Abstract
Background
Maintaining continuity of care (CoC) in the inpatient setting is dependent on aligning goals and tasks with the plan of care (POC) during multidisciplinary rounds (MDRs). A number of locally developed rounding tools exist, yet there is a lack of standard content and functional specifications for electronic tools to support MDRs within and across settings.
Objective
To identify content and functional requirements for an MDR tool to support CoC.
Materials and methods
We collected discrete clinical data elements (CDEs) discussed during rounds for 128 acute and critical care patients. To capture CDEs, we developed and validated an iPad-based observational tool based on informatics CoC standards. We observed 19 days of rounds and conducted eight group and individual interviews. Descriptive and bivariate statistics and network visualization were conducted to understand associations between CDEs discussed during rounds with a particular focus on the POC. Qualitative data were thematically analyzed. All analyses were triangulated.
Results
We identified the need for universal and configurable MDR tool views across settings and users and the provision of messaging capability. Eleven empirically derived universal CDEs were identified, including four POC CDEs: problems, plan, goals, and short-term concerns. Configurable POC CDEs were: rationale, tasks/‘to dos’, pending results and procedures, discharge planning, patient preferences, need for urgent review, prognosis, and advice/guidance.
Discussion
Some requirements differed between settings; yet, there was overlap between POC CDEs.
Conclusions
We recommend an initial list of 11 universal CDEs for continuity in MDRs across settings and 27 CDEs that can be configured to meet setting-specific needs.
Keywords: Multidisciplinary Rounds, Continuity of Care, Plan of Care, EHRs, Acute Care, Critical Care
Introduction
The delivery of patient-centered care in the acute and critical care setting is dependent on effective care planning that maintains continuity of care (CoC) by aligning intermediate (daily) goals and tasks with the plan of care during multidisciplinary rounds (MDRs).1 Currently, clinicians rely heavily on verbal communication, which may lead to information loss and points to a need for more effective tools to support information exchange and decision-making during rounds.2 Standardized and integrated documentation tools can increase the effectiveness of interdisciplinary communication of critical patient information and decision-making.3 Locally developed paper- and computer-based rounding tools exist in acute and critical care inpatient settings; yet, there remains a need to develop tools based on standard and empirically based content specifications to support MDR communication, documentation, care planning, and decision-making.2 A variety of mnemonics and acronyms have been published as standards to support inpatient CoC, particularly during handoff transitions, but a review of the literature indicated that these standards lack (1) specificity, (2) generalizability, or (3) both.4 There is a need for standard CoC content specifications in the inpatient setting, with universal concepts that can be applied across settings and specific concepts that can meet setting-specific needs. A CoC standard with universal and setting-specific concepts can be leveraged to support the formal, planned, and frequent communication events that are used to discuss and make decisions about patients’ care plans during rounds across a hospital's specialties’ settings.4 5 Therefore, the aim of this research was to determine specific content and related functional requirements for a standards-based MDR tool that is aligned with the plan of care to support CoC and decision-making during rounds.
Background and significance
Multidisciplinary care teams increase the effectiveness of team communication and coordination when they effectively leverage standard documentation to establish common ground related to patient care goals, tasks, roles, responsibilities, and other pertinent information; effective communication has been associated with decreased errors, increased efficiency, and decreased lengths of stay.5–13 In the hospital setting, verbal communication is most often used to establish common ground because of tradition, poor perceptions of electronic health record (EHR) information retrieval and information overload, and a lack of agreed-upon standards for inpatient transitions of care.2 13 Verbal communication, which is subject to information loss, is particularly concerning when relied upon for communication, care planning, and decision-making during MDRs.5 11 14–17 In response to these concerns, paper-based daily goals sheets have been implemented and shown to decrease both information loss and length of stay while increasing understanding of MDR goals.11 18 19 An electronic MDR tool populated with data from paper-based daily goals sheets could provide increased CoC function through broad information exchange and data reuse.15 20 Analysis of standards-based documentation tools for CoC in the inpatient setting is cited throughout the literature as a timely activity, but there is a lack of empirical evidence to direct the design and implementation of such tools.21 Our prior work extended the Continuity of Care Document (CCD), a standard for outpatient care transitions, to support CoC documentation by multidisciplinary care teams in the inpatient setting.4 This work resulted in the development of the Interdisciplinary Handoff Information Coding (IHIC) Framework, which, when combined with the CCD, captured clinical data elements (CDEs) critical for CoC in the inpatient setting.4 A total of 39 types of CDEs were identified from the combination of the CCD and IHIC Framework, and each of these CDEs has been mapped to the Health Level 7 Virtual Medical Record.22 Standardization of structure, format, and content of an electronic MDR tool would help to (1) minimize information overload, (2) increase interoperability of patient data, (3) facilitate the use of decision support tools, and (4) achieve the proposed stage 2 and 3 meaningful use quality measures, including effective care planning.23 24
Conceptual framework
This study is informed by the conceptual Model of EHR Interdisciplinary Information Exchange, which offers a proposed solution to improve the suboptimal processes of information and communication exchange within the EHR.25 This model includes a six-stage cyclical process of communicating and exchanging: (1) collaborative decisions; (2) explicit common goals; (3) safety double checks; (4) interventions; (5) assessments (eg, vital signs, laboratory values, clinical findings); and (6) evaluation of goals. These cyclical stages are based on the care planning process and support the development of: (1) EHR information tools that synthesize and summarize updates and events related to explicit goal generation, intervention, assessment, and evaluation; and (2) communication tools (eg, messaging tools) that allow clinicians to contextualize patient data and exchange domain-specific knowledge for collaborative decision-making and patient safety double checks 24 h a day. This model informed our conceptual approach to functional requirement specifications for CoC content by defining two functionalities that can be leveraged to support multidisciplinary CoC and clinical decision-making during rounds: (1) information tools to reuse, synthesize, and summarize clinical content across settings and clinician types; and (2) communication tools to send messages that contextualize data and share discipline-specific knowledge among the interdisciplinary members of the care team to provide a comprehensive story of the patient. In addition, the CDEs from the CCD and the IHIC Framework identified in our prior work informed our data collection and analysis approach for content specification of information and communication tools used during MDRs. Combined, the Model of EHR Interdisciplinary Information Exchange informed the conceptual aims and approach to data collection and analysis for functional specifications, while the CCD and IHIC categories informed the specific CDEs collected and analyzed for content specifications.
Objective
The study reported in this paper evaluated the feasibility and potential role of CoC standards to support specific content requirements and to identify related functional requirements for a standards-based MDR tool. There is a particular focus on plan of care content.
Materials and methods
We conducted a multi-methods study including quantitative and qualitative data collection and analysis related to MDRs in a cardiac intensive care unit (ICU) and a cardiac intermediate/acute care unit (ACU) in an academic medical center in Boston, Massachusetts, USA. The ICU is a 10-bed unit for critically ill non-surgical cardiac patients with a variable length of stay (1 day to multiple weeks) depending on severity of illness, required interventions, and recovery rate. The ACU is a 24-bed unit that cares primarily for patients before and after vascular procedures. Patients on the ACU have a short length of stay (1–3 days) and are discharged directly home or to a rehabilitation center typically 24 h after the procedure. All patient cases are discussed by members of the multidisciplinary care team during MDRs on both units. The length of these discussions varies widely between the ICU and ACU. MDRs in the ICU typically last 3–5 h and include a strong teaching component, focusing on discussing the patient’s diagnosis, current state, and interventions that comprise the plan. MDRs in the ACU are significantly shorter, lasting 15–30 min and are focused on the patient's plan for discharge. These two types of rounds were targeted to capture the continuity and variation of content and requirements between different types of MDRs in the hospital setting. Specifically, the selection of the two units provided (1) a common disease/condition focus of cardiac care and (2) distinct plan-of-care foci and patient trajectory (ie, stabilization from critical illness vs discharge home) between the units. Maintaining a similar disease-based focus between selected units allowed an increased ability to observe and understand the foci of rounds and varied plan-of-care concepts discussed between settings.
Our step-wise methodological process involved: (1) prior work leveraged to identify important CDEs discussed during inpatient transitions of care 4 14; (2) development and testing of the observational tool to collect CDEs discussed during rounds in real time for subsequent analysis; (3) quantitative data collection and analysis for empirically based content specification; (4) qualitative data collection and analysis for functional requirement specifications; and (5) triangulated data analysis of qualitative and quantitative findings to identify universal and configurable CDEs and their relation to functional requirements. Observations of ICU and ACU rounds for quantitative and qualitative data collection were conducted on weekdays between January and August 2012. This study was approved by the institutional review board at the academic medical center.
Prior work and development and testing of the observational tool
We developed a web-based observational tool to be used on an iPad—the Data Observation and Collection Tool (DOCT). The DOCT contains 38 of the 39 types of CDE developed in our prior work on the CCD and IHIC Framework.4 We combined two CDEs—‘plan’ and ‘discharge plan’—because, during our initial testing, we found that, while discussing a patient's plan, clinicians discussed these two data types as if they were one concept. More accurate data could be obtained by capturing these concepts under one data type named ‘plans’. Ten of the 38 CDEs related to the plan of care as defined in previous work4 (box 1).
Box 1. Clinical data elements (CDEs) related to plan of care.
Patient preferences
Need for urgent review
Prognosis
Rationale of primary team
Plan
Tasks/‘to dos’
Goals
Pending results and procedures
Advice and anticipatory guidance
Short-term concerns
The DOCT allowed the observer to select the clinical setting being observed, the clinicians present at rounds, and the data types discussed by the team per patient. Length of time discussing each patient was automatically recorded. All data recorded via the DOCT was saved directly to a database in discrete, structured fields to ensure consistent data capture and facilitate statistical analysis.
The DOCT was pilot tested and validated during 3 days of interobserver reliability testing by SC and SL, both nurses with clinical experience in cardiac and critical care. SC and SL observed the same patient rounds and independently recorded observed data on separate iPads. Each user's recording of observed data was compared by calculating Cohen's κ statistic for each type of CDE.26
Quantitative data collection and analysis
Quantitative data collection techniques were used to capture the types of discrete CDEs discussed during rounds. Specifically, the same observers who conducted the interobserver reliability testing observed rounds and recorded the types of CDEs discussed using the DOCT to obtain the quantitative data used in this study.
Descriptive statistics were computed, and bivariate statistical analyses were performed to detect associations between discrete CDEs discussed during rounds, clinicians present at rounds, and length of rounds. Specific tests of association performed using SPSS included: (1) χ2 (or Fisher's exact test when expected cell values <5); (2) Student's t test; and (3) analysis of variance. χ2 and Fisher's exact test were used to learn if two CDEs were statistically more or less likely to be discussed together for a patient during rounds. Student's t test (two-tailed, independent samples with Levene's test for equality of variances) was used to detect an association between (1) length of rounds and the types of clinicians present and (2) length of rounds and the type of CDE discussed. Analysis of variance (with fixed-effects model and testing to confirm homoscedasticity) was used to examine potential differences between the four attending physicians who led rounds and the length of those rounds. Aligned with the focus of this study on decision-making and plans of care, our analysis was particularly focused on the 10 CDEs related to the plan of care (box 1).
Network visualization was performed using NodeXL software to visually represent all statistically significant χ2 (or Fisher's exact test) associations between two CDEs discussed during rounds. NodeXL is an open-source template for Microsoft Excel that allows a user to view and explore network graphs. We used NodeXL to visualize associations between the two CDEs found to be significantly more likely to be discussed together at rounds rather than being discussed alone. Only statistically significant associations were imported for viewing in NodeXL. Consistent with the rationale for using visualization techniques to increase understanding, this approach allowed us to display all of the significant relationships detected by our χ2 and Fisher's exact test statistical analysis at one time. The network visualizations were generated using the Fruchterman–Reingold layout algorithm and Girvan–Newman cluster algorithm in NodeXL.
Qualitative data analysis
Two sources of qualitative data included (1) group and individual interviews and (2) unconstrained observations during MDRs, prior to using the iPad data collection tool. Clinicians who were key participants with diverse roles in MDRs were asked to participate in the interviews. Interviews focused on learning their information and decision-making needs in the context of MDRs for understanding the distinct and overlapping communication and documentation needs to maintain CoC during MDRs. Please see online supplementary appendix for the semistructured interview guide that was used. All interviews were audio recorded and transcribed. Nine MDRs were observed using ethnographic techniques with recorded field notes. These sessions were also used to iteratively develop and test the DOCT. Qualitative data were thematically analyzed using Nvivo qualitative analysis software for MDR tool requirements and triangulated with quantitative findings. All data analyses were vetted in small-group sessions by members of the research team.
Triangulated data analysis
Results from qualitative and quantitative data analysis were triangulated to identify universal and configurable CDEs and requirements for an MDR tool. Each CDE was ranked according to three criteria from our quantitative data analysis: (1) frequency discussed; (2) association with length of rounds; and (3) association with other CDEs. This ranking was triangulated with results from our qualitative data analysis of CDEs that were part of a critical functional requirement identified by clinicians.
Results
Data collection
A total of 19 days of observations of ICU and ACU morning rounds were conducted between January and August 2012. The sequence of observations with their purpose and number of days was: (1) 4 days of ethnographic data collection, requirements analysis, and iterative testing of the DOCT; (2) 2 days of training observers with the DOCT; (3) 3 days of interobserver reliability data collection; and (4) 10 days of quantitative data collection of discrete data using the DOCT. The final version of the DOCT can be accessed online at http://clinicalinformatics.partners.org/MDRT/DataCollect.asp. During the 10 days of quantitative data collection, 18 h of rounds were observed for 128 patients. Interobserver reliability was >0.60 (substantial agreement Cohen's κ) for all reported data.26
Five individual and three group interviews were conducted with clinicians who had participated in ICU and ACU rounds. Individual interviews were conducted with the nutritionist and the attending physician from the ICU and the attending physician, nurse manager, and physical therapist from the ACU. The first group interview was conducted with the cardiac access nurse, charge nurse, nurse manager, physical therapist, social worker, nurse educator, nutritionist, and staff nurse from the ACU. The second group interview was conducted with two staff nurses from the ICU. The third group interview was conducted with two resident physicians from the ICU. Participants had an average of 18 years of clinical experience (average 11 years of experience at the study site institution) with a range of 2–34 years of clinical experience. All of the participants, except one, self-rated their computer skills as average or above average, and all reported that they are comfortable conducting internet searches and using email.
Quantitative data findings: rounding content
We found significant associations between: (1) CDEs discussed; (2) clinicians present at rounds; and (3) length of rounds. Interestingly, presence of a particular type of clinician was associated with increased or decreased likelihood of discussing particular CDEs (see table 1 for statistically significant results). In the ACU, when the intern was present, the team was more likely to discuss tasks/‘to dos’ and the patient's demographic characteristics, problems, and plans, and less likely to discuss procedures, medications, results, and assistive equipment. When the student was present, the team was more likely to discuss problems and updates. When the cardiac access nurse was present, the team was more likely to discuss patient information and less likely to discuss information related to social supports (eg, family contact information). When the physical therapist was present, the team was more likely to discuss medications and less likely to discuss the patient's problems. In the ICU, when the charge nurse was present, the team was more likely to discuss the patient's anticoagulation status and was less likely to discuss the patient's hospital course.
Table 1.
Clinician presence at ICU rounds associated with discussion of clinical data elements
| Unit | Clinician | CDE | Association* | p Value |
|---|---|---|---|---|
| ICU | Charge nurse | Anticoagulation status | Positive | 0.03 |
| ICU | Charge nurse | Hospital course | Negative | 0.05† |
| ACU | Intern | Task and ‘to dos’ | Positive | 0.03 |
| ACU | Intern | Patient information | Positive | 0.01 |
| ACU | Intern | Problems | Positive | <0.0001 |
| ACU | Intern | Procedures | Negative | 0.01 |
| ACU | Intern | Medications | Negative | 0.01 |
| ACU | Intern | Results | Negative | 0.03† |
| ACU | Intern | Assistive equipment | Negative | <0.0001 |
| ACU | Intern | All plans | Positive | <0.0001 |
| ACU | Student | Problems | Positive | 0.03 |
| ACU | Student | Updates | Positive | <0.0001 |
| ACU | Nurse manager | Patient information | Positive | <0.0001 |
| ACU | Nurse manager | Payers | Negative | 0.05 |
| ACU | Cardiac access nurse | Patient information | Positive | <0.0001 |
| ACU | Cardiac access nurse | Supports | Negative | 0.02 |
| ACU | Physician's assist | Procedures | Positive | 0.05 |
| ACU | Physician's assist | Medications | Positive | 0.04 |
| ACU | Social worker | Advice guidance | Negative | 0.02 |
| ACU | Social worker | Goals | Negative | 0.02 |
| ACU | Social worker | Consultations | Positive | 0.05 |
| ACU | Physical therapist | Problems | Negative | 0.02 |
| ACU | Physical therapist | Medications | Positive | 0.02† |
| ACU | Care coordinator | Goals | Negative | 0.05 |
| ACU | Care coordinator | Patient information | Negative | 0.02 |
| ACU | Care coordinator | Procedures | Negative | 0.03 |
| ACU | Care coordinator | Assistive equipment | Negative | 0.02 |
All p values were calculated using Fisher's exact test for 2×2 contingency table because of an expected cell count <5, except where noted with † to indicate that χ2 analysis was performed because of adequate sample size.
*Positive association: more likely to be discussed when clinician present at rounds; negative association: less likely to be discussed when clinician present at rounds.
ACU, intermediate/acute care unit; CDE, clinical data element; ICU, intensive care unit.
Time spent discussing individual patients during ICU rounds was significantly longer than during ACU rounds (18.5 min/patient vs 0.37 min/patient, p<0.0001, t test statistic=−9.8, df=56.06). ICU patient discussions during MDRs lasted significantly longer when the staff nurse was present (22.84 min/patient vs 15.36 min/patient, p=0.01, t test statistic=−2.84, df=15.92) and varied in length depending on which attending physician was present (mean range 18.52 min/patient vs 14.1 min/patient, p=<0.0001, F statistic=6.67). For one attending physician, ICU rounds lasted significantly longer when specific types of data were included in the rounds discussion (see table 2 for mean time and statistical significance per CDE). On the ACU, rounds were significantly shorter when the cardiac access nurse was present (14.82 s/patient vs 28.73 s/patient, p<0.0001, t test statistic=2.86, df=48.25) and when the physical therapist was present (14.89 s/patient vs 24.69 s/patient, p=0.01, t test statistic=2.74, df=52.85).
Table 2.
Length of rounds per clinical data element (CDE) discussed
| CDE | Time (min/patient) if CDE was not discussed | Time (min/patient) if CDE was discussed | Mean difference | p Value | t Test statistic | Degrees of freedom |
|---|---|---|---|---|---|---|
| Rationale | 9.41 | 23.82 | 14.41 | <0.0001 | −4.31 | 55 |
| Advice guidance | 13.12 | 23.71 | 10.59 | <0.0001 | −3.07 | 55 |
| Short-term concerns | 13.85 | 24.47 | 10.62 | <0.0001 | −3.05 | 55 |
| Goals | 13.79 | 23.75 | 9.96 | 0.01 | −2.85 | 55 |
| Problems | 12.35 | 25.35 | 13 | <0.0001 | −3.94 | 55 |
| Updates | 2.51 | 22.78 | 20.27 | <0.0001 | −9.31 | 53.46 |
| Functional status | 1.34 | 21.31 | 19.97 | <0.0001 | −10.47 | 51.9 |
| Social history | 15.72 | 25.67 | 9.95 | 0.01 | −2.53 | 55 |
| Procedures | 12.21 | 25.50 | 13.29 | <0.0001 | −4.05 | 55 |
| Medications | 0.87 | 19.84 | 18.97 | <0.0001 | −9.81 | 54.71 |
| Results | 1.34 | 21.31 | 19.97 | <0.0001 | −10.47 | 51.9 |
| Fluid balance | 7.40 | 21.17 | 13.77 | <0.0001 | −3.16 | 55 |
| Prophylaxis | 9.93 | 25.67 | 15.74 | <0.0001 | −4.38 | 55 |
| Advanced directive | 15.14 | 23.14 | 8 | 0.03 | −2.21 | 55 |
| Past history | 11.22 | 23.09 | 11.87 | <0.0001 | −3.41 | 55 |
| Hospital course | 13.65 | 22.30 | 8.65 | 0.02 | −2.42 | 55 |
| Alerts | 15.49 | 31.13 | 15.64 | <0.0001 | −3.69 | 55 |
| Vital signs | 1.28 | 22.17 | 20.89 | <0.0001 | −11.21 | 48.37 |
| Admission information | 14.41 | 24.57 | 10.16 | 0.01 | −2.87 | 55 |
| Plans | 4.50 | 20.47 | 15.97 | <0.0001 | −3.03 | 55 |
| Orders | 10.95 | 26.69 | 15.74 | <0.0001 | −3.31 | 28 |
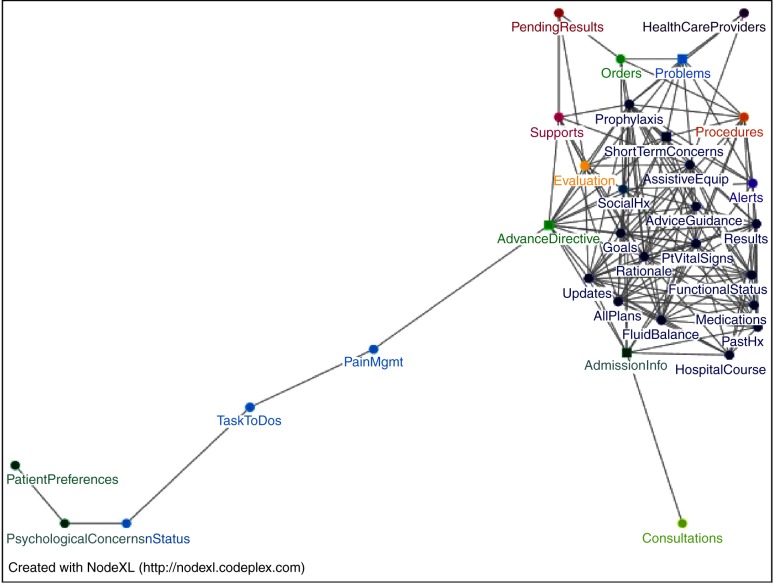
Figure 1 is a network visualization of CDEs discussed during ICU rounds that were significantly more likely to be discussed together. The nodes in the network are each CDE. Each edge connects two CDEs and indicates that, if one of those CDEs was discussed during rounds, the other was significantly more likely to be discussed also. Only CDEs that were significantly more likely to be discussed when other CDEs were also discussed (indicated by significant χ2 or Fisher's exact test) are displayed in the network. The large cluster in figure 1 demonstrates the high degree of connectedness among many of the CDEs discussed during ICU rounds. Conversely, the CDEs on the bottom left side of the figure are more likely to be discussed together, but are not highly connected to other types of CDE.
Figure 1.
Network visualization of data elements discussed together during intensive care unit rounds. Hx, history; Mgmt, management; Pt, patient.
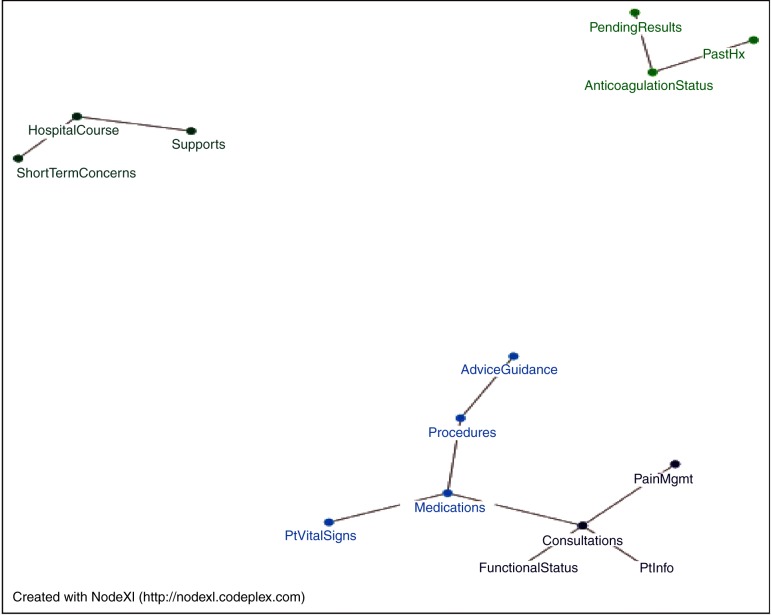
Figure 2 is a network visualization for the significant associations between CDEs discussed during ACU rounds. The three separate clusters in figure 2 indicate CDEs that are discussed together during ACU rounds. In the ACU, a patient's plan was less likely to be discussed if the patient's pending results (Fisher's exact test, p value=0.01), procedures (Fisher's exact test, p value <0.0001), or anticoagulation status (Fisher's exact test, p value <0.0001) were discussed.
Figure 2.
Network visualization of data elements discussed together during intermediate/acute care unit rounds. Hx, history; Mgmt, management; Pt, patient.
Qualitative data findings: rounding functions
Two themes emerged from our qualitative data analysis: (1) enabling remote communication functionality through mobile devices; and (2) building shared and configurable views.
Remote communication for updates, goals, and patient preferences
Remote communication through mobile devices should allow: (1) messaging by consulting clinicians who are not physically present on the unit to ensure issues they believe to be important are discussed during rounds; (2) messaging by nurses that need to alert the team to a serious abnormal clinical finding for a patient who is not currently being discussed during rounds; (3) viewing a rounding schedule to facilitate clinician presence at rounds; and (4) viewing updates throughout the day and after rounds. An example of a message by a consulting clinician is a nutritionist reminding the team that an ICU patient who has had ‘nothing by mouth’ is malnourished and needs to start a diet regimen. Messages by nurses in the ICU are essential because rounds typically last many hours, and, during this time, communication about urgent issues is frequently necessary, but is often performed through verbal interruptions.27 Interruptions should be minimized during rounds. Building an infrastructure to enable urgent messaging to a designated individual, while queuing less urgent messages that can be dealt with after rounds, may help clinicians balance their responsibilities to all patients while focusing on the rounds discussion. For example, such an infrastructure could enable a nurse to send a message that a patient's electrolytes are abnormally low and an immediate intervention is required that must be ordered by a physician. An urgent message placed to a designated physician during rounds may enable efficient execution of the order and intervention instead of waiting many hours for the ICU team to complete their rounds on all patients and attend to outstanding order requests—or interrupt the entire team's discussion. A rounding schedule was requested to assist consulting clinicians working on another unit, and clinicians caring for patients on the same unit, to anticipate and organize their time to ensure that they can be present at rounds for a specific patient. This request was consistent with our observation that clinicians volunteered patient data beyond the data expected to be discussed by the rounding team based on patient-specific states and needs. To be present at a round to volunteer specific patient data, the clinician needs to be able to anticipate when rounds will occur for that patient.
The ICU team filled out a separate paper-based daily goals sheet for each patient. This sheet was placed on the wall of each patient's room—but not integrated into other aspects of the patient record. The sheet was filled out during rounds by the resident, but, during our observations of rounds, we observed that the resident routinely filled it out, but that it was not discussed among the team. When asked specifically about the daily goals sheet during interviews, the clinicians cited that is was useful as a reference to the goals of care for the day if a clinician was not able to be present at rounds. However, because the daily goals sheet was not integrated into the record and could not be accessed electronically, it was not updated throughout the day, limiting its usefulness.
During interviews, the nurses emphasized the importance of incorporating patient preferences when formulating daily goals. The ICU is a challenging environment in which to include patient preferences because many patients are sedated. The nurses noted that, when the family is present at the bedside and can participate in rounds, the patient's preferences are made known and are readily incorporated as a critical factor in the decision-making process. However, family members are often unable to be present during rounds because of their own personal and professional responsibilities during the workday. The incorporation of patient preferences from previous discussions with family members to the rounds discussion is critical and would benefit from a formal method of documentation and communication. In fact, the nurses stated that the patient's daily goal may be to talk to the family and confirm the patient's preferences. One nurse discussed a patient case as an exemplar of the importance of incorporating patient preferences: “So [doing a procedure to place] an [inferior vena cava] umbrella [to prevent blood clots] would probably be the only thing we could do for her. But why aren't we sending her right down for an umbrella [procedure]? Because we want to talk to her brother, who is her healthcare proxy to see if this is something they would like. Or would they prefer to go home and should we get hospice?… The goals of today will be to talk to family and decide what is best for her.” Inclusion of daily goals and patient preferences in a shared electronic MDR tool that could be updated frequently was perceived as potentially useful for clinicians who could not be present at rounds or to communicate changes made during rounds.
Shared views complemented by role-based configurable views
In the ICU and ACU, rounds were highly structured, with specific clinician roles of being responsible for reciting data from the patient record to facilitate the care team in establishing common ground about the patient's history and current state. In the ICU, the resident was responsible for reciting current patient data and history to the care team, and the pharmacist was responsible for reciting the medication list. In the ACU, the physician's assistant and intern were responsible for reciting all current patient data and history to the care team. These verbal recitations among the team based on data from the record indicate that shared views are critical for an MDR tool. Patient data and tasks/‘to dos’ discussed during rounds should be displayed on a large electronic white board view to convey temporal associations of data, particularly in the ICU. Outcomes of the rounds discussion should be available on a shared view that can be accessed remotely, especially the patient's plan, problems, and short-term concerns. Configurable views should facilitate the specialized foci and attention of each clinician type during rounds. For example, in the ICU, the pharmacist was expected to (1) recite detailed medication information to the group, and (2) actively recognize any conflicting medication information or information loss by comparing past and current medication lists. Therefore, these medication details should be included on the pharmacists ‘home-page view’, but, perhaps, could be on a secondary view for other types of clinician. Each clinical setting should be able to configure the types and order of the CDEs that should be prominently displayed on the home screen as well to enable efficient information retrieval and documentation during rounds.
Triangulated data findings: content and functional specifications for MDR tools
Triangulation of our quantitative and qualitative multi-methodology analyses resulted in 11 universal CDEs that should be shared in MDR tools across settings and 27 configurable CDEs that may be used to meet setting-specific needs. Table 3 includes the universal CDEs and table 4 includes the configurable CDEs. These tables were determined by ranking each CDE according to four criteria from our triangulated data analysis: (1) the frequency with which it was discussed; (2) if the length of rounds increased when that CDE was discussed; (3) if the CDE was significantly associated with the discussion of any other type of CDE; and (4) if the CDE was part of a critical functional requirement from our qualitative data analysis. These criteria are indicated in the keys at the bottom of tables 3 and 4. Additionally, based on our qualitative data, we distinguished the CDEs that should have a messaging functionality within an MDR tool.
Table 3.
Universal clinical data elements (CDEs) discussed at multidisciplinary rounds
| Frequency discussed | ||
|---|---|---|
| Universal CDEs | ICU | ACU |
| Plans | 87.72%*†‡ | 91.43%*‡ |
| Patient-identifying information | 98.25% | 88.57%†‡ |
| Consultations | 59.65%†‡§ | 32.86%†‡§ |
| Results | 85.96%*†‡ | 18.57%* |
| Problems | 47.37%*†‡ | 17.14%‡ |
| Medications | 92.98%*†‡ | 15.71%† |
| Procedures | 47.37%*† | 14.29%†‡ |
| Short-term concerns§ | 43.86%*†‡ | 4.29%*†‡ |
| Past medical/surgical history | 61.4%*† | 2.86%*†‡ |
| Goals | 47.37%*†‡ | 4.29%‡ |
| Admission demographics | 0.00% | 0.00%‡ |
*Increased length of rounds.
†Significant association among data discussed.
‡Qualitative analysis requirement.
§Messaging functionality.
ACU, intermediate/acute care unit; ICU, intensive care unit.
Table 4.
Configurable clinical data elements (CDEs) discussed at acute and critical care rounds
| Menu set CDEs | Frequency discussed | Configurable recommendation | |
|---|---|---|---|
| ICU | ACU | ||
| Functional status | 85.96%*†‡ | 7.14%†‡ | ICU and ACU |
| Patient vital signs | 82.46%*†‡ | 8.57%† | ICU and ACU |
| Fluid balance | 80.7%*† | 1.43% | ICU and ACU |
| Updates | 78.95%*†‡ | 5.71%‡§ | ICU and ACU |
| Rationale | 63.16%*†‡ | 0.00% | ICU |
| Hospital course | 56.14%*† | 8.57%† | ICU and ACU |
| Assistive equipment | 52.63%† | 8.57% | ICU and ACU |
| Advice guidance | 50.88%*†‡§ | 4.29%†‡§ | ICU and ACU |
| Prophylaxis | 49.12%*†‡ | 0.00% | ICU |
| Pending results | 43.86%† | 8.57%† | ICU and ACU |
| Advance directive | 42.11%*†‡ | 0.00% | ICU |
| Admission information | 40.35%*† | 1.43% | ICU and ACU |
| Supports | 35.09%†‡ | 8.57%†‡ | ICU and ACU |
| Social history | 28.07%*†‡ | 7.14%‡ | ICU and ACU |
| Tasks/‘to dos’ | 22.81%†‡ | 8.57%‡ | ICU and ACU |
| Evaluation | 21.05%† | 0.00% | ICU |
| Anticoagulation status | 19.30%† | 5.71%† | ICU and ACU |
| Alerts | 19.3%*† | 0.00% | ICU |
| Orders | 17.54%† | 0.00% | ICU |
| Pain management | 15.79%† | 10.00%† | ICU and ACU |
| Psychosocial concerns | 12.28%† | 4.29%* | ICU and ACU |
| Healthcare providers | 10.53%† | 0.00% | ICU |
| Patient preferences | 5.26%†‡ | 2.86% | ICU and ACU |
| Prognosis | 3.51% | 0.00% | ICU |
| Payers | 0.00% | 4.29% | ACU |
| Patient education | 0.00% | 0.00% | Unknown |
| Need for urgent review | 0.00%ठ| 0.00% | ICU |
*Increased length of rounds.
†Significant association among data discussed.
‡Qualitative analysis requirement.
§Messaging functionality.
ACU, intermediate/acute care unit; ICU, intensive care unit.
Specifically related to plan-of-care CDEs, a universal shared view should include the patient's problems, plan, goals, and short-term concerns. Configurable plan-of-care content should include rationale, tasks/‘to dos’, pending results and procedures, patient preferences, need for urgent review, prognosis, and advice and anticipatory guidance. Tailored messaging functionality should enable clinicians to communicate before, during, and after rounds specifically about short-term concerns, advice and anticipatory guidance, need for urgent review, updates, and notification of new consultations.
Discussion
Three specific findings from our data are critically relevant to requirements for development of an MDR tool: (1) the focus of the rounds discussion is influenced by the clinicians present; (2) the discussion of specific types of data influence length of rounds; and (3) there is probably a universal set of empirically derived CDEs discussed during rounds. Our findings confirm our conceptual framework through our identified requirements that an MDR tool should include information tools to convey universal and configurable sets of CDEs and communication tools to facilitate messaging with members of the care team who cannot be present at rounds. In addition, the conceptual framework's six cyclical stages of the care planning process (collaborative decisions, explicit common goals, safety double checks, interventions, assessments, and evaluation of goals) may be a useful framework for organizing CDEs on an MDR tool's shared and configurable views.
Clinician presence and the focus of rounds
The first finding—that the focus of the rounds discussion is influenced by the clinicians present—is important because it provides empirical evidence that the multidisciplinary nature of rounds enriches the discussion and may influence the establishment of common ground among members of the care team. The intent of our analysis is not to interpret the relative importance of specific clinicians or CDEs or to demonstrate causality, as that cannot be demonstrated with the methods used. Our findings provide a starting point to begin to think about what these associations might mean, such as how and why the charge nurse presence is positively correlated with the CDE of anticoagulation status. For example, one duty of the charge nurse is to know the clinical state of each patient on the ICU in order to anticipate future transitions of care or therapeutic interventions that may require increased nurse staffing for subsequent shifts. Anticoagulation management is dependent on a patient's acuity (intravenous vs oral agents) and plan (before and after the procedure), which affects patient/nurse staffing ratios and readiness for discharge. Therefore, it is possible that the charge nurse attends rounds for patients who are known to be in a state of transition, and anticoagulation status is an indicator of patients in a state of transition. However, it is challenging and largely meaningless to interpret each association in isolation. Yet, in aggregate, our analysis demonstrates that a relationship exists between the clinicians who participate in rounds and the focus of the rounds discussion. This association is possibly linked to clinical duties and has implications for the focus of the plan of care, establishment of common ground, and care delivered for a patient. These findings are useful for informing the focus of future studies analyzing the contribution and significance of each clinician's role and duties in MDRs as a distributed and collaborative system of care.5 25 Likewise, we can leverage our network visualizations to help direct the focus of future research on closely connected associations or on CDEs that are not closely connected, but are viewed as clinically important to drive best practice.
A major theme that emerged from our qualitative data analysis was the functional requirement to enable remote messaging and information exchange for clinicians who cannot be physically present at rounds. Increased knowledge of the importance of each clinician’s contribution to rounds is needed to increase our conceptual understanding of the significance of MDRs and to inform the appropriate development and targeting of messaging tools for clinicians who cannot be physically present at rounds. This requirement from our qualitative findings was specifically to allow clinicians to send messages to remind the team of important issues to discuss during rounds, such as a nutritionist reminding the team that an ICU patient is malnourished and needs to start a diet regimen. Given our triangulation of findings, indicating clinician presence as an important variable, it is important to (1) design tools that facilitate remote communication from members of the care team for patient-tailored messages and reminders and (2) continue to further investigate the relationships between clinicians’ roles, participation in rounds, plan-of-care foci, and impact on patient outcomes.
The finding that clinician presence is associated with discussion of particular CDEs supports the requirement from our qualitative data to design tools with configurable views to facilitate the specialized foci and attention of each clinician type during rounds. However, we posit that configurable views should facilitate, not distract, clinicians from collaborative rounding discussions to establish common ground. Prior work has demonstrated that rounds is a time to make sense of patient data (ie, sense making) through discussions to establish common ground and facilitate decision-making and planning.5 25 The recitation of patient data from the patient record may be a central component of collaborative sense-making. It is possible that the association between clinicians’ presence and data discussed are related to three phenomena that occur during rounds to promote sense-making and decision-making: (1) role-based responsibility to recite current and historical patient data; (2) clinicians’ volunteering of information based on dynamic patient changes and needs; and (3) clinicians’ duty-based selective attendance at rounds for specific types of patient who are more likely to have specific types of data discussed.
Type of data discussed and length of rounds
The second finding— discussion of specific types of data influences the length of rounds—supports the notion that rounds are a time of significant information needs and/or exchange and discussion of patient data. The significantly increased length of time, on average, ranged from 8 to almost 21 min, depending on the type of CDE. This simple test of association does not account for other variables that may have influenced the increased length of time, but it does associate the length of the discussion with specific types of content in the discussion. Triangulated with our qualitative data analysis, this association may be a result of unmet information needs, teaching items, or collaborative team decision-making discussions for particular types of clinical content, such as the patient's current clinical state and plan of care.
There may be a number of important implications to consider if further work confirms that increased time of rounds is a result of unmet information needs. First, an interesting notion is that deciding whether or not to engage in information-seeking forces an upfront evaluation of the potential value of the data sought compared with the cost of seeking it. This may contribute to clinicians’ active sense-making of information needs and patient data, which may affect decision-making and planning. However, the potential benefit of increased sense-making through the act of information-seeking must be balanced with the cost of decisions based on imperfect information (if information is not sought) and time spent searching for information. Prior work has demonstrated that, when clinicians perceive that the process of extracting information from the EHR has a high time cost, they are more likely to verbally ask other clinicians for patient information.2 These actions have a number of implications: (1) increased interruptions; (2) increased cost to other clinicians’ time; and (3) increased perceptions that EHR data are out of date, leading to a lack of personal motivation to document patient data in real time.2 15 Therefore, the CDEs associated with an increased length of rounds shown in table 2 are probably important for inclusion in an MDR tool to meet information needs, support teaching, and capture decisions made for the plan of care.
It is important to emphasize that the CDEs collected for content specifications in this study were in the form of ‘data types’, which are generic categories of types of data that allow comparisons across patients. For example, some of the data types were ‘plans’, ‘vital signs’, and ‘functional status’. Based on our triangulated analysis of content specifications and functional requirements during rounds, we propose that rounding tools utilize multiple configurable views of data types: (1) home screens that include frequently accessed data types to meet known information needs during rounds; and (2) secondary screens that include potentially relevant, although less frequently sought, data types. This suggestion is aligned with our recommendation for configurable views based on the type of clinician and setting using the tool. Our findings indicate that the type of data discussed during rounds may be categorized into three layers to inform the development of universal and configurable views: (1) a set of universal data types that are predictably discussed across settings, users, and patients (table 3); (2) a set of configurable data types that may be predicted for specific settings, users, or patient types (table 4); (3) a set of configurable data types that may be needed on an inconsistent basis across settings, users, and patient types (table 4). Of note, our findings also indicate that some of these data types require messaging capabilities.
Universal set of CDEs discussed at rounds
We propose a set of 11 empirically derived CDEs as an initial version of a universal set of CDEs to be included in an MDR tool. Our findings indicate that significant associations among CDEs are different between acute and critical care rounds; yet, there was overlap between some plan-of-care data types discussed during rounds in the ACU and the ICU. Problems, plan, goals, and short-term concerns were important ‘universal plan-of-care’ CDEs because they were discussed significantly in both the ACU and the ICU. Rationale, tasks/‘to dos,’ pending results and procedures, discharge planning, patient preferences, need for urgent review, prognosis, and advice and guidance were important ‘configurable plan-of-care’ CDEs in the ICU and the ACU because they were discussed significantly in one of these settings. Future work should determine which configurable CDEs are used consistently versus inconsistently in specific settings, users, or patient types. This is also a potentially significant area of research for the development of documentation tools that are part of a learning health system, which is defined by the Institute of Medicine as a system that drives the process of best practice discovery as a natural outgrowth of patient care.28
It is important to note that these universal and configurable CDEs are based on empirical data on what was discussed during rounds across settings and not what ideally should be discussed during rounds to enhance care within and across settings. We especially point out that patient preferences were discussed at a low rate in both settings and that the network visualization was particularly useful for displaying and communicating this finding. However, our qualitative data findings indicate that inclusion of this CDE in an MDR tool may facilitate discussion of patient preferences and the recording of past discussions with the patient and family, which is, perhaps, a desired effect for the delivery of patient-centered CoC. The network visualization was particularly useful during our triangulation of data to highlight CDEs that clinicians stated were important during our qualitative interviews, but were not discussed with high frequency or highly connected with other types of data during rounds. Further work should evaluate the impact of inclusion of specific CDEs on the delivery of care by leveraging similar triangulated data collection and analyses.
This research is a significant contribution because it (1) developed and validated an observational data collection tool, the DOCT, to capture discrete CDEs based on CoC standards, (2) provides foundational content and functional requirements for the development of a documentation tool for use by multiple clinical disciplines to facilitate plan-of-care decision-making, and (3) provides empirical data evaluating existing CoC standards for use in the inpatient setting to enhance the capability of these standards to meet shared content requirements across care settings. Finally, this is the second study to confirm the relevance of the IHIC Framework as an extension of CoC standards for the inpatient setting.4 14 Prior work confirmed the framework in a cardiac ICU in a large academic medical center in New York City based on multidisciplinary handoff transitions.14 In this study, on the basis of qualitative and quantitative data examining MDRs, we corroborated the IHIC Framework in a cardiac ICU and cardiac ACU in an independent large academic medical center in Boston.
Limitations
As noted above, the quantitative findings in this study were based on our observations of what was discussed during rounds and are not an evaluation of what should be discussed during rounds for effective patient care. However, our methods included a qualitative analysis of clinicians’ perceptions of rounds for effective decision-making and CoC. Further work should evaluate our findings in the context of their impact on patient care. Second, this study took place in two clinical units in one academic medical center, and further research is needed to test the generalizability of our findings. However, as mentioned above, this study is an extension of prior work in other settings and confirmed the generalizability of the IHIC Framework. Finally, the validation and use of the DOCT was by nurse researchers who are experienced clinicians and therefore familiar with the clinical environment, including its nuances, language, and conventions. Further research is needed to test the interobserver reliability of the tool when used by researchers who are not experienced clinicians.
Conclusion
This study evaluated the content and functional requirements for an MDR tool and established that CoC CDEs based on current standards were discussed at rounds, have significant associations, and can be used as empirical data to inform tool design. On the basis of our multi-method analysis, we defined an initial set of universal and configurable CDEs for an MDR tool. We recommend an extension of CoC standards for the inpatient setting based on CDEs from the IHIC Framework.
Recommendations for the development of an MDR tool include the development of shared universal views across settings, configurable views that are setting- and clinician-specific, and mobile messaging functionality to communicate short-term concerns, advice and guidance, need for urgent review, updates, and notification of new consultations. Future work should further specify data entry and data view requirements for each type of CDE, explore the impact of clinician presence at rounds and information needs on plan of care and decision-making, validate our observational tool for requirements analysis in other settings, and develop and test an MDR tool based on our findings.
Supplementary Material
Acknowledgments
The authors acknowledge funding support from, and the participation of, the clinical leadership and staff from the study units.
Footnotes
Contributors: SC led the conception and design of the study with contributions from ACH, PCD, AB, and FYC. SC, ACH, PCD, FYC, ARI, AB, and SL contributed to acquisition, analysis and interpretation of data. SC, ACH, PCD, FYC, ARI, AB, and SL contributed to the drafting and critical revisions of the manuscript for important intellectual content and to the final approval of the version to be published.
Funding: This work was supported by the Partners-Siemens Research Council grant number 2011A053050.
Competing interests: None.
Ethics approval: Partners Healthcare Systems.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: We have all raw and aggregate deidentified data and analysis that can be shared if requested.
References
- 1.Dykes PC, Dadamio RR, Goldsmith D, et al. Leveraging standards to support patient-centric interdisciplinary plans of care. AMIA Annu Symp Proc 2011;2011:356–63 [PMC free article] [PubMed] [Google Scholar]
- 2.Collins S, Bakken S, Vawdrey D, et al. Discuss now, document Later : CIS/CPOE Perceived to be a “Shift Behind” in the ICU. Stud Health Technol Inform 2010;160:178–82 [PMC free article] [PubMed] [Google Scholar]
- 3.Keenan G, Yakel E. Promoting safe nursing care by bringing visibility to the disciplinary aspects of interdisciplinary care. AMIA Annu Symp Proc 2005;2005:385–9 [PMC free article] [PubMed] [Google Scholar]
- 4.Collins S, Stein DM, Vawdrey DK, et al. Content overlap in nurse and physician handoff artifacts and the potential role of electronic health records: a systematic review. J Biomed Inform 2011;44:704–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins S, Bakken S, Vawdrey DK, et al. Agreement between common goals discussed and documented in the ICU. J Am Med Inform Assoc 2011;18:45–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fagin CM. Collaboration between nurses and physicians: no longer a choice. Acad Med 1992;67:295–303 [DOI] [PubMed] [Google Scholar]
- 7.Larson E. The impact of physician-nurse interaction on patient care. Holist Nurs Pract 1999;13:38–46 [DOI] [PubMed] [Google Scholar]
- 8.Sexton JB, Thomas EJ, Helmreich RL. Error, stress, and teamwork in medicine and aviation: cross sectional surveys. BMJ 2000;320:745–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zwarenstein M, Reeves S. Working together but apart: barriers and routes to nurse—physician collaboration. Jt Comm J Qual Improv 2002;28:242–7, 209 [DOI] [PubMed] [Google Scholar]
- 10.Jain M, Miller L, Belt D, et al. Decline in ICU adverse events, nosocomial infections and cost through a quality improvement initiative focusing on teamwork and culture change. Qual Saf Health Care 2006;15:235–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pronovost P, Berenholtz S, Dorman T, et al. Improving communication in the ICU using daily goals. J Crit Care 2003;18:71–5 [DOI] [PubMed] [Google Scholar]
- 12.Pronovost P, Wu A, Sexton J. Acute decompensation after removing a central line: practical approaches to increasing safety in the intensive care unit. Ann Intern Med 2004;140:1025–33 [DOI] [PubMed] [Google Scholar]
- 13.Reader TW, Flin R, Mearns K, et al. Developing a team performance framework for the intensive care unit. Crit Care Med 2009;37:1787–93 [DOI] [PubMed] [Google Scholar]
- 14.Collins S, Mamykina L, Jordan D, et al. In Search of Common Ground in Handoff Documentation in an Intensive Care Unit. J Biomed Inform 2012;45:307–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coiera E. When conversation is better than computation. J Am Med Inform Assoc 2000;7:277–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller A, Scheinkestel C, Hospital A, et al. Uni- and Interdisciplinary Effects on Round and Handover Content in Intensive Care Units. Hum Factors 2009;51:339–53 [DOI] [PubMed] [Google Scholar]
- 17.Mador RL, Shaw NT. The impact of a Critical Care Information System (CCIS) on time spent charting and in direct patient care by staff in the ICU: a review of the literature. Int J Med Inform 2009;78:435–45 [DOI] [PubMed] [Google Scholar]
- 18.Phipps LM, Thomas NJ. The use of a daily goals sheet to improve communication in the paediatric intensive care unit. Intensive Crit Care Nurs 2007;23:264–71 [DOI] [PubMed] [Google Scholar]
- 19.Narasimhan M, Eisen LA, Mahoney CD, et al. Improving nurse-physician communication and satisfaction in the intensive care unit with a daily goals worksheet. Am J Crit Care 2006;15:217–22 [PubMed] [Google Scholar]
- 20.Hutchins E. Cognition in the Wild. Cambridge, MA: The MIT Press, 1995 [Google Scholar]
- 21.Fung KW, McDonald C, Srinivasan S. The UMLS-CORE project: a study of the problem list terminologies used in large healthcare institutions. J Am Med Inform Assoc 2010;17:675–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Illa A, Dykes P, Hurley A, et al. Mapping HL7 vMR to CCD and Hospital Handoff Codes. AMIA Annu Symp Proc 2012;2012:1786 [Google Scholar]
- 23.Centers for Medicare & Medicaid Services. Quality Measures. CMS.gov. 2012. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityMeasures/index.html?redirect=/QualityMeasures/03_ElectronicSpecifications.asp
- 24.Benson S. Meaningful use and clinical documentation. J AHIMA 2011;82:36–7 [PubMed] [Google Scholar]
- 25.Collins S, Bakken S, Vawdrey DK, et al. Model development for EHR interdisciplinary information exchange of ICU common goals. Int J Med Inform 2011;80:e141–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Viera A, Garrett J. Understanding interobserver agreement: the kappa statistic. Fam Med 2005;37:360–3 [PubMed] [Google Scholar]
- 27.Collins S, Currie L, Bakken S, et al. Interruptions during the use of a CPOE system for MICU rounds. AMIA Annu Symp Proc 2006;2006:895. [PMC free article] [PubMed] [Google Scholar]
- 28.Institute of Medicine (IOM). Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: The National Academies Press, 2013 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.