Abstract
Mindfulness-based interventions are at a pivotal point in their future development. Spurred on by an ever-increasing number of studies and breadth of clinical application, the value of such approaches may appear self-evident. We contend, however, that the public health impact of mindfulness-based interventions can be enhanced significantly by situating this work in a broader framework of clinical psychological science. Utilizing the National Institute of Health stage model (Onken, Carroll, Shoham, Cuthbert, & Riddle, 2014), we map the evidence base for mindfulness-based cognitive therapy and mindfulness-based stress reduction as exemplars of mindfulness-based interventions. From this perspective, we suggest that important gaps in the current evidence base become apparent and, furthermore, that generating more of the same types of studies without addressing such gaps will limit the relevance and reach of these interventions. We offer a set of 7 recommendations that promote an integrated approach to core research questions, enhanced methodological quality of individual studies, and increased logical links among stages of clinical translation in order to increase the potential of MBIs to impact positively the mental health needs of individuals and communities.
Keywords: mindfulness, psychotherapy, mindfulness-based stress reduction, mindfulness-based cognitive therapy
The science and practice of mindfulness-based intervention (MBI) stands at a crossroads. It has witnessed exponential growth and interest in the last 15 years, with the establishment of research and clinical centers dedicated to the study and delivery of MBIs and an attendant proliferation of academic journals, magazines, and books. Given this context of expansion, we invite a pause in the forward movement to reflect on the durability and public health impact of this work. Our view is that such reflection is best promoted by considering MBIs in the broader framework of clinical psychological science and the recently proposed National Institute of Health (NIH) stage model (Onken et al., 2014). The NIH stage model emerged from an interest in shaping the training of future generations of clinical scientists by providing a well-articulated view of the goals and process of clinical psychological science. Specifically, as presented by Onken and colleagues (2014), the stage model is anchored in a vision “intended to unify various aspects of clinical science toward the common goal of developing maximally potent and implementable interventions, while unveiling new avenues of science in which basic and applied goals are of equally high importance…to propel the field to fulfill the public health goal of producing implementable and effective treatment and prevention interventions” (p. 22). In this paper, we use this framework to map MBI research, identify gaps in our knowledge and methods, and underscore priority questions and dilemmas for the future. Doing so allows us to identify both strengths and early indications of fault lines in the foundation of this rapidly developing field.
We first describe the use of the NIH stage model as a map for organizing the MBI evidence base. Next, with the aim of increasing the public health impact of MBI science and practice, we apply the NIH stage model. We identify strengths of the evidence base and limitations, including stages that have been under or overemphasized and pathways between stages that are weak or underdeveloped. We also outline seven stage-based sets of recommendations for ways in which the science and practice of MBI can be advanced to increase public health impact. It is our hope that by providing a broad and integrative framework at this critical juncture, we can help chart a course that supports deliberate, intentional, effective, and coordinated work on MBIs.
Mapping the MBI Evidence Base
Articles were identified through searches of the PsycINFO and PubMed databases. Database records were queried using the search terms MBCT (i.e., mindfulness-based cognitive therapy), MBSR (i.e., mindfulness-based stress reduction), and mindful* in the title or abstract fields for PubMed and in the title or subject fields for PsycINFO, and were limited to those conducted with human subjects and published between January 1, 1985 and December 31, 2013, in English, and in a peer-reviewed journal. Records for the total number of articles returned from each query were compiled and duplicates were removed, yielding 3,217 articles in the initial search. Research assistants reviewed the title and abstract of these records to confirm relevance to the topic based on the article title and abstract. Articles were included if they addressed MBCT or MBSR using case reports, open trials, controlled trials, or development of intervention fidelity measurement tools. Articles were excluded if they primarily examined topics such as trait or state mindfulness, trait or state mindfulness rating scales, basic research on mindfulness techniques without a clinical focus, and samples of experienced meditators. Interviews, personal essays or narratives, theoretical and review articles, and meta-analyses also were excluded. Final inclusion decisions were made the authors, resulting in a total of 309 articles (MBCT n = 118, MBSR n = 191). These were categorized by the authors for intervention type and target problem or population, and within each treatment model, by the appropriate stage based on Onken et al. (2014) using the descriptions that follow. See Tables 1 and 2 for the categorizations of the evidence base for MBCT and MBSR, respectively.
Table 1.
NIH Stage Model Classification of Mindfulness Based Cognitive Therapy Evidence Base
| Stage 0: Basic (Studies that integrate basic research as part of later stage intervention studies are denoted at the relevant later stage with an asterisk). | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Target Problem or Population |
Stage I: Intervention Generation/ Refinement |
Stage II: Efficacy in Research Clinic | Stage III: Efficacy in Community Clinic |
Stage IV: Effectiveness |
Stage V: Implementation and Dissemination |
|
|
| ||||||
| WLC or TAU control |
Active control |
|||||
| Anxiety | - | - | - | |||
| Bipolar | - | - | - | - | ||
| Borderline Personality Disorder |
|
- | - | - | - | - |
| Care Givers | - | - | - | - | - | |
| Child/Family | - | - | - | - | ||
| Depression (Residual Depressive Symptoms, Acute, and Sub-clinical) |
|
|
- | - | - | |
| Depression (Relapse Prevention) | - | |||||
| Disordered Eating | - | - | - | - | ||
| Elderly | - | - | - | - | - | |
| Healthcare students | - | - | - | - | - | |
| Heterogeneous/Unspecified | - | - | - | - | - | |
| Medical Comorbidity | - | |||||
| Pregnancy | - | - | - | - | - | |
| Problem Gambling | - | - | - | - | - | |
| Psychosis | - | - | - | - | - | |
| Sleep | - | - | - | - | ||
Table 2.
NIH Stage Model Classification of Mindfulness Based Stress Reduction Evidence Base
| Stage 0: Basic (Studies that integrate basic research as part of later stage intervention studies are denoted at the relevant later stage with an asterisk). | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Target Problem or Population |
Stage I: Intervention Generation/ Refinement |
Stage II: Efficacy in Research Clinic | Stage III: Efficacy in Community Clinic |
Stage IV: Effectiveness |
Stage V: Implementation and Dissemination |
|
| WLC or TAU control |
Active control |
|||||
| Adolescents | - | - | - | |||
| Anxiety | - | - | - | |||
| Arthritis | - | - | - | - | - | |
| Asthma | - | - | - | - | - | |
| Cancer |
|
- | - | - | ||
| Care Givers | - | - | - | - | ||
| Chronic Pain | - | - | - | - | ||
| Depression History | - | - | - | - | - | |
| Diabetes | - | - | - | - | ||
| Disordered Eating | - | - | - | - | - | |
| Fibromyalgia | - | - | - | |||
| Healthcare Clinicians or Students | - | - | - | |||
| Healthy Individuals | - | - | - | |||
| Heart Disease |
|
- | - | - | ||
| Heterogeneous or Unspecified |
|
- | - | - | ||
| HIV | - | - | - | |||
| Hot Flashes | - | - | - | - | ||
| IBS | ||||||
| Insomnia | - | - | - | - | - | |
| Intimate Partner Violence / Abuse | - | - | - | - | - | |
| Older Adults | - | - | - | - | ||
| Personality Disorder Symptoms | - | - | - | - | - | |
| Pregnant Women | - | - | - | - | - | |
| Prisoners | - | - | - | - | - | |
| Psoriasis | - | - | - | - | - | |
| PTSD / trauma (among veterans) | - | - | - | - | ||
| Smoking | - | - | - | - | - | |
| Somatization | - | - | - | - | ||
| Stress | - | - | - | - | - | |
| Stroke / TBI | - | - | - | - | ||
| Substance Abuse | - | - | - | - | - | |
| Teachers | - | - | - | - | - | |
| Tinnitus | - | - | - | - | - | |
| Transplant | - | - | - | - | ||
Specifically, we map at Stage 0 studies that use neuroscience and behavioral, cognitive, affective and social science methods to explicate the target of intervention and mechanisms of change. Two broad categories of basic research are relevant to clinical intervention. First, basic research studies can be conducted “upstream,” or temporally preceding the other stages of research at any level of analysis that informs intervention development or modification. This work can offer a critical scientific foundation for why and how an intervention may be helpful for a particular problem or population. Second, basic research methods can be conducted in an integrated manner in tandem with intervention research by assessing intervention outcomes on levels that extend beyond mental health symptom report and by answering questions about how an intervention works and for whom.
The scope of “upstream” basic research on the problems targeted by MBIs is vast and beyond the scope of this review (e.g., studies identifying the pathophysiology of major depression or anxiety disorders, etc.). Thus our mapping focuses on the second category of basic research—that which is integrated with applied research at Stages I–V. These studies encompass varying degrees of methodological rigor; however, they share the common element of seeking to understand whether an MBI works beyond simply symptom report as well as how and for whom. Because this work integrates basic research paradigms as part of later stage intervention studies, it is mapped with an asterisk at the relevant later-stage study.
We include studies that examine multiple units of analysis to measure treatment outcome (e.g., measurement of neural circuits, physiology, performance on behavioral or cognitive tasks, etc.). For example, in a study testing MBSR with HIV-positive patients, Creswell, Myers, Cole, and Irwin (2009) examined the effects on biological markers of disease progression (e.g., CD4+ T lymphocytes); as this study integrates basic research methods to characterize precise biological outcomes within the context of a “Stage II” study, it is denoted with an asterisk in Table 2. We also include studies that test mediation or moderation of intervention outcomes (even if only limited to one unit of analysis such as self-report). For example, Arch and Ayers (2013) measured self-report of baseline clinical severity and examined the extent to which such information could identify which treatment worked better for which patients; as this study integrated a focus on treatment moderation in the context of a Stage II study, it is denoted in Table 2 with an asterisk.
Onken et al. (2014) define Stage 1 as “all activities related to the creation of a new intervention, or the modification, adaptation, or refinement of an existing intervention (Stage IA), as well as feasibility and pilot testing (Stage IB)” (p. 28). This stage also is defined to encompass a focus on the development of training, supervision, and fidelity promotion materials. Our mapping at this stage includes mainly feasibility and pilot testing studies including nonrandomized open-trial designs of an MBI, whether conducted in the research lab or community settings. Most of these studies focus on extending the MBI to a novel problem or population, although some also represent early phase work in extending an MBI to a new setting. Some of these studies may examine as well the relationship between intervention exposure and outcome (e.g., dosage effects).
As defined by Onken et al. (2014), “Stage II is consists of testing of promising behavioral interventions in research settings, with research therapists/providers…Stage III is similar to Stage II research, except that instead of research providers and settings, it consists of testing in a community context while maintaining a high level of control necessary to establish internal validity” (page 29). We map at Stage II efficacy trials of promising MBIs conducted in research settings, and at Stage III efficacy trials conducted in community settings, using community providers. These studies place a premium on internal validity, and focus on testing efficacy and identifying mechanisms of change. We extend the NIH model by mapping separately at Stage II studies that use randomized designs that test efficacy, with comparisons often to treatment-as-usual (TAU) or waitlist control (WLC) conditions, and randomized designs that test comparative or specific efficacy, with comparisons to an active control or an established treatment. Although the distinction between active control and other comparison groups is relevant for Stages III–V, we have not mapped those separately due to the paucity of work at those stages. As more studies at these stages are conducted, it will be vital for future efforts to map the nature of the control and comparison conditions in finer granularity. Although Onken et al. (2014) allow for the inclusion of nonrandomized designs at Stage II, we view the methodological rigor of randomized controlled trials as of specific value for the future of research on MBI; thus, we map all nonrandomized designs at Stage I.
Stages IV and V cover effectiveness research and implementation and dissemination research, respectively. As defined by Onken et al. (2014), effectiveness research (Stage IV) places a premium on external validity, as researchers examine interventions as implemented by community providers under routine conditions “in the real world.” Stage V places relatively less emphasis on the intervention itself and instead foregrounds the study of methods to increase the adoption, integration, scaling up, and sustainability of an intervention in everyday settings. An important contribution of the NIH model is defining these stages as integral components of the clinical science endeavor. The inclusion of these stages codifies an inherent value that “intervention development is incomplete until the intervention is maximally potent and implementable for the population for which it was developed” (Onken et al., 2014, p. 25).
The Clinical Application of Mindfulness and Current Evidence Base: A “Bird’s Eye View”
MBSR originated in the work of Jon Kabat Zinn and colleagues in 1979 at the University of Massachusetts Medical Center (Kabat-Zinn, 1990). Nearly a decade later, Segal, Williams and Teasdale (2012) built upon this early foundation with the development of MBCT, extending and integrating the framework and practices of MBSR with cognitive-behavioral therapy. Both of these interventions are organized around the use of mindfulness meditation as a core intervention component, and engage such specific practices as sitting meditation, walking meditation, body scan meditation, yoga stretching, and a range of forms of daily informal practice (e.g., mindful eating). These practices are taught to support participants in developing mindfulness as skills or means to personal goals (e.g., prevention of depression or reduction of stress) and, to borrow from Lutz, Jha, Dunne, and Saron (2015), “a way of life.” Each session is delivered using an eight-session, weekly structure featuring extended experiential practice and inquiry about practice. The essential role of daily formal and informal mindfulness practices is emphasized throughout. The role of the instructor in these interventions is multilayered and comprises guiding practice (e.g., in person during classes and via audio recorded practice guides for participants to use between classes), embodying “mindfulness” using the broadest conceptualization of this term (J. M. G. Williams & Kabat-Zinn, 2011), and delivering intervention specific content (e.g., about stress or depression risk). Instructors are asked to teach from a foundation of their own personal mindfulness meditation practice.
Although other conceptually and clinically related interventions developed in parallel to MBSR and MBCT exist (e.g., acceptance and commitment therapy; Hayes, Strosahl, & Wilson, 1999; and dialectical behavior therapy; Linehan, 1993), MBSR and MBCT are distinguished by the predominant focus on mindfulness meditation practices, the 8-week course structure, active daily home practice of mindfulness meditation and the role and training requirements of the instructor. Moreover, since the first studies of MBCT and MBSR were published, multiple “next generation” MBI models have been developed. We focus, however, on MBCT and MBSR as the target interventions for this review because each has amassed a sufficient empirical record to enable mapping of this nature. In a final section, we offer reflections about “next generation” interventions and recent findings that reflect promising advancements in the field. As the field develops, we expect that updates to our mapping will be required for MBSR, MBCT, and next generation interventions.
Multiple meta-analytic studies including MBSR and MBCT trials have been published in recent years (Goyal et al., 2014; Hofmann, Sawyer, Witt, & Oh, 2010; Piet & Hougaard, 2011), with generally convergent findings. These meta-analyses have been focused largely on the question “do MBIs work?” And, although most have emphasized problems with the methodological quality of many individual studies, the overall consensus appears to be “yes.” We concur with these interpretations, and building on this foundation, we think the field is ripe for considering the evidence base from the broader “bird’s eye view” of the NIH stage model.
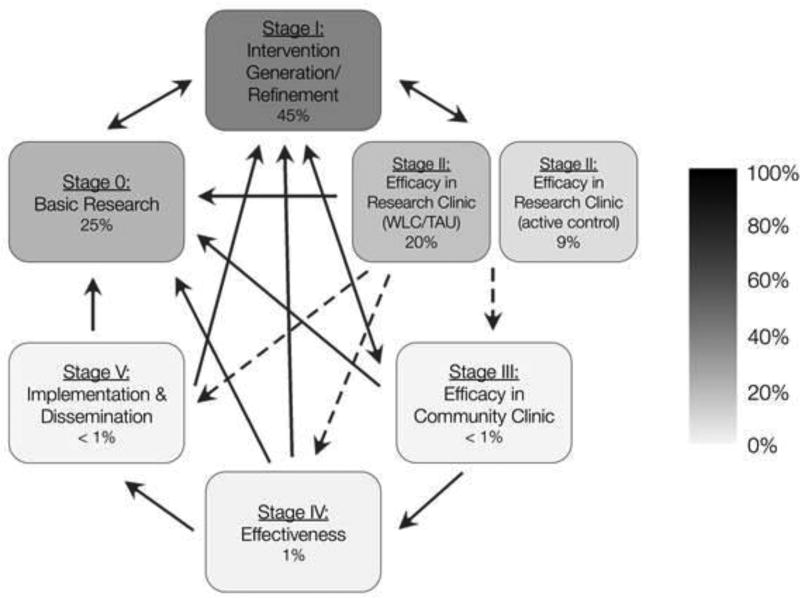
Figure 1 illustrates the core stages of the NIH model with the color saturation of each stage corresponding to the proportional amount of published research on MBCT and MBSR, considered together, at each given stage. The NIH stage model is proposed not as a fixed and linear set of steps to take in chronological order, but rather as a set of overlapping and mutually informing points along a continuum of research. Within this context, there are indications that some stages and the links between stages warrant greater attention. The greatest focus of activity in the MBI field has been dedicated to the development and exploration of applications of MBIs with novel populations and target problems. This pattern may be implicit in the early development of a field; however, it also represents a point of vulnerability. If the weight of clinical and scientific attention remains devoted to increasing the range of applications rather than the depth of the evidence base, public health impact may be limited. Or, put simply, with reference to Tables 1 and 2, it would be misguided to prioritize increasing the number of rows in each table, without emphasizing simultaneously the development and integration of studies across the columns. Here, we offer a set of seven recommendations for increasing the public health impact of this work.
Figure 1.
Evidence base for MBIs (i.e., MBSR and MBCT) mapped according to the adapted NIH Stage Model. Recommended pathways between stages are represented with solid arrows; pathways that should be undertaken with caution are represented with dotted arrows. Color saturation represents the proportion of the total number of published studies of MBIs mapped at a given stage, with the specific percentage indicated at each stage.
Stage-based Recommendations to Increase the Public Health Impact of MBI Research
Recommendation 1. Attend to the Basics: Specify Intervention Targets and Populations
A close link between basic and intervention research exists in the foundation of clinical innovation and research on MBIs. For example, the first application of mindfulness meditation for the prevention of depression was rooted in basic research on the nature of depressive relapse. In such studies, formerly depressed patients were compared to healthy controls before and after a sad mood induction; formerly depressed patients showed greater increases in depressogenic thinking styles, suggesting that a history of depression was associated with increased access to depressive cognition in the context of mild sad mood (Teasdale, 1988). Moreover, studies suggested that such increased access prospectively predicted relapse risk (Segal et al., 2006). This work identified a potential target for intervention (i.e., ruminative emotion linked cognitive processes), a population for whom this target was relevant and identifiable (i.e., individuals with histories of recurrent depression), and a logical basis for the application of mindfulness meditation (i.e., to enable regulation of dysphoric mood states in ways that inhibited the activation of habitual, mood-linked mental content) (Teasdale, Segal, & Williams, 1995).
The rapid proliferation of new potential indications for MBIs risks neglecting the link between Stage 0 and subsequent stages. In an era in which specification of clear intervention targets and meditating processes of change is increasingly prioritized, failure to attend to the “basics” may undermine the potential public health impact of research on MBIs. A glance at the range of problems for which MBIs are being applied suggests possible vulnerability in this regard. For example, recent studies have extended MBCT to other populations and problems (e.g., bipolar disorder, psychosis) based on the evidence of care-gaps in the psychosocial treatment of these groups; however, they have less frequently identified the targets that mindfulness practice is intended to engage, nor have they identified the degree to which the interventions alter (or fail to alter) the target when they achieve their intended clinical effects. Although intervention studies suggest that MBCT has promise for such patients, the basic research necessary to support a rationale for “why” is often lacking (although, see final section for recent exceptions).
Moreover, our mapping indicates that only a small number of studies have explored candidate mediators or moderators of outcome; and of these, even fewer have tested mediation formally or incorporated recent methods that move the field closer to a personalized medicine framework in which patient characteristics determine treatment selection (e.g., DeRubeis et al., 2014). Exceptions include the work of Vøllestad, Sivertsen, and Nielsen (2011) who describe a well-conceived analysis in which mindfulness statistically mediated changes in anxiety symptoms following MBSR, but owing to the absence of temporal precedence for these changes did not demonstrate true mediation. Such efforts represent an advance beyond work that simply reports the magnitude of pre-post intervention change of a potential mediator. Arch and Ayers (2013) provide another instructive example, in which patients with anxiety disorders were randomized to MBSR or cognitive behavioral therapy, with results indicating the response to intervention depended in part on baseline depressive symptom severity comorbidity and anxiety sensitivity. Similarly, studies of MBCT suggest that effects may be moderated by vulnerability factors, including more recurrent depressive episode histories (Ma & Teasdale, 2004; Teasdale et al., 2000) and residual depressive symptoms (Segal et al., 2010).
Underemphasizing links to basic research and precise specification of for whom and how a treatment works risks situating the study of MBI less as science and more as pseudoscience in which mindfulness is seen as a panacea for all problems. Absence of clear attention to both “boundary conditions” and “scientific plausibility” is often cited as hallmarks of pseudoscience (Lilienfeld, 2003). Future work on MBI will be strengthened by attending to these requirements—specifying both what mindfulness is not likely to help with, and, not only predicting that an MBI will produce clinical benefit, but also specifying plausible mechanisms by which such benefits are attained. Moreover, extensions of MBSR, MBCT, and other MBIs to new populations and conditions may require modifications and tailoring to address their salient pathogenic mechanisms; such work represents the heart of Stage 1 but requires close and iterative links to Stage 0 methods and concepts. Many basic research studies have investigated correlates of mindfulness meditation (see Lutz et al., 2015) and provide methods or proxy markers to consider for integration in applied trials. Studies identified with asterisks in Stages I–V provide examples of movement to such integration.
Recommendation 2. Don’t Conflate Promise With Efficacy
In contrast to the relative paucity of Stage 0 studies, research efforts have saturated heavily Stage I. The non-randomized and, most often, uncontrolled studies, mapped here at Stage I, clearly support valid excitement about the use of MBI in clinical settings across a wide range of target populations and problems. This excitement, however, must be tempered, given the risk that the field will fail to advance if Stage I research is seen as a sufficient “green light” to proceed to broad dissemination and implementation of MBI, or if the field “stalls out” by simply amassing more studies at Stage I. Thus, the NIH stage model underscores the value of the full cycle of research stages, and notably does not specify a direct pathway from Stage I to Stages IV or V. Among problems targeted by MBCT, only work on depression and comorbid health and mental health conditions, and within MBSR studies, primarily work with patients with cancer, show incremental progression from Stage I to subsequent stages. The sheer quantity of promising uncontrolled studies cannot substitute for later stage studies; researchers, practitioners, and the public must be cautious not to conflate a lot of studies at Stage I with indications of efficacy or effectiveness.
Moreover, as the field focuses more on the incremental progression of MBI research from Stage I to V, it will be important to consider directly indications of both failure and harm. In fact, a “failed” individual trial in which the MBI does not outperform the comparator intervention may be a “success” when viewing the advancement of the field broadly. Such findings help to inform the “boundary conditions” necessary for scientific progress and strengthen the pathway between Stage I and Stage 0, in which failures in one context create fertile ground in the other. The field will be well served by frank acknowledgement of failure rather than obscuring such findings with multiple or ambiguous primary and secondary outcomes or falling victim to the “file drawer” problem in which failed trials simply are not published. An instructive example is provided by Craigie, Rees, Marsh, and Nathan (2008) regarding the relatively poor performance of MBCT in an open trial when compared to benchmarks of cognitive behavioral therapy in other studies targeting generalized anxiety disorder. They highlight valuable questions that can be “sent back” to Stage 0 about potential maintaining factors in generalized anxiety disorder. In addition to addressing directly “failed” trials, it also will be important to consider potential harmful effects of MBI. With the exception of recent work by Britton and colleagues (2012), it is notable that few publications have reported data on adverse effects of MBI. This area will be important for future investigators to address directly, consistent with recommendations for psychotherapy interventions generally (e.g., Dimidjian & Hollon, 2010).
Recommendation 3. Engage the Thorny Question of Clinician Training
To be considered “complete,” stage I work requires attention not only to questions of “promise” but also to the thorny questions of clinician training. These questions are of particular salience given the unique expectations for MBI instructors, which require a personal practice in mindfulness meditation in addition to professional training in the clinical approach. This element may challenge future implementation efforts and has received surprisingly little attention to date in the scientific literature. Operationalizing this requirement and developing scaffolding resources for instructors learning MBI are gaps that exist currently at Stage I. In fact, few studies have examined measures of instructor fidelity (R. S. Crane et al., 2013; Segal, Teasdale, Williams, & Gemar, 2002). The lack of attention to developing formal measures, methods, and standards for determining instructor quality may have its roots in core guiding principles about how MBI is best delivered. For example, in a cautionary note about overreliance on formal guidelines, Kabat-Zinn expressed, “It has always felt to me that MBSR is at its healthiest and best when the responsibility to ensure its integrity, quality, and standards of practice is being carried by each MBSR instructor him or herself…to keep it very real and close to our everyday experience held in awareness with kindness and discernment.” It will be important for the field to grapple directly with tensions that may exist in the very foundation of the scientific study of MBI and that may be accentuated as research on these interventions expands from early Stage I work to larger, more distributed later stage studies.
Recommendation 4. It’s Time to Get Specific About the Specific Effects of MBI
The main strength of Stage II research is the use of randomized designs and intervention controls that support inference about causality. As Tables 1 and 2 illustrate, such work has been conducted with a greater emphasis on randomized comparisons to WLC or TAU than to active controls. Such designs permit valid inference about whether the MBI produces an effect on the measured outcome but not about what, specifically, is driving the effect. MBIs are multimodal interventions. Although a frequent and automatic assumption is that mindfulness meditation is the “active ingredient,” findings are equivocal.
Segal et al. (2010) compared MBCT to maintenance pharmacotherapy, the current standard of care for preventing depressive relapse, and a pill placebo condition. The lack of differences in relapse prevention between MBCT and maintenance pharmacotherapy among patients with residual depressive symptoms suggested that MBCT offers benefit on par with pharmacological treatment, and the superiority of MBCT relative to the placebo control suggested that such benefits are specific to components of MBCT rather than factors common to clinical care that were also present in the placebo condition—a credible rationale, clear guidelines for action, expectancies for improvement, and a positive working alliance with a treatment provider. However, this comparison did not control for other relevant dimensions such as time with clinicians, group support, and completing home practices. Thus, the question remains: is the mindfulness meditation component specifically efficacious?
MBCT showed no significant benefit as compared to an educational control for caregivers of dementia patients, although both active treatments outperformed a respite only control (Oken et al., 2010). In contrast, MBCT demonstrated superiority to psychoeducational controls for treatment of refractory depressed patients (Chiesa, Mandelli, & Serretti, 2012), and specific benefits on some outcomes as compared to a relaxation control for patients with tinnitus (Philippot, Nef, Clauw, de Romree, & Segal, 2012).
Studies of MBSR provide similarly complex findings, reporting failure to outperform an active control on primary outcomes but often mixed results on secondary outcomes. Studies of MBSR among patients with chronic pain have reported no significant differences on subjective reports, such as pain intensity, distress, quality of life, and mood, as compared to a multidisciplinary pain intervention (S. Y. S. Wong et al., 2011) or active control or waitlist (Schmidt et al., 2011). A comparison of MBSR and stress management education among patients with generalized anxiety disorder also found no evidence of superiority for MBSR on the primary outcome of anxiety symptom severity, but reported advantage on secondary anxiety outcomes (Hoge et al., 2013). Finally, among nonclinical participants, comparison between MBSR and an active control, the Health Enhancement Program, which was matched to MBSR in elements that were known to reduce stress but were not tied to the practice of mindfulness (e.g. group support, physical activity), indicated no significant benefit associated with MBSR on subjective reports of well being, some benefit on a behavioral pain task (MacCoon et al., 2012), and benefit on biological indices of stress provoked inflammatory response (Rosenkranz et al., 2013).
Interpretation of the mixed findings from studies using active control conditions is complicated even further by the fact that few active controls have been truly matched to MBSR or MBCT on all components except the mindfulness. For example, the degree to which participants in control conditions are provided with equivalent support for home practice is difficult to determine from many published reports; MBSR and MBCT protocols typically include written and audio guide support for daily home practice and it is not clear whether active controls match this element. Moreover, although some active controls carefully match the frequency and duration of sessions (e.g., Philippot et al., 2012), others are structurally different, involving shorter sessions (e.g., Y. W. Kim et al., 2009). Also, few studies have tested the degree to which instructors find the interventions they are delivering to be credible, thus introducing the possibility of allegiance effects contributing to differences in outcomes across groups. Even comprehensive active controls such as the Health Enhancement Program introduce different teachers for each module of the curriculum, unlike MBSR or MBCT in which the same teacher guides the group for the entire eight sessions (MacCoon et al., 2012). The challenge of developing credible and structurally equivalent psychosocial protocols to control for common factors is not new to psychotherapy research, but it is an important task for the field in order to answer clearly the question of whether mindfulness meditation is an “active ingredient” of MBI. This recommendation is consistent with a recent meta-analysis of the clinical applications of meditation (Goyal et al., 2014), which reported small to moderate effects and little evidence of specific efficacy.
Testing the assumption that mindfulness meditation is specifically efficacious is necessary but not sufficient to advance the field. It is important also to understand more precisely about the importance of mindfulness meditation practice itself. Just how much meditation (if any) is required to achieve clinical benefit? The studies that touch upon this question are mapped currently at Stage I because they rely largely on post hoc analyses of the association between practice time or class attendance and change in symptoms or self-reported mindfulness skill. Findings are mixed, with some studies supporting an association between amount of practice and clinical outcomes (Beddoe & Murphy, 2004; Carmody & Baer, 2008; Collard, Avny, & Boniwell, 2008; del Re, Flückiger, Goldberg, & Hoyt, 2013; Farb, Segal, & Anderson, 2013; Cynthia R. Gross et al., 2004; Rosenzweig et al., 2010; Shapiro, Bootzin, Figueredo, Lopez, & Schwartz, 2003; Shapiro, Jazaieri, & Goldin, 2012), but not all (Carlson, Speca, Patel, & Goodey, 2004; Dobkin & Zhao, 2011; A. Hopkins & Proeve, 2013; MacCoon et al., 2012). The field requires Stage II randomized controlled trials that manipulate dosage or intervention duration as a primary aim. Similarly, basic research studies that examine the validity of methods of assessing practice time and quality are essential. Such findings will bear directly on subsequent stages of research. One can easily imagine patients, referring providers, and health plan administrators asking questions such as, “Can we deliver this in six sessions instead of eight?” or, “Does it really matter if I practice 10 minutes a day rather than 45 minutes?” Stage II studies are well poised to answer such questions.
Recommendation 5. Consider Skipping to but Not Over Stage III
Stage III has been underemphasized in studies of MBI (and clinical psychological science generally). As defined by Onken et al. (2014), a Stage III study is “a well-controlled, internally valid study in a community setting with community therapists/providers” (page 29). This stage of work has two primary functions in the domain of MBI. First, it is well suited for efficacy tests of the type of self-guided materials that are widely available, including workbooks and audio-guides, and is relevant for testing future applications of MBI using web-based or other technology-based delivery tools. Such interventions do not require clinician training materials because they target the patient directly; thus, it may be warranted, in some cases, for studies to proceed directly from Stage I to Stage III. In such cases, the recommendations regarding appropriate control conditions at Stage II are of particular importance at Stage III. Stage III studies of self-guided materials benefit from comparison to TAU to establish evidence of equivalent or superior benefit to standard of care in various healthcare domains. However, comparisons to active controls are critical to validate the specific efficacy of the mindfulness components over and above expectancies, contact time, and other potentially active ingredients. Although there were insufficient studies at Stage III to allow us to map them at this level of granularity, we think such distinctions are critical for the future development of the field. Second, tests of efficacy of instructor delivered MBI in the community help to determine whether results from Stage II studies will “hold up” when the MBI is delivered in routine settings by community providers. Thus, researchers are cautioned against “skipping” this stage of work; it is crucial for informing which interventions justify movement to Stage IV.
Of the studies we reviewed, only two were identified that approached the criteria for Stage III. This classification is arguable given the pilot nature of the work and the hybrid use of community and research clinicians; however, both studies provide instructive examples of the ways in which an MBI can be delivered in an innovative manner directly to recipients in the community. N. J. Thompson et al. (2010) compared “distance delivery” of MBCT via telephone or internet for patients with epilepsy and depressive symptoms (N = 40), as compared to WLC, and the intervention was co-facilitated by a layperson with epilepsy and a master's of public health student. Similarly, (Niles et al., 2012) conducted a feasibility test (N = 33) of a mixed delivery format in which veterans with PTSD were randomized to either an MBSR intervention or a psychoeducation control, both of which included two in person and six telephone-based sessions.
Recommendation 6. Efficacy is Necessary but Not Sufficient for Effectiveness
Only two trials of MBCT and one of MBSR were published prior to 2014 that addressed questions of effectiveness, with two focused specifically on economic outcomes. Specifically, Kuyken et al. (2008) examined the effects of MBCT as compared to maintenance pharmacotherapy among patients treated in primary care, with results suggesting comparable relapse prevention and cost effectiveness as well as advantage to MBCT on indices of reducing residual depressive symptoms, psychiatric comorbidity, and quality of life. van Ravesteijn, Lucassen, Bor, van Weel, and Speckens (2013) examined the cost-effectiveness of MBCT compared with TAU among patients with persistent medically unexplained symptoms, with results indicating lower hospital costs and higher mental health care costs among patients receiving MBCT. Fjorback, Arendt, et al. (2013) also examined economic outcomes of MBSR as compared to care as usual for somatic symptom disorders, and significant benefits for MBSR were reported on disability pension outcomes.
Studies like these make good use of the “care as usual” control groups that can be a progress-limiting factor for earlier stage work. The frequent calls for more rigorous active control groups and caution about care-as-usual comparisons miss the public health relevance of such designs at Stage IV. Care-as-usual comparisons, particularly in the context of healthcare settings in which such care can be precisely described, allow us to determine whether MBI add incremental benefit to what is available. Such studies provide a necessary foundation for Stage IV and V work.
Recommendation 7. Beware of Developing Orphan Innovations, Falling Off the Implementation Cliff, and Getting Caught in “Implementation Limbo”
Only three studies, two of which are purely descriptive, addressed as a primary aim questions relevant to the dissemination or broad implementation of MBI. Specifically, R. S. Crane and Kuyken (2013) conducted a survey with participants in a workshop on implementation of MBCT and an online national survey of MBCT teachers and stakeholders. Results described a range of barriers and facilitators to MBCT implementation, including structural, political, cultural, educational, emotional and physical or technological factors. Lab and colleagues (2012) examined preferences of employees from large healthcare organizations for MBCT targeting depression relapse prevention delivered by in-person group, online group, in-person individual, and telephone-based individual format. Finally, Patten and Meadows (2009) examined data were from the Canadian Community Health Survey to construct a simulation model that estimated population density required to support sustained delivery of in-person MBCT. Results suggested that implementation of such group-based in-person approaches may be challenging in small population centers.
The lack of attention to Stage V work is a serious gap in an effort to develop a clinical science of MBI. Current estimates suggest that, at best, only one in three people who struggle with mental health problems will receive “at least minimally adequate treatment” (Wang et al., 2005). There is a tremendous unmet need for care. If MBI approaches are to have a meaningful impact, they must overcome not only barriers to dissemination and implementation that are common to other approaches (e.g., service costs, waiting lists, and distance to access intervention), but also unique barriers due to instructor competencies.
Given its early stage of development as a field, researchers and practitioners of MBIs may benefit from lessons learned in the study of efforts to disseminate and implement other psychosocial interventions. Three cautions are particularly salient. First, based on their experience developing and disseminating a method of redistributing “edible but not sellable” fresh produce to low income populations, Evans and Clarke (2011) describe the problem of “orphan innovations,” in which effort is dedicated to the design and initial testing of an intervention but little care is allocated to the task of spreading the intervention to contexts of need. Second, Weisz, Ng, and Bearman (2014) refer to the “implementation cliff” to describe the “voltage drop” that often occurs as interventions move through the clinical science process. As interventions are “scaled up” for dissemination in community settings or are delivered in successive generations following the original intervention developer, outcomes suffer. Third, Weisz (2014) also describe the problem of “implementation limbo” in which resource constraints set the “bar” for training providers at ever lower levels: “If there is no evidence that 4 days of expert-led training, and subsequent individual clinician supervision, are required to maintain fidelity and benefit, then why not reduce cost with a 2-day training and group supervision and have local clinical staff conduct the training and supervision?” (p. 60).
Although it is too early to render definitive judgment on the clinical science of MBI, the saturation of studies at Stage I and Stage II using WLC or TAU controls, and the relative paucity of studies at later stages, highlights the risk of neglecting promising interventions as “orphans” early in the research process. Moreover, the relative lack of attention to studying methods of training instructors that can be broadly implemented may make MBI approaches vulnerable to both the implementation cliff and limbo. Fortunately, the emerging field of MBI also stands to learn from the successes of others. Recent discussions have focused, in particular, on the model of “disruptive innovation” in which new technologies may be integrated in the service of increasing reach and access of MBI. Recommendations within general psychotherapy domains have included the examination of novel delivery formats such as self-management and self-help formats, brief or more parsimonious adaptations, technology and media driven delivery formats, and integration within broader healthcare packages (Kazdin & Blase, 2011; Rotheram-Borus, Swendeman, & Chorpita, 2012). Such avenues may represent great promise for the dissemination and implementation of MBI; however, they are likely also to raise complex questions that the field must tackle. As Simon and Ludman (2009) note in a discussion of disruptive innovation for cognitive behavioral treatments, “Traditional therapists might be horrified by the prospect of an overseas cognitive behavioural call centre or live-chat centre, available whenever patients choose. But the expectations of health-care providers are not the same as evidence. And the evidence that matters concerns clinical benefit and economic value to patients, rather than appeal or value to providers” (p. 595). It will be essential for clinical innovators and researchers to examine methods of delivery for MBI that will provide such evidence.
Indications of Promise
There are encouraging indications that the field is moving in the directions highlighted in this review. Although our comprehensive mapping was limited to studies published through 2013, the field is advancing rapidly, and an examination of notable studies published since 2014 indicates significant advances in three domains.
First, we find indicators that the field is becoming more programmatic in its approach by anchoring clinical intervention in basic research that specifies clear targets of intervention and by testing proposed mechanisms of change. This is evident, for example, in recent work on substance use disorders that represent novel “next generation” interventions combining elements of MBSR or MBCT, singly, or with other interventions in novel ways. Garland and colleagues (2014) tested both clinical outcomes and mediators of an MBI developed specifically for chronic pain and prescription opioid misuse (mindfulness-oriented recovery enhancement) in the context of a Stage II randomized clinical trial with an active control (supportive group therapy). It may be valuable to use the mapping approach undertaken here to chart the development of these next generation MBIs and the ways in which the structure and content of the interventions are modified to fit the nature of the target problem or population. Moreover, an increased recent emphasis on identifying mediators of change in MBI represents an important step in advancing research in an integrated and systematic manner (Gu, Strauss, Bond, & Cavanagh, 2015; van der Velden et al., 2015).
Second, more studies are incorporating active control conditions that can help to address questions of specific efficacy. J. M. G. Williams et al. (2014) compared MBCT to TAU and to a cognitive psychoeducation program developed to emphasize the didactic elements of relapse prevention without the experiential mindfulness practice. The results indicated no difference in relapse rates over a 1-year follow-up among the three groups—a finding that challenges the specific efficacy of the mindfulness meditation component of MBCT. A subgroup analysis of patients with histories of childhood trauma, however, indicated significant benefit for MBCT. It is possible that MBCT may show specific benefit for more vulnerable individuals, as was the case in the original studies that examined differences by number of prior episodes (Ma & Teasdale, 2004; Teasdale et al., 2000). Although caution should be exercised in the interpretation of post hoc subgroup analyses, such findings may warrant “returning” to work at Stage 0 to help understand the nature of such vulnerabilities, including mechanisms that might be preferentially addressed through training in mindfulness meditation for such individuals.
Third, given that the stage model was developed to maximize public health impact of psychosocial treatments, it is encouraging that investigators are extending promising work at Stage I and II to examine questions of effectiveness, dissemination, and implementation. The work of Bowen et al. (2014) provides an excellent example of rigorous movement toward Stage III research in which the MBI developed for preventing relapse in substance abuse disorders (mindfulness-based relapse prevention) was tested in a randomized clinical trial with comparison to an active control (cognitive behavioral relapse prevention) and TAU. This study represented a hybrid of Stage II and III research because research clinicians delivered the 8-week intervention in community chemical dependency treatment facilities. Moreover, although TAU comparison groups have been highly heterogeneous in prior studies, this study represents an advance by implementing the study in the context of a specific healthcare setting that allowed, TAU to be clearly defined and measured. The use of comparison conditions that address questions of high relevance to healthcare consumers also signals an important advance. For example, the trial comparing MBCT (with support to discontinue antidepressant medication) to maintenance antidepressant medication (Kuyken et al., 2015) has the potential to address the questions that are at the forefront for many patients seeking care. Specifically, patients and providers want to know how does the MBI compare to other available options. Findings from Kuyken et al. (2015) indicate that relapse rates are statistically equivalent in MBCT and maintenance antidepressant medication, the current standard of care for recurrent depression. Finally, the potential for broad dissemination via web-based delivery also may help to accelerate the pace of Stage III–V research (Boettcher et al., 2014; Dimidjian et al., 2014).
Summary
The science and practice of MBI has reached an important point in its development. The last decade has witnessed an exponential rate of increase in the number of studies and the breadth of clinical problems and populations targeted. We contend that the public health impact of this work is likely to be enhanced by situating work on MBI in a broader framework of clinical psychological science. Doing so highlights important lessons and gaps in our current evidence base. Simply accumulating a greater number of the same types of studies without addressing such gaps is unlikely to advance the field. Although there are indications from recent studies that the field is moving in a positive direction, an integrated and systematic approach to core research questions, to the methodological quality of individual studies at each stage, and to increasing logical links between the stages, will enhance our ability to impact positively the mental health needs of individuals and communities.
Acknowledgments
Dimidjian and Segal receive royalties from Guilford Press for work related to Mindfulness-Based Cognitive Therapy and are on the advisory board of Mindful Noggins, which is part of NogginLabs, a private company specializing in customized web based learning.
Biographies


Contributor Information
Sona Dimidjian, University of Colorado Boulder.
Zindel V. Segal, University of Toronto Scarborough
References
- Abercrombie PD, Zamora A, Korn AP. Lessons learned: providing a mindfulness-based stress reduction program for low-income multiethnic women with abnormal pap smears. Holistic Nursing Practice. 2007;21(1):26–34. doi: 10.1097/00004650-200701000-00006. [DOI] [PubMed] [Google Scholar]
- Alberts HJ, Thewissen R, Raes L. Dealing with problematic eating behaviour. The effects of a mindfulness-based intervention on eating behaviour, food cravings, dichotomous thinking and body image concern. Appetite. 2012;58(3):847–851. doi: 10.1016/j.appet.2012.01.009. [DOI] [PubMed] [Google Scholar]
- Allen M, Bromley A, Kuyken W, Sonnenberg SJ. Participants' experiences of mindfulness-based cognitive therapy: "It changed me in just about every way possible". Behavioural and Cognitive Psychotherapy. 2009;37(4):413–430. doi: 10.1017/S135246580999004X. [DOI] [PubMed] [Google Scholar]
- Altschuler A, Rosenbaum E, Gordon P, Canales S, Avins AL. Audio recordings of mindfulness-based stress reduction training to improve cancer patients’ mood and quality of life—a pilot feasibility study. Supportive Care in Cancer. 2012;20(6):1291–1297. doi: 10.1007/s00520-011-1216-7. [DOI] [PubMed] [Google Scholar]
- Andersen SR, Wurtzen H, Steding-Jessen M, Christensen J, Andersen KK, Flyger H, Dalton SO. Effect of mindfulness-based stress reduction on sleep quality: results of a randomized trial among Danish breast cancer patients. Acta Oncologica. 2013;52(2):336–344. doi: 10.3109/0284186x.2012.745948. [DOI] [PubMed] [Google Scholar]
- Anderson ND, Lau MA, Segal ZV, Bishop SR. Mindfulness-based stress reduction and attentional control. Clinical Psychology & Psychotherapy. 2007;14(6):449–463. doi: 10.1002/cpp.544. [DOI] [Google Scholar]
- Arch JJ, Ayers CR. Which treatment worked better for whom? Moderators of group cognitive behavioral therapy versus adapted mindfulness based stress reduction for anxiety disorders. Behaviour Research and Therapy. 2013;51(8):434–442. doi: 10.1016/j.brat.2013.04.004. [DOI] [PubMed] [Google Scholar]
- Arch JJ, Ayers CR, Baker A, Almklov E, Dean DJ, Craske MG. Randomized clinical trial of adapted mindfulness-based stress reduction versus group cognitive behavioral therapy for heterogeneous anxiety disorders. Behaviour Research and Therapy. 2013;51(4–5):185–196. doi: 10.1016/j.brat.2013.01.003. doi: http://dx.doi.org/10.1016/j.brat.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Azulay J, Smart CM, Mott T, Cicerone KD. A pilot study examining the effect of mindfulness-based stress reduction on symptoms of chronic mild traumatic brain injury/postconcussive syndrome. Journal of Head Trauma Rehabilitation. 2013;28(4):323–331. doi: 10.1097/HTR.0b013e318250ebda. [DOI] [PubMed] [Google Scholar]
- Baer RA, Carmody J, Hunsinger M. Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2012;68(7):755–765. doi: 10.1002/jclp.21865. [DOI] [PubMed] [Google Scholar]
- Baer RA, Fischer S, Huss DB. Mindfulness-based cognitive therapy applied to binge eating: A case study. Cognitive and Behavioral Practice. 2005;12(3):351–358. doi: http://dx.doi.org/10.1016/S1077-7229(05)80057-4. [Google Scholar]
- Baer RA, Fischer S, Huss DB. Mindfulness and acceptance in the treatment of disordered eating. Journal of Rational-Emotive and Cognitive-Behavior Therapy. 2005;23(4):281–300. doi: http://dx.doi.org/10.1007/s10942-005-0015-9. [Google Scholar]
- Bailie C, Kuyken W, Sonnenberg S. The experiences of parents in mindfulness-based cognitive therapy. Clinical Child Psychology and Psychiatry. 2012;17(1):103–119. doi: 10.1177/1359104510392296. [DOI] [PubMed] [Google Scholar]
- Barbosa P, Raymond G, Zlotnick C, Wilk J, Toomey R, III, Mitchell J., III Mindfulness-based stress reduction training is associated with greater empathy and reduced anxiety for graduate healthcare students. Education for Health: Change in Learning & Practice. 2013;26(1):9–14. doi: 10.4103/1357-6283.112794. [DOI] [PubMed] [Google Scholar]
- Barnhofer T, Crane C, Hargus E, Amarasinghe M, Winder R, Williams JMG. Mindfulness-based cognitive therapy as a treatment for chronic depression: A preliminary study. Behaviour Research and Therapy. 2009;47(5):366–373. doi: 10.1016/j.brat.2009.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnhofer T, Duggan D, Crane C, Hepburn S, Fennell MJV, Williams JMG. Effects of meditation on frontal [alpha]-asymmetry in previously suicidal individuals. Neuroreport. 2007;18(7):709–712. doi: 10.1097/WNR.0b013e3280d943cd. [DOI] [PubMed] [Google Scholar]
- Bazarko D, Cate RA, Azocar F, Kreitzer MJ. The impact of an innovative mindfulness-based stress reduction program on the health and well-being of nurses employed in a corporate setting. Journal of Workplace Behavioral Health. 2013;28(2):107–133. doi: 10.1080/15555240.2013.779518. doi: http://dx.doi.org/10.1080/15555240.2013.779518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bédard M, Felteau M, Gibbons C, Klein R, Mazmanian D, Fedyk K, Mack G. A mindfulness-based intervention to improve quality of life among individuals who sustained traumatic brain injuries: One year follow-up. Journal of Cognitive Rehabilitation. 2005;23(1):8–13. doi: 10.1080/0963828031000090489. [DOI] [PubMed] [Google Scholar]
- Bédard M, Felteau M, Mazmanian D, Fedyk K, Klein R, Richardson J, Minthorn-Biggs MB. Pilot evaluation of a mindfulness-based intervention to improve quality of life among individuals who sustained traumatic brain injuries. Disability and Rehabilitation. 2003;25(13):722–731. doi: 10.1080/0963828031000090489. [DOI] [PubMed] [Google Scholar]
- Beddoe AE, Murphy SO. Does mindfulness decrease stress and foster empathy among nursing students? Journal of Nursing Education. 2004;43(7):305–312. doi: 10.3928/01484834-20040701-07. [DOI] [PubMed] [Google Scholar]
- Bergen-Cico D, Possemato K, Cheon S. Examining the efficacy of a brief mindfulness-based stress reduction (brief MBSR) program on psychological health. Journal of American College Health. 2013;61(6):348–360. doi: 10.1080/07448481.2013.813853. doi: http://dx.doi.org/10.1080/07448481.2013.813853. [DOI] [PubMed] [Google Scholar]
- Bermudez D, Benjamin MT, Porter SE, Saunders PA, Myers NA, Dutton MA. A qualitative analysis of beginning mindfulness experiences for women with post-traumatic stress disorder and a history of intimate partner violence. Complementary Therapies in Clinical Practice. 2013;19(2):104–108. doi: 10.1016/j.ctcp.2013.02.004. [DOI] [PubMed] [Google Scholar]
- Biegel GM, Brown KW, Shapiro SL, Schubert CM. Mindfulness-based stress reduction for the treatment of adolescent psychiatric outpatients: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77(5):855–866. doi: 10.1037/a0016241. [DOI] [PubMed] [Google Scholar]
- Bieling PJ, Hawley LL, Bloch RT, Corcoran KM, Levitan RD, Young LT, Segal ZV. Treatment-specific changes in decentering following mindfulness-based cognitive therapy versus antidepressant medication or placebo for prevention of depressive relapse. Journal of Consulting and Clinical Psychology. 2012;80(3):365–372. doi: 10.1037/a0027483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnie K, Garland SN, Carlson LE. Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR) Psycho-Oncology. 2010;19(9):1004–1009. doi: 10.1002/pon.1651. [DOI] [PubMed] [Google Scholar]
- Birnie K, Speca M, Carlson LE. Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR) Stress and Health: Journal of the International Society for the Investigation of Stress. 2010;26(5):359–371. doi: http://dx.doi.org/10.1002/smi.1305. [Google Scholar]
- Boettcher J, Astrom V, Pahlsson D, Schenstrom O, Andersson G, Carlbring P. Internet-based mindfulness treatment for anxiety disorders: a randomized controlled trial. Behavior Therapy. 2014;45(2):241–253. doi: 10.1016/j.beth.2013.11.003. [DOI] [PubMed] [Google Scholar]
- Bondolfi G, Jermann F, Van der Linden M, Gex-Fabry M, Bizzini L, Rouget BW, Bertschy G. Depression relapse prophylaxis with Mindfulness-Based Cognitive Therapy: Replication and extension in the Swiss health care system. Journal of Affective Disorders. 2010;122(3):224–231. doi: 10.1016/j.jad.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostanov V, Keune PM, Kotchoubey B, Hautzinger M. Event-related brain potentials reflect increased concentration ability after mindfulness-based cognitive therapy for depression: A randomized clinical trial. Psychiatry Research. 2012;199(3):174–180. doi: 10.1016/j.psychres.2012.05.031. [DOI] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, Larimer ME. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry. 2014;71(5):547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady S, O'Connor N, Burgermeister D, Hanson P. The impact of mindfulness meditation in promoting a culture of safety on an acute psychiatric unit. Perspectives in Psychiatric Care. 2012;48(3):129–137. doi: 10.1111/j.1744-6163.2011.00315.x. [DOI] [PubMed] [Google Scholar]
- Bränström R, Kvillemo P, Åkerstedt T. Effects of mindfulness training on levels of cortisol in cancer patients. Psychosomatics: Journal of Consultation and Liaison Psychiatry. 2013;54(2):158–164. doi: 10.1016/j.psym.2012.04.007. doi: http://dx.doi.org/10.1016/j.psym.2012.04.007. [DOI] [PubMed] [Google Scholar]
- Britton WB, Haynes PL, Fridel KW, Bootzin RR. Polysomnographic and subjective profiles of sleep continuity before and after mindfulness-based cognitive therapy in partially remitted depression. Psychosomatic Medicine. 2010;72(6):539–548. doi: 10.1097/PSY.0b013e3181dc1bad. [DOI] [PubMed] [Google Scholar]
- Britton WB, Haynes PL, Fridel KW, Bootzin RR. Mindfulness-based cognitive therapy improves polysomnographic and subjective sleep profiles in antidepressant users with sleep complaints. Psychotherapy and Psychosomatics. 2012;81:296–304. doi: 10.1159/000332755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton WB, Shahar B, Szepsenwol O, Jacobs WJ. Mindfulness-Based Cognitive Therapy Improves Emotional Reactivity to Social Stress: Results from a Randomized Controlled Trial. Behavior Therapy. 2012;43(2):365–380. doi: 10.1016/j.beth.2011.08.006. doi: http://dx.doi.org/10.1016/j.beth.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotto LA, Erskine Y, Carey M, Ehlen T, Finlayson S, Heywood M, Miller D. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecologic Oncology. 2012;125(2):320–325. doi: 10.1016/j.ygyno.2012.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell TS, Labelle LE, Bacon SL, Faris P, Carlson LE. Impact of Mindfulness-Based Stress Reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer: a waitlist-controlled study. Journal of Behavioral Medicine. 2012;35(3):262–271. doi: 10.1007/s10865-011-9357-1. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. International Journal of Behavioral Medicine. 2005;12(4):278–285. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain, Behavior, and Immunity. 2007;21(8):1038–1049. doi: 10.1016/j.bbi.2007.04.002. doi: http://dx.doi.org/10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosomatic Medicine. 2003;65(4):571–581. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29(4):448–474. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine. 2008;31(1):23–33. doi: 10.1007/s10865-007-9130-7. doi: http://dx.doi.org/10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology. 2009;65(6):627–638. doi: 10.1002/jclp.20555. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA, B LEL, Olendzki N. An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2009;65(6):613–626. doi: 10.1002/jclp.20579. [DOI] [PubMed] [Google Scholar]
- Carmody J, Crawford S, Churchill L. A pilot study of mindfulness-based stress reduction for hot flashes. Menopause. 2006;13(5):760–769. doi: 10.1097/01.gme.0000227402.98933.d0. [DOI] [PubMed] [Google Scholar]
- Carmody J, Crawford S, Salmoirago-Blotcher E, Leung K, Churchill L, Olendzki N. Mindfulness training for coping with hot flashes: results of a randomized trial. Menopause (New York, NY) 2011;18(6):611. doi: 10.1097/gme.0b013e318204a05c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmody J, Reed G, Kristeller J, Merriam P. Mindfulness, spirituality, and health-related symptoms. Journal of Psychosomatic Research. 2008;64:393–403. doi: 10.1016/j.jpsychores.2007.06.015. [DOI] [PubMed] [Google Scholar]
- Carroll D, Lange B, Liehr P, Raines S, Marcus MT. Evaluating mindfulness-based stress reduction: Analyzing stories of stress to formulate focus group questions. Archives of Psychiatric Nursing. 2008;22(2):107–109. doi: 10.1016/j.apnu.2007.12.004. doi: http://dx.doi.org/10.1016/j.apnu.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cebolla i Martí A, Barrachina MTM. The effects of mindfulness-based cognitive therapy: A qualitative approach. Psychology in Spain. 2009;13(1):9–16. [Google Scholar]
- Chambers SK, Foley E, Galt E, Ferguson M, Clutton S. Mindfulness groups for men with advanced prostate cancer: a pilot study to assess feasibility and effectiveness and the role of peer support. Supportive Care in Cancer. 2012;20(6):1183–1192. doi: 10.1007/s00520-011-1195-8. [DOI] [PubMed] [Google Scholar]
- Chang VY, Palesh O, Caldwell R, Glasgow N, Abramson M, Luskin F, Koopman C. The effects of a mindfulness-based stress reduction program on stress, mindfulness self-efficacy, and positive states of mind. Stress and Health. 2004;20(3):141–147. doi: 10.1002/smi.1011. [DOI] [Google Scholar]
- Chiesa A, Mandelli L, Serretti A. Mindfulness-based cognitive therapy versus psycho-education for patients with major depression who did not achieve remission following antidepressant treatment: A preliminary analysis. The Journal of Alternative & Complementary Medicine. 2012;18(8):756–760. doi: 10.1089/acm.2011.0407. [DOI] [PubMed] [Google Scholar]
- Cohen-Katz J, Wiley S, Capuano T, Baker DM, Deitrick L, Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout: a qualitative and quantitative study, part III. Holistic Nursing Practice. 2005;19(2):78–86. doi: 10.1097/00004650-200503000-00009. [DOI] [PubMed] [Google Scholar]
- Cohen-Katz J, Wiley SD, Capuano T, Baker DM, Kimmel S, Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout, Part II: A quantitative and qualitative study. Holistic Nursing Practice. 2005;19(1):26–35. doi: 10.1097/00004650-200501000-00008. [DOI] [PubMed] [Google Scholar]
- Cohen-Katz J, Wiley SD, Capuano T, Baker DM, Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout: a quantitative and qualitative study. Holistic Nursing Practice. 2004;18(6):302–308. doi: 10.1097/00004650-200411000-00006. [DOI] [PubMed] [Google Scholar]
- Collard P, Avny N, Boniwell I. Teaching Mindfulness Based Cognitive Therapy (MBCT) to students: The effects of MBCT on the levels of Mindfulness and Subjective Well-Being. Counselling Psychology Quarterly. 2008;21(4):323–336. doi: http://dx.doi.org/10.1080/09515070802602112. [Google Scholar]
- Collip D, Geschwind N, Peeters F, Myin-Germeys I, van Os J, Wichers M. Putting a hold on the downward spiral of paranoia in the social world: A randomized controlled trial of mindfulness-based cognitive therapy in individuals with a history of depression. PloS One. 2013;8(6) doi: 10.1371/journal.pone.0066747. doi: http://dx.doi.org/10.1371/journal.pone.0066747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordon SL, Brown KW, Gibson PR. The role of mindfulness-based stress reduction on perceived stress: Preliminary evidence for the moderating role of attachment style. Journal of Cognitive Psychotherapy. 2009;23(3):258–569. doi: http://dx.doi.org/10.1891/0889-8391.23.3.258. [Google Scholar]
- Craigie MA, Rees CS, Marsh A, Nathan P. Mindfulness-based Cognitive Therapy for Generalized Anxiety Disorder: A Preliminary Evaluation. Behavioural and Cognitive Psychotherapy. 2008;36(5):553–568. doi: 10.1017/s135246580800458x. [DOI] [Google Scholar]
- Crane C, Barnhofer T, Duggan DS, Hepburn S, Fennell MV, Williams JMG. Mindfulness-based cognitive therapy and self-discrepancy in recovered depressed patients with a history of depression and suicidality. Cognitive Therapy and Research. 2008;32(6):775–787. doi: 10.1007/s10608-008-9193-y. [DOI] [Google Scholar]
- Crane C, Williams JMG. Factors associated with attrition from mindfulness-based cognitive therapy in patients with a history of suicidal depression. Mindfulness. 2010;1(1):10–20. doi: 10.1007/s12671-010-0003-8. doi: http://dx.doi.org/10.1007/s12671-010-0003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane C, Winder R, Hargus E, Amarasinghe M, Barnhofer T. Effects of mindfulness-based cognitive therapy on specificity of life goals. Cognitive Therapy and Research. 2012;36(3):182–189. doi: 10.1007/s10608-010-9349-4. doi: http://dx.doi.org/10.1007/s10608-010-9349-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane RS, Eames C, Kuyken W, Hastings RP, Williams JM, Bartley T, Surawy C. Development and validation of the mindfulness-based interventions - teaching assessment criteria (MBI:TAC) Assessment. 2013;20(6):681–688. doi: 10.1177/1073191113490790. [DOI] [PubMed] [Google Scholar]
- Crane RS, Kuyken W. The implementation of mindfulness-based cognitive therapy: Learning from the UK health service experience. Mindfulness (N Y) 2013;4:246–254. doi: 10.1007/s12671-012-0121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD, Irwin MR, Burklund LJ, Lieberman MD, Arevalo JM, Ma J, Cole SW. Mindfulness-Based Stress Reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain, Behavior, and Immunity. 2012;26(7):1095–1101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD, Myers HF, Cole SW, Irwin MR. Mindfulness meditation training effects on CD4+ T lymphocytes in HIV-1 infected adults: a small randomized controlled trial. Brain, Behavior, and Immunity. 2009;23(2):184–188. doi: 10.1016/j.bbi.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Fleming MF, Bonus KA, Baker TB. A pilot study on mindfulness based stress reduction for smokers. BMC Complementary and Alternative Medicine. 2007;7:2. doi: 10.1186/1472-6882-7-2. [PubMed] [Cross Ref] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deckersbach T, Holzel BK, Eisner LR, Stange JP, Peckham AD, Dougherty DD, Nierenberg AA. Mindfulness-based cognitive therapy for nonremitted patients with bipolar disorder. CNS Neuroscience & Therapeutics. 2012;18(2):133–141. doi: 10.1111/j.1755-5949.2011.00236.x. [Cross Ref] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degi CL, Szilagy T. Mindfulness-based stress reduction intervention in Romanian breast cancer inpatients. Cognition, Brain, Behavior: An Interdisciplinary Journal. 2013;17(2):135–148. [Google Scholar]
- de Lisle SM, Dowling NA, Allen JS. Mindfulness-based cognitive therapy for problem gambling. Clinical Case Studies. 2011;10(3):210–228. doi: http://dx.doi.org/10.1177/1534650111401016. [Google Scholar]
- del Re AC, Flückiger C, Goldberg SB, Hoyt WT. Monitoring mindfulness practice quality: An important consideration in mindfulness practice. Psychotherapy Research. 2013;23(1):54–66. doi: 10.1080/10503307.2012.729275. doi: http://dx.doi.org/10.1080/10503307.2012.729275. [DOI] [PubMed] [Google Scholar]
- De Raedt R, Baert S, Demeyer I, Goeleven E, Raes A, Visser A, Speckens A. Changes in attentional processing of emotional information following mindfulness-based cognitive therapy in people with a history of depression: Towards an open attention for all emotional experiences. Cognitive Therapy and Research. 2012;36(6):612–620. doi: http://dx.doi.org/10.1007/s10608-011-9411-x. [Google Scholar]
- DeRubeis RJ, Cohen ZD, Forand NR, Fournier JC, Gelfand LA, Lorenzo-Luaces L. The Personalized Advantage Index: translating research on prediction into individualized treatment recommendations. A demonstration. PloS One. 2014;9(1):e83875. doi: 10.1371/journal.pone.0083875. [PubMed] [Cross Ref] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deyo M, Wilson KA, Ong J, Koopman C. Mindfulness and rumination: does mindfulness training lead to reductions in the ruminative thinking associated with depression? Explore (NY) 2009;5(5):265–271. doi: 10.1016/j.explore.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Beck A, Felder JN, Boggs JM, Gallop R, Segal ZV. Web-based Mindfulness-based Cognitive Therapy for reducing residual depressive symptoms: An open trial and quasi-experimental comparison to propensity score matched controls. Behaviour Research and Therapy. 2014;63:83–89. doi: 10.1016/j.brat.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD. How would we know if psychotherapy were harmful? American Psychologist. 2010;65(1):21–33. doi: 10.1037/a0017299. [DOI] [PubMed] [Google Scholar]
- Dobkin PL. Mindfulness-based stress reduction: what processes are at work? Complementary Therapies in Clinical Practice. 2008;14(1):8–16. doi: 10.1016/j.ctcp.2007.09.004. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Zhao Q. Increased mindfulness–The active component of the mindfulness-based stress reduction program? Complementary Therapies in Clinical Practice. 2011;17(1):22–27. doi: 10.1016/j.ctcp.2010.03.002. [DOI] [PubMed] [Google Scholar]
- Duncan LG, Moskowitz JT, Neilands TB, Dilworth SE, Hecht FM, Johnson MO. Mindfulness-based stress reduction for HIV treatment side effects: a randomized, wait-list controlled trial. Journal of Pain and Symptom Management. 2012;43(2):161–171. doi: 10.1016/j.jpainsymman.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn C, Hanieh E, Roberts R, Powrie R. Mindful pregnancy and childbirth: effects of a mindfulness-based intervention on women's psychological distress and well-being in the perinatal period. Arch Womens Ment Health. 2012;15(2):139–143. doi: 10.1007/s00737-012-0264-4. [DOI] [PubMed] [Google Scholar]
- Dutton MA, Bermudez D, Matás A, Majid H, Myers NL. Mindfulness-based stress reduction for low-income, predominantly African American women with PTSD and a history of intimate partner violence. Cognitive and Behavioral Practice. 2013;20(1):23–32. doi: 10.1016/j.cbpra.2011.08.003. doi: http://dx.doi.org/10.1016/j.cbpra.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisendrath S, Chartier M, McLane M. Adapting mindfulness-based cognitive therapy for treatment-resistant depression. Cognitive and Behavioral Practice. 2011;18(3):362–370. doi: 10.1016/j.cbpra.2010.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein-Lubow G, McBee L, Darling E, Armey M, Miller IW. A pilot investigation of mindfulness-based stress reduction for caregivers of frail elderly. Mindfulness. 2011;2(2):95–102. doi: http://dx.doi.org/10.1007/s12671-011-0047-4. [Google Scholar]
- Ernst S, Welke J, Heintze C, Gabriel R, Zollner A, Kiehne S, Esch T. Effects of mindfulness-based stress reduction on quality of life in nursing home residents: a feasibility study. Forsch Komplementmed. 2008;15(2):74–81. doi: 10.1159/000121479. [DOI] [PubMed] [Google Scholar]
- Esmer G, Blum J, Rulf J, Pier J. Mindfulness-based stress reduction for failed back surgery syndrome: a randomized controlled trial. JAOA: Journal of the American Osteopathic Association. 2010;110(11):646–652. [PubMed] [PubMed] [Google Scholar]
- Evans SH, Clarke P. Disseminating Orphan Innovations. Stanford Social Innovation Review. 2011:42–47. [Google Scholar]
- Evans S, Ferrando S, Carr C, Haglin D. Mindfulness-based stress reduction (MBSR) and distress in a community-based sample. Clinical Psychology & Psychotherapy. 2011;18(6):553–558. doi: 10.1002/cpp.727. doi: http://dx.doi.org/10.1002/cpp.727. [DOI] [PubMed] [Google Scholar]
- Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D. Mindfulness-based cognitive therapy for generalized anxiety disorder. Journal of Anxiety Disorders. 2008;22(4):716–721. doi: 10.1016/j.janxdis.2007.07.005. doi. [DOI] [PubMed] [Google Scholar]
- Fang CY, Reibel DK, Longacre ML, Rosenzweig S, Campbell DE, Douglas SD. Enhanced psychosocial well-being following participation in a mindfulness-based stress reduction program is associated with increased natural killer cell activity. The Journal of Alternative and Complementary Medicine. 2010;16(5):531–538. doi: 10.1089/acm.2009.0018. doi: http://dx.doi.org/10.1089/acm.2009.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NAS, Segal ZV, Anderson AK. Mindfulness meditation training alters cortical representations of interoceptive attention. Social Cognitive and Affective Neuroscience. 2013;8(1):15–26. doi: 10.1093/scan/nss066. doi: http://dx.doi.org/10.1093/scan/nss066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finucane A, Mercer SW. An exploratory mixed methods study of the acceptability and effectiveness of Mindfulness-Based Cognitive Therapy for patients with active depression and anxiety in primary care. BMC Psychiatry. 2006;6:14. doi: 10.1186/1471-244X-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick L, Simpson J, Smith A. A qualitative analysis of mindfulness-based cognitive therapy (MBCT) in Parkinson's disease. Psychology and Psychotherapy: Theory, Research and Practice. 2010;83(2):179–192. doi: 10.1348/147608309X471514. [DOI] [PubMed] [Google Scholar]
- Fjorback LO, Arendt M, Ornbol E, Walach H, Rehfeld E, Schroder A, Fink P. Mindfulness therapy for somatization disorder and functional somatic syndromes: Randomized trial with one-year follow-up. Journal of Psychosomatic Research. 2013;74(1):31–40. doi: 10.1016/j.jpsychores.2012.09.006. [DOI] [PubMed] [Google Scholar]
- Fjorback LO, Carstensen T, Arendt M, Ørnbøl E, Walach H, Rehfeld E, Fink P. Mindfulness therapy for somatization disorder and functional somatic syndromes: Analysis of economic consequences alongside a randomized trial. Journal of Psychosomatic Research. 2013;74(1):41–48. doi: 10.1016/j.jpsychores.2012.09.010. doi: http://dx.doi.org/10.1016/j.jpsychores.2012.09.010. [DOI] [PubMed] [Google Scholar]
- Flugel Colle KF, Vincent A, Cha SS, Loehrer LL, Bauer BA, Wahner-Roedler DL. Measurement of quality of life and participant experience with the mindfulness-based stress reduction program. Complementary Therapies in Clinical Practice. 2010;16(1):36–40. doi: 10.1016/j.ctcp.2009.06.008. [DOI] [PubMed] [Google Scholar]
- Foley E, Baillie A, Huxter M, Price M, Sinclair E. Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2010;78(1):72–79. doi: 10.1037/a0017566. [DOI] [PubMed] [Google Scholar]
- Frisvold MH, Lindquist R, McAlpine CP. Living life in the balance at midlife: Lessons learned from mindfulness. Western Journal of Nursing Research. 2012;34(2):265–278. doi: 10.1177/0193945911424171. doi: http://dx.doi.org/10.1177/0193945911424171. [DOI] [PubMed] [Google Scholar]
- Gallegos AM, Hoerger M, Talbot NL, Krasner MS, Knight JM, Moynihan JA, Duberstein PR. Toward identifying the effects of the specific components of Mindfulness-Based Stress Reduction on biologic and emotional outcomes among older adults. Journal of Alternative and Complementary Medicine. 2013;19(10):787–792. doi: 10.1089/acm.2012.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallegos AM, Hoerger M, Talbot NL, Moynihan JA, Duberstein PR. Emotional benefits of mindfulness-based stress reduction in older adults: The moderating roles of age and depressive symptom severity. Aging & Mental Health. 2013;17(7):823–829. doi: 10.1080/13607863.2013.799118. doi: http://dx.doi.org/10.1080/13607863.2013.799118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gans JJ, O’Sullivan P, Bircheff V. Mindfulness based tinnitus stress reduction pilot study. Mindfulness. 2013;5(4):322–333. doi: 10.1007/s12671-012-0184-4. [DOI] [Google Scholar]
- Garland EL, Gaylord SA, Palsson O, Faurot K, Mann JD, Whitehead WE. Therapeutic mechanisms of a mindfulness-based treatment for IBS: Effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. Journal of Behavioral Medicine. 2012;35(6):591–602. doi: 10.1007/s10865-011-9391-z. doi: http://dx.doi.org/10.1007/s10865-011-9391-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Manusov EG, Froeliger B, Kelly A, Williams JM, Howard MO. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: results from an early-stage randomized controlled trial. Journal of Consulting and Clinical Psychology. 2014;82(3):448–459. doi: 10.1037/a0035798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland SN, Carlson LE, Cook S, Lansdell L, Speca M. A non-randomized comparison of mindfulness-based stress reduction and healing arts programs for facilitating post-traumatic growth and spirituality in cancer outpatients. Supportive Care in Cancer. 2007;15(8):949–961. doi: 10.1007/s00520-007-0280-5. [DOI] [PubMed] [Google Scholar]
- Garland SN, Tamagawa R, Todd SC, Speca M, Carlson LE. Increased mindfulness is related to improved stress and mood following participation in a mindfulness-based stress reduction program in individuals with cancer. Integrative Cancer Therapies. 2013;12(1):31–40. doi: 10.1177/1534735412442370. [DOI] [PubMed] [Google Scholar]
- Gayner B, Esplen MJ, DeRoche P, Wong J, Bishop S, Kavanagh L, Butler K. A randomized controlled trial of mindfulness-based stress reduction to manage affective symptoms and improve quality of life in gay men living with HIV. Journal of Behavioral Medicine. 2012;35(3):272–285. doi: 10.1007/s10865-011-9350-8. [DOI] [PubMed] [Google Scholar]
- Geary C, Rosenthal SL. Sustained impact of MBSR on stress, well-being, and daily spiritual experiences for 1 year in academic health care employees. The Journal of Alternative and Complementary Medicine. 2011;17(10):939–944. doi: 10.1089/acm.2010.0335. doi: http://dx.doi.org/10.1089/acm.2010.0335. [DOI] [PubMed] [Google Scholar]
- Geschwind N, Peeters F, Drukker M, van Os J, Wichers M. Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2011;79(5):618–628. doi: 10.1037/a0024595. doi: http://dx.doi.org/10.1037/a0024595. [DOI] [PubMed] [Google Scholar]
- Geschwind N, Peeters F, Huibers M, van Os J, Wichers M. Efficacy of mindfulness-based cognitive therapy in relation to prior history of depression: randomised controlled trial. British Journal of Psychiatry. 2012;201(4):320–325. doi: 10.1192/bjp.bp.111.104851. [DOI] [PubMed] [Google Scholar]
- Gex-Fabry M, Jermann F, Kosel M, Rossier MF, Van der Linden M, Bertschy G, Aubry J-M. Salivary cortisol profiles in patients remitted from recurrent depression: One-year follow-up of a mindfulness-based cognitive therapy trial. Journal of Psychiatric Research. 2012;46(1):80–86. doi: 10.1016/j.jpsychires.2011.09.011. doi: http://dx.doi.org/10.1016/j.jpsychires.2011.09.011. [DOI] [PubMed] [Google Scholar]
- Godfrin KA, van Heeringen C. The effects of mindfulness-based cognitive therapy on recurrence of depressive episodes, mental health and quality of life: A randomized controlled study. Behaviour Research and Therapy. 2010;48(8):738–746. doi: 10.1016/j.brat.2010.04.006. [DOI] [PubMed] [Google Scholar]
- Gold E, Smith A, Hopper I, Herne D, Tansey G, Hulland C. Mindfulness-based stress reduction (MBSR) for primary school teachers. Journal of Child and Family Studies. 2010;19(2):184–189. [Google Scholar]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10(1):83–91. doi: 10.1037/a0018441. [PubMed] [Cross Ref] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P, Ramel W, Gross J. Mindfulness meditation training and self-referential processing in social anxiety disorder: Behavioral and neural effects. Journal of Cognitive Psychotherapy. 2009;23(3):242–257. doi: 10.1891/0889-8391.23.3.242. [PubMed] [Cross Ref] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P, Ziv M, Jazaieri H, Gross JJ. Randomized controlled trial of mindfulness-based stress reduction versus aerobic exercise: effects on the self-referential brain network in social anxiety disorder. Frontiers in Human Neuroscience. 2012;6:295. doi: 10.3389/fnhum.2012.00295. [PubMed] [Cross Ref] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P, Ziv M, Jazaieri H, Hahn K, Gross JJ. MBSR vs aerobic exercise in social anxiety: fMRI of emotion regulation of negative self-beliefs. Social Cognitive and Affective Neuroscience. 2013;8(1):65–72. doi: 10.1093/scan/nss054. doi: http://dx.doi.org/10.1093/scan/nss054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, Haythornthwaite JA. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [PubMed] [Cross Ref] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green SM, Bieling PJ. Expanding the Scope of Mindfulness-Based Cognitive Therapy: Evidence for Effectiveness in a Heterogeneous Psychiatric Sample. Cognitive and Behavioral Practice. 2012;19(1):174–180. doi: 10.1016/j.cbpra.2011.02.006. [DOI] [Google Scholar]
- Greeson JM, Webber DM, Smoski MJ, Brantley JG, Ekblad AG, Suarez EC, Wolever RQ. Changes in spirituality partly explain health-related quality of life outcomes after Mindfulness-Based Stress Reduction. Journal of Behavioral Medicine. 2011;34(6):508–518. doi: 10.1007/s10865-011-9332-x. doi: http://dx.doi.org/10.1007/s10865-011-9332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths K, Camic PM, Hutton JM. Participant experiences of a mindfulness-based cognitive therapy group for cardiac rehabilitation. Journal of Health Psychology. 2009;14(5):675–681. doi: 10.1177/1359105309104911. doi: http://dx.doi.org/10.1177/1359105309104911. [DOI] [PubMed] [Google Scholar]
- Gross CR, Kreitzer MJ, Reilly-Spong M, Wall M, Winbush NY, Patterson R, Cramer-Bornemann M. Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: a randomized controlled clinical trial. Explore: The Journal of Science and Healing. 2011;7(2):76–87. doi: 10.1016/j.explore.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross CR, Kreitzer MJ, Russas V, Treesak C, Frazier PA, Hertz MI. Mindfulness meditation to reduce symptoms after organ transplant: A pilot study. Advances in Mind-Body Medicine. 2004;20(2):20–29. [PubMed] [Google Scholar]
- Gross CR, Kreitzer MJ, Thomas W, Reilly-Spong M, Cramer-Bornemann M, Nyman JA, Ibrahim HN. Mindfulness-based stress reduction for solid organ transplant recipients: a randomized controlled trial. Alternative Therapies in Health and Medicine. 2010;16(5):30–38. [PMC free article] [PubMed] [Google Scholar]
- Grossman P, Tiefenthaler-Gilmer U, Raysz A, Kesper U. Mindfulness training as an intervention for fibromyalgia: Evidence of postintervention and 3-year follow-up benefits in well-being. Psychotherapy and Psychosomatics. 2007;76(4):226–233. doi: 10.1159/000101501. [DOI] [PubMed] [Google Scholar]
- Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006. [DOI] [PubMed] [Google Scholar]
- Hargus E, Crane C, Barnhofer T, Williams JM. Effects of mindfulness on meta-awareness and specificity of describing prodromal symptoms in suicidal depression. Emotion. 2010;10(1):34–42. doi: 10.1037/a0016825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann M, Kopf S, Kircher C, Faude-Lang V, Djuric Z, Augstein F, Nawroth PP. Sustained effects of a mindfulness-based stress-reduction intervention in type 2 diabetic patients: design and first results of a randomized controlled trial (the Heidelberger Diabetes and Stress-study) Diabetes Care. 2012;35(5):945–947. doi: 10.2337/dc11-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawtin H, Sullivan C. Experiences of mindfulness training in living with rheumatic disease: An interpretative phenomenological analysis. The British Journal of Occupational Therapy. 2011;74(3):137–142. doi: http://dx.doi.org/10.4276/030802211X12996065859283. [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: The Guilford Press; 1999. [Google Scholar]
- Hazlett-Stevens H. Mindfulness-based stress reduction for comorbid anxiety and depression: Case report and clinical considerations. Journal of Nervous and Mental Disease. 2012;200(11):999–1003. doi: 10.1097/NMD.0b013e3182718a61. doi: http://dx.doi.org/10.1097/NMD.0b013e3182718a61. [DOI] [PubMed] [Google Scholar]
- Heeren A, Van Broeck N, Philippot P. The effects of mindfulness on executive processes and autobiographical memory specificity. Behaviour Research and Therapy. 2009;47(5):403–409. doi: 10.1016/j.brat.2009.01.017. [DOI] [PubMed] [Google Scholar]
- Henderson VP, Clemow L, Massion AO, Hurley TG, Druker S, Hebert JR. The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Cancer Research and Treatment. 2012;131(1):99–109. doi: 10.1007/s10549-011-1738-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepburn SR, Crane C, Barnhofer T, Duggan DS, Fennell MJV, Williams JMG. Mindfulness-based cognitive therapy may reduce thought suppression in previously suicidal participants: Findings from a preliminary study. British Journal of Clinical Psychology. 2009;48:209–215. doi: 10.1348/014466509x414970. [DOI] [PubMed] [Google Scholar]
- Herdt J, Bührlen B, Bader K, Hänny C. Participation in an dapted version of MBCT in psychiatric care. Mindfulness. 2012;3(3):218–226. doi: 10.1007/s12671-012-0120-7. [DOI] [Google Scholar]
- Hertenstein E, Rose N, Voderholzer U, Heidenreich T, Nissen C, Thiel N, Kulz AK. Mindfulness-based cognitive therapy in obsessive-compulsive disorder - a qualitative study on patients' experiences. BMC Psychiatry. 2012;12:185. doi: 10.1186/1471-244x-12-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman CJ, Ersser SJ, Hopkinson JB. Mindfulness-based stress reduction in breast cancer: a qualitative analysis. Complementary Therapies in Clinical Practice. 2012;18(4):221–226. doi: 10.1016/j.ctcp.2012.06.008. [DOI] [PubMed] [Google Scholar]
- Hoffman CJ, Ersser SJ, Hopkinson JB, Nicholls PG, Harrington JE, Thomas PW. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: a randomized, controlled trial. Journal of Clinical Oncology. 2012;30(12):1335–1342. doi: 10.1200/jco.2010.34.0331. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. doi: http://dx.doi.org/10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, Simon NM. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. Journal of Clinical Psychiatry. 2013;74(8):786–792. doi: 10.4088/JCP.12m08083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Carmody J, Evans KC, Hoge EA, Dusek JA, Morgan L, Lazar SW. Stress reduction correlates with structural changes in the amygdala. Social Cognitive and Affective Neuroscience. 2010;5(1):11–17. doi: 10.1093/scan/nsp034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Carmody J, Vangel M, Congleton C, Yerramsetti SM, Gard T, Lazar SW. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research: Neuroimaging. 2011;191(1):36–43. doi: 10.1016/j.pscychresns.2010.08.006. doi: http://dx.doi.org/10.1016/j.pscychresns.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins A, Proeve M. Teaching mindfulness-based cognitive therapy to trainee psychologists: Qualitative and quantitative effects. Counselling Psychology Quarterly. 2013;26(2):115–130. doi: http://dx.doi.org/10.1080/09515070.2013.792998. [Google Scholar]
- Hopkins V, Kuyken W. Benefits and barriers to attending MBCT reunion meetings: An insider perspective. Mindfulness. 2012;3(2):139–150. doi: http://dx.doi.org/10.1007/s12671-012-0088-3. [Google Scholar]
- Howells FM, Ives-Deliperi VL, Horn NR, Stein DJ. Mindfulness based cognitive therapy improves frontal control in bipolar disorder: A pilot EEG study. BMC Psychiatry. 2012;12 doi: 10.1186/1471-244X-12-15. doi: http://dx.doi.org/10.1186/1471-244X-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huss DB, Baer RA. Acceptance and Change: The Integration of Mindfulness-Based Cognitive Therapy Into Ongoing Dialectical Behavior Therapy in a Case of Borderline Personality Disorder With Depression. Clinical Case Studies. 2007;6(1):17–33. doi: http://dx.doi.org/10.1177/1534650106290374. [Google Scholar]
- Imel Z, Baldwin S, Bonus K, MacCoon D. Beyond the individual: Group effects in mindfulness-based stress reduction. Psychotherapy Research. 2008;18(6):735–742. doi: 10.1080/10503300802326038. doi: http://dx.doi.org/10.1080/10503300802326038. [DOI] [PubMed] [Google Scholar]
- Ives-Deliperi VL, Howells F, Stein DJ, Meintjes EM, Horn N. The effects of mindfulness-based cognitive therapy in patients with bipolar disorder: A controlled functional MRI investigation. Journal of Affective Disorders. 2013;150(3):1152–1157. doi: 10.1016/j.jad.2013.05.074. doi: http://dx.doi.org/10.1016/j.jad.2013.05.074. [DOI] [PubMed] [Google Scholar]
- Jam S, Imani AH, Foroughi M, Seyed Alinaghi SA, Koochak HE, Mohraz M. The effects of mindfulness-based stress reduction (MBSR) program in Iranian HIV/AIDS patients: A pilot study. Acta Medica Iranica. 2010;48(2):101–106. [PubMed] [Google Scholar]
- Jastrowski Mano KE, Salamon KS, Hainsworth KR, Anderson Khan KJ, Ladwig RJ, Davies WH, Weisman SJ. A randomized, controlled pilot study of mindfulness-based stress reduction for pediatric chronic pain. Alternative Therapies in Health and Medicine. 2013;19(6):8–14. [PubMed] [Google Scholar]
- Jazaieri H, Goldin PR, Werner K, Ziv M, Gross JJ. A randomized trial of MBSR versus aerobic exercise for social anxiety disorder. Journal of Clinical Psychology. 2012;68(7):715–731. doi: 10.1002/jclp.21863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen CG, Vangkilde S, Frokjaer V, Hasselbalch SG. Mindfulness Training Affects Attention—Or Is It Attentional Effort? Journal of Experimental Psychology: General. 2012;141(1):106–123. doi: 10.1037/a0024931. [DOI] [PubMed] [Google Scholar]
- Jermann F, Van der Linden M, Gex-Fabry M, Guarin A, Kosel M, Bertschy G, Bondolfi G. Cognitive functioning in patients remitted from recurrent depression: Comparison with acutely depressed patients and controls and follow-up of a Mindfulness-Based Cognitive Therapy Trial. Cognitive Therapy and Research. 2013;37(5):1004–1014. [Google Scholar]
- Jha AP, Krompinger J, Baime MJ. Mindfulness training modifies subsystems of attention. Cognitive, Affective and Behavioral Neuroscience. 2007;7(2):109–119. doi: 10.3758/cabn.7.2.109. [DOI] [PubMed] [Google Scholar]
- Johansson B, Bjuhr H, Ronnback L. Mindfulness-based stress reduction (MBSR) improves long-term mental fatigue after stroke or traumatic brain injury. Brain Injury. 2012;26(13–14):1621–1628. doi: 10.3109/02699052.2012.700082. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York, NY: Bantam Books; 1990. [Google Scholar]
- Kabat-Zinn J. Some reflections on the origins of MBSR, skillful means, and the trouble with maps. Contemporary Buddhism. 2011;12(01):281–306. [Google Scholar]
- Kabat-Zinn J, Wheeler E, Light T, Skillings A, Scharf MJ, Cropley TG, Bernhard JD. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA) Psychosomatic Medicine. 1998;60(5):625–632. doi: 10.1097/00006842-199809000-00020. [DOI] [PubMed] [Google Scholar]
- Kaplan KH, Goldenberg DL, Galvin-Nadeau M. The impact of a meditation-based stress reduction program on fibromyalgia. General Hospital Psychiatry. 1993;15(5):284–289. doi: 10.1016/0163-8343(93)90020-o. doi: http://dx.doi.org/10.1016/0163-8343(93)90020-O. [DOI] [PubMed] [Google Scholar]
- Kaviani H, Hatami N, Javaheri F. The impact of Mindfulness-based Cognitive Therapy (MBCT) on mental health and quality of life in a sub-clinically depressed population. Archives of Psychiatry and Psychotherapy. 2012;14(1):21–28. [Google Scholar]
- Kaviani H, Javaheri F, Hatami N. Mindfulness-based cognitive therapy (MBCT) reduces depression and anxiety induced by real stressful setting in non-clinical population. International Journal of Psychology and Psychological Therapy. 2011;11(2):285–296. [Google Scholar]
- Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on Psychological Science. 2011;6(1):21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Association of participation in a mindfulness program with measures of PTSD, depression and quality of life in a veteran sample. Journal of Clinical Psychology. 2012;68(1):101–116. doi: 10.1002/jclp.20853. doi: http://dx.doi.org/10.1002/jclp.20853. [DOI] [PubMed] [Google Scholar]
- Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: a randomized controlled pilot study. Journal of Clinical Psychology. 2013;69(1):14–27. doi: 10.1002/jclp.21911. [DOI] [PubMed] [Google Scholar]
- Kearney DJ, McDermott K, Martinez M, Simpson TL. Association of participation in a mindfulness programme with bowel symptoms, gastrointestinal symptom-specific anxiety and quality of life. Alimentary Pharmacology and Therapeutics. 2011;34(3):363–373. doi: 10.1111/j.1365-2036.2011.04731.x. [DOI] [PubMed] [Google Scholar]
- Kearney DJ, Milton ML, Malte CA, McDermott KA, Martinez M, Simpson TL. Participation in mindfulness-based stress reduction is not associated with reductions in emotional eating or uncontrolled eating. Nutrition Research. 2012;32(6):413–420. doi: 10.1016/j.nutres.2012.05.008. [DOI] [PubMed] [Google Scholar]
- Keng S-L, Smoski MJ, Robins CJ, Ekblad AG, Brantley JG. Mechanisms of change in mindfulness-based stress reduction: Self-compassion and mindfulness as mediators of intervention outcomes. Journal of Cognitive Psychotherapy. 2012;26(3):270–280. doi: http://dx.doi.org/10.1891/0889-8391.26.3.270. [Google Scholar]
- Kennedy SH, Lam RW, Parikh SV, Patten SB, Ravindran AV. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. Journal of Affective Disorders. 2009;117:s5–s14. doi: 10.1016/j.jad.2009.06.044. [DOI] [PubMed] [Google Scholar]
- Kenny MA, Williams JMG. Treatment-resistant depressed patients show a good response to Mindfulness-based Cognitive Therapy. Behaviour Research and Therapy. 2007;45(3):617–625. doi: 10.1016/j.brat.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr CE, Josyula K, Littenberg R. Developing an observing attitude: An analysis of meditation diaries in an MBSR clinical trial. Clinical Psychology & Psychotherapy. 2011;18(1):80–93. doi: 10.1002/cpp.700. doi: http://dx.doi.org/10.1002/cpp.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerrigan D, Johnson K, Stewart M, Magyari T, Hutton N, Ellen JM, Sibinga EM. Perceptions, experiences, and shifts in perspective occurring among urban youth participating in a mindfulness-based stress reduction program. Complementary Therapies in Clinical Practice. 2011;17(2):96–101. doi: 10.1016/j.ctcp.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Keune PM, Bostanov V, Hautzinger M, Kotchoubey B. Mindfulness-based cognitive therapy (MBCT), cognitive style, and the temporal dynamics of frontal EEG alpha asymmetry in recurrently depressed patients. Biological Psychology. 2011;88(2–3):243–252. doi: 10.1016/j.biopsycho.2011.08.008. [DOI] [PubMed] [Google Scholar]
- Kieviet-Stijnen A, Visser A, Garssen B, Hudig W. Mindfulness-based stress reduction training for oncology patients: Patients' appraisal and changes in well-being. Patient Education and Counseling. 2008;72(3):436–442. doi: 10.1016/j.pec.2008.05.015. doi: http://dx.doi.org/10.1016/j.pec.2008.05.015. [DOI] [PubMed] [Google Scholar]
- Kilpatrick LA, Suyenobu BY, Smith SR, Bueller JA, Goodman T, Creswell JD, Naliboff BD. Impact of mindfulness-based stress reduction training on intrinsic brain connectivity. NeuroImage. 2011;56(1):290–298. doi: 10.1016/j.neuroimage.2011.02.034. doi: http://dx.doi.org/10.1016/j.neuroimage.2011.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim B, Lee SH, Kim YW, Choi TK, Yook K, Suh SY, Yook KH. Effectiveness of a mindfulness-based cognitive therapy program as an adjunct to pharmacotherapy in patients with panic disorder. Journal of Anxiety Disorders. 2010;24(6):590–595. doi: 10.1016/j.janxdis.2010.03.019. [DOI] [PubMed] [Google Scholar]
- Kim YW, Lee SH, Choi TK, Suh SY, Kim B, Kim CM, Yook KH. Effectiveness of mindfulness-based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depression and Anxiety. 2009;26(7):601–606. doi: 10.1002/da.20552. [DOI] [PubMed] [Google Scholar]
- Kimbrough E, Magyari T, Langenberg P, Chesney M, Berman B. Mindfulness intervention for child abuse survivors. Journal of Clinical Psychology. 2010;66(1):17–33. doi: 10.1002/jclp.20624. [DOI] [PubMed] [Google Scholar]
- King AP, Erickson TM, Giardino ND, Favorite T, Rauch SAM, Robinson E, Liberzon I. A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD) Depression and Anxiety. 2013;30(7):638–645. doi: 10.1002/da.22104. doi: http://dx.doi.org/10.1002/da.22104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingston T, Dooley B, Bates A, Lawlor E, Malone K. Mindfulness-based cognitive therapy for residual depressive symptoms. Psychology and Psychotherapy: Theory, Research and Practice. 2007;80(2):193–203. doi: 10.1348/147608306X116016. [DOI] [PubMed] [Google Scholar]
- Klatt MD, Buckworth J, Malarkey WB. Effects of low-dose mindfulness-based stress reduction (MBSR-ld) on working adults. Health Education & Behavior. 2009;36(3):601–614. doi: 10.1177/1090198108317627. [DOI] [PubMed] [Google Scholar]
- Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behaviour Research and Therapy. 2007;45(10):2518–2526. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Kreitzer MJ, Gross CR, Ye X, Russas V, Treesak C. Longitudinal impact of mindfulness meditation on illness burden in solid-organ transplant recipients. Progress in transplantation (Aliso Viejo, Calif.) 2005;15(2):166. doi: 10.1177/152692480501500210. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K, Teasdale JD. Mindfulness-Based Cognitive Therapy to Prevent Relapse in Recurrent Depression. Journal of Consulting and Clinical Psychology. 2008;76(6):966–978. doi: 10.1037/a0013786. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Hayes R, Barrett B, Byng R, Dalgleish T, Kessler D, Byford S. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. The Lancet. 2015 doi: 10.1016/s0140-6736(14)62222-4. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, Dalgleish T. How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy. 2010;48(11):1105–1112. doi: 10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Kvillemo P, Bränström R. Experiences of a mindfulness-based stress-reduction intervention among patients with cancer. Cancer Nursing. 2011;34(1):24–31. doi: 10.1097/NCC.0b013e3181e2d0df. doi: http://dx.doi.org/10.1097/NCC.0b013e3181e2d0df. [DOI] [PubMed] [Google Scholar]
- Labelle LE, Campbell TS, Carlson LE. Mindfulness-based stress reduction in oncology: Evaluating mindfulness and rumination as mediators of change in depressive symptoms. Mindfulness. 2010;1(1):28–40. doi: http://dx.doi.org/10.1007/s12671-010-0005-6. [Google Scholar]
- Langdon S, Jones FW, Hutton J, Holttum S. A grounded-theory study of mindfulness practice following mindfulness-based cognitive therapy. Mindfulness. 2011;2(4):270–281. doi: http://dx.doi.org/10.1007/s12671-011-0070-5. [Google Scholar]
- Lange B. Cocreating a communicative space to develop a mindfulness meditation manual for women in recovery from substance abuse disorders. Advances in Nursing Science. 2011;34(3):E1–E13. doi: 10.1097/ANS.0b013e3182272405. [DOI] [PubMed] [Google Scholar]
- Langer ÁI, Cangas AJ, Salcedo E, Fuentes B. Applying mindfulness therapy in a group of psychotic individuals: A controlled study. Behavioural and Cognitive Psychotherapy. 2012;40(1):105–109. doi: 10.1017/S1352465811000464. doi: http://dx.doi.org/10.1017/S1352465811000464. [DOI] [PubMed] [Google Scholar]
- Lau MA, Colley L, Willett BR, Lynd LD. Employee’s preferences for access to mindfulness-based cognitive therapy to reduce the risk of depressive relapse—A discrete choice experiment. Mindfulness. 2012;3(4):318–326. doi: http://dx.doi.org/10.1007/s12671-012-0108-3. [Google Scholar]
- Lee J, Semple RJ, Rosa D, Miller L. Mindfulness-based cognitive therapy for children: Results of a pilot study. Journal of Cognitive Psychotherapy. 2008;22(1):15–28. doi: 10.1891/0889.8391.22.1.15. [DOI] [Google Scholar]
- Lengacher CA, Johnson-Mallard V, Barta M, Fitzgerald S, Moscoso MS, Post-White J, Kip KE. Feasibility of a mindfulness-based stress reduction program for early-stage breast cancer survivors. Journal of Holistic Nursing. 2011;29(2):107–117. doi: 10.1177/0898010110385938. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Johnson-Mallard V, Post-White J, Moscoso MS, Jacobsen PB, Klein TW, Kip KE. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-Oncology. 2009;18(12):1261–1272. doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Kip KE, Barta M, Post-White J, Jacobsen PB, Groer M, Shelton MM. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. Journal of Holistic Nursing. 2012;30(3):170–185. doi: 10.1177/0898010111435949. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Kip KE, Post-White J, Fitzgerald S, Newton C, Barta M, Klein TW. Lymphocyte recovery after breast cancer treatment and mindfulness-based stress reduction (MBSR) therapy. Biological Research for Nursing. 2013;15(1):37–47. doi: 10.1177/1099800411419245. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Reich RR, Post-White J, Moscoso M, Shelton MM, Barta M, Budhrani P. Mindfulness based stress reduction in post-treatment breast cancer patients: an examination of symptoms and symptom clusters. Journal of Behavioral Medicine. 2012;35(1):86–94. doi: 10.1007/s10865-011-9346-4. [DOI] [PubMed] [Google Scholar]
- Lerman R, Jarski R, Rea H, Gellish R, Vicini F. Improving symptoms and quality of life of female cancer survivors: a randomized controlled study. Annals of Surgical Oncology. 2012;19(2):373–378. doi: 10.1245/s10434-011-2051-2. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO, Lynn SJ, Lohr JM. Science and Pseudoscience in Clinical Psychology. New York, NY.: Guilford Publications; 2003. [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York, NY, US: Guilford Press; 1993. [Google Scholar]
- Lovas DA, Barsky AJ. Mindfulness-based cognitive therapy for hypochondriasis, or severe health anxiety: a pilot study. Journal of Anxiety Disorders. 2010;24(8):931–935. doi: 10.1016/j.janxdis.2010.06.019. [DOI] [PubMed] [Google Scholar]
- Lush E, Salmon P, Floyd A, Studts JL, Weissbecker I, Sephton SE. Mindfulness meditation for symptom reduction in fibromyalgia: psychophysiological correlates. Journal of Clinical Psychology in Medical Settings. 2009;16(2):200–207. doi: 10.1007/s10880-009-9153-z. [DOI] [PubMed] [Google Scholar]
- Lutz A, Jha AP, Dunne J, Saron CD. Investigating the phenomenological matrix of mindfulness-related practices from a neurocognitive perspective. American Psychologist. XX:xxx–xxx. doi: 10.1037/a0039585. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology. 2004;72(1):31–40. doi: 10.1037/0022-006x.72.1.31. [DOI] [PubMed] [Google Scholar]
- MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, Lutz A. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behaviour Research and Therapy. 2012;50(1):3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie MJ, Carlson LE, Munoz M, Speca M. A qualitative study of self-perceived effects of Mindfulness-based Stress Reduction (MBSR) in a psychosocial oncology setting. Stress and Health: Journal of the International Society for the Investigation of Stress. 2007;23(1):59–69. doi: http://dx.doi.org/10.1002/smi.1120. [Google Scholar]
- Manicavasgar V, Parker G, Perich T. Mindfulness-based cognitive therapy vs cognitive behaviour therapy as a treatment for non-melancholic depression. Journal of Affective Disorders. 2011;130(1–2):138–144. doi: 10.1016/j.jad.2010.09.027. [DOI] [PubMed] [Google Scholar]
- Marcus MT, Fine M, Moeller FG, Khan MM, Pitts K, Swank PR, Liehr P. Change in stress levels following mindfulness-based stress reduction in a therapeutic community. Addictive Disorders & Their Treatment. 2003;2(3):63–68. doi: http://dx.doi.org/10.1097/00132576-200302030-00001. [Google Scholar]
- Martín-Asuero A, García-Banda G. The mindfulness-based stress reduction program (MBSR) reduces stress-related psychological distress in healthcare professionals. The Spanish Journal of Psychology. 2010;13(2):897–905. doi: 10.1017/s1138741600002547. doi: http://dx.doi.org/10.1017/S1138741600002547. [DOI] [PubMed] [Google Scholar]
- Mason O, Hargreaves I. A qualitative study of mindfulness-based cognitive therapy for depression. British Journal of Medical Psychology. 2001;74(2):197–212. doi: http://dx.doi.org/10.1348/000711201160911. [PubMed] [Google Scholar]
- Matchim Y, Armer JM, Stewart BR. Effects of Mindfulness-Based Stress Reduction (MBSR) on health among breast cancer survivors. Western Journal of Nursing Research. 2011;33(8):996–1016. doi: 10.1177/0193945910385363. doi: http://dx.doi.org/10.1177/0193945910385363. [DOI] [PubMed] [Google Scholar]
- Mathew KL, Whitford HS, Kenny MA, Denson LA. The long-term effects of Mindfulness-based Cognitive Therapy as a relapse prevention treatment for major depressive disorder. Behavioural and Cognitive Psychotherapy. 2010;38(5):561–576. doi: 10.1017/S135246581000010X. doi: http://dx.doi.org/10.1017/S135246581000010X. [DOI] [PubMed] [Google Scholar]
- Matousek RH, Pruessner JC, Dobkin PL. Changes in the cortisol awakening response (CAR) following participation in mindfulness-based stress reduction in women who completed treatment for breast cancer. Complementary Therapies in Clinical Practice. 2011;17(2):65–70. doi: 10.1016/j.ctcp.2010.10.005. [DOI] [PubMed] [Google Scholar]
- McManus F, Surawy C, Muse K, Vazquez-Montes M, Williams JM. A randomized clinical trial of mindfulness-based cognitive therapy versus unrestricted services for health anxiety (hypochondriasis) Journal of Consulting and Clinical Psychology. 2012;80(5):817–828. doi: 10.1037/a0028782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melloni M, Sedeño L, Couto B, Reynoso M, Gelormini C, Favaloro R, Ibanez A. Preliminary evidence about the effects of meditation on interoceptive sensitivity and social cognition. Behavioral and Brain Functions. 2013;9 doi: 10.1186/1744-9081-9-47. doi: http://dx.doi.org/10.1186/1744-9081-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak J, Heidenirich T, Meibert P, Schulte D. Mindfulness predicts relapse/recurrence in major depressive disorder after mindfulness-based cognitive therapy. Journal of Nervous and Mental Disease. 2008;196(8):630–633. doi: 10.1097/NMD.0b013e31817d0546. [DOI] [PubMed] [Google Scholar]
- Michalak J, Holz A, Teismann T. Rumination as a predictor of relapse in mindfulness-based cognitive therapy for depression. Psychology and Psychotherapy: Theory, Research and Practice. 2011;84(2):230–236. doi: 10.1348/147608310x520166. [DOI] [PubMed] [Google Scholar]
- Michalak J, Troje NF, Heidenreich T. The effects of mindfulness-based cognitive therapy on depressive gait patterns. Journal of Cognitive and Behavioral Psychotherapies. 2011;11(1):13–27. [Google Scholar]
- Miklowitz DJ, Alatiq Y, Goodwin GM, Geddes JR, Fennell MJV, Dimidjian S, Williams JMG. A pilot study of mindfulness-based cognitive therapy for bipolar disorder. International Journal of Cognitive Therapy. 2009;2(4):373–382. [Google Scholar]
- Miller JJ, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. General Hospital Psychiatry. 1995;17:192–200. doi: 10.1016/0163-8343(95)00025-m. doi: http://dx.doi.org/10.1016/0163-8343(95)00025-M. [DOI] [PubMed] [Google Scholar]
- Minor HG, Carlson LE, Mackenzie MJ, Zernicke K, Jones L. Evaluation of a mindfulness-based stress reduction (MBSR) program for caregivers of children with chronic conditions. Social Work in Health Care. 2006;43(1):91–109. doi: 10.1300/J010v43n01_06. doi: http://dx.doi.org/10.1300/J010v43n01_06. [DOI] [PubMed] [Google Scholar]
- Morone NE, Lynch CP, Losasso VJ, III, Liebe K, Greco CM. Mindfulness to reduce psychosocial stress. Mindfulness. 2012;3(1):22–29. doi: http://dx.doi.org/10.1007/s12671-011-0076-z. [Google Scholar]
- Moynihan JA, Chapman BP, Klorman R, Krasner MS, Duberstein PR, Brown KW, Talbot NL. Mindfulness-based stress reduction for older adults: Effects on executive function, frontal alpha asymmetry and immune function. Neuropsychobiology. 2013;68(1):34–43. doi: 10.1159/000350949. doi: http://dx.doi.org/10.1159/000350949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munshi K, Eisendrath S, Delucchi K. Preliminary long-term follow-up of mindfulness-based cognitive therapy-induced remission of depression. Mindfulness. 2013;4(4):354–361. doi: 10.1007/s12671-012-0135-0. doi: http://dx.doi.org/10.1007/s12671-012-0135-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naranjo JR, Schmidt S. Is it me or not me? Modulation of perceptual-motor awareness and visuomotor performance by mindfulness meditation. BMC Neuroscience. 2012;13:88. doi: 10.1186/1471-2202-13-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niles BL, Klunk-Gillis J, Ryngala DJ, Silberbogen AK, Paysnick A, Wolf EJ. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(5):538–547. doi: 10.1037/a0026161. [DOI] [Google Scholar]
- Nyklicek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Annals of Behavioral Medicine. 2008;35(3):331–340. doi: 10.1007/s12160-008-9030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyklíček I, Mommersteeg PMC, Van Beugen S, Ramakers C, Van Boxtel GJ. Mindfulness-based stress reduction and physiological activity during acute stress: A randomized controlled trial. Health Psychology. 2013;32(10):1110–1113. doi: 10.1037/a0032200. doi: http://dx.doi.org/10.1037/a0032200. [DOI] [PubMed] [Google Scholar]
- Nyklíček I, Van Beugen S, Denollet J. Effects of mindfulness-based stress reduction on distressed (type D) personality traits: a randomized controlled trial. Journal of Behavioral Medicine. 2013;36(4):361–370. doi: 10.1007/s10865-012-9431-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Haver Day P, Horton-Deutsch S. Using mindfulness-based therapeutic interventions in psychiatric nursing practice--part I: Description and empirical support for mindfulness-based interventions. Archives of Psychiatric Nursing. 2004;18(5):164–169. doi: 10.1016/j.apnu.2004.07.003. [DOI] [PubMed] [Google Scholar]
- Oken BS, Fonareva I, Haas M, Wahbeh H, Lane JB, Zajdel D, Amen A. Pilot controlled trial of mindfulness meditation and education for dementia caregivers. Journal of Alternative and Complementary Medicine. 2010;16(10):1031–1038. doi: 10.1089/acm.2009.0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oman D, Shapiro SL, Thoresen CE, Plante TG, Flinders T. Meditation lowers stress and supports forgiveness among college students: a randomized controlled trial. Journal of American College Health. 2008;56(5):569–578. doi: 10.3200/jach.56.5.569-578. [DOI] [PubMed] [Google Scholar]
- Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science: Unifying the discipline to improve the public health. Clinical Psychological Science. 2014;2(1):22–34. doi: 10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palta P, Page G, Piferi RL, Gill JM, Hayat MJ, Connolly AB, Szanton SL. Evaluation of a mindfulness-based intervention program to decrease blood pressure in low-income African-American older adults. Journal of Urban Health. 2012;89(2):308–316. doi: 10.1007/s11524-011-9654-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra-Delgado M, Latorre-Postigo JM. Effectiveness of mindfulness-based cognitive therapy in the treatment of fibromyalgia: A randomised trial. Cognitive Therapy and Research. 2013;37(5):1015–1026. doi: http://dx.doi.org/10.1007/s10608-013-9538-z. [Google Scholar]
- Patel SR, Carmody J, Simpson HB. Adapting mindfulness-based stress reduction for the treatment of obsessive-compulsive disorder: A case report. Cognitive and Behavioral Practice. 2007;14(4):375–380. doi: http://dx.doi.org/10.1016/j.cbpra.2006.08.006. [Google Scholar]
- Patten SB, Kennedy SH, Lam RW, O'Donovan C, Filteau MJ, Parikh SV, Ravindran AV the Canadian Network for Mood and Anxiety Treatments (CANMAT) Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults: I. Classification, burden and principles of management. Journal of Affective Disorders. 2009;118:S5–S14. doi: 10.1016/j.jad.2009.06.044. https://dx.doi.org/10.1016/j.jad.2009.06.044. [DOI] [PubMed] [Google Scholar]
- Patten SB, Meadows GM. Population-based service planning foriImplementation of MBCT: Linking epidemiologic data to practice. Psychiatric Services. 2009;60(11):1540–1542. doi: 10.1176/ps.2009.60.11.1540. doi: http://dx.doi.org/10.1176/appi.ps.60.11.1540. [DOI] [PubMed] [Google Scholar]
- Pbert L, Madison JM, Druker S, Olendzki N, Magner R, Reed G, Carmody J. Effect of mindfulness training on asthma quality of life and lung function: a randomised controlled trial. Thorax. 2012;67(9):769–776. doi: 10.1136/thoraxjnl-2011-200253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perich T, Manicavasagar V, Mitchell PB, Ball JR. The association between meditation practice and treatment outcome in Mindfulness-based Cognitive Therapy for bipolar disorder. Behaviour Research and Therapy. 2013;51(7):338–343. doi: 10.1016/j.brat.2013.03.006. [DOI] [PubMed] [Google Scholar]
- Perich T, Manicavasagar V, Mitchell PB, Ball JR, Hadzi-Pavlovic D. A randomized controlled trial of mindfulness-based cognitive therapy for bipolar disorder. Acta Psychiatrica Scandinavica. 2013;127(5):333–343. doi: 10.1111/acps.12033. [DOI] [PubMed] [Google Scholar]
- Philippot P, Nef F, Clauw L, de Romree M, Segal Z. A randomized controlled trial of mindfulness-based cognitive therapy for treating tinnitus. Clinical Psychology & Psychotherapy. 2012;19(5):411–419. doi: 10.1002/cpp.756. [DOI] [PubMed] [Google Scholar]
- Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clinical Psychology Review. 2011;31(6):1032–1040. doi: 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Piet J, Hougaard E, Hecksher MS, Rosenberg NK. A randomized pilot study of mindfulness-based cognitive therapy and group cognitive-behavioral therapy for young adults with social phobia. Scandinavian Journal of Psychology. 2010;51(5):403–410. doi: 10.1111/j.1467-9450.2009.00801.x. [DOI] [PubMed] [Google Scholar]
- Plews-Ogan M, Owens JE, Goodman M, Wolfe P, Schorling J. A pilot study evaluating mindfulness-based stress reduction and massage for the management of chronic pain. Journal of General Internal Medicine. 2005;20(12):1136–1138. doi: 10.1111/j.1525-1497.2005.0247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradhan EK, Baumgarten M, Langenberg P, Handwerger B, Gilpin AK, Magyari T, Berman BM. Effect of Mindfulness-Based Stress Reduction in rheumatoid arthritis patients. Arthritis & Rheumatism (Arthritis Care & Research) 2007;57(7):1134–1142. doi: 10.1002/art.23010. [DOI] [PubMed] [Google Scholar]
- Raes F, Dewulf D, Van Heeringen C, Williams JMG. Mindfulness and reduced cognitive reactivity to sad mood: Evidence from a correlational study and a non-randomized waiting list controlled study. Behaviour Research and Therapy. 2009;47(7):623–627. doi: 10.1016/j.brat.2009.03.007. doi: http://dx.doi.org/10.1016/j.brat.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Ramel W, Goldin PR, Carmona PE, McQuaid JR. The Effects of Mindfulness Meditation on Cognitive Processes and Affect in Patients With Past Depression. Cognitive Therapy and Research. 2004;28(4):433–455. [Google Scholar]
- Rapgay L, Bystritsky A, Dafter RE, Spearman M. New strategies for combining mindfulness with integrative cognitive behavioral therapy for the treatment of generalized anxiety disorder. Journal of Rational-Emotive and Cognitive-Behavior Therapy. 2011;29(2):92–119. doi: 10.1007/s10942-009-0095-z. doi: http://dx.doi.org/10.1007/s10942-009-0095-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ree MJ, Craigie MA. Outcomes following mindfulness-based cognitive therapy in a heterogeneous sample of adult outpatients. Behaviour Change. 2007;24(2):70–86. doi: http://dx.doi.org/10.1375/bech.24.2.70. [Google Scholar]
- Reibel DK, Greeson JM, Brainard GC, Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. General Hospital Psychiatry. 2001;23(4):183–192. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- Rimes KA, Wingrove J. Pilot study of Mindfulness-Based Cognitive Therapy for trainee clinical psychologists. Behavioural and Cognitive Psychotherapy. 2011;39(2):235–241. doi: 10.1017/S1352465810000731. doi: http://dx.doi.org/10.1017/S1352465810000731. [DOI] [PubMed] [Google Scholar]
- Rimes KA, Wingrove J. Mindfulness-based cognitive therapy for people with chronic fatigue syndrome still experiencing excessive fatigue after cognitive behaviour therapy: a pilot randomized study. Clinical Psychology & Psychotherapy. 2013;20(2):107–117. doi: 10.1002/cpp.793. [DOI] [PubMed] [Google Scholar]
- Robert McComb JJ, Tacon A, Randolph P, Caldera Y. A pilot study to examine the effects of a mindfulness-based stress-reduction and relaxation program on levels of stress hormones, physical functioning, and submaximal exercise responses. Journal of Alternative and Complementary Medicine. 2004;10(5):819–827. doi: 10.1089/acm.2004.10.819. [DOI] [PubMed] [Google Scholar]
- Robins CJ, Keng SL, Ekblad AG, Brantley JG. Effects of mindfulness-based stress reduction on emotional experience and expression: A randomized controlled trial. Journal of Clinical Psychology. 2012;68(1):117–131. doi: 10.1002/jclp.20857. doi: http://dx.doi.org/10.1002/jclp.20857. [DOI] [PubMed] [Google Scholar]
- Robinson FP, Mathews HL, Witek-Janusek L. Psycho-endocrine-immune response to mindfulness-based stress reduction in individuals infected with the human immunodeficiency virus: a quasiexperimental study. The Journal of Alternative & Complementary Medicine. 2003;9(5):683–694. doi: 10.1089/107555303322524535. [DOI] [PubMed] [Google Scholar]
- Rosenkranz MA, Davidson RJ, Maccoon DG, Sheridan JF, Kalin NH, Lutz A. A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain, Behavior, and Immunity. 2013;27(1):174–184. doi: 10.1016/j.bbi.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. Journal of Psychosomatic Research. 2010;68(1):29–36. doi: 10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- Rosenzweig S, Reibel DK, Greeson JM, Brainard GC, Hojat M. Mindfulness-based stress reduction lowers psychological distress in medical students. Teaching and Learning in Medicine. 2003;15(2):88–92. doi: 10.1207/S15328015TLM1502_03. [DOI] [PubMed] [Google Scholar]
- Rosenzweig S, Reibel DK, Greeson JM, Edman JS, Jasser SA, McMearty KD, Goldstein BJ. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Alternative Therapies in Health and Medicine. 2007;13(5):36–38. [PubMed] [Google Scholar]
- Roth B. Mindfulness-based stress reduction in the inner city. Advances. 1997;13(4):50–58. [Google Scholar]
- Roth B, Creaser T. Mindfulness meditation-based stress reduction: experience with a bilingual inner-city program. Nurse Practitioner. 1997;22(3):150–152. 154. 157 passim. [PubMed] [Google Scholar]
- Roth B, Robbins D. Mindfulness-based stress reduction and health-related quality of life: Findings from a bilingual inner-city patient population. Psychosomatic Medicine. 2004;66(1):113–123. doi: 10.1097/01.psy.0000097337.00754.09. [DOI] [PubMed] [Google Scholar]
- Roth B, Stanley TW. Mindfulness-based stress reduction and healthcare utilization in the inner city: preliminary findings. Alternative Therapies in Health and Medicine. 2002;8(1):60–62. 64–66. [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, Chorpita BF. Disruptive innovations for designing and diffusing evidence-based interventions. American Psychologist. 2012;67(6):463–476. doi: 10.1037/a0028180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruths FA, de Zoysa N, Frearson SJ, Hutton J, Williams JMG, Walsh J. Mindfulness-based cognitive therapy for mental health professionals—A pilot study. Mindfulness. 2013;4(4):289–295. doi: http://dx.doi.org/10.1007/s12671-012-0127-0. [Google Scholar]
- Sachse S, Keville S, Feigenbaum J. A feasibility study of mindfulness-based cognitive therapy for individuals with borderline personality disorder. Psychology and Psychotherapy: Theory, Research and Practice. 2010;84(2):184–200. doi: 10.1348/147608310X516387. [DOI] [PubMed] [Google Scholar]
- Salmoirago-Blotcher E, Hunsinger M, Morgan L, Fischer D, Carmody J. Mindfulness-based stress reduction and change in health-related behaviors. Journal of Evidence-Based Complementary & Alternative Medicine. 2013;18(4):243–247. doi: http://dx.doi.org/10.1177/2156587213488600. [Google Scholar]
- Samuelson M, Carmody J, Kabat-Zinn J, Bratt MA. Mindfulness-based stress reduction in Massachusetts correctional facilities. The Prison Journal. 2007;87(2):254–268. doi: http://dx.doi.org/10.1177/0032885507303753. [Google Scholar]
- Saxe GA, Hebert JR, Carmody JF, Kabat-Zinn J, Rosenzweig PH, Jarzobski D, Blute RD. Can diet in conjunction with stress reduction affect the rate of increase in prostate specific antigen after biochemical recurrence of prostate cancer? Journal of Urology. 2001;166(6):2202–2207. [PubMed] [Google Scholar]
- Schmidt S, Grossman P, Schwarzer B, Jena S, Naumann J, Walach H. Treating fibromyalgia with mindfulness-based stress reduction: results from a 3-armed randomized controlled trial. Pain. 2011;152(2):361–369. doi: 10.1016/j.pain.2010.10.043. [DOI] [PubMed] [Google Scholar]
- Schroevers MJ, Brandsma R. Is learning mindfulness associated with improved affect after mindfulness-based cognitive therapy? British Journal of Psychology. 2010;101(1):95–107. doi: 10.1348/000712609X424195. doi: http://dx.doi.org/10.1348/000712609X424195. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Bieling P, Young T, MacQueen G, Cooke R, Martin L, Levitan RD. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Archives of General Psychiatry. 2010;67(12):1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Kennedy S, Gemar M, Hood K, Pedersen R, Buis T. Cognitive reactivity to sad mood provocation and the prediction of depressive relapse. Archives of General Psychiatry. 2006;63(7):749–755. doi: 10.1001/archpsyc.63.7.749. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Teasdale JD, Williams JM, Gemar MC. The mindfulness-based cognitive therapy adherence scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology & Psychotherapy. 2002;9(2):131–138. doi: 10.1002/cpp.320. [DOI] [Google Scholar]
- Segal ZV, Williams JM, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York, NY.: Guilford Press; 2002. [Google Scholar]
- Semple RJ, Lee J, Rosa D, Miller LF. A Randomized Trial of Mindfulness-Based Cognitive Therapy for Children: Promoting Mindful Attention to Enhance Social-Emotional Resiliency in Children. Journal of Child and Family Studies. 2010;19(2):218–229. doi: 10.1007/s10826-009-9301-y. [DOI] [Google Scholar]
- Sephton SE, Salmon P, Weissbecker I, Ulmer C, Floyd A, Hoover K, Studts JL. Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: results of a randomized clinical trial. Arthritis & Rheumatism. 2007;57(1):77–85. doi: 10.1002/art.22478. [DOI] [PubMed] [Google Scholar]
- SeyedAlinaghi S, Jam S, Foroughi M, Imani A, Mohraz M, Djavid GE, Black DS. Randomized controlled trial of mindfulness-based stress reduction delivered to human immunodeficiency virus-positive patients in Iran: effects on CD4(+) T lymphocyte count and medical and psychological symptoms. Psychosomatic Medicine. 2012;74(6):620–627. doi: 10.1097/PSY.0b013e31825abfaa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahar B, Britton WB, Sbarra DA, Figueredo AJ, Bootzin RR. Mechanisms of change in mindfulness-based cognitive therapy for depression: Preliminary evidence from a randomized controlled trial. International Journal of Cognitive Therapy. 2010;3(4):402–418. doi: http://dx.doi.org/10.1521/ijct.2010.3.4.402. [Google Scholar]
- Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness-based stress reduction for health care professionals: Results from a randomized trial. International Journal of Stress Management. 2005;12(2):164–176. doi: 10.1037/1072-5245.12.2.164. [DOI] [Google Scholar]
- Shapiro SL, Bootzin RR, Figueredo AJ, Lopez AM, Schwartz GE. The efficacy of mindfulness-based stress reduction in the treatment of sleep disturbance in women with breast cancer: An exploratory study. Journal of Psychosomatic Research. 2003;54(1):85–91. doi: 10.1016/s0022-3999(02)00546-9. doi: http://dx.doi.org/10.1016/S0022-3999(02)00546-9. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Brown KW, Biegel GM. Teaching self-care to caregivers: Effects of mindfulness-based stress reduction on the mental health of therapists in training. Training and Education in Professional Psychology. 2007;1(2):105–115. doi: http://dx.doi.org/10.1037/1931-3918.1.2.105. [Google Scholar]
- Shapiro SL, Brown KW, Thoresen C, Plante TG. The moderation of mindfulness-based stress reduction effects by trait mindfulness: Results from a randomized controlled trial. Journal of Clinical Psychology. 2011;67(3):267–277. doi: 10.1002/jclp.20761. doi: http://dx.doi.org/10.1002/jclp.20761. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Jazaieri H, Goldin PR. Mindfulness-based stress reduction effects on moral reasoning and decision making. The Journal of Positive Psychology. 2012;7(6):504–515. doi: http://dx.doi.org/10.1080/17439760.2012.723732. [Google Scholar]
- Shapiro SL, Oman D, Thoresen CE, Plante TG, Flinders T. Cultivating mindfulness: Effects on well-being. Journal of Clinical Psychology. 2008;64(7):840–862. doi: 10.1002/jclp.20491. doi: http://dx.doi.org/10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. Journal of Behavioral Medicine. 1998;21(6):581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- Sharma MP, Sudhir PM, Narayan R. Effectiveness of mindfulness-based cognitive therapy in persons with depression: A preliminary investigation. Journal of the Indian Academy of Applied Psychology. 2013;39(1):43–50. [Google Scholar]
- Sharplin GR, Jones SB, Hancock B, Knott VE, Bowden JA, Whitford HS. Mindfulness-based cognitive therapy: an efficacious community-based group intervention for depression and anxiety in a sample of cancer patients. Medical Journal of Australia. 2010;193(5):S79. doi: 10.5694/j.1326-5377.2010.tb03934.x. [DOI] [PubMed] [Google Scholar]
- Sibinga EM, Stewart M, Magyari T, Welsh CK, Hutton N, Ellen JM. Mindfulness-based stress reduction for HIV-infected youth: a pilot study. Explore (NY) 2008;4(1):36–37. doi: 10.1016/j.explore.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Sibinga EMS, Kerrigan D, Stewart M, Johnson K, Magyari T, Ellen JM. Mindfulness-based stress reduction for urban youth. The Journal of Alternative and Complementary Medicine. 2011;17(3):213–218. doi: 10.1089/acm.2009.0605. doi: http://dx.doi.org/10.1089/acm.2009.0605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibinga EMS, Perry-Parrish C, Chung S-e, Johnson SB, Smith M, Ellen JM. School-based mindfulness instruction for urban male youth: A small randomized controlled trial. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2013;57(6):799–801. doi: 10.1016/j.ypmed.2013.08.027. doi: http://dx.doi.org/10.1016/j.ypmed.2013.08.027. [DOI] [PubMed] [Google Scholar]
- Simon GE, Ludman EJ. It’s time for disruptive innovation in psychotherapy. 2009;374 doi: 10.1080/165060708. www.thelancet.com. [DOI] [PubMed] [Google Scholar]
- Simpson J, Mapel T. An investigation into the health benefits of mindfulness-based stress reduction (MBSR) for people living with a range of chronic physical illnesses in New Zealand. New Zealand Medical Journal. 2011;124(1338):68–75. [PubMed] [Google Scholar]
- Skovbjerg S, Hauge CR, Rasmussen A, Winkel P, Elberling J. Mindfulness-based cognitive therapy to treat multiple chemical sensitivities: A randomized pilot trial. Scandinavian Journal of Psychology. 2012;53(3):233–238. doi: 10.1111/j.1467-9450.2012.00950.x. [DOI] [PubMed] [Google Scholar]
- Smith A, Graham L, Senthinathan S. Mindfulness-based Cognitive Therapy for recurring depression in older people: A qualitative study. Aging & Mental Health. 2007;11(3):346–357. doi: 10.1080/13607860601086256. [DOI] [PubMed] [Google Scholar]
- Smith BW, Shelley BM, Dalen J, Wiggins K, Tooley E, Bernard J. A pilot study comparing the effects of mindfulness-based and cognitive-behavioral stress reduction. Journal of Alternative and Complementary Medicine. 2008;14(3):251–258. doi: 10.1089/acm.2007.0641. [DOI] [PubMed] [Google Scholar]
- Smith BW, Shelley BM, Leahigh L, Vanleit B. A preliminary study of the effects of a modified mindfulness intervention on binge eating. Complementary Health Practice Review. 2006;11(3):133–143. doi: http://dx.doi.org/10.1177/1533210106297217. [Google Scholar]
- Splevins K, Smith A, Simpson J. Do improvements in emotional distress correlate with becoming more mindful? A study of older adults. Aging & Mental Health. 2009;13(3):328–335. doi: 10.1080/13607860802459807. [DOI] [PubMed] [Google Scholar]
- Stange JP, Eisner LR, Hölzel BK, Peckham AD, Dougherty DD, Rauch SL, Deckersbach T. Mindfulness-based cognitive therapy for bipolar disorder: Effects on cognitive functioning. Journal of Psychiatric Practice. 2011;17(6):410–419. doi: 10.1097/01.pra.0000407964.34604.03. doi: http://dx.doi.org/10.1097/01.pra.0000407964.34604.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanton SL, Wenzel J, Connolly AB, Piferi RL. Examining mindfulness-based stress reduction: perceptions from minority older adults residing in a low-income housing facility. BMC Complementary and Alternative Medicine. 2011;11:44. doi: 10.1186/1472-6882-11-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tacón AM. Mindfulness: Existential, loss, and grief factors in women with breast cancer. Journal of Psychosocial Oncology. 2011;29(6):643–656. doi: 10.1080/07347332.2011.615382. doi: http://dx.doi.org/10.1080/07347332.2011.615382. [DOI] [PubMed] [Google Scholar]
- Tacón AM, Caldera YM, Ronaghan C. Mindfulness-based stress reduction in women with breast cancer. Families, Systems, & Health. 2004;22(2):193–203. doi: 10.1037/1091-7527.22.2.193. [DOI] [Google Scholar]
- Tacón AM, McComb J, Caldera Y, Randolph P. Mindfulness meditation, anxiety reduction, and heart disease: A pilot study. Family & Community Health: The Journal of Health Promotion & Maintenance. 2003;26(1):25–33. doi: 10.1097/00003727-200301000-00004. [DOI] [PubMed] [Google Scholar]
- Teasdale JD. Cognitive vulnerability to persistent depression. Cognition and Emotion. 1988;2:247–274. [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: Empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70(2):275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JMG. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy. 1995;33(1):25–39. doi: 10.1016/0005-7967(94)e0011-7. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68(4):615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- Thompson B. Mindfulness-based stress reduction for people with chronic conditions. The British Journal of Occupational Therapy. 2009;72(9):405–410. [Google Scholar]
- Thompson NJ, Walker ER, Obolensky N, Winning A, Barmon C, Diiorio C, Compton MT. Distance delivery of mindfulness-based cognitive therapy for depression: project UPLIFT. Epilepsy & Behavior. 2010;19(3):247–254. doi: 10.1016/j.yebeh.2010.07.031. [DOI] [PubMed] [Google Scholar]
- Troy AS, Shallcross AJ, Davis TS, Mauss IB. History of mindfulness-based cognitive therapy is associated with increased cognitive reappraisal ability. Mindfulness. 2013;4(3):213–222. doi: 10.1007/s12671-012-0114-5. doi: http://dx.doi.org/10.1007/s12671-012-0114-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang SCH, Mok ESB, Lam SC, Lee JKL. The benefit of mindfulness-based stress reduction to patients with terminal cancer. Journal of Clinical Nursing. 2012;21(17–18):2690–2696. doi: 10.1111/j.1365-2702.2012.04111.x. doi: http://dx.doi.org/10.1111/j.1365-2702.2012.04111.x. [DOI] [PubMed] [Google Scholar]
- Vallejo Z, Amaro H. Adaptation of mindfulness-based stress reduction program for addiction relapse prevention. The Humanistic Psychologist. 2009;37(2):192–206. doi: http://dx.doi.org/10.1080/08873260902892287. [Google Scholar]
- van Aalderen JR, Donders ART, Giommi F, Spinhoven P, Barendregt HP, Speckens AEM. The efficacy of mindfulness-based cognitive therapy in recurrent depressed patients with and without a current depressive episode: A randomized controlled trial. Psychological Medicine. 2012;42(5):989–1001. doi: 10.1017/S0033291711002054. [DOI] [PubMed] [Google Scholar]
- van den Hurk PAM, van Aalderen JR, Giommi F, Donders RART, Barendregt HP, Speckens AEM. An investigation of the role of attention in mindfulness-based cognitive therapy for recurrently depressed patients. Journal of Experimental Psychopathology. 2012;3(1):103–120. [Google Scholar]
- van der Lee ML, Garssen B. Mindfulness-based cognitive therapy reduces chronic cancer-related fatigue: A treatment study. Psycho-Oncology. 2012;21(3):264–272. doi: 10.1002/pon.1890. [DOI] [PubMed] [Google Scholar]
- van der Velden AM, Kuyken W, Wattar U, Crane C, Pallesen KJ, Dahlgaard J, Piet J. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clinical Psychology Review. 2015;37:26–39. doi: 10.1016/j.cpr.2015.02.001. [DOI] [PubMed] [Google Scholar]
- van Ravesteijn H, Lucassen P, Bor H, van Weel C, Speckens A. Mindfulness-based cognitive therapy for patients with medically unexplained symptoms: A randomized controlled trial. Psychotherapy and Psychosomatics. 2013;82(5):299–310. doi: 10.1159/000348588. [DOI] [PubMed] [Google Scholar]
- van Son J, Nyklicek I, Pop VJ, Blonk MC, Erdtsieck RJ, Spooren PF, Pouwer F. The effects of a mindfulness-based intervention on emotional distress, quality of life, and HbA(1c) in outpatients with diabetes (DiaMind): a randomized controlled trial. Diabetes Care. 2013;36(4):823–830. doi: 10.2337/dc12-1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch Womens Ment Health. 2008;11(1):67–74. doi: 10.1007/s00737-008-0214-3. [DOI] [PubMed] [Google Scholar]
- Vøllestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: evaluation in a randomized controlled trial. Behaviour Research and Therapy. 2011;49(4):281–288. doi: 10.1016/j.brat.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Walach H, Nord E, Zier C, Dietz-Waschkowski B, Kersig S, Schüpbach H. Mindfulness-based stress reduction as a method for personnel development: A pilot evaluation. International Journal of Stress Management. 2007;14(2):188–198. doi: http://dx.doi.org/10.1037/1072-5245.14.2.188. [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States - Results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Weber B, Jermann F, Gex-Fabry M, Nallet A, Bondolfi G, Aubry JM. Mindfulness-based cognitive therapy for bipolar disorder: a feasibility trial. European Psychiatry. 2010;25(6):334–337. doi: 10.1016/j.eurpsy.2010.03.007. [DOI] [PubMed] [Google Scholar]
- Weiss M, Nordlie JW, Siegel EP. Mindfulness-based stress reduction as an adjunct to outpatient psychotherapy. Psychotherapy and Psychosomatics. 2005;74(2):108–112. doi: 10.1159/000083169. doi: http://dx.doi.org/10.1159/000083169. [DOI] [PubMed] [Google Scholar]
- Weissbecker I, Salmon P, Studts JL, Floyd AR, Dedert EA, Sephton SE. Mindfulness-based stress reduction and sense of coherence among women with fibromyalgia. Journal of Clinical Psychology in Medical Settings. 2002;9(4):297–307. [Google Scholar]
- Weisz JR. Building Robust Psychotherapies for Children and Adolescents. Perspectives on Psychological Science. 2014;9(1):81–84. doi: 10.1177/1745691613512658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, Ng MY, Bearman SK. Odd couple? Reenvisioning the relation between science and practice in the dissemination-implementation era. Clinical Psychological Science. 2014;2(1):58–74. doi: 10.1177/2167702613501307. [DOI] [Google Scholar]
- Weitz MV, Fisher K, Lachman VD. The journey of women with breast cancer who engage in mindfulness-based stress reduction: a qualitative exploration. Holistic Nursing Practice. 2012;26(1):22–29. doi: 10.1097/HNP.0b013e31823c008b. [DOI] [PubMed] [Google Scholar]
- Whitebird RR, Kreitzer M, Crain AL, Lewis BA, Hanson LR, Enstad CJ. Mindfulness-based stress reduction for family caregivers: A randomized controlled trial. Gerontologist. 2013;53(4):676–686. doi: 10.1093/geront/gns126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG, Alatiq Y, Crane C, Barnhofer T, Fennell MJV, Duggan DS, Goodwin GM. Mindfulness-based Cognitive Therapy (MBCT) in bipolar disorder: Preliminary evaluation of immediate effects on between-episode functioning. Journal of Affective Disorders. 2008;107(1–3):275–279. doi: 10.1016/j.jad.2007.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG, Crane C, Barnhofer T, Brennan K, Duggan DS, Fennell MJ, Russell IT. Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: a randomized dismantling trial. Journal of Consulting and Clinical Psychology. 2014;82(2):275–286. doi: 10.1037/a0035036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG, Duggan DS, Crane C, Fennell MJV. Mindfulness-based cognitive therapy for prevention of recurrence of suicidal behavior. Journal of Clinical Psychology. 2006;62(2):201–210. doi: 10.1002/jclp.20223. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Kabat-Zinn J. Mindfulness: diverse perspectives on its meaning, origins, and multiple applications at the intersection of science and dharma. Contemporary Buddhism. 2011;12(1):1–18. doi: 10.1080/14639947.2011.564811. [DOI] [Google Scholar]
- Williams JMG, Teasdale JD, Segal ZV, Soulsby J. Mindfulness-based cognitive therapy reduces overgeneral autobiographical memory in formerly depressed patients. Journal of Abnormal Psychology. 2000;109(1):150–155. doi: 10.1037//0021-843x.109.1.150. [DOI] [PubMed] [Google Scholar]
- Williams MJ, McManus F, Muse K, Williams JMG. Mindfulness-based cognitive therapy for severe health anxiety (hypochondriasis): an interpretative phenomenological analysis of patients' experiences. British Journal of Clinical Psychology. 2011;50(4):379–397. doi: 10.1111/j.2044-8260.2010.02000.x. [DOI] [PubMed] [Google Scholar]
- Witek-Janusek L, Albuquerque K, Chroniak KR, Chroniak C, Durazo-Arvizu R, Mathews HL. Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain, Behavior, and Immunity. 2008;22(6):969–981. doi: 10.1016/j.bbi.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SYS, Chan FWK, Wong RLP, Chu MC, Kitty Lam YY, Mercer SW, Ma SH. Comparing the effectiveness of mindfulness-based stress reduction and multidisciplinary intervention programs for chronic pain: A randomized comparative trial. The Clinical Journal of Pain. 2011;27(8):724–734. doi: 10.1097/AJP.0b013e3182183c6e. [DOI] [PubMed] [Google Scholar]
- Worsfold KE. Embodied reflection in mindfulness-based cognitive therapy for depression. The Humanistic Psychologist. 2013;41(1):54–69. doi: http://dx.doi.org/10.1080/08873267.2012.732154. [Google Scholar]
- Würtzen H, Dalton SO, Andersen KK, Elsass P, Flyger HL, Sumbundu A, Johansen C. Who participates in a randomized trial of mindfulness-based stress reduction (MBSR) after breast cancer? A study of factors associated with enrollment among Danish breast cancer patients. Psycho-Oncology. 2013;22(5):1180–1185. doi: 10.1002/pon.3094. [DOI] [PubMed] [Google Scholar]
- Wurtzen H, Dalton SO, Elsass P, Sumbundu AD, Steding-Jensen M, Karlsen RV, Johansen C. Mindfulness significantly reduces self-reported levels of anxiety and depression: results of a randomised controlled trial among 336 Danish women treated for stage I–III breast cancer. European Journal of Cancer. 2013;49(6):1365–1373. doi: 10.1016/j.ejca.2012.10.030. [DOI] [PubMed] [Google Scholar]
- Yook K, Lee S, Ryu M, Kim K, Choi TK, Suh SY, Kim M. Usefulness of mindfulness-based cognitive therapy for treating insomnia in patients with anxiety disorders: A pilot study. Journal of Nervous and Mental Disease. 2008;196(6):501–503. doi: 10.1097/NMD.0b013e31817762ac. [DOI] [PubMed] [Google Scholar]
- Young LA, Baime MJ. Mindfulness-based stress reduction: Effect on emotional distress in older adults. Complementary Health Practice Review. 2010;15(2):59–64. doi: 10.1177/1533210110387687. [DOI] [Google Scholar]
- Young LE, Bruce A, Turner L, Linden W. Evaluation of mindfulness-based stress reduction intervention. Canadian Nurse. 2001;97(6):23–26. [PubMed] [Google Scholar]
- Zernicke KA, Campbell TS, Blustein PK, Fung TS, Johnson JA, Bacon SL, Carlson LE. Mindfulness-based stress reduction for the treatment of irritable bowel syndrome symptoms: A randomized wait-list controlled trial. International Journal of Behavioral Medicine. 2013;20(3):385–396. doi: 10.1007/s12529-012-9241-6. [DOI] [PubMed] [Google Scholar]