: results from NESARC. J Clin Psychiatry. 2008 Sep;69(9):1354–63. doi: 10.4088/jcp.v69n0902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Budney AJ. Are specific dependence criteria necessary for different substances: how can research on cannabis inform this issue? Addiction. 2006 Sep;101(Suppl 1):125–33. doi: 10.1111/j.1360-0443.2006.01582.x. [DOI] [PubMed] [Google Scholar]
- 110.Vandrey RG, Budney AJ, Hughes JR, Liguori A. A within-subject comparison of withdrawal symptoms during abstinence from cannabis, tobacco, and both substances. Drug Alcohol Depend. 2008 Jan 1;92(1-3):48–54. doi: 10.1016/j.drugalcdep.2007.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Vandrey RG, Budney AJ, Moore BA, Hughes JR. A cross-study comparison of cannabis and tobacco withdrawal. Am J Addict. 2005 Jan;14(1):54–63. doi: 10.1080/10550490590899853. [DOI] [PubMed] [Google Scholar]
- 112.Budney AJ, Vandrey RG, Hughes JR, Thostenson JD, Bursac Z. Comparison of cannabis and tobacco withdrawal: severity and contribution to relapse. J Subst Abuse Treat. 2008 Dec;35(4):362–8. doi: 10.1016/j.jsat.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pergadia ML, Heath AC, Martin NG, Madden PA. Genetic analysis of DSM-IV nicotine withdrawal in adult twins. Psychol Med. 2006;36:963–72. doi: 10.1017/S0033291706007495. [DOI] [PubMed] [Google Scholar]
- 114.Gillespie NA, Kendler KS, Neale MC. Psychometric modeling of cannabis initiation and use and the symptoms of cannabis abuse, dependence and withdrawal in a sample of male and female twins. Drug Alcohol Depend. 2011 Apr. doi: 10.1016/j.drugalcdep.2011.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Budney AJ, Moore BA, Rocha HL, Higgins ST. Clinical trial of abstinence-based vouchers and cognitive-behavioral therapy for cannabis dependence. J Consult Clin Psychol. 2006 Apr;74(2):307–16. doi: 10.1037/0022-006X.4.2.307. [DOI] [PubMed] [Google Scholar]
- 116.Kadden RM, Litt MD, Kabela-Cormier E, Petry NM. Abstinence rates following behavioral treatments for marijuana dependence. Addict Behav. 2007 Jun;32(6):1220–36. doi: 10.1016/j.addbeh.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Shelef K, Diamond GS, Diamond GM, Myers MG. Changes in tobacco use among adolescent smokers in substance abuse treatment. Psychol Addict Behav. 2009 Jun;23(2):355–61. doi: 10.1037/a0014517. [DOI] [PubMed] [Google Scholar]
- 118.Vandrey R, Budney AJ, Kamon JL, Stanger C. Cannabis withdrawal in adolescent treatment seekers. Drug Alcohol Depend. 2005 May 9;78(2):205–10. doi: 10.1016/j.drugalcdep.2004.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.de Dios MA, Vaughan EL, Stanton CA, Niaura R. Adolescent tobacco use and substance abuse treatment outcomes. J Subst Abuse Treat. 2009 Jul;37(1):17–24. doi: 10.1016/j.jsat.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gray KM, Riggs PD, Min SJ, Mikulich-Gilbertson SK, Bandyopadhyay D, Winhusen T. Cigarette and cannabis use trajectories among adolescents in treatment for attention-deficit/hyperactivity disorder and substance use disorders. Drug Alcohol Depend. 2011 Sep 1;117(2-3):242–7. doi: 10.1016/j.drugalcdep.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Moore BA, Budney AJ. Abstinence at intake for marijuana dependence treatment predicts response. Drug Alcohol Depend. 2002 Aug 1;67(3):249–57. doi: 10.1016/s0376-8716(02)00079-0. [DOI] [PubMed] [Google Scholar]
- 122.Stapleton JA, Keaney F, Sutherland G. Illicit drug use as a predictor of smoking cessation treatment outcome. Nicotine Tob Res. 2009 Jun;11(6):685–9. doi: 10.1093/ntr/ntp050. [DOI] [PubMed] [Google Scholar]
- 123.Gourlay SG, Forbes A, Marriner T, Pethica D, McNeil JJ. Prospective study of factors predicting outcome of transdermal nicotine treatment in smoking cessation. BMJ. 1994 Oct 1;309(6958):842–6. doi: 10.1136/bmj.309.6958.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Humfleet G, Munoz R, Sees K, Reus V, Hall S. History of alcohol or drug problems, current use of alcohol or marijuana, and success in quitting smoking. Addict Behav. 1999 Jan;24(1):149–54. doi: 10.1016/s0306-4603(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 125.Kalman D, Kim S, DiGirolamo G, Smelson D, Ziedonis D. Addressing tobacco use disorder in smokers in early remission from alcohol dependence: the case for integrating smoking cessation services in substance use disorder treatment programs. Clin Psychol Rev. 2010 Feb;30(1):12–24. doi: 10.1016/j.cpr.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Prochaska JJ, Delucchi K, Hall SM. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. J Consult Clin Psychol. 2004 Dec;72(6):1144–56. doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- 127.Joseph AM, Nichol KL, Anderson H. Effect of treatment for nicotine dependence on alcohol and drug treatment outcomes. Addict Behav. 1993 Nov;18(6):635–44. doi: 10.1016/0306-4603(93)90017-4. [DOI] [PubMed] [Google Scholar]
- 128.U.S.Department of Heath and Human Services Treating Tobacco Use and Dependence. The Clinical Practice Guideline. 2008 accessed on. [Google Scholar]
- 129.Budney AJ, Roffman R, Stephens RS, Walker D. Marijuana dependence and its treatment. Addiction Science and Clinical Practice. 2007;4(1):4–16. doi: 10.1151/ascp07414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991 Sep;86(9):1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]