Abstract
On September 11, 2001, a terrorist attack occurred in the U.S. (9/11). Research on 9/11 and psychiatric outcomes has focused on individual disorders rather than the broader internalizing (INT) and externalizing (EXT) domains of psychopathology, leaving unknown whether direct and indirect 9/11 exposure differentially impacted these domains rather than individual disorders. Further, whether such effects were exacerbated by earlier childhood maltreatment (i.e. stress sensitization) is unknown. 18,713 participants from a U.S. national sample with no history of psychiatric disorders prior to 9/11 were assessed using a structured in-person interview. Structural equation modeling conducted in a sample who endorsed no psychiatric history prior to 9/11, indicated that indirect exposure to 9/11 (i.e. media, friends/family) was related to both EXT (alcohol, nicotine, and cannabis dependence, and antisocial personality disorder) and INT (major depression, generalized anxiety, and post-traumatic stress disorder (PTSD)) dimensions of psychopathology (EXT: β = 0.10, p < 0.001; INT: β = 0.11, p < 0.001) whereas direct exposure was associated with the INT dimension only (β = 0.11, p < 0.001). For individuals who had experienced childhood maltreatment, the risk for EXT and INT dimensions associated with 9/11 was exacerbated (Interactions: β = 0.06, p < 0.01; β = 0.07, p < 0.001, respectively). These findings indicate that 9/11 impacted latent liability to broad domains of psychopathology in the US general population rather than specific disorders with the exception of PTSD, which had independent effects beyond INT (as indicated by a significant (p < 0.05) improvement in modification indices). Findings also indicated that childhood maltreatment increases the risk associated with adult trauma exposure, providing further evidence for the concept of stress sensitization.
Keywords: 9/11, World Trade Center, Child abuse, Child neglect, Externalizing, Internalizing, Stress sensitization, Psychopathology, Substance use, NESARC
1. Introduction
On September 11, 2001, a large-scale terrorist attack occurred in New York City (9/11) (Galea et al., 2002). Since then, studies have linked 9/11 exposure to adverse psychological outcomes, including depression, anxiety, and substance use disorders (Breslau et al., 2010; Henriksen et al., 2010; Neria et al., 2011; Perlman et al., 2011; Lucchini et al., 2012). Individuals directly impacted by 9/11 have been studied in depth (Welch et al., 2012). However, most of the US population experienced 9/11 indirectly, through relatives, friends, or media exposure, e.g., television news (Dougall et al., 2005). Such indirect 9/11 exposures were also associated with depression, anxiety, and problem drinking, particularly in vulnerable groups, such as those with prior psychiatric disorders (Lengua et al., 2005; Pollack et al., 2006; Otto et al., 2007; Holman et al., 2011; Barnes et al., 2012; Pietrzak et al., 2012). However, many aspects of the associations between 9/11 exposures and psychological outcomes remain unknown. Outstanding issues involve the relationships between direct and indirect 9/11 exposure, their impact on broad underlying dimensions of psychopathology rather than specific individual disorders, and whether such relationships are altered by prior exposure to other well-documented risk factors such as childhood maltreatment or a history of parental mental illness.
Risk factors for one disorder tend to predispose individuals to other disorders (Kendler et al., 2003; Carr et al., 2013). The high comorbidity of substance and psychiatric disorders (Kessler et al., 1994; Compton et al., 2007; Hasin et al., 2007b) has been conceptualized as forming a meta-structure of broader internalizing and externalizing latent dimensions (Krueger et al., 2002; Kendler et al., 2003; Eaton et al., 2012; Krueger and Markon, 2014). In a US national sample, childhood maltreatment affected the risk for specific adult mood, anxiety, personality, and substance use disorders primarily through the broader internalizing and externalizing dimensions rather than impacting the risk for specific individual psychiatric disorders (Keyes et al., 2012). Further, in another US national sample, familial aggregation of mood, personality, and substance use disorders was explained by underlying vulnerabilities to internalizing and externalizing dimensions transmitted across generations (Kendler et al., 1997). However, up to now, 9/11 research has focused on individual disorders rather than the broader internalizing and externalizing dimensions, leaving unknown whether 9/11 effects are primarily through these domains, whether such effects differ between the internalizing or externalizing domains, and whether additional effects would be found for specific individual disorders. Further, differential effects on the internalizing and externalizing dimensions among those directly or indirectly exposed to 9/11 remain unknown. Addressing such questions is important not only to understanding 9/11 effects, but to building broader knowledge about the effects of large-scale traumatic events that affect major segments of the general population.
Incorporation of prior risk factors including negative childhood events (e.g., childhood maltreatment, parental psychopathology) can aid in building this understanding. Studies indicate that individuals who experience an earlier negative life event may be more sensitized to the effects of a subsequent trauma, and therefore more likely to develop mental health problems. This process has been termed stress sensitization (Van Winkel et al., 2008; Heim and Nemeroff, 2009; Pratchett and Yehuda, 2011). For example, several studies found that childhood maltreatment moderates the association between an adult traumatic event and adult psychopathology, such that those who experienced childhood maltreatment have more severe symptoms after later trauma than those who did not experience maltreatment (Keyes et al., 2014; Pratchett and Yehuda, 2011; Young-Wolff et al., 2012; van Winkel et al., 2013). However, stress sensitization has not been examined in the context of an unanticipated, mass traumatic event such as 9/11. Evidence that negative childhood experiences moderate risk associated with direct and indirect exposure to events such as 9/11 would assist in the identification of individuals at risk of adverse psychological outcomes, and provide further insight into the concept of stress sensitization.
We therefore investigated two research questions related to 9/11 exposure and subsequent psychiatric disorders in a sample of household residents in the US, the National Epidemiologic Study on Alcohol Related Conditions (NESARC). Our first goal was to examine the association between direct and indirect 9/11 exposure and post-9/11 onsets of psychopathology in the internalizing and externalizing dimensions of psychiatric and substance use disorders, prior to and after accounting for childhood maltreatment and/or parental history of mental illness (depression, alcohol or drug dependence, antisocial behavior). Our second goal was to investigate whether the experience of childhood maltreatment increased risk for externalizing and internalizing disorders associated with greater exposure to 9/11 (i.e. stress sensitization).
2. Methods
2.1. Study design and sample
NESARC is a survey of non-institutionalized US adults residing in homes or group quarters. NESARC data were collected at two time points: Wave 1 (2001–2002) with 43,093 participants and Wave 2 (2004–2005) with 34,653 of the original participants (cumulative Wave 2 response rate, 70.2%). Young, Black and Hispanic individuals were oversampled. Data were weighted to reflect the demographic characteristics of the US population based on the 2000 census (Grant et al., 2004; Grant et al., 2005). The research protocol, including written informed consent, received approval from the US Census Bureau and the US Office of Management and Budget. Further study details are described elsewhere (Grant et al., 2004; Grant et al., 2005; Ruan et al., 2008).
The present study included Wave 2 participants, as the Wave 2 interview included all relevant variables. Of the 34,653 participants assessed at Wave 2, 46.0% (N = 15,940) had a prior psychiatric diagnosis (lifetime), and were excluded from the present analyses. This was done so that we can specifically examine the lifetime onset of psychiatric symptoms following 9/11 exposure, versus the reoccurrence of prior lifetime psychiatric symptoms. The present analyses included 18,713 participants with no history of psychiatric disorders prior to 9/11. As shown in Table 1, participants were 58% female with an age range of 21–90 (Mean = 49.1, Standard Deviation (SD) = 17.3). White participants comprised 58.2% of the sample, African Americans 19.0%, Hispanics 18.4%, Asian or Pacific Islanders 2.8% and American Indians and Alaska Natives 1.7%.
Table 1.
Analytic sample characteristics by 9/11 exposure.
| 9/11 Exposure
| |||||
|---|---|---|---|---|---|
| All (Irrespective of 9/11 exposure) | No exposure (n = 7791) | Indirectly experienced (n = 25,239) | Close friend or relative directly experienced (n = 1241) | Directly experienced (n = 170) | |
| N (%) | |||||
| Sex | |||||
| Male | 14,564 (42.0) | 3133 (46.9) | 10,692 (47.9) | 555 (51.1) | 90 (61.0) |
| Female | 20,089 (58.0) | 4658 (53.1) | 14,547 (52.1) | 686 (48.9) | 80 (39.0) |
| Age | |||||
| 18–29 | 4913 (14.2) | 1036 (15.4) | 3633 (16.5) | 207 (19.6) | 24 (17.5) |
| 30–44 | 10,603 (30.6) | 2179 (27.7) | 7851 (30.0) | 443 (34.1) | 62 (33.9) |
| 45–64 | 11,960 (34.5) | 2484 (31.6) | 8863 (35.4) | 488 (37.6) | 65 (34.9) |
| 65+ | 7177 (20.7) | 2092 (25.3) | 4892 (18.1) | 103 (8.7) | 19 (13.8) |
| Race | |||||
| White, Non-Hispanic | 20,161 (58.2) | 3847 (63.0) | 15,368 (73.2) | 753 (72.9) | 87 (63.9) |
| Black, Non-Hispanic | 6587 (19.0) | 1954 (15.2) | 4331 (9.8) | 226 (12.0) | 41 (17.2) |
| Hispanic, any | 6359 (18.4) | 1654 (15.0) | 4429 (10.8) | 202 (8.9) | 30 (8.4) |
| American Indian, Alaska Native, Non-Hispanic | 578 (1.7) | 111 (2.0) | 442 (2.3) | 19 (1.4) | 0 (0.0) |
| Asian/Hawaiian/Other Pacific Islander, Non-Hispanic | 968 (2.8) | 225 (4.8) | 669 (4.0) | 41 (4.9) | 12 (10.5) |
2.2. Measures
Participants were interviewed in person with the Alcohol Use Disorder and Associated Disabilities Interview Schedule, DSM-IV version (AUDADIS-IV), a fully structured instrument designed for lay interviewers.
2.2.1. Outcomes
2.2.1.1. Psychiatric disorders
Psychiatric disorders were defined using the DSM-IV criteria (American Psychological Association, 2000), as assessed by the AUDADIS-IV (Grant et al., 2003), including alcohol dependence (AD), cannabis dependence (CD), nicotine dependence (ND), and antisocial personality disorders (ASPD), major depressive disorder (MDD), generalized anxiety disorder (GAD), and post-traumatic stress disorder (PTSD), as described elsewhere (Compton et al., 2005; Grant et al., 2005; Hasin et al., 2006). AUDADIS diagnoses have fair to excellent test–retest reliability (k = 0.42–0.84) in clinical and general population samples (Hasin et al., 2007, 2012), and good to excellent validity in US (Hasin et al., 1994, 1997b; Hasin and Paykin, 1999; Canino et al., 1999; Grant et al., 2003; Ruan et al., 2008) populations. We analyzed disorders with lifetime initial onset after 9/11.
2.2.2. Predictors
2.2.2.1. 9/11 Exposure
Questions on 9/11 included the type of exposure to the attacks. From these, we used an ordinal NESARC 9/11 variable with four exposure levels, as described elsewhere (Henriksen et al., 2010): (1) No exposure; (2) Indirect exposure through media, news, etc.; (3) Had a close friend or family member injured or killed; and (4) Direct exposure (respondent at the scene of the terrorist attack and/or injured). If a respondent experienced 9/11 in more than one way, they were coded at the highest level of exposure they experienced. The four levels were dummy-coded for comparisons of different exposure levels.
2.2.2.2. Childhood maltreatment
Nineteen items adapted from two empirically validated scales (Straus, 1979, 1990; Wyatt, 1985) were used to assess maltreatment before age 18. Scales of these items have excellent reliability (intraclass coefficients, 0.79–0.88 (Ruan et al., 2008)). A factor analysis of these 19 items conducted previously (Keyes et al., 2012) indicated that a five-factor model with a latent dimension for each maltreatment type (sexual abuse, physical abuse, physical neglect, emotional abuse, and emotional neglect) provided excellent fit to the data. This five-factor model was used in the present analyses.
2.2.2.3. Parental history
Parental histories of problems with alcohol, drugs, antisocial behavior and depression were ascertained using the AUDADIS-IV. In assessing family history, interviewers read definitions to respondents that included examples of observable manifestations of the diagnostic criteria, since these are the mostly likely to be known to family members, increasing sensitivity (Andreasen et al., 1977; Zimmerman et al., 2004; Heiman et al., 2008). Interviewers then asked whether respondents’ biological mother and father experienced the condition as defined. AUDADIS-IV family history variables have very good to excellent test–retest reliability (Grant et al., 1995, 2003; Hasin et al., 1997a). From this information, four separate variables were created representing parental histories of alcohol, drug, depression, and antisocial behavior problems. For example, participants were coded as positive for parental alcohol problems if either their mother or father had such problems.
2.3. Statistical analyses
2.3.1. Latent meta-structure of psychiatric disorders
To examine the relationships between 9/11 exposure and subsequent psychopathology, we used a latent dimensional approach. Model fit indices included Comparative Fit Index (CFI), Tucker–Lewis Index (TLI), and Root Mean Square Error of Approximation (RMSEA). Individuals who had never used the relevant substance were coded as zero for each disorder (since wave 1, 7804 individuals (41.7%) had not consumed alcohol; 1632 individuals (87.2%) had not used nicotine, and 17,947 individuals (95.9%) had not used cannabis). Individuals with psychiatric diagnoses prior to 9/11 were excluded from all analyses. Psychiatric and substance use diagnoses, and family history variables were, analyzed as ordered categorical variables (0, 1) implementing these models with a weighted least squares estimator (WLSMV). Missing data were addressed via full-information maximum likelihood in Mplus version 6.12 (Muthén and Muthén, 2000). Estimates were weighted and standard errors adjusted for the complex sample design of the NESARC survey.
In preliminary analyses to ensure that 9/11 exposure was associated with each disorder indicating the latent dimensions and that single disorders were not driving the effects observed in INT and EXT, we explored associations between 9/11 exposure and each diagnosis. Using the established meta-structure for these disorders (Eaton et al., 2013), we created an externalizing (EXT) factor (AD, ND, CD, ASPD) and an internalizing (INT) factor (MDD, GAD, PTSD), using confirmatory factor analysis. A two-factor solution provided an excellent fit to the data (CFI = 0.99, TLI = 0.99, RMSEA = 0.02).
2.3.2. 9/11 Exposure, risk factors, and latent meta-structure of psychiatric disorders
Next, we estimated a structural equation model (SEM) simultaneously regressing two latent factors (INT, EXT) on (1) 9/11 exposure (one four-level observed variable), (2) childhood maltreatment (one latent variable with five latent indicators), and (3) parental histories (alcohol, drugs, depression, antisocial behavior; four binary observed variables). All models were adjusted for demographic variables, and latent variables were allowed to correlate with each other. For each of the latent variables, the paths to the first indicator were set to 1 to establish the metric of the latent variable as has been suggested by Muthén and Muthèn (2000). As mentioned above, preliminary association analyses between 9/11 exposure and each individual disorder were conducted to ensure that single disorders were not entirely driving the effects observed in INT and EXT. Additionally, there are both theoretical and empirical (Henriksen et al., 2010) reasons to expect a particularly strong relationship between trauma exposure (9/11 exposure, childhood maltreatment) and certain disorders, such as PTSD. Thus, in further consideration of any individual disorder effects that are not captured by the latent INT and EXT dimensions, we also evaluated modification indices to determine whether residual correlation between 9/11 exposure and specific disorders would appreciably improve the model fit, with an a priori rule that direct effects between INT and EXT and individual disorders would be included in the model if the model fit improvement was above 3.96, corresponding to a p-value of 0.05 (Keyes et al., 2012).
2.3.3. Moderation by childhood maltreatment
The interaction between 9/11 exposure and childhood maltreatment was assessed by including a multiplicative interaction term (9/11 Exposure*childhood maltreatment) to predict each latent dimension in the SEM (Muthén and Muthén, 2000).
2.3.4. Post-hoc analyses
Finally, post-hoc analyses were conducted to probe the significant direct and interaction effects on INT and EXT dimensions for each of the four levels of 9/11 exposure. In these analyses, dummy codes for each level of exposure (reference group (0): No exposure; (1): Indirect exposure through media, news, etc.; (2): Had a close friend or family member injured or killed; and (3): Direct exposure) were first included in place of the categorical exposure variable in the main effects model. Subsequently, interaction terms between each dummy code and each childhood adversity variable were included.
3. Results
3.1. Descriptives
Demographic characteristics of the sample are shown in Table 1 by 9/11 exposure level. The majority (77.5%) of respondents reported exposure to 9/11. Most (72.8%) reported exposure indirectly: through media outlets (i.e. television, news), 3.6% had a close friend or relative injured or killed, while 0.5% (n = 170) directly experienced 9/11. Among participants who experienced 9/11 directly, males were overrepresented, whereas females were over-represented among those who experienced 9/11 indirectly. Overall, age did not vary significantly by 9/11 exposure. However participants over age 65 were less likely to have experienced 9/11 directly. Conversely, race/ethnicity did vary significantly by 9/11 exposure, with White participants being more likely to report experiencing 9/11 directly. Further details on these 9/11 exposure groups, including tests assessing differences among key descriptive variables are provided in Henriksen et al., 2010.
Frequencies of 9/11 exposure, substance and psychiatric disorders are shown in Table 2. Rates of disorders that began after 9/11 ranged from 0.4% (CD) to 13.7% (ND). All disorder pairs were significantly correlated (tetrachoric correlations (r), 0.04–0.35), except GAD and ASPD. Regarding childhood maltreatments, 35.9% experienced at least one form of maltreatment. Over one-third (35.2%) of individuals reported a parental history of at least one form of psychopathology. Childhood maltreatment factors and parental histories of problems were correlated (r: 0.07–0.26), with the lowest correlations between emotional neglect and parental history of drug use (r = 0.07) and depression (r = 0.09), and the highest correlations between emotional abuse and parental alcohol problems (r = 0.21) and antisocial behavior (0.26).
Table 2.
Severity of 9/11 exposure and subsequent psychiatric disorders.
| % Within 9/11 exposure | Frequency (%) | 9/11 Exposure
|
|||
|---|---|---|---|---|---|
| No exposure | Indirectly experienced | Close Friend/Relative | Directly experienced | ||
| Psychiatric Dx (Since 9/11) | 8003 (23.1%) | 25,239 (72.8%) | 1241 (3.6%) | 170 (0.5%) | |
| Alcohol Dependence | |||||
| No | 32,842 (94.8%) | 7681 (96.0%) | 23,843 (94.5%) | 1160 (93.5%) | 158 (92.9%) |
| Yes | 1811 (5.2%) | 322 (4.0%) | 1396 (5.5%) | 81 (6.5%) | 12 (7.1%) |
| Odds Ratio (95% CI) | reference | 1.40 (1.23, 1.58) | 1.67 (1.30, 2.14) | 1.83 (1.00, 3.29) | |
| p-value | <0.0001 | <0.0001 | 0.051 | ||
| Nicotine Dependence | |||||
| No | 29,899 (86.3%) | 7108 (88.8%) | 21,572 (85.5%) | 1054 (84.9%) | 155 (91.2%) |
| Yes | 4764 (13.7%) | 895 (11.2%) | 3667 (14.5%) | 187 (15.1%) | 15 (8.8%) |
| Odds Ratio (95% CI) | reference | 1.35 (1.25, 1.46) | 1.41 (1.19, 1.67) | 0.77 (0.45, 1.31) | |
| p-value | <0.0001 | <0.0001 | 0.334 | ||
| Marijuana Dependence | |||||
| No | 34,498 (99.6%) | 7983 (99.8%) | 25,113 (99.5%) | 1233 (99.4%) | 169 (99.4%) |
| Yes | 155 (0.4%) | 20 (0.2%) | 126 (0.5%) | 8 (0.6%) | 1 (0.6%) |
| Odds Ratio (95% CI) | reference | 2.00 (1.25, 3.21) | 2.59 (1.14, 5.89) | 2.36 (0.32, 17.70) | |
| p-value | 0.004 | 0.023 | 0.403 | ||
| Major Depression | |||||
| No | 31,080 (89.7%) | 7314 (91.4%) | 22,551 (89.3%) | 1065 (85.8%) | 150 (88.2%) |
| Yes | 3573 (10.3%) | 689 (8.6%) | 2688 (10.7%) | 176 (14.2%) | 20 (11.8%) |
| Odds Ratio (95% CI) | reference | 1.27 (1.16, 1.38) | 1.75 (1.47, 2.09) | 1.42 (0.88, 2.27) | |
| p-value | <0.0001 | <0.0001 | 0.150 | ||
| Generalized Anxiety | |||||
| No | 33,103 (95.5%) | 7739 (96.7%) | 24,053 (95.3%) | 1151 (92.7%) | 160 (94.1%) |
| Yes | 1550 (4.5%) | 264 (3.3%) | 1186 (4.7%) | 90 (7.3%) | 10 (5.9%) |
| Odds Ratio (95% CI) | reference | 1.45 (1.26, 1.66) | 2.29 (1.79, 2.94) | 1.83 (0.96, 3.51) | |
| p-value | <0.0001 | <0.0001 | 0.068 | ||
| Post-Traumatic Stress Disorder | |||||
| No | 31,868 (92.0%) | 7550 (94.3%) | 23,081 (91.4%) | 1097 (88.4%) | 140 (82.4%) |
| Yes | 2785 (8.0%) | 453 (5.7%) | 2158 (8.6%) | 144 (11.6%) | 30 (17.6%) |
| Odds Ratio (95% CI) | reference | 1.56 (1.40, 1.73) | 2.19 (1.80, 2.67) | 3.57 (2.38, 5.36) | |
| p-value | <0.0001 | <0.0001 | <0.0001 | ||
Bold font indicates that the Odds Ratio is significantly different than zero (p-value < 0.05). However, the bold can be removed since the p-value is described in the table.
3.2. 9/11 Exposure, risk factors, and latent meta-structure of psychiatric disorders
Preliminary analyses indicated that participants had increased odds of meeting criteria for each disorder since 9/11 (Table 2) if they indirectly experienced 9/11 (i.e. media, news) or had a close friend or relative directly impacted, compared with those not exposed. Directly experiencing the events of 9/11 was significantly associated with increased odds of PTSD, with the effects on AD approaching significance.
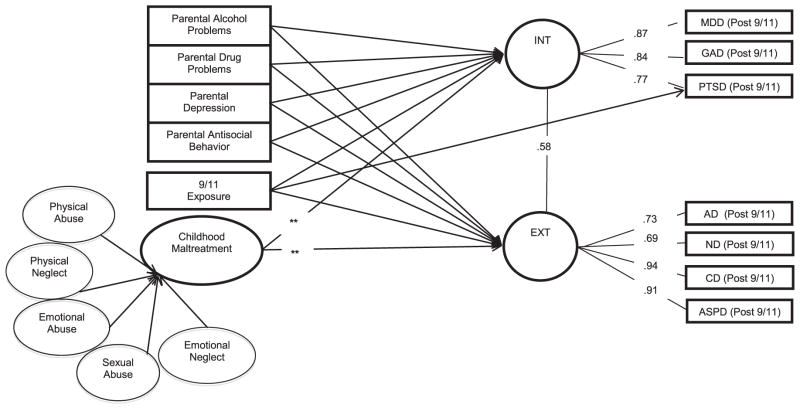
The main effects model (Fig. 1) explained 20% and 21% of the variance in the INT and EXT dimensions, respectively. The full model that included main and interaction effects (9/11 exposure*childhood adversities) explained 21% and 22% of the variance in the INT and EXT dimensions, respectively. The full model provided an excellent fit to the data (CFI = 0.996, TLI = 0.994, RMSEA = 0.003). INT and EXT were correlated (r = 0.58). Participants had higher INT and EXT levels if they were exposed to 9/11 (EXT: β = 0.10, p < 0.001; INT: β = 0.11, p < 0.001). These results did not change significantly after adjusting for childhood maltreatment and parental psychopathology. Further, modification indices did not suggest that any associations between 9/11 exposure and individual disorders were unmediated by the association with the disorder with the latent dimensions (no difference in model fit exceeded a priori significance threshold of greater than 3.96), with the exception of PTSD. According to these criteria, there was significant model fit improvement when a direct effect of 9/11 exposure on the individual diagnosis of PTSD was included in the model (Modification = 5.66, p < 0.05).
Fig. 1.
The Association between 9/11 exposure, childhood adversities (maltreatment and parental histories of psychopathology) and latent dimensions of subsequent internalizing and externalizing disorders in the NESARC (Wave 2).
Note: Covariances between all predictors (with the exception of 9/11 exposure) were included in the model (ranged from 0.14 to 0.62), but excluded from this figure for clarity. Asterisks represent significant moderation (or Interactions). All pathways adjusted for age, sex, race.
Childhood maltreatment was related to INT (β = 0.39, p < 0.001) and EXT (β = 0.29, p < 0.001). Parental history of alcohol problems was associated with INT (β = 0.03, p < 0.01) and EXT (β = 0.06, p < 0.01), as was parental history of drug problems (INT β = 0.01, p < 0.01; EXT β = 0.05, p < 0.001), antisocial behavior (INT β = 0.02, p < 0.01; EXT β = 0.10, p < 0.001) and depression (INT (β = 0.16, p < 0.001; EXT β = 0.10, p < 0.01)).
3.3. Moderation by childhood maltreatment
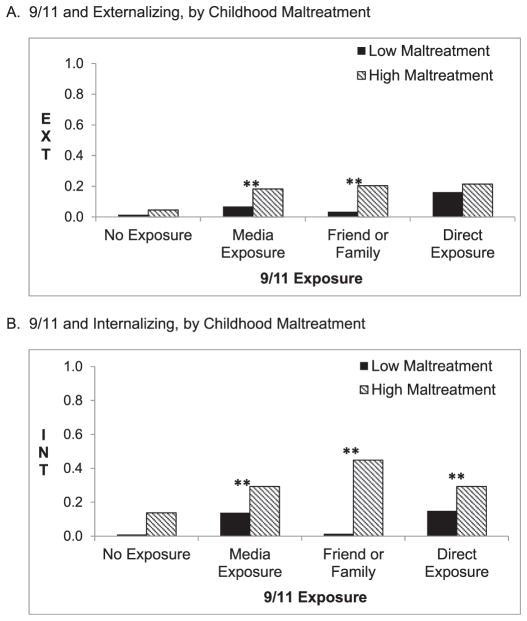
Childhood maltreatment and level of 9/11 exposure showed a significant interaction effect on the INT and EXT dimensions (β = 0.06, p < 0.01; β = 0.07, p < 0.001, respectively). The association between 9/11 exposure and each latent dimension of psychopathology (INT and EXT) was stronger among those who experienced childhood maltreatment compared with those who did not (depicted in Fig. 2a and b).
Fig. 2.
Interaction effects of Childhood Maltreatment and 9/11 Exposure on Externalizing (A) and Internalizing (B) Disorders in the NESARC Note: **denote differences significant at p < 0.05.
3.4. Post-hoc analyses
Post-hoc analyses further evaluated the effects on INT and EXT at each level of 9/11 exposure. Compared to those unexposed, participants had increased risk on the EXT dimension if they indirectly experienced 9/11 (β = 0.10, p < 0.001) or had a close friend or relative directly impacted by 9/11 (β = 0.15, p < 0.001), but not if they directly experienced 9/11. Compared to those unexposed to 9/11, participants had increased risk on the INT dimension if they indirectly experienced 9/11 (β = 0.11, p < 0.001), had a close friend or relative directly impacted by 9/11 (β = 0.27, p < 0.001), or if they had directly experienced the events of 9/11 (β = 0.29, p < 0.001). The association between indirect exposure to 9/11 and EXT was greater among those who experienced childhood maltreatment than those who did not (Fig. 2a). The association between indirect and direct exposure to 9/11 and INT was greater among those who experienced childhood maltreatment than those who did not (Fig. 2b); Interaction effects on INT between childhood maltreatment and 9/11 were significant for those who indirectly experienced 9/11 through the media or through family/friends, or who experienced 9/11 directly as compared with those who were not exposed to 9/11.
4. Discussion
In this study, we expanded upon previous work on the experience of 9/11 and negative mental health outcomes in the US population in several important ways. First, we showed that level of 9/11 exposure significantly predicted latent dimensions of both internalizing and externalizing pathology in a sample who endorsed no psychiatric history prior to 9/11. These effects of the level of 9/11 exposure remained associated with these latent dimensions even after accounting for two robust risk factors for psychopathology, childhood maltreatment and parental history of mental illness. Second, post-hoc analyses revealed significant associations between indirect exposure to 9/11 as experienced through media outlets, friends or family and INT and EXT dimensions of subsequent psychiatric and substance use disorders, whereas direct exposure to 9/11 was only related to the INT dimension. Finally, childhood adversities increased the risk associated with direct and indirect 9/11 exposure for developing INT and EXT disorders following 9/11 exposure. Post-hoc analyses showed that specifically, childhood maltreatment increased the risk for developing INT and EXT disorders among those with 9/11 exposure.
4.1. 9/11 Exposure, risk factors, and latent meta-structure of psychiatric disorders
The majority of the US population was exposed to 9/11 indirectly, through media outlets such as news programs, and through family and friends. Thus, examining the health consequences of mass traumatic events experienced through media and technology outlets is increasingly important. Consistent with previous findings (Breslau et al., 2010; McLaughlin et al., 2010b), the current study found that those who directly experienced 9/11 had an increased risk of subsequent INT disorders, an effect that was largely driven by PTSD. However, those who experienced 9/11 through the media, family or friends had increased risk on both the INT and EXT dimensions, which may indicate that these individuals had a broader range of psychological consequences following 9/11. It is important to consider however, that the non-significant EXT effects observed for those with direct exposure may be due to the smaller sample size (and related lack of power to detect an effect), rather than 9/11 direct exposure being less impactful than 9/11 indirect exposure.
In this study, we examined the relationship between parental history of psychopathology and latent dimensions of offspring psychopathology (new onsets following 9/11) in a representative sample of Americans. Consistent with previous studies (Kendler et al., 1997), we found that parental problems with alcohol, drug, antisocial behavior, and depression were related to both INT and EXT. Consistent with prior expectations, parental alcohol, drug, and antisocial behavior problems were more closely related to EXT, while parental depression was more closely related to INT. In addition, we found associations between childhood maltreatment and initial onset of dimensions of psychopathology after 9/11.
4.2. Moderation by childhood maltreatment
In this study, childhood maltreatment increased the risk associated with 9/11 exposure for developing INT and EXT disorders following 9/11. This is consistent with the concept of stress sensitization, which posits that early exposure alters stress response systems such that these systems are primed to respond in ways that increase risk for distress after exposure to later trauma (McLaughlin et al., 2010a; Pratchett and Yehuda, 2011). While the mechanisms by which stress sensitization occurs remains unclear, much evidence suggests that trauma early in life may alter neurobiologic and behavioral systems, thereby influencing subsequent stress responses (Pratchett and Yehuda, 2011). Studies find that childhood adversity is associated with HPA axis dysfunction, that may lead to later development of adult psychopathology (Watson et al. 2007; Newport et al., 2004). Increased behavioral stress reactivity has also been identified among adults who were maltreated as children. For example, individuals with a history of childhood sexual abuse display stronger emotional responses to everyday stressors than those never abused or sexually abused after age 18 (Thakkar and McCanne, 2000). These complex biological and interpersonal systems are influenced by various factors, including the time in development that the adverse events occur, nature of the individual’s social support systems, and related resilience and coping mechanisms. Prospective longitudinal studies are required to delineate the mechanisms involved in the progression from childhood trauma to adult psychopathology.
4.3. Implications
Our results have etiologic and clinical implications that challenge the current conceptualization of psychopathology as consisting of specific, individual psychiatric or substance use disorders. These disorders show considerable comorbidity due to shared variance at an underlying (i.e., latent) level. Clinicians may better serve patients with comorbid mood/anxiety, or substance use and impulsivity-related disorders, if their comorbidity is seen as an indication of high INT and EXT dimension levels, rather than as multiple specific disorders (Livesley, 2008; Eaton et al., 2011). Additionally, clinical interventions could focus on a cluster of symptoms and behavioral problems related to a particular dimension of psychopathology instead of using treatments tailored for one particular disorder. Further, research on the etiology of mental and substance use disorders should focus on understanding genetic and environmental predispositions towards INT and/or EXT as well as the additional specific factors that may determine how this liability is expressed for each individual (Kendler et al., 2008; Torgersen et al., 2008).
4.4. Strengths and limitations
Study limitations are noted. First, NESARC diagnostic interviews were administered by trained lay interviewers rather than clinicians. This limitation is somewhat mitigated by the AUDADIS-IV’s structured design and good psychometric properties. Second, this is a study of adults providing retrospective reports of adverse experiences, including childhood adversity and adult exposure to 9/11. Self-reports may be unstable over time (Fergusson et al., 2000; Polanczyk et al., 2009), typically underestimating adversity prevalence. Third, while this study used measures of parental history of mental illness similar to those used in many other studies, such measures reflect the participant’s perception of their parents’ history of problems and may be influenced by participants’ own experiences (Kendler, 1991). However, a recent study comparing the prevalence of child’s perception of family alcohol problems to true prevalence supports use of such family history measures (Kendler et al., 2012). Forth, our findings are based on DSM-IV diagnoses of mood, anxiety, personality and substance use disorders and should be replicated using DSM-5 diagnoses. Fifth, the rates reported for disorders in this study could be underestimated due to attrition. However, attrition between the Wave 1 and Wave 2 NESARC was small (13.3%) and the Wave 2 data were adjusted for nonresponse associated with socio-demographic characteristics (Grant et al., 2009). Finally, the present analyses only included participants with no history of psychiatric disorders prior to 9/11. This was done so that we could be clear that what we were examining was the new onset of psychiatric symptoms following 9/11 exposure, rather than a mixed group of new onsets plus relapses of prior lifetime psychiatric symptoms that were in remission prior to 9/11. However, this analytic strategy does limit the generalization of these findings in that the associations with 9/11 exposure, and childhood maltreatment might be different for this subpopulation of individuals with no prior history of psychiatric or substance use disorders from those with a prior history who were previously in remission at the time of the 9/11 attack. This is particularly relevant given the strong relationship between childhood maltreatment and psychopathology (Keyes et al., 2012) and should be formally explored in future research. These limitations are counterbalanced by several study strengths. The NESARC is the largest psychiatric epidemiological survey of the US general population conducted to date, with rich measures of childhood maltreatment, exposure to traumatic life events, and a wide range of psychiatric disorders. Our results build on the stress-sensitization literature by providing a unique insight into the relationship between childhood maltreatment, adult exposure to 9/11, and the structure of common psychiatric disorders.
This study was the first to explore associations between 9/11 exposure and latent dimensions of psychopathology. We found that in a sample who endorsed no psychiatric history prior to 9/11, indirect exposure (i.e. media, friends/family) was related to both INT and EXT dimensions of psychopathology, whereas direct exposure was associated with the INT dimension only. The associations between 9/11 and these outcomes went beyond the effects of two indicators of childhood adversity, childhood maltreatment and parental history of mental illness, and for individuals who had experienced these forms of childhood adversity, the risk for INT and EXT dimensions associated with 9/11 was exacerbated. Taken together, these findings indicate the broad psychological impact of 9/11 on the US general population, and provide further evidence that early adversity increases the psychological risk associated with later trauma exposure. These results highlight the need for mental health clinicians to incorporate assessments of childhood maltreatment and parental history of psychopathology into assessments of mental health service users, in order to provide suitable, evidence-based treatment to individuals who report such experiences. In addition, clinicians treating patients for disaster-related psychopathology (both direct and indirect exposure) should be attuned to the role of childhood adversity in exacerbating symptoms. Finally, these findings suggest that research on the etiology of mental and substance use disorders should examine predispositions towards INT and/or EXT as well as the additional specific risk factors that may determine how this liability is expressed for each individual (Kendler et al., 2008; Torgersen et al., 2008).
Acknowledgments
Role of funding source
Grant Support: This research was funded by National Institutes of Health grants U01AA018111 (Hasin), T32MH13043 (Meyers/Link). Other: New York State Psychiatric Institute (Hasin).
This research was funded by National Institutes of Health grants U01AA018111, T32MH13043 (Meyers/Link), the New York State Psychiatric Institute (Hasin).
Footnotes
Authors contribution
JLM, SRL, and DH were responsible for the study concept and design. BFG contributed to the study design and acquisition of the National Epidemiologic Study on Alcohol Related Conditions data. JLM conducted data analysis and SRL, NRE, and RK assisted with interpretation of findings. JLM and SRL drafted the manuscript. NRE, RK, BFG, and DH provided critical revision of the manuscript for important intellectual content. All authors critically reviewed content and approved final version for publication.
Declaration of interest
The authors have no conflicts of interest.
References
- Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Reliab Validity. Arch of Gen Psychiatr. 1977 Oct;34(10):1229–35. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- American Psychological Association; American Psychiatric, editor. Diagnostic and statistical manual of mental disorders. 4. Washington D.C: 2000. [Google Scholar]
- Ben Barnes J, Dickstein BD, Maguen S, Neria Y, Litz BT. The distinctiveness of prolonged grief and posttraumatic stress disorder in adults bereaved by the attacks of September 11th. J Affect Disord. 2012 Feb;136(3):366–9. doi: 10.1016/j.jad.2011.11.022. [DOI] [PubMed] [Google Scholar]
- Breslau N, Bohnert KM, Koenen KC. The 9/11 terrorist attack and posttraumatic stress disorder revisited. J Nerv Ment Dis. 2010 Aug;198(8):539–43. doi: 10.1097/NMD.0b013e3181ea1e2f. [DOI] [PubMed] [Google Scholar]
- Canino G, Bravo M, Ramirez R, Febo VE, Rubio-Stipec M, Fernandez RL, et al. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol. 1999;60(6):790–9. doi: 10.15288/jsa.1999.60.790. 1999/12/22. [DOI] [PubMed] [Google Scholar]
- Carr CP, Martins CMS, Stingel AM, Lemgruber VB, Juruena MF. The role of early life stress in adult psychiatric disorders: a systematic review according to childhood trauma subtypes. J Nerv Ment Dis. 2013 Dec;201(12):1007–20. doi: 10.1097/NMD.0000000000000049. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005 Jun;66(6):677–85. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatr. 2007 May;64(5):566–76. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Dougall AL, Hayward MC, Baum A. Media exposure to bioterrorism: stress and the anthrax attacks. Psychiatry. 2005 Jan;68(1):28–42. doi: 10.1521/psyc.68.1.28.64188. [DOI] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, et al. An invariant dimensional liability model of gender differences in mental disorder prevalence: evidence from a national sample. J Abnorm Psychol. 2012 Feb;121(1):282–8. doi: 10.1037/a0024780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Noordhof A, Skodol AE, Markon KE, et al. Ethnicity and psychiatric comorbidity in a national sample: evidence for latent comorbidity factor invariance and connections with disorder prevalence. Soc Psychiatry Psychiatr Epidemiol. 2013 May;48(5):701–10. doi: 10.1007/s00127-012-0595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, et al. Borderline personality disorder comorbidity: relationship to the internalizing-externalizing structure of common mental disorders. Psychol Med [Internet] 2011 May;41(5):1041–50. doi: 10.1017/S0033291710001662. cited 2014 May 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Woodward LJ. The stability of child abuse reports: a longitudinal study of the reporting behaviour of young adults. Psychol Med [Internet] 2000 May;30(3):529–44. doi: 10.1017/s0033291799002111. cited 2013 Mar 15. [DOI] [PubMed] [Google Scholar]
- Galea S, Resnick H, Ahern J, Gold J, Bucuvalas M, Kilpatrick D, et al. Posttraumatic stress disorder in Manhattan, New York City, after the September 11th terrorist attacks. J Urban Heal : Bull N Y Acad Med [Internet] 2002 Sep;79(3):340–53. doi: 10.1093/jurban/79.3.340. cited 2014 May 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend [Internet] 2003;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. 2003/06/25. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, et al. Socio-demographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry [Internet] 2009 Nov;14(11):1051–66. doi: 10.1038/mp.2008.41. cited 2014 Jul 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend [Internet] 1995;39(1):37–44. doi: 10.1016/0376-8716(95)01134-k. 1995/07/01. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, June Ruan W, Goldstein RB, et al. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med [Internet] 2005 Dec;35(12):1747–59. doi: 10.1017/S0033291705006069. cited 2013 Sep 9. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatr [Internet] 2004 Apr;61(4):361–8. doi: 10.1001/archpsyc.61.4.361. cited 2014 May 21. [DOI] [PubMed] [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend [Internet] 1997a;44(2–3):133–41. doi: 10.1016/s0376-8716(97)01332-x. 1997/03/14. [DOI] [PubMed] [Google Scholar]
- Hasin D, Paykin A. Alcohol dependence and abuse diagnoses: concurrent validity in a nationally representative sample. Alcohol Clin Exp Res [Internet] 1999 Jan;23(1):144–50. cited 2014 Jul 2. [PubMed] [Google Scholar]
- Hasin D, Samet S, Nunes E, Meydan J, Matseoane K, Waxman R. Diagnosis of comorbid psychiatric disorders in substance users assessed with the psychiatric research interview for substance and mental disorders for DSM-IV. Am J Psychiatry [Internet] 2006 Apr;163(4):689–96. doi: 10.1176/ajp.2006.163.4.689. cited 2013 May 8. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Fenton MC, Beseler C, Park JY, Wall MM. Analyses related to the development of DSM-5 criteria for substance use related disorders: 2. Proposed DSM-5 criteria for alcohol, cannabis, cocaine and heroin disorders in 663 substance abuse patients. Drug Alcohol Dependence [Internet] 2012 Apr 1;122(1–2):28–37. doi: 10.1016/j.drugalcdep.2011.09.005. cited 2013 Mar 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Keyes KM, Hatzenbuehler ML, Aharonovich EA, Alderson D. Alcohol consumption and posttraumatic stress after exposure to terrorism: effects of proximity, loss, and psychiatric history. Am J Public Health [Internet] 2007a;97(12):2268–75. doi: 10.2105/AJPH.2006.100057. 2007/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Muthuen B, Wisnicki KS, Grant B. Validity of the bi-axial dependence concept: a test in the US general population. Addict (Abingdon, Engl [Internet] 1994 May;89(5):573–9. doi: 10.1111/j.1360-0443.1994.tb03333.x. cited 2014 Jul 2. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Van Rossem R, McCloud S, Endicott J. Differentiating DSM-IV alcohol dependence and abuse by course: community heavy drinkers. J Subst Abuse [Internet] 1997b;9:127–35. doi: 10.1016/s0899-3289(97)90011-0. cited 2014 Jul 2. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatr [Internet] 2007b;64(7):830–42. doi: 10.1001/archpsyc.64.7.830. cited 2014 Mar 31. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. Neurobiology of posttraumatic stress disorder. CNS spectrums [Internet] 2009 Jan;14(Suppl 1):13–24. cited 2014 May 12. [PubMed] [Google Scholar]
- Heiman GA, Ogburn E, Gorroochurn P, Keyes KM, Hasin D. Evidence for a two-stage model of dependence using the NESARC and its implications for genetic association studies. Drug Alcohol Depend [Internet] 2008 Jan 1;92(1–3):258–66. doi: 10.1016/j.drugalcdep.2007.08.007. cited 2013 Apr 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henriksen CA, Bolton JM, Sareen J. The psychological impact of terrorist attacks: examining a dose-response relationship between exposure to 9/11 and Axis I mental disorders. Depress Anxiety [Internet] 2010 Nov;27(11):993–1000. doi: 10.1002/da.20742. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Holman EA, Lucas-Thompson RG, Lu T. Social constraints, genetic vulnerability, and mental health following collective stress. J Trauma Stress [Internet] 2011 Oct;24(5):497–505. doi: 10.1002/jts.20671. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Kendler KS. The family history method: whose psychiatric history is measured? American Psychiatric Association Am J Psychiatry [Internet] 1991 Nov 1;148(11):1501–4. doi: 10.1176/ajp.148.11.1501. cited 2013 Nov 13. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Czajkowski N, Røysamb E, Tambs K, Torgersen S, et al. The structure of genetic and environmental risk factors for DSM-IV personality disorders: a multivariate twin study. Arch Gen Psychiatr [Internet] 2008 Dec;65(12):1438–46. doi: 10.1001/archpsyc.65.12.1438. cited 2014 May 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Davis CG, Kessler RC. The familial aggregation of common psychiatric and substance use disorders in the National Comorbidity Survey: a family history study. Br J Psychiatr : J Ment Sci [Internet] 1997 Jun;170:541–8. doi: 10.1192/bjp.170.6.541. cited 2014 May 21. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch General Psychiatr [Internet] 2003 Sep;60(9):929–37. doi: 10.1001/archpsyc.60.9.929. cited 2013 Feb 4. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Sundquist K, Ohlsson H, Palmér K, Maes H, Winkleby MA, et al. Genetic and familial environmental influences on the risk for drug abuse: a national Swedish adoption study. Arch Gen Psychiatr [Internet] 2012 Jul;69(7):690–7. doi: 10.1001/archgenpsychiatry.2011.2112. cited 2013 Sep 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatr [Internet] 1994 Jan;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. cited 2013 Aug 28. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, et al. Childhood maltreatment and the structure of common psychiatric disorders. Br J Psychiatry : J Ment Sci [Internet] 2012 Feb;200(2):107–15. doi: 10.1192/bjp.bp.111.093062. cited 2014 May 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Shmulewitz D, Greenstein E, McLaughlin K, Wall M, Aharonovich E, et al. Exposure to the Lebanon War of 2006 and effects on alcohol use disorders: the moderating role of childhood maltreatment. Drug Alcohol Depend [Internet] 2014 Jan 1;134:296–303. doi: 10.1016/j.drugalcdep.2013.10.014. cited 2014 May 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol [Internet] 2002 Aug;111(3):411–24. cited 2013 Jan 29. [PubMed] [Google Scholar]
- Krueger RF, Markon KE. The role of the DSM-5 personality trait model in moving toward a quantitative and empirically based approach to classifying personality and psychopathology. Annu Rev Clin Psychol [Internet] 2014 Jan;10:477–501. doi: 10.1146/annurev-clinpsy-032813-153732. cited 2014 Jul 19. [DOI] [PubMed] [Google Scholar]
- Lengua LJ, Long AC, Smith KI, Meltzoff AN. Pre-attack symptomatology and temperament as predictors of children’s responses to the September 11 terrorist attacks. J Child Psychol Psychiatry, Allied Discip [Internet] 2005 Jun;46(6):631–45. doi: 10.1111/j.1469-7610.2004.00378.x. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Livesley WJ. Research trends and directions in the study of personality disorder. Psychiatric Clin N Am [Internet] 2008 Sep;31(3):545–559. ix. doi: 10.1016/j.psc.2008.03.014. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Lucchini RG, Crane MA, Crowley L, Globina Y, Milek DJ, Boffetta P, et al. The World Trade Center health surveillance program: results of the first 10 years and implications for prevention. G Ital Med del Lav Ergon [Internet] 2012;34(3 Suppl):529–33. cited 2014 May 12. [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication II: associations with persistence of DSM-IV disorders. Arch Gen Psychiatr [Internet] 2010a Feb;67(2):124–32. doi: 10.1001/archgenpsychiatry.2009.187. cited 2014 May 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Keyes KM. Responses to discrimination and psychiatric disorders among Black, Hispanic, female, and lesbian, gay, and bisexual individuals. Am J Public Health [Internet]. American Public Health Association. 2010b Aug 20;100(8):1477–84. doi: 10.2105/AJPH.2009.181586. cited 2013 Sep 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Los Angeles: Muthén & Muthén; 2000. [Google Scholar]
- Neria Y, DiGrande L, Adams BG. Posttraumatic stress disorder following the September 11, 2001, terrorist attacks: a review of the literature among highly exposed populations. Am Psychol [Internet] 2011 Sep;66(6):429–46. doi: 10.1037/a0024791. cited 2014 May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newport DJ, Heim C, Bonsall R, Miller AH, Nemeroff CB. Pituitary-adrenal responses to standard and low-dose dexamethasone suppression tests in adult survivors of child abuse. Biol Psychiatry [Internet] 2004 Jan 1;55(1):10–20. doi: 10.1016/s0006-3223(03)00692-9. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Otto MW, Henin A, Hirshfeld-Becker DR, Pollack MH, Biederman J, Rosenbaum JF. Posttraumatic stress disorder symptoms following media exposure to tragic events: impact of 9/11 on children at risk for anxiety disorders. J Anxiety Disord [Internet] 2007 Jan;21(7):888–902. doi: 10.1016/j.janxdis.2006.10.008. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Perlman SE, Friedman S, Galea S, Nair HP, Eros-Sarnyai M, Stellman SD, et al. Short-term and medium-term health effects of 9/11. Lancet [Internet] 2011 Sep 3;378(9794):925–34. doi: 10.1016/S0140-6736(11)60967-7. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Schechter CB, Bromet EJ, Katz CL, Reissman DB, Ozbay F, et al. The burden of full and subsyndromal posttraumatic stress disorder among police involved in the World Trade Center rescue and recovery effort. J Psychiatr Res [Internet] 2012 Jul;46(7):835–42. doi: 10.1016/j.jpsychires.2012.03.011. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Polanczyk G, Caspi A, Williams B, Price TS, Danese A, Sugden K, et al. Protective effect of CRHR1 gene variants on the development of adult depression following childhood maltreatment: replication and extension. Arch Gen Psychiatr [Internet] 2009 Sep;66(9):978–85. doi: 10.1001/archgenpsychiatry.2009.114. cited 2013 Jul 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack MH, Simon NM, Fagiolini A, Pitman R, McNally RJ, Nierenberg AA, et al. Persistent posttraumatic stress disorder following September 11 in patients with bipolar disorder. J Clin Psychiatry [Internet] 2006 Mar;67(3):394–9. doi: 10.4088/jcp.v67n0309. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Pratchett LC, Yehuda R. Foundations of posttraumatic stress disorder: does early life trauma lead to adult posttraumatic stress disorder? Dev Psychopathol [Internet] 2011 May;23(2):477–91. doi: 10.1017/S0954579411000186. cited 2014 May 1. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, et al. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend [Internet] 2008 Jan 1;92(1–3):27–36. doi: 10.1016/j.drugalcdep.2007.06.001. cited 2014 Apr 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA. Measuring introfamily conflict and violence: the conflict tactice (CT) scales. J Marriage Fam. 1979;41:75–88. [Google Scholar]
- Straus MA. In: Physical violence in American families: risk factors and adaptations to violence in 8,145 families. Press T, editor. 1990. [Google Scholar]
- Thakkar RR, McCanne TR. The effects of daily stressors on physical health in women with and without a childhood history of sexual abuse. Child Abuse Negl [Internet] 2000 Feb;24(2):209–21. doi: 10.1016/s0145-2134(99)00129-5. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Torgersen S, Czajkowski N, Jacobson K, Reichborn-Kjennerud T, Røysamb E, Neale MC, et al. Dimensional representations of DSM-IV cluster B personality disorders in a population-based sample of Norwegian twins: a multivariate study. Psychol Med [Internet] 2008 Nov;38(11):1617–25. doi: 10.1017/S0033291708002924. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Watson LF, Taft AJ, Lee C. Associations of self-reported violence with age at menarche, first intercourse, and first birth among a national population sample of young Australian women. Women’s Health Issues : Off Publ Jacobs Inst Women’s Health [Internet] 2007;17(5):281–9. doi: 10.1016/j.whi.2007.06.003. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Welch AE, Caramanica K, Debchoudhury I, Pulizzi A, Farfel MR, Stellman SD, et al. A qualitative examination of health and health care utilization after the September 11th terror attacks among World Trade Center Health Registry enrollees. BMC Public Health [Internet] 2012 Jan;12:721. doi: 10.1186/1471-2458-12-721. cited 2014 May 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Winkel R, Van Nierop M, Myin-Germeys I, Van Os J. Childhood trauma as a cause of psychosis: linking genes, psychology, and biology. Can J Psychiatry Revue Can de Psychiatrie [Internet] 2013 Jan;58(1):44–51. doi: 10.1177/070674371305800109. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Van Winkel R, Stefanis NC, Myin-Germeys I. Psychosocial stress and psychosis. A review of the neurobiological mechanisms and the evidence for gene-stress interaction. Schizophr Bull [Internet] 2008 Nov;34(6):1095–105. doi: 10.1093/schbul/sbn101. cited 2014 Apr 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt GE. The sexual abuse of Afro-American and white-American women in childhood. Child Abuse Negl [Internet] 1985 Jan;9(4):507–19. doi: 10.1016/0145-2134(85)90060-2. cited 2014 May 12. [DOI] [PubMed] [Google Scholar]
- Young-Wolff KC, Kendler KS, Prescott CA. Interactive effects of childhood maltreatment and recent stressful life events on alcohol consumption in adulthood. J Stud Alcohol Drugs [Internet] 2012 Jul;73(4):559–69. doi: 10.15288/jsad.2012.73.559. cited 2014 May 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M, Sheeran T, Young D. The Diagnostic Inventory for Depression: a self-report scale to diagnose DSM-IV major depressive disorder. J Clin Psychol [Internet] 2004 Jan;60(1):87–110. doi: 10.1002/jclp.10207. cited 2013 May 1. [DOI] [PubMed] [Google Scholar]