Executive summary
Unprecedented global forces are shaping the health and wellbeing of the largest generation of 10 to 24 year olds in human history. Population mobility, global communications, economic development, and the sustainability of ecosystems are setting the future course for this generation and, in turn, humankind.1,2 At the same time, we have come to new understandings of adolescence as a critical phase in life for achieving human potential. Adolescence is characterised by dynamic brain development in which the interaction with the social environment shapes the capabilities an individual takes forward into adult life.3 During adolescence, an individual acquires the physical, cognitive, emotional, social, and economic resources that are the foundation for later life health and wellbeing. These same resources define trajectories into the next generation. Investments in adolescent health and wellbeing bring benefits today, for decades to come, and for the next generation.
Better childhood health and nutrition, extensions to education, delays in family formation, and new technologies offer the possibility of this being the healthiest generation of adolescents ever. But these are also the ages when new and different health problems related to the onset of sexual activity, emotional control, and behaviour typically emerge. Global trends include those promoting unhealthy lifestyles and commodities, the crisis of youth unemployment, less family stability, environmental degradation, armed conflict, and mass migration, all of which pose major threats to adolescent health and wellbeing.
Adolescents and young adults have until recently been overlooked in global health and social policy, one reason why they have had fewer health gains with economic development than other age groups. The UN Secretary-General’s Global Strategy for Women’s, Children’s and Adolescents’ Health initiated, in September, 2015, presents an outstanding opportunity for investment in adolescent health and wellbeing.4 However, because of limits to resources and technical capacities at both the national and the global level, effective response has many challenges. The question of where to make the most effective investments is now pressing for the international development community. This Commission outlines the opportunities and challenges for investment at both country and global levels (panel 1).
Panel 1. Messages, opportunities, and challenges.
Key messages
Investments in adolescent health and wellbeing bring a triple dividend of benefits now, into future adult life, and for the next generation of children.
Adolescents are biologically, emotionally, and developmentally primed for engagement beyond their families. We must create the opportunities to meaningfully engage with them in all aspects of their lives.
Inequities, including those linked to poverty and gender, shape all aspects of adolescent health and wellbeing: strong multisectoral actions are needed to grow the resources for health and wellbeing and offer second chances to the most disadvantaged.
Adolescents and young adults face unprecedented social, economic, and cultural change. We must transform our health, education, family support, and legal systems to keep pace with these changes.
Outstanding opportunities
Guaranteeing and supporting access to free, quality secondary education for all adolescents presents the single best investment for health and wellbeing.
Tackling preventable and treatable adolescent health problems including infectious diseases, undernutrition, HIV, sexual and reproductive health, injury, and violence will bring huge social and economic benefits. This is key to bringing a grand global convergence in health in all countries by 2030.
The most powerful actions for adolescent health and wellbeing are intersectoral, multilevel, and multi-component: information and broadband technologies present an exceptional opportunity for building capacity within sectors and coordinating actions between them.
Establishing systems for the training, mentoring, and participation of youth health advocates has the potential to transform traditional models of health-care delivery to create adolescent-responsive health systems.
Challenges ahead
Rapid global rises in adolescent health risks for later-life non-communicable diseases will require an unprecedented extent of coordination across sectors from the global to the local level.
Non-communicable diseases of adolescents including mental and substance use disorders, and chronic physical illnesses are becoming the dominant health problems of this age group. Substantial investment in the health-care system and approaches to prevention are required.
Health information systems to support actions in adolescent health remain weak: greater harmonisation and broadening of data collection systems to neglected problems and younger ages will be needed.
Inequalities in health and wellbeing are evident in socially and economically marginalised adolescents, including ethnic minorities, refugees, young offenders, Indigenous, and LGBT adolescents; engagement of adolescents and reconfiguration of service systems to ensure equity of access regardless of sex, ethnic, or socioeconomic status will be essential.
Adolescent health profiles differ greatly between countries and within nation states. These differences usually reflect a country’s progress through an epidemiological transition in which reductions in mortality and fertility shift both population structures and predominating patterns of disease. Just over half of adolescents grow up in multi-burden countries, characterised by high levels of all types of adolescent health problems, including diseases of poverty (HIV and other infectious diseases, undernutrition, and poor sexual and reproductive health), injury and violence, and noncommunicable diseases (NCDs). These countries continue to have high adolescent fecundity and high unmet need for contraception, particularly in unmarried, sexually active adolescents. For these countries, addressing the diseases of poverty is a priority, at the same time as putting in place strategies to avoid sharp rises in injury, mental disorders, and NCD risks. One in eight adolescents grow up in injury excess countries, characterised by high persisting levels of unintentional injury or violence and high adolescent birth rates, and have generally made little progress in reducing these problems in recent decades. For this group of countries there is a need to redouble efforts to reduce injury, violence, and adolescent births as well as avoid sharp rises in mental disorders and NCD risks. Just over a third of adolescents grow up in countries that are NCD predominant, where the major adolescent burden lies in mental and substance use disorders, and chronic physical illness. For this group, the priority is now about universal health coverage and finding effective and scalable prevention strategies for these neglected conditions.
Adolescents and young adults have many unmet needs for health care, and experience barriers that include their inexperience and lack of knowledge about accessing health care, and heightened sensitivity to confidentiality breaches. Further barriers arise from restrictive legislative frameworks, out-of-pocket costs, stigma, and community attitudes. Health-care providers need attitudes, knowledge, and skills that foster engagement with adolescents while maintaining a level of engagement with families. Universal health coverage requires accessible packages of care matched to local need and acceptable to adolescents and young adults. The most effective health service systems include high-quality health worker training, adolescent responsive facilities, and broad community engagement.
Laws have profound effects on adolescent health and wellbeing. Some protect adolescents from harms (eg, preventing child marriage); others could be damaging in limiting access to essential services and goods such as contraception. Although nearly all countries have signed and ratified the UN Convention on the Rights of the Child, there are profound differences in the legal frameworks underpinning adolescent health across countries. Even where national legal frameworks exist, customary or religious laws often take precedence, leaving the rights of adolescents to health too often neglected and undermined.
The expansion of secondary education in many countries, particularly for girls, offers remarkable opportunities for health and wellbeing. Participation in quality secondary education enhances cognitive abilities, improves mental health and sexual and reproductive health, and lowers risks for later-life NCDs. Schools also provide a platform for health promotion that extends from the provision of essential knowledge for health, including comprehensive sexuality education, to maintaining lifestyles that minimise health risks. Equally, avoiding early pregnancy, infectious diseases, mental disorder, injury-related disability, and under-nutrition are essential for achieving the educational and economic benefits that extensions to secondary school offer.
Digital media and broadband technologies offer outstanding new possibilities for engagement and service delivery. Adolescents are biologically, emotionally, and developmentally primed for engagement beyond their families. That engagement is essential for their social and emotional development. It is also a force for change and accountability within communities. Social networking technologies have the potential to galvanise, connect, and mobilise this generation as never before. We must create opportunities to extend youth engagement into the real world. This requires financial investment, strong partnerships with adults, training and mentorship, and the creation of structures and processes that allow adolescent and young adult involvement in decision making.
The most effective actions for adolescent health and wellbeing are intersectoral and multi-component. They could include structural, media, community, online, and school-based elements as well as the provision of preventive and treatment health services. The neglect of adolescent health and wellbeing has resulted in minimal investments in programming, human resources, and technical capacity compared with other age groups. As a consequence there are major gaps in our understanding of adolescent health needs, in the evidence base for action, in civil society structures for advocacy, and the systems for intersectoral action. Within any country there are marked differences in health between different regions and within different adolescent groups, with poverty, gender, and social marginalisation important determinants. Groups such as ethnic minorities, LGBT (lesbian, gay, bisexual, or transgender) youth, those with disabilities, or who are homeless or in juvenile detention have the greatest health needs. Sound information underpins any efficient response. Yet because information systems on health and wellbeing are piecemeal, the needs of these groups are invisible and unmet. A capacity to understand local health needs inclusive of all adolescents, regardless of age, sex, marital status, or socioeconomic status, is essential.
In the face of global change, continued inaction jeopardises the health and wellbeing of this generation and the next. But there are grounds for optimism. The Global Strategy for Women’s, Children’s and Adolescents’ Health offers a framework to drive and coordinate investment, capacity building, research, and evaluation.4 Global strategies to extend education, to reduce gender inequalities and empower women, to improve food security and nutrition, and to promote vocational skills and opportunities for employment are all likely to benefit adolescents and young adults.5 Digital technologies and global communications offer exceptional opportunities for catch-up in training and education, creation of inclusive health information systems, meaningful youth engagement, and cooperation across sectors. This generation of adolescents and young adults can transform all of our futures; there is no more pressing task in global health than ensuring they have the resources to do so.
Introduction
The second Lancet Series on adolescent health concluded that a “Failure to invest in the health of the largest generation of adolescents in the world’s history jeopardises earlier investments in maternal and child health, erodes future quality and length of life, and escalates suffering, inequality, and social instability”.6 The response of the international development community to this and other calls has been striking. From September, 2015, the Every Woman, Every Child agenda has become the Global Strategy for Women’s, Children’s and Adolescents’ Health, supported by a Global Financing Facility.4 This Commission on Adolescent Health and Wellbeing outlines where those investments should be in the years to 2030.
This Commission was established as a network of academics, policy makers, practitioners, and young health advocates with broad expertise in adolescent health. We brought together leading academic institutions in global health (Columbia University, the London School of Hygiene & Tropical Medicine, University College London, and the University of Melbourne). The Commission’s 30 members bring experience from Africa, Asia, Australia, Europe, the Middle East, North America, and South America. They represent diverse disciplines including public health and medicine, behavioural and neuroscience, education, law, economics, and political and social science.
First, we consider the place of adolescent health within the life course, with particular reference to the health capital that accrues or is diminished across these years. We also consider the global forces shaping adolescent and young adult health and our new understanding of healthy development across these years. In the section, Enabling and protective systems, we consider the rapidly changing social and structural determinants of adolescent health and their implications for health promotion and prevention. In the section, The global health profile of adolescents and young adults, we used available data on adolescent and young adult health to provide a global profile that takes into consideration the differing health needs of adolescents as their countries pass through the epidemiological transition. Actions for health summarises a series of reviews of reviews of our current knowledge base for action in adolescent health, concluding with an example of matching country level actions to health needs. We also consider the different roles of health service systems for adolescents. In the section, Adolescent and young adult engagement, we consider models for youth engagement and for accountability in adolescent health and wellbeing. The Commission’s recommendations are detailed in the conclusion.
Adolescence was historically considered to begin with puberty, and to end with transitions into marriage and parenthood.7 In today’s context, the endpoints are often less clear-cut and more commonly around the adoption of other adult roles and responsibilities, including the transition to employment, financial independence, as well as the formation of life partnerships. These events occur at different ages in different parts of the world and local cultural concepts of adolescence vary greatly. Given this variability we have adopted an inclusive age definition of 10 to 24 years for this report. Panel 2 summarises terms that are commonly used to describe this age group.8–10 In general we use the terminology of adolescents and young adults, although in some instances we abbreviate this to adolescents. Given that the field commonly uses the terms youth engagement and youth participation, we have retained these terms.
Panel 2. Definitions of adolescence and young adulthood.
Adolescence is defined by WHO as between 10 and 19 years, while youth refers to 15–24 years. Young people refers to the 10–24-year-old age group, as does the composite term adolescents and young adults. This is the age group and term that is used through the Commission report.
Emerging adulthood has been used to describe the phase of life from the late teens to the late twenties when an individual acquires some of the characteristics of adulthood without having reached the milestones that historically define fully fledged adulthood.
The Convention on the Rights of the Child (1989) defines a child as below the age of 18 years, unless majority is attained earlier under the laws applicable to the child.
The legal age of majority, the point at which an individual is considered an adult, in many countries is 18 years. In law there is no single definition of adulthood but rather a collection of laws that bestow the status of adulthood at differing ages for different activities. These include laws related to the age of consent, the minimum age that young people can legally work, leave school, drive, buy alcohol, marry, be held accountable for criminal action, and the age young people are deemed able to make medical decisions.
When reporting age-disaggregated data, the 10–24-year-old age range is increasingly divided into 5-year age categories. Early adolescence refers to 10–14 years, late adolescence to 15–19 years, and young adulthood to 20–24 years.
Definitions of wellbeing are diverse and range from the subjective to more objective. We adopted a broad, capabilities-based approach to wellbeing, emphasising adolescents’ opportunities to achieve developmentally important goals (eg, access to education, opportunities for civic engagement) in the context of their emerging physical, emotional, and cognitive abilities.11,12
Why adolescent health and wellbeing?
Adolescence is often considered the healthiest time of life. In most countries, adolescence is the point of lowest mortality across the life course, sitting between the peaks of early life mortality and of chronic disease in later adulthood. It is a time where many attributes of good health are at their height,13 and from the perspective of health services, adolescents appear to have fewer needs than those in early childhood or in later years. This dominant view of adolescent health has been the reason why adolescents and young adults have attracted so little interest and investment in global health policy.
However, even from a perspective of conspicuous health needs, there has been a shift in attitude towards adolescents and their health.14 Changes in the health of other age groups is one reason. Mortality has fallen sharply in younger children in high-income and middle-income countries compared with older adolescents and young adults.15 By 2013, mortality in 1 to 4 year olds had fallen to around a quarter of 1980 levels (appendix figure 1). By contrast, deaths in 20 to 24 year olds had only fallen to around 60% of 1980 levels. Deaths in many high-income and middle-income countries are now higher in older male adolescents and young male adults than in 1 to 4 year olds.15
From three perspectives, adolescence and young adulthood have an altogether different significance. Firstly, health and wellbeing underpin the crucial developmental tasks of adolescence including the acquisition of the emotional and cognitive abilities for independence, completion of education and transition to employment, civic engagement, and formation of lifelong relationships. Secondly, adolescence and young adulthood can be seen as the years for laying down the foundations for health that determine health trajectories across the life course. Lastly, adolescents are the next generation to parent; these same health reserves do much to determine the healthy start to life they provide for their children.
The adolescent and young adult years are central in the development of capabilities related to health and wellbeing. These emergent capabilities are dependent on available opportunities (eg, availability of a school), having the resources to use those opportunities (eg, family finances that allow school attendance), and for those who have been socially marginalised, access to second chances (eg, access to education for married girls who have left school).16 Adolescents with longer participation in education, fewer health risks, and slower transitions into marriage and parenthood generally accrue greater capabilities and resources for health. Conversely, early marriage and parenthood, little education, and early exposure to economic and social adversity are likely to diminish an individual’s health and capabilities. Premature autonomy with early disengagement from parents and school and high levels of health risk behaviours predict poorer health and wellbeing.17 The extent to which an individual’s health and wellbeing is fostered or compromised during these years has consequences across the life course as well as influencing the healthy start to life of the next generation.18
Health capital is the set of resources that determine trajectories of health across the lifecourse,19 which typically peak during adolescence and young adulthood. Physical fitness peaks around the age of 20 and remains high until the early 30s when it declines steadily through to old age.20 Those with the highest fitness levels in their 20s are more likely to stay physically healthy throughout life, with less health service use as they age.20 Adolescent cardiorespiratory fitness, muscular strength, and body composition are also predictive of lower rates of all-cause mortality and lower rates of cardiovascular disease in later life than in those who are less fit.21 Adolescence is similarly central in skeletal health. Bone mineral density, a primary determinant of later-life osteoporosis and its complications, peaks in the late teens to early 20s.22 In the 2 years of peak skeletal growth, adolescents accumulate over 25% of their adult bone mass, with patterns of physical activity and adolescent nutrition important modifiable influences.23,24
A growing understanding that neurodevelopment extends across the second and into the third decade of life has implications for both adolescent health and the capacities that underpin wellbeing across the life course (panel 3).25–34 Many cognitive abilities increase markedly from late childhood to peak in the early 20s and then undergo slow decline from the early 30s.35 Analogous to physical health, educational attainment between late childhood and the mid-20s is a strong and independent predictor of cognitive capacity in midlife.36 These cognitive reserves predict later-life physical health and longevity37 and are protective against cognitive decline.36 Equally, maturation of the neural systems underpinning emotional processes might be one reason for higher risks for mental and substance use disorders during these years.38 Maturation of these systems similarly has profound implications for emotional development and the capacities that adolescents bring into their future roles as parents, citizens, and workers.39
Panel 3. Psychological and emotional development through adolescence.
Early adolescence (10–14 years) is biologically dominated by puberty and the effects of the rapid rise in pubertal hormones on body morphology, and sexual and brain development. Adolescence is a time of remodelling of the brain’s reward system. Psychologically it is characterised by low resistance to peer influences, low levels of future orientation, and low risk perception, often leading to increases in risk taking behaviour and poor self-regulation. It is a time of identity formation and development of new interests including emerging interest in sexual and romantic relationships. School and family environments are critical social contexts during this period.
Late adolescence (15–19 years) is also characterised by pubertal maturation, especially in boys, but in ways that are less visually obvious. At this time the brain continues to be extremely developmentally active, particularly in terms of the development of the prefrontal cortex and the increased connectivity between brain networks. This later phase in adolescent brain development brings continued development of executive and self-regulatory skills, leading to greater future orientation and an increased ability to weigh up the short-term and long-term implications of decisions. Family influences become distinctly different during this phase of life, as many adolescents enjoy greater autonomy, even if they still live with their families. Likewise, education settings remain important, although not all adolescents are still engaged in school at this age, especially in low-income and middle-income countries.
Young adulthood (typically 20–24 years) is accompanied by maturation of the prefrontal cortex and associated reasoning and self-regulatory functions. It marks the end of a period of high brain plasticity associated with adolescence whereby the final phase of the organisation of the adult brain occurs. This often corresponds to the adoption of adult roles and responsibilities, including entering the workforce or tertiary education, marriage, childbearing, and economic independence. Secular trends in many developed nations point towards an increase in the age that many of these adult roles are attained, if they are attained at all.
Adolescence and young adulthood are also the years in which an individual establishes the social, cultural, emotional, educational, and economic resources to maintain their health and wellbeing across the life course.40 Hormonal changes that lead to sexual maturation commence with adrenarche in mid-childhood, and continue through puberty. This is a time of adaptation to social and cultural complexity and the point at which gender differences in social and emotional styles, including gender roles, typically crystallise. The foundations for success in the transitions to an independent healthy lifestyle, to employment, and to supportive life partnerships, marriage, and parenthood are also laid in these years.16
Conversely, adolescent health problems and health risks diminish peak fitness and lifetime health. Sexual health risks that result in teenage pregnancy have profound effects on the health and wellbeing of young women across the life course. Pregnancy (and early marriage) typically denotes the end of formal education, restricts opportunities for employment, heightens poverty, and might limit growth in undernourished girls.41 In many countries of low and middle income, adolescents and young adults remain at high risk for infectious diseases, such as HIV that now commonly has a chronic course, while others such as meningitis, tuberculosis, and neglected tropical diseases can similarly have major and persisting effects on health, social and economic adjustment, and wellbeing, albeit for different reasons.42 A range of health risks including tobacco and alcohol use, greater sedentary behaviour, diminished physical activity, increasing overweight, and obesity emerge across adolescence and young adulthood, reducing fitness and ultimately posing major risks for cardiovascular disease and type 2 diabetes in later life.43 Mental disorders commonly emerge during these years with many persisting into adulthood with consequences for mental health across the life course, social adjustment, and economic productivity.44 Substance use during adolescence diminishes fitness, increases risks for many later-life NCDs, and heightens the risk for later substance use disorders.45 Some forms of substance use can also affect adolescent cognitive development and ultimately reduce peak cognitive abilities.46 Injuries, both intentional and unintentional, disproportionately affect adolescents and young adults. They are not only a common cause of adolescent and young adult death in many countries, but also a major cause of disability, including acquired brain injury, leading to diminished health capacity that persists across the life course.
These same resources that underpin life course health and wellbeing are primary determinants of the health and development of the next generation of children. Maternal preconception nutritional deficiencies, whether micronutrients (eg, folate) or macronutrients (eg, protein energy malnutrition), have profound consequences for fetal and infant development with the effects extending to neonatal and early childhood mortality, and stunting.47 Chronic adolescent infectious diseases such as HIV, and chronic physical conditions such as type 1 diabetes mellitus and congenital heart disease require proactive management from adolescence into pregnancy. Adolescent obesity, tobacco and alcohol use, and mental health problems are similarly risks for poor pregnancy outcomes in infants as well as in mothers.48,49 A possibility of trans-generational epigenetic inheritance, whereby preconception influences alter patterns of gene expression that might pass to the next generation, has further heightened interest in preconception parent health, behaviours, and nutrition.50 From this perspective, investment in adolescent health and wellbeing, including lifestyles, knowledge, social, and financial resources for health, can equally be seen as an investment in the next generation.51
In many countries, the focus of health policy is shifting from infectious diseases in early life to NCDs in older adults.52 The life course trajectories of health capital and wellbeing are largely set by young adulthood. The case for optimising health, fitness, and capabilities as well as minimising risks to health and wellbeing are reasons to bring adolescents into sharper focus,18 as is the knowledge that inequalities established by young adulthood persist and account for many of the disparities in health (including cardiovascular disease, cancer, type 2 diabetes, and other NCDs) and wellbeing in later life.
Developing adolescent brains
Neuroscience is shedding new light on changing cognitive and emotional capacities across adolescence. Adolescence can now be understood as a dynamic period of brain development, second only to infancy in the extent and significance of the changes occurring within neural systems (panel 3).53 Much of the research that has led to this understanding has only emerged in the last 20 years. Adolescent brain development differs from that in earlier life, both in its form and regions of greatest activity. It follows the childhood increase in dendritic outgrowth and synaptogenesis and is then characterised by synaptic pruning during the second decade that continues into young adulthood. Pubertal processes, including gonadal hormone changes, have been implicated in maturation of subcortical structures with dimorphic patterns that might be relevant to understanding sex differences in the pattern of mental and behavioural disorders that emerge during adolescence.54 Neurodevelopment is also considerably affected by social and nutritional environments, as well as by exposures, such as substance use.6
Adolescent neurodevelopment has far-reaching implications for the influence of social environments on health.6 The capacity for greater social and emotional engagement that emerges around puberty is likely to have had adaptive advantages in the social contexts in which modern humans evolved.55 Plasticity in neurodevelopment underpins the acquisition of culturally adapted interpersonal and emotional skills that are essential for the more complex social, sexual, and parenting roles that until recently occurred soon after pubertal maturation.56 These biological foundations of adaptive learning also underpin the acquisition of health and human capital from late childhood through to young adulthood. However, the social networks and roles of adolescents today differ markedly from those of earlier, historical environments. The quality, security, and stability of social contexts in which younger adolescents are growing up is likely to be particularly important for the acquisition of skills in emotional processing and social cognition (eg, the capacity to infer the thoughts, intentions, and beliefs of others).28 It is perhaps not surprising that late childhood and early adolescence are often when the first symptoms of most mental disorders emerge.
The ways in which adolescents make decisions, including those affecting their health, differ from those of older adults. One notable difference is the effect of peer presence that affects the processing of social information, with a consequent greater sensitivity to reputational enhancement and damage.57 This sensitivity develops in the transition through puberty and is likely to have had adaptive advantages in an evolutionary context. It is in part related to the way in which younger adolescents differ in terms of a heightened response to the emotional displays of others,58 and is one reason why adolescents spend increased time with peers.59
In a contemporary context, there are often marked differences between peer and family values. The great salience of peers means that for adolescents, peer influences on health and wellbeing are greater than at any other time in the life course.6,60 This sensitivity to peers in decision making is often targeted by teen-oriented entertainment and marketing. In this way the media, particularly social media, shapes attitudes, values, and behaviours in this age group more than any other.61 The media’s contribution to adolescent sexual health risks in east Asian cities, for example, is equivalent to the influence of peers, families, or schools.62 In health promotion and prevention, just as in marketing, interventions that affect the attitudes, values, and behaviours of the peer group are likely to be more powerful than at any other point in the life course.
When making decisions, adolescents seek out and are more influenced by exciting, arousing, and stressful situations compared with adults.27 Adolescents differ from adults in their capacity to over-ride so called hot emotions that arise in emotionally charged situations. This is particularly relevant in the context of sexual activity and one of the reasons why cool-headed intentions fail to predict adolescent behaviour. It is an important reason why relying on condoms for contraception is not wholly effective. It is also one reason why interventions that either avoid hot emotions or are effective irrespective of the emotional context are important. One example is long-acting reversible contraception (LARCs), such as IUDs and implantable contraceptives. The effectiveness of LARCs (that have a 0·2% per annum failure rate in the USA, in comparison to 18·0% for condoms) reflects their consistent presence regardless of the sexual and emotional context.
Adolescent predisposition to sensation seeking is relevant in considering the effects of the digital technology revolution. Adolescents are rapid adopters and high-end consumers of exciting digital and social media.63 Girls tend to use social media more than boys, whose focus is more likely to be on gaming.63 There are potentially great benefits from strong social digital connections during this time, but these same media can equally amplify vulnerabilities from intense emotions.64 The potential of the new media to amplify social contagion is already apparent around adolescent violence, mental health, suicide, and self-harm.65 Extremist groups are increasingly using social media to offer prospects of adventure, belonging, and fulfilment that many adolescents find missing in ordinary life.66
Ultimately, actions to support adolescent health, development, and wellbeing should consider decision-making processes. An adolescent’s perception of their power and agency affects the balance between short-term and long-term goal setting.67 Supporting an adolescent’s capacity to make reflective decisions, considering risks and consequences, has been called “autonomy-enhancing paternalism”.68 Progressively empowering adolescents in decision making as they mature also affects their perception of agency around health. These strategies are particularly important for socially marginalised adolescents such as adolescent girls in contexts of gender inequality. Creation of a sense of agency is an important reason that there is value in creating opportunities for adolescents to exercise self-determination through meaningful participation, supported and facilitated by adults, in decision making that affects their lives and their communities.
The demographic transition and changes in adolescence
The demographic transition describes a country’s shift from high birth and death rates to low fertility, low mortality, and longer life expectancy. The process comes about as a result of economic development. The demographic transition began in many of today’s high-income countries after the Industrial Revolution and is now proceeding rapidly in most countries. This transition is typically accompanied by an epidemiological transition with reductions in maternal mortality, falling rates of infectious disease, and greater child survival into adolescence. One consequence of the demographic and epidemiological transitions has been the survival into adolescence of the largest cohort of adolescents and young adults, relative to other ages, that the world has ever seen (figure 1). The around 1·8 billion people aged 10–24 years represent almost a quarter of the world’s population.70
Figure 1. Adolescents and young adults as a proportion of country population in 2013.
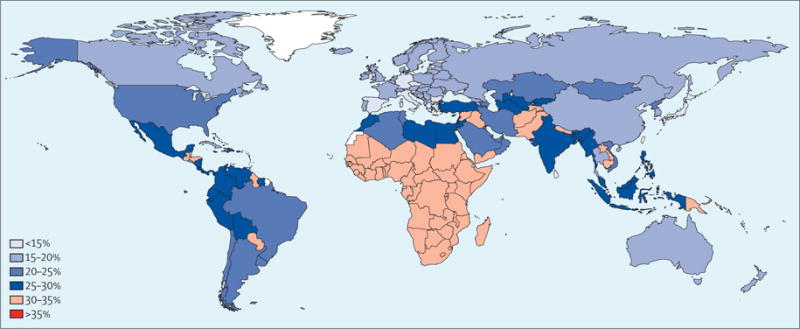
Percentage of total country population aged 10–24 years. Data from Global Health Data Exchange.69
The demographic transition is, in turn, linked to a decline in the ratio of dependants (children and the elderly) to those in the active workforce. This lowered dependency ratio presents a potential demographic dividend for countries to expand their economies and reduce poverty. Although the demographic dividend has now passed for many of today’s high-income countries, it still lies ahead for many low-income countries. The health and human capital of today’s adolescents will be a determinant of future economic and social development in these countries.71
The demographic transition has typically been accompanied by changing patterns of adolescent growth and social development. One consequence of changing patterns of childhood infectious disease and nutrition is a fall in the age of onset of puberty in many countries.72 Conversely, transitions to marriage and parenthood are taking place later than in previous generations. As a result, adolescence now takes up a larger proportion of the life course than ever before. This expansion places adolescence more centrally in the creation of health and human capital than ever before. The greater duration of contemporary adolescence, particularly in the context of rapidly changing consumer and youth cultures, increases the possibility of health risks emerging during these years, with detrimental consequences well into later life.
In pre-industrial societies, the gap between physical maturation and parenthood was generally around 2 years for girls and four years for boys.56 Adolescence was not specifically recognised as the distinct phase of life that it is now in most high-income and middle-income countries. In many high-income countries, first marriage and parenthood now commonly occur 10 to 15 years after the onset of puberty. Indeed, a transition to heterosexual marriage in many places is being replaced by other forms of stable union, including cohabitation and same-sex partnerships. Inter-related drivers of this upward extension of adolescence include economic development, industrialisation, length of education, and urbanisation.73 There are often differences in the timing of the transitions into marriage and parenthood between adolescents in wealthier urban settings compared with those in poorer rural settings, especially in countries of low and middle incomes. In a growing number of countries in which marriage and parenthood are very delayed or where it is no longer rare for marriage or parenthood not to occur, these events no longer signal the end of adolescence.74 Traditional linear sequences of social role transitions such as finishing school, getting a job, getting married, and having children are also increasingly less well defined.74
Changes in the timing and duration of adolescence are accompanied by dramatic alterations in patterns of health risk, particularly around sexual and reproductive health. A delayed transition into marriage and parenthood in high-income and middle-income countries has brought great benefits for young women. When accompanied with ready access to modern contraception, good antenatal care, and legal and safe abortion, the shift has brought extraordinary reductions in maternal mortality and morbidity. Opportunities have opened to extend education and take advantage of social contexts well beyond the immediate family and community, which, in turn, brings greater maturity and experience to later parental roles, in addition to the huge contribution to economic development. Conversely, earlier age of first sexual intercourse and later marriage have created new vulnerabilities, particularly in sexual health, where a pattern of premarital serial sexual relationships creates a period of vulnerability to sexually transmitted infections (STIs) and unplanned pregnancy.75 These changing patterns of risk could be further heightened with the availability of new social media that promote casual sexual intercourse.76
In the past, transitions into marriage and child-rearing were assumed to be a safe haven as they were accompanied by a maturing out of health risks, with benefits including reduced tobacco, alcohol, and illicit substance use, particularly for young men.77 Yet, for many young women, the transition to marriage is accompanied by increasing sexual and reproductive health risks including HIV and sexually transmitted infections, interpersonal violence, and mental disorders.78 With delayed and falling rates of marriage, as well as a growth in other partnerships, the historic benefits of marriage on health risks could diminish. The demographic transition has in many countries been accompanied by changing health risks in adolescents that carry forward into later life. Perhaps the most striking has been a shift from undernutrition and growth stunting to increasing rates of obesity. First in high-income countries and now in countries of low and middle income, there has been a dietary switch toward greater consumption of foods high in addded sugars, salt, and unhealthy fats, and low in important micronutrients. Combined with decreases in physical activity, these patters have fuelled the global rise in obesity.
Adolescents in many countries are also initiating health risk behaviours related to alcohol and other substance use at an earlier age. An additional change is the increasing participation of girls in these same behaviours, continuing into childbearing years. Girls are increasingly coming to marriage and parenthood with more established and heavier patterns of alcohol and other substance use. In the absence of pregnancy planning, these shifting patterns of adolescent health risks create distinct risks for maternal health and fetal development from the preconception through to the postnatal period.79
Enabling and protective systems
Adolescent development takes place within a complex web of family, peer, school, community, media, and broader cultural influences.55 Puberty triggers greater engagement beyond an individual’s family, with a shift to peers, youth cultures, and the social environments created and fostered by new media. This wider social engagement is an important aspect of healthy development in which young people test the values and ideas that have shaped their childhood lives.28 Not only is the range of social influences greater and more complex, but also an extended adolescence increases the duration of their effect into young adulthood and ultimately their significance for health and wellbeing.
Beyond local and national trends, powerful global megatrends increasingly shape the evolution of society, health, and individual development.1 These include growth in educational participation, global patterns of economic development and employment, technological change, changing patterns of migration and conflict, growing urbanisation, political and religious extremism, and environmental degradation. The adolescent and young adult years are increasingly shaped by these global shifts, for better and for worse. For example, growing up in urban settings might lessen family poverty and bring better access to education and health services. Conversely, urban upbringing can heighten risks for mental health problems, substance use, obesity, and physical inactivity. Urban migration might involve whole families, parents, or young people alone, bringing different degrees of separation from the support of family and community. For adolescents living outside of families, urban settings can bring additional risks of sexual exploitation, unsafe employment, and human trafficking.
The digital revolution has the potential to transform the social environment and social networks of today’s adolescents. It has brought mobile phones to the great majority of young people, even in countries of low and middle income.80 The potential benefits in terms of economic development, education, health care, and promotion of democracy are great.1 For adolescents and young adults, new media promote access to an extended social network, without geographic or cultural constraints, bringing the potential for engagement with new ideas and like-minded individuals. Yet the digital revolution also brings new risks for adolescent health. Digital media have extended the marketing of unhealthy commodities and promoted stronger consumer cultures which in turn affect lifestyles, health, and wellbeing.81 Access to global media could accentuate the experience of economic disadvantage as adolescents come to understand the extent of material advantage elsewhere. Online safety has emerged as a further concern, especially for younger adolescents. Experiences of cyber-bullying, grooming for sex, sharing of sexual images, and social contagion around self-harm; mass shootings; radicalisation; and eating disorders have the potential to cause great harm.82 Rising rates of adolescent sleep disturbance and addiction to gaming have also been linked to the new media.83
The social determinants of health are the conditions in which people are born, grow, develop, live, work, and age.55 Within the lifecourse, adolescence is the time of greatest change and diversity in exposure to social determinants, particularly those closest to young people (figure 2). The influence of families remains strong, although family relationships change markedly with adolescents’ greater capacity for autonomy. Inequalities in health related to gender, ethnicity, and sexual orientation tend to increase following puberty.55
Figure 2. Changing proximal social determinants of health across the life course.
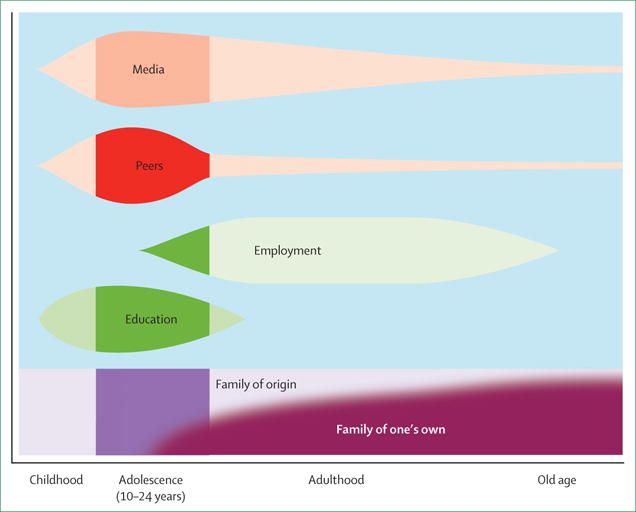
During adolescence, social determinants from outside the family become greater, with major influences of peers, media, education, and the beginning of workplace influences. Community and structural determinants remain consistently influential, as shown by the background shading.
Young people growing up in contemporary societies differ in fundamental ways from those of past generations.84 Key among these differences are changes in the structure and function of families, greater engagement with education, and greater exposure to media influences. Each influence can function as an important enabling and protective system for health.
Family function, structure, and adolescent health
Families provide the primary structure within which children are born, grow, and develop, and from which adolescents transition to adult lives.85 Families are the main protective and enabling setting for children’s health, growth, and wellbeing. Economic development has generally brought changes in family structure, stability, and patterns of transition to the next generation of families. Parents have fewer children, allowing greater investment of family resources for each child.86 Smaller families mean parents can afford to invest more in education.73 This is important in the context where delayed transition into marriage and the formation of the next generation of families necessitates a longer period of parental investment. In the next 10 years, spending on education is projected to grow fastest in countries with the most rapid economic development and declines in fertility.87
Globally, countries outside of sub-Saharan Africa and south Asia have largely moved away from early marriage (appendix figure 2). In the majority of remaining countries with high rates of child marriage there is also a trend to later marriage. In north Africa and the Middle East, scarcity of employment and the financial resources for family formation have created a phase of “waithood”, in which young adults are unable to muster the resources needed for family formation.88 This has in turn been linked to a rise in civil unrest and conflict with potentially devastating effects on health and wellbeing.89
Families take an increasing variety of forms. In most countries, most adolescents still live at home with two parents. Cohabitation of parents rather than marriage is increasingly common, especially in high-income countries where there is also less stigma about single unmarried parents. Parental relationships have become less stable with parental separation now common in many countries. Together with declines in marriage, parental deaths from HIV in some countries, and parental migration for employment in others, there has been a global trend towards more single parent families.85 Living with only one or neither parent is now common in much of sub-Saharan Africa and Latin America.90,91 In Asia, the Middle East, sub-Saharan Africa, Central America, and South America, large numbers of adolescents now live with extended family members rather than parents.85
In high-income countries, many adolescents experience parental divorce, parental remarriage, or change in cohabitation during adolescence. In North America and Europe, around one-fifth of adolescents live in single parent households.85 By 2030 single parent families will make up to 40% of families in many countries.92 Increasing numbers of single parent families could increase adolescent exposure to poverty and lower uptake of education.92 Family instability is linked with poorer outcomes for adolescents including teenage parenthood, early marriage, and later life course trajectories that are themselves characterised by family instability.84,93
Puberty brings major shifts in parent–child relationships, with increases in both conflict and distance as adolescents seek greater independence and more autonomy.94 Such changes in parent–child interactional patterns are normal, but parental difficulty in managing these changes predicts adolescent health risks.95 Parenting capacities, such as those around monitoring and supervision of activities, are important for reducing health risks.84 Beyond this function, families are likely to have a central role in how adolescents learn to respond to new emotional experiences that emerge in and around puberty.96 Parents and peers are both important reference points for the adolescent in learning how to respond to more intense experiences of sadness, anxiety, and anger. The extent to which parents are able to express and respond to emotions is likely to have a major effect on this capacity in their adolescent children.96
Families also have the potential to harm. Family norms might promote gender inequity and attitudes towards violence with profound effects on identity development, reproductive health, mental health, and risks for violence.97 Female genital cutting or mutilation is prevalent across Africa and the Arab world, often perpetuated by families from cultural beliefs that it is necessary to prepare girls for marriage.98 Family violence and abuse have profound effects on adolescent mental health. Adolescents exposed to family violence are more likely to have educational failure and early school leaving, develop substance abuse, and engage in abusive relationships themselves.99
In the context of such secular changes in families and the greater complexity of adolescent social and emotional development, there are important questions about what strategies might best support families to nurture adolescents.92 There have been few systematic studies of the effects of family functioning on adolescent health. In response, we undertook a review of reviews to address the question of how family characteristics are associated with adolescent reproductive health, violence, and mental health (appendix table 2). The vast majority of identified studies focused on younger children with scant evidence around families of adolescents. Most of these studies focused on the effects of parent-adolescent communication. Limited but consistent evidence indicates that parent–adolescent communication (particularly mother–daughter communication) about sex led to delayed initiation of sex, and promoted contraception use.100 Better parent–adolescent communication is also linked to adolescent self-esteem and self-worth,101 better social functioning,102 and fewer mental health problems.101 For LGBT youth, supportive parent– adolescent relationships are protective against risky behaviours.103 Limited but consistent evidence indicates that lower family socioeconomic status and parental education are associated with higher rates of teenage pregnancy.104 Adolescents living in non-intact families or families with problems have higher odds of suicide, substance abuse, depression, and eating problems.102
Given that families and parents remain the most important figures in the lives of most adolescents, the paucity of rigorous research into family influences on adolescent health and wellbeing is a striking knowledge gap.
Education and adolescent health
Education is a powerful determinant of adolescent health and human capital and driver of socioeconomic progress.55,105 Those who are more educated live longer lives with less ill health. This is true in both rich and poor countries and is likely to have a causal relationship.105 The benefits are generally greater for women than men in high-income countries, particularly in terms of mortality, self-reported health, mental health, and obesity.106 Amongst adolescents in countries of low and middle income, higher education is associated with reduced teenage births and older age at marriage.107 Education also has intergenerational effects; improved education for women could account for up to half of the global improvement in child mortality since 1970.108
To date, research on the value of education for health in countries of low and middle income has largely focused on early childhood and primary education.109 There has been little study of the benefits of secondary education for adolescents in countries of low and middle income, despite a dramatic global expansion in the length of education in the past 30 years. Figure 3 shows estimates of global educational attainment. Young women aged 15–24 years had a global average of 9·5 years of education in 2015 in comparison to 9·9 years in young men. Primary education only (mean of 7 years of education or less) was the norm for young men in 22% of countries and for young women in 26% of countries. A minimum of lower secondary education (8–10 years of education) was the norm in 34% of countries for young men and in 18% for young women. Upper secondary or beyond (11 or more years of education) was the norm in 44% of countries for young men and 56% for young women.110
Figure 3. Educational participation of 15–24 year olds for 188 countries.
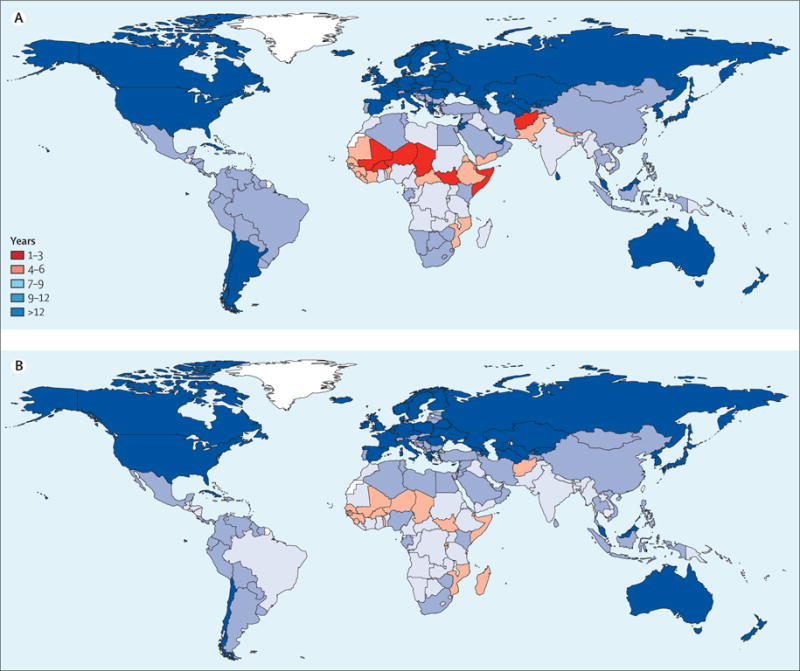
(A) Mean years of education attained in women and girls aged 15–24 years in 2013. (B) Mean years of education attained in men and boys aged 15–24 years in 2013. Data from Global Health Data Exchange.69
The health benefits of secondary education for adolescents have been poorly studied in countries of low and middle income. In high-income countries there might be a threshold effect at the upper secondary level for self-reported health, mental health, and alcohol use, with little additional benefit from tertiary education.106 With primary education now widespread in countries of low and middle income, expansion of participation in secondary education offers an achievable strategy for improving health across the life course and into the next generation.106 In countries that already have high secondary education participation, facilitating schools to more explicitly promote health has the potential for leverage above and beyond the health benefits of educational participation alone.
We used recent data on average years of education for young men and young women aged 15–24 years for 187 countries from 1970 to 2015 and data from UN sources on adolescent fertility and mortality to examine the links between participation in secondary education and health (figure 4, appendix figures 3, 4, 5). Strong associations were found between the average years of education for 15–24-year-old women and girls and adolescent birth rates, all-cause and injury mortality among 15–19-year-old boys and girls, and maternal mortality amongst 15–24 year olds. Each additional year of education for girls was associated with 9·2 fewer births per 1000 girls per year. Countries in which young women generally attended lower secondary education (ie, received 8–10 years of education) had approximately 48 fewer births per 1000 girls per year than those with primary education alone. Those where most young women obtained upper secondary education (11 years or more) had an average of 68 fewer births per 1000 girls per year (figure 4). We then modelled the effect of trends in education on adolescent fertility from 1990 to 2012. Both economic development and increases in education were independently associated with total birth rate. Each additional year of education again decreased adolescent birth rates annually by 8·5 births per 1000 girls per year across all countries when adjusted for growth in national wealth. Accelerating investments to 12 years of education for girls would bring very marked reductions in total adolescent birth rates (appendix figure 5).
Figure 4. Country-level association between adolescent birth rates and years of education in 2010–12.
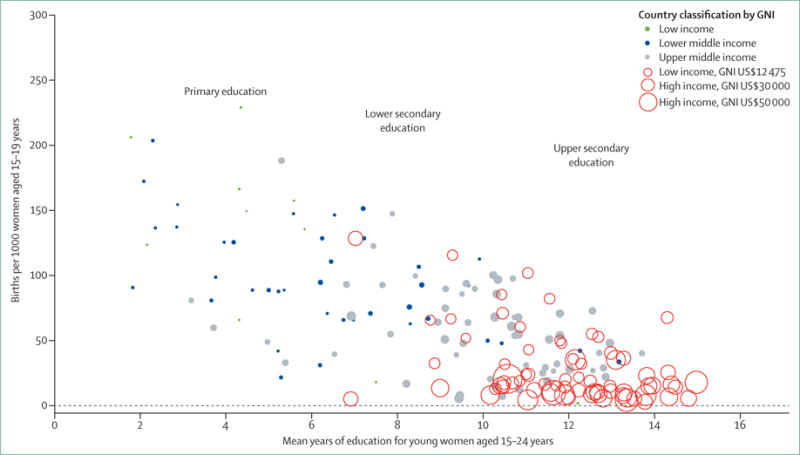
Each additional year of education is associated with an average of nine fewer births per 1000 adolescent girls per country. GNI=gross national income.
Higher average levels of education were associated with lower total adolescent mortality in both sexes, injury mortality (boys only), and maternal mortality, after adjustment for national wealth. Each additional year of education was associated with 13 fewer deaths per 100 000 15–19-year-old boys per year after adjustment for national wealth with a similar but smaller association for girls. For young women 15–24 years, pregnancy-related maternal mortality, while at relatively low levels in most countries providing data, was strongly associated with education. Each additional year of education for young women was associated with 0·4 fewer maternal deaths per 100 000 girls per year in 15–24 year olds after accounting for national wealth. Findings were similar when analyses were rerun using education data for 25–34 year olds instead of 15–24 year olds.
We next identified six cohorts from countries of low and middle income in which it was possible to examine the associations of secondary education participation with health (figure 5, appendix figure 6). In each country, we estimated the association between participation in lower or upper secondary school compared with attending primary school on a range of health outcomes, using structural marginal models and controlling for a range of potential confounders. In each cohort, higher secondary completion was associated with health independent of wealth, age, sex, parental education, and cognitive ability. In one cohort in the Philippines, adolescents with later secondary education had a greater than 50% lower rate of various health problems than those with primary education alone (figure 5). The benefits were most consistent for mental health, alcohol use, and sexual health. Despite being based on observational data, the consistency across cohorts supports secondary education as a major resource for adolescent health and wellbeing extending across the life course.
Figure 5. Association between health at 18 years of age and level of education in the Cebu cohort study, Philippines.
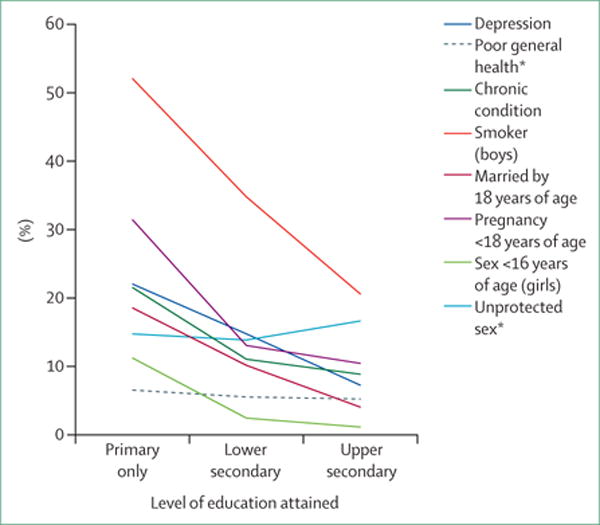
Data from Global Health Data Exchange.69 *These associations were not significant.
Characteristics of health-promoting schools
We reviewed evidence from existing systematic reviews on the school characteristics predictive of health for young people across all country types (appendix text box 1). We addressed the effects of schools’ environments on violence, substance use, and sexual health risks. We focused on these outcomes as each is common, almost entirely initiated during adolescence, and has substantial consequences for health and wellbeing.
The traditional way in which schools address these behaviours is through health education delivered in classrooms, for which there is established evidence of small to moderate effects although implementation is often patchy and effects not sustained.111 The ways that schools operate more widely have great effects on health and wellbeing.112 For this reason actions that address the school environment are more likely to be effective. A school’s ethos extends to the physical and social environment, management and organisation, teaching, discipline, pastoral care, school health services, wholeschool health promotion, and extra-curricular activities.
We found clear evidence that a positive school ethos is associated with health (table 1). One medium quality review113 found that in schools where attainment and attendance are better than predicted based on student sociodemographic factors, rates of adolescent smoking, alcohol use, and drug use and, in one study, violence were lower. Another medium quality review114 found that student connection to school and to teachers was associated with reduced drug use, alcohol use, and smoking. A low quality review115 suggested there were lower rates of violence in schools with positive student–teacher relationships, with students who were aware of rules and accepted these were fair. Another low quality review116 that specifically focused on outcomes for LGBT students found that schools with more supportive policies had lower rates of victimisation. The evidence around school characteristics affecting sexual health were insufficient to draw firm conclusions. Expansion of secondary education in countries with high adolescent fertility and sexual health risks suggests that this is an important question for research and evaluation.
Table 1.
Summary of school effects on adolescent health from a systematic review of reviews of observational studies
| Sexual health | Violence | Tobacco | Alcohol | Drugs | |
|---|---|---|---|---|---|
| Value added education | No or inconsistent evidence | Limited evidence for some benefit | Rigorous evidence for some benefit | Rigorous evidence for some benefit | Rigorous evidence for some benefit |
| Student connection to school or teachers | No or inconsistent evidence | Limited evidence for some benefit | Limited evidence for some benefit | Limited evidence for some benefit | Limited evidence for some benefit |
| School rules or policies | No or inconsistent evidence | Limited evidence for some benefit | No or inconsistent evidence | No or inconsistent evidence | No or inconsistent evidence |
| Physical environment | No or inconsistent evidence | Limited evidence for some benefit | No or inconsistent evidence | Limited evidence for some benefit | Limited evidence for some benefit |
| Student norms | No or inconsistent evidence | Limited evidence for some benefit | Limited evidence for some benefit | Limited evidence for some benefit | No or inconsistent evidence |
| Student socio-demographics | No or inconsistent evidence | Limited evidence for some benefit | No or inconsistent evidence | No or inconsistent evidence | No or inconsistent evidence |
The health and wellbeing benefits of expansion of secondary education accrue through multiple mechanisms, including healthier behaviours, greater cognitive capacity, and longer productive adult lives for the current generation, better health and lower mortality among their children, and overall greater productivity in the future workforce.73 However, many forces operate to exclude or divert adolescents from secondary education. Prominent among these are the costs of education and the costs to families of the loss of adolescent labour, especially in rural areas. In many countries of low and middle income, poor adolescents are less likely to attend secondary school.117 Early marriage accounts for higher dropout rates in girls in many low-income and middle-income countries. Most interventions to increase access to and retention in education in these settings have been in younger adolescents, largely in primary schools. Scholarships, school fee reductions, cash transfers conditional on remaining in school, decrease in grade repetition, school proximity, and education in the mother tongue are cost-effective actions.118,119 Free school uniforms and abolishing school fees are among the most cost-effective interventions, while school meals and financial support to parent–teacher associations are less cost-effective. Building schools close to students is cost-effective, as one school can serve children for many years.118 Addressing gender disparities in access and targeting more resources to the poorest regions as well as to disadvantaged students (notably children affected by armed conflict, children whose home language is not used at school, and children with disabilities) are critical to closing equity gaps.120 There is also a need for greater non-formal or flexible learning strategies for children without access to mainstream education (eg, child labourers and married adolescents who have left school).121 Health interventions including comprehensive sexuality education and providing access to modern contraception are likely to have major benefits in reducing school dropout in settings where early pregnancy is common.122,123
Academic achievement on standardised tests (eg, the Programme for International Student Assessment)124 has commonly been used as an index of school quality. On these measures schools in low-income and middle-income countries lag far behind Organisation for Economic Co-operation and Development (OECD) countries. Yet in higher income settings, narrowly focused international metrics of student attainment have been criticised as the main driver of school performance and educational focus. There is a risk that schools will de-emphasise their essential role in social development, marginalise health actions and health-related education,125 and potentially undermine mental health. Particularly for low achieving students, a narrow focus on academic achievement diminishes self-esteem126 and increases student disengagement, a predisposing factor for academic failure, poor mental health, substance use, violence, and sexual risks.127 Potentially harmful directions in current educational policy that overly focus on academic performance could be mitigated by including health and wellbeing indices alongside educational attainment metrics in school performance management systems.128 Ultimately, promotion of education and health are synergistic goals, both of which are essential for wellbeing and generating human capital; health and wellbeing interventions boost educational attainment while education boosts health and wellbeing.129
Transition into the workforce
The workplace has historically been a major social influence on health from mid-adolescence. A reduction in the number of 10–24 year olds working has followed increased retention in secondary and tertiary education.73 Yet in countries of low and middle income, many adolescents younger than 15 years of age still work. Of these, a substantial minority work in hazardous occupations with poor lifelong earning prospects.130 Over 47·5 million young people aged 15 to 17 years are estimated to work in jobs that expose them to environmental hazards, excessive hours, or physical, psychological, or sexual abuse.130 Young women are more likely than young men to have difficulty finding safe and stable work in non-hazardous occupations.130
Longer education and reduced exposure to occupational health hazards have positive health effects, but new risks are emerging related to unemployment. Transitioning from education into the workforce has become more diffi cult in many countries.73 Transitions are now slower with a poorer selection of jobs. Many young adults are in unstable, informal employment, or unable to get jobs.131 Global youth unemployment is estimated at 12·5%, with youth almost three times more likely than adults to be unemployed.131 Those who leave school to be unemployed or inactive (not in employment, education, or training [NEET]) make up around 13% of the youth population across the OECD but up to 30% in rapidly developing countries of low and middle income such as South Africa and India, and close to 50% in some OECD countries such as Spain and Greece.132 Those who are NEET at the end of schooling are more likely to have lower earnings, greater unemployment, and employment instability through adult life.133 Poor health and diffi cult transitions into the workplace go hand in hand; those who are NEET have high rates of mental health problems, suicide risk, and substance abuse.134,135
Peers, media, youth culture, and marketing
The emergence of strong peer relationships is a central feature of early adolescence, with significant implications for health and wellbeing.55 Modern adolescence differs markedly from a pre-industrial context in both the number and diversity of peers.136 Later marriage and parenthood and prolongation of education have acted to expand the role of peers within the lives of adolescents. Social media is further expanding the role of peers and youth cultures in the lives of adolescents across all countries.137
Peers can have strong positive or negative influences on adolescent health.138 Peer connection, peer modelling, and awareness of peer norms can be protective against violence, substance use, and sexual risks.139 Peers can also increase risks, with peer participation in risk behaviours likely to increase smoking initiation and persistence, alcohol initiation and use, sexual risks, and violence.140,141 Other peer characteristics, such as sexual partner communication and negotiation skills, influence sexual and HIV risks.139,142
Social media use further extends the influence of peers on health.143 Online spaces have changed adolescent developmental tasks such as relationship and identity building which were previously mainly negotiated in face-to-face communications with peers.136 For many adolescents, identity formation incorporates local influences with new elements derived from global culture, particularly youth cultures.144 There is continued debate over whether exposure to digital media, including a greatly expanded social network, might adversely affect adolescent social, emotional, and cognitive develop ment.145 To date, the development of the new media has been so rapid that research efforts to understand their effects have failed to keep pace with their growing influence.
There is, however, little doubt that rapid changes in the media environment have changed patterns of marketing to adolescents and young adults. Again, the speed of change has been such that research on the consequences has lagged far behind marketing practices. To assess current knowledge of the effects of marketing on adolescent health, we conducted a review of reviews of research around the effects of media on sexual and reproductive health, substance use, and obesity, using diverse strategies (table 2). Although most research is on traditional media, we included reviews on digital media where available (appendix text box 2).
Table 2.
Strength of evidence for effects of media and marketing on adolescent health risks
| Tobacco use | Alcohol use | Obesity | Sexual risks | |
|---|---|---|---|---|
|
Distal exposures
| ||||
| Point of sale advertising (POS) | Strong | Moderate | Strong (food choice) | NA |
| Imagery in films/movies | Strong | Strong | Moderate (amount of food) | NA |
| Imagery in television | Moderate | Moderate | Strong (food choice/amount) Strong (food purchase request) |
Moderate |
| Music videos/MTV | No studies | Moderate | No studies | Low |
| Cartoon media characters | No studies | No studies | Moderate (food choice & purchase request) | No studies |
| Magazines | Moderate | Moderate | No studies | No studies |
| Outdoor advertising | NA | Moderate | No studies | No studies |
| Imagery on Internet | Low | NA | No studies | Low |
| Online social networking sites | Low | NA | No studies | NA |
| Concessional stands at events | No studies | Moderate | No studies | No studies |
| Radio advertising | No studies | Low | No studies | No studies |
| Composite (multiple media) | No studies | Moderate | No studies | No studies |
| Advertising (media unspecified) | Moderate | No studies | Strong (food choice/amount) | No studies |
|
Intermediate exposures | ||||
| Ownership of promotional items | Strong | Moderate | No studies | No studies |
| Approval of advertising | Moderate | No studies | No studies | No studies |
| Receptivity to marketing | Moderate | No studies | No studies | No studies |
| Media use | No studies | NA | Strong | No studies |
| Favourite star smoking | Moderate | No studies | No studies | No studies |
| Favourite ad/brand recall | Moderate | No studies | No studies | No studies |
| Attending a promotional event | Low | No studies | No studies | No studies |
Strong=strong evidence level based on consistency, temporality, dose-response in cohort studies or experimental study/meta-analysis. Moderate=moderate evidence level based on consistency and temporality from cohort studies. Low=low evidence level based on cross-sectional surveys. NA=limited/insufficient evidence.
The evidence of the influence of marketing through traditional media on adolescent tobacco use is compelling. Point of sale advertising and smoking imagery in films had the clearest evidence. There is moderate evidence around the importance of smoking imagery in other settings including television and magazines, particularly among girls. A range of factors linked to marketing and media use were also predictors of tobacco initiation with the strongest evidence for ownership of a promotional item.
There was moderately strong evidence for marketing affecting alcohol initiation, consumption, maintenance, and heavy drinking. Depiction of drinking in movies, television, music and rap videos, advertisements in magazines, point of sale displays, and advertising on radio and concessional stands at promotional events all had effects. In general, the effects of multiple media exposures on alcohol consumption were greater than for specific individual media.
Links between marketing and adolescent obesity are less well defined, in part due to the greater time lag between exposure and outcome. Yet links between marketing and intermediate outcomes that are strongly predictive of later obesity are clear. Food imagery in television, imagery in films, and point of sale advertising had moderate evidence for outcomes including food choice and amount. Overall media use (TV, computer, and video games) showed the strongest evidence of association with overweight and obesity although a major mediator is likely to be sedentary behaviour and diminished physical activity.
There have been fewer studies of media effects on sexual health risks. Moderate evidence indicates an association between frequent viewing of sexual content on TV with early sexual intercourse and increasing levels of non-coital sexual activity. There is weaker evidence around associations between exposure to pornography and early sexual debut, higher number of lifetime partners and higher-risk sexual activity such as engaging in unprotected anal intercourse.
Most studies on the effects of marketing have been in high-income countries where there is solid evidence of their effects on adolescent health risks. Few studies have extended either to countries of low and middle income or to new media. Yet industries which have until recently largely used traditional marketing media are now using digital media to promote unsolicited content and advertise their products. This marketing extends beyond national borders and is more tailored to individuals. Given that marketing is likely to become even more powerful and increasingly cross national borders, policy responses at both national and global levels are necessary. The WHO Framework Convention on Tobacco Control, now ratified by 180 countries, provides perhaps the best indication of what might be needed. Even strategies such as these can be ineffective in the face of international trade pacts that protect the interests of global corporations ahead of a country’s capacity to implement regulatory controls.146 There is need to both extend current global health frameworks to other unhealthy commodities and access to essential health goods and ensure that these are included in international trade and investment agreements.147
Legal frameworks
Laws affect adolescents and their future health by governing both access to resources for health and protection from hazards. Some specifically address health (eg, access to health care including effective contraception); others address health risks (eg, consumption of alcohol, access to tobacco); and others address social determinants of health (eg, age of marriage, protection from hazardous work). These laws reflect ever-evolving, complex, and often contradictory perspectives on young people that have been informed by historical, social, economic, religious, and other cultural forces. Inadequate and inconsistent legal frameworks can powerfully affect the health, rights, and potential of adolescents and young adults.
Complex articulation of legal principles of adolescent capacity
Courts have long recognised varying levels of adolescent capacity in decision making and the need to protect adolescents by taking age into account. However, it was not until the 20th century that more consistent adolescent legal frameworks emerged at the international level. The 1989 United Nations Convention on the Rights of the Child (UNCRC) recognised children as bearers of human rights rather than parental property, with liberties and responsibilities appropriate to their age.5 It states that when adolescent freedoms and liberties are restricted, such imposition should be consistent with human rights principles and the concept of evolving capacities. As adolescents acquire greater competency and maturity, there is a lesser need for adult guidance and an increased capacity for autonomy in decision making.
Almost all countries have signed and ratified the UNCRC, with the USA and Somalia notable exceptions. Despite this, there remains great diversity in adolescent legal frameworks. We selected six countries with varying wealth, geographic locations, cultures, and religions to illustrate the differences in legal frameworks and their implementation (table 3, appendix table 1). Variation in the ages at which these protections or acquisition of rights apply are slowly becoming more uniform. Rights might be applied differently according to sex or sexuality. For example, where homosexuality is legal, there might be a higher age of consent for sex between same-sex partners.148 Irrespective of some changes in response to the UNCRC, major differences persist across and within countries that profoundly affect the health, rights, and life chances of adolescents.
Table 3.
Comparison by age (years) of adolescent legal frameworks across six countries
| India | Lebanon | Nigeria | Peru | Sweden | USA | |
|---|---|---|---|---|---|---|
| Age of majority* | 15–18 | 18 | 21 | 18 | 18 | 18–21 |
| Customary or religious law exception | Yes | Yes | Yes | None | None | None |
| Other exceptions | Marriage | Marriage | Marriage | Marriage | State varience | |
|
| ||||||
| Minimum working age | None | 13 | None | 14 | 13–18 | 14 |
| Customary or religious law exception | None | None | None | None | None | None |
| Other exceptions | Nature of work | Work nature | ||||
|
| ||||||
| Minimum drinking age | 18 or Illegal | 16 or Illegal | 18 or Illegal | 18 | None–20 | 21 |
| Customary or religious law exception | Yes | Yes | Yes | None | None | None |
| Other exceptions | State varience | Alcohol strength | ||||
|
| ||||||
| Minimum smoking age | 18 | None | None | 18 | 18 | None–20 |
| Customary or religious law exception | None | None | None | None | None | None |
| Other exceptions | State variance | |||||
|
| ||||||
| Age of criminal responsibility† | 7 | 7 | None | 12–18 | 15 | 6–14 |
| Customary or religious law exception | None | None | Yes | None | None | None |
| Other exceptions | State variance | |||||
|
| ||||||
| Minimum age of marriage | Puberty–21 | 9–18 | 9–18 | 16 | 18 | 16–21 |
| Customary or religious law exception | Yes | Yes | Yes | None | None | None |
| Other exceptions | Gender | Gender | Gender | Special reason | None State variance | |
|
| ||||||
| Heterosexual age of sexual consent | None–18 | None–15 | Puberty–18 | 14 | 15 | 16–18 |
| Customary or religious law exception | Yes | Yes | Yes | None | None | |
| Other exceptions | Marriage, gender | Maturity | State variance | State variance, gender | ||
|
| ||||||
| Same-sex age of sexual consent | No information | No information | No information | 14 | 15 | 16–18 |
| Customary or religious law exception | None | None | None | None | None | None |
| Other exceptions | Legally restricted | Legally restricted | Legally restricted | State variance | ||
|
| ||||||
| Age of consent to medical treatment | 12 or 18 | 18 | 16 | 18 | 18 | 12–18 |
| Customary or religious law exception | None | None | None | None | None | None |
| Other exceptions | Maturity | State variance | ||||
|
| ||||||
| Age to access contraceptives‡ | None | 18 | Unknown | None | None | Varies |
| Customary or religious law exception | Yes | Yes | Yes | None | None | None |
| Other exception | Provider discretion | Marriage | State variance | |||
|
| ||||||
| Age to access abortion§ | 18 | Illegal | Illegal | Illegal | None | 18 |
| Customary or religious law exception | Yes | Yes | Yes | None | None | None |
| Other exception | Marriage | Mother’s life | Mother’s life | Mother’s health¶ | State variance | |
|
| ||||||
| Age of consent to HIV test‖ | None | Unknown | 18 | 18 | None | 12 |
| Customary or religious law exception | None | None | None | None | None | None |
| Other exception | State variance | |||||
Range of ages reflects variation within a country, such as by state.
Age of majority: the age at which a person, formerly a minor or infant, is recognized by law to be an adult.
Age of criminal responsibility: the age at which an individual can be seen as capable of committing a criminal offence and stand trial and be convicted.
Age to access contraceptives: the age at which adolescents or minors can access contraceptives without parental consent.
Age to access abortion: the age at which adolescents or minors can consent to an abortion without parental consent.
Age of consent to an HIV test: the age at which adolescents or minors can consent to an HIV test without parental consent.
Avoid grave and permanent harm to the woman.
Prevailing legal frameworks fail adolescents both in their framing and implementation. They reflect neither the principles of the UNCRC, nor a thoughtful assessment of adolescents’ actual and differing capacities. Rather, they mirror historical, economic, social, cultural, and sometimes religious priorities of the State, as well as traditional assumptions about what is necessary to protect adolescents.149 In some areas where legislation has a proven role in protecting health (eg, minimum age to smoke tobacco, working age), laws often do not exist. In others, such as legal frameworks around sexual and reproductive health, there is little consistency between countries in the age of marriage, access to contraception, and availability of safe abortion. Indeed, there is often variability within the one country.
Countries with plural or multiple legal systems allow various sources of law to govern, including English common law, French civil or other law, statutory law, customary law, and religious law or practice.150 Although international conventions have contributed to national consensus on norms and statutory laws, other laws often dominate practice. Customary and religious laws enjoy binding status in law or practice in most countries in the African region and a number in Asia and the Americas.151 These laws permit the persistence of cultural and religious customs and practices, some of which are discriminatory and have profound health effects.
Child marriage violates many internationally recognised rights. The Convention on the Elimination of All Forms of Discrimination against Women requires States to ensure that men and women have equal rights to enter into marriage and to freely choose a spouse with their free and full consent. Free and full consent is defined as a capacity to understand the meaning and responsibility of marriage, to have access to full information about her future spouse, knowledge about the institution of marriage, and her right to exercise a choice about whether to marry, who to marry, and when to marry.152 Consent to marriage cannot be free and full when one of the parties involved is insuffi ciently mature and experienced to make an informed decision about a life partner.153 Yet 15 million girls around the world marry each year before 18 years.154 In developing countries, a third of girls are married before 18 years, and one in nine before 15 years.155
Girls who marry young face diminished opportunities for education, greater sexual exploitation, and violence that can sometimes extend to enslavement. Child brides are also exposed to health risks from early pregnancy, have greater maternal and infant mortality, and heightened vulnerability to HIV/AIDS and other sexually transmitted diseases.156 34 countries permit girls to marry before 18 years, some still permit marriage before 15 years, and a few specify no minimum age.157 An even more important barrier to progress around child marriage lies in the discrepancy between legislation and actual marriage practices, largely the result of legal pluralism. At least 40 countries allow customary or religious law to over-ride specific age of marriage legislation. Even in countries which have ratified international rights treaties applicable to age of marriage, loopholes exist for laws and practices in personal, family, religious, or private matters. In many places an absence of marriage registration is a further barrier that limits monitoring of implementation of international treaties. The barriers to implementation are further illustrated in the case examples in panel 4154,158–168 and appendix text box 3.
Panel 4. Country case study on legal frameworks for child marriage.
Child marriage is common in India, declining very slowly. 47% of women are married before 18 years. The highest prevalence is in five states: Madhya Pradesh (73%), Andhra Pradesh (71%), Rajasthan (68%), Bihar (67%), and Uttar Pradesh (64%). The urban–rural differential is substantial, with rural girls marrying younger than 18 years at nearly twice the rate of urban girls. Girls marrying before 18 years report physical violence twice as often and sexual violence three times as often as those marrying later. The Prohibition of Child Marriage Act set the legal age of marriage at 18 years for girls and 21 years for boys. The Compulsory Registration of Marriages Act requires registration of all marriages across India. Close examination of the law reveals many customary and religious loopholes. Each religious community has separate personal status laws which over-ride national legislation in matters relating to the family, including marriage. 80% of the Indian population, including Hindus, Sikhs, Buddhists, and Jains, are governed by the Hindu Marriage Act, which validates marriages, once solemnised, even for parties under 18 years. Under Muslim personal law, marriage can occur at the age of puberty. The Prohibition of Child Marriage Act does not prevent or criminalise these marriages, it only makes them voidable at the option of a contracting party. In addition, there is an explicit exception for Muslim marriage where the voidable provision only applies when a girl is under 15 years at the time of marriage. The Compulsory Registration of Marriages Act “does not affect any right recognised or acquired by any party to the marriage under law, custom or usage”, meaning religious marriages are also exempt from registration. The Government of India has also filed a reservation to Article 16(2) of the Convention on the Elimination of All Forms of Discrimination against Women, which mandates compulsory registration of marriages stating, “...the Republic of India declares that though in principle it fully supports the principle of compulsory registration of marriages, it is not practical in a vast country like India with its variety of customs, religions, and level of literacy”.
Developmentally informed legal frameworks
More rational legal frameworks governing adolescents would take greater account of evolving adolescent cognitive and emotional capacities. Developmental neuroscience is beginning to offer new insights into adolescents’ capacities. With access to knowledge, they demonstrate similar or even greater cognitive capacity than adults to make good judgments in calm and emotionally-neutral contexts.60 Yet in emotionally-charged situations of stress or excitement, particularly with peers, emotions are more likely to drive decision making.60,169 Adolescents are also often more influenced by short-term than longer-term outcomes.28
Capacity for consent (or competence) has a basis in evolving cognitive and emotional capacities, as well as knowledge and experience.170 Legal frameworks should take both factors into account in framing legislation on age of consent. Restricting an adolescent’s right to smoke is therefore justified from their greater vulnerability to poor decision making in emotionally-charged contexts with peers, as well as from their still evolving capacity to understand the extent of future health consequences of smoking.
Yet in addition to protecting adolescents from harm, legal frameworks should also support and promote adolescent autonomy. Developmental neuroscience provides some principles for how legal and social policy frameworks could operate more effectively for adolescents. Given knowledge, and with appropriate safeguards, adolescents are competent to make effective decisions about almost all important matters in their lives, including their health. Legal and policy frameworks should reflect these evolving cognitive and emotional abilities with age-appropriate autonomy, freedoms, and rights. Most adolescents are capable of voting from 16 years and doing so both empowers adolescents and promotes civic engagement. Yet, adolescents need legal and policy safeguards and support for decisions made in contexts where heightened emotion affects the choices an adolescent might make. This includes many decisions around substance use and sexual behaviours. Permitting access to effective contraception (eg, long-acting reversible contraceptives) for those sexually active under 18 years is one example of how the law can protect adolescents’ health. Lastly, the capacity for adolescent learning should be exploited through graduated legal and policy frameworks. This includes supporting skills and decision making around driving (panel 5),171–174 and preventing custodial sentences for young offenders (panel 6).5,175–179
Panel 5. Graduated driving licences balance protection and autonomy.
Australia, New Zealand, and many US states have introduced graduated driving licences. Restrictions on adolescent drivers and those without requisite levels of driving experience are intended to address the disproportionately high numbers of teenage automobile accidents, injuries, and fatalities. In California, for example, a three-step process to obtaining a full driving licence recognises the increased risk associated with peer influence and alcohol consumption during this period. The first stage requires all teenage drivers to complete 50 h of driving while supervised by an adult over the age of 25 years, including 6 h of a driver training course. Completion of this stage must be certified in writing by the young person’s parent or guardian. In the subsequent second stage, which lasts 12 months, those under 18 years old are prohibited from driving passengers under 20 years old or between 2300 h and 0500 h, unless accompanied by a licensed driver aged 25 years or older. This reflects concerns about peer influences while driving. A full driving licence is only awarded as a third stage of graduation if the driver completes the second stage without any court-ordered driving restrictions, suspensions, or probations on their record. In parallel, up until the age of 21 years, a zero tolerance law prohibits any alcohol consumption prior to driving. An evaluation across 43 US states suggests an 18–21% reduction in the involvement of 16 year olds in crashes in those states with the most extensive graduated driving licence programmes. The greatest reductions were seen in 16 year olds, where a strict permit stage was associated with a 58% reduction in fatal crash risks with similar reductions for injury-associated crashes. The success of graduated approaches for driving suggests consideration should now be given to applying graduated approaches to other aspects of adolescent policy, such as alcohol and other licit substance use, particularly where similar public health concerns are apparent.
Panel 6. Second chances for young offenders.
Adolescents and young adults are more often both the victims and perpetrators of criminal offences than older age groups. Offending in the young might be increasing in many places, with urbanisation a contributing factor. Many offences occur within the context of gangs, where peer influence is a major contributor. Young offenders have some of the worst health profiles of any group of adolescents and young adults. In high-income countries, deaths of young offenders are around ten times higher than in other adolescents due largely to drug overdose, suicide, accidental injury, and homicide. A separation of youth from adult justice systems began in high-income countries in the late 19th century with a rationale of acting in the best interest of the child. The UN Convention of the Rights of the Child has more recently stressed the importance of a consciousness of rights within the operation of youth justice systems. In particular, it stressed the use of detention and imprisonment as measures of last resort. Yet in many settings, political pressures have re-emerged for adolescents to be held fully accountable for their actions. In many places, custodial detention (incarceration), including pre-trial detention, is still used with first-time adolescent and young adult offenders, even for minor offences such as cannabis or other substance use, shop-lifting or minor theft—even though most first-time offenders do not reoffend.
Alternative approaches that provide second chances, promote emotional learning, and ultimately better life (including health) outcomes have been implemented in a range of jurisdictions. Diversion programmes have been designed both to keep adolescents out of the criminal justice system and, when tied with family interventions, to reduce recidivism. Restorative justice approaches address the needs of both victims and offenders, and bring offenders, victims, families, and sometimes other community members together. They too reduce rates of recidivism. Other approaches to protect young offenders include the use of welfare-oriented hearings for younger offenders, ensuring that convictions before 18 years can later lapse from an individual’s criminal record, and extending youth justice approaches to the age of 21 years for those considered emotionally immature.
The global health profile of adolescents and young adults
The epidemiological transition has changed health profiles across all age groups. Adolescents and young adults have also benefited from the control of infectious diseases, including diarrhoeal disease, lower respiratory tract infections, tuberculosis, and malaria. Adolescent girls and young women have benefited from gains in maternal health, though there is ongoing debate as to whether gains have been as great in this younger age group.180 However, the epidemiological transition often brings an increase in other health problems of adolescents, including road traffi c injuries and suicide.181,182 In some contexts, such as Latin America and eastern Europe, these problems have extended to homicide, mostly in young men.182 Although young men are the main perpetrators and victims of homicide in these settings, young women’s lives are profoundly restricted by both violence and fear of violence.183 The link with economic conditions is evident in the rise of mortality and alcohol-related disease burden in eastern European countries following the fall of the Soviet Union in 1991.184 A high proportion of young men competing for limited economic opportunities is also likely to be a factor underlying the recent civil unrest and armed conflict across the Middle East, north Africa, and sub-Saharan Africa.185
Other adolescent health problems become more prominent during the epidemiological transition. Mental health problems, including self-harm and suicide, assume greater significance. In part this is likely to reflect their greater prominence after reductions in infectious, nutritional, and sexual and reproductive health problems. It might also, in part, reflect a true increase in the prevalence of adolescent mental health problems that has been described in recent decades in developed economies.186 Mental disorders typically have their onset in late childhood and adolescence. Because many persist into adulthood, adolescent mental disorders make a greater contribution to adult disease than ever before.44
HIV is a further reason why adolescents and young adults, particularly in southern and eastern sub-Saharan Africa, have seen fewer benefits from the epidemiological transition. New HIV infections are largely concentrated in young adults, and adolescents and young adults have not experienced equivalent mortality declines recently seen in other age groups.187
With ageing populations and a convergence to a disease burden dominated by NCDs in later life, adolescent health risks assume greater significance.188 NCD risks that usually emerge during adolescence include tobacco use, physical inactivity, obesity, alcohol and illicit substance use, and poor diet. Without specific policy interventions, the combination of increasing wealth and unrestrained marketing will see adolescent health risks continue to rise in prevalence.
Defining adolescent health needs across the epidemiological transition
We adapted the conceptual model of the 2012 Lancet Series on adolescent health18 to define health needs at three levels (figure 6): current health problems and causes of adolescent and young adult deaths; health risks for health problems in adolescence, adulthood, or the next generation; and important proximal social determinants of health during the adolescent and young adult years.18 These include education and employment, marriage and parenthood, marketing and digital media, and quality of universal health coverage. The three categories of diseases outlined in figure 7 reflect conditions that change in prominence with the epidemiological transition. Thus diseases of poverty are conditions that are prominent prior to a country passing through the epidemiological transition and include undernutrition, major sexual and reproductive health problems (eg, maternal deaths, high rates of sexually transmitted infections), and infectious diseases including HIV. Panel 7, appendix text boxes 4 and 5, and appendix table 3 further describe both the categorisation of disease burden and the methods used to derive these three categories of countries.
Figure 6.
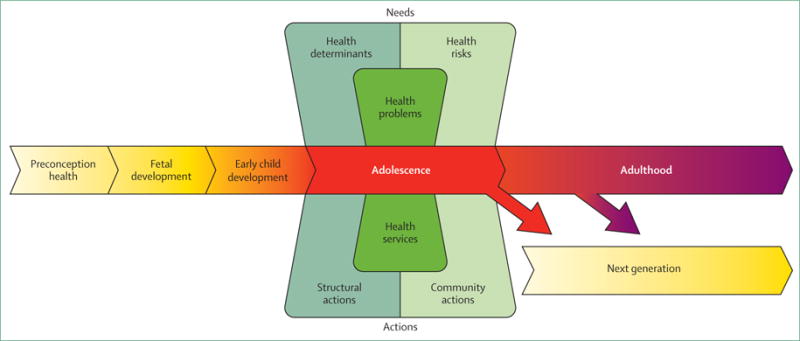
Conceptual framework for defining health needs and actions in adolescents and young adults
Figure 7. Country categorisation based on adolescent burden of disease.
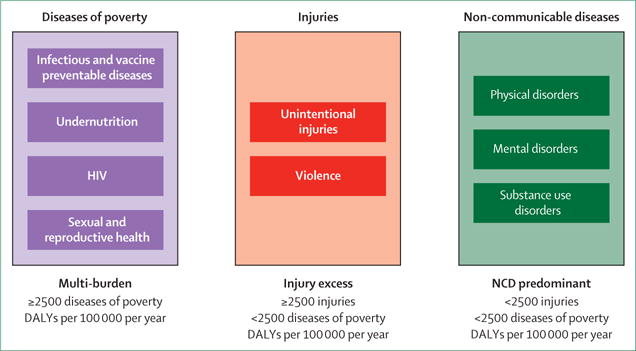
Categorisation of countries into three groups according to adolescent burden of disease and reflecting passage through epidemiological transition. DALYs=disability-adjusted life-years. NCD=non-communicable diseases.
Panel 7. Categorisation of country health profiles for adolescents.
We aggregated the 236 causes of disability-adjusted life-years (DALYs) and deaths among 10–24 year olds from the 2013 Global Burden of Disease study into nine categories reflecting changing disease burden with progression through the epidemiological transition. This resulted in three broad categories of health problems as summarised in figure 7. Countries were then classified into one of three categories depending on their pattern of disease burden, using the definitions below, and shown in figure 8:
Multi-burden countries were those with little evidence of having yet passed through an epidemiological transition. DALYs due to infectious diseases, nutritional deficiency and sexual and reproductive health, together with HIV, were grouped. Countries with a total DALY rate within this group of conditions of 2500 per 100 000 per year or more were defined as higher burden multiple problem.
Injury excess countries were those where the burden of disease showed evidence of having passed through the first phase of the epidemiological transition but where rates of preventable injury remained high. We combined the DALY rates for unintentional injuries and violence and defined a group of countries with an injury burden of 2500 per 100 000 per year or more and DALY rates for infectious diseases, nutritional deficiencies, and sexual and reproductive health and HIV less than 2500 per 100 000 per year.
NCD predominant countries were defined as those with DALY rates of less than 2500 per 100 000 for both groups, namely infectious diseases, nutritional deficiencies, sexual and reproductive health and HIV, as well as for unintentional injuries and violence.
Further details are provided in supplementary text box 4 in the online appendix.
68 countries are classified as multi-burden countries (figure 8). Many are in southern and eastern sub-Saharan Africa where HIV has been a growing contributor to disease burden in adolescents and young adults. Some are also in southeast Asia and Oceania. 51% of the world’s adolescents live in these countries, but they account for 62·5% of all disability-adjusted life-years (DALYs). These countries have made some progress in the past 15 years in reducing infectious diseases other than HIV and sexual and reproductive health and nutritional deficiencies. (figure 9). Reductions in unintentional injuries have been less than for diseases of poverty, especially in men and boys.
Figure 8. Country categorisation based on patterns of DALYs in 10–24 year olds.
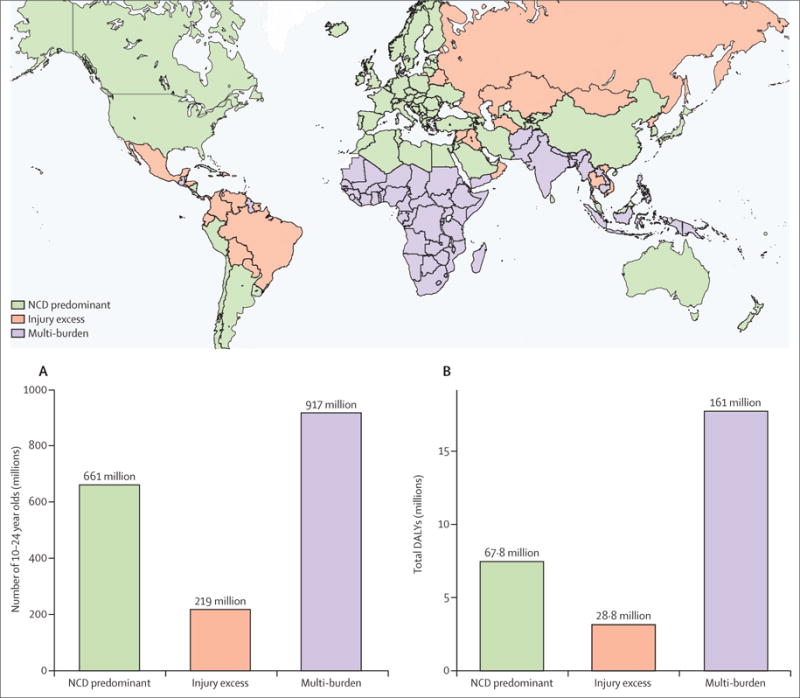
(A) Population of 10–24 year olds across country categories. (B) Total DALYs across country groups. DALY=disability-adjusted life-years. NCD=non-communicable diseases. Data from Global Health Data Exchange.69
Figure 9. Changes in disease burden in 10–24 year olds between 1990 and 2013.
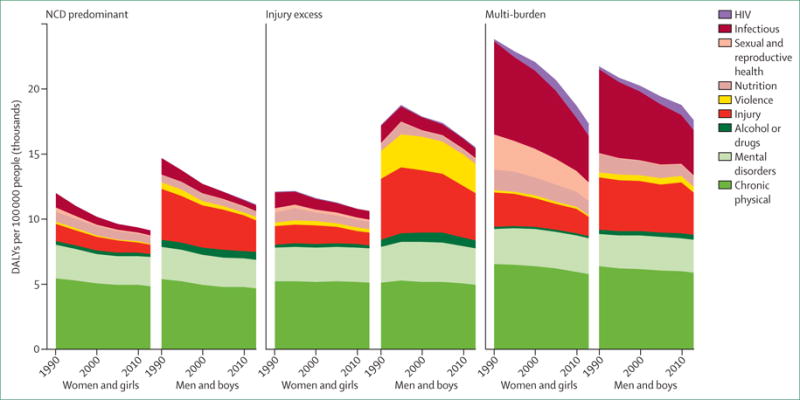
Disease burden changes across the three country categories; NCD predominant, injury excess, and multi-burden. DALY=disability-adjusted life-years. SRH=sexual and reproductive health. NCD=non-communicable diseases. Data from Global Health Data Exchange.69
28 countries are in the injury excess category. They make up 12% of the global population and 11% of DALYs. 22 of these 28 countries have made little progress since 2000 in reducing the burden of disease affecting adolescents and young adults. These include Syria and Iraq, countries that have been affected by conflict. The remaining countries are to a large extent in Latin America and central Asia. Six countries, including Russia, Thailand, Colombia, and Bolivia, have made good progress in reducing DALYs from unintentional injuries and to a lesser extent violence.
92 countries fall into the category of NCD predominant countries. 37% of the world’s adolescents live in these countries, where they account for a little over a quarter of all DALYs (26·3%). These countries include North America, most of western Europe, Latin America, and Australasia. 74 countries have been relatively static in their adolescent disease burden since 2000. 18 countries, including China and a number of countries in eastern Europe and the Middle East, stood out as having made substantial reductions in the adolescent disease burden since 2000. In general, this group has made some progress in reducing unintentional injuries. By contrast, they have made little progress in reducing the disease burden from chronic physical disorders, mental disorders, and substance use disorders. As a result the proportion of disease burden due to these conditions has continued to rise.
Eight countries have had an increase in their total DALY rate since 2000. Two are conflict affected (Georgia and Syria), three are violence-affected Latin American countries (Mexico, Venezuela, and Paraguay), and two have been particularly affected by HIV (Lesotho and Swaziland). Overall, since 2000 the most consistent gains have been in reducing infectious diseases, sexual and reproductive health problems, and nutritional deficiencies in multi-burden countries. Unintentional injuries have reduced across all three country groups. By contrast, progress in reducing violence has been limited. HIV contributes a greater proportion of disease burden in adolescents in 2013 than it did 13 years earlier. Alcohol and other drug problems have also increased over that time, with increases most pronounced in NCD predominant countries.
Figure 10 illustrates the changing burden of disease from early adolescence to young adulthood in male and female adolescents. Particularly striking changes occur in rates of injury with age in boys, in both injury excess countries and multi-burden countries. In girls, the most striking changes with age in multi-burden countries are the increasing burden of sexual and reproductive health problems and injuries. In all country groups, there is a large increase in disease burden from chronic physical disorders, substance use disorders, and mental disorders with increasing age across adolescence.
Figure 10. Patterns of disease burden by age and sex across 10–24 year olds.
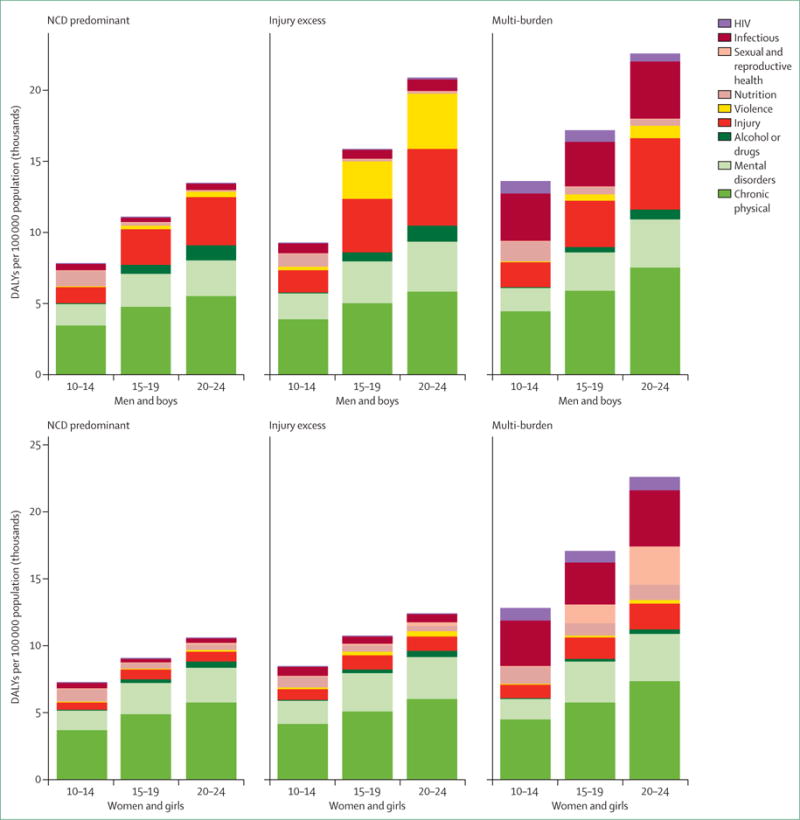
Patterns of disease burden in different age groups across the three country categories; NCD predominant, injury excess, and multi-burden. DALY=disability-adjusted life-years. SRH=sexual and reproductive health. NCD=non-communicable diseases. Data from Global Health Data Exchange.69
Figure 11 uses the example of China to illustrate the variation in disease burden within a country. Both total disease burden and its contributors vary substantially by province. Although China as a whole is classified as NCD predominant, four provinces (Tibet, Xinjiang, Qinghia, and Hebei) would fall into the injury excess classification due to unintentional injuries remaining at a high level.
Figure 11. Summary profile of disease burden in 10–24 year olds across Chinese provinces.
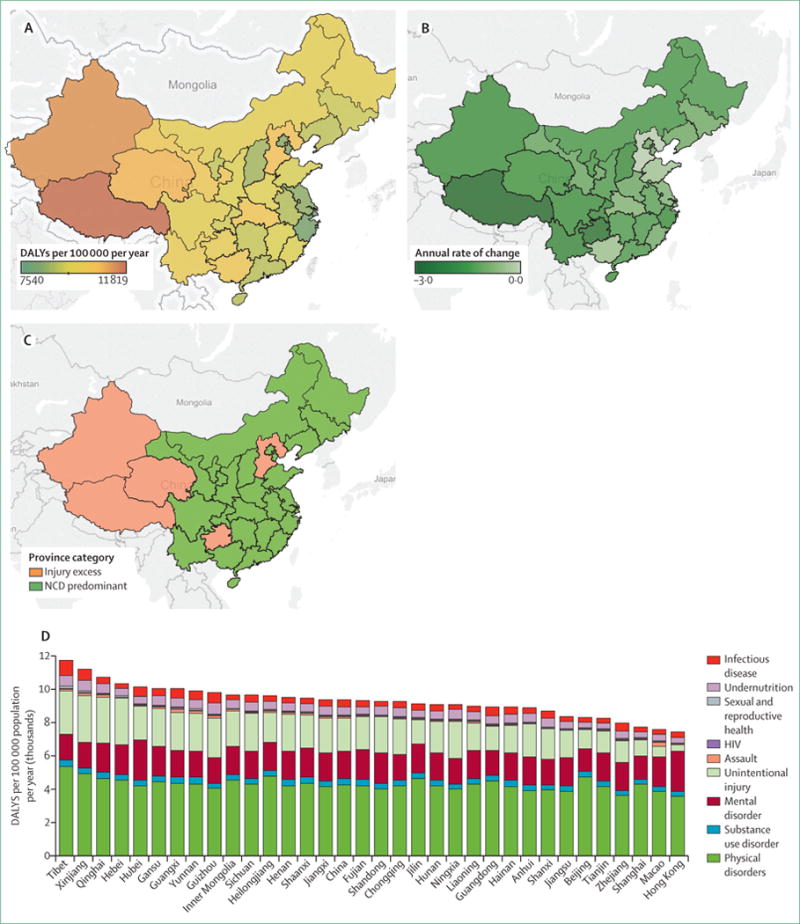
(A) DALYs per 100 000 19–24 year olds in 2013. (B) Annual percentage rate of change in total DALYs 2000–13. (C) Categorisation of Chinese provinces by major contributors to disease burden. (D) Contributors to disease burden in 10–24 year olds across Chinese provinces. DALY=disability-adjusted life-years. NCD=noncommunicable diseases.
Major adolescent health risks
Tobacco use is a major risk factor for NCDs later in life, which overwhelmingly has its onset in adolescence. Maternal smoking during pregnancy is also a well-established risk factor for poor fetal growth as well as later-life illness in offspring.189 Tobacco use has declined across all three country groups, but progress has been mixed (appendix). Rates of daily smoking remain above 15% in 10–24 year olds across most European countries. In Russia, one in four 10–24 year olds smoke daily. Across all groups of countries, daily smoking is more common in men and boys than in women and girls. A number of countries in sub-Saharan Africa, eastern Europe, and the Middle East have seen rises. Many non-signatories to the Framework Convention on Tobacco Control have not seen any fall in adolescent and young adult tobacco use.
Alcohol use disorders typically begin during the young adult years. As with nicotine addiction, younger age of drinking is a particular risk factor.190,191 Alcohol consumption in adulthood is now linked to eight different cancers, hypertension, haemorrhagic stroke and atrial fibrillation, various forms of liver disease, and pancreatitis.166 Greater use of alcohol in pregnancy has prominent intergenerational harms in the form of fetal alcohol syndrome.192 Binge drinking was considerably more prevalent in men and boys than women and girls in every country grouping (appendix figure 8). Binge drinking rates were highest in NCD predominant and injury excess countries where around a quarter of 15 to 24-year-old men and boys report at least one occasion in the past 12 months. There has been little progress in reducing adolescent and young adult binge drinking since 1990. Indeed, a trend for increasing binge drinking is now clear for both boys and girls in injury excess and multi-burden countries; injury excess countries are likely to overtake the NCD predominant countries in binge drinking in the coming years.
Overweight and obesity increase markedly across adolescence and young adulthood with very high persistence, particularly for obesity.193 The risks in later life include premature mortality, chronic disability, type 2 diabetes, ischaemic heart disease, hypertension, and cerebrovascular disease.194 Preconception maternal obesity increases risks for miscarriage, gestational diabetes, operative delivery, pre-eclampsia, infant perinatal mortality, and macrosomia.195 Adolescent overweight and obesity have increased in prevalence in almost all countries since 1990, as shown in figure 12. Notable exceptions are Iran, Turkey, Bulgaria, Argentina, and a number of countries in central sub-Saharan Africa. The annual increase has been around 10% in China and Vietnam, but there have also been marked increases in other countries across southeast Asia as well as in sub-Saharan Africa. The prevalence of overweight and obesity is around one in five young people in NCD predominant and injury excess countries. Although lower, about one in ten young people in multi-burden countries are also overweight or obese. If the recent increase in obesity continues, injury excess countries will soon outstrip NCD predominant countries in rates of overweight and obesity.
Figure 12. Overweight and obesity in 10–24 year olds between 1990 and 2013.

(A) Prevalence in 2013. (B) Annual percentage change from 1990 to 2013. NCD=non-communicable diseases. Data from Global Health Data Exchange.69
Across sub-Saharan African and Latin American countries with available data, 10–20% of 15 to 24 year olds report having first sexual intercourse before the age of 15 years (appendix figure 9). Condom use in the context of having had two or more partners in the past year shows great variability between countries, but remains under 50% for adolescents in multi-burden countries. Rates of women giving birth before 18 years remain high across western, central, and eastern sub-Saharan Africa, and for a number of countries in south Asia. Overall around one in five women in multi-burden countries report giving birth by the age of 18 years. Unmet need for contraception refers to young women aged 15–24 years currently married or in union and not wanting to become pregnant within the next 2 years, who report not using any method of contraception. Rates of unmet need were high across sub-Saharan Africa, though there was substantial variation between countries. Although fewer data are available in other regions, high rates of unmet need for contraception remain in countries in Oceania, Latin America, and south Asia. Where data exist, the profile of sexual and reproductive health risks is generally poorer in multi-burden countries. One exception is the high rate of intimate partner violence for young women in injury excess countries (appendix figure 10).
Lower adolescent fecundity benefits young women by making it more likely that they remain in education, delay marriage, enter the workforce, and achieve economic independence. In many countries the age of onset of sexual activity has remained similar while the age of marriage and first pregnancy has risen substantially. This shift in the age of first sexual intercourse relative to the age of marriage has taken place in many countries in all regions, with enormous implications for the provision of contraception for young women.196
Figure 13 illustrates the very large variation in adolescent fecundity by country. The highest rates remain in sub-Saharan Africa but rates are also high across Latin America and in many countries in south Asia and Oceania. Globally there have been strong trends towards reduced adolescent fecundity but these are less prominent in sub-Saharan Africa and Latin America. Adolescent fecundity is high in multi-burden and injury excess country groupings. Injury excess countries have made little progress in reducing adolescent birth rates and are likely to overtake multi-burden countries in having the highest adolescent fecundity.
Figure 13. Profile of adolescent fecundity.
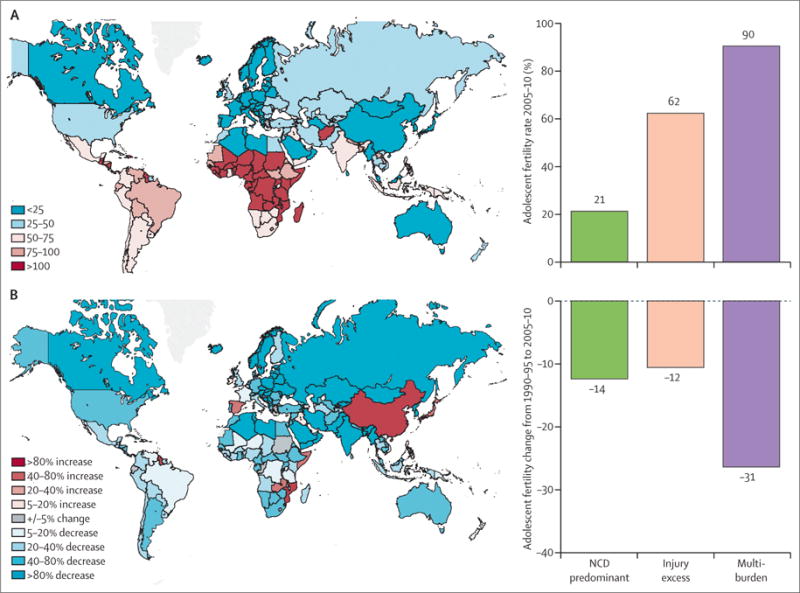
(A) Births per 1000 girls aged 15–19 years in 2010. (B) Percentage change in births per 1000 girls aged 15–19 years per year between 1990–95 and 2005–10. NCD=non-communicable diseases. Data from Global Health Data Exchange.69
Actions for health
Investments in adolescent health extend from those directed toward conspicuous health problems to health risks that emerge during these years and to the broader social determinants of health (figure 6). Yet there are challenges in responding to these health needs, whether through health services, community actions, or structural actions. Adolescents and young adults have the poorest level of universal health coverage of any age group.197 Social and environmental determinants of adolescent health lie largely outside the health service sector.55 There are shifts in these determinants as young people mature through adolescence, such that strategies suited to younger adolescents might be inappropriate or ineffective with young adults.55 Strategies that are effective and appropriate for girls might be less effective in boys. The settings for health actions mirror those of determinants and extend from health services, schools, and education settings, to families and communities, places of employment, road transport, media, and structural, legal, and policy environments.
Health services
Health services for adolescents and young adults have a number of essential roles. Firstly, adolescents have acute health-care needs. Secondly, health services need to respond to emerging health needs, including health actions around normative conditions such as the provision of contraception for sexually active adolescents and maternal care for pregnant young women, as well as early and effective responses to the many health problems that emerge in adolescence such as nutritional deficiencies, HIV and other infectious diseases (eg, STIs, tuberculosis), and mental and substance use disorders.198,199 Thirdly, health services play a central part in the management of chronic health conditions, including physical disorders and HIV/AIDS, mental disorders, and injury-related disability, all problems that can have profound implication for social, educational, and economic adjustment.
Despite having clear needs, adolescents and young adults often fail to access health care. Unmet sexual health care needs have been the best described. These needs are high in many countries and include lack of access to reliable contraception in both married and unmarried adolescent girls. In Tanzania for example, where 58% of 20–24-year-old girls were sexually active before 18 years (14% before 15 years), the unmet need for contraception is 16% in married 15–19 year olds and 64% in those who are sexually active but unmarried.200 In most African countries, the proportion of married 15–19-year-old girls with unmet contraception need is at least 25%, and as high as 64% in Ghana.200 Unmarried 15–19-year-old girls have approximately double the unmet need for contraception than married girls of the same age. Such striking figures are not restricted to Africa. In Asia, for example, the unmet need for contraception ranges from 25% in Kazakhstan, to 94% in Laos. In most countries in Latin American and the Caribbean, between a third and a half of unmarried sexually active 15–19-year-old girls have unmet needs.200
Rates of contraceptive failure are higher in adolescents than in older women, with younger women more likely to abandon contraception despite ongoing need.201 Reasons include poor understanding of pregnancy risks, concerns about the effect of contraceptives on health or fertility and opposition from partners. Lack of knowledge of services, cost, shyness, and community stigma about sexual activity, and disapproving attitudes from providers are further barriers.202 One study in the US found contraceptive failure was almost twice as high in under 21 year olds using oral contraceptive pills, transdermal patch, and the vaginal ring. By contrast the failure rate of LARCs is extremely low in all age groups.203 Yet despite increased use of LARCs in the US since 2007, 15–24 year olds are less likely to use LARCs than 25–39-year-old women.204 Given their impressive effectiveness at reducing unplanned pregnancy, LARCs should be a critical component of universal health care for sexually active adolescent girls and young women, notwithstanding higher upfront costs.
An estimated 22 million unsafe abortions occur annually worldwide, of which about 15% (about 3·2 million) are in girls under the age of 20 years. Young women experience a higher risk of abortion-related deaths than women over 25 years, are more likely to terminate pregnancy after the first trimester, and are more likely to use unregulated providers.200 One nationally representative study in Ghana identified younger women as having the highest risks for unsafe abortion. In those who obtained an abortion, 44% of those under 20 years old did so with a safe provider, compared with 57% of 20–29 year olds and 65% of women aged 30 years and older.200 Even after controlling for various sociodemographic factors, knowledge of the legal status of abortion and partner support, adolescents were 77% less likely to obtain a safe abortion compared with women aged 30 years and older.
Irrespective of increased prevalence across adolescence, evidence suggests that most adolescents and young adults with mental health problems do not receive treatment from health professionals.205 One European study of mental health care in adults showed that about 6% of the sample was in need of mental health care but 48% of those people reported no formal health-care use. Those aged 18–24 years reported least use of services.206 Actions to reduce barriers include promotion of mental health literacy and combat of stigma, particularly in countries of low and middle income where the scaling up of mental health services has not yet been a priority.207
Barriers to universal health coverage
Two sets of barriers diminish universal health coverage for adolescents and young adults. The first set are external to health services and include legal frameworks governing health actions, out-of-pocket costs, and cultural and community attitudes. Although not unique to adolescents, they assume a greater magnitude in the young. Both legal and financial barriers to health service access are greater in adolescents than in other age groups. Even when national legislation allows a particular health response, a provider’s attitudes and beliefs about the appropriateness of an action in the context of age, marital status, or partner or parental consent could affect their response to an adolescent.208 Financial barriers might arise from limited eligibility for tax and insurance based funding schemes.209 18–24 year olds report more frequent cost barriers than older adults.210 Socially marginalised adolescents are particularly vulnerable to catastrophic medical events.
The second set of barriers arise more from the developmental context of adolescence. Adolescence brings an increasing desire for privacy and confidentiality, with embarrassment, shame, and fear of being judged restricting access to health care. A particular concern is that their parents will be informed about sensitive issues, such as substance use, mental health, and sexual behaviours.211 In the USA, for example, the leading concern of adolescents who had foregone health care was that they did not want their parents to find out.212 Difficulties also arise when policies and procedures for claiming health-care benefits inadvertently expose adolescents to confidentiality breaches through routine communication, such as when itemised bills are sent to policy holders (typically parents).213
Adolescents are less experienced users of health care, with a consequence that time is required to engage them in consultations, especially around sensitive issues. Inexperience also results in a majority of adolescents not appreciating that health risks, such as substance use, bullying, or overweight, can be raised with health professionals.214 Adolescents welcome such discussions as long as they are sensitively and confidentially addressed.215
A young child’s involvement with health-care providers is typically mediated through parents or family. With age, support, and experience, the maturing adolescent develops greater capacity to engage in decision making about their own health care. A task for health professionals is to help set expectations with adolescents and parents about an adolescent taking greater responsibility for their health care. With increasing age, providers need to explicitly engage young people themselves, which ideally includes consulting with them alone for at least part of the consultation. Engaging adolescents in a friendly, respectful, and non-judgmental manner helps them to gain the confidence and skills to increasingly make decisions about their health and wellbeing.197 Consulting with young people alone can be challenging to parents’ perceptions of their role.216 It requires careful explanation, even in settings in which it is more culturally acceptable.217
In general, treatment adherence diminishes as children with chronic physical health conditions enter adolescence. This has consequences for the management and outcomes of a range of significant chronic illnesses such as type 1 diabetes, allergy and asthma, HIV, and inflammatory bowel disease.218,219 Providing information alone is ineffective in achieving greater adherence in adolescents.220 Additional strategies such as behavioural management, family engagement, and understanding the young person’s emotional responses to illness are important elements within the clinician’s response.221 Peer strategies are effective at improving health outcomes of adolescents, especially when linked to wider school and community strategies.222 There is much interest in the role of apps and other technologies in promoting adherence in adolescents with chronic physical conditions but as yet there are few studies of benefit.
Transition to adult health care poses important challenges for continuity of health care. This is now well recognised in high-income countries for adolescents with conditions such as type 1 diabetes, spina bifida, and cystic fibrosis.223 Engagement with adult services requires repeated discussion with young people and families, detailed planning and care coordination with adult services, and enhanced follow-up by adult services to maximise continuity of care.224 More recently, the extent that young people with HIV/AIDS are dropping out of adult health care in countries of low and middle income after transferring from specialist paediatric services has become apparent, leading to failure of adherence to antiretroviral therapy, and greater risks to self and others.225 Health-system deficiencies commonly include inadequate pre-transfer communication and planning from child health services, and adult services that do not meet young people’s needs—or both.224 Such experiences are consistent with the less positive experiences of 18–24 year olds than older adult users of health services in high-income countries,210 which reinforces recent efforts to bring greater attention to the health experiences and outcomes of young adults as well as younger adolescents.226
Adolescent-responsive health care
What adolescents view as responsive or youth-friendly health care is similar across countries of all income levels.227 They value patient-centred care with an emphasis on respect, coordination of care, appropriate provision of information, high-quality communication, involvement in decisions about care, and the ability of health-care providers to listen to their needs.228 These align with the principles of adolescent-friendly health care, a framework developed by WHO, that emphasises equity of access, effectiveness, accessibility, acceptability to young people, and appropriateness of care offered.229 These are applicable across all health services (eg, clinic, school health service, hospital).
As clinicians generally find consulting with adolescents more challenging than with other age groups, extending the competence of health-care providers to ensure they have the attitudes, knowledge, and skills to appropriately engage with and respond to adolescents’ health needs is required.197 The inexperience of adolescents places particular responsibility on health-care providers to identify young people’s conspicuous and emerging health-care needs. Health-care providers also need competence to maintain an appropriate level of engagement with family, and how to negotiate relationships with adolescents and their family in the context of local laws. It often requires individualised assessments of the competence of adolescents to make autonomous decisions about their health.230 Access to broadband and digital technology platforms such as Massive Open Online Courses offer exceptional opportunities to build competency in health-care professionals but face-to-face training will still be required.231
We are now clearer about the steps needed to make sexual and reproductive health services more adolescent responsive in countries of low and middle income.232 Training health workers without making changes to facilities does not increase service or contraceptive use. Equally, creating stand-alone services for adolescent sexual and reproductive health is not, of itself, effective.229 The most effective strategies use a combination of high-quality health-worker training, adolescent-friendly facility improvements, and broad information dissemination via the community, schools, and mass media to drive demand.233 Other elements within a multifaceted approach might include promotion of adolescents’ literacy about their own health, engagement of community leaders, an appropriate package of services, ensuring provider competencies, improving facilities, promoting equity and non-discrimination, collecting data for quality improvement, and engaging adolescents around practice policies.234 In England, the You’re Welcome criteria provide guidelines to health services to more consistently provide quality care to adolescents.235
Health-care services depend on adolescent help-seeking. School-based promotion of services, mass media campaigns, and social media all have potential roles to reduce developmental barriers to accessing health care by promotion of health literacy and help-seeking.236 Web-based or other technologies might improve help-seeking, although a recent systematic review found little evidence to date.237 In countries of low and middle income, school-based health services will have greater salience as participation in secondary education grows. Service models range from fully equipped and permanently staffed centres with medical, nursing, and counselling staff to clinics offering nursing services only a few hours a week. The predominant focus so far has been on provision of sexual and reproductive health care, where the evidence for the effectiveness of school-based health services without on-site provision of contraceptives is mixed.238 Better matching of health actions to adolescent health needs is an opportunity for all health services, including school-based health services.
Preventive health actions
We conducted a series of systematic reviews of systematic reviews to assess current knowledge on the effectiveness for preventive interventions outside formal health-care settings across the nine areas of health need specified in figure 7 (unpublished). We included both specific health outcomes and health risks. Some responses (eg, policy measures such as taxation or some forms of legislation such as gun control) are not directly targeted at young people but might have particular benefits for young people compared to other age groups. Other actions (eg, legislation around age of marriage or employment, or actions taken through schools) target adolescents directly. Between March 15 and March 30, 2015, we searched the following databases; CINAHL, Education Research Complete, ERIC, MEDLINE, PsycINFO, and Cochrane Database of Systematic Reviews. Levels of evidence were classified according to the criteria given in appendix text box 6. Highly recommended interventions are those with at least 50% of review studies reporting positive outcomes. These were often supported by some evidence on cost-effectiveness. Interventions with some positive evidence not reaching this threshold have a moderate recommendation with further research needed. Some other actions are unlikely to be effective in isolation but are recommended as part of multi-component interventions. Other investigators (unpublished) also reviewed the available literature on the economic case for health investments through the adolescent years. Due to the relative scarcity of cost-effectiveness studies of interventions that target adolescents, a review of reviews approach was infeasible and a review of primary studies was undertaken. These findings were incorporated into the evidence summaries.
Sexual and reproductive health including HIV
More than any other area of health, the sexual and reproductive health of adolescents and young adults is affected by a country’s cultural, religious, legal, political, and economic contexts. In many settings these underlying determinants overlap with the determinants of violence and substance abuse.183 Actions for sexual and reproductive health must take these contexts, as well as age and gender, into account. In responding, health actions are needed at each level—from structural, through to community settings including schools, and health services (table 4, appendix table 4). The most effective programmes are typically multi-component and target one or more of these settings.239
Table 4.
Evidence of effectiveness and cost-effectiveness of sexual and reproductive health interventions, including those for HIV
| Key findings | Comments | Cost-Recommendation | effectiveness | |
|---|---|---|---|---|
|
School-based interventions
| ||||
| Comprehensive sex education; A curriculum-based approach that aims to provide young people with the knowledge, attitudes, and skills to make informed decisions about their sexuality and sexual and reproductive health. Some incorporate contraceptive services or encourage young people to use contraception | Knowledge and attitudes: high quality evidence of moderate benefit from studies in high-income countries and countries of low income and middle income. Both adult-led and peer-led interventions have shown benefit Safe-sex behaviours: moderate quality evidence of mixed impact on service use. Significant but minimal beneficial impact on safe-sex behaviours, including condom use, number of sexual partners, initiation of first sex and risky sexual behavior STI or HIV prevalence and incidence: no evidence of benefit; high-quality evidence of some benefit with added contraception provision Pregnancy: high quality evidence of benefit of combining education and contraceptive promotion; moderate quality evidence of the effectiveness of multi-component interventions, particularly with intensive case management by a culturally matched social worker |
Few studies of interventions involving provision of contraceptives in countries of low income and middle income Few assess impact on biological outcomes Most studies of effects on pregnancy have been in high-income countries No evidence of heightening premature sexual activity |
Some evidence of cost-effectiveness in USA and Europe | Ensure that all adolescents and young adults’ rights to essential health information are met, including comprehensive sexuality education |
| Abstinence-only education | High-quality evidence that abstinence-only education is ineffective in preventing HIV, incidence of sexually transmitted infections and adolescent pregnancy | NA | Abstinence-only education is not recommended | |
| School-based health services: these range from fully equipped, with permanent medical, nursing, and other health staff to nurse clinics a few hours per week | Safe-sex behaviours: moderate quality evidence of mixed impact on contraceptive behaviours, more effective if on-site provision of contraceptives Pregnancy: some moderate quality evidence of benefit if contraception provision is on site |
Most studies in high-income countries. In countries of low income and middle income, linkages with health services might increase uptake of some sexual and reproductive health services |
NA | Provision of essential resources for health in schools and easy access to adolescent health services including condoms and modern contraception |
|
Community-based interventions | ||||
| Generating community support: for interventions in schools and health services through social marketing, public hearings, meetings, dialogues, and fairs | Sexually transmitted infection or HIV prevalence and incidence: South African Stepping Stones programme–showed reductions in herpes simplex virus-2 incidence Pregnancy: some moderate quality evidence of benefit particularly studies including access to sexual and reproductive health services Early marriage: some moderate quality evidence for the effectiveness of integrated programmes that focus on empowerment and incentives |
In countries of low income and middle income, it is likely to play a key role in the effectiveness of interventions in other settings | NA | Plays a key role in the success of interventions within other settings and should feature in multi-component interventions |
| Positive youth development programmes focus on school retention and academic success as well as social support and skill development—eg, family or parent engagement, life skills training, or peer mentoring | Knowledge and attitudes: some moderate quality evidence for effect Safe-sex behaviours: some moderate quality evidence around use of contraception, delayed sexual initiation and number of sexual partners Pregnancy: moderate quality evidence of no benefit Early marriage: moderate quality evidence of mixed impact |
Programmes may also incorporate adolescent participation and leadership and are likely to have broad educational and social benefits | NA | Promising intervention; further research is needed |
| Youth-friendly venues in which young people access information and services that address sexual and reproductive health needs | Moderate quality evidence of mixed impact on uptake of services; ineffective in changing safe-sex behaviours, HIV or sexually transmitted infection prevalence or incidence, and adolescent pregnancy | Main users are often older than the target age group | High costs so cost-effectiveness likely to be low | Not recommended in current form |
| Interventions to shift social norms around early marriage and pregnancy Cash transfers (in countries of low income and middle income) may be unconditional, with payments going to individuals who are not required to do anything to receive these, or conditional, with payments tied to risk states (eg, remaining sexually transmitted infection or HIV free), staying in school, or not becoming pregnant | Early marriage: moderate quality evidence of mixed effect Safe sex behaviours: some moderate quality evidence for the impact of both unconditional and conditional cash transfers Sexually transmitted infection and HIV prevalence and incidence: mixed results of conditional cash transfers for remaining STI or HIV free. A programme providing cash transfers for young women (the Zomba programme) to remain in school showed a reduction in HIV prevalence at 18-month follow-up Pregnancy: moderate quality evidence of some benefit Early marriage: moderate quality evidence for interventions that support school attendance–eg, provision of school uniforms and supplies |
More research needed around payment amounts and frequency The Zomba conditional cash transfer programme decreased teenage pregnancy rates among girls who had previously dropped out of school, but not among schoolgirls | Some evidence of cost-effectiveness in sub-Saharan Africa | Promising intervention; further research is needed |
| Peer education: education delivered by young people to their peers | Safe-sex behaviours: some moderate quality evidence for impact in countries of low income and middle income of programme that include provision of contraception Health service use: moderate quality evidence of mixed impact in countries of low income and middle income Moderate quality evidence that peer education in Europe was ineffective in changing knowledge and attitudes, sexually transmitted infection or HIV prevalence and incidence, or adolescent pregnancy |
NA | Promising intervention in countries of low income and middle income; further research is needed. | |
|
Family-based interventions | ||||
| Interventions to improve parent–child communication about sexual health and sexuality | Some moderate quality evidence of effect on parent–child communication and safe-sex behaviours | NA | Should feature in multi-component interventions | |
|
Online interventions | ||||
| Group and individually tailored Internet and computer-based theory and behavioural skills-based interventions | Knowledge and attitudes: high quality evidence of moderate benefit Safe-sex behaviours: high quality evidence of significant but minimal benefits Sexually transmitted infection or HIV prevalence or incidence: high quality evidence of significant but minimal benefits |
All studies conducted in high-income countries | NA | Promising intervention; further research is needed, particularly in countries of low income and middle income |
|
Promoting universal health coverage | ||||
| Health service interventions involve the provision of information and counselling, contraception, prenatal and postnatal care and delivery, abortion services and post-abortion care, treatment and prevention of sexually transmitted infections, HIV testing and counselling, and care for sexual and gender-based violence | Safe-sex behaviours: moderate quality evidence of mixed impact on contraceptive behaviours; some moderate quality evidence that making services more adolescent friendly increases service use Sexually transmitted infection or HIV prevalence or incidence: moderate quality evidence of ineffectiveness |
Quality of provider training likely to be an important factor in the success of interventions | NA | Health services should provide all essential health-care responses, including modern contraception and safe abortion regardless of age, marital, and socioeconomic status; providers should have the skills to provide confidential and non-judgmental care |
The provision of accessible and quality health care (eg, provision of contraception, STI screening including HIV testing, treatment of STIs, provision of continuous care for HIV-positive adolescents), and high-quality, comprehensive sexuality education are likely to be effective, although much more so in conjunction with a broader suite of actions. Although legislation is essential in protecting adolescents from sexual coercion, early marriage, and early pregnancy, discrepancies between statutory legislation and actual practices are a barrier to implementation. Such laws will often be ineffective without actions to change community and professional attitudes. Together with quality health care, comprehensive sexuality education, amelioration of family poverty, and access to quality education, legislation is one essential element within the suite of interventions for adolescent sexual and reproductive health.
Infectious and vaccine-preventable diseases
Vaccination against infectious diseases has received far less attention in adolescents than in children. Yet vaccination of adolescents is also important for ensuring completion of immunisation schedules (eg, measles-rubella, hepatitis B vaccine [HBV]), administering booster doses (eg, diphtheria-tetanus), and for primary immunisation (eg, human papilloma virus [HPV]). Rubella vaccination is important for adolescent girls in terms of intergeneration risks, while HBV is important for both sexes given the adult burden of disease from hepatitis B. Others to consider according to local prevalence and cost are BCG, influenza, and meningitis vaccines.
Recent developments have brought new attention to adolescent vaccination as a strategy to prevent adult cancers as well as STIs (eg, HBV, HPV). HPV immunisation for young girls is cost-effective across different regions.240,241 There are few cost-effectiveness studies in males.242 Cost-effectiveness has been calculated from preventing cancer but quadravalent and multivalent vaccines have additional value in reducing anogenital warts. In high-income countries, school-based HPV vaccination programmes have a higher uptake than other approaches.
Lack of basic knowledge has hindered responses to common infectious diseases in adolescents. For example, in contrast to diarrhoeal disease in children, the aetiological agents, proportion of vaccine-preventable morbidity and mortality, and comorbidities are largely unknown in adolescents. Similarly, very little attention has been given to adolescent tuberculosis, despite it being the leading contributor to the burden of infectious diseases in young adults in multi-burden countries (figure 14). It could, in part, reflect the predominance of adults presenting to clinical services. In Africa, estimates of tuberculosis prevalence range from 160 to 462 per 100 000 adolescents and young adults (unpublished). In Asia, the range is from 39 to 142 per 100 000. Because adolescents are prone to adult-type pulmonary manifestations, including cavitation and smear-positive disease, they are a potent source of infection to others.240 Yet there is little age-disaggregated data with studies typically referring to participants as children, or adults.
Figure 14. DALY rate from infectious diseases per 100 000 adolescents in multi burden countries.
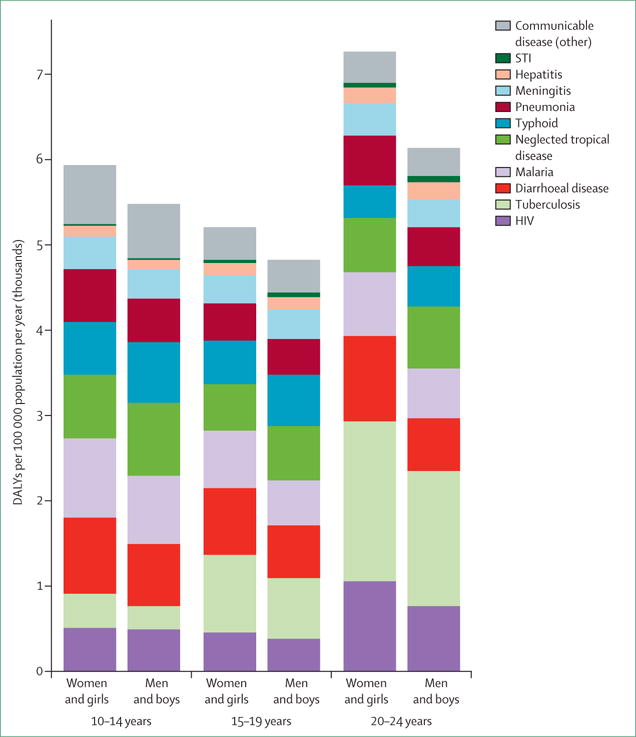
DALY=disability-adjusted life-years. Data from Global Health Data Exchange.69
Adolescents also carry a substantial burden from malaria in Africa. In high transmission areas, rates of malaria infection are higher in young women, who also encounter further risks in pregnancy.241 In endemic regions, childhood immunity provides relative protection for adolescents, but in areas of lower transmission, clinical disease is more common in adolescents and young adults. As infection in endemic areas is controlled, the risk for adolescents will increase. In low transmission regions, the adolescent incidence of malaria reflects their use of individual preventive interventions such as insecticide-treated bednets. A study from Nigeria,243 where 50% of the community is estimated to experience an episode of malaria each year, showed that only 8·5% of 13–18 year-old-students reported sleeping under insecticide-treated bednets. Over half had learnt about malaria prevention from traditional media (radio, TV).
Undernutrition
Adolescent nutrition is relevant for current, future, and intergenerational health.244 The causes of adolescent nutritional deficiencies are complex with contributors at the individual, household, and population level.245 There is currently no direct evidence of the benefit of interventions targeting adolescents specifically, or the effects of broader interventions on adolescents as a separate age group. Even the effect of iron deficiency anaemia on learning and educational attainment in adolescents is largely unknown. There is, however, good evidence for interventions targeting nutrition-related problems that often affect adolescents.
Iron requirements increase sharply during adolescence to support pubertal growth, and for adolescent girls to meet additional needs relating to menstruation.246 Adolescents, particularly girls, are therefore vulnerable to iron deficiency anaemia. Iron fortification of staple foods, such as flour, can be implemented through government policy or market-based mechanisms. It is cost-effective and can reduce iron deficiency anaemia at a population level by up to 63%.247 WHO recommends intermittent iron and folic acid supplementation for all menstruating adolescent girls and adult women in populations with 20% or greater prevalence of anaemia.248 Interventions addressing food insecurity, could also improve iron levels. For example, conditional cash transfer programmes,249 and home garden programmes250 have both been successful in improving iron levels in some participants.
The increased energy intake required for optimal growth during and following puberty means that adolescents are also vulnerable to protein-energy malnutrition.246 Interventions that can reduce protein-energy malnutrition, including balanced protein-energy supplementation,249 cash transfers,247 and improved household food storage systems,251 might therefore have particular benefits for them.34 Although school-based meal programmes might increasingly extend to include adolescents, recent reviews have found only small effects on patterns of undernutrition and school attendance in primary school-aged children.252 Using schoolchildren as a distribution point for household food packages decreased adolescent anaemia, but had little effect on protein-energy malnutrition.253 Because few interventions have been evaluated for adolescent populations, we know little of the benefits or side-effects (eg, obesity) of interventions targeting protein-energy malnutrition in adolescents.
Children born to adolescent girls are more likely to have low birthweight, independent of socioeconomic or maternal preconception nutrition status.254 This might be due to greater maternal–fetal competition for energy and nutrients as pregnant adolescents’ energy and nutrient reserves are still important for their own growth.255 Pregnant adolescent girls’ growth can slow or stop during pregnancy.256 They might experience weight loss, depleted fat body mass and lean body mass.257 Pregnant and lactating adolescent girls are also at increased risk of iron deficiency, which is in turn linked with low birthweight.254 For these reasons, preconception interventions to increase the availability of energy and micronutrients are likely to be of particular benefit. These include multiple micronutrient supplementation or iron and folic acid supplementation continuing into pregnancy, deworming to reduce nutrient loss, delaying first pregnancies and spacing of later births, and antenatal nutrition counselling and education.249 Because of maternal–fetal competition for calcium, pregnant adolescents are at increased risk for gestational hypertension and pre-eclampsia and are therefore likely to benefit from calcium supplementation.258
Stunted adolescent girls who become pregnant are at increased risk of complications such as vesico-ureteric fistulae and obstructed labour, and their children are at increased risk of low birthweight and preterm birth.249 We know little about the scope for catch-up growth among stunted adolescents whether before or during the pubertal growth spurt.259 However, any opportunity for catch-up will be restricted by early pregnancy and for that reason, delaying first pregnancy is essential in stunted adolescent girls.255
Specific nutritional interventions should ideally be considered in a broader context of actions. Delayed childbearing is a related priority.249 Therefore interventions that improve girls’ access to contraception, reduce early marriage, reduce coerced sex, and prevent early pregnancy through sexuality education are all linked.260 Nutritional interventions should ideally be integrated with strategies to empower young women through access to education and health care or to increase their control over household resources.261
Unintentional injury
Road traffic injuries dominate the picture of adolescent unintentional injury in most countries. Developmental immaturity, risky behaviour, and poor decision making in response to hot emotions increase the risks, particularly among boys and young men.262 Adolescents and young adults, particularly those in countries of low and middle income, are at high risk as they are more likely to be vulnerable road users, such as pedestrians, cyclists, and motorcyclists. For these reasons, they will disproportionately benefit from actions to promote safer road infrastructure and regulate road safety risks.263
In high-income countries, improvements in road design, equipment and maintenance, traffic control (notably speed reducing devices), vehicle design and protective devices, driver training and regulation (eg, drink driving), police enforcement and sanctions, public education and information, and post-crash care (from training of first responders such as ambulance services through to trauma surgery), have brought substantial reductions in the burden of disease.264
Effective action to reduce road traffic injury in adolescents and young adults is necessarily multifaceted and ultimately benefits all road users. The introduction of graduated licensing systems (panel 5)171–174 in which the young driver has an extended learner period increases low-risk supervised driving experience prior to licensure. Such systems might regulate exposure to high-risk settings such as unsupervised late night driving, driving with other young passengers, or alcohol use during an initial licensing period.265 Robust testing of competence before issuing of licences is generally an essential element. Legislation and enforcement of helmet-wearing in countries where a high proportion of adolescents and young adults ride motorcycles are likely to be cost-effective.266 Investment in pedestrian safety in regions where pedestrian injuries are common (eg, sub-Saharan Africa) could be beneficial. Effective actions include lowering speed limits on lengths of road where pedestrians mix with other traffic (and enforcement of these limits),267 regulation including police enforcement of the behaviour of drivers and riders at pedestrian crossings,268 improved pedestrian facilities (footpaths and crossings),269 separating pedestrians and vehicles,270 and increasing the visibility of pedestrians.271
These interventions could be supplemented by education programmes, with input from young drivers where possible.272 However, school-age driver education programmes, that focus on selecting a driving instructor, theory, and practical tests should be avoided as they could encourage earlier driving leading to greater risk of accidents.273
Intersectoral coordination has been a feature in countries that have made progress in reducing road traffic injury. In addition to the specific interventions outlined here, underpinning factors have included strong information systems, clear governance, civil society advocacy, and a capacity to implement effectively within the different sectors. Road traffic injury therefore provides a powerful illustration of the strategies needed for effective intersectoral action in adolescent health.188
Violence
Many individual, community, cultural, and economic factors are linked to violence in adolescents and young adults.97,274 Individual factors include personality attributes such as impulsivity, substance use and abuse, low educational attainment, and childhood aggression. Family conflict and poor family management, involvement of peers in problem behaviours, poor community social cohesion, high levels of residential mobility, drug trafficking, and unemployment might all be interlinked contributors. Social and economic inequality, availability of weapons, and laws and cultural norms that support violence are further factors. All could be targets for intervention.275
There is some evidence that single interventions such as legislation and school-based interventions targeting at-risk students can reduce rates of violence. However, most effective interventions, including those targeting homicide, require a multifaceted approach tailored to the risk profile of the particular community.276 Policy responses might include those directed to inequality, lack of access to education, unemployment, availability of weapons, and laws and cultural norms that support violence.277
Evidence of the effectiveness of interventions for preventing intimate partner violence and sexual violence in adolescents and young adults is largely lacking. In many cases, particularly in countries of low and middle income, studies are of poor quality with small sample sizes, varied outcome measures, and short follow-up periods.
Legislative and justice sector responses are again likely to be important elements. Indeed the number of countries with relevant legislation has grown considerably in recent decades. However legislation has not been shown to reduce intimate partner and sexual violence, and there is a need for system-wide changes to overcome resistance from the police and judiciary.278
Educational and skills-based programmes implemented in school or tertiary institution settings (principally in the USA) have been the most commonly used interventions to target adolescents and young adults. They aim to prevent or reduce dating and relationship violence by promoting gender-equitable norms and healthy relationships. While the programmes might change knowledge and attitudes, they have not been shown to affect behaviours.279
Community-based programmes that aim to promote gender-equitable norms have been the most commonly evaluated in countries of low and middle income. Evidence on their effectiveness is mixed.280 There is an absence of evidence on programmes that more fully address risk factors for intimate partner violence and sexual violence (eg, alcohol misuse, family-derived attitudes to violence, social norms that condone violence, and gender inequality), are tailored to local contexts, include families where appropriate, and target adolescents at highest risk (including those in emergency and humanitarian situations).278,281 Studies of violence against those of sexual minority status are rare (appendix table 5).
Mental disorders
The significance of adolescent mental disorders across the life course has only become clear in the past few decades.282 Studies in adults suggest that most mental disorders begin before 25 years of age, most often between 11–18 years.283 Recent prospective studies have found that while mental health problems are very common during adolescence, not all persist into adulthood, particularly if the episodes are brief.44,284 These understandings have put a growing emphasis on early clinical interventions through more accessible and better resourced primary health care or in some countries, through adolescent-focused mental health services.285 While there is evidence that access to health services is increasing in some places, there is as yet no evidence that these increases have led to detectable improvements in adolescent mental health.286
So far, evaluation studies have focused on a narrow set of preventive interventions that are readily testable in randomised controlled trials (RCTs). The dominant approach has been to take effective clinical treatments, such as cognitive-behavioural therapies (CBT), and apply these to the general population of adolescents or to at-risk subgroups to test if they prevent disorders developing. A systematic review and meta-analysis of RCTs287 of prevention interventions for depression or anxiety in children and adolescents had mixed findings on the effectiveness of this strategy. The investigators concluded that these interventions produced minimal to moderate reduction in symptoms in the shortterm but no effect beyond 12 months of follow-up. For a group of disorders that often persist for decades, there is clearly a need for innovation and more sustained effects of interventions. Approaches that focus on developmental mental health risks such as bullying, interpersonal violence, and social media risks are worth testing. Although digital and social media have been implicated as risk factors, online and mobile-phone interventions could play a positive part in prevention and promotion of access to clinical services.287
Suicide prevention
Risks for suicide increase in adolescence and young adulthood, particularly for the socially marginalised.288 Risks include depression, alcohol abuse, mental disorders, antisocial behaviour, sexual abuse, physical abuse, poor peer relationships, suicidal behaviour by friends, family discord, family suicidal behaviour, unsupportive parents, and living apart from parents.289 Social contagion is a further factor in up to 60% of adolescent and young adult suicides.290 Deliberate self-harm is also common in adolescents, particularly in females, and heightens risks for subsequent suicide.291
Adolescent-specific suicide prevention strategies have been implemented in three principal settings: schools, the community, and the health system.292 Goals range from increasing help-seeking for suicidal thoughts and behaviours; identification and referral of at-risk young people (eg, by health professionals, teachers, parents, or peers); reduction of risk factors for suicide; and promotion of mental health. School-based interventions are the most evaluated, with some systematic reviews focused solely on these.293 Universal interventions have been shown to improve knowledge of and attitudes about suicide293 but the gains are not maintained at follow-up. Gatekeeper training improves knowledge of and attitudes about suicide, and confidence in providing help.293 There is mixed evidence for universal school-based interventions, gatekeeper training, public education and mass-media interventions, screening, or postvention (after suicide) programmes on help-seeking behaviour,294 help-giving behaviour, suicidal ideation, or suicide attempts. Health practitioner education to increase the recognition of depression and evaluate suicide risk shows some benefits in preventing suicide across all ages and is therefore likely to also benefit adolescents and young adults.295
Evidence for prevention of suicide in adolescents and young adults is largely lacking in countries of low and middle income. The studies that exist are often of poor quality. Reducing suicide in adolescents and young adults is likely to require a multifaceted approach that includes limiting access to means (eg, gun control legislation, medication packaging, safe storage of pesticides), health practitioner training in risk assessment, and effective treatment of risk factors, such as depression and substance use.296 Help-seeking is likely to differ between males and females and future evaluations of preventive actions should address gender differences in effect.297
Physical health and health risks
Prevention of overweight and obesity
The prevalence of overweight and obesity rises in mid-adolescence, with the trend continuing into early adulthood.298 Because adolescent obesity strongly predicts adult obesity and associated morbidity, adolescence is an essential life phase for action.299 The case is even stronger when considering the maternal and intergenerational health risks of obesity in young women.300
Modifiable risks for obesity also change rapidly across adolescence. Physical activity commonly decreases and sedentary behaviour increases.301 In addition, adolescents have greater autonomy around food choices and are more likely to eat out of the home, which often leads to less healthy food choices.302 Exposure to media influences and susceptibility to processed food marketing also increase.303 Treatment of obesity in adolescents and young adults is necessary for the prevention and treatment of type 2 diabetes and other comorbidities, but is diffi cult. The rapidity of change in the prevalence and severity of obesity means that prevention in childhood and adolescence is of the highest importance.
Evidence on the effectiveness and cost-effectiveness of interventions for the prevention of obesity and promotion of physical activity is included in appendix table 6. Few reviews focused on adolescents, although some report on studies of children that include younger adolescents.304 Multi-component interventions that incorporate policy measures, environmental changes that promote physical activity, and education about a healthy diet and physical activity are more likely to be effective than single interventions.305 More work is needed on interventions that capitalise on peer and social network influences, and further research is needed to explore the impact of gender on response to obesity prevention interventions.306 Barriers to participation for girls might be greater than for boys and might include cultural or body image sensitivities (especially in mixed-gender settings); a focus on competitive sports and lack of facilities in schools (eg, changing rooms, toilets, and showers).305 There is also a need for further research into interventions that target adolescents and young adults who are not in educational settings, minority groups, and socially disadvantaged adolescents.307 In addition, there is a need for evaluation, including economic evaluation, of obesity-related interventions in countries of low and middle income. Consistent with the reductions in substance use that fiscal and marketing interventions have brought, the potential benefits from interventions to limit food marketing and increase the relative cost of unhealthy products are likely to benefit adolescents in particular.
Alcohol, illicit drugs, and tobacco
Consumption of alcohol and illicit drugs often begins and then increases during the adolescent years, with some evidence suggesting that adolescents are using substances at increasingly early ages.308 Early initiation of alcohol use is linked to later binge drinking, heavy drinking, and alcohol-related problems in adolescence and adulthood.309 There is also evidence that early consumption can lead to impairment of neurological development (appendix table 7).310
Regulatory or statutory enforcement interventions show the most benefit in the prevention of tobacco and harmful use of alcohol. Regulating the availability of alcoholic beverages through restricted times of sale and reducing the demand for alcohol through taxation and pricing are two of the most cost-effective strategies, while regulating access to alcohol through restrictions on purchasing age is particularly effective for preventing alcohol-related harms in adolescent and young adults. The great majority of this evidence is from high-income countries. Interventions should be tailored to the local context with consideration to levels of alcohol consumption, age-related and gender-related drinking patterns, and levels of harm.
Treatment and rehabilitation services and harm minimisation strategies have been the main focus in reducing the adverse consequences of illicit drug use. Harm minimisation strategies are essential in preventing transmission of blood-borne viruses, including HIV and hepatitis, and can include needle and syringe exchange programmes, drug substitution programmes that switch users from illegal drugs to legal drugs dispensed by health professionals, HIV testing and counselling, prevention of and services for the management of STIs, overdose prevention, and education relating to wound and vein care.311 Strategies need to be tailored to the local context, including drug use patterns and related levels of harm.
Whether or not an adolescent initiates tobacco use depends on diverse factors, such as gender, concerns with bodyweight and attitudes to smoking, parental, peer, and community smoking, socioeconomic status, and level of education.312 School, family, community, and media-based intervention can be beneficial but the effects are small, and should ideally form part of more comprehensive strategies, as outlined in the Framework Convention for Tobacco Control.
Limits in current knowledge
For most health problems and risks, there is a scarcity of published literature on the effectiveness of interventions for adolescents and young adults. Furthermore, with the exception of sexual and reproductive health, available evidence at the systematic review level is from high-income countries, particularly the USA. Different cultures, beliefs, knowledge, lifestyles, and health systems affect implementation and effectiveness in different settings. The costs of interventions will also vary markedly between countries with different salary structures, health systems, other unit costs, and methods of implementation. Costs are largely unavailable for many settings and evidence on cost-effectiveness scarcer still. Comparison of cost-effectiveness is further complicated by differences in outcome measures, methods, and thresholds for what is considered cost-effective. A move towards a common outcome measure such as the cost per disability-adjusted lifeyear averted would be valuable.313
Developing more comprehensive responses
The social and environmental determinants of adolescent health and wellbeing act at different levels and across different settings. Furthermore, many social and structural determinants affect multiple and interconnected aspects of adolescent health and wellbeing. The most effective responses operate at different levels of relevant settings.55 Table 5 outlines six platforms for action in adolescent health and recommendations for actions from each. These platforms offer scope for action in nearly all countries.
Table 5.
Recommended action bundles for adolescent and young adult health problems and risks
| Structural | Social marketing | Community interventions including family | Electronic health, mobile health | Schools | Health service sector | |
|---|---|---|---|---|---|---|
| Sexual and reproductive health, including HIV |
Legislation 18 years as the minimum age of marriage Allow provision of contraception to legal minors Legalise abortion |
Promote community support for sexual and reproductive health, and HIV health access for adolescents |
Cash transfer programmes, with payments linked to staying in school Positive youth development Peer education |
Target knowledge, attitudes, and risk behaviours |
Quality secondary education Comprehensive sexuality education Safe schools with clean toilets and facilities for menstrual care School-based health services with condoms and modern contraceptives |
Condoms and affordable modern contraception including long-acting reversible contraception Early HIV and STI diagnosis and treatment Male circumcision Antenatal, delivery, and postnatal care Transition to adult care for HIV |
| Under-nutrition | Fortification of foods—eg, iron and folate |
Micronutrient supplements (particularly in pregnancy) Protein-energy supplementation Deworming Cash transfer programme Nutrition education |
Micronutrient supplements Healthy school meals | Screening and micronutrient supplementation | ||
| Infectious diseases |
Deworming Bednet distribution |
HPV vaccination Deworming |
Early identification and treatment Adolescent vaccinations (human papilloma virus, childhood catch-up) Deworming Bednet distribution Seasonal malaria chemoprevention |
|||
| Violence |
Gun control Legalise homosexuality and protect women from violence and sexual coercion Youth justice reforms to promote second chances and diversion from custody 16 years as the minimum age for criminal responsibility |
Promote knowledge of the effects of violence and available services |
Promote parent skills and parent–child communication Positive youth development Promote gender equality Economic empowerment Group training for awareness, knowledge, and skills |
Multi-component interventions that target violent behaviour and substance use | Trauma care | |
| Unintentional injury |
Graduated licensing Mandatory helmet wearing Multi-component traffic injury control |
Promote knowledge of risks | Police enforcement of traffi c injury control | Trauma care, including first responders (eg, ambulances) | ||
| Alcohol and illicit drugs |
Limit alcohol sales to underage adolescents Taxation on alcohol Drink-driving legislation Restrict illicit alcohol Interventions in licensed premises Diversion from youth justiceand custody Graduated drinking |
Advertising restrictions(br/)Campaigns to build community awareness |
Promote parent–child communication and parenting skills Needle-syringe exchange access Mentoring |
Target knowledge, attitudes, and risk behaviours | Alcohol-free policies | Risk screening and motivational interviewing |
| Tobacco |
Tobacco control including taxation, pricing, and advertising control Youth access restrictions Legislation for smoke-free air |
Anti-tobacco campaigns | Interventions to promote parent skills and parent–child communication | Text messaging adjunct to quitting | Smoke-free policies Multi-component | Routine screening and motivation interviewing to promote cessation |
| Mental disorders and suicide | Restriction of access to means | Promote adolescent mental health literacy | Gatekeeper training | Electronic mental health interventions |
Educational interventions Gatekeeper training School-based mental health services |
Practitioner training in depression recognition and treatment Routine assessment of mental health, including self-harm and suicide risk |
| Chronic physical disorders | Peer support initiatives | School-based health services |
Promote self-management Promote transition to adult health care |
|||
| Overweight and obesity |
Taxation of high-sugar, high-salt, and high-fat foods Front-of-pack nutrition labels Restriction of fast food advertising |
Promote physical activity | Create opportunities for maintenance of physical activity in daily life | Interactive or personalised feedback interventions | Multi-component interventions, involving education about healthy diet and increasing opportunities for physical education | Manage comorbidities of obesity |
Bold are actions where there is an evidence base and italics represent actions that are promising but without yet a strong evidence base in adolescents and young adults.
Structural interventions
Legislation, taxation, and implementation of policies bringing investment in families, communities, schools, and health services are essential elements of adolescent health action in all places. They lie at the core of actions for health risks such as tobacco and alcohol, prevention of road traffic injury, violence, obesity, and sexual and reproductive health. Structural interventions are dependent on sound governance, a capacity to implement within the relevant sectors, and good information systems to monitor implementation and health outcomes. Legal reforms are unlikely to be successful without addressing the values, knowledge, attitudes, and behaviour of the judiciary and police responsible for their implementation. Structural actions are more difficult as the government systems for implementation are generally weak. In many countries, information systems to support structural interventions are also weak.
Media and social marketing
Most social marketing and mass media approaches will not only target the attitudes and values of adolescents and young adults but also their families and broader communities. The South African multimedia so-called edutainment programme, Soul City, helped change social norms around HIV/AIDS and domestic violence, contributed to increased individual knowledge about condom use and domestic violence, and more widely contributed to the empowerment of local communities.314 Partnerships with civil society and media professionals are powerful in exploiting the potential of these platforms. One such coalition, MTV Staying Alive Ignite, has aimed to prevent the spread of HIV by attempting to change attitudes, behaviours, and national norms. Building on a confronting television drama, the accompanying multimedia campaign challenged young people in Kenya, Trinidad and Tobago, and Ukraine to ignite a wider social movement to stop the spread of HIV.
Community interventions
The lives of young people are affected by the behaviour, norms, and values of adults and other adolescents around them. Community interventions usually involve local government, families, youth-focused and religious organisations, and schools. Positive youth development programmes are, for example, often community based and seek to promote life skills and positive attitudes including self-confidence and empowerment, social and emotional skills, and good problem solving. The strategies employed range from sport, survival skills, and outdoor education to theatre, music and art, leadership training, and mentorship. An intervention such as the promotion of sport in girls has the potential to bring benefits in physical health and fitness, as well as empowering girls through challenging harmful traditional gender norms.315 The most effective interventions have generally incorporated elements that build on available community structures, use good information on adolescent health and wellbeing, adopt a multi-component strategy, and monitor progress. One well established approach has been the Communities that Care framework that has been trialled in a number of sites in the USA with clear benefits and evidence for cost-effectiveness.275
Online interventions
Young people are the earliest adopters of information and communication technologies such as mobile phones, instant messaging, the internet, and social media—a phenomenon seen in countries of low and middle income, as well as in high-income countries.316 New social media has the potential to provide a powerful voice for adolescents and young adults to actively engage with each other and their communities. They also have the potential to transform health knowledge and delivery systems worldwide.317
Trends in using digital media are global, but the means of accessing information varies widely (eg, mobile phones, personal or public computers). In sub-Saharan Africa, growth in access to mobile phones has meant that digital media are even available in many remote places.318 In Bangladesh, for example, over 70% of women of reproductive age have access to a mobile phone within the household.319 These new tools provide a platform for health education in their own right as well as the capacity to augment health-care delivery and other preventive actions including those within schools.320 Social media offers a possibility of reaching diverse groups including geographically and socially marginalised adolescents. This is a platform of great promise but as yet there is little consensus about the most effective strategies for use with adolescents. Evidence on effectiveness is also very limited both in terms of longer term benefits and harder health endpoints.
School interventions
For children who go to them, schools are the site of the most important relationships outside of the family ie, with teachers and peers. The global growth in secondary education has the potential to greatly increase actions for health among adolescents through schools. Yet despite the evidence that enhancing school environments brings major health benefits, most school-based interventions have been limited to the provision of health education. The most effective actions from this platform are multi-component with curriculum elements, a focus on a school’s social and physical environment, together with engagement of families and the community.321 These types of actions show consistently positive outcomes for adolescent sexual health, violence, and tobacco smoking and might be beneficial for other health risks.321,322
Health service interventions
Health care has distinct functions in responding to conspicuous health problems, emerging health issues, and chronic adolescent health problems. Health-care providers need the knowledge and skills to respond to these complex health issues, but they also require non-judgmental attitudes, a willingness to maintain confidentiality, and skills to engage with adolescents and young adults, while maintaining an appropriate engagement with families. Strengthening health systems, including health financing, creating health-care human resources, and leadership will also benefit adolescents. However, given the barriers they face, delivery of universal health care to adolescents also requires targeted investments.
Taking action at country level
Many interventions found to be effective in research settings are under used.275 One important reason is failure to match actions to need. Where it is unclear what the health priorities are, it is difficult to make the case for investment. Scalability is a further consideration and determined by the costs of operating at scale and the acceptability of an intervention in the local context.323 For comprehensive sexuality education, intra-curricular programmes in schools have great potential to be scaled up because of their compulsory nature. However, quality depends on teacher training, smaller class sizes, more lessons, and working with the local community context which are elements that increase costs. Advocacy is a significant cost component of early implementation that is likely to decrease as programmes become more accepted.324 As an intervention is successfully scaled up, its cost-effectiveness is likely to increase.325
Interventions need to be designed and implemented with an equity lens to ensure that benefits also reach the most hard-to-reach adolescents and young adults.326 Scaling up should give careful consideration to gender, race, ethnicity, sexuality, geography, socioeconomic status, and disability.327 Some actions might not reach vulnerable groups and could actually worsen inequities. For example, in budget-constrained contexts, financing tertiary education could be prioritised over universal quality primary and secondary education, which would further disadvantage the most marginalised adolescents.118
Figures 15 and 16 illustrate the complex picture of adolescent health in Nigeria, a multi-burden country. Nigeria has a continuing high disease burden related to maternal health. Adolescent fecundity is high, as are rates of early marriage, although with differences across states. Adolescent pregnancy rates in Nigeria’s northern states are more than four times higher than in the south. There is a 4-year lower median age of marriage in rural settings (16·6 years) compared to urban regions (20·8 years). Nigeria has an emerging HIV epidemic, particularly in the north-central zone, although this is not as advanced as in southern sub-Saharan Africa. Rates of unsafe sexual activity are high. Infectious diseases other than HIV, though diminishing, are still prominent contributors to burden of disease among adolescents with malaria and neglected tropical diseases notable among these.328 While these diseases of poverty are priorities, road traffic injury and sexual violence are also prominent. Haemoglobinopathies (eg, sickle cell anaemia, iron deficiency anaemia) figure prominently within chronic physical illnesses and rates of obesity are rising in both sexes.
Figure 15. Health outcomes for 10–24 year olds in Nigeria.
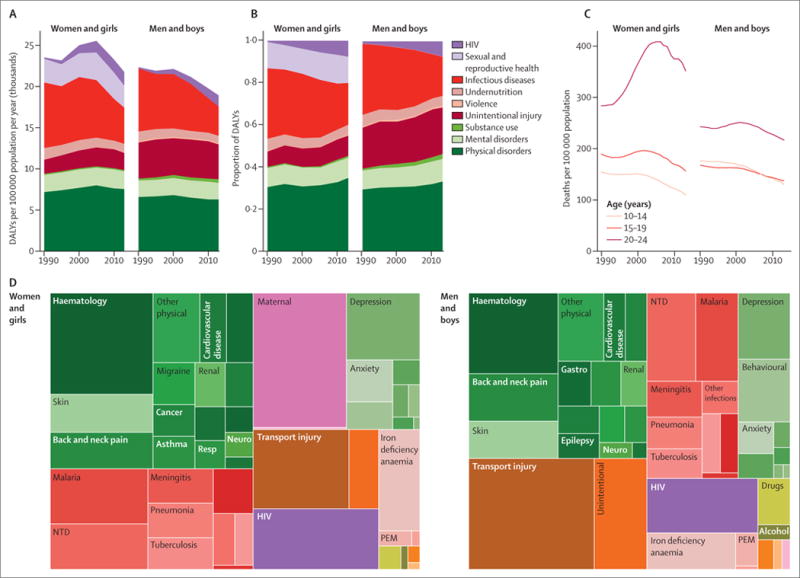
(A) DALYs per 100 000 adolescents aged 10–24 years, by cause and sex, 1990–2013. (B) Proportion of DALYs across 9 categories by sex in adolescents aged 10–24 years, 1990–2013. (C) Deaths per 100 000 adolescents aged 10–24 years per year, 1990–2013. (D) Causes of DALYs in adolescents aged 10–24 years, 2013, by sex. DALYs=disability-adjusted life years. NTD=neglected tropical diseases. PEM=protein energy malnutrition.
Figure 16. An overview of Nigeria’s health profiles for 10–24 year olds.
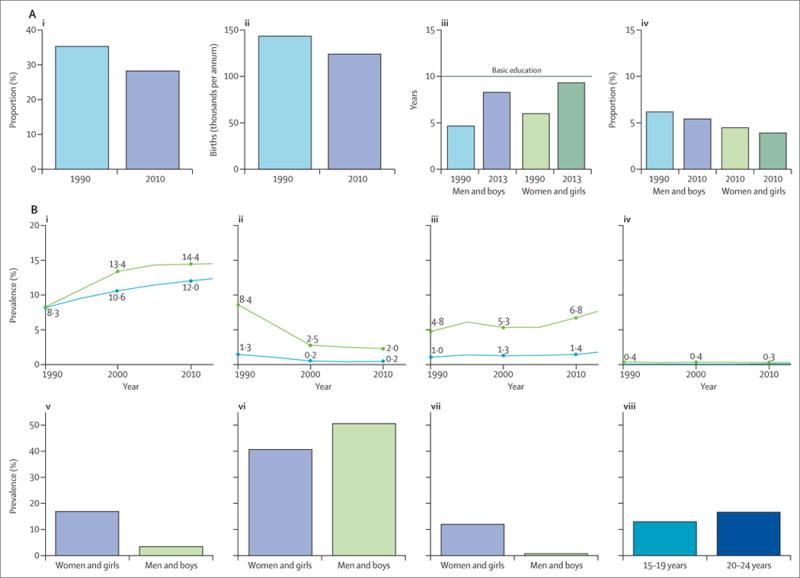
Social determinants. (i) Currently married women and girls aged 15–19 years. (ii) Birth rate in adolescent girls. (iii) Mean years of education attained in adolescents aged 15–24 years. (iv) Unemployment in adolescents aged 15–24 years. (B) Health risks. (i) Overweight and obesity in adolescents aged 10–24 years. (ii) Daily tobacco smoking in adolescents aged 10–24 years. (iii) Binge drinking in the past 12 months in adolescents aged 10–24 years. (iv) Lifetime use of injectable drugs in adolescents aged 10–24 years. (v) Adolescents aged 10–24 years reporting sex before age 15 years (2004–14). (vi) Adolescents aged 10–24 years reporting condom use at last occasion of high risk sex (2004–14). (vii) Intimate partner violence in adolescents aged 10–24 years (2013). (viii) Unmet need for contraception in women and girls aged 10–24 years, married or in civil union (2009–14). DALYs=disability-adjusted life-years. NCD=non-communicable diseases.
Responses to Nigeria’s adolescent health profile are outlined in panel 8. Because Nigeria has a low density of health workers, scaling up of health-service coverage is essential for maternal health care, greater contraceptive coverage, treatment of HIV and other infectious diseases, and responding to adolescent chronic physical health problems. Retention in secondary education is increasing but fewer than 50% of adolescents and young adults are receiving a basic level of education (9 years). For both health services and schools, there is a need for scaling up the country’s capacity. At the same time emerging health priorities of road traffic injury and obesity warrant specific policy and legislative responses.
Panel 8. Priority health actions for 10–24 year olds in Nigeria.
Sexual and reproductive health
Adolescent fecundity and maternal health, new HIV infections, and HIV morbidity and mortality
Comprehensive sexuality education (in and out of school)
Promotion of condom use
Voluntary male circumcision
Contraception, abortion care, and maternal health services
HIV testing, treatment, and care
Enforcement of legislation prohibiting child marriage
Increase participation in education
Infectious diseases
Malaria morbidity and mortality, tuberculosis, neglected tropical diseases, meningitis, pneumonia
Access to quality health services for diagnosis and treatment
Ensure completion of childhood vaccination, catch-up vaccination, and additional vaccines (eg, human papilloma virus, meningococcal)
Improved water, sanitation and hygiene, nutrition, and provision of bednets
Unintentional injury
Road traffic accidents
Legislation for graduated licensing, motorcycle helmet use, speed control, pedestrian safety measures, and alcohol and driving control
Access to high quality trauma care
Physical disorders and non-communicable disease risks
Chronic physical disorders, overweight, and obesity
Adolescent-friendly health services
Prevention of overweight and obesity through taxation of unhealthy foods, restriction of fast food advertising, and promotion of physical activity in school and in the community.
Adolescent and young adult engagement
Two ideas around youth engagement have gained traction in international development. The first is that adolescents and young adults make an essential contribution to the design and implementation of programmes and policies that affect them and their peers. The second is that with structures, support, and processes to do so effectively, meaningful engagement leads to healthier, more just, and egalitarian communities.329
The UN’s definition of youth participation is “the active and meaningful involvement of young people in all aspects of their own, and their communities’ development, including their empowerment to contribute to decisions about their personal, family, social, economic, and political development”.330 The UN further affirms that societal progress is based in part on a capacity to incorporate the contributions of youth in “building and designing the future”.331 From a UN perspective, meaningful youth participation is both a fundamental right and captures the unique contributions and social mobilisation skills of young people.332
Developmental perspectives further support meaningful engagement as an essential positive influence on social and emotional development. The transition through puberty brings a shift in a child’s orientation from one focused on self and family towards one that takes on the perspectives of others.333 By adolescence, most individuals have gained the cognitive capacities to allow their greater engagement in social, community, and political life. Adolescents are emotionally primed to engage. Developmental neurobiologist Ron Dahl has described early adolescence as a phase of igniting passions, during which structures, processes, and support for positive and meaningful engagement shape trajectories of development into adulthood.333 Equally, social contexts that value antisocial forms of engagement including violence, substance abuse, or extremism (of any sort) will shape development to the detriment of the individual and the broader community. A lack of social and emotional engagement brings risks for mental disorders including depression.28
History has seen many examples of how this growing positive engagement, along with the energy, enthusiasm, and passion that young people bring, inspires social change movements. Adolescents and young adults have led movements for democracy in Asia and the Middle East, for LGBT rights, for gender equality, and for action on climate change. Conversely, where opportunities for positive engagement are absent, we have seen adolescents and young adults drawn into violent extremism and gang violence, with catastrophic health and societal outcomes.183
Meaningful engagement of young people in health advocacy
The idea that meaningful engagement of adolescents and young adults contributes to improvements in health policies and services, and in turn improved health and broader societal outcomes is well established. More than 20 years ago, WHO cited the importance of youth in its call for community participation in health, noting that effective adolescent health programmes require youth involvement at local, national, and international levels. This initiative extends from setting programme objectives to policy development and allocation of resources.329 UNICEF, United Nations Population Fund (UNFPA), UNAIDS, and international non-governmental organisations such as the International Planned Parenthood Federation have followed suit, recommending, and sometimes mandating, youth participation in the governance of service systems, as well as in the oversight and implementation of health-related policies (appendix text box 7).
Young health advocates themselves recognise the crucial importance of meaningful youth participation in health policy making and programming. The Lancet Commission on Adolescent Health and Wellbeing includes two young members, who were selected through a competitive online process. As the Commission also sought to incorporate the views of a more globally representative sample of young people, we conducted an online survey to capture a broad range of inputs. The survey was promoted to youth health advocates through the networks of the Commissioners and their organisations. We sought the opinions of youth advocates about priority areas for investment and which key messages are likely to be most effective with decision makers. More than 500 adolescents and young adults from 89 countries working across a range of health issues participated. The idea that “Adolescents and youth should be supported and empowered to contribute to designing, implementing and assessing policies, programs and systems that contribute to their health and wellbeing” was considered the single most important theme by them.
Even though the rationale for youth engagement in health is strong, there have been few syntheses of the evidence on its effectiveness. We reviewed available studies of models of youth engagement, leadership, and participation, and their effectiveness (unpublished). Few studies examined the effects of adolescent and young adult engagement on health outcomes. In contrast to the scarcity of effectiveness studies, there is a growing literature about the essential elements for meaningful youth engagement.
A crucial starting point is a rejection of presumptions that adults know best. Rather, successful engagement emphasises the capacities of adolescents and young adults to work in partnership with adults. This generally requires both processes to promote active youth participation (training young people to speak), and the responses of adults (training adults to listen). Ideally, partnerships with adults begin early. Typically, it begins with shared decision making in the family. It should extend to growing engagement in school life and local community groups that provide enabling and protective environments for adolescents to learn the skills for effective engagement. With growing capacities, adolescents can further engage more meaningfully in policies, systems, and programmes that affect them and their peers.
Adolescents and young adults depend on systems and structures for engagement that are put in place and supported by adults. To engage most effectively, youth need resources (including financial), training, ongoing mentorship, and sensitisation to political and management processes (figure 17). They also need platforms and mechanisms for engagement. In different settings, adolescents and young adults face very different opportunities and limits on their ability to engage and advocate meaningfully. Social, cultural, economic, and political forces shape both the opportunities for and the form of youth engagement and the strategies needed to promote it.334
Figure 17.
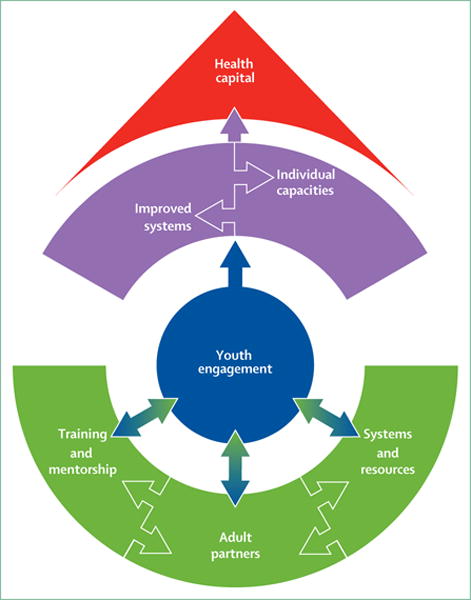
Conceptual framework of the essential elements in meaningful youth engagement
Existing models range from tokenism to those that are completely youth led.335 More egalitarian relations between young people and adults are essential for meaningful engagement but decisions are still often taken through an adult lens that overlooks youth perspectives.336 In general, the greater the level of youth control and responsibility, the greater is the effectiveness of engagement, whether around their own health or around policies and programmes that affect others.335
Adolescent and young adult engagement around health can start with the individual and can move to the clinic and community levels, and on to national and international platforms. Below, we discuss some of the ways in which young people have engaged in health decision making, policy making, and programming. We point to both promising strategies and recommendations for how these efforts might be leveraged to achieve greater impact.
Approaches to youth engagement and advocacy in health
Peer education, or the promotion of healthy behaviours for young people by young people, is the most evaluated youth engagement strategy in the health sector. Such interventions have shown positive outcomes for the young people conducting the programming (ie, the peer educators themselves).337 Peer promoters themselves have greater self-confidence, improved communications, leadership and interpersonal skills, higher aspirations, and lower rates of health risk behaviours. Although better evaluated than most, there has been little testing of their effectiveness in changing health outcomes for the broader population of young people they are meant to reach. This reflects a particular challenge in resource-constrained settings, and a tension between a wish to scale up promising approaches and the value of undertaking smaller scale interventions with rigorous methodologies.337
Youth engagement in health-related advocacy has increased over the past two decades, fostered at a global level by the UN and other international organisations. Similar processes have occurred at country and community levels within organisations delivering services to young people. Panel 9 uses the example of Education as a Vaccine from Nigeria to illustrate one recent example of national youth advocacy.338,339
Panel 9. Youth advocacy in health.
Education as a Vaccine, a Nigerian non-governmental organisation focused on the needs of vulnerable children and adolescents, supported a Youth Advocacy Group (YAG) of ten young Nigerians, aged 18–24, to educate peers, adult gatekeepers, and policy makers in sexual and reproductive health policies for young people. In 2010, a draft national HIV/AIDS anti-discrimination bill was tabled that failed to take into account the stigma and discrimination faced by young people. The YAG developed and presented a position paper to the House of Representatives, highlighting youth-specific recommendations.
A specific goal was to ensure that the bill made reference to protecting the rights of young people. The YAG then actively engaged other youth across Nigeria in support of their recommendations. The YAG created a video screened at university campus education events in three states. At each event, a YAG member led discussions on the policy.
A petition calling for the inclusion of the youth recommendations collected 1500 signatures. Once the bill passed the House, with the YAG recommendations included, the group generated postcards from nearly 2200 young people in advocating with the Senate. The bill was signed in 2015 and included language recommended by the YAG. The experience illustrated common challenges for young advocates. They faced a culture that discouraged young people from speaking out, based on an erroneous perception that they lacked the knowledge and expertise for a meaningful contribution. Youth groups across the country were poorly resourced making communication difficult. Lastly, lack of financial support limited the capacity to engage other youth. Despite the challenges YAG members gained leadership skills and a capacity to, in the words of one member, “be responsible not just for myself but for others”.
Community-based participatory action research has become popular in work with marginalised adolescents. It has the potential to shift the power dynamic from one in which adolescents are subjects of research to one where they are active partners.340 Engaging young people in this way gives insight into the lives and realities of young people. Photovoice is an example of this approach, as illustrated in figure 18.341–344
Figure 18. Photovoice: using images to communicate and advocate.

Photovoice is a participatory action research strategy commonly used with disadvantaged and marginalised groups. Photos are used to document personal and community issues and provide a basis for storytelling. It is a powerful tool for youth engagement, raising awareness of important aspects of the lives of adolescents. It is a useful way of levelling power differentials between adults and young participants. The strategy can be a means to catalyse community action, as the development of a story narrative facilitates the engagement of all participants in engaging in social change. It has been used across a wide variety of settings including health care (eg, young survivors of childhood cancer in South Korea), prevention and health promotion (eg, obesity prevention in the USA, reproductive health and empowerment programme targeting married adolescent girls in Ethiopia), and in youth engagement more broadly (adolescents identifying community strengths in Kenya). The images powerfully engage public interest in the daily lives and health challenges faced by young people.
There are reasons to be optimistic about the scope for extending meaningful youth engagement around their health and wellbeing. The growth of democratic processes in many countries brings new opportunities.345 The greater involvement of adolescents and young adults in education, employment, and local community and youth organisations also offers new contexts for meaningful engagement. Social networking and digital media make it possible to access information, communicate, and mobilise with other advocates as well as draw in resources in unprecedented ways. New media promote more active engagement as adolescents and young adults can independently generate their own content.346 These possibilities allow broader collaboration which in turn can generate political leverage. Time, privacy, and the need to convince adolescents that their voices will be heard remain barriers. For these reasons capitalising on these new possibilities is likely to require a shift in approaches to communication for both government and civil society organisations.347
One unique challenge is that as young people grow, their places as young leaders must be taken by the next generation. More than any other field of health, youth engagement requires ongoing renewal.348 Attitudes of adults towards young people and their capabilities, together with young people’s lack of confidence in engagement processes, are a common barrier.349 Attitudinal barriers commonly arise from cultural contexts where young people are perceived as subordinate to adults, that exclude young women, and that further stigmatise socially marginalised groups.350,351 Inflexible bureaucratic arrangements, insufficient investment to support ongoing engagement, and restrictive policies, such as limiting the participation of adolescents in research, might be further limiting factors.352
For these reasons, most youth engagement in health falls short of sustainability, and top-down, adult-driven approaches remain the most common.336 In programmes that do engage young people, those selected are often already confident, articulate, and naturally identified leaders.352 In practice, few efforts meaningfully involve the most marginalised young people, who could include ethnic minorities, HIV-positive youth, married adolescents, youth with disabilities, LGBT youth, youth living in poverty, those with lower educational levels, and very young adolescents.353 In many circumstances, adolescent girls and young women face inequitable systems and structures which limit their participation. Yet meaningful engagement of vulnerable young people is feasible. One programme with homeless youth in the Skid Row of Los Angeles, California, and their adult mentors used the sharing of personal stories to inform community activism and policy advocacy, and successfully gained educational rights for homeless students.354
More effective and meaningful engagement will require systems and processes that exist in few programmes and structures today. Mentorship between adults and youth; the building of young people’s capacity, skills, and knowledge; the establishment of new forums; and the growth of new methods of communication can create a sustainable environment for young people to engage around their health and that of their communities. The growth in mobile devices together with social networking and digital technologies provide unparalleled opportunities for engagement. Although the evidence of the effectiveness of new communication technologies in promoting engagement remains limited,355 many global organisations including WHO, UNFPA, and the Lancet Commission itself are using online technologies, including social media and surveys, to gather information about health priorities directly from young people to inform strategies and policies.
Data and accountability
Global health and development frameworks have tended to include a cycle of three elements of monitoring, review, and appropriate responses. These have been criticised for failing to adequately address governance and instead relying on voluntary and non-binding commitments to outcomes.356,357 The limits of this approach have led to calls for independent accountability and for ensuring that monitoring and evaluation processes are participatory and inclusive.65 The newly-adopted 2030 Agenda for Sustainable Development has recognised a need for greater accountability particularly at country level.358 The Global Strategy for Women’s, Children’s and Adolescents’ Health notes the importance of transparent and accessible data, for the inclusion of sectors beyond health service delivery, and for the engagement of civil society.4 Other global health agendas have also called for increased accountability, with participatory frameworks proposed across a range of areas relevant to young people including HIV, NCD risks, obesity, women’s health, mental health, and nutrition.359–361
Such participatory approaches to accountability could provide settings for meaningful youth engagement. Young health advocates have the energy and optimism to challenge corruption and harmful traditional practices, and drive governance, advocacy, and accountability for decades to come. To date, adolescents and young adults have generally been an afterthought in global and country health initiatives.
Kraak and colleagues357 reviewed 15 interdisciplinary frameworks for accountability, including trade and international development, human rights, business finance, public health policy, and global health. On this basis they outlined a four-step process for accountability. We have adapted this four-step framework to consider the particular elements of effective accountability for adolescent and young adult health and wellbeing, as outlined in figure 19.357
Figure 19.
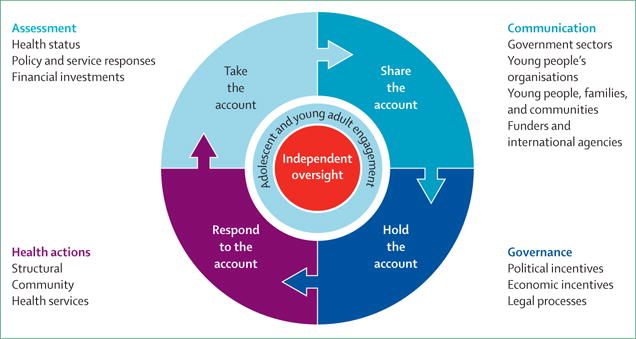
Four-step accountability framework for adolescent health and wellbeing
The limits of current data systems
Planning responses to adolescent health requires data that is timely, developmentally relevant, age disaggregated and sex disaggregated, and defined to a local level. Ideally, these data would allow comparisons over time and tracking of inequalities within and between countries. In reality existing global data systems for adolescents are uncoordinated, inconsistent in coverage and timing, inadequately disaggregated, missing large groups of adolescents, and fail to deal with the spectrum of health problems and their determinants (appendix text box 6).362 This matters as countries of low and middle income are, to a large extent, dependent on global surveys, such as Demographic and Health Surveys, for data for health policy and programming.
Recent developments in health metrics seem unlikely to provide the impetus for change. The Global Reference List of 100 Core Health Indicators, proposed by WHO to guide responses at global, regional, and national levels illustrates some of the difficulties.363 Younger adolescents are largely missing, both in specific indicators and age disaggregation with counting generally starting from the age of 15 years. Although some age disaggregation is proposed from the age of 15, adolescent fertility rate is the only adolescent-specific indicator included.331 The list does not include indicators around mental and substance use disorders or violence. The gaps in health risks are even more compelling with obesity, physical activity, and fruit and vegetable intake indicators proposed only from 18 years. Important social determinants of adolescent health and wellbeing, including child marriage and lack of participation in secondary education, are not included in either the core or supplementary lists. These indicator gaps are further illustrated in appendix table 8.
The data gaps are compounded by the absence at a global level of any single agency with responsibility for processing available data to provide a more complete picture of adolescent health at either a global or country level. The patchwork approach to data collection is then mirrored in data analysis and reporting systems where responsibility for adolescent health and wellbeing data sits across a range of UN agencies (eg, UNFPA, WHO, United Nations Procurement Division, World Bank, UNICEF), global non-governmental organisations (eg, Population Council, Population Reference Bureau) and academic groups (eg, Institute for Health Metrics and Evaluation). The result is an incomplete and uneven picture. Similarly, for those wishing to understand the profile of adolescent health and wellbeing in any given country, there is typically no single “go-to” national department or agency.
These limits in global data systems pose major difficulties for countries in taking an adequate account of adolescent health needs. Yet even with better coverage of health areas, global surveys are unlikely to provide adequate data for national planning; none provide the finer-grained geographic information needed for monitoring progress and capturing inequalities at subnational levels. There is therefore a need for country-level technical capacity to extend current data collection and data processing systems. It is essential that data reporting extends to sectors such as education, transport, justice, and community environments. Ideally this would lead to country-level reports of health and wellbeing including inequalities and inequities across adolescent groups.
Digital media have the potential to transform the sharing and presentation of such data, to generate new data and assess its quality, and allow for communication to and with a much wider audience. It also has the potential to heighten the engagement of young people globally around adolescent health needs, as well as generating greater demand for data.
The process of communication around adolescent health and wellbeing requires engagement with different government ministries. In many countries, it extends to international agencies and global funders. However, this process also needs the involvement of civil society groups outside of government.166 These constituents include adolescents and young adults themselves, youth organisations, professionals working with adolescents, academics, and private industry. Young people and youth-focused organisations are essential stakeholders in this process. Their meaningful engagement can ensure a proper understanding of what the data mean, assess and inform the feasibility and appropriateness of potential actions, and support broader buy-in for such actions.
Coordinating responses
For the most part, the most effective actions for adolescent health and wellbeing are intersectoral and multi-component, tailored to local needs and capacities. This raises important questions about the structure and processes for governance. The creation of processes whereby civil society can hold government ministers to account for the investments made (or not made) depends on the cultural and political context.364 For governments less open to influence from civil society, the involvement of international agencies and use of financial and economic incentives might be needed for advancing adolescent health and wellbeing.
Holding industry to account is yet more challenging. Kraak and Story365 examined the Children’s Food and Beverage Advertising Initiative, which promoted the responsible use of cartoon brand mascots to promote food products to American children between 2000 and 2015. They found moderate progress in taking and sharing the account. This included public hearings in the US Congress, as well as dialogues between investors, businesses, public health researchers, advocates, and government officials. However, there was little actual progress in holding companies to account with the absence of a clearly empowered organisation to hold industry to account a major shortcoming. Such an organisation could encourage governments to play active roles through taxation, legislation, economic incentives, and social audits to influence the marketing and sales of products such as food, tobacco, alcohol, fashion, or illicit drugs—activities that directly and indirectly influence health and health risks for young people.1
Taking action also requires a sound evidence base of interventions that have been ideally adapted and trialled in similar contexts. Yet in areas such as mental disorders and sexual and intimate partner violence, there are not yet clearly effective and scalable interventions for adolescents. Some contexts that are of major importance in shaping the health and wellbeing of adolescents, including families and digital media, have received little attention in intervention studies. In many areas of health need, actions have been evaluated in high-income countries, and for the most part, have neither been adapted nor trialled in countries of low and middle income. Many innovative approaches have been piloted and sometimes rolled out on a larger scale but without evaluation. New platforms based on digital media offer great promise but in the absence of more systematic evaluation their broader usefulness is still uncertain. Lastly, the absence of good cost and cost-effectiveness data in different regions remains a barrier to implementing effective actions at scale.
These knowledge gaps arise in part from a lack of technical capacity. Unlike the fields of maternal and child health and HIV that have had considerable investments over decades, adolescent health has seen little technical investment. This is further compounded by the lack of any single agency with responsibility for pulling together the evidence base for action. Current policy and programming relevant to adolescent health and wellbeing sits within different agencies (eg, WHO, UNICEF, UNAIDS, UNESCO, UNFPA, World Bank, United Nations Offi ce on Drugs and Crime [UNODC]) as well as with various global non-governmental organisations (eg, Save the Children, Population Council). The absence of an overarching coordinating body around the evidence base has led to an inability to provide consistent guidance to countries on best buys or the how to of intersectoral implementation.
Limitations notwithstanding, there is sufficient knowledge for generating greater action at country level around adolescent health and wellbeing. A human and technical capacity to act is essential. This usually requires attention to the training of those across the relevant sectors (eg, pre-service and in-service training of teachers in adolescent development and youth engagement). There is a need for growing adequate country-level technical capacity in policy and programme evaluation. This technical capacity is not only important in ensuring fidelity in programme implementation but would also generate valuable data on both local effectiveness and resources required for implementation.
Key constituents
Adolescent health and wellbeing is increasingly shaped by diverse influences beyond the immediate family and community. These influences are themselves changing rapidly. Adolescent health and wellbeing increasingly depends on the engagement of a broad range of actors and constituencies from local communities to the global level.
Adolescents and young adults are central actors around their health and wellbeing. Their meaningful participation and engagement is essential for effective action aiming to enhance their health and wellbeing. This same engagement is essential for their own emotional and social development. There is need for sustainable systems and processes where meaningful engagement becomes a normal part of their lives.
The organisations with and working for young people have a particularly important role in their support and mentorship. The influence of religious leaders on community and family values, as well as directly on the attitudes, beliefs, and values of adolescents, makes these leaders important sources of direction.
Despite the rapidly changing social determinants of adolescent health and wellbeing, families provide the most important platform for the transition to adulthood. Families are also affected by rapid social and economic change. The knowledge, skills, financial resources, and community support available to parents remain essential determinants of adolescent health and wellbeing.
Professional groups such as teachers, health-care providers, community workers, sports trainers, and employers have increasingly important roles in young lives. For disadvantaged and marginalised youth these groups extend to the judiciary, police, youth justice workers, social, and accommodation service workers. Their capacity to engage and understand the health, social, and developmental needs of adolescents will determine their effectiveness in promoting health and wellbeing.
Because the major determinants of health lie outside the health service sector, other sectors within government have an essential role in adolescent health and wellbeing. Key portfolios for adolescent health include ministers for health, education, youth, finance, justice, transport, and industry. Effective actions are often multi-component and intersectoral. They require both a capacity for action within individual sectors and coordination of investment across different sectors. That coordination is dependent on understanding health needs, current investments, and effective actions, together with the structures and processes to coordinate across ministerial portfolios.
Private industry, including media and marketing organisations, increasingly shapes the health, lifestyle, attitude, and wellbeing of adolescents. Private industry also provides employment and many essential services for adolescents and their families. Establishing a dialogue with industry as essential partners in adolescent health and wellbeing is a pressing agenda.
The international development community has an essential role in resourcing and coordinating investments in adolescent health and wellbeing. This role will become greater with the Global Strategy for Women’s, Children’s and Adolescents’ Health. To date, efforts to support adolescent health have been piecemeal and poorly coordinated. Future investments require greater consideration of coordination, capacity building, and technical support at country level.
The academic community has the potential to partner with the international development community and governments in the development of health information systems, innovation and evaluation, and training service providers and youth health advocates. Many academic disciplines have a role in the promotion of adolescent health and wellbeing. However, the academic and research capacity in countries of low and middle income is at very low levels and in need of investment.
Independent oversight
Effective accountability requires independent review. A crucial question relates to the structures that would most effectively provide that oversight. Responsibility for adolescent health and wellbeing at a global level is currently dispersed across many agencies. For example, within the UN these include WHO, UNICEF, UNFPA, UNAIDS, UNESCO, and UNODC. Each agency has its own emphasis and particular age mandate. Greater coordination and stronger inter-agency partnerships, supported by funding partners, will be essential for progress. Whether this can be achieved without the creation of a global focal point for adolescent health and wellbeing within the UN system is an important question. The establishment of networks that bring together the global constituents for adolescent health and wellbeing will also be essential in galvanising and reviewing action, mobilising and growing global resources including funding, technical and research capacity, processes for youth advocacy, and frameworks for intersectoral action. This Commission on Adolescent Health and Wellbeing is an example of such a process. Its continuation as a Standing Commission on Adolescent Health and Wellbeing will allow a broadening of these activities in the coming years. The extension of the UN Secretary-General’s Every Woman, Every Child to adolescents, within the Sustainable Development Goal Agenda, provides the most important single opportunity for the health and wellbeing of the world’s adolescents, and its Independent Accountability Panel will play a crucial role in catalysing these processes in the coming years.
Within countries, responsibility for adolescent health and wellbeing is similarly often dispersed across sectors and government ministries. This presents challenges in engagement of constituents, in setting priorities for investment, and around coordination of action. It also means that the provision of independent oversight has considerable complexity. The appointment of dedicated and independent Youth Commissioners at levels from the national to the local would be one way forward. Various countries already have national Child Rights Commissioners who generally have a focus on implementation of international or national legislation designed to protect the rights of disadvantaged children.366 In many instances, this protective role extends to younger adolescents. Under a Youth Commissioner, that role would extend to the protection and empowerment of older adolescents and young adults. It would also include oversight of other elements in the accountability process: provision and communication of sound information, engagement of youth as active partners, and review of relevant policy implementation and service delivery systems. A National Youth Commission would require clear lines of engagement with the appropriate level of government and the ability to communicate with other relevant organisations, including international agencies and NGOs. A capacity to convene forums of constituents would be particularly important where the most effective actions for adolescent health and well-being may sit uncomfortably with local cultural and religious traditions. Youth Commissioners would therefore play both an essential role to hold government ministers to account, promote the empowerment of youth, and provide a point of engagement with other key constituents.
Establishing effective processes for accountability will ultimately allow us to invest more, invest more effi ciently, and innovate and evaluate where evidence does not currently exist. The current Commission has taken a step forward in providing a global overview of adolescent health and wellbeing. Moving forward requires an ongoing monitoring of progress. The SDG agenda and Global Strategy for Women’s, Children’s and Adolescents’ Health both emphasise a need for clarity around indicators and improvement in health information systems. Yet even with major investments now, a comprehensive global coverage of adolescent health and wellbeing remains years away. In this context we have proposed an interim set of twelve global indicators (table 6), that draw on this Commission’s conceptual framework (figure 6), and reflect measures used in this report. In each instance they can now be populated for most countries and with modest investment, estimates could be available for nearly all countries in the near future. With the largest generation of adolescents in human history facing unprecedented global change, keeping track and responding to their health and wellbeing is an essential investment in all our futures.
Table 6.
Indicators of adolescent health status, risks, and determinants with wide coverage and achievable targets for 2030
| Headline indicators | Stratification | 2030 targets | |
|---|---|---|---|
|
Social and structural determinants
| |||
| Extend secondary education completion | Completion of 12 or more years of education in 20–24 year olds | Female or male Rural or urban Bottom wealth quintile or top wealth quintile |
80% completion† |
| Reduce adolescent births | Birth rate per 1000 10–19-year-old girls per year | Female or male, married or unmarried Rural or urban Bottom wealth quintile or top wealth quintile |
Under 25 births per 1000 10–19-year-old girls per year* |
| Reduce early marriage | Marriage before 18 years in women aged 20–24 years | Rural or urban Bottom wealth quintile or top wealth quintile |
Under 10%* |
| Responsive health services367 | 15–24 year olds with met needs for modern contraception | Age band, married or unmarried Rural or urban Bottom wealth quintile or top wealth quintile |
80% met need |
| Reduce educational and employment marginalisation | Not in employment, education or training rates in 20–24 year olds | Female or male Rural or urban Bottom wealth quintile or top wealth quintile |
Under 10%* |
|
Health risks | |||
| Reduce tobacco use | Daily smoking in 10–24 year olds | Female or male Rural or urban Bottom wealth quintile or top wealth quintile |
Under 10%* |
| Reduce risky alcohol use | Binge drinking (>60 gm) in 15–19 year olds in past 30 days | Female or male Rural or urban Bottom wealth quintile or top wealth quintile† |
Under 10%* |
| Reduce overweight and obesity | Percentage of 10–24 year olds exceeding WHO guidelines for overweight | Female or male Rural or urban Bottom wealth quintile or top wealth quintile |
Under 20%* |
| Reduce undernutrition | Prevalence of iron deficiency anaemia in 10–24 year olds | Female or male Rural or urban Bottom wealth quintile or top wealth quintile |
Under 10%* |
|
Burden of disease | |||
| Reduce diseases of poverty | DALY estimates of diseases of poverty in 10–24 year olds | Female or male Rural or urban Bottom wealth quintile or top wealth quintile |
No country remains multi-burden by 2030 |
| Reduce injury and violence | DALY estimates due to unintentional injury and violence | Female or male Rural or urban Bottom wealth quintile or top wealth quintile |
No current country remains in the injury excess category by 2030 |
| Reduce non-communicable diseases (including mental disorders) | DALY estimates due to non-communicable diseases | Female or male Rural or urban Bottom wealth quintile or top wealth quintile |
Under 1500 DALYs from non-communicable diseases per 100 000 10–24 year olds per year* |
DALY=disability-adjusted life-years.
Based on convergence to best countries in 2015.
Stratification not available.
Responses and recommendations
Despite making up around a third of the population in many countries, adolescents and young adults are generally overlooked in health and social policies. The neglect has resulted in limited service development, and low human and technical capacities. Major investments are now needed to take advantage of the opportunities that come with the largest generation of adolescents in human history. The UN Secretary-General’s Global Strategy for Women’s, Children’s and Adolescents’ Health is an important starting point. Moving forward, investments in adolescents should reflect their numbers in the population and the opportunity to create health, wellbeing, and human capital. Here, we outline our recommendations for specific actions and investment.
Reframe adolescent health and wellbeing
There is a need for all constituencies to reconsider adolescent health and wellbeing and its place in policy. We need the following:
A broader concept of adolescent health
Such a concept starts with a comprehensive view of sexual and reproductive health and extends to include HIV and other infectious diseases, nutritional deficiencies, injury and violence, chronic physical health problems, and mental and substance use disorders, to ensure that adolescents are centrally placed in relevant and emerging agendas for NCDs, mental health, and maternal, newborn, and child health.
An appreciation of the triple dividend of investment in adolescents
Puberty initiates a second sensitive period in the development of health and human capabilities. Appropriate investments bring benefits during adolescence, across the life course, and into the next generation.
The development of policies sensitive to gender and evolving adolescent capacities
Understanding of the powerful interactions between biological development and social context is essential in formulating policies, laws, and programmes for adolescents.
An understanding of adolescence as a time for second chances
Providing optimal social, emotional, and nutritional environments in adolescence has the potential to reverse or reduce early-life disadvantage. Policies that target inequities related to poverty and gender during adolescence have the potential to reduce inequality across the life course and into the next generation.
Set clear objectives based on national and local needs
Different actions are needed in different places.
Multi-burden countries
No country should remain in the multi-burden group by 2030. Infectious diseases including HIV, sexual and reproductive health, and undernutrition remain preventable and treatable causes of disease burden that should be priorities for health service delivery and prevention. Policy measures to address injuries are also now essential in this group of countries.
Injury excess countries
All current injury excess countries should have NCD predominant profiles by 2030. For these countries, preventive efforts targeting the social and structural determinants of injuries, violence, and high rates of early pregnancy are priorities.
NCD predominant countries
The great variation in the pattern and level of adolescent NCD burden across all countries indicates great scope for accelerating investments in the treatment and prevention of adolescent NCDs and NCD risks.
A view to the future
All country groups must now tackle accelerating adolescent risks for NCDs to ensure that diseases of poverty and injury are not replaced by an unaffordable burden of later-life non-communicable diseases. All countries should identify and adopt international best practice (eg, tobacco and alcohol control, and taxation of unhealthy food) as well as evaluate promising new interventions for adolescent NCD risks.
Including socially and economically marginalised adolescents
Within all countries these groups, including ethnic minorities, young offenders, Indigenous, and LGBT adolescents, need particular responses reflecting their poorer health profiles and greater difficulty accessing resources for health and wellbeing.
Reconfigure health services for universal health coverage
Achieving universal health coverage for adolescents will require delivery platforms beyond traditional office-based health-care systems. These are likely to extend to school-based and community-based platform delivery models as well as the use of social and digital media. Services will need to embrace:
Breadth of coverage
Adolescents need services that extend beyond sexual and reproductive health care to all major health problems, including infectious diseases, mental disorders, and chronic physical illness regardless of gender, age, sexual orientation, marital, or socioeconomic status.
Effective early intervention
Early and effective treatment is essential for health problems that commonly emerge or have a particular significance for adolescents including HIV and other infectious diseases, nutritional deficiencies, and mental and substance use disorders.
Accessible preventive health care
Care should include guarantees of preventive care to all sexually active adolescents, maternal health care when necessary, and access to affordable modern contraception, particularly long-acting reversible contraceptives; if unwanted pregnancy does occur provide access to legal, safe abortion.
Training of health-care providers
It is essential that health-care professionals have the necessary knowledge, attitudes, and interpersonal skills to provide confidential, non-judgmental, and respectful health care to adolescents.
Create protective and empowering social scaffolds through intersectoral partnerships
The most effective actions for adolescent health and wellbeing lie in sectors beyond health service provision. Moreover, alignment of health service responses with preventive and promotional actions in other sectors is necessary for health service effectiveness. Essential investments by other sectors include:
Resources to complete quality secondary education
Access to free, quality secondary education regardless of sex, marital, and socioeconomic status should be guaranteed and should extend to reducing family financial barriers to quality education.
School as a setting for promoting health and wellbeing
Schools should employ a range of available strategies including the delivery of life skills for health and wellbeing, comprehensive sexuality education, and support of a positive school ethos.
Training of teachers and other professionals
Pre-service and in-service training for teachers and other professionals working with adolescents must be provided, including police and community workers, around empowering adolescents to make the best possible decisions about their health and wellbeing.
Laws that empower and protect
Governments must ensure that national and international legal frameworks designed to empower and protect adolescents actually do their intended purpose. Guaranteeing 18 years as the minimum age for marriage, for example, requires education and engagement of community leaders and professionals within the justice system.
Policy linkage
Individual elements of social scaffold for adolescent health and wellbeing include access to safe employment and education, universal health coverage, supported families and parents, opportunities for community engagement, and taxation and regulation of the marketing of unhealthy commodities to adolescents. Linkage of these single sector actions will create synergies for adolescent health and wellbeing, with effects greater than the sum of the parts.
Enhance the engagement of young people
Adolescence is intrinsically a time of extending social engagement beyond the family. Given the opportunity, adolescents and young adults are powerful agents for social change, including the promotion of their own health and wellbeing. The growing complexity of political and economic systems presents barriers to their engagement. New structures and processes are therefore needed, which include the following:
Training and mentoring of adolescents
Access to training, mentorship, and resources is essential for adolescents to play an effective role in governance and accountability processes around their health and wellbeing.
Establishment of forums for meaningful youth participation
National leaders should appoint Independent Youth Commissioners with appropriate resourcees to provide independent oversight of government actions to promote adolescent health and wellbeing. The Youth Commissioners should convene forums that bring together all constituents including adolescents and young adults, their families and community leaders, adolescent-focused organisations, international development partners, professionals groups, and academics. Such forums should extend to establishing and strengthening mechanisms for the meaningful participation of adolescents in the design, communication, and implementation and monitoring of policies and practices that affect their health and wellbeing. This is particularly important for socially and economically marginalised adolescents.
Growing knowledge and capacity
Long-standing neglect of adolescent and young adult health has left limited capacity with sectors and across service systems. There is a pressing need for investment in research, training, financing, and technical underpinnings, or progress in adolescent health and wellbeing will remain slow. Essential next steps include:
Creation of national profiles
Governments must work with international development partners, including funders and global data collection systems, to collect and report on a minimum set of priority indicators of adolescent health and wellbeing. National statistics agencies should report regularly on the health, development, and wellbeing of adolescents, disaggregated by age and sex, and ensure that this information is easily accessible to constituents. International data collection systems should be resourced to collect and report on data disaggregated by age and sex on all relevant global indicators of health and wellbeing for all adolescents, including those who are out of school and socially and economically marginalised.
Addressing knowledge gaps for effective actions
New approaches are particularly needed in the prevention and early intervention of mental disorders and violence. In general, there is a need to better understand what works for males and females, for different age groups of adolescents and for socially marginalised groups. The international development community and national governments must work together to create a more comprehensive evidence base for action in practice and policy.
Moving to scalable and sustainable action
The Global Strategy for Women’s, Children’s and Adolescents’ Health presents an outstanding opportunity for multi-burden countries to create the policy and legal frameworks, efficient systems, trained workforce, and technical capacity for adolescent health and wellbeing. Similar investments are needed in all countries.
Acknowledgments
The Bill & Melinda Gates Foundation (Seattle, WA, USA) provided a grant to assist with the production of the Commission. Additional funding came from the John D and Catherine T MacArthur Foundation, Australia India Institute, and the Murdoch Childrens Research Institute. The University of Melbourne, University College London, the London School of Hygiene & Tropical Medicine, and Columbia University provided financial or logistic support. All Commissioners were supported by their employing organisations to undertake the Commission’s work. The findings and recommendations are those of the authors and do not necessarily reflect recommendations or policies of the funders. Overall project Secretariat was provided by Molly O’Sullivan (MCRI), Kristina Bennett (MCRI), and Jennifer Heitel (Columbia). A very special thank you goes to all the research assistants from the five working groups who assisted with the conceptualisation, literature screening, data extraction, and synthesis of evidence. These include Dr Bidyut K Sarkar (UCL/PHFI), Dr Soumyadeep Bhaumik, Dr Kiran Saluja (PHFI), Kate Hinds (UCL), Kelly Dickson (UCL), Dr Farah Jamal (UCL), and Dr Nichola Shackleton (UCL) from Project 1. Sonia Haerizadeh JD (Columbia University), Dr Elia De la Cruz Toledo (Columbia University), and Dr Nathan Hughes (University of Birmingham) from Project 2. Dr Lydia K Murithi (ICRW), Preeti Dhillon (ICRW), Lilian Ghandour (AUB), Chaza Akik (AUB), Dr Elie Akl (AUB), Mariana Yaafar Jaafar (AUB), Noura El Salibi (AUB), Hala Najm (AUB), Tamara Lotfi (AUB), Jillian Grisel, and Caroline Zahm from Project 3. Donna Lorenze (MCRI), Dr Alana Deery (MCRI), Tim Gartland (MCRI), Liz Comrie-Thomson (Burnet Institute), Dr Jo Robinson (Orygen), Eric Howard (Whiting Moyne), Stephen Hearps (MCRI), Annie Haakenstad (Harvard School of Public Health), and Kara Estep (IHME) from Project 4, without whose hard work this report would not have been possible. Additional administrative support provided by Charmaine Sambathkumar, Dr Michelle Tollit (MCRI), Dr Anne-Lise Goddings (UCL) Jenelle Frances, Mary Boyle, Monica Chase, Stephanie Grilo, and Chelsea Kolff (Columbia University). Website and graphic support was provided by Adam Leadoux and Bill Reid (RCH). The authors also thank the peer reviewers who provided important feedback on earlier drafts of the report.
Footnotes
Contributors
The 2016 Lancet Commission on Adolescent Health and Wellbeing has been an international collaboration led by the University of Melbourne, Columbia University, London School of Hygiene & Tropical Medicine, and University College London. GCP, SMS, JSS, RMV, and DAR were the institutional leads who established the Commission.
The Commission undertook its work within five central working groups, which were responsible for the design, drafting, and review of their individual sections. All Commissioners (GCP, SMS, JSS, DAR, RMV, RA, NBA, WB, CB, ZB, CB, JD, AOF, JF, RK, JM, AM, TM, AHM, VP, SP, FS, KT, JW, DW) contributed to the overall report structure and concepts. PA, EK, MA, and NR were responsible for specific elements of the work-plan and contributed more broadly to their integration in the report. All authors had a role in reviewing the manuscript.
Declaration of interests
All authors declare that the work of the Commission on Adolescent Health and Wellbeing was supported by the Bill & Melinda Gates Foundation (Seattle, WA, USA), MacArthur Foundation (Chicago, IL, USA), Australia India Institute (Melbourne, VIC, Australia), and the Murdoch Childrens Research Institute (Melbourne, VIC, Australia). The funding covered travel, accommodation, and meals for the Commission meetings, as well as development of background papers, project management and research assistant time. 12 authors reported grants from either the Bill & Melinda Gates Foundation, MacArthur Foundation, or the University of Melbourne, during the conduct of the study. RA received personal fees from UNDP, outside the submitted work. SMS is a member of WHO’s Technical Advisory Committee for the Department of Maternal, Newborn, Child and Adolescent Health.
See Online for appendix
For more on the MTV Staying Alive Ignite campaign, see http://ignite.staying-alive.org/kenya
References
- 1.Lamy P, Bachelet M, Barber L, et al. Now for the long term: the report of the Oxford Martin commission for future generations. Oxford: Oxford Martin School; 2013. [Google Scholar]
- 2.Whitmee S, Haines A, Beyrer C, et al. The Rockefeller Foundation–Lancet Commission on planetary health. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation–Lancet Commission on planetary health. Lancet. 2015;386:1973–2028. doi: 10.1016/S0140-6736(15)60901-1. [DOI] [PubMed] [Google Scholar]
- 3.Blakemore SJ, Mills KL. Is adolescence a sensitive period for sociocultural processing? Annu Rev Psychol. 2014;65:187–207. doi: 10.1146/annurev-psych-010213-115202. [DOI] [PubMed] [Google Scholar]
- 4.United Nations Secretary-General. The global strategy for women’s, children’s and adolescentss health (2016–2030): survive thrive transform. 2015 http://www.who.int/life-course/partners/global-strategy/globalstrategyreport2016-2030-lowres.pdf?ua=1 (accessed April 3, 2016)
- 5.UN. Transforming our world: the 2030 agenda for sustainable development. New York: United Nations; 2015. [Google Scholar]
- 6.Resnick MD, Catalano RF, Sawyer SM, Viner R, Patton GC. Seizing the opportunities of adolescent health. Lancet. 2012;379:1564–67. doi: 10.1016/S0140-6736(12)60472-3. [DOI] [PubMed] [Google Scholar]
- 7.Feldman SS, Elliot GR. At the threshold: the developing adolescent. Cambridge, MA: Harvard University Press; 1990. [Google Scholar]
- 8.WHO. The Second Decade: Improving Adolescent Health and Development. Geneva: World Health Organization; 2001. [Google Scholar]
- 9.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–80. [PubMed] [Google Scholar]
- 10.United Nations General Assembly. (United Nations Treaty Series vol 1577).Convention on the rights of the child. 1989 [Google Scholar]
- 11.Sen A. Commodities and capabilities. New Delhi: Oxford University Press; 1999. [Google Scholar]
- 12.Nussbaum MC. Creating capabilities. Harvard University Press; 2011. [Google Scholar]
- 13.Graham P. The end of adolescence. New York: Oxford University Press; 2004. [Google Scholar]
- 14.Dick B, Ferguson BJ. Health for the world’s adolescents: a second chance in the second decade. J Adolesc Health. 2015;56:3–6. doi: 10.1016/j.jadohealth.2014.10.260. [DOI] [PubMed] [Google Scholar]
- 15.Viner R, Coffey C, Mather C, et al. 50-year mortality trends in children and young people: a study of 50 low-income, middle-income, and high-income countries. Lancet. 2011;377:1162–74. doi: 10.1016/S0140-6736(11)60106-2. [DOI] [PubMed] [Google Scholar]
- 16.World Bank. World Development Report 2007: Development and the next generation. Washington, DC: World Bank; 2007. [Google Scholar]
- 17.Dishion TJ, Nelson SE, Bullock BM. Premature adolescent autonomy: Parent disengagement and deviant peer process in the amplification of problem behaviour. J Adolesc. 2004;27:515–30. doi: 10.1016/j.adolescence.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 18.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. Lancet. 2012;379:1630–40. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 19.Grossman M. On the concept of health capital and the demand for health. J Polit Econ. 1972:223–55. [Google Scholar]
- 20.Rockwood K, Song X, Mitnitski A. Changes in relative fitness and frailty across the adult lifespan: evidence from the Canadian National Population Health Survey. Can Med Assoc J. 2011;183:E487–E94. doi: 10.1503/cmaj.101271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruiz JR, Castro-Piñero J, Artero EG, et al. Predictive validity of health-related fitness in youth: a systematic review. Br J Sports Med. 2009;43:909–23. doi: 10.1136/bjsm.2008.056499. [DOI] [PubMed] [Google Scholar]
- 22.Baxter-Jones AD, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res. 2011;26:1729–39. doi: 10.1002/jbmr.412. [DOI] [PubMed] [Google Scholar]
- 23.Whiting SJ, Vatanparast H, Baxter-Jones A, Faulkner RA, Mirwald R, Bailey DA. Factors that affect bone mineral accrual in the adolescent growth spurt. J Nutr. 2004;134:696S–700S. doi: 10.1093/jn/134.3.696S. [DOI] [PubMed] [Google Scholar]
- 24.Julián-Almárcegui C, Gómez-Cabello A, Huybrechts I, et al. Combined effects of interaction between physical activity and nutrition on bone health in children and adolescents: a systematic review. Nutr Rev. 2015;73:127–39. doi: 10.1093/nutrit/nuu065. [DOI] [PubMed] [Google Scholar]
- 25.Sisk CL, Foster DL. The neural basis of puberty and adolescence. Nat Neurosci. 2004;7:104–47. doi: 10.1038/nn1326. [DOI] [PubMed] [Google Scholar]
- 26.Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24:417–63. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- 27.Steinberg L. A social neuroscience perspective on adolescent risk-taking. Dev Rev. 2008;28:78–106. doi: 10.1016/j.dr.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crone EA, Dahl RE. Understanding adolescence as a period of social-affective engagement and goal flexibility. Nat Rev Neurosci. 2012;13:636–50. doi: 10.1038/nrn3313. [DOI] [PubMed] [Google Scholar]
- 29.Baker ST, Lubman DI, Yucel M, et al. Developmental changes in brain network hub connectivity in late adolescence. J Neurosci. 2015;35:9078–87. doi: 10.1523/JNEUROSCI.5043-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Giedd JN, Lalonde FM, Celano MJ, et al. Anatomical brain magnetic resonance imaging of typically developing children and adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48:465–70. doi: 10.1097/CHI.0b013e31819f2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giedd JN, Blumenthal J, Jeffries NO, et al. Brain development during childhood and adolescence: a longitudinal MRI study. Nat Neurosci. 1999;2:861–63. doi: 10.1038/13158. [DOI] [PubMed] [Google Scholar]
- 32.Tanner JL, Arnett JJ. Presenting “emerging adulthood”: what makes it developmentally distinctive? In: Arnett JJ, Kloep M, Hendry LB, Tanner JL, editors. Debating emerging adulthood: stage or process. Oxford: Oxford Scholarship Online; 2011. pp. 13–30. [Google Scholar]
- 33.Sawhill IV. Generation unbound. Washington, DC: Brookings Institution Press; 2014. [Google Scholar]
- 34.Prentice AM, Ward KA, Goldberg GR, et al. Critical windows for nutritional interventions against stunting. Am J Clin Nutr. 2013;97:911–18. doi: 10.3945/ajcn.112.052332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li S-C, Lindenberger U, Hommel B, Aschersleben G, Prinz W, Baltes PB. Transformations in the couplings among intellectual abilities and constituent cognitive processes across the life span. Psychol Sci. 2004;15:155–63. doi: 10.1111/j.0956-7976.2004.01503003.x. [DOI] [PubMed] [Google Scholar]
- 36.Richards M, Deary IJ. A life course approach to cognitive reserve: a model for cognitive aging and development? Ann Neurol. 2005;58:617–22. doi: 10.1002/ana.20637. [DOI] [PubMed] [Google Scholar]
- 37.Gottfredson LS, Deary IJ. Intelligence predicts health and longevity, but why? Curr Dir Psychol Sci. 2004;13:1–4. [Google Scholar]
- 38.Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability. Am J Psychiatry. 2014 doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martins A, Ramalho N, Morin E. A comprehensive meta-analysis of the relationship between emotional intelligence and health. Pers Individ Dif. 2010;49:554–64. [Google Scholar]
- 40.Engström L-M. Who is physically active? Cultural capital and sports participation from adolescence to middle age—a 38-year follow-up study. Phys Educ Sport Pedag. 2008;13:319–43. [Google Scholar]
- 41.Macleod CI, Tracey T. A decade later: follow-up review of South African research on the consequences of and contributory factors in teen-aged pregnancy. S Afr J Psychol. 2010;40:18–31. [Google Scholar]
- 42.Rosema S, Crowe L, Anderson V. Social function in children and adolescents after traumatic brain injury: A systematic review 1989–2011. J Neurotrauma. 2012;29:1277–91. doi: 10.1089/neu.2011.2144. [DOI] [PubMed] [Google Scholar]
- 43.Saydah S, Bullard KM, Imperatore G, Geiss L, Gregg EW. Cardiometabolic risk factors among US adolescents and young adults and risk of early mortality. Pediatrics. 2013;131:e679–86. doi: 10.1542/peds.2012-2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Patton GC, Coffey C, Romaniuk H, et al. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. Lancet. 2014;383:1404–11. doi: 10.1016/S0140-6736(13)62116-9. [DOI] [PubMed] [Google Scholar]
- 45.Behrendt S, Wittchen H-U, Höfler M, Lieb R, Beesdo K. Transitions from first substance use to substance use disorders in adolescence: is early onset associated with a rapid escalation? Drug Alcohol Depend. 2009;99:68–78. doi: 10.1016/j.drugalcdep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 46.Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;109:E2657–64. doi: 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mason E, McDougall L, Lawn JE, et al. From evidence to action to deliver a healthy start for the next generation. Lancet. 2014;384:455–67. doi: 10.1016/S0140-6736(14)60750-9. [DOI] [PubMed] [Google Scholar]
- 48.Draper CE, Micklesfield LK, Kahn K, et al. Application of intervention mapping to develop a community-based health promotion pre-pregnancy intervention for adolescent girls in rural South Africa: Project Ntshembo (Hope) BMC Public Health. 2014;14(suppl 2):S5. doi: 10.1186/1471-2458-14-S2-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Patton GC, Romaniuk H, Spry E, et al. Prediction of perinatal depression from adolescence and before conception (VIHCS): 20-year prospective cohort study. Lancet. 2015;386:875–83. doi: 10.1016/S0140-6736(14)62248-0. [DOI] [PubMed] [Google Scholar]
- 50.Smith GD. Epigenesis for epidemiologists: does evo-devo have implications for population health research and practice? Int J Epidemiol. 2012;41:236–47. doi: 10.1093/ije/dys016. [DOI] [PubMed] [Google Scholar]
- 51.Hanson M, Gluckman P. Developmental origins of health and disease–Global public health implications. Best Pract Res Clin Obstet Gynaecol. 2015;29:24–31. doi: 10.1016/j.bpobgyn.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 52.Murray CJ, Barber RM, Foreman KJ, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;10009:2145–91. doi: 10.1016/S0140-6736(15)61340-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci. 2008;31:183–91. doi: 10.1016/j.tins.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 54.Goddings A. Doctoral thesis. University College London; 2015. The impact of puberty on adolescent brain development. [Google Scholar]
- 55.Viner RM, Ozer EM, Denny S, et al. Adolescence and the social determinants of health. Lancet. 2012;379:1641–52. doi: 10.1016/S0140-6736(12)60149-4. [DOI] [PubMed] [Google Scholar]
- 56.Schlegel A, Barry H. Adolescence: an anthropological enquiry. New York: Free Press; 1991. [Google Scholar]
- 57.Somerville LH. The teenage brain sensitivity to social evaluation. Curr Dir Psychol Sci. 2013;22:121–27. doi: 10.1177/0963721413476512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pfeifer JH, Masten CL, Moore WE, et al. Entering adolescence: resistance to peer influence, risky behavior, and neural changes in emotion reactivity. Neuron. 2011;69:1029–36. doi: 10.1016/j.neuron.2011.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brown B. Adolescents’ relationships with peers In: Lerner R, Steinberg L, eds Handbook of Adolescent Psychology. New York: Wiley; 2004. [Google Scholar]
- 60.Steinberg L, Monahan KC. Age differences in resistance to peer influence. Dev Psychol. 2007;43:1531–43. doi: 10.1037/0012-1649.43.6.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brown JD, Halpern CT, L’Engle KL. Mass media as a sexual super peer for early maturing girls. J Adolesc Health. 2006;36:420–27. doi: 10.1016/j.jadohealth.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 62.Lou C, Cheng Y, Gao E, Zuo X, Emerson MR, Zabin LS. Media’s contribution to sexual knowledge, attitudes, and behaviors for adolescents and young adults in three Asian cities. J Adolesc Health. 2012;50:S26–36. doi: 10.1016/j.jadohealth.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Teens and Technology 2013. Washington, DC: Pew Research Center; 2014. [Google Scholar]
- 64.Morin-Major JK, Marin M-F, Durand N, Wan N, Juster R-P, Lupien SJ. Facebook behaviors associated with diurnal cortisol in adolescents: Is befriending stressful? Psychoneuroendocrinology. 2016;63:238–46. doi: 10.1016/j.psyneuen.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 65.Starcevic V, Aboujaoude E. Cyberchondria, cyberbullying, cybersuicide, cybersex:“new” psychopathologies for the 21st century? World Psychiatry. 2015;14:97–100. doi: 10.1002/wps.20195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Saltman EM, Smith M. Till martyrdom do us part. London: Institute for Strategic Dialogue; 2015. [Google Scholar]
- 67.Joshi PD, Fast NJ. Power and reduced temporal discounting. Psychol Sci. 2013;24:432–38. doi: 10.1177/0956797612457950. [DOI] [PubMed] [Google Scholar]
- 68.Binder M, Lades LK. Autonomy-enhancing paternalism. Kyklos. 2015;68:3–27. [Google Scholar]
- 69.Global Health Data Exchange. 2013 http://ghdx.healthdata.org/global-burden-disease-study-2013-gbd-2013-data-downloads (accessed April 3, 2016)
- 70.UNFPA. State of the World’s Population. The power of 1·8 billion-adolescents, youth, and the transformation of the future. http://www.unfpa.org/swop (accessed April 3, 2016)
- 71.Bloom DE. Youth in the balance. Finance Dev. 2012;49:7–11. [Google Scholar]
- 72.Song Y, Ma J, Agardh A, Lau PW, Hu P, Zhang B. Secular trends in age at menarche among Chinese girls from 24 ethnic minorities, 1985 to 2010. Glob Health Action. 2015;8:26929. doi: 10.3402/gha.v8.26929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.National Research Council and Institute of Medicine. Growing up global: the changing transitions to adulthood in developing countries. In: Lloyd CB, editor. Panel on transitions to adulthood in developing countries. Washington, DC: The National Academies Press; 2005. [Google Scholar]
- 74.Eisenberg ME, Spry E, Patton GC. From emerging to established: longitudinal patterns in the timing of transition events among australian emerging adults. Emerg Adulthood. 2015;3:277–281. [Google Scholar]
- 75.Bajos N, Bozon M, Beltzer N, et al. Changes in sexual behaviours: from secular trends to public health policies. AIDS. 2010;24:1185. doi: 10.1097/QAD.0b013e328336ad52. [DOI] [PubMed] [Google Scholar]
- 76.Ybarra ML, Mitchell KJ. “Sexting” and its relation to sexual activity and sexual risk behavior in a national survey of adolescents. J Adolesc Health. 2014;55:757–64. doi: 10.1016/j.jadohealth.2014.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Staff J, Schulenberg JE, Maslowsky J, et al. Substance use changes and social role transitions: proximal developmental effects on ongoing trajectories from late adolescence through early adulthood. Dev Psychopathol. 2010;22:917–32. doi: 10.1017/S0954579410000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Santhya K. Early marriage and sexual and reproductive health vulnerabilities of young women: a synthesis of recent evidence from developing countries. Curr Opin Obstet Gynecol. 2011;23:334–39. doi: 10.1097/GCO.0b013e32834a93d2. [DOI] [PubMed] [Google Scholar]
- 79.Meng Y, Holmes J, Hill-McManus D, Brennan A, Meier PS. Trend analysis and modelling of gender-specific age, period and birth cohort effects on alcohol abstention and consumption level for drinkers in Great Britain using the General Lifestyle Survey 1984–2009. Addiction. 2014;109:206–15. doi: 10.1111/add.12330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.World Bank. World Development Report 2014: Risk and opportunity: managing risk for development. Washington, DC: World Bank; 2013. [Google Scholar]
- 81.Furlong A, Cartmel F. Young people and social change: individualisation and risk in late modernity. Buckingham: Open University Press; 1997. [Google Scholar]
- 82.Bottino SMB, Bottino C, Regina CG, Correia AVL, Ribeiro WS. Cyberbullying and adolescent mental health: systematic review. Cad Saude Publica. 2015;31:463–75. doi: 10.1590/0102-311x00036114. [DOI] [PubMed] [Google Scholar]
- 83.Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014;18:75–87. doi: 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 84.Institute of Medicine (IOM) and National Research Council (NRC) of the National Academies. Toward and integrated science of research on families: workshop report. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 85.Elzakkers IF, Danner UN, Hoek HW, Schmidt U, van Elburg AA. Compulsory treatment in anorexia nervosa: a review. Int J Eat Disord. 2014;47:845–52. doi: 10.1002/eat.22330. [DOI] [PubMed] [Google Scholar]
- 86.UN DESA. World Marriage Patterns. New York: United Nations Department of Economic and Social Affairs (UN DESA) Population Division; 2011. [Google Scholar]
- 87.Euromonitor International. Special Report: The family structure of the future. 2013 http://blog.euromonitor.com/2013/07/special-report-the-family-structure-of-the-future.html (accessed Aug 12, 2015)
- 88.Dhillon N, Yousef T. Generation in waiting: The unfulfilled promise of young people in the Middle East. Washington, DC: Brookings Institution Press; 2009. [Google Scholar]
- 89.Snoubar Y, Hawal HH. Young communities and the impact of wars and conflicts on the healthy growth of young people: Middle East as a model study. EJIS. 1:129–36. [Google Scholar]
- 90.Boampong M. Adolescents and youth migration: harnessing the development potential while mitigating risk. 2011 http://www.voicesofyouth.org/posts/adolescents-and-youth-migration-harnessing-the-development-potential-while-mitigating-risk–2 (accessed Aug 21, 2015)
- 91.Cortés R. Adolescents’ rights, gender and migration: challenges for policy makers. 2011 http://www.globalmigrationgroup.org/sites/default/files/uploads/gmg-topics/mig-data/Adolescents-Rights-Gender-Migration-Final-Report-April-2011.pdf (accessed April 3, 2016)
- 92.OECD. The future of families to 2030: A synthesis report. Paris: Organisation for Economic Co-operation and Development; 2011. [Google Scholar]
- 93.Harris KM, Lee H, DeLeone FY. Marriage and health in the transition to adulthood: evidence for African Americans in the Add Health Study. J Fam Issues. 2010;31:1106–43. doi: 10.1177/0192513X10365823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Larson RW, Richards MH, Moneta G, Holmbeck G, Duckett E. Changes in adolescents’ daily interactions with their families from ages 10 to 18: disengagement and transformation. Dev Psychol. 1996;32:744. [Google Scholar]
- 95.Schwartz OS, Byrne ML, Simmons JG, et al. Parenting during early adolescence and adolescent-onset major depression—a 6-year prospective longitudinal study. Clin Psychol Sci. 2014;2:272–86. [Google Scholar]
- 96.Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Soc Dev. 2007;16:361–88. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360:1083–88. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 98.Garcia-Moreno C, Guedes A, Knerr W. Female Genital Mutilation: Understanding and addressing violence against women. Geneva: WHO; 2012. [Google Scholar]
- 99.Volpe JS. Effects of domestic violence on children and adolescents: an overview. 1996 http://www.aaets.org/article8.htm (accessed Aug 21, 2015)
- 100.Commendador KA. Parental influences on adolescent decision making and contraceptive use. Pediatr Nurs. 2010;36:147–56, 70. [PubMed] [Google Scholar]
- 101.McPherson KE, Kerr S, McGee E, et al. The association between social capital and mental health and behavioural problems in children and adolescents: an integrative systematic review. BMC Psychol. 2014;2:7. doi: 10.1186/2050-7283-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pilgrim NA, Blum RW. Adolescent mental and physical health in the English-speaking Caribbean. Rev Panam Salud Publica. 2012;32:62–69. doi: 10.1590/s1020-49892012000700010. [DOI] [PubMed] [Google Scholar]
- 103.Bouris A, Guilamo-Ramos V, Pickard A, et al. A systematic review of parental influences on the health and well-being of lesbian, gay, and bisexual youth: time for a new public health research and practice agenda. J Prim Prev. 2010;31:273–309. doi: 10.1007/s10935-010-0229-1. [DOI] [PubMed] [Google Scholar]
- 104.Penman-Aguilar A, Carter M, Snead MC, Kourtis AP. Socioeconomic disadvantage as a social determinant of teen childbearing in the U.S. Public Health Rep. 2013;128:5–22. doi: 10.1177/00333549131282S102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cutler DM, Lleras-Muney A. Education and health: insights from international comparisons. Cambridge, MA, USA: National Bureau of Economic Research (NBER); 2012. [Google Scholar]
- 106.Miyamoto K, Chevalier A. Education and health. In: OECD, editor. Improving health and social cohesion through education. Paris: Organisation for Economic Co-operation and Development; 2010. pp. 111–79. [Google Scholar]
- 107.McQueston K, Silverman R, Glassman A. The efficacy of interventions to reduce adolescent childbearing in low- and middle-income countries: a systematic review. Stud Fam Plann. 2013;44:369–88. doi: 10.1111/j.1728-4465.2013.00365.x. [DOI] [PubMed] [Google Scholar]
- 108.Gakidou E, Cowling K, Lozano R, Murray CJ. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: a systematic analysis. Lancet. 2010;376:959–74. doi: 10.1016/S0140-6736(10)61257-3. [DOI] [PubMed] [Google Scholar]
- 109.WHO. Closing the gap in a generation: health equity through action on the social determinants of health. Geneva: World Health Organization; 2008. [DOI] [PubMed] [Google Scholar]
- 110.IHME. Global Educational Attainment 1970–2015. Seattle, USA: Institute for Health Metrics and Evaluation (IHME); 2015. [Google Scholar]
- 111.Foxcroft DR, Tsertsvadze A. Universal school-based prevention programs for alcohol misuse in young people. Cochrane Database Syst Rev. 2011;5:Cd009113. doi: 10.1002/14651858.CD009113. [DOI] [PubMed] [Google Scholar]
- 112.Patton G, Bond L, Butler H, Glover S. Changing schools, changing health? Design and implementation of the Gatehouse Project. J Adolesc Health. 2003;33:231–39. doi: 10.1016/s1054-139x(03)00204-0. [DOI] [PubMed] [Google Scholar]
- 113.Bonell C, Parry W, Wells H, et al. The effects of the school environment on student health: a systematic review of multi-level studies. Health Place. 2013;21:180–91. doi: 10.1016/j.healthplace.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 114.Fletcher A, Bonell C, Hargreaves J. School effects on young people’s drug use: a systematic review of intervention and observational studies. J Adolesc Health. 2008;42:209–20. doi: 10.1016/j.jadohealth.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 115.Johnson SL. Improving the school environment to reduce school violence: a review of the literature. J Sch Health. 2009;79:451–65. doi: 10.1111/j.1746-1561.2009.00435.x. [DOI] [PubMed] [Google Scholar]
- 116.Black WW, Fedewa AL, Gonzalez KA. Effects of “Safe School” programs and policies on the social climate for sexual-minority youth: a review of the literature. J LGBT Youth. 2012;9:321–39. [Google Scholar]
- 117.UNESCO. Educational for all 2000–2015: achievements and challenges. Paris: UNESCO; 2015. [Google Scholar]
- 118.UNICEF. Investment case for education and equity. New York: UNICEF; 2015. [Google Scholar]
- 119.Glewwe P, Kremer M. Schools,teachers, and education outcomes in developing countries. In: Hanushek E, Welch F, editors. Handbook of the economics of education. Oxford: Elsevier; 2006. pp. 945–1017. [Google Scholar]
- 120.UNESCO Institute for Statistics, UNICEF. Fixing the broken promise of education for all: finding for the global initiative on out-of-school children. Montreal: UNESCO Institute for Statistics; 2015. [Google Scholar]
- 121.Yasunaga M. Non-formal education as a means to meet learning needs of out-of-school children and adolescents. Montreal: UNESCO Institute for Statistics; 2014. [Google Scholar]
- 122.Rosenberg M, Pettifor A, Miller WC, et al. Relationship between school dropout and teen pregnancy among rural South African young women. Int J Epidemiol. 2015;44:928–36. doi: 10.1093/ije/dyv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Azevedo WF, Diniz MB, Fonseca ES, Azevedo LM, Evangelista CB. Complications in adolescent pregnancy: systematic review of the literature. Einstein (São Paulo) 2015;13:618–26. doi: 10.1590/S1679-45082015RW3127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.OECD. PISA 2012 Results in Focus: What 15-year-olds know and what they can do with what they know. Geneva: OECD Programme for International Student Assessment; 2012. [Google Scholar]
- 125.Demissie Z, Brener ND, McManus T, Shanklin SL, Hawkins J, Kann L. School Health Profiles 2012: Characteristics of Health Programs Among Secondary Schools. Atlanta, GA: Centers for Disease Control and Prevention (CDC); 2013. [Google Scholar]
- 126.Harlen W, Deakin Crick R. Testing and motivation for learning. Assess Educ. 2003;10:169–207. [Google Scholar]
- 127.Kneale D, Fletcher A, Wiggins R, Bonell C. Distribution and determinants of risk of teenage-motherhood in three British longitudinal studies: implications for targeted prevention interventions. J Epidemiol Community Health. 2013;67:4855. doi: 10.1136/jech-2011-200867. [DOI] [PubMed] [Google Scholar]
- 128.Bonell C, Fletcher A, Sorhaindo A, Wells H, McKee M. How market-oriented education policies might influence young people’s health: development of a logic model from qualitative case studies in English secondary schools. J Epidemiol Community Health. 2012;66:e24. doi: 10.1136/jech.2011.137539. [DOI] [PubMed] [Google Scholar]
- 129.Bonell C, Humphrey N, Fletcher A, Moore L, Anderson R, Campbell R. Why schools should promote students’ health and wellbeing Education policy shouldn’t focus solely on academic attainment. Br Med J. 2014;348:g3078. doi: 10.1136/bmj.g3078. [DOI] [PubMed] [Google Scholar]
- 130.International Labour Organization. World report on child labour 2015: paving the way to decent work for young people. Geneva: International Labour Organization; 2015. [Google Scholar]
- 131.International Labour Organization. Global employment trends for youth 2013: a generation at risk. Geneva: International Labour Office; 2013. [Google Scholar]
- 132.OECD. Youth neither in employment, education nor training (NEETs) Society at a Glance 2014: OECD Social Indicators. Paris: OECD Publishing; 2014. [Google Scholar]
- 133.Hale DR, Bevilacqua L, Viner RM. Adolescent health and adult education and employment: a systematic review. Pediatrics. 2015;136:128–40. doi: 10.1542/peds.2014-2105. [DOI] [PubMed] [Google Scholar]
- 134.Benjet C, Hernández-Montoya D, Borges G, Méndez E, Medina-Mora ME, Aguilar-Gaxiola S. Youth who neither study nor work: mental health, education and employment. Salud Publica Mex. 2012;54:410–17. doi: 10.1590/s0036-36342012000400011. [DOI] [PubMed] [Google Scholar]
- 135.Baggio S, Iglesias K, Deline S, et al. Not in education, employment, or training status among young swiss men. Longitudinal associations with mental health and substance use. J Adolesc Health. 2015;56:238–43. doi: 10.1016/j.jadohealth.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 136.Tomasik MJ, Pavlova MK, Lechner CM, Blumenthal A, Korner A. Changing contexts of youth development: An overview of recent social trends and a psychological model. New Dir Youth Dev. 2012;135:27–38. doi: 10.1002/yd.20026. [DOI] [PubMed] [Google Scholar]
- 137.Larson RW, Willson S, Brown RB, Furstenberg FF, Verma S. Changes in adolescent’s interpersonal experiences: are they being prepared for adult relationships in the twenty-first century. J Res Adolesc. 2002;12:31–68. [Google Scholar]
- 138.Jaccard J, Blanton H, Dodge T. Peer influences on risk behavior: an analysis of the effects of a close friend. Dev Psychol. 2005;41:135–47. doi: 10.1037/0012-1649.41.1.135. [DOI] [PubMed] [Google Scholar]
- 139.Salazar LF, Santelli JS, Crosby RA, DiClemente RJ. Chapter 15: Sexually transmitted disease transmission and pregnancy among adolescents. In: DiClemente RJ, Santelli JS, Crosby RA, editors. Adolescent health: understanding and preventing risk behaviors. San Francisco, CA: Jossey-Bass; 2009. pp. 274–302. [Google Scholar]
- 140.Fisher LB, Miles IW, Austin SB, Camargo CA, Jr, Colditz GA. Predictors of initiation of alcohol use among US adolescents: findings from a prospective cohort study. Arch Pediatr Adolesc Med. 2007;161:959–66. doi: 10.1001/archpedi.161.10.959. [DOI] [PubMed] [Google Scholar]
- 141.Kretman SE, Zimmerman MA, Morrel-Samuels S, Hudson D. Chapter 12: Adolescent violence: Risk, resilience, and prevention In: DiClemente RJ, Santelli JS, Crosby RA, eds Adolescent health: understanding and preventing risk behaviors. San Francisco, CA: Jossey-Bass; 2009. pp. 213–32. [Google Scholar]
- 142.Taffa N, Klepp KI, Sundby J, Bjune G. Psychosocial determinants of sexual activity and condom use intention among youth in Addis Ababa, Ethiopia. Int J STD AIDS. 2002;13:714–19. doi: 10.1258/095646202760326480. [DOI] [PubMed] [Google Scholar]
- 143.Strasburger VC, Jordan AB, Donnerstein E. Health effects of media on children and adolescents. Pediatrics. 2010;125:756–67. doi: 10.1542/peds.2009-2563. [DOI] [PubMed] [Google Scholar]
- 144.Jensen LA, Arnett JJ. Going global: new pathways for adolescents and emerging adults in a changing world. J Soc Issues. 2012;68:4730492. [Google Scholar]
- 145.Bell V, Bishop DV, Przybylski AK. The debate over digital technology and young people. BMJ. 2015;351:h3064. doi: 10.1136/bmj.h3064. [DOI] [PubMed] [Google Scholar]
- 146.Stuckler D, McKee M, Ebrahim S, Basu S. Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med. 2012;9:695. doi: 10.1371/journal.pmed.1001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Thow AM, Snowdon W, Labonté R, et al. Will the next generation of preferential trade and investment agreements undermine prevention of noncommunicable diseases? A prospective policy analysis of the Trans Pacific Partnership Agreement. Health Policy. 2015;119:88–96. doi: 10.1016/j.healthpol.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 148.Ellis SJ, Kitzinger C. Denying equality: An analysis of arguments against lowering the age of consent for sex between men. J Community Appl Soc Psychol. 2002;12:167–80. [Google Scholar]
- 148.Lansdown G. Innocenti insight: the evolving capacities of the child. 2005 http://www.unicef-irc.org/publications/pdf/evolving-eng.pdf. (accessed April 11, 2015)
- 150.Plan International and Special Representative of the UN Secretary-General on Violence against Children. Protecting children from harmful practices in plural legal systems. 2012 https://plan-international.org/files/global/publications/protection/protecting-children-from-harmful-practices-in-plural-legal-systems (accessed April 15, 2015)
- 151.Ngwena C. Sexual health and human rights in the African region. 2011 http://www.ichrp.org/files/papers/185/140_Ngwena_Africa_2011.pdf (accessed June 23, 2014)
- 152.WHO. Keeping promises, measuring results: commission on information and accountability for women’s and children’s health. Geneva: World Health Organization; 2011. [Google Scholar]
- 153.U.S. Agency for International Development (USAID) The roadmap for health measurement and accountability. Washington, DC: USAID, World Bank, WHO; 2015. [Google Scholar]
- 154.UNICEF. Child Marriage and the Law. 2008 http://www.unicef.org/policyanalysis/files/Child_Marriage_and_the_Law(1).pdf (accessed April 20, 2015)
- 155.UNICEF. State of the World’s Children. 2013 http://www.unicef.org/sowc2013/ (accessed April 20, 2015)
- 156.Klugman J, Hanmer L, Twigg S, Hasan T, McCleary-Sills J, Santamaria J. Voice and agency: empowering women and girls for shared prosperity. Washington, DC: World Bank Group; 2014. [Google Scholar]
- 157.Forum on Marriage and the Rights of Women and Girls. Early marriage: whose right to choose? 2001 https://www.crin.org/en/library/publications/early-marriage-whose-right-choose (accessed April 20, 2015)
- 158.International Institute for Population Sciences (IIPS) National Family Health Survey (NFHS-1), India 1992–93. Mumbai, India: IIPS; 1995. [Google Scholar]
- 159.International Institute for Population Sciences (IIPS), Macro International. National Family Health Survey (NFHS-3), 2005–06: India: Volume I. Mumbai, India: IIPS; 2007. [Google Scholar]
- 160.Jain S, Kurz K. New Insights on preventing child marriage: a global analysis of factors and programs. Washington, DC: ICRW; 2007. [Google Scholar]
- 161.International Institute for Population Sciences (IIPS) District level household and facility survey 2007–08 (DLHS-3) Mumbai, India: IIPS; 2010. [Google Scholar]
- 162.ICRW. Development Initiative on Supporting Healthy Adolescents (DISHA) project: Analysis of quantitative baseline survey data conducted in 2004. Washington, DC: International Center for Research on Women (ICRW); 2005. [Google Scholar]
- 163.iERG. Every Woman, Every Child: Strengthening Equity and Dignity through Health: the second report of the independent Expert Review Group (iERG) on Information and Accountability for Women’s and Children’s health. Geneva: World Health Organization; 2013. [Google Scholar]
- 164.DNA India. Cabinet approves bill on compulsory marriage registration. 2012 http://www.dnaindia.com/india/report-cabinet-approves-bill-on-compulsory-marriage-registration-1674966 (accessed July 22, 2014)
- 165.Tandon U. Family planning in India: a study of law and policy. 2010 http://paa2010.princeton.edu/papers/101217 (accessed April 2, 2015)
- 166.Bhamra AS, Nagrath K, Niazi Role of non-state actors in monitoring and review for effective implementation of the post-2015 agenda: IRF2015. 2015 [Google Scholar]
- 167.Parry CD, Patra J, Rehm J. Alcohol consumption and non-communicable diseases: epidemiology and policy implications. Addiction. 2011;106:1718–24. doi: 10.1111/j.1360-0443.2011.03605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.ICRW. Delaying marriage for girls in India: a formative research to design interventions for changing norms. New Delhi, India: UNICEF; 2011. [Google Scholar]
- 169.Van Duijvenvoorde A, Crone E. The teenage brain a neuroeconomic approach to adolescent decision making. Curr Dir Psychol Sci. 2013;22:108–13. [Google Scholar]
- 170.Biegler P. The ethical treatment of depression: autonomy through psychotherapy. Cambridge, MA: MIT Press; 2011. [Google Scholar]
- 171.Johnson SB, Jones VC. Adolescent development and risk of injury: using developmental science to improve interventions. Inj Prev. 2011;17:50–54. doi: 10.1136/ip.2010.028126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.DriversEd.com. Graduated Drivers License (GDL) https://www.driversed.com/dmv/california/gdl.aspx (accessed April 20, 2015)
- 173.Chen L-H, Baker SP, Li G. Graduated driver licensing programs and fatal crashes of 16-year-old drivers: a national evaluation. Pediatrics. 2006;118:56–62. doi: 10.1542/peds.2005-2281. [DOI] [PubMed] [Google Scholar]
- 174.Lyon JD, Pan R, Li J. National evaluation of the effect of graduated driver licensing laws on teenager fatality and injury crashes. J Saf Res. 2012;43:29–37. doi: 10.1016/j.jsr.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 175.Coffey C, Veit F, Wolfe R, Cini E, Patton GC. Mortality in young offenders: retrospective cohort study. BMJ. 2003;326:1064–66. doi: 10.1136/bmj.326.7398.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Muncie J. International juvenile (in) justice: penal severity and rights compliance. Int J Crime Justice Social Democracy. 2013;2:43–62. [Google Scholar]
- 177.Schwalbe CS, Gearing RE, MacKenzie MJ, Brewer KB, Ibrahim R. A meta-analysis of experimental studies of diversion programs for juvenile offenders. Clin Psychol Rev. 2012;32:26–33. doi: 10.1016/j.cpr.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 178.Asquith S. The Kilbrandon report Children and Young Persons Scotland. Edinburgh: HMSO; 1995. [Google Scholar]
- 179.Dünkel F, Pruin I. Young adult offenders in juvenile and criminal justice systems in Europe. In: Losel F, Bottoms A, Farrington DP, editors. Young adult offenders: lost in transition. Oxford: Routledge; 2012. pp. 11–39. [Google Scholar]
- 180.Blanc AK, Winfrey W, Ross J. New findings for maternal mortality age patterns: Aggregated results for 38 countries. PLoS One. 2013;8:e59864. doi: 10.1371/journal.pone.0059864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Patel V, Ramasundarahettige C, Vijayakumar L, et al. Suicide mortality in India: a nationally representative survey. Lancet. 2012;379:2343–51. doi: 10.1016/S0140-6736(12)60606-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Patton GC, Coffey C, Sawyer SM, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet. 2009;374:881–92. doi: 10.1016/S0140-6736(09)60741-8. [DOI] [PubMed] [Google Scholar]
- 183.Moser CO, Van Bronkhorst B. Youth violence in Latin America and the Caribbean: costs, causes, and interventions: World Bank, Latin America and the Caribbean Region, environmentally and socially sustainable development. SMU. 1999 [Google Scholar]
- 184.Rehm J, Sulkowska U, Mańczuk M, et al. Alcohol accounts for a high proportion of premature mortality in central and eastern Europe. Int J Epidemiol. 2007;36:458–67. doi: 10.1093/ije/dyl294. [DOI] [PubMed] [Google Scholar]
- 185.Yair O, Miodownik D. Youth bulge and civil war: Why a country’s share of young adults explains only non-ethnic wars. Conflict Manage Peace Sci. 2014;33:25–44. [Google Scholar]
- 186.Collishaw S. Annual research review: secular trends in child and adolescent mental health. J Child Psychol Psychiatry. 2015;56:370–93. doi: 10.1111/jcpp.12372. [DOI] [PubMed] [Google Scholar]
- 187.Murray CJ, Ortblad KF, Guinovart C, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:1005–70. doi: 10.1016/S0140-6736(14)60844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Jamison DT, Summers LH, Alleyne G, et al. Global health 2035: a world converging within a generation. Lancet. 2013;382:1898–955. doi: 10.1016/S0140-6736(13)62105-4. [DOI] [PubMed] [Google Scholar]
- 189.Bruin JE, Gerstein HC, Holloway AC. Long-term consequences of fetal and neonatal nicotine exposure: a critical review. Toxicol Sci. 2010;116:364–74. doi: 10.1093/toxsci/kfq103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Bonomo YA, Patton GC, Bowes G. What are the longer term outcomes of adolescent alcohol consumption in young adulthood? Results from a 10-year cohort study. Alcoholism. 2006;30:117A. [Google Scholar]
- 191.Viner RM, Taylor B. Adult outcomes of binge drinking in adolescence: findings from a UK national birth cohort. J Epidemiol Community Health. 2007;61:902–07. doi: 10.1136/jech.2005.038117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Riley EP, McGee CL. Fetal alcohol spectrum disorders: an overview with emphasis on changes in brain and behavior. Exp Biol Med. 2005;230:357–65. doi: 10.1177/15353702-0323006-03. [DOI] [PubMed] [Google Scholar]
- 193.Patton GC, Coffey C, Carlin JB, et al. Overweight and obesity between adolescence and young adulthood: a 10-year prospective cohort study. J Adolesc Health. 2011;48:275–80. doi: 10.1016/j.jadohealth.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 194.Reilly J, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35:891–98. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 195.Yu C, Teoh T, Robinson S. Review article: obesity in pregnancy. BJOG. 2006;113:1117–25. doi: 10.1111/j.1471-0528.2006.00991.x. [DOI] [PubMed] [Google Scholar]
- 196.Lesthaeghe R. The second demographic transition: a concise overview of its development. Proc Natl Acad Sci USA. 2014;111:18112–15. doi: 10.1073/pnas.1420441111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Tylee A, Haller DM, Graham T, Churchill R, Sanci LA. Youth-friendly primary-care services: how are we doing and what more needs to be done? Lancet. 2007;369:1565–73. doi: 10.1016/S0140-6736(07)60371-7. [DOI] [PubMed] [Google Scholar]
- 198.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373:48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 199.Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369:1302–13. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- 200.Woog V, Singh S, Browne A, Philbin J. Adolescent women’s need for and use of sexual and reproductive health services in developing countries. New York NY: Guttmacher Institute; 2015. [Google Scholar]
- 201.Blanc AK, Tsui AO, Croft TN, Trevitt JL. Patterns and trends in adolescents’ contraceptive use and discontinuation in developing countries and comparisons with adult women. Int Perspect Sex Reprod Health. 2009;35:63–71. doi: 10.1363/ipsrh.35.063.09. [DOI] [PubMed] [Google Scholar]
- 202.Biddlecom AE, Munthali A, Singh S, Woog V. Adolescents’ views of and preferences for sexual and reproductive health services in Burkina Faso, Ghana, Malawi and Uganda. Afr J Reprod Health. 2007;11:99. [PMC free article] [PubMed] [Google Scholar]
- 203.Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366:1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 204.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertil Steril. 2012;98:893–97. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Vanheusden K, Van der Ende J, Mulder CL, van Lenthe FJ, Verhulst FC, Mackenbach JP. The use of mental health services among young adults with emotional and behavioural problems: equal use for equal needs? Soc Psychiatry Psychiatr Epidemiol. 2008;43:808–15. doi: 10.1007/s00127-008-0367-4. [DOI] [PubMed] [Google Scholar]
- 206.Alonso J, Codony M, Kovess V, et al. Population level of unmet need for mental healthcare in Europe. Br J Psychiatry. 2007;190:299–306. doi: 10.1192/bjp.bp.106.022004. [DOI] [PubMed] [Google Scholar]
- 207.Patel V, Araya R, Chatterjee S, et al. Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet. 2007;370:991–1005. doi: 10.1016/S0140-6736(07)61240-9. [DOI] [PubMed] [Google Scholar]
- 208.Calhoun LM, Speizer IS, Rimal R, et al. Provider imposed restrictions to clients’ access to family planning in urban Uttar Pradesh, India: a mixed methods study. BMC Health Serv Res. 2013;13:532. doi: 10.1186/1472-6963-13-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Waddington C, Sambo C. Financing health care for adolescents: a necessary part of universal health coverage. Bull World Health Organ. 2015;93:57–59. doi: 10.2471/BLT.14.139741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Hargreaves DS, Greaves F, Levay C, et al. Comparison of health care experience and access between young and older adults in 11 high-income countries. J Adolesc Health. 2015;57:413–20. doi: 10.1016/j.jadohealth.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 211.Ford CA, Millstein SG, Halpern-Felsher BL, Irwin CE. Influence of physician confidentiality assurances on adolescents’s willingness to disclose information and seek future health care. A randomised controlled trial. J Am Med Assoc. 1997;278:1029–34. [PubMed] [Google Scholar]
- 212.Schoen C, Davis K, DesRoches C, Shekhdar A. Health of adolescent boys: commonwealth fund survey findings. New York, NY: Commonweath Fund; 1998. [Google Scholar]
- 213.Sedlander E, Brindis CD, Bausch SH, Tebb KP. Options for assuring access to confidential care for adolescents and young adults in an explanation of benefits environment. J Adolesc Health. 2015;56:7–9. doi: 10.1016/j.jadohealth.2014.10.262. [DOI] [PubMed] [Google Scholar]
- 214.Sanci L. Clinical preventive services for adolescents: facing the challenge of proving “an ounce of prevention is worth a pound of cure”. J Adolesc Health. 2011;49:450–52. doi: 10.1016/j.jadohealth.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 215.Kadivar H, Thompson L, Wegman M, et al. Adolescent views on comprehensive health risk assessment and counseling: assessing gender differences. J Adolesc Health. 2014;55:24–32. doi: 10.1016/j.jadohealth.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sasse RA, Aroni RA, Sawyer SM, Duncan RE. Confidential consultations with adolescents: an exploration of Australian parents’ perspectives. J Adolesc Health. 2013;52:786–91. doi: 10.1016/j.jadohealth.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 217.Duncan RE, Jekel M, O’Connell MA, Sanci LA, Sawyer SM. Balancing parental involvement with adolescent friendly health care in teenagers with diabetes: are we getting it right? J Adolesc Health. 2014;55:59–64. doi: 10.1016/j.jadohealth.2013.11.024. [DOI] [PubMed] [Google Scholar]
- 218.Rausch JR, Hood KK, Delamater A, et al. Changes in treatment adherence and glycemic control during the transition to adolescence in type 1 diabetes. Diabetes Care. 2012;35:1219–24. doi: 10.2337/dc11-2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Kahana SY, Rohan J, Allison S, Frazier TW, Drotar D. A meta-analysis of adherence to antiretroviral therapy and virologic responses in HIV-infected children, adolescents, and young adults. AIDS Behav. 2013;17:41–60. doi: 10.1007/s10461-012-0159-4. [DOI] [PubMed] [Google Scholar]
- 220.Dean AJ, Walters J, Hall A. A systematic review of interventions to enhance medication adherence in children and adolescents with chronic illness. Arch Dis Child. 2010;95:717–23. doi: 10.1136/adc.2009.175125. [DOI] [PubMed] [Google Scholar]
- 221.Salema N-EM, Elliott RA, Glazebrook C. A systematic review of adherence-enhancing interventions in adolescents taking long-term medicines. J Adolesc Health. 2011;49:455–66. doi: 10.1016/j.jadohealth.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 222.Al-sheyab N, Gallagher R, Crisp J, Shah S. Peer-led education for adolescents with asthma in Jordan: a cluster-randomized controlled trial. Pediatrics. 2012;129:e106–12. doi: 10.1542/peds.2011-0346. [DOI] [PubMed] [Google Scholar]
- 223.Rosen DS, Blum RW, Britto M, Sawyer SM, Sigel DM. Transition to adult health care for adolescents and young adults with chronic conditions: position paper of the Society for Adolescent Medicine. J Adolesc Health. 2003;33:309–11. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- 224.Suris J-C, Akre C. Key elements for, and indicators of, a successful transition: an international Delphi study. J Adolesc Health. 2015;56:612–18. doi: 10.1016/j.jadohealth.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 225.Agwu AL, Lee L, Fleishman JA, et al. Aging and loss to follow-up among youth living with human immunodeficiency virus in the HIV Research Network. J Adolesc Health. 2015;56:345–51. doi: 10.1016/j.jadohealth.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Bonnie RJ, Stroud C, Breiner H. Investing in the health and well-being of young adults. Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- 227.Ambresin AE, Bennett K, Patton GC, Sanci LA, Sawyer SM. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolesc Health. 2013;52:670–81. doi: 10.1016/j.jadohealth.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 228.Luxford K, Piper D, Dunbar N, Poole N. Patient-centred care: improving quality and safety by focusing care on patients and consumers. 2010 http://www.safetyandquality.gov.au/wp-content/uploads/2012/01/PCCC-DiscussPaper.pdf (accessed April 3, 2016)
- 229.WHO. Adolescent friendly health services: an agenda for change. Geneva: World Health Organization (WHO); 2002. [Google Scholar]
- 230.Michaud P-A, Blum RW, Benaroyo L, Zermatten J, Baltag V. Assessing an adolescent’s capacity for autonomous decision-making in clinical care. J Adolesc Health. 2015;57:361–66. doi: 10.1016/j.jadohealth.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 231.Sawyer SM, Conn JJ, Reid KJ, et al. Working with young people: Evaluation of an education resource for medical trainees. J Paediatr Child Health. 2013;49:901–05. doi: 10.1111/jpc.12429. [DOI] [PubMed] [Google Scholar]
- 232.Denno DM, Hoopes AJ, Chandra-Mouli V. Effective strategies to provide adolescent sexual and reproductive health services and to increase demand and community support. J Adolesc Health. 2015;56(suppl):S22–41. doi: 10.1016/j.jadohealth.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 233.Chandra-Mouli V, Svanemyr J, Amin A, et al. Twenty years after International Conference on Population and Development: where are we with adolescent sexual and reproductive health and rights? J Adolesc Health. 2015;56:S1–S6. doi: 10.1016/j.jadohealth.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 234.Nair M, Baltag V, Bose K, Boschi-Pinto C, Lambrechts T, Mathai M. Improving the quality of health care services for adolescents, globally: a standards-driven approach. J Adolesc Health. 2015;57:288–98. doi: 10.1016/j.jadohealth.2015.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Hargreaves DS. Revised You’re Welcome criteria and future developments in adolescent healthcare. J Clin Res Pediatr Endocrinol. 2011;3:43. doi: 10.4274/jcrpe.v3i2.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Kesterton AJ, Cabral de Mello M. Generating demand and community support for sexual and reproductive health services for young people: a review of the literature and programs. Reprod Health. 2010;7:25. doi: 10.1186/1742-4755-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Kauer SD, Mangan C, Sanci L. Do online mental health services improve help-seeking for young people? A systematic review. J Med Internet Res. 2014;16:e66. doi: 10.2196/jmir.3103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Mason-Jones AJ, Crisp C, Momberg M, Koech J, De Koker P, Mathews C. A systematic review of the role of school-based healthcare in adolescent sexual, reproductive, and mental health. Syst Rev. 2012;1:49. doi: 10.1186/2046-4053-1-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Blank L, Baxter SK, Payne N, Guillaume LR, Pilgrim H. Systematic review and narrative synthesis of the effectiveness of contraceptive service interventions for young people, delivered in educational settings. J Pediatr Adolesc Gynecol. 2010;23:341–51. doi: 10.1016/j.jpag.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 240.Goldie SJ, Diaz M, Constenla D, Alvis N, Andrus JK, Kim S-Y. Mathematical models of cervical cancer prevention in Latin America and the Carribean. Vaccine. 2008;265:L59–72. doi: 10.1016/j.vaccine.2008.05.063. [DOI] [PubMed] [Google Scholar]
- 241.Goldie SJ, Diaz M, Kim S-Y, Levin CE, Minh HV, Kim JJ. Mathematical models of cervical cancer prevention in the Asia Pacific Region. Vaccine. 2008;265:M17–29. doi: 10.1016/j.vaccine.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 242.Chesson HW, Ekwueme DU, Saraiya M, Dunne EF, Markowitz LE. The cost-effectiveness of male HPV vaccination in the United States. Vaccine. 2011;29:8443–50. doi: 10.1016/j.vaccine.2011.07.096. [DOI] [PubMed] [Google Scholar]
- 243.Udonwa NE, Gyuse AN, Etokidem AJ. Malaria: knowledge and prevention practices among school adolescents in a coastal community in Calabar, Nigeria. Afr J Prim Health Care Fam Med. 2010;2:103. [Google Scholar]
- 244.Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371:340–57. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.United Nations. Children’s Fund Improving child nutrition: The achievable imperative for global progress. New York: UNICEF; 2013. [Google Scholar]
- 246.Haider R. Adolescent nutrition: a review of the situation in selected South-East Asian countries. New Delhi: Regional Offi ce for South-East Asia, World Health Organization (WHO); 2006. [Google Scholar]
- 247.DFID. The neglected crisis of undernutrition: evidence for action. London: Department for International Development (DFID); 2012. [Google Scholar]
- 248.WHO. Guideline: Intermittent iron and folic acid supplementation in menstruating women. Geneva: World Health Organization; 2011. [PubMed] [Google Scholar]
- 249.Bhutta ZA, Das JK, Rizvi A, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382:452–77. doi: 10.1016/S0140-6736(13)60996-4. [DOI] [PubMed] [Google Scholar]
- 250.World Bank. From agriculture to nutrition: pathways, synergies and outcomes. Washington, DC: World Bank; 2007. [Google Scholar]
- 251.Masset E, Haddad L, Cornelius A, Isanza-Castro J. A systematic review of agricultural interventions that aim to improve the nutritional status of children. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2011. [Google Scholar]
- 252.Bhutta ZA, Ahmed T, Black RE, et al. What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371:417–40. doi: 10.1016/S0140-6736(07)61693-6. [DOI] [PubMed] [Google Scholar]
- 253.Adelman S, Gilligan D, Konde-Lule J, Alderman H. School feeding reduces anemia prevalence in adolescent girls and other vulnerable household members in a cluster randomized controlled trial in Uganda. Washington, DC: International Food Policy Research Institute; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Gibbs CM, Wendt A, Peters S, Hogue CJ. The impact of early age at first childbirth on maternal and infant health. Paediatr Perinat Epidemiol. 2012;26:259–84. doi: 10.1111/j.1365-3016.2012.01290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.King JC. The risk of maternal nutritional depletion and poor outcomes increases in early or closely spaced pregnancies. J Nutr. 2003;133:1732S–36S. doi: 10.1093/jn/133.5.1732S. [DOI] [PubMed] [Google Scholar]
- 256.Casanueva E, Roselló-Soberón ME, De-Regil LM, Argüelles MdC, Céspedes MI. Adolescents with Adequate Birth Weight Newborns Diminish Energy Expenditure and Cease Growth. J Nutr. 2006;136:2498–501. doi: 10.1093/jn/136.10.2498. [DOI] [PubMed] [Google Scholar]
- 257.Rah JH, Christian P, Shamim AA, Arju UT, Labrique AB, Rashid M. Pregnancy and lactation hinder growth and nutritional status of adolescent girls in rural Bangladesh. J Nutr. 2008;138:1505–11. doi: 10.1093/jn/138.8.1505. [DOI] [PubMed] [Google Scholar]
- 258.WHO. Guideline: Calcium supplementation in pregnant women. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 259.Reinhardt K, Fanzo J. Addressing chronic malnutrition through multi-sectoral, sustainable approaches: a review of the causes and consequences. Front Nutr. 2014;1:13. doi: 10.3389/fnut.2014.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Chandra-Mouli V, Camacho AV, Michaud P-A. WHO Guidelines on preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries. J Adolesc Health. 2013;52:517–22. doi: 10.1016/j.jadohealth.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 261.Bushamuka V, de Pee S, Talukder A, et al. Impact of a homestead gardening program on household food security and empowerment of women in Bangladesh. Food Nutr Bull. 2005;26:17–25. doi: 10.1177/156482650502600102. [DOI] [PubMed] [Google Scholar]
- 262.Toroyan T, Peden M. Youth and Road Safety. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 263.Peden M, Scurfield R, Sleet D, et al. World report on road traffi c injury prevention. Geneva, Switzerland: WHO; 2004. [Google Scholar]
- 264.WHO. Global Status Report on Road Safety 2013: Supporting A Decade of Action. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 265.Simpson HM. The evolution and effectiveness of graduated licensing. J Safety Res. 2003;34:25–34. doi: 10.1016/s0022-4375(02)00077-4. [DOI] [PubMed] [Google Scholar]
- 266.Norton R, Hyder AA, Bishai D, Peden M Unintentional Injuries. In: Disease Control Priorities in Developing Countries. 2nd. Jamison DT, Breman JG, Measham AR, et al., editors. Washington, DC: World Bank; 2006. pp. 737–55. [Google Scholar]
- 267.Afukaar FK. Speed control in developing countries: issues, challenges and opportunities in reducing road traffi c injuries. Inj Control Saf Promot. 2003;10:77–81. doi: 10.1076/icsp.10.1.77.14113. [DOI] [PubMed] [Google Scholar]
- 268.Elvik R, Hoye A, Vaa T, Sorensen M. The handbook of road safety measures. 2nd. Bingley, UK: Emerald Group Publishing Limited; 2009. [Google Scholar]
- 269.Forjuoh SN. Traffic-related injury prevention interventions for low-income countries. Inj Control Saf Promot. 2003;10:109–18. doi: 10.1076/icsp.10.1.109.14115. [DOI] [PubMed] [Google Scholar]
- 270.Retting RA, Ferguson SA, McCartt AT. A review of evidence-based traffic engineering measures designed to reduce pedestrian-motor vehicle crashes. Am J Public Health. 2003;93:1456–63. doi: 10.2105/ajph.93.9.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Porchia BR, Baldasseroni A, Dellisanti C, Lorini C, Bonaccorsi G. Effectiveness of two interventions in preventing traffi c accidents: a systematic review. Ann Ig. 2014;26:63–75. doi: 10.7416/ai.2014.1959. [DOI] [PubMed] [Google Scholar]
- 272.Williams AF. Young driver risk factors: successful and unsuccessful approaches for dealing with them and an agenda for the future. Inj Prev. 2006;12:i4–8. doi: 10.1136/ip.2006.011783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Roberts IG, Kwan I. School-based driver education for the prevention of traffic crashes. Cochrane Database Syst Rev. 2001;3:CD003201. doi: 10.1002/14651858.CD003201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R. World report on violence and health. Geneva: WHO; 2002. [Google Scholar]
- 275.Catalano RF, Fagan AA, Gavin LE, et al. Worldwide application of prevention science in adolescent health. Lancet. 2012;379:1653–64. doi: 10.1016/S0140-6736(12)60238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Fagan AA, Catalano RF. What works in youth violence prevention: a review of the literature. Res Soc Work Pract. 2013;23:141–56. [Google Scholar]
- 277.WHO. Violence prevention: the evidence. Geneva: World Health Organization (WHO); 2010. [Google Scholar]
- 278.Ellsberg M, Arango DJ, Morton M, et al. Prevention of violence against women and girls: what does the evidence say? Lancet. 2015;385:1555–66. doi: 10.1016/S0140-6736(14)61703-7. [DOI] [PubMed] [Google Scholar]
- 279.Fellmeth GLT, Heffernan C, Nurse J, Habibula S, Sethi D. Educational and skills-based interventions for preventing relationship and dating violence in adolescents and young adults. Cochrane Database Syst Rev. 2013;6:CD004534. doi: 10.1002/14651858.CD004534.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Lundgren R, Amin A. Addressing intimate partner violence and sexual violence among adolescents: emerging evidence of effectiveness. J Adolesc Health. 2015;56:S42–50. doi: 10.1016/j.jadohealth.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 281.Whitaker DJ, Morrison S, Lindquist C, et al. A critical review of interventions for the primary prevention of perpetration of partner violence. Aggr Violent Behav. 2006;11:151–66. [Google Scholar]
- 282.Patton GC, Romaniuk H, Spry E, et al. Prediction of perinatal depression from adolescence and before conception (VICHS): 20-year prospective cohort study. Lancet. 386:875–83. doi: 10.1016/S0140-6736(14)62248-0. [DOI] [PubMed] [Google Scholar]
- 283.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 284.Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2011;50:252–61. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.McGorry P, Bates T, Birchwood M. Designing youth mental health services for the 21st century: examples from Australia, Ireland and the UK. Br J Psychiatry Suppl. 2013;54:s30–35. doi: 10.1192/bjp.bp.112.119214. [DOI] [PubMed] [Google Scholar]
- 286.Jorm AF. How effective are ‘headspace’ youth mental health services? Aust N Z J Psychiatry. 2015;49:861–62. doi: 10.1177/0004867415608003. [DOI] [PubMed] [Google Scholar]
- 287.Stockings E, Degenhardt L, Dobbins T, et al. Preventing depression and anxiety in young people: a review of the joint effi cacy of universal, selective and indicated prevention. Psychol Med. 2016;46:11–26. doi: 10.1017/S0033291715001725. [DOI] [PubMed] [Google Scholar]
- 288.Hunter E, Harvey D. Indigenous suicide in Australia, New Zealand, Canada and the United States. Emerg Med. 2002;14:14–23. doi: 10.1046/j.1442-2026.2002.00281.x. [DOI] [PubMed] [Google Scholar]
- 289.Evans E, Hawton K, Rodham K. Factors associated with suicidal phenomena in adolescents: a systematic review of population-based studies. Clin Psychol Rev. 2004;24:957–79. doi: 10.1016/j.cpr.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 290.Hazell P. Adolescent suicide clusters: evidence, mechanisms and prevention. Aust N Z J Psychiatry. 1993;27:653–65. doi: 10.3109/00048679309075828. [DOI] [PubMed] [Google Scholar]
- 291.Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182:537–42. doi: 10.1192/bjp.182.6.537. [DOI] [PubMed] [Google Scholar]
- 292.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42:386. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 293.Robinson J, Cox G, Malone A, et al. A systematic review of school-based interventions aimed at preventing, treating, and responding to suicide-related behavior in young people. Crisis. 2013;34:164–82. doi: 10.1027/0227-5910/a000168. [DOI] [PubMed] [Google Scholar]
- 294.Andriessen K. Suicide bereavement and postvention in major suicidology journals: lessons learned for the future of postvention. Crisis. 2014;35:338–48. doi: 10.1027/0227-5910/a000269. [DOI] [PubMed] [Google Scholar]
- 295.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–74. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 296.Robinson J, Hetrick SE, Martin C. Preventing suicide in young people: systematic review. Aust N Z J Psychiatry. 2011;45:3–26. doi: 10.3109/00048674.2010.511147. [DOI] [PubMed] [Google Scholar]
- 297.Klimes-Dougan B, Klingbeil DA, Meller SJ. The impact of universal suicide-prevention programs on the help-seeking attitudes and behaviors of youths. Crisis. 2013;34:82–97. doi: 10.1027/0227-5910/a000178. [DOI] [PubMed] [Google Scholar]
- 298.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 300.Ruager-Martin R, Hyde MJ, Modi N. Maternal obesity and infant outcomes. Early Hum Dev. 2010;86:715–22. doi: 10.1016/j.earlhumdev.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 301.Dumith SC, Gigante DP, Domingues MR, Kohl HW., 3rd Physical activity change during adolescence: a systematic review and a pooled analysis. Int J Epidemiol. 2011;40:685–98. doi: 10.1093/ije/dyq272. [DOI] [PubMed] [Google Scholar]
- 302.Niemeier HM, Raynor HA, Lloyd-Richardson EE, Rogers ML, Wing RR. Fast food consumption and breakfast skipping: predictors of weight gain from adolescence to adulthood in a nationally representative sample. J Adolesc Health. 2006;39:842–49. doi: 10.1016/j.jadohealth.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 303.Jordan AB, Kramer-Golinkoff EK, Strasburger VC. Does adolescent media use cause obesity and eating disorders? Adolesc Med State Art Rev. 2008;19:431–49. viii–ix. [PubMed] [Google Scholar]
- 304.Laska MN, Pelletier JE, Larson NI, Story M. Interventions for weight gain prevention during the transition to young adulthood: a review of the literature. J Adolesc Health. 2012;50:324–33. doi: 10.1016/j.jadohealth.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Pearson N, Braithwaite R, Biddle SJ. The effectiveness of interventions to increase physical activity among adolescent girls: a meta-analysis. Acad Pediatr. 2015;15:9–18. doi: 10.1016/j.acap.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 306.Rees R, Kavanagh J, Harden A, et al. Young people and physical activity: a systematic review matching their views to effective interventions. Health Educ Res. 2006;21:806–25. doi: 10.1093/her/cyl120. [DOI] [PubMed] [Google Scholar]
- 307.Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull. 2006;132:667–91. doi: 10.1037/0033-2909.132.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Francis JM, Grosskurth H, Changalucha J, Kapiga SH, Weiss HA. Systematic review and meta-analysis: prevalence of alcohol use among young people in eastern Africa. Trop Med Int Health. 2014;19:476–88. doi: 10.1111/tmi.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Bonomo YA, Bowes G, Coffey C, Carlin JB, Patton GC. Teenage drinking and the onset of alcohol dependence: a cohort study over seven years. Addiction. 2004;99:1520–28. doi: 10.1111/j.1360-0443.2004.00846.x. [DOI] [PubMed] [Google Scholar]
- 310.Feldstein Ewing SW, Sakhardande A, Blakemore S-J. The effect of alcohol consumption on the adolescent brain: A systematic review of MRI and fMRI studies of alcohol-using youth. Neuroimage Clin. 2014;5:420–37. doi: 10.1016/j.nicl.2014.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.WHO. Global health sector strategy on HIV/AIDS 2011–2015. Geneva: World Health Organization; 2011. [Google Scholar]
- 312.Warren CW, Lea V, Lee J, Jones NR, Asma S, McKenna M. Change in tobacco use among 13–15 year olds between 1999 and 2008: findings from the Global Youth Tobacco Survey. Glob Health Promot. 2009;16:38–90. doi: 10.1177/1757975909342192. [DOI] [PubMed] [Google Scholar]
- 313.Batura N, Hill Z, Haghparast-Bidgoli H, et al. Highlighting the evidence gap: how cost-effective are interventions to improve early childhood nutrition and development? Health Policy Plan. 2015;30:813–21. doi: 10.1093/heapol/czu055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Moyer-Gusé E. Toward a theory of entertainment persuasion: Explaining the persuasive effects of entertainment-education messages. Commun Theory. 2008;18:407–25. [Google Scholar]
- 315.Saavedra M. Dilemmas and opportunities in gender and sport-in-development. In: Levermore R, Beacom A, editors. Sport and international development. Basingstoke: Macmillan; 2009. pp. 124–55. [Google Scholar]
- 316.UNICEF. The State of the World’s Children 2011: Adolescence: an age of opportunity. 2011 http://www.unicef.org/sowc2011/ (accessed April 12, 2015)
- 317.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330:765. doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Lester R, Karanja S. Mobile phones: exceptional tools for HIV/AIDS, health, and crisis management. Lancet Infect Dis. 2008;8:738–39. doi: 10.1016/S1473-3099(08)70265-2. [DOI] [PubMed] [Google Scholar]
- 319.Labrique AB, Sikder SS, Mehara S, et al. Mobile phone ownership and widespread mHealth use in 168,231 women of reproductive age in rural Bangladesh. J Mob Technol Med. 2012;1:26. [Google Scholar]
- 320.Puccio JA, Belzer M, Olson J, et al. The use of cell phone reminder calls for assisting HIV-infected adolescents and young adults to adhere to highly active antiretroviral therapy: a pilot study. AIDS Patient Care STDS. 2006;20:438–44. doi: 10.1089/apc.2006.20.438. [DOI] [PubMed] [Google Scholar]
- 321.Harden A, Brunton G, Fletcher A, Oakley A. Teenage pregnancy and social disadvantage: systematic review integrating controlled trials and qualitative studies. BMJ. 2009;339:b4254. doi: 10.1136/bmj.b4254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Blank L, Baxter S, Goyder E, et al. Promoting well-being by changing behaviour: a systematic review and narrative synthesis of the effectiveness of whole secondary school behavioural interventions. Ment Health Rev J. 2010;15:43–53. [Google Scholar]
- 323.Milat AJ, King L, Newson R, et al. Increasing the scale and adoption of population health interventions: experiences and perspectives of policy makers, practitioners, and researchers. Health Res Policy Syst. 2014;12:18. doi: 10.1186/1478-4505-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Kivela J, Ketting E, Baltussen R. Cost analysis of school-based sexuality education programs in six countries. Cost Eff Resour Alloc. 2013;11:17. doi: 10.1186/1478-7547-11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Terris-Prestholt F, Kumaranayake L, Obasi AI, et al. From trial intervention to scale-up: costs of an adolescent sexual health program in Mwanza, Tanzania. Sex Transm Dis. 2006;33:S133–39. doi: 10.1097/01.olq.0000200606.98181.42. [DOI] [PubMed] [Google Scholar]
- 326.O’Neill J, Tabish H, Welch V, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol. 2014;67:56–64. doi: 10.1016/j.jclinepi.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 327.Chandra-Mouli V, Lane C, Wong S. What does not work in adolescent sexual and reproductive health: a review of evidence on interventions commonly accepted as best practices. Glob Health Sci Pract. 2015;3:333–40. doi: 10.9745/GHSP-D-15-00126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Hotez PJ, Asojo OA, Adesina AM. Nigeria:“Ground Zero” for the high prevalence neglected tropical diseases. PLoS Negl Trop Dis. 2012;6:e1600. doi: 10.1371/journal.pntd.0001600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Suleiman AB, Soleimanpour S, London J. Youth action for health through youth-led research. J Community Pract. 2006;14:125–45. [Google Scholar]
- 330.United Nations (DESA) World Youth Report 2007: Young People’s Transition to Adulthood. New York: United Nations; 2007. [Google Scholar]
- 331.United Nations. World Programme of Action on Youth. New York, NY: United Nations; 2010. [Google Scholar]
- 332.UNICEF. The State of the World’s Children Report 2003: Child Participation. 2002 http://www.unicef.org/adolescence/files/pub_sowc03_en.pdf (accessed April 12, 2015)
- 333.Dahl RE. Adolescent brain development: a period of vulnerabilities and opportunities. Keynote address. Ann N Y Acad Sci. 2004;1021:1–22. doi: 10.1196/annals.1308.001. [DOI] [PubMed] [Google Scholar]
- 334.Lansdown G. Rights based approach to programming: implications for children. 2005 http://www.savethechildren.org.uk.proxy.library.vcu.edu/sites/default/files/docs/Whats_the_Difference_1.pdf (accessed April 9, 2015)
- 335.Wong NT, Zimmerman MA, Parker EA. A typology of youth participation and empowerment for child and adolescent health promotion. Am J Community Psychol. 2010;46:100–14. doi: 10.1007/s10464-010-9330-0. [DOI] [PubMed] [Google Scholar]
- 336.Gibbs A, Campbell C, Maimane S, Nair Y. Mismatches between youth aspirations and participatory HIV/AIDS programmes in South Africa. Afr J AIDS Res. 2010;9:153–63. doi: 10.2989/16085906.2010.517482. [DOI] [PubMed] [Google Scholar]
- 337.Maticka-Tyndale E, Barnett JP. Peer-led interventions to reduce HIV risk of youth: A review. Eval Program Plann. 2010;33:98–112. doi: 10.1016/j.evalprogplan.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 338.Hochberg Z, Belsky J. Evo-devo of human adolescence: beyond disease models of early puberty. BMC Med. 2013;11:113. doi: 10.1186/1741-7015-11-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Akinfaderin-Agurau F, Fashola T. What business do youth have making HIV and AIDS laws in Nigeria? 2011 http://pubs.iied.org/pdfs/G03196.pdf (accessed April 2, 2015)
- 340.Jacquez F, Vaughn LM, Wagner E. Youth as partners, participants or passive recipients: A review of children and adolescents in community-based participatory research (CBPR) Am J Community Psychol. 2013;51:176–89. doi: 10.1007/s10464-012-9533-7. [DOI] [PubMed] [Google Scholar]
- 341.Yi J, Kim MA, An S. The experiences of Korean young adult survivors of childhood cancer a Photovoice study. Qual Health Res. 2015 doi: 10.1177/1049732315599374. published online Aug 11, 2015. [DOI] [PubMed] [Google Scholar]
- 342.Findholt NE, Michael YL, Jerofke LJ, Brogoitti VW. Environmental influences on children’s physical activity and eating habits in a rural Oregon County. Am J Health Promot. 2011;26:e74–85. doi: 10.4278/ajhp.100622-QUAL-210. [DOI] [PubMed] [Google Scholar]
- 343.Dakin EK, Parker SN, Amell JW, Rogers BS. Seeing with our own eyes: Youth in Mathare, Kenya use photovoice to examine individual and community strengths. Qual Soc Work. 2015;14:170–92. [Google Scholar]
- 344.Findholt NE, Michael YL, Davis MM. Photovoice engages rural youth in childhood obesity prevention. Public Health Nurs. 2011;28:186–92. doi: 10.1111/j.1525-1446.2010.00895.x. [DOI] [PubMed] [Google Scholar]
- 345.Shaw A, Brady B, McGrath B, Brennan MA, Dolan P. Understanding youth civic engagement: debates, discourses, and lessons from practice. Community Dev J. 2014;45:300–16. [Google Scholar]
- 346.Kaplan AM, Haenlein M. Users of the world, unite! The challenges and opportunities of Social Media. Bus Horiz. 2010;53:59–68. [Google Scholar]
- 347.Brandtzæg PB, Haugstveit IM, Lüders M, Følstad A. Participation barriers to youth civic engagement in social media. Ninth International AAAI Conference on Web and Social Media; Oxford, England. May 26–29, 2015. [Google Scholar]
- 348.Campbell C, Gibbs A, Maimane S, Nair Y, Sibiya Z. Youth participation in the fight against AIDS in South Africa: from policy to practice. J Youth Stud. 2009;12:93–109. [Google Scholar]
- 349.Coates D, Howe D. The importance and benefits of youth participation in mental health settings from the perspective of the headspace Gosford Youth Alliance in Australia. Child Youth Serv Rev. 2014;46:294–99. [Google Scholar]
- 350.Harden A, Oakley A, Oliver S. Peer-delivered health promotion for young people: a systematic review of different study designs. Health Educ J. 2001;60:339–53. [Google Scholar]
- 351.Iwasaki Y. Reflection on learnings from engaging and working with high-risk, marginalized youth. Relat Child Youth Care Pract. 2014;27:24–35. [Google Scholar]
- 352.Villa-Torres L, Svanemyr J. Ensuring youth’s right to participation and promotion of youth leadership in the development of sexual and reproductive health policies and programs. J Adolesc Health. 2015;56:S51–57. doi: 10.1016/j.jadohealth.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 353.Paterson BL, Panessa C. Engagement as an ethical imperative in harm reduction involving at-risk youth. Int J Drug Policy. 2008;19:24–32. doi: 10.1016/j.drugpo.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 354.Garcia AP, Minkler M, Cardenas Z, Grills C, Porter C. Engaging homeless youth in community-based participatory research: a case study from Skid Row, Los Angeles. Health Promot Pract. 2014;15:18–27. doi: 10.1177/1524839912472904. [DOI] [PubMed] [Google Scholar]
- 355.Bell J, Vromen A, Collin P. Rewriting the rules for youth participation: inclusion and diversity in government and community decision making. 2008 http://www.uws.edu.au/__data/assets/pdf_file/0009/476343/rewriting_the_rules_for_youth_participation.pdf (accessed April 9, 2015)
- 356.Bonita R, Magnusson R, Bovet P, et al. Country actions to meet UN commitments on non-communicable diseases: a stepwise approach. Lancet. 2013;381:575–84. doi: 10.1016/S0140-6736(12)61993-X. [DOI] [PubMed] [Google Scholar]
- 357.Kraak VI, Swinburn B, Lawrence M, Harrison P. An accountability framework to promote healthy food environments. Public Health Nutr. 2014;17:2467–83. doi: 10.1017/S1368980014000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.United Nations. Synthesis report of the Secretary-General on the post-2015 sustainable development agenda. New York, NY: United Nations; 2014. The road to dignity by 2030: ending poverty, transforming all lives and protecting the planet. [Google Scholar]
- 359.Collins C, Coates TJ, Szekeres G. Accountability in the global response to HIV: measuring progress, driving change. AIDS. 2008;22:S105–11. doi: 10.1097/01.aids.0000327442.66656.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Beaglehole R, Bonita R, Ezzati M, et al. NCD Countdown 2025: accountability for the 25 × 25 NCD mortality reduction target. Lancet. 2014;384:105–07. doi: 10.1016/S0140-6736(14)61091-6. [DOI] [PubMed] [Google Scholar]
- 361.Haddad L, Achadi E, Bendech MA, et al. The Global Nutrition Report 2014: actions and accountability to accelerate the world’s progress on nutrition. J Nutr. 2015;145:663–71. doi: 10.3945/jn.114.206078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Patton GC, Coffey C, Cappa C, et al. Health of the world’s adolescents: a synthesis of internationally comparable data. Lancet. 2012;379:1665–75. doi: 10.1016/S0140-6736(12)60203-7. [DOI] [PubMed] [Google Scholar]
- 363.WHO. Global Reference List of 100 Core Health Indicators. Geneva: World Health Organization; 2015. [Google Scholar]
- 364.de Andrade LOM, Pellegrini Filho A, Solar O, et al. Social determinants of health, universal health coverage, and sustainable development: case studies from Latin American countries. Lancet. 2015;385:1343–51. doi: 10.1016/S0140-6736(14)61494-X. [DOI] [PubMed] [Google Scholar]
- 365.Kraak VI, Story M. An accountability evaluation for the industry’s responsible use of brand mascots and licensed media characters to market a healthy diet to American children. Obes Rev. 2015;16:433–53. doi: 10.1111/obr.12279. [DOI] [PubMed] [Google Scholar]
- 366.Beaglehole R, Bonita R, Horton R. Independent global accountability for NCDs. Lancet. 2013;381:602–05. doi: 10.1016/S0140-6736(13)60101-4. [DOI] [PubMed] [Google Scholar]
- 367.Galati AJ. Onward to 2030: sexual and reproductive health and rights in the context of the Sustainable Development Goals. Guttmacher Pol Rev. 2015;18:77–84. [Google Scholar]


