Abstract
OBJECTIVE
Dietary interventions in patients with type 2 diabetes (T2D) are important for preventing long-term complications. Although a healthy diet is crucial, there is still uncertainty about the optimal macronutrient composition. We performed a meta-analysis comparing diets high in cis-monounsaturated fatty acids (MUFA) to diets high in carbohydrates (CHO) or in polyunsaturated fatty acids (PUFA) on metabolic risk factors in patients with T2D.
RESEARCH DESIGN AND METHODS
We systematically reviewed PubMed, MEDLINE, and Cochrane databases and prior systematic reviews and meta-analyses to identify interventions assessing HbA1c, fasting plasma glucose and insulin, LDL and HDL cholesterol, triglycerides, body weight, or systolic/diastolic blood pressure. Meta-analyses were conducted using both fixed- and random-effects models to calculate the weighted mean difference (WMD) and 95% CI.
RESULTS
We identified 24 studies totaling 1,460 participants comparing high-MUFA to high-CHO diets and 4 studies totaling 44 participants comparing high-MUFA to high-PUFA diets. When comparing high-MUFA to high-CHO diets, there were significant reductions in fasting plasma glucose (WMD −0.57 mmol/L [95% CI −0.76, −0.39]), triglycerides (−0.31 mmol/L [−0.44, −0.18]), body weight (−1.56 kg [−2.89, −0.23]), and systolic blood pressure (−2.31 mmHg [−4.13, −0.49]) along with significant increases in HDL cholesterol (0.06 mmol/L [0.02, 0.10]). When high-MUFA diets were compared with high-PUFA diets, there was a significant reduction in fasting plasma glucose (−0.87 mmol/L [−1.67, −0.07]). All of the outcomes had low to medium levels of heterogeneity, ranging from 0.0 to 69.5% for diastolic blood pressure (Phet = 0.011).
CONCLUSIONS
Our meta-analysis provides evidence that consuming diets high in MUFA can improve metabolic risk factors among patients with T2D.
Introduction
Dietary interventions in patients with type 2 diabetes (T2D) are an important adjunct to physical activity, medication, and insulin therapy in the prevention of diabetes-associated complications, particularly cardiovascular disease (CVD) (1). Current recommendations by the American Diabetes Association emphasize the inclusion of cis-monounsaturated fatty acids (MUFA) and polyunsaturated fatty acids (PUFA) in the diet of individuals with T2D over intake of saturated fats and trans fatty acids (2). Although the evidence for quantity of total fat intake is inconclusive, there is a growing body of evidence supporting the importance of the quality of fat (1,3) for the prevention of CVD in this group. Results from the PREvención con DIeta MEDiterránea (PREDIMED) trial, which recruited individuals with prevalent T2D, also showed that diets high in olive oil and nuts, foods that are rich in MUFA, prevented CVD events in a high-risk population (4). Foods rich in MUFA and PUFA have been shown to favorably impact blood lipid concentrations thus decreasing the risk of CVD (5,6). High-MUFA diets have gained significant attention as an alternative dietary pattern to the commonly recommended low-fat and high-carbohydrate (CHO) pattern. Several prior meta-analyses of randomized controlled trials (RCTs) suggested potential benefits of a high-MUFA diet compared with a high-CHO diet in improving metabolic factors, such as glycemic control, serum lipids, and blood pressure, among both healthy individuals and T2D patients (3,5,7) but were usually based on a relatively small number of studies/subjects or short duration of follow-up. Hence, there is still uncertainty regarding whether longer-term interventions that substitute MUFA for CHO will yield the same metabolic effects as short-term trials. Furthermore, many of the RCTs also implemented caloric restriction as part of the dietary intervention, which may impede long-term compliance. Thus we conducted an updated meta-analysis comparing high-MUFA to high-CHO diets on metabolic risk factors among patients with T2D. We also included a comparison between high-MUFA and high-PUFA diets, which has not been previously assessed in a systematic manner to our knowledge.
Research Design and Methods
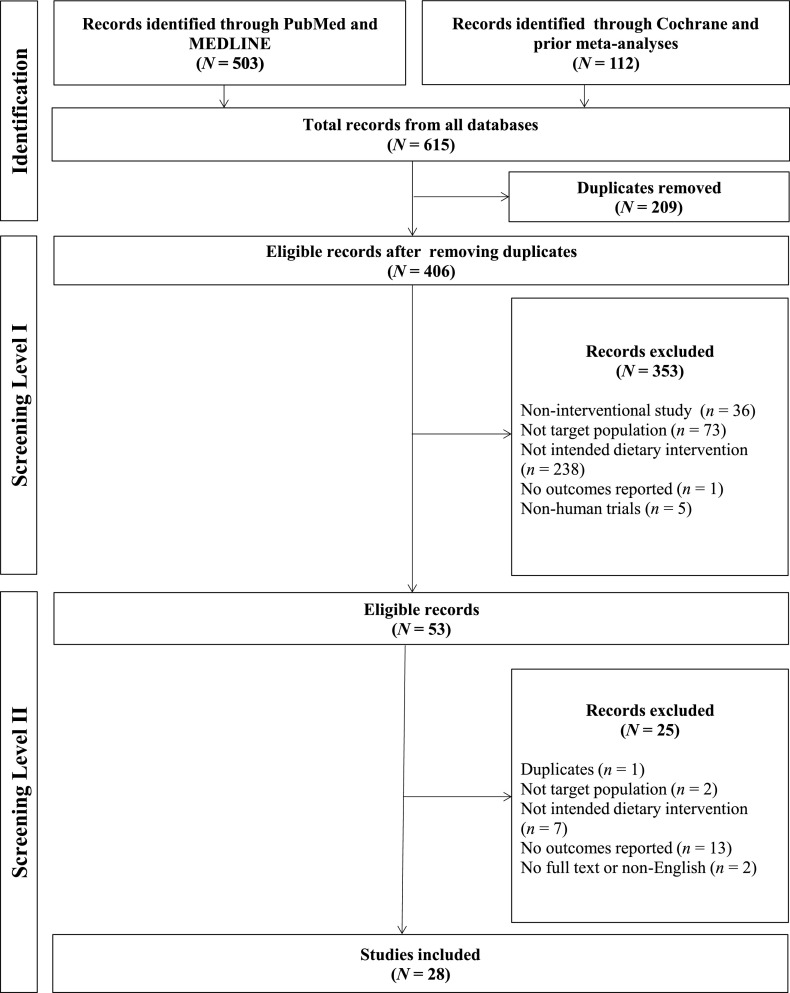
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Fig. 1) (8).
Figure 1.
PRISMA diagram on trials of MUFA or PUFA dietary interventions in patients with T2D.
Data Sources and Searches
We searched PubMed, MEDLINE, Cochrane Central Register of Controlled Trials, and prior meta-analyses for articles up through 31 March 2015. The key words used to identify studies included “type 2 diabetes” or “type II diabetes” or “non-insulin diabetes”; “monounsaturated fatty acid” or “MUFA”; “polyunsaturated fatty acid” or “PUFA”; “glycemic” or “glucose” or “HbA1c”; “lipid” or “cholesterol”; and “randomized” or “trial.” The search was limited to RCTs that were published in English and had an intervention and follow-up duration of at least 2 weeks. Full details on our search terms and strategy for PubMed are shown in Supplementary Fig. 1.
Study Selection
RCTs (either parallel or crossover designs) comparing the effects of high-CHO or high-PUFA diets (from plant sources or n-6) with those of high-MUFA diets on metabolic parameters among adults with T2D were included in the meta-analysis. Studies that included the additional use of medications or supplements, changes in physical activity, patients with type 1 diabetes or unconfirmed T2D/glucose intolerance, or interventions using n-3 fatty acids or other unspecified dietary changes were excluded. Detailed inclusion/exclusion criteria are shown in Supplementary Table 1. From the initial search results, one author (F.Q.) screened titles and abstracts and identified the full-text articles for inclusion in the meta-analysis. A second author (A.A.K.) confirmed that all articles that were included in the meta-analysis met the inclusion and exclusion criteria.
Data Extraction and Quality Assessment
Data were extracted independently by two authors (F.Q. and A.A.K.) and any discrepancies that arose were adjudicated by a third author (F.B.H.). The following information was extracted: study design (randomized parallel, randomized crossover, inpatient/outpatient), trial arms/sample size, study duration, mean dietary composition (percent of total energy), age of participants, baseline BMI, duration of diabetes, and means and SDs of changes in HbA1c (%), fasting plasma glucose (mmol/L), fasting insulin (pmol/L), LDL cholesterol (mmol/L), HDL cholesterol (mmol/L), triglycerides (mmol/L), body weight (kg), and 24-h measurements of systolic blood pressure (mmHg) and diastolic blood pressure (mmHg) from baseline to the end of follow-up. Data were extracted from the primary publications with proper transformations done to harmonize the units used. Authors of original publications were contacted when necessary to obtain additional data.
Study Quality and Risk of Bias
RCTs meeting the inclusion criteria above were evaluated for risk of bias using the Cochrane Collaboration’s tool for assessing risk of bias and were categorized as having a “high risk of bias,” “low risk of bias,” or “unclear risk of bias” (9). Specifically, RCTs were reviewed for allocation concealment, blinding approaches, approaches for incomplete outcome data, selective reporting, and bias due to problems arising from other issues.
Data Synthesis and Analysis
Our outcome of interest was the weighted mean difference (WMD) from baseline to the end of follow-up in the metabolic parameters listed above between the high-MUFA diet and the high-CHO or high-PUFA diets. WMD was calculated using both the random-effects and fixed-effects models. We considered random-effects analysis the main focus of our meta-analysis. Subgroup analyses were conducted based on the age of participants, baseline BMI, duration of diabetes, MUFA replacement (difference in percent energy from MUFA in the intervention and control arms), duration of follow-up (weeks), and study design (parallel vs. crossover). Heterogeneity between trial results was tested with a standard χ2 test. The I2 parameter was used to quantify any inconsistency: I2 = [(Q – d.f.)] ×100%, where Q is the χ2 statistic and d.f. is its degrees of freedom (10). Meta-regressions involving the above baseline characteristics as both continuous and categorical variables were also performed to identify potential sources of heterogeneity. Publication bias was assessed visually with funnel plots and with Egger and Begg-Mazudumar regression tests (11,12). Sensitivity analyses in which each study was removed in turn to assess the influence of that study on the overall effect size were also conducted. Statistical analyses were conducted with Stata 13.0, including the metan module (StataCorp, College Station, TX).
Results
Literature
A total of 615 records were identified in the initial search and 406 abstracts were selected for review after removing duplicates. After stage 1 screening, 53 records underwent full-text screening. Overall, 28 studies were included in the meta-analysis with 24 for MUFA vs. CHO diets (13–37), totaling 1,460 participants, and 4 for MUFA vs. PUFA diets (38–41), totaling 44 participants. The number of available comparisons for MUFA vs. CHO diets was 28 as some trials had more than two arms. The baseline characteristics of the included studies are shown in Table 1. Outcome results at the end of follow-up for each study were included in Supplementary Table 4. Because of a limited number of studies comparing high-MUFA and high-PUFA diets, only certain metabolic outcomes were analyzed in the meta-analysis for this comparison.
Table 1.
Baseline characteristics of published studies
| Study design |
Duration of intervention and follow-up (weeks) |
Trial arms |
Sample size* |
Intervention |
Control |
Difference in % of energy from MUFA |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) |
BMI (kg/m2) |
Duration of diabetes (years) |
Mean dietary composition (% of energy) |
Age (years) |
BMI (kg/m2) |
Duration of diabetes (years) |
Mean dietary composition (% of energy) |
||||||||||||||
| Protein | CHO | Fat | MUFA | PUFA | Protein | Carbohydrate | Fat | MUFA | PUFA | ||||||||||||
| High-MUFA vs. high-CHO diet | |||||||||||||||||||||
| Lasa 2014 (13) |
Parallel, outpatient |
52 |
MUFA (olive oil) vs. LF |
141 |
67.4 |
29.4 |
— |
16.5 |
38.6 |
42.0 |
22.1 |
— |
67.2 |
29.8 |
— |
17.0 |
41.2 |
39.3 |
19.6 |
— |
2.5 |
| Lasa 2014 (13) |
Parallel, outpatient |
52 |
MUFA (nuts) vs. LF |
117 |
67.1 |
30.1 |
— |
16.5 |
36.6 |
44.5 |
21.3 |
— |
67.2 |
29.8 |
— |
17.0 |
41.2 |
39.3 |
19.6 |
— |
1.7 |
| Itsiopoulos 2011 (14) |
Crossover, outpatient |
12 |
MED vs. control |
54 |
— |
— |
6.0 |
13.5 |
43.5 |
39.0 |
21.3 |
— |
— |
— |
6.0 |
18.2 |
46.4 |
31.5 |
11.1 |
— |
10.2 |
| Elhayany 2010 (15) |
Parallel, outpatient |
48 |
MED (low-CHO) vs. LF |
116 |
55.5 |
31.4 |
5.3 |
32.0 |
35.0 |
45.0 |
23.0 |
— |
56.0 |
31.8 |
5.3 |
20.0 |
50.0 |
30.0 |
10.0 |
— |
13.0 |
| Elhayany 2010 (15) |
Parallel, outpatient |
48 |
MED (traditional) vs. LF |
118 |
57.4 |
31.1 |
5.7 |
60.0 |
50.0 |
30.0 |
10.0 |
— |
56.0 |
31.8 |
5.7 |
20.0 |
50.0 |
30.0 |
10.0 |
— |
0.0 |
| Brehm 2009 (16) |
Parallel, outpatient |
48 |
MUFA vs. CHO |
95 |
56.5 |
35.9 |
— |
15.0 |
45.0 |
40.0 |
20.0 |
— |
56.5 |
35.9 |
— |
15.0 |
60.0 |
25.0 |
— |
— |
— |
| Esposito 2009 (17) |
Parallel, outpatient |
52 |
MED vs. LF |
215 |
52.4 |
29.7 |
0.0 |
18.3 |
42.7 |
39.0 |
18.0 |
— |
51.9 |
29.5 |
0.0 |
18.3 |
53.2 |
28.3 |
12.0 |
— |
6.0 |
| Wolever 2008 (18,19) |
Parallel, outpatient |
48 |
MUFA vs. HGI |
101 |
58.6 |
31.1 |
— |
19.1 |
39.3 |
40.1 |
18.3 |
— |
60.4 |
30.1 |
— |
20.4 |
46.5 |
30.8 |
12.3 |
— |
6.0 |
| Wolever 2008 (18,19) |
Parallel, outpatient |
48 |
MUFA vs. LGI |
108 |
58.6 |
31.1 |
— |
19.1 |
39.3 |
40.1 |
18.3 |
— |
60.6 |
31.6 |
— |
20.6 |
51.9 |
26.5 |
10.7 |
— |
7.6 |
| Brunerova 2007 (20) |
Parallel, outpatient |
12 |
MUFA vs. CHO |
27 |
54.7 |
33.4 |
— |
10.0 |
45.0 |
45.0 |
22.5 |
— |
51.2 |
34.7 |
— |
10.0 |
60.0 |
30.0 |
10.0 |
— |
12.5 |
| Leon-Sanz 2005 (21) |
Parallel, inpatient |
2 |
MUFA vs. CHO |
63 |
73.9 |
25.5 |
— |
16.7 |
37.5 |
50.1 |
34.2 |
— |
70.6 |
26.5 |
— |
13.6 |
50.0 |
28.8 |
8.7 |
— |
25.5 |
| Shah 2005 (22) |
Parallel, outpatient |
14 |
MUFA vs. CHO |
21 |
58.0 |
28.1 |
— |
15.0 |
40.0 |
45.0 |
25.0 |
— |
58.0 |
28.1 |
— |
15.0 |
55.0 |
30.0 |
10.0 |
— |
15.0 |
| Gerhard 2004 (23) |
Crossover, outpatient |
6 |
MUFA vs. LF |
22 |
50.4 |
37.2 |
— |
35.3 |
45.1 |
39.6 |
25.1 |
— |
50.4 |
37.2 |
— |
14.5 |
64.7 |
20.8 |
8.3 |
— |
16.8 |
| Rodriguez-Villar 2004 (24) |
Crossover, outpatient |
6 |
MUFA vs. CHO |
44 |
61.0 |
28.3 |
5.3 |
17.5 |
41.4 |
40.2 |
24.9 |
— |
61.0 |
28.3 |
5.3 |
18.9 |
52.3 |
27.9 |
13.6 |
— |
11.3 |
| Lovejoy 2002 (25) |
Crossover, outpatient |
4 |
HF vs. LF |
60 |
53.8 |
33.0 |
— |
14.9 |
45.8 |
39.0 |
22.5 |
— |
53.8 |
33.0 |
— |
14.7 |
58.1 |
27.2 |
15.5 |
— |
7.0 |
| Rodriguez-Villar 2000 (26) |
Crossover, outpatient |
6 |
MUFA vs. CHO |
24 |
— |
27.9 |
6.0 |
16.3 |
43.3 |
40.1 |
24.8 |
— |
— |
27.9 |
6.0 |
17.3 |
53.5 |
28.6 |
11.6 |
— |
13.2 |
| Tsihlias 2000 (27) |
Parallel, outpatient |
24 |
MUFA vs. HGI |
61 |
63.0 |
27.8 |
— |
17.8 |
43.2 |
37.2 |
17.5 |
— |
62.9 |
28.0 |
— |
17.0 |
53.5 |
28.9 |
11.3 |
— |
6.2 |
| Tsihlias 2000 (27) |
Parallel, outpatient |
24 |
MUFA vs. LGI |
62 |
63.0 |
27.8 |
— |
17.8 |
43.2 |
37.2 |
17.5 |
— |
61.8 |
27.7 |
— |
19.7 |
50.1 |
28.3 |
10.7 |
— |
6.8 |
| Gumbiner 1998 (28) |
Parallel, outpatient |
6 |
MUFA vs. CHO |
17 |
55.0 |
36.3 |
7.4 |
20.6 |
9.5 |
69.9 |
49.0 |
— |
51.0 |
37.2 |
7.4 |
19.5 |
70.1 |
10.3 |
1.0 |
— |
48.0 |
| McCargar 1998 (29) |
Parallel, inpatient |
4 |
MUFA vs. CHO |
32 |
55.0 |
28.4 |
4.5 |
17.6 |
33.0 |
50.0 |
32.4 |
— |
59.0 |
28.7 |
4.5 |
14.5 |
55.0 |
30.5 |
— |
— |
— |
| Campbell 1994 (30) |
Crossover, outpatient |
2 |
MUFA vs. CHO |
20 |
55.0 |
26.5 |
4.6 |
41.0 |
40.0 |
37.0 |
22.0 |
— |
55.0 |
26.5 |
4.6 |
23.0 |
55.0 |
22.0 |
8.0 |
— |
14.0 |
| Garg 1994 (31) |
Parallel, outpatient |
6 |
MUFA vs. CHO |
42 |
58.0 |
28.1 |
— |
15.0 |
40.0 |
45.0 |
25.0 |
— |
58.0 |
28.1 |
— |
15.0 |
55.0 |
30.0 |
10.0 |
— |
15.0 |
| Lerman-Garber 1994 (32) |
Crossover, outpatient |
4 |
MUFA vs. CHO |
24 |
56.0 |
28.0 |
— |
20.0 |
40.0 |
40.0 |
24.0 |
— |
56.0 |
28.0 |
— |
20.0 |
60.0 |
20.0 |
6.6 |
— |
17.4 |
| Rasmussen 1993 (33) |
Crossover, outpatient |
3 |
MUFA vs. CHO |
30 |
57.0 |
27.0 |
6.0 |
14.0 |
36.0 |
50.0 |
30.0 |
— |
57.0 |
27.0 |
6.0 |
17.0 |
49.0 |
32.0 |
11.0 |
— |
19.0 |
| Garg 1992 (34) |
Crossover, outpatient |
3 |
MUFA vs. CHO |
16 |
63.0 |
30.0 |
— |
15.0 |
35.0 |
50.0 |
32.0 |
— |
63.0 |
30.0 |
— |
15.0 |
60.0 |
25.0 |
12.0 |
— |
20.0 |
| Parillo 1992 (35) |
Crossover, outpatient |
2 |
MUFA vs. CHO |
20 |
52.7 |
26.7 |
8.4 |
20.0 |
40.0 |
40.0 |
29.0 |
— |
52.7 |
26.7 |
8.4 |
20.0 |
60.0 |
20.0 |
13.0 |
— |
16.0 |
| Rivellese 1990 (36) |
Crossover, outpatient |
2 |
MUFA vs. CHO |
16 |
45.0 |
22.0 |
5.0 |
— |
— |
— |
— |
— |
45.0 |
22.0 |
5.0 |
— |
— |
— |
— |
— |
— |
| Garg 1988 (37) |
Crossover, outpatient |
4 |
MUFA vs. CHO |
20 |
56.0 |
29.0 |
— |
15.0 |
35.0 |
50.0 |
33.0 |
— |
56.0 |
29.0 |
— |
15.0 |
60.0 |
25.0 |
9.0 |
— |
24.0 |
| High-MUFA vs. high-PUFA |
|||||||||||||||||||||
| Madigan 2005 (38) |
Crossover, outpatient |
2 |
MUFA vs. PUFA |
12 |
56.0 |
28.0 |
— |
— |
— |
— |
— |
— |
56.0 |
28.0 |
— |
— |
— |
— |
— |
— |
— |
| Brynes 2000 (39) |
Crossover, outpatient |
3 |
MUFA vs. PUFA |
18 |
56.0 |
29.8 |
3.0 |
13.5 |
47.2 |
39.1 |
20.3 |
4.2 |
56.0 |
29.8 |
3.0 |
12.4 |
46.5 |
41.1 |
11.7 |
13.4 |
8.6 |
| Thomsen 1995 (40) |
Crossover, outpatient |
3 |
MUFA vs. PUFA |
32 |
59.0 |
28.0 |
6.0 |
13.0 |
37.0 |
49.0 |
30.0 |
7.0 |
59.0 |
28.0 |
6.0 |
13.0 |
36.0 |
49.0 |
10.0 |
27.0 |
20.0 |
| Parfitt 1994 (41) | Crossover, outpatient | 6 | MUFA vs. PUFA | 26 | 58.0 | 28.4 | 4.2 | 14.6 | 34.4 | 50.2 | 28.2 | 6.8 | 59.0 | 28.4 | 4.2 | 18.0 | 34.3 | 46.5 | 15.1 | 16.7 | 13.1 |
HF, high fat; HGI, high glycemic index; LF, low fat; LGI, low glycemic index; MED, Mediterranean diet.
*For crossover trials, the sample size is double the number of actual participants because each participant received both interventions.
Of the 24 studies identified for the MUFA vs. CHO diet comparisons, 12 had a parallel design and 12 had a crossover design. The mean dietary composition for the high-MUFA arm was 17.0% protein, 39.4% CHO, 43.1% fat, and 24.5% MUFA; the mean dietary composition for the high-CHO arm was 17.3% protein, 54.1% CHO, 27.6% fat, and 11.0% MUFA. The mean and median duration of the interventions were 19.3 and 6 weeks, respectively.
All of the MUFA vs. PUFA diet comparisons used a crossover design. The mean dietary composition for the high-MUFA arm was 13.7% protein, 39.5% CHO, 46.1% fat, 26.2% MUFA, and 6.0% PUFA; the mean dietary composition for the high-PUFA arm was 14.5% protein, 38.9% CHO, 45.5% fat, 12.3% MUFA, and 19.0% PUFA. The mean and median duration of the interventions were 3.5 and 3 weeks, respectively.
Glycemic Control
The meta-analysis showed that a high-MUFA diet compared with a high-CHO diet resulted in a significant reduction in fasting plasma glucose (WMD −0.57 mmol/L [95% CI −0.76, −0.39]) and a nonsignificant reduction in HbA1c (%) and fasting insulin (pmol/L) (Table 2). There was a moderate level of heterogeneity for HbA1c (%) (I2 = 40.2%, Phet = 0.044). A high-MUFA diet compared with a high-PUFA diet resulted in significant reductions in fasting plasma glucose (−0.87 mmol/L [−1.67, −0.07]) and a nonsignificant reduction in fasting insulin (Table 3). Forest plots for all of these outcomes can be found in Supplementary Fig. 2.
Table 2.
Metabolic effects in T2D patients consuming a high-MUFA diet compared with a high-CHO diet
| Metabolic parameter | Number of studies | Number of participants | WMD (95% CI)* | WMD (95% CI)† | I2 (%) | Phet |
|---|---|---|---|---|---|---|
| HbA1c (%) |
14 |
925 |
−0.08 (−0.15, 0.00) |
−0.11 (−0.24, 0.02) |
40.2 |
0.044 |
| Fasting plasma glucose (mmol/L) |
22 |
1,283 |
−0.57 (−0.76, −0.39) |
−0.57 (−0.76, −0.39) |
0.0 |
0.521 |
| Fasting insulin (pmol/L) |
11 |
679 |
−3.98 (−9.83, 1.87) |
−3.98 (−9.83, 1.87) |
0.0 |
0.768 |
| LDL cholesterol (mmol/L) |
17 |
791 |
0.00 (−0.08, 0.08) |
0.05 (−0.07, 0.16) |
40.2 |
0.033 |
| HDL cholesterol (mmol/L) |
20 |
1,067 |
0.07 (0.05, 0.10) |
0.06 (0.02, 0.10) |
45.4 |
0.010 |
| Triglycerides (mmol/L) |
21 |
1,075 |
−0.29 (−0.36, −0.22) |
−0.31 (−0.44, −0.18) |
54.0 |
0.001 |
| Body weight (kg) |
16 |
1,081 |
−1.56 (−2.89, −0.23) |
−1.56 (−2.89, −0.23) |
0.0 |
1.000 |
| Systolic blood pressure (mmHg) |
6 |
529 |
−2.25 (−3.79, −0.70) |
−2.31 (−4.13, −0.49) |
16.5 |
0.304 |
| Diastolic blood pressure (mmHg) | 5 | 373 | −1.33 (−2.91, 0.25) | −2.64 (−5.91, 0.63) | 69.5 | 0.011 |
Values in boldface type indicate statistical significance at P < 0.05.
*Calculated using a fixed-effects model.
†Calculated using a random-effects model.
Table 3.
Metabolic effects in T2D patients consuming a high-MUFA diet compared with a high-PUFA diet
| Metabolic parameter | Number of studies | Number of participants | WMD (95% CI)* | WMD (95% CI)† | I2 (%) | Phet |
|---|---|---|---|---|---|---|
| Fasting plasma glucose (mmol/L) |
3 |
31 |
−0.87 (−1.67, −0.07) |
−0.87 (−1.67, −0.07) |
26.3 |
0.257 |
| Fasting insulin (pmol/L) |
2 |
15 |
−7.56 (−26.15, 11.03) |
−7.56 (−26.15, 11.03) |
0.0 |
0.516 |
| LDL cholesterol (mmol/L) |
4 |
44 |
−0.15 (−0.43, 0.13) |
−0.15 (−0.44, 0.14) |
5.9 |
0.363 |
| HDL cholesterol (mmol/L) |
4 |
44 |
0.04 (−0.07, 0.15) |
0.04 (−0.07, 0.15) |
0.0 |
0.848 |
| Triglycerides (mmol/L) | 3 | 31 | 0.01 (−0.46, 0.47) | 0.01 (−0.46, 0.47) | 0.0 | 0.941 |
HbA1c, weight, systolic blood pressure, and diastolic blood pressure were not included in this analysis due to the limited number of studies reporting these outcomes. Values in boldface type indicate statistical significance at P < 0.05.
*Calculated using a fixed-effects model.
†Calculated using a random-effects model.
Serum Lipids
On the basis of our meta-analysis, a high-MUFA diet compared with a high-CHO diet resulted in a nonsignificant increase in LDL cholesterol, a significant increase in HDL cholesterol (WMD 0.06 mmol/L [95% CI 0.02, 0.10]), and a significant reduction in triglycerides (−0.31 mmol/L [−0.44, −0.18]) (Table 2), although there was considerable heterogeneity (HDL cholesterol I2 = 45.4%, P = 0.010; triglycerides I2 = 54.0%, P = 0.001) (Table 2). Comparing a high-MUFA diet to a high-PUFA diet, there was a nonsignificant reduction in of LDL cholesterol and nonsignificant increases in HDL cholesterol and triglycerides (Table 3).
Other Metabolic Effects
Body Weight
A high-MUFA diet compared with a high-CHO diet resulted in a significant mean decrease in body weight (WMD −1.56 kg [95% CI −2.89, −0.23]), with low heterogeneity (I2 = 0.0%, P = 1.000) (Table 2).
Blood Pressure
In examining 24-h blood pressure monitoring, a high-MUFA diet compared with a high-CHO diet resulted in a significant reduction in systolic blood pressure (WMD −2.31 mmHg [95% CI −4.13, −0.49]) and a nonsignificant reduction in diastolic blood pressure, with significant heterogeneity (I2 = 69.5%, P = 0.011) (Table 2).
Subgroup Analysis and Meta-regression
For comparisons between high-MUFA and high-CHO diets, we conducted stratified analysis for HbA1c, fasting plasma glucose, LDL and HDL cholesterol, triglycerides, and body weight by age (<60, ≥60 years), baseline BMI (<30, ≥30 kg/m2), duration of diabetes (<5, ≥5 years), MUFA replacement (<15, ≥15% of energy), duration of study (≤6, >6 weeks), and trial design (parallel, crossover) to identify possible sources of heterogeneity (Table 4). For HbA1c, no considerable differences were observed within each of the subgroups assessed. For fasting plasma glucose, there was greater reduction among studies in which the mean age of participants was <60 years (WMD −0.63 mmol/L [95% CI −0.85, −0.41]) than studies in which mean age was ≥60 years (−0.32 mmol/L [−0.76, 0.12]). For HDL cholesterol, greater increases were observed in the subgroups in which trial duration was greater than 6 weeks or had a parallel design. There was a greater reduction in triglycerides for participants with a duration of diabetes of ≥5 years (−0.37 mmol/L [−0.57, −0.17]) compared with <5 years (−0.16 mmol/L [−0.44, 0.12]). The reduction in triglycerides also tended to be greater in subgroups that had trial duration greater than 6 weeks or had a parallel design. Among subgroups of patients who had mean age ≥60 years (0.38 mmol/L [−0.08, 0.85]) compared with patients <60 years (−0.05 mmol/L [−0.14, 0.03]), there tended to be greater increase in LDL cholesterol, though this difference was not statistically significant. Similarly, among subgroups of patients who had mean BMI <30 kg/m2 (0.23 mmol/L [−0.02, 0.48]) compared with patients with BMI ≥30 kg/m2 (−0.06 mmol/L [−0.15, 0.03]), there tended to be greater increase in LDL cholesterol, though this difference was also not significant. For body weight, we observed a statistically significant weight reduction in the subgroups with BMI <30 kg/m2 compared with BMI ≥30 kg/m2, MUFA replacement <15% compared with ≥15% of energy, trial time >6 weeks compared with ≤6 weeks, and parallel design compared with crossover design.
Table 4.
Subgroup analysis of metabolic effects on T2D patients consuming a high-MUFA diet compared with a high-CHO diet
| Metabolic parameter | Number of studies | Number of participants | WMD (95% CI)* | WMD (95% CI)† | I2 (%) | Phet |
|---|---|---|---|---|---|---|
| HbA1c (%) |
||||||
| Age (years) |
||||||
| <60 |
9 |
765 |
−0.08 (−0.16, 0.01) |
−0.12 (−0.28, 0.05) |
59.2 |
0.006 |
| ≥60 |
3 |
121 |
−0.08 (−0.38, 0.23) |
−0.08 (−0.38, 0.23) |
0.0 |
0.671 |
| BMI (kg/m2) |
||||||
| <30 |
6 |
382 |
−0.34 (−0.52, −0.16) |
−0.21 (−0.50, 0.07) |
36.1 |
0.153 |
| ≥30 |
7 |
506 |
−0.01 (−0.10, 0.07) |
−0.01 (−0.10, 0.07) |
0.0 |
0.545 |
| Duration of diabetes (years) |
||||||
| <5† |
— |
— |
— |
— |
— |
— |
| ≥5 |
4 |
240 |
−0.18 (−0.39, 0.02) |
−0.18 (−0.39, 0.02) |
0.0 |
0.561 |
| MUFA replacement (%)‡ |
||||||
| <15 |
8 |
580 |
−0.06 (−0.14, 0.02) |
−0.10 (−0.27, 0.07) |
58.2 |
0.010 |
| ≥15 |
4 |
71 |
−0.01 (−0.60, 0.59) |
−0.01 (−0.60, 0.59) |
0.0 |
0.787 |
| Trial time (weeks) |
||||||
| ≤6 |
7 |
135 |
0.03 (−0.29, 0.36) |
0.03 (−0.29, 0.36) |
63.6 |
0.003 |
| >6 |
7 |
790 |
−0.08 (−0.16, 0.00) |
−0.14 (−0.30, 0.02) |
0.0 |
0.955 |
| Study design |
||||||
| Parallel |
7 |
805 |
−0.08 (−0.16, 0.00) |
−0.13 (−0.30, 0.03) |
63.3 |
0.004 |
| Crossover |
7 |
120 |
0.00 (−0.31, 0.31) |
0.00 (−0.31, 0.31) |
0.0 |
0.924 |
| Fasting plasma glucose (mmol/L) |
||||||
| Age (years) |
||||||
| <60 |
15 |
713 |
−0.64 (−0.85, −0.43) |
−0.63 (−0.85, −0.41) |
5.9 |
0.387 |
| ≥60 |
5 |
375 |
−0.32 (−0.76, 0.12) |
−0.32 (−0.76, 0.12) |
0.0 |
0.627 |
| BMI (kg/m2) |
||||||
| <30 |
14 |
733 |
−0.64 (−0.89, −0.40) |
−0.64 (−0.89, −0.40) |
0.0 |
0.760 |
| ≥30 |
7 |
367 |
−0.49 (−0.77, −0.21) |
−0.40 (−0.82, 0.02) |
38.6 |
0.122 |
| Duration of diabetes (years) |
||||||
| <5 |
3 |
257 |
−0.90 (−1.36, −0.45) |
−0.90 (−1.36, −0.45) |
0.0 |
0.620 |
| ≥5 |
8 |
290 |
−0.69 (−1.01, −0.37) |
−0.69 (−1.01, −0.37) |
0.0 |
0.553 |
| MUFA replacement (%) |
||||||
| <15 |
9 |
625 |
−0.51 (−0.77, −0.24) |
−0.51 (−0.77, −0.24) |
1.2 |
0.430 |
| ≥15 |
9 |
188 |
−0.63 (−1.01, −0.25) |
−0.63 (−1.01, −0.25) |
0.0 |
0.931 |
| Trial time (weeks) |
||||||
| ≤6 |
15 |
302 |
−0.54 (−0.87, −0.21) |
−0.54 (−0.87, −0.21) |
0.0 |
0.901 |
| >6 |
7 |
825 |
−0.59 (−0.81, −0.37) |
−0.53 (−0.84, −0.23) |
40.6 |
0.087 |
| Study design |
||||||
| Parallel |
10 |
952 |
−0.58 (−0.79, −0.36) |
−0.54 (−0.81, −0.27) |
23.9 |
0.202 |
| Crossover |
12 |
175 |
−0.56 (−0.91, −0.21) |
−0.56 (−0.91, −0.21) |
0.0 |
0.783 |
| LDL cholesterol (mmol/L) |
||||||
| Age (years) |
||||||
| <60 |
11 |
558 |
−0.05 (−0.14, 0.03) |
−0.05 (−0.14, 0.03) |
0.0 |
0.969 |
| ≥60 |
4 |
174 |
0.45 (0.21, 0.69) |
0.38 (−0.08, 0.85) |
67.4 |
0.015 |
| BMI (kg/m2) |
||||||
| <30 |
10 |
182 |
0.26 (0.09, 0.43) |
0.23 (−0.02, 0.48) |
46.4 |
0.045 |
| ≥30 |
6 |
479 |
−0.06 (−0.15, 0.02) |
−0.06 (−0.15, 0.02) |
0.0 |
0.935 |
| Duration of diabetes (years) |
||||||
| <5† |
— |
— |
— |
— |
— |
— |
| ≥5 |
6 |
263 |
−0.07 (−0.23, 0.09) |
−0.07 (−0.23, 0.09) |
0.0 |
0.747 |
| MUFA replacement (%) |
||||||
| <15 |
7 |
348 |
0.01 (−0.08, 0.11) |
0.11 (−0.10, 0.32) |
70.5 |
0.001 |
| ≥15 |
7 |
161 |
0.05 (−0.19, 0.29) |
0.05 (−0.19, 0.29) |
0.0 |
0.984 |
| Trial time (weeks) |
||||||
| ≤6 |
12 |
243 |
−0.01 (−0.17, 0.15) |
−0.01 (−0.17, 0.15) |
0.0 |
0.993 |
| >6 |
5 |
548 |
0.01 (−0.08, 0.09) |
0.10 (−0.10, 0.30) |
75.8 |
<0.001 |
| Study design |
||||||
| Parallel |
6 |
626 |
0.01 (−0.08, 0.10) |
0.11 (−0.09, 0.30) |
72.7 |
<0.001 |
| Crossover |
11 |
165 |
−0.02 (−0.18, 0.14) |
−0.02 (−0.18, 0.14) |
0.0 |
0.992 |
| HDL cholesterol (mmol/L) |
||||||
| Age (years) |
||||||
| <60 |
14 |
844 |
0.07 (0.04, 0.09) |
0.06 (0.02, 0.10) |
41.3 |
0.043 |
| ≥60 |
4 |
184 |
0.08 (−0.05, 0.22) |
0.08 (−0.05, 0.22) |
71.3 |
0.007 |
| BMI (kg/m2) |
||||||
| <30 |
12 |
534 |
0.07 (0.03, 0.11) |
0.07 (0.02, 0.12) |
24.4 |
0.197 |
| ≥30 |
7 |
506 |
0.07 (0.04, 0.10) |
0.06 (0.00, 0.11) |
66.8 |
0.002 |
| Duration of diabetes (years) |
||||||
| <5 |
3 |
257 |
0.08 (0.02, 0.13) |
0.08 (0.02, 0.13) |
0.0 |
0.812 |
| ≥5 |
6 |
265 |
0.11 (0.07, 0.15) |
0.08 (0.00, 0.15) |
57.0 |
0.030 |
| MUFA replacement (%) |
||||||
| <15 |
9 |
590 |
0.05 (0.02, 0.09) |
0.05 (0.00, 0.10) |
40.4 |
0.079 |
| ≥15 |
8 |
171 |
0.04 (−0.02, 0.10) |
0.04 (−0.02, 0.10) |
0.0 |
0.815 |
| Trial time (weeks) |
||||||
| ≤6 |
13 |
277 |
0.02 (−0.03, 0.07) |
0.04 (−0.15, 0.24) |
0.0 |
0.884 |
| >6 |
7 |
790 |
0.09 (0.06, 0.11) |
0.09 (0.03, 0.14) |
68.5 |
0.001 |
| Study design |
||||||
| Parallel |
9 |
900 |
0.08 (0.06, 0.11) |
0.08 (0.03, 0.13) |
65.9 |
0.001 |
| Crossover |
11 |
167 |
0.03 (−0.02, 0.08) |
0.03 (−0.02, 0.08) |
0.0 |
0.941 |
| Triglycerides (mmol/L) |
||||||
| Age (years) |
||||||
| <60 |
15 |
852 |
−0.28 (−0.36, −0.21) |
−0.29 (−0.43, −0.15) |
61.2 |
0.001 |
| ≥60 |
4 |
184 |
−0.49 (−0.82, −0.16) |
−0.52 (−0.97, −0.07) |
44.0 |
0.129 |
| BMI (kg/m2) |
||||||
| <30 |
13 |
542 |
−0.21 (−0.34, −0.09) |
−0.26 (−0.41, −0.10) |
18.1 |
0.257 |
| ≥30 |
7 |
506 |
−0.33 (−0.42, −0.24) |
−0.33 (−0.55, −0.12) |
74.8 |
<0.001 |
| Duration of diabetes (years) |
||||||
| <5 |
3 |
257 |
−0.10 (−0.28, 0.08) |
−0.16 (−0.44, 0.12) |
37.3 |
0.203 |
| ≥5 |
7 |
273 |
−0.42 (−0.58, −0.26) |
−0.37 (−0.57, −0.17) |
26.5 |
0.217 |
| MUFA replacement (%) |
||||||
| <15 |
9 |
590 |
−0.24 (−0.33, −0.15) |
−0.26 (−0.44, −0.07) |
68.0 |
0.001 |
| ≥15 |
8 |
171 |
−0.31 (−0.52, −0.10) |
−0.31 (−0.52, −0.10) |
0.0 |
0.854 |
| Trial time (weeks) |
||||||
| ≤6 |
14 |
285 |
−0.26 (−0.41, −0.11) |
−0.26 (−0.41, −0.11) |
0.0 |
0.919 |
| >6 |
7 |
790 |
−0.30 (−0.39, −0.22) |
−0.36 (−0.57, −0.15) |
79.9 |
<0.001 |
| Study design |
||||||
| Parallel |
9 |
900 |
−0.31 (−0.39, −0.22) |
−0.37 (−0.56, −0.18) |
75.0 |
<0.001 |
| Crossover |
12 |
175 |
−0.23 (−0.39, −0.06) |
−0.23 (−0.39, −0.06) |
0.0 |
0.918 |
| Body weight (kg) |
||||||
| Age (years) |
||||||
| <60 |
11 |
741 |
−1.40 (−3.07, 0.27) |
−1.40 (−3.07, 0.27) |
0.0 |
1.000 |
| ≥60 |
4 |
312 |
−1.95 (−4.25, 0.35) |
−1.95 (−4.25, 0.35) |
0.0 |
0.987 |
| BMI (kg/m2) |
||||||
| <30 |
10 |
589 |
−1.64 (−3.26, −0.03) |
−1.64 (−3.26, −0.03) |
0.0 |
1.000 |
| ≥30 |
6 |
476 |
−1.39 (−3.75, 0.98) |
−1.39 (−3.75, 0.98) |
0.0 |
0.892 |
| Duration of diabetes (years) |
||||||
| <5 |
3 |
241 |
−1.53 (−4.09, 1.04) |
−1.53 (−4.09, 1.04) |
0.0 |
0.931 |
| ≥5 |
4 |
223 |
−1.69 (−4.38, 1.00) |
−1.69 (−4.38, 1.00) |
0.0 |
0.983 |
| MUFA replacement (%) |
||||||
| <15 |
8 |
724 |
−1.73 (−3.33, −0.12) |
−1.73 (−3.33, −0.12) |
0.0 |
0.989 |
| ≥15 |
5 |
51 |
−0.26 (−4.94, 4.42) |
−0.26 (−4.94, 4.42) |
0.0 |
0.999 |
| Trial time (weeks) |
||||||
| ≤6 |
8 |
111 |
−0.28 (−3.57, 3.01) |
−0.28 (−3.57, 3.01) |
0.0 |
1.000 |
| >6 |
7 |
954 |
−1.81 (−3.27, −0.35) |
−1.81 (−3.27, −0.35) |
0.0 |
0.976 |
| Study design |
||||||
| Parallel |
8 |
970 |
−1.78 (−3.23, −0.34) |
−1.78 (−3.23, −0.34) |
0.0 |
0.986 |
| Crossover | 8 | 95 | −0.29 (−3.75, 3.17) | −0.29 (−3.75, 3.17) | 0.0 | 1.000 |
Values in boldface type indicate statistical significance at P < 0.05.
*Calculated using a fixed-effects model.
†Calculated using a random-effects model.
‡Indicates % energy difference from MUFA in the intervention and control arms.
Meta-regressions were also performed for these outcomes using the baseline characteristics described above and we identified age (β = 0.50, P = 0.002) and BMI (β = −0.32, P = 0.011) as significant predictors for the effect on LDL cholesterol. This suggests that these factors may be potential sources of heterogeneity in these analyses.
Publication Bias and Risk of Bias
Statistically significant publication bias was not found for any of the main outcomes using both the Egger and the Begg-Mazudumar tests (Supplementary Table 2). This was also confirmed based on visual inspection of the corresponding funnel plot (Supplementary Fig. 3). No study exerted overt influence on the pooled effect size for any of the primary outcomes (data not shown). Furthermore, most studies were assessed to be of low risk for bias (Supplementary Table 3).
Conclusions
In our meta-analysis of RCTs, we observed beneficial effects of a high-MUFA diet compared with a high-CHO diet on glycemic control, serum lipids, and systolic blood pressure among individuals with T2D, whereas a beneficial effect on fasting plasma glucose was observed for high-MUFA compared with high-PUFA diets. These improvements are important in the prevention of long-term complications in this population.
In observational studies, substituting dietary MUFA for CHO or saturated fatty acids (SFA) has generally not been associated with a decreased risk of CVD (42–46). However, this may be due to the fact that the main source of MUFA in the Western diet is from animal-based foods, including dairy and meat, which contain comparably higher levels of SFA compared with plant sources of MUFA. In the current study, all of the trials evaluated plant sources of MUFA, such as olive oil, nuts, or avocado, which reduces the confounding by SFA intake observed in cohort studies. In several observational studies and meta-analyses, higher consumption of PUFA in place of SFA or CHO has been associated with lower rates of coronary events, though it is unclear whether substitution for MUFA would yield a similar benefit (43–46).
Better glycemic control and improved insulin sensitivity have often been observed in subjects consuming a high-MUFA diet, particularly when MUFA was used to replace CHO (47–49). The favorable increase in HDL cholesterol and reduction in triglycerides that we observed is also consistent with prior meta-analyses (5,50). These improvements are particularly important for the prevention of CVD among individuals with T2D given that the majority of this population has dyslipidemia. We observed a small reduction in systolic blood pressure, which is also consistent with the results from a prior meta-analysis (7). Our summary measures are consistent with a previous meta-analysis by Schwingshackl et al. (3) that reported significant reductions in HbA1c when comparing high-MUFA to high-CHO diets and nonsignificant reductions in plasma insulin, plasma glucose, and HOMA-insulin resistance. The nonsignificant results of this previous analysis could be due to the fact that fewer studies were included for these measures. Garg et al. (5) also reported significant reductions in fasting glucose and a nonsignificant reduction in plasma insulin, also possibly due to the inclusion of fewer trials. Overall, the results for glycemic control favor high-MUFA compared with high-CHO diets, especially in the reduction of fasting plasma glucose. Moreover, we observed a modest but statistically significant difference in body weight on high-MUFA compared with high-CHO diets, both overall and in several subgroups. This finding suggests that the effects of the high-MUFA diets on the metabolic risk factors could be partially mediated by changes in body weight, which has been shown in prior studies evaluating blood lipids, blood pressure, and glycemic control (51,52).
Out of the outcomes we evaluated comparing high-MUFA to high-PUFA diets, we only observed a reduction in fasting plasma glucose. The overall lack of difference observed between these two diets on the metabolic risk factors we evaluated could be due to small sample sizes or similar metabolic effects between these two diets. In addition, the length of follow-up in these trials may have been too short to observe meaningful changes in the biomarkers. The intervention foods in the high-PUFA regimens varied from study to study (sunflower oil, nuts, corn oil) each containing other components (macro- and micronutrients, antioxidants) that may have influenced the results of a given trial due to their association with glycemic control or serum lipid levels (53–56).
Potential physiological mechanisms for the metabolic benefits observed when replacing CHO with MUFA are diminished glycemic load, leading to reduced demand for insulin, greater insulin sensitivity (57), and increased hepatic LDL receptors, resulting in accelerated LDL cholesterol turnover while having no appreciable effect on total cholesterol synthesis (e.g., does not lower HDL cholesterol) (58). There is also growing evidence that MUFA-rich foods, including olive oil and avocados, contain numerous other beneficial compounds such as phenolic compounds, plant phytochemicals, and fat-soluble vitamins (59–61). Oleic acid, a MUFA, which is the primary component in olive oil, has been directly implicated in blood pressure reduction by increasing cell membrane fluidity and exerting hypotensive effects via the α2-adrenergic receptor system (62).
Our results are consistent with recent findings from the PREDIMED trial, which observed a decrease in CVD incidence among individuals with T2D who followed a Mediterranean diet compared with a low-fat diet. This suggests that changes in metabolic indices may be predictive of clinical end points (4). On the basis of our findings, body weight differed between the high-MUFA diet compared with the high-CHO diet. To account for the weight differences among these two diets, we performed a sensitivity analyses (Supplementary Table 5) in which we excluded trials that had a more than 1.5-kg difference in weight at the end of the trial, which included seven comparisons. Most of the outcomes were attenuated, although fasting plasma glucose (WMD −0.44 mmol/L [95% CI −0.74, −0.14]) and triglycerides (−0.19 mmol/L [−0.29, −0.10]) remained statistically significant. This is indicative of dietary composition having a favorable metabolic effect independent of weight reduction and is consistent with the results from the 2-year Dietary Intervention Randomized Controlled Trial (DIRECT) that observed that a Mediterranean-type diet resulted in greater weight loss and improved metabolic profile compared with a low-fat diet among obese individuals (63). However, whether such an effect would be observed among obese individuals with T2D is not clear. Additional longer-term trials are needed to assess whether greater weight loss can be achieved with a high-MUFA diet among individuals with diabetes.
Our stratified analysis found modestly greater changes in several metabolic factors including HbA1c, HDL cholesterol, and triglycerides in trials that were of longer duration (>6 vs. ≤6 weeks), suggesting that longer-term adherence to a high-MUFA diet may produce a more favorable metabolic profile. When we performed a sensitivity analysis and restricted the analysis to studies that were at least 3 months in duration, we observed a consistent or stronger effect on many of the metabolic parameters as in our overall analysis (Supplementary Table 6). Furthermore, this result is consistent with the nonsignificant reduction in HbA1c (%), which is likely due to the relatively short duration of most studies in the meta-analysis; HbA1c is more indicative of long-term glycemic control,over the span of 3–4 months. We tended to observe greater effects among studies using parallel rather than crossover designs, particularly for HDL cholesterol and triglycerides. This may be partially attributed to larger sample sizes in the parallel studies in our analysis. It is also possible that the duration of the wash-out period in the crossover trials was not sufficient to diminish a potential carryover effect. These subgroup findings may partially explain some of the heterogeneity observed in our effect estimates.
Our study has several strengths. We included both long-term and short-term studies in our overall and stratified analysis. In general, for studies evaluating MUFA compared with CHO diets, we selected studies that kept the percent of calories from protein and SFA consistent across the intervention and control arms. Similarly, for MUFA compared with PUFA diets, we selected studies that had minimal differences in the percent of calories from protein, CHO, and SFA. Furthermore, we sought to identify potential sources of heterogeneity in our study through both subgroup analysis and meta-regression, particularly for HbA1c, HDL cholesterol, and triglycerides. In addition, no outcome was observed to have potential publication bias based on our assessment (Supplementary Table 2), as we attempted to minimize bias by contacting authors to obtain unpublished results when necessary. There are several limitations to our study. Our study only included studies that examined individuals with T2D or noninsulin-dependent diabetes; hence, it is unclear whether these metabolic benefits can be extended to individuals with impaired glucose tolerance or type 1 diabetes, although some studies suggest a similar benefit (3,64). Furthermore, we examined only metabolic risk factors that were consistently measured and reported in each study, but the benefits of a high-MUFA diet may also be mediated through effects on inflammation (65), endothelial function (66), and body fat distribution (67), which all warrant further research. Most of the trials in our analysis were conducted among Western populations, which may limit the generalizability of our findings to other populations. In addition, comparisons of the foods consumed for the different diets in each study were generally not available. Hence, we cannot completely rule out the possibility that the metabolic differences we observed were attributable to some unmeasured dietary component. Finally, our analysis included a relatively small number of trials comparing high-MUFA to high-PUFA diets, which limits our conclusion regarding the metabolic effects of replacing MUFA with PUFA. Further studies are needed to examine whether replacement of CHO with PUFA exhibits similar metabolic benefits as MUFA among individuals with T2D.
In conclusion, our meta-analysis provides consistent evidence that replacing CHO with MUFA in the diet has beneficial effects on metabolic risk factors among individuals with T2D. Our findings have broad implications for dietary recommendations for this population.
Supplementary Material
Article Information
Funding. This research was supported by an American Diabetes Association Research Award, a National Institute of Diabetes and Digestive and Kidney Diseases grant DK58845, and a National Heart, Lung, and Blood Institute grant HL60712.
The funders had no role in the decision to conduct the meta-analyses, data analysis, or reporting of the results.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. F.Q. conducted the literature search, data extraction, data analysis, and manuscript writing. A.A.K. double-checked the data extraction and contributed to the data analysis and manuscript writing. V.M. contributed to the data analysis and reviewed and edited the manuscript. F.B.H. reviewed and edited the manuscript.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc16-0513/-/DC1.
References
- 1.Evert AB, Boucher JL, Cypress M, et al. . Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014;37(Suppl. 1):S120–S143 [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association Task Force for Writing Nutrition Principles and Recommendations for the Management of Diabetes and Related Complications American Diabetes Association position statement: evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. J Am Diet Assoc 2002;102:109–118 [DOI] [PubMed] [Google Scholar]
- 3.Schwingshackl L, Strasser B, Hoffmann G. Effects of monounsaturated fatty acids on glycaemic control in patients with abnormal glucose metabolism: a systematic review and meta-analysis. Ann Nutr Metab 2011;58:290–296 [DOI] [PubMed] [Google Scholar]
- 4.Estruch R, Ros E, Salas-Salvadó J, et al.; PREDIMED Study Investigators . Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368:1279–129023432189 [Google Scholar]
- 5.Garg A. High-monounsaturated-fat diets for patients with diabetes mellitus: a meta-analysis. Am J Clin Nutr 1998;67(Suppl.):577S–582S [DOI] [PubMed] [Google Scholar]
- 6.Ros E. Dietary cis-monounsaturated fatty acids and metabolic control in type 2 diabetes. Am J Clin Nutr 2003;78(Suppl.):617S–625S [DOI] [PubMed] [Google Scholar]
- 7.Shah M, Adams-Huet B, Garg A. Effect of high-carbohydrate or high-cis-monounsaturated fat diets on blood pressure: a meta-analysis of intervention trials. Am J Clin Nutr 2007;85:1251–1256 [DOI] [PubMed] [Google Scholar]
- 8.Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins JP, Altman DG, Gøtzsche PC, et al.; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–1101 [PubMed] [Google Scholar]
- 13.Lasa A, Miranda J, Bulló M, et al. . Comparative effect of two Mediterranean diets versus a low-fat diet on glycaemic control in individuals with type 2 diabetes. Eur J Clin Nutr 2014;68:767–772 [DOI] [PubMed] [Google Scholar]
- 14.Itsiopoulos C, Brazionis L, Kaimakamis M, et al. . Can the Mediterranean diet lower HbA1c in type 2 diabetes? Results from a randomized cross-over study. Nutr Metab Cardiovasc Dis 2011;21:740–747 [DOI] [PubMed] [Google Scholar]
- 15.Elhayany A, Lustman A, Abel R, Attal-Singer J, Vinker S. A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: a 1-year prospective randomized intervention study. Diabetes Obes Metab 2010;12:204–209 [DOI] [PubMed] [Google Scholar]
- 16.Brehm BJ, Lattin BL, Summer SS, et al. . One-year comparison of a high-monounsaturated fat diet with a high-carbohydrate diet in type 2 diabetes. Diabetes Care 2009;32:215–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Esposito K, Maiorino MI, Ciotola M, et al. . Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med 2009;151:306–314 [DOI] [PubMed] [Google Scholar]
- 18.Wolever TM, Mehling C, Chiasson JL, et al. . Low glycaemic index diet and disposition index in type 2 diabetes (the Canadian Trial of Carbohydrates in Diabetes): a randomised controlled trial. Diabetologia 2008;51:1607–1615 [DOI] [PubMed] [Google Scholar]
- 19.Wolever TM, Gibbs AL, Mehling C, et al. . The Canadian Trial of Carbohydrates in Diabetes (CCD), a 1-y controlled trial of low-glycemic-index dietary carbohydrate in type 2 diabetes: no effect on glycated hemoglobin but reduction in C-reactive protein. Am J Clin Nutr 2008;87:114–125 [DOI] [PubMed] [Google Scholar]
- 20.Brunerova L, Smejkalova V, Potockova J, Andel M. A comparison of the influence of a high-fat diet enriched in monounsaturated fatty acids and conventional diet on weight loss and metabolic parameters in obese non-diabetic and type 2 diabetic patients. Diabet Med 2007;24:533–540 [DOI] [PubMed]
- 21.León-Sanz M, García-Luna PP, Sanz-París A, et al.; Abbott SPAI-97-004 Study Cooperative Group . Glycemic and lipid control in hospitalized type 2 diabetic patients: evaluation of 2 enteral nutrition formulas (low carbohydrate-high monounsaturated fat vs high carbohydrate). JPEN J Parenter Enteral Nutr 2005;29:21–29 [DOI] [PubMed] [Google Scholar]
- 22.Shah M, Adams-Huet B, Bantle JP, et al. . Effect of a high-carbohydrate versus a high--cis-monounsaturated fat diet on blood pressure in patients with type 2 diabetes. Diabetes Care 2005;28:2607–2612 [DOI] [PubMed] [Google Scholar]
- 23.Gerhard GT, Ahmann A, Meeuws K, McMurry MP, Duell PB, Connor WE. Effects of a low-fat diet compared with those of a high-monounsaturated fat diet on body weight, plasma lipids and lipoproteins, and glycemic control in type 2 diabetes. Am J Clin Nutr 2004;80:668–673 [DOI] [PubMed] [Google Scholar]
- 24.Rodriguez-Villar C, Perez-Heras A, Mercade I, Casals E, Ros E. Comparison of a high-carbohydrate and a high-monounsaturated fat, olive oil-rich diet on the susceptibility of LDL to oxidative modification in subjects with type 2 diabetes mellitus. Diabet Med 2004;21:142–149 [DOI] [PubMed]
- 25.Lovejoy JC, Most MM, Lefevre M, Greenway FL, Rood JC. Effect of diets enriched in almonds on insulin action and serum lipids in adults with normal glucose tolerance or type 2 diabetes. Am J Clin Nutr 2002;76:1000–1006 [DOI] [PubMed] [Google Scholar]
- 26.Rodríguez-Villar C, Manzanares JM, Casals E, et al. . High-monounsaturated fat, olive oil-rich diet has effects similar to a high-carbohydrate diet on fasting and postprandial state and metabolic profiles of patients with type 2 diabetes. Metabolism 2000;49:1511–1517 [DOI] [PubMed] [Google Scholar]
- 27.Tsihlias EB, Gibbs AL, McBurney MI, Wolever TM. Comparison of high- and low-glycemic-index breakfast cereals with monounsaturated fat in the long-term dietary management of type 2 diabetes. Am J Clin Nutr 2000;72:439–449 [DOI] [PubMed] [Google Scholar]
- 28.Gumbiner B, Low CC, Reaven PD. Effects of a monounsaturated fatty acid-enriched hypocaloric diet on cardiovascular risk factors in obese patients with type 2 diabetes. Diabetes Care 1998;21:9–15 [DOI] [PubMed] [Google Scholar]
- 29.McCargar LJ, Innis SM, Bowron E, et al. . Effect of enteral nutritional products differing in carbohydrate and fat on indices of carbohydrate and lipid metabolism in patients with NIDDM. Mol Cell Biochem 1998;188:81–89 [PubMed] [Google Scholar]
- 30.Campbell LV, Marmot PE, Dyer JA, Borkman M, Storlien LH. The high-monounsaturated fat diet as a practical alternative for NIDDM. Diabetes Care 1994;17:177–182 [DOI] [PubMed] [Google Scholar]
- 31.Garg A, Bantle JP, Henry RR, et al. . Effects of varying carbohydrate content of diet in patients with non-insulin-dependent diabetes mellitus. JAMA 1994;271:1421–1428 [DOI] [PubMed] [Google Scholar]
- 32.Lerman-Garber I, Ichazo-Cerro S, Zamora-González J, Cardoso-Saldaña G, Posadas-Romero C. Effect of a high-monounsaturated fat diet enriched with avocado in NIDDM patients. Diabetes Care 1994;17:311–315 [DOI] [PubMed] [Google Scholar]
- 33.Rasmussen OW, Thomsen C, Hansen KW, Vesterlund M, Winther E, Hermansen K. Effects on blood pressure, glucose, and lipid levels of a high-monounsaturated fat diet compared with a high-carbohydrate diet in NIDDM subjects. Diabetes Care 1993;16:1565–1571 [DOI] [PubMed] [Google Scholar]
- 34.Garg A, Grundy SM, Unger RH. Comparison of effects of high and low carbohydrate diets on plasma lipoproteins and insulin sensitivity in patients with mild NIDDM. Diabetes 1992;41:1278–1285 [PubMed] [Google Scholar]
- 35.Parillo M, Rivellese AA, Ciardullo AV, et al. . A high-monounsaturated-fat/low-carbohydrate diet improves peripheral insulin sensitivity in non-insulin-dependent diabetic patients. Metabolism 1992;41:1373–1378 [DOI] [PubMed] [Google Scholar]
- 36.Rivellese AA, Giacco R, Genovese S, et al. . Effects of changing amount of carbohydrate in diet on plasma lipoproteins and apolipoproteins in type II diabetic patients. Diabetes Care 1990;13:446–448 [DOI] [PubMed] [Google Scholar]
- 37.Garg A, Bonanome A, Grundy SM, Zhang ZJ, Unger RH. Comparison of a high-carbohydrate diet with a high-monounsaturated-fat diet in patients with non-insulin-dependent diabetes mellitus. N Engl J Med 1988;319:829–834 [DOI] [PubMed] [Google Scholar]
- 38.Madigan C, Ryan M, Owens D, Collins P, Tomkin GH. Comparison of diets high in monounsaturated versus polyunsaturated fatty acid on postprandial lipoproteins in diabetes. Ir J Med Sci 2005;174:8–20 [DOI] [PubMed] [Google Scholar]
- 39.Brynes AE, Edwards CM, Jadhav A, Ghatei MA, Bloom SR, Frost GS. Diet-induced change in fatty acid composition of plasma triacylglycerols is not associated with change in glucagon-like peptide 1 or insulin sensitivity in people with type 2 diabetes. Am J Clin Nutr 2000;72:1111–1118 [DOI] [PubMed] [Google Scholar]
- 40.Thomsen C, Rasmussen OW, Hansen KW, Vesterlund M, Hermansen K. Comparison of the effects on the diurnal blood pressure, glucose, and lipid levels of a diet rich in monounsaturated fatty acids with a diet rich in polyunsaturated fatty acids in type 2 diabetic subjects. Diabet Med 1995;12:600–606 [DOI] [PubMed]
- 41.Parfitt VJ, Desomeaux K, Bolton CH, Hartog M. Effects of high monounsaturated and polyunsaturated fat diets on plasma lipoproteins and lipid peroxidation in type 2 diabetes mellitus. Diabet Med 1994;11:85–91 [DOI] [PubMed]
- 42.Jakobsen MU, O’Reilly EJ, Heitmann BL, et al. . Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr 2009;89:1425–1432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chowdhury R, Warnakula S, Kunutsor S, et al. . Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med 2014;160:398–406 [DOI] [PubMed] [Google Scholar]
- 44.dos Santos AL, Weiss T, Duarte CK, Gross JL, de Azevedo MJ, Zelmanovitz T. Dietary fat composition and cardiac events in patients with type 2 diabetes. Atherosclerosis 2014;236:31–38 [DOI] [PubMed] [Google Scholar]
- 45.Tanasescu M, Cho E, Manson JE, Hu FB. Dietary fat and cholesterol and the risk of cardiovascular disease among women with type 2 diabetes. Am J Clin Nutr 2004;79:999–1005 [DOI] [PubMed] [Google Scholar]
- 46.Soinio M, Laakso M, Lehto S, Hakala P, Rönnemaa T. Dietary fat predicts coronary heart disease events in subjects with type 2 diabetes. Diabetes Care 2003;26:619–624 [DOI] [PubMed] [Google Scholar]
- 47.Vessby B, Uusitupa M, Hermansen K, et al.; KANWU Study . Substituting dietary saturated for monounsaturated fat impairs insulin sensitivity in healthy men and women: The KANWU Study. Diabetologia 2001;44:312–319 [DOI] [PubMed] [Google Scholar]
- 48.Due A, Larsen TM, Hermansen K, et al. . Comparison of the effects on insulin resistance and glucose tolerance of 6-mo high-monounsaturated-fat, low-fat, and control diets. Am J Clin Nutr 2008;87:855–862 [DOI] [PubMed] [Google Scholar]
- 49.Gadgil MD, Appel LJ, Yeung E, Anderson CA, Sacks FM, Miller ER 3rd. The effects of carbohydrate, unsaturated fat, and protein intake on measures of insulin sensitivity: results from the OmniHeart trial. Diabetes Care 2013;36:1132–1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 2003;77:1146–1155 [DOI] [PubMed] [Google Scholar]
- 51.Wing RR, Lang W, Wadden TA, et al.; Look AHEAD Research Group . Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011;34:1481–1486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pi-Sunyer X, Blackburn G, Brancati FL, et al.; Look AHEAD Research Group . Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care 2007;30:1374–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pittas AG, Dawson-Hughes B, Li T, et al. . Vitamin D and calcium intake in relation to type 2 diabetes in women. Diabetes Care 2006;29:650–656 [DOI] [PubMed] [Google Scholar]
- 54.Wedick NM, Pan A, Cassidy A, et al. . Dietary flavonoid intakes and risk of type 2 diabetes in US men and women. Am J Clin Nutr 2012;95:925–933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jiang R, Manson JE, Stampfer MJ, Liu S, Willett WC, Hu FB. Nut and peanut butter consumption and risk of type 2 diabetes in women. JAMA 2002;288:2554–2560 [DOI] [PubMed] [Google Scholar]
- 56.Pan A, Sun Q, Manson JE, Willett WC, Hu FB. Walnut consumption is associated with lower risk of type 2 diabetes in women. J Nutr 2013;143:512–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tierney AC, Roche HM. The potential role of olive oil-derived MUFA in insulin sensitivity. Mol Nutr Food Res 2007;51:1235–1248 [DOI] [PubMed] [Google Scholar]
- 58.Fernandez ML, West KL. Mechanisms by which dietary fatty acids modulate plasma lipids. J Nutr 2005;135:2075–2078 [DOI] [PubMed] [Google Scholar]
- 59.Dreher ML, Davenport AJ. Hass avocado composition and potential health effects. Crit Rev Food Sci Nutr 2013;53:738–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bulotta S, Celano M, Lepore SM, Montalcini T, Pujia A, Russo D. Beneficial effects of the olive oil phenolic components oleuropein and hydroxytyrosol: focus on protection against cardiovascular and metabolic diseases. J Transl Med 2014;12:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alonso A, Ruiz-Gutierrez V, Martínez-González MA. Monounsaturated fatty acids, olive oil and blood pressure: epidemiological, clinical and experimental evidence. Public Health Nutr 2006;9:251–257 [DOI] [PubMed] [Google Scholar]
- 62.Terés S, Barceló-Coblijn G, Benet M, et al. . Oleic acid content is responsible for the reduction in blood pressure induced by olive oil. Proc Natl Acad Sci U S A 2008;105:13811–13816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shai I, Schwarzfuchs D, Henkin Y, et al.; Dietary Intervention Randomized Controlled Trial (DIRECT) Group . Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med 2008;359:229–241 [DOI] [PubMed] [Google Scholar]
- 64.Strychar I, Cohn JS, Renier G, et al. . Effects of a diet higher in carbohydrate/lower in fat versus lower in carbohydrate/higher in monounsaturated fat on postmeal triglyceride concentrations and other cardiovascular risk factors in type 1 diabetes. Diabetes Care 2009;32:1597–1599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Golan R, Tirosh A, Schwarzfuchs D, et al.; DIRECT Group . Dietary intervention induces flow of changes within biomarkers of lipids, inflammation, liver enzymes, and glycemic control. Nutrition 2012;28:131–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tentolouris N, Arapostathi C, Perrea D, Kyriaki D, Revenas C, Katsilambros N. Differential effects of two isoenergetic meals rich in saturated or monounsaturated fat on endothelial function in subjects with type 2 diabetes. Diabetes Care 2008;31:2276–2278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Paniagua JA, Gallego de la Sacristana A, Romero I, et al. . Monounsaturated fat-rich diet prevents central body fat distribution and decreases postprandial adiponectin expression induced by a carbohydrate-rich diet in insulin-resistant subjects. Diabetes Care 2007;30:1717–1723 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.