A previously healthy 14 month old child was transferred to our medical centre with a severe head injury. The father had collected the boy and his 3 year old brother from their mother at his workplace car park and taken them home while their mother went to work. The children had been watching television while the father prepared dinner. After hearing something fall, the father found the boy on the floor with the television covering the right side of the head and anterior chest. A homemade television stand was partially across the child's lower legs. His older brother stated, “television fell.” As soon as the father removed the television, he noticed the child's head beginning to swell. A neighbour drove them to the local hospital. According to the father and the neighbour, the child never stopped breathing and no resuscitative efforts were attempted.
Cranial computed tomography showed extensive head injuries. He had soft tissue swelling of the scalp, diffuse cerebral oedema with a subdural haematoma overlying the frontal convexities and layering along the falx cerebri, a left sided skull fracture adjacent to a widely diastatic coronal suture, cerebral contusions beneath the fracture, and a rightward midline shift measuring 8 mm. The paediatric ophthalmologist described bilateral dot and blot intraretinal haemorrhages, preretinal haemorrhages, and perimacular retinal folds (fig 1).
Fig 1.
Clinical image highlighting temporal portion of perimacular retinal fold at 2-3 o'clock area in left eye with a blood vessel bending over the fold (magnification ×6)
The child's condition deteriorated, and he died 18 hours after the incident. Child Protective Services removed the 3 year old sibling from the home because the retinal haemorrhages and retinal folds were considered diagnostic of abusive head trauma from shaking. This action was taken despite the father's repeated detailed, consistent account provided to emergency staff, the paediatric child abuse specialist, paediatric intensive care doctors, and law enforcement authorities.
Postmortem evidence
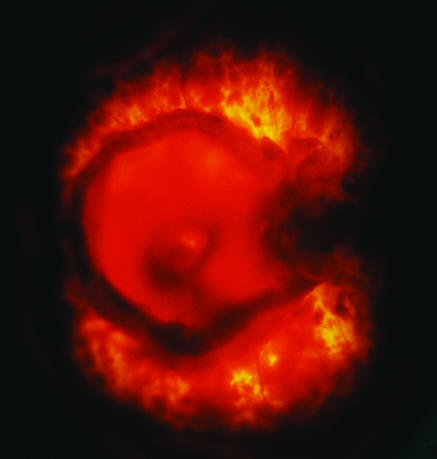
A forensic autopsy showed no direct trauma to the orbits or eyes. There were prominent bilateral scalp contusions with soft tissue and intramuscular haemorrhage, symmetrical parietal skull fractures with coronal sutural diastasis, and a lacerated dura mater with extrusion of brain and blood. In addition to bilateral subdural and subarachnoid haemorrhages, a thin epidural haematoma partially covered the frontoparietal, calvarial lamina interna. The brain showed bilateral cortical contusions, severe cerebral oedema, and diffuse anoxic-ischemic injury. Postmortem ocular examination showed haemorrhages of the optic nerve sheaths with subdural haemorrhage greater than subarachnoid haemorrhage. Both eyes had extensive retinal haemorrhages with perimacular retinal folds (fig 2). Retinoschisis and peripapillary intrascleral haemorrhages were evident, and the retinal haemorrhages extended from the posterior pole to the ora serrata affecting the preretinal, intraretinal, and subretinal layers.
Fig 2.
Transilluminated retinal image of right eye at autopsy showing circinate, elevated, perimacular retinal fold and extensive retinal haemorrhages
When investigators went to the house to recover the television before the family returned home, it was still on the carpeted floor. The 480 mm screen television with built in videocassette recorder weighed 19.5 kg. The homemade television stand measured 762 mm (height)×635 mm (width)×508 mm (depth) and had a bottom drawer that held videotapes. A greasy smudged area on the glass of the television corresponded with the impact site on the child's head.
A re-enactment in which a 11.4 kg weight (similar to the child's weight at autopsy of 11.8 kg) was placed on the partially opened drawer caused the television and television stand to readily topple forward. According to investigators, the family home was 7.8 km from the workplace and about 6 km from the local hospital. Based on the distance and estimated driving times plus workplace time clock records, the father was home with the children about 20 minutes when the incident happened. The day after the incident, while in foster care, the 3 year old sibling corroborated the father's account. Despite all this evidence, the paediatric ophthalmologist repeated that perimacular retinal folds coincident with retinal haemorrhages were considered specific for shaken baby syndrome secondary to retinal traction exerted by the oscillating vitreous.
Search for published evidence
We were unable to find a published report of perimacular retinal folds in a childhood non-abusive head injury. We therefore did a systematic review of the medical literature on perimacular retinal folds associated with abusive head trauma in infants and young children. Our background question became: “In infants and young children with an acute intracranial injury, are perimacular retinal folds specific for head injury from vitreoretinal traction occurring during cycles of acceleration and deceleration (shaken baby syndrome)?”
We searched the Medline (1966-2003) database using the terms retinal folds and child abuse and uncovered seven non-comparative case series articles.1-7 We also examined references cited in these articles plus review articles and book chapters on ocular findings in child abuse mentioning or discussing perimacular retinal folds relative to non-accidental head injury. Similar searches in the Cochrane Library, ISI Web of Science, and Ovid found no additional articles.
Results
We found 42 articles and book chapters discussing perimacular retinal folds in childhood abusive head trauma. Seventeen mentioned the presence of retinal folds in non-accidental head injury but did not comment on specificity or formative mechanism. A table on bmj.com gives details of the remaining articles. All but two of the articles are non-comparative clinical or autopsy case series, case reports, review articles, or book chapters.
The two studies that included controls both showed bias in selection of controls and contained no cases with perimacular retinal folds but discussed the postulated causal mechanism.8,9 In the prospective controlled study, the authors reported on 79 children younger than 3 years who had sustained head injuries.8 The manner of injury in one case was indeterminate. Three children, including one who died, had non-accidental head injury diagnosed, all of whom had retinal haemorrhages; 72 of the 75 children with non-abusive injuries were managed by observation alone. No perimacular retinal folds were observed; however, the presumed causative mechanism of traumatic retinoschisis and retinal folds was discussed.
The second controlled study was a prospective autopsy study that examined the presence and location of ocular findings in 169 childhood deaths.9 Ocular haemorrhages (retinal, peripheral retinal, optic nerve sheath and intrascleral) were more likely in craniocerebral trauma than in non-head injuries and natural diseases. Although case selection was purportedly random, the study contained a disproportionately high number of deaths from child abuse compared with natural and non-abusive causes. Case selection depended on the pathologist's willingness to participate in the study, and we were told by one of the authors that pathologists were more willing to participate when they believed that the deaths were abusive or suspicious (M Gilliland, personal communication, 2002). Perimacular retinal folds were not noted, but the authors concluded that acceleration-deceleration injury to the retina accounts for peripheral retinal haemorrhages and retinal folds.
Supporting evidence
The references cited to support statements about the specificity or causal mechanism of perimacular retinal folds and abusive head injury in the articles we found are all non-comparative observational reports, unsystematic review articles, and book chapters. Seventy per cent of the articles cited four non-comparative case series.1,2,3,10 We assessed the quality of this evidence.
Gaynon et al reported on two infants with presumed shaken baby syndrome who had retinal folds and concluded that these folds may be a hallmark of shaking injuries in child abuse victims.1 One infant reportedly fell 1.5 m to the floor while being carried down a stairway.
Massicotte et al reported the ocular findings at autopsy of three children with perimacular retinal folds.2 Two infants had sustained direct head trauma, but in the other there was no physical or forensic evidence of direct head trauma. They observed that the vitreous had partially separated from the retina but remained attached to the internal limiting membrane at the apices of the folds and the vitreous base. They concluded that their study confirmed the role of vitreous traction in formation of perimacular folds and proved that shaking alone caused these folds and shaking was never an accidental phenomenon.
Elner et al reviewed the ocular and autopsy findings in 10 consecutive children who died of suspected child abuse.3 Perimacular retinal folds were observed in three children, all of whom had evidence of blunt head injuries.
Greenwald et al reported five cases of children in whom definite or probable physical abuse during infancy was associated with traumatic retinoschisis.10 They hypothesised that when an infant is shaken, the head is subjected to repetitive accelerations and decelerations causing the relatively dense lens to move forward and back within the ocular fluids. Transmission of force through firm attachments between the lens, vitreous gel, and particularly the macular retina presumably would result in appreciable traction on the retina causing it to split and creating the surrounding folds.
Discussion
Statements in the medical literature that perimacular retinal folds are diagnostic of shaken baby syndrome are not supported by objective scientific evidence. Non-comparative observational reports and unsystematic narrative review articles contain insufficient evidence to provide unbiased support for or against diagnostic specificity, and inferences about associations, causal or otherwise, cannot be determined. Clinical and autopsy evidence of ocular lesions must therefore be considered alongside other physical findings and a thorough investigation before concluding whether a head injury is caused by abuse. The child in our case had ocular haemorrhages (peripheral retinal, optic nerve sheath and intrascleral) and retinoschisis, which again some people consider specific for child abuse. Unfortunately, the evidence for these assumptions has similar problems to that for perimacular retinal folds. An evidence based analyis of indexed medical publications on shaken baby syndrome from 1966-1998 uncovered a weak scientific evidence base.11 Selection bias, inappropriate controls, and the lack of precise criteria for case definition were identified as important problems with the data. Many studies committed a fallacy of assumption, selecting cases by the presence of the clinical findings that were sought as diagnostically valid. Unsystematic reviews and consensus statements often mingled opinion with facts and added no original supporting evidence.
Perimacular retinal folds are associated with increased neurological morbidity and mortality in infants and children with abusive head injuries.6 The reported incidence of perimacular retinal folds in shaken baby syndrome varies from 6% in a consecutive clinical case series to 50% in a sequential autopsy case series.5,12 Clinical and autopsy studies with appropriately matched controls are needed to determine the causal mechanism of perimacular retinal folds and their specificity for abusive head injury. Until good evidence is available, we urge caution in interpreting eye findings out of context.
Supplementary Material
 Details of the included studies are on bmj.com
Details of the included studies are on bmj.com
Editorials by Geddes and Plunkett and Harding et al
Contributors: PEL conceived the idea, collected the articles, and wrote the initial draft. All authors contributed to the review process, writing, and final editing of the paper. PEL is the guarantor.
Competing interests: None declared.
References
- 1.Gaynon MW, Koh K, Marmor MF, Frankel LR. Retinal folds in the shaken baby syndrome. Am J Ophthalmol 1988;106: 423-5. [DOI] [PubMed] [Google Scholar]
- 2.Massicotte SJ, Folberg R, Torczynski E, Gilliland MG, Luckenbach MW. Vitreoretinal traction and perimacular retinal folds in the eyes of deliberately traumatized children. Ophthalmology 1991;98: 1124-7. [DOI] [PubMed] [Google Scholar]
- 3.Elner SG, Elner VM, Arnall M Albert DM. Ocular and associated findings in suspected child abuse. A necropsy study. Arch Ophtlamol 1990;108: 1094-101. [DOI] [PubMed] [Google Scholar]
- 4.Han DP, Wilkinson WS. Late ophthalmic manifestations of the shaken baby syndrome. J Paediatr Ophthalmol Strabismus 1990;27: 299-303. [DOI] [PubMed] [Google Scholar]
- 5.Marshall DH, Brownstein S, Dorey MW, Addison DJ, Carpenter B. The spectrum of postmortem ocular findings in victims of shaken baby syndrome. Can J Ophthalmol 2001;36: 377-83. [DOI] [PubMed] [Google Scholar]
- 6.Mills M. Funduscopic lesions associated with mortality in shaken baby syndrome. J Am Assoc Pediatr Ophthalmol Strabismus 1998;2: 67-71. [DOI] [PubMed] [Google Scholar]
- 7.Munger CE, Peiffer RL, Bouldin TW, Kylstra JA, Thompson RL. Ocular and associated neuropathologic observations in suspected whiplash shaken infant syndrome: a retrospective study of 12 cases. Am J Forensic Med Pathol 1993;14: 193-200. [DOI] [PubMed] [Google Scholar]
- 8.Buys YM, Levin AV, Enzenauer RW, Elder JE, Letourneau MA, Humphreys RP, et al. Retinal findings after head trauma in infants and young children. Ophthalmology 1992;99: 1718-23. [DOI] [PubMed] [Google Scholar]
- 9.Gilliland MG, Luckenbach MW, Chenier TC. Systemic and ocular findings in 169 prospectively studied child deaths: retinal haemorrhages usually mean child abuse. Forensic Sci Int 1994;68: 117-32. [DOI] [PubMed] [Google Scholar]
- 10.Greenwald MJ, Weiss A, Oesterle CS, Friendly DS. Traumatic retinoschisis in battered babies. Ophthalmology 1986;93: 618-25. [DOI] [PubMed] [Google Scholar]
- 11.Donohoe M. Evidence-based medicine and shaken baby syndrome. Part 1: literature review, 1966-1998. Am J Forensic Med Pathol 2003;24: 239-42. [DOI] [PubMed] [Google Scholar]
- 12.Kivlin JD, Simons KB, Lazoritz S, Ruttum MS. Shaken baby syndrome. Ophthalmology 2000;107: 1246-54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.