Abstract
The aging process is associated with gradual and progressive loss of muscle mass along with lowered strength and physical endurance. This condition, sarcopenia, has been widely observed with aging in sedentary adults. Regular aerobic and resistance exercise programs have been shown to counteract most aspects of sarcopenia. In addition, good nutrition, especially adequate protein and energy intake, can help limit and treat age-related declines in muscle mass, strength, and functional abilities. Protein nutrition in combination with exercise is considered optimal for maintaining muscle function.
With the goal of providing recommendations for health care professionals to help older adults sustain muscle strength and function into older age, the European Society for Clinical Nutrition and Metabolism (ESPEN) hosted a Workshop on Protein Requirements in the Elderly, held in Dubrovnik on November 24 and 25, 2013. Based on the evidence presented and discussed, the following recommendations are made: (1) for healthy older people, the diet should provide at least 1.0 to 1.2 g protein/kg body weight/day (2) for older people who are malnourished or at risk of malnutrition because they have acute or chronic illness, the diet should provide 1.2 to 1.5 g protein/kg body weight/day, with even higher intake for individuals with severe illness or injury, and (3) daily physical activity or exercise (resistance training, aerobic exercise) should be undertaken by all older people, for as long as possible.
Keywords: aging, nutrition, protein, amino acids, exercise, sarcopenic obesity, kidney function
New insights in aging and declining muscle function
The natural aging process is associated with gradual and progressive loss of muscle mass, muscle strength, and endurance, i.e., a condition called sarcopenia.(1) Such changes have been considered inevitable consequences of aging. This concept has recently been challenged, as new study results suggest that mitochondrial dysfunction, reduced insulin sensitivity, and reduced physical endurance are related, at least in part, to physical inactivity and to increases in adiposity rather than to aging alone.(2) The study results show that regular exercise can help normalize some aspects of age-related mitochondrial dysfunction, in turn improving muscle function.(2) Good nutrition, especially adequate protein intake, also helps limit and treat age-related declines in muscle mass, strength, and functional abilities. Nutrition in combination with exercise is considered optimal for maintaining muscle function.(3)
With the goal of discussing recent research findings in order to develop recommendations to help adults sustain muscle strength and function into older age, the European Society for Clinical Nutrition and Metabolism (ESPEN) hosted a Workshop with the ESPEN Expert Group, Protein Requirements in the Elderly, held in Dubrovnik, Croatia on November 24 and 25, 2013. This article reflects practical guidance resulting from the presentations and discussions during the workshop. The aim of the workshop was to provide practical guidance for health professionals who care for older adults, i.e., to recommend optimal protein intake and to advise age- and condition-appropriate exercise.
We offer practical guidance for maintaining muscle health and physical function with aging (Table 1). We provide our rationale and the supporting evidence for these recommendations in the sections following.
Table 1.
Practical guidance for optimal dietary protein intake and exercise for older adults above 65 years
| Recommendations |
|---|
| For healthy older adults, we recommend a diet that includes at least 1.0 to 1.2 g protein/kg body weight/day. |
| For certain older adults who have acute or chronic illnesses, 1.2 to 1.5 g protein/kg body weight/day may be indicated, with even higher intake for individuals with severe illness or injury. |
| We recommend daily physical activity for all older adults, as long as activity is possible. We also suggest resistance training, when possible, as part of an overall fitness regimen. |
Changing protein intake and protein needs in older adults
Compared to younger adults, older adults usually eat less, including less protein.(4, 5) In Europe, up to 10% of community-dwelling older adults and 35% of those in institutional care fail to eat enough food to meet the estimated average requirement (EAR) for daily protein intake (0.7 g/kg body weight/day), a minimum intake level to maintain muscle integrity in adults of all ages.(6) At the same time, many older adults need more dietary protein than do younger adults.(7, 8) An imbalance between protein supply and protein need can result in loss of skeletal muscle mass because of a chronic disruption in the balance between muscle protein synthesis and degradation.(9) As a result, older adults may lose muscle mass and strength and eventually experience physical disability.(10, 11)
In recent years, an ever-increasing body of evidence builds the case for increasing protein intake recommendations for older adults (Table 2).
Table 2.
Recent studies on protein intake and exercise in older adults
| Study report | Study design and key findings |
|---|---|
| Gray-Donald et al. 2014 (8) |
|
| Tang et al 2014 (89) |
|
| Beasley et al. 2013 (11) |
|
| Breen et al. 2013 (32) |
|
| Bartali et al. 2012(90) |
|
| Kim et al. 2012 (60) |
|
| Tieland et al. 2012 (91) |
|
| Yang et al. 2012 (36) |
|
Dietary protein intake
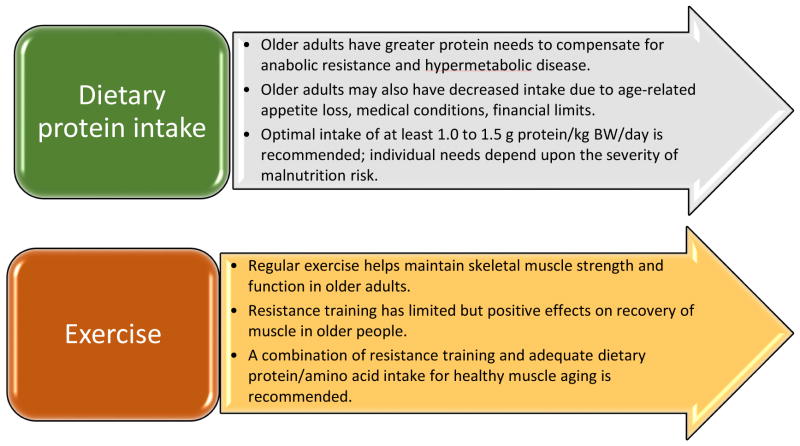
There are many reasons older adults fail to consume enough protein to meet needs—genetic predisposition to low appetite, physiological changes and medical conditions that lead to age- and disease-associated anorexia, physical and mental disabilities that limit shopping and food preparation, and food insecurity due to financial and social limitations (Figure 1).(5)
Figure 1.
Protein status: factors leading to lower protein intake in older persons
Dietary protein needs
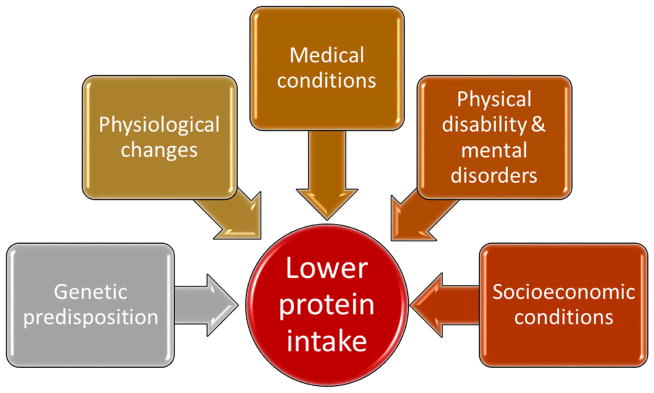
There are also many reasons older adults have higher protein needs (Figure 2). Physiologically, older adults may develop resistance to the positive effects of dietary protein on synthesis of protein, a phenomenon that limits muscle maintenance and accretion; this condition is termed anabolic resistance.(12, 13) Mechanisms underlying anabolic resistance and the resultant need for higher protein intake are: increased splanchnic sequestration of amino acids, decreased postprandial availability of amino acids, lower postprandial perfusion of muscle, decreased muscle uptake of dietary amino acids, reduced anabolic signaling for protein synthesis, and reduced digestive capacity.(7, 12, 14) Older adults likewise have higher protein needs to offset the elevated metabolism of inflammatory conditions such as heart failure, chronic obstructive pulmonary disease (COPD), or chronic kidney disease (CKD) undergoing dialysis. In healthy older adults and in a variety of disease, protein anabolism is related to net protein intake.(15) Most older adults will therefore benefit from higher protein intake.
Figure 2.
Protein status: factors leading to higher protein needs in older persons
Further, prolonged disuse of muscle, as with bed rest for illness or injury, leads to changes in protein synthesis and breakdown, which cause disuse atrophy of muscle. For example, bed rest for more than 10 days leads to a decline in basal and postprandial rates of muscle protein synthesis, especially in older adults.(16) Decreased muscle protein synthesis is the main mechanism for muscle loss, but there is also indirect evidence that an early and transient (1–5 days) increase in basal muscle protein breakdown may contribute to disuse atrophy.(16) While disuse due to acute illness or injury causes muscle atrophy, so too does physical inactivity due to sedentary lifestyle.(17)
In spite of many differences in general health status and physiology of old versus young adults, the recommended dietary allowance (RDA) has traditionally been set the same for healthy adults of all ages—0.8 g protein/kg body weight/day.(18) However, evidence continues to build in favor of increasing this recommendation for optimal protein intake to 1.0 to 1.2 g/kg body weight/day for adults older than 65 years.(5, 7, 19, 20)
Taken together, evidence shows that when usual dietary protein intake does not meet increased protein needs of older adults, negative nitrogen balance results and protein levels decline, especially skeletal muscle proteins.
Consequences of malnutrition and negative nitrogen balance
In older adults, age- or disease-related malnutrition leads to negative nitrogen balance and ultimately to frailty and primary or secondary sarcopenia.(1, 21) These conditions can result in disability, and eventually to loss of independence, falls and fractures, and death.(7) Primary (age-related) and secondary (disease-related) sarcopenia are difficult to distinguish in older adults because of the high prevalence of chronic disease in this population—92% after age 65 years, and 95% after age 80 years.(22) Frailty is defined as a biological syndrome with low reserve and low resistance to biomedical stressors; frailty results from cumulative declines across multiple biological systems, and worsening frailty is associated with disability.(23) Physical frailty and sarcopenia are closely linked.(24) While limited protein intake predicts incident frailty, it also predicts low bone mass.(25, 26) In fact, the presence of osteoporosis doubles risk for frailty.(27) Notably, frailty can be prevented or reversed by intervention, particularly by greater protein intake and exercise.(28, 29)
Physical activity and exercise can maintain or enhance muscle mass
Loss of muscle mass with aging is primarily due to decreased muscle protein synthesis rather than to increased muscle protein breakdown. While the basal level of post-absorptive myofibrillar protein synthesis may decline with age, this decline is minimal.(30) Inactivity with consequent anabolic resistance are major contributors to the development of sarcopenia.(30) This concept is supported by the observation that immobilization induces resistance of muscle to anabolic stimulation.(31) Similarly, reduction of step count for two weeks induces anabolic resistance in older adults, as shown by decreased response of muscle protein synthesis to protein ingestion, decreased insulin sensitivity, and lowered leg muscle mass.(32)
Aging muscle does respond to exercise, especially resistance exercise. In a classic study of nursing home residents older than 90 years, those who underwent 8 weeks of high-intensity resistance training experienced significant gains in muscle mass, strength, and walking speed.(33) A meta-analysis of studies on progressive resistance training in older adults showed clear benefits for improved physical function.(34) Resistance exercise may support these benefits by way of increased insulin sensitivity for (1) improved glucose utilization(35) and (2) enhanced myofibrillar protein synthesis.(36) Study results showed that resistance exercise was as effective in older adults as it was in young adults to reverse muscle loss and low muscle protein synthesis.(37) It was recently suggested that exercise-induced improvement in protein synthesis may be due to nutrient-stimulated vasodilation and nutrient delivery to muscle rather than to improved insulin signaling.(38)
In addition, the timing of protein ingestion relative to the exercise may be important for muscle mass accretion. In a study of younger adult men, the benefits of resistance exercise on protein synthesis persisted up to 24 hours post-exercise.(39) More research is needed to delineate mechanisms that link physical activity/nutrition to recovery of lost muscle protein in older adults.
Protein requirements without and with chronic diseases or conditions
Older adults are expected to benefit from increased dietary protein intake, especially those with anorexia and low protein intake along with higher needs due to inflammatory conditions such as heart failure, COPD, or CKD undergoing dialysis.(40) Further research is needed to identify and develop tools that can precisely define protein needs in older individuals with chronic conditions. Research is likewise needed to determine whether increased protein intake can measurably improve functional outcomes. The goal for future studies is to identify specific protein and amino acid needs for older adults, including those who are healthy and those with diseases common to aging.
Optimal protein or amino acid type and amount
A wide range of factors can affect the amount of dietary protein needed by an older person -digestibility and absorbability of protein in foods consumed, whether chewing capacity is normal or impaired, protein quality and amino acid content, sedentary lifestyle (including immobilization or inactivity due to medical condition), and presence of stress factors (inflammation and oxidative stress).
Amount of protein
Debate continues about whether a per-meal threshold amount of protein intake is needed to stimulate protein synthesis in older adults(41) or whether protein synthesis is linearly related to protein intake.(15) Either way, evidence suggests that older adults who consume more protein are able to maintain muscle mass and strength.(8, 10, 42, 43) Older adults who consumed 1.1 g protein/kg body weight/day lost less lean body mass (muscle) than did those who consumed only 0.7 to 0.9 g protein/kg body weight/day.(10) Among hospitalized older patients, at least 1.1 g protein/kg body weight/day was needed to achieve nitrogen balance, and safe intake was up to 1.6 g protein/kg body weight/day.(43)
Recent dietary recommendations for older adults are now including higher protein intake than for younger adults.(7, 44) The international PROT-AGE study group recommended 1.0–1.5 g protein/kg body weight/day for individuals older than 65 years(7) with or without disease, and the new Nordic Nutrition Recommendations suggest targeting 1.2–1.4 g protein/kg body weight/day with protein as 15–20% of total energy intake for healthy older adults.(44, 45)
Protein source, digestion, and absorption
Properties of the protein itself have the potential to affect digestion and absorption, e.g., whey, a milk protein, is considered a “fast” protein due to its quick release of amino acids, while casein, another milk protein, is a “slow” protein.(46, 47) In a study by Tang et al., ingestion of whey protein increased muscle protein synthesis more than casein.(48) However, it was shown that whey and casein resulted in equally increased protein synthesis when ingested after resistance exercise.(49) The difference between these studies is likely due to the form of casein used. Micellular casein, a form that leads to slower digestion, was used by (48), while calcium caseinate was used by (49).
From other perspectives, a person’s poor dentition can limit chewing capacity and protein availability (50), as can under- or over-cooking of protein foods.(51)
Protein intake pattern
While terminology used to describe patterns of protein intake varies, intake patterns in research studies were to “spread” protein evenly over 4 meals or to deliver protein mostly as a large “pulse” in a single meal. Results of several studies suggest that the pulse protein feeding pattern may be useful to improve feeding-induced stimulation of protein synthesis in older adults.(52–54) These results are seemingly contradictory to those suggesting that 4 doses of 20 gram of protein across 12 hours is the optimal pattern.(55) It is not clear whether the discrepancy between these studies is due to age differences, in inclusion of exercise, or most likely, the fact that 20 gram protein is not enough to maximally stimulate muscle protein synthesis in older adults. Further studies are needed to clarify optimal patterns of protein intake for older adults, and such studies must include protein synthesis as well as improvements in muscle strength and performance as outcome measures.
Specific amino acids and metabolites
Branched chain amino acids (BCAA), especially leucine, positively regulate signaling pathways for synthesis of muscle proteins.(56) A higher proportion of leucine was required for optimal stimulation of the rate of muscle protein synthesis in older adults, as compared to younger adults.(57) In adults who were critically ill, mixed BCAA likewise increased muscle protein synthesis.(58, 59) In a randomized, controlled study of exercise and nutrition in older sarcopenic adult women in the Japanese community, those who exercised and consumed supplemental amino acids rich in leucine showed increased leg muscle mass and strength, and faster walking speed.(60) Moreover, Borsheim et al. demonstrated that older adult who were given supplemental essential amino acids (EAA) for 16 weeks developed increased muscle mass and improved function, even in the absence of exercise interventions.(61) However, other study results showed that long-term leucine supplementation alone did not increase muscle mass or strength.(62, 63)
In addition, beta-hydroxy beta-methyl butyrate (β-HMB), an active metabolite of leucine, has been used by athletes to improve performance.(64) HMB ingestion increased muscle protein synthesis and reduced muscle protein breakdown in young adults in insulin-independent manner.(65) Further evidence shows that β-HMB may also help increase muscle mass and strength in older adults and in specific clinical populations (AIDS, cancer), and can help attenuate muscle loss in patients who are critically ill and require prolonged ICU care (ICU-acquired weakness).(66–68)
Sarcopenic obesity and protein intake
Sarcopenic obesity is a deficiency of skeletal muscle tissue mass relative to fat tissue (Table 3). Obesity and inactivity contribute to decreased muscle mass and to lower muscle quality, especially with aging.(69) Lower muscle quality is attributed in part to infiltration of fat into the muscle, which affects both muscle strength and muscle function.(70) Intramyocellular lipid accumulation also reduces synthesis of muscle proteins.(71)
Table 3.
Profile of sarcopenic obesity
| Feature | |
|---|---|
| Definition |
|
| Prevalence |
|
| Health consequences | |
| Clinical management |
|
Working definitions of sarcopenic obesity have been used in research studies, but there is not yet a universal definition for clinical practice.(72, 73) Sarcopenic obesity is under-diagnosed due to a lack of agreement on which body composition indices and cutoff points to use. A suitable definition should be based on a measure of fat mass along with a measure of skeletal muscle mass normalized for height (fat-free mass index, FFMI, or appendicular skeletal muscle mass index, SMI).(74) Age-specific reference values are more advantageous because FFMI or SMI may be misleading in adults of advanced age, in those with severe obesity, or in weight-reduced obese patients who have more connective tissue relative to lean mass. A simplified diagnosis of sarcopenic obesity can be based on a single image of muscle and adipose tissue of the thigh (magnetic resonance image or dual X-ray absorptiometry).(74) This method does have limitations; the ratio of skeletal muscle to fat tissue varies by sex and by body region in individuals with very high adiposity.(74)
In older adult men and women, low muscle mass and high fat infiltration into the muscle were associated with decreased strength and increased risk of losing mobility.(70) Similarly, low muscle mass correlated with low functionality.(70) The consequences of sarcopenic obesity are serious, including mobility limitations, lower quality of life, and risk of early death.(70, 75–77) Therefore, management of sarcopenic obesity aims primarily to sustain muscle strength and function and secondarily on weight loss with focus on losing fat but not muscle. Physical exercise is important in weight loss, as restriction of energy intake is otherwise likely to induce loss of skeletal muscle.(78) Taken together, the recommended strategy for management of sarcopenic obesity is a combination of moderate calorie restriction, increased protein intake, and exercise (endurance and resistance training).
Concerns about negative effects of higher protein intake in older adults
While the benefits of increased dietary protein are acknowledged for maintenance of muscle health in older adults, health professionals often express concern that high-protein diets will stress and worsen declining kidney function in this population. However, evidence shows that many healthy older adults have preserved kidney function.(79–81) On the other hand, those older adults who are unhealthy are more likely to develop mild kidney insufficiency or CKD. For such individuals with a short life expectancy, nutritional recommendations (such as restriction of dietary protein intake) should support quality of life in the short-term. Specifically, when making recommendations for protein intake, consider the balance between risk of disability/death and risk of developing end-stage renal disease.
Serum creatinine and creatinine clearance are poor markers of glomerular filtration rate (GFR) in older adults since these values are strongly determined by muscle mass, which is reduced in this population. For recommendation of dietary intake, it is helpful to use serum creatinine-derived formulas to estimate GFR. The Modification of Diet in Renal Disease (MDRD) Study equation, which incorporates information about age, sex, race, and serum creatinine concentration is most commonly used in clinical practice and in research studies.(82) However, it systematically under-estimates GFR in individuals with normal or near-normal GFR (> 60 ml/min/1.73 m2). The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) is a new and improved equation to estimate GFR, particularly in individuals with normal GFR (> 60 ml/min/1.73 m2).(83) Although these equations improve the estimation of GFR compared to serum creatinine in older adults, the MDRD equation still underestimates mean measured GFR by 25%, and the CKD-EPI equation by 16%, respectively, in this population. This bias may lead to misclassifying healthy older persons as having CKD.(84) Based on GFR estimates, kidney function is categorized as normal or mild dysfunction (GFR > 60 ml/min/1.73 m2), moderate dysfunction (30 < GFR < 60 ml/min/1.73 m2), or severe dysfunction (GFR < 30 ml/min/1.73 m2). It is notable that CKD can also result from defects in kidney structure or kidney function that are evident as proteinuria or other problems but not as altered GFR.(85)
For protein intake in patients with possible alteration of kidney function, the following guidance is offered:
In older adults with healthy kidneys or with only mild dysfunction, standard protein intake is safe.
In older patients with moderately impaired GFR or another form of CKD, physicians customarily assess the balance between risks and benefits, and use clinical judgment to make recommendations.
In patients with severe CKD, it is usual to recommend a lower protein intake of 0.6 to 0.8 g/kg/day with sufficient energy intake (about 30 kcal/kg/day). However, multi-morbid patients on palliative care are an exception to this rule. These individuals may benefit from unrestricted intake of dietary protein because the short-term risks associated with protein energy wasting are greater than the long-term risks of worsening renal function due to diet with standard protein content.
CONCLUSIONS
If the increasing life expectancy over the past two centuries continues at the same rate through the 21st century, many babies born since 2000 will celebrate their 100th birthdays.(86) In fact, average lifespan has increased 7 to 10 years in just 3 decades.(86)
What distinguishes a generally healthy, long-lived person today? A study of Japanese centenarians (100 years or older) found that those who remained autonomous, i.e., performed activities of daily living, had good cognition, and had good social networks, had more frequent intake of protein and regular exercise as distinguishing features compared to their non-autonomous peers.(87)
Adequate dietary protein intake and continuing exercise are important to healthy aging. Trajectories of greater muscle protein breakdown are more likely when older age is confounded by acute or chronic disease, e.g., cancer, heart failure, COPD, or CKD undergoing dialysis. If protein catabolism not offset by increasing protein intake, along with maintaining physical activity, older adults are at higher risk for sarcopenia, frailty, disability. Results of a recent study showed that low dietary protein intake can help prevent cancer and other diseases in young adults, while older adults need high protein intake to sustain healthy aging and longevity.(88)
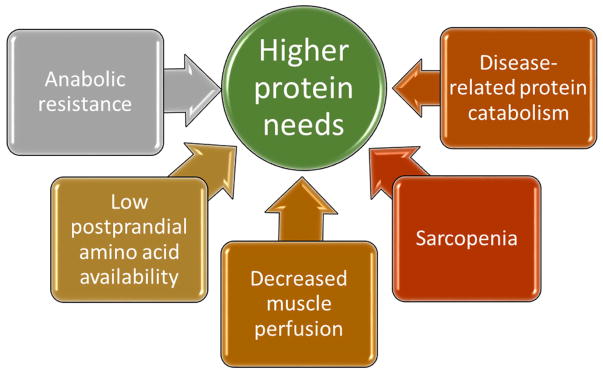
In order to help prevent or delay adverse consequences, we encourage increased intake of dietary protein for older adults (≥ 65 years) compared to younger adults, and continued participation in routine exercise or physical activities (Figure 3). At the same time, it is important for older people to balance total energy intake with total body energy demands—a rationale for consuming protein as a higher proportion of daily energy intake.
Figure 3.
Recommendations for maintaining healthy muscle with aging
Acknowledgments
The authors thank Dr. Cecilia Hofmann (C. Hofmann & Associates, Western Springs, IL, USA) for her capable assistance with writing, reference management, and editing.
Work by Nicolaas E. P. Deutz for this article was supported by Award Number R01HL095903 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of this authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–23. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lanza IR, Short DK, Short KR, Raghavakaimal S, Basu R, Joyner MJ, et al. Endurance exercise as a countermeasure for aging. Diabetes. 2008;57(11):2933–42. doi: 10.2337/db08-0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boirie Y. Physiopathological mechanism of sarcopenia. J Nutr Health Aging. 2009;13(8):717–23. doi: 10.1007/s12603-009-0203-x. [DOI] [PubMed] [Google Scholar]
- 4.Fulgoni VL., 3rd Current protein intake in America: analysis of the National Health and Nutrition Examination Survey, 2003–2004. Am J Clin Nutr. 2008;87(5):1554S–7S. doi: 10.1093/ajcn/87.5.1554S. [DOI] [PubMed] [Google Scholar]
- 5.Volpi E, Campbell WW, Dwyer JT, Johnson MA, Jensen GL, Morley JE, et al. Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? J Gerontol A Biol Sci Med Sci. 2013;68(6):677–81. doi: 10.1093/gerona/gls229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tieland M, Borgonjen-Van den Berg KJ, van Loon LJ, de Groot LC. Dietary protein intake in community-dwelling, frail, and institutionalized elderly people: scope for improvement. Eur J Nutr. 2012;51(2):173–9. doi: 10.1007/s00394-011-0203-6. [DOI] [PubMed] [Google Scholar]
- 7.Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, et al. Evidence-Based Recommendations for Optimal Dietary Protein Intake in Older People: A Position Paper From the PROT-AGE Study Group. J Am Med Dir Assoc. 2013;14(8):542–59. doi: 10.1016/j.jamda.2013.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Gray-Donald K, Arnaud-McKenzie DS, Gaudreau P, Morais JA, Shatenstein B, Payette H. Protein Intake Protects against Weight Loss in Healthy Community-Dwelling Older Adults. J Nutr. 2014;144(3):321–6. doi: 10.3945/jn.113.184705. [DOI] [PubMed] [Google Scholar]
- 9.Koopman R. Dietary protein and exercise training in ageing. Proc Nutr Soc. 2011;70(1):104–13. doi: 10.1017/S0029665110003927. [DOI] [PubMed] [Google Scholar]
- 10.Houston DK, Nicklas BJ, Ding J, Harris TB, Tylavsky FA, Newman AB, et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr. 2008;87(1):150–5. doi: 10.1093/ajcn/87.1.150. [DOI] [PubMed] [Google Scholar]
- 11.Beasley JM, Wertheim BC, LaCroix AZ, Prentice RL, Neuhouser ML, Tinker LF, et al. Biomarker-calibrated protein intake and physical function in the Women’s Health Initiative. J Am Geriatr Soc. 2013;61(11):1863–71. doi: 10.1111/jgs.12503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burd NA, Gorissen SH, van Loon LJ. Anabolic resistance of muscle protein synthesis with aging. Exercise and sport sciences reviews. 2013;41(3):169–73. doi: 10.1097/JES.0b013e318292f3d5. [DOI] [PubMed] [Google Scholar]
- 13.Rennie MJ. Anabolic resistance: the effects of aging, sexual dimorphism, and immobilization on human muscle protein turnover. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. 2009;34(3):377–81. doi: 10.1139/H09-012. [DOI] [PubMed] [Google Scholar]
- 14.Koopman R, Walrand S, Beelen M, Gijsen AP, Kies AK, Boirie Y, et al. Dietary protein digestion and absorption rates and the subsequent postprandial muscle protein synthetic response do not differ between young and elderly men. J Nutr. 2009;139(9):1707–13. doi: 10.3945/jn.109.109173. [DOI] [PubMed] [Google Scholar]
- 15.Deutz NE, Wolfe RR. Is there a maximal anabolic response to protein intake with a meal? Clin Nutr. 2013;32(2):309–13. doi: 10.1016/j.clnu.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wall BT, van Loon LJ. Nutritional strategies to attenuate muscle disuse atrophy. Nutr Rev. 2013;71(4):195–208. doi: 10.1111/nure.12019. [DOI] [PubMed] [Google Scholar]
- 17.Thomas DR. Loss of skeletal muscle mass in aging: examining the relationship of starvation, sarcopenia and cachexia. Clin Nutr. 2007;26(4):389–99. doi: 10.1016/j.clnu.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 18.Protein and amino acid requirements in human nutrition. World Health Organ Tech Rep Ser. 2007;(935):1–265. back cover. [PubMed] [Google Scholar]
- 19.Gaffney-Stomberg E, Insogna KL, Rodriguez NR, Kerstetter JE. Increasing dietary protein requirements in elderly people for optimal muscle and bone health. J Am Geriatr Soc. 2009;57(6):1073–9. doi: 10.1111/j.1532-5415.2009.02285.x. [DOI] [PubMed] [Google Scholar]
- 20.Morley JE, Argiles JM, Evans WJ, Bhasin S, Cella D, Deutz NE, et al. Nutritional recommendations for the management of sarcopenia. J Am Med Dir Assoc. 2010;11(6):391–6. doi: 10.1016/j.jamda.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 22.Hung WW, Ross JS, Boockvar KS, Siu AL. Recent trends in chronic disease, impairment and disability among older adults in the United States. BMC geriatrics. 2011;11:47. doi: 10.1186/1471-2318-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berrut G, Andrieu S, Araujo de Carvalho I, Baeyens JP, Bergman H, Cassim B, et al. Promoting access to innovation for frail old persons. IAGG (International Association of Gerontology and Geriatrics), WHO (World Health Organization) and SFGG (Societe Francaise de Geriatrie et de Gerontologie) Workshop--Athens January 20–21, 2012 Tool (GFST) J Nutr Health Aging. 2013;17(8):688–93. doi: 10.1007/s12603-013-0039-2. [DOI] [PubMed] [Google Scholar]
- 24.Cruz-Jentoft AJ, Michel JP. Sarcopenia: a useful paradigm for physical frailty. Eur Geriatr Med. 2013;4:102–5. [Google Scholar]
- 25.Beasley JM, LaCroix AZ, Neuhouser ML, Huang Y, Tinker L, Woods N, et al. Protein intake and incident frailty in the Women’s Health Initiative observational study. J Am Geriatr Soc. 2010;58(6):1063–71. doi: 10.1111/j.1532-5415.2010.02866.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meng X, Zhu K, Devine A, Kerr DA, Binns CW, Prince RL. A 5-year cohort study of the effects of high protein intake on lean mass and BMC in elderly postmenopausal women. J Bone Miner Res. 2009;24(11):1827–34. doi: 10.1359/jbmr.090513. [DOI] [PubMed] [Google Scholar]
- 27.Frisoli A, Jr, Chaves PH, Ingham SJ, Fried LP. Severe osteopenia and osteoporosis, sarcopenia, and frailty status in community-dwelling older women: results from the Women’s Health and Aging Study (WHAS) II. Bone. 2011;48(4):952–7. doi: 10.1016/j.bone.2010.12.025. [DOI] [PubMed] [Google Scholar]
- 28.Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med. 2006;166(4):418–23. doi: 10.1001/archinte.166.4.418. [DOI] [PubMed] [Google Scholar]
- 29.Dideriksen K, Reitelseder S, Holm L. Influence of amino acids, dietary protein, and physical activity on muscle mass development in humans. Nutrients. 2013;5(3):852–76. doi: 10.3390/nu5030852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dickinson JM, Volpi E, Rasmussen BB. Exercise and nutrition to target protein synthesis impairments in aging skeletal muscle. Exercise and sport sciences reviews. 2013;41(4):216–23. doi: 10.1097/JES.0b013e3182a4e699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glover EI, Phillips SM, Oates BR, Tang JE, Tarnopolsky MA, Selby A, et al. Immobilization induces anabolic resistance in human myofibrillar protein synthesis with low and high dose amino acid infusion. The Journal of physiology. 2008;586(Pt 24):6049–61. doi: 10.1113/jphysiol.2008.160333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Breen L, Stokes KA, Churchward-Venne TA, Moore DR, Baker SK, Smith K, et al. Two weeks of reduced activity decreases leg lean mass and induces “anabolic resistance” of myofibrillar protein synthesis in healthy elderly. J Clin Endocrinol Metab. 2013;98(6):2604–12. doi: 10.1210/jc.2013-1502. [DOI] [PubMed] [Google Scholar]
- 33.Fiatarone MA, Marks EC, Ryan ND, Meredith CN, Lipsitz LA, Evans WJ. High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA. 1990;263(22):3029–34. [PubMed] [Google Scholar]
- 34.Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;(3):CD002759. doi: 10.1002/14651858.CD002759.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breen L, Philp A, Shaw CS, Jeukendrup AE, Baar K, Tipton KD. Beneficial effects of resistance exercise on glycemic control are not further improved by protein ingestion. PLoS One. 2011;6(6):e20613. doi: 10.1371/journal.pone.0020613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang Y, Breen L, Burd NA, Hector AJ, Churchward-Venne TA, Josse AR, et al. Resistance exercise enhances myofibrillar protein synthesis with graded intakes of whey protein in older men. Br J Nutr. 2012:1–9. doi: 10.1017/S0007114511007422. [DOI] [PubMed] [Google Scholar]
- 37.Balagopal P, Schimke JC, Ades P, Adey D, Nair KS. Age effect on transcript levels and synthesis rate of muscle MHC and response to resistance exercise. Am J Physiol Endocrinol Metab. 2001;280(2):E203–8. doi: 10.1152/ajpendo.2001.280.2.E203. [DOI] [PubMed] [Google Scholar]
- 38.Timmerman KL, Dhanani S, Glynn EL, Fry CS, Drummond MJ, Jennings K, et al. A moderate acute increase in physical activity enhances nutritive flow and the muscle protein anabolic response to mixed nutrient intake in older adults. Am J Clin Nutr. 2012;95(6):1403–12. doi: 10.3945/ajcn.111.020800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Burd NA, West DW, Moore DR, Atherton PJ, Staples AW, Prior T, et al. Enhanced amino acid sensitivity of myofibrillar protein synthesis persists for up to 24 h after resistance exercise in young men. J Nutr. 2011;141(4):568–73. doi: 10.3945/jn.110.135038. [DOI] [PubMed] [Google Scholar]
- 40.Walrand S, Boirie Y. Optimizing protein intake in aging. Curr Opin Clin Nutr Metab Care. 2005;8(1):89–94. doi: 10.1097/00075197-200501000-00014. [DOI] [PubMed] [Google Scholar]
- 41.Paddon-Jones D, Leidy H. Dietary protein and muscle in older persons. Curr Opin Clin Nutr Metab Care. 2014;17(1):5–11. doi: 10.1097/MCO.0000000000000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scott D, Blizzard L, Fell J, Giles G, Jones G. Associations between dietary nutrient intake and muscle mass and strength in community-dwelling older adults: the Tasmanian Older Adult Cohort Study. J Am Geriatr Soc. 2010;58(11):2129–34. doi: 10.1111/j.1532-5415.2010.03147.x. [DOI] [PubMed] [Google Scholar]
- 43.Gaillard C, Alix E, Boirie Y, Berrut G, Ritz P. Are elderly hospitalized patients getting enough protein? J Am Geriatr Soc. 2008;56(6):1045–9. doi: 10.1111/j.1532-5415.2008.01721.x. [DOI] [PubMed] [Google Scholar]
- 44.Pedersen T, Cederholm T. Nordic Nutrition Recommendations. Food Nutr Res. 2014;58:23364. [Google Scholar]
- 45.Nordic Council of Ministers. Integrating nutrition and physical activity. 2014. Nordic Nutrition Recommendations 2012; pp. 1–627. [Google Scholar]
- 46.Boirie Y, Dangin M, Gachon P, Vasson MP, Maubois JL, Beaufrere B. Slow and fast dietary proteins differently modulate postprandial protein accretion. Proc Natl Acad Sci U S A. 1997;94(26):14930–5. doi: 10.1073/pnas.94.26.14930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boirie Y, Gachon P, Corny S, Fauquant J, Maubois JL, Beaufrere B. Acute postprandial changes in leucine metabolism as assessed with an intrinsically labeled milk protein. The American journal of physiology. 1996;271(6 Pt 1):E1083–91. doi: 10.1152/ajpendo.1996.271.6.E1083. [DOI] [PubMed] [Google Scholar]
- 48.Tang JE, Moore DR, Kujbida GW, Tarnopolsky MA, Phillips SM. Ingestion of whey hydrolysate, casein, or soy protein isolate: effects on mixed muscle protein synthesis at rest and following resistance exercise in young men. Journal of applied physiology. 2009;107(3):987–92. doi: 10.1152/japplphysiol.00076.2009. [DOI] [PubMed] [Google Scholar]
- 49.Reitelseder S, Agergaard J, Doessing S, Helmark IC, Lund P, Kristensen NB, et al. Whey and casein labeled with L-[1-13C]leucine and muscle protein synthesis: effect of resistance exercise and protein ingestion. Am J Physiol Endocrinol Metab. 2011;300(1):E231–42. doi: 10.1152/ajpendo.00513.2010. [DOI] [PubMed] [Google Scholar]
- 50.Remond D, Machebeuf M, Yven C, Buffiere C, Mioche L, Mosoni L, et al. Postprandial whole-body protein metabolism after a meat meal is influenced by chewing efficiency in elderly subjects. Am J Clin Nutr. 2007;85(5):1286–92. doi: 10.1093/ajcn/85.5.1286. [DOI] [PubMed] [Google Scholar]
- 51.Bax ML, Buffiere C, Hafnaoui N, Gaudichon C, Savary-Auzeloux I, Dardevet D, et al. Effects of meat cooking, and of ingested amount, on protein digestion speed and entry of residual proteins into the colon: a study in minipigs. PLoS One. 2013;8(4):e61252. doi: 10.1371/journal.pone.0061252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bouillanne O, Curis E, Hamon-Vilcot B, Nicolis I, Chretien P, Schauer N, et al. Impact of protein pulse feeding on lean mass in malnourished and at-risk hospitalized elderly patients: a randomized controlled trial. Clin Nutr. 2013;32(2):186–92. doi: 10.1016/j.clnu.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 53.Arnal MA, Mosoni L, Boirie Y, Houlier ML, Morin L, Verdier E, et al. Protein pulse feeding improves protein retention in elderly women. Am J Clin Nutr. 1999;69(6):1202–8. doi: 10.1093/ajcn/69.6.1202. [DOI] [PubMed] [Google Scholar]
- 54.Arnal MA, Mosoni L, Boirie Y, Houlier ML, Morin L, Verdier E, et al. Protein feeding pattern does not affect protein retention in young women. J Nutr. 2000;130(7):1700–4. doi: 10.1093/jn/130.7.1700. [DOI] [PubMed] [Google Scholar]
- 55.Areta JL, Burke LM, Ross ML, Camera DM, West DW, Broad EM, et al. Timing and distribution of protein ingestion during prolonged recovery from resistance exercise alters myofibrillar protein synthesis. J Physiol. 2013;591(Pt 9):2319–31. doi: 10.1113/jphysiol.2012.244897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Volpi E, Kobayashi H, Sheffield-Moore M, Mittendorfer B, Wolfe RR. Essential amino acids are primarily responsible for the amino acid stimulation of muscle protein anabolism in healthy elderly adults. Am J Clin Nutr. 2003;78(2):250–8. doi: 10.1093/ajcn/78.2.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Katsanos CS, Kobayashi H, Sheffield-Moore M, Aarsland A, Wolfe RR. A high proportion of leucine is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. American journal of physiology Endocrinology and metabolism. 2006;291(2):E381–7. doi: 10.1152/ajpendo.00488.2005. [DOI] [PubMed] [Google Scholar]
- 58.Biolo G, De Cicco M, Dal Mas V, Lorenzon S, Antonione R, Ciocchi B, et al. Response of muscle protein and glutamine kinetics to branched-chain-enriched amino acids in intensive care patients after radical cancer surgery. Nutrition. 2006;22(5):475–82. doi: 10.1016/j.nut.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 59.Marchesini G, Zoli M, Dondi C, Bianchi G, Cirulli M, Pisi E. Anticatabolic effect of branched-chain amino acid-enriched solutions in patients with liver cirrhosis. Hepatology. 1982;2(4):420–5. doi: 10.1002/hep.1840020405. [DOI] [PubMed] [Google Scholar]
- 60.Kim HK, Suzuki T, Saito K, Yoshida H, Kobayashi H, Kato H, et al. Effects of exercise and amino acid supplementation on body composition and physical function in community-dwelling elderly Japanese sarcopenic women: a randomized controlled trial. Journal of the American Geriatrics Society. 2012;60(1):16–23. doi: 10.1111/j.1532-5415.2011.03776.x. [DOI] [PubMed] [Google Scholar]
- 61.Borsheim E, Bui QU, Tissier S, Kobayashi H, Ferrando AA, Wolfe RR. Effect of amino acid supplementation on muscle mass, strength and physical function in elderly. Clin Nutr. 2008;27(2):189–95. doi: 10.1016/j.clnu.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Verhoeven S, Vanschoonbeek K, Verdijk LB, Koopman R, Wodzig WK, Dendale P, et al. Long-term leucine supplementation does not increase muscle mass or strength in healthy elderly men. Am J Clin Nutr. 2009;89(5):1468–75. doi: 10.3945/ajcn.2008.26668. [DOI] [PubMed] [Google Scholar]
- 63.Leenders M, Verdijk LB, van der Hoeven L, van Kranenburg J, Hartgens F, Wodzig WK, et al. Prolonged leucine supplementation does not augment muscle mass or affect glycemic control in elderly type 2 diabetic men. J Nutr. 2011;141(6):1070–6. doi: 10.3945/jn.111.138495. [DOI] [PubMed] [Google Scholar]
- 64.Vukovich MD, Dreifort GD. Effect of beta-hydroxy beta-methylbutyrate on the onset of blood lactate accumulation and V(O)(2) peak in endurance-trained cyclists. Journal of strength and conditioning research / National Strength & Conditioning Association. 2001;15(4):491–7. [PubMed] [Google Scholar]
- 65.Wilkinson DJ, Hossain T, Hill DS, Phillips BE, Crossland H, Williams J, et al. Effects of leucine and its metabolite beta-hydroxy-beta-methylbutyrate on human skeletal muscle protein metabolism. The Journal of physiology. 2013;591(Pt 11):2911–23. doi: 10.1113/jphysiol.2013.253203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fitschen PJ, Wilson GJ, Wilson JM, Wilund KR. Efficacy of beta-hydroxy-beta-methylbutyrate supplementation in elderly and clinical populations. Nutrition. 2013;29(1):29–36. doi: 10.1016/j.nut.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 67.Rahman A, Wilund K, Fitschen PJ, Jeejeebhoy K, Agarwala R, Drover JW, et al. Elderly Persons With ICU-Acquired Weakness: The Potential Role for beta-Hydroxy-beta-Methylbutyrate (HMB) Supplementation? JPEN J Parenter Enteral Nutr. 2013 doi: 10.1177/0148607113502545. [DOI] [PubMed] [Google Scholar]
- 68.Deutz NE, Pereira SL, Hays NP, Oliver JS, Edens NK, Evans CM, et al. Effect of beta-hydroxy-beta-methylbutyrate (HMB) on lean body mass during 10 days of bed rest in older adults. Clin Nutr. 2013;32(5):704–12. doi: 10.1016/j.clnu.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 69.Visser M. In: Epidemiology of muscle mass loss with age. Cruz-Jentoft A, Morley J, editors. Sarcopenia: John Wiley & Sons Ltd; 2012. pp. 1–7. [Google Scholar]
- 70.Visser M, Goodpaster BH, Kritchevsky SB, Newman AB, Nevitt M, Rubin SM, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. The journals of gerontology. 2005;60(3):324–33. doi: 10.1093/gerona/60.3.324. [DOI] [PubMed] [Google Scholar]
- 71.Guillet C, Masgrau A, Walrand S, Boirie Y. Impaired protein metabolism: interlinks between obesity, insulin resistance and inflammation. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2012;13(Suppl 2):51–7. doi: 10.1111/j.1467-789X.2012.01037.x. [DOI] [PubMed] [Google Scholar]
- 72.Stenholm S, Harris TB, Rantanen T, Visser M, Kritchevsky SB, Ferrucci L. Sarcopenic obesity: definition, cause and consequences. Curr Opin Clin Nutr Metab Care. 2008;11(6):693–700. doi: 10.1097/MCO.0b013e328312c37d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zamboni M, Mazzali G, Fantin F, Rossi A, Di Francesco V. Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis. 2008;18(5):388–95. doi: 10.1016/j.numecd.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 74.Schautz B, Later W, Heller M, Muller MJ, Bosy-Westphal A. Total and regional relationship between lean and fat mass with increasing adiposity--impact for the diagnosis of sarcopenic obesity. Eur J Clin Nutr. 2012;66(12):1356–61. doi: 10.1038/ejcn.2012.138. [DOI] [PubMed] [Google Scholar]
- 75.Benton MJ, Whyte MD, Dyal BW. Sarcopenic obesity: strategies for management. The American journal of nursing. 2011;111(12):38–44. doi: 10.1097/01.NAJ.0000408184.21770.98. quiz 5–6. [DOI] [PubMed] [Google Scholar]
- 76.Rantanen T, Harris T, Leveille SG, Visser M, Foley D, Masaki K, et al. Muscle strength and body mass index as long-term predictors of mortality in initially healthy men. J Gerontol A Biol Sci Med Sci. 2000;55(3):M168–73. doi: 10.1093/gerona/55.3.m168. [DOI] [PubMed] [Google Scholar]
- 77.Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364(13):1218–29. doi: 10.1056/NEJMoa1008234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Biolo G, Ciocchi B, Stulle M, Bosutti A, Barazzoni R, Zanetti M, et al. Calorie restriction accelerates the catabolism of lean body mass during 2 wk of bed rest. Am J Clin Nutr. 2007;86(2):366–72. doi: 10.1093/ajcn/86.2.366. [DOI] [PubMed] [Google Scholar]
- 79.Beasley JM, Aragaki AK, LaCroix AZ, Neuhouser ML, Tinker LF, Cauley JA, et al. Higher biomarker-calibrated protein intake is not associated with impaired renal function in postmenopausal women. J Nutr. 2011;141(8):1502–7. doi: 10.3945/jn.110.135814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Knight EL, Stampfer MJ, Hankinson SE, Spiegelman D, Curhan GC. The impact of protein intake on renal function decline in women with normal renal function or mild renal insufficiency. Ann Intern Med. 2003;138(6):460–7. doi: 10.7326/0003-4819-138-6-200303180-00009. [DOI] [PubMed] [Google Scholar]
- 81.Maw TT, Fried L. Chronic kidney disease in the elderly. Clin Geriatr Med. 2013;29(3):611–24. doi: 10.1016/j.cger.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 82.Levey AS, Coresh J, Greene T, Marsh J, Stevens LA, Kusek JW, et al. Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clinical chemistry. 2007;53(4):766–72. doi: 10.1373/clinchem.2006.077180. [DOI] [PubMed] [Google Scholar]
- 83.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nittaa K, Okada K, Yanaia M, Takahashi S. Aging and chronic kidney disease. Kidney Blood Press Res. 2013;38:109–20. doi: 10.1159/000355760. [DOI] [PubMed] [Google Scholar]
- 85.Stevens PE, Levin A Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group M. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825–30. doi: 10.7326/0003-4819-158-11-201306040-00007. [DOI] [PubMed] [Google Scholar]
- 86.Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374(9696):1196–208. doi: 10.1016/S0140-6736(09)61460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ozaki A, Uchiyama M, Tagaya H, Ohida T, Ogihara R. The Japanese Centenarian Study: autonomy was associated with health practices as well as physical status. J Am Geriatr Soc. 2007;55(1):95–101. doi: 10.1111/j.1532-5415.2006.01019.x. [DOI] [PubMed] [Google Scholar]
- 88.Levine ME, Suarez JA, Brandhorst S, Balasubramanian P, Cheng CW, Madia F, et al. Low Protein Intake Is Associated with a Major Reduction in IGF-1, Cancer, and Overall Mortality in the 65 and Younger but Not Older Population. Cell metabolism. 2014;19(3):407–17. doi: 10.1016/j.cmet.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tang M, McCabe GP, Elango R, Pencharz PB, Ball RO, Campbell WW. Assessment of protein requirement in octogenarian women with use of the indicator amino acid oxidation technique. Am J Clin Nutr. 2014;99(4):891–8. doi: 10.3945/ajcn.112.042325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bartali B, Frongillo EA, Stipanuk MH, Bandinelli S, Salvini S, Palli D, et al. Protein intake and muscle strength in older persons: does inflammation matter? J Am Geriatr Soc. 2012;60(3):480–4. doi: 10.1111/j.1532-5415.2011.03833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tieland M, Dirks ML, van der Zwaluw N, Verdijk LB, van de Rest O, de Groot LC, et al. Protein supplementation increases muscle mass gain during prolonged resistance-type exercise training in frail elderly people: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc. 2012;13(8):713–9. doi: 10.1016/j.jamda.2012.05.020. [DOI] [PubMed] [Google Scholar]