Deep brain stimulation (DBS) is a promising technique for modulating circuits underlying mental illnesses, but has not done well in clinical trials (Dougherty et al, 2015). Advocates have argued that the trial failures arise from a need to better define the anatomic target for stimulation (Riva-Posse et al, 2014). This ignores a larger issue: DBS is an open-loop, static therapy. Patients' disorders, on the other hand, are not static. Symptoms change over hours to days, but DBS programming visits occur every 4–12 weeks. To resolve that mismatch, investigators are now pursuing ‘closed-loop' DBS, where the device itself monitors patients' brain activity and self-titrates therapy to a desired endpoint (Figure 1). The challenge, however, is determining what to monitor. Verified neural biomarkers for psychiatric disorders remain elusive. Preliminary data suggest candidate markers (Widge et al, 2015), but they are far from the real-time algorithms needed for effective feedback-controlled DBS.
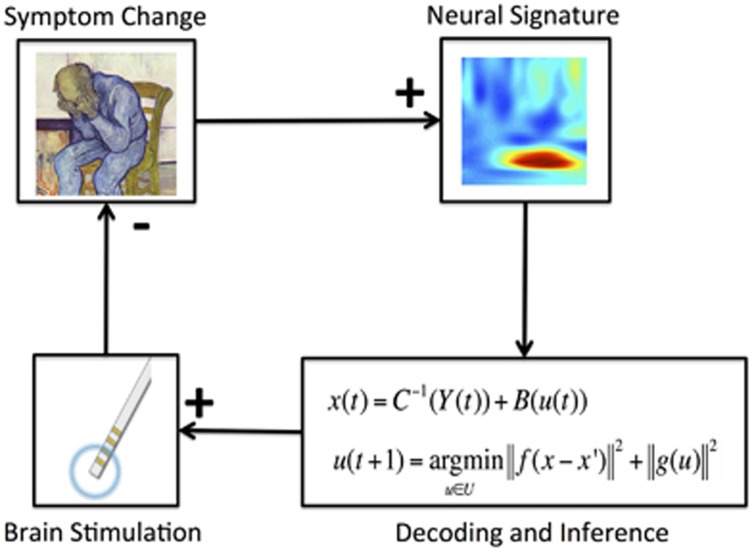
Figure 1.
Schematic of closed-loop DBS control. A change in psychiatric symptoms (likely a dimensional construct such as negative mood, over-generalized fear or hyper-arousal) leads to a stereotyped change in neural activity. This is detected by a neural decoding algorithm, which automatically adjusts brain stimulation parameters according to a pre-defined transfer function. The resulting change decreases the symptom level, which stabilizes the system in a homeostatic loop.
A different neuroscience community has had greater success in ‘reading out' the brain: brain–computer interface (BCI) researchers. Their technologies ‘decode' movement signals from the cortex, then convey movement goals to assistive devices. Closed-loop DBS researchers seek to do something similar, decoding a patient's emotional state. BCI investigators have uncovered two insights that could assist psychiatry's quest. First, encoding matters—decoding is better with a robust model of how cortical regions encode mental states. This matters for psychiatry, because disorders like depression and post-traumatic stress disorder are heterogeneous. Effective decoding may require identification of discrete circuit-based endophenotypes, analogous to research domain criteria constructs. For instance, preliminary data suggest that DBS response at the ventral striatum target may depend on changes in fronto-cingulate activity evoked by Stroop-like tasks (Widge et al, 2015). This cross-diagnostic approach may be broadly useful in dissecting DBS' mechanisms of action.
Second, neural plasticity can help. A recent surprise from BCI studies is that models are helpful, but not always necessary. A motivated subject can learn to skillfully control a prosthetic limb or an internal neurostimulator, even if the mapping between neural firing and device behavior does not match ‘natural' input–output relationships. As the user trains with the BCI, the brain re-maps its firing patterns to match the device's control scheme (Moritz and Fetz, 2011). In effect, the decoded patterns become a readout of the user's intention—what he/she wants the device to do at that moment. For a prosthetic limb, this is an instantaneous motion command. For psychiatry, it would be a stimulator command. For instance, one could place a recording electrode in an area that contains emotion-related signals, then link the amplitude of a DBS intervention to the intention-modulated signals in that area. The patient's signals in the recorded area would then ‘tune' the DBS intervention as needed. We recently showed that rodents can learn to use prefrontal cortex signals in precisely this fashion to activate DBS-like stimulation (Widge and Moritz, 2014). Similar strategies may be useful for modulating fear behaviors in anxiety disorders, using fronto-limbic networks as targets (Besnard and Sahay, 2015).
DBS remains an interesting technique, and closed-loop approaches may make it more useful for a broader group of patients. Despite recent clinical trial failures, the prospects for psychiatric DBS may be brighter than ever.
FUNDING AND DISCLOSURE
AS declares no conflict of interest. ASW is a named inventor on patent applications related to closed-loop techniques in psychiatric brain stimulation.
Acknowledgments
AS is supported by US National Institutes of Health Biobehavioral Research Awards for Innovative New Scientists (BRAINS) 1-R01MH104175, and the Ellison Medical Foundation New Scholar in Aging, Whitehall Foundation, Inscopix Decode and HSCI Development grants. ASW is supported by the Picower Family Foundation and the U.S. Army Research Office/Defense Advanced Research Projects Agency under Cooperative Agreement Number W911NF-14-2-0045.
References
- Besnard A, Sahay A (2015). Adult hippocampal neurogenesis, fear generalization, and stress. Neuropsychopharmacology (doi:10.1038/npp.2015.167; e-pub ahead of print). [DOI] [PMC free article] [PubMed]
- Dougherty DD, Rezai AR, Carpenter LL, Howland RH, Bhati MT, O'Reardon JP et al (2015). A randomized sham-controlled trial of deep brain stimulation of the ventral capsule/ventral striatum for chronic treatment-resistant depression. Biol Psychiatry 78: 240–248. [DOI] [PubMed] [Google Scholar]
- Moritz CT, Fetz EE (2011). Volitional control of single cortical neurons in a brain–machine interface. J Neural Eng 8: 025017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riva-Posse P, Choi KS, Holtzheimer PE, McIntyre CC, Gross RE, Chaturvedi A et al (2014). Defining critical white matter pathways mediating successful subcallosal cingulate deep brain stimulation for treatment-resistant depression. Biol Psychiatry 76: 963–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widge AS, Deckersbach T, Eskandar EN, Dougherty DD (2015). Deep brain stimulation for treatment-resistant psychiatric illnesses: what has gone wrong and what should we do next? Biol Psychiatry (doi:10.1016/j.biopsych.2015.06.005; e-pub ahead of print). [DOI] [PubMed]
- Widge AS, Moritz CT (2014). Pre-frontal control of closed-loop limbic neurostimulation by rodents using a brain-computer interface. J Neural Eng 11: 024001. [DOI] [PMC free article] [PubMed] [Google Scholar]