Abstract
In gliomas, the canonical Wingless/Int (WNT)/β-catenin pathway is increased while peroxisome proliferator-activated receptor gamma (PPAR-γ) is downregulated. The two systems act in an opposite manner. This review focuses on the interplay between WNT/β-catenin signaling and PPAR-γ and their metabolic implications as potential therapeutic target in gliomas. Activation of the WNT/β-catenin pathway stimulates the transcription of genes involved in proliferation, invasion, nucleotide synthesis, tumor growth, and angiogenesis. Activation of PPAR-γ agonists inhibits various signaling pathways such as the JAK/STAT, WNT/β-catenin, and PI3K/Akt pathways, which reduces tumor growth, cell proliferation, cell invasiveness, and angiogenesis. Nonsteroidal anti-inflammatory drugs, curcumin, antipsychotic drugs, adiponectin, and sulforaphane downregulate the WNT/β-catenin pathway through the upregulation of PPAR-γ and thus appear to provide an interesting therapeutic approach for gliomas. Temozolomide (TMZ) is an antiangiogenic agent. The downstream action of this opposite interplay may explain the TMZ-resistance often reported in gliomas.
Keywords: WNT/beta-catenin pathway, PPAR gamma, Glioma, STAT3 pathway, PI3K/Akt pathway, NSAID, Curcumin
Introduction
Glioma is the most frequent primary brain tumor, and accounts for ~ 30% of all central nervous system (CNS) tumors. They diffusely infiltrate into the surrounding normal brain tissue [1]. Glial cells contain multipotent tumor stem cells that have the potential to transform into normal neural progenitor cell variants [2, 3]. Gliomas are named according to the origin of the cell type with which they share histological characteristics. In the 2016 World Health Organization (WHO) classification, gliomas are classified into astrocytoma, oligoastrocytoma, oligodendroglioma, and glioblastoma based on histology, and each is further subdivided based on isocitrate dehydrogenase mutation status [4]. They have traditionally been categorized by the WHO grading system into grades I to IV based on their histological aggressiveness features [4]. Grade I and II gliomas are slow-growing and less aggressive whereas grade III and IV gliomas are malignant tumors characterized by a high proliferation rate (grade III) and angiogenic activity (grade IV). Low- and intermediate-grade gliomas (grades II and III) evolve inexorably to anaplastic transformation with a dismal prognosis, but over a very variable period of time. Malignant gliomas, considered to be the most frequent malignant brain tumors [5–7], account for 80% of these tumors [1] and are the most fatal human cancers [8, 9]. Patients with grade IV glioblastoma present the most aggressive form with a median overall survival of 15 months [10]. Despite considerable improvements in surgical resection and radiotherapy, as well as immune and gene therapy, the prognosis of glioblastoma is still dismal [11]. Thus, it is crucial to probe the underlying molecular mechanisms involved in the development of gliomas.
In numerous tissues, activation of the canonical Wingless/Int (WNT)/β-catenin pathway induces inactivation of peroxisome proliferator-activated receptor gamma (PPAR-γ), while PPAR-γ activation induces inhibition of the canonical WNT/β-catenin pathway [12–17]. In arrhythmogenic right ventricular dysplasia/cardiomyopathy, osteoporosis, bipolar disorder and schizophrenia, and certain neurodegenerative diseases [18] such as Alzheimer’s disease [19, 20], the WNT/β-catenin pathway is downregulated while PPAR-γ is upregulated. Conversely, in cancers [21–23], type 2 diabetes [24], and certain neurodegenerative diseases such as amyotrophic lateral sclerosis [25, 26], age-related macular degeneration [27, 28], multiple sclerosis, Huntington’s disease, and Friedreich’s ataxia, WNT/β-catenin signaling is upregulated while PPAR-γ is downregulated [18].
WNT/β-catenin, a determining factor in the evolution of numerous cancers [29–31], is upregulated in gliomas compared to normal brain, while PPAR-γ is downregulated [32, 33]. Activation of the WNT/β-catenin pathway plays a major role in the evolution of gliomas [34], cell proliferation [35], inhibition of apoptosis [36], and cell invasion [37].
PPAR-γ is expressed at low levels in the CNS and is present in neurons, astrocytes, oligodendrocytes, and microglia [38–41]. In many pathophysiological states, PPAR-γ activation induces inhibition of the WNT/β-catenin pathway [42–44]. The anti-inflammatory properties of PPARγ agonists may partly explain their beneficial therapeutic effects. PPAR-γ agonists diminish activation of the WNT/β-catenin pathway and represent a promising therapeutic target for glioma patients [21]. Several potential treatments for gliomas may operate through this interplay, such as non-steroidal anti-inflammatory drugs (NSAIDs), curcumin (Cur), antipsychotic drugs, adiponectin, sulforaphane (SFN), and basic leucine zipper ATF-like transcription factor 2 (BATF2).
The opposite interplay between the WNT/β-catenin pathway and PPAR-γ and its interactions with potential treatments in gliomas are reviewed here.
The Canonical WNT/β-Catenin Pathway
The WNT pathway has been implicated in numerous processes such as embryogenesis and the maintenance of neuronal homeostasis in adulthood [45–48]. Carcinogenesis involves the dysregulation of this pathway [35–37].
The WNT ligands are lipid-modified glycoproteins [49] secreted by both neurons and immune cells in the CNS [50]. They stimulate intracellular WNT signaling. In the presence of one of the 19 members of the WNT family [51], frizzled (FZD) and low-density lipoprotein-related receptors 5 and 6 (LRP5/6) receptors are activated. Then, the complex binds disheveled (DSH) and AXIN and inhibits glycogen synthase kinase 3 beta (GSK-3β) activity. β-catenin accumulates in the cytosol and then is translocated to the nucleus for binding to T-cell factor/lymphoid enhancer factor (TCF/LEF). This leads to the transcription of WNT-target genes, such as cyclin D1, c-Myc, PDK1 (pyruvate dehydrogenase kinase 1), and MCT-1 (monocarboxylate lactate transporter-1).
However, β-catenin is phosphorylated by GSK-3β in the absence of WNT ligands. β-catenin complexes with the GSK-3β/APC (adenomatous polyposis coli)/AXIN destruction complex and then is degraded by the proteasome.
Dikkopf-1 (DKK1) is an antagonist of WNT signaling [52]; it binds to LRP5/6 co-receptors and inhibits WNT signaling [53]. The β-catenin/TCF complex regulates DKK1 transcription via a negative feedback loop [54].
Secreted FZD-related proteins (SFRPs), a family of five glycoproteins, and WNT inhibitor protein (WIF) inhibit the WNT pathway upstream [53]. WIF acts as a WNT antagonist and tumor suppressor [17]. SFRPs and WIF-1 play major roles in development and tissue homeostasis. Their expression is downregulated in cancers [55].
GSK-3β is a major regulator of the WNT pathway [56]. It is a neuron-specific intracellular serine-threonine kinase which regulates several processes such as inflammation, neuronal polarity, and cell membrane signaling [57–59]; it inhibits the cytosolic stabilization and nuclear migration of β-catenin; and it is an inhibitor of the WNT/β-catenin pathway. Its dysregulation has been reported in several pathological disorders, including tumorigenesis [59]. The phosphatidylinositol 3-kinase/protein kinase B (PI3K/Akt) pathway regulates the expression of GSK-3β [60].
Peroxisome Proliferator-Activated Receptor Gamma
The ligand-activated transcriptional factor PPAR-γ belongs to the nuclear hormone receptor superfamily. It is expressed in different cell types, including adipose tissue, muscle, brain, and immune cells; it activates the expression of many genes and regulates glucose homeostasis, insulin sensitivity, lipid metabolism, immune responses, cell fate, and inflammation [13, 32]; and it is abundantly expressed in adipose tissue and at lower levels in heart, skeletal muscle, and liver [61]. PPAR-γ is expressed at a low level in the CNS in neurons, astrocytes, oligodendrocytes, and microglia [62]; its expression is mainly localized in the microglia and astrocytes; and it plays a major role in the inflammatory response [63]. The PPAR-γ agonists, thiazolidinediones (TZDs), improve insulin sensitivity in peripheral tissues [64] and ameliorate glucose tolerance in type 2 diabetes [65], as well as acting on the promoters of the glucose transporter and glucokinase in pancreatic β-cells and the liver. PPAR-γ also plays an important role in regulating cardiovascular rhythms by controlling circadian variations of blood pressure and heart rate through Bmal1 [66, 67]. PPAR-γ modulates the expression of several genes involved in inflammation, and regulates the activity of inflammation-related transcription factors such as nuclear factor-kappa B (NFκB) [68].
Interplay Between the Canonical WNT/β-Catenin Pathway and PPAR-γ
Several studies have shown a direct interaction between PPAR-γ and β-catenin [43, 69, 70]. The TZD agonists of PPAR-γ (troglitazone, thiazolidinedione, rosiglitazone, or pioglitazone) downregulate β-catenin transcription. This transcription is induced by β-catenin in a PPAR-γ-dependent manner [43, 44, 71]. The β-catenin inhibition by PPAR-γ agonists occurs at the post-transcriptional level. The functional interaction between PPAR-γ and β-catenin involves the binding domain of the TCF/LEF factors of β-catenin. Likewise, this interaction involves a binding domain of β-catenin in PPAR-γ [42]. Many studies have described the antagonism between PPAR-γ signaling and the β-catenin pathway in several tissues [44, 71]. Similarly, PPAR-γ inhibits the WNT/β-catenin pathway [44] and osteoblastogenesis but induces adipogenesis [72].
Inhibition of the WNT/β-catenin pathway increases PPAR-γ transcription. Overexpression of AXIN inhibits WNT signaling in pre-adipocytes and the cells differentiate into adipocytes. PPAR-γ with the canonical WNT/β-catenin pathway regulates the molecular switching between osteoblastogenesis and adipogenesis. PPAR-γ agonists appear to be potential therapeutic candidates during the fibrosis process by inhibiting the WNT/β-catenin pathway [73–75].
Arrhythmogenic right ventricular cardiomyopathy shows activation of PPAR-γ and inhibition of the WNT/β-catenin pathway [69, 76]. In transgenic mice, inhibition of the canonical WNT/β-catenin pathway by plakoglobin or γ-catenin induces the cardiomyopathy phenotype. This causes fat accumulation in cardiomyocytes and ventricular arrhythmias [69]. Plakoglobin (or γ-catenin) has similarities to β-catenin [36]; it competes with β-catenin leading to inhibition of the transcription factors TCF/LEF [77–79]. Thus, the removal of TCF/LEF1 factors induces adipogenesis and stimulates the phenotype of this human cardiomyopathy [69, 76, 80].
The Canonical WNT/β-Catenin Pathway in Gliomas
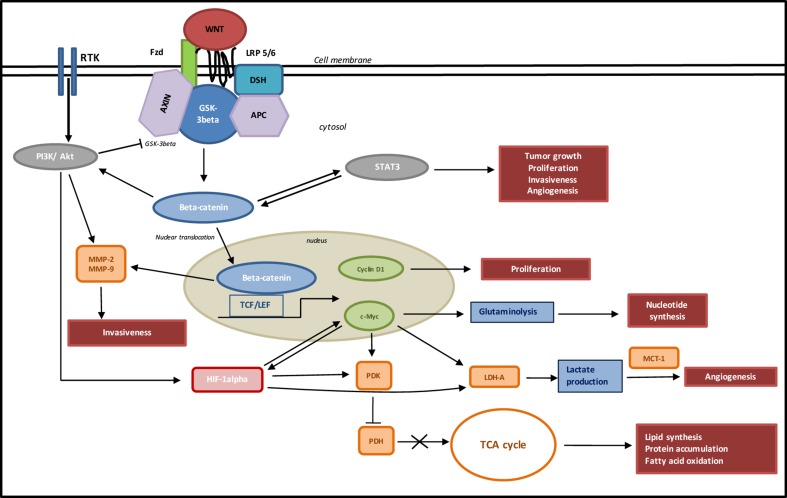
Hyper-activation of the canonical WNT/β-catenin pathway is associated with glioma development and malignant progression [81–83], invasion [84], prognosis [85], inhibition of cell differentiation, and an invasive phenotype [33, 86] (Fig. 1).
Fig. 1.
Role of WNT/beta-catenin signaling in gliomas. When the canonical WNT/β-catenin pathway is upregulated, binding of WNT to FZD leads to activation of DSH, which recruits the destruction complex to the plasma membrane. AXIN binds to the cytoplasmic tail of LRP5/6. WNT also binds LRP5/6. This initiates LRP phosphorylation and DSH-mediated FZD internalization. Activation of DSH leads to the inhibition of GSK-3β, which further reduces the phosphorylation and degradation of β-catenin. The β-catenin degradation complex AXIN/APC/GSK-3β is inactivated with the recruitment of AXIN to the plasma membrane. β-catenin phosphorylation is inhibited. Then, β-catenin accumulates into cytosol and translocates to the nucleus to bind the TCF–LEF co-transcription factors. This induces the canonical WNT-response gene transcription (c-Myc, cyclin D, PDK1, and MCT-1). The STAT3 signaling pathway upregulates the expression and transcriptional activity of β-catenin; in gliomas STAT3 is a tumor aggressiveness factor. In gliomas, overexpression of EGFR (a receptor tyrosine kinase: RTK) stimulates the PI3K/Akt pathway. PI3K/Akt signaling leads to the phosphorylation of GSK3β that leads to the nuclear translocation and stabilization of β-catenin. In the same way, the WNT/β-catenin pathway stimulates EGFR in gliomas. Akt signaling increases MMP-2 and MMP-9 activity, which induces the invasion of malignant cells into healthy brain near the glioma. Akt signaling induces HIF-1α (hypoxia-inducible factor-1 alpha), which stimulates PDK1. Overexpression of WNT/β-catenin also stimulates PDK1. PDK1 and Myc induce lactate dehydrogenase A (LDH-A), and cytosolic pyruvate is shunted into lactate through activation of LDH-A. Overexpression of MCT-1 exports lactate to the extracellular space. Lactate production activates angiogenesis. c-Myc-induced glutaminolysis supports mitochondrial integrity and the production of aspartate, and results in nucleotide biosynthesis. c-Myc and cyclin D stimulate the proliferation of gliomas.
The expression of WNT1 is higher in gliomas than in normal brain, and its overexpression is considered to be an independent prognostic factor for glioma patients [82]. Overexpression of WNT1 and WNT3a in glioma stem cells (GSCs) has been shown in the malignant transformation and progression of high-grade gliomas [87, 88].
WNT3a and the cytosolic/nuclear β-catenin ratio are associated with a worse prognosis in malignant gliomas [81, 89]. WNT2 and WNT5 are also overexpressed in gliomas. The knockdown of WNT2 by siRNA in human U251 glioma cells inhibits proliferation and invasion, and induces apoptosis [89, 90].
Moreover, the expression of β-catenin is positively correlated with the progression of gliomas [82, 83, 85, 90, 91] and is considered to be a prognostic marker for malignancy [82, 83]. The nuclear accumulation of β-catenin is responsible for the malignant progression, and its protein levels are correlated with malignancy and the expression of the Cyclin D1 and c-Myc genes [26, 83, 92].
The WNT/β-catenin pathway induces the transcription of genes implicated in cell proliferation, c-Myc (through glutaminolysis, nucleotide synthesis, and LDH-A activation) and Cyclin D (through G1) [93–96]. Indeed, the transcription of WNT-target genes is preceded by the cytosolic accumulation and nuclear translocation of β-catenin [81, 84]. The WNT target gene c-Myc drives glutaminolysis [94, 97] and induces glutamine uptake into the cell and mitochondria to promote the synthesis of aspartate [96]. Both c-Myc and HIF-1α (hypoxia-inducible factor-1 alpha) stimulate PDK1 and LDH-A [98]. PDK1, a key regulator of glycolysis by phosphorylating the pyruvate dehydrogenase (PDH) complex, inhibits the conversion of pyruvate into acetyl-CoA in mitochondria, and then LDH-A converts the pyruvate into lactate in cancer cells [99]. PDH is considered to be a potential mediator to reduce glioblastoma growth [100]. Activation of PDK1 induces angiogenesis [101, 102] and promotes neovascularization [103]. Angiogenesis is also induced by lactate produced through the activation of LDH-A [104]. Furthermore, high-grade gliomas have high rates of glycolysis and lactate production correlated with a high level of MCT-1 expression [105].
The nuclear translocation of β-catenin regulates the expression of matrix metalloproteinases (MMPs) [33, 106]. Many studies have reported the overexpression of MMPs in cancer cells, including glioma cells [107]. MMP-2 and MMP-9 induce the invasion of malignant cells into healthy brain near the glioma and their expression is positively correlated with tumor progression [108].
In contrast to other cancers, studies have shown no mutation at GSK-3β phosphorylation sites [109, 110], and truncation of APC has not been associated with gliomagenesis [41]. These reports suggest that unbalanced ligand/antagonist expression may deregulate the different pathways involved in tumor progression. Indeed, WNT antagonists appear to be repressed in glioblastomas [33]. Tumor suppressor WIF-1 expression decreases with malignancy in astrocytomas [41]. Primary de novo glioblastomas are associated with hypermethylation of the FZD-related protein (SFRP) promoters whereas secondary glioblastomas present hypermethylation of the promoter of the LRP antagonist DKK1 [109]. As regards glioma progression, hypermethylation of WNT pathway inhibitor genes, like SFRP and DKK1 in malignant astrocytic gliomas [109] and WIF-1 in glioblastomas, has been reported [38, 111].
PPAR-γ in Gliomas
PPARs control gene expression involved in adipogenesis, lipid metabolism, inflammation and metabolic homeostasis [112]; they have been found in developing and adult brain tissues [113]. Activation of the PPAR pathway plays a role in determining the viability of neurons in the developing midbrain [114]. PPAR-γ expression has been described in many cancers including colon, lung, bladder, breast, duodenum, and thyroid [115–121]. In gliomas, the cell-cycle is stopped in G0/G1 phase [122–124], and the proportion of cells entering S-phase is reduced by PPAR-γ agonists [123, 124]. Likewise, decreased c-Myc levels and Cyclin D1 have been detected upstream of the S-phase transition when PPAR-γ agonists are used [124, 125].
In gliomas, PPAR-γ agonists reduce local tissue invasiveness [125–127]. MMP-2 and MMP-9 expression is correlated with tumor progression [108]; they are downregulated after treatment with pioglitazone [125–127]. Pioglitazone, a PPAR-γ agonist, reduces β-catenin expression without changing its cellular localization [125, 128]. Reducing β-catenin expression could contribute to inhibiting the evolution of gliomas from a low to a high grade. High-grade gliomas show over-expression of β-catenin compared to low grade gliomas [129].
PPAR-γ agonists induce apoptosis by reducing cellular viability. This effect is mediated by a BAX (BCL2-associated X protein)-dependent pathway. BAX is upregulated after activation of PPAR-γ [123, 125–128, 130, 131]. Treatment with TZDs leads to apoptosis of glioma cells in a concentration-dependent fashion associated with cell-cycle arrest, while sparing normal primary astrocytes [122, 123, 125–128, 130, 131]. PPAR-γ agonists downregulate SOX2 (SRY-Box 2) [132]. SOX2, a stemness gene, maintains pluripotency in stem cells and inhibits neural differentiation while it is overexpressed in brain tumor-initiating cells. PPAR-γ agonists also increase the expression of N-cadherin, a neural differentiation marker [131]. Activation of the PPAR-γ pathway can regulate the differentiation of neural stem cells [133, 134].
Catalase is involved in the inhibition of reactive oxygen species (ROS) and possesses a PPAR genomic binding site [135]. The anti-cytotoxic effects of PPAR-γ agonists are partially mediated by enhanced redox reactions in glioma cells [135]. Activation of PPAR-γ transcription upregulates catalase activity in normal astrocytes and rat cell models. But this upregulation is not found in the C6 glioma cell line. This is abolished in cells transfected with a dominant-negative PPAR-γ construct [135].
Interactions Between β-Catenin Signaling and PPAR-γ Agonists Through STAT3 Signaling in Gliomas
Signal transducer and activator of transcription 3 (STAT3) stimulation has been implicated in many cancers, such as breast cancers, acute leukemia, colon cancers, and gliomas. The STAT3 pathway is involved in the regulation of proliferation [136], tumor growth, invasiveness, migration [137], and angiogenesis [138]. High levels of STAT3 signaling have been found in brain tumor-initiating cells [139]. In gliomas, STAT3 is a transcriptional factor necessary for mesenchymal transformation and tumor aggressiveness [140].
The biologically active phosphorylated STAT3 is mediated by EGFR and cytokine receptor in gliomas [141]. Phosphorylated STAT3 is regulated through multiple WNT/β-catenin-induced signaling pathways, such as (1) JAK/STAT signaling induced by EGFRs that bind to epidermal growth factors and by the stimulation of cytokine receptors that bind to the ligands interleukin (IL)-6, leukemia inhibitory factor, and EGF [142], (2) EGFR/PI3K/Akt/mTOR (mammalian target of rapamycin) signaling, and (3) WNT/β-catenin target gene transduction c-Myc via HIF-1α stabilization [22]. WNT/β-catenin-induced STAT3 signaling activates transcription of the target genes Bcl-2, Bcl-xl, and ki-67 [143], and via HIF-1α activation, the WNT/β-catenin target genes cyclin D1 and c-Myc in a positive feedback loop [22].
Inhibition of STAT3 arrests glioma cell growth, invasion, migration, differentiation, and cell cycle progression [144–146]. Several studies have shown that PPAR-γ agonists induce growth arrest and apoptosis in glioblastoma cells in culture without affecting primary astrocytes, and inhibit expansion and proliferation of CD133+ GSCs by inhibition of the EGF-induced JAK/STAT pathway [122, 147]. Troglitazone, a TZD PPAR-γ agonist, is considered to be an antagonist of STAT3 signaling [148]. In glioma cells, PPAR-γ agonists inhibit STAT3 signaling through the reduction of phosphotyrosine 705 STAT3 [149]. Inhibition of STAT3 proteins by PPAR-γ agonists underlies the inhibition of upstream tyrosine kinase 2 or its direct effect on STAT3 protein [119], or the activation of negative regulators, such as suppressor of cytokine signaling or SHP-1 proteins in GSCs [150].
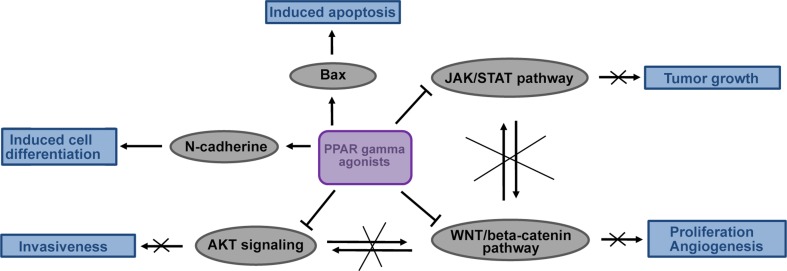
PPAR-γ agonists can act on the WNT/β-catenin pathway by inhibiting STAT3 signaling (Fig. 2). Indeed, inhibition of STAT3 downregulates several critical signaling pathways in malignant glioma cells, including the PI3K/Akt and WNT/β-catenin pathways, as well as the transcription of RTKs [144], and results in downregulation of the expression of the WNT-target genes cyclin D1 and c-Myc, leading to the death of glioma cells [149]. Furthermore, the downregulation of β-catenin signaling in malignant gliomas is associated with a decrease of phosphorylated Akt and STAT3 levels [152], supporting the idea that the β-catenin/TCF4 (transcription factor 4) complex directly binds to the STAT3 gene promoter [151]. The STAT3 pathway is regulated by a plausible opposite interplay between PPAR-γ agonists and the WNT/β-catenin pathway.
Fig. 2.
Potential effects of PPAR gamma agonists in gliomas: inhibition of the JAK/STAT pathway, then reduced tumor growth; inhibition of the WNT/β-catenin pathway, then proliferation and angiogenesis; inhibition of Akt signaling, then reduced invasiveness; activation of N-cadherin, then cell differentiation; activation of BAX, then apoptosis. Activation of PPAR-γ agonists may play major negative roles in regulating the progression and proliferation of gliomas.
Interactions Between β-Catenin Signaling and PPAR-γ Agonists Through EGFR/PI3K/Akt Signaling in Gliomas
The WNT/β-catenin pathway stimulates the activation of RTKs in gliomas [22]. Overexpression of EGFRs occurs in 30%–70% of primary glioblastomas [153]. EGFRs are the most common RTKs aberrantly overexpressed in glioblastomas involving EGFR gene amplification [154] and are major key regulators of the migration, differentiation, apoptosis, proliferation, and survival of glioblastoma cells by binding PI3K/Akt [155–158].
The actions of the PI3K/Akt pathway are multiple in cancer cells with increasing cell proliferation, cell survival and cell migration [159–161]. Moreover, Akt signaling increases MMP-2 and MMP-9 activity in cancer cells and then participates in the invasiveness [60].
The NF-κB proteins, a ubiquitous transcription factor family that mediates immune and inflammatory responses, are also activated by overexpressed EGF, and/or its mutationally-activated EGFR in gliomas, via numerous dysregulated signaling pathways, such as the PI3K/Akt, mTORC2, and IKK (IκB kinase) pathways [162–164]. Allelic loss of PTEN (phosphatase and tensin homolog protein), a tumor suppressor that negatively regulates PI3K activity and inhibits Akt signaling, occurs in many gliomas, and the lack of PTEN expression enables Akt to remain active and activate NF-κB [163, 164]. NF-κB activation subsequently induces the expression of NF-kB target genes promoting proliferation, tumor growth, and cell survival by anti-apoptotic responses [163, 164]. The increase of NF-κB activity in glioblastoma is correlated with the astrocytic tumor grade [164]. Peptidyl-prolyl-isomerase 1 (Pin1) enhances NF-κB signaling while the inhibitor of growth protein 4 (ING4) inhibits NF-κB activity [163, 164]. The protein kinase CK2 (casein kinase 2) positively regulates both the STAT3 and NF-κB signaling pathways [163]. STAT3 signaling is activated by NF-κB-driven IL-6 cytokines [163]. CK2 activates STAT3 signaling through activation of the JAK/STAT, Akt/mTORC, and Akt/EZH2 (a methyltransferase) signaling pathways [163]. CK2 activates NF-κB signaling directly via p65, and by activating the Akt/mTORC and IKK signaling pathways, and the inhibition of IκB [163]. MAPK (mitogen-activated protein kinase) signaling positively regulates both NF-κB and STAT3 signaling [163].
PI3K/Akt pathway signaling induces the activation of HIF-1α and protects against ROS, which activate PDK1 and then inhibit PDH [165]. Inhibition of PDH results in shunting of the TCA cycle and the conversion of pyruvate into lactate by activated LDH-A, leading to angiogenesis and aggressiveness [166].
The EGFR/PI3K/Akt pathway activates Pin1 that induces the isomerization of phosphorylated PKM2 (pyruvate kinase M2) [158], and facilitates the nuclear translocation of acetylated PKM2, which reduces its activity and targets PKM2 towards lysosome-dependent degradation [167]. Acetylated PKM2 participates in cell growth in gliomas by promoting glucose metabolism [168]. Nuclear PKM2 binds nuclear β-catenin that activates the c-Myc-mediated expression of glycolytic enzymes, such as the glucose transporter, LDH-A, PDK1, and PKM2 in a positive feedback loop [169]. Activated PKM2 directly stimulates growth factor receptors to promote cell division and tumor growth [170, 171].
The WNT/β-catenin pathway stimulates EGFR in gliomas [153]. Moreover, in glioma cells the inhibition of β-catenin signaling reduces stimulation of the β-catenin-induced EGFR/PI3K/Akt pathway [152]. Likewise, activation of the PI3K/Akt pathway directly stimulates β-catenin signaling [160] by inhibiting the activity of GSK-3β [60]. Furthermore, inhibition of the PI3K/Akt pathway by the PI3K inhibitor LY294002 decreases β-catenin/TCF activity in glioma cells [172]. Treatment with indomethacin-loaded lipid-core nanocapsules activates GSK-3β expression by inhibiting Akt signaling and then leads to decreased β-catenin levels in C6 glioma cells [173]. A positive interplay between the WNT/β-catenin pathway and PI3K/Akt signaling has been reported in gliomas [174].
Few studies have demonstrated the antagonistic role of PPAR-γ on the EGFR and PI3K/Akt pathways in glioma cells. However, ciglitazone, a TZD PPAR-γ agonist, induces apoptosis by downregulation of Akt activity, inducing mitochondrial membrane potential collapse [175] (Fig. 2). This leads to a plausible opposite interplay between PPAR-γ agonists and the WNT/β-catenin pathway through the EGFR/PI3K/Akt signaling. Moreover, in glioma cells, PPAR-γ activation increases the expression of PTEN, enabling Akt to remain inactive while decreasing the expression of cyclooxygenases-2 (COX-2), leading to lower the COX-2-induced conversion of arachidonic acid into prostaglandin E2 (PGE2), suggesting that PTEN likely acts as a negative regulator to COX-2 expression. [176]. COX-2 protein is overexpressed in all glioma types whereas normal glial cells do not express it. Increasing levels of COX-2 expression and prostaglandin E2 are associated with cell proliferation, invasion, and angiogenesis, and apoptosis inhibition, and the COX-2 expression level is positively correlated with glioma grade [177]. Furthermore, an aberrant positive feedback interaction between the COX-2/PGE2 and WNT pathways stimulates the self-renewal and proliferation of GSCs [178]. WNT signaling underlies GSC identity directly through COX-independent WNT signaling, and indirectly through COX/PGE2-dependent WNT signaling [178].
The Opposite Interplay Between the WNT/β-Catenin Pathway and PPAR-γ: A Potential Therapeutic Target in Gliomas
A Therapeutic Target for Non-steroidal Anti-inflammatory Drugs
NSAIDs reduce nuclear β-catenin levels and induce its degradation [179]. NSAIDs such as sulindac, exisulind, and celecoxib decrease β-catenin levels and then inhibit the transcriptional activity of the β-catenin/TCF/LEF complex [180]. Aspirin inhibits glioma cell proliferation and invasion by decreasing β-catenin/TCF transcription [181], arrests the glioma cell-cycle at G0/G1 and decreases invasion and tumor growth by reducing β-catenin/TCF activity [129, 181]. Moreover, NSAIDs inhibit the invasion of glioma cells in vitro by dephosphorylating Akt signaling and decreasing MMP-2 gene expression [60, 182].
NSAIDs inhibit COX-2 [183]. NSAIDs such as the COX-2 selective inhibitors potentiate the effects of TMZ by acting as PPAR-γ agonists in high-grade gliomas [184]. However, NSAIDs may have COX-independent anti-carcinogenic effects through the involvement of PPAR-γ [185, 186]. Indeed, NSAID effects are mediated by PPAR-γ [187, 188], and prostaglandins or their metabolites may be ligands of PPAR-γ [189].
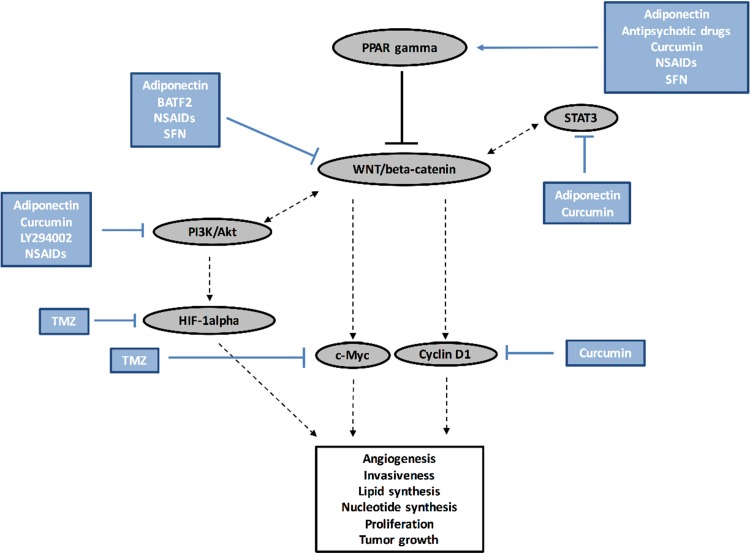
NSAIDs may act as PPAR-γ agonists while inhibiting the WNT/β-catenin pathway, highlighting the crosstalk between these two pathways (Fig. 3).
Fig. 3.
Different actions and interactions of potential treatments for gliomas with the opposite interplay between the WNT/beta-catenin pathway and PPAR gamma.
A Therapeutic Target for Curcumin
Cur, a diferuloylmethane derivative, is a polyphenol derived from a turmeric orange pigment. It is highly lipophilic, poorly hydrophilic, and stable at acidic pH [190]; it has many effects on tumor cells, such as anti-inflammatory, antioxidant, pro- and anti-apoptotic, anti-angiogenic, cytotoxic, and autophagic actions; and is an effective inhibitor of proliferation, migration, invasion, and viability by inducing apoptosis or autophagy of glioma cells [191–194]. Cur acts on numerous signaling pathways in glioma cells by downregulating proliferative and survival signaling pathways such as PI3K/Akt, NFκB, COX-2, STAT-3, c-Myc, Cyclin D1, Bcl-2, Bcl-xL, and Ki, downregulating invasiveness and angiogenesis signaling pathways such as MMPs and MAPK, and upregulating apoptosis or cell-cycle arrest signaling pathways such as ING4, p53, p21, Bax, and caspases [191–194] (Fig. 3).
Cur interacts with several signaling pathways including STAT3 and PPAR-γ [195, 196].
Cur administration decreases activity of the STAT3 pathway and leads to attenuated glioma growth [197]. The mechanism by which Cur activates PPAR-γ is not yet fully understood, but Cur can be considered a ligand of PPAR-γ and may directly bind PPAR-γ receptors [198]. Through the activation of PPAR-γ, Cur can repress both EGFR activation and cyclin D1 expression, a WNT target gene, to inhibit tumor growth [199].
Moreover, Cur treatment increases the mRNA level of GSK-3β in DAOY medulloblastoma cells and suppresses the WNT/β-catenin signaling pathway [200]. Autophagy in glioma cells is induced by Cur by inhibiting the PI3K/Akt/mTOR pathway [201]. By inhibiting the WNT/β-catenin pathway, Cur decreases cyclin D1 expression and then participates in the repression of the development and proliferation of gliomas [200].
Cur, a ligand of PPAR-γ, may act directly on the WNT/β-catenin pathway or indirectly on EGFR signaling and the STAT3 pathway to reduce glioma progression (Fig. 3).
A Therapeutic Target for Antipsychotic Drugs
Several antipsychotic drugs such as olanzapine, chlorpromazine, quetiapine, and risperidone have inhibitory effects on cancers [202]. These drugs downregulate β-catenin signaling and modulate Ca2+ homeostasis in the CNS [203]. Olanzapine, a D2/5-HT2 antagonist, inhibits the WNT/β-catenin pathway in gliomas [204]. In glioma cells, quetiapine acts as a PPAR-γ agonist and directly inhibits the WNT/β-catenin pathway [205] (Fig.3).
A Therapeutic Target for Adiponectin
Adiponectin is a pleiotropic cytokine produced by adipocytes [206]; it regulates several processes, such as glucose metabolism, lipid catabolism, insulin sensitivity, energy metabolism, and mitochondrial function [207]. In several cancers, adiponectin administration downregulates cell proliferation, cell invasion, and angiogenesis [208–210]. Low levels of adiponectin are correlated with the progression and development of malignancies [211]. Adiponectin administration inhibits the WNT/β-catenin pathway by interacting with the WNT co-activators LRP5/6. This inhibition occurs at the level of LRP6 phosphorylation and then inhibits β-catenin accumulation and the activation of target genes in a dose-dependent manner [212]. Adiponectin also decreases activity of the PI3K/Akt pathway and then attenuates the cell proliferation and development of gliomas [213] (Fig. 3).
However, adiponectin activates nuclear receptors of PPAR-γ [214], and also inhibits STAT3 signaling [215] in several diseases including cancers. In gliomas, the inhibition of both the WNT/β-catenin and PI3K/Akt pathways by adiponectin administration and the role of adiponectin as a PPAR-γ ligand in several diseases, including cancers, appear to be an interesting therapeutic target.
Temozolomide in Gliomas
TMZ is a 3-methyl derivative of mitozolomide. Survival benefits of TMZ associated with low toxicity have been reported [216]. TMZ is considered to be the first-line anticancer drug in glioma treatment [217]; it decreases HIF-1α and c-Myc expression during the hypoxic state in gliomas [218, 219] and then impairs VEGF (vascular endothelial growth factor) secretion [220].
However, TMZ-resistance is often found in gliomas with poor responses and has a dismal prognosis [221]; GSCs appear to be insensitive to chemotherapy with TMZ [222]. GSCs show overexpression of miR-125b [223] correlated with an aberrant WNT/β-catenin pathway [224]. TMZ has no effects on the WNT/β-catenin and PI3K/Akt pathways in GSCs, two upstream pathways of HIF-1α and c-Myc [222]. STAT3 signaling is involved in the resistance to TMZ [225]. However, the association of TMZ with LY294002, a PI3K inhibitor, decreases GSC proliferation and invasion [222, 226]. The cytotoxicity of TMZ induced by inhibition of PGE2 affords only a modest survival advantage and fails to prevent glioma progression because of COX-independent WNT activation [178]. Resistance to TMZ may be explained by targeting downstream targets of the WNT/β-catenin pathway, and the combination of inhibitors of WNT and/or PI3K, such as PPAR-γ agonists, with TMZ may enhance its effects (Fig. 3).
A Therapeutic Target for Sulforaphane
SFN (1-isothiocyanate-4-methylsulfinylbutane), a member of the isothiocyanate family, is naturally found in vegetables [227, 228]. It attenuates energy metabolism, apoptosis, and enzyme detoxification in cancers [229].
In gliomas, SFN inhibits miR-21 (micro-ARN 21) expression by downregulating the WNT/β-catenin/TCF4 pathway, reducing the proliferation and migration of glioma cells [230]. Moreover, by inhibiting miR-21 expression, it potentiates the apoptotic effects of TMZ in gliomas [230]. SFN also stimulates BAX signaling and inhibits Bcl-2 and caspase activity to induce apoptosis in glioma cells [230].
In tumor cells, SFN administration also increases the expression of PPAR-γ co-activator-1α (PGC-1α) to decrease HIF-1α expression, and then attenuates tumor development [231]. By inhibiting the WNT/β-catenin pathway in gliomas and acting as an activator of PGC-1α, SFN could be a potential therapeutic approach to overcome TMZ resistance in glioblastoma treatment (Fig. 3).
A Therapeutic Target for BATF2
Basic leucine zipper ATF-like transcription factor 2 (BATF2) is considered to be a new tumor suppressor of growth and migration in glioblastoma cells by suppressing the WNT/β-catenin pathway [222]. BATF2 also inhibits angiogenesis by reducing VEGF expression, which is stimulated by both the WNT/β-catenin and PI3K/Akt pathways [232]. Currently, the interactions of BATF2 with PPAR-γ have not yet been studied but its anti-inflammatory actions [233] and its role as a WNT/β-catenin pathway inhibitor in gliomas [222] could suggest several interactions with PPAR-γ (Fig. 3).
Conclusions
Gliomas inexorably evolve into anaplastic transformation with an extremely poor prognosis in an unpredictable period. In gliomas, the canonical WNT/β-catenin pathway and PPAR-γ act in an opposite manner. The WNT/β-catenin pathway activation via the direct activation of the WNT target genes c-Myc and Cyclin D1 involved in glioma development, stimulates the glycolytic enzymes PDK1, c-Myc, LDH-A, and lactate production, promoting angiogenesis, aggressiveness, and a poor prognosis. The activation of PPAR-γ agonists inhibits various signaling pathways such as the STAT3 and PI3K/Akt pathways, which downregulate the WNT/β-catenin pathway, leading to decreased proliferation, invasiveness, and angiogenesis. Moreover, PPAR-γ agonists also induce the activation of N-cadherin and BAX, leading to cell differentiation and apoptosis, respectively. Activation of PPAR-γ agonists may play a major role in regulating the progression and proliferation of glioma. NSAIDs, Cur, antipsychotic drugs, adiponectin, and SFN downregulate the WNT/β-catenin pathway through the plausible upregulation of PPAR-γ. TMZ, an antiangiogenic treatment, by targeting the downstream crosstalk between the WNT/β-catenin and PPAR-γ pathways may explain the resistance to TMZ. BATF2, a novel tumor suppressor, downregulates WNT/β-catenin and inflammation but its possible effect as a PPAR-γ agonist has not yet been demonstrated and deserves future clinical studies. In gliomas, the crosstalk between WNT/β-catenin signaling and PPAR-γ through the EGFR/PI3K/Akt and STAT3 signaling pathways, provides a better understanding of the mechanisms underlying the development and progression of gliomas, and constitutes a potentially effective therapeutic target.
Compliance with Ethical Standards
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of interest.
References
- 1.Goodenberger ML, Jenkins RB. Genetics of adult glioma. Cancer Genet. 2012;205:613–621. doi: 10.1016/j.cancergen.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 2.Galli R, Binda E, Orfanelli U, Cipelletti B, Gritti A, De Vitis S, et al. Isolation and characterization of tumorigenic, stem-like neural precursors from human glioblastoma. Cancer Res. 2004;64:7011–7021. doi: 10.1158/0008-5472.CAN-04-1364. [DOI] [PubMed] [Google Scholar]
- 3.Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, et al. Identification of human brain tumour initiating cells. Nature. 2004;432:396–401. doi: 10.1038/nature03128. [DOI] [PubMed] [Google Scholar]
- 4.Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol (Berl) 2016;131:803–820. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 5.Louis DN. Molecular pathology of malignant gliomas. Annu Rev Pathol. 2006;1:97–117. doi: 10.1146/annurev.pathol.1.110304.100043. [DOI] [PubMed] [Google Scholar]
- 6.Mamelak AN, Jacoby DB. Targeted delivery of antitumoral therapy to glioma and other malignancies with synthetic chlorotoxin (TM-601) Expert Opin Drug Deliv. 2007;4:175–186. doi: 10.1517/17425247.4.2.175. [DOI] [PubMed] [Google Scholar]
- 7.Ricard D, Idbaih A, Ducray F, Lahutte M, Hoang-Xuan K, Delattre JY, et al. Primary brain tumours in adults. Lancet Lond Engl. 2012;379:1984–1996. doi: 10.1016/S0140-6736(11)61346-9. [DOI] [PubMed] [Google Scholar]
- 8.Dolecek TA, Propp JM, Stroup NE, Kruchko C. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005-2009. Neuro-Oncol. 2012;14(Suppl 5):v1–v49. doi: 10.1093/neuonc/nos218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patil SA, Hosni-Ahmed A, Jones TS, Patil R, Pfeffer LM, Miller DD. Novel approaches to glioma drug design and drug screening. Expert Opin Drug Discov. 2013;8:1135–1151. doi: 10.1517/17460441.2013.807248. [DOI] [PubMed] [Google Scholar]
- 10.Zhu Y, Parada LF. The molecular and genetic basis of neurological tumours. Nat Rev Cancer. 2002;2:616–626. doi: 10.1038/nrc866. [DOI] [PubMed] [Google Scholar]
- 11.Clarke J, Butowski N, Chang S. Recent advances in therapy for glioblastoma. Arch Neurol. 2010;67:279–283. doi: 10.1001/archneurol.2010.5. [DOI] [PubMed] [Google Scholar]
- 12.Angers S, Moon RT. Proximal events in Wnt signal transduction. Nat Rev Mol Cell Biol. 2009;10:468–477. doi: 10.1038/nrm2717. [DOI] [PubMed] [Google Scholar]
- 13.Elbrecht A, Chen Y, Cullinan CA, Hayes N, Leibowitz Md, Moller DE, et al. Molecular cloning, expression and characterization of human peroxisome proliferator activated receptors gamma 1 and gamma 2. Biochem Biophys Res Commun. 1996;224:431–437. doi: 10.1006/bbrc.1996.1044. [DOI] [PubMed] [Google Scholar]
- 14.He TC, Sparks AB, Rago C, Hermeking H, Zawel L, da Costa LT, et al. Identification of c-MYC as a target of the APC pathway. Science. 1998;281:1509–1512. doi: 10.1126/science.281.5382.1509. [DOI] [PubMed] [Google Scholar]
- 15.Shtutman M, Zhurinsky J, Simcha I, Albanese C, D’Amico M, Pestell R, et al. The cyclin D1 gene is a target of the beta-catenin/LEF-1 pathway. Proc Natl Acad Sci U S A. 1999;96:5522–5527. doi: 10.1073/pnas.96.10.5522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siersbæk MS, Loft A, Aagaard MM, Nielsen R, Schmidt SF, Petrovic N, et al. Genome-wide profiling of peroxisome proliferator-activated receptor γ in primary epididymal, inguinal, and brown adipocytes reveals depot-selective binding correlated with gene expression. Mol Cell Biol. 2012;32:3452–3463. doi: 10.1128/MCB.00526-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang K, Zhang J, Han L, Pu P, Kang C. Wnt/beta-catenin signaling in glioma. J Neuroimmune Pharmacol Off J Soc NeuroImmune Pharmacol. 2012;7:740–749. doi: 10.1007/s11481-012-9359-y. [DOI] [PubMed] [Google Scholar]
- 18.Lecarpentier Y, Claes V, Duthoit G, Hébert JL. Circadian rhythms, Wnt/beta-catenin pathway and PPAR alpha/gamma profiles in diseases with primary or secondary cardiac dysfunction. Front Physiol. 2014;5:429. doi: 10.3389/fphys.2014.00429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vallée A, Lecarpentier Y, Guillevin R, Vallée JN. Effects of Cannabidiol interactions with Wnt/β-catenin pathway and PPARγ on oxidative stress and neuroinflammation in Alzheimer’s disease. Acta Biochim Biophys Sin 2017: 1–14. [DOI] [PubMed]
- 20.Vallée A, Lecarpentier Y. Alzheimer disease: crosstalk between the Canonical Wnt/beta-catenin pathway and PPARs alpha and gamma. Front Neurosci. 2016;10:459. doi: 10.3389/fnins.2016.00459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vallée A, Lecarpentier Y, Guillevin R, Vallée JN. Thermodynamics in gliomas: Interactions between the Canonical WNT/beta-catenin pathway and PPAR gamma. Front Physiol. 2017;8:352. doi: 10.3389/fphys.2017.00352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vallée A, Guillevin R, Vallée JN. Vasculogenesis and angiogenesis initiation under normoxic conditions through Wnt/β-catenin pathway in gliomas. Rev Neurosci. 2017 doi: 10.1515/revneuro-2017-0032. [DOI] [PubMed] [Google Scholar]
- 23.Lecarpentier Y, Claes V, Vallée A, Hébert JL. Thermodynamics in cancers: opposing interactions between PPAR gamma and the canonical WNT/beta-catenin pathway. Clin Transl Med. 2017;6:14. doi: 10.1186/s40169-017-0144-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lecarpentier Y, Claes V, Vallée A, Hébert JL. Interactions between PPAR gamma and the Canonical Wnt/beta-catenin pathway in type 2 diabetes and colon cancer. PPAR Res. 2017;2017:1–9. doi: 10.1155/2017/5879090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lecarpentier Y, Vallée A. Opposite interplay between PPAR gamma and Canonical Wnt/beta-catenin pathway in amyotrophic lateral sclerosis. Front Neurol. 2016;7:100. doi: 10.3389/fneur.2016.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Z, Chen H, Chen Y, Cheng X. Significance of beta-catenin and Cyclin D1 express in glioma. Chin J Cell Mol Immunol. 2009;25:1010–1012. [PubMed] [Google Scholar]
- 27.Vallée A, Lecarpentier Y, Guillevin R, Vallée JN. Aerobic glycolysis hypothesis through WNT/beta-catenin pathway in exudative age-related macular degeneration. J Mol Neurosci. 2017;62:368–379. doi: 10.1007/s12031-017-0947-4. [DOI] [PubMed] [Google Scholar]
- 28.Vallée A, Lecarpentier Y, Guillevin R, Vallée JN. PPARγ agonists: Potential treatments for exudative age-related macular degeneration. Life Sci. 2017 doi: 10.1016/j.lfs.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 29.Gruetter R. Glycogen: the forgotten cerebral energy store. J Neurosci Res. 2003;74:179–183. doi: 10.1002/jnr.10785. [DOI] [PubMed] [Google Scholar]
- 30.Thompson CB. Wnt meets Warburg: another piece in the puzzle? EMBO J. 2014;33:1420–1422. doi: 10.15252/embj.201488785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Warburg O. On the origin of cancer cells. Science. 1956;123:309–314. doi: 10.1126/science.123.3191.309. [DOI] [PubMed] [Google Scholar]
- 32.Fajas L, Auboeuf D, Raspé E, Schoonjans K, Lefebvre AM, Saladin R, et al. The organization, promoter analysis, and expression of the human PPARgamma gene. J Biol Chem. 1997;272:18779–18789. doi: 10.1074/jbc.272.30.18779. [DOI] [PubMed] [Google Scholar]
- 33.Nager M, Bhardwaj D, Cantí C, Medina L, Nogués P, Herreros J. β-Catenin signalling in glioblastoma multiforme and glioma-initiating cells. Chemother Res Pract. 2012;2012:192362. doi: 10.1155/2012/192362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jha MK, Suk K. Pyruvate dehydrogenase kinase as a potential therapeutic target for malignant gliomas. Brain Tumor Res Treat. 2013;1:57–63. doi: 10.14791/btrt.2013.1.2.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clevers H. Wnt/β-catenin signaling in development and disease. Cell. 2006;127:469–480. doi: 10.1016/j.cell.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 36.Moon RT, Bowerman B, Boutros M, Perrimon N. The promise and perils of Wnt signaling through beta-catenin. Science. 2002;296:1644–1646. doi: 10.1126/science.1071549. [DOI] [PubMed] [Google Scholar]
- 37.Nusse R. Wnt signaling in disease and in development. Cell Res. 2005;15:28–32. doi: 10.1038/sj.cr.7290260. [DOI] [PubMed] [Google Scholar]
- 38.Lambiv WL, Vassallo I, Delorenzi M, Shay T, Diserens AC, Misra A, et al. The Wnt inhibitory factor 1 (WIF1) is targeted in glioblastoma and has a tumor suppressing function potentially by induction of senescence. Neuro-Oncol. 2011;13:736–747. doi: 10.1093/neuonc/nor036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sarin S, Bernath A. Turcot syndrome (glioma polyposis): a case report. South Med J. 2008;101:1273–1274. doi: 10.1097/SMJ.0b013e3181883853. [DOI] [PubMed] [Google Scholar]
- 40.Wu J, Fang J, Yang Z, Chen F, Liu J, Wang Y. Wnt inhibitory factor-1 regulates glioblastoma cell cycle and proliferation. J Clin Neurosci. 2012;19:1428–1432. doi: 10.1016/j.jocn.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 41.Yang Z, Wang Y, Fang J, Chen F, Liu J, Wu J, et al. Downregulation of WIF-1 by hypermethylation in astrocytomas. Acta Biochim Biophys Sin. 2010;42:418–425. doi: 10.1093/abbs/gmq037. [DOI] [PubMed] [Google Scholar]
- 42.Liu J, Wang H, Zuo Y, Farmer SR. Functional interaction between peroxisome proliferator-activated receptor gamma and beta-catenin. Mol Cell Biol. 2006;26:5827–5837. doi: 10.1128/MCB.00441-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moldes M, Zuo Y, Morrison RF, Silva D, Park BH, Liu J, et al. Peroxisome-proliferator-activated receptor gamma suppresses Wnt/beta-catenin signalling during adipogenesis. Biochem J. 2003;376:607–613. doi: 10.1042/BJ20030426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sharma C, Pradeep A, Wong L, Rana A, Rana B. Peroxisome proliferator-activated receptor gamma activation can regulate beta-catenin levels via a proteasome-mediated and adenomatous polyposis coli-independent pathway. J Biol Chem. 2004;279:35583–35594. doi: 10.1074/jbc.M403143200. [DOI] [PubMed] [Google Scholar]
- 45.Harrison-Uy SJ, Pleasure SJ. Wnt signaling and forebrain development. Cold Spring Harb Perspect Biol. 2012;4:a008094. doi: 10.1101/cshperspect.a008094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ille F, Sommer L. Wnt signaling: multiple functions in neural development. Cell Mol Life Sci CMLS. 2005;62:1100–1108. doi: 10.1007/s00018-005-4552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oliva CA, Vargas JY, Inestrosa NC. Wnts in adult brain: from synaptic plasticity to cognitive deficiencies. Front Cell Neurosci. 2013;7:224. doi: 10.3389/fncel.2013.00224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Salinas PC. Wnt signaling in the vertebrate central nervous system: from axon guidance to synaptic function. Cold Spring Harb Perspect Biol 2012, 4. [DOI] [PMC free article] [PubMed]
- 49.Al-Harthi L. Wnt/β-catenin and its diverse physiological cell signaling pathways in neurodegenerative and neuropsychiatric disorders. J Neuroimmune Pharmacol. 2012;7:725–730. doi: 10.1007/s11481-012-9412-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marchetti B, Pluchino S. Wnt your brain be inflamed? Yes, it Wnt! Trends Mol Med. 2013;19:144–156. doi: 10.1016/j.molmed.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Caricasole A, Ferraro T, Iacovelli L, Barletta E, Caruso A, Melchiorri D, et al. Functional characterization of WNT7A signaling in PC12 cells: interaction with A FZD5 x LRP6 receptor complex and modulation by Dickkopf proteins. J Biol Chem. 2003;278:37024–37031. doi: 10.1074/jbc.M300191200. [DOI] [PubMed] [Google Scholar]
- 52.Semënov MV, Zhang X, He X. DKK1 antagonizes Wnt signaling without promotion of LRP6 internalization and degradation. J Biol Chem. 2008;283:21427–21432. doi: 10.1074/jbc.M800014200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kawano Y, Kypta R. Secreted antagonists of the Wnt signalling pathway. J Cell Sci. 2003;116:2627–2634. doi: 10.1242/jcs.00623. [DOI] [PubMed] [Google Scholar]
- 54.Niida A, Hiroko T, Kasai M, Furukawa Y, Nakamura Y, Suzuki Y, et al. DKK1, a negative regulator of Wnt signaling, is a target of the beta-catenin/TCF pathway. Oncogene. 2004;23:8520–8526. doi: 10.1038/sj.onc.1207892. [DOI] [PubMed] [Google Scholar]
- 55.Bovolenta P, Esteve P, Ruiz JM, Cisneros E, Lopez-Rios J. Beyond Wnt inhibition: new functions of secreted Frizzled-related proteins in development and disease. J Cell Sci. 2008;121:737–746. doi: 10.1242/jcs.026096. [DOI] [PubMed] [Google Scholar]
- 56.Aberle H, Bauer A, Stappert J, Kispert A, Kemler R. β-catenin is a target for the ubiquitin–proteasome pathway. EMBO J. 1997;16:3797–3804. doi: 10.1093/emboj/16.13.3797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ambacher KK, Pitzul KB, Karajgikar M, Hamilton A, Ferguson SS, Cregan SP. The JNK- and AKT/GSK3β-signaling pathways converge to regulate puma induction and neuronal apoptosis induced by trophic factor deprivation. PLoS One. 2012;7:e46885. doi: 10.1371/journal.pone.0046885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hur EM, Zhou FQ. GSK3 signalling in neural development. Nat Rev Neurosci. 2010;11:539–551. doi: 10.1038/nrn2870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wu D, Pan W. GSK3: a multifaceted kinase in Wnt signaling. Trends Biochem Sci. 2010;35:161–168. doi: 10.1016/j.tibs.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Paw I, Carpenter RC, Watabe K, Debinski W, Lo HW. Mechanisms regulating glioma invasion. Cancer Lett. 2015;362:1–7. doi: 10.1016/j.canlet.2015.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bright JJ, Kanakasabai S, Chearwae W, Chakraborty S. PPAR regulation of inflammatory signaling in CNS diseases. PPAR Res. 2008;2008:658520. doi: 10.1155/2008/658520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Braissant O, Foufelle F, Scotto C, Dauça M, Wahli W. Differential expression of peroxisome proliferator-activated receptors (PPARs): tissue distribution of PPAR-alpha, -beta, and -gamma in the adult rat. Endocrinology. 1996;137:354–366. doi: 10.1210/endo.137.1.8536636. [DOI] [PubMed] [Google Scholar]
- 63.Kapadia R, Yi JH, Vemuganti R. Mechanisms of anti-inflammatory and neuroprotective actions of PPAR-gamma agonists. Front Biosci J Virtual Libr. 2008;13:1813–1826. doi: 10.2741/2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rangwala SM, Lazar MA. Peroxisome proliferator-activated receptor gamma in diabetes and metabolism. Trends Pharmacol Sci. 2004;25:331–336. doi: 10.1016/j.tips.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 65.Picard F, Auwerx J. PPAR(gamma) and glucose homeostasis. Annu Rev Nutr. 2002;22:167–197. doi: 10.1146/annurev.nutr.22.010402.102808. [DOI] [PubMed] [Google Scholar]
- 66.Lecarpentier Y, Claes V, Hébert JL. PPARs, cardiovascular metabolism, and function: near- or far-from-equilibrium pathways. PPAR Res 2010, 2010. [DOI] [PMC free article] [PubMed]
- 67.Wang N, Yang G, Jia Z, Zhang H, Aoyagi T, Soodvilai S, et al. Vascular PPARgamma controls circadian variation in blood pressure and heart rate through Bmal1. Cell Metab. 2008;8:482–491. doi: 10.1016/j.cmet.2008.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ricote M, Glass CK. PPARs and molecular mechanisms of transrepression. Biochim Biophys Acta. 2007;1771:926–935. doi: 10.1016/j.bbalip.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Garcia-Gras E, Lombardi R, Giocondo MJ, Willerson JT, Schneider MD, Khoury DS, et al. Suppression of canonical Wnt/beta-catenin signaling by nuclear plakoglobin recapitulates phenotype of arrhythmogenic right ventricular cardiomyopathy. J Clin Invest. 2006;116:2012–2021. doi: 10.1172/JCI27751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jansson EA, Are A, Greicius G, Kuo IC, Kelly D, Arulampalam V, et al. The Wnt/beta-catenin signaling pathway targets PPARgamma activity in colon cancer cells. Proc Natl Acad Sci U S A. 2005;102:1460–1465. doi: 10.1073/pnas.0405928102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gerhold DL, Liu F, Jiang G, Li Z, Xu J, Lu M, et al. Gene expression profile of adipocyte differentiation and its regulation by peroxisome proliferator-activated receptor-gamma agonists. Endocrinology. 2002;143:2106–2118. doi: 10.1210/endo.143.6.8842. [DOI] [PubMed] [Google Scholar]
- 72.Takada I, Kouzmenko AP, Kato S. Wnt and PPARgamma signaling in osteoblastogenesis and adipogenesis. Nat Rev Rheumatol. 2009;5:442–447. doi: 10.1038/nrrheum.2009.137. [DOI] [PubMed] [Google Scholar]
- 73.Vallée A, Lecarpentier Y, Vallée JN. Thermodynamic aspects and reprogramming cellular energy metabolism during the fibrosis process. Int J Mol Sci 2017, 18. 10.3390/ijms18122537. [DOI] [PMC free article] [PubMed]
- 74.Vallée A, Lecarpentier Y, Guillevin R, Vallée JN. Interactions between TGF-β1, canonical WNT/β-catenin pathway and PPAR γ in radiation-induced fibrosis. Oncotarget. 2017;8:90579–90604. doi: 10.18632/oncotarget.21234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lecarpentier Y, Schussler O, Claes V, Vallée A. The myofibroblast: TGFβ-1, a conductor which plays a key role in fibrosis by regulating the balance between PPARγ and the Canonical WNT pathway. Nucl Receptor Res. 2017;4:23. [Google Scholar]
- 76.Djouadi F, Lecarpentier Y, Hébert JL, Charron P, Bastin J, Coirault C. A potential link between peroxisome proliferator-activated receptor signalling and the pathogenesis of arrhythmogenic right ventricular cardiomyopathy. Cardiovasc Res. 2009;84:83–90. doi: 10.1093/cvr/cvp183. [DOI] [PubMed] [Google Scholar]
- 77.Ben-Ze’ev A, Geiger B. Differential molecular interactions of beta-catenin and plakoglobin in adhesion, signaling and cancer. Curr Opin Cell Biol 1998, 10: 629–639. [DOI] [PubMed]
- 78.Maeda O, Usami N, Kondo M, Takahashi M, Goto H, Shimokata K, et al. Plakoglobin (gamma-catenin) has TCF/LEF family-dependent transcriptional activity in beta-catenin-deficient cell line. Oncogene. 2004;23:964–972. doi: 10.1038/sj.onc.1207254. [DOI] [PubMed] [Google Scholar]
- 79.Zhurinsky J, Shtutman M. Ben-Ze’ev A. Differential mechanisms of LEF/TCF family-dependent transcriptional activation by beta-catenin and plakoglobin. Mol Cell Biol. 2000;20:4238–4252. doi: 10.1128/mcb.20.12.4238-4252.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Corrado D, Basso C, Thiene G, McKenna WJ, Davies MJ, Fontaliran F, et al. Spectrum of clinicopathologic manifestations of arrhythmogenic right ventricular cardiomyopathy/dysplasia: a multicenter study. J Am Coll Cardiol. 1997;30:1512–1520. doi: 10.1016/s0735-1097(97)00332-x. [DOI] [PubMed] [Google Scholar]
- 81.Denysenko T, Annovazzi L, Cassoni P, Melcarne A, Mellai M, Schiffer D. WNT/β-catenin signaling pathway and downstream modulators in low- and high-grade glioma. Cancer Genomics Proteomics. 2016;13:31–45. [PubMed] [Google Scholar]
- 82.Liu C, Tu Y, Sun X, Jiang J, Jin X, Bo X, et al. Wnt/beta-Catenin pathway in human glioma: expression pattern and clinical/prognostic correlations. Clin Exp Med. 2011;11:105–112. doi: 10.1007/s10238-010-0110-9. [DOI] [PubMed] [Google Scholar]
- 83.Sareddy GR, Panigrahi M, Challa S, Mahadevan A, Babu PP. Activation of Wnt/beta-catenin/Tcf signaling pathway in human astrocytomas. Neurochem Int 2009, 55: 307–317. [DOI] [PubMed]
- 84.Kahlert UD, Maciaczyk D, Doostkam S, Orr BA, Simons B, Bogiel T, et al. Activation of canonical WNT/β-catenin signaling enhances in vitro motility of glioblastoma cells by activation of ZEB1 and other activators of epithelial-to-mesenchymal transition. Cancer Lett. 2012;325:42–53. doi: 10.1016/j.canlet.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 85.Rossi M, Magnoni L, Miracco C, Mori E, Tosi P, Pirtoli L, et al. β-catenin and Gli1 are prognostic markers in glioblastoma. Cancer Biol Ther. 2011;11:753–761. doi: 10.4161/cbt.11.8.14894. [DOI] [PubMed] [Google Scholar]
- 86.Zheng H, Ying H, Wiedemeyer R, Yan H, Quayle SN, Ivanova EV, et al. PLAGL2 regulates Wnt signaling to impede differentiation in neural stem cells and gliomas. Cancer Cell. 2010;17:497–509. doi: 10.1016/j.ccr.2010.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Riganti C, Salaroglio IC, Caldera V, Campia I, Kopecka J, Mellai M, et al. Temozolomide downregulates P-glycoprotein expression in glioblastoma stem cells by interfering with the Wnt3a/glycogen synthase-3 kinase/β-catenin pathway. Neuro-Oncol. 2013;15:1502–1517. doi: 10.1093/neuonc/not104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhang N, Wei P, Gong A, Chiu WT, Lee HT, Colman H, et al. FoxM1 promotes β-catenin nuclear localization and controls Wnt target-gene expression and glioma tumorigenesis. Cancer Cell. 2011;20:427–442. doi: 10.1016/j.ccr.2011.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kaur N, Chettiar S, Rathod S, Rath P, Muzumdar D, Shaikh ML, et al. Wnt3a mediated activation of Wnt/β-catenin signaling promotes tumor progression in glioblastoma. Mol Cell Neurosci. 2013;54:44–57. doi: 10.1016/j.mcn.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 90.Pu P, Zhang Z, Kang C, Jiang R, Jia Z, Wang G, et al. Downregulation of Wnt2 and beta-catenin by siRNA suppresses malignant glioma cell growth. Cancer Gene Ther. 2009;16:351–361. doi: 10.1038/cgt.2008.78. [DOI] [PubMed] [Google Scholar]
- 91.Yu JM, Jun ES, Jung JS, Suh SY, Han JY, Kim JY, et al. Role of Wnt5a in the proliferation of human glioblastoma cells. Cancer Lett. 2007;257:172–181. doi: 10.1016/j.canlet.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 92.Utsuki S, Sato Y, Oka H, Tsuchiya B, Suzuki S, Fujii K. Relationship between the expression of E-, N-cadherins and beta-catenin and tumor grade in astrocytomas. J Neurooncol. 2002;57:187–192. doi: 10.1023/a:1015720220602. [DOI] [PubMed] [Google Scholar]
- 93.Chafey P, Finzi L, Boisgard R, Caüzac M, Clary G, Broussard C, et al. Proteomic analysis of beta-catenin activation in mouse liver by DIGE analysis identifies glucose metabolism as a new target of the Wnt pathway. Proteomics. 2009;9:3889–3900. doi: 10.1002/pmic.200800609. [DOI] [PubMed] [Google Scholar]
- 94.Dang CV. Rethinking the Warburg effect with Myc micromanaging glutamine metabolism. Cancer Res. 2010;70:859–862. doi: 10.1158/0008-5472.CAN-09-3556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Niehrs C, Acebron SP. Mitotic and mitogenic Wnt signalling. EMBO J. 2012;31:2705–2713. doi: 10.1038/emboj.2012.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wise DR, DeBerardinis RJ, Mancuso A, Sayed N, Zhang XY, Pfeiffer HK, et al. Myc regulates a transcriptional program that stimulates mitochondrial glutaminolysis and leads to glutamine addiction. Proc Natl Acad Sci U S A. 2008;105:18782–18787. doi: 10.1073/pnas.0810199105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Osthus RC, Shim H, Kim S, Li Q, Reddy R, Mukherjee M, et al. Deregulation of glucose transporter 1 and glycolytic gene expression by c-Myc. J Biol Chem. 2000;275:21797–21800. doi: 10.1074/jbc.C000023200. [DOI] [PubMed] [Google Scholar]
- 98.Kim J, Gao P, Liu YC, Semenza GL, Dang CV. Hypoxia-inducible factor 1 and dysregulated c-Myc cooperatively induce vascular endothelial growth factor and metabolic switches hexokinase 2 and pyruvate dehydrogenase kinase 1. Mol Cell Biol. 2007;27:7381–7393. doi: 10.1128/MCB.00440-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Roche TE, Baker JC, Yan X, Hiromasa Y, Gong X, Peng T, et al. Distinct regulatory properties of pyruvate dehydrogenase kinase and phosphatase isoforms. Prog Nucleic Acid Res Mol Biol. 2001;70:33–75. doi: 10.1016/s0079-6603(01)70013-x. [DOI] [PubMed] [Google Scholar]
- 100.Adeva M, González-Lucán M, Seco M, Donapetry C. Enzymes involved in l-lactate metabolism in humans. Mitochondrion. 2013;13:615–629. doi: 10.1016/j.mito.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 101.McFate T, Mohyeldin A, Lu H, Thakar J, Henriques J, Halim ND, et al. Pyruvate dehydrogenase complex activity controls metabolic and malignant phenotype in cancer cells. J Biol Chem. 2008;283:22700–22708. doi: 10.1074/jbc.M801765200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sutendra G, Dromparis P, Kinnaird A, Stenson TH, Haromy A, Parker JMR, et al. Mitochondrial activation by inhibition of PDKII suppresses HIF1a signaling and angiogenesis in cancer. Oncogene. 2013;32:1638–1650. doi: 10.1038/onc.2012.198. [DOI] [PubMed] [Google Scholar]
- 103.Pate KT, Stringari C, Sprowl-Tanio S, Wang K, TeSlaa T, Hoverter NP, et al. Wnt signaling directs a metabolic program of glycolysis and angiogenesis in colon cancer. EMBO J. 2014;33:1454–1473. doi: 10.15252/embj.201488598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lu H, Forbes RA, Verma A. Hypoxia-inducible factor 1 activation by aerobic glycolysis implicates the Warburg effect in carcinogenesis. J Biol Chem. 2002;277:23111–23115. doi: 10.1074/jbc.M202487200. [DOI] [PubMed] [Google Scholar]
- 105.Froberg MK, Gerhart DZ, Enerson BE, Manivel C, Guzman-Paz M, Seacotte N, et al. Expression of monocarboxylate transporter MCT1 in normal and neoplastic human CNS tissues. Neuroreport. 2001;12:761–765. doi: 10.1097/00001756-200103260-00030. [DOI] [PubMed] [Google Scholar]
- 106.Liu Y, Yan W, Zhang W, Chen L, You G, Bao Z, et al. MiR-218 reverses high invasiveness of glioblastoma cells by targeting the oncogenic transcription factor LEF1. Oncol Rep. 2012;28:1013–1021. doi: 10.3892/or.2012.1902. [DOI] [PubMed] [Google Scholar]
- 107.Tonn JC, Goldbrunner R. Mechanisms of glioma cell invasion. Acta Neurochir Suppl. 2003;88:163–167. doi: 10.1007/978-3-7091-6090-9_22. [DOI] [PubMed] [Google Scholar]
- 108.Rao JS, Steck PA, Mohanam S, Stetler-Stevenson WG, Liotta LA, Sawaya R. Elevated levels of M(r) 92,000 type IV collagenase in human brain tumors. Cancer Res. 1993;53:2208–2211. [PubMed] [Google Scholar]
- 109.Götze S, Wolter M, Reifenberger G, Müller O, Sievers S. Frequent promoter hypermethylation of Wnt pathway inhibitor genes in malignant astrocytic gliomas. Int J Cancer. 2010;126:2584–2593. doi: 10.1002/ijc.24981. [DOI] [PubMed] [Google Scholar]
- 110.Polakis P. The oncogenic activation of beta-catenin. Curr Opin Genet Dev. 1999;9:15–21. doi: 10.1016/s0959-437x(99)80003-3. [DOI] [PubMed] [Google Scholar]
- 111.Kim SA, Kwak J, Nam HY, Chun SM, Lee BW, Lee HJ, et al. Promoter methylation of WNT inhibitory factor-1 and expression pattern of WNT/β-catenin pathway in human astrocytoma: pathologic and prognostic correlations. Mod Pathol Off J U S Can Acad Pathol Inc 2013, 26: 626–639. [DOI] [PubMed]
- 112.Barish GD, Narkar VA, Evans RM. PPAR delta: a dagger in the heart of the metabolic syndrome. J Clin Invest. 2006;116:590–597. doi: 10.1172/JCI27955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Escher P, Braissant O, Basu-Modak S, Michalik L, Wahli W, Desvergne B. Rat PPARs: quantitative analysis in adult rat tissues and regulation in fasting and refeeding. Endocrinology. 2001;142:4195–4202. doi: 10.1210/endo.142.10.8458. [DOI] [PubMed] [Google Scholar]
- 114.Park KS, Lee RD, Kang SK, Han SY, Park KL, Yang KH, et al. Neuronal differentiation of embryonic midbrain cells by upregulation of peroxisome proliferator-activated receptor-gamma via the JNK-dependent pathway. Exp Cell Res. 2004;297:424–433. doi: 10.1016/j.yexcr.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 115.Kroll TG, Sarraf P, Pecciarini L, Chen CJ, Mueller E, Spiegelman BM, et al. PAX8-PPARgamma1 fusion oncogene in human thyroid carcinoma [corrected] Science. 2000;289:1357–1360. doi: 10.1126/science.289.5483.1357. [DOI] [PubMed] [Google Scholar]
- 116.Mueller E, Sarraf P, Tontonoz P, Evans RM, Martin KJ, Zhang M, et al. Terminal differentiation of human breast cancer through PPAR gamma. Mol Cell. 1998;1:465–470. doi: 10.1016/s1097-2765(00)80047-7. [DOI] [PubMed] [Google Scholar]
- 117.Mueller E, Smith M, Sarraf P, Kroll T, Aiyer A, Kaufman DS, et al. Effects of ligand activation of peroxisome proliferator-activated receptor gamma in human prostate cancer. Proc Natl Acad Sci U S A. 2000;97:10990–10995. doi: 10.1073/pnas.180329197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sarraf P, Mueller E, Smith WM, Wright HM, Kum JB, Aaltonen LA, et al. Loss-of-function mutations in PPAR gamma associated with human colon cancer. Mol Cell. 1999;3:799–804. doi: 10.1016/s1097-2765(01)80012-5. [DOI] [PubMed] [Google Scholar]
- 119.Simula MP, Cannizzaro R, Canzonieri V, Pavan A, Maiero S, Toffoli G, et al. PPAR signaling pathway and cancer-related proteins are involved in celiac disease-associated tissue damage. Mol Med Camb Mass. 2010;16:199–209. doi: 10.2119/molmed.2009.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tseng CH, Tseng FH. Peroxisome proliferator-activated receptor agonists and bladder cancer: lessons from animal studies. J Environ Sci Health Part C Environ Carcinog Ecotoxicol Rev. 2012;30:368–402. doi: 10.1080/10590501.2012.735519. [DOI] [PubMed] [Google Scholar]
- 121.Tsubouchi Y, Sano H, Kawahito Y, Mukai S, Yamada R, Kohno M, et al. Inhibition of human lung cancer cell growth by the peroxisome proliferator-activated receptor-gamma agonists through induction of apoptosis. Biochem Biophys Res Commun. 2000;270:400–405. doi: 10.1006/bbrc.2000.2436. [DOI] [PubMed] [Google Scholar]
- 122.Chearwae W, Bright JJ. PPARgamma agonists inhibit growth and expansion of CD133+ brain tumour stem cells. Br J Cancer. 2008;99:2044–2053. doi: 10.1038/sj.bjc.6604786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Liu DC, Zang CB, Liu HY, Possinger K, Fan SG, Elstner E. A novel PPAR alpha/gamma dual agonist inhibits cell growth and induces apoptosis in human glioblastoma T98G cells. Acta Pharmacol Sin. 2004;25:1312–1319. [PubMed] [Google Scholar]
- 124.Zang C, Wächter M, Liu H, Posch MG, Fenner MH, Stadelmann C, et al. Ligands for PPARgamma and RAR cause induction of growth inhibition and apoptosis in human glioblastomas. J Neurooncol. 2003;65:107–118. doi: 10.1023/b:neon.0000003728.80052.a8. [DOI] [PubMed] [Google Scholar]
- 125.Wan Z, Shi W, Shao B, Shi J, Shen A, Ma Y, et al. Peroxisome proliferator-activated receptor γ agonist pioglitazone inhibits β-catenin-mediated glioma cell growth and invasion. Mol Cell Biochem. 2011;349:1–10. doi: 10.1007/s11010-010-0637-9. [DOI] [PubMed] [Google Scholar]
- 126.Grommes C, Landreth GE, Sastre M, Beck M, Feinstein DL, Jacobs AH, et al. Inhibition of in vivo glioma growth and invasion by peroxisome proliferator-activated receptor gamma agonist treatment. Mol Pharmacol. 2006;70:1524–1533. doi: 10.1124/mol.106.022194. [DOI] [PubMed] [Google Scholar]
- 127.Papi A, Tatenhorst L, Terwel D, Hermes M, Kummer MP, Orlandi M, et al. PPARgamma and RXRgamma ligands act synergistically as potent antineoplastic agents in vitro and in vivo glioma models. J Neurochem. 2009;109:1779–1790. doi: 10.1111/j.1471-4159.2009.06111.x. [DOI] [PubMed] [Google Scholar]
- 128.Cilibrasi C, Butta V, Riva G, Bentivegna A. Pioglitazone effect on glioma stem cell lines: really a promising drug therapy for glioblastoma? PPAR Res. 2016;2016:7175067. doi: 10.1155/2016/7175067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Liu X, Wang L, Zhao S, Ji X, Luo Y, Ling F. β-Catenin overexpression in malignant glioma and its role in proliferation and apoptosis in glioblastma cells. Med Oncol Northwood Lond Engl. 2011;28:608–614. doi: 10.1007/s12032-010-9476-5. [DOI] [PubMed] [Google Scholar]
- 130.Spagnolo A, Grant EN, Glick R, Lichtor T, Feinstein DL. Differential effects of PPARgamma agonists on the metabolic properties of gliomas and astrocytes. Neurosci Lett. 2007;417:72–77. doi: 10.1016/j.neulet.2007.02.036. [DOI] [PubMed] [Google Scholar]
- 131.Zander T, Kraus JA, Grommes C, Schlegel U, Feinstein D, Klockgether T, et al. Induction of apoptosis in human and rat glioma by agonists of the nuclear receptor PPARgamma. J Neurochem. 2002;81:1052–1060. doi: 10.1046/j.1471-4159.2002.00899.x. [DOI] [PubMed] [Google Scholar]
- 132.Schmitz M, Temme A, Senner V, Ebner R, Schwind S, Stevanovic S, et al. Identification of SOX2 as a novel glioma-associated antigen and potential target for T cell-based immunotherapy. Br J Cancer. 2007;96:1293–1301. doi: 10.1038/sj.bjc.6603696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kanakasabai S, Pestereva E, Chearwae W, Gupta SK, Ansari S, Bright JJ. PPARγ agonists promote oligodendrocyte differentiation of neural stem cells by modulating stemness and differentiation genes. PLoS One. 2012;7:e50500. doi: 10.1371/journal.pone.0050500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Pestereva E, Kanakasabai S, Bright JJ. PPARγ agonists regulate the expression of stemness and differentiation genes in brain tumour stem cells. Br J Cancer. 2012;106:1702–1712. doi: 10.1038/bjc.2012.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Khoo NKH, Hebbar S, Zhao W, Moore SA, Domann FE, Robbins ME. Differential activation of catalase expression and activity by PPAR agonists: implications for astrocyte protection in anti-glioma therapy. Redox Biol. 2013;1:70–79. doi: 10.1016/j.redox.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Leve F, Peres-Moreira RJ, Binato R, Abdelhay E, Morgado-Díaz JA. LPA induces colon cancer cell proliferation through a cooperation between the ROCK and STAT-3 pathways. PLoS One. 2015;10:e0139094. doi: 10.1371/journal.pone.0139094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Tsujita Y, Horiguchi A, Tasaki S, Isono M, Asano T, Ito K, et al. STAT3 inhibition by WP1066 suppresses the growth and invasiveness of bladder cancer cells. Oncol Rep. 2017;38:2197–2204. doi: 10.3892/or.2017.5902. [DOI] [PubMed] [Google Scholar]
- 138.Klein JD, Sano D, Sen M, Myers JN, Grandis JR, Kim S. STAT3 oligonucleotide inhibits tumor angiogenesis in preclinical models of squamous cell carcinoma. PLoS One. 2014;9:e81819. doi: 10.1371/journal.pone.0081819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Villalva C, Martin-Lannerée S, Cortes U, Dkhissi F, Wager M, Le Corf A, et al. STAT3 is essential for the maintenance of neurosphere-initiating tumor cells in patients with glioblastomas: a potential for targeted therapy? Int J Cancer. 2011;128:826–838. doi: 10.1002/ijc.25416. [DOI] [PubMed] [Google Scholar]
- 140.Carro MS, Lim WK, Alvarez MJ, Bollo RJ, Zhao X, Snyder EY, et al. The transcriptional network for mesenchymal transformation of brain tumours. Nature. 2010;463:318–325. doi: 10.1038/nature08712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Kim JE, Patel M, Ruzevick J, Jackson CM, Lim M. STAT3 activation in glioblastoma: Biochemical and therapeutic implications. Cancers. 2014;6:376–395. doi: 10.3390/cancers6010376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Harrison DA. The Jak/STAT pathway. Cold Spring Harb Perspect Biol 2012, 4. 10.1101/cshperspect.a011205.
- 143.Xiong A, Yang Z, Shen Y, Zhou J, Shen Q. Transcription factor STAT3 as a novel molecular target for cancer prevention. Cancers. 2014;6:926–957. doi: 10.3390/cancers6020926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kang SH, Yu MO, Park KJ, Chi SG, Park DH, Chung YG. Activated STAT3 regulates hypoxia-induced angiogenesis and cell migration in human glioblastoma. Neurosurgery 2010, 67: 1386–1395, discussion 1395. [DOI] [PubMed]
- 145.Li GH, Wei H, Lv SQ, Ji H, Wang DL. Knockdown of STAT3 expression by RNAi suppresses growth and induces apoptosis and differentiation in glioblastoma stem cells. Int J Oncol. 2010;37:103–110. [PubMed] [Google Scholar]
- 146.Sherry MM, Reeves A, Wu JK, Cochran BH. STAT3 is required for proliferation and maintenance of multipotency in glioblastoma stem cells. Stem Cells Dayt Ohio. 2009;27:2383–2392. doi: 10.1002/stem.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Mo C, Chearwae W, Bright JJ. PPARgamma regulates LIF-induced growth and self-renewal of mouse ES cells through Tyk2-Stat3 pathway. Cell Signal. 2010;22:495–500. doi: 10.1016/j.cellsig.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 148.Vitale G, Zappavigna S, Marra M, Dicitore A, Meschini S, Condello M, et al. The PPAR-γ agonist troglitazone antagonizes survival pathways induced by STAT-3 in recombinant interferon-β treated pancreatic cancer cells. Biotechnol Adv. 2012;30:169–184. doi: 10.1016/j.biotechadv.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 149.Stechishin OD, Luchman HA, Ruan Y, Blough MD, Nguyen SA, Kelly JJ, et al. On-target JAK2/STAT3 inhibition slows disease progression in orthotopic xenografts of human glioblastoma brain tumor stem cells. Neuro-Oncol. 2013;15:198–207. doi: 10.1093/neuonc/nos302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Park EJ, Park SY, Joe E, Jou I. 15d-PGJ2 and rosiglitazone suppress Janus kinase-STAT inflammatory signaling through induction of suppressor of cytokine signaling 1 (SOCS1) and SOCS3 in glia. J Biol Chem. 2003;278:14747–14752. doi: 10.1074/jbc.M210819200. [DOI] [PubMed] [Google Scholar]
- 151.Yan S, Zhou C, Zhang W, Zhang G, Zhao X, Yang S, et al. beta-Catenin/TCF pathway upregulates STAT3 expression in human esophageal squamous cell carcinoma. Cancer Lett. 2008;271:85–97. doi: 10.1016/j.canlet.2008.05.035. [DOI] [PubMed] [Google Scholar]
- 152.Yue X, Lan F, Yang W, Yang Y, Han L, Zhang A, et al. Interruption of β-catenin suppresses the EGFR pathway by blocking multiple oncogenic targets in human glioma cells. Brain Res. 2010;1366:27–37. doi: 10.1016/j.brainres.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 153.Popescu AM, Purcaru SO, Alexandru O, Dricu A. New perspectives in glioblastoma antiangiogenic therapy. Contemp Oncol Poznan Pol. 2016;20:109–118. doi: 10.5114/wo.2015.56122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Nakada M, Kita D, Watanabe T, Hayashi Y, Teng L, Pyko IV, et al. Aberrant signaling pathways in glioma. Cancers. 2011;3:3242–3278. doi: 10.3390/cancers3033242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Chakravarti A, Dicker A, Mehta M. The contribution of epidermal growth factor receptor (EGFR) signaling pathway to radioresistance in human gliomas: a review of preclinical and correlative clinical data. Int J Radiat Oncol. 2004;58:927–931. doi: 10.1016/j.ijrobp.2003.09.092. [DOI] [PubMed] [Google Scholar]
- 156.Mellinghoff IK, Wang MY, Vivanco I, Haas-Kogan DA, Zhu S, Dia EQ, et al. Molecular determinants of the response of glioblastomas to EGFR kinase inhibitors. N Engl J Med. 2005;353:2012–2024. doi: 10.1056/NEJMoa051918. [DOI] [PubMed] [Google Scholar]
- 157.Seshacharyulu P, Ponnusamy MP, Haridas D, Jain M, Ganti AK, Batra SK. Targeting the EGFR signaling pathway in cancer therapy. Expert Opin Ther Targets. 2012;16:15–31. doi: 10.1517/14728222.2011.648617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Vogt PK, Hart JR. PI3K and STAT3: a new alliance. Cancer Discov. 2011;1:481–486. doi: 10.1158/2159-8290.CD-11-0218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Fruman DA, Rommel C. PI3K and cancer: lessons, challenges and opportunities. Nat Rev Drug Discov. 2014;13:140–156. doi: 10.1038/nrd4204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sami A, Karsy M. Targeting the PI3K/AKT/mTOR signaling pathway in glioblastoma: novel therapeutic agents and advances in understanding. Tumour Biol J Int Soc Oncodevelopmental Biol Med. 2013;34:1991–2002. doi: 10.1007/s13277-013-0800-5. [DOI] [PubMed] [Google Scholar]
- 161.Wang L, Chen L, Wang Q, Wang L, Wang H, Shen Y, et al. Circulating endothelial progenitor cells are involved in VEGFR-2-related endothelial differentiation in glioma. Oncol Rep. 2014;32:2007–2014. doi: 10.3892/or.2014.3467. [DOI] [PubMed] [Google Scholar]
- 162.Cahill KE, Morshed RA, Yamini B. Nuclear factor-κB in glioblastoma: insights into regulators and targeted therapy. Neuro-Oncol. 2016;18:329–339. doi: 10.1093/neuonc/nov265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Gray GK, McFarland BC, Nozell SE, Benveniste EN. NF-κB and STAT3 in glioblastoma: therapeutic targets coming of age. Expert Rev Neurother. 2014;14:1293–1306. doi: 10.1586/14737175.2014.964211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Atkinson GP, Nozell SE, Benveniste ETN. NF-kappaB and STAT3 signaling in glioma: targets for future therapies. Expert Rev Neurother. 2010;10:575–586. doi: 10.1586/ern.10.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Lum JJ, Bui T, Gruber M, Gordan JD, DeBerardinis RJ, Covello KL, et al. The transcription factor HIF-1alpha plays a critical role in the growth factor-dependent regulation of both aerobic and anaerobic glycolysis. Genes Dev. 2007;21:1037–1049. doi: 10.1101/gad.1529107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Suda T, Takubo K, Semenza GL. Metabolic regulation of hematopoietic stem cells in the hypoxic niche. Cell Stem Cell. 2011;9:298–310. doi: 10.1016/j.stem.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 167.Lv L, Li D, Zhao D, Lin R, Chu Y, Zhang H, et al. Acetylation targets the M2 isoform of pyruvate kinase for degradation through chaperone-mediated autophagy and promotes tumor growth. Mol Cell. 2011;42:719–730. doi: 10.1016/j.molcel.2011.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Luan W, Wang Y, Chen X, Shi Y, Wang J, Zhang J, et al. PKM2 promotes glucose metabolism and cell growth in gliomas through a mechanism involving a let-7a/c-Myc/hnRNPA1 feedback loop. Oncotarget. 2015;6:13006–13018. doi: 10.18632/oncotarget.3514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Yang C, Iyer RR, Yu ACH, Yong RL, Park DM, Weil RJ, et al. β-Catenin signaling initiates the activation of astrocytes and its dysregulation contributes to the pathogenesis of astrocytomas. Proc Natl Acad Sci U S A. 2012;109:6963–6968. doi: 10.1073/pnas.1118754109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Hitosugi T, Kang S, Vander Heiden MG, Chung TW, Elf S, Lythgoe K, et al. Tyrosine phosphorylation inhibits PKM2 to promote the Warburg effect and tumor growth. Sci Signal 2009, 2: ra73. [DOI] [PMC free article] [PubMed]
- 171.Xu C, Wu X, Zhu J. VEGF promotes proliferation of human glioblastoma multiforme stem-like cells through VEGF receptor 2. ScientificWorldJournal. 2013;2013:417413. doi: 10.1155/2013/417413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Han L, Yang Y, Yue X, Huang K, Liu X, Pu P, et al. Inactivation of PI3K/AKT signaling inhibits glioma cell growth through modulation of β-catenin-mediated transcription. Brain Res. 2010;1366:9–17. doi: 10.1016/j.brainres.2010.09.097. [DOI] [PubMed] [Google Scholar]
- 173.Bernardi A, Frozza RL, Hoppe JB, Salbego C, Pohlmann AR, Battastini AMO, et al. The antiproliferative effect of indomethacin-loaded lipid-core nanocapsules in glioma cells is mediated by cell cycle regulation, differentiation, and the inhibition of survival pathways. Int J Nanomedicine. 2013;8:711–728. doi: 10.2147/IJN.S40284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhang J, Huang K, Shi Z, Zou J, Wang Y, Jia Z, et al. High β-catenin/Tcf-4 activity confers glioma progression via direct regulation of AKT2 gene expression. Neuro-Oncol. 2011;13:600–609. doi: 10.1093/neuonc/nor034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Lee MW, Kim DS, Kim HR, Kim HJ, Yang JM, Ryu S, et al. Cell death is induced by ciglitazone, a peroxisome proliferator-activated receptor γ (PPARγ) agonist, independently of PPARγ in human glioma cells. Biochem Biophys Res Commun. 2012;417:552–557. doi: 10.1016/j.bbrc.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 176.Lin CL, Wang MH, Qin YF, Fang M, Xie BB, Zhong XY. Differentiation of SWO-38 glioma cells induced by CDA-2 is mediated by peroxisome proliferator-activated receptor gamma. J Neurooncol. 2009;95:29–36. doi: 10.1007/s11060-009-9900-x. [DOI] [PubMed] [Google Scholar]
- 177.Qiu J, Shi Z, Jiang J. Cyclooxygenase-2 in glioblastoma multiforme. Drug Discov Today. 2017;22:148–156. doi: 10.1016/j.drudis.2016.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wu M, Guan J, Li C, Gunter S, Nusrat L, Ng S, et al. Aberrantly activated Cox-2 and Wnt signaling interact to maintain cancer stem cells in glioblastoma. Oncotarget. 2017;8:82217–82230. doi: 10.18632/oncotarget.19283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Gurpinar E, Grizzle WE, Piazza GA. NSAIDs inhibit tumorigenesis, but how? Clin Cancer Res Off J Am Assoc Cancer Res. 2014;20:1104–1113. doi: 10.1158/1078-0432.CCR-13-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Thompson WJ, Piazza GA, Li H, Liu L, Fetter J, Zhu B, et al. Exisulind induction of apoptosis involves guanosine 3’,5’-cyclic monophosphate phosphodiesterase inhibition, protein kinase G activation, and attenuated beta-catenin. Cancer Res. 2000;60:3338–3342. [PubMed] [Google Scholar]
- 181.Lan F, Yue X, Han L, Shi Z, Yang Y, Pu P, et al. Genome-wide identification of TCF7L2/TCF4 target miRNAs reveals a role for miR-21 in Wnt-driven epithelial cancer. Int J Oncol. 2012;40:519–526. doi: 10.3892/ijo.2011.1215. [DOI] [PubMed] [Google Scholar]
- 182.Lee HC, Park IC, Park MJ, An S, Woo SH, Jin HO, et al. Sulindac and its metabolites inhibit invasion of glioblastoma cells via down-regulation of Akt/PKB and MMP-2. J Cell Biochem. 2005;94:597–610. doi: 10.1002/jcb.20312. [DOI] [PubMed] [Google Scholar]
- 183.Wang D, Dubois RN. Eicosanoids and cancer. Nat Rev Cancer. 2010;10:181–193. doi: 10.1038/nrc2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Hau P, Kunz-Schughart L, Bogdahn U, Baumgart U, Hirschmann B, Weimann E, et al. Low-dose chemotherapy in combination with COX-2 inhibitors and PPAR-gamma agonists in recurrent high-grade gliomas - a phase II study. Oncology. 2007;73:21–25. doi: 10.1159/000120028. [DOI] [PubMed] [Google Scholar]
- 185.Tinsley HN, Gary BD, Keeton AB, Lu W, Li Y, Piazza GA. Inhibition of PDE5 by sulindac sulfide selectively induces apoptosis and attenuates oncogenic Wnt/β-catenin-mediated transcription in human breast tumor cells. Cancer Prev Res Phila Pa. 2011;4:1275–1284. doi: 10.1158/1940-6207.CAPR-11-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Tinsley HN, Grizzle WE, Abadi A, Keeton A, Zhu B, Xi Y, et al. New NSAID targets and derivatives for colorectal cancer chemoprevention. Recent Results Cancer Res. 2013;191:105–120. doi: 10.1007/978-3-642-30331-9_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Gilroy DW, Colville-Nash PR. New insights into the role of COX 2 in inflammation. J Mol Med Berl Ger. 2000;78:121–129. doi: 10.1007/s001090000094. [DOI] [PubMed] [Google Scholar]
- 188.Puhl AC, Milton FA, Cvoro A, Sieglaff DH, Campos JCL, Bernardes A, et al. Mechanisms of peroxisome proliferator activated receptor γ regulation by non-steroidal anti-inflammatory drugs. Nucl Recept Signal. 2015;13:e004. doi: 10.1621/nrs.13004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Andersen V, Vogel U. Systematic review: interactions between aspirin, and other nonsteroidal anti-inflammatory drugs, and polymorphisms in relation to colorectal cancer. Aliment Pharmacol Ther. 2014;40:147–159. doi: 10.1111/apt.12807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Jurenka JS. Anti-inflammatory properties of curcumin, a major constituent of Curcuma longa: a review of preclinical and clinical research. Altern Med Rev J Clin Ther. 2009;14:141–153. [PubMed] [Google Scholar]
- 191.Rodriguez GA, Shah AH, Gersey ZC, Shah SS, Bregy A, Komotar RJ, et al. Investigating the therapeutic role and molecular biology of curcumin as a treatment for glioblastoma. Ther Adv Med Oncol. 2016;8:248–260. doi: 10.1177/1758834016643518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Zhou H, Beevers CS, Huang S. The targets of curcumin. Curr Drug Targets. 2011;12:332–347. doi: 10.2174/138945011794815356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Sordillo LA, Sordillo PP, Helson L. Curcumin for the treatment of glioblastoma. Anticancer Res. 2015;35:6373–6378. [PubMed] [Google Scholar]
- 194.Luthra PM, Lal N. Prospective of curcumin, a pleiotropic signalling molecule from Curcuma longa in the treatment of Glioblastoma. Eur J Med Chem. 2016;109:23–35. doi: 10.1016/j.ejmech.2015.11.049. [DOI] [PubMed] [Google Scholar]
- 195.Joe B, Vijaykumar M, Lokesh BR. Biological properties of curcumin-cellular and molecular mechanisms of action. Crit Rev Food Sci Nutr. 2004;44:97–111. doi: 10.1080/10408690490424702. [DOI] [PubMed] [Google Scholar]
- 196.Menon VP, Sudheer AR. Antioxidant and anti-inflammatory properties of curcumin. Adv Exp Med Biol. 2007;595:105–125. doi: 10.1007/978-0-387-46401-5_3. [DOI] [PubMed] [Google Scholar]
- 197.Weissenberger J, Priester M, Bernreuther C, Rakel S, Glatzel M, Seifert V, et al. Dietary curcumin attenuates glioma growth in a syngeneic mouse model by inhibition of the JAK1,2/STAT3 signaling pathway. Clin Cancer Res. 2010;16:5781–5795. doi: 10.1158/1078-0432.CCR-10-0446. [DOI] [PubMed] [Google Scholar]
- 198.Mazidi M, Karimi E, Meydani M, Ghayour-Mobarhan M, Ferns GA. Potential effects of curcumin on peroxisome proliferator-activated receptor-γ in vitro and in vivo. World J Methodol. 2016;6:112–117. doi: 10.5662/wjm.v6.i1.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Chen A, Xu J. Activation of PPAR{gamma} by curcumin inhibits Moser cell growth and mediates suppression of gene expression of cyclin D1 and EGFR. Am J Physiol Gastrointest Liver Physiol. 2005;288:G447–G456. doi: 10.1152/ajpgi.00209.2004. [DOI] [PubMed] [Google Scholar]
- 200.He M, Li Y, Zhang L, Li L, Shen Y, Lin L, et al. Curcumin suppresses cell proliferation through inhibition of the Wnt/β-catenin signaling pathway in medulloblastoma. Oncol Rep. 2014;32:173–180. doi: 10.3892/or.2014.3206. [DOI] [PubMed] [Google Scholar]
- 201.Shinojima N, Yokoyama T, Kondo Y, Kondo S. Roles of the Akt/mTOR/p70S6K and ERK1/2 signaling pathways in curcumin-induced autophagy. Autophagy. 2007;3:635–637. doi: 10.4161/auto.4916. [DOI] [PubMed] [Google Scholar]
- 202.Ackenheil M, Weber K. Developments in antipsychotic therapy with regard to hypotheses for schizophrenia. Dialogues Clin Neurosci. 2002;4:426–431. doi: 10.31887/DCNS.2002.4.4/mackenheil. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Wiklund ED, Catts VS, Catts SV, Ng TF, Whitaker NJ, Brown AJ, et al. Cytotoxic effects of antipsychotic drugs implicate cholesterol homeostasis as a novel chemotherapeutic target. Int J Cancer. 2010;126:28–40. doi: 10.1002/ijc.24813. [DOI] [PubMed] [Google Scholar]
- 204.Guo QH, Yang HJ, Wang SD. Olanzapine inhibits the proliferation and induces the differentiation of glioma stem-like cells through modulating the Wnt signaling pathway in vitro. Eur Rev Med Pharmacol Sci. 2015;19:4455. [PubMed] [Google Scholar]
- 205.Wang Y, Huang N, Li H, Liu S, Chen X, Yu S, et al. Promoting oligodendroglial-oriented differentiation of glioma stem cell: a repurposing of quetiapine for the treatment of malignant glioma. Oncotarget. 2017;8:37511–37524. doi: 10.18632/oncotarget.16400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ouchi N, Parker JL, Lugus JJ, Walsh K. Adipokines in inflammation and metabolic disease. Nat Rev Immunol. 2011;11:85–97. doi: 10.1038/nri2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Shehzad A, Iqbal W, Shehzad O, Lee YS. Adiponectin: regulation of its production and its role in human diseases. Horm Athens Greece. 2012;11:8–20. doi: 10.1007/BF03401534. [DOI] [PubMed] [Google Scholar]
- 208.Fantuzzi G. Adiponectin in inflammatory and immune-mediated diseases. Cytokine. 2013;64:1–10. doi: 10.1016/j.cyto.2013.06.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Feng H, Liu Q, Zhang N, Zheng L, Sang M, Feng J, et al. Leptin promotes metastasis by inducing an epithelial-mesenchymal transition in A549 lung cancer cells. Oncol Res. 2013;21:165–171. doi: 10.3727/096504014X13887748696662. [DOI] [PubMed] [Google Scholar]
- 210.Kato S, Abarzua-Catalan L, Trigo C, Delpiano A, Sanhueza C, García K, et al. Leptin stimulates migration and invasion and maintains cancer stem-like properties in ovarian cancer cells: an explanation for poor outcomes in obese women. Oncotarget. 2015;6:21100–21119. doi: 10.18632/oncotarget.4228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Barb D, Williams CJ, Neuwirth AK, Mantzoros CS. Adiponectin in relation to malignancies: a review of existing basic research and clinical evidence. Am J Clin Nutr. 2007;86:s858–s866. doi: 10.1093/ajcn/86.3.858S. [DOI] [PubMed] [Google Scholar]
- 212.Reinke L, Lam AP, Flozak AS, Varga J, Gottardi CJ. Adiponectin inhibits Wnt co-receptor, Lrp6, phosphorylation and β-catenin signaling. Biochem Biophys Res Commun. 2016;470:606–612. doi: 10.1016/j.bbrc.2016.01.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Porcile C, Di Zazzo E, Monaco ML, D’Angelo G, Passarella D, Russo C, et al. Adiponectin as novel regulator of cell proliferation in human glioblastoma. J Cell Physiol. 2014;229:1444–1454. doi: 10.1002/jcp.24582. [DOI] [PubMed] [Google Scholar]
- 214.Polvani S, Tarocchi M, Tempesti S, Bencini L, Galli A. Peroxisome proliferator activated receptors at the crossroad of obesity, diabetes, and pancreatic cancer. World J Gastroenterol. 2016;22:2441–2459. doi: 10.3748/wjg.v22.i8.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Vansaun MN. Molecular pathways: adiponectin and leptin signaling in cancer. Clin Cancer Res Off J Am Assoc Cancer Res. 2013;19:1926–1932. doi: 10.1158/1078-0432.CCR-12-0930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Stedt H, Samaranayake H, Pikkarainen J, Määttä AM, Alasaarela L, Airenne K, et al. Improved therapeutic effect on malignant glioma with adenoviral suicide gene therapy combined with temozolomide. Gene Ther. 2013;20:1165–1171. doi: 10.1038/gt.2013.46. [DOI] [PubMed] [Google Scholar]
- 217.Wang XF, Wu DM, Li BX, Lu YJ, Yang BF. Synergistic inhibitory effect of sulforaphane and 5-fluorouracil in high and low metastasis cell lines of salivary gland adenoid cystic carcinoma. Phytother Res PTR. 2009;23:303–307. doi: 10.1002/ptr.2618. [DOI] [PubMed] [Google Scholar]
- 218.Li L, Lin X, Shoemaker AR, Albert DH, Fesik SW, Shen Y. Hypoxia-inducible factor-1 inhibition in combination with temozolomide treatment exhibits robust antitumor efficacy in vivo. Clin Cancer Res. 2006;12:4747–4754. doi: 10.1158/1078-0432.CCR-05-2842. [DOI] [PubMed] [Google Scholar]
- 219.Mathieu V, De Nève N, Le Mercier M, Dewelle J, Gaussin JF, Dehoux M, et al. Combining bevacizumab with temozolomide increases the antitumor efficacy of temozolomide in a human glioblastoma orthotopic xenograft model. Neoplasia N Y N. 2008;10:1383–1392. doi: 10.1593/neo.08928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Le Mercier M, Lefranc F, Mijatovic T, Debeir O, Haibe-Kains B, Bontempi G, et al. Evidence of galectin-1 involvement in glioma chemoresistance. Toxicol Appl Pharmacol. 2008;229:172–183. doi: 10.1016/j.taap.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 221.Yuan Y, Xue X, Guo RB, Sun XL, Hu G. Resveratrol enhances the antitumor effects of temozolomide in glioblastoma via ROS-dependent AMPK-TSC-mTOR signaling pathway. CNS Neurosci Ther. 2012;18:536–546. doi: 10.1111/j.1755-5949.2012.00319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Huang W, Zhang C, Cui M, Niu J, Ding W. Inhibition of Bevacizumab-induced epithelial-mesenchymal transition by BATF2 overexpression involves the suppression of Wnt/β-Catenin signaling in glioblastoma cells. Anticancer Res. 2017;37:4285–4294. doi: 10.21873/anticanres.11821. [DOI] [PubMed] [Google Scholar]
- 223.Chen J, Fu X, Wan Y, Wang Z, Jiang D, Shi L. miR-125b inhibitor enhance the chemosensitivity of glioblastoma stem cells to temozolomide by targeting Bak1. Tumour Biol J Int Soc Oncodevelopmental Biol Med. 2014;35:6293–6302. doi: 10.1007/s13277-014-1821-4. [DOI] [PubMed] [Google Scholar]
- 224.Zhang K, Zhu S, Liu Y, Dong X, Shi Z, Zhang A, et al. ICAT inhibits glioblastoma cell proliferation by suppressing Wnt/β-catenin activity. Cancer Lett. 2015;357:404–411. doi: 10.1016/j.canlet.2014.11.047. [DOI] [PubMed] [Google Scholar]
- 225.Kohsaka S, Wang L, Yachi K, Mahabir R, Narita T, Itoh T, et al. STAT3 inhibition overcomes temozolomide resistance in glioblastoma by downregulating MGMT expression. Mol Cancer Ther. 2012;11:1289–1299. doi: 10.1158/1535-7163.MCT-11-0801. [DOI] [PubMed] [Google Scholar]
- 226.Wang F, Xiao W, Sun J, Han D, Zhu Y. MiRNA-181c inhibits EGFR-signaling-dependent MMP9 activation via suppressing Akt phosphorylation in glioblastoma. Tumour Biol J Int Soc Oncodevelopmental Biol Med. 2014;35:8653–8658. doi: 10.1007/s13277-014-2131-6. [DOI] [PubMed] [Google Scholar]
- 227.Cornblatt BS, Ye L, Dinkova-Kostova AT, Erb M, Fahey JW, Singh NK, et al. Preclinical and clinical evaluation of sulforaphane for chemoprevention in the breast. Carcinogenesis. 2007;28:1485–1490. doi: 10.1093/carcin/bgm049. [DOI] [PubMed] [Google Scholar]
- 228.Vyas AR, Hahm ER, Arlotti JA, Watkins S, Stolz DB, Desai D, et al. Chemoprevention of prostate cancer by d, l-sulforaphane is augmented by pharmacological inhibition of autophagy. Cancer Res. 2013;73:5985–5995. doi: 10.1158/0008-5472.CAN-13-0755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Lenzi M, Fimognari C, Hrelia P. Sulforaphane as a promising molecule for fighting cancer. Cancer Treat Res. 2014;159:207–223. doi: 10.1007/978-3-642-38007-5_12. [DOI] [PubMed] [Google Scholar]
- 230.Lan F, Pan Q, Yu H, Yue X. Sulforaphane enhances temozolomide-induced apoptosis because of down-regulation of miR-21 via Wnt/β-catenin signaling in glioblastoma. J Neurochem. 2015;134:811–818. doi: 10.1111/jnc.13174. [DOI] [PubMed] [Google Scholar]
- 231.Negrette-Guzmán M, Huerta-Yepez S, Vega MI, León-Contreras JC, Hernández-Pando R, Medina-Campos ON, et al. Sulforaphane induces differential modulation of mitochondrial biogenesis and dynamics in normal cells and tumor cells. Food Chem Toxicol. 2017;100:90–102. doi: 10.1016/j.fct.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 232.Dai L, Cui X, Zhang X, Cheng L, Liu Y, Yang Y, et al. SARI inhibits angiogenesis and tumour growth of human colon cancer through directly targeting ceruloplasmin. Nat Commun. 2016;7:11996. doi: 10.1038/ncomms11996. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 233.Dash R, Su ZZ, Lee SG, Azab B, Boukerche H, Sarkar D, et al. Inhibition of AP-1 by SARI negatively regulates transformation progression mediated by CCN1. Oncogene. 2010;29:4412–4423. doi: 10.1038/onc.2010.194. [DOI] [PubMed] [Google Scholar]