Abstract
Objectives
To examine longitudinal pathways from multiple types of neighborhood restaurants and food stores to BMI, through dietary behaviors.
Methods
We used data from participants (n=5114) in the United States-based Coronary Artery Risk Development in Young Adults study and a structural equation model to estimate longitudinal (1985–86 to 2005–06) pathways simultaneously from neighborhood fast food restaurants, sit-down restaurants, supermarkets, and convenience stores to BMI through dietary behaviors, controlling for socioeconomic status (SES) and physical activity.
Results
Higher numbers of neighborhood fast food restaurants and lower numbers of sit-down restaurants were associated with higher consumption of an obesogenic fast food-type diet. The pathways from food stores to BMI through diet were inconsistent in magnitude and statistical significance.
Conclusions
Efforts to decrease the numbers of neighborhood fast food restaurants and to increase the numbers of sit-down restaurant options could influence diet behaviors. Availability of neighborhood fast food and sit-down restaurants may play comparatively stronger roles than food stores in shaping dietary behaviors and BMI.
Keywords: Geographic information systems, Neighborhood food environment, Longitudinal study, Diet, Structural equation model, Body mass index
1. Introduction
Since the mid-1980's, obesity increased dramatically across developed countries, such as the U.S., U.K., New Zealand, and Canada (World Health Organization, 2011) with socioeconomically disadvantaged populations disproportionately affected (McLaren, 2007; Ministry of Health, 2004). At the same time, a literature (albeit somewhat mixed) has developed suggesting a role for neighborhood SES in the availability of healthy foods, with lower SES communities having comparatively lower access to higher quality food sources (Block et al., 2004; Moore and Diez Roux, 2006; Morland and Filomena, 2007). Consequently, efforts to improve dietary behaviors and reduce obesity have targeted neighborhood restaurants, especially fast food restaurants, and lack of quality food stores in disadvantaged areas (Let's Move, 2012; The Food Trust, 2004). Yet, most of the evidence is based on cross-sectional studies that focused on a single part of the pathway, either direct associations for food stores and restaurants with dietary behaviors or with body mass index (BMI) (Caspi et al., 2012; Giskes et al., 2011). The extent to which changing food environments lead to individual-level dietary change and consequent reduction in obesity, through diet, is unknown.
International researchers suggest that comprehensive strategies are needed to address environmental and societal factors to reduce obesity disparities (Foresight, 2007; World Health Organization, 2013) Yet, socioeconomically disadvantaged subpopulations in developed countries remain disproportionately affected by obesity (McLaren, 2007; Ministry of Health, 2004). Thus, researchers have begun to examine how temporal changes in food environments impact diet and obesity (Burgoine et al., 2009; Cummins et al., 2014; Smith et al., 2010). But findings are mixed and studies examining temporal patterns in food environments are sparse [see review (Mackenbach et al., 2014)]. A large gap remains in long-term, population-based research in racially diverse samples with detailed time-varying food environment data.
Cross-sectional studies cannot link changes in neighborhood environments with changes in individual-level diet and body weight (Gary-Webb et al., 2010). The few longitudinal studies (Block et al., 2011; Boone-Heinonen et al., 2011; Gibson, 2011) have generally examined associations between a single type of restaurant or food store with a single outcome, such as BMI, obesity, or a broad diet behavior (e.g., diet quality) (Moore et al., 2009). Moreover, we posit that food stores and restaurants do not influence dietary behaviors in isolation; rather, alternative food resources within the same neighborhood may also be important. New approaches to modeling complex pathways that simultaneously account for multiple food store and restaurant options may help explain inconsistent findings in the literature on neighborhood environment and BMI (Ball et al., 2012; Mackenbach et al., 2014).
While neighborhood food stores and restaurants may influence obesity indirectly through dietary behaviors, presence of neighborhood food stores and restaurants may also relate to other neighborhood resources, such as street networks, presence of parks or other obesity-related amenities (Belon et al., 2014; Tseng et al., 2014). This necessitates control for a variety of other neighborhood characteristics through pathway-based approaches. Yet, a majority of research ignores complex pathways, instead using simple direct association. Use of simultaneous regression modeling via systems of equations may help clarify hypothesized pathways.
We used a single longitudinal structural equation model (SEM) in a large United States (U.S.)-based prospective cohort of adult black and white adults over 20 years to estimate simultaneous and separate pathways from neighborhood fast food restaurants, sit-down restaurants, supermarkets and convenience stores to individual-level diet behaviors and BMI. We have two central hypotheses: Hypothesis 1: neighborhood restaurants and food stores are indirectly associated with BMI through the consumption of specific foods typically acquired from specific types of restaurants and foods stores; and Hypothesis 2: associations between restaurants and food stores with dietary behaviors and BMI become stronger over time due to the increase in restaurants and food stores over time (Economic Research Service - USDA, 2004; Lenard, 2012; National Association of Convenience Stores (NACS), 2011; National Restaurant Association, 2013; The Reinvestment Fund, 2011) and the increase in away-from-home eating (Duffey et al., 2007; Smith et al., 2014; Zick and Stevens, 2006). We quantified indirect pathways from fast food restaurants, sit-down restaurants, supermarkets, and convenience stores to BMI, through consumption of specific foods typically acquired at each type of food resource. We also included direct pathways between fast food restaurants, sit-down restaurants, supermarkets, and convenience stores to BMI to capture neighborhood effects that occur through unmeasured factors that are independent of diet.
2. Methods
2.1. Study population
The Coronary Artery Risk Development in Young Adults (CARDIA) study is a longitudinal cohort with detailed diet, clinical, physical activity, environmental, and sociodemographic data collected for 5114 white or black U.S. adults aged 18–30 years originally from 4 centers: Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA. Participants were recruited in 1985–86 (baseline Year 0) with approximately equal numbers by race, gender, education (high school or less versus more than high school), age (18–24 years versus 25–30 years) within each center, and followed over 25 years. We used data from baseline and 4 exams during 1992–93 (Year 7), 1995–96 (Year 10), 2000–01 (Year 15), and 2005–06 (Year 20). Retention was 81%, 79%, 74%, and 72% (n=3549) of the surviving cohort at these four exams, respectively.
2.2. Body mass index
At each examination, participants' weight (nearest 0.2 kg) and height (nearest 0.5 cm) were measured and BMI (kg/m2) calculated. We used years 0, 7, and 20 to correspond with the primary diet measures described below.
2.3. Dietary assessment
An interviewer-administered CARDIA Diet History (McDonald et al., 1991) was used to assess diet at exam years 0, 7, and 20. The CARDIA diet history included a short questionnaire regarding general dietary practices followed by a comprehensive food frequency questionnaire about typical intake of foods using the previous month as a reference for recall. With a food-grouping system (University of Minnesota Nutrition Coordinating Center), we assigned foods to one of 13 food groups and 5 beverage groups [assessed as servings per day of constituent foods (Table 1)]. Since we did not have food purchase data, we selected foods and beverages we theorize are typically offered at fast food restaurants, sit-down restaurants, supermarkets, and convenience stores and that have been shown to be prospectively associated with weight change (Mozaffarian et al., 2011) and cardiometabolic outcomes (Duffey et al., 2012). We categorized dietary intakes (servings per day) and fast food restaurant visits (number per week) into low, medium or high by (1) year-specific tertiles or (2) as non-consumers (0 servings per day) versus upper and lower distributions of consumers (≥1 serving per day), with values defined in Table 2. Year-specific tertiles allowed for temporal changes in dietary behaviors.
Table 1.
Specific Foodsa and Beveragesa Included in Each Food Groupb to Model Latent Factors for Hypothesized Dietary behaviors.
| Food group | Foods |
|---|---|
| Beef | Beef |
| Butter | Butter |
| Cheese | Cheese (reduced- low-, whole-fat) |
| Chips | Snack chips, vegetable-based savory snack |
| Diet drinks | Artificially sweetened: fruit drinks, soft drinks, water, tea |
| Fried chicken/seafood | Fried: chicken, shellfish, fish |
| Fruit | Citrus fruit, non-citrus fruit, fried fruits, fruit-based savory snacks |
| Fruit juice | Citrus fruit juice, non-fruit juice |
| Low-fat milk | Low-fat milk |
| Nuts | Nuts, nut butter |
| Potatoes | White potatoes, fried potatoes |
| Processed meat | Cold cuts, meat snack, cured pork |
| Refined grains | Refined grain: flours, and dry mixes, crackers, bread/rolls, pasta, cereals, snack bars |
| SSB | Sweetened: fruit drinks, soft drinks, water, tea |
| Sweets | Candy, frosting or glaze, sugar, syrup, honey, jam, jelly, preserves, cakes, cookies, cobblers, pies, pastries, Danish, doughnuts, desserts, frozen desserts, pudding |
| Unprocessed red meat | Veal, lamb, pork |
| Vegetables | Dark green, deep yellow, and other vegetables, avocado, and tomato, vegetable juice, fried vegetables |
| Whole grains | Whole grain grains, flours, and dry mixes, crackers, bread/rolls, pasta, cereals, |
| Whole milk | Whole milk |
| Yogurt | Yogurt |
SSB: Sugar-sweetened beverages
Diet was assessed using an interviewer-administered CARDIA Diet History (McDonald et al., 1991) Interviewers asked open-ended questions about dietary consumption in the past month within 100 food categories that referenced 1609 separate food items.
Using a food-grouping system modified from the University of Minnesota Nutrition Coordinating Center we assigned foods into one of 13 food groups and 5 beverage groups.
Table 2.
Reported Dietary behaviors (Means, [SD] and Range) Classified Into Low, Medium, and High Categories Across Exam Year: the Coronary Artery Risk Development in Young Adults (CARDIA) Study, 1985–2006, n=5114.
| Year 0 |
Year 7 |
Year 20 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | Category | Mean (SD) | Range | Category | Mean (SD) | Range | Category | |
| Fast food consumption per week | |||||||||
| 2.0 (0.03) | 0.0–0.5 | L | 1.9 (0.04) | 0.0–0.1 | L | 1.7 (0.05) | 0.0–0.1 | L | |
| 0.7–1.8 | M | 0.1–0.4 | M | 0.1–0.4 | M | ||||
| 2.0–21.0 | H | 0.4–5.9 | H | 0.4–5.9 | H | ||||
| Reported consumption of foods within food group (servings per day) | |||||||||
| Beef | 2.3 (0.03) | 0.0–1.1 | L | 1.8 (0.03) | 0.0–0.3 | L | 1.3 (0.02) | 0.0–0.2 | L |
| 1.1–2.4 | M | 0.5–1.8 | M | 0.5–1.6 | M | ||||
| 2.4–40.1 | H | 2.0–24.0 | H | 1.8–25.0 | H | ||||
| Unprocessed red meat | 0.5 (0.01) | 0.0–0.1 | L | 0.4 (0.01) | 0.0–0.0 | L | 0.4 (0.01) | 0.0–0.1 | L |
| 0.1–0.5 | M | 0.0–0.5 | M | 0.2–0.9 | M | ||||
| 0.5–14.8 | H | 0.5–24.0 | H | 0.9–25.5 | H | ||||
| Processed meat | 1.2 (0.02) | 0.0–0.4 | L | 1.0 (0.02) | 0.0–1.6 | L | 1.1 (0.02) | 0.0–0.8 | L |
| 0.5–1.3 | M | 1.6–3.8 | M | 0.8–2.1 | M | ||||
| 1.3–47.0 | H | 3.8–35.1 | H | 2.1–59.0 | H | ||||
| Fried chicken/seafood | 0.1 (0.01) | 0.0–0.0 | L | 0.3 (0.01) | 0.0–0.1 | L | 0.2 (0.01) | 0.0–0.1 | L |
| 0.0–0.1 | M | 0.1–0.7 | M | 0.1–0.6 | M | ||||
| 0.1–17.3 | H | 0.7–17.2 | H | 0.6–26.1 | H | ||||
| Potato chips | 0.3 (0.01) | 0.0–0.1 | L | 0.4 (0.01) | 0.0–0.4 | L | 0.4 (0.01) | 0.0–0.3 | L |
| 0.1–0.3 | M | 0.4–0.8 | M | 0.3–0.7 | M | ||||
| 0.3–12.0 | H | 0.8–8.0 | H | 0.7–10.1 | H | ||||
| Potatoes/fries | 0.7 (0.01) | 0.0–0.3 | L | 0.8 (0.02) | 0.0–0.7 | L | 0.0–0.7 | L | |
| 0.3–0.8 | M | 0.7–1.7 | M | 0.5 (0.01) | 0.7–1.8 | M | |||
| 0.8–14.3 | H | 1.7–19.6 | H | 1.8–31.8 | H | ||||
| Fruit | 1.4 (0.02) | 0.0–0.5 | L | 1.6 (0.03) | 0.0–0.0 | L | 1.7 (0.03) | 0.0–0.0 | L |
| 0.6–1.4 | M | 0.0–0.1 | M | 0.0–0.3 | M | ||||
| 1.4–16.2 | H | 0.1–16.2 | H | 0.3–22.5 | H | ||||
| Fruit juice | 1.9 (0.03) | 0.0–0.7 | L | 1.4 (0.03) | 0.0–0.0 | L | 1.0 (0.03) | 0.0–0.0 | L |
| 0.7–2.0 | M | 0.0–0.1 | M | 0.0–0.2 | M | ||||
| 2.0–36.1 | H | 0.1–8.0 | H | 0.2–7.0 | H | ||||
| Nuts | 0.7 (0.02) | 0.0–0.1 | L | 0.7 (0.02) | 0.0–0.4 | L | 1.1 (0.04) | 0.0–0.2 | L |
| 0.1–0.6 | M | 0.4–1.4 | M | 0.2–1.0 | M | ||||
| 0.6–21.2 | H | 1.4–47.9 | H | 1.0–16.5 | H | ||||
| Vegetables | 2.9 (0.04) | 0.0–1.6 | L | 3.5 (0.05) | 0.0–3.3 | L | 3.5 (0.05) | 0.0–2.1 | L |
| 1.6–3.1 | M | 3.3–5.6 | M | 2.1–3.8 | M | ||||
| 3.1–33.8 | H | 5.6–30.9 | H | 3.9–29.3 | H | ||||
| Whole grains | 1.1 (0.02) | 0.0–0.3 | L | 1.3 (0.02) | 0.0–1.5 | L | 1.2 (0.02) | 0.0–1.1 | L |
| 0.3–1.2 | M | 1.5–3.1 | M | 1.1–2.7 | M | ||||
| 1.3–13.0 | H | 3.1–35.3 | H | 2.7–73.6 | H | ||||
| Refined grains | 4.3 (0.04) | 0.0–2.6 | L | 5.1 (0.05) | 0.1–2.0 | L | 3.4 (0.04) | 0.0–2.1 | L |
| 2.6–4.9 | M | 2.0–3.8 | M | 2.1–3.8 | M | ||||
| 4.9–23.4 | H | 3.8–39.7 | H | 3.8–44.0 | H | ||||
| Sweets | 2.9 (0.04) | 0.0–1.4 | L | 2.9 (0.04) | 0.0–0.3 | L | 2.8 (0.08) | 0.0–0.1 | L |
| 1.4–3.2 | M | 0.3–1.5 | M | 0.1–0.8 | M | ||||
| 3.2–30.5 | H | 1.5–24.3 | H | 0.8–16.9 | H | ||||
| Butter | 4.4 (0.06) | 0.0–2.2 | L | 3.6 (0.06) | 0.0–0.0 | L | 2.0 (0.05) | 0.0–0.0 | L |
| 2.2–4.8 | M | 0.0–0.4 | M | 0.0–0.4 | M | ||||
| 4.8–53.6 | H | 0.4–19.2 | H | 0.4–8.6 | H | ||||
| Cheese | 0.7 (0.01) | 0.0–0.4 | L | 0.7 (0.01) | 0.0–0.8 | L | 0.6 (0.01) | 0.0–0.6 | L |
| 0.4–0.8 | M | 0.9–2.0 | M | 0.6–1.3 | M | ||||
| 0.8–6.3 | H | 2.0–34.5 | H | 1.3–12.3 | H | ||||
| Yogurt | 0.1 (0.00) | 0.0–0.0 | L | 0.1 (0.00) | 0.0–0.4 | L | 0.2 (0.01) | 0.0–0.5 | L |
| 0.0–0.1 | M | 0.4–1.1 | M | 0.5–1.1 | M | ||||
| 0.1–3.9 | H | 1.1–24.7 | H | 1.2–12.5 | H | ||||
| Low-fat milk | 0.9 (0.02) | 0.0–0.1 | L | 0.8 (0.02) | 0.0–0.5 | L | 0.7 (0.02) | 0.0–0.4 | L |
| 0.1–0.6 | M | 0.5–1.5 | M | 0.4–1.3 | M | ||||
| 0.6–36.0 | H | 1.5–14.9 | H | 1.4–15.5 | H | ||||
| Whole milk | 0.6 (0.02) | 0.0–0.0 | L | 0.2 (0.01) | 0.0–0.1 | L | 0.2 (0.01) | 0.0–0.1 | L |
| 0.0–1.0 | M | 0.1–0.4 | M | 0.1–0.3 | M | ||||
| 1.0–16.1 | H | 0.4–14.5 | H | 0.3–30.1 | H | ||||
| Artificially sweetened drinks | 0.9 (0.05) | 0.0–0.0 | L | 1.1 (0.03) | 0.0–0.3 | L | 1.2 (0.04) | 0.0–0.2 | L |
| 0.0–0.3 | M | 0.4–0.8 | M | 0.2–0.5 | M | ||||
| 0.3–182.1 | H | 0.8–13.1 | H | 0.5–13.5 | H | ||||
| SSB | 1.6 (0.03) | 0.0–0.4 | L | 1.4 (0.03) | 0.0–0.0 | L | 1.0 (0.03) | 0.0–0.0 | L |
| 0.4–1.6 | M | 0.0–0.9 | M | 0.0–1.0 | M | ||||
| 1.6–21.9 | H | 0.9–16.4 | H | 1.0–29.1 | H | ||||
SSB: Sugar sweetened beverages, L: low, M: medium, H: high.
We set reported dietary behaviors and BMI to missing when participants had extreme energy intakes (Sijtsma et al., 2012) [<800 or >8000 kcal/d for men (n=73 at year 0, n=60 at year 7, and n=25 at year 20); and <600 or >6000 kcal/d for women (n=53 at year 0, n=34 at year 7, and n=29 at year 20)] or when women were pregnant (n=7 at year 0, n=62 at year 7, and n=6 at year 20).
2.4. Neighborhood food environment
We used a geographical information system (GIS) of restaurants, food stores, and U.S. Census data that we geographically and temporally linked to CARDIA participants' home locations at years 0, 7, and 20. Study data were collected under written informed consent at each exam and protocols approved by Institutional Review Boards at each study center and the University of North Carolina at Chapel Hill.
We obtained counts of chain fast-food restaurants (hereafter referred to as fast food restaurants), all other restaurants not classified as chain fast food (hereafter referred to as sit-down restaurants), supermarkets, and convenience stores from Dun and Bradstreet (D&B), using 8-digit Standard Industrial Classification (SIC) codes for years 7, 10, 15, and 20 and a combination of 4 digit SIC codes and matched business names at year 0 (Table 3). We used a 3-km Euclidean buffer around each respondent's home location for restaurants because our previous research suggests that a 3-km buffer may be an appropriate distance for examining associations between neighborhood restaurant availability and individual level behavior (Boone-Heinonen et al., 2011). We used an 8-km buffer for food stores because of evidence that when people shop for food they are more likely to travel farther than 3 km (Drewnowski et al., 2012; Hillier et al., 2011; Kerr et al., 2012). We created densities of restaurants and food stores relative to roadway network (representing commercial development) rather than raw food resource counts to reduce spurious associations due to higher commercial development (more details provided in eAppendix 1). We included variables reflecting urbanicity and development as these relate to obesity (Wang et al., 2013) and the food environment. Population density varies across roadway structure (Levinson, 2012) and across rural versus urban areas (United States Census Bureau, 2010). In our data, population density and roadway length, representing commercial development, were independently associated with counts of each of neighborhood fast food restaurants, sit-down restaurant, supermarket, and convenience store densities. However, population density and roadway length were not highly correlated (□=0.35) in our dataset. Therefore, we included population density (Census tract population per square km of land excluding water) and we scaled food resource counts by dividing food store and restaurant counts by roadway length (representing commercial development) in our analyses.
Table 3.
Detailed Food Store and Restaurant Types Based on 8-digit Standard Industrial Classification (SIC) Codes.
| Food Resource Type | Description | SIC |
|---|---|---|
| Fast food chain restaurant | Fast-food restaurant, chain | 58120307 |
| Pizzeria, chain | 58120601 | |
| Sit-down restaurant | Fast food restaurants and stands | 58120300 |
| Box lunch stand | 58120301 | |
| Carry-out only (except pizza) restaurant | 58120302 | |
| Chili stand | 58120303 | |
| Coffee shop | 58120304 | |
| Delicatessen (eating places) | 58120305 | |
| Drive-in restaurant | 58120306 | |
| Fast-food restaurant, independent | 58120308 | |
| Food bars | 58120309 | |
| Grills (eating places) | 58120310 | |
| Hamburger stand | 58120311 | |
| Hot dog stand | 58120312 | |
| Sandwiches and submarines shop | 58120313 | |
| Snack bar | 58120314 | |
| Snack shop | 58120315 | |
| Pizza restaurants | 58120600 | |
| Pizzeria, independent | 58120602 | |
| Mexican Restaurants | 58120112 | |
| Seafood Restaurants: Includes sushi restaurants, oyster bars & seafood shacks: | 58120114 | |
| 58120700 | ||
| 58120701 | ||
| 58120702 | ||
| Steak House & BBQ Restaurants: | 58120800 | |
| 58120801 | ||
| 58120802 | ||
| Chicken Restaurants | 58129904 | |
| Family-owned restaurant chain | 58120501 | |
| Family-owned restaurant, non-chain: | 58120500 | |
| 58120502 | ||
| Supermarkets | Supermarkets, chain | 54110101 |
| Supermarkets, greater than 100,000 square feet (hypermarket) | 54110103 | |
| Supermarkets, independent | 54110102 | |
| Supermarkets, 55,000 – 65,000 square feet (superstore) | 54110104 | |
| Supermarkets, 66,000 – 99,000 square feet | 54110105 | |
| Supermarkets | 54110100 | |
| Convenience Stores | Variety stores | 53310000 |
| Convenience stores | 54110200 | |
| Convenience stores, chain | 54110201 | |
| Convenience stores, independent | 54110202 | |
| Gasoline service stations | 55410000 | |
| Gasoline service stations, not elsewhere classified | 55419900 | |
| Filling stations, gasoline | 55419901 |
2.5. Area-level socioeconomic indicators
Neighborhood SES was derived at the U.S. census tract-level at all years; tract-level SES is more strongly associated with health outcomes than block group-level SES (Krieger et al., 2003; Krieger et al., 2002). We consider neighborhood SES a latent construct comprised of multiple SES domains such as income and wealth, education, occupation, and housing. Multiple aspects of neighborhood SES may track together over time, such as poverty and unemployment. However, there may also be other unmeasured aspects of neighborhood SES that drive commercial zoning policies or economic incentives for food retailers and also impact BMI. Thus, we used a categorical variable that we derived in a previously published latent class analysis (Author et al., in press) using 20 years of Census tract data: % race white, % education <high school, % poverty (below 150% federal poverty level (United States Census Bureau, 2014)), % unemployed, % professional/management occupation, median income, % vacant housing, aggregate housing value, % owner occupied, and median rent to control for cumulative exposure to neighborhood SES. Given the longitudinal nature of the exposure, we created a 4-level variable that captured each participant's neighborhood SES throughout the study period: upwardly mobile, downwardly mobile, stable low, and stable high neighborhood SES (Author et al., in press). For example, the downwardly mobile residents lived in neighborhoods that had an increase in area-level poverty and a decrease in median rent over time.
2.6. Individual-level confounders
We characterized individual-level socioedemographic and behavioral confounders using data from questionnaires collected at each exam year (described in eAppendix 2).
2.7. Statistical analyses
We performed descriptive analyses and multivariable models using Stata 13.0 (StataCorp, College Station, TX). We calculated means and standard deviations (continuous variables) and percentages (categorical variables) of individual-level characteristics at exam years 0, 7, 10, 15, and 20 in an individual-level analysis.
SEM is a pathway-based approach that can handle multi-equation models, and allows estimation among latent (unobserved) and observed variables of multiple effects transmitted over combinations of paths (Bollen, 1987). SEMs are well-suited to estimate a range of effects (VanderWeele, 2012). We used Mplus version 7.11(Muthén and Muthén, 1998–2010) with maximum likelihood and statistical significance was set at P<0.05 (2-sided). Maximum likelihood estimation accounts for missing data at random and allows our model to use available data with needing to use imputation methods (Arbuckle, 1996; Allison, 2003).
2.7.1. Latent factors used in structural equation modeling
Latent factors are underlying complex concepts that are not directly observed, but can be inferred mathematically from multiple observed variables. Thus, latent factors are useful to summarize a number of variables into one meaningful factor. We constructed latent factors for diet behaviors and food environments. Briefly, at each year we created four latent factors for each neighborhood food store and restaurant type (fast food restaurant, sit-down restaurant, supermarket and convenience stores). We also created four latent diet factors for each year (fast food restaurant-type diet; sit-down restaurant-type diet, supermarket-type diet, and convenience store-type diet) using intake categories of foods we considered, a priori, typically offered at each type of establishment (e.g., fries from fast food restaurants, fruits from supermarkets) (Fig. 1). Specifically, we hypothesized that foods consumed at/from fast food restaurants include fast foods (e.g., processed and unprocessed meats, fried chicken/seafood, fries, sugar-sweetened beverages [SSB]); foods consumed at/from sit-down restaurants consist of meats, SSB, fruits, vegetables, cheeses, and whole grain food; foods consumed at/from convenience stores include convenience foods/beverages; foods consumed at/from supermarkets included foods/beverages from all groups except fried chicken/seafood, which are typically sold ready-to-eat from restaurants. A full description of methods to create latent diet factors is provided in eAppendix 1.
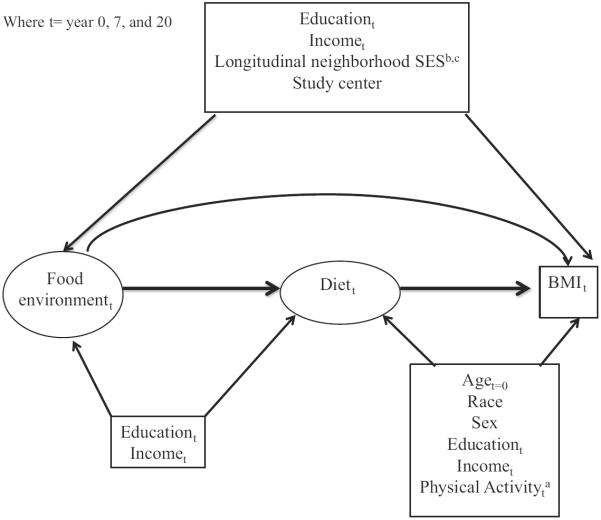
Fig. 1.
Dietary behaviors hypothesized to be associated with neighborhood restaurants and food stores.
2.7.2. Structural equation modeling
To test hypothesis 1 that neighborhood restaurants and food stores are associated with BMI through the consumption of specific foods we constructed a single SEM to examine longitudinal pathways from neighborhood food stores and restaurants to BMI, including direct and indirect pathways through dietary behaviors.
To test hypothesis 2 that the associations between neighborhood restaurants and food stores with dietary behaviors and BMI become stronger over time, we leveraged the longitudinal GIS and CARDIA data by including into our SEM longitudinal pathways. Fig. 2 presents our conceptual model of the longitudinal direct and indirect pathways of the food environment (neighborhood food stores and restaurants), BMI and diet, temporally related by auto-regression (linear association between time-lagged variables). The auto-correlation explicitly addresses the well-recognized tracking of health status and behaviors over time.
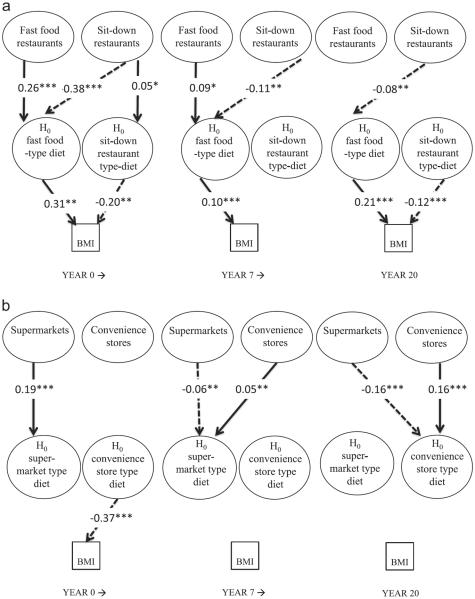
Fig. 2.
Conceptual model of temporal associations among direct pathways from neighborhood food environment to BMI, and indirect pathways through diet. BMI: Body mass index. Ovals represent latent (unobserved) variables and rectangles represent observed variables. Solid arrows represent causal relationships and dashed lines represent auto-regression (linear associations between time-lagged variables).
As described in Fig. 2, we hypothesized that tracking between the years closest in time is more relevant than across the full 20-year period, so we only included auto-regression between variables from years 0 to 7 and years 7 to 20. We hypothesized that the associations between the food environment, diet, and BMI operate concurrently, so we did not include pathways from the food environment to outcomes at later exams, except through tracking of the food environment over time. We also assumed that the food environment impacts diet, which in turn, impacts BMI and that the indirect effect of the food environment on BMI operates solely through diet. We allowed for direct effects of the food environment on BMI because there may be unmeasured factors in the food environment that influence BMI. For example, unmeasured features, such as the esthetics of natural and built environments, can be related to the numbers of and types of restaurants and food stores in the neighborhood and can also influence physical activity (Belon et al., 2014) and consequently BMI. We allowed BMI at time t to impact future diet at time t+1 by including pathways from BMI at year 0 to diet at year 7 and from BMI at year 7 to diet at year 20. For example, we included a pathway from BMI at year 0 to fast food-type diet at year 7. We assumed that all relationships were linear.
In addition, we considered several types of confounding variables (Fig. 3, with methods described in eAppendix 2). Briefly, we addressed confounding of associations between: (1) food environments and diet; (2) diet and BMI; and (3) food environments and BMI after excluding diet–BMI confounders that were likely affected by food environments (Cameron et al., 2013; Levinson, 2012; Valeri and Vanderweele, 2013; Zenk et al., 2006).
Fig. 3.
Conceptual model of confounding among the direct associations between neighborhood food and BMI, and indirect relationships through diet. BMI: Body mass index, SES: socioeconomics. Ovals represent latent (unobserved) variables and rectangles represent observed variables. aTime-varying physical activity was associated with baseline age, race, sex and current education and income. bDerived from latent class analysis (Richardson et al., 2014) using Mplus version 7.11 (Muthén and Muthén, 1998–2010). cLongitudinal neighborhood SES was associated with race, sex, baseline age, education, and income.
Our main interest was the indirect pathways from the food environment to BMI through diet, as presented in detail in Fig. 4. We hypothesized that stores and restaurants sell a variety of healthy and unhealthy foods, and dietary choices are theoretically made in the context of multiple offerings in the neighborhood (away-from-home eating involving a choice set of restaurants and in-home eating involving a choice set of food stores), rather than in isolation. We accounted for restaurant and food store options by including pathways from: fast food and sit-down restaurants to each of the fast food and sit-down restaurant diet factors; and supermarkets and convenience stores to each of the supermarket and convenience store diet factors.
Fig. 4.
Conceptual model of indirect pathways from neighborhood restaurants and food stores to BMI mediated through hypothesized diet behaviors. BMI: Body mass index. Ovals represent latent (unobserved) factors and rectangles represent observed variables. Solid arrows represent causal relationships. aLatent food environment factors indicated by: count of the food resources within 3 km (restaurants) or 8 km (food stores) Euclidean buffer per 10 km local/secondary roadway and population density Z-scores from U.S. Census-tract level data spatially linked to respondent residential locations and temporally linked to CARDIA exam years (Year 0, 1980; Years 7 and 10, 1990; Year 15 and 20, 2000). bLatent fast food-type diet indicated by: fast food consumption per week and servings per day of fried chicken/seafood, processed meats, unprocessed meats, beef, potatoes/fries, sweets/desserts, sugar-sweetened beverages, and diet drinks. cLatent sit-down restaurant-type diet indicated by: servings per day of processed meats, unprocessed meats, beef, potatoes/fries, sweets/desserts, sugar-sweetened beverages, diet drinks, butter, cheeses, refined grains, vegetables, and fruits. dLatent supermarket-type diet indicated by: servings per day of processed meats, unprocessed meats, beef, potatoes/fries, sweets/desserts, sugar-sweetened beverages, diet drinks, butter, cheeses, refined grains, vegetables, fruits, low-fat/skim milks, whole milks, yogurts, nuts, whole grains, 100% fruit juices, and potato chips. eLatent convenience store-type diet indicated by: servings per day of sweets/desserts, sugar-sweetened beverages, diet drinks, whole milks, 00% fruit juices, and potato chips.
2.7.2.1. Model fit
We defined good model fit as Root Mean Square Error of Approximation (RMSEA) <0.06 (Hu and Bentler, 1999), and Comparative Fit Index (CFI) (Bentler, 1990) and Tucker–Lewis Index (TLI) (Tucker and Lewis, 1973) values approaching 1.0.
2.7.2.2. Sensitivity analyses
There is less evidence about the salient buffer size to examine restaurants versus food stores, so we compared model fit for our models (restaurants within 3-km) to 1-km and 8-km buffer sizes.
Because our models were limited to years 0, 7, and 20, we assessed the impact of analyzing three versus five exam years of diet behavior measures collected from dietary survey. We used frequency of fast food restaurant visits (per week) collected from survey data at exam years 0, 7, 10, 15, and 20.
To contend with commercial development and density, we used roadway scaled counts of food stores and restaurants. However, such measures may not fully capture disparities of access (e.g., store size or other dimensions of access) and may be more difficult to draw policy implications from. Thus, we replicated our models using straight count variables for restaurants and foods stores. While counts of resources are typically skewed and zero-inflated, maximum likelihood tests in structural equation modeling are robust in cases when the normality assumptions are violated. (Browne, 1984; Satorra, 1990).
It is unclear how relationships between neighborhood food environments and obesity-related outcomes might vary by sex (Black and Macinko, 2010; Boone-Heinonen et al., 2011; Boone-Heinonen et al., 2010; Hou et al., 2010; Matheson et al., 2008), race (Black and Macinko, 2010; Borrell et al., 2004; Diez Roux et al., 2002; Kershaw et al., 2010; Schulz et al., 2008), and neighborhood socioeconomic status (SES) (Chichlowska et al., 2009; Matheson et al., 2008; Schulz et al., 2008). In addition, the CARDIA study centers are very different places (e.g., Birmingham versus Oakland) and relationships between neighborhood food environments and obesity-related outcomes might vary by geographic region (Ahern et al., 2011; Sharkey et al., 2009). Consequently, we tested interactions with two multi-group models (by sex, race, longitudinal neighborhood SES, and CARDIA study center): a model with freely estimated parameters for the pathways from the neighborhood fast food restaurants, sit-down restaurants, supermarkets, and convenience stores to diet and the pathways from the dietary behaviors to BMI; and a nested model with constrained parameters to equalize associations across groups. We used Likelihood Ratio tests to compare constrained versus freed models, where no statistically significant difference (P<0.05) indicated that parameters were similar between groups.
3. Results
3.1. Descriptive statistics
Mean income and years of schooling increased across 20 years of CARDIA exams, while physical activity decreased between year 0 and 7 then remained stable in later years (Table 4). Mean BMI increased from 24.5 to 29.4 kg/m2 between years 0 and 20. Diet behaviors changed throughout adulthood and the greatest differences were between exam years 0 and 7 (Table 2). Counts of neighborhood fast food and sit-down restaurants and convenience stores increased slightly, and supermarkets remained fairly stable over 20 years (Table 5). Fast food restaurants, sit-down restaurants, supermarkets, and convenience stores densities were correlated when pooled across years (p<0.0001) and pairwise correlations ranged from ρ=0.53 (supermarkets and sit-down restaurants) to ρ=0.72 (supermarkets and convenience stores). The majority of participants were classified by either high or low neighborhood SES stability versus upward and downward mobility based on 20 years of longitudinal neighborhood SES patterning.
Table 4.
Individual-level characteristics by exam year: Coronary Artery Risk Development in Young Adults (CARDIA), 1985/1986 to 2005/2006, n=5114.
| Year 0 | Year 7 | Year 10 | Year 15 | Year 20 | |
|---|---|---|---|---|---|
| N | 5114 | 4085 | 3949 | 3671 | 3549 |
| White race, % | 51.6 | 48.3 | 48.8 | 47.1 | 46.5 |
| Male sex, % | 45.5 | 44.9 | 44.4 | 44.1 | 43.3 |
| BMI (kg/m2), mean (SD) | 24.5 (0.1) | 26.7 (0.1) | 27.5 (0.1) | 28.7 (0.1) | 29.4 (0.1) |
| Educationa, mean (SD) y | 13.8 (0.0) | 14.7 (0.0) | 14.9 (0.0) | 15.2 (0.0) | 15.4 (0.0) |
| Incomeb, mean (SD) per $10,000 | 6.3 (0.1)a | 5.3 (0.1) | 5.6 (0.1) | 7.2 (0.1) | 8.0 (0.1) |
| Physical activity indexc, mean (SD) | 420 (4.2) | 338 (4.3) | 331 (4.4) | 347 (4.7) | 336 (4.6) |
BMI: Body mass index, SD: Standard deviation.
Highest year of education reported from year 0 through year 20.
Income per $10,000, inflated to year 20 and income was not queried at exam year 0 so closest measure at year 5 is used as a proxy.
Physical activity scores were calculated in exercise units based on frequency and intensity of each activity (Jacobs et al., 1989).
Table 5.
Neighborhood-level characteristics across exam year: the Coronary Artery Risk Development in Young Adults (CARDIA) Study, 1985–2006.
| Year 0 | Year 7 | Year 10 | Year 15 | Year 20 | |
|---|---|---|---|---|---|
| Number of census tracts | 799 | 2508 | 3406 | 3460 | 3645 |
| Counts of food resourcesa within 3 km (restaurants) or 8 km (food stores) Euclidean respondent residential buffer per 10 km of local and secondary roadways [median (interquartile range)]: | |||||
| Fast food restaurants | 0.2 (0.1,0.2) | 0.2 (0.1,0.3) | 0.2 (0.1,0.3) | 0.2 (0.1,0.3) | 0.4 (0.2,0.6) |
| Sit-down restaurants | 2.8 (1.4,5.1) | 3.4 (1.5,6.5) | 2.4 (1.2,4.7) | 2.7 (1.4,4.6) | 2.9 (1.5,5.3) |
| Supermarkets | 0.0 (0.0,0.1) | 0.1 (0.1,0.2) | 0.1 (0.0,0.1) | 0.1 (0.1,0.1) | 0.1 (0.1,0.2) |
| Convenience stores | 0.6 (0.5,0.7) | 1.0 (0.7,1.2) | 0.8 (0.6,0.9) | 0.7 (0.6,0.8) | 0.8 (0.6,1.0) |
| Longitudinal neighborhood SES residency patternb [% of participants] | |||||
| Downwardly mobile neighborhood SES | 19.8 | 17.7 | 18.0 | 17.1 | 17.2 |
| Stable low neighborhood SES | 30.9 | 30.0 | 29.9 | 29.6 | 28.5 |
| Upwardly mobile neighborhood SES | 13.0 | 13.9 | 14.1 | 14.8 | 15.2 |
| Stable high neighborhood SES | 36.3 | 38.3 | 38.0 | 38.6 | 39.1 |
Dunn & Bradstreet food resources.
Derived from latent class analysis using Mplus version 7.11 (Muthén and Muthén, 1998–2010) of Census tract-level data from exam years 0, 7, 10, 15, and 20: % race white, % education <high school, % poverty (below 150% federal poverty level), % unemployed, % professional/management occupation, median income, % vacant housing, aggregate housing value, % owner occupied, median rent (Richardson et al., 2014).
3.2. Structural equation modeling
The supplemental fit measures do not indicate good model fit to the data for Model 1 (Table 6). The, RMSEA is not less than 0.05 and the CFI, and TLI are near 0.6, far from ideal fit of 1. In contrast, the model fit indices improved for Model 2 after allowing the error terms to covary; RMSEA of 0.04 is less than 0.05 and CFI and TLI are approximately 0.8 which is closer to 1 than 0.5. Therefore we retained Model 2, which had better fit, as our final model.
Table 6.
Model fit estimates from structural equation models examining the pathways from neighborhood restaurants to BMI through hypothesized dietary behaviors: the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985–2006, n=5114.
| CFI | TLI | RMSEA | |
|---|---|---|---|
| Model 1 | 0.65 | 0.63 | 0.05 |
| Model 2 | 0.83 | 0.81 | 0.04 |
| Model 3 | 0.78 | 0.75 | 0.05 |
| Model 4 | 0.85 | 0.80 | 0.04 |
RMSEA: Root Mean Square Error of Approximation, CFI: Comparative Fit Index, TLI: Tucker–Lewis Index
Model 1: initial SEM tested as hypothesized in Fig. 4.
Model 2: Model 1+allowing the error terms to covary across and within the repeated neighborhood fast food restaurants, sit-down restaurants, supermarkets, convenience stores, dietary behaviors, BMI, education, income, and latent factors.
Model 3: Model 1 using counts of restaurants within 8 km Euclidean respondent residential buffer.
Model 4: Model 1 using counts of restaurants within 1 km Euclidean respondent residential buffer.
The standardized latent diet factor loadings reflected the degree to which dietary behaviors correlated with unique latent diet factors that we hypothesized would reflect the foods and beverages typically sold at different restaurants and food stores (Table 7).
Table 7.
Standardized factor loadings from structural equation measurement modelsa for latent neighborhood food resource and dietary behavior variables: the Coronary Artery Risk Development in Young Adults (CARDIA) Study, 1985–2006.
| Latent factors | Indicators | Factor loadings, λ (p-value) |
|||||
|---|---|---|---|---|---|---|---|
| Year 0 |
Year 7 |
Year 20 |
|||||
| λ | P-value | λ | P -value | λ | P -value | ||
| Neighborhood: | |||||||
| Fast food restaurants | Count of fast food restaurants within 3 km Euclidean buffer per 10 km of local and secondary roadwaysb,c | 1.00 | – | 1.00 | – | 1.00 | – |
| Population densityd | 0.12 | 0.000 | 0.17 | 0.000 | −0.09 | 0.000 | |
| Sit-down restaurants | Count of non-fast food restaurants within 3 km Euclidean buffer per 10 km of local and secondary roadwaysb,c | 1.00 | – | 1.00 | – | 1.00 | – |
| Population densityc | 0.38 | 0.000 | 0.36 | 0.000 | 0.53 | 0.000 | |
| Supermarkets | Count of supermarkets within 3 km Euclidean buffer per 10 km of local and secondary roadwaysb,c | 1.00 | – | 1.00 | – | 1.00 | – |
| Population densityd | −0.05 | 0.000 | 0.11 | 0.000 | 0.37 | 0.000 | |
| Convenience stores | Count of convenience stores within 3 km Euclidean buffer per 10 km of local and secondary roadwaysb,c | 1.00 | – | 1.00 | – | 1.00 | – |
| Population densityd | 0.40 | 0.000 | 0.34 | 0.000 | 0.19 | 0.000 | |
| Hypothesized dietary behaviors associated with: | |||||||
| Fast food restaurants | Fast food restaurant visits per weeke | 0.42 | 0.000 | 0.59 | 0.000 | 0.61 | 0.000 |
| Potatoes/fries | 0.25 | 0.000 | 0.10 | 0.854 | 0.10 | 0.005 | |
| Processed meats | 0.19 | 0.000 | 0.14 | 0.000 | 0.05 | 0.235 | |
| Beef | 0.13 | 0.003 | 0.11 | 0.000 | −0.06 | 0.137 | |
| Fried chicken/seafood | 0.08 | 0.001 | 0.51 | 0.000 | 0.47 | 0.000 | |
| Sweets/desserts | 0.20 | 0.000 | 0.04 | 0.172 | 0.04 | 0.234 | |
| SSB | 0.26 | 0.000 | 0.13 | 0.000 | 0.09 | 0.000 | |
| Diet drinks | 0.20 | 0.000 | 0.14 | 0.000 | 0.23 | 0.000 | |
| Sit-down restaurants | Refined grainse | 0.79 | 0.000 | 0.75 | 0.000 | 0.72 | 0.000 |
| Processed meats | 0.51 | 0.000 | 0.51 | 0.000 | 0.55 | 0.000 | |
| Potatoes/fries | 0.47 | 0.000 | 0.49 | 0.000 | 0.46 | 0.000 | |
| Beef | 0.67 | 0.000 | 0.66 | 0.000 | 0.69 | 0.000 | |
| Unprocessed red meat (pork/veal/lamb) | 0.53 | 0.000 | 0.51 | 0.000 | 0.43 | 0.000 | |
| Sweets/desserts | 0.18 | 0.000 | 0.29 | 0.000 | 0.19 | 0.000 | |
| SSB | 0.09 | 0.017 | 0.12 | 0.000 | 0.09 | 0.006 | |
| Diet drinks | −0.03 | 0.460 | 0.02 | 0.585 | −0.07 | 0.068 | |
| Cheese | 0.46 | 0.000 | 0.43 | 0.000 | 0.37 | 0.000 | |
| Vegetables | 0.33 | 0.000 | 0.24 | 0.000 | 0.06 | 0.013 | |
| Fruit | 0.15 | 0.000 | 0.02 | 0.243 | −0.06 | 0.000 | |
| Butter | 0.67 | 0.000 | 0.58 | 0.000 | 0.46 | 0.000 | |
| Supermarkets | Cheesee | 0.56 | 0.000 | 0.44 | 0.000 | 0.45 | 0.000 |
| Refined grains | 0.26 | 0.000 | 0.31 | 0.000 | 0.24 | 0.000 | |
| Potato chips | 0.19 | 0.002 | 0.23 | 0.000 | 0.18 | 0.000 | |
| Potatoes/fries | 0.29 | 0.000 | 0.26 | 0.000 | 0.17 | 0.000 | |
| Processed meats | 0.07 | 0.024 | 0.10 | 0.000 | 0.12 | 0.000 | |
| Unprocessed red meat (pork/veal/lamb) | 0.07 | 0.011 | 0.05 | 0.045 | 0.10 | 0.000 | |
| Beef | 0.24 | 0.000 | 0.14 | 0.000 | 0.20 | 0.000 | |
| Sweets/desserts | 0.36 | 0.000 | 0.34 | 0.000 | 0.29 | 0.000 | |
| SSB | −0.03 | 0.606 | 0.03 | 0.650 | 0.06 | 0.567 | |
| Diet drinks | 0.23 | 0.001 | 0.25 | 0.000 | 0.19 | 0.035 | |
| Vegetables | 0.69 | 0.000 | 0.64 | 0.000 | 0.58 | 0.000 | |
| Fruit | 0.45 | 0.000 | 0.46 | 0.000 | 0.41 | 0.000 | |
| Butter | 0.26 | 0.000 | 0.20 | 0.000 | 0.26 | 0.000 | |
| Juice | 0.50 | 0.000 | 0.43 | 0.000 | 0.41 | 0.000 | |
| Nuts | 0.35 | 0.000 | 0.27 | 0.000 | 0.41 | 0.000 | |
| Whole grains | 0.38 | 0.000 | 0.43 | 0.000 | 0.39 | 0.000 | |
| Yogurt | 0.49 | 0.000 | 0.43 | 0.000 | 0.39 | 0.000 | |
| Low-fat milk | 0.35 | 0.000 | 0.34 | 0.000 | 0.30 | 0.000 | |
| Whole milk | 0.06 | 0.508 | −0.05 | 0.494 | 0.06 | 0.146 | |
| Convenience stores | Whole milke | 0.50 | 0.000 | 0.38 | 0.000 | 0.20 | 0.000 |
| Sweets/desserts | 0.34 | 0.000 | 0.24 | 0.000 | 0.25 | 0.000 | |
| SSB | 0.24 | 0.000 | 0.36 | 0.000 | 0.52 | 0.000 | |
| Diet drinks | −0.39 | 0.000 | −0.40 | 0.000 | −0.48 | 0.000 | |
| Juice | 0.50 | 0.000 | 0.38 | 0.000 | 0.57 | 0.000 | |
| Potato chips | 0.50 | 0.000 | 0.20 | 0.000 | 0.18 | 0.000 | |
Derived from structural equation modeling using Mplus version 7.11 (Muthén and Muthén, 1998–2010)
Counts of Dunn & Bradstreet food resources.
Residual variances were set to zero to facilitate convergence.
Population density Z-scores from U.S. Census-tract level data spatially linked to respondent residential locations and temporally linked to CARDIA exam years (Year 0, 1980; Years 7, 1990; Year 15 and 20, 2000).
Referent indicator.
Throughout the 20-year study period, indirect pathways from fast food and sit-down restaurants to BMI, suggest statistically significant associations through dietary behaviors (P<0.05). Although derived simultaneously, we present the standardized beta coefficients (interpreted as the change in one standard deviation of the outcome per standard deviation change in the exposure) for restaurants in Fig. 5a and for food stores in Fig. 5b.
Fig. 5.
(a) Standardized estimates from structural equation models examining the indirect pathways from neighborhood restaurants to BMI through hypothesized diet behaviors: the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985–2006, n=5114. (b) Standardized estimates from structural equation models examining the indirect pathways from neighborhood food stores to BMI through hypothesized diet behaviors: the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985–2006, n=5114. Ovals represent latent (unobserved) variables and rectangles represent observed variables. The time varying and invariant covariates omitted from the figure for clarity were: longitudinal neighborhood SES residency pattern, center, age at year 0, race, and sex individual-level education, income, and physical activity. Arrows represent estimated associations. Further omitted for clarity were: direct pathways, pathways from BMI at time t to diet at time t+1, non-statistically significant associations (P≥0.05), indicators of latent variables, arrows for co-varying error terms, and the autoregressive pathways for the latent neighborhood fast food restaurants, sit-down restaurants, supermarkets, convenience stores, dietary behaviors, and the BMI measures. Model estimated with Mplus version 7.11 (Muthén and Muthén, 1998–2010) *P<0.05, **P<0.01, ***P<0.001.
Pathways from fast food restaurants to BMI and sit-down restaurants to BMI operated indirectly through a fast food-type diet. Greater numbers of neighborhood fast food restaurants were indirectly associated with higher BMI through greater consumption (year 0: β=0.27, P<0.001, year 7: β=0.08, P=0.04), while greater numbers of sit-down restaurants were indirectly associated with lower BMI through lower consumption (year 0: β=−0.39, P<0.001, year 7: β=−0.10, P=0.004, year 20: β=−0.07, P=0.02) of foods typically purchased from fast food restaurants. Consumption of a fast food-type diet was statistically significantly associated with higher BMI (year 0: β=0.36, P=0.001, year 7: β=0.10 P<0.001, year 20: β=0.21 P<0.001). Indirect pathways from supermarkets and convenience stores to BMI, through dietary behaviors were inconsistent. The SEM findings for restaurants were consistent with Hypothesis 1. Fast food and sit-down restaurants were associated with BMI through dietary behaviors (P<0.05). However, contrary to Hypothesis 2 the associations between fast food and sit-down restaurants, dietary behaviors and BMI did not change appreciably in magnitude or statistical significance over time.
For parsimony, we present separately the direct pathways and the temporal associations between BMI (time t) and diet (time t+1) findings in Table 8. There were only two statistically significant direct associations between the food environment and BMI: at baseline both fast food restaurants and sit-down restaurants were positively associated directly with BMI. There were three statistically significant associations between BMI and future fast food-, sit-down restaurant- and convenience store-type dietary behaviors, although the beta coefficients were close to zero in magnitude. We do not present the autoregressive associations, but all were positive and statistically significant (P<0.001), indicating tracking of exposures and outcomes over time.
Table 8.
Standardized estimates from structural equation modelsa examining the direct pathways from neighborhood food resources to BMI: the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985–2006, n=5114.
| β | P-value | ||
|---|---|---|---|
| Year 0 | |||
| BMI on: | Fast food restaurantsb | 0.13 | 0.002 |
| Sit-down restaurantsb | 0.12 | 0.03 | |
| Supermarketsb | 0.09 | 0.19 | |
| Convenience storesb | 0.01 | 0.56 | |
| Year 7 | |||
| BMI on: | Fast food restaurantsb | 0.02 | 0.31 |
| Sit-down restaurantsb | 0.00 | 0.93 | |
| Supermarketsb | 0.01 | 0.61 | |
| Convenience storesb | −0.02 | 0.06 | |
| Fast food-type diet on: | BMI at year 0 | −0.02 | <0.001 |
| Sit-down restaurant-type diet on: | BMI at year 0 | 0.01 | 0.002 |
| Supermarket-type diet on: | BMI at year 0 | 0.001 | 0.77 |
| Convenience store-type diet on: | BMI at year 0 | −0.002 | 0.75 |
| Year 20 | |||
| BMI on: | Fast food restaurantsb | −0.01 | 0.61 |
| Sit-down restaurantsb | 0.02 | 0.26 | |
| Supermarketsb | 0.02 | 0.22 | |
| Convenience storesb | −0.03 | 0.10 | |
| Fast food-type diet on: | BMI at year 7 | −0.005 | 0.24 |
| Sit-down restaurant-type diet on: | BMI at year 7 | −0.002 | 0.62 |
| Supermarket-type diet on: | BMI at year 7 | 0.003 | 0.46 |
| Convenience store-type diet on: | BMI at year 7 | −0.01 | 0.03 |
BMI: Body mass index.
Derived from structural equation modeling using Mplus version 7.11 (Muthén and Muthén, 1998–2010)
Latent factors modeled with by: counts of Dunn & Bradstreet food resources within Euclidean 3 km buffer per 10 km local and secondary roadways and population density (U.S. Census-tract level data spatially linked to respondent residential locations and temporally linked to CARDIA exam years (Year 0, 1980; Year 7, 1990; and 20, 2000).
By modeling neighborhood SES as a confounder we estimated the associations from neighborhood SES to the food environments and from neighborhood SES to BMI. We found a positive association between neighborhood socioeconomic advantage with higher density of restaurants and lower density of food stores at year 0, but in later years socioeconomic advantage was associated with lower density of restaurants and food stores. While the associations varied across the food stores and restaurants and by year, the overall pattern suggests that over time neighborhood socioeconomic disadvantage was associated with greater densities of restaurants and food stores (data not shown).
3.3. Sensitivity analyses
Our original model with 3-km buffer (Model 1) fit the data better than a model with an 8-km buffer (Model 3), and similar fit to a model with a 1-km buffer (Model 4), as shown in Table 6.
The patterns of association were similar in the model using weekly fast food restaurant visits measured at years 0, 7, and 20, compared to the identical model with fast food restaurant visits at all exam years (Web Fig. 1a and b).
Estimates from the sensitivity model using straight counts of restaurants and food stores were similar to the results from our central model which used counts scaled by roadway length (Web Fig. 2a and b). However, the estimated effects of restaurants on dietary behaviors were attenuated. The sensitivity model results for straight counts of food stores showed inconsistent results, similar to those for the roadway-scaled counts shown in the central analysis.
Tests for interactions by race (P=1.00), sex (P=1.00), long-itudinal neighborhood SES residency pattern (P=1.00), and center (P=1.00) were not statistically significant
4. Discussion
Using SEM, environmental- and individual-level data spanning two decades in the U.S., we found that pathways from neighborhood restaurants to BMI might operate through higher consumption of an obesogenic fast food-type diet (e.g., French fries and sugar sweetened beverages). Living near fast food restaurants was associated with greater consumption of foods typically consumed at fast food restaurants, while living near sit-down restaurants was associated with lower consumption of a fast food-type diet. Yet, we found no direct or indirect pathways from neighborhood supermarkets and convenience stores to BMI through dietary behaviors.
Research on the food environment, dietary behaviors, and body weight has proliferated over the past several years, yet most of this literature is cross-sectional and ignores multiple direct and indirect pathways from different types of restaurants and food stores to BMI through dietary behaviors (Ball et al., 2012; Hattori et al., 2013; Kegler et al., 2014; Pruchno et al., 2014). Further, the bulk of the literature involves a black box-step from the food environment to BMI and is largely mixed [see reviews (Giskes et al., 2011; Mackenbach et al., 2014)]. Inconsistent findings in the literature might relate to patterning by neighborhood SES (Baker et al., 2006; Borrell et al., 2004; Carson et al., 2007; Kershaw et al., 2010; Morland et al., 2002a; Morland et al., 2002b; Author et al., 2012; Author et al., in press; Zenk et al., 2005), by individual-level SES (Author et al., 2011) or by geographic location (Ahern et al., 2011; Sharkey et al., 2009). However, none of these studies accounted for complex pathways from neighborhood fast food restaurants, sit-down restaurants, supermarkets, and convenience stores to BMI through dietary behaviors.
Our findings support our hypothesis that fast food restaurants impact weight gain through diet behaviors. In contrast, in one of the few longitudinal studies in the Framingham Heart Study Offspring Cohort, Block et al. (2011) found no consistent association between neighborhood fast food and full-service restaurants with BMI. Yet, Block et al. (2011) used distance to nearest outlet to characterize the food environment, rather than the range of alternative neighborhood restaurants and food stores that we considered in our study. In (Author et al., 2011), we used longitudinal CARDIA data to examine fast food restaurant and supermarket availability in separate models where each model did not account for the availability of other restaurants and food stores. In the current study, we accounted for separate pathways in one model from fast food restaurants, sit-down restaurants, supermarkets and convenience stores to dietary behaviors hypothesized to be associated with restaurants, food stores and BMI.
We did not expect to find that higher numbers of sit-down restaurants could lead to reduced BMI through reduced consumption of foods typically consumed at fast food restaurants. While sit-down restaurants offer some of the same foods and beverages as fast food restaurants they typically offer a wider variety of foods with less obesogenic options (e.g., vegetables). It is also possible that presence of sit-down restaurants may reflect unmeasured features of the neighborhood.
Counter to our hypothesis, we found no statistically significant pathways from neighborhood supermarkets and convenience stores to BMI (either directly or through diet behaviors). In (Author et al., in press), we found that the most socioeconomically deprived neighborhoods (compared to socioeconomically advantaged neighborhoods) had consistently greater numbers of convenience stores, despite similar numbers of supermarkets.
The lack of pathways from supermarkets to BMI in our study suggests that the number of supermarkets in a neighborhood, regardless of the SES of that neighborhood, does not substantially relate to diet behaviors or BMI. This finding could relate to the rise in new food and beverage products from the mid-1990s through 2010 offered in food stores [e.g., candy and snacks] (Economic Research Service - USDA, 2013), which could allow consumers to purchase a fast food-style diet from supermarkets, particularly given that supermarkets and convenience stores sell a mix of unhealthy and healthy food options (Bodor et al., 2010; Gustafson et al., 2013; Hutchinson et al., 2012; Rose et al., 2010).
We found very few direct pathways from food environments to BMI. After accounting for indirect pathways from neighborhood restaurants and food stores to BMI through diet, direct pathways from neighborhood food environments to BMI did not contribute consistently to BMI. Findings from our model suggest that associations in previous studies between food environments and BMI (Mehta and Chang, 2008; Pruchno et al., 2014), reflect a combination of measured and unmeasured direct and indirect pathways. In addition, we did not find strong evidence that baseline BMI is associated with future dietary behaviors 7 or 13 years later.
Our study has limitations. Electronic business record data (e.g., D&B) are vulnerable to geospatial inaccuracy and misclassification (Bader et al., 2010; Fleischhacker et al., 2012). A ground-truthed study in Chicago and surrounding suburban/rural Census tracts found higher validity (D&B business listings compared to ground-truthed food store and restaurant locations) in white versus predominantly black race Census tracts and in high compared to low-to-middle income tracts (Powell et al., 2011). However differences could relate to urbanicity. The CARDIA study recruited participants from four major U.S. cities and after 20 years, over 90% of them were still living either in or less than a mile away from an urban area. Therefore, differential misclassification in our data by urbanicity is not likely.
We lacked diet history data from exam years 10 and 15, yet sensitivity models comparing three versus five exam years of fast food visit data indicated similar patterns of association between restaurants and BMI through dietary behaviors. Dietary recall may be biased; however, we had repeated measures of diet from three exam periods spanning 20 years. To facilitate model convergence we categorized dietary behaviors into low, medium, and high. However, this approach may miss temporal changes that reflect food environmental influences of diet and BMI. This could bias our findings either towards or away from the null.
Residential location choice is complex and driven by more than dietary preferences. However, individual diet preferences and behaviors may be tied to unobserved characteristics (e.g., health consciousness) that underlie an individual's residential location. Not accounting for this path (individual influence on environment) might bias any paths we estimate in the other direction (environment influence on individual), which requires a model of substantial recursive complexity that allows for individual variation and warrants future research.
We hypothesized that the associations between the food environment, diet, and BMI operate concurrently, so we did not include pathways from the food environment to outcomes at later exams, except through tracking of the food environment over time. Our rationale stems from the fact that at a single point in time a person is only able to consume foods that are present at that same point in time. Certainly neighborhoods today are a function of their past and people may tend to live in similar types of neighborhoods over time. Therefore, we include autoregressive pathways that account for the tracking of food environments over time. We did not include pathways from current food stores and restaurants to future diet behaviors. However, we allowed neighborhood SES to have a temporal influence because people may experience neighborhood SES changes over time as their neighborhoods change or as they move to new neighborhoods. Using this approach we controlled for the participant's longitudinal residential SES history.
We did not use raw counts of restaurant and food store in our main model because they may reflect commercial development and can create spurious associations. For example, low SES neighborhoods located in dense inner-city areas may have more convenience stores than high SES neighborhoods because they have more businesses in general, and not necessarily because of disparities in the food environment. Commercial development, dense and connected roadways, and population density can track together as businesses and infrastructure respond to population demand for and access to businesses. Thus, to separate restaurant and food store disparities from other contextual features of the neighborhoods, we addressed commercial development by scaling food resource measures by roadway length and controlling for population density. While we did not use network buffers, we addressed differences in food resources according to overall commercial activity by scaling counts by roadway length while holding Euclidean area constant across geographic areas varying in terrain and network distances. Thus, the resources relative to roadway lengths provides measures relative to road network, whereas the Euclidean buffers provide the salient geographic area of focus.
The above modeling approach allows us to compare neighborhood disparities across a spectrum of population and commercial densities. Access is a complex construct as it reflects more than just simple availability of stores and restaurants (e.g., store sizes may be larger in more dense areas). In sensitivity analyses, we replaced roadway-scaled counts of restaurants and food stores with straight counts. In general, findings were similar using counts except that the estimated effects of restaurants on dietary behaviors were attenuated. We opted for the roadway scaled measures (Romley et al., 2007) in the central analysis as we wished to account for commercial development and potential routes of travel. Indeed, that we observed stronger associations between restaurants and dietary behaviors using roadway-scaled relative to those using straight counts may reflect that access to restaurants along roadways may play a role in eating away-from-home. However, we acknowledge that there may remain unmeasured differences in access by commercial development or other social or economic factors. Nonetheless our count results shown in the Web Fig. 2a and b provide policy relevance in terms of a true count of physical restaurants and food stores.
Testing a linear trend over time in the estimated effect of food environment on BMI is not feasible in the SEM context. However, we can examine how the effect sizes of the associations between the food environments, dietary behaviors and BMI change over time. If a linear trend exists then we would expect the effects sizes to increase in magnitude as the exam year increased. We did not observe evidence that the effect of the food environments on BMI increased over time. Our findings do not support a linear trend of the food environment on obesity from young to late adulthood.
We assumed our estimates were not confounded by unmeasured factors, but sensitivity methods to address unmeasured bias (VanderWeele, 2010) do not exist for longitudinal SEMs. Thus, unmeasured confounding could bias our estimates away from or towards the null. Lastly, we present one causal model but there may be other valid causal models. While our findings shed light on the mechanism of how the food environment influences diet and BMI, they do not definitively clarify the underlying relationships between diet behaviors, restaurants and food stores.
Despite these limitations, this study had several strengths, including using a large and unique GIS capturing multiple types of neighborhood restaurants and food stores, spatial characteristics, and demographics, with detailed diet and anthropometric data. We modeled latent factors and hypothesized causal relationships with longitudinal data from a large cohort during early- to late-adulthood. We used multiple dietary behaviors we hypothesized would be associated with restaurants and food stores. We included separate direct and indirect (through dietary behaviors) associations from neighborhood food stores and restaurants on BMI. We accounted for other restaurant (fast food versus sit-down) and food store (supermarkets versus convenience stores) options. While we controlled for physical activity which declined over time there are other factors that could contribute to weight gain over 13 years, such as previous BMI, race/ethnicity, and SES. All are accounted for in our model. In addition, age is related to dietary behaviors and BMI, thus we included baseline age as a confounder of dietary behaviors and BMI. How people interact with their environments, what and where they choose to purchase and consume food is complex. Traditional regression models of a single exposure and a single outcome cannot capture these complexities. Pathway-based modeling is a step towards disentangling which features of the food environment should be modified to influence dietary behaviors and improve health outcomes.
5. Conclusion
The food environment consists of a variety of food stores and restaurants that can influence dietary intake. When we considered multiple direct and indirect pathways from fast food and sit-down restaurants, supermarkets, and convenience stores to BMI, through dietary behaviors, we found that neighborhood fast food and sit-down restaurants may play a comparatively greater role than food stores in relation to individual-level dietary behaviors and BMI.
Supplementary Material
Acknowledgments
The authors would like to acknowledge CARDIA Chief Reviewer Kiarri Kershaw, whose thoughtful suggestions improved the paper. The authors have no financial or other conflict of interest to disclose. Andrea Richardson had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis. All authors contributed significantly to this work. This work was funded by the National Heart, Lung, and Blood Institute (NHLBI) R01HL104580. The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the NHLBI, the Intramural Research Program of the National Institute on Aging (NIA), and an intra-agency agreement between NIA and NHLBI (AG0005). For general support, the authors are grateful to the Carolina Population Center, University of North Carolina at Chapel Hill (Grant R24HD050924 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development [NICHD]), the Nutrition Obesity Research Center (NORC), University of North Carolina (grant P30DK56350 from the National Institute for Diabetes and Digestive and Kidney Diseases [NIDDK]), and the UNC Center for Environmental Health and Susceptibility (CEHS), University of North Carolina (Grant P30ES010126 from the National Institute of Environmental Health Sciences [NIEHS]). NIH had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. This manuscript has been reviewed by CARDIA for scientific content. There were no potential or real conflicts of financial or personal interest with the financial sponsors of the scientific project.
Abbreviations
- BMI
Body mass index
- CARDIA
Coronary Artery Risk Development in Young Adults
- CFI
Comparative fit index
- kg
kilogram
- m
meter
- SEM
Structural equation modeling
- SES
Socioeconomic status
- SD
Standard deviation
- SSB
Sugar-sweetened beverage
- RMSEA
Root mean square error approximation
- TLI
Tucker–Lewis Index
Footnotes
Appendix A. Suplementary Information Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.healthplace.2015.09.003.
References
- Ahern M, Brown C, Dukas S. A national study of the association between food environments and county-level health outcomes. J. Rural Health Off. J. Am. Rural Health Assoc. Natl. Rural Health Care Assoc. 2011;27:367–379. doi: 10.1111/j.1748-0361.2011.00378.x. [DOI] [PubMed] [Google Scholar]
- Author, et al. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch. Intern. Med. 2011;171:1162–1170. doi: 10.1001/archinternmed.2011.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Author, et al. Are neighbourhood food resources distributed inequitably by income and race in the USA? Epidemiological findings across the urban spectrum. BMJ Open. 2012;2:e000698. doi: 10.1136/bmjopen-2011-000698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Author, et al. Neighborhood socioeconomic status and food environment: a 20-year longitudinal latent class analysis among CARDIA participants. Soc. Sci. Med. 2015 doi: 10.1016/j.healthplace.2014.08.011. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bader MD, Ailshire JA, Morenoff JD, House JS. Measurement of the local food environment: a comparison of existing data sources. Am. J. Epidemol. 2010;171:609–617. doi: 10.1093/aje/kwp419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker EA, Schootman M, Barnidge E, Kelly C. The role of race and poverty in access to foods that enable individuals to adhere to dietary guidelines. Prev. Chronic Dis. 2006;3:A76. [PMC free article] [PubMed] [Google Scholar]
- Ball K, Abbott G, Cleland V, Timperio A, Thornton L, Mishra G, Jeffery RW, Brug J, King A, Crawford D. Resilience to obesity among socioeconomically disadvantaged women: the READI study. Int. J. Obes. (Lond.) 2012;36:855–865. doi: 10.1038/ijo.2011.183. [DOI] [PubMed] [Google Scholar]
- Belon AP, Nieuwendyk LM, Vallianatos H, Nykiforuk CI. How community environment shapes physical activity: perceptions revealed through the PhotoVoice method. Soc. Sci. Med. 2014;116:10–21. doi: 10.1016/j.socscimed.2014.06.027. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative Fit Indexes in Structural Models. Psychol. Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Black JL, Macinko J. The changing distribution and determinants of obesity in the neighborhoods of New York City, 2003–2007. Am. J. Epidemiol. 2010;171:765–775. doi: 10.1093/aje/kwp458. [DOI] [PubMed] [Google Scholar]
- Block JP, Christakis NA, O'Malley AJ, Subramanian SV. Proximity to food establishments and body mass index in the Framingham Heart Study offspring cohort over 30 years. Am. J. Epidemiol. 2011;174:1108–1114. doi: 10.1093/aje/kwr244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. Am. J. Prev. Med. 2004;27:211–217. doi: 10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- Bodor JN, Rice JC, Farley TA, Swalm CM, Rose D. Disparities in food access: does aggregate availability of key foods from other stores offset the relative lack of supermarkets in African-American neighborhoods? Prev. Med. 2010;51:63–67. doi: 10.1016/j.ypmed.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA. Total, direct, and indirect effects in structural equation models. Sociol. Methodol. 1987;17:37–69. [Google Scholar]
- Boone-Heinonen J, Guilkey DK, Evenson KR, Gordon-Larsen P. Residential self-selection bias in the estimation of built environment effects on physical activity between adolescence and young adulthood. Int. J. Behav. Nutr. Phys. Act. 2010;7:70. doi: 10.1186/1479-5868-7-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell LN, Diez Roux AV, Rose K, Catellier D, Clark BL. Neighbourhood characteristics and mortality in the atherosclerosis risk in communities study. Int. J. Epidemiol. 2004;33:398–407. doi: 10.1093/ije/dyh063. [DOI] [PubMed] [Google Scholar]
- Browne MW. Asymptotically distribution-free methods for the analysis of covariance structures. Br. J. Math. Stat. Psychol. 1984;37(Pt 1):62–83. doi: 10.1111/j.2044-8317.1984.tb00789.x. [DOI] [PubMed] [Google Scholar]
- Burgoine T, Lake AA, Stamp E, Alvanides S, Mathers JC, Adamson AJ. Changing foodscapes 1980–2000, using the ASH30 study. Appetite. 2009;53:157–165. doi: 10.1016/j.appet.2009.05.012. [DOI] [PubMed] [Google Scholar]
- Cameron AJ, Thornton LE, McNaughton SA, Crawford D. Variation in supermarket exposure to energy-dense snack foods by socio-economic position. Public Health Nutr. 2013;16:1178–1185. doi: 10.1017/S1368980012002649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson AP, Rose KM, Catellier DJ, Kaufman JS, Wyatt SB, Diez-Roux AV, Heiss G. Cumulative socioeconomic status across the life course and subclinical atherosclerosis. Ann. Epidemiol. 2007;17:296–303. doi: 10.1016/j.annepidem.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18:1172–1187. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chichlowska KL, Rose KM, Diez-Roux AV, Golden SH, McNeill AM, Heiss G. Life course socioeconomic conditions and metabolic syndrome in adults: the Atherosclerosis Risk in Communities (ARIC) Study. Ann. Epidemiol. 2009;19:875–883. doi: 10.1016/j.annepidem.2009.07.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff. (Millwood) 2014;33:283–291. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Jacobs DR, Kiefe CI. Neighborhood characteristics and components of the insulin resistance syndrome in young adults: the coronary artery risk development in young adults (CARDIA) study. Diabetes Care. 2002;25:1976–1982. doi: 10.2337/diacare.25.11.1976. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Aggarwal A, Hurvitz PM, Monsivais P, Moudon AV. Obesity and supermarket access: proximity or price? Am. J. Public Health. 2012;102:e74–e80. doi: 10.2105/AJPH.2012.300660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffey KJ, Gordon-Larsen P, Jacobs DR, Jr., Williams OD, Popkin BM. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: the Coronary Artery Risk Development in Young Adults Study. Am. J. Clin. Nutr. 2007;85:201–208. doi: 10.1093/ajcn/85.1.201. [DOI] [PubMed] [Google Scholar]
- Duffey KJ, Steffen LM, Van Horn L, Jacobs DR, Jr., Popkin BM. Dietary patterns matter: diet beverages and cardiometabolic risks in the longitudinal Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am. J. Clin. Nutr. 2012;95:909–915. doi: 10.3945/ajcn.111.026682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Economic Research Service - USDA The Demans for Food Away from Home - Full Service or Fast Food. Agric. Econ. Rep. 2004;829 [Google Scholar]
- Economic Research Service - USDA . New Products. 2013. [Google Scholar]
- Fleischhacker SE, Rodriguez DA, Evenson KR, Henley A, Gizlice Z, Soto D, Ramachandran G. Evidence for validity of five secondary data sources for enumerating retail food outlets in seven American Indian communities in North Carolina. Int. J. Behav. Nutr. Phys. Act. 2012;9:137. doi: 10.1186/1479-5868-9-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foresight . Tackling Obesities: Future Choices – Obesenogenic Environments – Evidence Review. Government Office for Science; London: 2007. [Google Scholar]
- Gary-Webb TL, Baptiste-Roberts K, Pham L, Wesche-Thobaben J, Patricio J, Pi-Sunyer FX, Brown AF, Jones L, Brancati FL. Neighborhood and weight-related health behaviors in the Look AHEAD (Action for Health in Diabetes) study. BMC Public Health. 2010;10:312. doi: 10.1186/1471-2458-10-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson DM. The neighborhood food environment and adult weight status: estimates from longitudinal data. Am. J. Public Health. 2011;101:71–78. doi: 10.2105/AJPH.2009.187567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giskes K, van Lenthe F, Avendano-Pabon M, Brug J. A systematic review of environmental factors and obesogenic dietary intakes among adults: are we getting closer to understanding obesogenic environments? Obes. Rev. : Off. J. Int. Assoc. Study Obes. 2011;12:e95–e106. doi: 10.1111/j.1467-789X.2010.00769.x. [DOI] [PubMed] [Google Scholar]
- Gustafson A, Christian JW, Lewis S, Moore K, Jilcott S. Food venue choice, consumer food environment, but not food venue availability within daily travel patterns are associated with dietary intake among adults, Lexington Kentucky 2011. Nutr. J. 2013;12:17. doi: 10.1186/1475-2891-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattori A, An R, Sturm R. Neighborhood food outlets, diet, and obesity among California adults, 2007 and 2009. Prev. Chronic Dis. 2013;10:E35. doi: 10.5888/pcd10.120123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillier A, Cannuscio CC, Karpyn A, McLaughlin J, Chilton M, Glanz K. How far do low-income parents travel to shop for food? Empirical evidence from two urban neighborhoods. Urban Geogr. 2011;32:712–729. [Google Scholar]
- Hou N, Popkin BM, Jacobs DR, Jr., Song Y, Guilkey D, Lewis CE, Gordon-Larsen P. Longitudinal associations between neighborhood-level street network with walking, bicycling, and jogging: the CARDIA study. Health Place. 2010;16:1206–1215. doi: 10.1016/j.healthplace.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new laternatives. Struct. Equ. Model. 1999;6:1–55. [Google Scholar]
- Hutchinson PL, Nicholas Bodor J, Swalm CM, Rice JC, Rose D. Neigh-bourhood food environments and obesity in southeast Louisiana. Health Place. 2012;18:854–860. doi: 10.1016/j.healthplace.2012.03.006. [DOI] [PubMed] [Google Scholar]
- Jacobs DR, Hahn LP, Haskell WL, Pirie P, Sidney S. Validity and reliability of short physical activity history: Cardia and the Minnesota Heart Health Program. J. Cardiopulm. Rehabil. 1989;9:448–459. doi: 10.1097/00008483-198911000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kegler MC, Swan DW, Alcantara I, Feldman L, Glanz K. The influence of rural home and neighborhood environments on healthy eating, physical activity, and weight. Prev. Sci.: Off. J. Soc. Prev. Res. 2014;15:1–11. doi: 10.1007/s11121-012-0349-3. [DOI] [PubMed] [Google Scholar]
- Kerr J, Frank L, Sallis JF, Saelens B, Glanz K, Chapman J. Predictors of trips to food destinations. Int. J. Behav. Nutr. Phys. Act. 2012;9:58. doi: 10.1186/1479-5868-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Diez Roux AV, Carnethon M, Darwin C, Goff DC, Jr., Post W, Schreiner PJ, Watson K. Geographic variation in hypertension prevalence among blacks and whites: the multi-ethnic study of atherosclerosis. Am. J. Hypertens. 2010;23:46–53. doi: 10.1038/ajh.2009.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures – the public health disparities geocoding project. Am. J. Public Health. 2003;93:1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am. J. Epidemiol. 2002;156:471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- Lenard J. Convenience Store Growth. NACS Online. 2012 http://www.nacsonline.com/MAGAZINE/PASTISSUES/2012/February2012/Pages/Feature1.aspx.
- Let's Move. 2012 http://www.letsmove.gov/
- Levinson D. Network Structure and City Size. PloS one. 2012;7(1) doi: 10.1371/journal.pone.0029721. http://dx.doi.org/10.1371/journal.pone.0029721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenbach JD, Rutter H, Compernolle S, Glonti K, Oppert JM, Charreire H, De Bourdeaudhuij I, Brug J, Nijpels G, Lakerveld J. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health. 2014;14:233. doi: 10.1186/1471-2458-14-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson FI, Moineddin R, Glazier RH. The weight of place: a multilevel analysis of gender, neighborhood material deprivation, and body mass index among Canadian adults. Soc. Sci. Med. 2008;66:675–690. doi: 10.1016/j.socscimed.2007.10.008. [DOI] [PubMed] [Google Scholar]
- McDonald A, Van Horn L, Slattery M, Hilner J, Bragg C, Caan B, Jacobs D, Jr., Liu K, Hubert H, Gernhofer N, et al. The CARDIA dietary history: development, implementation, and evaluation. J. Am. Diet. Assoc. 1991;91:1104–1112. [PubMed] [Google Scholar]
- McLaren L. Socioeconomic status and obesity. Epidemiol. Rev. 2007;29:29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- Mehta NK, Chang VW. Weight status and restaurant availability a multilevel analysis. Am. J. Prev. Med. 2008;34:127–133. doi: 10.1016/j.amepre.2007.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health . A Portrait of Health: Key Results of the 2002/03 New Zealand Health Survey. Minist. Health; Wellingt: 2004. 2004. [Google Scholar]
- Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am. J. Public Health. 2006;96:325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR, Franco M. Fast-food consumption, diet quality, and neighborhood exposure to fast food: the multi-ethnic study of atherosclerosis. Am. J. Epidemiol. 2009;170:29–36. doi: 10.1093/aje/kwp090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K, Filomena S. Disparities in the availability of fruits and vegetables between racially segregated urban neighbourhoods. Public Health Nutr. 2007;10:1481–1489. doi: 10.1017/S1368980007000079. [DOI] [PubMed] [Google Scholar]
- Morland K, Wing S, Diez Roux A. The contextual effect of the local food environment on residents' diets: the atherosclerosis risk in communities study. Am. J. Public Health. 2002a;92:1761–1767. doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am. J. Prev. Med. 2002b;22:23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N. Engl. J. Med. 2011;364:2392–2404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. Muthén & Muthén; Los Angeles, CA: 1998&;2010. [Google Scholar]
- National Association of Convenience Stores (NACS) NACS State of the Industry Report of 2010 Data. 2011 http://www.vpcga.com/files/public/NACSIndustryOverview_6-2011.pdf.
- National Restaurant Association Facts at a glance. 2013 http://www.restaurant.org/News-Research/Research/Facts-at-a-Glance.
- Powell LM, Han E, Zenk SN, Khan T, Quinn CM, Gibbs KP, Pugach O, Barker DC, Resnick EA, Myllyluoma J, Chaloupka FJ. Field validation of secondary commercial data sources on the retail food outlet environment in the U. S. Health Place. 2011;17:1122–1131. doi: 10.1016/j.healthplace.2011.05.010. [DOI] [PubMed] [Google Scholar]
- Pruchno R, Wilson-Genderson M, Gupta AK. Neighborhood food environment and obesity in community-dwelling older adults: individual and neighborhood effects. Am. J. Public Health. 2014;104:924–929. doi: 10.2105/AJPH.2013.301788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romley JA, Cohen D, Ringel J, Sturm R. Alcohol and environmental justice: the density of liquor stores and bars in urban neighborhoods in the United States. J. Stud. Alcohol Drugs. 2007;68:48–55. doi: 10.15288/jsad.2007.68.48. [DOI] [PubMed] [Google Scholar]
- Rose D, Bodor JN, Hutchinson PL, Swalm CM. The importance of a multidimensional approach for studying the links between food access and consumption. J. Nutr. 2010;140:1170–1174. doi: 10.3945/jn.109.113159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satorra A. Robustness issues in structural equation modeling: a review of recent developments. Qual. Quant. 1990;24:367–386. [Google Scholar]
- Schulz AJ, Zenk SN, Israel BA, Mentz G, Stokes C, Galea S. Do neighborhood economic characteristics, racial composition, and residential stability predict perceptions of stress associated with the physical and social environment? Findings from a multilevel analysis in Detroit. J. Urban Health: Bull. N. Y. Acad. Med. 2008;85:642–661. doi: 10.1007/s11524-008-9288-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey JR, Horel S, Han D, Huber JC., Jr. Association between neighborhood need and spatial access to food stores and fast food restaurants in neighborhoods of colonias. Int. J. Health Geogr. 2009;8:9. doi: 10.1186/1476-072X-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sijtsma FP, Meyer KA, Steffen LM, Shikany JM, Van Horn L, Harnack L, Kromhout D, Jacobs DR., Jr. Longitudinal trends in diet and effects of sex, race, and education on dietary quality score change: the Coronary Artery Risk Development in Young Adults study. Am. J. Clin. Nutr. 2012;95:580–586. doi: 10.3945/ajcn.111.020719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DM, Cummins S, Taylor M, Dawson J, Marshall D, Sparks L, Anderson AS. Neighbourhood food environment and area deprivation: spatial accessibility to grocery stores selling fresh fruit and vegetables in urban and rural settings. Int. J. Epidemiol. 2010;39:277–284. doi: 10.1093/ije/dyp221. [DOI] [PubMed] [Google Scholar]
- Smith LP, Ng SW, Popkin BM. Resistant to the recession: low-income adults' maintenance of cooking and away-from-home eating behaviors during times of economic turbulence. Am. J. Public Health. 2014;104:840–846. doi: 10.2105/AJPH.2013.301677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Food Trust . Pennsylvania Fresh Food Financing Initiative 2010. 2004. [Google Scholar]
- The Reinvestment Fund . Understanding the Grocery Industry. In: Fund C, editor. Understanding the Grocery Industry. Capacity Building Inititative; 2011. [Google Scholar]
- Tseng M, Thornton LE, Lamb KE, Ball K, Crawford D. Is neighbourhood obesogenicity associated with body mass index in women? Application of an obesogenicity index in socioeconomically disadvantaged neighbourhoods. Health Place. 2014;30:20–27. doi: 10.1016/j.healthplace.2014.07.012. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. Reliability Coefficient for Maximum Likelihood Factor-Analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- United States Census Bureau 2010 Census Urban Area Facts: Most Densely Populated Areas. 2010 www.census.gov/geo/reference/ua/uafacts.html.
- United States Census Bureau How the Census Bureau Measures Poverty. Poverty. 2014 http://www.census.gov/hhes/www/poverty/about/overview/measure.html.
- Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol. Methods. 2013;18:137–150. doi: 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ. Bias formulas for sensitivity analysis for direct and indirect effects. Epidemiology. 2010;21:540–551. doi: 10.1097/EDE.0b013e3181df191c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ. Invited commentary: structural equation models and epidemiologic analysis. Am. J. Epidemiol. 2012;176:608–612. doi: 10.1093/aje/kws213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F, Wen M, Xu Y. Population-Adjusted Street Connectivity, Urbanicity and Risk of Obesity in the U.S. Appl. Geogr. 2013;41:1–14. doi: 10.1016/j.apgeog.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization WHO Global Infobase. 2011 https://apps.who.int/infobase/
- World Health Organization . Global Nutrition Policy Review: What Does it Take to Scale Up Nutrition Action? WHO Document Production Services Geneva; Switzerland: 2013. [Google Scholar]
- Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am. J. Public Health. 2005;95:660–667. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Fruit and vegetable access differs by community racial composition and socioeconomic position in Detroit, Michigan. Ethn. Dis. 2006;16:275–280. [PubMed] [Google Scholar]
- Zick CD, Stevens RB. Trends in Americans' food-related time use: 1975–2006. Public Health Nutr. 2006;13:1064–1072. doi: 10.1017/S1368980009992138. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.