Abstract
Skeletal muscle is a highly plastic tissue that plays a central role in human health and disease. Aging is associated with a decrease in muscle mass and function (sarcopenia) that is associated with a loss of independence and reduced quality of life. Gut microbiota, the bacteria, archaea, viruses, and eukaryotic microbes residing in the gastrointestinal tract are emerging as a potential contributor to age-associated muscle decline. Specifically, advancing age is characterized by a dysbiosis of gut microbiota that is associated with increased intestinal permeability, facilitating the passage of endotoxin and other microbial products (e.g., indoxyl sulfate) into the circulation. Upon entering the circulation, LPS and other microbial factors promote inflammatory signaling and skeletal muscle changes that are hallmarks of the aging muscle phenotype. This review will summarize existing literature suggesting cross-talk between gut microbiota and skeletal muscle health, with emphasis on the significance of this axis for mediating changes in aging skeletal muscle size, composition, and function.
Keywords: Skeletal muscle, Gut microbiota, Aging, Inflammation, Sarcopenia
Introduction
Skeletal muscle is the largest organ in the human body, comprising ~ 40% of total body mass [1]. The musculoskeletal system is best known for its role in locomotion and postural stabilization, but also serves as a large macronutrient reservoir, protects internal organs, maintains core temperature, and communicates with other bodily through the release of growth factors and cytokines [2]. For the past decade, the endocrine nature of skeletal muscle has been extensively examined, facilitating the characterization of a muscle secretome and providing unique insights into inter-organ communication networks [3, 4]. Equally as important as the effects of skeletal muscle secreted products on peripheral tissues are the ways in which external factors may act to modify skeletal muscle. One system with tremendous potential to impact host physiology is that of gut microbiota, the bacteria, archaea, viruses, and eukaryotic microbes that reside in the gastrointestinal tract [5]. The transformative power of gut microbiota on human physiology was emphasized in a groundbreaking study by Ridaura and colleagues [6], who demonstrated that fecal microbiota transplant from obese humans into lean animals precipitated body composition shifts consistent with the phenotype of their donor, highlighting the transmissible effects of metabolic phenotype via microbial exchange.
The human body is composed of an estimated 30 trillion cells living in symbiosis with diverse microbial communities [7]. In an effort to better understand our nature as human superorganisms, a decade ago the National Institute of Health launched the human microbiome project (HMP), an international public health initiative aimed at characterizing microorganisms associated with human health and disease [8]. Making use of advances in the field of metagenomics, HMP-associated studies employ high-throughput 16 s rRNA gene sequencing to streamline the analysis of gut microbial communities [8]. Human gut microbiota are mainly composed of Bacteroidetes and Firmicutes [9], which together account for more than 90% of all phylogenetic types, and are further subdivided to consist of more than 100 distinct bacterial species [10]. The composition of gut microbiota is shown to be dynamic throughout the lifespan, undergoing rapid changes from birth until ~ 3 years of age, after which greater stability is established [11, 12]. In later years (> 65 years), however, the proclivity for aberrant changes in microbial composition appears to accelerate [13–15]. Although the underlying cause(s) (host vs environment) of this apparent age-related microbial imbalance have yet to be defined, its relevance is underscored by the growing number of studies showing associations between gut ecology and cancer [16], cardiovascular disease [17], obesity [6], diabetes [18], and muscle wasting [19], some of the most prevalent conditions afflicting older members of society today.
Gut microbiota are emerging as a salient contributor to human health and disease [5], and their effects are particularly pronounced in older years [20]. As such, the interaction between gut microbiota and other organ systems (e.g., liver and brain) has been a recent focus of scientific inquiry [21, 22]. Furthermore, the existence of a gut-muscle communication pathway has been posited [23]. The purpose of this review will be to discuss existing literature suggesting communication between gut microbiota and skeletal muscle, with emphasis on the potential significance of this axis for mediating changes in aging muscle health. We will begin by reviewing the more well-recognized impact of gut microbiota on skeletal muscle metabolism before transitioning to the lesser acknowledged role of gut microbiota on the regulation of skeletal muscle size, composition, and function. To conclude, we will integrate these findings and propose a “gut-muscle axis” that we believe plays a role in the age-related loss of muscle mass and function (sarcopenia) [24].
Gut Microbiota and Skeletal Muscle Metabolism
Gut microbiota are intricately involved in helping to perform a number of necessary functions for their host. Given their gastrointestinal habitation, perhaps the more ostensible of these roles is their influence on metabolic function (e.g., nutrient absorption and amino acid synthesis) [25]. The importance of gut microbial health in energy metabolism is exemplified by cases of Kwashiorkor, a form of severe acute malnutrition accompanied by perturbations in amino acid and carbohydrate metabolism that can be transiently ameliorated by dietary therapeutics that promote microbial reconfiguration (increased Bifidobacterium, and Lactobacillus reuteri and gasseri) [26]. Meanwhile, excess nutrient uptake and storage (i.e., obesity) is associated with low microbial diversity and changes in the relative abundance of the major bacterial phyla (Bacteroidetes and Firmicutes) [27–29]. While these findings provide support for microbial regulation of local metabolic function, evidence also suggests that gut microbiota may impact distal metabolic activity in skeletal muscle tissues [23, 30].
In a pioneering study conducted in 2004, Backhed et al. infused germ-free (GF) mice, animals born and raised in sterile conditions and lacking a microbiome, with the cecal contents of conventionally raised animals, and demonstrated a 60% increase in body fat with reciprocal reductions in insulin sensitivity and glucose tolerance [31]. As skeletal muscle is an integral component of glucose disposal, these findings suggest microbial-mediated regulation of muscle metabolic function. In support of this sentiment, bacterial colonization of GF mice appears to decrease skeletal muscle metabolic efficiency, as evidenced by an increase in tricarboxylic acid cycle intermediates without an appreciable increase in high-energy phosphate stores [31]. To understand the seemingly superior metabolic phenotype in microbiome-deficient mice, the same research group compared skeletal muscle protein activity and gene expression in GF and conventionally raised animals [23]. Compared to mice with gut microbiota, skeletal muscle from GF mice was characterized by markedly greater activity of AMP-activated protein kinase (AMPK) and carnitine palmitoyl transferase-1 (CPT-1), indicative of an elevated oxidative capacity. Taken together, these early studies suggest that gut microbiota can influence body composition by means of regulating skeletal muscle bioenergetic pathways.
To identify a mechanistic link between microbial dysbiosis and metabolic derangement (i.e., skeletal muscle insulin resistance), Cani et al. [18] subjected young mice to a high-fat diet, which is known to induce chronic low-grade chronic inflammation (e.g., IL-1, IL-6, and TNF-α elevation), a reported contributor to insulin resistance [32, 33]. As expected, high-fat fed mice exhibited an increase in body weight and inflammatory markers as well as a decrease in glucose tolerance. In addition, circulating levels of lipopolysaccharide (LPS), a component of the outer membrane of gram negative bacteria, were 2- to-3-fold elevated in high-fat fed mice when compared with control fed animals. Pertinently, high-fat feeding is shown to compromise epithelial tight junctions and increase intestinal permeability [34, 35], evidence that suggests a role for high-fat induced leak of LPS from the intestine into the circulation.
To examine the contribution of circulating LPS (i.e., metabolic endotoxemia) to insulin insensitivity, the same research team subjected wild-type and CD-14 mutant mice, which lack an endotoxin receptor, to LPS infusion [18]. In support of LPS-mediated dysregulation of insulin signaling, pro-inflammatory cytokine induction and impairments in glucose tolerance were observed exclusively in the wild-type animals. Endotoxin-mediated reductions in glucose tolerance have been similarly shown in humans inoculated with LPS, as evidenced by significant increases in skeletal muscle NF-κβ binding activity and JNK phosphorylation, which synergistically inhibit insulin signaling [36]. These studies and others [30, 37], show that circulating LPS, a prominent component of gut microbiota, induces skeletal muscle inflammation and insulin resistance thereby contributing to the development of metabolic syndrome. While these findings implicate LPS and inflammation as causative agents in the process, inflammation-independent alterations in skeletal muscle metabolism have also been observed. For example, in response to the gut microbiota-specific metabolite indoxyl sulfate [38], C2C12 myoblasts exhibit an up-regulation of glycolysis and an increase in the activity of the pentose phosphate pathway [39]. Similarly, exposure of myotubes to gut microbial-derived extracellular vesicles induces insulin resistance [30], highlighting the multitude of ways in which gut microbiota may influence the metabolic function of skeletal muscle.
Insulin-resistant type 2 diabetes may occur at any age, but its prevalence is greater in older years (> 25% in persons ≥ 65 years) [40]. Older adults with diabetes are at an increased risk for cardiovascular complications, reduced functional status, loss of independence, and mortality [41]. With the relationship between inflammation and insulin resistance in mind, Ghosh et al. sought to assess the contribution of circulating endotoxin to this age-related inflammatory/insulin-resistant phenotype [42]. As hypothesized, in older individuals circulating LPS and skeletal muscle TLR4 (a receptor for LPS [43]) gene expression and protein content were higher, and insulin sensitivity (quantified by HOMA-IR) was lower than their younger counterparts. These findings suggest that an age-related increase in LPS levels might contribute to the greater occurrence of diabetes in older persons.
Gut Microbiota and Skeletal Muscle Size, Composition, and Function
Muscle Size
Age-related inflammation is associated with reductions in skeletal muscle size and function (sarcopenia) [44]. Furthermore, obesity appears to exacerbate the progression of sarcopenia by compounding inflammatory burden [45], resulting in a state of sarcopenic obesity, defined as inadequate muscle mass relative to total body size [24]. A variety of phenomena have been proposed to contribute to this age-related heightened inflammatory state including redox stress [46], immuno- and endocrine senescence [47, 48], DNA damage [49], epigenetic modification [50], and a distortion of gut microbial homeostasis [51] that is associated with increased levels of circulating endotoxin [42]. An extreme model of LPS-induced inflammation is the clinical condition sepsis, a life-threatening illness characterized by severe muscle wasting due to both increases in proteolytic degradation and reductions in protein synthesis [52]. Ubiquitously discussed in the context of skeletal muscle inflammation, TNF-α and IL-6 are strongly induced by circulating LPS [53] and elevated in aging individuals [54, 55]. Macrophage production of TNF-α is shown to occur early in the stress response, and has been demonstrated to stimulate protein degradation and apoptosis in cultured cells [56, 57]. Meanwhile, secreted by both macrophages and T-cells, studies in both animals and humans implicate IL-6 involvement in the repression of protein synthesis [58, 59]. Interpreted in unison, these findings demonstrate the ability of LPS-associated cytokines to determinately affect protein equilibrium (i.e., synthesis and breakdown), and suggest that elevated endotoxin levels with age may contribute to reductions in muscle mass. It is interesting to note that the tryptophan derivative indoxyl sulfate, which is similarly shown to increase with age [60], is reported to induce inflammatory cytokine expression (IL-6 and TNF-α) and markers of muscle atrophy (myostatin and atrogin-1) similar to that of LPS in cultured myocytes [61]. Furthermore, in vivo administration of indoxyl sulfate is shown to increase atrogene expression in conjunction with decreased muscle mass in mice [61]. These findings highlight the importance of comprehensively examining microbial metabolites for triggers of myocellular adaptation [62], rather than focusing on a single microbial byproduct.
From a feasibility standpoint, the ability to influence skeletal muscle size by altering the composition of gut microbiota is attractive, particularly in circumstances where muscle loading may be challenging (e.g., immobilization, hospitalization, spaceflight). One of the first studies to target gut microbiota as a means to affect lean tissue mass was conducted by Bindels et al. using a leukemic mouse model [19]. Microbial profiling in these cachectic mice revealed gut dysbiosis characterized by selective modulation of Lactobacillus spp. To restore lactobacilli levels, the leukemic mice were given an oral probiotic containing Lactobacillus reuteri and L. gasseri that appeared to decrease serum levels of inflammatory cytokines (IL-6 and MCP-1) and atrogene expression (MuRF1 and Atrogin-1) in conjunction with an increase in mass of the tibialis anterior. Interestingly, these effects appear to be bacterial species specific, as L. acidophilus supplementation did not appear to affect inflammatory or atrophy markers [19]. However, L. plantarum supplementation has demonstrated to increase lean mass and function (grip strength and swim time) in healthy young mice [63]. Taken together, these studies suggest a link between Lactobacillus species and skeletal muscle size that is worthy of further investigation in humans.
Prebiotics are fermented non-digestible compounds that support the proliferation of health-promoting bacteria [64] and thus may influence skeletal muscle health. The efficacy of prebiotic supplementation to support beneficial skeletal muscle changes was demonstrated in a study by Cani et al., who showed a decrease in circulating LPS and inflammation and an increase in muscle mass in obese mice fed the prebiotic fiber oligofructose [65]. Follow-up analyses confirmed the favorable effect of prebiotic feeding on gut microbiota, as was evidenced by a shift in the ratio of Bacteroidetes/Firmicutes in addition to increases in the levels of Lactobacillus and Bifidobacterium spp. [66]. In further support of a link between prebiotics with skeletal muscle, administration of a synbiotic containing inulin-type fructans and Lactobacillus reuteri was shown to reverse increases in Escherichia and promoted proliferation of Lactobacillus and Bifidobacterium in leukaemic mice [67]. Coupling of these microbial alterations with restoration of intestinal homeostasis (e.g., increase tight junction proteins) and a reduction in muscle wasting suggests that Lactobacillus and Bifidobacterium may influence gut-muscle communication and regulate muscle size. Interestingly, Bifidobacterium are shown to decrease with age [68], and are associated with lower intestinal [69] and circulating LPS levels [70]. Thus, an age-related decrease in gut Bifidobacterium content may underlie increases in circulating endotoxin that are shown to induce skeletal muscle atrophy [71]. While we were not able to identify any studies showing Bifidobacterium supplementation to increase muscle mass, data showing butyrate (associated with Bifidobacterium [72]) treatment to protect against age-related muscle atrophy [73] supports the idea that pre- and/or probiotic supplementation, which is shown to increase the abundance of Bifidobacterium and butyrate producers in older individuals [74, 75], may prophylactically moderate aging muscle loss.
Muscle Composition
While the age-associated loss of muscle mass is purported to play a role in the loss of strength and function [76, 77], strength declines far exceed reductions in muscle mass [78], suggesting a change in intrinsic muscle function (i.e., muscle quality). Although a number of factors have been implicated in aging muscle quality deficits [79, 80], adipose tissue infiltration in skeletal muscle (i.e., change in muscle composition) has been shown to increase with age [81] and is associated with mobility impairment [82]. To assess the relationship between gut microbiota, inflammation, and muscle composition, Collins et al. subjected young rats to a high-fat high-sucrose diet and found an increase in Enterobacteriaceae (gram-negative member of the Proteobacteria phylum) and a decrease in the abundance of Lactobacillus spp., changes that have been similarly reported with aging [83, 84]. Concomitant with these changes, the authors reported an increase in circulating inflammatory cytokines (IL-6, TNF-α, and MCP-1) and intramuscular fat after just 3 days [85], suggesting rapid dysregulation of these seemingly inter-connected systems. Regulation of muscle composition by gut microbiota is supported by associations between gut bacteria involved in energy metabolism and porcine intramuscular fat content [86]. Furthermore, age-related changes in gut microbiota have also been proposed to evoke fat infiltration into bone [87, 88], culminating in a triad of aberrant muscle, bone, and adipose tissue dysregulation (osteosarcopenic obesity). A limitation of these analyses is an inability to distinguish if changes in microbiota are a driver or a product of this compromise to bone and muscle integrity. However, probiotic rescue (Lactobacillus reuteri and gasseri) of inflammation and muscle/bone loss in mice proposes that gut microbiota initiate this relationship [19, 67, 89].
Also contributing to changes in muscle composition, aging has been associated with alterations in myosin heavy chain (MHC) distribution [90]. Specifically, aging muscle appears to undergo a fast-to-slow fiber-type shift [91], that is hypothesized to reduce whole muscle power and increase fall risk [92, 93]. Although a topic of intense scrutiny, studies have yet to elucidate a definitive mechanism underlying this phenomenon. It is thus interesting to note that over the course of the past year, two independent studies have observed changes in skeletal muscle MHC composition following interventions aimed at manipulating gut microbiota [63, 94]. Pertinently, in one of these studies by Yan and colleagues [94], transfer of gut microbiota from an obese pig to a GF mouse replicated the host myocellular phenotype, which mirrored that of aging skeletal muscle (i.e., fast fiber atrophy concomitant with a fast-to-slow fiber type shift). These findings highlight the possibility that gut microbiota can transfer muscle fiber characteristics, and open the door for studies investigating the transplant of microbiota from young to old as a means to improve skeletal muscle size and composition.
Muscle Function
Age-related changes in skeletal muscle size and composition summate to yield reductions in skeletal muscle function (strength and power) [77] that ultimately affect physical performance and the ability to live independently [95]. One of the first studies to link changes in gut microbiota with functional capacity was conducted by van Tongeren et al. [84], who studied fecal microbes in a relatively small cohort of advanced agers (n = 23; ~ 86 years). Upon stratifying subjects by frailty score, a unique bacterial signature characterized by marked reductions in Lactobacillus (~ 8-fold less) and commensurate increases in the quantity of Enterobacteriaceae (~ 6-fold more) in frail agers emerged. Moreover, higher functioning subjects may have been protected from dysbiotic shifts in gut microbiota by a greater abundance of butyrate-producing bacteria such as Faecalibacterium prausnitzii. Indeed, butyrate is shown to enhance intestinal barrier function by reinforcing tight junction assembly [96], which, in theory, should prevent endotoxin translocation and reduce circulating inflammation [97]. The association between butyrate-generating bacteria and functional capacity is supported by metagenomics findings in a larger sample of older adults (n = 178; ~ 78 years) [98] demonstrating that community-dwelling elders had more butyrate-producing microbes than those in long-stay residence. Additionally, institutionalized elderly had a greater abundance of Enterobacteriaceae and Escherichia/Shigella, and less gut microbial diversity when compared with the community dwellers. Given the corresponding change in diet (i.e., low in plant-based nutrients and fiber and high in sucrose and saturated fat) and microbial composition when individuals enter long-term care facilities [99], geriatric clinicians are encouraged to work with older individuals undergoing residence relocation to pursue nutritional strategies that aim to prevent the loss of healthy microbes (e.g., butyrate-producing bacteria). Relevantly, prebiotic supplementation (inulin plus fructooligosaccharides) has been shown to increase muscle strength (handgrip) and endurance (exhaustion) in frail older adults [100], thereby highlighting the utility of prebiotic supplementation as a treatment for age-associated deficits in muscle function.
Studies investigating gut microbiota of athletes provide unique insight into microbial characteristics associated with high levels of physical function. Comparison of these bacterial traits to those of populations with reduced functional capacity (e.g., mobility-limited older adults) can provide data-driven targets for therapeutic intervention. One of the first investigations to assess gut microbiota in athletes was conducted by Clarke et al. who studied elite rugby players, individuals with large quantities of lean muscle tissue [101]. Comparison of microbial diversity among these athletes and both healthy normal weight (BMI ≤ 25) and overweight (BMI ≥ 28) age-matched controls elicited a hierarchical pattern (athletes > healthy > overweight), suggesting an association between microbial diversity, body composition, and physical function. While these findings implicate exercise training as a possible therapy for favorably altering the gut microbiota, greater total energy and protein intake in the athlete group may have affected these results. However, correlations between microbial diversity and cardiorespiratory fitness [102] in concert with the exercise training mediated rescue of high-fat diet-induced microbial disturbance [103] support the idea that exercise training may impart beneficial effects on gut health. In particular, regular physical activity may help to combat reductions in butyrate-producing microbiota (Clostridiales, Roseburia, Lachnospiraceae, and Erysipelotrichaceae) [102] and Lactobacillus levels [103] that are commonly seen with aging [15, 84, 98]. The beneficial changes in gut health seen with exercise training implicate skeletal muscle contraction as a regulator of microbial composition, and provide evidence for bi-directional gut-muscle effects. As a result, the superior microbial milieu in exercise trained persons may explain lower levels of plasma endotoxin and inflammatory markers (plasminogen activator inhibitor type-1) in active vs sedentary individuals [104]. Interpreted as a whole, these findings advocate that exercise training is an effective means to promote beneficial changes in gut microbial health that seem to reduce circulating inflammation and support the maintenance of muscle mass and function.
Establishing an Aging Gut-Muscle Communication Axis
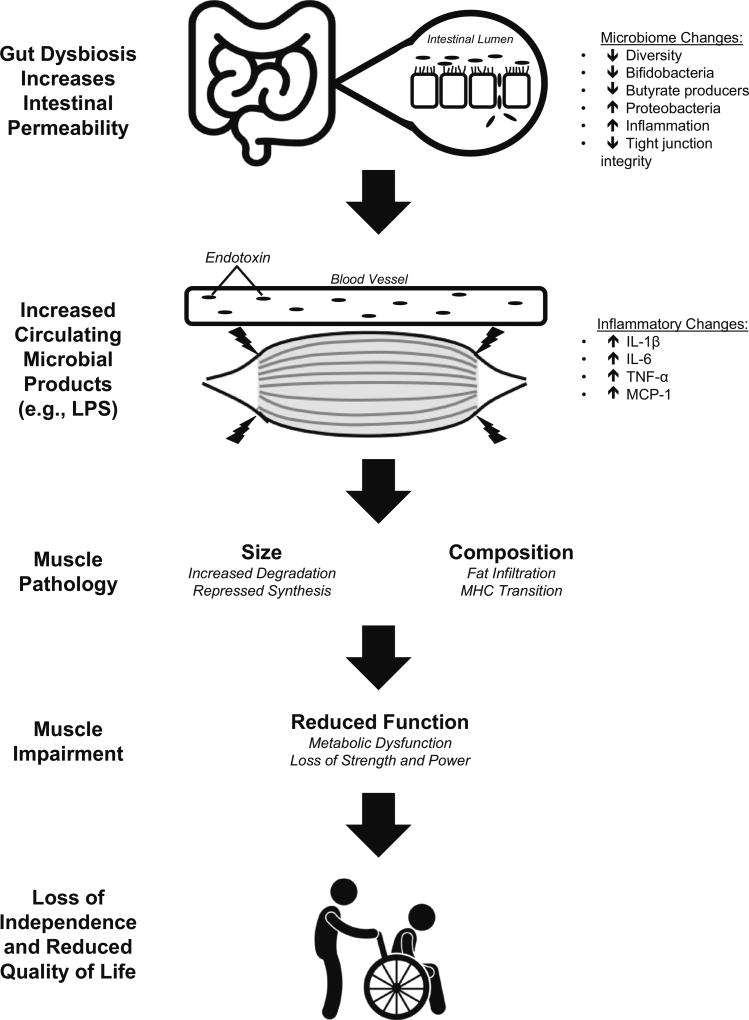
Inspection of the existing literature suggests that gut microbiota may play an important role in influencing aging skeletal muscle health (Fig. 1). We propose regulation of skeletal muscle by gut microbiota to occur in an endocrine manner, beginning with a disturbance in gut homeostasis and culminating with alterations in skeletal muscle characteristics. While changes in gut microbiota can be attributed to either host (genetics, age) or environmental (activity, diet) factors, we have focused on microbial dynamics with organismal aging. Although limited in number, investigations of age-related changes in gut microbiota describe a bacterial community that is both less diverse and lacking in microorganisms responsible for the production of butyrate (indicative of gastrointestinal health) [15, 84, 98, 99], and more abundant in pathogens belonging to the Proteobacteria phylum (e.g., Enterobacteriaceae) [15, 68, 83]. Associated with these changes is a decrease in the integrity of epithelial tight junctions and increased intestinal permeability [14], facilitating the translocation of microbial byproducts into circulation. Perhaps the most widely studied of these bacterial derivatives is LPS, the major component of the outer membrane of gram-negative bacteria that is found to be elevated in the circulation with aging [42]. Once in the blood, circulating endotoxin promotes systemic inflammation that appears to trigger maladaptation of skeletal muscle. As described throughout this review, these changes may manifest in older adults as decreases in muscle size and integrity that compromise physical function and ultimately detract from quality of life.
Fig. 1.
A gut-muscle axis that contributes to age-related changes in skeletal muscle size, composition, and function. Microbial shifts in the aging gut reduce tight junction integrity and increasing intestinal permeability allowing for the passage of microbial products (e.g., LPS, indoxyl sulfate, butyrate) into the blood. Once in the circulation, endotoxin and other microbial factors trigger pro-inflammatory signaling that is hypothesized to promote skeletal muscle atrophy concomitant with deleterious composition shifts. These changes lead to impairments in both the metabolic and contractile characteristics of skeletal muscle that reduce functional capacity and ultimately compromise functional independence and quality of life in older adults
Perspectives and Steps Forward
In 2008, the NIH launched the Human Microbiome Project as a public health initiative to characterize the microorganisms contributing to human health and disease. In just a decade’s time, high-throughput 16 s rRNA gene sequencing techniques have identified robust associations between gut microbial ecology and many of the leading causes of death worldwide (e.g., heart disease, cancer, and diabetes) [16–18]. Although this field is still in its infancy, the data presented here provide evidence to suggest a bidirectional communication network between gut microbiota and skeletal muscle. This relationship is exemplified by commensurate changes in gut health and skeletal muscle with aging. Research in murine models has begun to identify microbial targets with likely skeletal muscle ramifications. These findings lay the framework for strategic human interventions aiming to manipulate microbial ecology as a means to benefit skeletal muscle health and extend healthy life years in a rapidly expanding aging population.
Acknowledgments
Funding These ideas are based on work supported by the U.S. Department of Agriculture (USDA), under agreement No. 58-1950-4-003. Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the authors and do not necessarily reflect the view of the USDA. Mention of trade names or commercial products in this publication is solely for the purpose of providing specific information and does not imply recommendation or endorsement by the USDA. M.S.L. is supported by NIA K01 award #5K01AG050700-02.
Conflict of interest Dr. Fielding reports grants, personal fees, and other from Axcella Health; personal fees from Cytokinetics; grants and personal fees from Biophytis; personal fees from Amazentis; grants and personal fees from Nestlé; grants and personal fees from Astellas; personal fees from Glaxo Smithkline, outside the submitted work.
Footnotes
Author Contributions RAF proposed writing the manuscript. MSL and GJG conducted the literature search. GJG drafted the manuscript. All authors edited, revised, and approved the manuscript.
References
- 1.Guridi M, Tintignac LA, Lin S, Kupr B, Castets P, Ruegg MA. Activation of mTORC1 in skeletal muscle regulates whole-body metabolism through FGF21. Sci Signal. 2015;8:113. doi: 10.1126/scisignal.aab3715. [DOI] [PubMed] [Google Scholar]
- 2.Pedersen BK, Febbraio MA. Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol Rev. 2008;88:1379–1406. doi: 10.1152/physrev.90100.2007. [DOI] [PubMed] [Google Scholar]
- 3.Bortoluzzi S, Scannapieco P, Cestaro A, Danieli GA, Schiaffino S. Computational reconstruction of the human skeletal muscle secretome. Proteins. 2006;62:776–792. doi: 10.1002/prot.20803. [DOI] [PubMed] [Google Scholar]
- 4.Henningsen J, Rigbolt KT, Blagoev B, Pedersen BK, Kratchmarova I. Dynamics of the skeletal muscle secretome during myoblast differentiation. Mol Cell Proteomics. 2010;9:2482–2496. doi: 10.1074/mcp.M110.002113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shreiner AB, Kao JY, Young VB. The gut microbiome in health and in disease. Curr Opin Gastroenterol. 2015;31:69–75. doi: 10.1097/MOG.0000000000000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ridaura VK, Faith JJ, Rey FE, Cheng J, Alexis E, Kau AL, Griffin NW, Lombard V, Henrissat B, Bain JR, Muehlbauer MJ, Ilkayeva O, Semenkovich CF, Funai K, Hayashi DK, Lyle BJ, Martini MC, Luke K, Clemente JC, Treuren WV, Walters WA. Cultured gut microbiota from twins discordant for obesity modulate adiposity and metabolic phenotypes in mice. Science. 2014;341:1–22. doi: 10.1126/science.1241214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sender R, Fuchs S. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016;14:e1002533. doi: 10.1371/journal.pbio.1002533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The human microbiome project. Nature. 2007;449:804–810. doi: 10.1038/nature06244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, Gill SR, Nelson KE, Relman DA. Diversity of the human intestinal microbial flora. Science. 2005;308:1635–1638. doi: 10.1126/science.1110591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rajilic-Stojanovic M, de Vos WM. The first 1000 cultured species of the human gastrointestinal microbiota. FEMS Microbiol Rev. 2014;38:996–1047. doi: 10.1111/1574-6976.12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, Magris M, Hidalgo G, Baldassano RN, Anokhin AP, Heath AC, Warner B, Reeder J, Kuczynski J, Caporaso JG, Lozupone CA, Lauber C, Clemente JC, Knights D, Knight R, Gordon JI. Human gut microbiome viewed across age and geography. Nature. 2012;486:222–227. doi: 10.1038/nature11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hill CJ, Lynch DB, Murphy K, Ulaszewska M, Jeffery IB, O’Shea C, Watkins C, Dempsey E, Mattivi F, Tuohy K, Ross RP, Ryan CA, O’Toole P, Stanton C. Evolution of gut microbiota composition from birth to 24 weeks in the INFANTMET Cohort. Microbiome. 2017;5:4. doi: 10.1186/s40168-016-0213-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langille MG, Meehan CJ, Koenig JE, Dhanani AS, Rose RA, Howlett SE, Beiko RG. Microbial shifts in the aging mouse gut. Microbiome. 2014;2:50. doi: 10.1186/s40168-014-0050-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thevaranjan N, Puchta A, Schulz C, Naidoo A, Szamosi JC, Verschoor CP, Loukov D, Schenck LP, Jury J, Foley KP, Schertzer JDL, Maggie J, Davidson DJ, Verd EF, Surette MG, Bowdish D. Age-associated microbial dysbiosis promotes intestinal permeability, systemic inflammation, and macrophage dysfunction. Cell Host Microbe. 2017;21:455–466. doi: 10.1016/j.chom.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rampelli S, Candela M, Turroni S, Collino EB, Franceschi C, O’Toole PW, Brigidi P. Functional metagenomic profiling of intestinal microbiome in extreme ageing. Aging. 2013;5:902–912. doi: 10.18632/aging.100623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu LX, Yan HX, Liu Q, Yang W, Wu HP, Dong W, Tang L, Lin Y, He YQ, Zou SS, Wang C, Zhang HL, Cao GW, Wu MC, Wang HY. Endotoxin accumulation prevents carcinogen-induced apoptosis and promotes liver tumorigenesis in rodents. Hepatology. 2010;52:1322–1333. doi: 10.1002/hep.23845. [DOI] [PubMed] [Google Scholar]
- 17.Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, Wu Y, Hazen SL. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368:1575–1584. doi: 10.1056/NEJMoa1109400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, Ferrie J, Gibson GR, Casteilla L, Delzenne NM, Alessi MC. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56:1761–1772. doi: 10.2337/db06-1491. [DOI] [PubMed] [Google Scholar]
- 19.Bindels LB, Beck R, Schakman O, Martin JC, de Backer F, Sohet FM, Dewulf EM, Pachikian BD, Neyrinck AM, Thissen JP, Verrax J, Calderon PB, Pot B, Grangette C, Cani PD, Scott KP, Delzenne NM. Restoring specific lactobacilli levels decreases inflammation and muscle atrophy markers in an acute leukemia mouse model. PLoS ONE. 2012;7:1–10. doi: 10.1371/journal.pone.0037971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lustgarten MS. Classifying aging as a disease: the role of microbes. Front Genet. 2016;7:212. doi: 10.3389/fgene.2016.00212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28:203–209. [PMC free article] [PubMed] [Google Scholar]
- 22.Vajro P, Paolella G, Fasano A. Microbiota and gut-liver axis: a mini-review on their influences on obesity and obesity related liver disease. J Pediatr Gastroenterol. 2013;56:461–468. doi: 10.1097/MPG.0b013e318284abb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bäckhed F, Manchester JK, Semenkovich CF, Gordon JI. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci USA. 2007;104:979–984. doi: 10.1073/pnas.0605374104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, Abellan van Kan G, Andrieu S, Bauer J, Breuille D, Cederholm T, Chandler J, De Meynard C, Donini L, Harris T, Kannt A, Keime Guibert F, Onder G, Papanicolaou D, Rolland Y, Rooks D, Sieber C, Souhami E, Verlaan S, Zamboni M. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12:249–256. doi: 10.1016/j.jamda.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jumpertz R, Le DS, Turnbaugh PJ, Trinidad C, Bogardus C, Gordon JI, Krakoff J. Energy-balance studies reveal associations between gut microbes, caloric load, and nutrient absorption in humans. Am J Clin Nutr. 2011;94:58–65. doi: 10.3945/ajcn.110.010132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith MI, Yatsunenko T, Manary MJ, Trehan I, Mkakosya R, Cheng J, Kau AL, Rich SS, Concannon P, Mychaleckyj JC, Liu J, Houpt E, Li JV, Holmes E, Nicholson J, Knights D, Ursell LK, Knight R, Gordon JI. Gut microbiomes of malawian twin pairs discordant for kwashiorkor. Science. 2013;339:548–554. doi: 10.1126/science.1229000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vrieze A, Nood E, Holleman F, Salojärvi J, Kootte R, Bartelsman J, Dallinga G, Thie Ackermans M, Serlie M, Oozeer R, Derrien M, Druesne A, Van Hylckama Vlieg J, Bloks V, Groen A, Heilig H, Zoetendal E, Stroes E, De Vos W, Hoekstra J, Nieuwdorp M. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143:913–916. doi: 10.1053/j.gastro.2012.06.031. [DOI] [PubMed] [Google Scholar]
- 28.Turnbaugh PJ, Hamady M, Yatsunenko T, Cantarel BL, Duncan A, Ley RE, Sogin ML, Jones WJ, Roe BA, Affourtit JP, Egholm M, Henrissat B, Heath AC, Knight R, Gordon JI. A core gut microbiome in obese and lean twins. Nature. 2009;457:480–484. doi: 10.1038/nature07540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, Almeida M, Arumugam M, Batto J-M, Kennedy S, Leonard P, Li J, Burgdorf K, Grarup N, Jørgensen T, Brandslund I, Nielsen HB, Juncker AS, Bertalan M, Levenez F, Pons N, Rasmussen S, Sunagawa S, Tap J, Tims S, Zoetendal EG, Brunak S, Clément K, Doré J, Kleerebezem M, Kristiansen K, Renault P, Sicheritz-Ponten T, de Vos WM, Zucker J-D, Raes J, Hansen T, Bork P, Wang J, Ehrlich SD, Pedersen O, Guedon E, Delorme C, Layec S, Khaci G, van de Guchte M, Vandemeulebrouck G, Jamet A, Dervyn R, Sanchez N, Maguin E, Haimet F, Winogradski Y, Cultrone A, Leclerc M, Juste C, Blottière H, Pelletier E, LePaslier D, Artiguenave F, Bruls T, Weissenbach J, Turner K, Parkhill J, Antolin M, Manichanh C, Casellas F, Boruel N, Varela E, Torrejon A, Guarner F, Denariaz G, Derrien M, van Hylckama Vlieg JET, Veiga P, Oozeer R, Knol J, Rescigno M, Brechot C, M’Rini C, Mérieux A, Yamada T. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013;500:541–546. doi: 10.1038/nature12506. [DOI] [PubMed] [Google Scholar]
- 30.Choi Y, Kwon Y, Kim D-K, Jeon J, Jang SC, Wang T, Ban M, Kim M-H, Jeon SG, Kim M-S, Choi CS, Jee Y-K, Gho YS, Ryu SH, Kim Y-K. Gut microbe-derived extracellular vesicles induce insulin resistance, thereby impairing glucose metabolism in skeletal muscle. Sci Rep. 2015;5:15878. doi: 10.1038/srep15878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, Semenkovich CF, Gordon JI. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci USA. 2004;101:15718–15723. doi: 10.1073/pnas.0407076101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hotamisligil GS, Peraldi P, Budavari A, Ellis R, White MF, Spiegelman BM. IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-alpha- and obesity-induced insulin resistance. Science. 1996;271:665–668. doi: 10.1126/science.271.5249.665. [DOI] [PubMed] [Google Scholar]
- 33.Senn JJ, Klover PJ, Nowak IA, Mooney RA. Interleukin-6 induces cellular insulin resistance in hepatocytes. Diabetes. 2002;51:3391–3399. doi: 10.2337/diabetes.51.12.3391. [DOI] [PubMed] [Google Scholar]
- 34.Gulhane M, Murray L, Lourie R, Tong H, Sheng YH, Wang R, Kang A, Schreiber V, Wong KY, Magor G, Denman S, Begun J, Florin TH, Perkins A, Cuiv PO, McGuckin MA, Hasnain SZ. High fat diets induce colonic epithelial cell stress and inflammation that is reversed by IL-22. Sci Rep. 2016;6:28990. doi: 10.1038/srep28990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guo S, Al-Sadi R, Said HM, Ma TY. Lipopolysaccharide causes an increase in intestinal tight junction permeability in vitro and in vivo by inducing enterocyte membrane expression and localization of TLR-4 and CD14. Am J Pathol. 2013;182:375–387. doi: 10.1016/j.ajpath.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aguirre V, Uchida T, Yenush L, Davis R, White MF. The c-Jun NH(2)-terminal kinase promotes insulin resistance during association with insulin receptor substrate-1 and phosphorylation of Ser(307) J Biol Chem. 2000;275:9047–9054. doi: 10.1074/jbc.275.12.9047. [DOI] [PubMed] [Google Scholar]
- 37.Liang H, Hussey SE, Sanchez-Avila A, Tantiwong P, Musi N. Effect of lipopolysaccharide on inflammation and insulin action in human muscle. PLoS ONE. 2013;8:e63983. doi: 10.1371/journal.pone.0063983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wikoff WR, Anfora AT, Liu J, Schultz PG, Lesley SA, Peters EC, Siuzdak G. Metabolomics analysis reveals large effects of gut microflora on mammalian blood metabolites. Proc Natl Acad Sci USA. 2009;106:3698–3703. doi: 10.1073/pnas.0812874106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sato E, Mori T, Mishima E, Suzuki A, Sugawara S, Kurasawa N, Saigusa D, Miura D, Morikawa-Ichinose T, Saito R, Oba-Yabana I, Oe Y, Kisu K, Naganuma E, Koizumi K, Mokudai T, Niwano Y, Kudo T, Suzuki C, Takahashi N, Sato H, Abe T, Niwa T, Ito S. Metabolic alterations by indoxyl sulfate in skeletal muscle induce uremic sarcopenia in chronic kidney disease. Sci Rep. 2016;6:36618. doi: 10.1038/srep36618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, Huang ES, Korytkowski MT, Munshi MN, Odegard PS, Pratley RE, Swift CS. Diabetes in older adults. Diabetes Care. 2012;35:2650–2664. doi: 10.2337/dc12-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brown AF, Mangione CM, Saliba D, Sarkisian CA. Guidelines for improving the care of the older person with diabetes mellitus. J Am Geriatr Soc. 2003;51:S265–S280. doi: 10.1046/j.1532-5415.51.5s.1.x. [DOI] [PubMed] [Google Scholar]
- 42.Ghosh S, Lertwattanarak R, Garduno Jde J, Galeana JJ, Li J, Zamarripa F, Lancaster JL, Mohan S, Hussey S, Musi N. Elevated muscle TLR4 expression and metabolic endotoxemia in human aging. J Gerontol A Biol Sci Med Sci. 2015;70:232–246. doi: 10.1093/gerona/glu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chow JC, Young DW, Golenbock DT, Christ WJ, Gusovsky F. Toll-like receptor-4 mediates lipopolysaccharide-induced signal transduction. J Biol Chem. 1999;274:10689–10692. doi: 10.1074/jbc.274.16.10689. [DOI] [PubMed] [Google Scholar]
- 44.Jensen GL. Inflammation: roles in aging and sarcopenia. J Parenter Enteral Nutr. 2008;32:656–659. doi: 10.1177/0148607108324585. [DOI] [PubMed] [Google Scholar]
- 45.Cesari M, Kritchevsky SB, Baumgartner RN, Atkinson HH, Penninx BW, Lenchik L, Palla SL, Ambrosius WT, Tracy RP, Pahor M. Sarcopenia, obesity, and inflammation–results from the trial of angiotensin converting enzyme inhibition and novel cardiovascular risk factors study. Am J Clin Nutr. 2005;82:428–434. doi: 10.1093/ajcn.82.2.428. [DOI] [PubMed] [Google Scholar]
- 46.Sohal RS, Orr WC. The redox stress hypothesis of aging. Free Radic Biol Med. 2012;52:539–555. doi: 10.1016/j.freeradbiomed.2011.10.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Franceschi C, Bonafe M, Valensin S. Human immunosenescence: the prevailing of innate immunity, the failing of clonotypic immunity, and the filling of immunological space. Vaccine. 2000;18:1717–1720. doi: 10.1016/s0264-410x(99)00513-7. [DOI] [PubMed] [Google Scholar]
- 48.Maggio M, Basaria S, Ble A, Lauretani F, Bandinelli S, Ceda GP, Valenti G, Ling SM, Ferrucci L. Correlation between testosterone and the inflammatory marker soluble interleukin-6 receptor in older men. J Clin Endocrinol Metab. 2006;91:345–347. doi: 10.1210/jc.2005-1097. [DOI] [PubMed] [Google Scholar]
- 49.Cavanagh MM, Weyand CM, Goronzy JJ. Chronic inflammation and aging: DNA damage tips the balance. Curr Opin Immunol. 2012;24:488–493. doi: 10.1016/j.coi.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Munoz-Najar U, Sedivy JM. Epigenetic control of aging. Antioxid Redox Signal. 2011;14:241–259. doi: 10.1089/ars.2010.3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cevenini E, Caruso C, Candore G, Capri M, Nuzzo D, Duro G, Rizzo C, Colonna-Romano G, Lio D, Di Carlo D, Palmas MG, Scurti M, Pini E, Franceschi C, Vasto S. Age-related inflammation: the contribution of different organs, tissues and systems. How to face it for therapeutic approaches. Curr Pharm Des. 2010;16:609–618. doi: 10.2174/138161210790883840. [DOI] [PubMed] [Google Scholar]
- 52.Callahan LA, Supinski GS. Sepsis-induced myopathy. Crit Care Med. 2009;37:S354–S367. doi: 10.1097/CCM.0b013e3181b6e439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Frost RA, Nystrom GJ, Lang CH. Lipopolysaccharide regulates proinflammatory cytokine expression in mouse myoblasts and skeletal muscle. Am J Physiol Regul Integr Comp Physiol. 2002;283:R698–R709. doi: 10.1152/ajpregu.00039.2002. [DOI] [PubMed] [Google Scholar]
- 54.Bruunsgaard H, Andersen-Ranberg K, Jeune B, Pedersen AN, Skinhoj P, Pedersen BK. A high plasma concentration of TNF-alpha is associated with dementia in centenarians. J Gerontol A Biol Sci Med Sci. 1999;54:M357–M364. doi: 10.1093/gerona/54.7.m357. [DOI] [PubMed] [Google Scholar]
- 55.Maggio M, Guralnik JM, Longo DL, Ferrucci L. Interleukin-6 in aging and chronic disease: a magnificent pathway. J Gerontol A Biol Sci Med Sci. 2006;61:575–584. doi: 10.1093/gerona/61.6.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li YP, Chen Y, John J, Moylan J, Jin B, Mann DL, Reid MB. TNF-alpha acts via p38 MAPK to stimulate expression of the ubiquitin ligase atrogin1/MAFbx in skeletal muscle. FASEB J. 2005;19:362–370. doi: 10.1096/fj.04-2364com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Baxter GT, Kuo RC, Jupp OJ, Vandenabeele P, MacEwan DJ. Tumor necrosis factor-alpha mediates both apoptotic cell death and cell proliferation in a human hematopoietic cell line dependent on mitotic activity and receptor subtype expression. J Biol Chem. 1999;274:9539–9547. doi: 10.1074/jbc.274.14.9539. [DOI] [PubMed] [Google Scholar]
- 58.Haddad F, Zaldivar F, Cooper DM. Adams GR (2005) IL-6-induced skeletal muscle atrophy. J Appl Physiol. 1985;98:911–917. doi: 10.1152/japplphysiol.01026.2004. [DOI] [PubMed] [Google Scholar]
- 59.Cuthbertson D, Smith K, Babraj J, Leese G, Waddell T, Atherton P, Wackerhage H, Taylor PM, Rennie MJ. Anabolic signaling deficits underlie amino acid resistance of wasting, aging muscle. FASEB J. 2005;19:422–424. doi: 10.1096/fj.04-2640fje. [DOI] [PubMed] [Google Scholar]
- 60.Wyczalkowska-Tomasik A, Czarkowska-Paczek B, Giebultowicz J, Wroczynski P, Paczek L. Age-dependent increase in serum levels of indoxyl sulphate and p-cresol sulphate is not related to their precursors: tryptophan and tyrosine. Geriatr Gerontol Int. 2017;17:1022–1026. doi: 10.1111/ggi.12811. [DOI] [PubMed] [Google Scholar]
- 61.Enoki Y, Watanabe H, Arake R, Sugimoto R, Imafuku T, Tominaga Y, Ishima Y, Kotani S, Nakajima M, Tanaka M, Matsushita K, Fukagawa M, Otagiri M, Maruyama T. Indoxyl sulfate potentiates skeletal muscle atrophy by inducing the oxidative stress-mediated expression of myostatin and atrogin-1. Sci Rep. 2016;6:32084. doi: 10.1038/srep32084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lustgarten MS, Price LL, Chale A, Fielding RA. Metabolites related to gut bacterial metabolism, peroxisome proliferator-activated receptor-alpha activation, and insulin sensitivity are associated with physical function in functionally-limited older adults. Aging Cell. 2014;13:918–925. doi: 10.1111/acel.12251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen YM, Wei L, Chiu YS, Hsu YJ, Tsai TY, Wang MF, Huang CC. Lactobacillus plantarum TWK10 supplementation improves exercise performance and increases muscle mass in mice. Nutrients. 2016;8:205. doi: 10.3390/nu8040205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bindels LB, Delzenne NM, Cani PD, Walter J. Towards a more comprehensive concept for prebiotics. Nat Rev Gastroenterol Hepatol. 2015;12:303–310. doi: 10.1038/nrgastro.2015.47. [DOI] [PubMed] [Google Scholar]
- 65.Cani PD, Possemiers S, Van de Wiele T, Guiot Y, Everard A, Rottier O, Geurts L, Naslain D, Neyrinck A, Lambert DM, Muccioli GG, Delzenne NM. Changes in gut microbiota control inflammation in obese mice through a mechanism involving GLP-2-driven improvement of gut permeability. Gut. 2009;58:1091–1103. doi: 10.1136/gut.2008.165886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Everard A, Lazarevic V, Derrien M, Girard M, Muccioli GG, Neyrinck AM, Possemiers S, Van Holle A, Francois P, de Vos WM, Delzenne NM, Schrenzel J, Cani PD. Responses of gut microbiota and glucose and lipid metabolism to prebiotics in genetic obese and diet-induced leptin-resistant mice. Diabetes. 2011;60:2775–2786. doi: 10.2337/db11-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bindels LB, Neyrinck AM, Claus SP, Le Roy CI, Grangette C, Pot B, Martinez I, Walter J, Cani PD, Delzenne NM. Synbiotic approach restores intestinal homeostasis and prolongs survival in leukaemic mice with cachexia. ISME J. 2016;10:1456–1470. doi: 10.1038/ismej.2015.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Enck P, Zimmermann K, Rusch K, Schwiertz A, Klosterhalfen S, Frick JS. The effects of ageing on the colonic bacterial microflora in adults. Z Gastroenterol. 2009;47:653–658. doi: 10.1055/s-0028-1109055. [DOI] [PubMed] [Google Scholar]
- 69.Griffiths EA, Duffy LC, Schanbacher FL, Qiao H, Dryja D, Leavens A, Rossman J, Rich G, Dirienzo D, Ogra PL. In vivo effects of bifidobacteria and lactoferrin on gut endotoxin concentration and mucosal immunity in Balb/c mice. Dig Dis Sci. 2004;49:579–589. doi: 10.1023/b:ddas.0000026302.92898.ae. [DOI] [PubMed] [Google Scholar]
- 70.Cani PD, Neyrinck AM, Fava F, Knauf C, Burcelin RG, Tuohy KM, Gibson GR, Delzenne NM. Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia. 2007;50:2374–2383. doi: 10.1007/s00125-007-0791-0. [DOI] [PubMed] [Google Scholar]
- 71.Morales MG, Olguin H, Di Capua G, Brandan E, Simon F, Cabello-Verrugio C. Endotoxin-induced skeletal muscle wasting is prevented by angiotensin-(1–7) through a p38 MAPK-dependent mechanism. Clin Sci (Lond) 2015;129:461–476. doi: 10.1042/CS20140840. [DOI] [PubMed] [Google Scholar]
- 72.Belenguer A, Duncan SH, Calder AG, Holtrop G, Louis P, Lobley GE, Flint HJ. Two routes of metabolic cross-feeding between Bifidobacterium adolescentis and butyrate-producing anaerobes from the human gut. Appl Environ Microbiol. 2006;72:3593–3599. doi: 10.1128/AEM.72.5.3593-3599.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Walsh ME, Bhattacharya A, Sataranatarajan K, Qaisar R, Sloane L, Rahman MM, Kinter M, Van Remmen H. The histone deacetylase inhibitor butyrate improves metabolism and reduces muscle atrophy during aging. Aging Cell. 2015;14:957–970. doi: 10.1111/acel.12387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Eloe-Fadrosh EA, Brady A, Crabtree J, Drabek EF, Ma B, Mahurkar A, Ravel J, Haverkamp M, Fiorino AM, Botelho C, Andreyeva I, Hibberd PL, Fraser CM. Functional dynamics of the gut microbiome in elderly people during probiotic consumption. MBio. 2015 doi: 10.1128/mBio.00231-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vulevic J, Drakoularakou A, Yaqoob P, Tzortzis G, Gibson GR. Modulation of the fecal microflora profile and immune function by a novel trans-galactooligosaccharide mixture (B-GOS) in healthy elderly volunteers. Am J Clin Nutr. 2008;88:1438–1446. doi: 10.3945/ajcn.2008.26242. [DOI] [PubMed] [Google Scholar]
- 76.Trombetti A, Reid KF, Hars M, Herrmann FR, Pasha E, Phillips EM, Fielding RA. Age-associated declines in muscle mass, strength, power, and physical performance: impact on fear of falling and quality of life. Osteoporos Int. 2016;27:463–471. doi: 10.1007/s00198-015-3236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Reid KF, Naumova EN, Carabello RJ, Phillips EM, Fielding RA. Lower extremity muscle mass predicts functional performance in mobility-limited elders. J Nutr Health Aging. 2008;12:493–498. doi: 10.1007/BF02982711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, Simonsick EM, Tylavsky FA, Visser M, Newman AB. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61:1059–1064. doi: 10.1093/gerona/61.10.1059. [DOI] [PubMed] [Google Scholar]
- 79.Grosicki GJ, Standley RA, Murach KA, Raue U, Minchev K, Coen PM, Newman AB, Cummings S, Harris T, Kritchevsky S, Goodpaster BH. Trappe S (2016) Improved single muscle fiber quality in the oldest-old. J Appl Physiol. 1985;121:878–884. doi: 10.1152/japplphysiol.00479.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lustgarten MS, Price LL, Fielding RA. Analytes and metabolites associated with muscle quality in young, healthy adults. Med Sci Sports Exerc. 2015;47:1659–1664. doi: 10.1249/MSS.0000000000000578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Goodpaster BH, Carlson CL, Visser M, Kelley DE, Scherzinger A, Harris TB, Stamm E. Newman AB (2001) Attenuation of skeletal muscle and strength in the elderly: the health ABC study. J Appl Physiol. 1985;90:2157–2165. doi: 10.1152/jappl.2001.90.6.2157. [DOI] [PubMed] [Google Scholar]
- 82.Visser M, Kritchevsky SB, Goodpaster BH, Newman AB, Nevitt M, Stamm E, Harris TB. Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: the health, aging and body composition study. J Am Geriatr Soc. 2002;50:897–904. doi: 10.1046/j.1532-5415.2002.50217.x. [DOI] [PubMed] [Google Scholar]
- 83.Biagi E, Nylund L, Candela M, Ostan R, Bucci L, Pini E, Nikkila J, Monti D, Satokari R, Franceschi C, Brigidi P, De Vos W. Through ageing, and beyond: gut microbiota and inflammatory status in seniors and centenarians. PLoS ONE. 2010;5:e10667. doi: 10.1371/journal.pone.0010667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.van Tongeren S, Slaets J, Harmsen H, Welling G. Fecal microbiota composition and frailty. Appl Environ Microbiol. 2005;71:6438–6442. doi: 10.1128/AEM.71.10.6438-6442.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Collins KH, Paul HA, Hart DA, Reimer RA, Smith IC, Rios JL, Seerattan RA, Herzog W. A high-fat high-sucrose diet rapidly alters muscle integrity, inflammation and gut microbiota in male rats. Sci Rep. 2016;6:37278. doi: 10.1038/srep37278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fang S, Xiong X, Su Y, Huang L, Chen C. 16S rRNA gene-based association study identified microbial taxa associated with pork intramuscular fat content in feces and cecum lumen. BMC Microbiol. 2017;17:162. doi: 10.1186/s12866-017-1055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Liu Y, Tang GY, Tang RB, Peng YF, Li W. Assessment of bone marrow changes in postmenopausal women with varying bone densities: magnetic resonance spectroscopy and diffusion magnetic resonance imaging. Chin Med J (Engl) 2010;123:1524–1527. [PubMed] [Google Scholar]
- 88.Agrawal K, Agarwal Y, Chopra RK, Batra A, Chandra R, Thukral BB. Evaluation of MR spectroscopy and diffusion-weighted MRI in postmenopausal bone strength. Cureus. 2015;7:e327. doi: 10.7759/cureus.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Britton RA, Irwin R, Quach D, Schaefer L, Zhang J, Lee T, Parameswaran N, McCabe LR. Probiotic L. reuteri treatment prevents bone loss in a menopausal ovariectomized mouse model. J Cell Physiol. 2014;229:1822–1830. doi: 10.1002/jcp.24636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Frontera WR, Hughes VA, Fielding RA, Fiatarone MA, Evans WJ. Roubenoff R (2000) Aging of skeletal muscle: a 12-yr longitudinal study. J Appl Physiol. 1985;88:1321–1326. doi: 10.1152/jappl.2000.88.4.1321. [DOI] [PubMed] [Google Scholar]
- 91.Larsson L, Grimby G, Karlsson J. Muscle strength and speed of movement in relation to age and muscle morphology. J Appl Physiol Respir Environ Exerc Physiol. 1979;46:451–456. doi: 10.1152/jappl.1979.46.3.451. [DOI] [PubMed] [Google Scholar]
- 92.Korhonen MT, Cristea A, Alen M, Hakkinen K, Sipila S, Mero A, Viitasalo JT, Larsson L. Suominen H (2006) Aging, muscle fiber type, and contractile function in sprint-trained athletes. J Appl Physiol. 1985;101:906–917. doi: 10.1152/japplphysiol.00299.2006. [DOI] [PubMed] [Google Scholar]
- 93.Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev. 2012;40:4–12. doi: 10.1097/JES.0b013e31823b5f13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yan H, Diao H, Xiao Y, Li W, Yu B, He J, Yu J, Zheng P, Mao X, Luo Y, Zeng B, Wei H, Chen D. Gut microbiota can transfer fiber characteristics and lipid metabolic profiles of skeletal muscle from pigs to germ-free mice. Sci Rep. 2016;6:31786. doi: 10.1038/srep31786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bean JF, Leveille SG, Kiely DK, Bandinelli S, Guralnik JM, Ferrucci L. A comparison of leg power and leg strength within the InCHIANTI study: which influences mobility more? J Gerontol A Biol Sci Med Sci. 2003;58:728–733. doi: 10.1093/gerona/58.8.m728. [DOI] [PubMed] [Google Scholar]
- 96.Peng L, Li ZR, Green RS, Holzman IR, Lin J. Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase in Caco-2 cell monolayers. J Nutr. 2009;139:1619–1625. doi: 10.3945/jn.109.104638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cox MA, Jackson J, Stanton M, Rojas-Triana A, Bober L, Laverty M, Yang X, Zhu F, Liu J, Wang S, Monsma F, Vassileva G, Maguire M, Gustafson E, Bayne M, Chou CC, Lundell D, Jenh CH. Short-chain fatty acids act as antiinflammatory mediators by regulating prostaglandin E(2) and cytokines. World J Gastroenterol. 2009;15:5549–5557. doi: 10.3748/wjg.15.5549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Claesson MJ, Jeffery IB, Conde S, Power SE, O’Connor EM, Cusack S, Harris HMB, Coakley M, Lakshminarayanan B, O’Sullivan O, Fitzgerald GF, Deane J, O’Connor M, Harnedy N, O’Connor K, O’Mahony D, van Sinderen D, Wallace M, Brennan L, Stanton C, Marchesi JR, Fitzgerald AP, Shanahan F, Hill C, Ross RP, O’Toole PW. Gut microbiota composition correlates with diet and health in the elderly. Nature. 2012;9:178–184. doi: 10.1038/nature11319. [DOI] [PubMed] [Google Scholar]
- 99.Jeffery IB, Lynch DB, O’Toole PW. Composition and temporal stability of the gut microbiota in older persons. ISME J. 2016;10:170–182. doi: 10.1038/ismej.2015.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Buigues C, Fernández-Garrido J, Pruimboom L, Hoogland AJ, Navarro-Martínez R, Martínez-Martínez M, Verdejo Y, Mascarós MC, Peris C, Cauli O. Effect of a prebiotic formulation on frailty syndrome: a randomized, double-blind clinical trial. Int J Mol Sci. 2016;17:E392. doi: 10.3390/ijms17060932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Clarke SF, Murphy EF, O’Sullivan O, Lucey AJ, Humphreys M, Hogan A, Hayes P, O’Reilly M, Jeffery IB, Wood-Martin R, Kerins DM, Quigley E, Ross RP, O’Toole PW, Molloy MG, Falvey E, Shanahan F, Cotter PD. Exercise and associated dietary extremes impact on gut microbial diversity. Gut. 2014;63:1913–1920. doi: 10.1136/gutjnl-2013-306541. [DOI] [PubMed] [Google Scholar]
- 102.Estaki M, Pither J, Baumeister P, Little JP, Gill SK, Ghosh S, Ahmadi-Vand Z, Marsden KR, Gibson DL. Cardiorespiratory fitness as a predictor of intestinal microbial diversity and distinct metagenomic functions. Microbiome. 2016;4:42. doi: 10.1186/s40168-016-0189-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Denou E, Marcinko K, Surette MG, Steinberg GR, Schertzer JD. High-intensity exercise training increases the diversity and metabolic capacity of the mouse distal gut microbiota during diet-induced obesity. Am J Physiol Endocrinol Metab. 2016;310:E982–E993. doi: 10.1152/ajpendo.00537.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lira FS, Rosa JC, Pimentel GD, Souza HA, Caperuto EC, Carnevali LC, Seelaender M, Damaso AR, Oyama LM, de Mello MT, Santos RV. Endotoxin levels correlate positively with a sedentary lifestyle and negatively with highly trained subjects. Lipids Health Dis. 2010;9:82. doi: 10.1186/1476-511X-9-82. [DOI] [PMC free article] [PubMed] [Google Scholar]