Abstract
Background
Depression is related to increased morbidity and mortality in the general population and among patients with coronary artery disease (CAD). The prevalence of major depression is two-times higher in women than men in the general population, but whether this pattern holds true in the CAD population has not been established.
Objective
To test, through quantitative synthesis, whether women with CAD have a greater prevalence of major depression than men.
Method
MEDLINE, EMBASE, and PsycINFO electronic databases were searched. Authors of key articles were contacted to identify other relevant publications. The titles and abstracts were screened by the first author and the selected full-text articles were independently screened by the first and second authors based on pre-defined inclusion criteria. Major depression had to be diagnosed through structured clinical interviews during cardiac-related hospitalization or post-CAD hospitalization. Meta-analysis was undertaken using the Review Manager 5 software program. All pooled analyses were based on random-effects models.
Results
Eight eligible cohort and cross-sectional studies reporting data for 2072 participants (509 [24.6%] women) were included. Overall, major depression was observed in 95 (18.7%) women and 187 (12.0%) men. In the pooled analysis, prevalence of major depression was significantly greater in women compared to men (odds ratio=1.77, 95% confidence interval=1.21–2.58, p<.01). Heterogeneity was considered low to moderate (I2=36.0%).
Conclusion
Consistent with the general population, the prevalence of major depression is two-times greater in women than men with CAD. Women with CAD may warrant greater emphasis in efforts to identify and treat depression.
Keywords: Depression, Sex differences, Women, Men, Coronary artery disease
Cardiovascular Disease (CVD) is the leading cause of mortality worldwide,1 and is a significant contributor to morbidity and health-related costs.2 Recently, there has been growing interest in non-traditional cardiac risk factors such as psychosocial factors. Research shows that depression is related to a greater risk of coronary artery disease (CAD) onset, and poorer long-term prognosis among those with established CAD.3 Specifically, depressive symptomatology confers a relative risk between 1.5 and 2.5 for future cardiac morbidity and mortality,4 and a dose-response relationship has been established.5
In cardiac patients, the prevalence of major depression ranges around 15% to 20%,4 which is approximately three times higher than what is found in age-matched, community-based prevalence studies.6, 7 Further, the prevalence of elevated depression symptoms has been reported to be as high as 50%.5 A more recent systematic review of eight studies including a total of 10,785 patients demonstrated that major depression was identified in 19.8% of acute myocardial infarction patients.8
Beginning at puberty and persisting through adult life, the prevalence and incidence of depressive disorders are higher in females than in males.9 Specifically, depression is two times greater in women compared to men.10 Biological factors such as hormones, and psychosocial factors such as role overload have been postulated to explain this gender difference.11 Although it has been suggested that sex differences in the prevalence of major depression among cardiac patients exist,12, 13 to date, no systematic review or meta-analysis has examined this question. The higher burden of CVD- and CAD-related mortality among women, the greater prevalence of depression among women in the general population, and guidelines calling for depression screening in CHD patients, from which women in particular may benefit, emphasize the need to systematically assess the presence or absence of a gender gap in depression. The objective of this study was to examine whether women with CAD experience greater prevalence of major depression than men with CAD, through a systematic review and meta-analysis of all observational studies that have examined the prevalence of major depression among CAD patients by sex.
Method
Eligibility criteria
Types of studies
Observational studies presenting original, primary data on the prevalence of major depression in CAD, analyzed by sex, were considered. The exclusion criteria were: i) meta-analyses, systematic reviews, case-series, case reports, published letters, comments, editorials, non-peer reviewed publications (e.g., dissertations), and ii) studies published in a language other than English. No year of publication restriction was imposed. In the case of multiple publications of the same cohort, the most recent article that best addressed the research question was chosen.
Types of participants
Studies that assessed depression by sex in adults over the age of 18 with CAD were considered. Participants must have had a history of hospitalization for reasons related to CAD including the following: myocardial infarction, cardiac revascularization (coronary artery bypass graft surgery or percutaneous coronary intervention), or those with unstable angina.
Types of outcome measures
Major depression had to be diagnosed through structured clinical interviews during cardiac-related hospitalization or post-CAD hospitalization. Diagnoses of Major Depressive Disorder had to be consistent with diagnostic criteria presented in the Diagnostic and Statistical Manual, Fourth Edition, Text Revision (DSM-IV TR) criteria for Major Depression.14 In addition, depression prevalence had to be stratified and presented by sex.
Information sources
Studies were identified by searching electronic databases, scanning reference lists of articles, and consulting experts in the field. The Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effectiveness, MEDLINE, ISI Web of Science, Excerpta Medica Database (EMBASE), PsycINFO, and Google Scholar were searched for prior systematic reviews and meta-analysis. In addition, reference lists of chapters in the latest edition of the Canadian Guidelines for Cardiac Rehabilitation and Cardiovascular Disease Prevention15 were examined for reviews on sex differences in prevalence of major depression in CAD patients. MEDLINE (1950-Present), EMBASE (1980-Present), and PsycINFO (1806-Present) electronic databases were searched for primary articles. The last search was performed on March 12, 2010. Authors of key articles were contacted to identify other relevant publications. RefWorks16 was used to store the citations and a Microsoft Excel 2003 database was used to record the process. All database searches were conducted with the assistance of information specialists at the University Health Network library. The search strategies were reviewed by SS, SLG and KLR. The search strategy for MEDLINE is presented in Appendix A.
Study selection
Duplicate records from different databases were excluded. Using a conservative threshold for exclusion, the retrieved records were independently screened by title and abstract (SS). Any ambiguity in titles and abstracts led to the retrieval of the full-text article. The selected full-text articles were independently assessed for eligibility using a standardized form (SS and KLR), and differences were resolved by discussion with the senior author (SLG).
Data Extraction
A data extraction form was developed, pilot-tested on two randomly-selected included studies, and revised accordingly. The first author (SS) extracted data from studies that met inclusion criteria, while the second author (KLR) independently verified the material. Disagreements were reconciled through consensus in face-to-face meetings. If no agreement could be reached, consultation with the senior author (SLG) was undertaken.
The information extracted from each included study included sociodemographic variables (e.g., age, education level, family income), CAD diagnosis, method of CAD diagnosis, time elapsed between CAD diagnosis and diagnosis of depression, heart disease risk factors, cardiac medication use, interview used to evaluate major depression, and prevalence of major depression.
Quality Assessment
To determine the validity of eligible studies, a pair of reviewers (SS and KLR) working independently determined with adequate reliability the methodological quality of the included studies using the Newcastle-Ottawa Scale.17 The Newcastle-Ottawa Scale is a nine-point scale that allocates points on the basis of the process of selection of the cohorts (0 –4 points), of the comparability of the cohorts (0 –2 points), and of the identification of the exposure and of the outcomes of study participants (0 –3 points). In addition, the overall quality of evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE18) criteria. A summary of findings and evidence profile table were generated through the software GRADEpro.19
Statistical Approach
Meta-analysis was performed using the software Review Manager 5.20 The meta-analysis was performed using a random-effects model to compute odds ratios. Heterogeneity was tested with the Breslow-Day test and the method proposed by Higgins21 was used to measure inconsistency (i.e., the percentage of total variation across studies due to heterogeneity). For each study, we plotted the effect by the inverse of its standard error. Egger’s regression intercept of funnel plot asymmetry was computed to test the presence of publication bias.22
Results
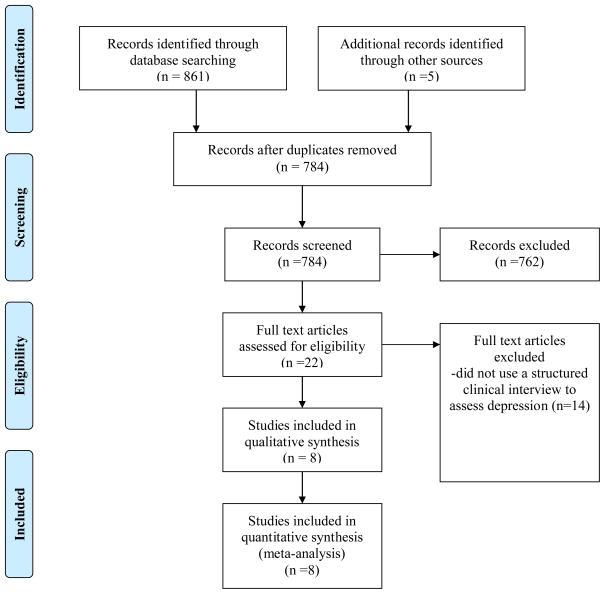
Figure 1 presents the flow diagram of study selection. A total of eight studies were identified for inclusion in the review. The search for previous reviews on this topic resulted in identification of one narrative review.13
Figure 1.
Flow diagram of study selection
Study characteristics
Table 1 displays the characteristics of the included studies. Three studies applied the Structured Clinical Interview for DSM Disorders (SCID23) to assess major depression, whereas the four other studies used one of the following structured clinical interview schedules: Diagnostic Interview Schedule, Modified version of the US National Institute of Mental Health Diagnostic Interview Schedule, Mini International Neuropsychiatric Interview, and Anxiety Disorders Interview Schedule-IV. One used the interviewer-administered semi-structured Hamilton Rating Scale for Depression. A decision was made to include the article as it was published in 1997, before the validation of the Depression Interview and Structured Hamilton (DISH).
Table 1.
Characteristics of included studies
| Authors, country, year of publication | Sample (size, CAD) | Clinical interview for assessment of major depression | Study design (time period) | Women | Men | Quality | ||
|---|---|---|---|---|---|---|---|---|
| Number | Major depression (%) | Number | Major depression (%) | |||||
| Carney et al., United States, 1987 | 50, CAD | Diagnostic Interview Schedule | Cross-sectional | 14 | 4 (29%) | 36 | 5 (14%) | 3 |
| Connerney et al., United States, 2001 | 309, CABG | Modified version of the US National Institute of Mental Health Diagnostic Interview Schedule | Longitudinal (follow up at 1 year) | 102 | 18 (18%) | 207 | 45 (22%) | 3 |
| Lesperance et al., Canada, 2004 | 481, ACS | Structured Clinical Interview for DSM Disorders | Cross-sectional | 91 | 12 (13%) | 390 | 23 (6%) | 3 |
| Mitchell et al., Canada, 2005 | 115, CABG | Mini International Neuropsychiatric Interview | Longitudinal (≤28 days pre-CABG, and follow-up between 6 and 12 weeks post-CABG) | 55 | 13 (25%) | 60 | 6 (10%) | 5 |
| Pedersen et al., Netherlands, 2008 | 710, PCI | Structured Clinical Interview for DSM Disorders | Longitudinal (baseline, and follow-up at 6 and 18 months) | 160 | 28 (18%) | 550 | 73 (13%) | 3 |
| Sullivan et al., United States, 1997 | 198, CAD | Hamilton Rating Scales for Depression (semi-structured clinical interview) | Longitudinal (baseline and follow-up at 1 year) | 34 | 8 (24%) | 164 | 17 (10%) | 3 |
| Swardfager et al., Canada. 2009 | 99, CAD | Structured Clinical Interview for DSM Disorders | Cross-sectional | 18 | 5 (28%) | 81 | 12 (15%) | 2 |
| Todaro et al., United States, 2005 | 110, CAD | Anxiety Disorders Interview Schedule-IV | Cross-sectional | 35 | 7 (20%) | 75 | 6 (8%) | 3 |
ACS, acute coronary syndrome; CAD, Coronary Artery Disease; MI, Myocardial Infarction; PCI, Percutaneous Coronary Intervention; CABG, Coronary Artery Bypass Graft
All studies were observational in design. The studies by Carney et al. (1987), Lesperance et al. (2004), Swardfager et al. (2009), and Todaro et al. (2005) were cross-sectional in design, whereas the other studies were longitudinal. The included studies observed 2072 participants in total, of which 509 (24.6%) were female. The studies were conducted in the United States, Canada, and Netherlands. No authors reported a source of study funding.
Quality of Evidence
The methodological quality of each study as assessed based on the Newcastle-Ottawa Scale for cohort studies17 is shown in Table 1. Table 2 shows the summary of findings and evidence profile of the included studies. Using the GRADE criteria,18 the overall quality of evidence was rated to be “low.” The primary reason for the low rating was the lack of adjustment for potential confounding variables.
Table 2.
Summary of findings and evidence profile of included studies
| Quality assessment | Summary of findings | Importance | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of patients | Effect | Quality | ||||||||||
| No of studies | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations | Females versus Males | control | Relative (95% CI) | Absolute | ||
| Major Depression | ||||||||||||
| 8 | observational studies | serious1 | serious2 | no serious indirectness | no serious imprecision | none | 95/509 (18.7%) | 187/1563 (12%) | OR 1.77 (1.21 to 2.58) | 74 more per 1000 (from 22 more to 140 more) | LOW | CRITICAL |
| 11.8% | 73 more per 1000 (from 21 more to 139 more) | |||||||||||
Confounding variables were not adjusted
I squared=36.0%
Meta-Analytic Results
Figure 2 shows the prevalence of major depression by sex for each included study, as well as the effect size and confidence interval. In the pooled analysis, prevalence of major depression was significantly greater in women compared to men with CAD (odds ratio=1.77, 95% confidence interval=1.21–2.58, p<.01).
Figure 2.
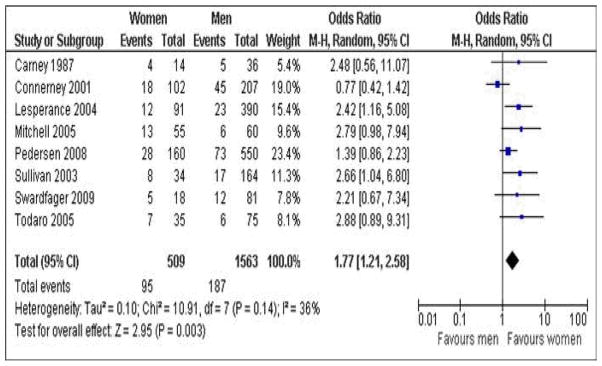
Forest plot of sex differences in prevalence of major depression in CAD patients
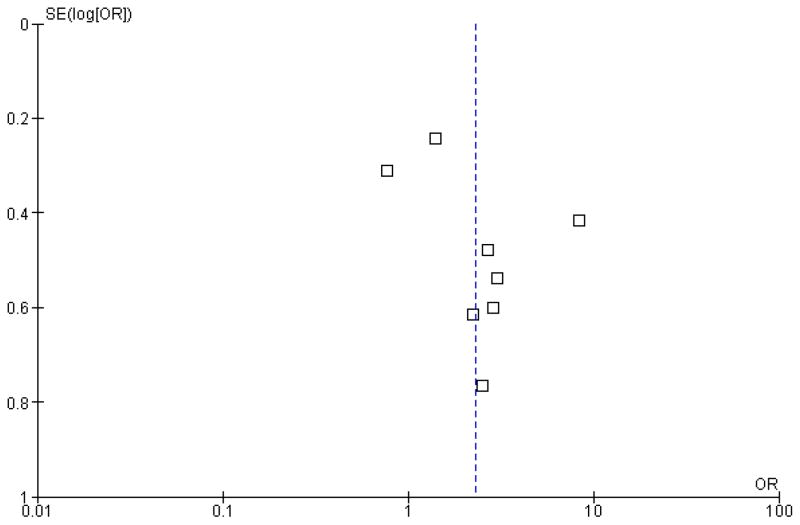
Heterogeneity was considered low to moderate (I2=36.0%). The shape of the funnel plot suggested lack of publication bias. Egger’s regression test provided no evidence of small sample bias. The size of estimate did not appear to vary with sample size, implying our results are not influenced by publication bias.
Two sensitivity analyses were performed by: (1) type of interview to assess depression and (2) sample size. For the former sensitivity analysis which examined the three studies that used the SCID,23 the prevalence of major depression was significantly different between women and men (odds ratio=1.68, 95% confidence interval=1.15–2.46, p<.05). For the latter, sensitivity analysis excluding Carney et al.’s study24 (sample size less than five for women), the prevalence of major depression was significantly greater in women compared to men (odds ratio=1.75, 95% confidence interval=1.17–2.63, p<.01).
Discussion
It has been demonstrated that comorbid depression is related to significantly poorer prognosis after coronary events,12, 25, 26 and that women in the general population have significantly greater burden of depression than men. This is the first meta-analysis to examine whether a sex difference exists in the prevalence of major depression in adults with CAD. In 1563 men and 509 women with CAD, results showed that women with CAD have approximately twice the prevalence of major depression as men. This is consistent in magnitude to the sex difference observed in the general population.10
The overall prevalence of comorbid major depression in men was 12.0% and in women was 18.7%. The overall depression rate in this study was approximately 14.3%, which is lower than the overall 19.8% prevalence reported in the systematic review of acute myocardial infarction patients by Thombs et al.8, 27 This discrepancy may be explained by the broader range of cardiac diagnosis included herein. Although no systematic review or meta-analysis has been published on sex differences to date, the findings herein are consistent with a previous narrative review13 and the burden reported in other chronic illnesses. For instance, the burden of major depression in stroke is estimated to be somewhat higher at 33%,28 but in this population the burden is similarly significantly higher among women than men.29 In contrast, a study examining gender disparity in depression rates in patients with advanced cancer reported no significant gender difference.30 The authors concluded that men and women may be equally likely to develop depression under highly stressful circumstances.
The multifactorial factors that may explain the greater prevalence of major depression in women than men in non-cardiac samples have been reviewed elsewhere.29 However, in the cardiac population, other explanatory factors may include physiological changes related to the menopausal transition in women, social factors such as role overload, role conflict, low socioeconomic status, and lower functional capacity among female cardiac patients than males.13
The findings herein hold important implications for depression treatment.The M-HART and ENRICHD trials of cardiac patients showed trends toward hazard and favoured usual care, respectively, for women.34–36 Given the greater burden of depression among women, clearly there is an urgent need to develop interventions shown to be safe and effective for this population. Recently, the COPES trial offering problem-solving therapy and/or pharmacotherapy and using a stepped-care approach showed promise in not only reducing depression, but also in counteracting the poorer health outcomes associated with comorbid depression.32 These positive effects in reducing depression were generalized to men and women. Most recently, the SUPRIM trial demonstrated that a cognitive behavioural therapy intervention with stress management resulted in significantly lower fatal and non-fatal first recurrent events and significantly fewer recurrent myocardial infarctions in adjusted analyses when compared to controls. Given the proven benefits of cardiac rehabilitation such as decrease in mortality and depression rates, health care providers should encourage both male and female cardiac patients to participate in these programs.
Limitations
Caution is warranted when interpreting these results. First, the overall quality of the evidence was rated as “low”, thus the results herein should be interpreted with caution. Second, the current study synthesized only studies published in English, which may limit the generalizability of these findings. Third, there was heterogeneity in the patient samples used in the included studies (e.g., post-myocardial infarction and revascularization patients). Fourth, most studies did not consider depression treatments (i.e., patients with effective treatment may not meet mood disorder criteria) or timing of depression in relation to their disease onset or hospitalization. Finally, multivariate analyses to adjust for potential confounding variables such as severity of depression, and receipt and type of depression treatment were not considered in any studies identified through the thorough search of the literature.
Conclusions
This meta-analysis demonstrated that, similar to the general population, the prevalence of major depression is approximately two-times greater in women with CAD compared to men. The prevalence of comorbid depression was high, even among men. Given the poorer prognosis associated with comorbid major depression in CAD, the findings emphasize the need to devote more attention to identify and address potential factors that could account for gender differences in depression.
Figure 3.
Funnel plot of sex differences in prevalence of major depression in CAD patients
Acknowledgments
We gratefully acknowledge the assistance of University Health Network information specialists Ms. Amy Faulkner and Ms. Rouhi Fazelzad in conducting the electronic database searches. We would also like to express gratitude to Dr. Elie Akl for his feedback on earlier versions of this manuscript.
Funding
Ms Shanmugasegaram is supported in her graduate studies by the Canadian Institutes of Health Research (CIHR) Frederick Banting and Charles Best Canada Graduate Scholarship -Doctoral Award. In addition, Dr. Grace is supported by CIHR salary award #MSH-80489. Role of funding source: CIHR played no role in study design, collection, analysis, interpretation of data, writing of the report, or in the decision to submit the paper for publication. It accepts no responsibility for the contents.
Appendix A. Search strategy: MEDLINE (OVID)
| CAD and related terms Component | |||
|
| |||
| 1 | Coronary Disease/ | 119195 | Advanced |
| 2 | Coronary Artery Disease/ | 23845 | Advanced |
| 3 | (coronary adj2 disease*).mp. | 173134 | Advanced |
| 4 | (coronary adj2 arterioscleros*).mp. | 740 | Advanced |
| 5 | Myocardial Infarction/ | 120285 | Advanced |
| 6 | (myocardia* adj2 infarct*).mp. | 154280 | Advanced |
| 7 | Coronary Artery Bypass/ | 35924 | Advanced |
| 8 | (coronary adj2 bypass*).mp. | 45005 | Advanced |
| 9 | (aortocoronary adj2 bypass*).mp. | 2438 | Advanced |
| 10 | CABG.mp. | 9027 | Advanced |
| 11 | Angioplasty, Transluminal, Percutaneous Coronary/ | 25153 | Advanced |
| 12 | (transluminal adj2 coronary).mp. | 27549 | Advanced |
| 13 | (angioplast* adj2 coronary).mp. | 11959 | Advanced |
| 14 | PTCA.mp. | 5873 | Advanced |
| 15 | PCI.mp. | 6596 | Advanced |
| 16 | Exp angina pectoris/ or exp angina, unstable/ | 36369 | Advanced |
| 17 | angina*.mp. | 53534 | Advanced |
| 18 | or/1–17 | 341894 | Advanced |
|
| |||
| Depression Component | |||
|
| |||
| 19 | Depression/ | 54525 | Advanced |
| 20 | depress*.mp. | 298712 | Advanced |
| 21 | Depressive Disorder, Major/ | 11850 | Advanced |
| 22 | (psychos?s adj2 involutional).mp. | 62 | Advanced |
| 23 | (melanchol* adj2 involutional).mp. | 63 | Advanced |
| 24 | or/19–23 | 298719 | Advanced |
| 25 | 18 and 24 | ||
|
| |||
| Gender differences and related terms Component | |||
|
| |||
| 26 | Sex Factors/ | 173460 | Advanced |
| 27 | (sex adj2 factor?).mp. | 175250 | Advanced |
| 28 | (sex adj2 differen*).mp. | 27146 | Advanced |
| 29 | (gender* adj2 differen*).mp. | 17503 | Advanced |
| 30 | (gender* adj2 compar*).mp. | 1125 | Advanced |
| 31 | (gender* adj2 factor?).mp. | 1358 | Advanced |
| 32 | or/26–31 | 204174 | Advanced |
|
| |||
| Combined Results (CAD, depression, and gender differences) limited to humans and adults | |||
|
| |||
| 33 | 25 and 32 | 373 | Advanced |
| 34 | Exp animals/ not (exp animals/ and exp humans/) | 3436332 | Advanced |
| 35 | 33 not 34 | 371 | Advanced |
| 36 | limit 33 to (“all infant (birth to 23 months)” or “all child (0 to 18 years)” or “newborn infant (birth to 1 month)” or “infant (1 to 23 months)” or “preschool child (2 to 5 years)” or “child (6 to 12 years)” or “adolescent (13 to 18 years)”) | 28 | Advanced |
| 37 | limit 33 to (“all adult (19 plus years)” or “young adult (19 to 24 years)” or “adult (19 to 44 years)” or “young adult and adult (19–24 and 19–44)” or “middle age (45 to 64 years)” or “middle aged (45 plus years)” or “all aged (65 and over)” or “aged (80 and over)”) | 323 | Advanced |
| 38 | 36 not 37 | 1 | Advanced |
| 39 | 33 not 38 | 370 | Advanced |
Footnotes
Contributors
SS contributed to writing the paper, initiating the study, designing the study, screening titles, abstracts and articles, analyzing the data, and assessing the methodological quality of individual studies and the overall quality of the evidence. KLR contributed to writing the paper and assisted with screening titles, abstracts and articles, and assessing the methodological quality of individual studies and the overall quality of the evidence. AHK contributed to writing the paper. DES contributed to writing the paper. SLG (the guarantor) and contributed to writing the paper, initiating the study, and monitoring progress.
References
- 1.World Health Organization. Cardiovascular diseases. Available at: http://www.who.int/mediacentre/factsheets/fs317/en/index.html.
- 2.Cardiac Care Network. The Ontario cardiac rehabilitation pilot project: Report and recommendations. 2002. [Google Scholar]
- 3.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosom Med. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 4.Lett HS, Blumenthal JA, Babyak MA, Strauman TJ, Robins C, Sherwood A. Social Support and Coronary Heart Disease: Epidemiologic Evidence and Implications for Treatment. Psychosom Med. 2005;67:869–878. doi: 10.1097/01.psy.0000188393.73571.0a. [DOI] [PubMed] [Google Scholar]
- 5.Lesperance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation. 2002;105:1049–1053. doi: 10.1161/hc0902.104707. [DOI] [PubMed] [Google Scholar]
- 6.Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. Am J Psychiatry. 1994;151:979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- 7.Lavie CJ, Milani RV, Cassidy MM, Gilliland YE. Effects of cardiac rehabilitation and exercise training programs in women with depression. Am J Cardiol. 1999;83:1480–3. A7. doi: 10.1016/s0002-9149(99)00127-7. [DOI] [PubMed] [Google Scholar]
- 8.Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21:30–38. doi: 10.1111/j.1525-1497.2005.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piccinelli M, Wilkinson G. Gender differences in depression. Critical review. Br J Psychiatry. 2000;177:486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- 10.Nolen-Hoeksema S, Larson J, Grayson C. Explaining the gender difference in depressive symptoms. J Pers Soc Psychol. 1999;77:1061–1072. doi: 10.1037//0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- 11.Kornstein S. Gender differences in depression: Implications for treatment. J Clin Psychiatry. 1997;58:12–8. [PubMed] [Google Scholar]
- 12.Frasure-Smith N, Lesperance F, Juneau M, Talajic M, Bourassa MG. Gender, depression, and one-year prognosis after myocardial infarction. Psychosom Med. 1999;61:26–37. doi: 10.1097/00006842-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Naqvi TZ, Naqvi SS, Merz CN. Gender differences in the link between depression and cardiovascular disease. Psychosom Med. 2005;67 (Suppl 1):S15–8. doi: 10.1097/01.psy.0000164013.55453.05. [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV. 4. Washington, D.C: American Psychiatric Association; 1994. [Google Scholar]
- 15.Stone JA, Arthur HM, Suskin N, editors. Canadian Association of Cardiac Rehabilitation. 3. Winnipeg, MB: 2009. Canadian guidelines for cardiac rehabilitation and cardiovascular disease prevention: Translating knowledge into action. Available from: http://www.cacr.ca/resources/guidelines.cfm. [Google Scholar]
- 16.ProQuest. RefWorks - COS. 2001 [Google Scholar]
- 17.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm2009.
- 18.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brozek J, Oxman A, Schünemann H. GRADEpro. 2008. 3.2 for Windows. [Google Scholar]
- 20.Review Manager (RevMan) Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2008. 5.0. [Google Scholar]
- 21.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Education and Debate. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.First MB, Spitzer RL, Gibbon M, Williams J. Structured clinical interview for DSM-IV axis I disorders-Patient edition (SCID-I/P, version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 24.Carney R, Rich M, Tevelde A, Saini J, Clark K, Jaffe A. Major depressive disorder in coronary artery disease. Am J Cardiol. 1987;60:1273. doi: 10.1016/0002-9149(87)90607-2. [DOI] [PubMed] [Google Scholar]
- 25.Albus C, De Backer G, Bages N, Deter HC, Herrmann-Lingen C, Oldenburg B, Sans S, Schneiderman N, Williams RB, Orth-Gomer K. Psychosocial factors in coronary heart disease --scientific evidence and recommendations for clinical practice. Gesundheitswesen. 2005;67:1–8. doi: 10.1055/s-2004-813907. [DOI] [PubMed] [Google Scholar]
- 26.Carney RM, Blumenthal JA, Catellier D, Freedland KE, Berkman LF, Watkins LL, Czajkowski SM, Hayano J, Jaffe AS. Depression as a risk factor for mortality after acute myocardial infarction. Am J Cardiol. 2003;92:1277–1281. doi: 10.1016/j.amjcard.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 27.Thombs BD, de Jonge P, Coyne JC, Whooley MA, Frasure-Smith N, Mitchell AJ, Zuidersma M, Eze-Nliam C, Lima BB, Smith CG, Soderlund K, Ziegelstein RC. Depression screening and patient outcomes in cardiovascular care: A systematic review. JAMA. 2008;300:2161–2171. doi: 10.1001/jama.2008.667. [DOI] [PubMed] [Google Scholar]
- 28.Hackett ML, Yappa C, Parag V, Anderson CS. Frequency of depression after stroke: A systematic review of observational studies. Stroke. 2005;36:1330–1340. doi: 10.1161/01.STR.0000165928.19135.35. [DOI] [PubMed] [Google Scholar]
- 29.Poynter B, Shuman M, Diaz-Granados N, Kapral M, Grace SL, Stewart DE. Sex differences in the prevalence of post-stroke depression: A systematic review. Psychosomatics. 2009;50:563–569. doi: 10.1176/appi.psy.50.6.563. [DOI] [PubMed] [Google Scholar]
- 30.Miller S, Lo C, Gagliese L, Hales S, Rydall A, Zimmermann C, Li M, Rodin G. Patterns of depression in cancer patients: An indirect test of gender-specific vulnerabilities to depression. Soc Psychiatry Psychiatr Epidemiol. 2010 doi: 10.1007/s00127-010-0246-7. [DOI] [PubMed] [Google Scholar]
- 31.Lichtman JH, Bigger JT, Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, American Heart Association Council on Clinical Cardiology, American Heart Association Council on Epidemiology and Prevention American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research, American Psychiatric Association. . Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 32.Davidson KW, Kupfer DJ, Bigger JT, Califf RM, Carney RM, Coyne JC, Czajkowski SM, Frank E, Frasure-Smith N, Freedland KE, Froelicher ES, Glassman AH, Katon WJ, Kaufmann PG, Kessler RC, Kraemer HC, Krishnan KR, Lesperance F, Rieckmann N, Sheps DS, Suls JM National Heart, Lung, and Blood Institute Working Group. Assessment and treatment of depression in patients with cardiovascular disease: National Heart, Lung, and Blood Institute Working Group Report. Psychosom Med. 2006;68:645–650. doi: 10.1097/01.psy.0000233233.48738.22. [DOI] [PubMed] [Google Scholar]
- 33.Thombs BD, Magyar-Russell G, Bass EB, Stewart KJ, Tsilidis KK, Bush DE, Fauerbach JA, McCann UD, Ziegelstein RC. Performance characteristics of depression screening instruments in survivors of acute myocardial infarction: Review of the evidence. Psychosomatics. 2007;48:185. doi: 10.1176/appi.psy.48.3.185. [DOI] [PubMed] [Google Scholar]
- 34.Carney RM, Blumenthal JA, Freedland KE, Youngblood M, Veith RC, Burg MM, Cornell C, Saab PG, Kaufmann PG, Czajkowski SM, Jaffe AS ENRICHD Investigators. . Depression and late mortality after myocardial infarction in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study. Psychosom Med. 2004;66:466–474. doi: 10.1097/01.psy.0000133362.75075.a6. [DOI] [PubMed] [Google Scholar]
- 35.Frasure-Smith N, Lesperance F, Prince RH, Verrier P, Garber RA, Juneau M, Wolfson C, Bourassa MG. Randomised trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. Lancet. 1997;350:473–479. doi: 10.1016/S0140-6736(97)02142-9. [DOI] [PubMed] [Google Scholar]
- 36.Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, Czajkowski SM, DeBusk R, Hosking J, Jaffe A, Kaufmann PG, Mitchell P, Norman J, Powell LH, Raczynski JM, Schneiderman N Enhancing Recovery in Coronary Heart Disease Patients Investigators (ENRICHD). . Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]