Abstract
Airway epithelium contributes significantly to the barrier function of airway tract. Mucociliary escalator, intercellular apical junctional complexes which regulate paracellular permeability and antimicrobial peptides secreted by the airway epithelial cells are the three primary components of barrier function of airway tract. These three components act cooperatively to clear inhaled pathogens, allergens and particulate matter without inducing inflammation and maintain tissue homeostasis. Therefore impairment of one or more of these essential components of barrier function may increase susceptibility to infection and promote exaggerated and prolonged innate immune responses to environmental factors including allergens and pathogens resulting in chronic inflammation. Here we review the regulation of components of barrier function with respect to chronic airways diseases.
Keywords: mucociliary clearance, antimicrobial peptides, COPD, asthma, airway epithelium, tight junctions
Besides the skin, the lung is the only organ that is in direct contact with the external environment. Given the fact that we inspire 6–12 L of air/min, the lung is constantly exposed to inhaled microbes, allergens and particulate material, which must be cleared without inducing inflammation, so as to maintain homeostasis. The airway tract mucosa plays an important role in protecting the lungs from environmental insults and maintaining homeostasis. The airway tract can be divided into two zones: the conducting zone and the respiratory zone. In the conducting zone, the inhaled air is moistened, warmed, and cleaned before it reaches the lower respiratory zone, where gas exchange occurs and blood is oxygenated. The conducting zone comprises the nasal cavities, pharynx, larynx, trachea, bronchi, and bronchioles, while the respiratory zone includes respiratory bronchioles, alveolar ducts, and alveolar sacs. The conducting airway tract starting from the trachea undergoes dichotomous branching leading to two bronchi, which further branch into series of bronchial and bronchiolar airways. The size of the airway tract progressively decreases from the trachea to the terminal bronchiole, the most distal part of the tract. The terminal bronchiole connects to alveolar ducts through a respiratory bronchiole which has features of both bronchiole and alveoli.1 This review will focus on the conducting airway tract as it comes in direct contact with the external environment and acts as a barrier by preventing invasion of inhaled environmental agents.
Cellular Diversity in the Conducting Airway Epithelium
The mammalian conducting airway can be broadly divided into two regions based on structure and function: the cartilaginous proximal airway starting from nasal cavities to bronchi and 2–3 generations of bronchioles, and non-cartilaginous distal airway consisting of terminal and respiratory bronchioles. Luminal surfaces of the entire conductive airway tract are lined by a continuous layer of epithelial cells which vary in relative distribution, abundance, and cell type depending on the airway region in which they are found. The proximal airway through the bronchi is lined with pseudostratified epithelium and is made up of three major cell types: ciliated cells, non-ciliated secretory cells, and basal cells (Fig. 1). As the bronchi branches into bronchioles and to terminal bronchioles the epithelium gradually changes from psuedostratified to simple cuboidal epithelium and the number of ciliated, goblet, and basal cells gradually decline and non-ciliated cells called Clara cells becomes the major cell type.2 In the proximal airway and cartilaginous bronchioles, the invagination of epithelium forms submucosal glands, which are characterized by a variable proportion of ciliated cells, goblet cells, and serous cells.3 Other minor cell types that are present in conducting airways are: (1) chemosensory or brush cells which contains apical tufts of microvilli and are thought to play a role in regulation of both airway surface fluid secretion and breathing,4,5 and (2) pulmonary neuroendocrine cells which are typically tall and pyramidal in shape and extend from the basal lamina of the epithelium and possess microvilli.6,7
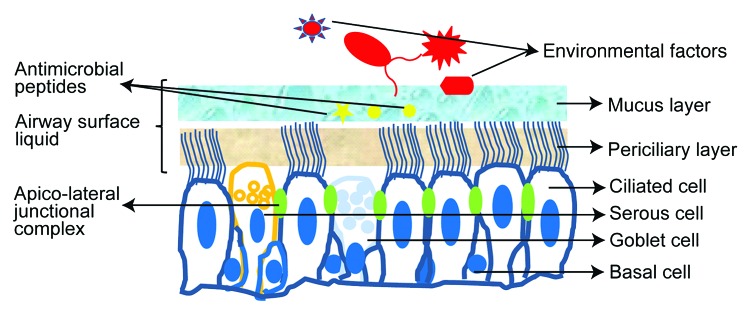
Figure 1. Components of airway tract epithelium. Cilia and airway surface fluid play a major role in mucociliary clearance of inhaled envirmental irritants; apicolateral junctional complex regulates paracellular permeability and prevents paracellular invasion of environmental factors; Antimicrobial peptides in the mucus layer kills inhaled pathogens.
Ciliated cells account for over 50% of all epithelial cells in the conducting airway.8 Approximately 200 to 300 cilia are found on the luminal surface of each ciliated cell, and in humans the length of the cilia ranges between 6 µM in the proximal airways to 3.6 µM in the seventh generation of bronchi.9 A large number of mitochondria are present right below the apical surface and provide energy to the cilia for coordinated ciliary beating.10 Ciliated cells are believed to be terminally differentiated and arise from basal or secretory cells.11,12 However, recent studies have suggested a remarkable plasticity and differentiation potential for ciliated cells. After injury, ciliated cells dedifferentiate into squamous, cuboidal or columnar cells, thereby playing a role in restoration and regeneration of bronchial epithelium.13,14 Ciliated cells have also been shown to transdifferentiate into goblet cells in a mouse model of allergic airway disease, which depends on IL-13 expression and persistent activation of epithelial growth factor (EGF) receptors.15
Goblet cells have electron lucent granules which contain acidic mucin glycoproteins in the apical region of cytoplasm, and contain a condensed nucleus on the basal side giving the cells a unique shape. In normal conductive airways the ratio of goblet cell to ciliated cells is approximately 1:5 and this ratio increases under the conditions of chronic airway diseases, such as asthma, chronic obstructive pulmonary disease, and cystic fibrosis. The goblet cells secrete high molecular weight mucin glycoproteins into the airway lumen, which trap and remove foreign particles, thus protecting the epithelial surface. Mucin secretion must be tightly regulated for normal functioning, as overproduction can block the airway and impair proper mucociliary clearance.
Serous cells are found at the distal ends of submucosal glands and resemble goblet cells morphologically, but their granule content is more electron-dense.16 Serous cells secrete the bulk of glandular fluid in response to secretogogues that use cAMP and/or Ca2+ as second messengers.17 The fluid secreted by these cells directly contributes to airway surface liquid (see later) volume, hydration of mucus released from goblet cells,18,19 and innate immunity.20
Basal cells are connected to the basement membrane via hemodesmosomes, providing the foundation for the attachment of ciliated and goblet cells to basal lamina, and also have the potential to regulate inflammatory responses, oxidant defense and transepithelial water movement.21 The most important feature of basal cells is their capacity to repopulate all the major cell types of conductive airway epithelium.22-24 Basal cells are therefore thought to be the progenitor cells or the transient amplifying cells of the airway epithelium,25 but this is yet to be confirmed.
The most prominent features of Clara cells are the membrane-bound electron dense secretory granules. Although these granules do not contain glycoprotein like in goblet cells, they secrete CC10 (or CCSP) protein which is used as a Clara cell marker.26,27 These cells also secrete surfactant proteins and antiproteinases that may protect bronchiolar epithelium.28,29 Clara cells have been long considered stem cells because of their ability to proliferate and repopulate terminal bronchioles.30 Although in vivo and in vitro studies have demonstrated the potential of Clara cells to differentiate into ciliated and goblet cells, immunohistochemistry studies in human lungs clearly indicates the presence of Clara cells only in the terminal bronchioles, and not in the proximal airways, suggesting that these cells may be important in maintenance of distal bronchioles.31
Barrier Function of Epithelium in Conducting Airways
The primary function of airway epithelium is to function as a physical barrier between the external environment and internal milieu. The three essential components that contribute to the barrier function of airway epithelium are: mucociliary escalators which trap and removes inhaled foreign particles from the airways,32 intercellular tight and adherens junctions33 that regulate epithelial paracellular permeability, and secreted antimicrobial products that kill inhaled pathogens.34
Mucociliary Function of the Airway Epithelium
The major players that contribute to the mucociliary function of airway epithelium are mucus and cilia. While the mucus traps inhaled pathogens and other particulate material, coordinated beating of cilia sweeps the trapped material away from the lungs toward the pharynx.35 The efficient transport of mucus is dependent on the rate of ciliary beating as well as the hydration of mucus, which contributes to its viscoelastic properties.36,37 In general, more hydrated mucus is cleared more efficiently from the lungs.
The airway mucus contains more than 200 proteins, and is secreted by both goblet cells and submucosal glands. The main component of airway mucus are mucins, which are high molecular weight glycoproteins that cross link to form the structural framework of the mucus barrier.38,39 At least 12 mucins are detected in human lungs. Of these, MUC5AC and MUC5B are the predominant mucins in normal airways.40 MUC5AC is mainly produced by goblet cells, while MUC5B is predominantly produced by submucosal glands.41,42 In healthy individuals, circadian rhythms regulate normal mucus secretion, principally through the vagal nerve. However in patients with inflammatory airway diseases, mucus hypersecretion from metaplastic and hyperplastic goblet cells contributes to obstruction of airways.43 Various inflammatory mediators, such as tumor necrosis factor -α, IL-1β, IL-13, IL-17, neutrophil elastase, growth factors such as EGF and TGF, and environmental factors such as cigarette smoke, allergens and microbial pathogens have all been shown to stimulate hypersecretion of mucus.44-49 Therapies targeted to limit exaggerated mucus hypersecretion in addition to modulating mucociliary clearance in chronic airways disease may prevent airways obstruction.
The rate of mucociliary clearance depends on the composition of the airway surface liquid (ASL) lining the airway surface. ASL is made up of two layers, an upper viscoelastic layer of mucins secreted by the goblet cells and submucosal glands,50 which floats on a lower periciliary layer containing large membrane-bound glyocproteins, as well as tethered mucins (muc-1, muc-4 and muc-16).51,52 The periciliary layer is relatively less viscous, approximately 7 µM in height which corresponds to a length of outstretched cilia and acts as a lubricating layer for cilia to beat.32,52,53 Hydration of ASL is regulated by coordinated activity of Chloride secretion (Cl-) and Sodium (Na+) absorption channels. The combination of Cl- secretion and reduced reabsorption of Na+ favors normal ASL hydration and efficient mucociliary clearance. In normal airways, the coordinated functioning of ATP-activated cystic fibrosis transmembrane conductance regulator (CFTR), calcium-activated Cl− channel (CaCC), outwardly rectifying Cl- channel (ORCC), Cl- channel 2 (CLC2), and epithelial Na+ channel (ENaC) regulate the ASL hydration.54 CFTR negatively regulates ENac and therefore absent or dsyfunctional CFTR increases ENaC activity leading to hyperabsorption of Na+, an increased driving force for fluid reabsorption resulting in reduced ASL depth and impaired mucociliary clearance as observed in the chronic airway disease cystic fibrosis.54 In cystic fibrosis patients this condition is further exacerbated by excessive mucus production due to goblet cell metaplasia and hyperplasia, and submucosal gland hypertrophy resulting in obstruction of airways.
Goblet cell metaplasia and hyperplasia are also observed in patients with other chronic airway diseases such as asthma and chronic obstructive pulmonary disease (COPD), and is induced by the coordinated action of EGFR and IL-13.55-59 Downstream of IL-13, several transcription factors, e.g., thyroid transcription factor (TTF)-1, Sam pointed domain-containing ETS transcription factor (SPDEF), and forkhead transcription factor (FOX)A2, regulate goblet cell development downstream of IL-13.60 While both TTF-1 and FOXA2 repress goblet cell metaplasia,61,62 SPDEF promotes goblet cell metaplasia by downregulating FOXA2 and TTF-1.62 Recently, increased SPDEF and decreased FOXA2 expression has been shown to contribute to the development of goblet cell hyperplasia in mouse models of asthma.63-66 SPDEF not only promotes goblet cell hyperplasia but also upregulates the network of genes associated with mucus production.65 Inhibition of aldose reductase or SERPINb3a, both of which are induced in asthma reduced SPDEF expression, attenuates development of goblet cell hyperplasia.63,64 Additionally, TTF-1 was significantly reduced in patients with asthma and mice deficient in TTF-1 were found to be prone to develop goblet cell metaplasia upon exposure to allergens.62 Therefore, strategies to modulate activities of TTF-1, FOXA2 or SPDEF may attenuate goblet cell metaplasia and mucus production, thus improving mucociliary function in patients with asthma and other chronic airway diseases.
Impaired mucociliary clearance may also be a direct result of defective ciliary function as observed in patients with ciliary dyskinesia. Although these patients have normal secretion of mucus, it is not cleared due to defective ciliary beating.67 On the other hand, in COPD patients the impaired mucociliary function may be due to a combination of excessive mucus production, increased viscosity of mucus due to acquired dysfunction of CFTR, and reduced ciliary beating.68-70 It has been shown that respiratory epithelial cells exposed to cigarette smoke extract or condensate showed shorter and 70% fewer cilia compared control cells.71 Although mice exposed to cigarette smoke showed slight increases in ciliary beat frequencies at 6 weeks and 3 mo, it was significantly reduced at 6 mo, and post-mortem examination revealed significant loss of tracheal ciliated cells.72 Recently Yaghi et al. provided direct evidence of suppressed ciliary beating in nasal epithelium from COPD patients.68 Such changes in number and function of cilia can significantly impair the mucociliary clearance function of airway epithelium.
Mucociliary dysfunction, in addition to causing obstruction of airways, may also promote recurrent and persistent respiratory infections as evidenced in patients with cystic fibrosis, ciliary dyskinesia, and COPD.73-76 Mucin glycoproteins have been shown to interact with several respiratory pathogens including Pseudomonas aeruginosa, Staphylococcus aureus, Heamophilus influenzae, Streptococcus pneumonia, Burkholderia cenocepacia, influenza virus, adenovirus, and coronavirus.77-83 The bound pathogens which are cleared under normal conditions may persist in the airway lumen when the mucociliary clearance is impaired, and initiate an inflammatory response which can damage the airway epithelium. However, the impact of the interaction of mucin glycoproteins with pathogens in vivo is yet to be established.
Apico-Lateral Junctional Complexes and Airway Epithelial Permeability
Tight and adherens junctions located at the apicolateral border of airway epithelial cells also contribute significantly to the barrier function of conductive airway tract epithelium. Like in other mucosal epithelium, paracellular permeability of airway epithelium is maintained through the cooperation of two mutually exclusive structural components: tight junctions and adherens junctions on the apicolateral membranes.33 While tight junctions regulate the transport of solutes and ions across epithelia, adherens junctions mediate cell to cell adhesion and promote formation of tight junctions.84-86 In normal airway epithelium, these intercellular junctions prevent inhaled pathogens and other environmental insults from injuring the airways, and also serve as signaling platforms that regulate gene expression, cell proliferation, and differentiation.87,88 Therefore, disassociation or sustained insults that affect junctional complexes will disrupt not only barrier function, but may also interfere with normal repair and differentiation of airway epithelium. Airway epithelium is leaky, hyperproliferative, and abnormally differentiated in smokers and in patients with asthma and COPD compared with airway epithelium in healthy smokers.89-92 Infection with viruses or bacteria can also cause transient disruption of tight or adherens junctions.93-95 Host factors, such as interferons and tumor necrosis factor-α expressed in response to infection may prolong tight junction disruption long after infection is cleared, enabling the passage of inhaled allergens and pollutants.96,97
The formation of apico-lateral junctional complexes is closely related to cell polarization. Recent gene arrays indicated the expression of two polarity complexes in airway epithelial cells: the Crumbs (CRB) complex and the partitioning defective (PAR) complex.90 The CRB complex consists of the integral membrane protein Crumbs3 and the scaffolding proteins, protein associated with Lin seven 1 (PALS1), and PALS1-associated tight junction protein (PATJ).98-100 The CRB complex plays a critical role in the formation of tight junctions, cell polarization, and ciliogenesis.101 Decreased expression of Crumbs3 delays formation of tight junctions and cilia.101,102 Depletion of PALS1 leads to the loss of PATJ, disruption of cell polarity, decreased TER, and altered trafficking of E-cadherin.103,104 Coronavirus envelope protein E binds to PALS1, and ectoexpression of protein E delays tight junction formation in MDCK cells.105 Recently, we showed that Crumbs3 is necessary for ciliogenesis in airway epithelial cells and is associated in the tip of mature cilia in mucociliary-differentiated bronchial airway epithelial cell cultures.106 The PAR complex is composed two scaffolding proteins, PAR3 and PAR6, and atypical protein kinase C,103 but the molecular actions of the PAR complex in airway epithelial polarity are not known.
Tight junctions are composed of several transmembrane proteins (including occludin, multiple claudins, junctional adhesion molecule (JAM)) and cytoplasmic scaffolding proteins containing PDZ-domains (zonula occludens(ZO-1, ZO-2, ZO-3), cingulin, and MUPP1. Transmembrane proteins in the junction connect the membranes of adjacent cells to make a tight seal, while scaffolding proteins anchor transmembrane proteins to the cytoskeleton. Claudins function to regulate the paracellular permeability in airway epithelium, whereas occludin has been shown to regulate de novo assembly of tight junctions.107 Although JAM association with tight junctions is well studied, its function at tight junctions remains unclear. In recent years, the coxsackievirus and adenovirus receptor (CAR), which serves as a receptor for viruses, was also shown to be a transmembrane protein located in the tight junction and interacts with ZO-1 in airway epithelial cells.108 Further, CAR expression was shown to be required for formation of functional tight junctions and limits permeability of macromolecules. Airway epithelial cells isolated from healthy smokers and patients with COPD show reduced expression of occludin and claudins, which may contribute to the observed barrier dysfunction in these subjects.90 Several respiratory viruses have been shown to increase permeability and decrease transepithelial resistance of airway epithelium by either interacting with tight junction proteins or by dissociating adherens junction complexes. Coxsackievirus and adenovirus bind to CAR, inducing disassembly of the tight junction and reduction in transepithelial resistance (TER).109,110 Previously, we demonstrated that rhinovirus (RV) dissociates ZO-1, occludin, and claudin 4 from the tight junctions and increases bacterial association and translocation across polarized airway epithelium.93,111,112 However, our studies have not shown binding of RV to tight junction proteins. Instead, RV-induced barrier dysfunction is dependent on ROS generation.93,111 Oxidative stress constitutes a well-studied mechanism of tight junction breakdown, inducing tyrosine phosphorylation and dissociation of occludin from the tight junction complex.113 Our on-going studies indicate that while normal differentiated airway epithelial cell cultures show restoration of barrier function at 4 d post-RV infection, similarly differentiated COPD cell cultures show barrier dysfunction up to 14 d after RV infection (Faris and Sajjan, unpublished results). Based on these preliminary observations, we speculate that RV infection in COPD patients may further damage airway epithelium, and this may in turn promote airway remodeling, increase the risk for acquiring secondary infections and alter innate immune responses to infection or other environmental insults ultimately leading to progression of lung disease. Therefore, strategies to inhibit barrier disruption or quickly restore barrier function after viral infection may prevent progression of lung disease in patients with COPD and possibly in subjects with other chronic airways disease such as cystic fibrosis and asthma.
Adherens junctions are located just below the tight junctions and mechanically connect adjacent cells and initiate the formation and maturation of cell-cell contacts. The principal proteins in adherens junctions are type I transmembrane glycoprotein, epithelial cadherin (E-cadherin),β-catenin, and α-catenin. An extracellular domain of E-cadherin of adjacent cells forms homotypic, calcium dependent adhesions between epithelial cells. E-cadherin associates with the armadillo protein family member β-catenin and α-catenin, which then forms an interface with the microtubule network and actin cytoskeleton.114,115 In addition, E-cadherin also regulates cell proliferation and differentiation by modulating EGFR and β-catenin activities. Under normal conditions, E-cadherin interacts and retains EGFR in adherens junctions of airway epithelium,116 thus preventing EGFR activation.117-119 Dissociation of E-cadherin from the adherens junction complex or reduced expression of E-cadherin, each of which may occur during epithelial to mesenchymal transition, may cause uncoupling and redistribution of EGFR from the adherens junction to the apical cell surface,120 where it is readily activated by EGF ligands. Excessive activation of EGFR not only promotes cell proliferation, but also development of goblet cell metaplasia/hyperplasia.57 In fact, enhanced surface expression and phosphorylation of EGF receptors in the airway epithelium has been observed in patients with asthma who show impaired mucosal barrier function.121 Recently, we demonstrated that EGF receptor phosphorylation is also increased in COPD airway epithelial cells, which retains the phenotype of goblet cell hyperplasia.122,123 β-catenin cooperates with E-cadherin to form adherens junctions.124 However, when dissociated from E-cadherin β-catenin translocates to the nucleus and activates canonical Wnt/β-catenin signaling, thus promoting cell proliferation and suppressing cell-differentiation.125,126 Since cigarette smoke causes aberrant activation of canonical Wnt/β-catenin signaling,127,128 it is plausible that chronic cigarette smoke exposure decreases barrier function and facilitates invasion of airway epithelium by environmental allergens, pollutants, and pathogens. In asthma however, allergens are thought to be primary stimulus responsible for airway remodeling. It was demonstrated that proteases present in the allergens disrupt not only tight junctions but also adherens junctions129,130 and this could lead to both EGFR activation and Wnt/β-catenin signaling ultimately resulting in development of goblet cell metaplasia/hyperplasia.
Antimicrobial Products of Airway Epithelium
In addition to being a physical barrier, airway epithelium also acts as a biochemical barrier against invading pathogens. Airway epithelial cells secrete a wide variety of antimicrobial substances such as enzymes, protease inhibitors, oxidants, and antimicrobial peptides, which accumulates in the ASL and kill inhaled pathogens. Lysozyme, an enzyme found in airway epithelial secretions, exerts antimicrobial effect against a wide range of gram-positive bacteria by degrading their peptidoglycan layer.131 Lysozyme is also effective against gram-negative bacteria in the presence of lactoferrin, which disrupts the outer membrane, allowing lysozyme to gain access to the peptidoglycan layer.132 Lactoferrin is an iron-chelator and inhibits microbial growth by sequestering iron which is essential for microbial respiration.133 Lactoferrin also displays antiviral activity against both RNA and DNA viruses by either inhibiting binding of the virus to host cells or by binding to the virus itself.134,135 Lactoferrin levels increase in response to bacterial and viral infections. In clinically stable COPD patients, lower levels of salivary lysozyme correlated with increased risk of exacerbations136 while reduced lysozyme levels in COPD is thought to be due to degradation by proteases elaborated by bacterial pathogens or neutrophils.137,138
Epithelial cells produce protease inhibitors, such as secretory leukoprotease inhibitor (SLPI), elastase inhibitor, α1-antiprotease, and antichymotrypsin. These protease inhibitors mitigate the effects of proteases expressed by pathogens and recruited innate immune cells. Maintaining the balance between antiproteases and proteases in the airway lumen during infection is pivotal in preventing lung inflammation and maintenance of tissue homeostasis. In COPD patients, levels of SLPI and lysozyme were shown to decrease with bacterial infection, while lactoferrin levels remain unchanged.139 This could be due to inactivation of SLPI by proteases or decreased expression of SLPI, but either way the end result under these conditions is an imbalance in the ratio of antiproteases to proteases in the airway lumen. Therefore, neutralization of proteases would be beneficial in this situation. Accordingly, administration of SLPI decreased the levels of IL-8 and elastase activity in airway secretion of cystic fibrosis patients, who also have reduced SLPI in their airway lumen.140
Human β defensins (hBD) are the most abundant antimicrobial peptides expressed on the surface of airway epithelium and are effective against a wide range of bacteria and viruses.141-143 While hBD1 is constitutively expressed, hBD2 to hBD4 expression is induced by LPS via NF-κB activation and by IL-1.144,145 hBD2 is induced by P. aeruginosa infection in normal but not in cystic fibrosis airway epithelia.146 Activity of hBD2 is also attenuated in cystic fibrosis patients due to increased salt concentration.147 Environmental factors such as air pollutants have also been shown to decrease the expression defensin genes in the airways.135 Herr et al. showed that hBD2 is significantly reduced in the pharyngeal wash and sputum of current or former smokers compared with non-smokers, and exposure of airway epithelium to cigarette smoke in vitro inhibited induction of HBD2 by bacteria.148 Cathelicidins are another class of antimicrobial peptides and LL37 is the only human cathelicidin identified to date. LL37 binds to lipopolysaccharides and inactivates its biological function. Overexpression of human LL37 in cystic fibrosis mouse models increased killing of P.aeruginosa and reduced the ability of this bacterium to colonize the airways.149
Airway epithelial cells also generate oxidants such as nitric oxide (NO) and hydrogen peroxide. Three NO synthases contribute to production of NO in airway epithelia: the constitutively expressed NOS1 and NOS3, and inducible NOS2. Viral infections and pro-inflammatory cytokines induce expression of NOS2 and defective NOS2 expression is responsible for increased viral replication in cystic fibrosis, while overexpression of NOS2 provides protection against viral infection.150,151 Recently we demonstrated that COPD airway epithelial cells show a trend in decreased expression of NOS2 and this was associated with impaired clearance of rhinovirus.123 Extracellular hydrogen peroxide is produced by dual oxidase 1 and 2. These belong to a family of NADPH oxidases and are located in the plasma membrane and secrete hydrogen peroxide to the extracellular milieu. The dual oxidase-generated hydrogen peroxide in combination with thiocyanate and lactoperoxidase generates the microbicidal oxidant hypothiocyanite, which effectively kills both gram positive and gram negative bacteria. This innate defense mechanism is defective in cystic fibrosis airway epithelium due to impaired transport of thiocyanate.152 COPD airway epithelial cells also show decreased expression of Duox 1 and 2, but their contribution to defective bacterial clearance in COPD is yet to be determined.123
Conclusions
The three barrier functions of airway epithelial tract, mucociliary clearance, intercellular apical junctional complexes and antimicrobial products of airway function together to effectively clear inhaled pathogens, allergens and pollutants from the lungs. The intercellular apical junctional complex not only regulates paracellular permeability, but also separates proteins of basolateral surface from apical surface and promotes normal differentiation of airway tract epithelial cells. This is critical for regulation of secretion of mucus and antimicrobial proteins and peptides, and also for maintenance of viscosity and depth of ASL, in which cilia beat. Barrier function of airway tract epithelium is compromised in patients with chronic airways disease due to repetitive injury and abnormal repair leading to airway remodeling. Understanding the molecular mechanisms of airway epithelial repair under normal and chronic disease conditions is necessary to develop therapies to prevent airway remodeling and promote normal epithelial repair. However, the field of airway epithelial repair is in its infancy, because airway epithelium is complex and comprises several cell types and the cells show remarkable plasticity. There also exists a controversy with respect to progenitor cells and lung stem cells that replenish injured airway epithelium. Further immortalized airway epithelial cells do not differentiate normally necessitating primary airway epithelial cells for these studies. Primary cells are not readily available and not amenable to transfection or transformation that is necessary to elucidate regulatory mechanisms. Development of appropriate methods to immortalize airway epithelial cells that maintain ability to differentiate and methods to express or knockdown genes of interest in primary epithelial cells will greatly advance the research in this field.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgments
This work was supported by the National Institute of Health, HL089772 and AT004793. We thank Mr. Brenton Kinker for editing the manuscript.
Footnotes
Previously published online: www.landesbioscience.com/journals/tissuebarriers/article/24997
References
- 1.Tyler WS. Comparative subgross anatomy of lungs. Pleuras, interlobular septa, and distal airways. Am Rev Respir Dis. 1983;128:S32–6. doi: 10.1164/arrd.1983.128.2P2.S32. [DOI] [PubMed] [Google Scholar]
- 2.Wright NA, Alison M. The Biology of epithelial cell populations. Oxford University Press, 1984. [Google Scholar]
- 3.De Poitiers W, Lord PW, Biles B, Whimster WF. Bronchial gland histochemistry in lungs removed for cancer. Thorax. 1980;35:546–51. doi: 10.1136/thx.35.7.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Osculati F, Bentivoglio M, Castellucci M, Cinti S, Zancanaro C, Sbarbati A. The solitary chemosensory cells and the diffuse chemosensory system of the airway. Eur J Histochem. 2007;51(Suppl 1):65–72. [PubMed] [Google Scholar]
- 5.Krasteva G, Canning BJ, Hartmann P, Veres TZ, Papadakis T, Mühlfeld C, et al. Cholinergic chemosensory cells in the trachea regulate breathing. Proc Natl Acad Sci U S A. 2011;108:9478–83. doi: 10.1073/pnas.1019418108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gustafsson BI, Kidd M, Chan A, Malfertheiner MV, Modlin IM. Bronchopulmonary neuroendocrine tumors. Cancer. 2008;113:5–21. doi: 10.1002/cncr.23542. [DOI] [PubMed] [Google Scholar]
- 7.Gosney JR, Sissons MC, Allibone RO. Neuroendocrine cell populations in normal human lungs: a quantitative study. Thorax. 1988;43:878–82. doi: 10.1136/thx.43.11.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spina D. Epithelium smooth muscle regulation and interactions. Am J Respir Crit Care Med. 1998;158:S141–5. doi: 10.1164/ajrccm.158.supplement_2.13tac100a. [DOI] [PubMed] [Google Scholar]
- 9.Serafini SM, Michaelson ED. Length and distribution of cilia in human and canine airways. Bull Eur Physiopathol Respir. 1977;13:551–9. [PubMed] [Google Scholar]
- 10.Harkema JR, Mariassy SA, George J, Hyde DM, Plopper CG. Epithelial cells of the Conducting airways: a species comparison. New york: Marcel Dekker, 1991. [Google Scholar]
- 11.Inayama Y, Hook GE, Brody AR, Jetten AM, Gray T, Mahler J, et al. In vitro and in vivo growth and differentiation of clones of tracheal basal cells. Am J Pathol. 1989;134:539–49. [PMC free article] [PubMed] [Google Scholar]
- 12.Ayers MM, Jeffery PK. Proliferation and differentiation in mammalian airway epithelium. Eur Respir J. 1988;1:58–80. [PubMed] [Google Scholar]
- 13.Lawson GW, Van Winkle LS, Toskala E, Senior RM, Parks WC, Plopper CG. Mouse strain modulates the role of the ciliated cell in acute tracheobronchial airway injury-distal airways. Am J Pathol. 2002;160:315–27. doi: 10.1016/S0002-9440(10)64375-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park KS, Wells JM, Zorn AM, Wert SE, Laubach VE, Fernandez LG, et al. Transdifferentiation of ciliated cells during repair of the respiratory epithelium. Am J Respir Cell Mol Biol. 2006;34:151–7. doi: 10.1165/rcmb.2005-0332OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tyner JW, Kim EY, Ide K, Pelletier MR, Roswit WT, Morton JD, et al. Blocking airway mucous cell metaplasia by inhibiting EGFR antiapoptosis and IL-13 transdifferentiation signals. J Clin Invest. 2006;116:309–21. doi: 10.1172/JCI25167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rogers AV, Dewar A, Corrin B, Jeffery PK. Identification of serous-like cells in the surface epithelium of human bronchioles. Eur Respir J. 1993;6:498–504. [PubMed] [Google Scholar]
- 17.Wu JV, Krouse ME, Wine JJ. Acinar origin of CFTR-dependent airway submucosal gland fluid secretion. Am J Physiol Lung Cell Mol Physiol. 2007;292:L304–11. doi: 10.1152/ajplung.00286.2006. [DOI] [PubMed] [Google Scholar]
- 18.Ballard ST, Inglis SK. Liquid secretion properties of airway submucosal glands. J Physiol. 2004;556:1–10. doi: 10.1113/jphysiol.2003.052779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ballard ST, Spadafora D. Fluid secretion by submucosal glands of the tracheobronchial airways. Respir Physiol Neurobiol. 2007;159:271–7. doi: 10.1016/j.resp.2007.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raphael GD, Jeney EV, Baraniuk JN, Kim I, Meredith SD, Kaliner MA. Pathophysiology of rhinitis. Lactoferrin and lysozyme in nasal secretions. J Clin Invest. 1989;84:1528–35. doi: 10.1172/JCI114329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evans MJ, Van Winkle LS, Fanucchi MV, Plopper CG. Cellular and molecular characteristics of basal cells in airway epithelium. Exp Lung Res. 2001;27:401–15. doi: 10.1080/019021401300317125. [DOI] [PubMed] [Google Scholar]
- 22.Hong KU, Reynolds SD, Watkins S, Fuchs E, Stripp BR. Basal cells are a multipotent progenitor capable of renewing the bronchial epithelium. Am J Pathol. 2004;164:577–88. doi: 10.1016/S0002-9440(10)63147-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hong KU, Reynolds SD, Watkins S, Fuchs E, Stripp BR. In vivo differentiation potential of tracheal basal cells: evidence for multipotent and unipotent subpopulations. Am J Physiol Lung Cell Mol Physiol. 2004;286:L643–9. doi: 10.1152/ajplung.00155.2003. [DOI] [PubMed] [Google Scholar]
- 24.Inayama Y, Hook GE, Brody AR, Cameron GS, Jetten AM, Gilmore LB, et al. The differentiation potential of tracheal basal cells. Lab Invest. 1988;58:706–17. [PubMed] [Google Scholar]
- 25.Hajj R, Baranek T, Le Naour R, Lesimple P, Puchelle E, Coraux C. Basal cells of the human adult airway surface epithelium retain transit-amplifying cell properties. Stem Cells. 2007;25:139–48. doi: 10.1634/stemcells.2006-0288. [DOI] [PubMed] [Google Scholar]
- 26.Widdicombe JG, Pack RJ. The Clara cell. Eur J Respir Dis. 1982;63:202–20. [PubMed] [Google Scholar]
- 27.Singh G, Katyal SL, Brown WE, Kennedy AL, Singh U, Wong-Chong ML. Clara cell 10 kDa protein (CC10): comparison of structure and function to uteroglobin. Biochim Biophys Acta. 1990;1039:348–55. doi: 10.1016/0167-4838(90)90270-P. [DOI] [PubMed] [Google Scholar]
- 28.Phelps DS, Floros J. Localization of pulmonary surfactant proteins using immunohistochemistry and tissue in situ hybridization. Exp Lung Res. 1991;17:985–95. doi: 10.3109/01902149109064330. [DOI] [PubMed] [Google Scholar]
- 29.De Water R, Willems LN, Van Muijen GN, Franken C, Fransen JA, Dijkman JH, et al. Ultrastructural localization of bronchial antileukoprotease in central and peripheral human airways by a gold-labeling technique using monoclonal antibodies. Am Rev Respir Dis. 1986;133:882–90. [PubMed] [Google Scholar]
- 30.Evans MJ, Cabral-Anderson LJ, Freeman G. Role of the Clara cell in renewal of the bronchiolar epithelium. Lab Invest. 1978;38:648–53. [PubMed] [Google Scholar]
- 31.Boers JE, Ambergen AW, Thunnissen FB. Number and proliferation of clara cells in normal human airway epithelium. Am J Respir Crit Care Med. 1999;159:1585–91. doi: 10.1164/ajrccm.159.5.9806044. [DOI] [PubMed] [Google Scholar]
- 32.Knowles MR, Boucher RC. Mucus clearance as a primary innate defense mechanism for mammalian airways. J Clin Invest. 2002;109:571–7. doi: 10.1172/JCI15217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pohl C, Hermanns MI, Uboldi C, Bock M, Fuchs S, Dei-Anang J, et al. Barrier functions and paracellular integrity in human cell culture models of the proximal respiratory unit. Eur J Pharm Biopharm. 2009;72:339–49. doi: 10.1016/j.ejpb.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 34.Bals R, Hiemstra PS. Innate immunity in the lung: how epithelial cells fight against respiratory pathogens. Eur Respir J. 2004;23:327–33. doi: 10.1183/09031936.03.00098803. [DOI] [PubMed] [Google Scholar]
- 35.Kilburn KH. A hypothesis for pulmonary clearance and its implications. Am Rev Respir Dis. 1968;98:449–63. doi: 10.1164/arrd.1968.98.3.449. [DOI] [PubMed] [Google Scholar]
- 36.Puchelle E, de Bentzmann S, Zahm JM. Physical and functional properties of airway secretions in cystic fibrosis--therapeutic approaches. Respiration. 1995;62(Suppl 1):2–12. doi: 10.1159/000196486. [DOI] [PubMed] [Google Scholar]
- 37.Tarran R, Grubb BR, Gatzy JT, Davis CW, Boucher RC. The relative roles of passive surface forces and active ion transport in the modulation of airway surface liquid volume and composition. J Gen Physiol. 2001;118:223–36. doi: 10.1085/jgp.118.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rose MC, Nickola TJ, Voynow JA. Airway mucus obstruction: mucin glycoproteins, MUC gene regulation and goblet cell hyperplasia. Am J Respir Cell Mol Biol. 2001;25:533–7. doi: 10.1165/ajrcmb.25.5.f218. [DOI] [PubMed] [Google Scholar]
- 39.Thornton DJ, Rousseau K, McGuckin MA. Structure and function of the polymeric mucins in airways mucus. Annu Rev Physiol. 2008;70:459–86. doi: 10.1146/annurev.physiol.70.113006.100702. [DOI] [PubMed] [Google Scholar]
- 40.Rose MC, Voynow JA. Respiratory tract mucin genes and mucin glycoproteins in health and disease. Physiol Rev. 2006;86:245–78. doi: 10.1152/physrev.00010.2005. [DOI] [PubMed] [Google Scholar]
- 41.Wickström C, Davies JR, Eriksen GV, Veerman EC, Carlstedt I. MUC5B is a major gel-forming, oligomeric mucin from human salivary gland, respiratory tract and endocervix: identification of glycoforms and C-terminal cleavage. Biochem J. 1998;334:685–93. doi: 10.1042/bj3340685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hovenberg HW, Davies JR, Carlstedt I. Different mucins are produced by the surface epithelium and the submucosa in human trachea: identification of MUC5AC as a major mucin from the goblet cells. Biochem J. 1996;318:319–24. doi: 10.1042/bj3180319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rogers DF. The airway goblet cell. Int J Biochem Cell Biol. 2003;35:1–6. doi: 10.1016/S1357-2725(02)00083-3. [DOI] [PubMed] [Google Scholar]
- 44.Dohrman A, Miyata S, Gallup M, Li JD, Chapelin C, Coste A, et al. Mucin gene (MUC 2 and MUC 5AC) upregulation by Gram-positive and Gram-negative bacteria. Biochim Biophys Acta. 1998;1406:251–9. doi: 10.1016/S0925-4439(98)00010-6. [DOI] [PubMed] [Google Scholar]
- 45.Borchers MT, Carty MP, Leikauf GD. Regulation of human airway mucins by acrolein and inflammatory mediators. Am J Physiol. 1999;276:L549–55. doi: 10.1152/ajplung.1999.276.4.L549. [DOI] [PubMed] [Google Scholar]
- 46.Gensch E, Gallup M, Sucher A, Li D, Gebremichael A, Lemjabbar H, et al. Tobacco smoke control of mucin production in lung cells requires oxygen radicals AP-1 and JNK. J Biol Chem. 2004;279:39085–93. doi: 10.1074/jbc.M406866200. [DOI] [PubMed] [Google Scholar]
- 47.Shao MX, Nakanaga T, Nadel JA. Cigarette smoke induces MUC5AC mucin overproduction via tumor necrosis factor-alpha-converting enzyme in human airway epithelial (NCI-H292) cells. Am J Physiol Lung Cell Mol Physiol. 2004;287:L420–7. doi: 10.1152/ajplung.00019.2004. [DOI] [PubMed] [Google Scholar]
- 48.Haswell LE, Hewitt K, Thorne D, Richter A, Gaça MD. Cigarette smoke total particulate matter increases mucous secreting cell numbers in vitro: a potential model of goblet cell hyperplasia. Toxicol In Vitro. 2010;24:981–7. doi: 10.1016/j.tiv.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 49.Casalino-Matsuda SM, Monzon ME, Day AJ, Forteza RM. Hyaluronan fragments/CD44 mediate oxidative stress-induced MUC5B up-regulation in airway epithelium. Am J Respir Cell Mol Biol. 2009;40:277–85. doi: 10.1165/rcmb.2008-0073OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rubin BK. Physiology of airway mucus clearance. Respir Care. 2002;47:761–8. [PubMed] [Google Scholar]
- 51.Sheehan JK, Kesimer M, Pickles R. Innate immunity and mucus structure and function. Novartis Found Symp. 2006;279:155–66. [PubMed] [Google Scholar]
- 52.Randell SH, Boucher RC, University of North Carolina Virtual Lung Group Effective mucus clearance is essential for respiratory health. Am J Respir Cell Mol Biol. 2006;35:20–8. doi: 10.1165/rcmb.2006-0082SF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tarran R. Regulation of airway surface liquid volume and mucus transport by active ion transport. Proc Am Thorac Soc. 2004;1:42–6. doi: 10.1513/pats.2306014. [DOI] [PubMed] [Google Scholar]
- 54.Zeitlin PL. Cystic fibrosis and estrogens: a perfect storm. J Clin Invest. 2008;118:3841–4. doi: 10.1172/JCI37778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grünig G, Warnock M, Wakil AE, Venkayya R, Brombacher F, Rennick DM, et al. Requirement for IL-13 independently of IL-4 in experimental asthma. Science. 1998;282:2261–3. doi: 10.1126/science.282.5397.2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wills-Karp M, Luyimbazi J, Xu X, Schofield B, Neben TY, Karp CL, et al. Interleukin-13: central mediator of allergic asthma. Science. 1998;282:2258–61. doi: 10.1126/science.282.5397.2258. [DOI] [PubMed] [Google Scholar]
- 57.Casalino-Matsuda SM, Monzón ME, Forteza RM. Epidermal growth factor receptor activation by epidermal growth factor mediates oxidant-induced goblet cell metaplasia in human airway epithelium. Am J Respir Cell Mol Biol. 2006;34:581–91. doi: 10.1165/rcmb.2005-0386OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Takeyama K, Fahy JV, Nadel JA. Relationship of epidermal growth factor receptors to goblet cell production in human bronchi. Am J Respir Crit Care Med. 2001;163:511–6. doi: 10.1164/ajrccm.163.2.2001038. [DOI] [PubMed] [Google Scholar]
- 59.Kim JH, Lee SY, Bak SM, Suh IB, Lee SY, Shin C, et al. Effects of matrix metalloproteinase inhibitor on LPS-induced goblet cell metaplasia. Am J Physiol Lung Cell Mol Physiol. 2004;287:L127–33. doi: 10.1152/ajplung.00047.2003. [DOI] [PubMed] [Google Scholar]
- 60.Park KS, Korfhagen TR, Bruno MD, Kitzmiller JA, Wan H, Wert SE, et al. SPDEF regulates goblet cell hyperplasia in the airway epithelium. J Clin Invest. 2007;117:978–88. doi: 10.1172/JCI29176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wan H, Kaestner KH, Ang SL, Ikegami M, Finkelman FD, Stahlman MT, et al. Foxa2 regulates alveolarization and goblet cell hyperplasia. Development. 2004;131:953–64. doi: 10.1242/dev.00966. [DOI] [PubMed] [Google Scholar]
- 62.Maeda Y, Chen G, Xu Y, Haitchi HM, Du L, Keiser AR, et al. Airway epithelial transcription factor NK2 homeobox 1 inhibits mucous cell metaplasia and Th2 inflammation. Am J Respir Crit Care Med. 2011;184:421–9. doi: 10.1164/rccm.201101-0106OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yadav UC, Aguilera-Aguirre L, Ramana KV, Boldogh I, Srivastava SK. Aldose reductase inhibition prevents metaplasia of airway epithelial cells. PLoS One. 2010;5:e14440. doi: 10.1371/journal.pone.0014440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sivaprasad U, Askew DJ, Ericksen MB, Gibson AM, Stier MT, Brandt EB, et al. A nonredundant role for mouse Serpinb3a in the induction of mucus production in asthma. J Allergy Clin Immunol. 2011;127:254–61. doi: 10.1016/j.jaci.2010.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen G, Korfhagen TR, Xu Y, Kitzmiller J, Wert SE, Maeda Y, et al. SPDEF is required for mouse pulmonary goblet cell differentiation and regulates a network of genes associated with mucus production. J Clin Invest. 2009;119:2914–24. doi: 10.1172/JCI39731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Park SW, Verhaeghe C, Nguyenvu LT, Barbeau R, Eisley CJ, Nakagami Y, et al. Distinct roles of FOXA2 and FOXA3 in allergic airway disease and asthma. Am J Respir Crit Care Med. 2009;180:603–10. doi: 10.1164/rccm.200811-1768OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Noone PG, Leigh MW, Sannuti A, Minnix SL, Carson JL, Hazucha M, et al. Primary ciliary dyskinesia: diagnostic and phenotypic features. Am J Respir Crit Care Med. 2004;169:459–67. doi: 10.1164/rccm.200303-365OC. [DOI] [PubMed] [Google Scholar]
- 68.Yaghi A, Zaman A, Cox G, Dolovich MB. Ciliary beating is depressed in nasal cilia from chronic obstructive pulmonary disease subjects. Respir Med. 2012;106:1139–47. doi: 10.1016/j.rmed.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 69.Liu Y, Di YP. Effects of second hand smoke on airway secretion and mucociliary clearance. Front Physiol. 2012;3:342. doi: 10.3389/fphys.2012.00342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sloane PA, Shastry S, Wilhelm A, Courville C, Tang LP, Backer K, et al. A pharmacologic approach to acquired cystic fibrosis transmembrane conductance regulator dysfunction in smoking related lung disease. PLoS One. 2012;7:e39809. doi: 10.1371/journal.pone.0039809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tamashiro E, Xiong G, Anselmo-Lima WT, Kreindler JL, Palmer JN, Cohen NA. Cigarette smoke exposure impairs respiratory epithelial ciliogenesis. Am J Rhinol Allergy. 2009;23:117–22. doi: 10.2500/ajra.2009.23.3280. [DOI] [PubMed] [Google Scholar]
- 72.Simet SM, Sisson JH, Pavlik JA, Devasure JM, Boyer C, Liu X, et al. Long-term cigarette smoke exposure in a mouse model of ciliated epithelial cell function. Am J Respir Cell Mol Biol. 2010;43:635–40. doi: 10.1165/rcmb.2009-0297OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bhowmik A, Chahal K, Austin G, Chakravorty I. Improving mucociliary clearance in chronic obstructive pulmonary disease. Respir Med. 2009;103:496–502. doi: 10.1016/j.rmed.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 74.Livraghi A, Randell SH. Cystic fibrosis and other respiratory diseases of impaired mucus clearance. Toxicol Pathol. 2007;35:116–29. doi: 10.1080/01926230601060025. [DOI] [PubMed] [Google Scholar]
- 75.Jansen HM, Sachs AP, van Alphen L. Predisposing conditions to bacterial infections in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1995;151:2073–80. doi: 10.1164/ajrccm.151.6.7767560. [DOI] [PubMed] [Google Scholar]
- 76.Sethi S. Bacterial infection and the pathogenesis of COPD. Chest. 2000;117(Suppl 1):286S–91S. doi: 10.1378/chest.117.5_suppl_1.286S. [DOI] [PubMed] [Google Scholar]
- 77.Plotkowski MC, Bajolet-Laudinat O, Puchelle E. Cellular and molecular mechanisms of bacterial adhesion to respiratory mucosa. Eur Respir J. 1993;6:903–16. [PubMed] [Google Scholar]
- 78.Matrosovich M, Klenk HD. Natural and synthetic sialic acid-containing inhibitors of influenza virus receptor binding. Rev Med Virol. 2003;13:85–97. doi: 10.1002/rmv.372. [DOI] [PubMed] [Google Scholar]
- 79.Ryan PA, Pancholi V, Fischetti VA. Group A streptococci bind to mucin and human pharyngeal cells through sialic acid-containing receptors. Infect Immun. 2001;69:7402–12. doi: 10.1128/IAI.69.12.7402-7412.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Walters RW, Pilewski JM, Chiorini JA, Zabner J. Secreted and transmembrane mucins inhibit gene transfer with AAV4 more efficiently than AAV5. J Biol Chem. 2002;277:23709–13. doi: 10.1074/jbc.M200292200. [DOI] [PubMed] [Google Scholar]
- 81.Landry RM, An D, Hupp JT, Singh PK, Parsek MR. Mucin-Pseudomonas aeruginosa interactions promote biofilm formation and antibiotic resistance. Mol Microbiol. 2006;59:142–51. doi: 10.1111/j.1365-2958.2005.04941.x. [DOI] [PubMed] [Google Scholar]
- 82.Sajjan SU, Forstner JF. Identification of the mucin-binding adhesin of Pseudomonas cepacia isolated from patients with cystic fibrosis. Infect Immun. 1992;60:1434–40. doi: 10.1128/iai.60.4.1434-1440.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sajjan US, Corey M, Karmali MA, Forstner JF. Binding of Pseudomonas cepacia to normal human intestinal mucin and respiratory mucin from patients with cystic fibrosis. J Clin Invest. 1992;89:648–56. doi: 10.1172/JCI115631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Schneeberger EE, Lynch RD. The tight junction: a multifunctional complex. Am J Physiol Cell Physiol. 2004;286:C1213–28. doi: 10.1152/ajpcell.00558.2003. [DOI] [PubMed] [Google Scholar]
- 85.Hartsock A, Nelson WJ. Adherens and tight junctions: structure, function and connections to the actin cytoskeleton. Biochim Biophys Acta. 20081778:660–9. doi: 10.1016/j.bbamem.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shin K, Fogg VC, Margolis B. Tight junctions and cell polarity. Annu Rev Cell Dev Biol. 2006;22:207–35. doi: 10.1146/annurev.cellbio.22.010305.104219. [DOI] [PubMed] [Google Scholar]
- 87.Balda MS, Matter K. Tight junctions and the regulation of gene expression. Biochim Biophys Acta. 2009;1788:761–7. doi: 10.1016/j.bbamem.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 88.Koch S, Nusrat A. Dynamic regulation of epithelial cell fate and barrier function by intercellular junctions. Ann N Y Acad Sci. 2009;1165:220–7. doi: 10.1111/j.1749-6632.2009.04025.x. [DOI] [PubMed] [Google Scholar]
- 89.Hogg JC, Timens W. The pathology of chronic obstructive pulmonary disease. Annu Rev Pathol. 2009;4:435–59. doi: 10.1146/annurev.pathol.4.110807.092145. [DOI] [PubMed] [Google Scholar]
- 90.Shaykhiev R, Otaki F, Bonsu P, Dang DT, Teater M, Strulovici-Barel Y, et al. Cigarette smoking reprograms apical junctional complex molecular architecture in the human airway epithelium in vivo. Cell Mol Life Sci. 2011;68:877–92. doi: 10.1007/s00018-010-0500-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.de Boer WI, Sharma HS, Baelemans SM, Hoogsteden HC, Lambrecht BN, Braunstahl GJ. Altered expression of epithelial junctional proteins in atopic asthma: possible role in inflammation. Can J Physiol Pharmacol. 2008;86:105–12. doi: 10.1139/Y08-004. [DOI] [PubMed] [Google Scholar]
- 92.Holgate ST. The sentinel role of the airway epithelium in asthma pathogenesis. Immunol Rev. 2011;242:205–19. doi: 10.1111/j.1600-065X.2011.01030.x. [DOI] [PubMed] [Google Scholar]
- 93.Sajjan U, Wang Q, Zhao Y, Gruenert DC, Hershenson MB. Rhinovirus disrupts the barrier function of polarized airway epithelial cells. Am J Respir Crit Care Med. 2008;178:1271–81. doi: 10.1164/rccm.200801-136OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Singh D, McCann KL, Imani F. MAPK and heat shock protein 27 activation are associated with respiratory syncytial virus induction of human bronchial epithelial monolayer disruption. Am J Physiol Lung Cell Mol Physiol. 2007;293:L436–45. doi: 10.1152/ajplung.00097.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kim JY, Sajjan US, Krasan GP, LiPuma JJ. Disruption of tight junctions during traversal of the respiratory epithelium by Burkholderia cenocepacia. Infect Immun. 2005;73:7107–12. doi: 10.1128/IAI.73.11.7107-7112.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kampf C, Relova AJ, Sandler S, Roomans GM. Effects of TNF-alpha, IFN-gamma and IL-beta on normal human bronchial epithelial cells. Eur Respir J. 1999;14:84–91. doi: 10.1034/j.1399-3003.1999.14a15.x. [DOI] [PubMed] [Google Scholar]
- 97.Coyne CB, Vanhook MK, Gambling TM, Carson JL, Boucher RC, Johnson LG. Regulation of airway tight junctions by proinflammatory cytokines. Mol Biol Cell. 2002;13:3218–34. doi: 10.1091/mbc.E02-03-0134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Roh MH, Fan S, Liu CJ, Margolis B. The Crumbs3-Pals1 complex participates in the establishment of polarity in mammalian epithelial cells. J Cell Sci. 2003;116:2895–906. doi: 10.1242/jcs.00500. [DOI] [PubMed] [Google Scholar]
- 99.Roh MH, Makarova O, Liu CJ, Shin K, Lee S, Laurinec S, et al. The Maguk protein, Pals1, functions as an adapter, linking mammalian homologues of Crumbs and Discs Lost. J Cell Biol. 2002;157:161–72. doi: 10.1083/jcb.200109010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hurd TW, Gao L, Roh MH, Macara IG, Margolis B. Direct interaction of two polarity complexes implicated in epithelial tight junction assembly. Nat Cell Biol. 2003;5:137–42. doi: 10.1038/ncb923. [DOI] [PubMed] [Google Scholar]
- 101.Fan S, Fogg V, Wang Q, Chen XW, Liu CJ, Margolis B. A novel Crumbs3 isoform regulates cell division and ciliogenesis via importin beta interactions. J Cell Biol. 2007;178:387–98. doi: 10.1083/jcb.200609096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fogg VC, Liu CJ, Margolis B. Multiple regions of Crumbs3 are required for tight junction formation in MCF10A cells. J Cell Sci. 2005;118:2859–69. doi: 10.1242/jcs.02412. [DOI] [PubMed] [Google Scholar]
- 103.Wang Q, Margolis B. Apical junctional complexes and cell polarity. Kidney Int. 2007;72:1448–58. doi: 10.1038/sj.ki.5002579. [DOI] [PubMed] [Google Scholar]
- 104.Straight SW, Shin K, Fogg VC, Fan S, Liu CJ, Roh M, et al. Loss of PALS1 expression leads to tight junction and polarity defects. Mol Biol Cell. 2004;15:1981–90. doi: 10.1091/mbc.E03-08-0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Teoh KT, Siu YL, Chan WL, Schlüter MA, Liu CJ, Peiris JS, et al. The SARS coronavirus E protein interacts with PALS1 and alters tight junction formation and epithelial morphogenesis. Mol Biol Cell. 2010;21:3838–52. doi: 10.1091/mbc.E10-04-0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Fan S, Whiteman EL, Hurd TW, McIntyre JC, Dishinger JF, Liu CJ, et al. Induction of Ran GTP drives ciliogenesis. Mol Biol Cell. 2011;22:4539–48. doi: 10.1091/mbc.E11-03-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rao R. Occludin phosphorylation in regulation of epithelial tight junctions. Ann N Y Acad Sci. 2009;1165:62–8. doi: 10.1111/j.1749-6632.2009.04054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cohen CJ, Shieh JT, Pickles RJ, Okegawa T, Hsieh JT, Bergelson JM. The coxsackievirus and adenovirus receptor is a transmembrane component of the tight junction. Proc Natl Acad Sci U S A. 2001;98:15191–6. doi: 10.1073/pnas.261452898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Coyne CB, Bergelson JM. Virus-induced Abl and Fyn kinase signals permit coxsackievirus entry through epithelial tight junctions. Cell. 2006;124:119–31. doi: 10.1016/j.cell.2005.10.035. [DOI] [PubMed] [Google Scholar]
- 110.Bergelson JM, Cunningham JA, Droguett G, Kurt-Jones EA, Krithivas A, Hong JS, et al. Isolation of a common receptor for Coxsackie B viruses and adenoviruses 2 and 5. Science. 1997;275:1320–3. doi: 10.1126/science.275.5304.1320. [DOI] [PubMed] [Google Scholar]
- 111.Comstock AT, Ganesan S, Chattoraj A, Faris AN, Margolis BL, Hershenson MB, et al. Rhinovirus-induced barrier dysfunction in polarized airway epithelial cells is mediated by NADPH oxidase 1. J Virol. 2011;85:6795–808. doi: 10.1128/JVI.02074-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chattoraj SS, Ganesan S, Jones AM, Helm JM, Comstock AT, Bright-Thomas R, et al. Rhinovirus infection liberates planktonic bacteria from biofilm and increases chemokine responses in cystic fibrosis airway epithelial cells. Thorax. 2011;66:333–9. doi: 10.1136/thx.2010.151431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rao R. Oxidative stress-induced disruption of epithelial and endothelial tight junctions. Front Biosci. 2008;13:7210–26. doi: 10.2741/3223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Drees F, Pokutta S, Yamada S, Nelson WJ, Weis WI. Alpha-catenin is a molecular switch that binds E-cadherin-beta-catenin and regulates actin-filament assembly. Cell. 2005;123:903–15. doi: 10.1016/j.cell.2005.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bajpai S, Correia J, Feng Y, Figueiredo J, Sun SX, Longmore GD, et al. alpha-Catenin mediates initial E-cadherin-dependent cell-cell recognition and subsequent bond strengthening. Proc Natl Acad Sci U S A. 2008;105:18331–6. doi: 10.1073/pnas.0806783105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Qian X, Karpova T, Sheppard AM, McNally J, Lowy DR. E-cadherin-mediated adhesion inhibits ligand-dependent activation of diverse receptor tyrosine kinases. EMBO J. 2004;23:1739–48. doi: 10.1038/sj.emboj.7600136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Sörby M, Ostman A. Protein-tyrosine phosphatase-mediated decrease of epidermal growth factor and platelet-derived growth factor receptor tyrosine phosphorylation in high cell density cultures. J Biol Chem. 1996;271:10963–6. doi: 10.1074/jbc.271.18.10963. [DOI] [PubMed] [Google Scholar]
- 118.Aicher B, Lerch MM, Müller T, Schilling J, Ullrich A. Cellular redistribution of protein tyrosine phosphatases LAR and PTPsigma by inducible proteolytic processing. J Cell Biol. 1997;138:681–96. doi: 10.1083/jcb.138.3.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Symons JR, LeVea CM, Mooney RA. Expression of the leucocyte common antigen-related (LAR) tyrosine phosphatase is regulated by cell density through functional E-cadherin complexes. Biochem J. 2002;365:513–9. doi: 10.1042/BJ20020381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wendt MK, Smith JA, Schiemann WP. Transforming growth factor-β-induced epithelial-mesenchymal transition facilitates epidermal growth factor-dependent breast cancer progression. Oncogene. 2010;29:6485–98. doi: 10.1038/onc.2010.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Xiao C, Puddicombe SM, Field S, Haywood J, Broughton-Head V, Puxeddu I, et al. Defective epithelial barrier function in asthma. J Allergy Clin Immunol. 2011;128:549–56 e1-12. doi: 10.1016/j.jaci.2011.05.038. [DOI] [PubMed] [Google Scholar]
- 122.Ganesan S, Unger BL, Comstock AT, Angel KA, Mancuso P, Martinez FJ, et al. Aberrantly activated EGFR contributes to enhanced IL-8 expression in COPD airways epithelial cells via regulation of nuclear FoxO3A. Thorax. 2013;68:131–41. doi: 10.1136/thoraxjnl-2012-201719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schneider D, Ganesan S, Comstock AT, Meldrum CA, Mahidhara R, Goldsmith AM, et al. Increased cytokine response of rhinovirus-infected airway epithelial cells in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;182:332–40. doi: 10.1164/rccm.200911-1673OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Xu W, Kimelman D. Mechanistic insights from structural studies of beta-catenin and its binding partners. J Cell Sci. 2007;120:3337–44. doi: 10.1242/jcs.013771. [DOI] [PubMed] [Google Scholar]
- 125.Tian D, Zhu M, Li J, Ma Y, Wu R. Cigarette smoke extract induces activation of beta-catenin/TCF signaling through inhibiting GSK3beta in human alveolar epithelial cell line. Toxicol Lett. 2009;187:58–62. doi: 10.1016/j.toxlet.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 126.Mazieres J, He B, You L, Xu Z, Jablons DM. Wnt signaling in lung cancer. Cancer Lett. 2005;222:1–10. doi: 10.1016/j.canlet.2004.08.040. [DOI] [PubMed] [Google Scholar]
- 127.Khan EM, Lanir R, Danielson AR, Goldkorn T. Epidermal growth factor receptor exposed to cigarette smoke is aberrantly activated and undergoes perinuclear trafficking. FASEB J. 2008;22:910–7. doi: 10.1096/fj.06-7729com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lemjabbar H, Li D, Gallup M, Sidhu S, Drori E, Basbaum C. Tobacco smoke-induced lung cell proliferation mediated by tumor necrosis factor alpha-converting enzyme and amphiregulin. J Biol Chem. 2003;278:26202–7. doi: 10.1074/jbc.M207018200. [DOI] [PubMed] [Google Scholar]
- 129.Vinhas R, Cortes L, Cardoso I, Mendes VM, Manadas B, Todo-Bom A, et al. Pollen proteases compromise the airway epithelial barrier through degradation of transmembrane adhesion proteins and lung bioactive peptides. Allergy. 2011;66:1088–98. doi: 10.1111/j.1398-9995.2011.02598.x. [DOI] [PubMed] [Google Scholar]
- 130.Wan H, Winton HL, Soeller C, Tovey ER, Gruenert DC, Thompson PJ, et al. Der p 1 facilitates transepithelial allergen delivery by disruption of tight junctions. J Clin Invest. 1999;104:123–33. doi: 10.1172/JCI5844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ibrahim HR, Aoki T, Pellegrini A. Strategies for new antimicrobial proteins and peptides: lysozyme and aprotinin as model molecules. Curr Pharm Des. 2002;8:671–93. doi: 10.2174/1381612023395349. [DOI] [PubMed] [Google Scholar]
- 132.Ellison RT, 3rd, Giehl TJ. Killing of gram-negative bacteria by lactoferrin and lysozyme. J Clin Invest. 1991;88:1080–91. doi: 10.1172/JCI115407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Ganz T. Antimicrobial polypeptides in host defense of the respiratory tract. J Clin Invest. 2002;109:693–7. doi: 10.1172/JCI15218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.van der Strate BW, Beljaars L, Molema G, Harmsen MC, Meijer DK. Antiviral activities of lactoferrin. Antiviral Res. 2001;52:225–39. doi: 10.1016/S0166-3542(01)00195-4. [DOI] [PubMed] [Google Scholar]
- 135.Laube DM, Yim S, Ryan LK, Kisich KO, Diamond G. Antimicrobial peptides in the airway. Curr Top Microbiol Immunol. 2006;306:153–82. doi: 10.1007/3-540-29916-5_6. [DOI] [PubMed] [Google Scholar]
- 136.Taylor DC, Cripps AW, Clancy RL. A possible role for lysozyme in determining acute exacerbation in chronic bronchitis. Clin Exp Immunol. 1995;102:406–16. doi: 10.1111/j.1365-2249.1995.tb03798.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Jacquot J, Tournier JM, Puchelle E. In vitro evidence that human airway lysozyme is cleaved and inactivated by Pseudomonas aeruginosa elastase and not by human leukocyte elastase. Infect Immun. 1985;47:555–60. doi: 10.1128/iai.47.2.555-560.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Taggart CC, Lowe GJ, Greene CM, Mulgrew AT, O’Neill SJ, Levine RL, et al. Cathepsin B, L, and S cleave and inactivate secretory leucoprotease inhibitor. J Biol Chem. 2001;276:33345–52. doi: 10.1074/jbc.M103220200. [DOI] [PubMed] [Google Scholar]
- 139.Parameswaran GI, Sethi S, Murphy TF. Effects of bacterial infection on airway antimicrobial peptides and proteins in COPD. Chest. 2011;140:611–7. doi: 10.1378/chest.10-2760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.McElvaney NG, Nakamura H, Birrer P, Hébert CA, Wong WL, Alphonso M, et al. Modulation of airway inflammation in cystic fibrosis. In vivo suppression of interleukin-8 levels on the respiratory epithelial surface by aerosolization of recombinant secretory leukoprotease inhibitor. J Clin Invest. 1992;90:1296–301. doi: 10.1172/JCI115994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ganz T. Defensins: antimicrobial peptides of innate immunity. Nat Rev Immunol. 2003;3:710–20. doi: 10.1038/nri1180. [DOI] [PubMed] [Google Scholar]
- 142.Kota S, Sabbah A, Chang TH, Harnack R, Xiang Y, Meng X, et al. Role of human beta-defensin-2 during tumor necrosis factor-alpha/NF-kappaB-mediated innate antiviral response against human respiratory syncytial virus. J Biol Chem. 2008;283:22417–29. doi: 10.1074/jbc.M710415200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.McCray PB, Jr., Bentley L. Human airway epithelia express a beta-defensin. Am J Respir Cell Mol Biol. 1997;16:343–9. doi: 10.1165/ajrcmb.16.3.9070620. [DOI] [PubMed] [Google Scholar]
- 144.Becker MN, Diamond G, Verghese MW, Randell SH. CD14-dependent lipopolysaccharide-induced beta-defensin-2 expression in human tracheobronchial epithelium. J Biol Chem. 2000;275:29731–6. doi: 10.1074/jbc.M000184200. [DOI] [PubMed] [Google Scholar]
- 145.Singh PK, Jia HP, Wiles K, Hesselberth J, Liu L, Conway BA, et al. Production of beta-defensins by human airway epithelia. Proc Natl Acad Sci U S A. 1998;95:14961–6. doi: 10.1073/pnas.95.25.14961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Dauletbaev N, Gropp R, Frye M, Loitsch S, Wagner TO, Bargon J. Expression of human beta defensin (HBD-1 and HBD-2) mRNA in nasal epithelia of adult cystic fibrosis patients, healthy individuals, and individuals with acute cold. Respiration. 2002;69:46–51. doi: 10.1159/000049369. [DOI] [PubMed] [Google Scholar]
- 147.Goldman MJ, Anderson GM, Stolzenberg ED, Kari UP, Zasloff M, Wilson JM. Human beta-defensin-1 is a salt-sensitive antibiotic in lung that is inactivated in cystic fibrosis. Cell. 1997;88:553–60. doi: 10.1016/S0092-8674(00)81895-4. [DOI] [PubMed] [Google Scholar]
- 148.Herr C, Beisswenger C, Hess C, Kandler K, Suttorp N, Welte T, et al. R Bals for the CAPNETZ Study Group Suppression of pulmonary innate host defence in smokers. Thorax. 2009;64:144–9. doi: 10.1136/thx.2008.102681. [DOI] [PubMed] [Google Scholar]
- 149.Bals R, Wang X, Zasloff M, Wilson JM. The peptide antibiotic LL-37/hCAP-18 is expressed in epithelia of the human lung where it has broad antimicrobial activity at the airway surface. Proc Natl Acad Sci U S A. 1998;95:9541–6. doi: 10.1073/pnas.95.16.9541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zheng S, De BP, Choudhary S, Comhair SA, Goggans T, Slee R, et al. Impaired innate host defense causes susceptibility to respiratory virus infections in cystic fibrosis. Immunity. 2003;18:619–30. doi: 10.1016/S1074-7613(03)00114-6. [DOI] [PubMed] [Google Scholar]
- 151.Zheng S, Xu W, Bose S, Banerjee AK, Haque SJ, Erzurum SC. Impaired nitric oxide synthase-2 signaling pathway in cystic fibrosis airway epithelium. Am J Physiol Lung Cell Mol Physiol. 2004;287:L374–81. doi: 10.1152/ajplung.00039.2004. [DOI] [PubMed] [Google Scholar]
- 152.Moskwa P, Lorentzen D, Excoffon KJ, Zabner J, McCray PB, Jr., Nauseef WM, et al. A novel host defense system of airways is defective in cystic fibrosis. Am J Respir Crit Care Med. 2007;175:174–83. doi: 10.1164/rccm.200607-1029OC. [DOI] [PMC free article] [PubMed] [Google Scholar]


