Abstract
Purpose
When surgeons disagree about the role of surgery, patient values and preferences should drive decision-making, but there is evidence that surgeon preferences have substantial influence. Surgeon preferences may relate to surgeon personality. Our primary null hypothesis is that specific personality characteristics (work styles) are not associated with the recommendation for operative treatment accounting for surgeon demographics.
Patients and Methods
We invited members of the Science of Variation Group to assess images of 15 upper extremity injuries with debatable indications for surgery, recommended operative or non-operative treatment, and grade their confidence in this decision (n = 270); subsequently, participants completed the validated Octogram Work and Leadership Style Test (n = 223). We selected injuries that could be treated either operatively or non-operatively including fractures of the clavicle, scapula, humerus, and radius fractures, and proximal and distal bicep ruptures.
Results
A higher proportion of recommendations for surgery was independently associated with a higher Octogram test pioneer score (β regression coefficient [β] 0.0054, partial R2 0.065, 95 % confidence interval [CI] 0.0027–0.0080, P < 0.001) and practice location outside North America and Europe (β 0.13, partial R2 0.079, 95% CI 0.073–0.020, P < 0.001) (adjusted R2 0.12, P < 0.001). No work styles were associated with more confidence in treatment.
Conclusions
A recommendation for discretionary surgery for musculoskeletal injury was related to surgeon personality. Surgeon self-awareness of how their work style can influence their recommendations might make them more receptive to techniques that ensure patient values have more influence than surgeon preferences on treatment decisions.
Electronic supplementary material
The online version of this article (doi:10.1007/s11552-015-9755-x) contains supplementary material, which is available to authorized users.
Keywords: Practice variation, Surgical decision-making, Work style
Introduction
There is substantial, largely unexplained, variation in the rate of surgery from surgeon to surgeon [2, 18, 19]. The study of unexplained variation and how to reduce it contributed to improved quality, safety, and resourcefulness in other fields [5], and many see the same potential in medicine [1, 2].
Disparity in illness burden and patient attitudes about medical intervention explain a small amount of the variation. Evidence suggests that surgical variation results mainly from differences in physician beliefs and variation in the extent to which patient preferences are incorporated into treatment decisions [2]. Physician beliefs seem related in part to training [7] and in part to personality characteristics, but we need more data. For instance, one study linked surgeon attitudes to readmission and reoperation rates [10].
Many conditions in orthopedic surgery can be treated with or without surgery. The likelihood a patient will choose surgery seems strongly related to the recommendations of their surgeon. Surgeons may not be aware of the influence they have on this decision, and they may not be aware of their reasons for their preferences. Incorporating patient preferences leads to more informed values-based choices and improved patient-practitioner communication [16]. Evidence that surgeon personality affects treatment recommendations might make surgeons more receptive to techniques that ensure patient values have more influence than surgeon preferences on treatment decisions.
Our primary null hypothesis is that specific work styles are not associated with the decision to operate accounting for surgeon demographics. Secondarily, we addressed [2] the influence of work style on surgeon confidence about their recommended treatment; and [18] the difference in confidence between surgeons recommending surgery or non-operative treatment.
Materials and Methods
Study Design
After the institutional review board approval, we approached 691 members of the Science of Variation Group of whom 270 (39 %) participated in this cross-sectional survey. This does not represent a response rate per se, because many of the surgeons we email do not regularly participate, and the email addresses have not been confirmed. Invitations were sent on June 6th 2014, followed by two reminders after 2 and 4 weeks to those who had not yet responded. The Science of Variation Group is an international collaboration of upper extremity surgeons that studies variation in the definition, interpretation, classification, and treatment of human illness. Acknowledgment, scientific curiosity, and camaraderie are the only incentives for participation.
Our survey was developed in an online survey tool (SurveyMonkey, Palo Alto, CA, USA) and consisted of 15 anonymized cases followed by a personality work style test. Cases consisted of a descriptive diagnosis (e.g., distal radius fracture), illustrated by one or two photos, radiographs, or 3D fracture reconstructions (Appendix 1), without additional patient information. We selected cases that could be treated either operatively or non-operatively including fractures of the clavicle, scapula, humerus, and radius fractures, and proximal and distal biceps ruptures (Table 1). Participants were asked: “What treatment do you recommend?” They had to choose either operative or non-operative. We calculated the proportion of cases treated operatively. We also asked participants: “How confident are you about this decision?” Confidence was graded on an 11-point ordinal scale, ranging from 0 (not at all confident) to 10 (very confident).
Table 1.
Proportion of operative versus non-operative treatment and confidence in treatment choice n = 270
| Case | Description | Operative treatment % (number) | Non-operative treatment % (number) | Mean confidence in treatment if chosen surgery ± SD | Mean confidence in treatment if chosen non-operative ± SD | P valuea |
|---|---|---|---|---|---|---|
| 1 | Displaced clavicle shaft fracture | 45 % (121) | 55 % (149) | 7.4 ± 2.0 | 7.6 ± 1.8 | 0.55 |
| 2 | Displaced lateral clavicle fracture | 70 % (188) | 30 % (82) | 8.0 ± 1.8 | 6.7 ± 1.8 | <0.001 |
| 3 | Displaced acromioclavicular joint dislocation | 17 % (47) | 83 % (223) | 7.6 ± 2.3 | 7.9 ± 2.2 | 0.37 |
| 4 | Acromion fracture | 50 % (134) | 50 % (136) | 7.3 ± 2.0 | 6.3 ± 2.2 | <0.001 |
| 5 | Coracoid fracture | 40 % (107) | 60 % (163) | 6.8 ± 2.2 | 6.5 ± 2.4 | 0.42 |
| 6 | Glenoid fracture | 37 % (100) | 63 % (170) | 7.8 ± 1.8 | 7.4 ± 1.9 | 0.068 |
| 7 | Proximal humerus surgical neck fracture | 78 % (210) | 22 % (60) | 8.1 ± 1.7 | 6.5 ± 1.7 | <0.001 |
| 8 | Proximal humerus greater tuberosity fracture | 13 % (36) | 87 % (234) | 7.6 ± 1.8 | 7.9 ± 1.8 | 0.32 |
| 9 | Proximal humerus valgus impacted fracture | 40 % (107) | 60 % (163) | 7.5 ± 1.8 | 7.3 ± 1.8 | 0.36 |
| 10 | Proximal diaphyseal humerus fracture | 34 % (91) | 66 % (179) | 7.6 ± 1.8 | 7.2 ± 1.7 | 0.086 |
| 11 | Proximal bicep rupture | 20 % (54) | 80 % (216) | 7.1 ± 1.9 | 7.8 ± 2.1 | 0.018 |
| 12 | Distal diaphyseal humerus fracture | 71 % (192) | 29 % (78) | 8.2 ± 1.6 | 7.1 ± 2.0 | <0.001 |
| 13 | Distal bicep rupture | 87 % (235) | 13 % (35) | 8.0 ± 1.9 | 6.3 ± 2.5 | <0.001 |
| 14 | Distal radius fracture (1) | 53 % (143) | 47 % (127) | 8.1 ± 1.8 | 7.2 ± 1.9 | <0.001 |
| 15 | Distal radius fracture (2) | 38 % (103) | 62 % (167) | 7.6 ± 1.9 | 7.8 ± 2.0 | 0.45 |
Confidence is on a scale between 0 (no confidence) and 10 (completely confident)
a Italicized indicates significant difference in confidence
SD standard deviation
After rating all cases, participants were directed to a separate website where they completed the Octogram Work and Leadership Style Test (short: Octogram test [Online Talent Manager, Breda, The Netherlands]).
Work Style Test
The Octogram Work and Leadership Style Test is a validated survey that focuses on the personality traits that drive behavior in the workplace [12]. Previously, Quinn and Rohrbaugh described that the aspects of effective company management are contradicting to one another (focus on flexibility versus control; individual employees versus the overall organization); they coined this as the “competing values framework” [15]. From this framework flowed eight fundamental management roles [14]. The Octogram test is designed to identify the eight work styles that underpin the competing values framework and its roles. This model groups two related styles within each of the four quadrants identified in the competing values framework; contradicting styles are placed opposite one another. Styles measured are [2] pioneer and [18] networker, [19] achiever and [5] strategist, [1] anchor and [7] analyst, and [10] team player and [16] helper (Fig. 1) [13].
Fig. 1.
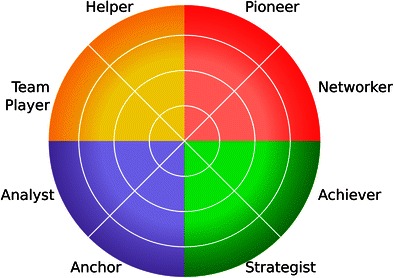
Graphical depiction of the Octogram with its eight work styles
The Octogram test consists of 36 questions asking the participant to rank four statements about their own behavior at work from most to least applicable. Each statement is linked to one of eight work styles. The statement that ranked first, adds four points to its related style; the statement that ranked second, adds three points; and so on, resulting in a possible score ranging from 18 to 72 per work style. All items within each of the eight traits have a Cronbach’s alpha score higher than 0.70 with the trait they measure [12].
Study Population
Among the 270 surgeons that completed the survey, 223 (83 %) also completed the Octogram test. Nine percent (22 of 270) were women, and the majority practiced in North America (51 % [138 of 270]) and Europe (34 % [92 of 270]). The majority supervised trainees (88 % [237 of 270]) (Table 2).
Table 2.
Baseline characteristics of participants
| Characteristics | Percentage (number) n = 270 |
|---|---|
| Women | 8.5 % (23) |
| Practice location | |
| North America | 51 % (138) |
| Europe | 34 % (92) |
| Other | 15 % (40) |
| Practice years | |
| 0–5 | 37 % (99) |
| 6–10 | 21 % (57) |
| 11–20 | 26 % (71) |
| 20–30 | 16 % (43) |
| Supervise trainees | 88 % (237) |
| Specialization | |
| General | 6.3 % (17) |
| Traumatology | 35 % (95) |
| Shoulder-elbow | 17 % (47) |
| Hand-wrist | 34 % (93) |
| Other | 2.6 % (7) |
| Resident | 4.1 % (11) |
| Work styles | Mean ± standard deviation (range) n = 223 |
| Pioneer | 40 ± 7.6 (24–62) |
| Networker | 34 ± 7.4 (18–59) |
| Achiever | 47 ± 8.8 (25–69) |
| Strategist | 48 ± 7.1 (29–63) |
| Anchor | 50 ± 8.1 (26–67) |
| Analyst | 53 ± 7.4 (28–68) |
| Team player | 44 ± 9.5 (23–66) |
| Helper | 45 ± 8.3 (27–63) |
The mean proportion of cases treated operatively was 0.46 (standard deviation ±0.17, range 0–0.87). Mean confidence score in the selected treatment was 7.5 (±1.1, range 2–9.7).
Statistical Analysis
We used frequencies to describe discrete variables; continuous variables are reported as means and standard deviations. To identify independent predictors for surgery and confidence, we performed two stepwise, backwards, multivariable linear regression analyses for all bivariate analyses (Appendix 2) with P < 0.10, after changing all categorical values into dummy variables with the first variable exempted from analysis. Multivariable analyses only included participants who rated all cases and completed the Octogram test. A P value < 0.05 was considered significant. Distribution of the data was assessed by visual inspection of histograms; subsequently, on bivariate analysis, we compared continuous and discrete variables by Student’s t test or one-way analysis of variance; two continuous variables are compared by Pearson correlation.
A priori power analysis indicated that a sample of 215 participants would provide 90 % statistical power with α = 0.05 for an effect size and f2 = 0.10 for regressions with ten main predictors.
Results
Accounting for potential interaction of variables using multivariable analysis, a higher proportion of recommendations for surgery was independently associated with a higher pioneer score (β regression coefficient [β] 0.0054, partial R2 0.065, 95 % confidence interval [CI] 0.0027–0.0080, P < 0.001) and practice location outside North America and Europe (β 0.13, partial R2 0.079, 95 % CI 0.073–0.020, P < 0.001) (adjusted R2 0.12, P < 0.001). The β regression coefficient indicates that a 1-point increase in pioneer score results in an average increase of 0.54 % recommending surgical treatment; the proportion of cases treated surgically differs 0.29 between highest and lowest possible pioneer scores. Practicing outside North America and Europe results in a 0.13 increase in recommending surgical treatment, as compared to practicing within the United States (Table 3).
Table 3.
Multivariable analyses of factors associated with operative treatment and confidence in recommended treatment
| Variable | β Regression coefficient (95 % confidence interval) | Standard error | P value | Partial R 2 | Adjusted R 2 |
|---|---|---|---|---|---|
| Operative treatment | |||||
| Pioneer | 0.0054 (0.0027–0.0080) | 0.0014 | <0.001 | 0.065 | 0.12 |
| Practice location outside United States and Europea | 0.13 (0.073–0.20) | 0.031 | <0.001 | 0.079 | |
| Confidence in recommended treatment | |||||
| Practice location outside United States and Europea | 0.75 (0.38–1.1) | 0.19 | <0.001 | 0.058 | 0.077 |
| Practice years: 11–20b | 0.41 (0.11–0.70) | 0.15 | 0.007 | 0.027 | |
Italicized indicates statistically significant association
aAs compared to surgeons practicing within the United States
bAs compared to surgeons 0–5 years in practice
No work styles were associated with more confidence in treatment. Accounting for interaction between variables in multivariable analysis, confidence in treatment was independently associated with practice location outside North America and Europe (β 0.75, partial R2 0.058, 95 % CI 0.38–1.1, P < 0.001) and 11–20 years in practice (β 0.41, partial R2 0.027, 95 % CI 0.11–0.70, P = 0.007) (adjusted R2 0.077, P < 0.001). This indicates that a surgeon practicing outside North America and Europe on average has a 0.75-point higher confidence score than someone practicing within the United States. Surgeons practicing 11–20 years on average have a 0.41-point higher confidence score than surgeons practicing 0–5 years (Table 3).
With the exception of a proximal biceps rupture, practitioners selecting surgery had equal (n = 8) or more confidence (n = 6) in their decision than surgeons selecting non-operative treatment. Average confidence per injury ranged between 6.3 ± 2.2 and 7.9 ± 1.8 for non-operative treatment and between 6.8 ± 2.2 and 8.2 ± 1.6 when surgery was recommended (Table 1).
Discussion
There is substantial unexplained variation in rates of orthopedic surgery by surgeon [2, 18, 19]. Practice variation is related to increased healthcare cost [1]. Evidence suggests that surgical variation in part results from differences in physician beliefs values and preferences [2]. This variation may relate in part to surgeon personality. We found a higher pioneer score to be associated with a higher rate of surgery.
This study has some limitations. Personality and attitudes are complex and difficult to capture in a single test; we only measured one part of personality, namely working style. The group of surgeons that participated may not be representative of the average surgeon. In particular, the group of surgeons that are neither American nor European was small, and the observed differences might be spurious.
A higher pioneer score is associated with innovation and creativity. But trying out new things also implies the tendency to accept a certain level of risk. New ideas and methods are often more likely to fail than established practice, and often times, surgery carries more risk than non-operative treatment. The tendency of surgeons with a higher pioneer score to accept a higher level of risk, might explain why they are more likely to recommend surgery. In aviation, pilots with a more cautious work style (agreeing with “I am a very careful pilot” and “I am a very cautious pilot”) had a lower risk of future accidents [9]. One previous study on hazardous attitudes among orthopedic surgeons found that higher macho attitude level—feeling the need to demonstrate superior ability [3]—explained 19 % of the variation in readmission and reoperation rate [10].
Previous work found a large variation in practice within the United States and United Kingdom [11, 17]. In our study, surgeons practicing outside Europe and North America differed in their recommendation for treatment and were more likely to recommend surgery.
Work styles measured by the Octogram Test were not associated with confidence in the recommended treatment. Previous study linked experience and being married to increased confidence in surgery trainees [4]. We found a slightly higher confidence score for surgeons 11–20 years in practice, but it is not clear how to interpret this finding, and it only explains a small amount of variation in confidence. As previous research linked higher confidence with increased job satisfaction in trauma surgeons [6], factors associated with confidence and their effect on treatment recommendation warrant additional study.
We found no difference in average confidence in a recommendation for surgery compared to a recommendation for non-operative treatment in eight of the 15 cases. Surgeons recommending opposite treatments can be equally confident about their decision.
Orthopedic surgeons tend to assume that variations in treatment are associated with variations in pathophysiology, and that patients with more advanced disease will seek more care. Our study builds on growing evidence that the decision for surgery is in part related to variations among surgeons’ preferences, which relates in part to their work style. Patients, on average, prefer to take the lead in medical decision-making [8], and achieving this leads to more informed values-based choices, and improved patient-practitioner communication [16]. Surgeon self-awareness of how their work style can influence their recommendations might help increase the adoption of methods designed to help the patient determine their preferences and values and remain involved in decision-making.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 4217 kb)
(PDF 89.7 kb)
Acknowledgments
We would like to thank Richard Still for his logistical support and the members of the Science of Variation Group: A.B.. Spoor, A. Chauhan, A. Shrivastava, A.L. Wahegaonkar, A.B.. Shafritz, A. Marcus, A.L. Terrono, A.S. Neviaser, A. Schmidt, A. Barquet, A. Kristan, T. Apard, A. Berner, A.K. Shyam, A. Ilyas, A.D. Mazzocca, A. Jubel, F.S.B. Batista, B.E. Kreis, G.C. Babis, B.W. Sears, B.F. Hearon, B.M. Nolan, B.A. Palmer, B.D. Crist, B.J. Cross, B.P.D. Wills, C. Ekholm, C. Swigart, C. Spath, C. Dario Oliveira Miranda, C. Zalavras, C. Cassidy, C.J. Wall, C.J. Walsh, C.M. Jones, C. Garnavos, C. Kleweno, C.L. Moreno-Serrano, C. Rodner, D.F.P. van Deurzen, D.A. Osei, D. Haverkamp, D. Polatsch, D. Beingessner, D.L. Nelson, D.M. Kalainov, D. Mercer, D. Eygendaal, D.M. McKee, D.O.F. Verbeek, M. Patel, G. Gradl, D. Brilej, E.T. Walbeehm, E. Harvey, E. Bonatz, E. Grosso, E. Stojkovska Pemovska, E. Hofmeister, E. Mark Hammerberg, E.D. Schumer, F.T.D. Kaplan, F. Suarez, C.H. Fernandes, E. Forigua Jaime, F.L. Walter, F. Frihagen, G. Gadbled, G.M. Pess, G.M. Huemer, G. Kontakis, G.S.M. Dyer, G. Kohut, G. R. Hernandez, G. Porcellini, G. Garrigues, G.J. Bayne, G. Merrell, G. DeSilva, H.B. Bamberger, H.W. Grunwald, H. Goost, H. Broekhuyse, H.L. Kimball, H. Durchholz, H. van der Heide, I. McGraw, I. Harris, J. Carel Goslings, J. Choueka, J. Ahn, J.S. Huntley, J. Abrams, J. Wint, J. Moriatis Wolf, J.I. Huang, J. Moreta-Suarez, J.N. Doornberg, J. Murachovsky, J.H. Scheer, J. Itamura, J. McAuliffe, J.T. Capo, J.L. Hobby, J.G. Boretto, J. Rubio, J.A. Ortiz, J.E. Grandi Ribeiro Filho, J. Abboud, J.M. Conflitti, J. Dines, J.M. Abzug, J.M. PatiÒo, J. Adams, J. Bishop, K. Kabir, K. Chivers, K. Zyto, K. Egol, K.J. Malone, K.M. Rumball, K.J. Ponsen, K. Dickson, K. Jeray, L.M.S.J. Poelhekke, L.A.B.. Campinhos, L. Mica, L.C. Borris, L.E. Adolfsson, L. Weiss, L.M. Schulte, L. Paz, L. Taitsman, L. Guenter, L. Catalano III, M. Waseem, M. Jason Palmer, M.A.M. Mulders, M.R. Krijnen, M.A.J. van de Sande, M.W.G.A. Bronkhorst, M.I. Abdel-Ghany, M.J. Richard, M. Rizzo, M. Oidtmann, M. Pirpiris, M. Di Micoli, M. Bonczar, M. Boyer, M. Richardson, M. Mormino, M. Menon, M. Calcagni, M. Beaumont-Courteau, M.M. Wood, S.A. Meylaerts, M. Baskies, M. Behrman, M.E. Miller, M.H. Amini, M. Nancollas, M. Prayson, M. Quinn, M.W. Grafe, M.W. Kessler, M.P.J. van den Bekerom, M. Ruiz-Suarez, M. Mckee, M. Merchant, M. Tyllianakis, M. Shafi, N.L. Shortt, N. Escobar Luis Felipe, N. Hoekzema, N.C. Chen, N. Saran, N. Wilson, N. Elias, N.M. Akabudike, N. van Dijk, N. Schep, N.W. Gummerson, N.G. Lasanianos, N.K. Kanakaris, O. Brink, O.M. Semenkin, P.V. van Eerten, P. Melvanki, P.W. Owens, P.A. Martineau, P. Althausen, P. Hahn, P. Kloen, P.R.G. Brink, P. Schandelmaier, P. Dantuluri, P. Andreas, P. Inna, Q. Wang, M. Quell, R.G. Gaston, R.W. Peters, R. Mohd Ramli, R.M. Costanzo, R. de Bedout, A.S. Ranade, R.H. Babst, R. Buckley, R. Jenkinson, R.L. Hutchison, R.S. Gilbert, R.S. Page, R. Papandrea, R.D. Zura, R.R. Slater, R.R.L. Gray, R. Pesantez, R. Liem, R.P. Calfee, S.H. van Helden, S. Moghtaderi, S. Mehta, S. Bouaicha, S. Spruijt, S. Kakar, S.F. Duncan, S.G. Kaar, S. Rowinski, S. Dodds, S.A. Kennedy, S. Kronlage, S. Petersen, S.J. Hattrup, G.S.I. Sulkers, T. Schepers, T.G. Guitton, T. Gosens, T. Baxamusa, C. Taleb, T. Tosounidis, T. Begue, T. DeCoster, T. Dienstknecht, T.F. Varecka, T. Higgins, T. Mittlmeier, T. Wright, T.J. Fischer, T. Omara, T.A. Schubkegel, T. Siff, T. Havlicek, T.M. McLaurin, V. Neuhaus, V.J. Sabesan, V.S. Nikolaou, M. Verhofstad, V. Philippe, V. Giordano, A.J.H. Vochteloo, W.A. Batson, W.C. Hammert, W.D. Belangero, W. Satora, Y. Weil, J.F. Nappi, K. Eng, and M. Swiontkowski.
Sources of Funding
No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
Conflict of Interest
Bert Goos is developer of the Octogram personality test used in this study and chief executive officer of Online Talent Manager, the company that provided the test.
David Ring certifies that he, or a member of his immediate family, has or may receive payments or benefits during the study period from Wright Medical (USD less than 10,000) (Memphis, TN, USA); Skeletal Dynamics (USD less than 10,000) (Miami, FL, USA); Biomet (USD less than 10,000) (Warsaw, IN, USA); AO North America (USD less than 10,000) (Paoli, PA, USA); and AO International (USD less than 10,000) (Dubendorf, Switzerland).
Teun Teunis declares that he has no conflict of interest.
Stein J Janssen declares that he has no conflict of interest.
Theirry Guitton declares that he has no conflict of interest.
Ana-Maria Vranceanu declares that she has no conflict of interest.
Statement of Human and Animal Rights
The work was performed at the Massachusetts General Hospital—Harvard Medical School. This study is approved by our institutional review board and is conducted in accordance with the Helsinki Declaration of 1975, as revised in 2000.
Statement of Informed Consent
Informed consent is not applicable to this study design as participants of the SOVG signed up for such projects.
Contributor Information
Teun Teunis, Email: teunteunis@gmail.com.
Stein J. Janssen, Email: steinjanssen@gmail.com
Thierry G. Guitton, Email: guitton@gmail.com
Ana-Maria Vranceanu, Email: avranceanu@mgh.harvard.edu.
Bert Goos, Email: b.goos@onlinetalentmanager.com.
David Ring, Phone: 617-726-4700, Email: dring@mgh.harvard.edu.
References
- 1.Becker SJ, Teunis T, Blauth J, et al. Medical services and associated costs vary widely among surgeons treating patients with hand osteoarthritis. Clinical orthopaedics and related research. 2014. [DOI] [PMC free article] [PubMed]
- 2.Birkmeyer JD, Reames BN, McCulloch P, et al. Understanding of regional variation in the use of surgery. Lancet. 2013;382(9898):1121–1129. doi: 10.1016/S0140-6736(13)61215-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buch G, Diehl A. An investigation of the effectiveness of pilot judgement training. Hum Factors. 1984;26:557–564. [Google Scholar]
- 4.Bucholz EM, Sue GR, Yeo H, et al. Our trainees’ confidence: results from a national survey of 4136 US general surgery residents. Arch Surg. 2011;146(8):907–914. doi: 10.1001/archsurg.2011.178. [DOI] [PubMed] [Google Scholar]
- 5.Escalante EJ. Quality and productivity improvement: a study of variation and defects in manufacturing. Qual Eng. 1999;11(3):427–442. doi: 10.1080/08982119908919259. [DOI] [Google Scholar]
- 6.Foulkrod KH, Field C, Brown CV. Trauma surgeon personality and job satisfaction: results from a national survey. Am Surg. 2010;76(4):422–427. doi: 10.1177/000313481007600422. [DOI] [PubMed] [Google Scholar]
- 7.Hageman MG, Guitton TG, Ring D, et al. How surgeons make decisions when the evidence is inconclusive. J Hand Surg. 2013;38(6):1202–1208. doi: 10.1016/j.jhsa.2013.02.032. [DOI] [PubMed] [Google Scholar]
- 8.Hageman MG, Kinaci A, Ju K, et al. Carpal tunnel syndrome: assessment of surgeon and patient preferences and priorities for decision-making. J Hand Surg. 2014;39(9):1799–1804. doi: 10.1016/j.jhsa.2014.05.035. [DOI] [PubMed] [Google Scholar]
- 9.Hunter DR. Retrospective and prospective validity of aircraft accident risk indicators. Hum Factors. 2001;43:509–518. doi: 10.1518/001872001775870412. [DOI] [PubMed] [Google Scholar]
- 10.Kadzielski J, McCormick F, Herndon JH, et al. Surgeons’ attitudes are associated with reoperation and readmission rates. Clinical orthopaedics and related research. 2014. [DOI] [PMC free article] [PubMed]
- 11.NHS Atlas of Variation in Healthcare. 2010; http://www.rightcare.nhs.uk/atlas/qipp_nhsAtlas-LOW_261110c.pdf. Accessed 02-26-2014.
- 12.Online Talent Manager. Octogram work and leadership style test—validation. 2015; http://www.octogram.net/en/validity. Accessed 01-17-2015.
- 13.OTM Education. The octogram work and leadership style test. 2013; https://www.youtube.com/watch?v=q625ZCzvsFg. Accessed 07-30-2014.
- 14.Quinn RE. Mastering the paradoxes and competing demands of high performance. San Francisco: Jossey-Bass; 1988. [Google Scholar]
- 15.Quinn RE, Rohrbaugh J. A competing values approach to organizational effectiveness. Public Product Rev. 1981;5(2):122–140. doi: 10.2307/3380029. [DOI] [Google Scholar]
- 16.Stacey D, Legare F, Col NF, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Data Syst Rev. 2014;1:CD001431. doi: 10.1002/14651858.CD001431.pub4. [DOI] [PubMed] [Google Scholar]
- 17.The Dartmouth atlas of healthcare. 2014; http://www.dartmouthatlas.org/. Accessed 02-26-2014.
- 18.Zhang Y, Baicker K, Newhouse JP. Geographic variation in medicare drug spending. N Engl J Med. 2010;363(5):405–409. doi: 10.1056/NEJMp1004872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y, Baicker K, Newhouse JP. Geographic variation in the quality of prescribing. N Engl J Med. 2010;363(21):1985–1988. doi: 10.1056/NEJMp1010220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 4217 kb)
(PDF 89.7 kb)


