BCR/ABL-induced chronic myeloid leukemia (CML) is a stem cell-induced but progenitor cell-driven disease, which usually starts as a relatively benign chronic phase (CML-CP), eventually progressing to a fatal blast crisis (CML-BC).1 The frequency of additional chromosomal abnormalities is approximately 7% in CML-CP and increases to 40–70% in the advanced phases.2 In addition, chromosomal aberrations have also been found in leukemia cells resistant to dasatinib and/or imatinib, and in patients relapsing after hematopoietic transplantation.3,4
The most frequently noticed chromosomal errors involve numerical gains and losses of chromosomes, isochromosome i(17q) causing loss of p53, reciprocal translocations 3;21 and 7;11 generating AML-1/Evi-1 and NUP98/HOXA9 fusion proteins, respectively, and other translocations and inversions associated with AML/myelodysplasia, such as inv(3) and t(15;17).5 Clinical and experimental observations strongly suggest that these aberrations may contribute to malignant progression/relapse of the disease.2,6-10
BCR/ABL kinase results from unfaithful repair of two DNA double-strand breaks (DSBs) generating t(9;22), which may represent a random event or result from preexisting conditions associated with genomic instability.5,11 Therefore, additional chromosomal aberrations accumulated during the course of CML may be promoted by preexisting condition responsible for t(9;22) and/or by BCR/ABL. The latter statement is supported by reports that BCR/ABL-positive cells acquire more DSBs than normal counterparts in response to endogenous reactive oxygen species (ROS) and genotoxic treatment12-15 and that BCR/ABL stimulates the efficiency but decreases the fidelity of DSB repair mechanisms.13,16,17 However, the former speculation cannot be ruled out because chromosome abnormalities were detected in t(9;22)-negative metaphases appearing during imatinib therapy in patients with newly diagnosed CML-CP.18,19
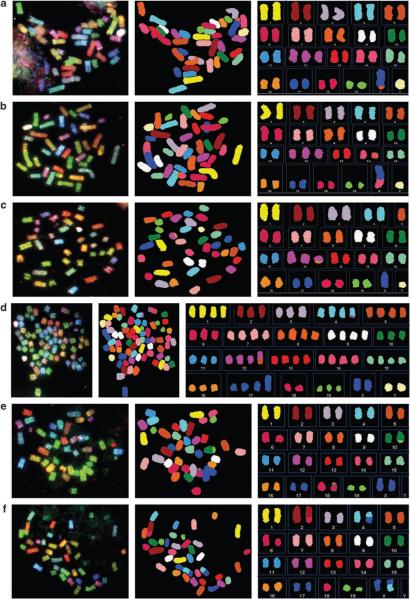
To test the hypothesis that BCR/ABL facilitates the accumulation of ROS-induced chromosomal aberrations, freshly established 32Dcl3-BCR/ABL and parental 32Dcl3-neo cells were continuously cultured in vitro for 8 weeks in the presence or absence of an antioxidant, vitamin E (VE) as described before,20 and then analyzed by SKY (spectral karyotype analysis) to detect acquired chromosomal aberrations. Although parental cells did not contain consistent chromosomal aberrations, one or two additional chromosomes 12 (+12, +12×2) were detected in all metaphases of 32Dcl3-BCR/ABL cells maintained in regular medium (Table 1, VE in vitro, P-C and B/A-C, respectively). Inhibition of ROS by VE was associated with approximately twofold reduction of the number of cells displaying +12 (Table 1, VE in vitro, B/A-VE, respectively). In addition, one or two der(X)t(X;8) chromosomal translocations (Figure 1a) were present in 9 of 10 metaphases of BCR/ABL cells, but the translocation was not detected if ROS was inhibited by VE. It is likely that BCR/ABL-positive cells containing +12×2 and der(X)t(X;8)×2 represent a clone derived from the +12, der(X)t(X;8) cell because they display 82, XY karyotype.
Table 1.
BCR/ABL promotes accumulation of ROS and radiation-induced chromosomal aberrations in vitro and in vivo
| Conditions | Cells (metaphases analyzed) |
Additional (+) and missing (−) chromosomes | T and T | T and T per metaphase |
Aberrations per metaphase |
|---|---|---|---|---|---|
| VE in vitro | P-C (10) | 0 | 0 | 0 | 0 |
| B/A-C (10) | +12 [7], +12 × 2 [3] | der(X)t(X;8) [6], der(X)t(X;8)x2 [3] | 1.2±0.6* | 2.5±1.1** | |
| B/A-VE (13) | +12 [7] | 0 | 0 | 0.5±0.5 | |
| VE in vivo | B/A-C (13) | +12 [13] | der(X)t(X;8) [6], der(14)t(8;14) [6], der(X)t(X;14), [6], der(X)t(X;9) [1] |
1.5±0.5* | 2.5±0.5** |
| B/A-VE (12) | +12 [8], −5 [1],−Y [1] | der(X)t(X;8) [8], der(14)t(8;14) [1], der(12)t(12;16) [3] | 1.0±0.0 | 1.8±0.6 | |
| γ-irradiation | P(10) | 0 | 0 | 0 | 0 |
| B/A (9) | 71–78, <4N>XXYY [9] | der(4)t(4;12) [9], met(17)t(17;17) [9], der(12)t(5;12) [1], der(9)t(9;13) [1] |
2.2±0.4* | N.C. | |
| bmc-B/A (15) | −18 [2], −2 [1], −4 [1], −11 [1], −13 [1], −X [1] |
del(6) [15], t(X;4) [10], der(6)t(X;6) [2], dic(2;7) [1], +der(4)t(4;11) [1], der(4)ins(4;11) [1], dic(2:18) [1], dic(5:18) [1], der(X)t(X;1) [1], +der(1)t(1;8) [1], der(3)t(3;13) [1], der(8)t(8;14) [1], der(14)t(3;14) [1], der(10)t(10;19) [1], del(11) [1], del(2) [1] |
2.8±1.1 | 3.3±1.9 |
Abbreviations: IL-3, interleukin-3; NC, not calculated; ROS, reactive oxygen species; SCF, stem cell factor; T and T, translocations and truncations; VE, vitamin E.
Metaphase spreads were analyzed by the Columbia University SKY core facility using the Applied Spectral Imaging software. Results indicate consistent chromosomal aberrations detected by SKY (number of metaphases displaying the chromosomal aberrations), and the statistical significance was probed by unpaired Student’s t-test.
VE in vitro: freshly established mixtures of 32Dcl3 clones expressing p210BCR/ABL (B/A) or empty plasmid (P) were obtained as described before (no chromosomal aberrations detected)20 and maintained in the continuous culture for 8 weeks in the absence (C) or presence of 200 μM VE (VE). VE decreased the level of ROS and did not affect cell proliferation rate in tissue culture.20
P<10−6 in comparison with P-C and B/A-VE group
P<10−6 and P<10−5 in comparison with P-C and B/A-VE groups, respectively.
VE in vivo: BCR/ABL-positive cells were harvested from leukemic SCID mice after 8 weeks of feeding with regular (B/A-C) or VE-rich (B/A-VE) chow to reduce ROS as described before.20
P = 0.005
P = 0.009 in comparison with corresponding VE groups.
γ-Irradiation: 32Dcl3-neo (P) and 32Dcl3-BCR/ABL (B/A) cells were described above. Bone marrow mononuclear cells from C57Bl/6 female mice (The Jackson Laboratory, Bar Harbor, ME, USA) were infected with BCR/ABL-IRES-GFP retroviral particles as described.17. GFP+ BCR/ABL-positive cells obtained by sorting were expanded for 2 weeks in the presence of pre-tested minimal concentrations of SCF+IL-3 required to maintain proliferation (bmc-B/A). Cells were irradiated from 137Cs source with 2, 3, and 4Gy in a weekly intervals to allow recovery of proliferation.13 One week after the last irradiation cells were analyzed by SKY.
P<10−6 in comparison to P group.
Figure 1.
Representative examples of SKY analyses of chromosomal aberrations described in Table 1: VE in vitro (a), VE in vivo (b, c) and γ-irradiation (B/A in d and bmc-B/A in e, f). Metaphases with spectral colors (left panel), metaphases with classified colors (middle panel), and metaphase panels (right panel) are shown. Chromosomal instability is demonstrated by the karyotype as follows: (a) 41,Y,der(X)t(X;8),+12; (b) 41,Y,der(X)t(X;14),der(14)t(8;14),+12; (c) 40,XY,der(12)t(12;16),-5,+12; (d) 71, XXYY, der(4)t(4;12), met(17)t(17;17), der(12)t(5;12); (e) 40, XX, del(6), der(10)t(10;19); and (f) 39, XX, del(6), t(X;4), dic (2;18).
SCID mice were injected with freshly established 32Dcl3-BCR/ABL cells and fed with control or VE-rich diet to reduce ROS.20 All analyzed metaphases of 32Dcl3-BCR/ABL leukemia cells obtained from mice fed with control chow contained an additional chromosome 12 and one or more chromosomal translocation, such as der(X)t(X;8), der(14)t(8;14), der(X)t(X;14) and der(X)t(X;9) (Table 1, VE in vivo, B/A). However, leukemia cells from the mice fed with VE-rich diet displayed no more than one of the chromosomal translocations, such as der(X)t(X;8), der(14)t(8;14) or der(12)t(12;16), and 75% of metaphases displayed +12 (Table 1, VE in vivo, B/A-VE). Metaphases containing some of the described aberrations are presented in Figures 1b and c. The relatively weaker antimutagenic effect of VE in vivo than in vitro may be due to less efficient inhibition of ROS in mice in comparison to tissue culture.
To test whether BCR/ABL promotes chromosomal aberrations after genotoxic treatment cells were allowed to recover after irradiation to detect errors which do not exert a negative impact on cell survival/proliferation as described by Libura et al.21 These aberrations may exert an effect on the disease path.
32Dcl3-neo cells did not display any consistent chromosomal abnormalities (Table 1, γ-irradiation, P). In sharp contrast, all metaphases of 32Dcl3-BCR/ABL cells contained close to 80 chromosomes and carried der(4)t(4;12) chromosomal translocation and metacentric chromosome 17, which is a fusion of the centromeres of two chromosome 17s (Table 1, γ-irradiation, B/A, Figure 1d). Moreover, two additional translocations der(12)t(5;12) and der(9)t(9;13) were detected in individual metaphases.
In addition, BCR/ABL-transformed murine bone marrow cells (bmc-B/A) surviving irradiation acquired numerous chromosomal defects (Table 1, γ-irradiation). Basically, del(6) is consistent in all 15 metaphases, but it does not appear to result from preexisting aberration because C67Bl/6 mice display normal karyotype. t(4;X) and der(6)t(X;6) is present in 10 of 15 and 2 of 15 metaphases, respectively. Other aberrations listed in Table 1 and shown in Figures 1e and f are detected in only one cell each representing individual breaks and exchanges due to irradiation. Cells expressing empty plasmid did not resume enough proliferation potential during the experiment to allow SKY analysis. This effect is in concordance with the report that normal murine hematopoietic stem cells are very sensitive to irradiation in comparison with BCR/ABL-positive counterparts.22
The experimental conditions applied here reflected two clinical situations where chromosomal instability is acquired spontaneously during the disease course (ROS-induced) and after high-dose chemo/radiotherapy treatment before hematopoietic transplantation (irradiation-induced) to address the dilemma whether the accumulation of additional chromosomal aberrations in CML is driven by BCR/ABL and/or by already preexisting mechanism(s) responsible for t(9;22). Our work demonstrated that the presence of BCR/ABL significantly enhanced chromosomal instability (aneuploidy, translocations, truncations) induced by ROS and γ-irradiation; however, we cannot exclude the possibility that preexisting conditions, which generate t(9;22), may work in concert with BCR/ABL to destabilize chromosomes. In addition, although viral sequences were integrated in both parental and BCR/ABL-positive cells, the possibility that viral integration combined with BCR/ABL kinase may exert some mutagenic effect in leukemia cells cannot be eliminated.
BCR/ABL-dependent mechanisms facilitating chromosomal aberrations are not known. BCR/ABL-positive cells in comparison with normal counterparts contain more DSBs induced by ROS and γ-irradiation, and demonstrate increased capability to survive DNA damage.12,13,22 In addition, leukemia cells have enhanced probability to accumulate chromosomal errors due to a negative effect of BCR/ABL kinase on the fidelity of DSBs repair.5 The potential role for unfaithful DSB repair mechanisms can be suggested, because BCR/ABL kinase enhances the expression of RAD51 and downregulates DNA-PKcs, key elements in two major mechanisms of DSBs repair, homologous recombination repair and non-homologous end-joining, respectively.17,23 Interestingly, overexpression of RAD51 and the inhibition of DNA-PKcs promoted aneuploidy and multiple chromosomal rearrangements.24,25 The negative effect of BCR/ABL kinase on the fidelity of DSB repair should be further elucidated to attenuate malignant progression and relapse of CML.
Acknowledgements
This work was supported by the grants from the Department of Defense W81XWH-05-1-0214 (to T Skorski), and NCI R01CA100159-4 and the Stewart Trust Foundation (to C Richardson).
Footnotes
Note added in proof
Dr Martin Carroll (University of Pennsylvania, Philadelphia, PA, USA) submitted the manuscript indicating that BCR/ABL induces chromosomal aberrations after genotoxic stress.
References
- 1.Melo JV, Barnes DJ. Chronic myeloid leukaemia as a model of disease evolution in human cancer. Nat Rev Cancer. 2007;7:441–453. doi: 10.1038/nrc2147. [DOI] [PubMed] [Google Scholar]
- 2.Bacher U, Haferlach T, Hiddemann W, Schnittger S, Kern W, Schoch C. Additional clonal abnormalities in Philadelphia-positive ALL and CML demonstrate a different cytogenetic pattern at diagnosis and follow different pathways at progression. Cancer Genet Cytogenet. 2005;157:53–61. doi: 10.1016/j.cancergencyto.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 3.Fabarius A, Haferlach C, Muller MC, Erben P, Lahaye T, Giehl M, et al. Dynamics of cytogenetic aberrations in Philadelphia chromosome positive and negative hematopoiesis during dasatinib therapy of chronic myeloid leukemia patients after imatinib failure. Haematologica. 2007;92:834–837. doi: 10.3324/haematol.11064. [DOI] [PubMed] [Google Scholar]
- 4.Huang Q, Wu Y, Snyder DS, Chang KL, Slovak ML, Gaal KK, et al. Clinical and pathologic analysis of 16 cases of relapsed chronic myeloid leukemia after stem cell transplantation. Am J Clin Pathol. 2007;128:565–570. doi: 10.1309/ECDWCRLG889K1GGD. [DOI] [PubMed] [Google Scholar]
- 5.Penserga ET, Skorski T. Fusion tyrosine kinases: a result and cause of genomic instability. Oncogene. 2007;26:11–20. doi: 10.1038/sj.onc.1209756. [DOI] [PubMed] [Google Scholar]
- 6.Johansson B, Fioretos T, Mitelman F. Cytogenetic and molecular genetic evolution of chronic myeloid leukemia. Acta Haematol. 2002;107:76–94. doi: 10.1159/000046636. [DOI] [PubMed] [Google Scholar]
- 7.Preti HA, O’Brien S, Giralt S, Beran M, Pierce S, Kantarjian HM. Philadelphia-chromosome-positive adult acute lymphocytic leukemia: characteristics, treatment results, and prognosis in 41 patients. Am J Med. 1994;97:60–65. doi: 10.1016/0002-9343(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 8.Skorski T, Nieborowska-Skorska M, Wlodarski P, Perrotti D, Martinez R, Wasik MA, et al. Blastic transformation of p53-deficient bone marrow cells by p210bcr/abl tyrosine kinase. Proc Natl Acad Sci USA. 1996;93:13137–13142. doi: 10.1073/pnas.93.23.13137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dash AB, Williams IR, Kutok JL, Tomasson MH, Anastasiadou E, Lindahl K, et al. A murine model of CML blast crisis induced by cooperation between BCR/ABL and NUP98/HOXA9. Proc Natl Acad Sci USA. 2002;99:7622–7627. doi: 10.1073/pnas.102583199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitani K, Ogawa S, Tanaka T, Miyoshi H, Kurokawa M, Mano H, et al. Generation of the AML1-EVI-1 fusion gene in the t(3;21)(q26;q22) causes blastic crisis in chronic myelocytic leukemia. EMBO J. 1994;13:504–510. doi: 10.1002/j.1460-2075.1994.tb06288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papadopoulos PC, Greenstein AM, Gaffney RA, Westbrook CA, Wiedemann LM. Characterization of the translocation breakpoint sequences in Philadelphia-positive acute lymphoblastic leukemia. Genes Chromosomes Cancer. 1990;1:233–239. doi: 10.1002/gcc.2870010308. [DOI] [PubMed] [Google Scholar]
- 12.Nowicki MO, Falinski R, Koptyra M, Slupianek A, Stoklosa T, Gloc E, et al. BCR/ABL oncogenic kinase promotes unfaithful repair of the reactive oxygen species-dependent DNA double-strand breaks. Blood. 2004;104:3746–3753. doi: 10.1182/blood-2004-05-1941. [DOI] [PubMed] [Google Scholar]
- 13.Slupianek A, Nowicki MO, Koptyra M, Skorski T. BCR/ABL modifies the kinetics and fidelity of DNA double-strand breaks repair in hematopoietic cells. DNA Repair (Amst) 2006;5:243–250. doi: 10.1016/j.dnarep.2005.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brady N, Gaymes TJ, Cheung M, Mufti GJ, Rassool FV. Increased error-prone NHEJ activity in myeloid leukemias is associated with DNA damage at sites that recruit key nonhomologous end-joining proteins. Cancer Res. 2003;63:1798–1805. [PubMed] [Google Scholar]
- 15.Nieborowska-Skorska M, Stoklosa T, Datta M, Czechowska A, Rink L, Slupianek A, et al. ATR-Chk1 axis protects BCR/ABL leukemia cells from the lethal effect of DNA double-strand breaks. Cell Cycle. 2006;5:994–1000. doi: 10.4161/cc.5.9.2722. [DOI] [PubMed] [Google Scholar]
- 16.Gaymes TJ, Mufti GJ, Rassool FV. Myeloid leukemias have increased activity of the nonhomologous end-joining pathway and concomitant DNA misrepair that is dependent on the Ku70/86 heterodimer. Cancer Res. 2002;62:2791–2797. [PubMed] [Google Scholar]
- 17.Slupianek A, Schmutte C, Tombline G, Nieborowska-Skorska M, Hoser G, Nowicki MO, et al. BCR/ABL regulates mammalian RecA homologs, resulting in drug resistance. Mol Cell. 2001;8:795–806. doi: 10.1016/s1097-2765(01)00357-4. [DOI] [PubMed] [Google Scholar]
- 18.Jabbour E, Kantarjian HM, Abruzzo LV, O’Brien S, Garcia-Manero G, Verstovsek S, et al. Chromosomal abnormalities in Philadelphia chromosome negative metaphases appearing during imatinib mesylate therapy in patients with newly diagnosed chronic myeloid leukemia in chronic phase. Blood. 2007;110:2991–2995. doi: 10.1182/blood-2007-01-070045. [DOI] [PubMed] [Google Scholar]
- 19.Deininger MW, Cortes J, Paquette R, Park B, Hochhaus A, Baccarani M, et al. The prognosis for patients with chronic myeloid leukemia who have clonal cytogenetic abnormalities in philadelphia chromosome-negative cells. Cancer. 2007;110:1509–1519. doi: 10.1002/cncr.22936. [DOI] [PubMed] [Google Scholar]
- 20.Koptyra M, Falinski R, Nowicki MO, Stoklosa T, Majsterek I, Nieborowska-Skorska M, et al. BCR/ABL kinase induces self-mutagenesis via reactive oxygen species to encode imatinib resistance. Blood. 2006;108:319–327. doi: 10.1182/blood-2005-07-2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Libura J, Slater DJ, Felix CA, Richardson C. Therapy-related acute myeloid leukemia-like MLL rearrangements are induced by etoposide in primary human CD34+ cells and remain stable after clonal expansion. Blood. 2005;105:2124–2131. doi: 10.1182/blood-2004-07-2683. [DOI] [PubMed] [Google Scholar]
- 22.Neering SJ, Bushnell T, Sozer S, Ashton J, Rossi RM, Wang PY, et al. Leukemia stem cells in a genetically defined murine model of blast-crisis CML. Blood. 2007;110:2578–2585. doi: 10.1182/blood-2007-02-073031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deutsch E, Dugray A, Karim B, Marangoni E, Maggiorella L, Vaganay S, et al. BCR-ABL down-regulates the DNA repair protein DNA-PKcs. Blood. 2001;97:2084–2090. doi: 10.1182/blood.v97.7.2084. [DOI] [PubMed] [Google Scholar]
- 24.Richardson C, Stark JM, Ommundsen M, Jasin M. Rad51 overexpression promotes alternative double-strand break repair pathways and genome instability. Oncogene. 2004;23:546–553. doi: 10.1038/sj.onc.1207098. [DOI] [PubMed] [Google Scholar]
- 25.Peng Y, Zhang Q, Nagasawa H, Okayasu R, Liber HL, Bedford JS. Silencing expression of the catalytic subunit of DNA-dependent protein kinase by small interfering RNA sensitizes human cells for radiation-induced chromosome damage, cell killing, and mutation. Cancer Res. 2002;62:6400–6404. [PubMed] [Google Scholar]