Abstract
Background
Cardio-metabolic risk factors are of increasing concern in HIV-infected individuals, particularly with the advent of antiretroviral therapy (ART) and the subsequent rise in longevity. However, the prevalence of cardio-metabolic abnormalities in this population and the differential contribution, if any, of HIV specific factors to their distribution, are poorly understood. Therefore, we conducted a systematic review and meta-analysis to estimate the global prevalence of metabolic syndrome (MS) in HIV-infected populations, its variation by the different diagnostic criteria, severity of HIV infection, ART used and other major predictive characteristics.
Methods
We performed a comprehensive search on major databases for original research articles published between 1998 and 2015. The pooled overall prevalence as well as by specific groups and subgroups were computed using random effects models.
Results
A total of 65 studies across five continents comprising 55094 HIV-infected participants aged 17–73 years (median age 41 years) were included in the final meta-analysis. The overall prevalence of MS according to the following criteria were: ATPIII-2001:16.7% (95%CI: 14.6–18.8), IDF-2005: 18% (95%CI: 14.0–22.4), ATPIII-2004-2005: 24.6% (95%CI: 20.6–28.8), Modified ATPIII-2005: 27.9% (95%CI: 6.7–56.5), JIS-2009: 29.6% (95%CI: 22.9–36.8), and EGIR: 31.3% (95%CI: 26.8–36.0). By some MS criteria, the prevalence was significantly higher in women than in men (IDF-2005: 23.2% vs. 13.4, p = 0.030), in ART compared to non-ART users (ATPIII-2001: 18.4% vs. 11.8%, p = 0.001), and varied significantly by participant age, duration of HIV diagnosis, severity of infection, non-nucleoside reverse transcriptase inhibitors (NNRTIs) use and date of study publication. Across criteria, there were significant differences in MS prevalence by sub-groups such as in men, the Americas, older publications, regional studies, younger adults, smokers, ART-naïve participants, NNRTIs users, participants with shorter duration of diagnosed infection and across the spectrum of HIV severity. Substantial heterogeneities across and within criteria were not fully explained by major study characteristics, while evidence of publication bias was marginal.
Conclusions
The similar range of MS prevalence in the HIV-infected and general populations highlights the common drivers of this condition. Thus, cardio-metabolic assessments need to be routinely included in the holistic management of the HIV-infected individual. Management strategies recommended for MS in the general population will likely provide similar benefits in the HIV-infected.
Introduction
The Global Burden of Disease Expert Group estimated that approximately 30 million people were infected with HIV worldwide in 2013, the majority of whom reside in sub-Saharan Africa [1]. Life expectancy and quality of life in those infected with HIV have improved dramatically with the introduction of effective antiretroviral therapy (ART). Between 1990 and 2013, ART saved an estimated 19.1 million life-years in HIV-infected adults [1].
With increased longevity in HIV-infected individuals other diseases are likely to develop, similar to the general population. These include obesity, type 2 diabetes mellitus (T2DM) and other cardio-metabolic diseases. Although exposure to risky behaviours of unhealthy diets and reduced physical activity levels contribute to these conditions [2], additional influences unique to HIV-infected populations further increase their susceptibility to cardio-metabolic abnormalities. For example, the use of ART is associated with body fat redistribution and cardio-metabolic abnormalities such as hypertension, dyslipidaemia, insulin resistance, and dysglycaemia [3]. Moreover, HIV infection itself through chronic inflammation and immune dysfunction mechanisms is assumed to be an important determinant of dyslipidaemia, atherosclerosis and T2DM [4].
Cardio-metabolic abnormalities frequently cluster and manifest as the metabolic syndrome (MS), a constellation of interrelated metabolic disorders comprising abdominal obesity, raised blood pressure, dyslipidaemia and hyperglycaemia. The importance of the MS is that it is a powerful predictor of future cardiovascular disease and T2DM [5]. Therefore, determining the magnitude of MS in a given population highlights the need for preventive and management strategies, and enables healthcare services planning.
This is particularly relevant in HIV-infected populations who have the potential to develop cardio-metabolic abnormalities and MS through multiple pathways. Notably, the prevalence of MS in HIV-infected populations and the differential contributions, if any, of HIV specific influences on the estimates have yet to be fully examined. Accordingly, we conducted a systematic review and meta-analysis to assess the MS prevalence and its relationship with HIV specific characteristics in the global HIV-infected population.
Methods
Identification of relevant studies
We undertook a comprehensive electronic search across major databases including Medline, CINAHL, Academic Search Premier, Africa-Wide Information and Scopus to identify relevant studies. The search terms comprised combinations of MESH terms, CINAHL headings, and free words relating to prevalence, metabolic syndrome, and HIV/AIDS (S1 Table). Additionally, we traced the citations of identified articles via the ISI Web of Knowledge, and scanned the reference lists of review papers and conference proceedings. We also examined publications on the websites of key organisations such as UNAIDS, WHO, and International AIDS Society. We limited the search to studies reported from January 1998 to April 2015 because highly active antiretroviral therapy (HAART) was introduced only in 1996 [6] and the first MS criteria were defined in 1998 [7]. The last search data was 30th April 2015.
Selection of included studies
Two investigators (KAN and NP) independently reviewed the studies by title, abstract and full text where relevant for inclusion. Disagreements were resolved by consensus or by consulting a third investigator (APK). Included studies had to: 1) be population- or hospital-based cross-sectional studies, 2) comprise adults diagnosed with HIV-infection, treated or not; 3) report the prevalence of MS overall and by different subgroups of interest, according to any of the internationally accepted diagnostic criteria for MS (S3 Table); or provide enough data to estimate this prevalence; and 4) be published in English or French. We made no restriction by sample size, sampling methods or study setting. For studies reported more than once, the article with the largest number of participants was used. If an article reported multiple surveys conducted in different countries, each survey was counted as a separate study (Fig 1).
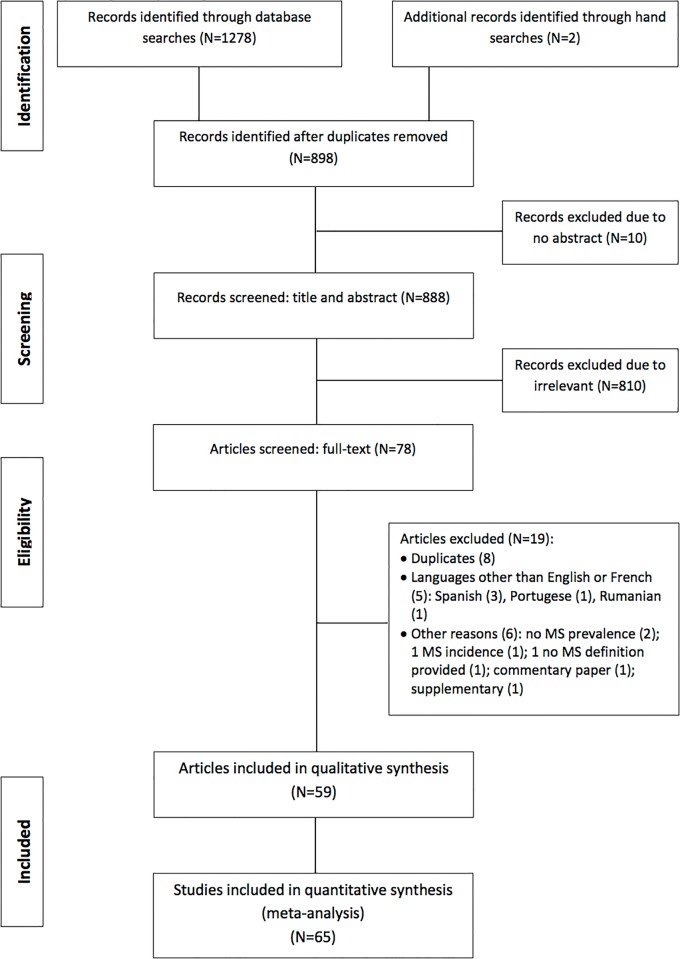
Fig 1. Flow diagram for the selection of studies.
Assessment of the methodological quality of included studies
We evaluated the methodological quality of the included studies using a checklist adapted from Hoy et al. [8]. It consists of nine questions that assesses the representativeness of the sample, the sampling technique, the response rate, the data collection method, the measurement tools, the case definitions, and the statistical reporting. Each checked question was scored either as “1” or “0” corresponding respectively to “low risk of bias” and “high risk of bias”. The total score ranged from 0 to 9 with the overall score categorised as follows: 7 to 9: “low risk of bias”, 4 to 6: “moderate risk”, and 0 to 3: “high risk” (S2 Table). For each included study, we also estimated the precision (C) or margin of error, considering the sample size (SS) and the observed prevalence (p) of MS from the formula SS = Z2*p*(1-p)/C2 where Z was the z-value fixed at 1.96 across studies (corresponding to 95% confidence interval). The desirable margin of error was 5% (0.05) or lower.
Data extraction
Relevant data for this review were extracted using a purposeful design and a piloted extraction form. The information extracted included 1) Author details [names and year of publication]; 2) Study characteristics [country, study design, setting, data source, sampling method, sample size, data collection period, response rate]; 3) Participants’ characteristics [age, gender, lifestyle habits (smoking, alcohol misuse), HIV-related factors [time since diagnosis, severity of the disease, ART regimens and duration of treatment]; and 4) MS characteristics [diagnostic criteria used, prevalence, number of participants tested and diagnosed with MS overall and by subgroups of interest].
Data synthesis and analysis
For each included study, the unadjusted prevalence of MS was estimated (number with MS/total number of participants tested) overall and across major subgroups of interest. We used DerSimonian-Laird random effects models to combine estimates from different studies to generate the overall prevalence of MS according to each diagnostic criteria. The random effects model was chosen over the fixed effects in anticipation of substantial variations in MS prevalence estimates across the included studies. To minimise the effect of extreme prevalence on the overall estimates, we first stabilised the variance of the raw prevalence with a single arcsine transformation before pooling the data [9].
To account for the small number of studies that applied some definition criteria, and also to account for similarities between some criteria, a decision was made to group together studies that applied the Adult Treatment Panel III (ATPIII)-2004 and ATPIII-2005 criteria into the ATPIII-2004-2005 group. Furthermore, studies that applied variants of the same criteria (e.g. through the substitution of variables) were assessed together with studies that applied the original criteria.
We assessed the heterogeneity between studies using the Cochran’s Q, I2 and H statistics [10]. Noteworthy is that statistical approaches to assess heterogeneity can yield spurious results within uncontrolled studies [11]. We explored the sources of heterogeneity by comparing the prevalence of MS between subgroups defined by naturally occurring categories (e.g. gender and geographic regions), or by using median values of the summary estimates of the continuous characteristics (e.g. age, ART duration) across all eligible studies. Subgroups comparisons then used the Q-test based on the Analysis of the Variance (ANOVA). Publication bias was assessed using the funnel plots supplemented by formal statistical assessments using the Egger test of bias [12]. All analyses were performed using the R programme (version 3.0.3 [2014-03-06]) and “meta” package.
The following sections report the findings of the systematic review and meta-analyses. The data are presented by the overall MS prevalence as well as by subgroups of age, gender, HIV-related factors, study location, publication year, sample size, and smoking status. Within each subgroup, MS prevalence is presented by the definition criteria used.
Results
The review process
The process for selecting the relevant studies is summarised in Fig 1. In total, 1280 records were identified via database searches. After removing all duplicates, we scanned the titles and abstracts of 888 articles, of which 78 articles were further reviewed via full-texts. Of these, 59 articles met the inclusion criteria and were selected for this review. One article reported surveys conducted in seven South American countries, leading to a total of 65 studies in the main analyses.
Methodological quality of included studies
In all, 18 studies were categorised as having a low risk of bias while the remainder had a moderate risk of bias. However, 37 studies did not indicate how participants were selected; seven studies reported some form of random selection whereas 21 studies indicated a non-random sampling technique. A total of 25 studies reported the response rates which ranged from 31.2% to 100% (median 88%).
Characteristics of included studies
The characteristics of the included studies are summarised in Table 1. Studies from all continents were represented as follows: Europe: 23, the Americas: 26, Africa: nine and Asia: four, while three studies were intercontinental. Of the 65 included studies, 33 were localised studies, mainly conducted in urban settings, while the rest had national coverage. With regards to the actual study sites, the majority (58) were solely hospital- or clinic-based, four were community-based and three studies involved both locales. While about half of the studies (34) collected data before or during 2007, only one-fifth (12 studies) were published in the same period.
Table 1. Characteristics of the studies included in the review.
| Reference | Publication year | Country | Area | Study site | Study type | Study period | Sampling | Sample size | Response rate (%) | Mean age (years) | Selection criteria | Quality grade * (Risk) | Precision (margin of error) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intercontinental | |||||||||||||
| Samaras, et al [25] | 2007 | USA, Europe, Australia, Asia, South America | National | Hospital + community | C/C | Not provided | Unspecified | 788 | NR | - | Age ≥ 17 years; not diagnosed with AIDS | Low | 0.03 |
| Wand, et al [28] | 2007 | Australia, Brazil, Canada, New Zealand, 17 Europrean countries | Urban | Hospital | C/S | 1999–2002 | Random | 881 | 94 | 38.7 | Adults not receiving ART | Low | 0.02 |
| Worm, et al [52] | 2010 | USA, Australia, 21 European countries | National | Hospital (212 clinics) | C/S | 2006–2007 | Not random | 23852 | NR | 38 | Adults on ART and regular follow-up | Low | 0.01 |
| Americas | |||||||||||||
| Baum, et al [16] | 2006 | USA | National | Community | C/S | 2002–2003 | Unspecified | 118 | NR | 41.7 | Adult chronic drug users | Moderate | 0.06 |
| Jacobson, et al [37] | 2006 | USA | Urban | Community | C/S | 2000–2003 | Unspecified | 477 | NR | - | Self-selected | Moderate | 0.04 |
| Johnsen, et al [27] | 2006 | USA | National | Hospital | C/C | 2002–2003 | Unspecified | 97 | NR | 41 | Women with BMI≥20 kg/m2 and only on ART chronic medications | Moderate | 0.09 |
| Mondy, et al [44] | 2007 | USA | Urban | Hospital | C/S | 2005 | Not random | 471 | 78 | - | All clinic attendees during the study period | Moderate | 0.04 |
| Adeyemi, et al [60] | 2008 | USA | Urban | Hospital | C/S | 2005–2006 | Unspecified | 121 | NR | 54 | Age ≥ 50 years; outpatient | Moderate | 0.09 |
| Sobieszczyk, et al [32] | 2008 | USA | Urban | Hospital + community | C/S | 2000–2004 | Unspecified | 1725 | NR | 40 | Women | Low | 0.02 |
| Sterling, et al [18] | 2008 | USA | Urban | Hospital | C/S | 1998–2006 | Unspecified | 222 | 82 | 45.4 | Adults co-infected with HCV | Moderate | 0.04 |
| Ances, et al [61] | 2009 | USA | National | Hospital | C/C | Not provided | Unspecified | 66 | NR | 41 | Cryptogenic stroke (case subgroup) | Moderate | 0.09 |
| Pullinger, et al [24] | 2010 | USA | Urban | Community | C/S | 2005–2007 | Unspecified | 296 | 84.6 | 45.3 | Age ≥ 18 years; diagnosed duration ≥3 months | Moderate | 0.05 |
| Krishnan, et al [38] | 2012 | USA | National | Hospital | C/S | 2001–2007 | random | 2247 | 88 | - | Age ≥13 years | Low | 0.02 |
| Hadigan, et al [62] | 2013 | USA | Urban | Hospital (2 clinics) | C/S | 2007–2011 | Not random | 182 | 72 | 45 | Absence of chronic NCDs or co-infection | Moderate | 0.05 |
| Tiozzo, et al [63] | 2015 | USA | Urban | Hospital | C/S | 2013 | Not random | 89 | 90 | 48 | Age ≥18 years on ART | Moderate | 0.1 |
| Da Silva, et al [64] | 2009 | Brazil | Urban | Hospital (7 centres) | C/S | 2004–2006 | Not random | 319 | NR | 39.5 | ART use ≥ 2 months, and no anti- lipid agents | Moderate | 0.04 |
| Cahn, et al [23] | 2010 | 7 Latin American countries | National | Hospital (61 centres) | C/S | 2006–2007 | Unspecified | 4010 | NR | 41.9 | ART use ≥1 month | Moderate | 0.01 |
| Leite, et al [30] | 2010 | Brazil | Urban | Hospital | C/S | 2008 | Unspecified | 100 | NR | - | - | Moderate | 0.1 |
| Ramirez-Marrero, et al [20] | 2010 | Puerto Rico | Urban | Hospital + community | C/S | 2003–2007 | Random | 897 | 31.2 | 44.7 | - | Low | 0.03 |
| Lauda, et al [65] | 2011 | Brazil | Urban | Hospital | C/S | 2007–2008 | Unspecified | 249 | NR | - | Age ≥18 years | Moderate | 0.05 |
| Alencastro, et al [66] | 2012 | Brazil | Urban | Hospital | C/S | Not provided | Not random | 1240 | 96 | 38.6 | Age 18–79 years | Low | 0.02 |
| Gasparotto, et al [67] | 2012 | Brazil | National | Hospital (multiple-centres) | C/S | Not provided | Unspecified | 614 | NR | 42.6 | Age ≥18 years; ART use ≥1 year; viral load ≤50 copies/ml | Moderate | 0.04 |
| Signorini, et al [43] | 2012 | Brazil | National | Hospital | C/S | 2005 | Unspecified | 819 | NR | 41 | Age ≥18 years | Low | 0.03 |
| Europe | NR | ||||||||||||
| Gazzaruso, et al [68] | 2003 | Italy | National | Hospital | C/S | Not provided | Unspecified | 287 | NR | 41 | ART use | Moderate | 0.05 |
| Jerico, et al [19] | 2005 | Spain | Urban | Hospital | C/S | 2003 | Unspecified | 710 | 88 | 41.9 | Age ≥20 years; no evidence of AIDS or ART disruption | Low | 0.03 |
| Bergersen, et al [69] | 2006 | Norway | Urban | Hospital | C/S | 2000–2001 | Not random | 263 | 78 | 43.3 | - | Moderate | 0.04 |
| Estrada, et al [70] | 2006 | Spain | National | Hospital | C/S | Not provided | Not random | 146 | NR | 40.6 | ART use ≥6 months, no active opportunistic affection | Moderate | 0.06 |
| Bonfanti, et al [71] | 2007 | Italy | Urban | Hospital (18 centers) | C/S | 2005 | Not random | 1243 | 98.4 | 43.2 | - | Moderate | 0.02 |
| Palacios, et al [51] | 2007 | Spain | National | Hospital | C/S | 2002–2003 | Unspecified | 60 | 81 | 40.9 | ART use ≥48 weeks | Moderate | 0.09 |
| Badiou, et al [49] | 2008 | France | National | Hospital | C/S | 1999 | Not random | 232 | NR | 41 | - | Low | 0.04 |
| Martin, et al (SHIVA study) [26] | 2008 | France | Urban | Hospital | C/S | 2003 | Unspecified | 140 | 86.9 | - | - | Moderate | 0.04 |
| Schillaci, et al [72] | 2008 | Italy | Urban | Hospital | C/C | Not provided | Unspecified | 39 | NR | 37 | Outpatients; no ART | Moderate | 0.12 |
| Hansen, et al [73] | 2009 | Denmark | National | Hospital | C/S | 2004–2006 | Unspecified | 566 | 75.7 | 44.1 | Age ≥18 years | Low | 0.04 |
| Young, et al [74] | 2009 | Switzerland | National | Hospital | C/S | 2000–2006 | Unspecified | 1644 | 70 | - | ART use | Low | 0.02 |
| Bonfanti, et al [50] | 2010 | Italy | Urban | Hospital (14 centers) | C/S | 2007 | Not random | 292 | NR | 37 | Age ≥18 years; ART naive | Moderate | 0.04 |
| Calza, et al [75] | 2011 | Italy | Urban | Hospital | C/S | 2009 | Not random | 755 | NR | 37 | Outpatients | Moderate | 0.02 |
| Cubero, et al [42] | 2011 | Spain | National | Hospital | C/S | Not provided | Not random | 159 | NR | 39 | 1st line ART regimen, no kidney or liver disease, no lipid modifying treatment or hormone use | Moderate | 0.07 |
| Elgalib, et al [41] | 2011 | UK | Urban; Peri-urban | Hospital (2 centers) | C/S | 2005–2006 | Random | 678 | 66.4 | 39.5 | - | Low | 0.03 |
| Freitas, et al [29] | 2011 | Portugal | National | Hospital | C/S | Not provided | Unspecified | 345 | NR | 43.8 | ART use lipodystrophy | Moderate | 0.05 |
| Guaraldi, et al [76] | 2011 | Italy | National | Hospital (2 centers) | C/S | 2007–2008 | Unspecified | 103 | NR | 46.9 | Age ≥18 years on ART | Moderate | 0.06 |
| Janiszewski et al [77] | 2011 | Italy | National | Hospital | C/S | 2005–2009 | Unspecified | 2322 | NR | - | ART use ≥ 18 months | Moderate | 0.02 |
| Biron, et al [47] | 2012 | France | National | Hospital (5 centers) | C/S | 2000–2007 | Not random | 269 | 85.7 | 43 | Aged ≥18 years, ART use for 1–4 years without disruption | Low | 0.05 |
| Guaraldi, et al [31] | 2012 | Italy | National | Hospital (2 centers) | C/S | 2009–2010 | Unspecified | 133 | NR | - | Men, sexually active in the 4 last weeks | Moderate | 0.07 |
| Maloberti, et al [54] | 2013 | Italy | National | Hospital | C/S | Not provided | Unspecified | 108 | NR | - | Free of known CVD risk factors | Moderate | 0.07 |
| De Socio, et al (HIV-Hy study) [21] | 2014 | Italy | National | Hospital | C/S | 2010–2011 | Not random | 765 | 93 | 45.6 | - | Moderate | 0.03 |
| Sawadogo, et al [22] | 2014 | Burkina Faso | Urban | Hospital | C/S | 2011 | Random | 400 | NR | 41.4 | Age ≥18 years; ART use ≥ 6 months | Moderate | 0.03 |
| Africa | |||||||||||||
| Zannou, et al [17] | 2009 | Benin | Urban | Hospital | C/S | 2004–2005 | Unspecified | 79 | 90 | 38 | Age ≥ 16 years; ART use; not obese | Moderate | 0.07 |
| Awotedu, et al [13] | 2010 | South Africa | Urban | Hospital | C/S | 2009–2010 | Not random | 196 | NR | 36.8 | No lipid modifying medications | Moderate | 0.07 |
| Fourie, et al [78] | 2010 | South Africa | Urban; Rural | Community | C/S | 2005 | Random | 300 | NR | 44 | Aged ≥35 years; no chronic medications or self-reported disease | Moderate | 0.05 |
| Ayodele, et al [48] | 2012 | Nigeria | Urban | Hospital | C/S | Not provided | Not random | 291 | 94 | 39.5 | No liver or thyroid disease or concurrent infections | Moderate | 0.05 |
| Berhane, et al [79] | 2012 | Ethiopia | Urban | Hospital | C/S | 2010 | Not random | 313 | 100 | - | Age ≥18 years, ART use ≥6 weeks | Moderate | 0.05 |
| Muhammad, et al [80] | 2013 | Nigeria | Urban | Hospital | C/S | 2009 | Not random | 200 | NR | 32.5 | Age ≥18 years; not diagnosed with hypertension, diabetes or dyslipidaemia before commencing ART | Moderate | 0.05 |
| Ngatchou, et al [15] | 2013 | Cameroon | Urban | Hospital | C/S | 2009–2010 | Not random | 108 | NR | 39 | ART-naïve adults; no documented diabetes, hypertension or dyslipidaemia | Moderate | 0.09 |
| Mbunkah, et al [46] | 2014 | Cameroon | National | Hospital | C/S | 2010–2011 | Unspecified | 173 | 100 | 38.7 | - | Low | 0.05 |
| Tesfaye, et al [45] | 2014 | Ethiopia | Urban | Hospital | C/S | 2013 | Random | 374 | 97.2 | 32.6 | Age ≥18 years | Low | 0.04 |
| Asia | |||||||||||||
| Gupta, et al [40] | 2011 | India | Urban | Hospital | C/S | 2007–2009 | Not random | 68 | NR | 35.9 | ART-naïve; no chronic medications | Moderate | 0.1 |
| Wu, et al [14] | 2012 | Taiwan | National | Hospital | C/S | 2008–2009 | Unspecified | 803 | 60.2 | - | Age ≥18 years | Low | 0.03 |
| Bajaj, et al [81] | 2013 | India | Urban | Hospital | C/S | 2010–2011 | Not random | 70 | NR | - | No comorbid diabetes or hypertension | Moderate | 0.09 |
| Jantarapakde, et al [82] | 2014 | Thailand | National | Hospital (6 centres) | C/S | 2009–2011 | Unspecified | 580 | 99 | 37 | Adults | Low | 0.03 |
BMI, body mass index; C/C, case-control; C/S, cross-sectional; HCV, hepatitis C virus; NCDs, non-communicable diseases; NR, not reported.
*Quality grades: Low risk (score range, 7–9), Moderate risk (score range, 4–6), and High risk (score range, 0–3).
The studies consisted of 39 to 23853 participants with men comprising 19–95% (median 70.7%) of the samples [13,14]. The median age of participants was 41 years (range 17–73 years). Smoking prevalence, reported in 47 studies, was 0–84% (median 39.8%) [15,16]. In the 37 studies with data on CD4 cell count, levels ranged from 105 cells/μL (Benin) [17] to 535 cells/μL (USA) [18] (median 394 cells/μL). The timespan of diagnosed HIV infection, reported in 20 studies, was 19.3 to 224.4 months [15,18] (median 67.6 months) while the duration of ART, described in 21 studies, was 14.6–78 months [17,19], (median 27 months). In the 28 studies that reported on ART usage, 45–94% of the HIV-infected participants, were on ART [20,21] (median 76.2%). Of those on ART, 17.3–61.5% (median 37.4%) were on protease inhibitors (PIs) [22,23], 19.4% (median 43.4%) on non-nucleoside reverse transcriptase inhibitors (NNRTIs) [22,24], and 1.5–85.5% (median 77.0%) on nucleoside reverse transcriptase inhibitors (NRTIs) [21,25]. Very few studies provided information on the stage of the disease (S4 Table).
The included studies applied various international criteria to diagnose MS (S5 Table). Fifty-one studies applied a single set of criteria; the most frequently used was the ATPIII-2001 in 30 studies followed by the ATPIII-2004-2005 (14 studies). The International Diabetes Federation (IDF)-2005, Joint Interim Statement (JIS)-2009 and modified ATPIII-2005 criteria were used in 2 studies each while the European Group for the Study of Insulin Resistance (EGIR)-2003 in one only. Of the 14 studies that compared the MS prevalence using two or more criteria, the following combinations were reported: two criteria: IDF-2005 + ATPIII-2001 (7 studies), and IDF-2005 + ATPIII-2005 (4 studies), and three criteria (1 study each): IDF-2005 + ATPIII-2005 + JIS-2009; IDF-2005 + ATPIII-2001 + EGIR-2003; IDF-2005 + ATPIII-2001 + EGIR-2003.
Overall prevalence of metabolic syndrome
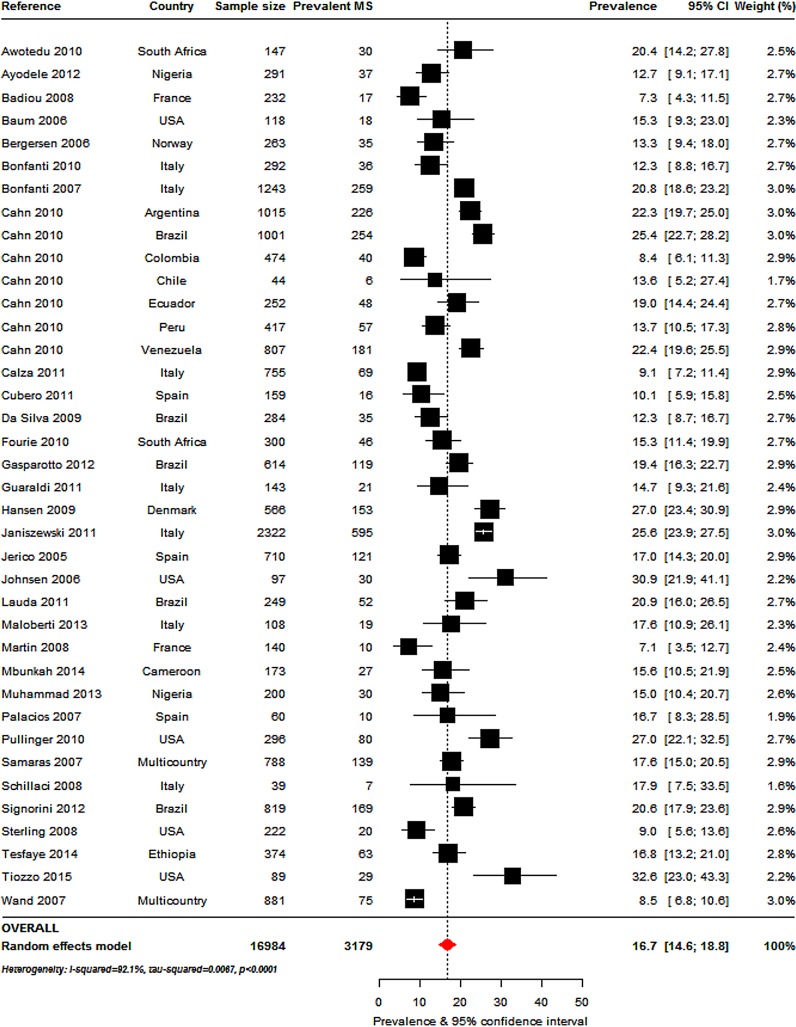
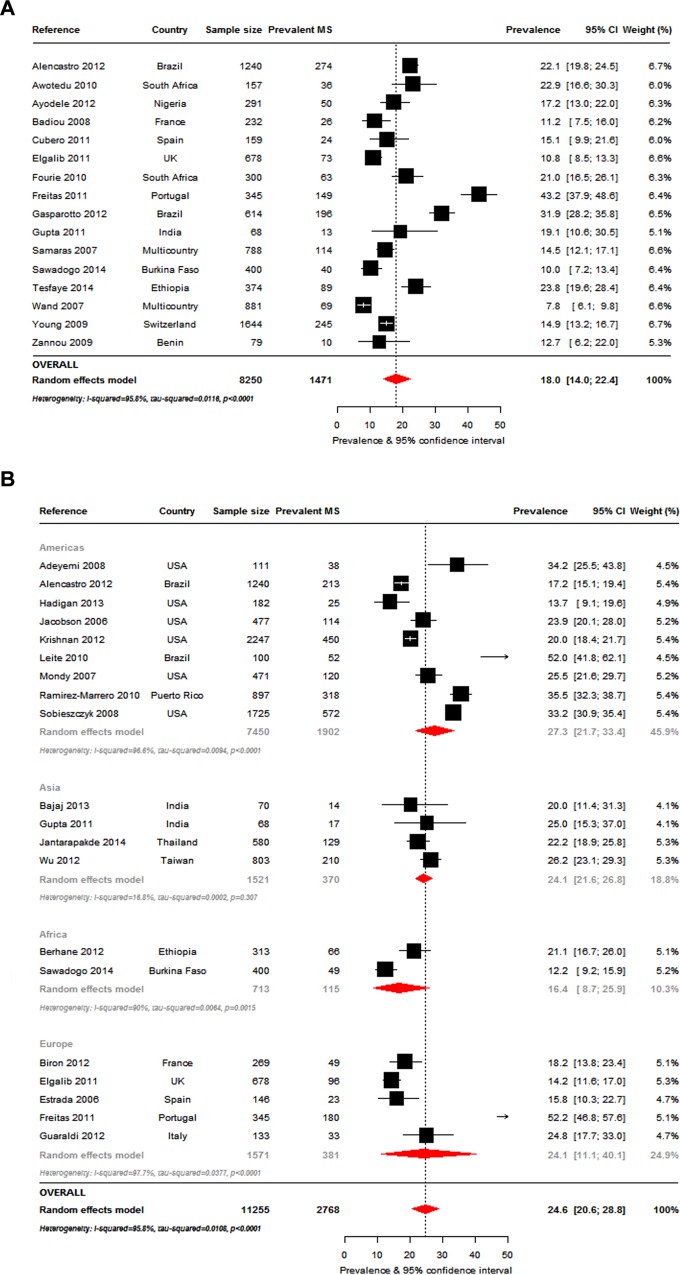
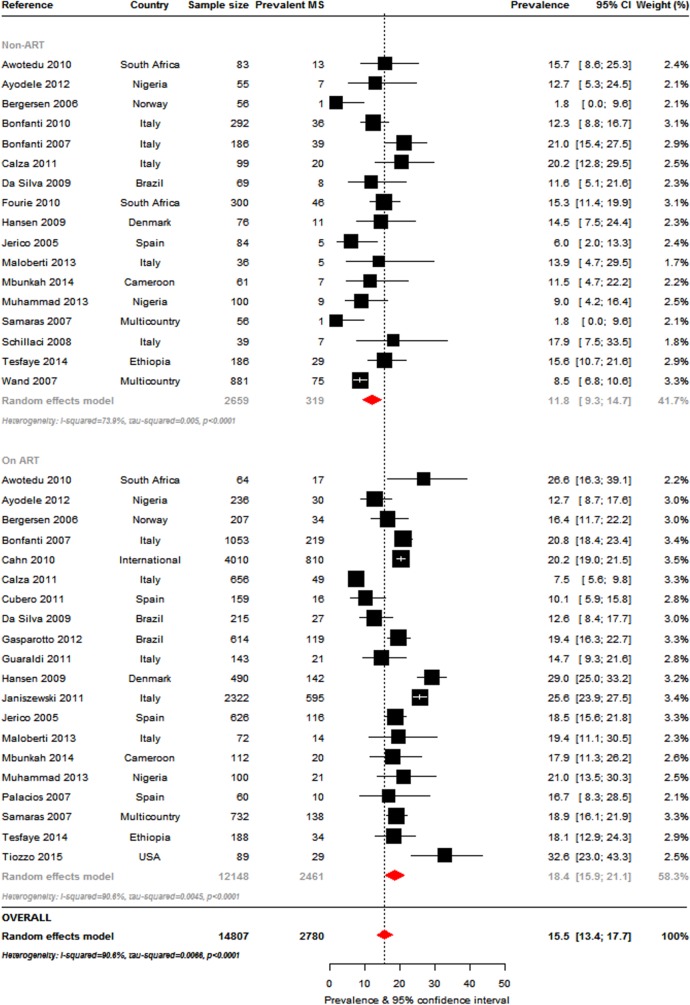
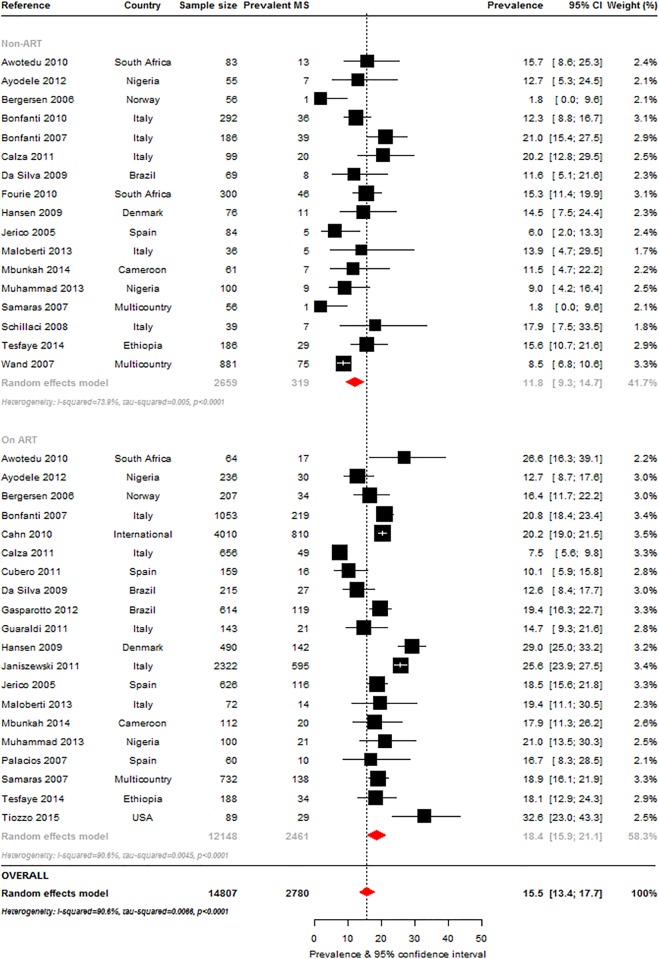
The most commonly used criteria to determine MS prevalence, alone or in combination with other criteria, were the ATPIII-2001 (Fig 2: 38 studies, n = 16984), IDF-2005 (Fig 3A: 16 studies, n = 8250) and ATPIII-2004-2005 definitions (Fig 3B: 20 studies, n = 11255). The overall MS prevalence rates by these criteria were 16.7% (95%CI, 14.6–18.8; I2 = 92.1%, p-heterogeneity<0.001), 18.0% (95%CI: 14.0–22.4; I2 = 95.8%, p<0.001) and 24.6% (95%CI: 20.6–28.8; I2 = 95.8%, p<0.001), respectively. The prevalence ranges were 7.2% [26] to 31% [27] (ATPIII 2001), 7.8% [28] to 43.2% [29] (IDF 2005) and 12.3% [22] to 52% [30] (ATPIII 2004–2005).
Fig 2. Overall metabolic syndrome prevalence in the HIV-infected: Adult Treatment Panel III (ATPIII) 2001 criteria.
For each study the black box represents the study estimate (prevalence of metabolic syndrome [MS]) and the horizontal bar about the 95% confidence intervals (95%CI). The size of the boxes is proportional to the inverse variance. The diamond at the lower tail of the figure is for the pooled effect estimates from random effects models. The proportional contribution of each study (weight) to the pooled estimates is also shown, together with the prevalence estimates and measures of heterogeneity. The dotted vertical line is centred on the pooled estimates.
Fig 3. Overall metabolic syndrome prevalence in the HIV-infected.
Figure panels are for the prevalence of metabolic syndrome according to the International Diabetes Federation 2005 criteria (panel a), and according to the Adult Treatment Panel III 2005 criteria overall and by continent (panel b). For each study the black box represents the study estimate (prevalence of metabolic syndrome [MS]) and the horizontal bar about the 95% confidence intervals (95%CI). The size of the boxes is proportional to the inverse variance. The diamond at the lower tail of the figure is for the pooled effect estimates from random effects models. The proportional contribution of each study (weight) to the pooled estimates is also shown, together with the prevalence estimates and measures of heterogeneity. The dotted vertical line is centred on the pooled estimates.
The highest overall MS prevalence was by the EGIR criteria (31.3%, 95%CI: 26.8–36.0; I2 = 9.8%, p = 0.300) used in two studies (n = 446) (S1 Fig). A similarly high prevalence by the JIS criteria (29.6%, 95%CI: 22.9–36.8; I2 = 91%, p<0.001) was based on four studies (n = 2404) (S2 Fig). MS prevalence by the modified ATPIII 2005 criteria, obtained from two studies (n = 23919), was also high at 27.9% (95%CI: 6.7–56.5; I2 = 95.8%, p<0.001) (S3 Fig). However, there were relatively few studies that determined the MS by these three criteria. The margin of error (precision) across studies ranged from 1% to 12%, with only 18 studies (28%) having a margin of error >5% (Table 1).
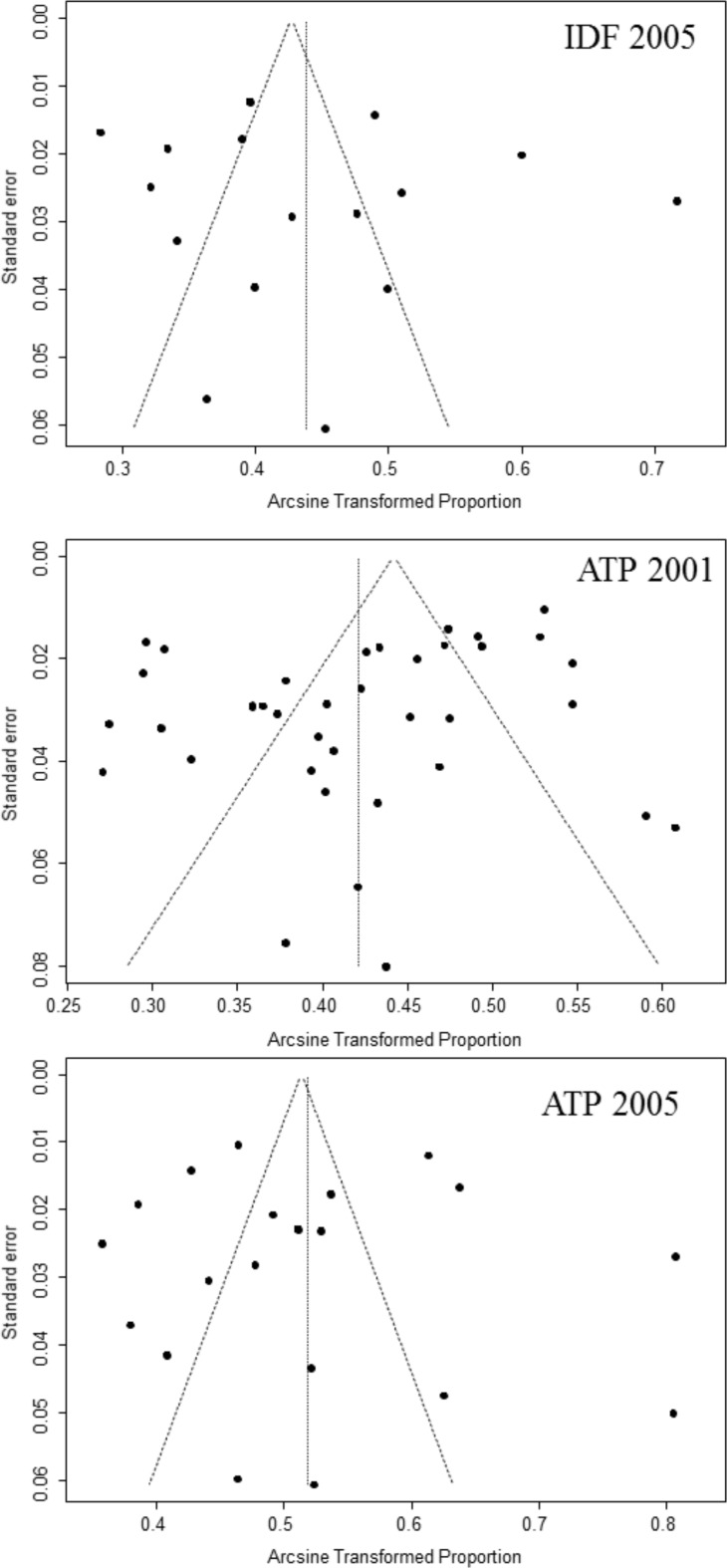
With a wide range of 16.7% to 31.3%, the pooled prevalence of MS differed significantly by the various diagnostic criteria (p<0.001). Unsurprisingly, however, MS prevalence by modified criteria was similar to that of studies that used the related original definition (S5 Table). There was insufficient evidence of publication bias (all p ≥0.060 for the Egger test) except for studies that used the ATPIII 2001 criteria (p-Egger test = 0.040; Fig 4)
Fig 4. Funnel plots for included studies across different diagnostic criteria for metabolic syndrome.
For each diagnostic criteria, the arcsine transformed proportion of participants with metabolic syndrome (relative to the total sample) for each relevant study (horizontal axis) is plotted against its standard error (vertical axis), and represented by the dots. When the dots distribute symmetrically in a funnel shape, this implies an absence of bias. A p-value <0.05 (Egger test) indicates significant publication bias.
Prevalence of metabolic syndrome within and across subgroups
Some of the findings are presented in the accompanying tables and figures while other data such as the prevalence of MS by age, intra-country location, duration of HIV infection, ART status, treatment period and year of publication are reported in the supplementary tables and figures.
Age
Older (>median age 41 years) compared with younger participants (≤41years) had higher MS prevalence (S6 Table): ATPIII-2001: 19.7% vs. 13.2%, p<0.001, ATIII 2004–2005: 26.6% vs. 21.5%, p = 0.479 and IDF-2005: 22.3% vs. 16.4%, p = 0.361. Substantial heterogeneity was apparent within age-groups regardless of the criteria (all p-heterogeneity<0.001).
Gender
Thirty-two of the 65 studies presented the MS data by gender; of these a single study was conducted in men only (Italy) [31] and two in women only (USA) [27,32]. The criteria most commonly used was the ATPIII 2001 in 16 studies for men (n = 8269) and 17 studies for women (n = 3971). This was followed by the ATPIII 2004–2005 (13 studies, men: n = 5742, women: n = 4470) and IDF 2005 definitions (11 studies, men: n = 3556, women: n = 2293). The MS prevalence in men and women was as follows: ATPIII 2001: 14.6% (95%CI: 11.5–18.1) and 17.5% (95%CI: 14.0–21.2); ATPIII 2004–2005: 23.7% (95%CI: 19.0–28.7) and 26.7% (95%CI: 20.8–33.0); and IDF 2005: 13.4% (95%CI: 8.7–18.9) and 23.2% (95%CI: 15.9–31.4); Fig 5 and S6 Table. MS prevalence by the various criteria was significantly different in men (p = 0.001) but not in women (p = 0.118). Heterogeneity presented within gender-groups across criteria (all p-heterogeneity<0.001).
Fig 5. Pooled metabolic syndrome prevalence in the HIV-infected presented by gender: International Diabetes Federation 2005 criteria.
For each study the black box represents the study estimate (prevalence of metabolic syndrome [MS]) and the horizontal bar about the 95% confidence intervals (95%CI). The size of the boxes is proportional to the inverse variance. The diamond at the lower tail of the figure is for the pooled effect estimates from random effects models. The proportional contribution of each study (weight) to the pooled estimates is also shown, together with the prevalence estimates and measures of heterogeneity. The dotted vertical line is centred on the pooled estimates. Furthermore, pooled effect estimates are provided separately by gender. The horizontal arrow head indicates that the representation of the effect estimates and 95% confidence intervals has been truncated.
HIV-related factors
Duration of diagnosed HIV infection: The prevalence of MS, categorised by the duration of diagnosed HIV infection (median cut-off point 68 months), differed across MS criteria (S6 Table). By the ATPIII-2001 definition, MS prevalence was significantly higher (p = 0.044) in participants with longer (20.6%, 95%CI: 13.8–28.4) compared to shorter duration of diagnosed HIV-infection (13.2%, 95%CI: 11.2–15.4). However, by the ATPIII-2004-2005, MS prevalence was not significantly different: longer: 32.0% vs. shorter: 19.1%, p = 0.251. There was substantial heterogeneity across and within criteria for MS prevalence by the duration of diagnosed HIV infection; all p-heterogeneity<0.030 for within criteria except for studies below the median duration which used the ATPIII-2001 criteria (p-heterogeneity = 0.581)
CD4 counts: Using a median cut-off point of 394 cells/μL, MS prevalence in participants with high CD4 counts was significantly lower than in those with low CD4 counts by the IDF 2005 criteria: 10.4% (8.2–12.9) vs. 17.5% (14.4–20.8), p<0.001 (S6 Table). However, there was little difference in MS prevalence by CD4 count levels using the ATPIII-2001 (17.4% vs. 15.6%, p = 0.514) and ATPIII-2004-2005 definitions (24.6% vs. 26.5%, p = 0.747). The prevalence across MS diagnostic criteria was significantly different by CD4 count levels (all p≤0.020). Substantial heterogeneity was noted in MS prevalence by CD4 count levels within studies that applied the ATPIII-2001 and ATPIII-2004-2005 criteria (all p-heterogeneity≤0.035) but not within studies that used the IDF-2005 definition (p-heterogeneity≥0.272).
Exposure to antiretroviral therapy: In studies that included treatment status (S6 Table), the most commonly used MS criteria was the ATPIII 2001 (ART-exposed: 20 studies, n = 12148, ART-naïve: 17 studies, n = 2659). MS prevalence, at 18.4% (95% CI: 15.9–21.1) in the ART-exposed, was significantly higher (p = 0.001) than in the ART-naïve (11.8%, 95%CI: 9.3–14.7) (Fig 6). MS prevalence by the IDF 2005 criteria was also higher in the ART-exposed (19.6%, 95%CI: 14.2–25.6) compared to the ART-naïve (14.9%, 95%CI: 8.6–22.6) but this difference was not significant; prevalence was similar by the ATPIII 2004–2005 definition (21.6%, 95%CI: 13.5–31.0 vs. 19.9%, 95%CI: 18.3–21.5). Interestingly, MS prevalence by the various criteria was similar in the ART-exposed (p = 0.730) but significantly different in the ART-naïve (p<0.001). Excluding the non-ART studies based on the ATPIII-2004-2005 where homogeneity was found (p-heterogeneity = 0.398), there was significant heterogeneity within ART-exposed and ART-naïve groups (all p-heterogeneity<0.001).
Fig 6. Pooled metabolic syndrome prevalence in the HIV-infected presented by antiretroviral therapy (ART) use: Adult Treatment Panel 2001 criteria.
For each study the black box represents the study estimate (prevalence of metabolic syndrome [MS]) and the horizontal bar about the 95% confidence intervals (95%CI). The size of the boxes is proportional to the inverse variance. The diamond at the lower tail of the figure is for the pooled effect estimates from random effects models. The proportional contribution of each study (weight) to the pooled estimates is also shown, together with the prevalence estimates and measures of heterogeneity. The dotted vertical line is centred on the pooled estimates. Furthermore, pooled effect estimates are provided separately by ART use. The horizontal arrow head indicates that the representation of the effect estimates and 95% confidence intervals has been truncated.
Proportions of ART users and duration of ART treatment: MS prevalence by a high or low proportion of ART users (median cut-off point 76.2%) was not significantly different within criteria: ATPIII 2001: 15.8% vs. 19.1%, p = 0.172; ATPIII 2004–2005: 38.3% vs. 23.8%, p = 0.256; IDF 2005: 14.4% vs. 19.4%, p = 0.176. Using a cut-off point of 27 months for the median length of ART use, MS prevalence was not significantly different for a longer or shorter treatment duration within MS criteria: ATPIII 2001: 17.1% vs. 15.6%, p = 0.649; ATPIII 2004–2005: 25.6% vs. 14.2%, p = 0.192; IDF 2005: 14.6% vs. 13.4%, p = 0.811. The prevalence within the two sub-groups was similar across MS criteria (all p≥0.111). Substantial heterogeneity was noted within all the above subgroups (all p-heterogeneity<0.001).
ART regimen: The median proportion of participants using PIs across the included studies was 37.4% (S6 Table). Using this cut-off point, the pooled MS prevalence in studies with more compared to fewer PI users by the IDF 2005 criteria was 18.5% (95%CI: 12.3–25.6) from six studies (n = 4927) versus 10.0% (95%CI: 7.2–13.4) (p = 0.016) in a single study (n = 400). However, the MS prevalence by proportion of PI users was not significantly different by the ATPIII 2001 (17.7% vs. 19.3%, p = 0.593) and ATPIII 2004–2005 definitions (25.8% vs. 30.4%, p = 0.517). MS prevalence, determined by the various criteria, differed across studies of PI users (p = 0.022) and in those with fewer median participants on PIs (p = 0.001).
The median proportion of participants using NNRTIs was 43.4%, the cut-off value used to determine a high and low proportion of users. The pooled MS prevalence in studies with more compared to fewer NNRTI users was 17.2% (95%CI: 9.5–26.6) versus 33.8% (95%CI: 23.4–45.1) (p = 0.020) by the ATPIII 2004–2005 criteria. MS prevalence according to NNRTI regimen status was not significantly different by the ATPIII 2001 (19.5% vs. 15.1%, p = 0.221) and IDF 2005 criteria (10.5% vs. 19.8%, p = 0.058). However, MS prevalence within the two NNRTI subcategories was significantly different by the various MS criteria (all p≤0.007), (S6 Table).
In studies with a high proportion of participants on NRTI (median >77.0%), the pooled prevalence by the ATPIII 2001 criteria was 17.9% (95%CI: 9.4–28.7) compared to 22.8% (95%CI: 14.3–32.7) in studies with fewer participants on NRTIs (p = 0.474) (S6 Table). There was insufficient data by the IDF 2005 and ATPIII 2004–2005 criteria for analysis.
Study location
Intercontinental: The ATPIII 2004–2005 MS criteria was the only one commonly used by studies across continents. The pooled MS prevalence by this criteria was the highest in the Americas (9 studies, n = 7450) at 27.3% (95%CI: 21.7–33.4; I2 = 96.6%, p<0.001). This was followed by Europe (5 studies, n = 1571) and Asia (4 studies, n = 1521) where the prevalence was similar. At 24.1% (95%CI: 11.2–40.1; I2 = 97.7%, p<0.001) in Europe and 24.1% (95%CI: 21.6–26.8; I2 = 16.8%, p = 0.307) in Asia, MS prevalence on these continents were almost as high as in the Americas. MS prevalence in Africa (2 studies, n = 713), however, was much lower at 16.4% (95%CI: 8.7–25.9; I2 = 90%, p = 0.002), (Fig 3B and S6 Table). The differences in prevalence across continents was not statistically significant (p = 0.284).
Intra-country: MS prevalence was similar across regional studies compared with the corresponding national data (ATPIII 2001: 16.0% vs. 17.1%, p = 0.607; ATPIII 2004–2005: 24.3% vs. 25.4%, p = 0.861; IDF 2005: 17.4% vs. 18.7%, p = 0.785) (S6 Table). According to the criteria used, the prevalence of MS within a country differed in regional studies (p = 0.024) but was not significantly different in national studies (p = 0.109).
Year of publication
The prevalence of MS in studies reported before, compared to after, 2010 was significantly higher by the ATPIII 2004–2005 criteria (30.6% vs. 21.5%, p = 0.012) but not by the other definitions (all p≥0.100). However, MS prevalence in the earlier publications differed significantly by criteria (16.4% vs. 30.6% vs. 14.5% for ATPIII-2001, ATPIII-2004-2005, IDF-2005 respectively, p<0.001).
Sample size and smoking status
The median number of participants per study was 292 with this sample size used to classify studies as either large or small. MS prevalence was similar in large and small studies within criteria: ATPIII 2001:18.3% vs. 15.1%, p = 0.115; ATPIII 2004–2005: 24.7% vs. 25.6%, p = 0.989; IDF 2005: 19.0% vs. 16.1%, p = 0.388. There was no significant difference in prevalence by sample size category across MS criteria (all p≥0.059).
Smoking status
The absence of a significant difference in the prevalence of MS in studies with a high or low proportion of smokers (median 39.8%) within criteria is demonstrated in S6 Table. The prevalence was as follows: ATPIII 2001: 14.8% vs. 17.6%, p = 0.234; ATPIII 2004–2005: 28.8% vs. 22.2%, p = 0.193; IDF 2005: 18.4% vs. 14.6%, p = 0.565. However, MS prevalence varied significantly across criteria in studies with a higher proportion of smokers (p = 0.010). There was substantial heterogeneity within all the above subgroups (all p-heterogeneity<0.001).
Discussion
Overview of MS prevalence
To our knowledge, this is the first comprehensive review and meta-analysis of the MS prevalence in the global HIV-infected population. Among the key findings was the high burden of MS in the HIV-infected population; 16.7–31.3% of HIV-infected adults had MS by the various definitions. The wide prevalence range is indicative of substantial heterogeneities across and within the diagnostic criteria. Two different criteria, the ATPIII-2001 and the EGIR-2003, reported the overall lowest and highest prevalences, respectively. Notably, the differences in prevalences were not fully explained by the major study characteristics. For example, variations in MS prevalence were also apparent within subgroups such as in younger participants, men, the Americas, regional studies, older publications and smokers.
Notably, the MS prevalence in the HIV-infected is within the range of the 17–46% reported in the general population. This highlights that the risk for developing MS in HIV-infected individuals is likely comparable to that in the general population. It also underscores the importance of traditional cardio-metabolic risk factors in the former; these are likely to exert an equal influence on HIV-infected individuals as they do in the general population. The wide range in MS prevalence in the general population mimics that found in this review and is possibly due to similar reasons discussed above [33–35].
The similar exposure to cardio-metabolic risk factors in the HIV-infected compared to the general population is likely attributable to the introduction of ART which has dramatically reduced HIV-related morbidity and mortality. ART has prolonged lifespans and subsequently enabled the HIV-infected to be exposed to the same risk factors and diseases as the general population. Reinforcing the likelihood of similar pathways in the development of MS in the HIV-infected and general populations was the higher MS prevalence in older compared to younger HIV-infected individuals, which is mirrored in general populations [33].
The higher MS prevalence in women compared to men in this analysis has also been shown in general populations but reports diverge in the latter [33–35]. Further research may be required to understand the differences in MS prevalence by gender which is usually driven by higher rates of obesity [36]. There may also be HIV specific factors that contribute to greater cardio-metabolic abnormalities in women compared to men that require further investigation.
MS prevalence by diagnostic criteria
Across the three major criteria (ATPIII 2001, ATPIII 2004–2005, and IDF 2005) used by most studies in this review, the estimated MS prevalence was highest by the ATPIII 2004–2005 definition (24.6%). This was not unexpected because the threshold for hyperglycaemia in the ATPIII 2004–2005 is lower than that for the ATPIII 2001criteria; this leads to more individuals diagnosed with MS by the former classification. Furthermore, the inclusion of lipid-lowering and/or antihypertensive medications in the ATPIII 2004–2005 definition also contributes to a higher MS diagnosis compared with the ATPIII 2001. In contrast, the compulsory incorporation of waist circumference in the IDF 2005 criteria excludes many HIV-infected participants with abnormal biochemical parameters but normal waist circumference from the diagnosis. This is of particular relevance and frequently reported in HIV studies [25,37–41].
Not surprisingly, few studies that used more than one definition to diagnose MS applied the same combination of criteria [25,42]. In this review, direct comparison of MS prevalence by the various criteria is not meaningful because there was substantial overlap of the confidence intervals around the prevalence estimates. Also, only few studies used multiple diagnostic criteria which would limit the value of such an analysis.
HIV-related influences on MS prevalence
Although HIV specific characteristics were associated with the prevalence of MS in the current analyses, these need to be interpreted with care because of the inability to control for the many confounding influences. Nonetheless, the association of MS prevalence with a greater duration of diagnosed HIV infection accords with the influence of HIV infection on the development of cardio-metabolic abnormalities. Then again, a longer interval since HIV diagnosis likely correlates with older age, which is a risk factor for MS in both the HIV-infected and general populations. It may also possibly reflect the specific effects of prolonged ART.
The relation between CD4 count and MS was unclear with some studies reporting a direct link [43,44] while others demonstrate the inverse [45] or no association [46,47]. However, these findings were based on only seven studies and did not report the viral loads [13,17,22,40,42,48,49]. Without such information it is difficult to draw conclusions on this relationship. A high viral load has been associated with the development of MS, possibly contributing to the high incidence of low high density lipoprotein cholesterol (HDL-C) levels and high triglycerides in some studies [16,50].
The higher MS prevalence in ART-exposed compared to ART-naïve participants by the ATPIII-2001 criteria was consistent with findings from prospective studies. One of these studies demonstrated an increase in MS prevalence from 16.6% to 25% with an incidence of 14/100 patients-year among participants initiated and maintained on the same HAART regimen for 48 weeks [51]. In another study, a large international, multicentre, randomised trial conducted for three years after the initiation of ART, the incidence of MS was 12/100 patients-year and 8/100 patients-year according to the ATPIII 2001 and the IDF 2005 criteria, respectively [28]. Also, the D:A:D study which followed HIV patients on ART over a long period, demonstrated a substantial increase in MS prevalence [52].
ART regimen was significantly associated with MS with notable differential findings by the class of drug used. The higher MS prevalence in studies with a greater compared to smaller proportion of PI users accords with four trials where PI-based regimens were found to accelerate progression to MS [37,38]. The initiation of ART leads to chronic inflammation and an incompletely restored immune system. This may perhaps be the link between PI use and the development of MS [53,54]. Furthermore, PI drugs have been reported to be associated with more severe dyslipidaemia compared to NNRTI, which is a feature of metabolic syndrome. This would explain at least in part the higher prevalence of MS in patients on PI. Patients on this regimen thus need to be closely monitored for the development of cardio-metabolic abnormalities. Moreover, once such abnormalities arise, it is important to review ART management and change to metabolically neutral regimens.
An alternative ART regimen to PIs in patients with MS may be NNRTIs because a lower MS prevalence, by some criteria, was detected in studies with a high compared to low proportion of participants on these drugs. Although our analyses were based on only seven studies [14,20,22,29,37,41,44] this suggests that, unlike PIs, NNRTIs do not adversely influence cardio-metabolic function and may possibly even have a beneficial impact. Indeed, a randomised controlled study reported improvements in cardio-metabolic profiles with increases in HDL-C levels in patients on nevirapine and nelfinavir [55]. On the other hand, several prospective trials have found no association between the use of NNRTIs and MS [37,38]. Further research is required to clearly describe the relationship between NNRTIs and cardio-metabolic functioning, particularly since there is a dearth of data on the influence of this class of ART on MS.
Other influences on MS prevalence
Although there was no difference in MS prevalence between studies with a high and low proportion of smokers, conclusions on the absence of an association should be cautioned against. The studies analysed included only current smokers with no consideration given to recent smoking cessation or ex-smokers. Reports describe the duration of smoking cessation to be inversely related to future cardiovascular disease risk to a moderate degree. Furthermore, aspects not considered in this review such as the smoking interval and the quantity smoked have been strongly correlated with the development of MS and atherosclerosis progression [56–58].
The lower MS prevalence by the ATPIII 2004–2005 criteria in recent compared to older publications was surprising. We expected the trend to mimic that of the general population with a rise in MS prevalence in the HIV-infected over time. Moreover, with the introduction and widespread uptake of ART leading to longevity, we anticipated the subsequent development of MS with age, which would be reported in recent publications. Nevertheless, our findings are elucidated by the differences in participant characteristics between the two publication periods. Participants in publications prior to 2010 were older and included more women who were shown to have a higher MS prevalence than men in this review.
Despite an unbalanced representation of studies worldwide, the prevalence of MS was essentially similar within and across the major regions including by continent and intra-country site, regardless of the definition criteria used. The absence of studies conducted specifically in rural settings with a likely lower MS prevalence than in urban centres, particularly in developing regions, may account for this finding. Alternatively, it may perhaps reflect the ubiquitous worldwide influence of globalisation and highlight the likelihood of similar influences on the development of MS in the HIV-infected population globally. Thus, broad-based general strategies may perhaps be devised to address the MS burden in all HIV-infected populations.
Strengths and limitations
Strengths
We searched multiple databases extensively, applying reproducible criteria to capture the most number of studies on MS prevalence worldwide. This allowed us to provide a comprehensive global perspective on the emerging burden of adverse cardio-metabolic profiles in the HIV-infected population. Furthermore, we used robust approaches to pool studies while minimising the effects of extreme studies. We also used a detailed approach to investigate the potential sources of heterogeneity. Our post-hoc power estimation revealed that over two-thirds of the included studies were adequately powered to provide precise estimates of the MS prevalence in the overall sample. This has likely translated into stable and robust pooled estimates by combining those primary studies.
Limitations
Our findings may not be generalizable to all HIV-infected individuals because most of the studies were conducted in non-randomly selected populations. The wide range in MS prevalence, because of the different criteria used across studies, although expected, made estimations of the actual burden difficult. Nevertheless, apart from differences in the criteria themselves that contributed to this wide range, other factors were also likely responsible. For example, MS prevalence would be expected to differ across time, particularly in the HIV-infected as access to care expanded, the uptake of ART increased and the effectiveness of therapy improved with the introduction of HAART. In some included studies, participants were selected with consideration to histories of existing CVD risk factors, which in turn can result in MS prevalence rates different from those in a broader population of HIV-infected individuals. This could possibly contribute to some of the heterogeneities observed across studies.
The infrequent reporting of the HIV specific markers of CD4 count and viral load precluded in-depth analyses of their effects on MS. Similarly, data were missing on key study characteristics which could be used in advanced analyses via meta-regressions. Furthermore, the inconsistent number of studies across subgroups precluded meta-regression analyses to investigate the possible contribution of each factor to MS prevalence. However, such comparisons would possibly have been biased by differences in study design and objectives, data collection techniques, laboratory facilities and participant characteristics, and could not have been fully accounted for in our meta-analyses. Especially difficult to control for would be HIV related characteristics such as differences in disease stage, fat distribution including lipodystrophy, obesity and co-existent infections such as hepatitis C and hepatitis B [59].
Conclusion and Implications
The MS prevalence in HIV-infected individuals worldwide appears to be similar to that found in the general population, suggesting similarities in the drivers of the syndrome, independent of HIV status. Indeed, despite suggestions of significant signals, the inconsistent association of HIV specific features including treatments with MS prevalence suggest that their contribution, if any, is of a lesser magnitude. Comparable with general populations, traditional risk factors are likely the major contributors to the burden of cardio-metabolic abnormalities and MS in HIV-infected individuals. Therefore, management strategies implemented in the general population for these conditions, will likely reap similar benefits in the HIV-infected. Nevertheless, the major challenge lies in devising and strengthening approaches to maximise cardio-metabolic care while simultaneously ensuring optimal HIV management.
Supporting Information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by Grand Challenge Canada, through the Global Alliance on Chronic Diseases initiative. KAN is supported by the NRF Innovation Doctoral Research Scholarship, Doctoral Scholarship and Yeoman Bequest Bursary through the University of Cape Town. These funding bodies had no involvement in the study. Global Evaluation Science provided support in the form of salaries for author EJM, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific role of this author is articulated in the ‘author contributions’ section.
References
- 1.Murray CJ, Ortblad KF, Guinovart C, Lim SS, Wolock TM, Roberts DA, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384: 1005–1070. 10.1016/S0140-6736(14)60844-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jaggers JR, Prasad VK, Dudgeon WD, Blair SN, Sui X, Burgess S, et al. (2014) Associations between physical activity and sedentary time on components of metabolic syndrome among adults with HIV. pp. 1387–1392. 10.1080/09540121.2014.920075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Wit S, Sabin CA, Weber R, Worm SW, Reiss P, Cazanave C, et al. Incidence and risk factors for new-onset diabetes in HIV-infected patients: the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. Diabetes Care. 2008;31: 1224–1229. 10.2337/dc07-2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Syed FF, Sani MU. Recent advances in HIV-associated cardiovascular diseases in Africa. Heart. 2013;99: 1146–1153. 10.1136/heartjnl-2012-303177 [DOI] [PubMed] [Google Scholar]
- 5.Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. Journal of the American College of Cardiology. 2007;49: 403–414. [DOI] [PubMed] [Google Scholar]
- 6.Authors N. New therapies: new hope. Reports from the International Nursing Satellite symposium and the Eleventh International Conference on AIDS, Vancouver, Canada, 6–12 July, 1996. Midwifery. 1996;12: 205–206. [DOI] [PubMed]
- 7.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15: 539–553. [DOI] [PubMed] [Google Scholar]
- 8.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65: 934–939. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 9.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67: 974–978. 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- 10.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21: 1539–1558. [DOI] [PubMed] [Google Scholar]
- 11.Mills EJ, Jansen JP, Kanters S. Heterogeneity in meta-analysis of FDG-PET studies to diagnose lung cancer. JAMA. 2015;313: 419. [DOI] [PubMed] [Google Scholar]
- 12.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Awotedu K, Ekpebegh C, Longo-Mbenza B, Iputo J. Prevalence of metabolic syndrome assessed by IDF and NCEP ATP 111 criteria and determinants of insulin resistance among HIV patients in the Eastern Cape Province of South Africa. Diabetes and Metabolic Syndrome: Clinical Research and Reviews. 2010;4: 210–214. [Google Scholar]
- 14.Wu PY, Hung CC, Liu WC, Hsieh CY, Sun HY, Lu CL, et al. Metabolic syndrome among HIV-infected Taiwanese patients in the era of highly active antiretroviral therapy: Prevalence and associated factors. Journal of Antimicrobial Chemotherapy. 2012;67: 1001–1009. 10.1093/jac/dkr558 [DOI] [PubMed] [Google Scholar]
- 15.Ngatchou W, Lemogoum D, Ndobo P, Yagnigni E, Tiogou E, Nga E, et al. Increased burden and severity of metabolic syndrome and arterial stiffness in treatment-naive HIV+ patients from Cameroon. Vascular health and risk management. 2013;9: 509–516. 10.2147/VHRM.S42350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baum MK, Rafie C, Lai S, Xue L, Sales S, Page JB, et al. Coronary Heart Disease (CHD) Risk Factors and Metabolic Syndrome in HIV-Positive Drug Users in Miami. American journal of infectious diseases. 2006;2: 173–179. [PMC free article] [PubMed] [Google Scholar]
- 17.Zannou DM, Denoeud L, Lacombe K, Amoussou-Guenou D, Bashi J, Akakpo J, et al. Incidence of lipodystrophy and metabolic disorders in patients starting non-nucleoside reverse transcriptase inhibitors in Benin. Antiviral therapy. 2009;14: 371–380. [DOI] [PubMed] [Google Scholar]
- 18.Sterling RK, Contos MJ, Smith PG, Stravitz RT, Luketic VA, Fuchs M, et al. Steatohepatitis: Risk factors and impact on disease severity in human immunodeficiency virus/hepatitis C virus coinfection. Hepatology. 2008;47: 1118–1127. 10.1002/hep.22134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jerico C, Knobel H, Montero M, Ordonez-Llanos J, Guelar A, Gimeno JL, et al. Metabolic syndrome among HIV-infected patients: prevalence, characteristics, and related factors. Diabetes Care. 2005;28: 132–137. [DOI] [PubMed] [Google Scholar]
- 20.Ramírez-Marrero FA, De Jesuś E, Santana-Bagur J, Hunter R, Frontera W, Joyner MJ. Prevalence of cardiometabolic risk factors in hispanics living with HIV. Ethnicity and Disease. 2010;20: 423–428. [PMC free article] [PubMed] [Google Scholar]
- 21.De Socio GV, Ricci E, Maggi P, Parruti G, Pucci G, Di Biagio A, et al. Prevalence, awareness, treatment, and control rate of hypertension in HIV-infected patients: The HIV-HY study. American Journal of Hypertension. 2014;27: 222–228. 10.1093/ajh/hpt182 [DOI] [PubMed] [Google Scholar]
- 22.Sawadogo A, Sanou S, Hema A, Kamboule BE, Kabore NF, Sore I, et al. Metabolic syndrome and cardiovascular risk patients under antiretrovirals in a hospital day at Bobo-Dioulasso (Burkina Faso). Bulletin de la Societe de Pathologie Exotique. 2014;107: 151–158. 10.1007/s13149-014-0371-8 [DOI] [PubMed] [Google Scholar]
- 23.Cahn P, Leite O, Rosales A, Cabello R, Alvarez CA, Seas C, et al. Metabolic profile and cardiovascular risk factors among Latin American HIV-infected patients receiving HAART. The Brazilian journal of infectious diseases: an official publication of the Brazilian Society of Infectious Diseases. 2010;14: 158–166. [DOI] [PubMed] [Google Scholar]
- 24.Pullinger CR, Aouizerat BE, Gay C, Coggins T, Movsesyan I, Davis H, et al. Metabolic abnormalities and coronary heart disease risk in human immunodeficiency virus-infected adults. Metabolic syndrome and related disorders. 2010;8: 279–286. 10.1089/met.2009.0094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samaras K, Wand H, Matthew L, Emery S, Cooper D, Carr A. Prevalence of metabolic syndrome in HIV-infected patients receiving highly active antiretroviral therapy using International Diabetes Foundation and Adult Treatment Panel III criteria: Associations with insulin resistance, disturbed body fat compartmentalization, elevated C-reactive protein, and hypoadiponectinemia. Diabetes care. 2007;30: 113–119. [DOI] [PubMed] [Google Scholar]
- 26.Martin Lde S, Pasquier E, Roudaut N, Vandhuick O, Vallet S, Bellein V, et al. Metabolic syndrome: a major risk factor for atherosclerosis in HIV-infected patients (SHIVA study). Presse medicale (Paris, France: 1983). 2008;37: 579–584. [DOI] [PubMed] [Google Scholar]
- 27.Johnsen S, Dolan SE, Fitch KV, Kanter JR, Hemphill LC, Connelly JM, et al. Carotid intimal medial thickness in human immunodeficiency virus-infected women: effects of protease inhibitor use, cardiac risk factors, and the metabolic syndrome. The Journal of clinical endocrinology and metabolism. 2006;91: 4916–4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wand H, Calmy A, Carey DL, Samaras K, Carr A, Law MG, et al. Metabolic syndrome, cardiovascular disease and type 2 diabetes mellitus after initiation of antiretroviral therapy in HIV infection. AIDS (London, England). 2007;21: 2445–2453. [DOI] [PubMed] [Google Scholar]
- 29.Freitas P, Carvalho D, Souto S, Santos AC, Xerinda S, Marques R, et al. Impact of Lipodystrophy on the prevalence and components of metabolic syndrome in HIV-infected patients. BMC infectious diseases. 2011;11: 246-2334-2311-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leite LHM, Sampaio ABMM. Dietary calcium, dairy food intake and metabolic abnormalities in HIV-infected individuals. Journal of Human Nutrition & Dietetics. 2010;23: 535–543. [DOI] [PubMed] [Google Scholar]
- 31.Guaraldi G, Beggi M, Zona S, Luzi K, Orlando G, Carli F, et al. Erectile Dysfunction Is Not a Mirror of Endothelial Dysfunction in HIV-Infected Patients. Journal of Sexual Medicine. 2012;9: 1114–1121. 10.1111/j.1743-6109.2011.02243.x [DOI] [PubMed] [Google Scholar]
- 32.Sobieszczyk ME, Hoover DR, Anastos K, Mulligan K, Tan T, Shi Q, et al. Prevalence and predictors of metabolic syndrome among HIV-infected and HIV-uninfected women in the women's interagency HIV Study. Journal of acquired immune deficiency syndromes. 2008;48: 272–280. 10.1097/QAI.0b013e31817af461 [DOI] [PubMed] [Google Scholar]
- 33.Grundy SM. Metabolic syndrome pandemic. Arteriosclerosis, Thrombosis, and Vascular Biology. 2008;28: 629–636. 10.1161/ATVBAHA.107.151092 [DOI] [PubMed] [Google Scholar]
- 34.Pan WH, Yeh WT, Weng LC. Epidemiology of metabolic syndrome in Asia. Asia Pacific Journal of Clinical Nutrition. 2008;17 Suppl 1: 37–42. [PubMed] [Google Scholar]
- 35.Marquez-Sandoval F, Macedo-Ojeda G, Viramontes-Horner D, Fernandez Ballart JD, Salas Salvado J, Vizmanos B. The prevalence of metabolic syndrome in Latin America: a systematic review. Public Health Nutr. 2011;14: 1702–1713. 10.1017/S1368980010003320 [DOI] [PubMed] [Google Scholar]
- 36.Garawi F, Devries K, Thorogood N, Uauy R. Global differences between women and men in the prevalence of obesity: is there an association with gender inequality? European Journal of Clinical Nutrition. 2014;68: 1101–1106. 10.1038/ejcn.2014.86 [DOI] [PubMed] [Google Scholar]
- 37.Jacobson DL, Tang AM, Spiegelman D, Thomas AM, Skinner S, Gorbach SL, et al. Incidence of metabolic syndrome in a cohort of HIV-infected adults and prevalence relative to the US population (National Health and Nutrition Examination Survey). Journal of acquired immune deficiency syndromes (1999). 2006;43: 458–466. [DOI] [PubMed] [Google Scholar]
- 38.Krishnan S, Schouten JT, Atkinson B, Brown T, Wohl D, McComsey GA, et al. Metabolic syndrome before and after initiation of antiretroviral therapy in treatment-naive HIV-infected individuals. Journal of acquired immune deficiency syndromes (1999). 2012;61: 381–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hadigan C, Meigs JB, Wilson PW, D'Agostino RB, Davis B, Basgoz N, et al. Prediction of coronary heart disease risk in HIV-infected patients with fat redistribution. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2003;36: 909–916. [DOI] [PubMed] [Google Scholar]
- 40.Gupta V, Biswas A, Sharma SK. Metabolic and body composition changes after six months of highly active antiretroviral therapy in northern Indian patients. International Journal of STD & AIDS. 2011;22: 46–49. [DOI] [PubMed] [Google Scholar]
- 41.Elgalib A, Aboud M, Kulasegaram R, Dimian C, Duncan A, Wierzbicki AS, et al. The assessment of metabolic syndrome in UK patients with HIV using two different definitions: CREATE 2 study. Current medical research and opinion. 2011;27: 63–69. 10.1185/03007995.2010.537212 [DOI] [PubMed] [Google Scholar]
- 42.Cubero JM, Domingo P, Sambeat M, Ordoñez-Llanos J, Rodriguez-Espinosa J, Sánchez-Quesada JL, et al. Prevalence of metabolic syndrome among human immunodeficiency virus-infected subjects is widely influenced by the diagnostic criteria. Metabolic Syndrome and Related Disorders. 2011;9: 345–351. 10.1089/met.2010.0129 [DOI] [PubMed] [Google Scholar]
- 43.Signorini DJHP, Monteiro MCM, de Andrade MFC, Signorini DH, Eyer-Silva WA. What should we know about metabolic syndrome and lipodystrophy in AIDS? Revista da Associacao Medica Brasileira. 2012;58: 70–75. [PubMed] [Google Scholar]
- 44.Mondy K, Overton ET, Grubb J, Tong S, Seyfried W, Powderly W, et al. Metabolic syndrome in HIV-infected patients from an urban, midwestern US outpatient population. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2007;44: 726–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tesfaye DY, Kinde S, Medhin G, Megerssa YC, Tadewos A, Tadesse E, et al. Burden of metabolic syndrome among HIV-infected patients in Southern Ethiopia. Diabetes & metabolic syndrome. 2014;8: 102–107. [DOI] [PubMed] [Google Scholar]
- 46.Mbunkah HA, Meriki HD, Kukwah AT, Nfor O, Nkuo-Akenji T. Prevalence of metabolic syndrome in human immunodeficiency virus—infected patients from the South-West region of Cameroon, using the adult treatment panel III criteria. Diabetology & metabolic syndrome. 2014;6: 92-5996-5996-5992. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Biron A, Bobin-Dubigeon C, Volteau C, Piroth L, Perre P, Leport C, et al. Metabolic syndrome in French HIV-infected patients: prevalence and predictive factors after 3 years of antiretroviral therapy. AIDS Research and Human Retroviruses. 2012;28: 1672–1678. 10.1089/AID.2012.0048 [DOI] [PubMed] [Google Scholar]
- 48.Ayodele OE, Akinboro AO, Akinyemi SO, Adepeju AA, Akinremi OA, Alao CA, et al. Prevalence and clinical correlates of metabolic syndrome in Nigerians living with human immunodeficiency virus/acquired immunodeficiency syndrome. Metabolic syndrome and related disorders. 2012;10: 373–379. [DOI] [PubMed] [Google Scholar]
- 49.Badiou S, Thiebaut R, Aurillac-Lavignolle V, Dabis F, Laporte F, Cristol JP, et al. Association of non-HDL cholesterol with subclinical atherosclerosis in HIV-positive patients. The Journal of infection. 2008;57: 47–54. 10.1016/j.jinf.2008.05.007 [DOI] [PubMed] [Google Scholar]
- 50.Bonfanti P, De Socio GL, Marconi P, Franzetti M, Martinelli C, Vichi F, et al. Is metabolic syndrome associated to HIV infection per se? Results from the HERMES study. Current HIV research. 2010;8: 165–171. [DOI] [PubMed] [Google Scholar]
- 51.Palacios R, Santos J, Gonzalez M, Ruiz J, Marquez M. Incidence and prevalence of the metabolic syndrome in a cohort of naive HIV-infected patients: prospective analysis at 48 weeks of highly active antiretroviral therapy. International Journal of STD & AIDS. 2007;18: 184–187. [DOI] [PubMed] [Google Scholar]
- 52.Worm SW, Friis-Moller N, Bruyand M, D'Arminio Monforte A, Rickenbach M, Reiss P, et al. High prevalence of the metabolic syndrome in HIV-infected patients: impact of different definitions of the metabolic syndrome. AIDS (London, England). 2010;24: 427–435. [DOI] [PubMed] [Google Scholar]
- 53.Farhangi MA, Keshavarz SA, Eshraghian M, Ostadrahimi A, Saboor-Yaraghi AA. White blood cell count in women: relation to inflammatory biomarkers, haematological profiles, visceral adiposity, and other cardiovascular risk factors. J Health Popul Nutr. 2013;31: 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Maloberti A, Giannattasio C, Dozio D, Betelli M, Villa P, Nava S, et al. Metabolic syndrome in human immunodeficiency virus-positive subjects: prevalence, phenotype, and related alterations in arterial structure and function. Metabolic syndrome and related disorders. 2013;11: 403–411. 10.1089/met.2013.0008 [DOI] [PubMed] [Google Scholar]
- 55.Fisac C, Virgili N, Ferrer E, Barbera MJ, Fumero E, Vilarasau C, et al. A comparison of the effects of nevirapine and nelfinavir on metabolism and body habitus in antiretroviral-naive human immunodeficiency virus-infected patients: a randomized controlled study. J Clin Endocrinol Metab. 2003;88: 5186–5192. [DOI] [PubMed] [Google Scholar]
- 56.Sanada S, Nishida M, Ishii K, Moriyama T, Komuro I, Yamauchi-Takihara K. Smoking promotes subclinical atherosclerosis in apparently healthy men: 2-year ultrasonographic follow-up. Circ J. 2012;76: 2884–2891. [DOI] [PubMed] [Google Scholar]
- 57.Wada T, Urashima M, Fukumoto T. Risk of metabolic syndrome persists twenty years after the cessation of smoking. Intern Med. 2007;46: 1079–1082. [DOI] [PubMed] [Google Scholar]
- 58.Onat A, Ugur M, Hergenc G, Can G, Ordu S, Dursunoglu D. Lifestyle and metabolic determinants of incident hypertension, with special reference to cigarette smoking: a longitudinal population-based study. Am J Hypertens. 2009;22: 156–162. 10.1038/ajh.2008.332 [DOI] [PubMed] [Google Scholar]
- 59.Chen JJ, Yu CB, Du WB, Li LJ. Prevalence of hepatitis B and C in HIV-infected patients: a meta-analysis. Hepatobiliary Pancreat Dis Int. 2011;10: 122–127. [DOI] [PubMed] [Google Scholar]
- 60.Adeyemi O, Rezai K, Bahk M, Badri S, Thomas-Gossain N. Metabolic syndrome in older HIV-infected patients: data from the CORE50 cohort. AIDS Patient Care and STDs. 2008;22: 941–945. 10.1089/apc.2008.0119 [DOI] [PubMed] [Google Scholar]
- 61.Ances BM, Bhatt A, Vaida F, Rosario D, Alexander T, Marquie-Beck J, et al. Role of metabolic syndrome components in human immunodeficiency virus-associated stroke. Journal of neurovirology. 2009;15: 249–256. 10.1080/13550280902962443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hadigan C, Edwards E, Rosenberg A, Purdy JB, Fleischman E, Howard L, et al. Microalbuminuria in HIV disease. American Journal of Nephrology. 2013;37: 443–451. 10.1159/000350384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tiozzo E, Konefal J, Adwan S, Martinez LA, Villabona J, Lopez J, et al. A cross-sectional assessment of metabolic syndrome in HIV-infected people of low socio-economic status receiving antiretroviral therapy Changes in metabolic syndrome status after initiation of antiretroviral therapy. Diabetol Metab Syndr. 2015;7: 15 10.1186/s13098-015-0008-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Silva EF, Bassichetto KC, Lewi DS. Lipid profile, cardiovascular risk factors and metabolic syndrome in a group of AIDS patients. Arquivos Brasileiros de Cardiologia. 2009;93: 113–118. [DOI] [PubMed] [Google Scholar]
- 65.Lauda LG, Mariath AB, Grillo LP. Metabolic syndrome and its components in HIV-infected individuals. Revista da Associacao Medica Brasileira (1992). 2011;57: 182–186. [DOI] [PubMed] [Google Scholar]
- 66.Alencastro PR, Wolff FH, Oliveira RR, Ikeda ML, Barcellos NT, Brandao AB, et al. Metabolic syndrome and population attributable risk among HIV/AIDS patients: comparison between NCEP-ATPIII, IDF and AHA/NHLBI definitions. AIDS research and therapy. 2012;9: 29-6405-6409-6429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gasparotto AS, Sprinz E, Lazzaretti RK, Kuhmmer R, Silveira JM, Basso RP, et al. Genetic polymorphisms in estrogen receptors and sexual dimorphism in fat redistribution in HIV-infected patients on HAART. AIDS (London, England). 2012;26: 19–26. [DOI] [PubMed] [Google Scholar]
- 68.Gazzaruso C, Bruno R, Garzaniti A, Giordanetti S, Fratino P, Sacchi P, et al. Hypertension among HIV patients: prevalence and relationships to insulin resistance and metabolic syndrome. Journal of hypertension. 2003;21: 1377–1382. [DOI] [PubMed] [Google Scholar]
- 69.Bergersen BM, Schumacher A, Sandvik L, Bruun JN, Birkeland K. Important differences in components of the metabolic syndrome between HIV-patients with and without highly active antiretroviral therapy and healthy controls. Scandinavian Journal of Infectious Diseases. 2006;38: 682–689. [DOI] [PubMed] [Google Scholar]
- 70.Estrada V, Martinez-Larrad MT, Gonzalez-Sanchez JL, de Villar NG, Zabena C, Fernandez C, et al. Lipodystrophy and metabolic syndrome in HIV-infected patients treated with antiretroviral therapy. Metabolism: clinical and experimental. 2006;55: 940–945. [DOI] [PubMed] [Google Scholar]
- 71.Bonfanti P, Giannattasio C, Ricci E, Facchetti R, Rosella E, Franzetti M, et al. HIV and metabolic syndrome: a comparison with the general population. Journal of acquired immune deficiency syndromes (1999). 2007;45: 426–431. [DOI] [PubMed] [Google Scholar]
- 72.Schillaci G, De Socio GV, Pucci G, Mannarino MR, Helou J, Pirro M, et al. Aortic stiffness in untreated adult patients with human immunodeficiency virus infection. Hypertension. 2008;52: 308–313. 10.1161/HYPERTENSIONAHA.108.114660 [DOI] [PubMed] [Google Scholar]
- 73.Hansen BR, Petersen J, Haugaard SB, Madsbad S, Obel N, Suzuki Y, et al. The prevalence of metabolic syndrome in Danish patients with HIV infection: The effect of antiretroviral therapy. HIV Medicine. 2009;10: 378–387. 10.1111/j.1468-1293.2009.00697.x [DOI] [PubMed] [Google Scholar]
- 74.Young J, Glass TR, Bernasconi E, Rickenbach M, Furrer H, Hirschel B, et al. Hierarchical modeling gave plausible estimates of associations between metabolic syndrome and components of antiretroviral therapy. Journal of clinical epidemiology. 2009;62: 632–641. 10.1016/j.jclinepi.2008.07.015 [DOI] [PubMed] [Google Scholar]
- 75.Calza L, Masetti G, Piergentili B, Trapani F, Cascavilla A, Manfredi R, et al. Prevalence of diabetes mellitus, hyperinsulinaemia and metabolic syndrome among 755 adult patients with HIV-1 infection. International Journal of STD and AIDS. 2011;22: 43–45. 10.1258/ijsa.2010.010256 [DOI] [PubMed] [Google Scholar]
- 76.Guaraldi G, Lonardo A, Ballestri S, Zona S, Stentarelli C, Orlando G, et al. Human immunodeficiency virus is the major determinant of steatosis and hepatitis C virus of insulin resistance in virus-associated fatty liver disease. Archives of Medical Research. 2011;42: 690–697. 10.1016/j.arcmed.2011.12.009 [DOI] [PubMed] [Google Scholar]
- 77.Janiszewski PM, Ross R, Despres JP, Lemieux I, Orlando G, Carli F, et al. Hypertriglyceridemia and waist circumference predict cardiovascular risk among HIV patients: a cross-sectional study. PLoS One. 2011;6: e25032 10.1371/journal.pone.0025032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fourie CM, Van Rooyen JM, Kruger A, Schutte AE. Lipid abnormalities in a never-treated HIV-1 subtype C-infected African population. Lipids. 2010;45: 73–80. 10.1007/s11745-009-3369-4 [DOI] [PubMed] [Google Scholar]
- 79.Berhane T, Yami A, Alemseged F, Yemane T, Hamza L, Kassim M, et al. Prevalence of lipodystrophy and metabolic syndrome among HIV positive individuals on highly active anti-retroviral treatment in Jimma, south west Ethiopia. Pan African Medical Journal. 2012;13. [PMC free article] [PubMed] [Google Scholar]
- 80.Muhammad S, Sani MU, Okeahialam BN. Cardiovascular disease risk factors among HIV-infected Nigerians receiving highly active antiretroviral therapy. Nigerian medical journal: journal of the Nigeria Medical Association. 2013;54: 185–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bajaj S, Tyagi SK, Bhargava A. Metabolic syndrome in human immunodeficiency virus positive patients. Indian journal of endocrinology and metabolism. 2013;17: 117–120. 10.4103/2230-8210.107821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jantarapakde J, Phanuphak N, Chaturawit C, Pengnonyang S, Mathajittiphan P, Takamtha P, et al. Prevalence of metabolic syndrome among antiretroviral-naive and antiretroviral-experienced HIV-1 infected thai adults. AIDS Patient Care and STDs. 2014;28: 331–340. 10.1089/apc.2013.0294 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.