Abstract
Background:
Being overweight constitutes a health risk, and the proportion of overweight and obese children is increasing. It has been argued that road traffic noise could be linked to adiposity through its influence on sleep and stress. Few studies, to our knowledge, have investigated whether noise and adiposity are associated. Most of them were on adults, and we are not aware of any longitudinal study using repeated measures.
Objectives:
The present longitudinal study investigated whether road traffic noise exposures in pregnancy (N = 6,963; obs = 22,975) or childhood (N = 6,403; obs = 14,585) were associated with body mass index (BMI) trajectories in children.
Methods:
We obtained information on BMI and covariates from questionnaires used in the Norwegian Mother and Child Cohort Study, Statistics Norway, and Medical Birth Registry of Norway. We modeled road traffic noise for the most exposed façade of children’s present and historical addresses at 6 time points from pregnancy to age 8. We investigated effects on BMI trajectories using repeated measures and linear mixed models.
Results:
The results indicated that BMI curves depended on road traffic noise exposure during pregnancy, but not on exposure during childhood. Children in the highest decile of traffic noise exposure had increased BMI, with 0.35 kg/m2 more than children in the lowest decile, from birth to age 8 years.
Conclusions:
The results indicate that exposure to road traffic noise during pregnancy may be associated with children’s BMI trajectories. Future studies should investigate this further, using anthropometric measures such as waist-hip ratio and skinfold thickness, in addition to BMI.
Keywords: Road traffic noise, Body mass index, BMI, Children, Norwegian Mother and Child Cohort Study
The prevalence of childhood overweight and obesity in Europe is estimated to be about 20%,1 and it has increased during the recent decades.2 Overweight and obesity are associated with negative health outcomes such as increased risk for type II diabetes, increased levels of cholesterol, elevated blood pressure, and reduced quality of life.3–6 Proposed causal factors include genetics, endocrine disorders, nutritional habits, and level of physical activity.7 In recent years, associations with environmental factors like air pollution have also been reported.8 A few studies have investigated whether road traffic noise is related to body mass index (BMI). Studies on adults found small positive associations between road traffic noise exposure and waist circumference and BMI, but these findings were not entirely consistent,9–11 and knowledge on these associations in children is scarce.12
An increasing number of children are daily exposed to road traffic noise exceeding recommended levels of Lden 55 dB.13,14 Environmental noise is associated with both physical and mental health effects, including impaired sleep.14–17 Noise-induced sleep impairments could be mediating a noise and overweight association. Children’s sleep duration is shown to be negatively associated with overweight in both cross-sectional and longitudinal studies18–21 possibly through the influence on the secretion of appetite regulating hormones such as leptin and ghrelin.22
Stress is another possible mechanism. Stress during pregnancy, which may be caused by exposure to noise, can affect fetal growth and physical development in childhood, including a heightened risk for childhood overweight and increased BMI.23,24 In addition, studies have found associations between traffic noise exposure and stress indicators in children.25 Stress in childhood may be 1 of the predictors of subsequent BMI in children.26 Thus, there is a possibility that high noise exposure during both pregnancy and childhood is associated with a lower BMI at birth, but a subsequent higher BMI during childhood.
To the best of our knowledge, no study to date has employed a longitudinal design with repeated measures to explore the relationship between road traffic noise and physical growth in children. The present study explored 2 different time windows of road traffic noise exposure. For exposure during pregnancy, we explored whether road traffic noise was associated with different BMI trajectories from birth to age 8 years. For exposure during childhood, we explored whether the average road traffic noise (between persons noise) was associated with different BMI trajectories from age 18 months to 8 years, and whether a change in road traffic noise level (within person noise) was associated with a corresponding change in BMI. We also explored the moderating role of household income, maternal education, and gender.
METHODS
Study Population
The study used questionnaire data from ages 6 and 18 months and 3, 5, 7 and 8 years from the Norwegian Mother and Child Cohort Study, MoBa.27 MoBa is a prospective population-based pregnancy cohort study conducted by the Norwegian Institute of Public Health. Participants were recruited from all over Norway from 1999 to 2008. The women consented to participation in 41% of the pregnancies. The cohort includes 114,500 children, 95,200 mothers, and 75,200 fathers. Mothers received invitations by mail, along with appointments for ultrasound scanning in week 17 or 18 of pregnancy. No exclusion criteria were used in the main study. MoBa is described in more detail elsewhere.27 Due to the limited availability of modeled road traffic noise, we used data only on Oslo residents. MoBa data were linked to the Medical Birth Registry of Norway, Statistics Norway, and to noise exposure estimations from the City of Oslo.
The participants in the present study were children born between 2000 and 2009. Inclusion criteria were (1) residential address in Oslo; (2) live birth; (3) single birth; (4) born to term (gestational age between 259 and 300 days28; (e) known date of birth. Children with address at confinement (granted hidden address, thus no address available), and older siblings also participating in the MoBa cohort, were excluded. Five hundred eighty-nine children were excluded due to preterm birth. There were 2 different but overlapping study samples: 1 for analyses of noise exposure during pregnancy (pregnancy sample), and 1 for analyses of noise exposure after birth (childhood sample), since both pregnancy and childhood noise might affect BMI trajectories through somewhat different mechanisms. The final pregnancy sample included 22,975 observations from 6,963 children, and the childhood sample included 14,585 observations from 6,403 children (Figure 1 and eTable 1; http://links.lww.com/EDE/B368). Four thousand five hundred eighty-seven children were part of both samples (1,816 only in childhood sample, 2,376 only in pregnancy sample).
FIGURE 1.
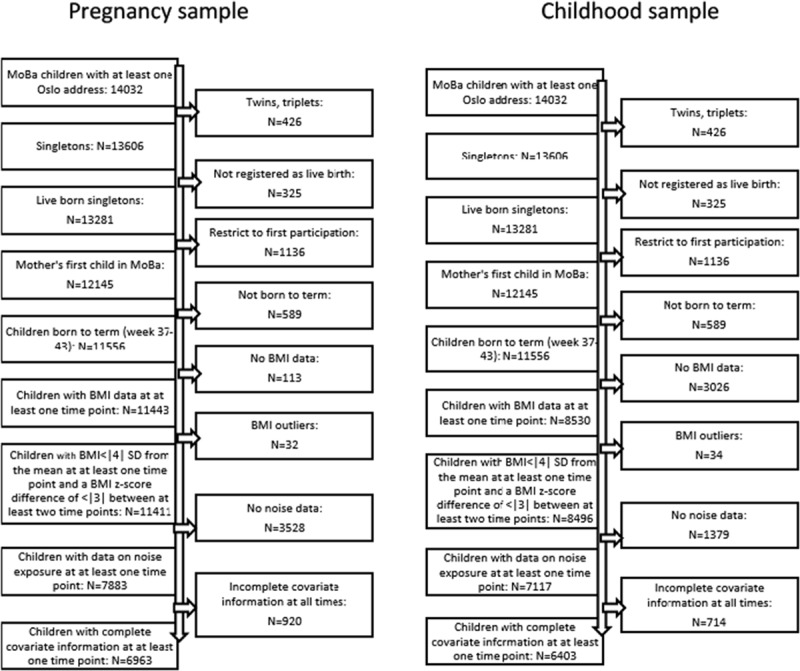
Flow chart for inclusion of the study sample.
Informed consent was obtained from each MoBa participant (mother) upon recruitment. MoBa and the present study were approved by The Regional Committee for Medical Research Ethics in South-Eastern Norway.
Noise Exposure Assessment
Estimations of road and rail traffic noise exposure were conducted by the Agency for Urban Environment, City of Oslo, in accordance with the Environmental Noise Directive.29 Noise exposure was modeled using the Nordic Prediction Method30,31 and the software program CadnaA version 4.3 (DataKustik, GmbH, Germany).32 A geographic information system approach was used to geocode all the residential addresses of the children’s mothers. Grid predictions of 5 × 5 m2 at 4 m height were used to assign noise level to the geocoded addresses. Noise exposure was assessed as Lden, and based on annual average daily traffic with diurnal distribution. Lden is the A-weighted (meaning that low audio frequencies are attenuated, since humans are less sensitive to low frequencies) day (07.00-19.00), evening (19.00–23.00), and night-time (23.00-07.00) equivalent noise level with a 5 dB and 10 dB penalty for the evening and nighttime noise, respectively. Estimation of road and rail traffic noise exposure is described in more detail elsewhere.33 The Lden was estimated for the most exposed façade. Noise exposure from road traffic and rail traffic in the pregnancy sample covered the whole pregnancy period (excluded if less than 180 days of exposure information). For childhood noise exposure, road traffic noise was a time-varying variable, calculated for 5 different exposure windows, each including 1 year before each of the questionnaire completion dates. The modeled Lden for road traffic took into account the residential history of each mother and was weighted by the time spent at each address.
We included road traffic noise was included as a continuous variable. Rail traffic noise was categorized as unexposed, exposed to Lden ≤ 30 dB, or Lden > 30 dB. Few were exposed to high rail traffic noise levels. Lden below 30 dB is below the background level and is almost negligible. Because the noise metric Lden is an average made up of a certain number of clearly distinct noise events, individuals exposed Lden less than 30 dB may still be disturbed by some events, although the average level is low.
Moving was the most important factor influencing noise exposure. Frequency of moves is given in eTable 1; http://links.lww.com/EDE/B368.
Outcome
We obtained measured values of length and weight at birth from the Medical Birth Registry of Norway. Maternal reports of length/height and weight from MoBa questionnaires at 18 months and 3, 5, 7, and 8 years. We used height and weight to compute BMI values as weight (kg) divided by height squared (m2).
Covariates
Covariate information was obtained from the MoBa 6 and 18- month-, and 3-, 5-, 7-, and 8-year questionnaires, the Medical Birth Registry of Norway, Statistics Norway, and the City of Oslo. Covariates were selected using Directed Acyclic Graphs (DAGs).34–36 Based on the DAG (see eFigure 1; http://links.lww.com/EDE/B368), we arrived at a minimal adjustment set containing gross household income and urbanicity, using the web-based software program dagitty.net.37 Urbanicity indicated proximity to the city center. Additional covariates included were BMI at birth (only childhood sample), ethnicity, maternal education, child’s age, gender, and mother’s BMI before pregnancy (Table 1). Diet, from questionnaires at ages 3 and 7, was based on New Nordic Diet.38 Physical activity, from questionnaire at age 7, was defined as hours a week physically active/doing sports when not in school: < 1 hour, 1–2, 3–4, 5–7, 8–10, or more than 11 hours. Air pollution estimates were based on Land Use Regression models fitted in the HELIX project.39–41 Air pollution included modeled levels of PM2.5, NO2, and NOX for the same exposure windows as the noise variables and were only used in sensitivity analyses.
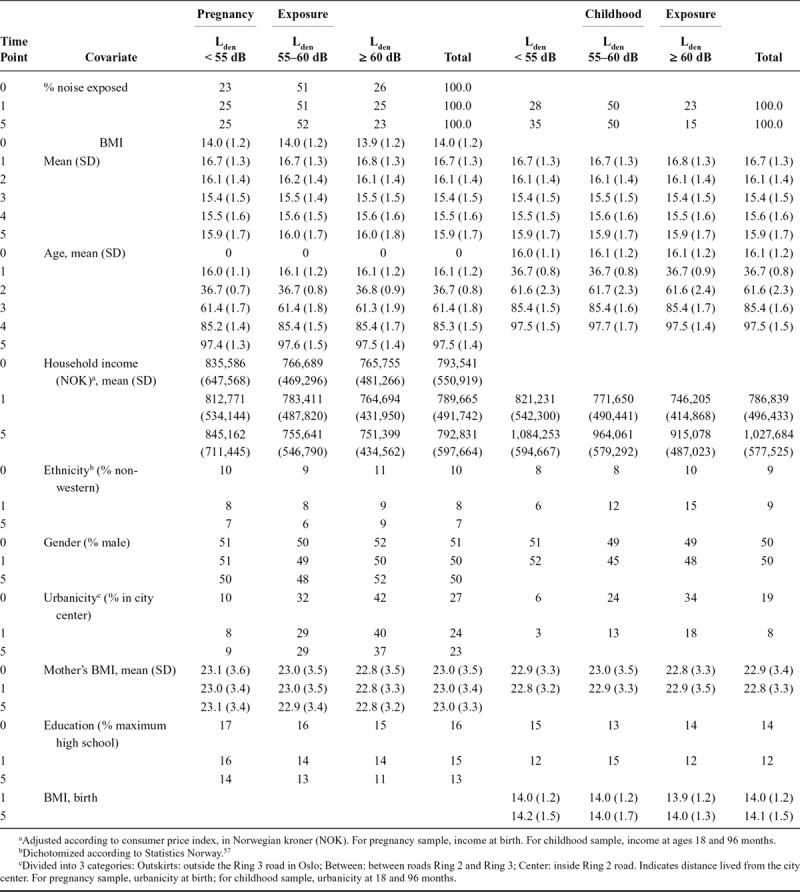
TABLE 1.
Characteristics of the Study Population
Statistical Analyses
The present study included repeated measurements of BMI from birth to 8 years. We used linear mixed models in the main analyses, and diagnostics were met, except for some heteroscedasticity observed in a standardized residuals versus fitted values plot. (See eAppendix 1; http://links.lww.com/EDE/B368 on model building and diagnostics.) We evaluated interactions and compared models using likelihood-ratio tests. The final models contained a random subject intercept, random slope for age, and an unstructured covariance matrix, and were estimated using maximum likelihood. The childhood models included an independent residual structure estimating a distinct variance for each time point, in order to account for heteroscedasticity. Akaike’s and Bayesian information criteria indicated that this residual structure gave a better model fit than an exponential structure, the latter taking into account the correlation between residuals, but not the heterogeneity of the variance. For the pregnancy sample model, an exponential residual structure fitted better. The basic models contained an interaction term between age (age splines) and gender. The factors of interest were the interaction terms between age and noise, because we wanted to explore the effect of noise on the BMI trajectory. The model of noise exposure during pregnancy was as follows:
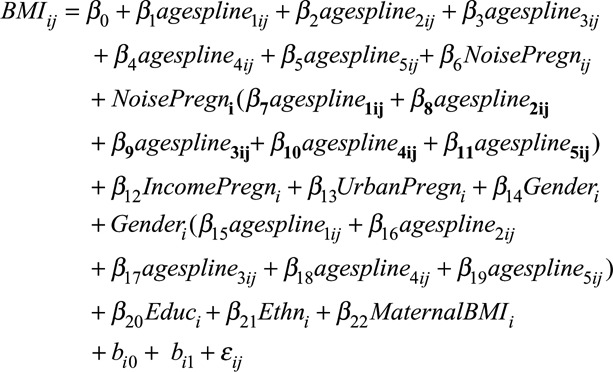 |
where i indicates subject and j indicates time point. bi0 is the random intercept (id-variable) and bi1 is random slope for age. εij is the error term. Cubic splines were made for age, with knots at 0, 18, 36, 60, 84, and 96 months.
The model of noise exposure during childhood, estimating the influence of averaged road traffic noise on the association between age and BMI, was as follows:
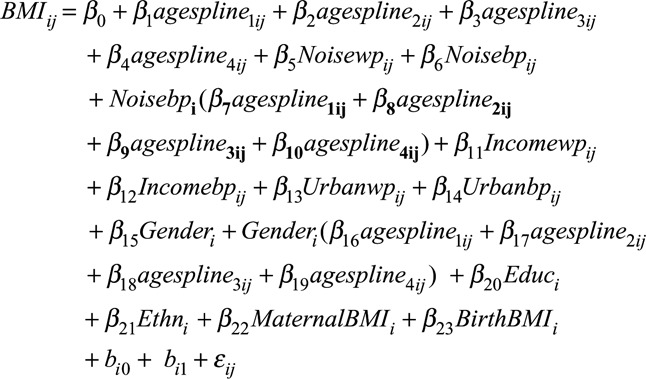 |
where wp = within person; bp = between persons. An intraclass correlation of 0.75 (95% CI = [.74, .76]) for road traffic noise, 0.72 (95% CI = [.71, .73]) for income and 0.81 (95% CI = [.80, .82]) for urbanicity indicated sufficient within-person variability to warrant decomposition into between and within person variables. This was done in the childhood sample to assess associations between children’s average noise exposure and BMI, and associations between change in noise exposure at a given time(s) and BMI. The between-persons component was the mean level of noise exposure for each child (the mean of all 1-year periods that were included in the study for a particular child). The within-person component was estimated by subtracting the child’s noise mean from the noise level at each time point. Income and urbanicity were decomposed in the same way.
We assessed associations between road traffic noise and BMI at specific ages using linear regression analyses. We performed sensitivity analyses for rail traffic noise and air pollutants PM2.5, NO2, and NOX, and for diet and physical activity. Graphs, predicted marginal means, and marginal effects for the linear mixed model results were obtained with the user-written Stata program marginscontplot.42
We used analysis of variance and chi-square tests to assess differences between nonparticipants and study samples at different time points. In addition to the main analyses on the original data, analyses on 50 multiple imputed data sets and on complete cases were also done, in order to address the impact of loss to follow-up (See eTables 1; http://links.lww.com/EDE/B368, 2, and eAppendix 2; http://links.lww.com/EDE/B368).
For the purpose of comparing with other studies, we calculated mean increase in BMI from birth to age 8 in the pregnancy sample for the lowest and highest deciles of noise exposure.
All analyses were done in Stata, version 14.0 (StataCorp, Texas).43
RESULTS
Population Characteristics
In the pregnancy sample, mean BMI at birth was 14.0 kg/m2 (SD = 1.2) and 16.7 kg/m2 (SD = 1.3) at 18 months. BMI decreased to age 5 years, then increased to 15.9 kg/m2 (SD = 1.7) at age 8 years (eFigure 2; http://links.lww.com/EDE/B368). Mean road traffic noise level during pregnancy was Lden 56.2 dB (SD = 8.4; range, 11–77). The mean BMI trajectory in the childhood sample was similar to that in the pregnancy sample. The mean road traffic noise level during childhood decreased with time, from Lden 55.4 (SD = 8.5; range, 11–80) at age 18 months, to Lden 53.3 (SD = 7.8) at age 8 years. The mean noise within-persons value was −0.025 (SD = 3.25) (Table 1, eTable 3; http://links.lww.com/EDE/B368).
Main Results
Pregnancy Sample
The BMI trajectory depended on road traffic noise exposure level during pregnancy (P =0.02; Figure 2, Table 2, eTable 4; http://links.lww.com/EDE/B368). Compared with children of mothers exposed to an average of Lden 45 dB during pregnancy (14.05 95% CI = [14.00, 14.10]), children of mothers exposed to Lden 65 dB (13.95, 95% CI = [13.91, 13.99]) had a lower predicted BMI at birth, but a higher BMI at 8 years (Lden 65 dB: 15.96 kg/m2, CI = [15.86, 16.05] vs. Lden 45 dB: 15.83 kg/m2, CI = [15.73, 15.94]) (eTable 4; http://links.lww.com/EDE/B368). Apart from at birth, we cannot rule out the possibility that these differences were due to chance. This was also shown in linear regression analyses with BMI at birth (B = −0.0039, 95% CI = [−0.0076, -0.0002]) and at age 8 years (0.0052, 95% CI = [−0.0052, 0.0155]) as outcomes (but see results for imputed data below). Children in the highest decile of road traffic noise exposure (≥ Lden 67.2 dB) increased their predicted BMI from birth to age 8 with 0.35 kg/m2 more than children in the lowest decile (≤ Lden 45 dB). The effect of road traffic noise did not depend on gender (P = 0.36), education (P = 0.52) or household income (P = 0.80) (Table 2).
FIGURE 2.
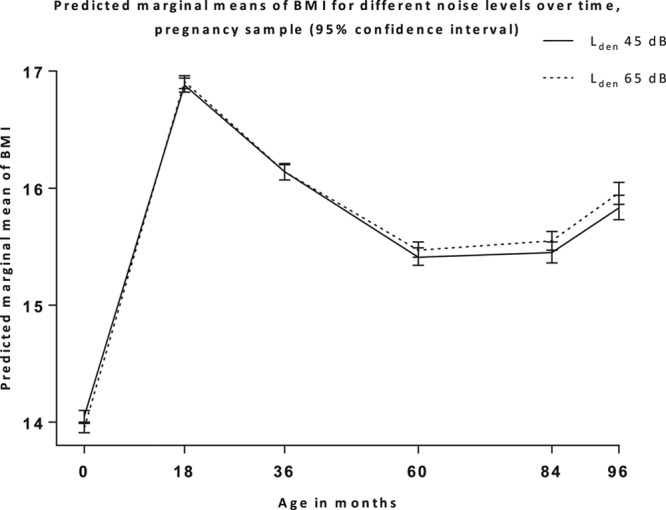
Predicted BMI trajectories for different levels of noise exposure during pregnancy, with 95% confidence intervals. BMI, body mass index.
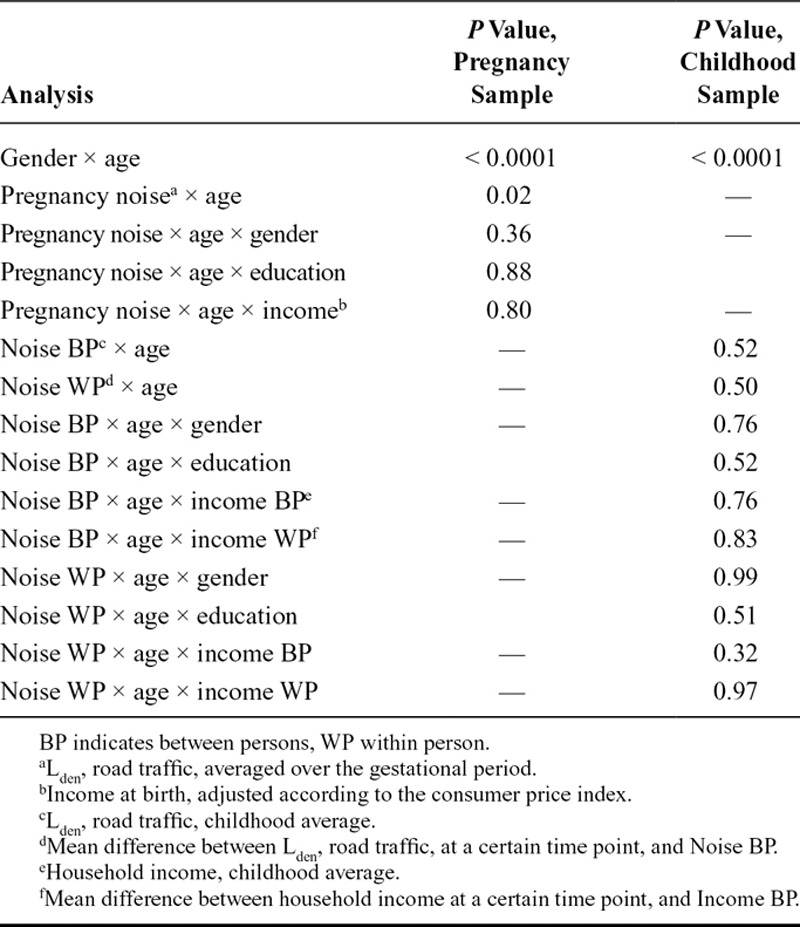
TABLE 2.
Main Results of Likelihood Ratio Tests
Childhood Sample
The BMI trajectory did not depend on average road traffic noise exposure level during childhood (P = 0.52; Table 2, eTable 5; http://links.lww.com/EDE/B368, Figure 3A). A change in road traffic noise exposure from 1 time window to the next (age and within-person noise interaction) was not associated with a corresponding change in BMI at that time point (P = 0.50; eTable 6; http://links.lww.com/EDE/B368, Figure 3B). The findings did not depend on gender, education, average household income, or change in household income (all P > 0.32; Table 2).
FIGURE 3.
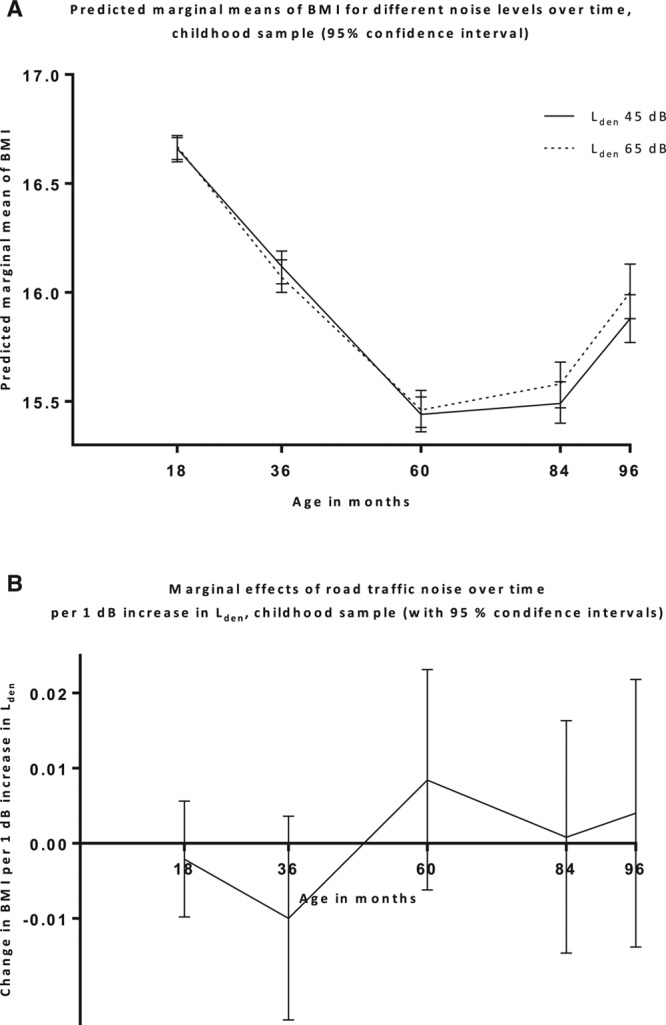
A, Predicted BMI trajectories for different average levels of noise exposure during childhood (solid lines), with 95% CIs, and predicted change in BMI per 1 dB increase in noise level at the different times, with 95 % CIs (B). CI, confidence interval.
Rail traffic noise, air pollution, diet and physical activity did not change the effect of road traffic noise in any of the models (eTables 7–10; http://links.lww.com/EDE/B368).
Average imputed values for covariates and predicted values of BMI for different noise categories were similar across imputed, original, and complete cases data (eTables 11, 12; http://links.lww.com/EDE/B368). A Wald test on the imputed data results showed evidence of an interaction between age and pregnancy road traffic noise (P = 0.03). Linear regression analyses on the imputed pregnancy sample data showed associations between road traffic noise and BMI at birth (B = −.0041, 95% CI = [−0.0078, −0.0004]) and BMI at age 8 years (0.0083, 95% CI = [0.0003, 0.0163]). There were no interactions between age and road traffic noise in the childhood sample.
DISCUSSION
Comparing with Previous Studies
Road traffic noise during pregnancy showed an association with the BMI trajectory in children. There was no effect modification by gender, household income, or maternal education. Rail traffic noise, air pollution, diet, and physical activity did not affect the results. For childhood road traffic noise exposure, no statistically significant effects on the BMI trajectory were found.
Our findings are partly in line with a Danish study12 that found no association between averaged lifetime noise exposure and BMI z-scores at age 7, using a linear regression analysis. In contrast with our study, they found no association between noise during pregnancy and BMI. The estimates reported in the Danish study were in the expected direction, though, and an association with overweight was found for both noise exposure windows. Due to the different study designs, direct comparisons are difficult. Compared with a study on air pollution and BMI with repeated measures,8 the magnitude of the effect of noise in our study was similar to the effect of air pollution in that study, where an increase in BMI of 0.4 kg/m2 was found for 10-year-olds in the highest decile of NOX exposure, compared with those in the lowest decile. In our study, the similar difference for noise during pregnancy was 0.35 kg/m2. An explanation for why we observed associations in the pregnancy sample, but not in the childhood sample, might be that adults are more easily disturbed by noise than children,44 and that the influence of noise on children goes mainly through the mother, in pregnancy.
In accordance with other studies on road traffic noise and adiposity markers, we found no influence of air pollution or rail traffic noise on the effect of road traffic noise.10,12 PM2.5 levels were somewhat lower in our study area compared with those typically found in other studies, whereas NO2 and NOX levels were higher.45 Diet and physical activity did not substantially change the effect of road traffic noise, indicating that the lack of complete diet and physical activity information was relatively unimportant, as was concluded in a comparable study.8
Children of mothers exposed to higher noise levels during pregnancy had, on average, a lower BMI at birth. Previous studies have found associations between pregnant women highly noise exposed at work and impaired fetal growth.23 Noise exposure at night can impact the mothers’ sleep, leading to increased stress.46–48 Noise-induced maternal stress during pregnancy may be 1 explanation for the different BMI trajectories for different noise exposure levels. A study by Li et al.24 compared Danish children whose mothers had or had not experienced a highly stressful life event during pregnancy. BMI and prevalence of overweight were higher in the exposed children at all ages from 7 to 13 years, especially from age 10 and onward. Both the studies by Li et al.24 and Jerrett et al.8, and our multiple imputation analyses, suggest that the effects of noise in the present study might have been larger for older children.
The mean trajectory for BMI was similar or slightly lower compared with that found in other studies, including 1 reporting growth references for Norwegian children, although children in the higher BMI range was somewhat underrepresented.28,49–51 Average BMI in the study samples was at most of the time points similar to the average BMI of nonparticipants.
The effect of road traffic noise did not depend on household income. Others have found no effect modification by other SES variables when investigating noise and BMI.12 Lower income has been associated with a steeper increase in BMI with age.52 There might be a threshold above which income level is too high to reveal an effect modification.
A large portion of missing data was due to children not living in Oslo at 1 or more points in time, children dropping out of the MoBa, or, for ages 7 and 8 years, the full MoBa data set not yet being available. Results of the multiple imputation analyses support the results obtained with the original data, indicating that loss to follow-up did not influence the results.
Strengths and Limitations
To the best of our knowledge, the present study is the first to examine road traffic noise and children’s BMI trajectories. The longitudinal design allowed a comparison of both within and between person effects of noise. The analyses were based on a large number of observations of many participants. Most covariate information was obtained from registries, reducing missing and increasing the reliance in the information. The noise exposure range was wide, increasing the chances of detecting effects of noise, if present.
The study had some limitations. Whereas BMI is a good indicator of excess adiposity in overweight children, BMI differences for thinner children can to a larger extent be due to fat-free mass (e.g., muscles, bones).53 Thus, it might be that road traffic noise is associated with adiposity, but that this association is not detected or is underestimated due to the moderate sensitivity of BMI. A recent study on adults11 found associations between road traffic noise and both waist circumference and waist-to-hip ratio, but no association with BMI. Unfortunately, anthropometrics other than BMI were unavailable in the present study.
BMI was based on parental reports. A recent article54 reported the results of a validation study done to assess the accuracy of parental-reported BMI in the MoBa study. The reported BMIs were compared with measured BMIs obtained in the Bergen Growth Study.55 The correlation was high: Pearson’s r = 0.86 (95% CI, [0.81, 0.90]), indicating that the parental-reported BMI was accurate (although misclassification cannot be completely ruled out).
Road traffic noise was modeled for the most exposed façade outside. Many participants probably had bedrooms facing the quiet side. Highly exposed were probably more likely to sleep with windows closed17 and have better façade insulation. Unfortunately, information about these factors was lacking. In another study on adults on road traffic noise and obesity, associations were stronger for men with bedrooms facing a road.10 Using noise outside the most exposed façade, the result is likely an underestimated association between noise and sleep for those with a bedroom facing the most exposed façade.56 Not accounting for these factors might have led to underestimation of the effects of road traffic noise.
Some heteroscedasticity was present in the models. We were not able to fully correct this, resulting in underestimation of high values and overestimation of lower values of BMI, but correct estimates of values in the middle range. This might also have led to underestimation of effects of road traffic noise on BMI.
CONCLUSIONS
The present longitudinal study found an association between road traffic noise exposure during pregnancy and BMI trajectories from birth to age 8 years. No association between exposure in childhood and BMI trajectories from age 18 months to 8 years was observed. Future studies should investigate the association between road traffic noise and BMI with repeated measures data, using measured BMI instead of or in addition to parental reports, as well as using additional anthropometric measures. Possible mechanisms should also be investigated.
ACKNOWLEDGMENTS
We are grateful to all the participating families in Norway who take part in MoBa. Thanks to Erik Aune at the City of Oslo’s Agency for Urban Environment, for providing the noise data.
Footnotes
The data are obtained from the Norwegian Mother and Child Cohort Study (dataaccess@fhi.no), Statistics Norway (http://www.ssb.no/en/omssb/kontakt-oss), the Norwegian Institute of Public Health (Medical Birth Registry of Norway; https://fhi.no/en/more/research--access-to-data/), and City of Oslo (https://tjenester.oslo.kommune.no/ekstern/snokweb/skjema/rad/rad002?execution=e2s1) Stata code can be handed out, upon request.
Supported by the Norwegian Research Council, Environmental Exposures and Health Outcomes (MILPAAHEL), project no.; 228142. The Norwegian Mother and Child Cohort Study is supported by the Norwegian Ministry of Health and Care Services and the Ministry of Education and Research, NIH/NIEHS (contract no N01-ES-75558), NIH/NINDS (grant no.1 UO1 NS 047537-01 and grant no.2 UO1 NS 047537-06A1).
The authors report no conflicts of interest.
REFERENCES
- 1.Wang Y, Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry. 2012;24:176–188.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103(6 Pt 1):1175–1182.. [DOI] [PubMed] [Google Scholar]
- 4.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150:12–17.e2.. [DOI] [PubMed] [Google Scholar]
- 5.Daniels SR. The consequences of childhood overweight and obesity. Future Child. 2006;16:47–67.. [DOI] [PubMed] [Google Scholar]
- 6.Wardle J, Cooke L. The impact of obesity on psychological well-being. Best Pract Res Clin Endocrinol Metab. 2005;19:421–440.. [DOI] [PubMed] [Google Scholar]
- 7.Gurnani M, Birken C, Hamilton J. Childhood obesity: causes, consequences, and management. Pediatr Clin North Am. 2015;62:821–840.. [DOI] [PubMed] [Google Scholar]
- 8.Jerrett M, McConnell R, Wolch J, et al. Traffic-related air pollution and obesity formation in children: a longitudinal, multilevel analysis. Environ Health. 2014;13:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christensen JS, Raaschou-Nielsen O, Tjønneland A, et al. Long-term exposure to residential traffic noise and changes in body weight and waist circumference: a cohort study. Environ Res. 2015;143(Pt A):154–161.. [DOI] [PubMed] [Google Scholar]
- 10.Oftedal B, Krog NH, Pyko A, et al. Road traffic noise and markers of obesity—a population-based study. Environ Res. 2015;138:144–153.. [DOI] [PubMed] [Google Scholar]
- 11.Pyko A, Eriksson C, Oftedal B, et al. Exposure to traffic noise and markers of obesity. Occup Environ Med. 2015;72:594–601.. [DOI] [PubMed] [Google Scholar]
- 12.Christensen JS, Hjortebjerg D, Raaschou-Nielsen O, Ketzel M, Sørensen TIA, Sørensen M. Pregnancy and childhood exposure to residential traffic noise and overweight at 7 years of age. Environ Int. 2016;94:170–176.. [DOI] [PubMed] [Google Scholar]
- 13.EEA. Noise in Europe 2014. 2014Luxembourg: European Environment Agency. [Google Scholar]
- 14.Statistics Norway. Barn og unges miljø og helse 2011. Utvalgte indikatorer om barn og unges fysiske og sosiale miljøfaktorer. 2012Norway: Statistics Norway, Oslo-Kongsvinger. [Google Scholar]
- 15.Ising H, Ising M. Chronic cortisol increases in the first half of the night caused by road traffic noise. Noise Health. 2002;4:13–21.. [PubMed] [Google Scholar]
- 16.Stansfeld S, Clark C. Health effects of noise exposure in children. Curr Environ Health Rep. 2015;2:171–178.. [DOI] [PubMed] [Google Scholar]
- 17.Öhrström E, Hadzibajramovic E, Holmes M, Svensson H. Effects of road traffic noise on sleep: studies on children and adults. J Environ Psychol. 2006;26:116–126.. [Google Scholar]
- 18.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–626.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring). 2008;16:265–274.. [DOI] [PubMed] [Google Scholar]
- 20.Landhuis CE, Poulton R, Welch D, Hancox RJ. Childhood sleep time and long-term risk for obesity: a 32-year prospective birth cohort study. Pediatrics. 2008;122:955–960.. [DOI] [PubMed] [Google Scholar]
- 21.O’Dea JA, Dibley MJ, Rankin NM. Low sleep and low socioeconomic status predict high body mass index: a 4-year longitudinal study of Australian school children. Pediatr Obes. 2012;7:295–303.. [DOI] [PubMed] [Google Scholar]
- 22.Hart CN, Cairns A, Jelalian E. Sleep and obesity in children and adolescents. Pediatr Clin North Am. 2011;58:715–733.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dzhambov AM, Dimitrova DD, Dimitrakova ED. Noise exposure during pregnancy, birth outcomes and fetal development: meta-analyses using quality effects model. Folia Medica. 2014;56:204–214.. [DOI] [PubMed] [Google Scholar]
- 24.Li J, Olsen J, Vestergaard M, Obel C, Baker JL, Sørensen TI. Prenatal stress exposure related to maternal bereavement and risk of childhood overweight. PLoS One. 2010;5:e11896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evans GW, Lercher P, Meis M, Ising H, Kofler WW. Community noise exposure and stress in children. J Acoust Soc Am. 2001;109:1023–1027.. [DOI] [PubMed] [Google Scholar]
- 26.Pervanidou P, Chrousos GP. Stress and obesity/metabolic syndrome in childhood and adolescence. Int J Pediatr Obes. 2011;6:21–28.. [DOI] [PubMed] [Google Scholar]
- 27.Magnus P, Birke C, Vejrup K, et al. Cohort profile update: The Norwegian Mother and Child Cohort Study (MoBa). Int J Epidemiol. 2016;45:382–388.. [DOI] [PubMed] [Google Scholar]
- 28.Chivers P, Hands B, Parker H, Beilin L, Kendall G, Bulsara M. Longitudinal modelling of body mass index from birth to 14 years. Obes Facts. 2009;2:302–310.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.EU. DIRECTIVE 2002/49/EC OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 25 June 2002 relating to the assessment and management of environmental noise. Official J Europ Communities. Available at: http://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32002L0049&from=EN. 2002;189:12–25. Accessed June 18, 2017.
- 30.Bendtsen H. The Nordic prediction method for road traffic noise. Sci Total Environ. 1999;235:331–338.. [Google Scholar]
- 31.Jonasson H, Nielsen HL. Road traffic noise—Nordic Prediction Method. TemaNord. 1996;525. [Google Scholar]
- 32.DataKustik. 4.3 edCadnaA. [Google Scholar]
- 33.Weyde KV, Krog NH, Oftedal B, et al. Road traffic noise and children’s inattention. Environ Health. 2017;16:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10:37–48.. [PubMed] [Google Scholar]
- 35.Pearl J. Causality: Models, Reasoning and Inference. 2000New York, NY: Cambridge University Press. [Google Scholar]
- 36.Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol. 2008;8:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Textor J, Hardt J, Knüppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22:745. [DOI] [PubMed] [Google Scholar]
- 38.Hillesund ER, Bere E, Haugen M, Øverby NC. Development of a new Nordic Diet score and its association with gestational weight gain and fetal growth—a study performed in the Norwegian Mother and Child Cohort Study (MoBa). Public Health Nutr. 2014;17:1909–1918.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beelen R, Hoek G, Vienneau D, et al. Development of NO2 and NOx land use regression models for estimating air pollution exposure in 36 study areas in Europe—The ESCAPE project. Atmospheric Environ. 2013;72:10–23.. [Google Scholar]
- 40.Eeftens M, Beelen R, de Hoogh K, et al. Development of land use regression models for PM(2.5), PM(2.5) absorbance, PM(10) and PM(coarse) in 20 European study areas; results of the ESCAPE project. Environ Sci Technol. 2012;46:11195–11205.. [DOI] [PubMed] [Google Scholar]
- 41.Vrijheid M, Slama R, Robinson O, et al. The human early-life exposome (HELIX): project rationale and design. Environ Health Perspect. 2014;122:535–544.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Royston P. marginscontplot: Plotting the marginal effects of continuous predictors. Stata J. 2013;13:510–527.. [Google Scholar]
- 43.Stata version 14.0. Texas: StataCorp. [Google Scholar]
- 44.Eberhardt JL. The influence of road traffic noise on sleep. J Sound Vibration. 1988;127:449–455.. [Google Scholar]
- 45.Gehring U, Gruzieva O, Agius RM, et al. Air pollution exposure and lung function in children: the ESCAPE project. Environ Health Perspect. 2013;121:1357–1364.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bolten MI, Wurmser H, Buske-Kirschbaum A, Papoušek M, Pirke KM, Hellhammer D. Cortisol levels in pregnancy as a psychobiological predictor for birth weight. Arch Womens Ment Health. 2011;14:33–41.. [DOI] [PubMed] [Google Scholar]
- 47.Minkel J, Moreta M, Muto J, et al. Sleep deprivation potentiates HPA axis stress reactivity in healthy adults. Health Psychol. 2014;33:1430–1434.. [DOI] [PubMed] [Google Scholar]
- 48.Pirrera S, De Valck E, Cluydts R. Nocturnal road traffic noise: a review on its assessment and consequences on sleep and health. Environ Int. 2010;36:492–498.. [DOI] [PubMed] [Google Scholar]
- 49.Hof MH, van Dijk AE, van Eijsden M, Vrijkotte TG, Zwinderman AH. Comparison of growth between native and immigrant infants between 0-3 years from the Dutch ABCD cohort. Ann Hum Biol. 2011;38:544–555.. [DOI] [PubMed] [Google Scholar]
- 50.Júlíusson PB, Roelants M, Nordal E, et al. Growth references for 0-19 year-old Norwegian children for length/height, weight, body mass index and head circumference. Ann Hum Biol. 2013;40:220–227.. [DOI] [PubMed] [Google Scholar]
- 51.Willers SM, Brunekreef B, Smit HA, et al. BMI development of normal weight and overweight children in the PIAMA study. PLoS One. 2012;7:e39517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Murasko JE. Associations between household income, height and BMI in contemporary US children: infancy through early childhood. Ann Hum Biol. 2014;41:488–496.. [DOI] [PubMed] [Google Scholar]
- 53.Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics. 2009;124:S23–S34.. [DOI] [PubMed] [Google Scholar]
- 54.Jensen ET, Daniels JL, Stürmer T, et al. Maternal hormonal contraceptive use and offspring overweight or obesity. Int J Obes (Lond). 2014;38:1275–1281.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Júlíusson PB, Roelants M, Hoppenbrouwers K, Hauspie R, Bjerknes R. Growth of Belgian and Norwegian children compared to the WHO growth standards: prevalence below -2 and above +2 SD and the effect of breastfeeding. Arch Dis Child. 2011;96:916–921.. [DOI] [PubMed] [Google Scholar]
- 56.Aasvang GM, Moum T, Engdahl B. Self-reported sleep disturbances due to railway noise: exposure-response relationships for nighttime equivalent and maximum noise levels. J Acoust Soc Am. 2008;124:257–268.. [DOI] [PubMed] [Google Scholar]
- 57.Høydal E. Innvandrerbegreper i statistikken: Vestlig og ikke-vestlig – ord som ble for store og gikk ut på dato. Samfunnsspeilet. 2008;4:66–69.. [Google Scholar]


