Abstract
Background:
The current paper includes a systematic search of the literature, a detailed presentation of the results, and a grading of treatment options in terms of efficacy and tolerability/safety.
Material and Methods:
The PRISMA method was used in the literature search with the combination of the words ‘bipolar,’ ‘manic,’ ‘mania,’ ‘manic depression,’ and ‘manic depressive’ with ‘randomized,’ and ‘algorithms’ with ‘mania,’ ‘manic,’ ‘bipolar,’ ‘manic-depressive,’ or ‘manic depression.’ Relevant web pages and review articles were also reviewed.
Results:
The current report is based on the analysis of 57 guideline papers and 531 published papers related to RCTs, reviews, posthoc, or meta-analysis papers to March 25, 2016. The specific treatment options for acute mania, mixed episodes, acute bipolar depression, maintenance phase, psychotic and mixed features, anxiety, and rapid cycling were evaluated with regards to efficacy. Existing treatment guidelines were also reviewed. Finally, Tables reflecting efficacy and recommendation levels were created that led to the development of a precise algorithm that still has to prove its feasibility in everyday clinical practice.
Conclusions:
A systematic literature search was conducted on the pharmacological treatment of bipolar disorder to identify all relevant random controlled trials pertaining to all aspects of bipolar disorder and graded the data according to a predetermined method to develop a precise treatment algorithm for management of various phases of bipolar disorder. It is important to note that the some of the recommendations in the treatment algorithm were based on the secondary outcome data from posthoc analyses.
Keywords: bipolar disorder, anticonvulsants, antidepressants, antipsychotics, evidence-based guidelines, lithium, mania, bipolar depression, mood stabilizers, treatment, clinical trials
Introduction
The current paper is the second in the series of The International College of Neuro-Psychopharmacology papers concerning the development of a precise algorithm and clinical guidelines for the treatment of bipolar disorder (BD) in adults for use in primary and secondary care. It includes a systematic search of the literature and a detailed presentation of the results concerning placebo-controlled randomized trials for all phases and aspects of BD. It also includes the grading of treatment options in terms of efficacy and tolerability/safety as well as a precise algorithm that still has to prove its feasibility in everyday clinical practice.
Materials and Methods
As described in the first paper concerning the CINP treatment guidelines for BD, the workgroup decided that the PRISMA method (Hopewell et al., 2008; Liberati et al., 2009; Moher et al., 2009) should be followed in the search of the literature. The method included the search for 3 kinds of papers:
Randomized controlled trials (RCTs; placebo controlled as well as clinical trials with an active comparator with the compounds used as monotherapy or add-on therapy).
Posthoc analyses of RCTs.
Meta-analyses and review papers.
Treatment guidelines papers.
For this purpose, MEDLINE was searched to March 25, 2016 with the following search strategies:
To locate RCTs, the combination of the words ‘bipolar,’ ‘manic,’ ‘mania,’ ‘manic depression,’ and ‘manic depressive’ and ‘randomized’ was used.
Web pages containing lists of clinical trials were scanned. These sites included http://clinicaltrials.gov and http://www.clinicalstudyresults.org as well as the official sites of all the pharmaceutical companies with products used for the treatment of BP.
Relevant review articles were scanned and their reference lists were utilized (Srisurapanont et al., 1995; Yatham et al., 1997; Davis et al., 1999; Burgess et al., 2001; Macritchie et al., 2001, 2003; Bech, 2002, 2006; Rendell et al., 2003; Gijsman et al., 2004; Fountoulakis et al., 2005; Gao et al., 2005; Cipriani et al., 2006a, 2006b, 2011; Rendell et al., 2006; Smith et al., 2007; Fountoulakis, 2008, 2012, 2015a, 2015b, 2015c; Fountoulakis et al., 2008a, 2009b, 2012a, 2012d; Fountoulakis and Vieta, 2008; Yildiz et al., 2010; Nivoli et al., 2011; Tarr et al., 2011; Nivoli et al., 2012).
The MEDLINE was searched with the combination of keywords ‘guidelines’ or ‘algorithm’ with ‘mania,’ ‘manic,’ ‘bipolar,’ ‘manic-depressive,’ or ‘manic depression.’
The treatment guidelines were also scanned and their reference lists were utilized.
It is difficult to locate unpublished studies, especially old ones, and even more difficult to retrieve their results. Thus, the main focus of this paper was on published studies that would have been peer-reviewed, are typically of higher quality, and provide more details than meeting abstracts or conference reports. However, whenever an unpublished trial was located, it is mentioned in that specific part of the manuscript. The authors decided not to seek additional information concerning unpublished trials from manufacturers as this might increase the retrieval bias.
Eventually the efficacy data were graded on the basis of a method developed by the authors and described in the first paper of the CINP guidelines for BD, that is also shown in Table 1. Agents were graded on the basis of safety and tolerability, and these grades are also shown in Table 1.
Table 1.
The Method for the Grading of Data on the Basis of Efficacy and Tolerability
| Grading on Basis of Efficacy | |
| Level 1 | Good research-based evidence, supported by at least 2 placebo controlled studies of sufficient magnitude and good quality. In case of the presence of negative RCTs, positive RCTs should outnumber negative ones. |
| Level 2 | Fair research-based evidence, from one randomized, double-blind placebo controlled trial. Also in case one or more trials exist, however, they fail to fulfil all the criteria above (e.g., very small sample size or no placebo control) as well as in case of positive meta-analysis alone. |
| Level 3 | Some evidence from comparative studies without placebo arm or from posthoc analyses. |
| Level 4 | Inconclusive data or poor quality of RCTs |
| Level 5 | Negative data |
| Grading on the basis of safety and tolerability | |
| Level 1 | Very good tolerability, few side effects that are not enduring, they do not cause significant distress, and are not life-threatening and they do not compromise the overall somatic health of the patient. |
| Level 2 | Moderate tolerability, many side effects that could be enduring and cause significant distress, but they are not life-threatening although they could compromise the overall somatic health of the patient. Agents with very good overall tolerability but with rare life-threatening adverse events, could be classified here only if the lethality risk can be essentially considered to be negligible with the application of procedures and protocols (e.g., laboratory testing, titration schedules etc.). |
| Level 3 | Poor tolerability, many side effects that are enduring, cause significant distress, compromise the overall somatic health of the patient, or are life-threatening. Agents with moderate overall tolerability and rare life-threatening adverse events should be classified here even in cases the lethality risk can be essentially considered to be negligible with the application of procedures and protocols (e.g., laboratory testing, titration schedules etc.). . |
| Recommendations for treatment (combination of efficacy and safety/tolerability) | |
| Level 1 | Level 1 or 2 for efficacy and 1 for safety/tolerability |
| Level 2 | Level 1 or 2 for efficacy and 2 for safety/tolerability |
| Level 3 | Level 3 for efficacy and 1 or 2 for safety/tolerability |
| Level 4 | Level 4 for efficacy or 3 for safety/tolerability |
| Level 5 | Level 5 for efficacy (not recommended) |
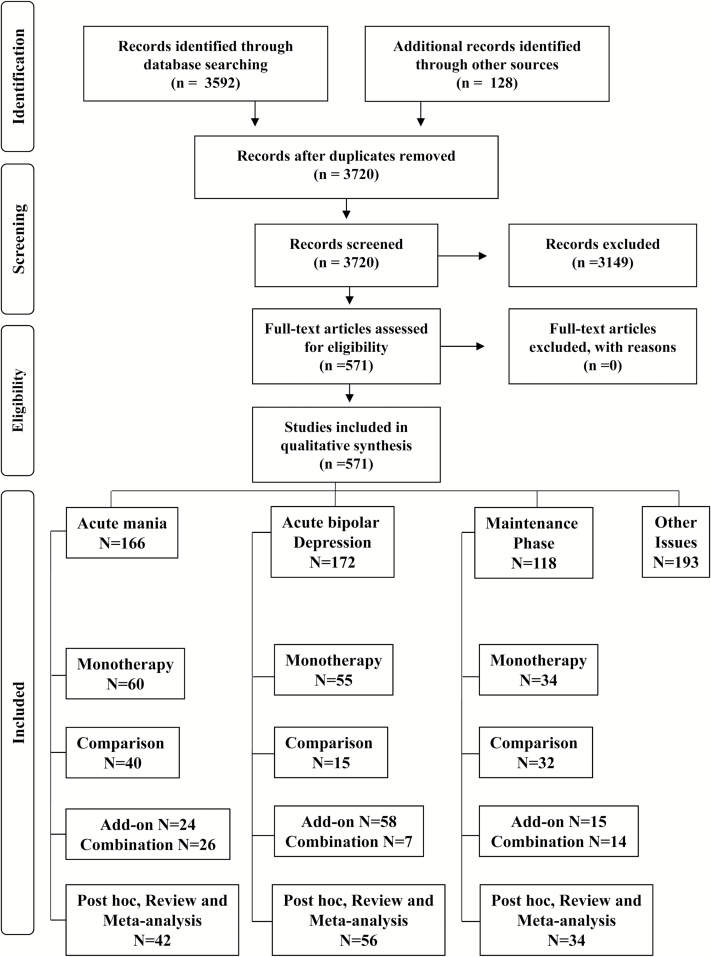
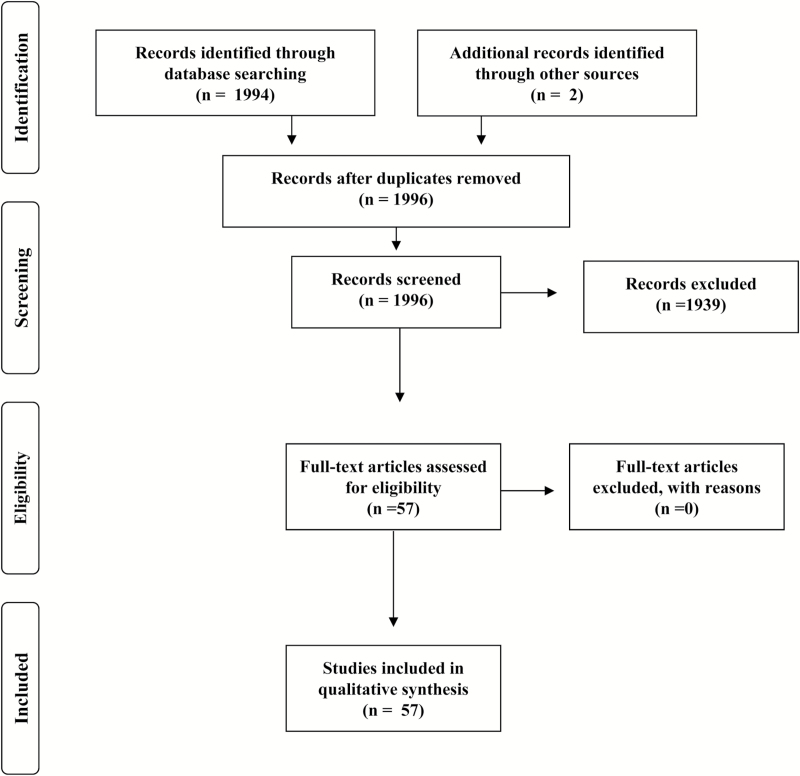
The PRISMA chart of the search process is shown in Figure 1 concerning RCTs and in Figure 2 concerning guidelines. Ultimately the current report was based on the analysis of 57 papers related to guidelines and 569 published papers concerning RCTs or other relevant papers (reviews, posthoc, or meta-analyses).
Figure 1.
PRISMA flowchart for RCTs literature search.
Figure 2.
PRISMA flowchart for treatment guidelines literature search
Efficacy Data
Acute Mania
The data on monotherapy and combination treatment for acute mania are shown in Table 2. As well, the table also includes grading of efficacy data for various features of mania such as psychotic features, mixed features, agitation, etc., most of that was based on the posthoc analyses of RCTs.
Table 2.
Acute Mania/Mixed Treatment Phase, Grading on Basis of Efficacy (Treatment Phase up to 12 Weeks)
| Acute Manic Episodes | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Agent/modality (alphabetical order) | Monotherapy | Combination with | ||||||||||
| Effect start day | Overall | Core manic | Depressive | Psychotic | Agitation | MS | Cbz | Lam | Li | Val | FGAs | |
| Allopurinol | - | - | - | - | - | - | 5 | - | - | 3 | - | 5 |
| Aripiprazole | 2–4 | 1 | - | 5 | 3 | - | 2 | - | - | - | - | - |
| Asenapine | 2 | 1 | - | 4 | - | - | 2 | - | - | - | - | - |
| Carbamazepine | 14 | 1 | - | 5 | - | - | - | - | - | - | - | - |
| Cariprazine | 4 | 1 | 3 | 5 | - | - | - | - | - | - | - | - |
| Celecoxib | - | - | - | - | - | - | - | - | - | - | 2 | - |
| Chlorpromazine | - | 4 | - | - | - | - | - | - | - | - | - | - |
| Clozapine | - | - | - | - | - | - | - | - | - | - | - | - |
| ECT | - | 3 | - | - | - | - | - | - | - | - | - | - |
| Eslicarbazepine | - | 5 | - | - | - | - | - | - | - | - | - | - |
| Gabapentin | - | 5 | - | - | - | - | 5 | - | - | - | - | - |
| Haloperidol | 4 | 1 | 5 | 5 | 3 | 3 | 2 | 2 | - | 2 | 2 | - |
| Lamotrigine | - | 5 | - | - | - | - | - | - | - | - | - | - |
| Levetiracetam | - | - | - | - | - | - | - | - | - | - | - | - |
| Licarbazepine | - | 5 | - | - | - | - | - | - | - | - | - | - |
| Lithium | 7 | 1 | 4 | 5 | 2 | - | - | 2 | - | - | - | - |
| Loxapine inhalant | - | - | - | - | - | 2 | - | - | - | - | - | - |
| Medroxyprogesterone | - | - | - | - | - | - | 5 | - | - | - | - | - |
| Olanzapine | 2–7 | 1 | 3 | 3 | 3 | 2 | 1 | 5 | - | - | 1 | - |
| Oxcarbazepine | - | 4 | - | - | - | - | - | - | - | 4 | - | - |
| Paliperidone | 2 | 1 | - | - | - | - | 5 | - | - | - | - | - |
| Pimozide | - | 4 | - | - | - | - | - | - | - | - | - | - |
| Quetiapine | 4 | 1 | - | 3 | 3 | - | 3 | - | - | 2 | - | - |
| Risperidone | 3 | 1 | - | 3 | 3 | - | 3 | - | - | - | 5 | - |
| Tamoxifen | 5 | 2 | 3 | 5 | 3 | - | 2 | - | - | 2 | - | - |
| TMS | - | 5 | - | - | - | - | - | - | - | - | - | - |
| Topiramate | - | 5 | - | - | - | - | 5 | - | - | - | - | - |
| Valproate | 5–15 | 1 | 5 | 5 | - | 3 | - | - | - | - | - | 2 |
| Verapamil | - | 5 | - | - | - | - | - | - | - | - | - | - |
| Ziprasidone | 2 | 1 | 3 | 5 | 3 | - | 5 | - | - | - | - | - |
Abbreviations: -, no data; Cbz, carbamazepine; ECT, electroconvulsive therapy; FGA, first generation antipsychotic; Lam, lamotrigine; Li, lithium; MS, mood stabilizer; TMS, transcranial magnetic stimulation; Val, valproate.
The treatment options are rated according to the rating system shown in Table 1.
Monotherapy
Lithium.
The first study investigating the efficacy of lithium against acute mania was conducted in 1971, but it did not follow a methodology that is accepted today as scientific standard (Stokes et al., 1971). Since then 4 placebo-controlled RCTs using modern clinical trial methodology starting in 1994 have been published. All of them utilized a period of 3 weeks vs placebo, and if a comparator was included, there was an extension phase without placebo (Bowden et al., 1994, 2005b; Kushner et al., 2006; Keck et al., 2009).
Overall there are 5 RCTs supporting the efficacy of lithium in comparison with placebo in acutely manic or mixed BD patients. All 5 are positive and the results are consistent. The overall response rate suggests a rough number needed to treat (NNT) around 5 to 6. The therapeutic effect appears after 7 days of treatment, that is, later in comparison with antipsychotics. There are limited data about the effect of lithium on the core symptoms of mania, but there are some suggestive of an effect on psychotic features (Bowden et al., 2005b). Its effect specifically on mixed episodes is unknown, and a posthoc analysis (Swann et al., 1997) of one of these RCTs (Bowden et al., 1994) confirmed the efficacy of lithium only in classic manic but not mixed patients albeit the number of mixed patients was too small to allow firm conclusion. It exerts a therapeutic effect on manic-psychotic symptoms, but probably there is no therapeutic effect on concomitant depressive symptoms. The drop-out rate in these trials was comparable with placebo with probably more patients on placebo withdrawing from the study because of lack of efficacy, while side effects were the more common reasons for withdrawal in patients taking lithium. The most common adverse events with lithium were nausea, vomiting, dizziness headache, insomnia, asthenia, constipation, diarrhoea, tremor, and weight gain.
Antiepileptics.
Valproate
Limited data concerning the efficacy of valproate in acute mania exist from earlier studies (Emrich et al., 1980, 1981; McElroy et al., 1989). The first study with modern methodology on the efficacy and safety of valproate in the treatment of acute mania was published in 1991 (Pope et al., 1991). Since then 3 positive (Pope et al., 1991; Bowden et al., 1994, 2006) and 2 failed RCTs (Tohen et al., 2008b; Hirschfeld et al., 2010) were published. Another study on a heterogeneous sample consisting of bipolar spectrum disorder patients was negative (McElroy et al., 2010a). A posthoc analysis of one of the RCTs (Bowden et al., 1994) did not find any preferential effect for divalproex in classic vs mixed manic patients (Swann et al., 1997). Overall the data support the usefulness of valproate against acute mania, although a number of issues need clarification. Its effect on psychotic symptoms is unknown and there seems to be no effect on concomitant depressive symptoms. The NNT for response is probably around 10 and the therapeutic effect is present after 5 to 15 days. Although the dosages utilized in these studies were higher than those usually used in everyday clinical practice (15–30 mg/kg/d), they hardly achieved the target serum concentrations (50–100 microg/mL). The most frequent adverse events were somnolence, nausea, dizziness, asthenia, constipation, twitching, and vomiting.
Carbamazepine
The earlier studies demonstrating the efficacy of carbamazepine in acute mania were published in the 1980s (Ballenger and Post, 1980; Post et al., 1987). Three large clinical trials using modern methodology have been published since 2000, all of that have confirmed the efficacy of carbamazepine (Weisler et al., 2004, 2005; Zhang et al., 2007).
Thus, the data concerning the efficacy and safety of carbamazepine at dosages 400 to 1600 mg/d and a mean plasma level of 8.9 μg/mL are robust. The reported NNT is approximately 5 for response, that starts around week 2. It is unknown whether carbamazepine has a beneficial effect on the core manic symptoms, in mixed patients, or against psychotic symptoms. There seems to be a beneficial effect on concomitant depressive symptoms only in mixed patients but not in manic patients (Weisler et al., 2005). The most frequent adverse events related to carbamazepine treatment were dizziness, nausea, somnolence, and an increase in total cholesterol that was composed of increases in both high-density and low-density lipoproteins.
Other antiepileptics
There is one negative (BIA-2093–203) and one fixed-dosage failed (BIA-2093–204) trial for eslicarbazepine (Robertson et al., 2010). Three unpublished RCTs (NCT00107926, NCT00107939, and NCT00099229) concerning the racemic mixture licarbazepine were also negative. There are 2 unpublished negative trials concerning lamotrigine in treating acute manic episodes (SCAA2008/GW609 and SCAA2009/GW610) (Goldsmith et al., 2003). Four trials concerning topiramate were all negative (Kushner et al., 2006). One small RCT evaluated the efficacy and safety of lamotrigine and gabapentin monotherapy vs placebo in 31 patients with refractory bipolar and unipolar mood disorders. Although lamotrigine differed significantly from placebo, gabapentin did not (Frye et al., 2000). Thus the data are negative for all other antiepileptics except for valproic acid and carbamazepine, that suggests that there is no class effect concerning antiepileptics in the treatment of BD (Rosa et al., 2009; Fountoulakis et al., 2011b).
Antipsychotics.
The earlier studies on antipsychotics supported the efficacy of chlorpromazine (Klein, 1967) and suggested that antipsychotics acted more rapidly, although lithium was more globally effective (Shopsin et al., 1975).
Haloperidol
The efficacy and safety of haloperidol (up to 30 mg/d) was studied in 5 RCTs and all were positive (McIntyre et al., 2005; Smulevich et al., 2005; Young et al., 2009; Vieta et al., 2010a; Katagiri et al., 2012). The results suggest a NNT roughly equal to 5 to 8 for response. The therapeutic effect is apparent as early as day 4 (Goikolea et al., 2013a). However it is important to note that there is a signal for the induction of depression in the short term (Goikolea et al., 2013b). One study reported no effect on the core symptoms of mania. However, although haloperidol might be particularly efficacious in psychotic patients, its effect on mixed patients is unknown. Adverse events most commonly reported with haloperidol treatment were somnolence, extrapyramidal symptoms (EPS), weight gain, and constipation.
Olanzapine
There are 6 positive trials supporting the efficacy of olanzapine (5–20 mg/d) for the treatment of manic or mixed episodes and concomitant psychotic features (Tohen et al., 1999, 2000, 2008b; McIntyre et al., 2009a, 2010b; Katagiri et al., 2012). The NNT is approximately around 5 for response (defined as a 50% drop in Young Mania Rating Scale [YMRS]). Olanzapine seems to have a beneficial effect on the core symptoms of mania and on psychotic symptoms, treats mixed patients as well as rapid cycling, possibly improves coexisting depressive symptoms, and response occurs as early as days 2 to 7. Olanzapine does not seem to induce a switch to depression. The most common adverse events related with olanzapine treatment were somnolence, dizziness, dry mouth, thirst, and weight gain. EPS occur but at a lower rate than with haloperidol.
Quetiapine
There exist 4 positive studies supporting the efficacy of quetiapine up to 800 mg/d for the treatment of acute mania (Bowden et al., 2005b; McIntyre et al., 2005; Vieta et al., 2010b; Cutler et al., 2011). Quetiapine does not seem to induce depression; on the contrary there is a clear beneficial effect on concomitant depressive symptoms. However, there is some doubt concerning its efficacy against mixed episodes (such patients were excluded in most quetiapine trials), concomitant psychotic features, and in rapid cycling patients. The NNT is around 4 to 6 for response. The most common adverse events associated with quetiapine treatment included sedation, dry mouth, somnolence, headache, dizziness, and postural hypotension.
Aripiprazole
There are 5 positive (Keck et al., 2003b, 2009; Sachs et al., 2006; Young et al., 2009; Kanba et al., 2014) and one negative fixed dosage study (El Mallakh et al., 2010) concerning the efficacy of aripiprazole 15 to 30 mg/d for the treatment of acute manic and mixed episodes. One study was not completed and reported no results. Again the effect on the core symptoms of mania is unknown. There is a significant effect in mixed and rapid cycling patients, and it also treats concomitant positive psychotic features and agitation. Aripiprazole does not seem to induce depression, but it does not seem to have any effect on concomitant depressive symptoms either. The NNT is approximately around 5 to 10 for response. Nausea, dyspepsia, somnolence, anxiety, vomiting, insomnia, light-headedness, constipation, and akathisia were the most common adverse events. There were no significant effects on body weight, serum prolactin, or QTc prolongation.
Risperidone
The efficacy of risperidone 1 to 6 mg/d for the treatment of acute manic and mixed episodes is supported by 3 positive studies (Hirschfeld et al., 2004; Khanna et al., 2005; Smulevich et al., 2005). The therapeutic effect is evident from day 3 onwards. It seems also effective in the treatment of positive psychotic symptoms and agitation and concomitant depressive symptoms. The NNT is approximately around 3 to 5 for response. It is unknown whether risperidone has an effect on the core symptoms of mania or whether it is beneficial for rapid cycling patients. It does not seem to induce a switch to depression. Somnolence, dyspepsia, nausea, and EPS were the most common adverse events.
Ziprasidone
Three positive studies (Keck et al., 2003a; Potkin et al., 2005; Vieta et al., 2010a) support the efficacy of ziprasidone 80 to 160 mg/d for the treatment of acute manic and mixed episodes. It has a treatment effect on the core symptoms of mania and on concomitant positive psychotic symptoms. It does not seem to have any significant effect on depressive symptoms, but it also does not seem to induce a switch to depression. Its effect in rapid cycling patients is unknown. The NNT is approximately 6 for response. The most common adverse events with ziprasidone treatment were EPS, somnolence, dizziness, anxiety, and dyspepsia. There were no significant effects on body weight or serum lipids. There was a small and clinically not significant QTc prolongation reported
Asenapine
Three positive trials (McIntyre et al., 2009a, 2010b; Landbloom et al., 2016) support the efficacy of asenapine 10 to 20 mg/d for the treatment of acute manic and mixed episodes with efficacy as early as day 2. It is unknown whether it has a treatment effect on the core symptoms of mania, and while in one of the studies a positive effect on the total Possitive and Negative Symptoms Scale (PANSS) score is reported, the specific effect on concomitant positive or negative psychotic features is unknown. Also unknown is the efficacy in rapid cycling patients. The data are equivocal concerning the effect on depressive symptoms, but also it does not seem to induce depression. The NNT is between 6 and 12 for response. The most common adverse events related with asenapine treatment were EPS, somnolence, dizziness, sedation, fatigue, oral hypesthesia, dry mouth, weight gain, and EPS.
Paliperidone
Two studies (Vieta et al., 2010b; Berwaerts et al., 2012b) provide support for the efficacy of 12 mg/d of paliperidone ER for the treatment of acute manic and mixed episodes, while the data for lower dosages is conflicting. Paliperidone is effective as early as day 2. It is not reported whether it has a treatment effect on the core symptoms of mania, positive psychotic symptoms, and depression and the effect in rapid cycling patients is unknown. It is unclear whether paliperidone ER can induce switches to depression. The most common adverse events related with paliperidone ER treatment were headache, somnolence, EPS, and prolactin elevation.
Cariprazine
Three studies (Calabrese et al., 2015; Durgam et al., 2015, 2016; Sachs et al., 2015) confirmed the efficacy of cariprazine (3–12 mg daily) vs placebo in the treatment of acute manic or mixed episodes. The NNT for response or remission is approximately 4 to 7. Cariprazine is reported to improve the core symptoms of mania but had no effect on the Mondgomery Asberg Depression Rating Scale (MADRS). It improves the total PANSS but the specific effect on the PANSS positive subscale is unknown. Its efficacy in mixed and rapid cycling patients is unknown.
Other agents and treatment modalities.
Overall, the data for tamoxifen are positive; however, the total patient sample is still small (Zarate et al., 2007; Yildiz et al., 2008). One NIMH-sponsored clinical trial (NCT00026585) has not reported results yet. One small 3-week study was negative for verapamil (Janicak et al., 1998). The data concerning repetitive Transcranial Magnetic Stimulation (rTMS) are conflicting. There are two RCTs, one negative (Kaptsan et al., 2003) and one positive (Praharaj et al., 2009).
Summary of monotherapy trials for acute mania.
Overall there are sufficient data in the literature to support the general efficacy of a number of agents in the treatment of acute mania; however, many details remain to be explored concerning many of the agents. Lithium, valproate, carbamazepine, haloperidol, olanzapine, quetiapine, aripiprazole, risperidone, ziprasidone, asenapine, paliperidone, cariprazine, and probably tamoxifen are efficacious in the treatment of acute manic episodes. It should be mentioned that haloperidol probably induces depression. It is unsatisfactory that there are no controlled data concerning the usefulness of electrocunvulsive treatment (ECT).
A significant problem for the everyday clinical practice is that the average clinician often utilizes the so-called “class effect” to easily navigate among therapeutic options. However, what needs to be stressed is that while antipsychotics seem to possess a class effect specific to the treatment of acute mania (possibly an antidopaminergic effect; Brugue and Vieta, 2007), there is no such effect in anticonvulsants concerning any phase of BD (Rosa et al., 2009; Fountoulakis et al., 2011b).
Comparison of Agents
Lithium vs others.
In 2 studies comparing lithium with valproate, the 2 agents were found to be equivalent. There was a tendency of valproate to manifest fewer adverse events and dropouts, but its signal for efficacy in RCTs might be driven by its effect in patients with mixed features (Freeman et al., 1992; Bowden et al., 1994). A similar finding restricting the efficacy of carbamazepine to an undefined subgroup of patients in contrast to a wider efficacy of lithium was reported by another study as well (Lerer et al., 1987). Overall the efficacy was similar to carbamazepine but with fewer adverse events (Okuma et al., 1990; Small et al., 1991). There has been a comparison of carbamazepine with lamotrigine that should be considered to be a failed study (Ichim et al., 2000). It should be noted however that lamotrigine is not an effective antimanic agent.
The comparison of lithium to chlorpromazine suggested that although chlorpromazine acts faster and might be more efficacious in more agitated patients, this might be due to sedation alone, while lithium has again a broader effect on the core manic symptomatology (Platman, 1970; Prien et al., 1972; Shopsin et al., 1975). In contrast, the comparison of haloperidol and lithium suggested that haloperidol had a stronger and more rapid effect, especially on behavior and motor activity but without sedation, while lithium acted more evenly and comprehensively on the entire range of manic symptomatology (Shopsin et al., 1975; Garfinkel et al., 1980).
Lithium was found to have equal efficacy to carbamazepine (Lerer et al., 1987; Okuma et al., 1990; Small et al., 1991), olanzapine (Berk et al., 1999; Niufan et al., 2008; Shafti, 2010), quetiapine (Bowden et al., 2005b; Li et al., 2008), and aripiprazole (Keck et al., 2009). In severely psychotic patients, it seems inferior to haloperidol (Shopsin et al., 1975; Garfinkel et al., 1980). Overall, lithium has a wider antimanic effect than valproate and carbamazepine but a weaker effect on psychotic symptoms and a slower onset of action in comparison with antipsychotics. Overall, lithium demonstrated a more favorable adverse effect profile in comparison with all other agents except aripiprazole and valproate.
Valproate vs others.
In comparison with lithium, valproate was less efficacious and with a tendency to cause fewer adverse events and dropouts, but its efficacy might be restricted to that specific group of patients with mixed features (Freeman et al., 1992; Bowden et al., 1994). In one small study, it was superior to carbamazepine and had a faster onset of action (Vasudev et al., 2000). In another study, it was superior to oxcarbazepine but with more frequent adverse events (Kakkar et al., 2009). It might be less efficacious in comparison with olanzapine and with a slower onset of action, but also with fewer adverse events (Tohen et al., 2002a, 2008b; Zajecka et al., 2002).
Carbamazepine vs others.
Carbamazepine was reported to be equally effective in comparison with lithium but with a higher rate of adverse events. Its efficacy appeared somewhat restricted to an undefined subgroup of patients in contrast to a broader spectrum of efficacy of lithium (Lerer et al., 1987; Okuma et al., 1990; Small et al., 1991). In another study carbamazepine was inferior to valproate and had a slower onset of action (Vasudev et al., 2000). In 2 other studies carbamazepine was found equal to chlorpromazine but with fewer adverse events (Okuma et al., 1979) and equal to haloperidol but with a slower onset of action (Brown et al., 1989).
Other antiepileptics.
There is one study on lamotrigine vs lithium that should be considered as failed probably because it was underpowered (Ichim et al., 2000). In another study, oxcarbazepine was found to be inferior to valproate but with fewer adverse events (Kakkar et al., 2009).
Haloperidol vs others.
The comparison of haloperidol with lithium suggested that haloperidol is more efficacious in severely psychotic patients and exerts its effect earlier, especially on behavior and motor activity but without sedation, while lithium acted more evenly and comprehensively on the entire range of manic symptomatology (Shopsin et al., 1975; Garfinkel et al., 1980). Haloperidol was found equally effective to carbamazepine but with a faster onset of action (Brown et al., 1989). Haloperidol had a faster onset of action than olanzapine but with more dropouts, and olanzapine was superior in the nonpsychotic patients. Both agents were equally effective in reducing the HDRS score in mixed patients and in patients with higher depressive scores. Switch to depression occurred significantly more rapidly with haloperidol than with olanzapine. More EPS were reported with haloperidol and more weight gain with olanzapine (Tohen et al., 2003b; Katagiri et al., 2012). Haloperidol was reported to be overall superior to quetiapine and more efficacious in psychotic patients. In contrast to quetiapine it had no effect on depressive symptoms. Haloperidol-treated patients had more dropouts and more EPS (McIntyre et al., 2005). It was reported as not superior to aripiprazole and did not improve the depressive symptoms measured with the MADRS. In comparison with aripiprazole, more haloperidol-treated patients switched to depression, more dropped out, and EPSs were more frequent with haloperidol (Vieta et al., 2005b; Young et al., 2009). Haloperidol was found similarly efficacious to risperidone (Segal et al., 1998; Smulevich et al., 2005) and superior to ziprasidone but also with more drop outs and adverse events (Vieta et al., 2010a). The comparison of 25 mg/d vs 5 mg/d haloperidol revealed that the higher haloperidol dosage produced greater improvement than did the low dose but with more side effects (Chou et al., 1999).
In summary, haloperidol was similar in efficacy as carbamazepine (Brown et al., 1989) and olanzapine (Tohen et al., 2003b; Katagiri et al., 2012), risperidone (Segal et al., 1998; Smulevich et al., 2005), and aripiprazole (Vieta et al., 2005b; Young et al., 2009). It was found to be superior to quetiapine (McIntyre et al., 2005) and ziprasidone (Vieta et al., 2010a) and in severely psychotic patients to lithium (Shopsin et al., 1975; Garfinkel et al., 1980). It acted faster in comparison with lithium (Shopsin et al., 1975; Garfinkel et al., 1980), carbamazepine (Brown et al., 1989), and olanzapine (Tohen et al., 2003b; Katagiri et al., 2012). Overall it demonstrated superior efficacy in psychotic patients but less improvement (if any) on depressive symptoms. It also showed more adverse events (especially EPS), switching to depression and dropouts more than the comparators.
Olanzapine vs others.
Olanzapine was reported to be equally effective to lithium but with more adverse events, mainly weight gain (Berk et al., 1999; Niufan et al., 2008; Shafti, 2010). It might be superior and faster acting in comparison with valproate (although this could be a function of dosage) but again with more adverse events (Tohen et al., 2002a, 2008b; Zajecka et al., 2002). It was found to be similar in efficacy to haloperidol but with a slower onset of action and fewer dropouts. The data suggest that during the acute phase both agents were equally effective in reducing the HDRS score in mixed patients and in patients with higher depressive scores. More EPSs were registered with haloperidol and more weight gain with olanzapine (Tohen et al., 2003b; Katagiri et al., 2012). Olanzapine was found superior to asenapine in manic and mixed patients and also significantly improved the MADRS score, that asenapine did not. Olanzapine-treated patients had more weight gain (McIntyre et al., 2009a, 2010b).
Olanzapine was found to have similar efficacy as risperidone in patients without psychotic features in terms of YMRS, HAM-D, and MADRS change. The 2 agents were also equal in the subgroup of rapid cycling patients. Fewer olanzapine-treated patients dropped out of the head-to-head comparison but there was more weight gain in the olanzapine group (Perlis et al., 2006b). Finally, an unpublished study of olanzapine vs ziprasidone (NCT00329108) was stopped prematurely due to poor recruitment (2009).
Quetiapine vs others.
Quetiapine is reported to be comparable with lithium but with more dropouts and adverse events (Bowden et al., 2005b; Li et al., 2008). Also it is reported to be inferior to haloperidol, with fewer dropouts and less frequent EPS, and also less efficacious in psychotic patients. In contrast to haloperidol it had an effect on depressive symptoms (McIntyre et al., 2005).
Quetiapine is reported to be equal to paliperidone and both agents had a similar effect in manic and mixed patients. Body weight increase was more frequent in the quetiapine group, but more patients with paliperidone switched to depression (Vieta et al., 2010b).
Other antipsychotics.
Chlorpromazine was found equal to pimozide with faster action, probably due to its greater sedative effect. Sedation was the side effect most frequent with chlorpromazine and EPS were more frequent with pimozide (Cookson et al., 1981).
The following studies have already been reported and discussed above; however, it is important to consider them again from a reverse angle. Risperidone was found equal to haloperidol (Segal et al., 1998; Smulevich et al., 2005) and olanzapine (Perlis et al., 2006b). Aripiprazole was found equal to lithium (Keck et al., 2009) and haloperidol (Vieta et al., 2005b; Young et al., 2009). Asenapine was found inferior to olanzapine (McIntyre et al., 2009a, 2010b) and paliperidone equal to quetiapine (Vieta et al., 2010b). There is one unpublished study comparing ziprasidone with olanzapine that did not report any results (2009) and another one finding it inferior to haloperidol (Vieta et al., 2010a). Finally, there are 2 studies comparing chlorpromazine with lithium (Platman, 1970; Prien et al., 1972) and one with carbamazepine (Okuma et al., 1979), suggesting equal efficacy.
Summary of the comparison of agents.
Overall, comparison studies suggest that the greater the efficacy the more frequent the adverse events are. Although there are no sufficient data to support a big difference between agents, it seems that antipsychotics and lithium are more efficacious than valproate and carbamazepine unless a loading strategy for these anticonvulsants is applied. Also it seems clear that antipsychotics act earlier in comparison with the other compounds. The effect on depressive symptoms is unclear, but it seems that haloperidol-treated patients might switch more often to depression.
Earlier studies suggested that lithium could be specifically useful against the more “classic” cases of euphoric mania, while antiepileptics might have a better efficacy for patients with mixed features and those with comorbidity. This is not supported by more recent data (Fountoulakis et al., 2012b). A factor that could have affected the results is the so-called lithium-discontinuation-related refractoriness (Post et al., 1992), because of that patients enrolled in RCTs could constitute a sample more refractory to lithium treatment than expected. However, the assumption for the existence of lithium-discontinuation-related refractoriness is not supported by studies reporting that even when samples enriched for lithium refractoriness were used, no inferiority of lithium to the other agent was documented (Bowden et al., 1994). Also a recent meta-analysis of all published cases concluded that there is not sufficient data to support such a concept (de Vries et al., 2013).
Combination and Add-On Treatment
Several studies examined the efficacy and safety of agents given not as monotherapy but combined treatments. The study samples range from patients being refractory to an initial treatment to drug-naive patients. In the first instance, an agent is used as adjunct or add-on therapy on a preexisting treatment to that the patient has shown unsatisfactory response. In the second instance the study tests a combination treatment against monotherapy and both agents are initiated simultaneously. Although essentially both designs provide information on how to treat patients with an unsatisfactory response to monotherapy, the conclusions and the generalizability might differ.
Combination Treatment
Adding valproate to First Generation Antipsychotics (FGAs; haloperidol or perazine in this study) produced higher response rates in manic patients (70% vs 46%) compared with FGA plus placebo (Muller-Oerlinghausen et al., 2000). Similarly, combination of lithium (600–1800 mg/d) and quetiapine XR (400–800 mg/d) was superior to quetiapine plus placebo (Bourin et al., 2014) in treating acute mania. Three studies that reported on combinations of mood stabilizing agents with haloperidol vs haloperidol monotherapy are equivocal as the outcome depended on the haloperidol dosage (Garfinkel et al., 1980; Klein et al., 1984; Chou et al., 1999).
Other studies reported on the efficacy of an antipsychotic agent and a mood stabilizer in comparison with mood stabilizer alone. In general, antipsychotic and carbamazepine combination is not superior to carbamazepine alone, primarily due to the effect of carbamazepine inducing the metabolism of antipsychotics in the combination group, thus resulting in lower plasma levels of antipsychotics. One 6-week international trial of olanzapine (10–30 mg/d) vs placebo add on to carbamazepine (400–1200 mg/d) was negative. In the olanzapine group, however, the triglyceride levels were significantly higher and potentially clinically significant weight gain occurred more frequently. Furthermore, carbamazepine significantly reduced olanzapine serum concentrations (Tohen et al., 2008a). Similarly, in another study, carbamazepine significantly reduced the serum levels of risperidone (Yatham et al., 2003) that contributed to the negative findings of this study on the primary efficacy measure.
Overall the data on the combination of lithium with other agents support the conclusion that the combinations of lithium with haloperidol, lorazepam, carbamazepine, tamoxifen, and allopurinol are superior to lithium alone, but not the combination of lithium plus ziprasidone or dipyridamole. Most of these combinations had more adverse events in comparison with monotherapy (Garfinkel et al., 1980; Lenox et al., 1992; Small et al., 1995; Weisler et al., 2003; Bowden, 2005; Machado-Vieira et al., 2008; Amrollahi et al., 2010). Adding allopurinol to treatment as usual was not more effective compared with treatment as usual (Weiser et al., 2014). On the contrary, positive results were reported by the addition of 400 mg/d celecoxib on valproate in nonrapid cycling and nonpsychotic patients (Arabzadeh et al., 2015) but negative when added on ECT (Kargar et al., 2015).
A number of trials investigated the combination of an atypical antipsychotic or other agents with addition of an agent on top of lithium or valproate, since these 2 constituted the backbone of the treatment of BD for decades. Overall the data are in support of combining lithium or valproate with asenapine, olanzapine, risperidone, haloperidol, and tamoxifen but negative concerning gabapentin and medroxyprogesterone (Pande et al., 2000; Sachs et al., 2002; Yatham et al., 2003; Kulkarni et al., 2006; Szegedi et al., 2012; Kulkarni et al., 2014; Xu et al., 2015b). The addition of folic acid to valproate has equivocal support (Behzadi et al., 2009) and the addition of omega-3 fatty acids has negative data (Chiu et al., 2005). Adding the herbal agent Free and Easy Wanderer Plus (FEWP) on carbamazepine was not better than carbamazepine alone, but it was in comparison with placebo while carbamazepine monotherapy was not. Technically it does not support the use of FEWP in acute mania, but a number of other interpretations also exist, for example that adding FEWP compensates for the drop in carbamazepine levels (Zhang et al., 2007). However, that study did not define an a-priori primary outcome and therefore its quality is low. Finally, one study suggested that the valnoctamide plus risperidone combination was more effective than risperidone alone (Bersudsky et al., 2010).
In summary, there are few but still important data suggesting that specific combinations are superior to monotherapy in nonrefractory or otherwise selected samples, although it is difficult to assess the quality of many study samples. Despite the very small number of trials and the problems with the data quality, one could generalize that the combination of an antipsychotic plus lithium or valproate is superior to lithium or valproate alone, with the caveat of greater side-effect burden. Tamoxifen and probably allopurinol are also valuable agents to use in combination with mood stabilizers.
Add-On Treatment
In patients refractory to haloperidol treatment, the addition of phenytoin has been shown to be beneficial (Mishory et al., 2000). In patients refractory to lithium, adding 600 to 1200 mg/d carbamazepine or oxcarbazepine improved the outcome (Juruena et al., 2009), but that study was of poor quality, questionable phase of the disorder and outcome, and without any a-priory defined primary outcome. Adding lovastatin on lithium was negative (Ghanizadeh et al., 2014).
In patients refractory to lithium, valproate, or carbamazepine, it is beneficial to add haloperidol, olanzapine, quetiapine, aripiprazole, or asenapine (Szegedi et al., 2012) (Sachs et al., 2002, 2004; Tohen et al., 2002b; Yatham et al., 2007; Vieta et al., 2008b) but not ziprasidone, topiramate, risperidone, or paliperidone (Roy Chengappa et al., 2006; Berwaerts et al., 2011; Sachs et al., 2012a, 2012b; Moosavi et al., 2014). One study that used a mixed population with some patients entering after a minimum of 2 weeks of mood stabilizer therapy, and others starting a mood stabilizer and risperidone in parallel, provided inconclusive data for risperidone (Yatham et al., 2003) as the results were likely confounded by the effects of carbamazepine on serum levels of risperidone. Allopurinol was not beneficial in patients refractory to lithium, valproic acid, carbamazepine, or atypical antipsychotic medications (Fan et al., 2012), although there are some data suggesting a beneficial effect on patients refractory to valproate (Jahangard et al., 2014). Adding the melatonin agonist ramelteon was also not efficacious in patients refractory to treatment as usual (McElroy et al., 2010b). There is only one sham-controlled trial of ECT as adjunctive treatment to chorpromazine (600 mg/d) in 30 acutely manic patients. That study supported the efficacy of ECT with a faster rate of improvement (Sikdar et al., 1994)
A recent placebo-controlled 4-week RCT in 180 acutely manic patients supported the efficacy and safety of the purinergic agents allopurinol (600 mg/d) and dipyridamole (200 mg/d) as adjunctive to lithium in acute bipolar mania (Machado-Vieira et al., 2008). Folic acid was also found to be useful as an adjunct to valproate in treating acute mania (Behzadi et al., 2009). There is one 5-week trial from Israel on 32 recently admitted manic inpatients that compared valnoctamide (600–1200 mg/d; n=15) vs placebo (n=17) on top of risperidone (1–6 mg/d). All medications were started at day 1. In all efficacy measures the valnoctamide plus risperidone combination was more effective than risperidone plus placebo from week 3 to week 5. Valnoctamide is an anticonvulsant analogue of valproate that does not undergo biotransformation to the corresponding free acid, and in mice it has been shown to be distinctly less teratogenic than valproate (Bersudsky et al., 2010). A pilot 8-week study in 21 acutely manic outpatients on the usefulness of adjunctive ramelteon in acute mania/mixed states failed (McElroy et al., 2010b), while another 2 on the cholinesterase inhibitor donepezil were negative (Eden Evins et al., 2006a; Chen et al., 2013).
Overall, the data in partial responders or refractory patients support the addition of specific antipsychotics to lithium or valproate and also the use of allopurinol and the combination of lithium with carbamazepine or maybe oxcarbazepine.
Posthoc Analyses and Meta-Analytic Studies
A very important posthoc analysis of individual patient data reported that patients with impaired insight (as measured with the use of item 11 of the YMRS) responded better; therefore treatment should be initiated immediately and the therapist should not wait until the patient gains sufficient insight (Welten et al., 2016).
Overall, posthoc and meta-analytic studies confirm the efficacy of specific agents vs placebo (Emilien et al., 1996; Yatham et al., 2004; Perlis et al., 2006a; Scherk et al., 2007; Tamayo et al., 2010) and also confirm the superiority of antipsychotics vs lithium, valproate, and carbamazepine both in terms of faster onset of action but also in terms of the overall outcome in the short-term treatment of acute mania. However, they also confirm that this higher efficacy comes with the cost of more frequent adverse events, mainly EPS, weight gain, and somnolence (Correll et al., 2010; Tarr et al., 2010). These conclusions should be received with caution, taking into consideration both the limitations of meta-analytical methods and the frequent conflicting results.
Haloperidol might be the fastest acting of all (Goikolea et al., 2013a) but also the most likely one to induce depression (Goikolea et al., 2013b). Olanzapine was efficacious against mixed episodes, depressive symptoms, and psychotic features as well as in rapid cycling patients (Baker et al., 2002; Baldessarini et al., 2003b; Chengappa et al., 2003; Suppes et al., 2005, 2008b). Quetiapine was proven efficacious for all YMRS individual items, depressive symptoms, and also against psychotic features (Vieta et al., 2005a). Risperidone vs placebo caused higher remission rate and the drop-out rate because lack of efficacy was lower, while the drop-out rate because of adverse events was similar to that of placebo (Gopal et al., 2005). Asenapine was efficacious against depressive symptoms (Szegedi et al., 2011) and mixed episodes (Azorin et al., 2013; McIntyre et al., 2013) and has an effect on the core symptoms of mania (Cazorla et al., 2013). Aripiprazole had no effect in patients aged >55 years but was effective against psychotic symptoms (Suppes et al., 2008b; Fountoulakis et al., 2009a; Sayyaparaju et al., 2014). Aripiprazole, lithium, and haloperidol overall are not efficacious against concomitant depressive features (Ostacher et al., 2015b). Ziprasidone was efficacious against dysphoric mania (Ketter et al., 2010; Stahl et al., 2010). The data of oxcarbazepine appear to be insufficient (Vasudev et al., 2011). A posthoc analysis of a lithium study (Bowden et al., 1994) confirmed the efficacy of lithium in classic manic but not mixed patients (Swann et al., 1997), while another posthoc study confirmed the lack of efficacy of eslicarbazepine although there seems to be some signal in the secondary outcomes (Grunze et al., 2015).
Meta-analytic studies also suggest that combination treatment is superior to monotherapy at the cost of more frequent adverse events; however, these meta-analyses do not distinguish between add-on and combination studies and populations (Scherk et al., 2007; Smith et al., 2007; Tarr et al., 2011; Ogawa et al., 2014). One meta-analysis reported that studies outside the United States had higher effect size and the baseline YMRS predicted the outcome (Tarr et al., 2011), probably because of a mathematical structural coupling effect (Fountoulakis and Kontis, 2012). Year of study publication was not associated with YMRS score change. Furthermore, the study size, number of study sites, YMRS score required for study entry, inclusion of patients with mixed mania or treatment resistance, and inclusion of inpatients vs outpatients had no significant influence on the outcome (Tarr et al., 2011).
Two recent meta-analyses attempted to rank antimanic agents according to efficacy. The first one utilized the method of multiple-treatments meta-analysis and reported that the ranking in terms of efficacy was haloperidol, risperidone, olanzapine, lithium, quetiapine, aripiprazole, carbamazepine, asenapine, valproate, and ziprasidone. According to that meta-analysis, overall, antipsychotics were significantly more effective than mood stabilizers; however, the results of that analysis do not fully support such a conclusion (Cipriani et al., 2011). This meta-analysis has been criticized both concerning the overall methodology but also concerning the incomplete list of RCTs that was utilized (Fountoulakis and Siamouli, 2012). A more balanced meta-analysis confirmed that the response to antipsychotics was greater and more rapid in comparison with lithium, valproate, or carbamazepine, but it did not confirm any difference between haloperidol and second generation antipsychotics (Yildiz et al., 2010). A more recent network meta analysis did not support the superiority of any agent vs another except for risperidone vs aripiprazole and valproate (Yildiz et al., 2015).
A meta-analysis that pooled data from 9 randomized, double-blind, placebo-controlled, acute studies of ziprasidone reported that the discontinuation rate due to adverse events or 7% or greater weight gain between ziprasidone and placebo was not significant for all psychiatric conditions. In acute mania the risk for akathisia with ziprasidone had a number needed to harm (NNH)=12, the risk for overall EPS had a NNH=12, and the reported somnolence had NNH=7 (Gao et al., 2013). Finally, a recent network meta-analysis reported that aripiprazole, olanzapine, quetiapine, risperidone, and valproate had less all-cause discontinuation rates than placebo and that there is a similar efficacy profile for haloperidol, second-generation antipsychotics, and mood stabilizers (Yildiz et al., 2014) while a meta-analysis of combination studies confirmed the higher rate of adverse events in comparison with monotherapy (Galling et al., 2015).
The analysis of the data concerning the usefulness of the cholinesterase inhibitors galantamine and donepezil as well as the glutamate receptor antagonist memantine was negative (Veronese et al., 2016).
Acute Bipolar Depression
Bipolar depression is not well studied, and the common practice among clinicians is to extrapolate the clinical data and wisdom from the treatment of unipolar to bipolar depression. However, the clinical trials that examined the efficacy of various agents have raised questions about the validity of such strategy.
The agents are listed below in a historical sequence with lithium and anticonvulsants first, then antidepressants, and finally with antipsychotics on the basis of the year of the first study they were investigated.
The data on monotherapy and combination treatment for acute bipolar depression and its special characteristics are shown in Table 3.
Table 3.
Acute Depression Treatment Phase, Grading on Basis of Efficacy (Treatment Phase up to 12 Weeks)
| Monotherapy | Combination | Anxiety | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Agent/modality (alphabetical order) | Overall | BD-I | BD-II | Depressive core | MS | Cbz | Lam | Li | Val | |
| Agomelatine | - | - | - | - | 5 | - | - | 5 | 5 | - |
| Aripiprazole | 3 | 3 | - | - | - | - | - | 5 | - | - |
| Armodafinil | - | - | - | - | 4 | - | - | - | - | - |
| Bupropion | - | - | - | - | 5 | - | - | - | - | - |
| Carbamazepine | 3 | - | - | - | - | - | - | - | - | - |
| Celecoxib | - | - | - | - | 5 | - | - | - | - | - |
| Donepezil | 5 | - | - | - | - | - | - | 5 | - | - |
| Escitalopram | - | - | 2 | - | - | - | - | - | - | - |
| Fluoxetine | 2 | - | 3 | - | - | - | - | 4 | - | - |
| FEWP | - | - | - | - | - | 4 | - | - | - | - |
| Gabapentin | 5 | - | - | - | - | - | - | - | - | - |
| Imipramine | 3 | - | - | - | - | - | - | 5 | - | - |
| Ketamine | - | - | - | - | 2 | - | - | - | - | - |
| Lamotrigine | 3 | 3 | 3 | 3 | - | - | - | 2 | - | - |
| Levetiracetam | - | - | - | - | 5 | - | - | - | - | - |
| Levothyroxine (L-T4) | - | - | - | - | 4 | - | - | - | - | - |
| Lisdexamfetamine | - | - | - | - | 5 | - | - | - | - | - |
| Lithium | 4 | - | - | - | - | - | 2 | - | - | 5 |
| L-sulpiride | - | - | - | - | - | - | - | 3 | - | - |
| Lurasidone | 2 | 2 | - | 3 | 2 | - | - | - | - | 3 |
| Memantine | - | - | - | - | - | - | 5 | - | - | - |
| Modafinil | - | - | - | - | 2 | - | - | - | - | - |
| OFC | 2 | 2 | - | 3 | - | - | - | - | - | - |
| Olanzapine | 1 | 1 | - | 3 | - | - | - | - | - | - |
| Oxcarbazepine | - | - | - | - | - | - | - | 4 | - | - |
| Paroxetine | 5 | 5 | 5 | - | 5 | Neg | - | 5 | 5 | 3 |
| Phenelzin | 3 | - | - | - | - | - | - | - | - | - |
| Pioglitazone | - | - | - | - | - | - | - | 2 | - | - |
| Pramipexole | - | - | - | - | 2 | - | - | - | - | - |
| Pregnenolone | - | - | - | - | 5 | - | - | - | - | - |
| Quetiapine | 1 | 3 | 3 | 3 | - | - | - | - | - | 3 |
| Risperidone | - | - | - | - | 5 | - | - | - | - | 5 |
| TMS | 5 | - | - | - | - | - | - | - | - | - |
| Tranylcypromine | 4 | 4 | 4 | - | - | - | - | - | - | - |
| Valproate | 3 | 3 | 5 | 3 | - | - | - | - | - | 3 |
| Venlafaxine | 4 | 4 | 4 | - | - | - | - | - | - | - |
| Ziprasidone | 5 | 5 | - | - | 5 | - | 5 | 5 | 5 | 5 |
Abbreviations: -, no data; Cbz, carbamazepine; ECT, electroconvulsive therapy; FEWP, Free and Easy Wanderer Plus; Lam, lamotrigine; Li, lithium; MS, Mood Stabilizer; OFC, Olanzapine Fluoxetine Combination; TMS, transcranial magnetic stimulation; Val, valproate.
The treatment options are rated according to the rating system shown in Table 1.
Monotherapy
Lithium.
The earlier studies on the efficacy of lithium against bipolar depression provided some positive data but are difficult to interpret (Goodwin et al., 1969, 1972; Greenspan et al., 1970; Stokes et al., 1971; Noyes and Dempsey, 1974; Noyes et al., 1974; Baron et al., 1975; Mendels, 1976; Donnelly et al., 1978; Srisurapanont et al., 1995). There is only one modern and rigorously conducted RCT (EMBOLDEN I) and it was negative for lithium while positive for quetiapine. While in this particular study the mean lithium serum levels were 0.61 mEq/lt, with 34.9% of patients having levels <0.6 mEq/lt, a posthoc analysis reported that the results were negative also in patients with lithium levels >0.8 mEq/lt and also in patients who completed the study. Furthermore, lithium level did not correlate with change in depression rating scores (Young et al., 2010).
Antiepileptics.
Valproate
There are 3 small positive trials (Davis et al., 2005; Ghaemi et al., 2007; Muzina et al., 2010) and one failed (Sachs et al., 2001), that is not published and can be assessed only through 2 meta-analytic papers (Bond et al., 2010; Smith et al., 2010). Taken together, these studies suggest that there are some data (though somewhat inconsistent and not sufficient), coming from small trials supporting the efficacy of valproate (titrated up to 2500 mg/d) in bipolar depression, especially in BD-I patients and on the core symptoms of depression. There is possibly some efficacy against concomitant anxiety.
Carbamazepine
The old, small withdrawal studies concerning carbamazepine efficacy against bipolar depression were positive (Ballenger and Post, 1980; Post et al., 1983, 1986) but also suggested that plasma levels do not correlate with the treatment effect (Post et al., 1983). A more recent 12-week double-blind, randomized, placebo-controlled study from China had equivocal results (Zhang et al., 2007).
Lamotrigine
There are 5 trials that investigated the efficacy and safety of lamotrigine in the treatment of acute bipolar depression (SCA100223/NCT00274677, SCA30924/NCT00056277, SCA40910, SCAA2010, and SCAB2001). One included BD-II patients alone and one a mixed population of BD-I and BD-II patients. All were negative concerning the primary outcome (Calabrese et al., 1999; Goldsmith et al., 2003; Ostacher et al., 2008), although in one study lamotrigine separated from placebo on MADRS, an important secondary outcome measure (Calabrese et al., 1999). A small double-blind, randomized study with crossover series of three 6-week monotherapy evaluations in a mixed unipolar-bipolar population reported that lamotrigine was superior to placebo (Frye et al., 2000). Overall the data are negative concerning the efficacy of lamotrigine in acute bipolar depression, although the presence of a weak signal cannot be ruled out.
Antidepressant Monotherapy
Despite the fact that antidepressants have established efficacy in unipolar depression, that defines them as a class of drugs that includes different kinds of molecules, such a “class effect” does not appear to be present for bipolar depression (Fountoulakis et al., 2011b). Although the data are problematic, the use of antidepressants is neither encouraged nor prohibited by all treatment algorithms, that however consistently advise the concomitant use of an antimanic agent. The current view is that antidepressant monotherapy should not be used in bipolar depression (Vieta, 2014). Older placebo-controlled studies were mostly positive but difficult to judge on the basis of modern criteria and understanding of methodology.
An early study reported superiority of tranylcypromine vs placebo in anergically depressed patients and suggested that tranylcypromine could be efficacious against bipolar depression since anergic depression most typically occurs in BD and in pseudounipolar affective illnesses (Himmelhoch et al., 1982). However, the methodology of this study has been criticized.
The first trial reported that fluoxetine and imipramine were efficacious vs placebo, but the interpretation of the results of this study is complicated by the concomitant use of lithium, especially in the fluoxetine group (Cohn et al., 1989). A second small trial was negative for fluoxetine and olanzapine monotherapy and also for the olanzapine-fluoxetine combination (OFC) (Amsterdam and Shults, 2005a). Another small placebo-controlled, cross-over study lasting 9 months in 10 BD-II depressed patients suggested that escitalopram might be better than placebo as monotherapy for depression and without worsening of illness course (Parker et al., 2006). The only properly conducted study on a sample of adequate size was an international trial on 740 patients with bipolar depression (both BD-I and BD-II). This study was negative for paroxetine 20 mg/d while it was positive for quetiapine. However, paroxetine produced a significant improvement in anxiety in terms of change of HAM-A scale score from baseline but was not efficacious concerning depressive symptoms in any subgroup of patients. The most frequent adverse events were dry mouth, sedation, headache, insomnia, and nausea with paroxetine treatment (McElroy et al., 2010c).
In conclusion, given that the efficacy data are conflicting along with concerns about manic/hypomanic switch, the use of antidepressant monotherapy is strongly discouraged.
Antipsychotics
Olanzapine.
An international trial supported the superiority of olanzapine (5–20 mg/d) vs placebo in the treatment of bipolar depression. However, olanzapine monotherapy was proven inferior to OFC and furthermore, the analysis of individual MADRS items suggested that in contrast with OFC, olanzapine monotherapy had no effect on the core symptoms of depression (Tohen et al., 2003c). Also, a further small study was underpowered and negative (Amsterdam and Shults, 2005a). Another small study was positive (Wang et al., 2014). It is important to note that to demonstrate a true antidepressive effect, an effect on the “core items” of depression should be demonstrated (Bech, 2001; Lecrubier and Bech, 2007). To answer this question, another trial was conducted and the results again suggested that olanzapine (5–20 mg/d) was superior to placebo, but again no effect of olanzapine was observed on the core depressive symptoms according to LOCF analysis but surprisingly MMRM analysis showed a significant effect on core symptoms (Tohen et al., 2012). Overall, while olanzapine separated from placebo in 2 large clinical trials of bipolar depression, the data concerning its efficacy on the core symptoms of depression are equivocal.
Quetiapine.
Overall, there are 6 studies concerning the efficacy of quetiapine in bipolar depression. All of them were positive. Quetiapine IR or XR is reported to be efficacious at dosages of both 300 and 600 mg/d. It is important to note that quetiapine had a similar efficacy in BD-I and BD-II patients as well as in rapid cycling, and it significantly improved all the MADRS items corresponding to the core symptoms of depression and also improved concomitant anxiety (Calabrese et al., 2005b; Thase et al., 2006; McElroy et al., 2010c; Suppes et al., 2010; Young et al., 2010; Li et al., 2016)
Aripiprazole.
Two identically designed, 8-week, multicentre, randomized, double-blind, placebo-controlled studies (CN138-096 and CN138-146) to evaluate the efficacy and safety of aripiprazole monotherapy in depressed BD-I outpatients without psychotic features were both negative for aripiprazole (Thase et al., 2008). It has been argued that the failure of these 2 trials was due to the “catching up” of the placebo group after week 6 rather than because of a lack of efficacy of aripiprazole; however, at endpoint the placebo response in terms of MADRS score change in the aripiprazole studies (-10.6 and -11.5) was similar to what was observed also in the quetiapine studies (from -10.3 to -11.9), while the aripiprazole response (-11.9 and -12.3) was clearly lower to the response observed with quetiapine (from -15.4 to -17.4). Another confounding factor in these studies was that transient use of hypnotics was permitted but not after 4 weeks into the trial.
Ziprasidone.
There are 2 negative trials (NCT00141271 and (NCT00282464) concerning ziprasidone, that were published in a single paper (Lombardo et al., 2012). The placebo responses in these trials were >50%, that might have contributed to negative results. One trial of ziprasidone in bipolar spectrum depressed patients was negative (Patkar et al., 2015).
Lurasidone.
One 6-week trial in bipolar depressed patients without psychotic features reported that lurasidone (20–60 mg/d or 80–120 mg/d) was superior to placebo. Lurasidone had an effect on the core symptoms of depression. Both lurasidone groups also experienced significant improvements compared with placebo in anxiety symptoms and in patient-reported measures of quality of life and functional impairment (Loebel et al., 2014a). As this was a 6-week study, and having in mind the negative findings at endpoint (week 8) for aripiprazole while the data was positive at week 6, one might be cautious concerning the interpretation of the lurasidone data. However, the magnitude of improvement and the absolute values of lurasidone and placebo-induced change in the MADRS score argue in favor of lurasidone.
Other agents and treatment options.
There is a small number of early studies on very small samples concerning the α2-adrenergic agonist clonidine, the α2-adrenergic antagonist idaxozan, and Thyrotropin-releasing hormone (Kastin et al., 1972; Jimerson et al., 1980; Osman et al., 1989). A trial concerning the usefulness of ECT has been announced (Kessler et al., 2010), but its results have not been published until now. Three other uncontrolled trials suggested that bipolar depressives respond to ECT, and conflicting results exist as to whether unipolar or bipolar depression respond better although probably to a lesser extent in comparison with unipolars (Daly et al., 2001; Medda et al., 2009; Bailine et al., 2010). A recent study showed ECT to be superior to a pharmacotherapy algorithm (Schoeyen et al., 2015). There is one negative study of rTMS (Nahas et al., 2003). There is a small positive study on the usefulness of cranial electrotherapy stimulation in BD-II depression (McClure et al., 2015).
Comparison of Treatment Options
Since only a limited number of options for the treatment of bipolar depression exist, comparison studies are limited and often they compare agents with unproven efficacy. Some early studies were too small and are problematic concerning their methodology (Coppen et al., 1972; Kessell and Holt, 1975; Aberg-Wistedt, 1982). Overall the comparison data are sparse and they suggest antidepressants are equal in efficacy but with a different adverse events profile (Baumhackl et al., 1989; Cohn et al., 1989; Himmelhoch et al., 1991; Grossman et al., 1999; Amsterdam and Garcia-Espana, 2000; Silverstone, 2001; Vieta et al., 2002). Clomipramine might be more efficacious than imipramine in refractory BD depressed patients (Thase et al., 1992).
However, the efficacy of antidepressants should be considered in combination with the negative monotherapy data for paroxetine. The frequent use of concomitant mood stabilizers as “background” medication complicates the interpretation of results. OFC is superior to olanzapine alone (Tohen et al., 2003c) and to lamotrigine (Brown et al., 2006) and has an effect on the core symptoms of depression. The comparison of paroxetine with venlafaxine suggests a higher switching risk for patients treated with venlafaxine (Vieta et al., 2002). The relatively higher risk of treatment emergent affective switches with venlafaxine compared with sertraline or bupropion has also been reported (Post et al., 2006). However, a more recent study reported that venlafaxine was equal to lithium and without any increase in the switch rate (Lorenzo-Luaces et al., 2016).
Combination and add-on treatment.
Combination treatment
There is one trial in BD-I depressed patients that suggested that the OFC (6 and 25, 6 and 50, or 12 and 50 mg/d) was superior both to olanzapine monotherapy and to placebo. The OFC arm was relatively small (only 86 patients) and this was one of the limitations of the study. The analysis of individual MADRS items suggested that OFC had an effect on the core symptoms of depression. In comparison with placebo and olanzapine, the OFC arm also had a lower number of inpatients, less frequent psychotic features, more rapid cycling (that may translate in higher rates of “spontaneous remission”), and lower number of centers. All these could translate into better response and limit interpretation (Tohen et al., 2003c). Another small study was negative but also underpowered to detect any treatment effect (Amsterdam and Shults, 2005a). A second study from the United States (STEP-BD) utilized a combination treatment by adding paroxetine or bupropion or placebo to a mood stabilizer. The results suggested that the 2 antidepressant arms did not perform significantly better than placebo on top of a mood stabilizer after 26 weeks in terms of recovery rates or transient remission. The switch rates were similar as was the drop-out rate (Sachs et al., 2007), and neither response to treatment nor switching were dose dependent (Tada et al., 2015). The third trial was a 12-week double-blind, randomized, placebo-controlled study from China that reported that carbamazepine plus the herbal FEWP (36 g/d) was superior to carbamazepine alone and to placebo, but the quality of this study is considered to be low because there was no a-priori defined primary outcome (Zhang et al., 2007).
In a small study, 21 patients with acute BD-II depression, being on therapeutic levels of lithium or valproate, were randomly assigned to treatment with the dopamine D2/D3 antagonist pramipexole (n=10) or placebo (n=11) for 6 weeks. All subjects except for one in each group completed the study. There was a superiority of pramipexole in terms of response (60% vs 9%; P=.02). One subject on pramipexole and 2 on placebo developed hypomanic symptoms (Zarate et al., 2004). Another small study randomized 17 BD depressed patients to receive adjunctive inositol or placebo for 6 weeks on lithium or valproate. The results were numerically in favor of inositol in terms of response rates (44% vs 0%; P=.053) (Eden Evins et al., 2006b).
Add-on treatment
Overall, the data suggest that in bipolar depressed patients who experience depression while under lithium treatment, it is appropriate to add lamotrigine (van der Loos et al., 2009, 2010, 2011), the D2 antagonist L-sulpiride (Bocchetta et al., 1993), or maybe oxcarbazepine (Juruena et al., 2009) but not imipramine (Nemeroff et al., 2001). The data on adding paroxetine and amitriptyline are equivocal (Bocchetta et al., 1993; Bauer et al., 1999a; Pilhatsch et al., 2010; van der Loos et al., 2010). Imipramine and venlafaxine might pose the patients at an increased risk of switching to the opposite pole without any visible therapeutic benefit in comparison with other antidepressants (Nemeroff et al., 2001; Vieta et al., 2002)
In BD patients experiencing depression during treatment with lithium or valproate, ketamine or lurasidone could be added. Lurasidone also improves anxiety and ketamine improves suicidality in these patients. Response to a single ketamine infusion appears within minutes but does not last more than 3 to 4 days (Young et al., 2000; Diazgranados et al., 2010; Zarate et al., 2012; Loebel et al., 2014b; Xu et al., 2015a). However, there is one unpublished failed study with lurasidone as add-on to lithum or valproate (Suppes et al., 2013; Sanford and Dhillon, 2015). A small placebo-controlled adjunctive study of aripiprazole to lithium and citalopram was negative. However, the study was underpowered and the study sample was too small to detect any differences (Quante et al., 2010).
The data on the options to treat BD patients who experience a depressed episode during treatment with mood stabilizers suggest that it is not appropriate to add ziprasidone (Sachs et al., 2011), and the data are also negative also concerning bipolar spectrum depressed patients (Patkar et al., 2015). The antiepileptic agent topiramate and levitiracetam should be avoided because there is a risk of worsening depression and inducing suicidality (Fountoulakis et al., 2012c, 2015; Siamouli et al., 2014). Imipramine and venlafaxine increased the risk of switching to the opposite pole without any visible therapeutic benefits in comparison with other antidepressants (Sachs et al., 1994, 2011; Post et al., 2001, 2006; Shelton and Stahl, 2004; Schaffer et al., 2006; Altshuler et al., 2009; Saricicek et al., 2010).
The data are negative concerning the addition of memantine to lamotrigine (Anand et al., 2012) or valproate (Lee et al., 2014a, 2014b), ketamine to ECT (Abdallah et al., 2012), lisdexamfetamine to treatment as usual (McElroy et al., 2015), and the melatonergic antidepressant agomelatine to lithium or valproate (Yatham et al., 2016).
Another placebo-controlled study in 85 bipolar depressive patients with adjunctive modafinil (a wake-promoting agent; mean dose 177 mg/d) demonstrated improved outcomes of bipolar depression without switching to mania or hypomania. Both the response and remission rates were significantly higher in the modafinil group (44% and 39%) compared with the placebo group (23% and 18%) (Frye et al., 2007). Although that study did not report a higher risk for manic switches, it has been reported that modafinil could cause subclinical switches (Fountoulakis et al., 2008c). One published study for the treatment of acute BD-I depression with adjunct armodafinil (the longer lasting isomer of modafinil; dosage 150 mg/d; n=128) on lithium, valproate, or olanzapine was positive (Calabrese et al., 2010, 2014). However 2 other studies were reported to be negative (Ostacher, 2014; Ketter et al., 2015). One small study on the efficacy of the antidiabetic agent pioglitazone as add-on to lithium in bipolar patients without diabetes mellitus was positive (Zeinoddini et al., 2015). A trial of celecoxib (400 mg/d) did not support its efficacy as an adjunct in the treatment of depressive or mixed episodes (Nery et al., 2008). One study with add-on pregnenolone (titrated to 500mg/d) was negative (Brown et al., 2014), while a very small placebo controlled trial without an a-priori defined primary outcome suggested that adding supraphysiologic doses of levothyroxine (L-T4) to a mood stabilizer improves the outcome (Bauer et al., 2016).
Some data support the usefulness of omega-3 fatty acids as adjunctive therapy in bipolar depression but not mania, but the data are conflicting and inconclusive (Stoll et al., 1999; Chiu et al., 2005; Frangou et al., 2006; Keck et al., 2006b; Frangou et al., 2007; Murphy et al., 2012; Sarris et al., 2012; Sylvia et al., 2013)
Although there is a wide consensus on the usefulness of ECT both against acute mania and acute bipolar depression and in refractory cases, controlled hard data are scant (Loo et al., 2010). A recent study suggests that ECT may be more effective than pharmacotherapy for treatment-resistant bipolar depression (Schoeyen et al., 2015). Another potential tool could be TMS; however, it has been poorly investigated in bipolar depression (Dell’Osso et al., 2009). Sleep deprivation and other noninvasive circadian-related interventions could be useful add-on treatments to accelerate and sustain the antidepressant response (Wu et al., 2009). One study on bright light therapy in bipolar depression was negative (Dauphinais et al., 2012).
Posthoc, Review, and Meta-Analytic Studies
Posthoc analyses of controlled trials.
A posthoc analysis of the OFC and olanzapine data (Tohen et al., 2003c) reported patients with bipolar depression receiving olanzapine or OFC had greater improvement in health-related quality of life than those receiving placebo, and additionally OFC treatment is superior to olanzapine alone (Shi et al., 2004b). A second posthoc analysis of the same data set data reported that the beneficial effect was already present at day 7. A number of alternative methods of analysis of the data (pattern analysis, survival analysis, and mixed-effects regression analysis) confirmed the superiority of both olanzapine and OFC vs placebo (Dube et al., 2007). A subanalysis of Japanese subpopulation from the second olanzapine study (Tohen et al., 2012) further supported the efficacy of olanzapine in the treatment of bipolar depression (Katagiri et al., 2013). A pooled analysis of the 2 olanzapine studies (Tohen et al., 2003c, 2012) that utilized last observation carried forward data supported the efficacy of olanzapine on the core depressive items (Tohen et al., 2013).
One posthoc analysis included 2 quetiapine trials (Calabrese et al., 2005b; Thase et al., 2006) and confirmed the efficacy of quetiapine as monotherapy, in comparison with placebo, for the treatment of acute depressive episodes in BD-II disorder (Suppes et al., 2008a). Another posthoc analysis of only one of these trials (Calabrese et al., 2005b) concluded that quetiapine significantly improved quality of life from week 4 onwards as well as quality of sleep (Endicott et al., 2007). A further posthoc analysis of the same study reported that the NNT was 5 for both response and remission for quetiapine (600 and 300 mg/d) compared with placebo (Cookson et al., 2007). Another posthoc analysis of these 2 quetiapine trials reported that quetiapine was effective in BD-I depressed patients already from week 1 onwards (Weisler et al., 2008).
One posthoc analysis of pooled data from 2 similarly designed trials who assessed the impact of aripiprazole monotherapy (Thase et al., 2008) reported that at endpoint aripiprazole was not efficacious in the more severely depressed patients (Thase et al., 2012). The posthoc analysis of the 2 negative unpublished ziprasidone monotherapy trials confirmed that ziprasidone did not show superiority over placebo at week 6 in the treatment of bipolar depression and was not efficacious in the more or less severely depressed patients (Lombardo et al., 2012).
A posthoc analysis of a 6-week trial of imipramine, phenelzine or placebo reported that BD-II depressive patients respond in a similar way to unipolar patients (Agosti and Stewart, 2007).
An interesting posthoc analysis of the lurasidone studies developed a mathematical model for the drug and placebo responses and trajectories (Chapel et al., 2016), while a meta-analysis of combination studies confirmed the higher rate of adverse events in comparison with monotherapy (Galling et al., 2015). A third analysis suggested a beneficial effect of lurasidone on functioning that was partially mediated through the improvement of depressive symptoms and partially a direct effect (Rajagopalan et al., 2016).
The meta-analysis of ketamine studies support its efficacy but suggest the data are conflicting as to whether the therapeutic effect extends beyond day 4 and up to day 7 (Lee et al., 2015; Romeo et al., 2015).
Review and meta-analytic studies.
A review confirmed that lamotrigine had only negative data concerning the primary outcome in acute bipolar depression (Amann et al., 2010); however, there was some kind of positive signal in some of the secondary outcomes. The pooling of raw data from the lamotrigine studies found a significant effect in terms of response (HAM-D score, RR=1.27, 95% CI 1.09–1.47, P=.002) and remission rates (MADRS score, RR=1.21, 95% CI 1.03–1.42, P=.021). There was a significant change in the MADRS total score from baseline (P=.04) but not in the HAM-D (P=.08). Baseline severity of depression seemed to play a significant role, and lamotrigine was superior to placebo in patients with HAM-D score >24 (RR=1.47, P=.001) but not in those with HAM-D score ≤24 (RR=1.07, P=.445). This meta-analysis reported an admixture of contradictory results, with lamotrigine being efficacious according to one outcome but not according to another (e.g., according to MADRS but not to HAM-D and vice versa). Also the interaction by severity was because of a higher response rate in the placebo group in the moderately ill patients, while the response rate to lamotrigine was independent of severity (Geddes et al., 2009). The efficacy of carbamazepine was supported by 2 other reviews (Srisurapanont et al., 1995; Yatham et al., 1997).
A number of meta-analyses that were published later reported that only quetiapine, OFC, lurasidone, and to a lesser extend olanzapine monotherapy exert efficacy in the treatment of bipolar depression. They also reported negative results for lamotrigine and aripiprazole, lithium as well as for adjunctive inositol (Cruz et al., 2010; Kemp et al., 2010; Tamayo et al., 2010; Vieta et al., 2010c; De Fruyt et al., 2011, 2012; Gao et al., 2011; Silva et al., 2013; Citrome et al., 2014; Mukai et al., 2014; Suttajit et al., 2014). Also, it was reported that patients who do not respond in the first 2 weeks of treatment are unlikely to respond eventually and would benefit from a change in treatment (Kemp et al., 2010).
Two meta-analyses using identical studies suggested there is some weak efficacy for valproate (Bond et al., 2010; Smith et al., 2010) and one suggested the same for aripiprazole (Fountoulakis et al., 2011a). Another one suggested that treatment with ziprasidone increases the risk for akathisia and reported somnolence that seemed to be dose dependent (Gao et al., 2013). There are 3 meta-analysis with conflicting conclusions concerning the efficacy of antidepressants (Gijsman et al., 2004; Sidor and Macqueen, 2010, 2012; Vazquez et al., 2013) However, it is clear that a class effect is not present concerning antidepressants in bipolar depression (Fountoulakis et al., 2011b). Another meta-analysis suggested that mood stabilizer monotherapy is efficacious but the addition of an antidepressant does not increase efficacy (Van Lieshout and MacQueen, 2010).
One meta-analysis that focused on depressed patients with BD-II reported that quetiapine had compelling evidence supporting its efficacy, while there was some support for the efficacy of lithium, antidepressants, and pramipexole. The data for lamotrigine were equivocal (Swartz and Thase, 2011), while some data suggest the efficacy of stimulants, especially modafinil (Corp et al., 2014), ketamine (Fond et al., 2014; McGirr et al., 2014), and antiinflammatory agents compared with conventional therapy alone in the treatment of bipolar depression (Rosenblat et al., 2016).
Two reviews investigated the issue of the treatment of refractory bipolar depression and concluded that the available hard data are extremely scarce and most of the strategies remain essentially experimental; however, there seem to be some that are potentially efficacious and promising (Aan Het Rot et al., 2012; Sienaert et al., 2013).
One meta-analysis compared the efficacy of ECT in unipolar vs bipolar depression and identified 6 relevant studies. It reported a similar rate of response in both disorders (50.9% vs 53.2%) (Dierckx et al., 2012).
Finally, a meta-analysis reported that the probability of receiving placebo, baseline illness severity, and trial duration correlate with placebo response rates and/or clinical trial outcome in RCTs of pharmacotherapy for bipolar depression (Nierenberg et al., 2015), while another one was negative concerning the usefulness of galantamine, donepezil, and memantine (Veronese et al., 2016).
Maintenance Treatment
The efficacy data for monotherapy for the maintenance treatment phase are shown in Table 4. The data concerning the combination treatment are shown in Table 5.
Table 4.
Monotherapy Treatment during the Maintenance Phase, Grading on Basis of Efficacy
| Agent/modality (alphabetical order) | Index episode | Enriched sample | Any episode | Manic | Depressive |
|---|---|---|---|---|---|
| Aripiprazole | m* | Yes | - | 1 | 5 |
| Carbamazepine | - | - | 4 | 4 | 4 |
| Fluoxetine | d | Yes | - | - | 2 |
| Imipramine | d | ? | 5 | 5 | 5 |
| Lamotrigine | m/d | Yes | 1 | 3 | 1 |
| Lithium | m/d | No | 1 | 1 | 3 |
| Olanzapine | m | Yes/No | 1 | 1 | 1 |
| Paliperidone | m | Yes | 1 | 2 | 5 |
| Quetiapine | m/d | Yes | 2 | 2 | 2 |
| Risperidone, LAI | m | Yes | 1 | 1 | 5 |
| Valproate | m | Yes | 4 | 4 | 3 |
Abbreviations: -, no data; m, mania/mixed; d, depression; m/d, both mania and depression.
The treatment options are rated according to the rating system shown in Table 1. Enriched sample: the sample is enriched on the basis of remission after treatment with the agent under consideration during the acute phase (index episode).
Table 5.
Combination treatment during the maintenance phase, grading on basis of efficacy.
| Overall | Manic | Depressive | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Agent/modality (alphabetical order) | Index episode | Enriched sample | MS | Lam | Li | Val | MS | Lam | Li | MS | Lam | Li | Val |
| Aripiprazole | m* | Yes | 2 | 5 | - | 5 | 2 | 5 | - | 5 | 5 | - | - |
| CBT | D | No | 2 | - | - | - | - | - | - | - | - | - | - |
| Gabapentin | - | - | - | - | - | - | 4 | - | - | - | - | - | - |
| Imipramine | D | ? | - | - | 5 | - | - | - | - | - | - | - | |
| Lamotrigine | m/d | Yes | - | - | 4 | - | - | - | - | - | - | 5 | |
| Lithium | m/d | No | - | 4 | - | - | - | - | - | - | - | - | - |
| Memantine | - | - | - | - | - | 5 | - | - | - | - | - | - | - |
| N-acetyl cysteine | D | Yes | 4 | - | - | - | - | - | - | - | - | - | - |
| Olanzapine | M | Yes/No | 4 | - | - | - | - | - | - | - | - | - | - |
| Oxcarbazepine | - | - | - | - | 5 | - | - | - | 5 | - | - | 5 | - |
| Paroxetine | - | - | 3 | - | - | - | - | - | - | 3 | - | - | - |
| Perphenazine | m | Yes | 5 | - | - | - | - | - | - | - | - | - | - |
| Phenytoin | euth | No | 2 | - | - | - | - | - | - | - | - | - | - |
| Quetiapine | m/d | Yes | 1 | - | - | - | 1 | - | - | 1 | - | - | - |
| Risperidone, long-acting injectable | m | Yes | 2 | - | - | - | 2 | - | - | - | - | - | - |
| Valproate | m | Yes | - | - | - | - | - | - | - | - | 5 | - | - |
| Ziprasidone | m | Yes | 2 | - | - | - | - | - | - | - | - | - | - |
Abbreviations: -, no data; CBT, cognitive behavioral therapy; Cbz, carbamazepine; d, depression; Lam: Lamotrigine; Li: Lithium; m, mania/mixed; m/d, both mania and depression; MS, mood stabilizer; Val, valproate.
The treatment options are rated according to the rating system shown in Table 1. Enriched sample: the sample is enriched on the basis of remission after treatment with the agent under consideration during the acute phase (index episode).
Monotherapy
Lithium.
There are a number of historic small studies that investigated the usefulness of lithium in the maintenance treatment of BD (Baastrup et al., 1970; Melia, 1970; Small et al., 1971; Cundall et al., 1972; Hullin et al., 1972; Persson, 1972; Prien et al., 1973b; Prien et al., 1973a; Dunner et al., 1976; Fieve et al., 1976; Fyro and Petterson, 1977; Klein et al., 1981; Christodoulou and Lykouras, 1982; Kane et al., 1982; Margo and McMahon, 1982; Mander and Loudon, 1988; Post et al., 1992). All of them reported positive findings; however, a number of drawbacks including the obsolete methodological approach and the utilization of mixed and small samples make the results of these trials difficult to interpret.
Overall there are 4 randomized placebo controlled studies concerning the efficacy of lithium in the maintenance treatment of BD. One is negative/failed (Bowden et al., 2000) and 3 are positive (Bowden et al., 2003; Calabrese et al., 2003b; Weisler et al., 2011). The fourth is a small discontinuation study (Kafantaris et al., 2004). Two of the positive studies support the usefulness of lithium in the prevention of manic but not depressive episodes irrespective of the polarity of the index episodes (Bowden et al., 2003; Calabrese et al., 2003b). The third study also supports its usefulness in the prevention of depressive episodes (Weisler et al., 2011). There are no data on the efficacy concerning the prevention of mixed episodes or for rapid cycling patients. It is important to note that the study samples were not enriched for response to lithium. On the contrary, one study had a sample enriched for response to quetiapine (Weisler et al., 2011), while 2 others had samples enriched for lamotrigine (Bowden et al., 2003; Calabrese et al., 2003b), that, however, is not efficacious against acute mania. There are some problems with the design of the studies, especially concerning the magnitude of improvement during the acute treatment phase and the duration the patients were required to be stable before entering the double-blind phase. With a few exceptions, most are essentially relapse prevention, not maintenance studies.
Antiepileptics.
Valproate
As mentioned above, there is one properly conducted trial (Bowden et al., 2000) in that valproate was the agent under investigation. Lithium served as active control, and since, as shown above, lithium has proven efficacy during the maintenance phase of BD, this specific trial is best considered to be a failed study and not negative for valproate.
Carbamazepine
Concerning carbamazepine, there is only one small placebo controlled study. Although carbamazepine was effective in 60% of cases relative to 22% in the placebo group, the differences were not significant likely due to lack of power. Further, there were methodological issues with the study design and hence, the data are difficult to interpret (Okuma et al., 1981).
Lamotrigine
Overall there are 3 placebo controlled RCTs concerning the efficacy of lamotrigine in the maintenance treatment of BD. Two of them suggest lamotrigine is efficacious in the prevention of depressive but not manic episodes irrespective of the polarity of the index episodes (Bowden et al., 2003; Calabrese et al., 2003b). There are no data concerning index mixed episodes. The only study in rapid cycling patients was negative concerning the primary outcome (Calabrese et al., 2000). All studies were enriched for tolerability to lamotrigine, but one should keep in mind that lamotrigine is neither efficacious against acute mania nor acute bipolar depression. There were some problems with the design of the studies, particularly concerning the magnitude of improvement during the acute treatment phase and the duration the patients were stable before entering the double-blind phase. Essentially they were relapse prevention, not maintenance studies.
Antidepressants.
There are 2 small, old negative studies concerning the efficacy of imipramine (Prien et al., 1973a; Kane et al., 1982), while on the contrary, 3 other small studies in BD-II patients provide some support for the usefulness of fluoxetine monotherapy in the prevention of depressive episodes (Amsterdam et al., 1998; Amsterdam and Shults, 2005b, 2010).
Antipsychotics.
Olanzapine
Three trials provide suport for the efficacy of olanzapine in the prevention of manic, depressive, or mixed episodes in patients with an index manic or mixed episode that responded to olanzapine treatment during the acute phase (Tohen et al., 2006; Berwaerts et al., 2012a; Vieta et al., 2012). There are some data to support the notion that the efficacy of olanzapine is not restricted to those patients who responded to olanzapine during the acute phase. Its long-term effects in rapid cycling patients are unknown.
Aripiprazole
There are 2 trials that support the efficacy of aripiprazole in the prevention of manic but not depressive episodes in BD patients after an index manic or mixed episode who responded to aripiprazole during the acute phase (Keck et al., 2006a; Keck et al., 2007). These 2 trials utilize a methodology that satisfies stringent criteria concerning the definition of “maintenance” treatment.
Quetiapine
There is one published positive study that investigated the efficacy and safety of quetiapine IR monotherapy (300–800 mg/d) as maintenance treatment in BD-I patients compared with switching to placebo or lithium. The time to recurrence of any mood event was significantly longer for both quetiapine and lithium vs placebo. Both quetiapine and lithium significantly increased time to recurrence of both manic and depressive episodes compared with placebo (Weisler et al., 2011). A second study in patients who had recovered from bipolar depression reported that quetiapine prevented depressive but not manic episodes (Young et al., 2014).
Paliperidone
There is one positive study that supports the usefulness of paliperidone in the prevention of manic but not depressive recurrences in patients with index manic or mixed episodes who responded to paliperidone during the acute phase (Berwaerts et al., 2012a).
Risperidone long-acting injectable (RLAI)
Two studies support the efficacy of RLAI in the prevention of manic but not depressive episodes in BD-I patients with a manic or mixed index episode who responded to oral risperidone or RLAI during the acute phase (Quiroz et al., 2010; Vieta et al., 2012).
Conclusion of monotherapy trials.
Lithium, olanzapine, quetiapine, aripiprazole, paliperidone, and RLAI are efficacious in the prevention of manic episodes in patients who recovered from an index manic or mixed episode. Olanzapine and quetiapine are also efficacious in the prevention of depressive episodes. Quetiapine was efficacious irrespective of the index episode. Olanzapine was also efficacious in the prevention of mixed episodes. There is a lack of data concerning carbamazepine or valproate.
Lamotrigine is efficacious in the prevention of depressive but not manic episodes irrespective of index episode. It was not efficacious in the prevention of mixed episodes or in rapid cycling patients. The literature does not support the efficacy of imipramine, while, on the contrary, it gives some support for the efficacy of fluoxetine but only in BD-II patients.
All except lithium and olanzapine were proven efficacious only in samples enriched for response or tolerability during the acute phase. Except from the negative data for lamotrigine there are no data concerning rapid cycling patients. Also, except from the data concerning olanzapine, there are no data concerning specifically the prevention of mixed episodes or the response of patients with an index mixed episode.
Comparison of Treatments
Lithium vs others.
There are a number of studies comparing lithium with carbamazepine (Placidi et al., 1986; Watkins et al., 1987; Lusznat et al., 1988; Stoll et al., 1989; Small et al., 1991; Coxhead et al., 1992; Simhandl et al., 1993; Denicoff et al., 1997; Hartong et al., 2003) including the MAP study (Greil et al., 1997; Greil and Kleindienst, 1999a, 199b; Kleindienst and Greil, 2000, 2002), and overall the data suggested that both agents are comparable in terms of efficacy. There are some data in favor of a superiority of lithium in the treatment of more “classic” patients, but in the rest of patients the 2 agents seem to be comparable. Lithium was also comparable to valproate in terms of prevention of mood episodes (Bowden et al., 2000; Calabrese et al., 2005a) and suicidality (Oquendo et al., 2011) to olanzapine (Tohen et al., 2005) and also to aripiprazole (El-Mallakh et al., 2012)
Furthermore, there was a difference in the clinical profiles of lithium and lamotrigine. As mentioned before, 3 placebo-controlled RCTs suggest that lamotrigine was more efficacious in the prevention of depressive episodes and lithium in the prevention of manic, hypomanic, and mixed episodes (Bowden et al., 2003; Calabrese et al., 2003b).
When compared with antidepressants, the available data suggest that lithium is superior to imipramine for the prevention of depression in BD-I patients episodes (Prien et al., 1973a; Prien et al., 1984) but inferior to fluoxetine in BD-II patients (Amsterdam and Shults, 2010).
A maintenance study reported equal efficacy between venlafaxine and lithium in the prevention of depressive relapses, although there was a tendency of better performance for venlafaxine (Amsterdam et al., 2015)
Antiepileptics vs others.
The studies comparing valproate with lithium have already been discussed above (Bowden et al., 2000; Calabrese et al., 2005a; Oquendo et al., 2011). Two trials suggested valproate is comparable with olanzapine (Tohen et al., 2003a) and with a similar cost to healthcare system (Zhu et al., 2005). Carbamazepine has been studied only in comparison with lithium, and these studies have been discussed previously in the paragraph concerning lithium (Placidi et al., 1986; Watkins et al., 1987; Lusznat et al., 1988; Small et al., 1991; Coxhead et al., 1992; Simhandl et al., 1993; Denicoff et al., 1997; Greil et al., 1997; Greil and Kleindienst, 1999a; Kleindienst and Greil, 2000, 2002; Hartong et al., 2003).
Olanzapine vs others.
The comparison of olanzapine with lithium (Tohen et al., 2005) and valproate (Tohen et al., 2003a; Zhu et al., 2005) has been discussed above.
One study that constituted the extension of an acute phase trial suggested that olanzapine is comparable with asenapine (McIntyre et al., 2010a), while another suggested that it is superior to paliperidone ER (Berwaerts et al., 2012a) and to long-acting risperidone (Vieta et al., 2012).
Other comparisons.
The comparisons of aripiprazole (El-Mallakh et al., 2012), fluoxetine (Amsterdam and Shults, 2010), imipramine (Prien et al., 1984), and lamotrigine (Bowden et al., 2003; Calabrese et al., 2003b) with lithium, and of asenapine (McIntyre et al., 2010a), paliperidone, and risperidone with olanzapine (Berwaerts et al., 2012a; Vieta et al., 2012) have been discussed previously.
One 25-week RCT comparing the OFC vs lamotrigine in the prevention of bipolar depression reported that bipolar depressive patients who responded to OFC do better on long-term OFC in comparison with spontaneously improved patients on long-term lamotrigine (Brown et al., 2009). The result is difficult to interpret as there was an enrichment of the OFC arm, but not the lamotrigine arm. Finally, one study compared the efficacy of venlafaxine in the prevention of bipolar vs unipolar depression and reported no difference between groups (Amsterdam and Garcia-Espana, 2000).
Combination and Add-On Treatment
Combination treatment.
There are 3 early studies that investigated the combination of lithium with another agent. The lithium plus imipramine combination was not more efficacious than lithium monotherapy (Kane et al., 1982; Prien et al., 1984) and lithium or carbamazepine monotherapy was not inferior to their combination that, however, was more efficacious in rapid cycling patients (Denicoff et al., 1997). Also the combination of lithium, carbamazepine, or valproate with perphenazine was not better than mood stabilizer monotherapy; on the contrary, combination treatment was associated with a shorter time to depressive relapse, more drop-outs, and increased rates of dysphoria and depressive symptoms (Zarate and Tohen, 2004). Similarly negative were the results for the lithium or valproate combination with olanzapine (Tohen et al., 2004) while, on the contrary, the combination with quetiapine had significant advantages irrespective of index episode, mood stabilizer and rapid cycling status (Vieta et al., 2008a; Suppes et al., 2009). Positive results were also reported for their combination with ziprasidone (Bowden et al., 2010). Results were negative for aripiprazole plus valproate (Woo et al., 2011) or lamotrigine (Carlson et al., 2012).
The OFC was similar to lamotrigine in terms of incidence of relapse, but overall bipolar depressive patients who responded to OFC do better on long-term OFC in comparison with spontaneously improved patients on long-term lamotrigine (Brown et al., 2009). Lamotrigine plus divalproex was not superior to lamotrigine alone concerning the time to depressive episode (Bowden et al., 2012).
The open-label BALANCE study results neither reliably confirmed nor refuted a benefit of valproate-lithium combination therapy compared with lithium monotherapy, but clearly demonstrated that it is superior to valproate alone (Geddes et al., 2010). Another study reported that risperidone or olanzapine adjunctive therapy for 24 weeks is beneficial but continuation of risperidone beyond this period does not reduce the risk of relapse. Whether continuation of olanzapine beyond this period reduces relapse risk remains unclear but the potential benefit needs to be weighed against an increased risk of weight gain (Yatham et al., 2015).
Overall, there is no compelling data that combination treatment in general does better than monotherapy. Patients stabilized on combination treatment might, however, do worse if shifted to monotherapy, and combination treatment with quetiapine or ziprasidone plus a mood stabilizer might work better than a mood stabilizer alone.
Add-on treatment.
A small study supported the adding of phenytoin to treatment as usual (Mishory et al., 2003) as did another small one for gabapentin (but not on top of antipsychotics) (Vieta et al., 2006). The data are negative for the addition of oxcarbazepine (Vieta et al., 2008c) and equivocal for lamotrigine (van der Loos et al., 2011) to lithium. Negative data were also reported from a trial of adjunctive pramipexole to treatment as usual (TAU) in stabilized BD patients with the aim to improve neurocognition (Burdick et al., 2011), and from a trial of N-acetyl cysteine on TAU in patients after an index episode of bipolar depression (Berk et al., 2012). It is interesting that adjunctive RLAI on TAU significantly prolongs the time to relapse in rapid cycling patients (Macfadden et al., 2009). Adding aripiprazole to lithium or valproate also supplied positive results (Marcus et al., 2011).
It is reported that patients who respond to treatment with lithium, valproate, or carbamazepine plus antidepressants are more likely to maintain response with continuation of the combined treatment; however, those patients who manifest only a partial acute response are unlikely to further improve when the same treatment is continued (Altshuler et al., 2009). Also adjunctive asenapine to lithium or valproate was well tolerated for up to 52 weeks, but no efficacy data were reported from that trial (Szegedi et al., 2012).
Two trials investigated the efficacy of adjunctive N-acetyl cysteine (NAC). The first one randomized 75 BD patients during the maintenance phase and reported that NAC treatment caused a significant improvement on the MADRS score in comparison with placebo (P=.002). Improvements were lost after washout. There was no effect of NAC on time to a mood episode and no significant between-group differences in adverse events (Berk et al., 2008). The second randomized 14 patients (not all of them with high depression scores) and reported a superiority of the NAC group vs placebo in terms of remission (P=.031) (Magalhaes et al., 2011b). One maintenance study supported the usefulness of ramelteon in the prevention of relapse in BD patients (Norris et al., 2013). Negative results have been reported for the usefulness of memantine in patients on valproate treatment (Lee et al., 2014b).
There are some studies suggesting that there is a role for various nutritional supplements such as n-3 fatty acids, chromium, choline, magnesium, and tryptophan alone or in combination with pharmacotherapies for the treatment of BD, but the data are of low quality (Sylvia et al., 2013).
Posthoc, Reviews, and Meta-Analytic Studies
Posthoc analyses.
A number of posthoc analyses exist and attempt to answer questions that the original papers did not address. Posthoc analysis can be informative but can also be a major source of publication bias (Vieta, 2007). A subanalysis of the MAP study reported that lithium was superior in classical BD-I patients and comparable with carbamazepine in the rest. An additional subanalysis including mixed states as an additional nonclassical feature confirmed the results (Greil et al., 1998).
Concerning the usefulness of antidepressants, one posthoc analysis suggested that the discontinuation rate for any reason was lower among patients in the divalproex group taking a selective serotonin re-uptake inhibitor (SSRI) than among patients in the placebo group taking an SSRI (Gyulai et al., 2003b), while the application of 4 different remission criteria suggested that the application of different definitions of remission does not make any significant difference concerning the results (Pae et al., 2012). The addition of an atypical antipsychotic-antimanic agent in some BD patients might help to reduce suicidal ideation (Houston et al., 2006). Olanzapine might be more beneficial if started at an earlier stage of the disease (Ketter et al., 2006), and it is also efficacious in patients with an index mixed episode (Tohen et al., 2009).
Concerning lithium, it has been reported that only at plasma levels between 0.6 and 1.2 mEq/lt it is efficacious in the prevention of both manic and depressive episodes (Nolen and Weisler, 2013). Another posthoc analysis did not confirm its efficacy in the prevention of depressive episodes while it confirmed the efficacy of lamotrigine in the prevention of both manic and depressive episodes irrespective of index episode (Calabrese et al., 2003a; Goodwin et al., 2004). These results still held true when early relapses that occurred in the first 90 or 180 days were excluded from the analysis (Calabrese et al., 2006). The lack of efficacy of lithium in a subgroup of patients might be due to lithium induced thyroid function abnormalities in a subpopulation of patients (Frye et al., 2009). Overall, lamotrigine performed better in comparison with lithium in terms of remission and the persistence of subsyndromal symptoms (Frye et al., 2006). Some positive results for NAC were also suggested by 2 posthoc analysis (Magalhaes et al., 2011a, 2013).
Review and meta-analyses.
One review confirmed the efficacy of lithium but reported that there is no definitive evidence as to whether or not lithium has an anti-suicidal effect (Burgess et al., 2001). A more recent meta-analysis confirmed the antisuicidal effect of lithium vs placebo but not its superiority over other agents except carbamazepine (Cipriani et al., 2013). Two other studies support the usefulness of RLAI (Bobo and Shelton, 2010) and of ziprasidone for the maintenance treatment of BD-I disorder in adults as an adjunct to lithium or valproate (Citrome, 2010). Another review identified 4 issues that limit the interpretation of trials (insufficient duration, enriched sample, possible conflation with iatrogenic adverse effects by abrupt medication discontinuation with beneficial effects on treatment, and a low overall completion rate) (Tsai et al., 2011).
Concerning meta-analysis, the first one for carbamazepine failed to prove the prophylactic efficacy (Dardennes et al., 1995). A second one concluded that the data for oxcarbazepine are of very low quality not allowing firm conclusions (Vasudev et al., 2008). A fair number of meta-analyses focused on lithium. One confirmed its efficacy but failed to find sufficient evidence to prove that a lithium-withdrawal relapse phenomenon exists, that is patients relapse soon after stopping lithium and the symptomatology turns refractory to treatment (Davis et al., 1999). Another one supported an antisuicidal efficacy of lithium (Tondo et al., 2001). Three others confirmed the prophylactic antimanic efficacy of lithium but were equivocal for the prophylactic efficacy against depressive episodes (Burgess et al., 2001; Geddes et al., 2004; Severus et al., 2014).
Furthermore, a number of meta-analytic studies confirmed the prophylactic antimanic efficacy of specific agents and the antidepressant of others. It is important to mention that among other more or less expected results, the antidepressant efficacy of valproate and imipramine was supported (Beynon et al., 2009) as well as of lithium (Popovic et al., 2010), while the prophylactic antidepressant efficacy of olanzapine was questioned (Cipriani et al., 2010). Antipsychotics might be superior to lithium and anticonvulsants but with more adverse effects (Vazquez et al., 2015a, 2015b).
The issue of combination treatment has been the focus of 2 meta-analyses. They both reported negative conclusions for the addition of antidepressants (Ghaemi et al., 2008; Beynon et al., 2009). A third analysis suggested that no monotherapy was associated with a significantly reduced risk for both manic/mixed and depressive relapse, and only quetiapine plus lithium or divalproex was associated with a significantly reduced risk for relapse towards both the manic/mixed and depressive pole (Vieta et al., 2011). This specific meta-analysis also pointed out that the majority of studies included samples enriched for response to a specific agent during the acute phase.
Finally, pharmaco-epidemiological data suggest that valproate and lithium might have a protective effect against any psychiatric hospitalization for patients with BD in a real world setting, while lamotrigine and carbamazepine might exert protective effects solely against depressive and manic episodes, respectively (Joas et al., 2015).
Treatment of Mixed Episodes
Mixed episodes are no longer accepted as a diagnostic entity by DSM-5; instead “mixed features” is included as a specifier and this creates a degree of confusion for future treatment recommendations, since the 2 concepts differ significantly (Fountoulakis, 2015d). So far, mixed episodes have been combined with pure manic episodes in RCTs and results have been reported together. Only a few papers, usually posthoc analyses, report the results concerning mixed episodes separately. Unfortunately all data on mixed episodes stem from trials of acute mania and only one trial reports on the efficacy of lurasidone in bipolar depressive patients with mixed features. That trial supported the efficacy of lurasidone in these patients for the improvement of both depressive and manic symptoms (McIntyre et al., 2015; Suppes et al., 2015). Another important limitation is that the results reported usually concern only the manic but not the depressive component of the mixed episode (Fountoulakis et al., 2012b). The ranking of the data for the treatment of mixed episodes is shown in Table 6.
Table 6.
Treatment of Mixed Episodes
| Acute Phase | Maintenance Phase | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Monotherapy | Combination with MS | Monotherapy | Combination | |||||||
| Agent/modality (alphabetical order) | Manic component | Depressive component | Manic component | Depressive component | MS | Cbz | Lam | Li | Val | |
| Aripiprazole | 3 | 3 | - | - | - | 2 | - | 5 | - | - |
| Asenapine | 4 | 4 | - | - | - | - | - | - | - | - |
| Carbamazepine | 3 | 3 | - | - | - | - | - | - | - | - |
| Celecoxib | - | - | 5 | 5 | - | - | - | - | - | - |
| Haloperidol | - | - | 5 | 5 | - | - | - | - | - | - |
| Lithium | 5 | - | - | - | - | - | - | - | - | - |
| OFC | 4 | 4 | - | - | - | - | - | - | - | - |
| Olanzapine | 3 | 3 | 2 | 2 | 1 | - | - | - | - | - |
| Paliperidone | 3 | 5 | - | - | - | - | - | - | - | - |
| Quetiapine | 5 | - | - | - | - | - | - | - | - | - |
| Risperidone | 3 | - | 5 | 5 | - | - | - | - | - | - |
| Valproate | 3 | 4 | - | - | - | - | - | - | - | - |
| Ziprasidone | 4 | 4 | - | - | - | - | - | - | - | - |
Abbreviations: -, no data; Cbz, carbamazepine; Lam, lamotrigine; Li, lithium; MS, mood stabilizer; OFC, olanzapine-fluoxetine combination; Val, valproate.
The treatment options are rated on the basis of efficacy according to the rating system shown in Table 1.
Treatment of Acute Mixed Episodes
Aripiprazole and carbamazepine were found efficacious in the treatment of both the manic and the depressive component of acute mixed episodes (Keck et al., 2003b; Weisler et al., 2004, 2005, 2006; Sachs et al., 2006; Suppes et al., 2008b). Ziprasidone was also found to be efficacious against both components, but the definition of mixed states was different from the DSM.
Olanzapine and valproate were reported to be efficacious against mania but the data are inconclusive concerning the depressive component (Tohen et al., 1999, 2000; Baker et al., 2003; Baldessarini et al., 2003b; Shi et al., 2004a; Bowden et al., 2006; Ghaemi et al., 2007; McIntyre et al., 2009b). The posthoc analysis of the 2 bipolar depressive trials suggested that olanzapine was efficacious in those patients with mixed features suggesting an effect also on the depressive component (Tohen et al., 2014). Furthermore, risperidone but not asenapine is reported to be efficacious against the manic component, but no data exist concerning their efficacy on the depressive component (Khanna et al., 2005; McIntyre et al., 2009b). A posthoc analysis suggested that asenapine but not olanzapine improved the quality of life in mixed patients (Michalak et al., 2014), and another 2 suggested that asenapine improved both the manic and depressive component in comparison with placebo and was also found superior to olanzapine concerning the manic but not the depressive component (McIntyre et al., 2013; Berk et al., 2015). However, a more recent trial was negative (Landbloom et al., 2016). Paliperidone was efficacious only against the manic component (Vieta et al., 2010c; Berwaerts et al., 2012b). One study for quetiapine was a failed one (Cutler et al., 2011).
The combination of olanzapine olanzapine plus lithium or valproate have positive data concerning both components (Tohen et al., 2002b; Baker et al., 2004; Houston et al., 2006, 2009, 2011). In mixed depression the OFC was comparable with olanzapine and both were superior to placebo, but due to the small number of subjects the report does not permit to derive conclusions (Tohen et al., 2003c; Benazzi et al., 2009). The data concerning the combination of haloperidol or risperidone plus lithium or valproate were negative (Sachs et al., 2002). Overall it seems that second generation antipsychotics (SGAs) are effective in treating acute mixed episodes of BD, with predominant manic symptoms. Their efficacy in treating depressed mixed episodes remains unclear (Muralidharan et al., 2013).
The only trial in patients in bipolar depressive episode with mixed features supported the efficacy of lurasidone in these patients for the improvement of both depressive and manic symptoms (McIntyre et al., 2015; Suppes et al., 2015).
Maintenance Treatment of Mixed Bipolar Episodes
The data so far suggest that olanzapine prolongs time to relapse into any episode in patients with an index mixed episode (Tohen et al., 2006, 2009) while on the contrary, lithium and valproate had negative results in patients with a dysphoric manic index episode (Bowden et al., 2005a). Additionally, the data are in support of the combination of quetiapine plus lithium or valproate (Vieta et al., 2008a; Suppes et al., 2009) but are negative concerning aripiprazole in patients with an index mixed episode (Yatham et al., 2013a).
Treatment of Rapid Cycling Patients
The treatment of rapid cycling patients constitutes a challenge. Often their course frustrates the therapist and the evaluation of treatment is difficult because of the rapid switching from one pole to another (Fountoulakis et al., 2013). The ranking of the treatment of rapid cycling patients is shown in Table 7.
Table 7.
Treatment of Rapid Cycling Patients during the Different Phases of BD
| Agent/modality (alphabetical order) | ACUTE mania | Depression | Maintenance |
|---|---|---|---|
| Aripiprazole | 3 | - | 3 |
| Carbamazepine | - | - | 2 (Li + Cbz) |
| Lamotrigine | - | - | 5 |
| Lithium | 4 | 3 | 2 (Li, Li + Cbz) |
| Olanzapine | 3 | - | - |
| Paroxetine | - | 5 | - |
| Quetiapine | 3 | 2 | 2 (Quet+ Val/Li) |
| Risperidone, long-acting injectable | - | - | 2 (RLAI+TAU) |
| Valproate | 4 | 4 | - |
Abbreviations: -, no data; Cbz, carbamazepine; Li, lithium; Quet, quetiapine; RLAI, risperidone long-acting injectable; TAU, treatment as usual; Val, valproate.
The treatment options are rated on the basis of efficacy according to the rating system shown in Table 1.
Treatment of Acute Episodes in Rapid Cycling Patients
Olanzapine is effective in reducing symptoms of mania and was well tolerated in rapid cycling BD-I patients as shown by a secondary analysis (Sanger et al., 2003). The pooling of data from 2 RCTs reported that improvement of mania with olanzapine was similar in rapid cyclers and non-rapid cyclers. However, rapid cyclers showed an earlier response (Vieta et al., 2004). One trial was also positive concerning aripiprazole in acutely manic rapid cycling patients (Sachs et al., 2006).
Although one study on acute mania in rapid cycling patients was a failed one (Cutler et al., 2011), one a priori planned subanalysis of data from rapid cycling patients with acute BD-I or BD-II depression suggested that quetiapine monotherapy (300–600 mg/d) was effective and well tolerated (Vieta et al., 2007). The posthoc analysis of the rapid cycling subsample of bipolar depressives from the BOLDER study confirmed this (Cookson et al., 2007), and finally the subanalysis of the data from a small number of depressed rapid cycling BD patients again suggested that 300 mg of quetiapine monotherapy was superior to placebo (Suppes et al., 2010).
It seems that lithium has a week but positive effect (Young et al., 2010) and also there are some positive but equivocal data for valproate (Muzina et al., 2010). On the other hand, the data are clearly negative for paroxetine (McElroy et al., 2010c).
The combination of lithium and divalproex was not effective and the further addition of lamotrigine did not seem to add anything in Terms of efficacy (Kemp et al., 2012b)
Relapse Prevention in Rapid Cycling Patients
For the prevention phase, the data so far suggest that divalproex is not more effective than lithium (Calabrese et al., 2005a) and also that the combination of lithium plus divalproex is not better than lithium alone (Kemp et al., 2009). One small study reported that the combination of lithium plus carbamazepine did better than either agent alone (Denicoff et al., 1997). It is interesting that the data are negative for lamotrigine, although in some secondary outcomes there was a beneficial signal especially in BD-II patients (Calabrese et al., 2000). Overall, the widely believed concept among clinicians that divalproex is more effective than lithium in the long-term management of rapid-cycling BD was not supported by a trial on 139 patients (Findling et al., 2005).
One posthoc analysis suggested that aripiprazole was efficacious (Muzina et al., 2008). There are no data on other antipsychotics in monotherapy concerning the maintenance phase. A posthoc analysis reported that rapid cycling patients did less well during the extended observation period than nonrapid cycling patients, regardless of treatment and that overall olanzapine and divalproex appeared comparable (Suppes et al., 2005).
Another study confirmed the efficacy and safety of quetiapine add-on to lithium or divalproex in the prevention of mood episodes in rapid cycling BD-I patients with most recent episode manic/mixed or depressive (Vieta et al., 2008a). There was a North American study with a similar design as the previous one reporting similar results (Suppes et al., 2009). A large controlled trial that evaluated adjunctive maintenance treatment with RLAI on TAU in 240 BD-I patients with at least 4 mood episodes in the 12 months prior to study entry yielded positive results (Macfadden et al., 2009).
The results of the STEP-BD support a role of antidepressants in the development of rapid cycling in a subpopulation of BD patients (Schneck et al., 2008; Ghaemi et al., 2010). A similar conclusion came from earlier randomized controlled study of rapid cycling patients using a double-blind on-off-on-off design with the use of tricyclic antidepressants (Wehr et al., 1988)
Finally, the data are negative concerning the administration of 6 g/d of ethyl-eicosapentanoate as augmentation of treatment with mood stabilizers in rapid cycling patients with bipolar depression (Keck et al., 2006b).
One meta-analysis suggested that lithium is at least partially efficacious in rapid cycling patients (Kupka et al., 2003), another one suggested there is no clear advantage of any treatment option vs the others (Tondo et al., 2003), while a third one proposed that some atypical antipsychotics (especially quetiapine and olanzapine) may be considered as the first-line treatment options (Cruz et al., 2010). The meta-analysis of 20 studies published from 1974 to 2002 comparing subjects with rapid and nonrapid cycling BD reported that in contrast to common beliefs, lithium prophylaxis has at least partial efficacy in a considerable number of rapid cyclers, especially when antidepressants are avoided. Hypothyroidism may be associated with mood destabilization in vulnerable patients (Kupka et al., 2003).
Treatment of Special Conditions
Treatment of Comorbid Conditions
Comorbidities are common in bipolar patients and often need more elaborated therapeutic interventions (Fountoulakis, 2015e, 2015f, 2015g).
Treatment of comorbid substance abuse disorder (SUD).
There are 2 placebo controlled trials suggesting that the combination of valproate and lithium in BD patients with co-occurring alcohol dependence improves both mood and alcohol use symptoms (Salloum et al., 2005, 2007) and that lithium treatment in BD adolescents improves mood and substance use symptoms (Cerullo and Strakowski, 2007). Lithium can be used for the treatment of concomitant substance and polysubstance abuse (Geller et al., 1992, 1998), and quetiapine and risperidone can reduce drug craving (Nejtek et al., 2008). On the contrary, the data concerning quetiapine for alcohol abuse are negative (Brown et al., 2008; Sherwood Brown et al., 2014). For bipolar patients with alcohol dependence, the opiate receptor antagonist naltrexone could be useful (Sherwood Brown et al., 2009), and a preliminary report is positive for acamprosate (Tolliver et al., 2012) but negative concerning the treatment of any substance use with NAC (Bernardo et al., 2009). One trial on the usefulness of citicoline in the treatment of cocaine use was inconclusive (Brown et al., 2015) as was one study with the use of topiramate in alcohol dependence (Sylvia et al., 2016).
There are open-label medication trials that provide limited support to quetiapine, aripiprazole, bupropion, and lamotrigine for the treatment of BD patients with cocaine dependence. Also, aripiprazole might be helpful in patients with alcohol use disorders (Cerullo and Strakowski, 2007; Sepede et al., 2014).
Overall, while some data are available for alcohol, cannabis, and cocaine use comorbid with BD, the evidence is sparse concerning heroin, amphetamine, methamphetamine, and polysubstance SUD comorbid with BD (Beaulieu et al., 2012).
Treatment of comorbid anxiety and disorders.
A posthoc analysis of anxiety symptoms with data from 2 RCTs of 8-week duration of quetiapine (300 or 600 mg/d) (Calabrese et al., 2005b; Thase et al., 2006) reported that at endpoint there was no difference between treatment groups and placebo concerning the total HAM-A score, but there was a difference both for the psychic and the somatic anxiety subscale scores in comparison with placebo (P<.001) (Lydiard et al., 2009). Also, quetiapine XR (50–300 mg/d) was superior both to divalproex ER (500–3000 mg/d) and placebo in the improvement of anxiety in BD patients with comorbid panic attacks or generalized anxiety disorder (GAD) (Sheehan et al., 2013). In another study, again quetiapine (300 or 600 mg/d) and paroxetine (20 mg/d) produced a significant improvement in anxiety in terms of change of HAM-A scale score from baseline in acutely depressed BD patients (McElroy et al., 2010c). Of note, quetiapine (300–600 mg/d) also significantly improved the HAM-D score from baseline, while this was not the case with paroxetine (600–1800 mg/d; P=.279) (Young et al., 2010). However, another study was negative for quetiapine concerning its effect on depression in BD patients with GAD (Gao et al., 2014).
Lurasidone (20–60 mg/d; n=166 or 80–120 mg/d) also significantly improved anxiety symptoms in comparison with placebo (Loebel et al., 2014a). On the contrary, risperidone monotherapy was not an effective anxiolytic for BD patients with comorbid panic disorder or GAD in doses of 0.5–4 mg/d over 8 weeks of treatment (Sheehan et al., 2009), and similar results were obtained with ziprasidone (Suppes et al., 2014).
The data concerning divalproex (rapidly titrated up to 2500 mg/d, as tolerated, to a target serum level of 50–100 mg/dL) are equivocal, because the only positive study was based on a very small study sample (25 outpatients with BD-I depression) (Davis et al., 2005).
It is reasonable to suggest that also benzodiazepines can be used as adjunctive medication for sedation or for the treatment of anxiety, although abuse, tolerance, and dependence constitute important problems. Although approved for the treatment of GAD, pregabalin has no data in BD. However, again it is reasonable to suggest it might be a useful agent for the treatment of anxiety disorders that commonly accompany BD and could substitute for benzodiazepines. A significant advantage is that it is not metabolized by the liver.
There is one study suggesting that adjunctive topiramate could be beneficial in the treatment of BD with comorbid obsessive compulsive disorder, but the overall design and reporting of results does not permit reliable conclusions (Sahraian et al., 2014).
The ranking of the treatment of comorbid anxiety is shown in Table 3.
Weight gain.
Topiramate is not effective in the treatment of BD per se; however, it is unique because of its ability to cause weight loss at dosages of 50 to 200 mg/d. A review reported that more than 70% of patients taking topiramate for a mean duration of 5 months lost a mean of 5 to 6 kilograms (Arnone, 2005). However, topiramate might cause de novo depression and suicidality in some patients, although no completed suicides related to topiramate have been reported (Fountoulakis et al., 2012c).
Treatment of agitation.
Probably most clinicians would choose antipsychotics in severely agitated bipolar patients, and this option is supported by a double blind clinical trial that reported that intramuscular haloperidol (5–10 mg) was equal in efficacy but faster acting in comparison with intramuscular clonazepam (1–2 mg) in agitated mania at 0, 30, and 60 minutes (Chouinard et al., 1993). Similarly, i.m. olanzapine (10 mg, first 2 injections; 5 mg, third injection) was reported to be superior to lorazepam (2 mg, first 2 injections; 1 mg, third injection) for the control of agitation in manic patients. Already 2 hours after the first injection, patients treated with olanzapine showed a significantly greater reduction in scores on all agitation scales compared with patients treated with either placebo or lorazepam (Meehan et al., 2001).
Valproate oral loading of 20 mg/kg/d was reported to be comparable with haloperidol 0.2 mg/kg/d for the treatment of exited manic patients in a single blind study and the effect was evident within 3 days from starting (McElroy et al., 1996). Overall, valproate loading up to 30 mg/kg/d was reported to be safe and well tolerated (Hirschfeld et al., 1999).
Inhaled loxapine exerted an antiagitation effect at 10 minutes at both the 5- and 10-mg doses and was superior to placebo at all time points measured. For safety reasons it has been recommended that inhaled loxapine should be restricted to a single dose in 24 hours and needs to be subject to a Risk Evaluation and Mitigation Strategy program (Citrome, 2012; Kwentus et al., 2012). In Europe, 2 doses are allowed (the second must be given 2 hours after the initial inhalation) (Popovic et al., 2015).
The issue of agitation with aripiprazole is controversial. As an adverse event it is not reported in the dataset and on the contrary, aripiprazole is a recommended evidence based treatment against agitation associated with schizophrenia or bipolar mania (Sanford and Scott, 2008; Gonzalez et al., 2013; Citrome et al., 2016). However, it has been reported under naturalistic conditions (Di Lorenzo et al., 2007) and especially in vulnerable populations such as elderly patients (Coley et al., 2009). Agitation has also been described when initiating aripiprazole in patients after prolonged treatment with potent D2 blocking agents that may result in an upregulation of postsynaptic dopamine receptors (Lea et al., 2007). However, a major obstacle for a fair estimate of the rate of agitation with aripiprazole is that akathisia can easily be mistaken as agitation (Thomas et al., 2015), especially by less experienced raters.
Treatment of Neurocognitive Deficits
The presence of a significant neurocognitive deficit in BD patients has been solidly shown and it concerns all phases of the disorder, including periods of euthymia (Tsitsipa and Fountoulakis, 2015). Galantamine may have specific benefits for episodic memory, but not processing speed, in patients with cognitive impairment as part of BD (Ghaemi et al., 2009). One study reported that pramipexole may improve neurocognition in euthymic patients only (Burdick et al., 2012) while the data are negative for NAC (Dean et al., 2012).
Adjunctive intranasal insulin (40 IU q.i.d.; n=34) had a beneficial effect on executive function but not on the other neurocognitive measures in euthymic patients (McIntyre et al., 2012a). Also adjunctive mifepristone, which is a synthetic steroid, at 600 mg/d improved spatial working memory in BD depressed patients, and this was evident also 7 weeks after the cessation of treatment (Watson et al., 2012)
ECT was reported to produce an improvement in neurocognitive function similar to that of algorithm-based pharmacological treatment (Kessler et al., 2014).
Suicide
There is much discussion concerning the potential antisuicidal efficacy of specific drugs and especially of lithium. However, almost all the data come from studies of naturalistic and epidemiological nature and no controlled studies exist.
There is only one posthoc analysis that investigated suicidality in BD-I patients during treatment with olanzapine in combination with lithium or divalproex. In mixed patients with residual suicidality, suicidal thoughts were associated with somatic discomfort, agitated depression, and psychosis. It seems that combination therapy with olanzapine plus lithium (n=36) vs lithium alone (n=22) significanlty reduced the score in the suicidal item of the HAM-D by 58% vs 29% (P<.05) within 1 week and all associated symptoms within 2 weeks by averages of 31% vs 12% (P<.05) (Houston et al., 2006). The analysis of pharmaco-epidemiological data suggests that treatment with lithium but not with valproate is associated with lower suicidality (Goodwin et al., 2003; Song et al., 2015).
Nonbiological Treatment Options
There are some but overall limited data concerning the usefulness of specific adjunctive psychotherapies (Reinares et al., 2014; Miziou et al., 2015). Research so far has focused on acute depression and the maintenance phase but not on acute mania. These studies suffer from the same limitations and methodological problems as all psychotherapy trials do. There is no universally accepted standardized method to conduct this kind of study and blinding and the nature of the control intervention are unresolved limitations. The grading of these treatment options is shown in Table 8.
Table 8.
Grading of the Evidence for the Efficacy of Nonbiological Treatment Options
| Intervention | Efficacy | |||||
|---|---|---|---|---|---|---|
| Relapse/ recurrence | Manic symptoms | Depressive symptoms | Anxiety | Neurocognition | Overall functioning | |
| CBT | 5 | - | 3 | - | - | - |
| Psychoeducation | 3 | 5 | 5 | - | - | 3 |
| IPSRT | 4 | - | - | - | - | - |
| Family intervention | 5 | 5 | 5 | - | - | 5 |
| Intensive psychosocial intervention | - | - | - | - | - | - |
| Cognitive remediation | 5 | 5 | 5 | - | 5 | 5 |
| Mindfulness based interventions | 5 | 5 | 5 | 3 | - | - |
Abbreviations: -, no data; CBT, cognitive behavioral treatment; IPSRT, InterPersonal and Social Rhythms Therapy.
The treatment options are rated according to the rating system shown in Table 1.
Cognitive-Behavioral Therapy (CBT)
The overall data for the long-term efficacy of CBT either as monotherapy or as add on to psychoeducation and in comparison with TAU are negative concerning relapse prevention. However, there are some positive results for the acute depressive phase in BD (Ball et al., 2006; Scott et al., 2006; Zaretsky et al., 2008; Costa et al., 2011; Gomes et al., 2011; Meyer and Hautzinger, 2012; Gonzalez Isasi et al., 2014). A posthoc analysis suggested that CBT could be more effective than TAU in patients with <12 previous episodes, but less effective in those with more episodes (Scott et al., 2006). In BD patiens with insomnia, CBT for insomnia was superior to psychoeducation concerning manic relapses (Harvey et al., 2015).
Psychoeducation
The data on adjunctive psychoeducation suggest that in comparison with TAU or nonspecific intervention, it prevents relapse to both poles if administered to patients in clinical remission (Perry et al., 1999; Colom et al., 2003, 2009; Lobban et al., 2010; de Barros et al., 2013) but it has no effect on biological rhythms (Cardoso Tde et al., 2015). Again a posthoc analysis suggested that patients with more than 7 episodes did not show significant improvement with group psychoeducation for time to recurrence, and those with more than 14 episodes did not benefit from the treatment in terms of time spent ill (Colom et al., 2010). A systematic review confirmed the above (Bond and Anderson, 2015).
Interpersonal and Social Rhythm Therapy (IPSRT)
Overall there are no convincing data on the usefulness of IPSRT during the maintenance phase of BD; however, there are some data suggesting that if applied early and particularly already during the acute phase, it might prolong the time to relapse (Frank et al., 2005, 2008; Swartz et al., 2012; Inder et al., 2015).
Family Focus Treatment
Overall the literature supports the idea that interventions that focus on families and caregivers exert a beneficial impact especially on family members, but the effect on the patients themselves is controversial and uncontrolled. Probably it improves issues like treatment adherence and family dynamics (Miklowitz et al., 2000, 2003; Rea et al., 2003; Reinares et al., 2004, 2008; D’Souza et al., 2010)
Intensive Psychosocial Intervention
“Intensive” psychotherapy is another option but it is of unknown efficacy with limited research support (Miklowitz et al., 2007a, 2007b). The term refers to up to 30 sessions of CBT, IPSRT, or family focus treatment within 9 months.
Cognitive Remediation and Functional Remediation
The data are positive in improving functioning, that is the critical endpoint, but mostly negative concerning cognitive outcomes when using cognitive remediation techniques as add on to TAU in BD patients (Martinez-Aran et al., 2011; Lahera et al., 2013; Torrent et al., 2013), although a more recent posthoc analysis was promising (Sole et al., 2014).
Mindfulness-Based Interventions (MBCT)
Overall the data do not support a beneficial effect of MBCT on the core symptoms of BD but also suggest that MBCT could be useful in the reduction of anxiety in BD patients. So far there are no data supporting its efficacy in the prevention of recurrences (Williams et al., 2008; Ives-Deliperi et al., 2013; Perich et al., 2013a, 2013b).
Internet-Based Interventions
There is only one randomized trial that compared a completely Internet-based preventive program for BD, adjunctive to usual pharmacological management vs a control intervention. The results suggested no differences between treatment groups (Barnes et al., 2015). The design of the study precludes deriving general conclusions for the efficacy of web-based approaches. Another study that combined psychoeducation with mobile phone technology did not show any benefit vs paper and pencil method, however this could mean that a mobile phone approach could be an important alternative without compromising the outcome (Depp et al., 2015).
Safety Issues With Pharmacotherapy of BD
A comprehensive grading of all agents in terms of their safety and tolerability profile is shown in Table 9.
Table 9.
Grading of Treatment Options According to Safety Issues (According to the System Shown in Table 1)
| Agent/modality (alphabetical order) | Grade | Comments |
|---|---|---|
| Agomelatine | 2 | Liver enzymes induction |
| Allopurinol | 2 | Swelling of mouth and lips, severe skin rashes, infections, eye irritation, hepatitis, appetite and weight loss, and painful or bloody urination |
| Aripiprazole | 1 | |
| Armodafinil/modafinil | 2 | Stimulant, risk for abuse |
| Asenapine | 1 | |
| Bupropion | 1 | |
| Carbamazepine | 2 | Hepatic enzymes induction, many adverse effects |
| Cariprazine | 1 | |
| Celecoxib | 1 | |
| Chlorpromazine | 1 | |
| Clozapine | 3 | Potentially lethal agranulocytosis, metabolic syndrome |
| Donepezil | 1 | |
| ECT | 2 | Not preferred by patients, mild cognitive problems |
| Escitalopram | 1 | |
| Eslicarbazepine | 1 | |
| Fluoxetine | 1 | |
| FEWP | 1 | |
| Gabapentin | 1 | |
| Haloperidol | 2 | EPS, Tardive dyskinesia, neuroleptic malignant syndrome, switch risk |
| Imipramine | 2 | Cardiac side effects, many adverse effects, switch risk |
| Ketamine | 3 | Stimulant |
| L-sulpiride | 1 | |
| Lamotrigine | 2 | Good overall tolerability but potentially lethal skin reaction that can be avoided by slow titration |
| Levetiracetam | 3 | Induction of suicidality |
| levothyroxine (L-T4) | 2 | Mild cardiovascular, skin and bone adverse effects |
| Licarbazepine | 1 | |
| Lisdexamfetamine | 3 | High risk for abuse and dependence |
| Lithium | 2 | Many adverse effects, weight gain, toxicity |
| Loxapine inhalant | 1 | |
| Lurasidone | 1 | |
| N-acetyl cysteine | 1 | |
| Memantine | 1 | |
| Medroxyprogesterone | 1 | |
| Modafinil | 2 | Stimulant, risk for abuse |
| Olanzapine | 2 | Metabolic syndrome |
| Oxcarbazepine | 1 | |
| Paliperidone | 1 | |
| Paroxetine | 1 | |
| Perphenazine | 2 | Switch risk, EPS, tardive dyskinesia, neuroleptic malignant syndrome |
| Phenytoin | 2 | Many adverse effects |
| Phenelzin | 2 | Many adverse effects |
| Pimozide | 2 | EPS, tardive dyskinesia, neuroleptic malignant syndrome |
| Pioglitazone | 2 | Not recommended in patients with diabetes mellitus type I and in liver disease. Absolute contraindication in heart failure patients |
| Pramipexole | 2 | Adverse effects include the induction of problematic behaviours and psychotic symptoms |
| Pregnenolone | 2 | Not well studied |
| Quetiapine | 1 | |
| Risperidone | 1 | |
| RLAI | 1 | |
| Sertraline | 1 | |
| Tamoxifen | 3 | Deep vein thrombosis, cognitive disorder |
| TMS | 1 | |
| Topiramate | 3 | Induction of depression and suicidality |
| Tranylcypromine | 2 | Many adverse effects |
| Valproate | 1 | Cautious use in women of childbearing age |
| Venlafaxine | 2 | Switch risk |
| Verapamil | 1 | |
| Ziprasidone | 2 | QTc prolongation, patients should undergo cardiologic examination before receiving ziprasidone |
Abbreviations: ECT, electroconvulsive therapy; EPS, extrapyramidal signs; FEWP, Free and Easy Wanderer Plus; RLAI, risperidone long-acting injectable; TMS, transcranial magnetic stimulation.
Lithium
Lithium has a narrow therapeutic window concerning its dosage and plasma levels (recommended plasma level 0.6–1.2 mmol/L), and laboratory testing and thorough investigation before starting lithium treatment (ECG; kidney function etc.) is necessary. Unfortunately this often delays the initiation of treatment. Adverse events are more frequent with higher doses, while “rebound mania” has been described upon withdrawal. The most frequent adverse events include neurological, endocrinological (more often from the thyroid), cardiovascular, renal, gastrointestinal, hematological, and dermatological manifestations, and lithium intoxication is not rare. In clinical practice patients often complain of sedation and tremor and sometimes a decline in creative thinking (Shaw et al., 1986; Engelsmann et al., 1988; Stoll et al., 1996). A general negative impact of lithium on neurocognitive function has been reported (Karniol et al., 1978; Kropf and Muller-Oerlinghausen, 1979; Reus et al., 1979; Squire et al., 1980; Connelly et al., 1982; Lund et al., 1982; Shaw et al., 1987; Engelsmann et al., 1988; Maarbjerg et al., 1988; Kocsis et al., 1993; Kessing, 1998; Honig et al., 1999; Bora et al., 2007; Senturk et al., 2007; Goldberg, 2008). It seems that there is a complex relationship between lithium treatment, female gender, hypothyroidism, and rapid cycling (Cowdry et al., 1983; Bauer and Whybrow, 1990; Bauer et al., 1990; Gyulai et al., 2003a; Fountoulakis et al., 2008b). While most authors argue that lithium is neuroprotective, a neurotoxic effect is also possible in the long term, even at therapeutic levels, especially in combination with antipsychotics (Fountoulakis et al., 2008b). Comprehensive guidelines concerning lithium treatment and optimal therapeutic serum levels are available and should be applied (Malhi et al., 2011), and a recent review provides up-to-date information on its safety (Murru et al., 2015).
Antiepileptics
The recommended therapeutic valproate serum concentration is 50 to 150 mg/mL. It is not recommended to be used in women of childbearing age because of the high frequency of unplanned pregnancies in bipolar females and the relatively high teratogenicity of valproate. Other potential acute side effects are weight gain and hair loss. Its use has been associated with polycystic ovary syndrome (PCOS). It is to be noted however, that similar to epilepsy, there is an association between PCOS and major psychiatric disorders, including BD. An increased risk can also be demonstrated in their siblings suggestive of shared familial factors between PCOS and psychiatric disorders (Cesta et al., 2016).
The typical dosage of carbamazepine in the treatment of acute mania is 600 to 1800 mg/d (serum concentration 4–12 mg/mL). After several weeks under carbamazepine, an induction of hepatic enzymes (CYP 3A4) occurs and the drug levels drop and may require additional upward dose titration (Bertilsson and Tomson, 1986). The dosage-related adverse effects include double or blurred vision, dizziness, sedation, ataxia, vertigo, gastrointestinal disturbances, cognitive impairment, hematological effects, and Stevens-Johnson syndrome including its related dermatologic effects (Tohen et al., 1991, 1995; Blackburn et al., 1998).
The most significant drawback of lamotrigine treatment is the need to initiate it at 25 mg/d for 2 weeks, then 50 mg/d for another 2 weeks and then by increments of 25 to 50 mg/d thereafter to avoid a moderately high incidence of rash (Seo et al., 2010).
Carbamazepine decreases lamotrigine concentrations by approximately 50%, and in combination therapy, lamotrigine can be started with higher dosages and faster titration. Vice versa, when combined with valproate a slower titration scheme is needed for lamotrigine, carbamazepine induces the metabolism of other agents as well, for example, risperidone (Ono et al., 2002).
It is also important to note the adverse effects of topiramate because although it is not used in the treatment of BD per se, it is often administered in BD patients in order to lose weight or to treat a comorbid substance abuse disorder. It is reported that topiramate impairs attention, verbal memory, psychomotor speed, and word-finding even at very low dosages (25–50 mg/d). This impairment is reversible after discontinuation of the drug (Salinsky et al., 2005; Goldberg, 2008).
An important recent development was the safety warning by the FDA after a meta analysis that suggested that antiepileptics might double the suicidal risk (FDA, 2008). The field remains uncertain, with some reports and authors supporting the FDA warning (Nilsson et al., 2002; Mula and Sander, 2007; Gibbons et al., 2009; Andersohn et al., 2010; Arana et al., 2010; Olesen et al., 2010; Patorno et al., 2010; VanCott et al., 2010; Ziemba et al., 2010; Wen et al., 2011; Fountoulakis et al., 2012c; Pugh et al., 2012; Siamouli et al., 2014). It is important to note that suicidality data came from the registration of adverse events rather than from systematically collected data (Hesdorffer and Kanner, 2009). However, it seems clear that topiramate, lamotrigine, and levetiracetam are related to increased suicidality in nonpsychiatric patients and this should be the focus of further research.
Antipsychotics
The adverse effects of FGAs include EPS, tardive dyskinesia, and hyperprolactinaemia and the life-threatening but rather rare neuroleptic malignant syndrome, while the most frequent side effects of chlorpromazine are EPS, tardive dyskinesia, postural hypotension, and hepatotoxicity.
On the other hand, the most significant problem with some of the SGAs is weight gain, hyperlipidaemia, and diabetes mellitus. The treatment of these somatic conditions is difficult and the methods proposed have produced rather unsatisfactory results so far. Hyperprolactinaemia and EPS are the most frequent adverse effects with amisulpride. Akathisia and EPS are the adverse effects most often reported with aripiprazole.
Concerning olanzapine, the most frequent adverse effects include dry mouth, weight gain, increased appetite, diabetes mellitus and metabolic syndrome, and somnolence. The main adverse effects of quetiapine are persistent sedation and weight gain, however, to a lower extent than olanzapine. Maybe the XR formulation of quetiapine induces less sedation in comparison with the IR formulation (Riesenberg et al., 2012). The main side effects of risperidone are dose-related EPS, weight gain, sedation, and hyperprolactinemia. Somnolence, akathisia, and EPS as well as a significant QTc prolongation are the main adverse effects of ziprasidone treatment; however, ziprasidone is not associated with the metabolic syndrome (Kemp et al., 2012a).
Reports on antipsychotics concerning adverse effects on neurocognition are rare and conflicting (Holmes et al., 2008; Goldberg and Chengappa, 2009; Pan et al., 2011). There are data suggesting that an executive function deficit is correlated with years of exposure to antipsychotic drugs (Zubieta et al., 2001). This latter finding could reflect either the toxic effect of chronic psychosis, the toxic effect of long-term medication, or both. Current antipsychotic treatment in BD patients is reported to relate to worse performance in sustained attention and visuomotor speed, across all executive function tests as well as in semantic fluency, verbal learning, and recognition memory, even when studies were controlled for differences in clinical features (King, 1994; Altshuler et al., 2004; Frangou et al., 2005; Jamrozinski et al., 2009).
Antidepressants
There is a number of different adverse effects caused by antidepressants. Most of them are not severe and may cause significant burden to the patients but usually improve with time (NHS, 2014).
The adverse effects of SSRIs and serotonin and norepinephrine re-uptake inhibitors include agitation, shakiness, anxiety or feeling of being sick, indigestion, stomach aches, diarrhoea or constipation, loss of appetite, dizziness, insomnia and other sleep disorders, or, on the contrary, hypersomnia and sedation, headache, loss of libido, weight gain, excessive sweating, hyponatriaemia (especially in the elderly), and sexual dysfunction. The adverse effects of tricyclic antidepressants include: dry mouth, blurred vision, constipation, dysuria, drowsiness, dizziness, weight gain, excessive sweating, and heart rhythm problems. A rare but potentially life-threatening adverse event is the serotonin syndrome whose symptoms include confusion, agitation, muscle twitching, sweating, shivering, and diarrhea. Rare but serious cases may manifest with very high fever, epileptic fits, arrhythmia, and coma. All classes of antidepressants have been linked to an increased risk of developing type 2 diabetes, but the causality is uncertain.
There is a warning issued by the FDA (black box warning) concerning the risk of suicidality in pediatric patients taking SSRIs for depression (Libby et al., 2007), and a number of papers suggest that antidepressants are related to an increased risk for suicidal behavior (Rouillon et al., 1991; Khan et al., 2000, 2001, 2003; Luoma et al., 2002; Baldessarini et al., 2003a; Healy, 2003) but not for completed suicide (Whittington et al., 2004). This might constitute one of the most interesting paradoxes of our contemporary psychiatry, since antidepressants prevent suicidal behavior among severely ill, frequently suicidal “real life” unipolar depressives but may provoke such behavior sometimes in less severe, actually nonsuicidal unipolar depressives (Leon et al., 1999; Angst et al., 2002; Yerevanian et al., 2004; Simon et al., 2006; Gibbons et al., 2007). It has been suggested that antidepressants induce suicidality essentially only in pseudo-unipolar patients (Akiskal and Benazzi, 2005; Rihmer and Akiskal, 2006; Perlis et al., 2007b), while the data from the STAR*D trial suggest the presence of a genetic vulnerability predisposing to the manifestation of new suicidal ideation after antidepressant treatment (Laje et al., 2007; Perlis et al., 2007a, 2007b).
Switching to the Opposite Pole
It is widely accepted among psychiatrists that both antidepressants and FGAs can induce a mood switch to the opposite pole, or a chronic, dysphoric, mixed, or irritable state in BD patients and may accelerate episode frequency and/or may cause other forms of course destabilization in patients with BD. However, hard evidence is limited and the bulk of evidence comes from chart reviews and retrospective and open studies. A comprehensive summary of the risk to induce switching for all agents during the 3 phases of treatment is shown in Table 10.
Table 10.
Risk of Various Agents to Induce the Opposite Mood Pole (Switch Risk)
| Treatment phase | |||
|---|---|---|---|
| Agent/modality (alphabetical order) | Acute mania | Depression | Maintenance |
| Aripiprazole | 5 | 5 | 5 |
| Asenapine | 5 | - | 5 |
| Bupropion | - | 5 | - |
| Carbamazepine | 5 | - | 5 |
| ECT | - | 4 | - |
| Escitalopram | - | 5 | - |
| Fluoxetine | - | - | 5 |
| Haloperidol | 4 | - | 4 |
| Imipramine | - | 3 | 2 |
| Lamotrigine | 5 | - | 5 |
| Lithium | 5 | - | 5 |
| OFC | - | 5 | 5 |
| Olanzapine | 5 | 5 | 5 |
| Paliperidone | 5 | - | 5 |
| Paroxetine | - | 5 | 5 |
| Perphenazine | 4 | - | 2 |
| Quetiapine | 5 | 5 | 5 |
| RLAI | 5 | - | 5 |
| Sertraline | - | - | 5 |
| Valproate | 5 | - | 5 |
| Venlafaxine | - | 3 | - |
| Ziprasidone | 5 | - | 5 |
Abbreviations: -, no data; ECT, electroconvulsive therapy; OFC, olanzapine-fluoxetine combination; RLAI, risperidone long-acting injectable.
The treatment options are rated in an analogous way to the rating system shown in Table 1 as “efficacy to induce the opposite pole.”
The literature suggests that without the concomitant use of an antimanic agent the switch rate to mania or hypomania is around 20 to 40% (Bottlender et al., 2001, 2004; Goldberg and Truman, 2003), while with the concomintant use of an antimanic agent the rate is reduced to 14% or below (Nemeroff et al., 2001; Post et al., 2001, 2006; Harel and Levkovitz, 2008; Licht et al., 2008; Tondo et al., 2010). More recent reports suggest that switching is exclusively related to antidepressant monotherapy, while the concomitant use of an antimanic agent has a robust protective effect (Viktorin et al., 2014). The results of the STEP-BD support the potentially harmful role of antidepressants in the long-term course of BD (Truman et al., 2007; El-Mallakh et al., 2008, 2015). According to that study switching to the opposite pole was not dose dependent (Tada et al., 2015). However, a number of larger RCTs reported negative data concerning switching with paroxetine and bupropion (Sachs et al., 2007), fluoxetine, even as monotherapy in BD-II patients (Amsterdam et al., 2004), and citalopram (Schaffer et al., 2006). There are some data suggesting a higher risk of switching while on treatment with venlafaxine (Amsterdam and Garcia-Espana, 2000; Vieta et al., 2002; Altshuler et al., 2006, 2009; Leverich et al., 2006; Post et al., 2006) and imipramine (Himmelhoch et al., 1991; Nemeroff et al., 2001; Silverstone, 2001), but a more recent study reported that venlafaxine was equal to lithium and without any increase in the switch rate (Lorenzo-Luaces et al., 2016).
It is important to mention that switching to mania or hypomania during treatment of comorbid OCD (White et al., 1986; Steiner, 1991; Vieta and Bernardo, 1992; Rihmer et al., 1996; Perugi et al., 2002) or panic disorder with antidepressants have been reported (Pecknold and Fleury, 1986; Sholomskas, 1990).
The switch risk is probably as high as 18.2% in the short term and 35.6% during the continuation phase (Post et al., 2003) and is higher in BD-I patients in comparison with BD-II (14.2% vs 7.1% in acute trials and 23.4% vs 13.9% in maintenance studies). The rates of switching in unipolar patients are lower than those of bipolar (1.5% in acute trials and 6.0% in maintenance studies) (Bond et al., 2008; Tondo et al., 2010).
Haloperidol and perphenazine treatment have been associated with the development of dysphoria and depression, although the data are inconclusive for haloperidol (Tohen et al., 2003b; Zarate and Tohen, 2004). On the contrary, SGAs do not appear to induce depression, while some authors suggest they possess a mild protective property against switching (Tohen et al., 2003c; Amsterdam and Shults, 2005a; Calabrese et al., 2005b; Keck et al., 2005; Thase et al., 2006; Benazzi et al., 2009). A recent meta-analysis reported that treating acute mania with SGAs is associated with a 42% lower risk of switch to depression than with haloperidol. Nevertheless, caution should be taken when considering this to be a class effect, as only olanzapine, quetiapine, and ziprasidone may show these advantages (Goikolea et al., 2013b).
Overall there are no data to suggest a generalized and class effect for antidepressants or FGAs concerning the induction of an affective switch. There are negative data concerning all SSRIs and SGAs studied and positive data only concerning venlafaxine, imipramine, and perphenazine. Some authors believe that at least the switch risk and perhaps also the risk for rapid cycling and new-onset suicidality have been overinterpreted (Grunze, 2008), and thus the issue of switching is still open and further research is needed. Also negative for the presence of a treatment-induced switch are the longitudinal data of Jules Angst (Angst, 1985). For a safe use of antidepressants in BD, clinicians may follow the recommendations of the International Society for Bipolar Disorders Task Force (Pacchiarotti et al., 2013).
Review of Existing Guidelines for BD
A number of treatment guidelines were identified and their reference lists were utilized (APA, 1994, 1995, 2002; Suppes et al., 1995, 2001, 2002, 2003; Frances et al., 1996; 1997; AACAP, 1997; Goodwin et al., 1997, 2003, 2009, 2016; Jobson, 1997; Kusumakar et al., 1997; McClellan and Werry, 1997; Gilbert et al., 1998; Barreira et al., 1999; Bauer et al., 1999b; Rush et al., 1999, 2003; Dennehy, 2000; Goldberg, 2000; Sachs et al., 2000; Allen et al., 2001; Montgomery, 2001; Grunze et al., 2002, 2003, 2004, 2009, 2010, 2011, 2013; Licht et al., 2003; Hirschfeld, 2005; Yatham et al., 2005, 2006, 2008, 2009, 2013b, 2013c; National Collaborating Centre for Mental Health, 2006; O’Dowd, 2006; Nolen et al., 2008; Jon et al., 2009; Ng et al., 2009; Beaulieu et al., 2012; Bond et al., 2012; McIntyre et al., 2012b; Rosenbluth et al., 2012; Schaffer et al., 2012; Mohammad and Osser, 2014; Malhi et al., 2015; Ostacher et al., 2015a; Woo et al., 2015). An additional source was the National Institute of Clinical Excellence (NICE) guideline concerning BD (NICE, 2014), while the latest version of the guidelines of the British Association of Psychopharmacology (Goodwin et al., 2016) were included, although they were published after the date of last literature search.
A description of the most important and most recent guidelines (after 2005) will be included in the text that follows. In Tables 17, 21, and 25 there is a detailed description of difference between the current CINP guidelines and previously developed guidelines by other bodies.
Table 17.
Comparison of the Detailed Algorithm to Previously Developed Guidelines for Acute Mania
| CINP 2016 | WFSBP 2013a | CANMAT and ISBD 2013 | NICE 2014 b | BAP 2016b | |
|---|---|---|---|---|---|
| Aripiprazole | 1 | 1 | 1 | - | 3 |
| Asenapine | 1 | 3 | 1 | - | 3 |
| Cariprazine | 1 | - | 3 | - | 3 |
| Paliperidone | 1 | 3 | 1 | - | 3 |
| Quetiapine | 1 | 3 | 1 | 1 | 1 |
| Risperidone | 1 | 1 | 1 | 1 | 1 |
| Valproate | 1 | 1 | 1 | 1 | 2 |
| Carbamazepine | 2 | 3 | 2 | - | 3 |
| Haloperidol | 2 | 3 | 2 | 1 | 1 |
| Lithium | 2 | 3 | 1 | 1 | 3 |
| Olanzapine | 2 | 3 | 1 | 1 | 1 |
| Ziprasidone | 2 | 1 | 1 | - | 3 |
| ECT | 3 | 4 | 2 | - | 3 |
| Oxcarbazepine | 4 | 4 | 3 | - | - |
| Chlorpromazine | 4 | 3 | 3 | - | 3 |
| Pimozide | 4 | 3 | - | - | 3 |
| Tamoxifen | 4 | 3 | 3 | - | - |
| Eslicarbazepine | NR | - | - | - | - |
| Gabapentin | NR | NR | NR | NR | - |
| Lamotrigine | NR | NR | NR | NR | - |
| Licarbazepine | NR | - | - | - | - |
| rTMS | NR | - | - | - | - |
| Topiramate | NR | NR | NR | NR | - |
| Verapamil | NR | - | - | - | - |
| Phenytoin | - | 3 | - | - | - |
| Clozapine | - | 4 | 3 | - | 3 |
| Amisulpride | - | 4 | - | - | 3 |
| Clonazepam | - | 4 | - | - | - |
| Leviracetam | - | 4 | - | - | - |
| Lorazepam | - | 4 | - | - | - |
Abbreviations: ECT, electroconvulsive treatment; NR, not recommended; rTMS, repetitive Transcranial Magnetic Stimulation.
The grading is not uniform; instead it reflects the grading utilized by individual guidelines and the table aims only to give an image of how different guidelines prioritize treatment options.
Numbers correspond to steps not to efficacy ranking.
aNICE and BAP ordering is on the basis of line of treatment.
bStep 2 in the WFSBP guideline would be a combination of 2 grade “1” recommended medication, or switch from one grade “1” medication to another.
Table 21.
Comparison of the Presise Algorithm to Previously Developed Guidelines for Acute Bipolar Depression Concerning Monotherapy
| CINP 2016 | WFSBP 2013a | CANMAT and ISBD 2013 | NICE 2014 b | BAP 2016b | |
|---|---|---|---|---|---|
| Lurasidone | 1 | - | 2 | - | 1 |
| Quetiapine | 1 | 1 | 1 | 1 | 1 |
| Escitalopram | 2c | - | - | - | 3 |
| Fluoxetine | 2c | 1 | - | - | 3 |
| Olanzapine | 2 | 1 | 3 | 1 | 1 |
| OFC | 2 | 1 | 1 | 1 | 1 |
| Aripiprazole | 3 | NR | NR | - | - |
| Imipramine | 3 | 4 | |||
| Lamotrigine | 3 | 1 | 1 | 1 | 2 |
| Phenelzin | 3 | - | |||
| Valproate | 3 | 1 | 2 | 1 | - |
| Carbamazepine | 3 | 1 | 3 | - | - |
| Lithium | 4 | 1 | 1 | 1 | 3 |
| Tranylcypromine | 4 | - | - | - | 4 |
| ECT | 5 | - | 3 | - | 5 |
| Gabapentin | NR | - | NR | - | - |
| Leviracetam | - | - | NR | - | - |
| L-thyroxine | - | - | - | - | - |
| Paroxetine | NR | NR | - | - | 3 |
| Risperidone | - | - | NR | - | - |
| rTMS | NR | - | - | - | - |
| Ziprasidone | NR | NR | NR | - | - |
Abbreviations: ECT, electroconvulsive treatment; NR, not recommended;
OFC, olanzapine-fluoxetine combination; rTMS, repetitive Transcranial Magnetic Stimulation.
The grading is not uniform; instead it reflects the grading utilized by individual guidelines and the table aims only to give an image of how different guidelines prioritize treatment options. Numbers correspond to steps not to efficacy ranking.
aWFSBP: Recommendation only reflects monotherapy not considering evidence derived from combination treatment (except OFC).
bNICE and BAP ordering is on the basis of line of treatment.
cAgainst BD-II depression.
NICE ordering is on the basis of line of treatment.
Table 25.
Comparison of the Presise Algorithm to Previously Developed Guidelines for Maintenance Phase Concerning Monotherapy
| CINP 2016 | WFSBP 2013a | CANMAT and ISBD 2013 | NICE 2014 b | BAP 2016b | |
|---|---|---|---|---|---|
| Aripiprazole | 1 | 1 | 1 | - | 3 |
| Lithium | 1 | 1 | 1 | 1 | 1 |
| Olanzapine | 1 | 2 | 1 | 1 | 2 |
| Paliperidone | 1 | 3 | 2 | - | 3 |
| Quetiapine | 1 | 1 | 1 | 1 | 2 |
| Risperidone | 1 | 2 | - | - | 3 |
| RLAI | 1 | - | 1 | - | 2 |
| OFC | 2 | - | 2 | - | - |
| Lamotrigine | 2 | 1 | 1 | - | 2 |
| Carbamazepine | 3 | 4 | 2 | - | 2 |
| Valproate | 3 | 3 | 1 | 1 | 2 |
| Haloperidol | 4 | - | - | - | 3 |
| Venlafaxine | 4 | - | - | - | - |
| ECT | 5 | 4 | 3 | - | - |
| Ziprasidone | 5 | 3 | - | - | 3 |
| Continue most recent episode treatment | NR | - | - | 1 | - |
| Antidepressants | - | 3 | NR | - | 4 |
| Asenapine | - | 4 | 3 | - | 3 |
| Gabapentine | - | 4 | NR | NR | - |
| Topiramate | - | 4 | NR | - | - |
Abbreviations: ECT, electroconvulsive treatment; NR, not recommended; OFC, olanzapine-fluoxetine combination; RLAI, Risperidone Long-Acting Injectable.
The grading is not uniform; instead it reflects the grading utilized by individual guidelines and the Table aims only to give an image of how different guidelines prioritize treatment options.
Numbers correspond to steps not to efficacy ranking.
aWFSBP: Recommendation grades and subsequent positioning could be either based on efficacy in the prevention of mania, depression or any episode. Thus, numbers do not reflect the sequence of treatment in an individual patient.
bNICE and BAP ordering is on the basis of line of treatment.
American Psychiatric Association Treatment Guidelines for BD
In 2008 the APA developed a draft of new guidelines after a thorough review of the literature. However, they were never published because of unresolved issues pertaining to the conflict of interest.
The Canadian Network for Mood and Anxiety Treatments and International Society on Bipolar Disorder Guidelines
The most recent 2013 version of the Canadian Network for Mood and Anxiety Treatments and International Society on Bipolar Disorder guidelines (Yatham et al., 2013c) suggests that for the treatment of acute manic episodes the first line recommendation is monotherapy with lithium, divalproex, divalproex ER, olanzapine, risperidone, quetiapine, quetiapine XR, aripiprazole, ziprasidone, asenapine, or paliperidone ER, and adjunctive therapy with risperidone, quetiapine, olanzapine, aripiprazole, asenapine on lithium, or divalproex. The second line includes monotherapy with carbamazepine, carbamazepine ER, ECT, or haloperidol and combination therapy with lithium plus divalproex. The third line of treatment includes monotherapy with chlorpromazine, clozapine, oxcarbazepine, tamoxifen, or cariprazine and combination therapy with lithium or divalproex plus haloperidol, lithium plus carbamazepine, or adjunctive tamoxifen. They do not recommend monotherapy with gabapentin, topiramate, lamotrigine, verapamil, or tiagabine and combination therapy with risperidone or olanzapine plus carbamazepine.
For the treatment of acute BD-I depression as first line option they recommend monotherapy with lithium, lamotrigine, quetiapine, or quetiapine XR and combination therapy with lithium or divalproex or olanzapine plus an SSRI, lithium plus divalproex and lithium, or divalproex plus bupropion. The second line includes monotherapy with divalproex or lurasidone and combination therapy with quetiapine plus an SSRI, adjunctive modafinil, and lithium or divalproex plus lamotrigine or lurasidone. The third line includes monotherapy with carbamazepine, olanzapine, or ECT or combination therapy with lithium plus carbamazepine or pramipexole, lithium or divalproex plus venlafaxine, lithium plus MAOI, lithium or divalproex or atypical antipsychotic plus a TCA, lithium or divalproex or carbamazepine plus an SSRI plus lamotrigine, and quetiapine plus lamotrigine. They do not recommend monotherapy with gabapentin, aripiprazole, or ziprasidone and combination therapy with adjunctive ziprasidone or levetiracetam.
For the maintenance treatment, the first line recommendation includes monotherapy with lithium, lamotrigine, divalproex, olanzapine, quetiapine, risperidone LAI, and aripiprazole and adjunctive therapy with quetiapine, risperidone LAI, aripiprazole,e or ziprasidone on lithium or divalproex. The second line monotherapy includes carbamazepine and paliperidone ER and combination therapy with lithium plus divalproex or carbamazepine, lithium or divalproex plus olanzapine, risperidone or lamotrigine, and olanzapine plus fluoxetine. The third line monotherapy includes asenapine and the adjunctive therapy includes phenytoin, clozapine, ECT, topiramate, omega-3-fatty acids, oxcarbazepine, gabapentin, and asenapine. They do not recommend monotherapy with gabapentin, topiramate, or antidepressants and adjunctive therapy with flupenthixol.
The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of BD
The latest WFSBP guidelines utilized a modified version of the PORT method to grade the data concerning efficacy (Grunze et al., 2009, 2010, 2013) and afterwards utilized a secondary classification to include also safety and tolerability.
For the treatment of acute mania, as first choice agents are ranked aripiprazole, valproate, risperidone, and ziprasidone. As second choice, olanzapine, quetiapine, asenapine, carbamazepine, haloperidol, and lithium were recommended. The third choice includes chlorpromazine, paliperidone, phenytoin, pimozide, and tamoxifen. The fourth includes amisulpride, clonazepam, clozapine, levetiracetam, lorazepam, nimodipine, oxcarbazepine, retigabine, zonisamide, zotepine, and ECT. The fifth and final choice includes verapamil. With the utilization of this classification, the WFSBP suggests that concerning the treatment of acute mania the first step includes monotherapy with first choice agents. The second step would be switching to another first-choice agent or combine 2 first choice agents. Similarly the third step includes combination of 2 first-choice agents. The fourth and fifth steps include combinations of agents essentially according to the judgement of the therapist.
For the treatment of acute bipolar depression, the WFSBP guidelines suggest that first choice agent is only quetiapine, while the next-best option includes olanzapine, fluoxetine, lamotrigine, valproate, OFC, lithium plus lamotrigine, adjunctive modafinil, NAC on lithium or valproate, and FEWP plus carbamazepine. A variety of combinations are proposed as next steps.
For the treatment during the maintenance phase the guidance is more complex and on the basis of the available data the WFSBP guidelines suggest the use of aripiprazole, lamotrigine, lithium, quetiapine, olanzapine, and risperidone, but they note that not all of them prevent both mania and depression. They also note the problems because of the metabolic syndrome induced by some of these agents when used for prolonged periods of time. They also suggest the avoidance of typical antipsychotics because of the risk to induce tardive dyskinesia.
British Association for Psychopharmacology
The 2016 British Association for Psychopharmacology guidelines for the treatment of BD (Goodwin et al., 2016) recommend for acute mania antidopaminergic agents, lithium, or valproate. For acute bipolar depression they recommend quetiapine, olanzapine, olanzapine plus fluoxetine, antidepressants, lurasidone, and lamotrigine as combination. It also recommends family focused therapy, IPSRT, and CBT as add-on to medication but also CBT as monotherapy as an extrapolation of unipolar depression studies. For the maintenance phase they recommend lithium (for mania, depression, and suicide), dopamine antagonists, and partial agonists as well as valproate (mainly for mania), lamotrigine (for depression), and family focused therapy, CBT, and IPSRT as add-on to medication.
The UK NICE Treatment Guidelines for BD
Concerning acute mania, the 2014 NICE (NICE, 2014) guidelines recommend the use of olanzapine, risperidone, quetiapine, or haloperidol. If the patient does not respond it is recommended to change to another antipsychotic, and the choice should be made also on the basis of previous response if it exists. If the patient is already under treatment with lithium or valproate then the recommendation is to increase dosage to the highest permitted, and reassessment should follow before the changing of medication. If an antidepressant is in place, it should be discontinued. The second step includes combination of lithium or valproate plus an antipsychotic and the third step demands hospitalization. The NICE warns against the use of gabapentin, lamotrigine, and topiramate in acute mania.
For acute bipolar depression, the NICE recommends olanzapine, OFC, quetiapine, lamotrigine, lithium, and valproate. If the patient is already under treatment with lithium or valproate then the recommendation is to increase the dosage to the highest permitted, and reassessment should follow before the changing of medication. The next step includes combination of lithium or valproate plus quetiapine or OFC. The third step includes lithium plus lamotrigine or olanzapine and valproate plus lamotrigine. The NICE warns against the use of gabapentin and topiramate.
During the maintenance phase, the NICE guidelines recommend as first line treatment the continuation of the treatment the patient received during the acute phase and led to the resolution of the symptoms. Irrespective of predominant polarity the continuation of this treatment should be done for at least 3 to 6 months. In case the patient does not wish to follow this, it is recommended to change treatment to lithium, olanzapine, quetiapine, valproate, or lithium plus valproate. Again, NICE warns against the use of gabapentin and topiramate.
The procedure and the interpretation of evidence as presented in the NICE guidelines have been criticized (Jauhar et al., 2016).
Efficacy, Recommendation Level, and Precise Treatment Algorithm
The detailed table of the efficacy level for all treatment options during all phases and against specific features of BD is shown in web appendix 1. The detailed table of the recommendation level for all treatment options during all phases and against specific features of BD is shown in web appendix 2. Add-on and combination data were merged for the sake of simplicity. Additionally, the detailed precise algorithm that was developed is shown in web appendix 3.
The levels of recommendation concerning monotherapy in acute mania and recommended dosages for medication options are shown in Table 11, while the recommendation levels for combination treatment are shown in Table 12. Recommendation levels concerning treatment options for rapid cycling patients are shown in Table 13 and the effects on concomitant depressive and psychotic features are shown in Table 14. The recommendation levels for monotherapy and combination treatment in patients with a DSM-IV-TR mixed episode and the specific effects on the manic and the depressive component are shown in Table 15 (provided here for academic reasons).
Table 11.
Levels of Recommendation Concerning Monotherapy in Acute Mania and Recommended Dosages for Medication Options
| Agent/modality | Recommendation level | Recommended dosage (mg/d) |
|---|---|---|
| Aripiprazole | 1 | 15–30 mg/d |
| Asenapine | 1 | 10–20 mg/d |
| Cariprazine | 1 | 3–12 mg/d |
| Paliperidone | 1 | 3–12 mg/d |
| Quetiapine | 1 | 400–800 mg/d |
| Risperidone | 1 | 2–6 mg/d |
| Valproate | 1 | 1200–3000 mg/d (loading dose 20–30 mg/kg body weight; serum level 75–150 mg) |
| Carbamazepine | 2 | 600–1200 mg/d (serum level 4–15 mg/L) |
| Haloperidol | 2 | 5–20 mg/d |
| Lithium | 2 | 600–1200 mg/d (serum level 0.8–1.3 mmol) |
| Olanzapine | 2 | 10–20 mg/d |
| ECT | 3 | |
| Oxcarbazepine | 4 | 900–1800 mg/d |
| Chlorpromazine | 4 | 300–1000 mg/d |
| Pimozide | 4 | 2–16 mg/d |
| Tamoxifen | 4 | 40–80 mg/d |
| Ziprasidone | 4 | 80–160 mg/d` |
| Eslicarbazepine | 5 | |
| Gabapentin | 5 | |
| Lamotrigine | 5 | |
| Licarbazepine | 5 | |
| TMS | 5 | |
| Topiramate | 5 | |
| Verapamil | 5 |
Abbreviations: ECT, electroconvulsive therapy; NR: not recommended; TMS, transcranial magnetic stimulation.
Table 12.
Recommendation levels for combination treatment for acute mania
| Agent/modality | MS | Li | Val | Cbz | FGAs |
|---|---|---|---|---|---|
| Asenapine | 1 | - | - | - | - |
| Haloperidol | 2 | 2 | 2 | 2 | - |
| Olanzapine | 2 | - | 2 | 5 | - |
| Aripiprazole | 2 | - | - | - | - |
| Medroxyprogesterone | 5 | - | - | - | - |
| Celecoxib | - | - | 2 | - | - |
| Quetiapine | 3 | 3 | - | - | - |
| Risperidone | 3 | - | 5 | - | - |
| Tamoxifen | 4 | 4 | - | - | - |
| Allopurinol | 5 | 2 | - | - | 5 |
| Paliperidone | 5 | - | - | - | - |
| Ziprasidone | 5 | - | - | - | - |
| Gabapentin | 5 | - | - | - | - |
| Topiramate | 5 | - | - | - | - |
| Lamotrigine | - | - | - | - | - |
| Lithium | - | - | - | 2 | - |
| Oxcarbazepine | - | 4 | - | - | - |
| Valproate | - | - | - | - | 2 |
Abbreviaitons: Cbz, carbamazepine; FGA, first generation antipsychotic; Li, lithium; MS, mood stabilizer; Val, valproate.
Table 13.
Recommendation Levels for Monotherapy in Rapid Cycling Patients in an Acute Manic Episode
| Agent/modality | Recommendation level |
|---|---|
| Quetiapine | 3 |
| Aripiprazole | 3 |
| Olanzapine | 3 |
| Valproate | 4 |
| Lithium | 4 |
Table 14.
Recommendation Levels for Monotherapy in Patients in an Acute Manic Episode and the Specific Effect on Concomitant Depressive Symptoms (Mixed Features) and Psychotic Features
| Agent/modality | Therapeutic effect on | ||
|---|---|---|---|
| Overall on manic episode | Concomitant Depressive symptoms | Psychotic symptoms | |
| Quetiapine | 1 | 3 | 3 |
| Risperidone | 1 | 3 | 3 |
| Aripiprazole | 1 | 5 | 3 |
| Asenapine | 1 | 5 | - |
| Olanzapine | 2 | 3 | 3 |
| Carbamazepine | 2 | 5 | - |
| Cariprazine | 1 | 5 | - |
| Haloperidol | 2 | 5 | 3 |
| Lithium | 2 | 5 | 3 |
| Tamoxifen | 4 | 5 | 4 |
| Valproate | 1 | 5 | - |
| Ziprasidone | 2 | 5 | 3 |
Table 15.
Recommendation Levels for Monotherapy and Combination Treatment in Patients in a DSM-IV-TR Mixed Episode and the Specific Effect on the Manic and the Depressive Component
| Monotherapy | Combination with MS | |||
|---|---|---|---|---|
| Agent/modality | Manic component | Depressive component | Manic component | Depressive component |
| Olanzapine | 3 | 3 | 2 | 2 |
| Asenapine | 3 | 3 | - | - |
| Aripiprazole | 3 | 3 | - | - |
| Carbamazepine | 3 | 3 | - | - |
| Valproate | 3 | 4 | - | - |
| Paliperidone | 3 | 5 | - | - |
| Risperidone | 3 | - | 5 | 5 |
| OFC | 4 | 4 | - | - |
| Ziprasidone | 4 | 4 | - | - |
| Lithium | 5 | - | - | - |
| Quetiapine | 5 | - | - | - |
| Celecoxib | - | - | 5 | 5 |
| Haloperidol | - | - | 5 | 5 |
Abbreviations: MS, mood stabilizer; OFC, olanzapine-fluoxetine combination.
The chart of the algorithm for acute mania/hypomania on the basis of strict evidence and by taking into consideration specific clinical features is shown in Table 16. The comparison of this algorithm to previously developed guidelines for acute mania is shown in Table 17.
Table 16.
Precise Evidence-Based Alrogithm to Treat Acute Manic Episodes on the Basis of Specific Clinical Characteristics
| Step | First | Second | Third | Fourth | Fifth |
|---|---|---|---|---|---|
| All cases | Discontinue treatment with antidepressants | ||||
| Rapid cycling | Start with aripiprazole or quetiapine monotherapy. In nonpsychotic cases valproate is also an option Take into consideration the previous history of psychotic features. | Olanzapine or lithium monotherapy | Combination treatment of lithium or valproate with quetiapine, or risperidone. | Apply ECT on top of pharmacological treatment. Monotherapy with chlorpromazine, pimozide, or tamoxifen. Options are also combination treatments of lithium or valproate plus tamoxifen or the combination of risperidone or oxcarbazepine plus lithium | Various combinations of medication according to anecdotal knowledge or the personal experience of the therapist, ECT if not applied earlier |
| Nonrapid cycling with psychotic features | Start with aripiprazole, cariprazine, paliperidone, quetiapine, or risperidone monotherapy. | Monotherapy with haloperidol, lithium, olanzapine or ziprasidone or combination treatment of lithium or valproate with aripiprazole, haloperidol or olanzapine. Lithium combinations with allopurinol* is also an option. Another combination is valproate plus an FGA. | |||
| Nonrapid cycling without psychotic features | All options that are suitable in the presence of psychotic features and also valproate and asenapine monotherapy are a choice. Take into consideration the previous history of psychotic features. | All options that are suiTable in the presence of psychotic features and also monotherapy with carbamazepine or valproate plus celecoxib* are an option Take into consideration the previous history of psychotic features. | |||
| Mixed Features | Start with quetiapine or risperidone monotherapy. | Olanzapine monotherapy | |||
| All other cases | If the patient is already under one of the above ‘first step’ monotherapy or under combination therapy of any kind and response is unsatisfactory, switch into another ‘first step’ monotherapy. | ||||
| In case the personal history of the patient suggests this is not an option, proceed to next step and switch to the closest second step treatment option. | Proceed to next step | ||||
| Mixed episode | Start with combination of olanzapine plus valproate or maybe lithium | Monotherapy with olanzapine, aripiprazole, or carbamazepine. | Valproate monotherapy | OFC or ziprasidone monotherapy. |
Abbreviations: CBT, cognitive behavioral treatment; Cbz, carbamazepine; ECT, electroconvulsive therapy; IPSRT, InterPersonal and Social Rhythms Therapy; Lam, lamotrigine; Li, lithium; MS, mood stabilizer; OFC, olanzapine fluoxetine combination; rTMS, repetitive Transcranial Magnetic Stimulation; Val, valproate.
*No wide clinical experience.
The levels of recommendation concerning monotherapy in acute bipolar depression, in comorbid conditions, and rapid cycling patients and recommended dosages for medication options are shown in Table 18, while the levels of recommendation concerning combination treatment are shown in Table 19.
Table 18.
Level of Recommendation Concerning Monotherapy in Acute Bipolar Depression, in Comorbid Conditions and Rapid Cycling Patients, and Recommended Dosages for Medication Options
| Agent/modality | Overall | BD-I | BD-II | Depressive core | Comorbid anxiety | Rapid cycling | Recommended dosage (mg/d) |
|---|---|---|---|---|---|---|---|
| Quetiapine | 1 | 3 | 3 | 3 | 3 | 2 | 300–600 mg/d |
| Lurasidone | 1 | - | - | 3 | 3 | - | 20–120 mg/d |
| OFC | 2 | 2 | - | 3 | - | - | 6 + 25; 6 + 50; 12 + 50 mg/d |
| Escitalopram | - | - | 1 | - | - | - | 10 mg/d |
| Fluoxetine | 2 | - | 3 | - | - | - | 20–80 mg/d |
| Olanzapine | 2 | 4 | - | 3 | - | - | 5–20 mg/d |
| Carbamazepine | 3 | - | - | - | - | - | 300–800 mg/d |
| Valproate | 3 | 3 | 5 | 3 | 3 | 4 | 500–2500 mg/d (50–100 mcg/mL) |
| Aripiprazole | 3 | 3 | - | - | - | - | 5–30 mg/d |
| Imipramine | 3 | - | - | - | - | - | 75–300 mg/d |
| Lamotrigine | 3 | 3 | 3 | 3 | - | - | 50–200 mg/d |
| Phenelzine | 3 | - | - | - | - | - | 15–90 mg/d |
| Lithium | 4 | - | 4 | - | 5 | 3 | 600–1800 mg/d |
| Tranylcypromine | 4 | 4 | 4 | - | - | - | 20–30 mg/d |
| Venlafaxine | 4 | 4 | 4 | - | - | - | 75–225 mg/d |
| Paroxetine | 5 | 5 | 5 | - | 3 | 5 | 20 mg/d |
| Ziprasidone | 5 | 5 | - | - | 5 | - | |
| Gabapentin | 5 | - | - | - | - | - | |
| rTMS | 5 | - | - | - | - | - | |
| Risperidone | - | - | - | - | 5 | - |
Abbreviations: NR, not recommended; OFC, olanzapine-fluoxetine combination; rTMS, repetitive Transcranial Magnetic Stimulation.
Table 19.
Level of Recommendation Concerning Combination Treatment in Acute Bipolar Depression
| Agent/modality | MS | Cbz | Lam | Li | Val |
|---|---|---|---|---|---|
| Lurasidone | 2 | - | - | - | - |
| Modafinil | 2 | - | - | - | - |
| Pramipexole | 2 | - | - | - | - |
| Pioglitazone | - | - | - | 2 | - |
| Armodafinil | 4 | - | - | - | - |
| Ketamine | 4 | - | - | - | - |
| Paroxetine | 5 | 5 | - | 5 | 5 |
| Ziprasidone | 5 | - | 5 | 5 | 5 |
| Bupropion | 5 | - | - | - | - |
| Celecoxib | 5 | - | - | - | - |
| Levetiracetam | 5 | - | - | - | - |
| Levothyroxine (L-T4) | 4 | - | - | - | - |
| Risperidone | 5 | - | - | - | - |
| Lithium | - | - | 2 | - | - |
| Memantine | - | - | 5 | - | - |
| FEWP | - | 4 | - | - | - |
| Oxcarbazepine | - | - | - | 4 | - |
| Lamotrigine | - | - | - | 2 | - |
| L-sulpiride | - | - | - | 3 | - |
| Fluoxetine | - | - | - | 4 | - |
| Agomelatine | 5 | - | - | 5 | 5 |
| Aripiprazole | - | - | - | 5 | - |
| Imipramine | - | - | - | 5 | - |
Abbreviations: Cbz, carbamazepine; FEWP, Free and Easy Wanderer Plus (herbal agent); Lam, lamotrigine; MS, mood stabilizer; Val, valproate.
The chart of the algorithm for acute bipolar depression is shown in Table 20. The comparison of this algorithm to previously developed guidelines for acute bipolar depression is shown in Table 21.
Table 20.
Precise Algorithm to Treat Acute Bipolar Depressive Episodes on the Basis of Specific Clinical Characteristics
| Steps | First | Second | Third | Fourth | Fifth |
|---|---|---|---|---|---|
| Overall | Start with quetiapine or lurasidone Consider CBT as add-on to medication and according to the patient preference and to availability. Never consider CBT as monotherapy |
Add a mood stabilizer on lurasidone, modafinil or pramipexole Lithium plus lamotrigine, or pioglitazone* Olanzapine monotherapy or OFC |
Valproate, aripiprazole, imipramine, phenelzin, carbamazepine or lamotrigine monotherapy Lithium plus L-sulpiride |
Tranylcypromine or lithium monotherapy Venlafaxine preferably in combination with an antimanic agent Armodafinil or ketamine on a mood stabilizer Lithium plus fluoxetine Carbamazepine plus FEWP Mood stabilizer plus levothyroxine (L-T4) Lithium plus oxcarbazepine |
ECT or various combinations of medication according to anecdotal knowledge or the personal experience of the therapist |
| Rapid cycling | If BD-I start with valproate, in BD-II with lithium | ||||
| No rapid cycling | If BD-II start with escitalopram or fluoxetine monotherapy | ||||
| Comorbid anxiety |
Add paroxetine, quetiapine, valproate or lurasidone and consider Mindfulness based interventions as add-on to these agents |
Abbreviations: CBT, cognitive behavioral treatment; Cbz, carbamazepine; ECT, electroconvulsive therapy; FEWP, Free and Easy Wanderer Plus (herbal agent); IPSRT, InterPersonal and Social Rhythms Therapy; Lam, lamotrigine; Li, lithium; MS, mood stabilizer
OFC, olanzapine fluoxetine combination; rTMS, repetitive Transcranial Magnetic Stimulation; Val, valproate.
*No wide clinical experience.
The levels of recommendation concerning monotherapy during the maintenance phase and in relationship to index episode, composition of the sample, presence of rapid cycling, and the efficacy in the prevention of manic, mixed, or depressive episodes as well as recommended dosages are shown in Table 22, while the levels of recommendation concerning combination treatment during the maintenance phase are shown in Table 23.
Table 22.
Level of Recommendation Concerning Monotherapy during the Maintenance Phase and in Relationship to Index Episode, Composition of the sample, Presence of Rapid Cycling and the Efficacy in the Prevention of Mainic, Mixed or Depressive Episodes as Well as Recommended Dosages
| Agent/modality | Index episode | Enriched sample | Manic | Depressive | Mixed | Rapid cycling | Recommended dosage |
|---|---|---|---|---|---|---|---|
| Quetiapine | m/d | Yes | 2 | 2 | - | Quet+ Val/Li (3) | 300–800 mg/d |
| Olanzapine | m | Yes/No | 2 | 2 | 2 | - | 5–20 mg/d |
| Lithium | m/d | No | 2 | 3 | - | Li, Li + Cbz (3) | 0.6–1.2 mEq/L |
| Lamotrigine | m/d | Yes | 3 | 2 | - | 5 | 50–400 mg/d |
| Aripiprazole | m | Yes | 1 | 5 | - | 3 | 10–30 mg/d |
| RLAI | m | Yes | 1 | 5 | - | RLAI+TAU (3) | 25–50 mg/biweekly |
| Paliperidone | m | Yes | 2 | 5 | - | - | 3–12 mg/d |
| Valproate | m | Yes | 4 | 3 | - | - | 45–100 mg/L |
| Ziprasidone | m | Yes | - | - | - | - | 80–160 mg/d |
| Perphenazine | m | Yes | - | - | - | - | |
| Imipramine | d | ? | 5 | 5 | - | - | |
| Fluoxetine | d | Yes | - | 2 | - | - | 10–40 mg/d |
| CBT | d | No | - | - | - | - | |
| N-acetyl cysteine | d | Yes | - | - | - | - | |
| Carbamazepine | - | - | 4 | 4 | - | Li + Cbz (3) | 4–12 mg/L |
Abbreviations: CBT, cognitive behavioral therapy; Cbz, carbamazepine; Li, lithium; Quet, quetiapine; RLAI, Risperidone Long Acting Injection; TAU, treatment as usual; Val, valproate.
Enriched sample: the sample is enriched on the basis of remission after treatment with the agent under consideration during the acute phase (index episode).
Table 23.
Level of Recommendation Concerning Combination Treatment during the Maintenance Phase
| Agent/modality | MS | Cbz | Lam | Li | Val |
|---|---|---|---|---|---|
| Quetiapine | 1 | - | - | - | - |
| Aripiprazole | 2 | - | 5 | - | 5 |
| RLAI | 2 | - | - | - | - |
| CBT | 2 | - | - | - | - |
| Phenytoin | 2 | - | - | - | - |
| Paroxetine | 3 | - | - | - | - |
| Psychoeducation | 3 | - | - | - | - |
| Olanzapine | 4 | - | - | - | - |
| Ziprasidone | 4 | - | - | - | - |
| N-acetyl cysteine | 4 | - | - | - | - |
| Imipramine | - | - | - | 5 | - |
| Memantine | 5 | - | - | - | - |
| Oxcarbazepine | - | - | - | 5 | - |
| Lithium | - | - | 4 | - | - |
| Perphenazine | 5 | - | - | - | - |
Abbreviations: CBT, cognitive behavioral therapy; Cbz, carbamazepine; Lam, lamotrigine; Li, lithium; MS, mood stabilizer; RLAI, Risperidone Long Acting Injection; Val, valproate.
The chart of the algorithm for the maintenance phase is shown in Table 24. The comparison of this algorithm to previously developed guidelines for the maintenance phase is shown in Table 25.
Table 24.
Precise Algorithm to Treatment during the Maintenance Phase for BD on the Basis of Specific Clinical Characteristics
| Step | First | Second | Third | Fourth | Fifth |
|---|---|---|---|---|---|
| Depressive predominant polarity or No predominant polarity |
Quetiapine or olanzapine monotherapy | Add fluoxetine or lamotrigine | Add N-acetylcysteine | If depressive episodes keep emerging add an agent with proven efficacy against acute bipolar depression no matter whether it has proven maintenance efficacy. Consider adding venlafaxine or lithium plus lamotrigine. | Consider any combinations from steps 1–4 that have not been tried. Consider maintenance ECT Various combinations of medication according to anecdotal knowledge or the personal experience of the therapist Consider IPSRT as add- on to medication on the basis of clinical judgement of the therapist and according to the patient preference and to availability. Never consider IPSRT as monotherapy |
| Manic predominant polarity | Start with lithium, aripiprazole, olanzapine, paliperidone, quetiapine or risperidone (including RLAI) monotherapy | Add lithium on the first step option Lithium plus carbamazepine Quetiapine plus lithium or valproate |
If manic episodes keep emerging add RLAI on current treatment if not already in place Add N-acetylcysteine |
If manic episodes keep emerging add an agent that has proven efficacy against acute mania no matter whether it has proven maintenance efficacy. Consider haloperidol or lithium plus lamotrigine | |
| Mixed episodes are frequent | Olanzapine or aripiprazole plus a mood stabilizer | Add valproate, carbamazepine, or lamotrigine on second step treatment | Proceed to next step | ||
| Rapid cycling | Lithium monotherapy | ||||
| All cases | Consider CBT or psychoeducation as add-on to medication on the basis of clinical judgement of the therapist and according to the patient preference and to availability. Never consider CBT or psychoeducation as monotherapy | ||||
Abbreviations: CBT, cognitive behavioral treatment; Cbz, carbamazepine; ECT, electroconvulsive therapy; IPSRT, InterPersonal and Social Rhythms Therapy; Lam, lamotrigine; Li, lithium; MS, mood stabilizer.
Overall the algorithm consists of the stepwise approach in Tables 16, 20, and 24 and in web appendix 3. However, a more fundamental approach would be to utilize web appendix 2 that includes a table with the recommendation levels by clinical indication for all the treatment options. The utilization of this table could be more precise and accurate in comparison with the stepwise description. Until then, the clinician can handle the table in a manual way. First he or she should decide on the phase of the disorder (acute manic vs mixed vs depressive episode vs maintenance phase). Then he or she should choose the combination of the clinical features under the specific phase and finally he or she will identify that treatment options best fit the clinical syndrome. For example, if the patient is in an acute manic episode with some accompanying depressive symptoms (mixed features) and psychotic symptoms and his or her history suggests he or she is also a rapid cycling, then the only agents that treats all these conditions are olanzapine and quetiapine followed by lithium that is second choice. If the patient is BD-II in a depressive episode with anxiety, then the only suitable agent is quetiapine. Of course such an algorithm might be too restrictive; however, the clinician can use the table to produce combinations of treatment options to satisfy all clinical needs on the basis on research data.
Discussion
The current paper represents a systematic search of the literature on the treatment of BD. By using an established approach we identified all relevant RCTs pertaining to all faces and special issues of BD and graded the data according to a predetermined method. Finally, a recommendation level was assigned to all treatment options depending on the clinical situation.
It was interesting to see that except for rare cases, the concept of mood stabilizers is not supported by the available data, especially for those agents traditionally considered as such.
It is obvious that, by far, the body of evidence originates from RCTs that were conducted with agents that have been launched in the last 2 decades. This constitutes a significant bias in the literature, and one should be cautious in the way that the accumulated clinical experience concerning those agents and treatment modalities with poor evidence-based support should also be taken into account.
A low grade of evidence for these old and poorly studied agents and modalities (e.g., carbamazepine, clozapine, ECT, etc.) does not necessarily mean a lower effectiveness and safety in comparison with other drugs, but it still implies that the clinicians should be cautious in their application in patients with BD. Yet it is irrational to use different standards; on the one hand to study carefully and seek flaws in the design of major RCTs and on the other hand to accept a wide recommendation of agents with poor evidence-based support because of historical reasons. The authors of the current paper spent much time and effort to grade the agents on the basis of quantitative but also qualitative characteristics of the data available. This effort resulted in the development of a precise algorithm on the basis of a reproducible methodology.
Also, the results on those areas of interest that are not targeted as primary outcomes are reported in a nonsystematic way and therefore the grading of evidence is lower. Unfortunately these areas constitute the overwhelming clinical picture of BD.
As with many other guidelines, the inherent limitations of the literature as well as the unavoidable subjectivity of experts when making a recommendation (even when based on evidence) should be taken seriously into consideration by the clinicians when reading the current paper. Also negative results (level 5) should be taken very seriously into consideration, as they should be considered to be scientifically stronger in comparison with positive ones.
Further limitations include the heterogeneity of the RCTs that served as basis for the recommendations and the lack of trials assessing specific subpopulations, following the rules of stratified medicine (Schumann et al., 2014), or applying staging methods to psychopharmacology (Grande et al., 2015), in search of more precision when treating individual patients (Vieta, 2015). However, these CINP guidelines represent the most up-to-date effort to condense the current knowledge on the management of BD from an international perspective.
Statement of Interest
K.N.F. has received grants and served as consultant, advisor, or CME speaker for the following entities: AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Ferrer, Gedeon Richter, Janssen, Lundbeck, Otsuka, Pfizer, the Pfizer Foundation, Sanofi-Aventis, Servier, Shire, and others.
E.V. has received grants and served as consultant, advisor, or CME speaker for the following entities: Allergan, AstraZeneca, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Ferrer, Forest Research Institute, Gedeon Richter, Glaxo-Smith-Kline, Janssen, Lilly, Lundbeck, Otsuka, Pfizer, Roche, Sanofi-Aventis, Servier, Shire, Sunovion, Takeda, the Brain and Behaviour Foundation, the Spanish Ministry of Science and Innovation (CIBERSAM), the Seventh European Framework Programme (ENBREC), and the Stanley Medical Research Institute.
A.H.Y. is employed by King’s College London, is Honorary Consultant SLaM (NHS UK), has paid lectures by and participated in advisory boards for all major pharmaceutical companies with drugs used in affective and related disorders, and has no share holdings in pharmaceutical companies. He was lead investigator for Embolden Study (AZ), BCI Neuroplasticity Study, and Aripiprazole Mania Study; investigator-initiated studies from AZ, Eli Lilly, Lundbeck, and Wyeth; and has received grant funding (past and present) from NIHR-BRC (UK); NIMH (USA); CIHR (Canada); NARSAD (USA); Stanley Medical Research Institute (USA); MRC (UK); Wellcome Trust (UK); Royal College of Physicians (Edin); BMA (UK); UBC-VGH Foundation (Canada); WEDC (Canada); CCS Depression Research Fund (Canada); MSFHR (Canada); and NIHR (UK).
H.G. within the last 3 years received grant/research support from NIHR UK, MRC UK, and NTW NHS Foundation Trust and receipt of honoraria or consultation fees from Gedeon-Richter, Lundbeck, and Hofmann-LaRoche and participated in a company-sponsored speaker’s bureau for BMS, Ferrer, Janssen-Cilag, Otsuka, Lundbeck, and Pfizer.
L.Y. has been on speaker/advisory boards for or has received research grants from Alkermes, Allergan, AstraZeneca, Bristol Myers Squibb, CANMAT, CIHR, Eli Lilly, Forest, GlaxoSmithKline, Intas, Janssen, the Michael Smith Foundation for Health Research, Pfizer, Servier, Sumitomo Dainippon, Sunovion, and the Stanley Foundation.
S.K. within the last 3 years received grants/research support, consulting fees, and honoraria from Angelini, AOP Orphan Pharmaceuticals AG, AstraZeneca, Eli Lilly, Janssen, KRKA-Pharma, Lundbeck, Neuraxpharm, Pfizer, Pierre Fabre, Schwabe, and Servier.
H.J.M. received honoraria for lectures or for advisory activities or received grants by the following pharmaceutical companies: Lundbeck, Servier, Schwabe, and Bayer. He was president or in the executive board of the following organizations: CINP, ECNP, WFSBP, and EPA and chairman of the WPA-section on Pharmacopsychiatry.
P.B. has received research grants and honoraria for participation in advisory boards from and/or gave presentations to: Allergan, Astra Zeneca, Bristol Myers Squibb, Canadian Institute for Health Research, Eli Lilly, Lundbeck, Janssen, Ontario Brain Institute, Meda-Valeant, Merck, Otsuka, Pierre Fabre Medicaments, Pfizer, Shire, Sunovion, and Takeda.
Supplementary Material
Acknowledgments
The authors thank Professor Guy Goodwin for his valuable input in the authoring of this manuscript.
References
- (1997) Expert consensus guidelines are released for the treatment of bipolar disorder. Consensus Development Conferences. Am Fam Physician 55:1447–1449. [PubMed] [Google Scholar]
- (2008) International Consensus Group on the evidence-based pharmacologic treatment of bipolar I and II depression. J Clin Psychiatry 69:1632–1646. [DOI] [PubMed] [Google Scholar]
- (2009) NCT00329108 study results. In. [Google Scholar]
- AACAP (1997) AACAP official action. Practice parameters for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 36:138–157. [DOI] [PubMed] [Google Scholar]
- Aan Het Rot M, Zarate CA, Jr, Charney DS, Mathew SJ. (2012) Ketamine for depression: where do we go from here? Biol Psychiatry 72:537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdallah CG, Fasula M, Kelmendi B, Sanacora G, Ostroff R. (2012) Rapid antidepressant effect of ketamine in the electroconvulsive therapy setting. J ECT 28:157–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aberg-Wistedt A. (1982) Comparison between zimelidine and desipramine in endogenous depression. A cross-over study. Acta Psychiatr Scand 66:129–138. [DOI] [PubMed] [Google Scholar]
- Agosti V, Stewart JW. (2007) Efficacy and safety of antidepressant monotherapy in the treatment of bipolar-II depression. Int Clin Psychopharmacol 22:309–311. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Benazzi F. (2005) Psychopathologic correlates of suicidal ideation in major depressive outpatients: is it all due to unrecognized (bipolar) depressive mixed states? Psychopathology 38:273–280. [DOI] [PubMed] [Google Scholar]
- Allen MH, Currier GW, Hughes DH, Reyes-Harde M, Docherty JP. (2001) The Expert Consensus Guideline Series. Treatment of behavioral emergencies. Postgrad Med:1–88; quiz 89–90. [PubMed] [Google Scholar]
- Altshuler LL, Ventura J, van Gorp WG, Green MF, Theberge DC, Mintz J. (2004) Neurocognitive function in clinically sTable men with bipolar I disorder or schizophrenia and normal control subjects. Biol Psychiatry 56:560–569. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Suppes T, Black DO, Nolen WA, Leverich G, Keck PE, Jr, Frye MA, Kupka R, McElroy SL, Grunze H, Kitchen CM, Post R. (2006) Lower switch rate in depressed patients with bipolar II than bipolar I disorder treated adjunctively with second-generation antidepressants. Am J Psychiatry 163:313–315. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Post RM, Hellemann G, Leverich GS, Nolen WA, Frye MA, Keck PE, Jr, Kupka RW, Grunze H, McElroy SL, Sugar CA, Suppes T. (2009) Impact of antidepressant continuation after acute positive or partial treatment response for bipolar depression: a blinded, randomized study. J Clin Psychiatry 70:450–457. [DOI] [PubMed] [Google Scholar]
- Amann B, Born C, Crespo JM, Pomarol-Clotet E, McKenna P. (2010) Lamotrigine: when and where does it act in affective disorders? A systematic review. J Psychopharmacol 10:1289–1294. [DOI] [PubMed] [Google Scholar]
- Amrollahi Z, Rezaei F, Salehi B, Modabbernia AH, Maroufi A, Esfandiari GR, Naderi M, Ghebleh F, Ahmadi-Abhari SA, Sadeghi M, Tabrizi M, Akhondzadeh S. (2010) Double-blind, randomized, placebo-controlled 6-week study on the efficacy and safety of the tamoxifen adjunctive to lithium in acute bipolar mania. J Affect Disord 129:327–331. [DOI] [PubMed] [Google Scholar]
- Amsterdam JD, Garcia-Espana F. (2000) Venlafaxine monotherapy in women with bipolar II and unipolar major depression. J Affect Disord 59:225–229. [DOI] [PubMed] [Google Scholar]
- Amsterdam JD, Shults J. (2005. a) Comparison of fluoxetine, olanzapine, and combined fluoxetine plus olanzapine initial therapy of bipolar type I and type II major depression--lack of manic induction. J Affect Disord 87:121–130. [DOI] [PubMed] [Google Scholar]
- Amsterdam JD, Shults J. (2005. b) Fluoxetine monotherapy of bipolar type II and bipolar NOS major depression: a double-blind, placebo-substitution, continuation study. Int Clin Psychopharmacol 20:257–264. [DOI] [PubMed] [Google Scholar]
- Amsterdam JD, Shults J. (2010) Efficacy and safety of long-term fluoxetine versus lithium monotherapy of bipolar II disorder: a randomized, double-blind, placebo-substitution study. Am J Psychiatry 167:792–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amsterdam JD, Shults J, Brunswick DJ, Hundert M. (2004) Short-term fluoxetine monotherapy for bipolar type II or bipolar NOS major depression - low manic switch rate. Bipolar Disord 6:75–81. [DOI] [PubMed] [Google Scholar]
- Amsterdam JD, Lorenzo-Luaces L, Soeller I, Li SQ, Mao JJ, DeRubeis RJ. (2015) Safety and effectiveness of continuation antidepressant versus mood stabilizer monotherapy for relapse-prevention of bipolar II depression: A randomized, double-blind, parallel-group, prospective study. J Affect Disord 185:31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amsterdam JD, Garcia-Espana F, Fawcett J, Quitkin FM, Reimherr FW, Rosenbaum JF, Schweizer E, Beasley C. (1998) Efficacy and safety of fluoxetine in treating bipolar II major depressive episode. J Clin Psychopharmacol 18:435–440. [DOI] [PubMed] [Google Scholar]
- Anand A, Gunn AD, Barkay G, Karne HS, Nurnberger JI, Mathew SJ, Ghosh S. (2012) Early antidepressant effect of memantine during augmentation of lamotrigine inadequate response in bipolar depression: a double-blind, randomized, placebo-controlled trial. Bipolar Disord 14:64–70. [DOI] [PubMed] [Google Scholar]
- Andersohn F, Schade R, Willich SN, Garbe E. (2010) Use of antiepileptic drugs in epilepsy and the risk of self-harm or suicidal behavior. Neurology 75:335–340. [DOI] [PubMed] [Google Scholar]
- Angst F, Stassen HH, Clayton PJ, Angst J. (2002) Mortality of patients with mood disorders: follow-up over 34–38 years. J Affect Disord 68:167–181. [DOI] [PubMed] [Google Scholar]
- Angst J. (1985) Switch from depression to mania--a record study over decades between 1920 and 1982. Psychopathology 18:140–154. [DOI] [PubMed] [Google Scholar]
- APA (1994) Practice guideline for the treatment of patients with bipolar disorder. Am J Psychiatry 151:1–36. [DOI] [PubMed] [Google Scholar]
- APA (1995) American Psychiatric Association releases treatment guideline for bipolar disease. Am Fam Physician 51:1605–1606. [PubMed] [Google Scholar]
- APA (2002) Practice guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry 159:1–50. [PubMed] [Google Scholar]
- Arabzadeh S, Ameli N, Zeinoddini A, Rezaei F, Farokhnia M, Mohammadinejad P, Ghaleiha A, Akhondzadeh S. (2015) Celecoxib adjunctive therapy for acute bipolar mania: a randomized, double-blind, placebo-controlled trial. Bipolar Disord 17:606–614. [DOI] [PubMed] [Google Scholar]
- Arana A, Wentworth CE, Ayuso-Mateos JL, Arellano FM. (2010) Suicide-related events in patients treated with antiepileptic drugs. N Engl J Med 363:542–551. [DOI] [PubMed] [Google Scholar]
- Arnone D. (2005) Review of the use of Topiramate for treatment of psychiatric disorders. Ann Gen Psychiatry 4:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azorin JM, Sapin C, Weiller E. (2013) Effect of asenapine on manic and depressive symptoms in bipolar I patients with mixed episodes: results from post hoc analyses. J Affect Disord 145:62–69. [DOI] [PubMed] [Google Scholar]
- Baastrup PC, Poulsen JC, Schou M, Thomsen K, Amdisen A. (1970) Prophylactic lithium: double blind discontinuation in manic-depressive and recurrent-depressive disorders. Lancet 2:326–330. [DOI] [PubMed] [Google Scholar]
- Bailine S, Fink M, Knapp R, Petrides G, Husain MM, Rasmussen K, Sampson S, Mueller M, McClintock SM, Tobias KG, Kellner CH. (2010) Electroconvulsive therapy is equally effective in unipolar and bipolar depression. Acta Psychiatr Scand 121:431–436. [DOI] [PubMed] [Google Scholar]
- Baker RW, Goldberg JF, Tohen M, Milton DR, Stauffer VL, Schuh LM. (2002) The impact of response to previous mood stabilizer therapy on response to olanzapine versus placebo for acute mania. Bipolar Disord 4:43–49. [DOI] [PubMed] [Google Scholar]
- Baker RW, Tohen M, Fawcett J, Risser RC, Schuh LM, Brown E, Stauffer VL, Shao L, Tollefson GD. (2003) Acute dysphoric mania: treatment response to olanzapine versus placebo. J Clin Psychopharmacol 23:132–137. [DOI] [PubMed] [Google Scholar]
- Baker RW, Brown E, Akiskal HS, Calabrese JR, Ketter TA, Schuh LM, Trzepacz PT, Watkin JG, Tohen M. (2004) Efficacy of olanzapine combined with valproate or lithium in the treatment of dysphoric mania. Br J Psychiatry 185:472–478. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L, Hennen J. (2003. a) Lithium treatment and suicide risk in major affective disorders: update and new findings. J Clin Psychiatry 64Suppl 5:44–52. [PubMed] [Google Scholar]
- Baldessarini RJ, Hennen J, Wilson M, Calabrese J, Chengappa R, Keck PE, Jr, McElroy SL, Sachs G, Vieta E, Welge JA, Yatham LN, Zarate CA, Jr, Baker RW, Tohen M. (2003. b) Olanzapine versus placebo in acute mania: treatment responses in subgroups. J Clin Psychopharmacol 23:370–376. [DOI] [PubMed] [Google Scholar]
- Ball JR, Mitchell PB, Corry JC, Skillecorn A, Smith M, Malhi GS. (2006) A randomized controlled trial of cognitive therapy for bipolar disorder: focus on long-term change. J Clin Psychiatry 67:277–286. [DOI] [PubMed] [Google Scholar]
- Ballenger JC, Post RM. (1980) Carbamazepine in manic-depressive illness: a new treatment. Am J Psychiatry 137:782–790. [DOI] [PubMed] [Google Scholar]
- Barnes CW, Hadzi-Pavlovic D, Wilhelm K, Mitchell PB. (2015) A web-based preventive intervention program for bipolar disorder: outcome of a 12-months randomized controlled trial. J Affect Disord 174:485–492. [DOI] [PubMed] [Google Scholar]
- Baron M, Gershon ES, Rudy V, Jonas WZ, Buchsbaum M. (1975) Lithium carbonate response in depression. Prediction by unipolar/bipolar illness, average-evoked response, catechol-O-methyl transferase, and family history. Arch Gen Psychiatry 32:1107–1111. [DOI] [PubMed] [Google Scholar]
- Barreira P, Duckworth K, Goff D, Flannery RB., Jr (1999) Clinical practice guidelines: the Massachusetts experience in psychiatry. Harv Rev Psychiatry 7:230–232. [PubMed] [Google Scholar]
- Bauer M, Zaninelli R, Muller-Oerlinghausen B, Meister W. (1999. a) Paroxetine and amitriptyline augmentation of lithium in the treatment of major depression: a double-blind study. J Clin Psychopharmacol 19:164–171. [DOI] [PubMed] [Google Scholar]
- Bauer M, Berman S, Stamm T, Plotkin M, Adli M, Pilhatsch M, London ED, Hellemann GS, Whybrow PC, Schlagenhauf F. (2016) Levothyroxine effects on depressive symptoms and limbic glucose metabolism in bipolar disorder: a randomized, placebo-controlled positron emission tomography study. Molecular psychiatry 21:229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer MS, Whybrow PC. (1990) Rapid cycling bipolar affective disorder. II. Treatment of refractory rapid cycling with high-dose levothyroxine: a preliminary study. Arch Gen Psychiatry 47:435–440. [DOI] [PubMed] [Google Scholar]
- Bauer MS, Whybrow PC, Winokur A. (1990) Rapid cycling bipolar affective disorder. I. Association with grade I hypothyroidism. Arch Gen Psychiatry 47:427–432. [DOI] [PubMed] [Google Scholar]
- Bauer MS, Callahan AM, Jampala C, Petty F, Sajatovic M, Schaefer V, Wittlin B, Powell BJ. (1999. b) Clinical practice guidelines for bipolar disorder from the Department of Veterans Affairs. J Clin Psychiatry 60:9–21. [DOI] [PubMed] [Google Scholar]
- Baumhackl U, Biziere K, Fischbach R, Geretsegger C, Hebenstreit G, Radmayr E, Stabl M. (1989) Efficacy and tolerability of moclobemide compared with imipramine in depressive disorder (DSM-III): an Austrian double-blind, multicentre study. The British journal of psychiatry Supplement:78–83. [PubMed] [Google Scholar]
- Beaulieu S, Saury S, Sareen J, Tremblay J, Schutz CG, McIntyre RS, Schaffer A, Canadian Network for M, Anxiety Treatments Task F (2012) The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid substance use disorders. Ann Clin Psychiatry 24:38–55. [PubMed] [Google Scholar]
- Bech P. (2001) Meta-analysis of placebo-controlled trials with mirtazapine using the core items of the Hamilton Depression Scale as evidence of a pure antidepressive effect in the short-term treatment of major depression. Int J Neuropsychopharmacol 4:337–345. [DOI] [PubMed] [Google Scholar]
- Bech P. (2002) The Bech-Rafaelsen Mania Scale in clinical trials of therapies for bipolar disorder: a 20-year review of its use as an outcome measure. CNS Drugs 16:47–63. [DOI] [PubMed] [Google Scholar]
- Bech P. (2006) The full story of lithium. A tribute to Mogens Schou (1918–2005). Psychother Psychosom 75:265–269. [DOI] [PubMed] [Google Scholar]
- Behzadi AH, Omrani Z, Chalian M, Asadi S, Ghadiri M. (2009) Folic acid efficacy as an alternative drug added to sodium valproate in the treatment of acute phase of mania in bipolar disorder: a double-blind randomized controlled trial. Acta Psychiatr Scand 120:441–445. [DOI] [PubMed] [Google Scholar]
- Benazzi F, Berk M, Frye MA, Wang W, Barraco A, Tohen M. (2009) Olanzapine/fluoxetine combination for the treatment of mixed depression in bipolar I disorder: a post hoc analysis. J Clin Psychiatry 70:1424–1431. [DOI] [PubMed] [Google Scholar]
- Berk M, Ichim L, Brook S. (1999) Olanzapine compared with lithium in mania: a double-blind randomized controlled trial. Int Clin Psychopharmacol 14:339–343. [DOI] [PubMed] [Google Scholar]
- Berk M, Tiller JW, Zhao J, Yatham LN, Malhi GS, Weiller E. (2015) Effects of asenapine in bipolar I patients meeting proxy criteria for moderate-to-severe mixed major depressive episodes: a post hoc analysis. J Clin Psychiatry 76:728–734. [DOI] [PubMed] [Google Scholar]
- Berk M, Copolov DL, Dean O, Lu K, Jeavons S, Schapkaitz I, Anderson-Hunt M, Bush AI. (2008) N-acetyl cysteine for depressive symptoms in bipolar disorder--a double-blind randomized placebo-controlled trial. Biol Psychiatry 64:468–475. [DOI] [PubMed] [Google Scholar]
- Berk M, Dean OM, Cotton SM, Gama CS, Kapczinski F, Fernandes B, Kohlmann K, Jeavons S, Hewitt K, Moss K, Allwang C, Schapkaitz I, Cobb H, Bush AI, Dodd S, Malhi GS. (2012) Maintenance N-acetyl cysteine treatment for bipolar disorder: a double-blind randomized placebo controlled trial. BMC Med 10:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardo M, Dodd S, Gama CS, Copolov DL, Dean O, Kohlmann K, Jeavons S, Schapkaitz I, Anderson-Hunt M, Bush AI, Berk M. (2009) Effects of N-acetylcysteine on substance use in bipolar disorder: A randomised placebo-controlled clinical trial. Acta Neuropsychiatr 21:285–291. [DOI] [PubMed] [Google Scholar]
- Bersudsky Y, Applebaum J, Gaiduk Y, Sharony L, Mishory A, Podberezsky A, Agam G, Belmaker RH. (2010) Valnoctamide as a valproate substitute with low teratogenic potential in mania: a double-blind, controlled, add-on clinical trial. Bipolar Disord 12:376–382. [DOI] [PubMed] [Google Scholar]
- Bertilsson L, Tomson T. (1986) Clinical pharmacokinetics and pharmacological effects of carbamazepine and carbamazepine-10,11-epoxide. An update. Clin Pharmacokinet 11:177–198. [DOI] [PubMed] [Google Scholar]
- Berwaerts J, Melkote R, Nuamah I, Lim P. (2012. a) A randomized, placebo- and active-controlled study of paliperidone extended-release as maintenance treatment in patients with bipolar I disorder after an acute manic or mixed episode. J Affect Disord 138:247–258. [DOI] [PubMed] [Google Scholar]
- Berwaerts J, Xu H, Nuamah I, Lim P, Hough D. (2012. b) Evaluation of the efficacy and safety of paliperidone extended-release in the treatment of acute mania: a randomized, double-blind, dose-response study. J Affect Disord 136:e51–60. [DOI] [PubMed] [Google Scholar]
- Berwaerts J, Lane R, Nuamah IF, Lim P, Remmerie B, Hough DW. (2011) Paliperidone extended-release as adjunctive therapy to lithium or valproate in the treatment of acute mania: A randomized, placebo-controlled study. J Affect Disord 129:252–260. [DOI] [PubMed] [Google Scholar]
- Beynon S, Soares-Weiser K, Woolacott N, Duffy S, Geddes JR. (2009) Pharmacological interventions for the prevention of relapse in bipolar disorder: a systematic review of controlled trials. J Psychopharmacol 23:574–591. [DOI] [PubMed] [Google Scholar]
- Blackburn S, Oliart A, Garcia Rodriguez L, Perez Gutthann S. (1998) Antiepileptics and blood dyscrasias: A cohort study. Pharmacotherapy 18:1277. [PubMed] [Google Scholar]
- Bobo WV, Shelton RC. (2010) Risperidone long-acting injecTable (Risperdal Consta(R)) for maintenance treatment in patients with bipolar disorder. Expert Rev Neurother 10:1637–1658. [DOI] [PubMed] [Google Scholar]
- Bocchetta A, Bernardi F, Burrai C, Pedditzi M, Del Zompo M. (1993) A double-blind study of L-sulpiride versus amitriptyline in lithium-maintained bipolar depressives. Acta Psychiatr Scand 88:434–439. [DOI] [PubMed] [Google Scholar]
- Bond DJ, Lam RW, Yatham LN. (2010) Divalproex sodium versus placebo in the treatment of acute bipolar depression: a systematic review and meta-analysis. J Affect Disord 124:228–234. [DOI] [PubMed] [Google Scholar]
- Bond DJ, Noronha MM, Kauer-Sant’Anna M, Lam RW, Yatham LN. (2008) Antidepressant-associated mood elevations in bipolar II disorder compared with bipolar I disorder and major depressive disorder: a systematic review and meta-analysis. J Clin Psychiatry 69:1589–1601. [DOI] [PubMed] [Google Scholar]
- Bond DJ, Hadjipavlou G, Lam RW, McIntyre RS, Beaulieu S, Schaffer A, Weiss M, Canadian Network for M, Anxiety Treatments Task F (2012) The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid attention-deficit/hyperactivity disorder. Ann Clin Psychiatry 24:23–37. [PubMed] [Google Scholar]
- Bond K, Anderson IM. (2015) Psychoeducation for relapse prevention in bipolar disorder: a systematic review of efficacy in randomized controlled trials. Bipolar Disord 17:349–362. [DOI] [PubMed] [Google Scholar]
- Bora E, Vahip S, Akdeniz F, Gonul AS, Eryavuz A, Ogut M, Alkan M. (2007) The effect of previous psychotic mood episodes on cognitive impairment in euthymic bipolar patients. Bipolar Disord 9:468–477. [DOI] [PubMed] [Google Scholar]
- Bottlender R, Rudolf D, Strauss A, Moller HJ. (2001) Mood-stabilisers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patients. J Affect Disord 63:79–83. [DOI] [PubMed] [Google Scholar]
- Bottlender R, Sato T, Kleindienst N, Strauss A, Moller HJ. (2004) Mixed depressive features predict maniform switch during treatment of depression in bipolar I disorder. J Affect Disord 78:149–152. [DOI] [PubMed] [Google Scholar]
- Bourin MS, Severus E, Schronen JP, Gass P, Szamosi J, Eriksson H, Chandrashekar H. (2014) Lithium as add-on to quetiapine XR in adult patients with acute mania: a 6-week, multicenter, double-blind, randomized, placebo-controlled study. International journal of bipolar disorders 2:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowden CL. (2005) Atypical antipsychotic augmentation of mood stabilizer therapy in bipolar disorder. J Clin Psychiatry 66Suppl 3:12–19. [PubMed] [Google Scholar]
- Bowden CL, Vieta E, Ice KS, Schwartz JH, Wang PP, Versavel M. (2010) Ziprasidone plus a mood stabilizer in subjects with bipolar I disorder: a 6-month, randomized, placebo-controlled, double-blind trial. J Clin Psychiatry 71:130–137. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Collins MA, McElroy SL, Calabrese JR, Swann AC, Weisler RH, Wozniak PJ. (2005. a) Relationship of mania symptomatology to maintenance treatment response with divalproex, lithium, or placebo. Neuropsychopharmacology 30:1932–1939. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Singh V, Weisler R, Thompson P, Chang X, Quinones M, Mintz J. (2012) Lamotrigine vs lamotrigine plus divalproex in randomized, placebo-controlled maintenance treatment for bipolar depression. Acta Psychiatr Scand 126:342–350. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Grunze H, Mullen J, Brecher M, Paulsson B, Jones M, Vagero M, Svensson K. (2005. b) A randomized, double-blind, placebo-controlled efficacy and safety study of quetiapine or lithium as monotherapy for mania in bipolar disorder. J Clin Psychiatry 66:111–121. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Swann AC, Calabrese JR, Rubenfaer LM, Wozniak PJ, Collins MA, Abi-Saab W, Saltarelli M, Depakote ERMSG (2006) A randomized, placebo-controlled, multicenter study of divalproex sodium extended release in the treatment of acute mania. J Clin Psychiatry 67:1501–1510. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Brugger AM, Swann AC, Calabrese JR, Janicak PG, Petty F, Dilsaver SC, Davis JM, Rush AJ, Small JG, et al. (1994) Efficacy of divalproex vs lithium and placebo in the treatment of mania. The Depakote Mania Study Group. Jama 271:918–924. [PubMed] [Google Scholar]
- Bowden CL, Calabrese JR, Sachs G, Yatham LN, Asghar SA, Hompland M, Montgomery P, Earl N, Smoot TM, DeVeaugh-Geiss J, Lamictal 606 Study G (2003) A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently manic or hypomanic patients with bipolar I disorder. Arch Gen Psychiatry 60:392–400. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Calabrese JR, McElroy SL, Gyulai L, Wassef A, Petty F, Pope HG, Jr, Chou JC, Keck PE, Jr, Rhodes LJ, Swann AC, Hirschfeld RM, Wozniak PJ. (2000) A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Divalproex Maintenance Study Group. Arch Gen Psychiatry 57:481–489. [DOI] [PubMed] [Google Scholar]
- Brown D, Silverstone T, Cookson J. (1989) Carbamazepine compared with haloperidol in acute mania. Int Clin Psychopharmacol 4:229–238. [DOI] [PubMed] [Google Scholar]
- Brown E, Dunner DL, McElroy SL, Keck PE, Adams DH, Degenhardt E, Tohen M, Houston JP. (2009) Olanzapine/fluoxetine combination vs lamotrigine in the 6-month treatment of bipolar I depression. Int J Neuropsychopharmacol 12:773–782. [DOI] [PubMed] [Google Scholar]
- Brown EB, McElroy SL, Keck PE, Jr, Deldar A, Adams DH, Tohen M, Williamson DJ. (2006) A 7-week, randomized, double-blind trial of olanzapine/fluoxetine combination versus lamotrigine in the treatment of bipolar I depression. J Clin Psychiatry 67:1025–1033. [DOI] [PubMed] [Google Scholar]
- Brown ES, Garza M, Carmody TJ. (2008) A randomized, double-blind, placebo-controlled add-on trial of quetiapine in outpatients with bipolar disorder and alcohol use disorders. J Clin Psychiatry 69:701–705. [DOI] [PubMed] [Google Scholar]
- Brown ES, Park J, Marx CE, Hynan LS, Gardner C, Davila D, Nakamura A, Sunderajan P, Lo A, Holmes T. (2014) A randomized, double-blind, placebo-controlled trial of pregnenolone for bipolar depression. Neuropsychopharmacology 39:2867–2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown ES, Todd JP, Hu LT, Schmitz JM, Carmody TJ, Nakamura A, Sunderajan P, Rush AJ, Adinoff B, Bret ME, Holmes T, Lo A. (2015) A Randomized, Double-Blind, Placebo-Controlled Trial of Citicoline for Cocaine Dependence in Bipolar I Disorder. Am J Psychiatry 172:1014–1021. [DOI] [PubMed] [Google Scholar]
- Brugue E, Vieta E. (2007) Atypical antipsychotics in bipolar depression: neurobiological basis and clinical implications. Prog Neuropsychopharmacol Biol Psychiatry 31:275–282. [DOI] [PubMed] [Google Scholar]
- Burdick KE, Braga RJ, Nnadi CU, Shaya Y, Stearns WH, Malhotra AK. (2011) Placebo-controlled adjunctive trial of pramipexole in patients with bipolar disorder: targeting cognitive dysfunction. J Clin Psychiatry 73:103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdick KE, Braga RJ, Nnadi CU, Shaya Y, Stearns WH, Malhotra AK. (2012) Placebo-controlled adjunctive trial of pramipexole in patients with bipolar disorder: targeting cognitive dysfunction. J Clin Psychiatry 73:103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess S, Geddes J, Hawton K, Townsend E, Jamison K, Goodwin G. (2001) Lithium for maintenance treatment of mood disorders. Cochrane Database Syst Rev:CD003013. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Vieta E, Shelton MD. (2003. a) Latest maintenance data on lamotrigine in bipolar disorder. Eur Neuropsychopharmacol 13Suppl 2:S57–66. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Frye MA, Yang R, Ketter TA, Armodafinil Treatment Trial Study N (2014) Efficacy and safety of adjunctive armodafinil in adults with major depressive episodes associated with bipolar I disorder: a randomized, double-blind, placebo-controlled, multicenter trial. J Clin Psychiatry 75:1054–1061. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Bowden CL, Sachs GS, Ascher JA, Monaghan E, Rudd GD. (1999) A double-blind placebo-controlled study of lamotrigine monotherapy in outpatients with bipolar I depression. Lamictal 602 Study Group. J Clin Psychiatry 60:79–88. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Ketter TA, Youakim JM, Tiller JM, Yang R, Frye MA. (2010) Adjunctive armodafinil for major depressive episodes associated with bipolar I disorder: a randomized, multicenter, double-blind, placebo-controlled, proof-of-concept study. J Clin Psychiatry 71:1363–1370. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Shelton MD, Rapport DJ, Youngstrom EA, Jackson K, Bilali S, Ganocy SJ, Findling RL. (2005. a) A 20-month, double-blind, maintenance trial of lithium versus divalproex in rapid-cycling bipolar disorder. Am J Psychiatry 162:2152–2161. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Goldberg JF, Ketter TA, Suppes T, Frye M, White R, DeVeaugh-Geiss A, Thompson TR. (2006) Recurrence in bipolar I disorder: a post hoc analysis excluding relapses in two double-blind maintenance studies. Biol Psychiatry 59:1061–1064. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Keck PE, Jr, Starace A, Lu K, Ruth A, Laszlovszky I, Nemeth G, Durgam S. (2015) Efficacy and safety of low- and high-dose cariprazine in acute and mixed mania associated with bipolar I disorder: a double-blind, placebo-controlled study. J Clin Psychiatry 76:284–292. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Keck PE, Jr, Macfadden W, Minkwitz M, Ketter TA, Weisler RH, Cutler AJ, McCoy R, Wilson E, Mullen J. (2005. b) A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. Am J Psychiatry 162:1351–1360. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Suppes T, Bowden CL, Sachs GS, Swann AC, McElroy SL, Kusumakar V, Ascher JA, Earl NL, Greene PL, Monaghan ET. (2000) A double-blind, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. Lamictal 614 Study Group. J Clin Psychiatry 61:841–850. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Bowden CL, Sachs G, Yatham LN, Behnke K, Mehtonen OP, Montgomery P, Ascher J, Paska W, Earl N, DeVeaugh-Geiss J, Lamictal 605 Study G (2003. b) A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder. J Clin Psychiatry 64:1013–1024. [DOI] [PubMed] [Google Scholar]
- Cardoso Tde A, Campos Mondin T, Reyes AN, Zeni CP, Souza LD, da Silva RA, Jansen K. (2015) Biological Rhythm and Bipolar Disorder: Twelve-Month Follow-Up of a Randomized Clinical Trial. The Journal of nervous and mental disease 203:792–797. [DOI] [PubMed] [Google Scholar]
- Carlson BX, Ketter TA, Sun W, Timko K, McQuade RD, Sanchez R, Vester-Blokland E, Marcus R. (2012) Aripiprazole in combination with lamotrigine for the long-term treatment of patients with bipolar I disorder (manic or mixed): a randomized, multicenter, double-blind study (CN138-392). Bipolar Disord 14:41–53. [DOI] [PubMed] [Google Scholar]
- Cazorla P, Zhao J, Mackle M, Szegedi A. (2013) Asenapine effects on individual Young Mania Rating Scale items in bipolar disorder patients with acute manic or mixed episodes: a pooled analysis. Neuropsychiatric disease and treatment 9:409–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerullo MA, Strakowski SM. (2007) The prevalence and significance of substance use disorders in bipolar type I and II disorder. Subst Abuse Treat Prev Policy 2:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesta CE, Mansson M, Palm C, Lichtenstein P, Iliadou AN, Landen M. (2016) Polycystic ovary syndrome and psychiatric disorders: Co-morbidity and heritability in a nationwide Swedish cohort. Psychoneuroendocrinology 73:196–203. [DOI] [PubMed] [Google Scholar]
- Chapel S, Chiu YY, Hsu J, Cucchiaro J, Loebel A. (2016) Lurasidone Dose Response in Bipolar Depression: A Population Dose-response Analysis. Clin Ther 38:4–15. [DOI] [PubMed] [Google Scholar]
- Chen J, Lu Z, Zhang M, Zhang J, Ni X, Jiang X, Xu H, Heeramun-Aubeeluck A, Hu Q, Jin H, Davis JM. (2013) A randomized, 4-week double-blind placebo control study on the efficacy of donepezil augmentation of lithium for treatment of acute mania. Neuropsychiatric disease and treatment 9:839–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chengappa KN, Baker RW, Shao L, Yatham LN, Tohen M, Gershon S, Kupfer DJ. (2003) Rates of response, euthymia and remission in two placebo-controlled olanzapine trials for bipolar mania. Bipolar Disord 5:1–5. [DOI] [PubMed] [Google Scholar]
- Chiu CC, Huang SY, Chen CC, Su KP. (2005) Omega-3 fatty acids are more beneficial in the depressive phase than in the manic phase in patients with bipolar I disorder. J Clin Psychiatry 66:1613–1614. [DOI] [PubMed] [Google Scholar]
- Chou JC, Czobor P, Charles O, Tuma I, Winsberg B, Allen MH, Trujillo M, Volavka J. (1999) Acute mania: haloperidol dose and augmentation with lithium or lorazepam. J Clin Psychopharmacol 19:500–505. [DOI] [PubMed] [Google Scholar]
- Chouinard G, Annable L, Turnier L, Holobow N, Szkrumelak N. (1993) A double-blind randomized clinical trial of rapid tranquilization with I.M. clonazepam and I.M. haloperidol in agitated psychotic patients with manic symptoms. Can J Psychiatry 38:S114–121. [PubMed] [Google Scholar]
- Christodoulou GN, Lykouras EP. (1982) Abrupt lithium discontinuation in manic-depressive patients. Acta Psychiatr Scand 65:310–314. [DOI] [PubMed] [Google Scholar]
- Cipriani A, Rendell JM, Geddes JR. (2006. a) Haloperidol alone or in combination for acute mania. Cochrane Database Syst Rev 3:CD004362. [DOI] [PubMed] [Google Scholar]
- Cipriani A, Rendell J, Geddes JR. (2010) Olanzapine in the long-term treatment of bipolar disorder: a systematic review and meta-analysis. J Psychopharmacol 24:1729–1738. [DOI] [PubMed] [Google Scholar]
- Cipriani A, Hawton K, Stockton S, Geddes JR. (2013) Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ 346:f3646. [DOI] [PubMed] [Google Scholar]
- Cipriani A, Smith K, Burgess S, Carney S, Goodwin G, Geddes J. (2006. b) Lithium versus antidepressants in the long-term treatment of unipolar affective disorder. Cochrane Database Syst Rev:CD003492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cipriani A, Barbui C, Salanti G, Rendell J, Brown R, Stockton S, Purgato M, Spineli LM, Goodwin GM, Geddes JR. (2011) Comparative efficacy and acceptability of antimanic drugs in acute mania: a multiple-treatments meta-analysis. Lancet 378:1306–1315. [DOI] [PubMed] [Google Scholar]
- Citrome L. (2010) Ziprasidone HCl capsules for the adjunctive maintenance treatment of bipolar disorder in adults. Expert Rev Neurother 10:1031–1037. [DOI] [PubMed] [Google Scholar]
- Citrome L. (2012) Inhaled loxapine for agitation revisited: focus on effect sizes from 2 Phase III randomised controlled trials in persons with schizophrenia or bipolar disorder. Int J Clin Pract 66:318–325. [DOI] [PubMed] [Google Scholar]
- Citrome L, Ketter TA, Cucchiaro J, Loebel A. (2014) Clinical assessment of lurasidone benefit and risk in the treatment of bipolar I depression using number needed to treat, number needed to harm, and likelihood to be helped or harmed. J Affect Disord 155:20–27. [DOI] [PubMed] [Google Scholar]
- Citrome L, Du Y, Risinger R, Stankovic S, Claxton A, Zummo J, Bose A, Silverman BL, Ehrich EW. (2016) Effect of aripiprazole lauroxil on agitation and hostility in patients with schizophrenia. Int Clin Psychopharmacol 31:69–75. [DOI] [PubMed] [Google Scholar]
- Cohn JB, Collins G, Ashbrook E, Wernicke JF. (1989) A comparison of fluoxetine imipramine and placebo in patients with bipolar depressive disorder. Int Clin Psychopharmacol 4:313–322. [DOI] [PubMed] [Google Scholar]
- Coley KC, Scipio TM, Ruby C, Lenze EJ, Fabian TJ. (2009) Aripiprazole prescribing patterns and side effects in elderly psychiatric inpatients. Journal of psychiatric practice 15:150–153. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Sanchez-Moreno J, Palomino-Otiniano R, Reinares M, Goikolea JM, Benabarre A, Martinez-Aran A. (2009) Group psychoeducation for stabilised bipolar disorders: 5-year outcome of a randomised clinical trial. BrJPsychiatry 194:260–265. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Martinez-Aran A, Reinares M, Goikolea JM, Benabarre A, Torrent C, Comes M, Corbella B, Parramon G, Corominas J. (2003) A randomized trial on the efficacy of group psychoeducation in the prophylaxis of recurrences in bipolar patients whose disease is in remission. ArchGenPsychiatry 60:402–407. [DOI] [PubMed] [Google Scholar]
- Colom F, Reinares M, Pacchiarotti I, Popovic D, Mazzarini L, Martinez AA, Torrent C, Rosa AR, Palomino-Otiniano R, Franco C, Bonnin CM, Vieta E. (2010) Has number of previous episodes any effect on respones to group psychoeducation in bipolar patients? Acta Neuropsychiatrica 22:50–53. [DOI] [PubMed] [Google Scholar]
- Connelly CE, Davenport YB, Nurnberger JI., Jr (1982) Adherence to treatment regimen in a lithium carbonate clinic. Arch Gen Psychiatry 39:585–588. [DOI] [PubMed] [Google Scholar]
- Cookson J, Silverstone T, Wells B. (1981) Double-blind comparative clinical trial of pimozide and chlorpromazine in mania. A test of the dopamine hypothesis. Acta Psychiatr Scand 64:381–397. [DOI] [PubMed] [Google Scholar]
- Cookson J, Keck PE, Jr, Ketter TA, Macfadden W. (2007) Number needed to treat and time to response/remission for quetiapine monotherapy efficacy in acute bipolar depression: evidence from a large, randomized, placebo-controlled study. Int Clin Psychopharmacol 22:93–100. [DOI] [PubMed] [Google Scholar]
- Coppen A, Whybrow PC, Noguera R, Maggs R, Prange AJ., Jr (1972) The comparative antidepressant value of L-tryptophan and imipramine with and without attempted potentiation by liothyronine. Arch Gen Psychiatry 26:234–241. [DOI] [PubMed] [Google Scholar]
- Corp SA, Gitlin MJ, Altshuler LL. (2014) A review of the use of stimulants and stimulant alternatives in treating bipolar depression and major depressive disorder. J Clin Psychiatry 75:1010–1018. [DOI] [PubMed] [Google Scholar]
- Correll CU, Sheridan EM, DelBello MP. (2010) Antipsychotic and mood stabilizer efficacy and tolerability in pediatric and adult patients with bipolar I mania: a comparative analysis of acute, randomized, placebo-controlled trials. Bipolar Disord 12:116–141. [DOI] [PubMed] [Google Scholar]
- Costa RT, Cheniaux E, Rosaes PA, Carvalho MR, Freire RC, Versiani M, Range BP, Nardi AE. (2011) The effectiveness of cognitive behavioral group therapy in treating bipolar disorder: a randomized controlled study. Revista brasileira de psiquiatria 33:144–149. [DOI] [PubMed] [Google Scholar]
- Cowdry RW, Wehr TA, Zis AP, Goodwin FK. (1983) Thyroid abnormalities associated with rapid-cycling bipolar illness. Arch Gen Psychiatry 40:414–420. [DOI] [PubMed] [Google Scholar]
- Coxhead N, Silverstone T, Cookson J. (1992) Carbamazepine versus lithium in the prophylaxis of bipolar affective disorder. Acta Psychiatr Scand 85:114–118. [DOI] [PubMed] [Google Scholar]
- Cruz N, Sanchez-Moreno J, Torres F, Goikolea JM, Valenti M, Vieta E. (2010) Efficacy of modern antipsychotics in placebo-controlled trials in bipolar depression: a meta-analysis. Int J Neuropsychopharmacol 13:5–14. [DOI] [PubMed] [Google Scholar]
- Cundall RL, Brooks PW, Murray LG. (1972) A controlled evaluation of lithium prophylaxis in affective disorders. Psychol Med 2:308–311. [DOI] [PubMed] [Google Scholar]
- Cutler AJ, Datto C, Nordenhem A, Minkwitz M, Acevedo L, Darko D. (2011) Extended-release quetiapine as monotherapy for the treatment of adults with acute mania: a randomized, double-blind, 3-week trial. Clin Ther 33:1643–1658. [DOI] [PubMed] [Google Scholar]
- D’Souza R, Piskulic D, Sundram S. (2010) A brief dyadic group based psychoeducation program improves relapse rates in recently remitted bipolar disorder: a pilot randomised controlled trial. J Affect Disord 120:272–276. [DOI] [PubMed] [Google Scholar]
- Daly JJ, Prudic J, Devanand DP, Nobler MS, Lisanby SH, Peyser S, Roose SP, Sackeim HA. (2001) ECT in bipolar and unipolar depression: differences in speed of response. Bipolar Disord 3:95–104. [DOI] [PubMed] [Google Scholar]
- Dardennes R, Even C, Bange F, Heim A. (1995) Comparison of carbamazepine and lithium in the prophylaxis of bipolar disorders. A meta-analysis. Br J Psychiatry 166:378–381. [DOI] [PubMed] [Google Scholar]
- Dauphinais DR, Rosenthal JZ, Terman M, DiFebo HM, Tuggle C, Rosenthal NE. (2012) Controlled trial of safety and efficacy of bright light therapy vs negative air ions in patients with bipolar depression. Psychiatry Res 196:57–61. [DOI] [PubMed] [Google Scholar]
- Davis JM, Janicak PG, Hogan DM. (1999) Mood stabilizers in the prevention of recurrent affective disorders: a meta-analysis. Acta Psychiatr Scand 100:406–417. [DOI] [PubMed] [Google Scholar]
- Davis LL, Bartolucci A, Petty F. (2005) Divalproex in the treatment of bipolar depression: a placebo-controlled study. J Affect Disord 85:259–266. [DOI] [PubMed] [Google Scholar]
- de Barros PK, de OCL, Silval KI, Dias VV, Roso MC, Bandeira M, Colom F, Moreno RA. (2013) Efficacy of psychoeducation on symptomatic and functional recovery in bipolar disorder. Acta PsychiatrScand 127:153–158. [DOI] [PubMed] [Google Scholar]
- De Fruyt J, Deschepper E, Audenaert K, Constant E, Floris M, Pitchot W, Sienaert P, Souery D, Claes S. (2012) Second generation antipsychotics in the treatment of bipolar depression: a systematic review and meta-analysis. J Psychopharmacol 26:603–617. [DOI] [PubMed] [Google Scholar]
- de Vries C, van Bergen A, Regeer EJ, Benthem E, Kupka RW, Boks MP. (2013) The effectiveness of restarted lithium treatment after discontinuation: reviewing the evidence for discontinuation-induced refractoriness. Bipolar Disord 15:645–649. [DOI] [PubMed] [Google Scholar]
- Dean OM, Bush AI, Copolov DL, Kohlmann K, Jeavons S, Schapkaitz I, Anderson-Hunt M, Berk M. (2012) Effects of N-acetyl cysteine on cognitive function in bipolar disorder. Psychiatry Clin Neurosci 66:514–517. [DOI] [PubMed] [Google Scholar]
- Dell’Osso B, Mundo E, D’Urso N, Pozzoli S, Buoli M, Ciabatti M, Rosanova M, Massimini M, Bellina V, Mariotti M, Altamura AC. (2009) Augmentative repetitive navigated transcranial magnetic stimulation (rTMS) in drug-resistant bipolar depression. Bipolar Disord 11:76–81. [DOI] [PubMed] [Google Scholar]
- Denicoff KD, Smith-Jackson EE, Disney ER, Ali SO, Leverich GS, Post RM. (1997) Comparative prophylactic efficacy of lithium, carbamazepine, and the combination in bipolar disorder. J Clin Psychiatry 58:470–478. [DOI] [PubMed] [Google Scholar]
- Dennehy EB. (2000) Guidelines for treatment of bipolar disorder. Curr Psychiatry Rep 2:316–321. [DOI] [PubMed] [Google Scholar]
- Depp CA, Ceglowski J, Wang VC, Yaghouti F, Mausbach BT, Thompson WK, Granholm EL. (2015) Augmenting psychoeducation with a mobile intervention for bipolar disorder: a randomized controlled trial. J Affect Disord 174:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Lorenzo R, Amoretti A, Forghieri M, Fiorini F, Genedani S, Rigatelli M. (2007) Aripiprazole: effectiveness and safety under naturalistic conditions. Experimental and clinical psychopharmacology 15:569–575. [DOI] [PubMed] [Google Scholar]
- Diazgranados N, Ibrahim L, Brutsche NE, Newberg A, Kronstein P, Khalife S, Kammerer WA, Quezado Z, Luckenbaugh DA, Salvadore G, Machado-Vieira R, Manji HK, Zarate CA., Jr (2010) A randomized add-on trial of an N-methyl-D-aspartate antagonist in treatment-resistant bipolar depression. Arch Gen Psychiatry 67:793–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dierckx B, Heijnen WT, van den Broek WW, Birkenhager TK. (2012) Efficacy of electroconvulsive therapy in bipolar versus unipolar major depression: a meta-analysis. Bipolar Disord 14:146–150. [DOI] [PubMed] [Google Scholar]
- Donnelly EF, Goodwin FK, Waldman IN, Murphy DL. (1978) Prediction of antidepressant responses to lithium. Am J Psychiatry 135:552–556. [DOI] [PubMed] [Google Scholar]
- Dube S, Tollefson GD, Thase ME, Briggs SD, Van Campen LE, Case M, Tohen M. (2007) Onset of antidepressant effect of olanzapine and olanzapine/fluoxetine combination in bipolar depression. Bipolar Disord 9:618–627. [DOI] [PubMed] [Google Scholar]
- Dunner DL, Stallone F, Fieve RR. (1976) Lithium carbonate and affective disorders. V: A double-blind study of prophylaxis of depression in bipolar illness. Arch Gen Psychiatry 33:117–120. [DOI] [PubMed] [Google Scholar]
- Durgam S, Starace A, Li D, Migliore R, Ruth A, Nemeth G, Laszlovszky I. (2015) The efficacy and tolerability of cariprazine in acute mania associated with bipolar I disorder: a phase II trial. Bipolar Disord 17:63–75. [DOI] [PubMed] [Google Scholar]
- Durgam S, Earley W, Lipschitz A, Guo H, Laszlovszky I, Nemeth G, Vieta E, Calabrese JR, Yatham LN. (2016) An 8-Week randomized, double-blind, placebo-controlled evaluation of the safety and efficacy of cariprazine in patients with bipolar I depression. Am J Psychiatry 173:271–281. [DOI] [PubMed] [Google Scholar]
- Eden Evins A, Demopulos C, Nierenberg A, Culhane MA, Eisner L, Sachs G. (2006. a) A double-blind, placebo-controlled trial of adjunctive donepezil in treatment-resistant mania. Bipolar Disord 8:75–80. [DOI] [PubMed] [Google Scholar]
- Eden Evins A, Demopulos C, Yovel I, Culhane M, Ogutha J, Grandin LD, Nierenberg AA, Sachs GS. (2006. b) Inositol augmentation of lithium or valproate for bipolar depression. Bipolar Disord 8:168–174. [DOI] [PubMed] [Google Scholar]
- El-Mallakh RS, Marcus R, Baudelet C, McQuade R, Carson WH, Owen R. (2012) A 40-week double-blind aripiprazole versus lithium follow-up of a 12-week acute phase study (total 52 weeks) in bipolar I disorder. J Affect Disord 136:258–266. [DOI] [PubMed] [Google Scholar]
- El-Mallakh RS, Ghaemi SN, Sagduyu K, Thase ME, Wisniewski SR, Nierenberg AA, Zhang HW, Pardo TA, Sachs G. (2008) Antidepressant-associated chronic irriTable dysphoria (ACID) in STEP-BD patients. J Affect Disord 111:372–377. [DOI] [PubMed] [Google Scholar]
- El-Mallakh RS, Vohringer PA, Ostacher MM, Baldassano CF, Holtzman NS, Whitham EA, Thommi SB, Goodwin FK, Ghaemi SN. (2015) Antidepressants worsen rapid-cycling course in bipolar depression: a STEP-BD randomized clinical trial. J Affect Disord 184:318–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Mallakh RS, Vieta E, Rollin L, Marcus R, Carson WH, McQuade R. (2010) A comparison of two fixed doses of aripiprazole with placebo in acutely relapsed, hospitalized patients with bipolar disorder I (manic or mixed) in subpopulations (CN138-007). Eur Neuropsychopharmacol 20:776–783. [DOI] [PubMed] [Google Scholar]
- Emilien G, Maloteaux JM, Seghers A, Charles G. (1996) Lithium compared with valproic acid and carbamazepine in the treatment of mania: a statistical meta-analysis. Eur Neuropsychopharmacol 6:245–252. [DOI] [PubMed] [Google Scholar]
- Emrich HM, von Zerssen D, Kissling W, Moller HJ. (1981) Therapeutic effect of valproate in mania. Am J Psychiatry 138:256. [DOI] [PubMed] [Google Scholar]
- Emrich HM, von Zerssen D, Kissling W, Moller HJ, Windorfer A. (1980) Effect of sodium valproate on mania. The GABA-hypothesis of affective disorders. Archiv Psychiatrie Nervenkrankheiten 229:1–16. [DOI] [PubMed] [Google Scholar]
- Endicott J, Rajagopalan K, Minkwitz M, Macfadden W, Group BS. (2007) A randomized, double-blind, placebo-controlled study of quetiapine in the treatment of bipolar I and II depression: improvements in quality of life. Int Clin Psychopharmacol 22:29–37. [DOI] [PubMed] [Google Scholar]
- Engelsmann F, Katz J, Ghadirian AM, Schachter D. (1988) Lithium and memory: a long-term follow-up study. J Clin Psychopharmacol 8:207–212. [PubMed] [Google Scholar]
- Fan A, Berg A, Bresee C, Glassman LH, Rapaport MH. (2012) Allopurinol augmentation in the outpatient treatment of bipolar mania: a pilot study. Bipolar Disord 14:206–210. [DOI] [PubMed] [Google Scholar]
- FDA (2008) statistical review and evaluation: antiepileptic drugs and suicidality. Available online http://www.fda.gov/ohrms/dockets/ac/08/briefing/2008-4372b1-01-FDA.pdf. [Google Scholar]
- Fieve RR, Kumbaraci T, Dunner DL. (1976) Lithium prophylaxis of depression in bipolar I, bipolar II, and unipolar patients. Am J Psychiatry 133:925–929. [DOI] [PubMed] [Google Scholar]
- Findling RL, McNamara NK, Youngstrom EA, Stansbrey R, Gracious BL, Reed MD, Calabrese JR. (2005) Double-blind 18-month trial of lithium versus divalproex maintenance treatment in pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry 44:409–417. [DOI] [PubMed] [Google Scholar]
- Fond G, Loundou A, Rabu C, Macgregor A, Lancon C, Brittner M, Micoulaud-Franchi JA, Richieri R, Courtet P, Abbar M, Roger M, Leboyer M, Boyer L. (2014) Ketamine administration in depressive disorders: a systematic review and meta-analysis. Psychopharmacology (Berl) 231:3663–3676. [DOI] [PubMed] [Google Scholar]
- Fountoulakis K. (2015. a) Treatment guidelines. In: Bipolar disorder: an evidence-based guide to manic depression (Fountoulakis K, ed), pp 643–658. Berlin Heidelberg: Springer-Verlag. [Google Scholar]
- Fountoulakis K. (2015. b) Biological therapies. In: Bipolar disorder: an evidence-based guide to manic depression (Fountoulakis K, ed), pp 461–625. Berlin Heidelberg: Springer-Verlag. [Google Scholar]
- Fountoulakis K. (2015. c) Psychosocial Treatment and interventions. In: Bipolar disorder: an evidence-based guide to manic depression (Fountoulakis K, ed), pp 627–642. Berlin Heidelberg: Springer-Verlag. [Google Scholar]
- Fountoulakis K. (2015. d) Classification and epidemiology. In: Bipolar disorder: an evidence-based guide to manic depression (Fountoulakis K, ed), pp 341–360. Berlin Heidelberg: Springer-Verlag. [Google Scholar]
- Fountoulakis K. (2015. e) Comorbidity. In: Bipolar disorder: an evidence-based guide to manic depression (Fountoulakis K, ed), pp 225–340. Berlin Heidelberg: Springer-Verlag. [Google Scholar]
- Fountoulakis K. (2015. f) Personality Disorders (narcissistic, antisocial, borderline). In: Bipolar disorder: an evidence-based guide to manic depression (Fountoulakis K, ed), pp 197–204. Sp Berlin Heidelberg: Springer-Verlag. [Google Scholar]
- Fountoulakis K. (2015. g) Alcohol and substance use in BD patients. In: Bipolar disorder: an evidence-based guide to manic depression (Fountoulakis K, ed), pp 205–223. Berlin Heidelberg: Springer-Verlag. [Google Scholar]
- Fountoulakis KN. (2008) The contemporary face of bipolar illness: complex diagnostic and therapeutic challenges. CNS Spectr 13:763–774, 777-769. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN. (2012) Refractoriness in bipolar disorder: definitions and evidence-based treatment. CNS Neurosci Ther 18:227–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fountoulakis KN, Vieta E. (2008) Treatment of bipolar disorder: a systematic review of available data and clinical perspectives. Int J Neuropsychopharmacol 11:999–1029. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Kontis D. (2012) Mathematical coupling and the true role of baseline severity in acute mania trials. Neuropsychopharmacology 37:850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fountoulakis KN, Siamouli M. (2012) Comparative efficacy of anti-manic drugs in acute mania. Lancet 379:893–894; author reply 894. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Vieta E, Schmidt F. (2011. a) Aripiprazole monotherapy in the treatment of bipolar disorder: a meta-analysis. J Affect Disord 133:361–370. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Kelsoe JR, Akiskal H. (2012. a) Receptor targets for antidepressant therapy in bipolar disorder: an overview. J Affect Disord 138:222–238. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Giannakopoulos P, Kovari E, Bouras C. (2008. a) Assessing the role of cingulate cortex in bipolar disorder: neuropathological, structural and functional imaging data. Brain research reviews 59:9–21. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Gonda X, Vieta E, Schmidt F. (2009. a) Treatment of psychotic symptoms in bipolar disorder with aripiprazole monotherapy: a meta-analysis. Ann Gen Psychiatry 8:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fountoulakis KN, Gonda X, Siamouli M, Rihmer Z. (2009. b) Psychotherapeutic intervention and suicide risk reduction in bipolar disorder: a review of the evidence. J Affect Disord 113:21–29. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Gonda X, Vieta E, Rihmer Z. (2011. b) Class effect of pharmacotherapy in bipolar disorder: fact or misbelief? Ann Gen Psychiatry 10:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fountoulakis KN, Kontis D, Gonda X, Yatham LN. (2013) A systematic review of the evidence on the treatment of rapid cycling bipolar disorder. Bipolar Disord 15:115–137. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Kontis D, Gonda X, Siamouli M, Yatham LN. (2012. b) Treatment of mixed bipolar states. Int J Neuropsychopharmacol 15:1015–1026. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Vieta E, Sanchez-Moreno J, Kaprinis SG, Goikolea JM, Kaprinis GS. (2005) Treatment guidelines for bipolar disorder: a critical review. J Affect Disord 86:1–10. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Vieta E, Bouras C, Notaridis G, Giannakopoulos P, Kaprinis G, Akiskal H. (2008. b) A systematic review of existing data on long-term lithium therapy: neuroprotective or neurotoxic? Int J Neuropsychopharmacol 11:269–287. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Siamouli M, Panagiotidis P, Magiria S, Kantartzis S, Iacovides A, Kaprinis GS. (2008. c) Ultra short manic-like episodes after antidepressant augmentation with modafinil. Prog Neuropsychopharmacol Biol Psychiatry 32:891–892. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Gonda X, Samara M, Siapera M, Karavelas V, Ristic DI, Iacovides A. (2012. c) Antiepileptic drugs and suicidality. J Psychopharmacol 26:1401–1407. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Kasper S, Andreassen O, Blier P, Okasha A, Severus E, Versiani M, Tandon R, Moller HJ, Vieta E. (2012. d) Efficacy of pharmacotherapy in bipolar disorder: a report by the WPA section on pharmacopsychiatry. Eur Arch Psychiatry Clin Neurosci 262:1–48. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Gonda X, Baghai TC, Baldwin DS, Bauer M, Blier P, Gattaz W, Hasler G, Moller HJ, Tandon R, Vieta E, Kasper S. (2015) Report of the WPA section of pharmacopsychiatry on the relationship of antiepileptic drugs with suicidality in epilepsy. Int J Psychiatry Clin Pract 19:158–167. [DOI] [PubMed] [Google Scholar]
- Frances A, Docherty J, Kahn D. (1996) The expert consensus guideline series: treatment of bipolar disorder. J Clin Psychiatry 57:1–88. [Google Scholar]
- Frangou S, Lewis M, McCrone P. (2006) Efficacy of ethyl-eicosapentaenoic acid in bipolar depression: randomised double-blind placebo-controlled study. Br J Psychiatry 188:46–50. [DOI] [PubMed] [Google Scholar]
- Frangou S, Lewis M, Wollard J, Simmons A. (2007) Preliminary in vivo evidence of increased N-acetyl-aspartate following eicosapentanoic acid treatment in patients with bipolar disorder. J Psychopharmacol 21:435–439. [DOI] [PubMed] [Google Scholar]
- Frangou S, Donaldson S, Hadjulis M, Landau S, Goldstein LH. (2005) The Maudsley Bipolar Disorder Project: executive dysfunction in bipolar disorder I and its clinical correlates. Biol Psychiatry 58:859–864. [DOI] [PubMed] [Google Scholar]
- Frank E, Soreca I, Swartz HA, Fagiolini AM, Mallinger AG, Thase ME, Grochocinski VJ, Houck PR, Kupfer DJ. (2008) The role of interpersonal and social rhythm therapy in improving occupational functioning in patients with bipolar I disorder. AmJPsychiatry 165:1559–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz HA, Fagiolini AM, Grochocinski V, Houck P, Scott J, Thompson W, Monk T. (2005) Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. ArchGenPsychiatry 62:996–1004. [DOI] [PubMed] [Google Scholar]
- Freeman TW, Clothier JL, Pazzaglia P, Lesem MD, Swann AC. (1992) A double-blind comparison of valproate and lithium in the treatment of acute mania. Am J Psychiatry 149:108–111. [DOI] [PubMed] [Google Scholar]
- Frye MA, Yatham LN, Calabrese JR, Bowden CL, Ketter TA, Suppes T, Adams BE, Thompson TR. (2006) Incidence and time course of subsyndromal symptoms in patients with bipolar I disorder: an evaluation of 2 placebo-controlled maintenance trials. J Clin Psychiatry 67:1721–1728. [DOI] [PubMed] [Google Scholar]
- Frye MA, Ha K, Kanba S, Kato T, McElroy SL, Ozerdem A, Vazquez G, Vieta E. (2011) International consensus group on depression prevention in bipolar disorder. J Clin Psychiatry 72:1295–1310. [DOI] [PubMed] [Google Scholar]
- Frye MA, Ketter TA, Kimbrell TA, Dunn RT, Speer AM, Osuch EA, Luckenbaugh DA, Cora-Ocatelli G, Leverich GS, Post RM. (2000) A placebo-controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clin Psychopharmacol 20:607–614. [DOI] [PubMed] [Google Scholar]
- Frye MA, Yatham L, Ketter TA, Goldberg J, Suppes T, Calabrese JR, Bowden CL, Bourne E, Bahn RS, Adams B. (2009) Depressive relapse during lithium treatment associated with increased serum thyroid-stimulating hormone: results from two placebo-controlled bipolar I maintenance studies. Acta Psychiatr Scand 120:10–13. [DOI] [PubMed] [Google Scholar]
- Frye MA, Grunze H, Suppes T, McElroy SL, Keck PE, Jr, Walden J, Leverich GS, Altshuler LL, Nakelsky S, Hwang S, Mintz J, Post RM. (2007) A placebo-controlled evaluation of adjunctive modafinil in the treatment of bipolar depression. Am J Psychiatry 164:1242–1249. [DOI] [PubMed] [Google Scholar]
- Fyro B, Petterson U. (1977) A double-blind study of the prophylactic effect of lithium in manic-depressive disease. Acta Psychiatr Scand 269:17–22. [Google Scholar]
- Galling B, Garcia MA, Osuchukwu U, Hagi K, Correll CU. (2015) Safety and tolerability of antipsychotic-mood stabilizer co-treatment in the management of acute bipolar disorder: results from a systematic review and exploratory meta-analysis. Expert opinion on drug safety 14:1181–1199. [DOI] [PubMed] [Google Scholar]
- Gao K, Gajwani P, Elhaj O, Calabrese JR. (2005) Typical and atypical antipsychotics in bipolar depression. J Clin Psychiatry 66:1376–1385. [DOI] [PubMed] [Google Scholar]
- Gao K, Pappadopulos E, Karayal ON, Kolluri S, Calabrese JR. (2013) Risk for adverse events and discontinuation due to adverse events of ziprasidone monotherapy relative to placebo in the acute treatment of bipolar depression, mania, and schizophrenia. J Clin Psychopharmacol 33:425–431. [DOI] [PubMed] [Google Scholar]
- Gao K, Kemp DE, Fein E, Wang Z, Fang Y, Ganocy SJ, Calabrese JR. (2011) Number needed to treat to harm for discontinuation due to adverse events in the treatment of bipolar depression, major depressive disorder, and generalized anxiety disorder with atypical antipsychotics. J Clin Psychiatry 72:1063–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao K, Wu R, Kemp DE, Chen J, Karberg E, Conroy C, Chan P, Ren M, Serrano MB, Ganocy SJ, Calabrese JR. (2014) Efficacy and safety of quetiapine-XR as monotherapy or adjunctive therapy to a mood stabilizer in acute bipolar depression with generalized anxiety disorder and other comorbidities: a randomized, placebo-controlled trial. J Clin Psychiatry 75:1062–1068. [DOI] [PubMed] [Google Scholar]
- Garfinkel PE, Stancer HC, Persad E. (1980) A comparison of haloperidol, lithium carbonate and their combination in the treatment of mania. J Affect Disord 2:279–288. [DOI] [PubMed] [Google Scholar]
- Geddes JR, Calabrese JR, Goodwin GM. (2009) Lamotrigine for treatment of bipolar depression: independent meta-analysis and meta-regression of individual patient data from five randomised trials. Br J Psychiatry 194:4–9. [DOI] [PubMed] [Google Scholar]
- Geddes JR, Burgess S, Hawton K, Jamison K, Goodwin GM. (2004) Long-term lithium therapy for bipolar disorder: systematic review and meta-analysis of randomized controlled trials. Am J Psychiatry 161:217–222. [DOI] [PubMed] [Google Scholar]
- Geddes JR, Goodwin GM, Rendell J, Azorin JM, Cipriani A, Ostacher MJ, Morriss R, Alder N, Juszczak E. (2010) Lithium plus valproate combination therapy versus monotherapy for relapse prevention in bipolar I disorder (BALANCE): a randomised open-label trial. Lancet 375:385–395. [DOI] [PubMed] [Google Scholar]
- Geller B, Cooper TB, Watts HE, Cosby CM, Fox LW. (1992) Early findings from a pharmacokinetically designed double-blind and placebo-controlled study of lithium for adolescents comorbid with bipolar and substance dependency disorders. Prog Neuropsychopharmacol Biol Psychiatry 16:281–299. [DOI] [PubMed] [Google Scholar]
- Geller B, Cooper TB, Sun K, Zimerman B, Frazier J, Williams M, Heath J. (1998) Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 37:171–178. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Wingo AP, Filkowski MA, Baldessarini RJ. (2008) Long-term antidepressant treatment in bipolar disorder: meta-analyses of benefits and risks. Acta Psychiatr Scand 118:347–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaemi SN, Gilmer WS, Dunn RT, Hanlon RE, Kemp DE, Bauer AD, Chriki L, Filkowski MM, Harvey PD. (2009) A double-blind, placebo-controlled pilot study of galantamine to improve cognitive dysfunction in minimally symptomatic bipolar disorder. J Clin Psychopharmacol 29:291–295. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Gilmer WS, Goldberg JF, Zablotsky B, Kemp DE, Kelley ME, Bauer AD, Fleck J, Filkowski MM, Stan VA, Dunn RT. (2007) Divalproex in the treatment of acute bipolar depression: a preliminary double-blind, randomized, placebo-controlled pilot study. J Clin Psychiatry 68:1840–1844. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Ostacher MM, El-Mallakh RS, Borrelli D, Baldassano CF, Kelley ME, Filkowski MM, Hennen J, Sachs GS, Goodwin FK, Baldessarini RJ. (2010) Antidepressant discontinuation in bipolar depression: a Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry 71:372–380. [DOI] [PubMed] [Google Scholar]
- Ghanizadeh A, OmraniSigaroodi M, Javadpour A, Dabbaghmanesh MH, Shafiee S. (2014) Lovastatin as an adjuvant to lithium for treating manic phase of bipolar disorder: a 4-week, randomized, double-blind, placebo-controlled clinical trial. Depression Res Treatment 2014:730505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons RD, Hur K, Brown CH, Mann JJ. (2009) Relationship between antiepileptic drugs and suicide attempts in patients with bipolar disorder. Arch Gen Psychiatry 66:1354–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons RD, Brown CH, Hur K, Marcus SM, Bhaumik DK, Erkens JA, Herings RM, Mann JJ. (2007) Early Evidence on the effects of regulators’ suicidality warnings on SSRI prescriptions and suicide in children and adolescents. Am J Psychiatry 164:1356–1363. [DOI] [PubMed] [Google Scholar]
- Gijsman HJ, Geddes JR, Rendell JM, Nolen WA, Goodwin GM. (2004) Antidepressants for bipolar depression: a systematic review of randomized, controlled trials. Am J Psychiatry 161:1537–1547. [DOI] [PubMed] [Google Scholar]
- Gilbert DA, Altshuler KZ, Rago WV, Shon SP, Crismon ML, Toprac MG, Rush AJ. (1998) Texas Medication Algorithm Project: definitions, rationale, and methods to develop medication algorithms. J Clin Psychiatry 59:345–351. [PubMed] [Google Scholar]
- Goikolea JM, Colom F, Capapey J, Torres I, Valenti M, Grande I, Undurraga J, Vieta E. (2013. a) Faster onset of antimanic action with haloperidol compared with second-generation antipsychotics. A meta-analysis of randomized clinical trials in acute mania. Eur Neuropsychopharmacol 23:305–316. [DOI] [PubMed] [Google Scholar]
- Goikolea JM, Colom F, Torres I, Capapey J, Valenti M, Undurraga J, Grande I, Sanchez-Moreno J, Vieta E. (2013. b) Lower rate of depressive switch following antimanic treatment with second-generation antipsychotics versus haloperidol. J Affect Disord 144:191–198. [DOI] [PubMed] [Google Scholar]
- Goldberg J. (2008) Adverse cognitive effects of psychotropic medications. In: Cognitive dysfunction in bipolar disorder: a guide for clinicians (Goldberg J, Burdick K, eds), pp 137–158. Washington, DC: American Psychiatric Press. [Google Scholar]
- Goldberg JF. (2000) Treatment guidelines: current and future management of bipolar disorder. J Clin Psychiatry 61:12–18. [PubMed] [Google Scholar]
- Goldberg JF, Truman CJ. (2003) Antidepressant-induced mania: an overview of current controversies. Bipolar Disord 5:407–420. [DOI] [PubMed] [Google Scholar]
- Goldberg JF, Chengappa KN. (2009) Identifying and treating cognitive impairment in bipolar disorder. Bipolar Disord 11:123–137. [DOI] [PubMed] [Google Scholar]
- Goldsmith DR, Wagstaff AJ, Ibbotson T, Perry CM. (2003) Lamotrigine: a review of its use in bipolar disorder. Drugs 63:2029–2050. [DOI] [PubMed] [Google Scholar]
- Gomes BC, Abreu LN, Brietzke E, Caetano SC, Kleinman A, Nery FG, Lafer B. (2011) A randomized controlled trial of cognitive behavioral group therapy for bipolar disorder. PsychotherPsychosom 80:144–150. [DOI] [PubMed] [Google Scholar]
- Gonzalez D, Bienroth M, Curtis V, Debenham M, Jones S, Pitsi D, George M. (2013) Consensus statement on the use of intramuscular aripiprazole for the rapid control of agitation in bipolar mania and schizophrenia. Curr Med Res Opin 29:241–250. [DOI] [PubMed] [Google Scholar]
- Gonzalez Isasi A, Echeburua E, Liminana JM, Gonzalez-Pinto A. (2014) Psychoeducation and cognitive-behavioral therapy for patients with refractory bipolar disorder: a 5-year controlled clinical trial. Eur Psychiatry 29:134–141. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Murphy DL, Bunney WE., Jr (1969) Lithium-carbonate treatment in depression and mania. A longitudinal double-blind study. Arch Gen Psychiatry 21:486–496. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Murphy DL, Dunner DL, Bunney WE., Jr (1972) Lithium response in unipolar versus bipolar depression. Am J Psychiatry 129:44–47. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Fireman B, Simon GE, Hunkeler EM, Lee J, Revicki D. (2003) Suicide risk in bipolar disorder during treatment with lithium and divalproex. JAMA 290:1467–1473. [DOI] [PubMed] [Google Scholar]
- Goodwin G, Bourgeois M, Conti L. (1997) Treatment of bipolar depressive mood disorders: algorithms for pharmacotherapy. Int J Psychiatry Clin Pract 1:S9–S12. [DOI] [PubMed] [Google Scholar]
- Goodwin GM. (2003) Evidence-based guidelines for treating bipolar disorder: recommendations from the British Association for Psychopharmacology. J Psychopharmacol 17:149–173; discussion 147. [DOI] [PubMed] [Google Scholar]
- Goodwin GM. (2009) Evidence-based guidelines for treating bipolar disorder: revised second edition--recommendations from the British Association for Psychopharmacology. J Psychopharmacol 23:346–388. [DOI] [PubMed] [Google Scholar]
- Goodwin GM, Bowden CL, Calabrese JR, Grunze H, Kasper S, White R, Greene P, Leadbetter R. (2004) A pooled analysis of 2 placebo-controlled 18-month trials of lamotrigine and lithium maintenance in bipolar I disorder. J Clin Psychiatry 65:432–441. [DOI] [PubMed] [Google Scholar]
- Goodwin GM, et al. (2016) Evidence-based guidelines for treating bipolar disorder: revised third edition recommendations from the British Association for Psychopharmacology. J Psychopharmacol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopal S, Steffens DC, Kramer ML, Olsen MK. (2005) Symptomatic remission in patients with bipolar mania: results from a double-blind, placebo-controlled trial of risperidone monotherapy. J Clin Psychiatry 66:1016–1020. [DOI] [PubMed] [Google Scholar]
- Grande I, Berk M, Birmaher B, Vieta E. (2015) Bipolar disorder. Lancet. [DOI] [PubMed] [Google Scholar]
- Greenspan K, Schildkraut JJ, Gordon EK, Baer L, Aronoff MS, Durell J. (1970) Catecholamine metabolism in affective disorders. 3. MHPG and other catecholamine metabolites in patients treated with lithium carbonate. J Psychiatr Res 7:171–183. [DOI] [PubMed] [Google Scholar]
- Greil W, Kleindienst N. (1999. a) The comparative prophylactic efficacy of lithium and carbamazepine in patients with bipolar I disorder. Int Clin Psychopharmacol 14:277–281. [PubMed] [Google Scholar]
- Greil W, Kleindienst N. (1999. b) Lithium versus carbamazepine in the maintenance treatment of bipolar II disorder and bipolar disorder not otherwise specified. Int Clin Psychopharmacol 14:283–285. [PubMed] [Google Scholar]
- Greil W, Kleindienst N, Erazo N, Muller-Oerlinghausen B. (1998) Differential response to lithium and carbamazepine in the prophylaxis of bipolar disorder. J Clin Psychopharmacol 18:455. [DOI] [PubMed] [Google Scholar]
- Greil W, Ludwig-Mayerhofer W, Erazo N, Schochlin C, Schmidt S, Engel RR, Czernik A, Giedke H, Muller-Oerlinghausen B, Osterheider M, Rudolf GA, Sauer H, Tegeler J, Wetterling T. (1997) Lithium versus carbamazepine in the maintenance treatment of bipolar disorders--a randomised study. J Affect Disord 43:151–161. [DOI] [PubMed] [Google Scholar]
- Grossman F, Potter WZ, Brown EA, Maislin G. (1999) A double-blind study comparing idazoxan and bupropion in bipolar depressed patients. J Affect Disord 56:237–243. [DOI] [PubMed] [Google Scholar]
- Grunze H, Kasper S, Goodwin G, Bowden C, Moller HJ. (2004) The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders, part III: maintenance treatment. World J Biol Psychiatry 5:120–135. [DOI] [PubMed] [Google Scholar]
- Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Moller HJ, Kasper S. (2009) The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2009 on the treatment of acute mania. World J Biol Psychiatry 10:85–116. [DOI] [PubMed] [Google Scholar]
- Grunze H, Kotlik E, Costa R, Nunes T, Falcao A, Almeida L, Soares-da-Silva P. (2015) Assessment of the efficacy and safety of eslicarbazepine acetate in acute mania and prevention of recurrence: experience from multicentre, double-blind, randomised phase II clinical studies in patients with bipolar disorder I. J Affect Disord 174:70–82. [DOI] [PubMed] [Google Scholar]
- Grunze H, Kasper S, Goodwin G, Bowden C, Baldwin D, Licht R, Vieta E, Moller HJ. (2002) World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of bipolar disorders. Part I: Treatment of bipolar depression. World J Biol Psychiatry 3:115–124. [DOI] [PubMed] [Google Scholar]
- Grunze H, Kasper S, Goodwin G, Bowden C, Baldwin D, Licht RW, Vieta E, Moller HJ. (2003) The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders, Part II: Treatment of Mania. World J Biol Psychiatry 4:5–13. [DOI] [PubMed] [Google Scholar]
- Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Moller HJ, Kasper S, Disorders WTFOTGFB. (2010) The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders: Update 2010 on the treatment of acute bipolar depression. World J Biol Psychiatry 11:81–109.20148751 [Google Scholar]
- Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Moller HJ, Kasper S, Disorders WTFoTGfB (2013) The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2012 on the long-term treatment of bipolar disorder. World J Biol Psychiatry 14:154–219.23480132 [Google Scholar]
- Grunze HC. (2008) Switching, induction of rapid cycling, and increased suicidality with antidepressants in bipolar patients: fact or overinterpretation? CNS Spectr 13:790–795. [DOI] [PubMed] [Google Scholar]
- Gyulai L, Bauer M, Bauer MS, Garcia-Espana F, Cnaan A, Whybrow PC. (2003. a) Thyroid hypofunction in patients with rapid-cycling bipolar disorder after lithium challenge. Biol Psychiatry 53:899–905. [DOI] [PubMed] [Google Scholar]
- Gyulai L, Bowden CL, McElroy SL, Calabrese JR, Petty F, Swann AC, Chou JC, Wassef A, Risch CS, Hirschfeld RM, Nemeroff CB, Keck PE, Jr, Evans DL, Wozniak PJ. (2003. b) Maintenance efficacy of divalproex in the prevention of bipolar depression. Neuropsychopharmacology 28:1374–1382. [DOI] [PubMed] [Google Scholar]
- Harel EV, Levkovitz Y. (2008) Effectiveness and safety of adjunctive antidepressants in the treatment of bipolar depression: a review. Isr J Psychiatry Relat Sci 45:121–128. [PubMed] [Google Scholar]
- Hartong EG, Moleman P, Hoogduin CA, Broekman TG, Nolen WA, LitCar G. (2003) Prophylactic efficacy of lithium versus carbamazepine in treatment-naive bipolar patients. J Clin Psychiatry 64:144–151. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Soehner AM, Kaplan KA, Hein K, Lee J, Kanady J, Li D, Rabe-Hesketh S, Ketter TA, Neylan TC, Buysse DJ. (2015) Treating insomnia improves mood state, sleep, and functioning in bipolar disorder: a pilot randomized controlled trial. Journal of consulting and clinical psychology 83:564–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy D. (2003) Lines of evidence on the risks of suicide with selective serotonin reuptake inhibitors. Psychother Psychosom 72:71–79. [DOI] [PubMed] [Google Scholar]
- Hesdorffer DC, Kanner AM. (2009) The FDA alert on suicidality and antiepileptic drugs: Fire or false alarm? Epilepsia 50:978–986. [DOI] [PubMed] [Google Scholar]
- Himmelhoch JM, Fuchs CZ, Symons BJ. (1982) A double-blind study of tranylcypromine treatment of major anergic depression. The Journal of nervous and mental disease 170:628–634. [DOI] [PubMed] [Google Scholar]
- Himmelhoch JM, Thase ME, Mallinger AG, Houck P. (1991) Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry 148:910–916. [DOI] [PubMed] [Google Scholar]
- Hirschfeld R. (2005) Guideline Watch for the Practice Guideline for the Treatment of Patients With Bipolar Disorder. In. Arlington, VA: American Psychiatric Association. [Google Scholar]
- Hirschfeld RM, Allen MH, McEvoy JP, Keck PE, Jr, Russell JM. (1999) Safety and tolerability of oral loading divalproex sodium in acutely manic bipolar patients. J Clin Psychiatry 60:815–818. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Bowden CL, Vigna NV, Wozniak P, Collins M. (2010) A randomized, placebo-controlled, multicenter study of divalproex sodium extended-release in the acute treatment of mania. J Clin Psychiatry 71:426–432. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Keck PE, Jr, Kramer M, Karcher K, Canuso C, Eerdekens M, Grossman F. (2004) Rapid antimanic effect of risperidone monotherapy: a 3-week multicenter, double-blind, placebo-controlled trial. Am J Psychiatry 161:1057–1065. [DOI] [PubMed] [Google Scholar]
- Holmes MK, Erickson K, Luckenbaugh DA, Drevets WC, Bain EE, Cannon DM, Snow J, Sahakian BJ, Manji HK, Zarate CA., Jr (2008) A comparison of cognitive functioning in medicated and unmedicated subjects with bipolar depression. Bipolar Disord 10:806–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honig A, Arts BM, Ponds RW, Riedel WJ. (1999) Lithium induced cognitive side-effects in bipolar disorder: a qualitative analysis and implications for daily practice. Int Clin Psychopharmacol 14:167–171. [PubMed] [Google Scholar]
- Hopewell S, Clarke M, Moher D, Wager E, Middleton P, Altman DG, Schulz KF, Group C. (2008) CONSORT for reporting randomized controlled trials in journal and conference abstracts: explanation and elaboration. PLoS Med 5:e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston JP, Ahl J, Meyers AL, Kaiser CJ, Tohen M, Baldessarini RJ. (2006) Reduced suicidal ideation in bipolar I disorder mixed-episode patients in a placebo-controlled trial of olanzapine combined with lithium or divalproex. J Clin Psychiatry 67:1246–1252. [DOI] [PubMed] [Google Scholar]
- Houston JP, Tohen M, Degenhardt EK, Jamal HH, Liu LL, Ketter TA. (2009) Olanzapine-divalproex combination versus divalproex monotherapy in the treatment of bipolar mixed episodes: a double-blind, placebo-controlled study. J Clin Psychiatry 70:1540–1547. [DOI] [PubMed] [Google Scholar]
- Houston JP, Ketter TA, Case M, Bowden C, Degenhardt EK, Jamal HH, Tohen M. (2011) Early symptom change and prediction of subsequent remission with olanzapine augmentation in divalproex-resistant bipolar mixed episodes. J Psychiatr Res 45:169–173. [DOI] [PubMed] [Google Scholar]
- Hullin RP, McDonald R, Allsopp MN. (1972) Prophylactic lithium in recurrent affective disorders. Lancet 1:1044–1046. [DOI] [PubMed] [Google Scholar]
- Ichim L, Berk M, Brook S. (2000) Lamotrigine compared with lithium in mania: a double-blind randomized controlled trial. Ann Clin Psychiatry 12:5–10. [DOI] [PubMed] [Google Scholar]
- Inder ML, Crowe MT, Luty SE, Carter JD, Moor S, Frampton CM, Joyce PR. (2015) Randomized, controlled trial of Interpersonal and Social Rhythm Therapy for young people with bipolar disorder. Bipolar Disord 17:128–138. [DOI] [PubMed] [Google Scholar]
- Ives-Deliperi VL, Howells F, Stein DJ, Meintjes EM, Horn N. (2013) The effects of mindfulness-based cognitive therapy in patients with bipolar disorder: A controlled functional MRI investigation. JAffectDisord. [DOI] [PubMed] [Google Scholar]
- Jahangard L, Soroush S, Haghighi M, Ghaleiha A, Bajoghli H, Holsboer-Trachsler E, Brand S. (2014) In a double-blind, randomized and placebo-controlled trial, adjuvant allopurinol improved symptoms of mania in in-patients suffering from bipolar disorder. Eur Neuropsychopharmacol 24:1210–1221. [DOI] [PubMed] [Google Scholar]
- Jamrozinski K, Gruber O, Kemmer C, Falkai P, Scherk H. (2009) Neurocognitive functions in euthymic bipolar patients. Acta Psychiatr Scand 119:365–374. [DOI] [PubMed] [Google Scholar]
- Janicak PG, Sharma RP, Pandey G, Davis JM. (1998) Verapamil for the treatment of acute mania: a double-blind, placebo-controlled trial. Am J Psychiatry 155:972–973. [DOI] [PubMed] [Google Scholar]
- Jauhar S, McKenna PJ, Laws KR. (2016) NICE guidance on psychological treatments for bipolar disorder: searching for the evidence. The lancet Psychiatry. [DOI] [PubMed] [Google Scholar]
- Jimerson DC, Post RM, Stoddard FJ, Gillin JC, Bunney WE., Jr (1980) Preliminary trial of the noradrenergic agonist clonidine in psychiatric patients. Biol Psychiatry 15:45–57. [PubMed] [Google Scholar]
- Joas E, Karanti A, Lichtenstein P, Land M. (2015) Effectiveness of medication in preventing hospitalization of bipolar patients - a register based study of mood stabilizing medication with lithium and anticonvulsants in Sweden. Bipolar Disord 17:136. [Google Scholar]
- Jobson K. (1997) International Psychopharmacology Algorithm Project: Algorithms in psychopharmacology. Int J Psychiatry Clin Pract 1:S3–S8. [DOI] [PubMed] [Google Scholar]
- Jon DI, Bahk WM, Yoon BH, Shin YC, Cho HS, Lee E, Ha K, Kim W, Chung SK, Seo JS, Min KJ. (2009) Revised Korean medication algorithm for bipolar disorder. World J Biol Psychiatry 10:846–855. [DOI] [PubMed] [Google Scholar]
- Juruena MF, Ottoni GL, Machado-Vieira R, Carneiro RM, Weingarthner N, Marquardt AR, Fleig SS, Broilo L, Busnello EA. (2009) Bipolar I and II disorder residual symptoms: oxcarbazepine and carbamazepine as add-on treatment to lithium in a double-blind, randomized trial. Prog Neuropsychopharmacol Biol Psychiatry 33:94–99. [DOI] [PubMed] [Google Scholar]
- Kafantaris V, Coletti DJ, Dicker R, Padula G, Pleak RR, Alvir JM. (2004) Lithium treatment of acute mania in adolescents: a placebo-controlled discontinuation study. J Am Acad Child Adolesc Psychiatry 43:984–993. [DOI] [PubMed] [Google Scholar]
- Kakkar AK, Rehan HS, Unni KE, Gupta NK, Chopra D, Kataria D. (2009) Comparative efficacy and safety of oxcarbazepine versus divalproex sodium in the treatment of acute mania: a pilot study. Eur Psychiatry 24:178–182. [DOI] [PubMed] [Google Scholar]
- Kanba S, Kawasaki H, Ishigooka J, Sakamoto K, Kinoshita T, Kuroki T. (2014) A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole for the treatment of acute manic or mixed episodes in Asian patients with bipolar I disorder (the AMAZE study). World J Biol Psychiatry 15:113–121. [DOI] [PubMed] [Google Scholar]
- Kane JM, Quitkin FM, Rifkin A, Ramos-Lorenzi JR, Nayak DD, Howard A. (1982) Lithium carbonate and imipramine in the prophylaxis of unipolar and bipolar II illness: a prospective, placebo-controlled comparison. Arch Gen Psychiatry 39:1065–1069. [DOI] [PubMed] [Google Scholar]
- Kaptsan A, Yaroslavsky Y, Applebaum J, Belmaker RH, Grisaru N. (2003) Right prefrontal TMS versus sham treatment of mania: a controlled study. Bipolar Disord 5:36–39. [DOI] [PubMed] [Google Scholar]
- Kargar M, Yoosefi A, Akhondzadeh S, Artonian V, Ashouri A, Ghaeli P. (2015) Effect of Adjunctive Celecoxib on BDNF in Manic Patients Undergoing Electroconvulsive Therapy: a Randomized Double Blind Controlled Trial. Pharmacopsychiatry 48:268–273. [DOI] [PubMed] [Google Scholar]
- Karniol IG, Dalton J, Lader MH. (1978) Acute and chronic effects of lithium chloride on physiological and psychological measures in normals. Psychopharmacology (Berl) 57:289–294. [DOI] [PubMed] [Google Scholar]
- Kastin AJ, Ehrensing RH, Schalch DS, Anderson MS. (1972) Improvement in mental depression with decreased thyrotropin response after administration of thyrotropin-releasing hormone. Lancet 2:740–742. [DOI] [PubMed] [Google Scholar]
- Katagiri H, Takita Y, Tohen M, Higuchi T, Kanba S, Takahashi M. (2012) Efficacy and safety of olanzapine in the treatment of Japanese patients with bipolar I disorder in a current manic or mixed episode: a randomized, double-blind, placebo- and haloperidol-controlled study. J Affect Disord 136:476–484. [DOI] [PubMed] [Google Scholar]
- Katagiri H, Tohen M, McDonnell DP, Fujikoshi S, Case M, Kanba S, Takahashi M, Gomez JC. (2013) Efficacy and safety of olanzapine for treatment of patients with bipolar depression: Japanese subpopulation analysis of a randomized, double-blind, placebo-controlled study. BMC Psychiatry 13:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keck PE, Orsulak PJ, Cutler AJ, Sanchez R, Torbeyns A, Marcus RN, McQuade RD, Carson WH, Group CNS (2009) Aripiprazole monotherapy in the treatment of acute bipolar I mania: a randomized, double-blind, placebo- and lithium-controlled study. J Affect Disord 112:36–49. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, Versiani M, Potkin S, West SA, Giller E, Ice K, Ziprasidone in Mania Study G (2003. a) Ziprasidone in the treatment of acute bipolar mania: a three-week, placebo-controlled, double-blind, randomized trial. Am J Psychiatry 160:741–748. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, Marcus R, Tourkodimitris S, Ali M, Liebeskind A, Saha A, Ingenito G, Aripiprazole Study G (2003. b) A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry 160:1651–1658. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, Corya SA, Altshuler LL, Ketter TA, McElroy SL, Case M, Briggs SD, Tohen M. (2005) Analyses of treatment-emergent mania with olanzapine/fluoxetine combination in the treatment of bipolar depression. J Clin Psychiatry 66:611–616. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, Calabrese JR, McQuade RD, Carson WH, Carlson BX, Rollin LM, Marcus RN, Sanchez R, Aripiprazole Study G (2006. a) A randomized, double-blind, placebo-controlled 26-week trial of aripiprazole in recently manic patients with bipolar I disorder. J Clin Psychiatry 67:626–637. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, Calabrese JR, McIntyre RS, McQuade RD, Carson WH, Eudicone JM, Carlson BX, Marcus RN, Sanchez R, Aripiprazole Study G (2007) Aripiprazole monotherapy for maintenance therapy in bipolar I disorder: a 100-week, double-blind study versus placebo. J Clin Psychiatry 68:1480–1491. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, Mintz J, McElroy SL, Freeman MP, Suppes T, Frye MA, Altshuler LL, Kupka R, Nolen WA, Leverich GS, Denicoff KD, Grunze H, Duan N, Post RM. (2006. b) Double-blind, randomized, placebo-controlled trials of ethyl-eicosapentanoate in the treatment of bipolar depression and rapid cycling bipolar disorder. Biol Psychiatry 60:1020–1022. [DOI] [PubMed] [Google Scholar]
- Kemp DE, Gao K, Ganocy SJ, Elhaj O, Bilali SR, Conroy C, Findling RL, Calabrese JR. (2009) A 6-month, double-blind, maintenance trial of lithium monotherapy versus the combination of lithium and divalproex for rapid-cycling bipolar disorder and Co-occurring substance abuse or dependence. J Clin Psychiatry 70:113–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp DE, Karayal ON, Calabrese JR, Sachs GS, Pappadopulos E, Ice KS, Siu CO, Vieta E. (2012. a) Ziprasidone with adjunctive mood stabilizer in the maintenance treatment of bipolar I disorder: Long-term changes in weight and metabolic profiles. Eur Neuropsychopharmacol 22:123–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp DE, Gao K, Fein EB, Chan PK, Conroy C, Obral S, Ganocy SJ, Calabrese JR. (2012. b) Lamotrigine as add-on treatment to lithium and divalproex: lessons learned from a double-blind, placebo-controlled trial in rapid-cycling bipolar disorder. Bipolar Disord 14:780–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp DE, Ganocy SJ, Brecher M, Carlson BX, Edwards S, Eudicone JM, Evoniuk G, Jansen W, Leon AC, Minkwitz M, Pikalov A, Stassen HH, Szegedi A, Tohen M, Van Willigenburg AP, Calabrese JR. (2010) Clinical value of early partial symptomatic improvement in the prediction of response and remission during short-term treatment trials in 3369 subjects with bipolar I or II depression. J Affect Disord 130:171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessell A, Holt NF. (1975) A controlled study of a tetracyclic antidepressant--maprotiline (Ludiomil). The Medical journal of Australia 1:773–776. [DOI] [PubMed] [Google Scholar]
- Kessing LV. (1998) Cognitive impairment in the euthymic phase of affective disorder. Psychol Med 28:1027–1038. [DOI] [PubMed] [Google Scholar]
- Kessler U, Vaaler AE, Schoyen H, Oedegaard KJ, Bergsholm P, Andreassen OA, Malt UF, Morken G. (2010) The study protocol of the Norwegian randomized controlled trial of electroconvulsive therapy in treatment resistant depression in bipolar disorder. BMC Psychiatry 10:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler U, Schoeyen HK, Andreassen OA, Eide GE, Malt UF, Oedegaard KJ, Morken G, Sundet K, Vaaler AE. (2014) The effect of electroconvulsive therapy on neurocognitive function in treatment-resistant bipolar disorder depression. J Clin Psychiatry 75:e1306–1313. [DOI] [PubMed] [Google Scholar]
- Ketter TA, Yang R, Frye MA. (2015) Adjunctive armodafinil for major depressive episodes associated with bipolar I disorder. J Affect Disord 181:87–91. [DOI] [PubMed] [Google Scholar]
- Ketter TA, Agid O, Kapur S, Loebel A, Siu CO, Romano SJ. (2010) Rapid antipsychotic response with ziprasidone predicts subsequent acute manic/mixed episode remission. J Psychiatr Res 44:8–14. [DOI] [PubMed] [Google Scholar]
- Ketter TA, Houston JP, Adams DH, Risser RC, Meyers AL, Williamson DJ, Tohen M. (2006) Differential efficacy of olanzapine and lithium in preventing manic or mixed recurrence in patients with bipolar I disorder based on number of previous manic or mixed episodes. J Clin Psychiatry 67:95–101. [DOI] [PubMed] [Google Scholar]
- Khan A, Warner HA, Brown WA. (2000) Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: an analysis of the Food and Drug Administration database. Arch Gen Psychiatry 57:311–317. [DOI] [PubMed] [Google Scholar]
- Khan A, Khan SR, Leventhal RM, Brown WA. (2001) Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: a replication analysis of the Food and Drug Administration Database. Int J Neuropsychopharmacol 4:113–118. [DOI] [PubMed] [Google Scholar]
- Khan A, Khan S, Kolts R, Brown WA. (2003) Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry 160:790–792. [DOI] [PubMed] [Google Scholar]
- Khanna S, Vieta E, Lyons B, Grossman F, Eerdekens M, Kramer M. (2005) Risperidone in the treatment of acute mania: double-blind, placebo-controlled study. Br J Psychiatry 187:229–234. [DOI] [PubMed] [Google Scholar]
- King DJ. (1994) Psychomotor impairment and cognitive disturbances induced by neuroleptics. Acta Psychiatr Scand Suppl 380:53–58. [DOI] [PubMed] [Google Scholar]
- Klein DF. (1967) Importance of psychiatric diagnosis in prediction of clinical drug effects. Arch Gen Psychiatry 16:118–126. [DOI] [PubMed] [Google Scholar]
- Klein E, Bental E, Lerer B, Belmaker RH. (1984) Carbamazepine and haloperidol v placebo and haloperidol in excited psychoses. A controlled study. Arch Gen Psychiatry 41:165–170. [DOI] [PubMed] [Google Scholar]
- Klein HE, Broucek B, Greil W. (1981) Lithium withdrawal triggers psychotic states. Br J Psychiatry 139:255–256. [DOI] [PubMed] [Google Scholar]
- Kleindienst N, Greil W. (2000) Differential efficacy of lithium and carbamazepine in the prophylaxis of bipolar disorder: results of the MAP study. Neuropsychobiology 42Suppl 1:2–10. [DOI] [PubMed] [Google Scholar]
- Kleindienst N, Greil W. (2002) Inter-episodic morbidity and drop-out under carbamazepine and lithium in the maintenance treatment of bipolar disorder. Psychol Med 32:493–501. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Shaw ED, Stokes PE, Wilner P, Elliot AS, Sikes C, Myers B, Manevitz A, Parides M. (1993) Neuropsychologic effects of lithium discontinuation. J Clin Psychopharmacol 13:268–275. [PubMed] [Google Scholar]
- Kropf D, Muller-Oerlinghausen B. (1979) Changes in learning, memory, and mood during lithium treatment. Approach to a research strategy. Acta Psychiatr Scand 59:97–124. [DOI] [PubMed] [Google Scholar]
- Kulkarni J, Garland KA, Scaffidi A, Headey B, Anderson R, de Castella A, Fitzgerald P, Davis SR. (2006) A pilot study of hormone modulation as a new treatment for mania in women with bipolar affective disorder. Psychoneuroendocrinology 31:543–547. [DOI] [PubMed] [Google Scholar]
- Kulkarni J, Berk M, Wang W, Mu L, Scarr E, Van Rheenen TE, Worsley R, Gurvich C, Gavrilidis E, de Castella A, Fitzgerald P, Davis SR. (2014) A four week randomised control trial of adjunctive medroxyprogesterone and tamoxifen in women with mania. Psychoneuroendocrinology 43:52–61. [DOI] [PubMed] [Google Scholar]
- Kupka RW, Luckenbaugh DA, Post RM, Leverich GS, Nolen WA. (2003) Rapid and non-rapid cycling bipolar disorder: a meta-analysis of clinical studies. J Clin Psychiatry 64:1483–1494. [DOI] [PubMed] [Google Scholar]
- Kushner SF, Khan A, Lane R, Olson WH. (2006) Topiramate monotherapy in the management of acute mania: results of four double-blind placebo-controlled trials. Bipolar Disord 8:15–27. [DOI] [PubMed] [Google Scholar]
- Kusumakar V, Yatham L, Parikh S. (1997) Bipolar disorder: a summary of clinical issues and treatment options. In. Halifax, Nova Scotia: CANMAT Monograph. [Google Scholar]
- Kwentus J, Riesenberg RA, Marandi M, Manning RA, Allen MH, Fishman RS, Spyker DA, Kehne JH, Cassella JV. (2012) Rapid acute treatment of agitation in patients with bipolar I disorder: a multicenter, randomized, placebo-controlled clinical trial with inhaled loxapine. Bipolar Disord 14:31–40. [DOI] [PubMed] [Google Scholar]
- Lahera G, Benito A, Montes JM, Fernandez-Liria A, Olbert CM, Penn DL. (2013) Social cognition and interaction training (SCIT) for outpatients with bipolar disorder. JAffectDisord 146:132–136. [DOI] [PubMed] [Google Scholar]
- Laje G, Paddock S, Manji H, Rush AJ, Wilson AF, Charney D, McMahon FJ. (2007) Genetic markers of suicidal ideation emerging during citalopram treatment of major depression. Am J Psychiatry 164:1530–1538. [DOI] [PubMed] [Google Scholar]
- Landbloom RL, Mackle M, Wu X, Kelly L, Snow-Adami L, McIntyre RS, Mathews M, Hundt C. (2016) Asenapine: Efficacy and safety of 5 and 10mg bid in a 3-week, randomized, double-blind, placebo-controlled trial in adults with a manic or mixed episode associated with bipolar I disorder. J Affect Disord 190:103–110. [DOI] [PubMed] [Google Scholar]
- Lea JW, Stoner SC, Lafollette J. (2007) Agitation associated with aripiprazole initiation. Pharmacotherapy 27:1339–1342. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y, Bech P. (2007) The Ham D(6) is more homogenous and as sensitive as the Ham D(17). Eur Psychiatry 22:252–255. [DOI] [PubMed] [Google Scholar]
- Lee EE, Della Selva MP, Liu A, Himelhoch S. (2015) Ketamine as a novel treatment for major depressive disorder and bipolar depression: a systematic review and quantitative meta-analysis. General hospital psychiatry 37:178–184. [DOI] [PubMed] [Google Scholar]
- Lee SY, Chen SL, Chang YH, Chen SH, Chu CH, Huang SY, Tzeng NS, Wang CL, Wang LJ, Lee IH, Yeh TL, Yang YK, Hong JS, Lu RB. (2014. a) Genotype variant associated with add-on memantine in bipolar II disorder. Int J Neuropsychopharmacol 17:189–197. [DOI] [PubMed] [Google Scholar]
- Lee SY, Chen SL, Chang YH, Chen PS, Huang SY, Tzeng NS, Wang YS, Wang LJ, Lee IH, Wang TY, Yeh TL, Yang YK, Hong JS, Lu RB. (2014. b) The effects of add-on low-dose memantine on cytokine levels in bipolar II depression: a 12-week double-blind, randomized controlled trial. J Clin Psychopharmacol 34:337–343. [DOI] [PubMed] [Google Scholar]
- Lenox RH, Newhouse PA, Creelman WL, Whitaker TM. (1992) Adjunctive treatment of manic agitation with lorazepam versus haloperidol: a double-blind study. J Clin Psychiatry 53:47–52. [PubMed] [Google Scholar]
- Leon AC, Keller MB, Warshaw MG, Mueller TI, Solomon DA, Coryell W, Endicott J. (1999) Prospective study of fluoxetine treatment and suicidal behavior in affectively ill subjects. Am J Psychiatry 156:195–201. [DOI] [PubMed] [Google Scholar]
- Lerer B, Moore N, Meyendorff E, Cho SR, Gershon S. (1987) Carbamazepine versus lithium in mania: a double-blind study. J Clin Psychiatry 48:89–93. [PubMed] [Google Scholar]
- Leverich GS, Altshuler LL, Frye MA, Suppes T, McElroy SL, Keck PE, Jr, Kupka RW, Denicoff KD, Nolen WA, Grunze H, Martinez MI, Post RM. (2006) Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry 163:232–239. [DOI] [PubMed] [Google Scholar]
- Li H, Ma C, Wang G, Zhu X, Peng M, Gu N. (2008) Response and remission rates in Chinese patients with bipolar mania treated for 4 weeks with either quetiapine or lithium: a randomized and double-blind study. Curr Med Res Opin 24:1–10. [DOI] [PubMed] [Google Scholar]
- Li H, et al. (2016) Efficacy and safety of quetiapine extended release monotherapy in bipolar depression: a multi-center, randomized, double-blind, placebo-controlled trial. Psychopharmacology (Berl) 233:1289–1297. [DOI] [PubMed] [Google Scholar]
- Libby AM, Brent DA, Morrato EH, Orton HD, Allen R, Valuck RJ. (2007) Decline in treatment of pediatric depression after FDA advisory on risk of suicidality with SSRIs. Am J Psychiatry 164:884–891. [DOI] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licht RW, Gijsman H, Nolen WA, Angst J. (2008) Are antidepressants safe in the treatment of bipolar depression? A critical evaluation of their potential risk to induce switch into mania or cycle acceleration. Acta Psychiatr Scand 118:337–346. [DOI] [PubMed] [Google Scholar]
- Licht RW, Vestergaard P, Kessing LV, Larsen JK, Thomsen PH. (2003) Psychopharmacological treatment with lithium and antiepileptic drugs: suggested guidelines from the Danish Psychiatric Association and the Child and Adolescent Psychiatric Association in Denmark. Acta Psychiatr Scand 108Suppl 419:1–22. [DOI] [PubMed] [Google Scholar]
- Lobban F, Taylor L, Chandler C, Tyler E, Kinderman P, Kolamunnage-Dona R, Gamble C, Peters S, Pontin E, Sellwood W, Morriss RK. (2010) Enhanced relapse prevention for bipolar disorder by community mental health teams: cluster feasibility randomised trial. BrJPsychiatry 196:59–63. [DOI] [PubMed] [Google Scholar]
- Loebel A, Cucchiaro J, Silva R, Kroger H, Hsu J, Sarma K, Sachs G. (2014. a) Lurasidone monotherapy in the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry 171:160–168. [DOI] [PubMed] [Google Scholar]
- Loebel A, Cucchiaro J, Silva R, Kroger H, Sarma K, Xu J, Calabrese JR. (2014. b) Lurasidone as adjunctive therapy with lithium or valproate for the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry 171:169–177. [DOI] [PubMed] [Google Scholar]
- Lombardo I, Sachs G, Kolluri S, Kremer C, Yang R. (2012) Two 6-week, randomized, double-blind, placebo-controlled studies of ziprasidone in outpatients with bipolar I depression: did baseline characteristics impact trial outcome? J Clin Psychopharmacol 32:470–478. [DOI] [PubMed] [Google Scholar]
- Loo C, Katalinic N, Mitchell PB, Greenberg B. (2010) Physical treatments for bipolar disorder: A review of electroconvulsive therapy, stereotactic surgery and other brain stimulation techniques. J Affect Disord 132:1–13. [DOI] [PubMed] [Google Scholar]
- Lorenzo-Luaces L, Amsterdam JD, Soeller I, DeRubeis RJ. (2016) Rapid versus non-rapid cycling bipolar II depression: response to venlafaxine and lithium and hypomanic risk. Acta Psychiatr Scand. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund Y, Nissen M, Rafaelsen OJ. (1982) Long-term lithium treatment and psychological functions. Acta Psychiatr Scand 65:233–244. [DOI] [PubMed] [Google Scholar]
- Luoma JB, Martin CE, Pearson JL. (2002) Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry 159:909–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lusznat RM, Murphy DP, Nunn CM. (1988) Carbamazepine vs lithium in the treatment and prophylaxis of mania. Br J Psychiatry 153:198–204. [DOI] [PubMed] [Google Scholar]
- Lydiard RB, Culpepper L, Schioler H, Gustafsson U, Paulsson B. (2009) Quetiapine monotherapy as treatment for anxiety symptoms in patients with bipolar depression: a pooled analysis of results from 2 double-blind, randomized, placebo-controlled studies. Prim Care Companion J Clin Psychiatry 11:215–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maarbjerg K, Aagaard J, Vestergaard P. (1988) Adherence to lithium prophylaxis: I. Clinical predictors and patient’s reasons for nonadherence. Pharmacopsychiatry 21:121–125. [DOI] [PubMed] [Google Scholar]
- Macfadden W, Alphs L, Haskins JT, Turner N, Turkoz I, Bossie C, Kujawa M, Mahmoud R. (2009) A randomized, double-blind, placebo-controlled study of maintenance treatment with adjunctive risperidone long-acting therapy in patients with bipolar I disorder who relapse frequently. Bipolar Disord 11:827–839. [DOI] [PubMed] [Google Scholar]
- Machado-Vieira R, Soares JC, Lara DR, Luckenbaugh DA, Busnello JV, Marca G, Cunha A, Souza DO, Zarate CA, Jr, Kapczinski F. (2008) A double-blind, randomized, placebo-controlled 4-week study on the efficacy and safety of the purinergic agents allopurinol and dipyridamole adjunctive to lithium in acute bipolar mania. J Clin Psychiatry 69:1237–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macritchie K, Geddes JR, Scott J, Haslam D, de Lima M, Goodwin G. (2003) Valproate for acute mood episodes in bipolar disorder. Cochrane Database Syst Rev:CD004052. [DOI] [PubMed] [Google Scholar]
- Macritchie KA, Geddes JR, Scott J, Haslam DR, Goodwin GM. (2001) Valproic acid, valproate and divalproex in the maintenance treatment of bipolar disorder. Cochrane Database Syst Rev:CD003196. [DOI] [PubMed] [Google Scholar]
- Magalhaes PV, Dean OM, Bush AI, Copolov DL, Malhi GS, Kohlmann K, Jeavons S, Schapkaitz I, Anderson-Hunt M, Berk M. (2011. a) N-acetylcysteine for major depressive episodes in bipolar disorder. Revista brasileira de psiquiatria 33:374–378. [DOI] [PubMed] [Google Scholar]
- Magalhaes PV, Dean OM, Bush AI, Copolov DL, Malhi GS, Kohlmann K, Jeavons S, Schapkaitz I, Anderson-Hunt M, Berk M. (2011. b) N-acetyl cysteine add-on treatment for bipolar II disorder: a subgroup analysis of a randomized placebo-controlled trial. J Affect Disord 129:317–320. [DOI] [PubMed] [Google Scholar]
- Magalhaes PV, Dean OM, Bush AI, Copolov DL, Malhi GS, Kohlmann K, Jeavons S, Schapkaitz I, Anderson-Hunt M, Berk M. (2013) A preliminary investigation on the efficacy of N-acetyl cysteine for mania or hypomania. Aust N Z J Psychiatry 47:564–568. [DOI] [PubMed] [Google Scholar]
- Malhi GS, Tanious M, Gershon S. (2011) The lithiumeter: a measured approach. Bipolar Disord 13:219–226. [DOI] [PubMed] [Google Scholar]
- Malhi GS, Bassett D, Boyce P, Bryant R, Fitzgerald PB, Fritz K, Hopwood M, Lyndon B, Mulder R, Murray G, Porter R, Singh AB. (2015) Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry 49:1087–1206. [DOI] [PubMed] [Google Scholar]
- Mander AJ, Loudon JB. (1988) Rapid recurrence of mania following abrupt discontinuation of lithium. Lancet 2:15–17. [DOI] [PubMed] [Google Scholar]
- Marcus R, Khan A, Rollin L, Morris B, Timko K, Carson W, Sanchez R. (2011) Efficacy of aripiprazole adjunctive to lithium or valproate in the long-term treatment of patients with bipolar I disorder with an inadequate response to lithium or valproate monotherapy: a multicenter, double-blind, randomized study. Bipolar Disord 13:133–144. [DOI] [PubMed] [Google Scholar]
- Margo A, McMahon P. (1982) Lithium withdrawal triggers psychosis. Br J Psychiatry 141:407–410. [DOI] [PubMed] [Google Scholar]
- Martinez-Aran A, Torrent C, Sole B, Bonnin CM, Rosa AR, Sanchez-Moreno J, Vieta E. (2011) Functional remediation for bipolar disorder. ClinPractEpidemiolMentHealth 7:112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClellan J, Werry J. (1997) Practice parameters for the assessment and treatment of children and adolescents with bipolar disorder. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry 36:157S–176S. [DOI] [PubMed] [Google Scholar]
- McClure D, Greenman SC, Koppolu SS, Varvara M, Yaseen ZS, Galynker (2015) A Pilot Study of Safety and Efficacy of Cranial Electrotherapy Stimulation in Treatment of Bipolar II Depression. The Journal of nervous and mental disease 203:827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy SL, Keck PE, Jr, Pope HG, Jr, Hudson JI. (1989) Valproate in psychiatric disorders: literature review and clinical guidelines. J Clin Psychiatry 50 Suppl:23–29. [PubMed] [Google Scholar]
- McElroy SL, Keck PE, Stanton SP, Tugrul KC, Bennett JA, Strakowski SM. (1996) A randomized comparison of divalproex oral loading versus haloperidol in the initial treatment of acute psychotic mania. J Clin Psychiatry 57:142–146. [PubMed] [Google Scholar]
- McElroy SL, Martens BE, Creech RS, Welge JA, Jefferson L, Guerdjikova AI, Keck PE., Jr (2010. a) Randomized, double-blind, placebo-controlled study of divalproex extended release loading monotherapy in ambulatory bipolar spectrum disorder patients with moderate-to-severe hypomania or mild mania. J Clin Psychiatry 71:557–565. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Martens BE, Mori N, Blom TJ, Casuto LS, Hawkins JM, Keck PE., Jr (2015) Adjunctive lisdexamfetamine in bipolar depression: a preliminary randomized, placebo-controlled trial. Int Clin Psychopharmacol 30:6–13. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Winstanley EL, Martens B, Patel NC, Mori N, Moeller D, McCoy J, Keck PE., Jr (2010. b) A randomized, placebo-controlled study of adjunctive ramelteon in ambulatory bipolar I disorder with manic symptoms and sleep disturbance. Int Clin Psychopharmacol 26:48–53. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Weisler RH, Chang W, Olausson B, Paulsson B, Brecher M, Agambaram V, Merideth C, Nordenhem A, Young AH, Investigators EI. (2010. c) A double-blind, placebo-controlled study of quetiapine and paroxetine as monotherapy in adults with bipolar depression (EMBOLDEN II). J Clin Psychiatry 71:163–174. [DOI] [PubMed] [Google Scholar]
- McGirr A, Berlim MT, Bond DJ, Fleck MP, Yatham LN, Lam RW. (2014) A systematic review and meta-analysis of randomized, double-blind, placebo-controlled trials of ketamine in the rapid treatment of major depressive episodes. Psychol Med:1–12. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Brecher M, Paulsson B, Huizar K, Mullen J. (2005) Quetiapine or haloperidol as monotherapy for bipolar mania--a 12-week, double-blind, randomised, parallel-group, placebo-controlled trial. Eur Neuropsychopharmacol 15:573–585. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Tohen M, Berk M, Zhao J, Weiller E. (2013) DSM-5 mixed specifier for manic episodes: evaluating the effect of depressive features on severity and treatment outcome using asenapine clinical trial data. J Affect Disord 150:378–383. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Cucchiaro J, Pikalov A, Kroger H, Loebel A. (2015) Lurasidone in the treatment of bipolar depression with mixed (subsyndromal hypomanic) features: post hoc analysis of a randomized placebo-controlled trial. J Clin Psychiatry 76:398–405. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Cohen M, Zhao J, Alphs L, Macek TA, Panagides J. (2009. a) A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord 11:673–686. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Cohen M, Zhao J, Alphs L, Macek TA, Panagides J. (2010. a) Asenapine for long-term treatment of bipolar disorder: a double-blind 40-week extension study. J Affect Disord 126:358–365. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Cohen M, Zhao J, Alphs L, Macek TA, Panagides J. (2010. b) Asenapine in the treatment of acute mania in bipolar I disorder: a randomized, double-blind, placebo-controlled trial. J Affect Disord 122:27–38. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Soczynska JK, Woldeyohannes HO, Miranda A, Vaccarino A, Macqueen G, Lewis GF, Kennedy SH. (2012. a) A randomized, double-blind, controlled trial evaluating the effect of intranasal insulin on neurocognitive function in euthymic patients with bipolar disorder. Bipolar Disord 14:697–706. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Muzina DJ, Adams A, Lourenco MT, Law CW, Soczynska JK, Woldeyohannes HO, Nathanson J, Kennedy SH. (2009. b) Quetiapine XR efficacy and tolerability as monotherapy and as adjunctive treatment to conventional antidepressants in the acute and maintenance treatment of major depressive disorder: a review of registration trials. Expert Opin Pharmacother 10:3061–3075. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Alsuwaidan M, Goldstein BI, Taylor VH, Schaffer A, Beaulieu S, Kemp DE, Canadian Network for M, Anxiety Treatments Task F (2012. b) The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid metabolic disorders. Ann Clin Psychiatry 24:69–81. [PubMed] [Google Scholar]
- Medda P, Perugi G, Zanello S, Ciuffa M, Cassano GB. (2009) Response to ECT in bipolar I, bipolar II and unipolar depression. J Affect Disord 118:55–59. [DOI] [PubMed] [Google Scholar]
- Meehan K, Zhang F, David S, Tohen M, Janicak P, Small J, Koch M, Rizk R, Walker D, Tran P, Breier A. (2001) A double-blind, randomized comparison of the efficacy and safety of intramuscular injections of olanzapine, lorazepam, or placebo in treating acutely agitated patients diagnosed with bipolar mania. J Clin Psychopharmacol 21:389–397. [DOI] [PubMed] [Google Scholar]
- Melia PI. (1970) Prophylactic lithium: a double-blind trial in recurrent affective disorders. Br J Psychiatry 116:621–624. [DOI] [PubMed] [Google Scholar]
- Mendels J. (1976) Lithium in the treatment of depression. Am J Psychiatry 133:373–378. [DOI] [PubMed] [Google Scholar]
- Meyer TD, Hautzinger M. (2012) Cognitive behaviour therapy and supportive therapy for bipolar disorders: relapse rates for treatment period and 2-year follow-up. PsycholMed 42:1429–1439. [DOI] [PubMed] [Google Scholar]
- Michalak EE, Guiraud-Diawara A, Sapin C. (2014) Asenapine treatment and health-related quality of life in patients experiencing bipolar I disorder with mixed episodes: post-hoc analyses of pivotal trials. Curr Med Res Opin 30:711–718. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, George EL, Richards JA, Simoneau TL, Suddath RL. (2003) A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. ArchGenPsychiatry 60:904–912. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Simoneau TL, George EL, Richards JA, Kalbag A, Sachs-Ericsson N, Suddath R. (2000) Family-focused treatment of bipolar disorder: 1-year effects of a psychoeducational program in conjunction with pharmacotherapy. BiolPsychiatry 48:582–592. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Wisniewski SR, Kogan JN, Nierenberg AA, Calabrese JR, Marangell LB, Gyulai L, Araga M, Gonzalez JM, Shirley ER, Thase ME, Sachs GS. (2007. a) Psychosocial treatments for bipolar depression: a 1-year randomized trial from the Systematic Treatment Enhancement Program. ArchGenPsychiatry 64:419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Kogan JN, Sachs GS, Thase ME, Calabrese JR, Marangell LB, Ostacher MJ, Patel J, Thomas MR, Araga M, Gonzalez JM, Wisniewski SR. (2007. b) Intensive psychosocial intervention enhances functioning in patients with bipolar depression: results from a 9-month randomized controlled trial. AmJPsychiatry 164:1340–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishory A, Winokur M, Bersudsky Y. (2003) Prophylactic effect of phenytoin in bipolar disorder: a controlled study. Bipolar Disord 5:464–467. [DOI] [PubMed] [Google Scholar]
- Mishory A, Yaroslavsky Y, Bersudsky Y, Belmaker RH. (2000) Phenytoin as an antimanic anticonvulsant: a controlled study. Am J Psychiatry 157:463–465. [DOI] [PubMed] [Google Scholar]
- Miziou S, Tsitsipa E, Moysidou S, Karavelas V, Dimelis D, Polyzoidou V, Fountoulakis KN. (2015) Psychosocial treatment and interventions for bipolar disorder: a systematic review. Annals of general psychiatry 14:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad O, Osser DN. (2014) The psychopharmacology algorithm project at the Harvard South Shore Program: an algorithm for acute mania. Harv Rev Psychiatry 22:274–294. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery DB. (2001) ECNP Consensus Meeting March 2000 Nice: guidelines for investigating efficacy in bipolar disorder. European College of Neuropsychopharmacology. Eur Neuropsychopharmacol 11:79–88. [DOI] [PubMed] [Google Scholar]
- Moosavi SM, Ahmadi M, Monajemi MB. (2014) Risperidone versus risperidone plus sodium valproate for treatment of bipolar disorders: a randomized, double-blind clinical-trial. Global journal of health science 6:36424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukai T, Kishi T, Matsuda Y, Iwata N. (2014) A meta-analysis of inositol for depression and anxiety disorders. Hum Psychopharmacol 29:55–63. [DOI] [PubMed] [Google Scholar]
- Mula M, Sander JW. (2007) Suicidal ideation in epilepsy and levetiracetam therapy. Epilepsy Behav 11:130–132. [DOI] [PubMed] [Google Scholar]
- Muller-Oerlinghausen B, Retzow A, Henn FA, Giedke H, Walden J. (2000) Valproate as an adjunct to neuroleptic medication for the treatment of acute episodes of mania: a prospective, randomized, double-blind, placebo-controlled, multicenter study. European Valproate Mania Study Group. J Clin Psychopharmacol 20:195–203. [DOI] [PubMed] [Google Scholar]
- Muralidharan K, Ali M, Silveira LE, Bond DJ, Fountoulakis KN, Lam RW, Yatham LN. (2013) Efficacy of second generation antipsychotics in treating acute mixed episodes in bipolar disorder: a meta-analysis of placebo-controlled trials. J Affect Disord 150:408–414. [DOI] [PubMed] [Google Scholar]
- Murphy BL, Stoll AL, Harris PQ, Ravichandran C, Babb SM, Carlezon WA, Jr, Cohen BM. (2012) Omega-3 fatty acid treatment, with or without cytidine, fails to show therapeutic properties in bipolar disorder: a double-blind, randomized add-on clinical trial. J Clin Psychopharmacol 32:699–703. [DOI] [PubMed] [Google Scholar]
- Murru A, Popovic D, Pacchiarotti I, Hidalgo D, Leon-Caballero J, Vieta E. (2015) Management of adverse effects of mood stabilizers. Curr Psychiatry Rep 17:603. [DOI] [PubMed] [Google Scholar]
- Muzina DJ, Momah C, Eudicone JM, Pikalov A, McQuade RD, Marcus RN, Sanchez R, Carlson BX. (2008) Aripiprazole monotherapy in patients with rapid-cycling bipolar I disorder: an analysis from a long-term, double-blind, placebo-controlled study. Int J Clin Pract 62:679–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzina DJ, Gao K, Kemp DE, Khalife S, Ganocy SJ, Chan PK, Serrano MB, Conroy CM, Calabrese JR. (2010) Acute efficacy of divalproex sodium versus placebo in mood stabilizer-naive bipolar I or II depression: a double-blind, randomized, placebo-controlled trial. J Clin Psychiatry 72:813–819. [DOI] [PubMed] [Google Scholar]
- Nahas Z, Kozel FA, Li X, Anderson B, George MS. (2003) Left prefrontal transcranial magnetic stimulation (TMS) treatment of depression in bipolar affective disorder: a pilot study of acute safety and efficacy. Bipolar Disord 5:40–47. [DOI] [PubMed] [Google Scholar]
- National Collaborating Centre for Mental Health (2006) Bipolar disorder.The management of bipolar disorder in adults, children and adolescents, in primary and secondary care. CG38 NICE Guideline. [Google Scholar]
- Nejtek VA, Avila M, Chen LA, Zielinski T, Djokovic M, Podawiltz A, Kaiser K, Bae S, Rush AJ. (2008) Do atypical antipsychotics effectively treat co-occurring bipolar disorder and stimulant dependence? A randomized, double-blind trial. J Clin Psychiatry 69:1257–1266. [DOI] [PubMed] [Google Scholar]
- Nemeroff CB, Evans DL, Gyulai L, Sachs GS, Bowden CL, Gergel IP, Oakes R, Pitts CD. (2001) Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry 158:906–912. [DOI] [PubMed] [Google Scholar]
- Nery FG, Monkul ES, Hatch JP, Fonseca M, Zunta-Soares GB, Frey BN, Bowden CL, Soares JC. (2008) Celecoxib as an adjunct in the treatment of depressive or mixed episodes of bipolar disorder: a double-blind, randomized, placebo-controlled study. Hum Psychopharmacol 23:87–94. [DOI] [PubMed] [Google Scholar]
- Ng F, Mammen OK, Wilting I, Sachs GS, Ferrier IN, Cassidy F, Beaulieu S, Yatham LN, Berk M. (2009) The International Society for Bipolar Disorders (ISBD) consensus guidelines for the safety monitoring of bipolar disorder treatments. Bipolar Disord 11:559–595. [DOI] [PubMed] [Google Scholar]
- NHS U (2014) Antidepressants - Side effects In. [Google Scholar]
- NICE (2014) Bipolar disorder. In. [Google Scholar]
- Nierenberg AA, Ostergaard SD, Iovieno N, Walker RS, Fava M, Papakostas GI. (2015) Predictors of placebo response in bipolar depression. Int Clin Psychopharmacol 30:59–66. [DOI] [PubMed] [Google Scholar]
- Nilsson L, Ahlbom A, Farahmand BY, Asberg M, Tomson T. (2002) Risk factors for suicide in epilepsy: a case control study. Epilepsia 43:644–651. [DOI] [PubMed] [Google Scholar]
- Niufan G, Tohen M, Qiuqing A, Fude Y, Pope E, McElroy H, Ming L, Gaohua W, Xinbao Z, Huichun L, Liang S. (2008) Olanzapine versus lithium in the acute treatment of bipolar mania: A double-blind, randomized, controlled trial. J Affect Disord 105:101–108. [DOI] [PubMed] [Google Scholar]
- Nivoli AM, Colom F, Murru A, Pacchiarotti I, Castro-Loli P, Gonzalez-Pinto A, Fountoulakis KN, Vieta E. (2011) New treatment guidelines for acute bipolar depression: a systematic review. J Affect Disord 129:14–26. [DOI] [PubMed] [Google Scholar]
- Nivoli AM, Murru A, Goikolea JM, Crespo JM, Montes JM, Gonzalez-Pinto A, Garcia-Portilla P, Bobes J, Saiz-Ruiz J, Vieta E. (2012) New treatment guidelines for acute bipolar mania: a critical review. J Affect Disord 140:125–141. [DOI] [PubMed] [Google Scholar]
- Nolen W, Kupka R, Schulte P, Knoppert-van der Klein E, Honig A, Reichart C. (2008) Richtlijn bipolaire stoornissen. 2 ed. Utrecht: De Tijdstrom Uitgerverij BV. [Google Scholar]
- Nolen WA, Weisler RH. (2013) The association of the effect of lithium in the maintenance treatment of bipolar disorder with lithium plasma levels: a post hoc analysis of a double-blind study comparing switching to lithium or placebo in patients who responded to quetiapine (Trial 144). Bipolar Disord 15:100–109. [DOI] [PubMed] [Google Scholar]
- Norris ER, Karen B, Correll JR, Zemanek KJ, Lerman J, Primelo RA, Kaufmann MW. (2013) A double-blind, randomized, placebo-controlled trial of adjunctive ramelteon for the treatment of insomnia and mood stability in patients with euthymic bipolar disorder. J Affect Disord 144:141–147. [DOI] [PubMed] [Google Scholar]
- Noyes R, Jr, Dempsey GM. (1974) Lithium treatment of depression. Diseases of the nervous system 35:573–576. [PubMed] [Google Scholar]
- Noyes R, Jr, Dempsey GM, Blum A, Cavanaugh GL. (1974) Lithium treatment of depression. Compr Psychiatry 15:187–193. [DOI] [PubMed] [Google Scholar]
- O’Dowd A. (2006) NICE issues new guidance to improve the treatment of bipolar disorder. Bmj 333:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogawa Y, Tajika A, Takeshima N, Hayasaka Y, Furukawa TA. (2014) Mood stabilizers and antipsychotics for acute mania: a systematic review and meta-analysis of combination/augmentation therapy versus monotherapy. CNS Drugs 28:989–1003. [DOI] [PubMed] [Google Scholar]
- Okuma T, Inanaga K, Otsuki S, Sarai K, Takahashi R, Hazama H, Mori A, Watanabe M. (1979) Comparison of the antimanic efficacy of carbamazepine and chlorpromazine: a double-blind controlled study. Psychopharmacology (Berl) 66:211–217. [DOI] [PubMed] [Google Scholar]
- Okuma T, Inanaga K, Otsuki S, Sarai K, Takahashi R, Hazama H, Mori A, Watanabe S. (1981) A preliminary double-blind study on the efficacy of carbamazepine in prophylaxis of manic-depressive illness. Psychopharmacology (Berl) 73:95–96. [DOI] [PubMed] [Google Scholar]
- Okuma T, Yamashita I, Takahashi R, Itoh H, Otsuki S, Watanabe S, Sarai K, Hazama H, Inanaga K. (1990) Comparison of the antimanic efficacy of carbamazepine and lithium carbonate by double-blind controlled study. Pharmacopsychiatry 23:143–150. [DOI] [PubMed] [Google Scholar]
- Olesen JB, Hansen PR, Erdal J, Abildstrom SZ, Weeke P, Fosbol EL, Poulsen HE, Gislason GH. (2010) Antiepileptic drugs and risk of suicide: a nationwide study. Pharmacoepidemiol Drug Saf 19:518–524. [DOI] [PubMed] [Google Scholar]
- Ono S, Mihara K, Suzuki A, Kondo T, Yasui-Furukori N, Furukori H, de Vries R, Kaneko S. (2002) Significant pharmacokinetic interaction between risperidone and carbamazepine: its relationship with CYP2D6 genotypes. Psychopharmacology (Berl) 162:50–54. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Galfalvy HC, Currier D, Grunebaum MF, Sher L, Sullivan GM, Burke AK, Harkavy-Friedman J, Sublette ME, Parsey RV, Mann JJ. (2011) Treatment of suicide attempters with bipolar disorder: a randomized clinical trial comparing lithium and valproate in the prevention of suicidal behavior. Am J Psychiatry 168:1050–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman OT, Rudorfer MV, Potter WZ. (1989) Idazoxan: a selective alpha 2-antagonist and effective sustained antidepressant in two bipolar depressed patients. Arch Gen Psychiatry 46:958–959. [DOI] [PubMed] [Google Scholar]
- Ostacher MJ. (2014) When positive isn’t positive: the hopes and disappointments of clinical trials. J Clin Psychiatry 75:e1186–1187. [DOI] [PubMed] [Google Scholar]
- Ostacher MJ, Tandon R, Suppes T. (2015. a) Florida Best Practice Psychotherapeutic Medication Guidelines for Adults With Bipolar Disorder: a novel, practical, patient-centered guide for clinicians. J Clin Psychiatry. [DOI] [PubMed] [Google Scholar]
- Ostacher MJ, Suppes T, Swann AC, Eudicone JM, Landsberg W, Baker RA, Carlson BX. (2015. b) Patterns of response to aripiprazole, lithium, haloperidol, and placebo across factor scores of mania. International journal of bipolar disorders 3:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostacher MJ, Nierenberg AA, Iosifescu DV, Eidelman P, Lund HG, Ametrano RM, Kaczynski R, Calabrese J, Miklowitz DJ, Sachs GS, Perlick DA. (2008) Correlates of subjective and objective burden among caregivers of patients with bipolar disorder. Acta PsychiatrScand 118:49–56. [DOI] [PubMed] [Google Scholar]
- Pacchiarotti I, et al. (2013) The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am J Psychiatry 170:1249–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pae CU, Masand PS, Mandel FS, O’Gorman C. (2012) Achieving and sustaining remission in bipolar I disorder with ziprasidone: a post hoc analysis of a 24-week, double-blind, placebo-controlled study. Clin Drug Investig 32:747–754. [DOI] [PubMed] [Google Scholar]
- Pan YJ, Hsieh MH, Liu SK. (2011) Visuospatial working memory deficits in remitted patients with bipolar disorder: susceptibility to the effects of GABAergic agonists. Bipolar Disord 13:365–376. [DOI] [PubMed] [Google Scholar]
- Pande AC, Crockatt JG, Janney CA, Werth JL, Tsaroucha G. (2000) Gabapentin in bipolar disorder: a placebo-controlled trial of adjunctive therapy. Gabapentin Bipolar Disorder Study Group. Bipolar Disord 2:249–255. [DOI] [PubMed] [Google Scholar]
- Parker G, Tully L, Olley A, Hadzi-Pavlovic D. (2006) SSRIs as mood stabilizers for Bipolar II Disorder? A proof of concept study. J Affect Disord 92:205–214. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Pae CU, Vohringer PA, Mauer S, Narasimhan M, Dalley S, Loebel A, Masand PS, Ghaemi SN. (2015) A 13-week, randomized double-blind, placebo-controlled, cross-over trial of ziprasidone in bipolar spectrum disorder. J Clin Psychopharmacol 35:319–323. [DOI] [PubMed] [Google Scholar]
- Patorno E, Bohn RL, Wahl PM, Avorn J, Patrick AR, Liu J, Schneeweiss S. (2010) Anticonvulsant medications and the risk of suicide, attempted suicide, or violent death. JAMA 303:1401–1409. [DOI] [PubMed] [Google Scholar]
- Pecknold JC, Fleury D. (1986) Alprazolam-induced manic episode in two patients with panic disorder. Am J Psychiatry 143:652–653. [DOI] [PubMed] [Google Scholar]
- Perich T, Manicavasagar V, Mitchell PB, Ball JR. (2013. a) The association between meditation practice and treatment outcome in Mindfulness-based Cognitive Therapy for bipolar disorder. BehavResTher 51:338–343. [DOI] [PubMed] [Google Scholar]
- Perich T, Manicavasagar V, Mitchell PB, Ball JR, Hadzi-Pavlovic D. (2013. b) A randomized controlled trial of mindfulness-based cognitive therapy for bipolar disorder. Acta PsychiatrScand 127:333–343. [DOI] [PubMed] [Google Scholar]
- Perlis RH, Welge JA, Vornik LA, Hirschfeld RM, Keck PE., Jr (2006. a) Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry 67:509–516. [DOI] [PubMed] [Google Scholar]
- Perlis RH, Baker RW, Zarate CA, Jr, Brown EB, Schuh LM, Jamal HH, Tohen M. (2006. b) Olanzapine versus risperidone in the treatment of manic or mixed States in bipolar I disorder: a randomized, double-blind trial. J Clin Psychiatry 67:1747–1753. [DOI] [PubMed] [Google Scholar]
- Perlis RH, Purcell S, Fava M, Fagerness J, Rush AJ, Trivedi MH, Smoller JW. (2007. a) Association between treatment-emergent suicidal ideation with citalopram and polymorphisms near cyclic adenosine monophosphate response element binding protein in the STAR*D study. Arch Gen Psychiatry 64:689–697. [DOI] [PubMed] [Google Scholar]
- Perlis RH, Beasley CM, Jr, Wines JD, Jr, Tamura RN, Cusin C, Shear D, Amsterdam J, Quitkin F, Strong RE, Rosenbaum JF, Fava M. (2007. b) Treatment-associated suicidal ideation and adverse effects in an open, multicenter trial of fluoxetine for major depressive episodes. Psychother Psychosom 76:40–46. [DOI] [PubMed] [Google Scholar]
- Perry A, Tarrier N, Morriss R, McCarthy E, Limb K. (1999) Randomised controlled trial of efficacy of teaching patients with bipolar disorder to identify early symptoms of relapse and obtain treatment. BMJ 318:149–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson G. (1972) Lithium prophylaxis in affective disorders. Acta Psychiatr Scand 48:462–479. [Google Scholar]
- Perugi G, Toni C, Frare F, Travierso MC, Hantouche E, Akiskal HS. (2002) Obsessive-compulsive-bipolar comorbidity: a systematic exploration of clinical features and treatment outcome. J Clin Psychiatry 63:1129–1134. [PubMed] [Google Scholar]
- Pilhatsch M, Wolf R, Winter C, Lewitzka U, Bauer M. (2010) Comparison of paroxetine and amitriptyline as adjunct to lithium maintenance therapy in bipolar depression: a reanalysis of a randomized, double-blind study. J Affect Disord 126:453–457. [DOI] [PubMed] [Google Scholar]
- Placidi GF, Lenzi A, Lazzerini F, Cassano GB, Akiskal HS. (1986) The comparative efficacy and safety of carbamazepine versus lithium: a randomized, double-blind 3-year trial in 83 patients. J Clin Psychiatry 47:490–494. [PubMed] [Google Scholar]
- Platman SR. (1970) A comparison of lithium carbonate and chlorpromazine in mania. Am J Psychiatry 127:351–353. [DOI] [PubMed] [Google Scholar]
- Pope HG, Jr, McElroy SL, Keck PE, Jr, Hudson JI. (1991) Valproate in the treatment of acute mania. A placebo-controlled study. Arch Gen Psychiatry 48:62–68. [DOI] [PubMed] [Google Scholar]
- Popovic D, Nuss P, Vieta E. (2015) Revisiting loxapine: a systematic review. Ann Gen Psychiatry 14:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popovic D, Reinares M, Amann B, Salamero M, Vieta E. (2010) Number needed to treat analyses of drugs used for maintenance treatment of bipolar disorder. Psychopharmacology (Berl) 213:657–667. [DOI] [PubMed] [Google Scholar]
- Post R, Leverich G, Altshuler L, Mikalauskas K. (1992) Lithium-discontinuation-induced refractoriness: Preliminary observations. Am J Psychiatry 149:1727. [DOI] [PubMed] [Google Scholar]
- Post RM, Uhde TW, Roy-Byrne PP, Joffe RT. (1986) Antidepressant effects of carbamazepine. Am J Psychiatry 143:29–34. [DOI] [PubMed] [Google Scholar]
- Post RM, Uhde TW, Roy-Byrne PP, Joffe RT. (1987) Correlates of antimanic response to carbamazepine. Psychiatry Res 21:71–83. [DOI] [PubMed] [Google Scholar]
- Post RM, Uhde TW, Ballenger JC, Chatterji DC, Greene RF, Bunney WE., Jr (1983) Carbamazepine and its -10,11-epoxide metabolite in plasma and CSF. Relationship to antidepressant response. Arch Gen Psychiatry 40:673–676. [DOI] [PubMed] [Google Scholar]
- Post RM, Altshuler LL, Frye MA, Suppes T, Rush AJ, Keck PE, Jr, McElroy SL, Denicoff KD, Leverich GS, Kupka R, Nolen WA. (2001) Rate of switch in bipolar patients prospectively treated with second-generation antidepressants as augmentation to mood stabilizers. Bipolar Disord 3:259–265. [PubMed] [Google Scholar]
- Post RM, Leverich GS, Nolen WA, Kupka RW, Altshuler LL, Frye MA, Suppes T, McElroy S, Keck P, Grunze H, Walden J, Stanley Foundation Bipolar N (2003) A re-evaluation of the role of antidepressants in the treatment of bipolar depression: data from the Stanley Foundation Bipolar Network. Bipolar Disord 5:396–406. [DOI] [PubMed] [Google Scholar]
- Post RM, Altshuler LL, Leverich GS, Frye MA, Nolen WA, Kupka RW, Suppes T, McElroy S, Keck PE, Denicoff KD, Grunze H, Walden J, Kitchen CM, Mintz J. (2006) Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry 189:124–131. [DOI] [PubMed] [Google Scholar]
- Potkin SG, Keck PE, Jr, Segal S, Ice K, English P. (2005) Ziprasidone in acute bipolar mania: a 21-day randomized, double-blind, placebo-controlled replication trial. J Clin Psychopharmacol 25:301–310. [DOI] [PubMed] [Google Scholar]
- Praharaj SK, Ram D, Arora M. (2009) Efficacy of high frequency (rapid) suprathreshold repetitive transcranial magnetic stimulation of right prefrontal cortex in bipolar mania: a randomized sham controlled study. J Affect Disord 117:146–150. [DOI] [PubMed] [Google Scholar]
- Prien RF, Caffey EM, Jr, Klett CJ. (1972) Comparison of lithium carbonate and chlorpromazine in the treatment of mania. Report of the Veterans Administration and National Institute of Mental Health Collaborative Study Group. Arch Gen Psychiatry 26:146–153. [DOI] [PubMed] [Google Scholar]
- Prien RF, Klett CJ, Caffey EM., Jr (1973. a) Lithium carbonate and imipramine in prevention of affective episodes. A comparison in recurrent affective illness. Arch Gen Psychiatry 29:420–425. [DOI] [PubMed] [Google Scholar]
- Prien RF, Caffey EM, Jr, Klett CJ. (1973. b) Prophylactic efficacy of lithium carbonate in manic-depressive illness. Report of the Veterans Administration and National Institute of Mental Health collaborative study group. Arch Gen Psychiatry 28:337–341. [DOI] [PubMed] [Google Scholar]
- Prien RF, Kupfer DJ, Mansky PA, Small JG, Tuason VB, Voss CB, Johnson WE. (1984) Drug therapy in the prevention of recurrences in unipolar and bipolar affective disorders. Report of the NIMH Collaborative Study Group comparing lithium carbonate, imipramine, and a lithium carbonate-imipramine combination. Arch Gen Psychiatry 41:1096–1104. [DOI] [PubMed] [Google Scholar]
- Pugh MJ, Copeland LA, Zeber JE, Wang CP, Amuan ME, Mortensen EM, Tabares JV, Van Cott AC, Cooper TL, Cramer JA. (2012) Antiepileptic drug monotherapy exposure and suicide-related behavior in older veterans. J Am Geriatr Soc 60:2042–2047. [DOI] [PubMed] [Google Scholar]
- Quante A, Zeugmann S, Luborzewski A, Schommer N, Langosch J, Born C, Anghelescu I, Wolf J. (2010) Aripiprazole as adjunct to a mood stabilizer and citalopram in bipolar depression: a randomized placebo-controlled pilot study. Hum Psychopharmacol 25:126–132. [DOI] [PubMed] [Google Scholar]
- Quiroz JA, Yatham LN, Palumbo JM, Karcher K, Kushner S, Kusumakar V. (2010) Risperidone long-acting injecTable monotherapy in the maintenance treatment of bipolar I disorder. Biol Psychiatry 68:156–162. [DOI] [PubMed] [Google Scholar]
- Rajagopalan K, Bacci ED, Wyrwich KW, Pikalov A, Loebel A. (2016) The direct and indirect effects of lurasidone monotherapy on functional improvement among patients with bipolar depression: results from a randomized placebo-controlled trial. International journal of bipolar disorders 4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rea MM, Tompson MC, Miklowitz DJ, Goldstein MJ, Hwang S, Mintz J. (2003) Family-focused treatment versus individual treatment for bipolar disorder: results of a randomized clinical trial. JConsult ClinPsychol 71:482–492. [DOI] [PubMed] [Google Scholar]
- Reinares M, Sanchez-Moreno J, Fountoulakis KN. (2014) Psychosocial interventions in bipolar disorder: what, for whom, and when. J Affect Disord 156:46–55. [DOI] [PubMed] [Google Scholar]
- Reinares M, Vieta E, Colom F, Martinez-Aran A, Torrent C, Comes M, Goikolea JM, Benabarre A, Sanchez-Moreno J. (2004) Impact of a psychoeducational family intervention on caregivers of stabilized bipolar patients. PsychotherPsychosom 73:312–319. [DOI] [PubMed] [Google Scholar]
- Reinares M, Colom F, Sanchez-Moreno J, Torrent C, Martinez-Aran A, Comes M, Goikolea JM, Benabarre A, Salamero M, Vieta E. (2008) Impact of caregiver group psychoeducation on the course and outcome of bipolar patients in remission: a randomized controlled trial. BipolarDisord 10:511–519. [DOI] [PubMed] [Google Scholar]
- Rendell JM, Gijsman HJ, Keck P, Goodwin GM, Geddes JR. (2003) Olanzapine alone or in combination for acute mania. Cochrane Database Syst Rev:CD004040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendell JM, Gijsman HJ, Bauer MS, Goodwin GM, Geddes GR. (2006) Risperidone alone or in combination for acute mania. Cochrane Database Syst Rev:CD004043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reus VI, Targum SD, Weingarter H, Post RM. (1979) Effect of lithium carbonate on memory processes of bipolar affectively ill patients. Psychopharmacology (Berl) 63:39–42. [DOI] [PubMed] [Google Scholar]
- Riesenberg RA, Baldytcheva I, Datto C. (2012) Self-reported sedation profile of quetiapine extended-release and quetiapine immediate-release during 6-day initial dose escalation in bipolar depression: a multicenter, randomized, double-blind, phase IV study. Clin Ther 34:2202–2211. [DOI] [PubMed] [Google Scholar]
- Rihmer Z, Akiskal H. (2006) Do antidepressants t(h)reat(en) depressives? Toward a clinically judicious formulation of the antidepressant-suicidality FDA advisory in light of declining national suicide statistics from many countries. J Affect Disord 94:3–13. [DOI] [PubMed] [Google Scholar]
- Rihmer Z, Barsi J, Belso N, Pestality P, Gyorgy S. (1996) Antidepressant-induced hypomania in obsessive-compulsive disorder. Int Clin Psychopharmacol 11:203–205. [DOI] [PubMed] [Google Scholar]
- Robertson B, Grunze H, Versavel M, Costa R, Almeida L, Soares-da-Silva P. (2010) Results of a double-blind, randomized, dose-titration, placebo controlled multicenter trial (SCO/BIA-2093–203 study) on safety and efficacy of eslicarbazepine acetate (BIA 2–093) for acute manic episodes associated with biopolar I disorder. Bipolar Disord:46. [Google Scholar]
- Romeo B, Choucha W, Fossati P, Rotge JY. (2015) Meta-analysis of short- and mid-term efficacy of ketamine in unipolar and bipolar depression. Psychiatry Res 230:682–688. [DOI] [PubMed] [Google Scholar]
- Rosa AR, Fountoulakis K, Siamouli M, Gonda X, Vieta E. (2009) Is anticonvulsant treatment of mania a class effect? Data from randomized clinical trials. CNS Neurosci Ther 17:167–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblat JD, Kakar R, Berk M, Kessing LV, Vinberg M, Baune BT, Mansur RB, Brietzke E, Goldstein BI, McIntyre RS. (2016) Anti-inflammatory agents in the treatment of bipolar depression: a systematic review and meta-analysis. Bipolar Disord 18:89–101. [DOI] [PubMed] [Google Scholar]
- Rosenbluth M, Macqueen G, McIntyre RS, Beaulieu S, Schaffer A, Canadian Network for M, Anxiety Treatments Task F (2012) The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid personality disorders. Ann Clin Psychiatry 24:56–68. [PubMed] [Google Scholar]
- Rouillon F, Serrurier D, Miller HD, Gerard MJ. (1991) Prophylactic efficacy of maprotiline on unipolar depression relapse. J Clin Psychiatry 52:423–431. [PubMed] [Google Scholar]
- Roy Chengappa KN, Schwarzman LK, Hulihan JF, Xiang J, Rosenthal NR, Clinical Affairs Product Support Study I (2006) Adjunctive topiramate therapy in patients receiving a mood stabilizer for bipolar I disorder: a randomized, placebo-controlled trial. J Clin Psychiatry 67:1698–1706. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Crismon ML, Kashner TM, Toprac MG, Carmody TJ, Trivedi MH, Suppes T, Miller AL, Biggs MM, Shores-Wilson K, Witte BP, Shon SP, Rago WV, Altshuler KZ. (2003) Texas Medication Algorithm Project, phase 3 (TMAP-3): rationale and study design. J Clin Psychiatry 64:357–369. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Rago WV, Crismon ML, Toprac MG, Shon SP, Suppes T, Miller AL, Trivedi MH, Swann AC, Biggs MM, Shores-Wilson K, Kashner TM, Pigott T, Chiles JA, Gilbert DA, Altshuler KZ. (1999) Medication treatment for the severely and persistently mentally ill: the Texas Medication Algorithm Project. J Clin Psychiatry 60:284–291. [DOI] [PubMed] [Google Scholar]
- Sachs G, Chengappa KN, Suppes T, Mullen JA, Brecher M, Devine NA, Sweitzer DE. (2004) Quetiapine with lithium or divalproex for the treatment of bipolar mania: a randomized, double-blind, placebo-controlled study. Bipolar Disord 6:213–223. [DOI] [PubMed] [Google Scholar]
- Sachs G, Sanchez R, Marcus R, Stock E, McQuade R, Carson W, Abou-Gharbia N, Impellizzeri C, Kaplita S, Rollin L, Iwamoto T, Aripiprazole Study G (2006) Aripiprazole in the treatment of acute manic or mixed episodes in patients with bipolar I disorder: a 3-week placebo-controlled study. J Psychopharmacol 20:536–546. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Printz DJ, Kahn DA, Carpenter D, Docherty JP. (2000) The Expert Consensus Guideline Series: Medication Treatment of Bipolar Disorder 2000. Postgrad Med Spec No:1–104. [PubMed] [Google Scholar]
- Sachs GS, Grossman F, Ghaemi SN, Okamoto A, Bowden CL. (2002) Combination of a mood stabilizer with risperidone or haloperidol for treatment of acute mania: a double-blind, placebo-controlled comparison of efficacy and safety. Am J Psychiatry 159:1146–1154. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Lafer B, Stoll AL, Banov M, Thibault AB, Tohen M, Rosenbaum JF. (1994) A double-blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry 55:391–393. [PubMed] [Google Scholar]
- Sachs GS, Ice KS, Chappell PB, Schwartz JH, Gurtovaya O, Vanderburg DG, Kasuba B. (2011) Efficacy and safety of adjunctive oral ziprasidone for acute treatment of depression in patients with bipolar I disorder: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 72:1413–1422. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Vanderburg DG, Edman S, Karayal ON, Kolluri S, Bachinsky M, Cavus I. (2012. a) Adjunctive oral ziprasidone in patients with acute mania treated with lithium or divalproex, part 1: results of a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 73:1412–1419. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Vanderburg DG, Edman S, Karayal ON, Kolluri S, Bachinsky M, Cavus I. (2012. b) Adjunctive oral ziprasidone in patients with acute mania treated with lithium or divalproex, part 2: influence of protocol-specific eligibility criteria on signal detection. J Clin Psychiatry 73:1420–1425. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Collins MA, Altshuler LL, Ketter TA, Suppes T, Rasgon NL, Frye MA, Wozniak P. (2001) Divalproex sodium versus placebo in the treatment of bipolar depression. In: 40th Annual Meeting of the American College of Neuropsychopharmacology. San Juan, Puerto Rico. [Google Scholar]
- Sachs GS, Greenberg WM, Starace A, Lu K, Ruth A, Laszlovszky I, Nemeth G, Durgam S. (2015) Cariprazine in the treatment of acute mania in bipolar I disorder: a double-blind, placebo-controlled, phase III trial. J Affect Disord 174:296–302. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Nierenberg AA, Calabrese JR, Marangell LB, Wisniewski SR, Gyulai L, Friedman ES, Bowden CL, Fossey MD, Ostacher MJ, Ketter TA, Patel J, Hauser P, Rapport D, Martinez JM, Allen MH, Miklowitz DJ, Otto MW, Dennehy EB, Thase ME. (2007) Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med 356:1711–1722. [DOI] [PubMed] [Google Scholar]
- Sahraian A, Bigdeli M, Ghanizadeh A, Akhondzadeh S. (2014) Topiramate as an adjuvant treatment for obsessive compulsive symptoms in patients with bipolar disorder: a randomized double blind placebo controlled clinical trial. J Affect Disord 166:201–205. [DOI] [PubMed] [Google Scholar]
- Salinsky MC, Storzbach D, Spencer DC, Oken BS, Landry T, Dodrill CB. (2005) Effects of topiramate and gabapentin on cognitive abilities in healthy volunteers. Neurology 64:792–798. [DOI] [PubMed] [Google Scholar]
- Salloum IM, Cornelius JR, Daley DC, Kirisci L, Himmelhoch JM, Thase ME. (2005) Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind placebo-controlled study. Arch Gen Psychiatry 62:37–45. [DOI] [PubMed] [Google Scholar]
- Salloum IM, Douaihy A, Cornelius JR, Kirisci L, Kelly TM, Hayes J. (2007) Divalproex utility in bipolar disorder with co-occurring cocaine dependence: a pilot study. Addictive behaviors 32:410–415. [DOI] [PubMed] [Google Scholar]
- Sanford M, Scott LJ. (2008) Intramuscular aripiprazole: a review of its use in the management of agitation in schizophrenia and bipolar I disorder. CNS Drugs 22:335–352. [DOI] [PubMed] [Google Scholar]
- Sanford M, Dhillon S. (2015) Lurasidone: a review of its use in adult patients with bipolar I depression. CNS Drugs 29:253–263. [DOI] [PubMed] [Google Scholar]
- Sanger TM, Tohen M, Vieta E, Dunner DL, Bowden CL, Calabrese JR, Feldman PD, Jacobs TG, Breier A. (2003) Olanzapine in the acute treatment of bipolar I disorder with a history of rapid cycling. J Affect Disord 73:155–161. [DOI] [PubMed] [Google Scholar]
- Saricicek A, Maloney K, Muralidharan A, Ruf B, Blumberg HP, Sanacora G, Lorberg B, Pittman B, Bhagwagar Z. (2010) Lvetiracetam in the management of bipolar depression: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 72:744–750. [DOI] [PubMed] [Google Scholar]
- Sarris J, Mischoulon D, Schweitzer I. (2012) Omega-3 for bipolar disorder: meta-analyses of use in mania and bipolar depression. J Clin Psychiatry 73:81–86. [DOI] [PubMed] [Google Scholar]
- Sayyaparaju KK, Grunze H, Fountoulakis KN. (2014) When to start aripiprazole therapy in patients with bipolar mania. Neuropsychiatric disease and treatment 10:459–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaffer A, Zuker P, Levitt A. (2006) Randomized, double-blind pilot trial comparing lamotrigine versus citalopram for the treatment of bipolar depression. J Affect Disord 96:95–99. [DOI] [PubMed] [Google Scholar]
- Schaffer A, McIntosh D, Goldstein BI, Rector NA, McIntyre RS, Beaulieu S, Swinson R, Yatham LN, Canadian Network for M, Anxiety Treatments Task F (2012) The CANMAT task force recommendations for the management of patients with mood disorders and comorbid anxiety disorders. Ann Clin Psychiatry 24:6–22. [PubMed] [Google Scholar]
- Scherk H, Pajonk FG, Leucht S. (2007) Second-generation antipsychotic agents in the treatment of acute mania: a systematic review and meta-analysis of randomized controlled trials. Arch Gen Psychiatry 64:442–455. [DOI] [PubMed] [Google Scholar]
- Schneck CD, Miklowitz DJ, Miyahara S, Araga M, Wisniewski S, Gyulai L, Allen MH, Thase ME, Sachs GS. (2008) The Prospective Course of Rapid-Cycling Bipolar Disorder: Findings From the STEP-BD. Am J Psychiatry. [DOI] [PubMed] [Google Scholar]
- Schoeyen HK, Kessler U, Andreassen OA, Auestad BH, Bergsholm P, Malt UF, Morken G, Oedegaard KJ, Vaaler A. (2015) Treatment-resistant bipolar depression: a randomized controlled trial of electroconvulsive therapy versus algorithm-based pharmacological treatment. Am J Psychiatry 172:41–51. [DOI] [PubMed] [Google Scholar]
- Schumann G, et al. (2014) Stratified medicine for mental disorders. Eur Neuropsychopharmacol 24:5–50. [DOI] [PubMed] [Google Scholar]
- Scott J, Paykel E, Morriss R, Bentall R, Kinderman P, Johnson T, Abbott R, Hayhurst H. (2006) Cognitive-behavioural therapy for severe and recurrent bipolar disorders: randomised controlled trial. BrJPsychiatry 188:313–320. [DOI] [PubMed] [Google Scholar]
- Segal J, Berk M, Brook S. (1998) Risperidone compared with both lithium and haloperidol in mania: a double-blind randomized controlled trial. Clin Neuropharmacol 21:176–180. [PubMed] [Google Scholar]
- Senturk V, Goker C, Bilgic A, Olmez S, Tugcu H, Oncu B, Atbasoglu EC. (2007) Impaired verbal memory and otherwise spared cognition in remitted bipolar patients on monotherapy with lithium or valproate. Bipolar Disord 9Suppl 1:136–144. [DOI] [PubMed] [Google Scholar]
- Seo HJ, Chiesa A, Lee SJ, Patkar AA, Han C, Masand PS, Serretti A, Pae CU. (2010) Safety and tolerability of lamotrigine: results from 12 placebo-controlled clinical trials and clinical implications. Clin Neuropharmacol 34:39–47. [DOI] [PubMed] [Google Scholar]
- Sepede G, Di lorio G, Lupi M, Sarchione F, Acciavatti T, Fiori F, Santacroce R, Martinotti G, Gambi F, Di Giannantonio M. (2014) Bupropion as an add-on therapy in depressed bipolar disorder type I patients with comorbid cocaine dependence. Clin Neuropharmacol 37:17–21. [DOI] [PubMed] [Google Scholar]
- Severus E, Taylor MJ, Sauer C, Pfennig A, Ritter P, Bauer M, Geddes JR. (2014) Lithium for prevention of mood episodes in bipolar disorders: systematic review and meta-analysis. International journal of bipolar disorders 2:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafti SS. (2010) Olanzapine vs lithium in management of acute mania. J Affect Disord 122:273–276. [DOI] [PubMed] [Google Scholar]
- Shaw ED, Mann JJ, Stokes PE, Manevitz AZ. (1986) Effects of lithium carbonate on associative productivity and idiosyncrasy in bipolar outpatients. Am J Psychiatry 143:1166–1169. [DOI] [PubMed] [Google Scholar]
- Shaw ED, Stokes PE, Mann JJ, Manevitz AZ. (1987) Effects of lithium carbonate on the memory and motor speed of bipolar outpatients. J Abnorm Psychol 96:64–69. [PubMed] [Google Scholar]
- Sheehan DV, Harnett-Sheehan K, Hidalgo RB, Janavs J, McElroy SL, Amado D, Suppes T. (2013) Randomized, placebo-controlled trial of quetiapine XR and divalproex ER monotherapies in the treatment of the anxious bipolar patient. J Affect Disord 145:83–94. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, McElroy SL, Harnett-Sheehan K, Keck PE, Jr, Janavs J, Rogers J, Gonzalez R, Shivakumar G, Suppes T. (2009) Randomized, placebo-controlled trial of risperidone for acute treatment of bipolar anxiety. J Affect Disord 115:376–385. [DOI] [PubMed] [Google Scholar]
- Shelton RC, Stahl SM. (2004) Risperidone and paroxetine given singly and in combination for bipolar depression. J Clin Psychiatry 65:1715–1719. [DOI] [PubMed] [Google Scholar]
- Sherwood Brown E, Carmody TJ, Schmitz JM, Caetano R, Adinoff B, Swann AC, John Rush A. (2009) A randomized, double-blind, placebo-controlled pilot study of naltrexone in outpatients with bipolar disorder and alcohol dependence. Alcohol Clin Exp Res 33:1863–1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwood Brown E, Davila D, Nakamura A, Carmody TJ, Rush AJ, Lo A, Holmes T, Adinoff B, Caetano R, Swann AC, Sunderajan P, Bret ME. (2014) A randomized, double-blind, placebo-controlled trial of quetiapine in patients with bipolar disorder, mixed or depressed phase, and alcohol dependence. Alcohol Clin Exp Res 38:2113–2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Schuh LM, Trzepacz PT, Huang LX, Namjoshi MA, Tohen M. (2004. a) Improvement of Positive and Negative Syndrome Scale cognitive score associated with olanzapine treatment of acute mania. Curr Med Res Opin 20:1371–1376. [DOI] [PubMed] [Google Scholar]
- Shi L, Namjoshi MA, Swindle R, Yu X, Risser R, Baker RW, Tohen M. (2004. b) Effects of olanzapine alone and olanzapine/fluoxetine combination on health-related quality of life in patients with bipolar depression: secondary analyses of a double-blind, placebo-controlled, randomized clinical trial. Clin Ther 26:125–134. [DOI] [PubMed] [Google Scholar]
- Sholomskas AJ. (1990) Mania in a panic disorder patient treated with fluoxetine. Am J Psychiatry 147:1090–1091. [DOI] [PubMed] [Google Scholar]
- Shopsin B, Gershon S, Thompson H, Collins P. (1975) Psychoactive drugs in mania. A controlled comparison of lithium carbonate, chlorpromazine, and haloperidol. Arch Gen Psychiatry 32:34–42. [DOI] [PubMed] [Google Scholar]
- Siamouli M, Samara M, Fountoulakis KN. (2014) Is antiepileptic-induced suicidality a data-based class effect or an exaggeration? A comment on the literature. Harv Rev Psychiatry 22:379–381. [DOI] [PubMed] [Google Scholar]
- Sidor MM, Macqueen GM. (2010) Antidepressants for the acute treatment of bipolar depression: a systematic review and meta-analysis. J Clin Psychiatry 72:156–167. [DOI] [PubMed] [Google Scholar]
- Sidor MM, MacQueen GM. (2012) An update on antidepressant use in bipolar depression. Curr Psychiatry Rep 14:696–704. [DOI] [PubMed] [Google Scholar]
- Sienaert P, Lambrichts L, Dols A, De Fruyt J. (2013) Evidence-based treatment strategies for treatment-resistant bipolar depression: a systematic review. Bipolar Disord 15:61–69. [DOI] [PubMed] [Google Scholar]
- Sikdar S, Kulhara P, Avasthi A, Singh H. (1994) Combined chlorpromazine and electroconvulsive therapy in mania. Br J Psychiatry 164:806–810. [DOI] [PubMed] [Google Scholar]
- Silva MT, Zimmermann IR, Galvao TF, Pereira MG. (2013) Olanzapine plus fluoxetine for bipolar disorder: a systematic review and meta-analysis. J Affect Disord 146:310–318. [DOI] [PubMed] [Google Scholar]
- Silverstone T. (2001) Moclobemide vs imipramine in bipolar depression: a multicentre double-blind clinical trial. Acta Psychiatr Scand 104:104–109. [DOI] [PubMed] [Google Scholar]
- Simhandl C, Denk E, Thau K. (1993) The comparative efficacy of carbamazepine low and high serum level and lithium carbonate in the prophylaxis of affective disorders. J Affect Disord 28:221–231. [DOI] [PubMed] [Google Scholar]
- Simon GE, Savarino J, Operskalski B, Wang PS. (2006) Suicide risk during antidepressant treatment. Am J Psychiatry 163:41–47. [DOI] [PubMed] [Google Scholar]
- Small JG, Small IF, Moore DF. (1971) Experimental withdrawal of lithium in recovered manic-depressive patients: a report of five cases. Am J Psychiatry 127:1555–1558. [DOI] [PubMed] [Google Scholar]
- Small JG, Klapper MH, Marhenke JD, Milstein V, Woodham GC, Kellams JJ. (1995) Lithium combined with carbamazepine or haloperidol in the treatment of mania. Psychopharmacol Bull 31:265–272. [PubMed] [Google Scholar]
- Small JG, Klapper MH, Milstein V, Kellams JJ, Miller MJ, Marhenke JD, Small IF. (1991) Carbamazepine compared with lithium in the treatment of mania. Arch Gen Psychiatry 48:915–921. [DOI] [PubMed] [Google Scholar]
- Smith LA, Cornelius V, Warnock A, Tacchi MJ, Taylor D. (2007) Acute bipolar mania: a systematic review and meta-analysis of co-therapy vs monotherapy. Acta Psychiatr Scand 115:12–20. [DOI] [PubMed] [Google Scholar]
- Smith LA, Cornelius VR, Azorin JM, Perugi G, Vieta E, Young AH, Bowden CL. (2010) Valproate for the treatment of acute bipolar depression: systematic review and meta-analysis. J Affect Disord 122:1–9. [DOI] [PubMed] [Google Scholar]
- Smulevich AB, Khanna S, Eerdekens M, Karcher K, Kramer M, Grossman F. (2005) Acute and continuation risperidone monotherapy in bipolar mania: a 3-week placebo-controlled trial followed by a 9-week double-blind trial of risperidone and haloperidol. Eur Neuropsychopharmacol 15:75–84. [DOI] [PubMed] [Google Scholar]
- Sole B, Bonnin CM, Mayoral M, Amann BL, Torres I, Gonzalez-Pinto A, Jimenez E, Crespo JM, Colom F, Tabares-Seisdedos R, Reinares M, Ayuso-Mateos JL, Soria S, Garcia-Portilla MP, Ibanez A, Vieta E, Martinez-Aran A, Torrent C, the CFRG (2014) Functional remediation for patients with bipolar II disorder: Improvement of functioning and subsyndromal symptoms. Eur Neuropsychopharmacol. [DOI] [PubMed] [Google Scholar]
- Song J, Sjolander A, Bergen S, Larsson H, Land M, Lichtenstein P. (2015) Suicide risk in bipolar disorder during treatment with lithium and valproate. Bipolar Disord 17:94. [Google Scholar]
- Squire LR, Judd LL, Janowsky DS, Huey LY. (1980) Effects of lithium carbonate on memory and other cognitive functions. Am J Psychiatry 137:1042–1046. [DOI] [PubMed] [Google Scholar]
- Srisurapanont M, Yatham LN, Zis AP. (1995) Treatment of acute bipolar depression: a review of the literature. Canadian journal of psychiatry 40:533–544. [DOI] [PubMed] [Google Scholar]
- Stahl S, Lombardo I, Loebel A, Mandel FS. (2010) Efficacy of ziprasidone in dysphoric mania: Pooled analysis of two double-blind studies. J Affect Disord 122:39–45. [DOI] [PubMed] [Google Scholar]
- Steiner W. (1991) Fluoxetine-induced mania in a patient with obsessive-compulsive disorder. Am J Psychiatry 148:1403–1404. [DOI] [PubMed] [Google Scholar]
- Stokes PE, Shamoian CA, Stoll PM, Patton MJ. (1971) Efficacy of lithium as acute treatment of manic-depressive illness. Lancet 1:1319–1325. [DOI] [PubMed] [Google Scholar]
- Stoll AL, Locke CA, Vuckovic A, Mayer PV. (1996) Lithium-associated cognitive and functional deficits reduced by a switch to divalproex sodium: a case series. J Clin Psychiatry 57:356–359. [PubMed] [Google Scholar]
- Stoll AL, Severus WE, Freeman MP, Rueter S, Zboyan HA, Diamond E, Cress KK, Marangell LB. (1999) Omega 3 fatty acids in bipolar disorder: a preliminary double-blind, placebo-controlled trial. Arch Gen Psychiatry 56:407–412. [DOI] [PubMed] [Google Scholar]
- Stoll K, Goncalves N, Krober H, Demisch K, Bellaire W. (1989) Use of Carbamazepine in affective illness. In: New directions in affective disorders (Lerer G, Gershon S, eds), pp 540–544. New York: Springer-Verlag. [Google Scholar]
- Suppes T, Calabrese J, Silva R. (2013) Lurasidone adjunctive therapy with lithium or valproate for the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study (PREVAIL 3). Neuropsychopharmacology 38:abstract no. W147. [DOI] [PubMed] [Google Scholar]
- Suppes T, Brown E, Schuh LM, Baker RW, Tohen M. (2005) Rapid versus non-rapid cycling as a predictor of response to olanzapine and divalproex sodium for bipolar mania and maintenance of remission: post hoc analyses of 47-week data. J Affect Disord 89:69–77. [DOI] [PubMed] [Google Scholar]
- Suppes T, Hirschfeld RM, Vieta E, Raines S, Paulsson B. (2008. a) Quetiapine for the treatment of bipolar II depression: analysis of data from two randomized, double-blind, placebo-controlled studies. World J Biol Psychiatry 9:198–211. [DOI] [PubMed] [Google Scholar]
- Suppes T, Eudicone J, McQuade R, Pikalov A, 3rd, Carlson B. (2008. b) Efficacy and safety of aripiprazole in subpopulations with acute manic or mixed episodes of bipolar I disorder. J Affect Disord 107:145–154. [DOI] [PubMed] [Google Scholar]
- Suppes T, Calabrese J, Mitchell P, Pazzaglia P, Potter W, Zarin D. (1995) Algorithms for the treatment of bipolar manic-depressive illness. Psychopharmacol Bull 31:469–474. [PubMed] [Google Scholar]
- Suppes T, Vieta E, Liu S, Brecher M, Paulsson B, Trial I. (2009) Maintenance treatment for patients with bipolar I disorder: results from a north american study of quetiapine in combination with lithium or divalproex (trial 127). Am J Psychiatry 166:476–488. [DOI] [PubMed] [Google Scholar]
- Suppes T, Datto C, Minkwitz M, Nordenhem A, Walker C, Darko D. (2010) Effectiveness of the extended release formulation of quetiapine as monotherapy for the treatment of acute bipolar depression. J Affect Disord 121:106–115. [DOI] [PubMed] [Google Scholar]
- Suppes T, McElroy SL, Sheehan DV, Hidalgo RB, Cosgrove VE, Gwizdowski IS, Feldman NS. (2014) A randomized, double-blind, placebo-controlled study of ziprasidone monotherapy in bipolar disorder with co-occurring lifetime panic or generalized anxiety disorder. J Clin Psychiatry 75:77–84. [DOI] [PubMed] [Google Scholar]
- Suppes T, Silva R, Cucchiaro J, Mao Y, Targum S, Streicher C, Pikalov A, Loebel A. (2015) Lurasidone for the Treatment of Major Depressive Disorder With Mixed Features: A Randomized, Double-Blind, Placebo-Controlled Study. Am J Psychiatry:appiajp201515060770. [DOI] [PubMed] [Google Scholar]
- Suppes T, Swann AC, Dennehy EB, Habermacher ED, Mason M, Crismon ML, Toprac MG, Rush AJ, Shon SP, Altshuler KZ. (2001) Texas Medication Algorithm Project: development and feasibility testing of a treatment algorithm for patients with bipolar disorder. J Clin Psychiatry 62:439–447. [PubMed] [Google Scholar]
- Suppes T, Dennehy EB, Swann AC, Bowden CL, Calabrese JR, Hirschfeld RM, Keck PE, Jr, Sachs GS, Crismon ML, Toprac MG, Shon SP. (2002) Report of the Texas Consensus Conference Panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry 63:288–299. [DOI] [PubMed] [Google Scholar]
- Suppes T, Rush AJ, Dennehy EB, Crismon ML, Kashner TM, Toprac MG, Carmody TJ, Brown ES, Biggs MM, Shores-Wilson K, Witte BP, Trivedi MH, Miller AL, Altshuler KZ, Shon SP. (2003) Texas Medication Algorithm Project, phase 3 (TMAP-3): clinical results for patients with a history of mania. J Clin Psychiatry 64:370–382. [DOI] [PubMed] [Google Scholar]
- Suttajit S, Srisurapanont M, Maneeton N, Maneeton B. (2014) Quetiapine for acute bipolar depression: a systematic review and meta-analysis. Drug design, development and therapy 8:827–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swann AC, Bowden CL, Morris D, Calabrese JR, Petty F, Small J, Dilsaver SC, Davis JM. (1997) Depression during mania. Treatment response to lithium or divalproex. Arch Gen Psychiatry 54:37–42. [DOI] [PubMed] [Google Scholar]
- Swartz HA, Thase ME. (2011) Pharmacotherapy for the treatment of acute bipolar II depression: current evidence. J Clin Psychiatry 72:356–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz HA, Frank E, Cheng Y. (2012) A randomized pilot study of psychotherapy and quetiapine for the acute treatment of bipolar II depression. BipolarDisord 14:211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sylvia LG, Peters AT, Deckersbach T, Nierenberg AA. (2013) Nutrient-based therapies for bipolar disorder: a systematic review. Psychother Psychosom 82:10–19. [DOI] [PubMed] [Google Scholar]
- Sylvia LG, Gold AK, Stange JP, Peckham AD, Deckersbach T, Calabrese JR, Weiss RD, Perlis RH, Nierenberg AA, Ostacher MJ. (2016) A randomized, placebo-controlled proof-of-concept trial of adjunctive topiramate for alcohol use disorders in bipolar disorder. The American journal on addictions / American Academy of Psychiatrists in Alcoholism and Addictions 25:94–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szegedi A, Zhao J, van Willigenburg A, Nations KR, Mackle M, Panagides J. (2011) Effects of asenapine on depressive symptoms in patients with bipolar I disorder experiencing acute manic or mixed episodes: a post hoc analysis of two 3-week clinical trials. BMC Psychiatry 11:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szegedi A, Calabrese JR, Stet L, Mackle M, Zhao J, Panagides J, Apollo Study G (2012) Asenapine as adjunctive treatment for acute mania associated with bipolar disorder: results of a 12-week core study and 40-week extension. J Clin Psychopharmacol 32:46–55. [DOI] [PubMed] [Google Scholar]
- Tada M, Uchida H, Mizushima J, Suzuki T, Mimura M, Nio S. (2015) Antidepressant dose and treatment response in bipolar depression: reanalysis of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) data. J Psychiatr Res 68:151–156. [DOI] [PubMed] [Google Scholar]
- Tamayo JM, Zarate CA, Vieta E, Vazquez G, Tohen M. (2010) Level of response and safety of pharmacological monotherapy in the treatment of acute bipolar I disorder phases: a systematic review and meta-analysis. Int J Neuropsychopharmacol 13:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamayo JM, Sutton VK, Mattei MA, Diaz B, Jamal HH, Vieta E, Zarate CA, Jr, Fumero I, Tohen M. (2009) Effectiveness and safety of the combination of fluoxetine and olanzapine in outpatients with bipolar depression: an open-label, randomized, flexible-dose study in Puerto Rico. J Clin Psychopharmacol 29:358–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarr GP, Glue P, Herbison P. (2010) Comparative efficacy and acceptability of mood stabilizer and second generation antipsychotic monotherapy for acute mania--a systematic review and meta-analysis. J Affect Disord 134:14–19. [DOI] [PubMed] [Google Scholar]
- Tarr GP, Herbison P, de la Barra SL, Glue P. (2011) Study design and patient characteristics and outcome in acute mania clinical trials. Bipolar Disord 13:125–132. [DOI] [PubMed] [Google Scholar]
- Thase ME, Mallinger AG, McKnight D, Himmelhoch JM. (1992) Treatment of imipramine-resistant recurrent depression, IV: A double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry 149:195–198. [DOI] [PubMed] [Google Scholar]
- Thase ME, Bowden CL, Nashat M, Eudicone JM, Marcus R, McQuade RD, Carlson BX. (2012) Aripiprazole in bipolar depression: a pooled, post-hoc analysis by severity of core depressive symptoms. Int J Psychiatry Clin Pract 16:121–131. [DOI] [PubMed] [Google Scholar]
- Thase ME, Macfadden W, Weisler RH, Chang W, Paulsson B, Khan A, Calabrese JR, Group BIS. (2006) Efficacy of quetiapine monotherapy in bipolar I and II depression: a double-blind, placebo-controlled study (the BOLDER II study). J Clin Psychopharmacol 26:600–609. [DOI] [PubMed] [Google Scholar]
- Thase ME, Jonas A, Khan A, Bowden CL, Wu X, McQuade RD, Carson WH, Marcus RN, Owen R. (2008) Aripiprazole monotherapy in nonpsychotic bipolar I depression: results of 2 randomized, placebo-controlled studies. J Clin Psychopharmacol 28:13–20. [DOI] [PubMed] [Google Scholar]
- Thomas JE, Caballero J, Harrington CA. (2015) The incidence of akathisia in the treatment of schizophrenia with aripiprazole, asenapine and lurasidone: a meta-analysis. Curr Neuropharmacol 13:681–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tohen M, Katagiri H, Fujikoshi S, Kanba S. (2013) Efficacy of olanzapine monotherapy in acute bipolar depression: a pooled analysis of controlled studies. J Affect Disord 149:196–201. [DOI] [PubMed] [Google Scholar]
- Tohen M, Castillo J, Baldessarini RJ, Zarate C, Jr, Kando JC. (1995) Blood dyscrasias with carbamazepine and valproate: a pharmacoepidemiological study of 2,228 patients at risk. Am J Psychiatry 152:413–418. [DOI] [PubMed] [Google Scholar]
- Tohen M, Sutton VK, Calabrese JR, Sachs GS, Bowden CL. (2009) Maintenance of response following stabilization of mixed index episodes with olanzapine monotherapy in a randomized, double-blind, placebo-controlled study of bipolar 1 disorder. J Affect Disord 116:43–50. [DOI] [PubMed] [Google Scholar]
- Tohen M, Kanba S, McIntyre RS, Fujikoshi S, Katagiri H. (2014) Efficacy of olanzapine monotherapy in the treatment of bipolar depression with mixed features. J Affect Disord 164:57–62. [DOI] [PubMed] [Google Scholar]
- Tohen M, Castillo J, Cole JO, Miller MG, de los Heros R, Farrer RJ. (1991) Thrombocytopenia associated with carbamazepine: a case series. J Clin Psychiatry 52:496–498. [PubMed] [Google Scholar]
- Tohen M, McDonnell DP, Case M, Kanba S, Ha K, Fang YR, Katagiri H, Gomez JC. (2012) Randomised, double-blind, placebo-controlled study of olanzapine in patients with bipolar I depression. Br J Psychiatry 201:376–382. [DOI] [PubMed] [Google Scholar]
- Tohen M, Calabrese JR, Sachs GS, Banov MD, Detke HC, Risser R, Baker RW, Chou JC, Bowden CL. (2006) Randomized, placebo-controlled trial of olanzapine as maintenance therapy in patients with bipolar I disorder responding to acute treatment with olanzapine. Am J Psychiatry 163:247–256. [DOI] [PubMed] [Google Scholar]
- Tohen M, Baker RW, Altshuler LL, Zarate CA, Suppes T, Ketter TA, Milton DR, Risser R, Gilmore JA, Breier A, Tollefson GA. (2002. a) Olanzapine versus divalproex in the treatment of acute mania. Am J Psychiatry 159:1011–1017. [DOI] [PubMed] [Google Scholar]
- Tohen M, Ketter TA, Zarate CA, Suppes T, Frye M, Altshuler L, Zajecka J, Schuh LM, Risser RC, Brown E, Baker RW. (2003. a) Olanzapine versus divalproex sodium for the treatment of acute mania and maintenance of remission: a 47-week study. Am J Psychiatry 160:1263–1271. [DOI] [PubMed] [Google Scholar]
- Tohen M, Bowden CL, Smulevich AB, Bergstrom R, Quinlan T, Osuntokun O, Wang WV, Oliff HS, Martenyi F, Kryzhanovskaya LA, Greil W. (2008. a) Olanzapine plus carbamazepine v. carbamazepine alone in treating manic episodes. Br J Psychiatry 192:135–143. [DOI] [PubMed] [Google Scholar]
- Tohen M, Jacobs TG, Grundy SL, McElroy SL, Banov MC, Janicak PG, Sanger T, Risser R, Zhang F, Toma V, Francis J, Tollefson GD, Breier A. (2000) Efficacy of olanzapine in acute bipolar mania: a double-blind, placebo-controlled study. The Olanzipine HGGW Study Group. Arch Gen Psychiatry 57:841–849. [DOI] [PubMed] [Google Scholar]
- Tohen M, Chengappa KN, Suppes T, Baker RW, Zarate CA, Bowden CL, Sachs GS, Kupfer DJ, Ghaemi SN, Feldman PD, Risser RC, Evans AR, Calabrese JR. (2004) Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. Br J Psychiatry 184:337–345. [DOI] [PubMed] [Google Scholar]
- Tohen M, Sanger TM, McElroy SL, Tollefson GD, Chengappa KN, Daniel DG, Petty F, Centorrino F, Wang R, Grundy SL, Greaney MG, Jacobs TG, David SR, Toma V. (1999) Olanzapine versus placebo in the treatment of acute mania. Olanzapine HGEH Study Group. Am J Psychiatry 156:702–709. [DOI] [PubMed] [Google Scholar]
- Tohen M, Chengappa KN, Suppes T, Zarate CA, Jr, Calabrese JR, Bowden CL, Sachs GS, Kupfer DJ, Baker RW, Risser RC, Keeter EL, Feldman PD, Tollefson GD, Breier A. (2002. b) Efficacy of olanzapine in combination with valproate or lithium in the treatment of mania in patients partially nonresponsive to valproate or lithium monotherapy. Arch Gen Psychiatry 59:62–69. [DOI] [PubMed] [Google Scholar]
- Tohen M, Goldberg JF, Gonzalez-Pinto Arrillaga AM, Azorin JM, Vieta E, Hardy-Bayle MC, Lawson WB, Emsley RA, Zhang F, Baker RW, Risser RC, Namjoshi MA, Evans AR, Breier A. (2003. b) A 12-week, double-blind comparison of olanzapine vs haloperidol in the treatment of acute mania. Arch Gen Psychiatry 60:1218–1226. [DOI] [PubMed] [Google Scholar]
- Tohen M, Vieta E, Calabrese J, Ketter TA, Sachs G, Bowden C, Mitchell PB, Centorrino F, Risser R, Baker RW, Evans AR, Beymer K, Dube S, Tollefson GD, Breier A. (2003. c) Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 60:1079–1088. [DOI] [PubMed] [Google Scholar]
- Tohen M, Vieta E, Goodwin GM, Sun B, Amsterdam JD, Banov M, Shekhar A, Aaronson ST, Bardenstein L, Grecu-Gabos I, Tochilov V, Prelipceanu D, Oliff HS, Kryzhanovskaya L, Bowden C. (2008. b) Olanzapine versus divalproex versus placebo in the treatment of mild to moderate mania: a randomized, 12-week, double-blind study. J Clin Psychiatry 69:1776–1789. [DOI] [PubMed] [Google Scholar]
- Tohen M, Greil W, Calabrese JR, Sachs GS, Yatham LN, Oerlinghausen BM, Koukopoulos A, Cassano GB, Grunze H, Licht RW, Dell’Osso L, Evans AR, Risser R, Baker RW, Crane H, Dossenbach MR, Bowden CL. (2005) Olanzapine versus lithium in the maintenance treatment of bipolar disorder: a 12-month, randomized, double-blind, controlled clinical trial. Am J Psychiatry 162:1281–1290. [DOI] [PubMed] [Google Scholar]
- Tolliver BK, Desantis SM, Brown DG, Prisciandaro JJ, Brady KT. (2012) A randomized, double-blind, placebo-controlled clinical trial of acamprosate in alcohol-dependent individuals with bipolar disorder: a preliminary report. Bipolar Disord 14:54–63. [DOI] [PubMed] [Google Scholar]
- Tondo L, Hennen J, Baldessarini RJ. (2001) Lower suicide risk with long-term lithium treatment in major affective illness: a meta-analysis. Acta Psychiatr Scand 104:163–172. [DOI] [PubMed] [Google Scholar]
- Tondo L, Hennen J, Baldessarini RJ. (2003) Rapid-cycling bipolar disorder: effects of long-term treatments. Acta Psychiatr Scand 108:4–14. [DOI] [PubMed] [Google Scholar]
- Tondo L, Vazquez G, Baldessarini RJ. (2010) Mania associated with antidepressant treatment: comprehensive meta-analytic review. Acta Psychiatr Scand 121:404–414. [DOI] [PubMed] [Google Scholar]
- Torrent C, et al. (2013) Efficacy of functional remediation in bipolar disorder: a multicenter randomized controlled study. AmJPsychiatry 170:852–859. [DOI] [PubMed] [Google Scholar]
- Truman CJ, Goldberg JF, Ghaemi SN, Baldassano CF, Wisniewski SR, Dennehy EB, Thase ME, Sachs GS. (2007) Self-reported history of manic/hypomanic switch associated with antidepressant use: data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). J Clin Psychiatry 68:1472–1479. [DOI] [PubMed] [Google Scholar]
- Tsai AC, Rosenlicht NZ, Jureidini JN, Parry PI, Spielmans GI, Healy D. (2011) Aripiprazole in the maintenance treatment of bipolar disorder: a critical review of the evidence and its dissemination into the scientific literature. PLoS Med 8:e1000434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsitsipa E, Fountoulakis KN. (2015) The neurocognitive functioning in bipolar disorder: a systematic review of data. Ann Gen Psychiatry 14:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Loos ML, Mulder P, Hartong EG, Blom MB, Vergouwen AC, van Noorden MS, Timmermans MA, Vieta E, Nolen WA, LamLit Study G (2010) Efficacy and safety of two treatment algorithms in bipolar depression consisting of a combination of lithium, lamotrigine or placebo and paroxetine. Acta Psychiatr Scand 122:246–254. [DOI] [PubMed] [Google Scholar]
- van der Loos ML, Mulder P, Hartong EG, Blom MB, Vergouwen AC, van Noorden MS, Timmermans MA, Vieta E, Nolen WA, LamLit Study G (2011) Long-term outcome of bipolar depressed patients receiving lamotrigine as add-on to lithium with the possibility of the addition of paroxetine in nonresponders: a randomized, placebo-controlled trial with a novel design. Bipolar Disord 13:111–117. [DOI] [PubMed] [Google Scholar]
- van der Loos ML, Mulder PG, Hartong EG, Blom MB, Vergouwen AC, de Keyzer HJ, Notten PJ, Luteijn ML, Timmermans MA, Vieta E, Nolen WA, LamLit Study G (2009) Efficacy and safety of lamotrigine as add-on treatment to lithium in bipolar depression: a multicenter, double-blind, placebo-controlled trial. J Clin Psychiatry 70:223–231. [DOI] [PubMed] [Google Scholar]
- Van Lieshout RJ, MacQueen GM. (2010) Efficacy and acceptability of mood stabilisers in the treatment of acute bipolar depression: systematic review. Br J Psychiatry 196:266–273. [DOI] [PubMed] [Google Scholar]
- VanCott AC, Cramer JA, Copeland LA, Zeber JE, Steinman MA, Dersh JJ, Glickman ME, Mortensen EM, Amuan ME, Pugh MJ. (2010) Suicide-related behaviors in older patients with new anti-epileptic drug use: data from the VA hospital system. BMC Med 8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasudev A, Macritchie K, Watson S, Geddes JR, Young AH. (2008) Oxcarbazepine in the maintenance treatment of bipolar disorder. Cochrane Database Syst Rev:CD005171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasudev A, Macritchie K, Vasudev K, Watson S, Geddes J, Young AH. (2011) Oxcarbazepine for acute affective episodes in bipolar disorder. Cochrane Database Syst Rev 12:CD004857. [DOI] [PubMed] [Google Scholar]
- Vasudev K, Goswami U, Kohli K. (2000) Carbamazepine and valproate monotherapy: feasibility, relative safety and efficacy, and therapeutic drug monitoring in manic disorder. Psychopharmacology (Berl) 150:15–23. [DOI] [PubMed] [Google Scholar]
- Vazquez GH, Tondo L, Undurraga J, Baldessarini RJ. (2013) Overview of antidepressant treatment of bipolar depression. Int J Neuropsychopharmacol 16:1673–1685. [DOI] [PubMed] [Google Scholar]
- Vazquez GH, Holtzman JN, Tondo L, Baldessarini RJ. (2015. a) Efficacy and tolerability of treatments for bipolar depression. J Affect Disord 183:258–262. [DOI] [PubMed] [Google Scholar]
- Vazquez GH, Holtzman JN, Lolich M, Ketter TA, Baldessarini RJ. (2015. b) Recurrence rates in bipolar disorder: Systematic comparison of long-term prospective, naturalistic studies versus randomized controlled trials. Eur Neuropsychopharmacol 25:1501–1512. [DOI] [PubMed] [Google Scholar]
- Veronese N, Solmi M, Luchini C, Lu RB, Stubbs B, Zaninotto L, Correll CU. (2016) Acetylcholinesterase inhibitors and memantine in bipolar disorder: A systematic review and best evidence synthesis of the efficacy and safety for multiple disease dimensions. J Affect Disord 197:268–280. [DOI] [PubMed] [Google Scholar]
- Vieta E. (2007) Psychiatry: from interest in conflicts to conflicts of interest. World psychiatry: official journal of the World Psychiatric Association 6:27–29. [PMC free article] [PubMed] [Google Scholar]
- Vieta E. (2014) Antidepressants in bipolar I disorder: never as monotherapy. Am J Psychiatry 171:1023–1026. [DOI] [PubMed] [Google Scholar]
- Vieta E. (2015) [Personalised medicine applied to mental health: Precision psychiatry]. Revista de psiquiatria y salud mental 8:117–118. [DOI] [PubMed] [Google Scholar]
- Vieta E, Bernardo M. (1992) Antidepressant-induced mania in obsessive-compulsive disorder. Am J Psychiatry 149:1282–1283. [DOI] [PubMed] [Google Scholar]
- Vieta E, Mullen J, Brecher M, Paulsson B, Jones M. (2005. a) Quetiapine monotherapy for mania associated with bipolar disorder: combined analysis of two international, double-blind, randomised, placebo-controlled studies. Curr Med Res Opin 21:923–934. [DOI] [PubMed] [Google Scholar]
- Vieta E, Calabrese JR, Goikolea JM, Raines S, Macfadden W, Group BS. (2007) Quetiapine monotherapy in the treatment of patients with bipolar I or II depression and a rapid-cycling disease course: a randomized, double-blind, placebo-controlled study. Bipolar Disord 9:413–425. [DOI] [PubMed] [Google Scholar]
- Vieta E, Suppes T, Eggens I, Persson I, Paulsson B, Brecher M. (2008. a) Efficacy and safety of quetiapine in combination with lithium or divalproex for maintenance of patients with bipolar I disorder (international trial 126). J Affect Disord 109:251–263. [DOI] [PubMed] [Google Scholar]
- Vieta E, Ramey T, Keller D, English PA, Loebel AD, Miceli J. (2010. a) Ziprasidone in the treatment of acute mania: a 12-week, placebo-controlled, haloperidol-referenced study. J Psychopharmacol 24:547–558. [DOI] [PubMed] [Google Scholar]
- Vieta E, Martinez-Aran A, Goikolea JM, Torrent C, Colom F, Benabarre A, Reinares M. (2002) A randomized trial comparing paroxetine and venlafaxine in the treatment of bipolar depressed patients taking mood stabilizers. J Clin Psychiatry 63:508–512. [DOI] [PubMed] [Google Scholar]
- Vieta E, Nuamah IF, Lim P, Yuen EC, Palumbo JM, Hough DW, Berwaerts J. (2010. b) A randomized, placebo- and active-controlled study of paliperidone extended release for the treatment of acute manic and mixed episodes of bipolar I disorder. Bipolar Disord 12:230–243. [DOI] [PubMed] [Google Scholar]
- Vieta E, Montgomery S, Sulaiman AH, Cordoba R, Huberlant B, Martinez L, Schreiner A. (2012) A randomized, double-blind, placebo-controlled trial to assess prevention of mood episodes with risperidone long-acting injecTable in patients with bipolar I disorder. Eur Neuropsychopharmacol 22:825–835. [DOI] [PubMed] [Google Scholar]
- Vieta E, Manuel Goikolea J, Martinez-Aran A, Comes M, Verger K, Masramon X, Sanchez-Moreno J, Colom F. (2006) A double-blind, randomized, placebo-controlled, prophylaxis study of adjunctive gabapentin for bipolar disorder. J Clin Psychiatry 67:473–477. [DOI] [PubMed] [Google Scholar]
- Vieta E, T’Joen C, McQuade RD, Carson WH, Jr, Marcus RN, Sanchez R, Owen R, Nameche L. (2008. b) Efficacy of adjunctive aripiprazole to either valproate or lithium in bipolar mania patients partially nonresponsive to valproate/lithium monotherapy: a placebo-controlled study. Am J Psychiatry 165:1316–1325. [DOI] [PubMed] [Google Scholar]
- Vieta E, Locklear J, Gunther O, Ekman M, Miltenburger C, Chatterton ML, Astrom M, Paulsson B. (2010. c) Treatment options for bipolar depression: a systematic review of randomized, controlled trials. ` 30:579–590. [DOI] [PubMed] [Google Scholar]
- Vieta E, Gunther O, Locklear J, Ekman M, Miltenburger C, Chatterton ML, Astrom M, Paulsson B. (2011) Effectiveness of psychotropic medications in the maintenance phase of bipolar disorder: a meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol 14:1029–1049. [DOI] [PubMed] [Google Scholar]
- Vieta E, Calabrese JR, Hennen J, Colom F, Martinez-Aran A, Sanchez-Moreno J, Yatham LN, Tohen M, Baldessarini RJ. (2004) Comparison of rapid-cycling and non-rapid-cycling bipolar I manic patients during treatment with olanzapine: analysis of pooled data. J Clin Psychiatry 65:1420–1428. [DOI] [PubMed] [Google Scholar]
- Vieta E, Bourin M, Sanchez R, Marcus R, Stock E, McQuade R, Carson W, Abou-Gharbia N, Swanink R, Iwamoto T, Aripoprazole Study G (2005. b) Effectiveness of aripiprazole v. haloperidol in acute bipolar mania: double-blind, randomised, comparative 12-week trial. Br J Psychiatry 187:235–242. [DOI] [PubMed] [Google Scholar]
- Vieta E, Cruz N, Garcia-Campayo J, de Arce R, Manuel Crespo J, Valles V, Perez-Blanco J, Roca E, Manuel Olivares J, Morinigo A, Fernandez-Villamor R, Comes M. (2008. c) A double-blind, randomized, placebo-controlled prophylaxis trial of oxcarbazepine as adjunctive treatment to lithium in the long-term treatment of bipolar I and II disorder. Int J Neuropsychopharmacol 11:445–452. [DOI] [PubMed] [Google Scholar]
- Viktorin A, Lichtenstein P, Thase ME, Larsson H, Lundholm C, Magnusson PK, Landen M. (2014) The risk of switch to mania in patients with bipolar disorder during treatment with an antidepressant alone and in combination with a mood stabilizer. Am J Psychiatry 171:1067–1073. [DOI] [PubMed] [Google Scholar]
- Wang M, Tong JH, Huang DS, Zhu G, Liang GM, Du H. (2014) Efficacy of olanzapine monotherapy for treatment of bipolar I depression: a randomized, double-blind, placebo controlled study. Psychopharmacology (Berl) 231:2811–2818. [DOI] [PubMed] [Google Scholar]
- Watkins SE, Callender K, Thomas DR, Tidmarsh SF, Shaw DM. (1987) The effect of carbamazepine and lithium on remission from affective illness. Br J Psychiatry 150:180–182. [DOI] [PubMed] [Google Scholar]
- Watson S, Gallagher P, Porter RJ, Smith MS, Herron LJ, Bulmer S, Young AH, Ferrier IN. (2012) A randomized trial to examine the effect of mifepristone on neuropsychological performance and mood in patients with bipolar depression. Biol Psychiatry 72:943–949. [DOI] [PubMed] [Google Scholar]
- Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. (1988) Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 145:179–184. [DOI] [PubMed] [Google Scholar]
- Weiser M, Burshtein S, Gershon AA, Marian G, Vlad N, Grecu IG, Tocari E, Tiugan A, Hotineanu M, Davis JM. (2014) Allopurinol for mania: a randomized trial of allopurinol versus placebo as add-on treatment to mood stabilizers and/or antipsychotic agents in manic patients with bipolar disorder. Bipolar Disord 16:441–447. [DOI] [PubMed] [Google Scholar]
- Weisler R, Dunn J, English P. (2003) Adjunctive Ziprasidone for acute bipolar mania: randomized, placebo-controlled trial. In: 4th International Forum on Mood and Anxiety Disorders. Monte Carlo, Monaco. [Google Scholar]
- Weisler RH, Kalali AH, Ketter TA, Group SPDS. (2004) A multicenter, randomized, double-blind, placebo-controlled trial of extended-release carbamazepine capsules as monotherapy for bipolar disorder patients with manic or mixed episodes. J Clin Psychiatry 65:478–484. [DOI] [PubMed] [Google Scholar]
- Weisler RH, Nolen WA, Neijber A, Hellqvist A, Paulsson B, Trial 144 Study I (2011) Continuation of quetiapine versus switching to placebo or lithium for maintenance treatment of bipolar I disorder (Trial 144: a randomized controlled study). J Clin Psychiatry 72:1452–1464. [DOI] [PubMed] [Google Scholar]
- Weisler RH, Keck PE, Jr, Swann AC, Cutler AJ, Ketter TA, Kalali AH, Group SPDS (2005) Extended-release carbamazepine capsules as monotherapy for acute mania in bipolar disorder: a multicenter, randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 66:323–330. [DOI] [PubMed] [Google Scholar]
- Weisler RH, Calabrese JR, Thase ME, Arvekvist R, Stening G, Paulsson B, Suppes T. (2008) Efficacy of quetiapine monotherapy for the treatment of depressive episodes in bipolar I disorder: a post hoc analysis of combined results from 2 double-blind, randomized, placebo-controlled studies. J Clin Psychiatry 69:769–782. [DOI] [PubMed] [Google Scholar]
- Weisler RH, Hirschfeld R, Cutler AJ, Gazda T, Ketter TA, Keck PE, Swann A, Kalali A, Group SPDS. (2006) Extended-release carbamazepine capsules as monotherapy in bipolar disorder: pooled results from two randomised, double-blind, placebo-controlled trials. CNS Drugs 20:219–231. [DOI] [PubMed] [Google Scholar]
- Welten CC, Koeter MW, Wohlfarth TD, Storosum JG, van den Brink W, Gispen-de Wied CC, Leufkens HG, Denys DA. (2016) Does Insight Affect the Efficacy of Antipsychotics in Acute Mania?: An Individual Patient Data Regression Meta-Analysis. J Clin Psychopharmacol 36:71–76. [DOI] [PubMed] [Google Scholar]
- Wen X, Meador KJ, Loring DW, Eisenschenk S, Segal R, Hartzema AG. (2011) Is antiepileptic drug use related to depression and suicidal ideation among patients with epilepsy? Epilepsy Behav 19:494–500. [DOI] [PubMed] [Google Scholar]
- White K, Keck PE, Jr, Lipinski J. (1986) Serotonin-uptake inhibitors in obsessive-compulsive disorder: a case report. Compr Psychiatry 27:211–214. [DOI] [PubMed] [Google Scholar]
- Whittington CJ, Kendall T, Fonagy P, Cottrell D, Cotgrove A, Boddington E. (2004) Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data. Lancet 363:1341–1345. [DOI] [PubMed] [Google Scholar]
- Williams JM, Alatiq Y, Crane C, Barnhofer T, Fennell MJ, Duggan DS, Hepburn S, Goodwin GM. (2008) Mindfulness-based Cognitive Therapy (MBCT) in bipolar disorder: preliminary evaluation of immediate effects on between-episode functioning. JAffectDisord 107:275–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo YS, Bahk WM, Chung MY, Kim DH, Yoon BH, Lee JH, Ahn YM, Chung SK, Kim JG, Lee KH, Paik KC. (2011) Aripiprazole plus divalproex for recently manic or mixed patients with bipolar I disorder: a 6-month, randomized, placebo-controlled, double-blind maintenance trial. Hum Psychopharmacol 26:543–553. [DOI] [PubMed] [Google Scholar]
- Woo YS, Lee JG, Jeong JH, Kim MD, Sohn I, Shim SH, Jon DI, Seo JS, Shin YC, Min KJ, Yoon BH, Bahk WM. (2015) Korean Medication Algorithm Project for Bipolar Disorder: third revision. Neuropsychiatric disease and treatment 11:493–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu JC, Kelsoe JR, Schachat C, Bunney BG, DeModena A, Golshan S, Gillin JC, Potkin SG, Bunney WE. (2009) Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry 66:298–301. [DOI] [PubMed] [Google Scholar]
- Xu AJ, Niciu MJ, Lundin NB, Luckenbaugh DA, Ionescu DF, Richards EM, Vande Voort JL, Ballard ED, Brutsche NE, Machado-Vieira R, Zarate CA., Jr (2015. a) Lithium and Valproate Levels Do Not Correlate with Ketamine’s Antidepressant Efficacy in Treatment-Resistant Bipolar Depression. Neural plasticity 2015:858251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L, Lu Y, Yang Y, Zheng Y, Chen F, Lin Z. (2015. b) Olanzapine-valproate combination versus olanzapine or valproate monotherapy in the treatment of bipolar I mania: a randomized controlled study in a Chinese population group. Neuropsychiatric disease and treatment 11:1265–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatham LN, Paulsson B, Mullen J, Vagero AM. (2004) Quetiapine versus placebo in combination with lithium or divalproex for the treatment of bipolar mania. J Clin Psychopharmacol 24:599–606. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Grossman F, Augustyns I, Vieta E, Ravindran A. (2003) Mood stabilisers plus risperidone or placebo in the treatment of acute mania. International, double-blind, randomised controlled trial. Br J Psychiatry 182:141–147. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Vieta E, Young AH, Moller HJ, Paulsson B, Vagero M. (2007) A double blind, randomized, placebo-controlled trial of quetiapine as an add-on therapy to lithium or divalproex for the treatment of bipolar mania. Int Clin Psychopharmacol 22:212–220. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Kusumakar V, Parikh SV, Haslam DR, Matte R, Sharma V, Kennedy S. (1997) Bipolar depression: treatment options. Can J Psychiatry 42:87S–91S. [PubMed] [Google Scholar]
- Yatham LN, Fountoulakis KN, Rahman Z, Ammerman D, Fyans P, Marler SV, Baker RA, Carlson BX. (2013. a) Efficacy of aripiprazole versus placebo as adjuncts to lithium or valproate in relapse prevention of manic or mixed episodes in bipolar I patients stratified by index manic or mixed episode. J Affect Disord 147:365–372. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Vieta E, Goodwin GM, Bourin M, de Bodinat C, Laredo J, Calabrese J, Agomelatine Study G (2016) Agomelatine or placebo as adjunctive therapy to a mood stabiliser in bipolar I depression: randomised double-blind placebo-controlled trial. Br J Psychiatry 208:78–86. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Kennedy SH, O’Donovan C, Parikh SV, MacQueen G, McIntyre RS, Sharma V, Beaulieu S, Guidelines Group C (2006) Canadian Network for Mood and Anxiety Treatments (CANMAT) guidelines for the management of patients with bipolar disorder: update 2007. Bipolar Disord 8:721–739. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Beaulieu S, Alda M, O’Donovan C, Macqueen G, McIntyre RS, Sharma V, Ravindran A, Young LT, Milev R, Bond DJ, Frey BN, Goldstein BI. (2013. b) The evolution of CANMAT Bipolar Disorder Guidelines: past, present, and future. Bipolar Disord 15:58–60. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Kennedy SH, Schaffer A, Parikh SV, Beaulieu S, O’Donovan C, MacQueen G, McIntyre RS, Sharma V, Ravindran A, Young LT, Young AH, Alda M, Milev R, Vieta E, Calabrese JR, Berk M, Ha K, Kapczinski F. (2009) Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2009. Bipolar Disord 11:225–255. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Kennedy SH, O’Donovan C, Parikh S, MacQueen G, McIntyre R, Sharma V, Silverstone P, Alda M, Baruch P, Beaulieu S, Daigneault A, Milev R, Young LT, Ravindran A, Schaffer A, Connolly M, Gorman CP, Canadian Network for M , Anxiety T. (2005) Canadian Network for Mood and Anxiety Treatments (CANMAT) guidelines for the management of patients with bipolar disorder: consensus and controversies. Bipolar Disord 7Suppl 3:5–69. [DOI] [PubMed] [Google Scholar]
- Yatham LN, et al. (2013. c) Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2013. Bipolar Disord 15:1–44. [DOI] [PubMed] [Google Scholar]
- Yatham LN, et al. (2016) Optimal duration of risperidone or olanzapine adjunctive therapy to mood stabilizer following remission of a manic episode: a CANMAT randomized double-blind trial. Molecular Psychiatry 21:1050–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yerevanian BI, Koek RJ, Feusner JD, Hwang S, Mintz J. (2004) Antidepressants and suicidal behaviour in unipolar depression. Acta Psychiatr Scand 110:452–458. [DOI] [PubMed] [Google Scholar]
- Yildiz A, Vieta E, Leucht S, Baldessarini RJ. (2010) Efficacy of antimanic treatments: meta-analysis of randomized, controlled trials. Neuropsychopharmacology 36:375–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildiz A, Guleryuz S, Ankerst DP, Ongur D, Renshaw PF. (2008) Protein kinase C inhibition in the treatment of mania: a double-blind, placebo-controlled trial of tamoxifen. Arch Gen Psychiatry 65:255–263. [DOI] [PubMed] [Google Scholar]
- Yildiz A, Nikodem M, Vieta E, Correll CU, Baldessarini RJ. (2014) A network meta-analysis on comparative efficacy and all-cause discontinuation of antimanic treatments in acute bipolar mania. Psychol Med:1–19. [DOI] [PubMed] [Google Scholar]
- Yildiz A, Nikodem M, Vieta E, Correll CU, Baldessarini RJ. (2015) A network meta-analysis on comparative efficacy and all-cause discontinuation of antimanic treatments in acute bipolar mania. Psychol Med 45:299–317. [DOI] [PubMed] [Google Scholar]
- Young AH, McElroy SL, Olausson B, Paulsson B, Embolden I, Embolden III. (2014) A randomised, placebo-controlled 52-week trial of continued quetiapine treatment in recently depressed patients with bipolar I and bipolar II disorder. World J Biol Psychiatry 15:96–112. [DOI] [PubMed] [Google Scholar]
- Young AH, Oren DA, Lowy A, McQuade RD, Marcus RN, Carson WH, Spiller NH, Torbeyns AF, Sanchez R. (2009) Aripiprazole monotherapy in acute mania: 12-week randomised placebo- and haloperidol-controlled study. Br J Psychiatry 194:40–48. [DOI] [PubMed] [Google Scholar]
- Young AH, McElroy SL, Bauer M, Philips N, Chang W, Olausson B, Paulsson B, Brecher M, Investigators EI. (2010) A double-blind, placebo-controlled study of quetiapine and lithium monotherapy in adults in the acute phase of bipolar depression (EMBOLDEN I). J Clin Psychiatry 71:150–162. [DOI] [PubMed] [Google Scholar]
- Young LT, Joffe RT, Robb JC, MacQueen GM, Marriott M, Patelis-Siotis I. (2000) Double-blind comparison of addition of a second mood stabilizer versus an antidepressant to an initial mood stabilizer for treatment of patients with bipolar depression. Am J Psychiatry 157:124–126. [DOI] [PubMed] [Google Scholar]
- Zajecka JM, Weisler R, Sachs G, Swann AC, Wozniak P, Sommerville KW. (2002) A comparison of the efficacy, safety, and tolerability of divalproex sodium and olanzapine in the treatment of bipolar disorder. J Clin Psychiatry 63:1148–1155. [DOI] [PubMed] [Google Scholar]
- Zarate CA, Jr, Tohen M. (2004) Double-blind comparison of the continued use of antipsychotic treatment versus its discontinuation in remitted manic patients. Am J Psychiatry 161:169–171. [DOI] [PubMed] [Google Scholar]
- Zarate CA, Jr, Singh JB, Carlson PJ, Quiroz J, Jolkovsky L, Luckenbaugh DA, Manji HK. (2007) Efficacy of a protein kinase C inhibitor (tamoxifen) in the treatment of acute mania: a pilot study. Bipolar Disord 9:561–570. [DOI] [PubMed] [Google Scholar]
- Zarate CA, Jr, Payne JL, Singh J, Quiroz JA, Luckenbaugh DA, Denicoff KD, Charney DS, Manji HK. (2004) Pramipexole for bipolar II depression: a placebo-controlled proof of concept study. Biol Psychiatry 56:54–60. [DOI] [PubMed] [Google Scholar]
- Zarate CA, Jr, Brutsche NE, Ibrahim L, Franco-Chaves J, Diazgranados N, Cravchik A, Selter J, Marquardt CA, Liberty V, Luckenbaugh DA. (2012) Replication of ketamine’s antidepressant efficacy in bipolar depression: a randomized controlled add-on trial. Biol Psychiatry 71:939–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaretsky A, Lancee W, Miller C, Harris A, Parikh SV. (2008) Is cognitive-behavioural therapy more effective than psychoeducation in bipolar disorder? Can J Psychiatry 53:441–448. [DOI] [PubMed] [Google Scholar]
- Zeinoddini A, Sorayani M, Hassanzadeh E, Arbabi M, Farokhnia M, Salimi S, Ghaleiha A, Akhondzadeh S. (2015) Pioglitazone adjunctive therapy for depressive episode of bipolar disorder: a randomized, double-blind, placebo-controlled trial. Depression Anxiety 32:167–173. [DOI] [PubMed] [Google Scholar]
- Zhang ZJ, Kang WH, Tan QR, Li Q, Gao CG, Zhang FG, Wang HH, Ma XC, Chen C, Wang W, Guo L, Zhang YH, Yang XB, Yang GD. (2007) Adjunctive herbal medicine with carbamazepine for bipolar disorders: a double-blind, randomized, placebo-controlled study. J Psychiatr Res 41:360–369. [DOI] [PubMed] [Google Scholar]
- Zhu B, Tunis SL, Zhao Z, Baker RW, Lage MJ, Shi L, Tohen M. (2005) Service utilization and costs of olanzapine versus divalproex treatment for acute mania: results from a randomized, 47-week clinical trial. Curr Med Res Opin 21:555–564. [DOI] [PubMed] [Google Scholar]
- Ziemba KS, O’Carroll CB, Drazkowski JF, Wingerchuk DM, Hoffman-Snyder C, Wellik KE, Demaerschalk BM. (2010) Do antiepileptic drugs increase the risk of suicidality in adult patients with epilepsy?: a critically appraised topic. Neurologist 16:325–328. [DOI] [PubMed] [Google Scholar]
- Zubieta JK, Huguelet P, O’Neil RL, Giordani BJ. (2001) Cognitive function in euthymic bipolar I disorder. Psychiatry Res 102:9–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.