Supplemental Digital Content is available in the text.
Abstract
Background:
Road traffic is a major source of air pollution and noise. Both exposures have been associated with hypertension in adults, but pregnant women have been less studied.
Methods:
We examined single and joint effects of ambient air pollution and road traffic noise on pre-eclampsia and pregnancy-induced hypertensive disorders among 72,745 singleton pregnancies (1997–2002) from the Danish National Birth Cohort with complete covariate data and residential address history from conception until live born birth. Nitrogen dioxide (NO2) and noise from road traffic (Lden) were modeled at all addresses. Outcome and covariate data were derived from registries, hospital records, and questionnaires.
Results:
A 10-µg/m3 increase in NO2 exposure during first trimester was associated with increased risk of pre-eclampsia (n = 1,880, adjusted odds ratio = 1.07 [95% confidence interval = 1.01, 1.14]) and pregnancy-induced hypertensive disorders (n = 2,430, adjusted odds ratio = 1.07 [1.01, 1.13]). A 10 dB higher road traffic noise was also associated with increased risk of pre-eclampsia (1.10 [1.02, 1.18]) and pregnancy-induced hypertensive disorders (1.08 [1.02, 1.15]). For both exposures, the associations were strongest for mild pre-eclampsia (n = 1,393) and early-onset pre-eclampsia (n = 671), whereas higher risk for severe pre-eclampsia (n = 487) was not evident. In mutually adjusted models, estimates for both exposures decreased and only the association between NO2 and mild pre-eclampsia remained.
Conclusions:
Road traffic may increase the risk of pre-eclampsia and hypertensive disorders in pregnancy through exposure to both ambient air pollution and noise, although associations with the two exposures were generally not found to be independent of one another. See video abstract, http://links.lww.com/EDE/B112.
Gestational hypertension and pre-eclampsia are common complications of pregnancy affecting 3% to 9% and 1% to 4% of pregnancies, respectively.1 Hypertensive disorders of pregnancy pose a risk of maternal and neonatal morbidity and mortality.2 Gestational hypertension is diagnosed as systolic and/or a diastolic blood pressure above 140 and/or 90 mmHg, respectively, after 20 weeks of pregnancy in previously normotensive women.1 Pre-eclampsia is a heterogeneous group of multisystem disorders, most commonly defined as hypertension and proteinuria in the second half of pregnancy. However, definitions of pre-eclampsia, and the differentiation between mild and severe conditions, are being debated.2 Early-onset (diagnosed before week 34 of pregnancy) and late-onset (diagnosed after week 34 of pregnancy) pre-eclampsia have been reported to have different prevalence and prognosis and possibly different pathogenesis and risk factors.3
There is increasing evidence that exposure to ambient air pollution contributes to the risks of hypertension and other cardiovascular events in adults and elderly.4 Recently, associations between ambient air pollution exposure and the risk of hypertensive disorders during pregnancy have also been reported, but some of the studies rely on crude assessment of exposure and/or limited information on potential confounders.5
The etiology of pre-eclampsia is not well understood. Abnormal placentation, damage to blood vessels, inflammation, oxidative stress, and immunological changes can result in increases in blood pressure and development of pre-eclampsia and related hypertensive outcomes,2,3 all of which have been proposed as mechanisms for the health effects of air pollution.5
Road traffic is the main source of both air and noise pollution and mutual confounding is of concern.6 Exposure to road traffic noise may be relevant to a broad range of hypertensive disorders in pregnancy, yet no studies of road traffic noise and pre-eclampsia and related outcomes have taken into account exposure to traffic-related air pollution.
Exposure to traffic noise has been associated with adverse birth outcomes,7 such as reduced birth weight,8 gestational hypertension,9 hypertension,10 and cardiovascular disease in adults.11,12 Exposure to traffic noise may induce a stress response and disturb sleep,13 which has been associated with increased blood pressure and heart rate, higher levels of stress hormone,14 immunological changes, and endothelial dysfunction.15Maternal stress and/or disturbances of sleep during pregnancy is associated with increased risk of hypertensive disorders during pregnancy.16,17
The objective of our study was to estimate single and joint associations between exposure to ambient air pollution and road traffic noise and pregnancy-induced hypertensive disorders in a large prospective cohort of pregnant women.
METHODS
Study Population
This study includes women who participated in the Danish National Birth Cohort.18
In brief, all general practitioners in Denmark were invited nationwide to recruit pregnant women for the cohort. In total, 50% of the general practitioners participated, and 60% of the women invited agreed to participate. Enrollment occurred in gestational weeks 6 to 10 from 1996 to 2002 and computer-assisted telephone interview with follow-up interviews starting at about the 12th week of gestation. Women were ineligible if they did not speak sufficient Danish or intended not to carry their pregnancy to term. Written informed consent was obtained from all participants at enrollment. The Danish Data Protection Agency reviewed and approved the present study before initiation (J.nr. 2014-41-3286).
A total number of 101,002 pregnancies enrolled in DNBC (Figure). We excluded women from the original cohort due to multiple pregnancies, abortions, molar or extrauterine pregnancies, unknown, emigration or death, stillborn birth, and withdrawals of participation in the study. Women who reported pre-existing hypertension from the pregnancy interview or those who had a diagnosis of pre-existing chronic hypertension and/or diabetes before pregnancy were excluded. Information on diagnosis of the relevant disease codes used for exclusion of women were retrieved from the Danish National Patient Register (NPR),19 which was based on the International Classification of Diseases, 10th Revision (ICD-10 codes O10 for hypertension before pregnancy, I10–I15 for hypertensive diseases, and O24.1–O24.3 for pre-existing diabetes) and self-reported information on pre-existing hypertension from the pregnancy interviews. Furthermore, we excluded women with missing information on exposure, outcomes, and covariates. Finally, we excluded data from later pregnancies for women who had participated in the cohort with more than one pregnancy. This rendered a total of 72,745 women in the present study.
FIGURE.
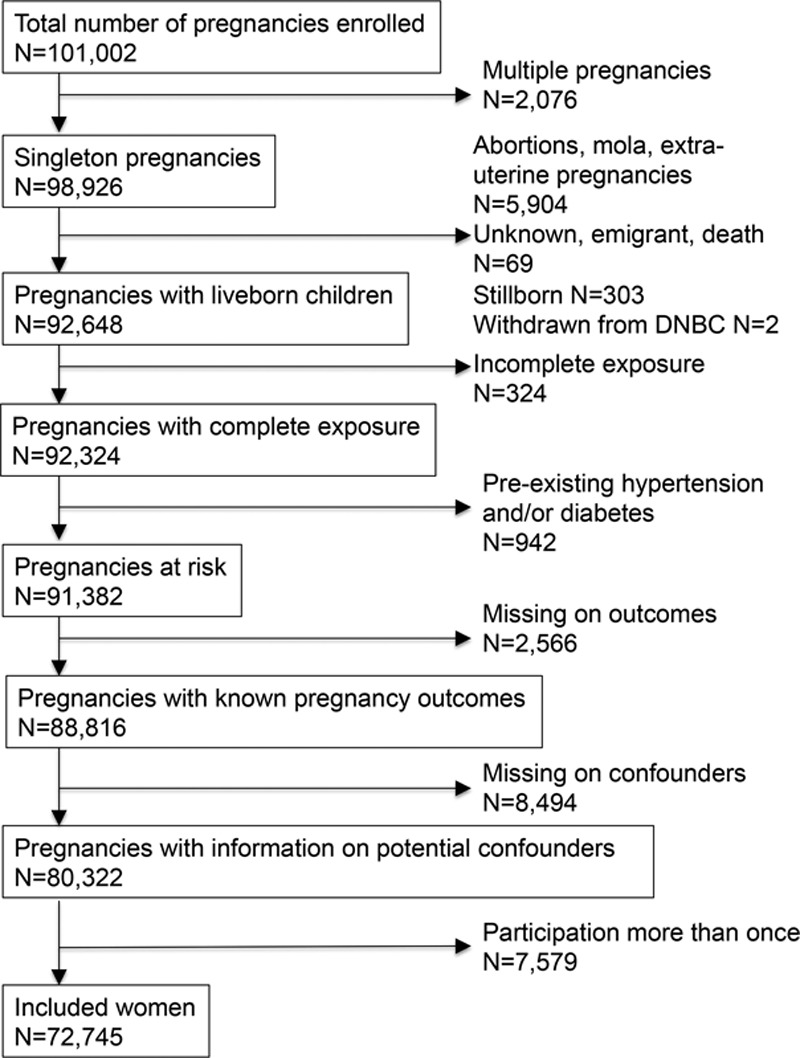
Study population.
Pregnancy Outcomes
We obtained diagnoses and dates of diagnosis from the NPR.19 Dates of last menstrual period (LMP), status of birth, dates of delivery, and/or dates of termination of pregnancy were gathered from the Danish Medical Birth Registry,20and used to identify the participating women who had been diagnosed for pregnancy-induced hypertensive disorders during the index pregnancies and/or in any previous pregnancies. The duration of gestation was based on LMP and, when LMP was uncertain, ultrasound was used.
We defined seven different hypertensive outcomes because there is controversy as to whether pre-eclampsia and gestational hypertension are a spectrum of the same disease or different diseases.2 Severe pre-eclampsia refers to severe pre-eclampsia, hemolysis-elevated liver enzymes and low platelet count (HELLP), and eclampsia, corresponding to the following ICD-10 codes: O141, O142, O150, O151, O152, and O159.21,22 Pre-eclampsia of all subtypes furthermore included mild to moderate pre-eclampsia O140 and unspecified pre-eclampsia O149,21 which we also assessed separately. Finally, we classified pre-eclampsia as early onset when it was diagnosed before gestational week 34 and as late onset if diagnosed in or after week 34.3 Gestational hypertension refers to O139,21 and hypertensive disorders in pregnancy included O139, O140, O41, O142, O150, O151, and O152. Klemmensen et al.21 have reviewed all the information available from hospital charts and interviews on pre-eclampsia and gestational hypertension in a large subset of the DNBC participants, and concluded that the registry had acceptable validity, whereas the usefulness of self-reported information may be limited. Therefore, the current study relies on the validated registry-based outcomes.
Exposure Assessment
We collected residential address history from conception until delivery, including dates of moving, from the Civil Registration System.23 All home addresses were geocoded.
Ambient air pollution with nitrogen dioxide (NO2) concentration (µg/m3) was used as a marker for the mixture of air pollution from traffic and calculated using the advanced AirGIS dispersion model.24–27 AirGIS provides estimates of traffic-related air pollution with high temporal and address-level spatial resolution. Air pollution at 2 m height at the façade of each address’ building was calculated as the sum of (1) local air pollution from street traffic, calculated from traffic data(intensity and type) for individual roads, emission data from the Danish car fleet, street and building geometry, building height, and meteorological data; (2) urban background, calculated from data on urban vehicle emission density, city dimensions, and building heights; and (3) regional background, estimated from trends obtained from rural monitoring stations and vehicle emission data. This method has been applied and validated in several studies.24–27 The correlations between the modeled and measured NO2concentrations at 204 locations in Copenhagen (1994–1995),26 and in a busy street canyon in Copenhagen (1995–2006)25 were high (r = 0.90 and r = 0.67, respectively).
Road traffic noise was calculated at the most exposed facade of each home address of the participants using SoundPLAN.12,27–29 The following input variables were used for calculation of both exposures: geographical coordinates, road links with information on annual average daily traffic, vehicle distribution, travel speed, and road type; and building polygons and building height for all Danish buildings. Traffic volume for all Danish roads with more than 1,000 vehicles per day were obtained from the municipalities and a national database.24 Modeled traffic noise levels have shown good correlation with the percentage of people feeling annoyed by noise.30 Road traffic noise was calculated as the equivalent continuous A-weighted sound pressure level (LAeq) for the day (Ld; 07:00–19:00 hours), evening (Le; 19:00–22:00 hours), and night (Ln; 22:00–07:00 hours) and expressed as Lden (as an indicator of the overall noise level during the day, evening and night) in decibels (dB) by applying a 5-dB penalty for the evening and a 10-dB penalty for the night. dB is a natural logarithmic scale and a 10-dB increase in noise level corresponds to a 10-fold increase in acoustical energy, which is perceived as a doubling in loudness.
Exposure to railway noise was calculated for all addresses using SoundPLAN, with implementation of NORD2000,12,29 and expressed as Lden at the most exposed façade. Input variables were geographical coordinate, railway links with information on annual average daily train lengths, train types, travel speed, building heights (polygons), and noise barriers along the railway. The noise impact from all Danish airports and airfields was determined from information obtained from local authorities and transformed into digital maps and linked to each address.
Exposure to traffic-related air pollution was estimated as daily means; road traffic noise was estimated as annual means and both exposures were fitted as time-weighted means for the preceding full pregnancy period (taking all present and historical addresses during that period into account) or as trimester-specific time-weighted average exposures. We also evaluated the effects of exposure to railway noise for each trimester and for the full pregnancy period (yearly mean at the main address for each period).
Ambient temperature was obtained from the European Climate Assessment Dataset,31 and used to estimate the time-weighted temperature average levels during each trimester and the full pregnancy period measured at the station located nearest to the home address(es).
Statistical Analysis
We evaluated the assumption of linearity (on a log scale) of air pollution and noise from traffic in relation to the pregnancy outcomes by fitting models with the exposure variables on a continuous scale simultaneously with a quadratic term of the exposure variables. All the relationships were found to be linear and exposure variables were fitted on continuous scales. In addition to modeling exposure as continuous linear variables, we estimated associations with exposure quartiles relative to lowest quartile category (results not shown).
We estimated odds ratios (ORs) and their 95% confidence intervals (CIs) for the pregnancy outcomes using logistic regression models; estimates are per 10 μg/m3 higher NO2 and per 10 dB higher road traffic noise. Analyses were done without adjustment and repeated with different levels of covariate adjustment. We selected adjustment variables a priori and fitted models with variables on a continuous scale as the fit was better than when categorical variables of BMI, height, and age was used. Basic adjusted models included information on parity (0, 1+), maternal height (cm), maternal prepregnancy BMI (kg/m2), and height (cm) obtained from the first interview; maternal age (years) and season of conception (four seasons); maternal education in the year before LMP (low, middle, high), household disposable income (after taxation and interest per person, adjusted for number of household persons and divided into tertiles based on the Danish background population), and the year before LMP gathered from Statistic Denmark. Further adjustment included maternal smoking (none, occasional, <15 cigarettes/day, ≥15 cigarettes/day) and physical activity (quartiles of min/day) from the first interview in early pregnancy,22 and railway (dB) and airport noise (yes/no) at the end of first trimester.
We examined the independence of the associations of air pollution and road traffic noise by first fitting separate models for the two exposures and then including both exposures in the same model. Potential interaction between air pollution and noise was evaluated by including an interaction term between air pollution and noise.
We also examined potential effect modification by parity, prepregnancy BMI, education, smoking, physical activity, change of address, and area of living. Furthermore, for road traffic noise, we tested effect modification by exposure to railway noise. Potential interaction and effect modification was tested by the Wald test. An alpha level of 5% (two sided) was used to define statistical significance. Sensitivity analyses included further adjustment for gestational diabetes mellitus and ambient temperature; restriction to women with no previous pregnancies with pre-eclampsia; and finally, we repeated analyses for a larger study population, which included women with pre-existing hypertension. Finally, we also repeated analyses using generalized estimating equation (GEE) for the larger sample that included the later pregnancies (n = 7,529) of women participating more than once.
Statistical analyses were performed using SAS version 9.3 (SAS Institute Inc. Cary, NC).
RESULTS
Study Population
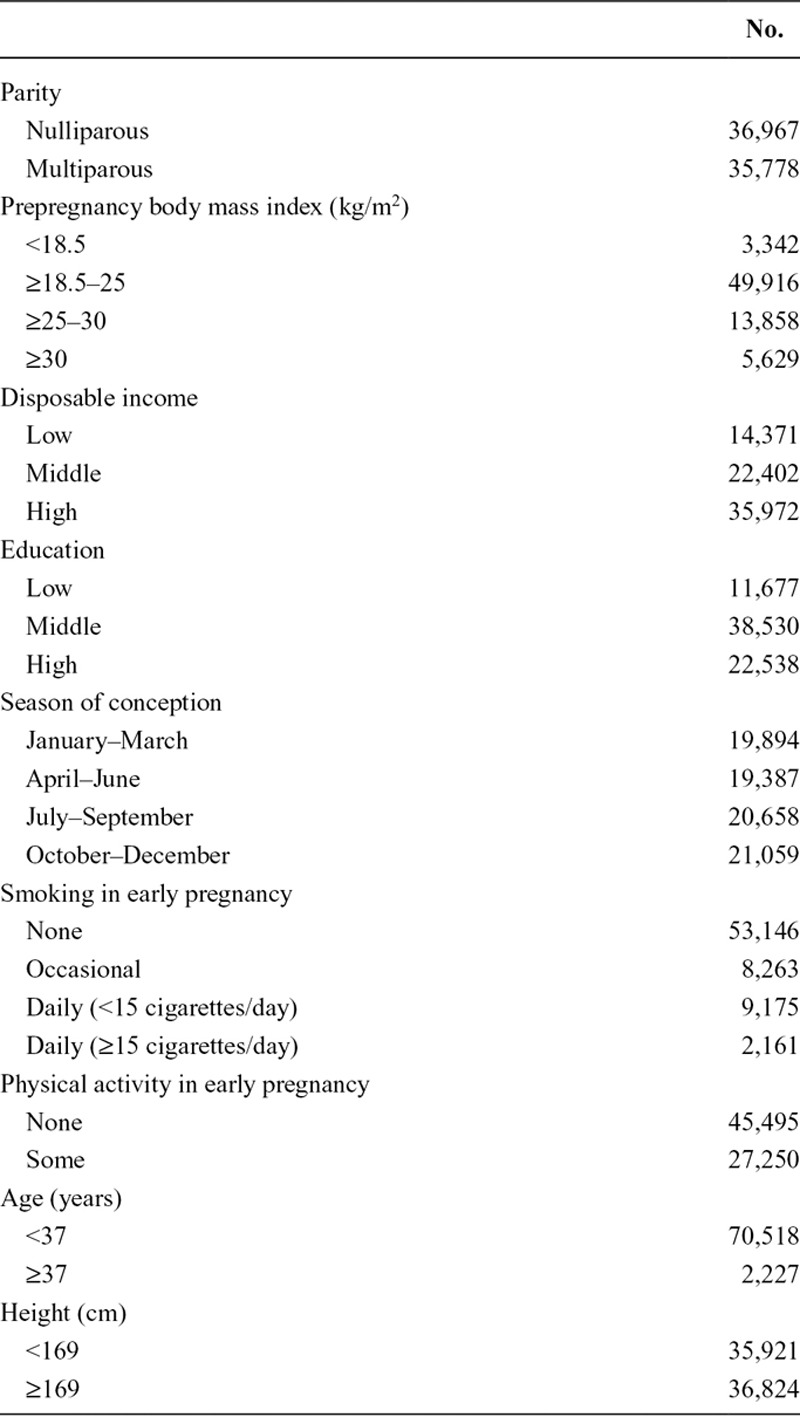
The participating women mainly have middle to high education, are nonsmokers in their late 20s to early 30s with prepregnancy BMI in a range of 18.5–24.9 kg/m2(Table 1). Half of the participating women have given birth before the index pregnancy.
TABLE 1.
Study Population Characteristics (N = 72,745)
We included 72,745 pregnancies, which correspond to 72% of the pregnancies enrolled in the cohort (Figure). The overall prevalence of pre-eclampsia was 3% and the prevalence of pre-eclampsia was similar for the included and excluded pregnancies (eTable 1; http://links.lww.com/EDE/B111). In contrast, the prevalence of gestational hypertension was higher among the excluded pregnancies than the included pregnancies (1.4% vs. 1%). The median exposures of included pregnancies to NO2 and road traffic noise during the first trimester were slightly higher than those of excluded pregnancies (11.5 vs. 11.1 μg/m3and 57.5 vs. 57.3 dB, respectively).
The home residences of the participating women were spread out over Denmark and women living in cities had the highest exposures to NO2. The median (and the interquartile range) exposure during the first trimester to NO2 and Lden road was 11.5 (6.7) μg/m3 and 57.5 (9.6) dB, respectively (eFigure 1; http://links.lww.com/EDE/B111). The exposure distribution during each trimester and the full pregnancy is summarized in eTable 2; http://links.lww.com/EDE/B111. Few of the pregnancies were coexposed to a median noise level from railways (n = 12,351 [17%] of 51.3 dB at the first trimester) or airports (n = 760 [1%] of 50.0 dB). The Spearman Rank correlation coefficients (r) between air pollution and noise exposures are presented in eTable3; http://links.lww.com/EDE/B111. The correlation between NO2 and Lden road during the first trimester was 0.44. Because annual means were used in the modeling for road noise and daily means were used for NO2, exposure to road noise among trimesters showed high correlations, whereas correlations among trimesters for NO2were modestly correlated. The correlation between first trimester and third trimester exposure means was modest for NO2 (r = 0.38), whereas it was highly correlated for Lden road (0.90). The correlation between Lden road and Lden railway among the participants exposed to railway noise (n = 13,593) was weak (0.03).
Air Pollution, Noise, and Pregnancy-induced Hypertensive Disorders
Both exposures to NO2 and Lden road were significantly associated with increased risks of pre-eclampsia (all subtypes) and hypertensive disorders in pregnancy in single-exposure models (Table 2). For both exposures, the associations were strongest for mild pre-eclampsia and pre-eclampsia with early onset. In contrast to all other outcomes, increased risks were not evident for severe pre-eclampsia, which includes eclampsia. For pre-eclampsia with late onset and gestational hypertension, the 95% CIs included 1.
TABLE 2.
Ambient Air Pollution and Road Traffic Noise During First Trimester in Associations with Hypertensive Disorders in Pregnancy (N = 72,745)
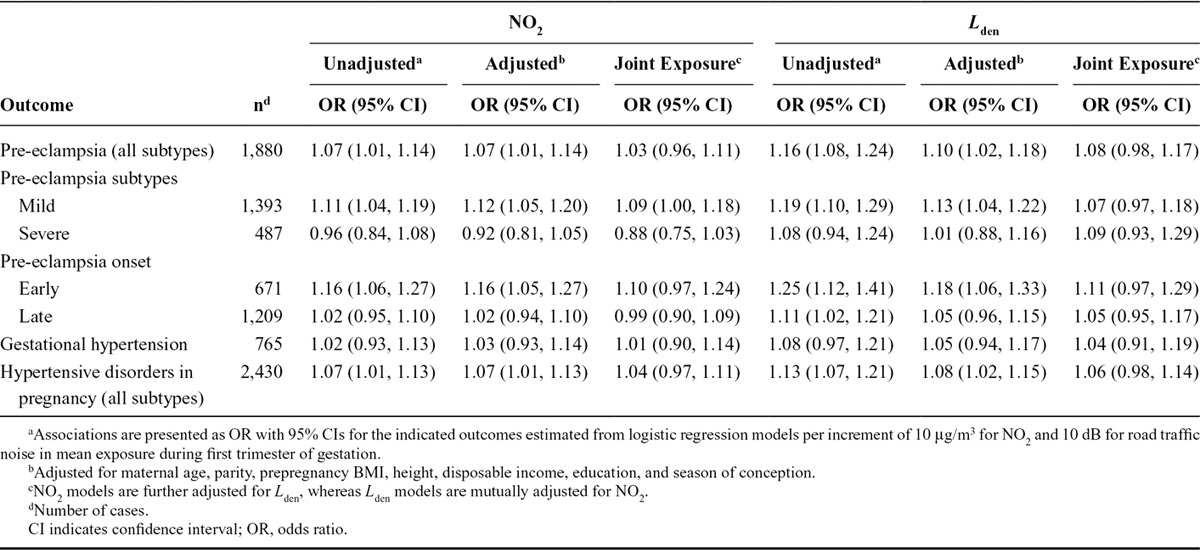
The adjusted effect estimates were slightly smaller than the crude estimates (Table 2). Further adjustment for maternal smoking and physical activity did not change the effect estimates (eTable4; http://links.lww.com/EDE/B111). To evaluate exposures preceding the development of hypertensive disorders, we report associations with first trimester in the main tables, but the estimated effect sizes were generally similar across different time periods during pregnancy for both exposure to NO2 and Lden (eTable5; http://links.lww.com/EDE/B111).
In mutually adjusted models, estimates for both air pollution and road traffic noise decreased and only the association between NO2 and mild pre-eclampsia remained unchanged (Table 2). Exposures to railway noise were not associated with higher risk for any of the outcomes (eTable6; http://links.lww.com/EDE/B111).
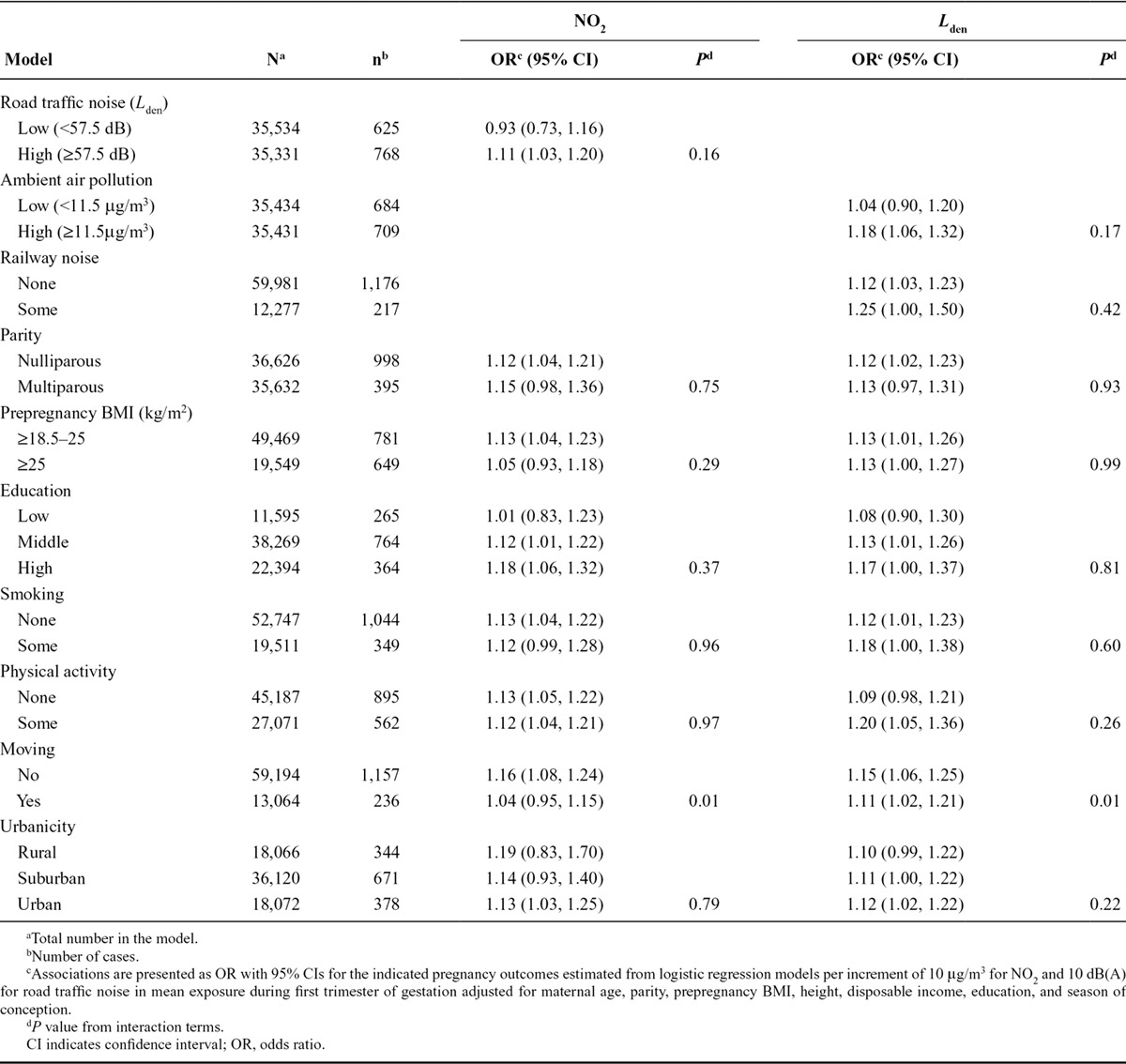
There were no interactions between NO2 and Lden (Table 3).The effects estimates of NO2 and Lden exposure associated with mild pre-eclampsia among primiparous women were similar to those of the multiparous population (Table 3). There was also no discernible difference between effect estimates for mild pre-eclampsia among socioeconomic groups for both exposures. Likewise, there were no evidences for effect modification of associations of NO2 and Lden exposure on risk of mild pre-eclampsia by any of the risk factors examined. For both NO2 and road Lden associations were stronger among nonmovers as compared with women who changed address (Table 3).
TABLE 3.
Effect Modification of the Associations Between Exposure to Ambient Air Pollution, Road Traffic Noise During First Trimester and Mild Pre-eclampsia
Similar effect estimates were found for all outcomes after additional adjustment for gestational diabetes and temperature to those summarized in Table 2 (eTable7; http://links.lww.com/EDE/B111). There was no change in the reported effect estimates after inclusion of women with pre-existing hypertension or after inclusion of the later pregnancies using GEE.
DISCUSSION
In a prospective cohort study with 72,745 women residing in Denmark with fairly low exposures to NO2 (P5–P95: 5.8–27.4 μg/m3), we observed a 7% increase in the risks of pre-eclampsia for each 10 µg/m3 increase in NO2 exposure estimated at the home address(es) during first trimester. A 10-dB increase in road traffic noise was associated with a 10% increase in the risk of pre-eclampsia. These associations were stronger for the mild subtypes of pre-eclampsia and pre-eclampsia with early onset, whereas an increased risk for severe pre-eclampsia was not evident. Associations for pre-eclampsia with late onset and gestational hypertension were consistent with those of higher risk.
Our results for NO2 are consistent with previous studies,5 for which a 10 µg/m3 increase in NO2 was associated with a random-effect meta-analysis combined odds ratio of 1.10 for pre-eclampsia with little evidence of heterogeneity and a consistent pattern of increased risks between 4% and 23% in the individual studies.
To our knowledge, our study is the first to estimate effects of exposure to road traffic noise on the risk of pre-eclampsia and to control for potential confounding or effect modification by air pollution. One small study (N = 3,211) from Lithuania has reported a nonsignificant association between noise from road traffic and gestational hypertension,9 but exposure to air pollution and other related outcomes were not examined in this study.
Occupational noise has been associated with increased risk of pre-eclampsia and gestational hypertension in some, but not all studies.6 Exposure to occupational noise usually occurs during daytime, whereas residential exposures are during the night, which has been found to be associated with sleep disturbance. Thus, direct extrapolation of findings from occupational noise studies to environmental exposures is problematic.
We found no association between exposure to railway noise and pregnancy hypertensive disorders, which might be partly explained by previous studies reporting that road traffic noise is associated with more sleep disturbance,12 and perceived as more disturbing than railway noise.13
Our study suggests that exposure to both traffic-related air pollution and noise may be determinants of pre-eclampsia and gestational hypertension with the strongest evidence for pre-eclampsia. Differences in the etiology may explain, in part, the differences in the strength of the observed effect on the two outcomes. Another possible explanation in the differential associations could be differences in the outcome validity. A higher positive predictive value for the registry diagnosis of pre-eclampsia than for gestational hypertension (74% vs. 56%) has been reported in a large validation study conducted in a subset of the present cohort.21
The lack of findings for severe pre-eclampsia are in contrast to the Swedish findings, in which the adjusted ORs associated with the highest versus the lowest quartiles of NOX were 1.51 for mild pre-eclampsia and 1.48 for severe pre-eclampsia.32 Our findings for severe pre-eclampsia are on the other hand in line with the null findings for severe pre-eclampsia associated with both NO2 and fine particulate matter (PM2.5) of a large study from New York City.33 Other previous studies evaluating the associations between air pollution and pre-eclampsia have only reported the effect estimates for pre-eclampsia without using detailed clinical data to assess subtypes of pre-eclampsia.5
In joint exposure models, the estimates for both exposures were generally decreased, suggesting that we did not have sufficient power to separate the effects of the two exposures. Ambient air pollution with NO2 and road traffic noise are correlated in the present study, reflecting that road traffic is a source of both exposures. The modest correlation between exposures to air pollution and noise in our study area may also explain why the associations were difficult to separate from one another. The NO2 estimate associated with mild pre-eclampsia had a higher precision as compared with the Lden estimate in mutually adjusted models and only the association between NO2 and mild pre-eclampsia remained evident in mutually adjusted models estimates for both air pollution and road traffic noise. The two exposures could be mutually confounded in a positive direction, which would tend to attenuate effects when coadjusted. However, we cannot rule out that the air pollution models predict air pollution levels more precisely than the noise model predicts road traffic noise, which could potentially explain the apparent more robust association with air pollution.
Major strengths of our study are the large size, prospective cohort design with relatively detailed information on exposure and on important potential confounding factors and that exposure was estimated independently from and in time periods before the outcome, which eliminates the risk of recall bias or reverse causation. The large sample size enabled us to adjust for a large number of potential confounders, to examine pre-eclampsia risk in analyses restricted to subgroups, and to study subtypes of pre-eclampsia.
We used Lden (day, evening, and night) as there is a high correlation between the Lden and Lnight road (Ln; 22:00–07:00 hours) for each trimester and the entire pregnancy period (0.97).28 Our assessment of exposure to both NO2 and road traffic was based on state-of-the-art methods. The level of traffic noise varies over very short time periods due to factors such as the movement of vehicles relative to the observer and the strong influence of weather on the propagation of traffic noise. It is therefore extremely difficult if not impossible to get reliable long-term noise exposure data by use of direct measurements. However, recently, more accurate and reliable prediction methods for traffic noise have been developed for relatively flat areas like Denmark.
Our study had limitations as well. Our exposure assessment was limited to home address(es) during pregnancy, and exposures elsewhere were not estimated, because detailed information about time-activity patterns, occupational exposures, or personal measures were not available. To minimize exposure misclassification, it might be important to consider, for example, exposures at other locations where the women spend their time, the location of their bedroom, the preferred mode of commuting, and the average duration of their commute to work/study. The stronger associations among nonmovers as compared with movers could reflect a more precise exposure assessment for the nonmovers as it could be that the time spend at home differs between women who moved and those who did not, but in contrast to most studies,5,33 we were able to account for moving and the exact location of the maternal residence during the entire pregnancy.
Air pollution exposure was based on NO2 only. No data on exposure to inhalable particulate matter or other potential toxic air pollutants were available for this study. Although, stronger risk for pre-eclampsia have been reported for PM2.5 in meta-analyses,5 nitrogen oxides are highly correlated to particulate matter in Danish streets.25,34
We cannot rule out residual confounding or confounding by factors not adjusted such as nonresidential exposure to air pollution and noise, occupational exposures, exposure to green space, or certain unmeasured factors such as diet. Although the similar unadjusted and adjusted estimates in our study provide some support for that the associations observed may not be confounded by social and lifestyle factors included smoking in our analysis. Furthermore, we found no evidence of effect modification by urban versus rural area of living.
In conclusion, road traffic may be associated with increased risk of pre-eclampsia and hypertensive disorders in pregnancy through exposure to both air pollution and noise, although the effects were generally difficult to separate.
ACKNOWLEDGMENTS
We thank all the participants and collaborators of the Danish National Birth Cohort. We thank Nick Martinussen for assistance on data preparation and Leslie T. Stayner for proof reading.
Supplementary Material
Footnotes
The authors report no conflicts of interest.
The Danish Council for Independent Research (Grant DFF-4004-00179) funded the study. Estimation of air pollution and noise exposure was financed by the European Research Council, EU 7th Research Framework Programme (the QUIET project, Grant 281760). The Danish National Research Foundation has established the Danish Epidemiology Science Centre that initiated and created the Danish National Birth Cohort. The cohort is furthermore a result of a major grant from this foundation. Additional support for the Danish National Birth Cohort is obtained from the Pharmacy Foundation, the Egmont Foundation, the March of Dimes Birth Defects Foundation, the Augustinus Foundation, and the Health Foundation.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com).
REFERENCES
- 1.Roberts CL, Ford JB, Algert CS, et al. Population-based trends in pregnancy hypertension and pre-eclampsia: an international comparative study. BMJ Open. 2011;1:e000101. doi: 10.1136/bmjopen-2011-000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376:631–644. doi: 10.1016/S0140-6736(10)60279-6. [DOI] [PubMed] [Google Scholar]
- 3.Trogstad L, Magnus P, Stoltenberg C. Pre-eclampsia: risk factors and causal models. Best Pract Res Clin Obstet Gynaecol. 2011;25:329–342. doi: 10.1016/j.bpobgyn.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 4.Shah AS, Langrish JP, Nair H, et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet. 2013;382:1039–1048. doi: 10.1016/S0140-6736(13)60898-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pedersen M, Stayner L, Slama R, et al. Ambient air pollution and pregnancy-induced hypertensive disorders: a systematic review and meta-analysis. Hypertension. 2014;64:494–500. doi: 10.1161/HYPERTENSIONAHA.114.03545. [DOI] [PubMed] [Google Scholar]
- 6.Tétreault LF, Perron S, Smargiassi A. Cardiovascular health, traffic-related air pollution and noise: are associations mutually confounded? A systematic review. Int J Public Health. 2013;58:649–666. doi: 10.1007/s00038-013-0489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ristovska G, Laszlo HE, Hansell AL. Reproductive outcomes associated with noise exposure - a systematic review of the literature. Int J Environ Res Public Health. 2014;11:7931–7952. doi: 10.3390/ijerph110807931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gehring U, Tamburic L, Sbihi H, Davies HW, Brauer M. Impact of noise and air pollution on pregnancy outcomes. Epidemiology. 2014;25:351–358. doi: 10.1097/EDE.0000000000000073. [DOI] [PubMed] [Google Scholar]
- 9.Bendokiene I, Grazuleviciene R, Dedele A. Risk of hypertension related to road traffic noise among reproductive-age women. Noise Health. 2011;13:371–377. doi: 10.4103/1463-1741.90288. [DOI] [PubMed] [Google Scholar]
- 10.van Kempen E, Babisch W. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J Hypertens. 2012;30:1075–1086. doi: 10.1097/HJH.0b013e328352ac54. [DOI] [PubMed] [Google Scholar]
- 11.Babisch W. Road traffic noise and cardiovascular risk. Noise Health. 2008;10:27–33. doi: 10.4103/1463-1741.39005. [DOI] [PubMed] [Google Scholar]
- 12.Sørensen M, Hvidberg M, Andersen ZJ, et al. Road traffic noise and stroke: a prospective cohort study. Eur Heart J. 2011;32:737–744. doi: 10.1093/eurheartj/ehq466. [DOI] [PubMed] [Google Scholar]
- 13.Miedema HM, Vos H. Associations between self-reported sleep disturbance and environmental noise based on reanalyses of pooled data from 24 studies. Behav Sleep Med. 2007;5:1–20. doi: 10.1207/s15402010bsm0501_1. [DOI] [PubMed] [Google Scholar]
- 14.Selander J, Bluhm G, Theorell T, et al. HYENA Consortium. Saliva cortisol and exposure to aircraft noise in six European countries. Environ Health Perspect. 2009;117:1713–1717. doi: 10.1289/ehp.0900933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 16.László KD, Liu XQ, Svensson T, et al. Psychosocial stress related to the loss of a close relative the year before or during pregnancy and risk of preeclampsia. Hypertension. 2013;62:183–189. doi: 10.1161/HYPERTENSIONAHA.111.00550. [DOI] [PubMed] [Google Scholar]
- 17.Haney A, Buysse DJ, Okun M. Sleep and pregnancy-induced hypertension: a possible target for intervention? J Clin Sleep Med. 2013;9:1349–1356. doi: 10.5664/jcsm.3290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olsen J, Melbye M, Olsen SF, et al. The Danish National Birth Cohort–its background, structure and aim. Scand J Public Health. 2001;29:300–307. doi: 10.1177/14034948010290040201. [DOI] [PubMed] [Google Scholar]
- 19.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 suppl):30–33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 20.Knudsen LB, Olsen J. The Danish Medical Birth Registry. Dan Med Bull. 1998;45:320–323. [PubMed] [Google Scholar]
- 21.Klemmensen AK, Olsen SF, Osterdal ML, Tabor A. Validity of preeclampsia-related diagnoses recorded in a national hospital registry and in a postpartum interview of the women. Am J Epidemiol. 2007;166:117–124. doi: 10.1093/aje/kwm139. [DOI] [PubMed] [Google Scholar]
- 22.Østerdal ML, Strøm M, Klemmensen AK, et al. Does leisure time physical activity in early pregnancy protect against pre-eclampsia? Prospective cohort in Danish women. BJOG. 2009;116:98–107. doi: 10.1111/j.1471-0528.2008.02001.x. [DOI] [PubMed] [Google Scholar]
- 23.Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(7 suppl):22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 24.Jensen SS, Hvidberg M, Pedersen J, et al. Gis-based national street and traffic data base 1960–2005. Roskilde: National Environmental Research Institute, Aarhus University; NERI Technical Report No. 678. [Google Scholar]
- 25.Ketzel M, Berkowicz R, Hvidberg M, Jensen SS, Raaschou-Nielsen O. Evaluation of AirGIS: a GIS-based air pollution and human exposure modelling system. Int J Environ Pollution. 2011;47:226–238. [Google Scholar]
- 26.Berkowicz R, Ketzel M, Jensen SS, Hvidberg M. Raaschou- Nielsen O. Evaluation and application of OSPM for traffic pollution assessment for large number of street locations. Environ Model Software. 2008;23:296–303. [Google Scholar]
- 27.Ritz B, Lee PC, Hansen J, et al. Traffic-related air pollution and Parkinson’s disease in Denmark: a case-control study. Environ Health Perspect. 2016;124:351–356. doi: 10.1289/ehp.1409313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hjortebjerg D, Andersen AM, Garne E, Raaschou-Nielsen O, Sørensen M. Non-occupational exposure to paint fumes during pregnancy and risk of congenital anomalies: a cohort study. Environ Health. 2012;11:54. doi: 10.1186/1476-069X-11-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bendtsen H. The nordic prediction method for road traffic noise. SciTotal Environ. 1999;235:331–338. [Google Scholar]
- 30.Bodin T, Björk J, Ohrström E, Ardö J, Albin M. Survey context and question wording affects self reported annoyance due to road traffic noise: a comparison between two cross-sectional studies. Environ Health. 2012;11:14. doi: 10.1186/1476-069X-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klein–Tank AMG, Wijngaard JB, Können GP, et al. Daily dataset of 20th–century surface air temperature and precipitation series for the European climate assessment. Int J Climatol. 2002;22:1441–1453. [Google Scholar]
- 32.Malmqvist E, Jakobsson K, Tinnerberg H, Rignell-Hydbom A, Rylander L. Gestational diabetes and preeclampsia in association with air pollution at levels below current air quality guidelines. Environ Health Perspect. 2013;121:488–493. doi: 10.1289/ehp.1205736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Savitz DA, Elston B, Bobb JF, et al. Ambient fine particulate matter, nitrogen dioxide, and hypertensive disorders of pregnancy in New York City. Epidemiology. 2015;26:748–757. doi: 10.1097/EDE.0000000000000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ketzel M, Wahlin P, Berkowicz R, Palmgren F. Particle and trace gas emission factors under urban driving conditions in Copenhagen based on street and roof level observations. Atmos Environ. 2003;37:2735–2749. [Google Scholar]


