Abstract
Background and Purpose
Evaluation at Primary Stroke Centers (PSCs) has the potential to improve outcomes for patients with stroke. We looked for differences in evaluation at Joint Commission certified PSCs by race, education, income, and geography (urban vs. non-urban; southeastern stroke belt vs. non-belt).
Methods
Community-dwelling, black and white participants from the national REasons for Geographic and Racial Differences in Stroke (REGARDS) prospective population-based cohort were enrolled between 1/2003 and 10/2007. Participants were contacted at 6 month intervals for suspected stroke events. For suspected stroke events it was determined if the evaluating hospital was a certified PSC.
Results
Of 1000 suspected strokes, 204 (20.4%) were evaluated at a PSC. A smaller proportion of women than men (17.8% vs. 23.0%, p=0.04), those with a previous stroke (15.1% vs. 21.6%, p=0.04), those living in the stroke belt (14.7% vs. 27.3%, p<0.001) and in a non-urban area (9.1% vs. 23.1%, p<0.001) were evaluated at a PSC. There were no differences by race, education, or income. In multivariable analysis, subjects were less likely to be evaluated at a PSC if they lived in a non-urban area (OR=0.39, 95% CI 0.22–0.67), lived in the stroke belt (OR=0.54, 95% CI 0.38–0.77) or had a prior stroke (OR=0.46, 95% CI 0.27–0.78).
Conclusion
Disparities in evaluation by PSCs are predominately related to geographic factors but not to race, education, or low income. Despite an increased burden of cerebrovascular disease in the stroke belt, subjects there were less likely to be evaluated at certified hospitals.
Keywords: stroke centers, disparities, access to care, stroke
INTRODUCTION
Despite being both preventable and treatable, stroke remains one of the leading causes of death and disability in the United States.1 The public health burden of stroke is not evenly distributed across the United States, both among types of people as well as the places people live. Black Americans have a risk of first stroke that is twice that of white Americans with a 2–3 fold increase in age specific stroke mortality.2,3 There may be an increased burden in people below the poverty line.4 There is considerable geographic variability as well. Rural areas may have more cerebrovascular disease than urban areas, and there is a well described excess burden of stroke in the Southeastern United States, the “stroke belt.”5,6 Relatively little is known about why geographic disparities exist. Proposed explanations include differences in vascular risk factors, socioeconomic status, and access to care.5
One possible driver of geographic disparities is the variable availability of stroke care across the US. Studies have shown that organized stroke care reduces mortality after stroke.7–9 The Joint Commission (TJC), a non-profit organization that accredits healthcare organizations, began certifying Primary Stroke Centers (PSCs) in December 2003. The impact of TJC PSCs on population health is not fully understood. At the hospital level, PSCs have modestly lower 30-day mortality than non-PSCs; although, this may be attributable to baseline differences in performance rather than certification.10–12 Recent studies have demonstrated greater rt-PA utilization at TJC PSCs than non-PSCs, suggesting a benefit of certification.13,14 The Brain Attack Coalition and American Stroke Association/American Heart Association have recommended developing systems of care based upon an organized hierarchy of hospitals, similar to the US trauma system.15–17 PSCs are the basic building block of these systems and there are over 900 TJC PSCs spread across 48 states.18
Although TJC certifies PSCs, there is no oversight of which facilities apply to become PSCs. As a result, PSCs are not evenly distributed throughout the US.19 Differences in geographic accessibility may lead to disparities in realized access to PSCs. We aimed to determine if there were disparities in realized access to TJC PSCs on the basis of race, education, socioeconomic status, and geography for persons with suspected stroke events within a cohort of black and white community dwelling individuals in the United States.
METHODS
Study Design
The REasons for Geographic And Racial Differences in Stroke (REGARDS) study is a prospective, longitudinal national cohort study of adults ≥45. The study sample was recruited between January 2003 and October 2007 using mail and telephone with a 33% telephone response rate and a 49% cooperation rate. Study sampling was stratified by geography, race (non-Hispanic blacks and whites only), and sex. The study oversampled blacks and residents of the stroke belt(Alabama, Arkansas, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, and Tennessee). The study achieved a sample of 30,239; 42% were black and 56% lived in the stroke belt. Data on medical history and socioeconomic status were obtained by telephone and in-home interview, including phlebotomy, blood pressure, and anthropometry. The protocol was approved by the Institutional Review Boards at participating institutions and all participants provided informed consent. The objectives and design of REGARDS have been published in detail elsewhere.20
After enrollment, subjects were contacted by telephone at 6 month intervals to ascertain hospitalizations, emergency department visits, rehabilitation and nursing homes admissions, and deaths. Subjects were asked the reason for all medical encounters and the name of the facility where they received the majority of their evaluation and treatment. Transfers were not recorded. Medical records were obtained for suspected stroke, transient ischemic attack, death, sudden weakness, numbness, trouble speaking, loss of vision, headache, brain aneurysm, brain hemorrhage, and other stroke symptoms. For proxy reported deaths, an interview was conducted with next of kin. The present study was limited to subjects who sought care for suspected stroke events between 12/9/2005 and 1/6/2011. We limited the analysis to suspected strokes occurring after 12/5/2005 to allow time for hospitals to become certified. The 200th PSC was certified by TJC on this date. A list of all TJC certified PSCs with the date of initial certification was obtained directly from TJC on May 17th, 2011 (personal communication, TJC). At that time, data on suspected events was available until January 6th, 2011, setting the time period for the study.
Only the first suspected stroke event for each subject was used. Suspected strokes were used in the analysis rather than adjudicated strokes recognizing that people cannot reliably diagnose themselves prior to seeking care. For each suspected stroke, it was determined if the evaluating center was certified as a PSC on the date of admission and if the center would become certified by May 17th, 2011. This determination was performed blinded to all subject characteristics. Participants evaluated at outpatient clinics were categorized as evaluated at non-PSCs.
Covariates
Subjects were described in terms of sex and race. Smoking was categorized as ever vs. never by participant report. History of stroke and carotid endarterectomy prior to enrollment were obtained by participant report. Hypertension was defined as SBP>140 mm Hg or DBP >90 mm Hg or use of antihypertensive medications. Heart disease was defined as any self-reported myocardial infarction (MI), coronary artery bypass surgery, coronary angioplasty or stenting, or evidence of MI from ECG. Diabetes was defined as a fasting glucose level >126 ml/dL, non-fasting level >200 ml/dL, or self-reported medication use for glucose control. Chronic kidney disease was defined by a glomerular filtration rate <60 mL/min/1.73 m calculated using the Modification of Diet in Renal Disease equation. Socioeconomic status was described using annual household income (dichotomized to <$20,000 and >$20,000 to approximate the poverty threshold) and education (dichotomized to high school graduate or not). Geographic location was described by region and rurality. Region was dichotomized as stroke belt residence or not and rurality was dichotomized as urban or non-urban. Urban was defined by residence in a census tract that was ≥75% urban by the US Census. A significant proportion of subjects (11.8%) refused to provide income. There was minimal (<1%) missing data for all other variables.
Statistical Analysis
The primary dependent variable was PSC certification by TJC at the evaluating facility at the time of the suspected stroke event. Subjects evaluated at PSCs were compared to those evaluated atnon-PSCs using χ2 tests for categorical variables. All variables were then included in a multivariable model to determine independent associations. In addition to exploring the primary relation between exposure variables and evaluation at a TJC certified PSC, we tested for interactions between rurality and region, race and region, and rurality and race. Recognizing that it may take years for a hospital to develop the necessary resources and protocols to become certified and that there has been a dramatic increase in PSCs over time, a secondary analysis was conducted in which the outcome was evaluation at a hospital which would become certified by May 17th, 2011, rather than at the time of the event. At that time there were 835 PSCs in the United States. All analysis was conducted using SAS 9.2 (Cary, North Carolina).
RESULTS
There were 1,000 suspected strokes included in the analysis, of which 383 occurred in blacks and 617 in whites; there were 546 suspected strokes in the stroke belt and 454 outside the stroke belt. There were 204 subjects evaluated at hospitals that were TJC certified PSCs at the time of the event and 796 subjects evaluated at non-certified hospitals. A lower proportion of women than men (17.8% vs. 23.0%, p=0.04), subjects with a self-reported history of stroke prior to enrollment (15.1% vs 21.6%, p=0.04), stroke belt residents(14.7% vs. 27.3%, p<0.001), and non-urban residents (9.1% vs. 23.9%, p<0.001) were evaluated at PSCs. Complete univariate analysis is presented in Table 1.
Table 1.
Demographics, n=1000
| Total # | Evaluated at PSC (%) | P-Value | |
|---|---|---|---|
| Age | 0.39 | ||
| <65 | 289 | 18.7% | |
| ≥65 | 711 | 21.1% | |
| Race | 0.21 | ||
| Black | 383 | 22.5% | |
| White | 617 | 19.1% | |
| Sex | 0.04 | ||
| Women | 501 | 17.8% | |
| Men | 499 | 23.0% | |
| Hypertension | |||
| No | 295 | 17.6% | 0.15 |
| Yes | 702 | 21.7% | |
| Diabetes | |||
| No | 647 | 21.0% | 0.80 |
| Yes | 310 | 20.3% | |
| Chronic Kidney Disease | 0.98 | ||
| No | 764 | 20.9% | |
| Yes | 182 | 20.9% | |
| Current Smoker | 0.69 | ||
| No | 854 | 20.6% | |
| Yes | 146 | 19.2% | |
| Prior Carotid Endarterectomy | 0.57 | ||
| No | 951 | 20.3% | |
| Yes | 47 | 21.3% | |
| Prior Coronary Artery Disease | 0.27 | ||
| No | 681 | 21.6% | |
| Yes | 297 | 18.5% | |
| Prior Stroke | 0.04 | ||
| No | 809 | 21.6% | |
| Yes | 186 | 15.1% | |
| Education | 0.49 | ||
| No High School | 862 | 20.8% | |
| High School Grad | 137 | 18.2% | |
| Income | 0.52 | ||
| Income <$20,000 | 205 | 22.0% | |
| Income>$20,000 | 677 | 19.4% | |
| Region | <0.001 | ||
| Stroke Belt | 546 | 14.7% | |
| Non-Belt | 454 | 27.3% | |
| Urbanicity | <0.001 | ||
| Non-Urban | 198 | 9.1% | |
| Urban | 712 | 23.9% | |
In a multivariable logistic regression model which incorporated age, race, sex, past medical history (prior stroke, diabetes, hypertension, coronary artery disease) and geography (urban vs. non-urban, belt vs. non-belt), subjects living in non-urban areas were less likely to be evaluated at TJC PSCs(OR 0.39, 95% CI 0.22–0.67). Even after accounting for rurality, subjects residing within the stroke belt were less likely to be evaluated at a PSC (OR 0.54, 95% CI 0.38–0.77). Subjects with a prior history of stroke were also less likely to be evaluated at a PSC (OR 0.46, 95% CI 0.27–0.78). Men (OR=1.75, 95% CI 1.19–2.50), subjects with hypertension (OR=1.64, 95% CI 1.08–2.44), subjects with an income <$20,000 (OR=1.72, 95% CI 1.10–2.70), and subjects who refused to provide their income (OR=2.08, 95% CI 1.10–3.57) were more likely to be evaluated at a PSC. Full model results are presented in Table 2. There was no interaction between rurality and region (p=0.98), race and region (p=0.27), or race and rurality (p=0.40).
Table 2.
Odds of Evaluation at a PSC, multivariable analysis
| OR | 95% CI | |
|---|---|---|
| Non-urban location | 0.39 | (0.22, 0.67) |
| Stroke Belt Residence | 0.54 | (0.38, 0.77) |
| Hx of prior stroke | 0.46 | (0.27, 0.78) |
| Hx of Hypertension | 1.64 | (1.08, 2.44) |
| Black Race | 1.20 | (0.82, 1.75) |
| Male Sex | 1.75 | (1.19, 2.50) |
| No High School degree | 0.77 | (0.58, 1.32) |
| Income | ||
| >$20,000 | Ref | --- |
| <$20,000 | 1.72 | (1.10, 2.70) |
| Refused | 2.08 | (1.10, 3.57) |
Adjusted for: age, smoking, diabetes, coronary artery disease
In the secondary analysis, looking for disparities in evaluation at hospitals which would become TJC certified PSCs by May 17th, 2011, non-urban location (OR=0.38, 95% CI 0.24–0.59) and stroke belt residence (OR 0.46, 95% CI 0.34–0.63) were associated with a reduced odds of evaluation at an eventual PSC. Black race (OR 1.47, 95% CI 1.06–2.08), hypertension (OR=1.56, 95% CI 1.10–2.22), and refusal to provide income (OR 1.85, 95% CI 1.15–2.94) were associated with an increased odds of evaluation at a PSC. Sex, income <$20,000, and history of prior stroke were no longer significantly associated with evaluation at a PSC.
DISCUSSION
A health disparity is defined as a “health difference that is closely linked with social, economic, and/or environmental disadvantage.”21 Our study found that subjects living in stroke belt states were less likely to be evaluated at TJC certified PSCs, even after adjusting for rurality, confirming a significant environmental disadvantage. There were no observed disparities in access to PSCs on the basis of race, despite previously described racial differences in EMS utilization, emergency department wait time, and thrombolysis between racial groups.22 There were also no observed disparities on the basis of education, or low-income.
Access to care is a multi-dimensional concept that depends upon system level variables (e.g. organization and distribution of hospitals/physicians) and individual characteristics (e.g. socioeconomic status, attitudes toward care, trust/mistrust of providers).23–4 Accessibility, or geographic access, is the component of access which encompasses the relationship between the location of healthcare resources and the location of patients incorporating time, distance, and cost. For an unplanned, time-critical condition like stroke, geographic access is extremely important.25–26 Persons with suspected stroke need to be rapidly transported to hospitals that are prepared to efficiently evaluate them and, if the diagnosis is confirmed, administer acute therapies. Paradoxically, our results suggest that those living in areas with a high burden of stroke had less access than those living in other areas.
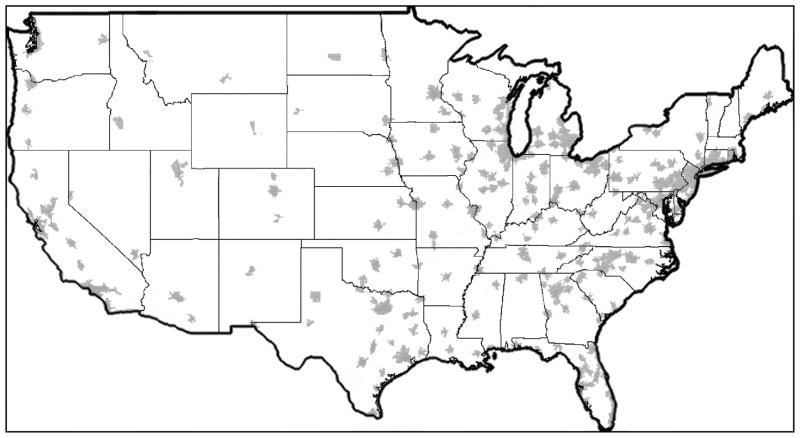
TJC certified PSCs are quickly proliferating throughout the United States. As of July 2012, 925 hospitals were certified, representing 18.6% of US non-federal short term general hospitals.27 There are 15 states which require or recognize TJC certification for PSC designation.18 Unfortunately there is significant geographic variability in access to these centers. As of November 2008, there were 11 states in the US in which < 25% of the population had 60 minute access to a TJC PSC.19 Five of those states were in the stroke belt, despite an increased burden of cerebrovascular disease in that region.5,19,28,29 Maps of PSC access in 2010 show that this disparity continues to exist, and also demonstrate the lack of TJC PSCs in rural areas of the US (Figure 1).
Figure 1.
60 Minute Access to TJC PSCs by Ground Ambulance, 2010 (continental US).
Adapted with permission from www.strokemaps.org
Currently, the decision to pursue certification occurs primarily at the individual hospital level. Optimally, certification decisions would occur at the societal level, balancing the local supply of and demand for acute stroke care.30 A system designed in this way would maximize its impact on population health. Because we did not find racial or socioeconomic disparities in access, such a system would likely benefit all people equally. Although public policy interventions should be able to improve geographic disparities by incentivizing certification of specific hospitals in areas of need, developing a comprehensive stroke care system poses several significant challenges. It may not be feasible to place a PSC in all areas with high stroke mortality rates because of limited healthcare resource availability. Telemedicine, hub-spoke complexes, and other regional partnerships may be able to increase specialized stroke care in these areas.31 Outcome measures relevant to population health must be developed to quantify the impact of the developing system of care and ensure that all patients are benefitting equally. Finally, there must be support and cooperation from professional societies, pre-hospital care providers, hospitals, and legislators. Despite these hurdles, there is some precedent for this approach. A county based acute stroke care system in Orange County, CA was recently reported to substantially improve thrombolysis rates.32 In the United Kingdom, the National Health Service dramatically overhauled the delivery of acute stroke care in London in 2010. Preliminary results suggest a major increase in thrombolysis rates with reduced length of stay and lower than average 30-day mortality.33
This study has several limitations. As in all cohort studies, there is potential for selection bias as those who participated may not be representative of the general population. Our cooperation rate compares favorably with other observational cardiovascular studies.34 The evaluating hospital in this study represents the location where patients received the majority of their care. As a result, we are unable to asses for differences in the initial point of care, transfers, and telemedicine. Telemedicine may improve access, particularly in non-urban areas; although, telestroke care often focuses on acute stroke therapy which is only one component of PSC care. We are not able to determine transfers, and use of telemedicine. whether disparities in evaluation at PSCs are changing over time as the number of certified PSCs has increased. Our secondary analysis, which looked at hospitals which would become certified PSCs by May 2011 showed the same geographic disparities as our primary analysis. Though not truly longitudinal, this suggests that geographic disparities are relatively stable. Location at stroke onset was not known so home address was used as a proxy. This should have a limited impact as prior studies show that > 75% of strokes occur at home.35 Though we hypothesize that the observed disparities are due to geographic differences in the availability of PSCs, we have not directly quantified distance or transportation time to the nearest PSC for each event. Such calculations may be informative in future work investigating access to PSCs. We defined PSCs using certification by the Joint Commission because TJC provides a standardized, nationwide definition of specialized stroke care. This ignores state-based certification programs and quality improvement initiatives, such as Get with the Guidelines. As of July 2010, 14 states have their own PSC certification process (Connecticut, Georgia, Illinois, Maryland, Massachusetts, Missouri, New Jersey, New York, North Dakota, Oklahoma, Rhode Island, Texas, Virginia, and Washington).36 Since only 1 of these states is within the stroke belt, accounting for state based stroke centers would likely increase the regional disparity which we observed. The relationship between race and access to a certified PSC may vary in urban, suburban, and rural areas or in different regions of the country. We attempted to evaluate for this by testing for interactions between race, region and rurality. These tests were not statistically significant; although, the relatively low number of events limits power to detect an interaction, even if it truly exists. Finally, it should be noted that REGARDS, by design, does not include individuals of Hispanic ethnicity and future research is needed to assess potential disparities in this population.22
In conclusion, disparities in evaluation by TJC certified PSCs are related to geographic factors including region (Southeastern stroke-belt vs. non-belt) and urbanicity (urban vs. non-urban). Importantly, participants living in stroke belt states were less likely to be evaluated at a TJC PSC, despite an increased burden of cerebrovascular disease in this area. The geographic disparities that we observed are likely attributable to a reduced number of TJC PSCs in the stroke belt and in rural areas. Public policy and systems planning should ensure specialized stroke care is rapidly accessible in areas with the greatest need.
Acknowledgments
Jean Range, MS, RN, CPHQ, Executive Director of Disease Specific Care, The Joint Commission for providing information on PSCs.
FUNDING SOURCES
The REGARDS research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health (NIH), Department of Health and Human Service. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Other funding: Mullen NHLBI K12 HL083772, Judd, Rhodes, Kleindorfer and Howard NINDS U01 NS041588, Branas and Carr AHRQ R01 HS018362, Albright AHRQ T32 HS013852-10 and NIMHD NIH P60 MD000502-08S1
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS, NIH or AHRQ.
Footnotes
DISCLOSURES
Dr. Mullen, Judd, Howard, Kasner, Branas, Rhodes, Albright and Kleindorfer: None.
Dr. Carr spends time as a Senior Policy Analyst in the Office of the Assistant Secretary for Preparedness and Response. The findings/conclusions of this report are those of the author and do not necessarily represent the views of the Department of Health and Human Services or its components
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, et al. Heart disease and stroke statistics--2012 update. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Disparities in deaths from stroke among persons aged <75 years--united states, 2002. MMWR Morb Mortal Wkly Rep. 2005;54:477–481. [PubMed] [Google Scholar]
- 3.Incidence and Prevalence. 2006 CDC Chart Book on Cardiovacsular and Lung Diseases. Bethesda, MD: National Heart, Lung, and Blood Institute; 2006. [Accessed October 31st, 2011]. Available at: http://www.nhlbi.nih.gov/resources/docs/06a_ip_chtbk.pdf. [Google Scholar]
- 4.Mensah GA. State of disparities in cardiovascular health in the united states. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 5.Howard G. Why do we have a stroke belt in the southeastern united states? A review of unlikely and uninvestigated potential causes. The American journal of the medical sciences. 1999;317:160–167. doi: 10.1097/00000441-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Adams PF, Hendershot GE, Marano MA. Current estimates from the national health interview survey, 1996. Vital Health Stat. 1999;10:1–203. [PubMed] [Google Scholar]
- 7.Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2007:CD000197. doi: 10.1002/14651858.CD000197. [DOI] [PubMed] [Google Scholar]
- 8.Seenan P, Long M, Langhorne P. Stroke units in their natural habitat: Systematic review of observational studies. Stroke. 2007;38:1886–1892. doi: 10.1161/STROKEAHA.106.480871. [DOI] [PubMed] [Google Scholar]
- 9.Smith EE, Hassan KA, Fang J, Selchen D, Kapral MK, Saposnik G. Do all ischemic stroke subtypes benefit from organized inpatient stroke care? Neurology. 2010;75:456–462. doi: 10.1212/WNL.0b013e3181ebdd8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lichtman JH, Allen NB, Wang Y, Watanabe E, Jones SB, Goldstein LB. Stroke patient outcomes in us hospitals before the start of the joint commission primary stroke center certification program. Stroke. 2009;40:3574–3579. doi: 10.1161/STROKEAHA.109.561472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xian Y, Holloway RG, Chan PS, Noyes K, Shah MN, Ting HH, et al. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011;305:373–380. doi: 10.1001/jama.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lichtman JH, Allen NB, Wang Y, Wantanabe E, Jones SB, Goldstein LB. Outcomes after ischemic stroke for hospitals with and without joint commission-certified primary stroke centers. Neurology. 2011 doi: 10.1212/WNL.0b013e31821e54f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kleindorfer DO, Mullen MT, Hogan C, Adeoye O, Khatri P, Mackey J, et al. Primary Stroke Center Certification and the Impact on Thrombolysis Use for Acute Ischemic Stroke. International Stroke Conference. 2012 (abstract) [Google Scholar]
- 14.Mullen MT, Kasner SE, Kallan MJ, Kleindorfer DO, Albright KC, Carr BG. Joint Commission Primary Stroke Centers Utilize More rt-PA in the Nationwide Inpatient Sample. JAHA. doi: 10.1161/JAHA.112.000071. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alberts MJ, Hademenos G, Latchaw RE, Jagoda A, Marler JR, Mayberg MR, et al. Recommendations for the establishment of primary stroke centers. Brain attack coalition. JAMA. 2000;283:3102–3109. doi: 10.1001/jama.283.23.3102. [DOI] [PubMed] [Google Scholar]
- 16.Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, et al. Recommendations for comprehensive stroke centers: A consensus statement from the brain attack coalition. Stroke. 2005;36:1597–1616. doi: 10.1161/01.STR.0000170622.07210.b4. [DOI] [PubMed] [Google Scholar]
- 17.Schwamm LH. Recommendations for the establishment of stroke systems of care: Recommendations from the american stroke association’s task force on the development of stroke systems. Circulation. 2005;111:1078–1091. doi: 10.1161/01.CIR.0000154252.62394.1E. [DOI] [PubMed] [Google Scholar]
- 18. [Accessed 8/28/2012];Facts About Primary Stroke Centers [Website] 2012 Available at: http://www.jointcommission.org/assets/1/18/Facts_about_Primary_Stroke_Center_Certification.pdf.
- 19.Albright KC, Branas CC, Meyer BC, Matherne-Meyer DE, Zivin JA, Lyden PD, et al. Access: Acute cerebrovascular care in emergency stroke systems. Arch Neurol. 2010;67:1210–1218. doi: 10.1001/archneurol.2010.250. [DOI] [PubMed] [Google Scholar]
- 20.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 21.Healthy People 2020 Heart Disease and Stroke Objectives. [PDF] [Accessed October 31st 2011];Healthy People 2020 Heart Disease and Stroke Summary of Objectives. 2011 Available at: www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HeartDiseaseStroke.pdf.
- 22.Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, et al. Racial-ethnic disparities in stroke care: The american experience. Stroke. 2011;42:2091–211. doi: 10.1161/STR.0b013e3182213e24. [DOI] [PubMed] [Google Scholar]
- 23.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208–220. [PMC free article] [PubMed] [Google Scholar]
- 24.Penchansky R, Thomas JW. The concept of access: Definition and relationship to consumer satisfaction. Medical care. 1981;19:127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Carr BG, Conway PH, Meisel ZF, Steiner CA, Clancy C. Defining the emergency care sensitive condition: A health policy research agenda in emergency medicine. Annals of emergency medicine. 2010;56:49–51. doi: 10.1016/j.annemergmed.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 26.Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: An updated pooled analysis of ecass, atlantis, ninds, and epithet trials. Lancet. 2010;375:1695–1703. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- 27.American Hospital Association. [Accessed January 3rd, 2012.];Fast Facts About US Hospitals [Website] 2011 Available at: http://www.aha.org/research/rc/stat-studies/101207fastfacts.pdf.
- 28.Howard G, Evans GW, Pearce K, Howard VJ, Bell RA, Mayer EJ, et al. Is the stroke belt disappearing? An analysis of racial, temporal, and age effects. Stroke. 1995;26:1153–1158. doi: 10.1161/01.str.26.7.1153. [DOI] [PubMed] [Google Scholar]
- 29.Perry HM, Roccella EJ. Conference report on stroke mortality in the southeastern united states. Hypertension. 1998;31:1206–1215. doi: 10.1161/01.hyp.31.6.1206. [DOI] [PubMed] [Google Scholar]
- 30.Leira EC, Fairchild G, Segre AM, Rushton G, Froehler MT, Polgreen PM. Primary stroke centers should be located using maximal coverage models for optimal access. Stroke. 2012;43:2417–2422. doi: 10.1161/STROKEAHA.112.653394. [DOI] [PubMed] [Google Scholar]
- 31.Kazley AS, Wilkerson RC, Jauch E, Adams RJ. Access to expert stroke care with telemedicine: Reach musc. Frontiers in neurology. 2012;3:44. doi: 10.3389/fneur.2012.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cramer SC, Stradling D, Brown DM, Carrillo-Nunez IM, Ciabarra A, Cummings M, et al. Organization of a united states county system for comprehensive acute stroke care. Stroke. 2012;43:1089–1093. doi: 10.1161/STROKEAHA.111.635334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu SD, Rudd A, Davie C. Hyper acute stroke unit services. Clin Med. 2011;11:213–214. doi: 10.7861/clinmedicine.11-3-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Annals of neurology. 2011;69:619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kelly-Hayes M, Wolf PA, Kase CS, Brand FN, McGuirk JM, D’Agostino RB. Temporal patterns of stroke onset. The framingham study. Stroke. 1995;26:1343–1347. doi: 10.1161/01.str.26.8.1343. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention. A summary of primary stroke center policy in the United States. Atlanta: U.S. Department of Health and Human Services; 2011. [Accessed November 11th, 2012]. Available online: http://www.cdc.gov/dhdsp/pubs/docs/Primary_Stroke_Center_Report.pdf. [Google Scholar]