Abstract
INTRODUCTION:
Restless legs syndrome (RLS) is etiologically divided into primary and secondary syndromes. However, a comparative description of both types is lacking in the literature. We compared primary and secondary RLS with respect to demographic determinants, associated risk factors, and comorbidities.
METHODS:
Following a cross-sectional survey on the prevalence of RLS in a Saudi population, RLS cases were identified using the International RLS Study Group (IRLSSG) criteria. Cases were assessed with an interview-based questionnaire regarding baseline characteristics, risk factors, and comorbidities and with lower limb examinations and laboratory measurements. RLS severity was assessed using the IRLSSG Severity Rating Scale.
RESULTS:
In total, 78 patients with RLS, including 50 (64.1%) primary and 28 (35.9%) secondary cases, were examined. Of the primary cases, 35 (70%) were male; of the secondary cases, 25 (89.3%) were female (P < 0.001). Multivariate regression confirmed the association of male gender with primary RLS (odds ratio = 14.53, 95% confidence interval [2.9–75], P = 0.001). There were more dark- and black-skinned participants in the primary RLS group (38, 72%) than in the secondary group (15, 28%) (P = 0.042). Iron deficiency was observed in most (26, 92%) of the secondary cases. More severe symptoms were reported in secondary than in primary RLS cases (P < 0.05).
CONCLUSIONS:
Primary RLS is more common but less severe than secondary RLS. Male gender and ethnicity play significant roles in primary RLS, whereas female gender and iron deficiency may be the main risk factors associated with secondary RLS.
Keywords: Primary, restless legs syndrome, restless legs syndrome severity, secondary
In 1672, Sir Thomas Willis described a medical condition that caused restlessness and unpleasant sensations in the limbs, mostly during rest periods or before sleep.[1] However, it was not until three centuries later, in 1945, that Dr. Ekbom provided a detailed description of the disease currently known as restless legs syndrome (RLS) or Willis–Ekbom disease.[2] Similarly, the diagnostic criteria of RLS were not well established until 50 years later.[3]
RLS is a chronic sensorimotor neurological disorder affecting mostly the limbs, causing an unpleasant sensation that triggers an irresistible urge to move the affected limb, which provides temporary relief. RLS mostly occurs during rest and at sleep time and can severely affect quality of life by causing chronic insomnia, sleep deprivation, anxiety, depression,[4] decreased cognition,[5] and even cardiovascular disorders.[6]
RLS is classified based on its etiology as primary and secondary, but both types are similar in their clinical presentation.[7] The primary disease can be familial (25%–75% of cases)[8,9] and shows autosomal dominant or recessive inheritance, early onset, and slow progression. However, to date, the true etiology of the primary RLS remains unknown. In contrast, secondary cases of RLS develop as the result of a specific disease, factor, or drug. The prevalence of secondary cases depends on the prevalence of the underlying condition. These cases typically have late onset with fast progression and increasing severity over time. Some of the known secondary conditions include iron deficiency anemia, pregnancy, renal failure, and peripheral neuropathy.[10,11,12,13,14,15]
The overall prevalence of RLS in adults was estimated to be 8.4% of the Saudi general public.[16] However, an estimated 20%–50% of patients on dialysis were found to suffer from RLS symptoms.[17,18] Of the numerous epidemiological studies on RLS published locally and globally, most have focused on the prevalence of the cardinal symptoms of RLS and its variation among different geographical areas and sociodemographic variants. Published studies that have assessed and compared primary and secondary RLS with respect to its risk factors and comorbidities are scarce. The aim of this study is to compare primary with secondary RLS in terms of demographic determinants, associated risk factors, and comorbidities.
Methods
This study followed a cross-sectional survey on the prevalence of RLS in middle-aged people in the western region of Saudi Arabia.[16] The survey revealed that 224 (8.4%) of the 2682 participants suffered from RLS, with a 95% confidence interval (CI) from 7.35 to 9.45%.
The present study was conducted from September 2015 to November 2016 in the metropolitan city of Jeddah, Saudi Arabia. All RLS patients identified from the survey who were not lost to follow-up were contacted by phone and invited to participate. Signed informed consent form was obtained from the participants, who were then invited to the Sleep Problems Research Center at King Abdul Aziz University (KAU) Hospital for further assessment.
Patients with primary RLS were defined as those who met all five of the updated International RLS Study Group (IRLSSG) diagnostic criteria.[19] Patients with secondary RLS were defined as outlined for primary RLS patients but included at least one known comorbid condition known to cause RLS, such as iron deficiency, anemia, uremia, peripheral neuropathy, multiple sclerosis, spinal cord pathology, or medications.
Data collection
Six trained physicians (3 males and 3 females) interviewed all participants. Each interview session consisted of the following: (1) a study questionnaire consisting of questions on baseline sociodemographic factors (age, sex, racial background, education level, occupation, monthly income, marital status, consanguinity, and smoking habits), medical history, and medications; in addition, a screening section consisting of the IRLSSG diagnostic criteria,[19] the RLS Severity Rating Scale,[20,21,22] and the Epworth Sleepiness Scale for daytime sleepiness[23] was employed; (2) a physical examination that included weight, height, and body mass index (BMI) measurements in addition to a detailed lower limb examination for neurological, vascular, and musculoskeletal disorders; and (3) blood tests to determine complete blood count, electrolyte analysis, liver and renal function tests, bone profile, hemoglobin A1c measurement, thyroid function tests, an iron study, and Vitamin B12 assessment.
The original data collected divided BMI into 4 BMI categories – underweight, normal, overweight, and obese – but since the number of normal and underweight participants was very small, the data were analyzed based on BMI at risk for RLS cutoff categories: under and normal weight, BMI <25 = no risk for RLS; overweight or obese, BMI >25 at increased risk.[24,25]
The school employees who constituted the study population were classified according to their government jobs and required educational level into either teachers or service workers: the former required a university or postgraduate degree and the latter required a high school or lesser degree. The average monthly household income in Saudi Arabia, as reported by the general statistics authority in Saudi Arabia, was 10,723 SR in 2013 (the most recent update). The original data were categorized and collected as <5000, 5000–10,000, >10,000–20,000, and >20,000. However, since there were no participants in the <5000 or >20,000 categories, the participants were divided and analyzed as below or above average (below or above 10,000 SR).[26]
Data analysis
Data were entered manually and analyzed using Stata Version 13.0. Corp. 2013 (Stata Statistical Software: Release 13, Stata Corp. LP, College Station, TX, USA). All tests were two tailed, with a significance level (alpha) of <0.05, and a 95% CI was calculated for the estimated scores. Quantitative data are described as means and standard deviations. Qualitative data are summarized as frequency distributions and percentages. Bivariate analysis using Pearson's correlation, independent two sample t-test and Chi-square test. ANOVA was used to compare means of the severity scores.
Univariate and stepwise multivariate logistic regression models were utilized to detect risk factors that were independently associated with primary RLS. The entry level was P ≤ 0.1, and the removal level was P ≥ 0.101.
This study conforms to the ethical standards of the Helsinki Declaration.[27] Approval was obtained from the Research Ethics Committee at KAU Hospital. An invitation letter and an information sheet were provided to the participants, and written consent was obtained from all participants before participation in the study.
Results
Seventy-eight participants were included in this analysis. Fifty patients (64.1%) were diagnosed with primary RLS, and the remaining 28 participants (35.9%) were diagnosed with secondary RLS. The patients' flowchart is presented in Figure 1.
Figure 1.
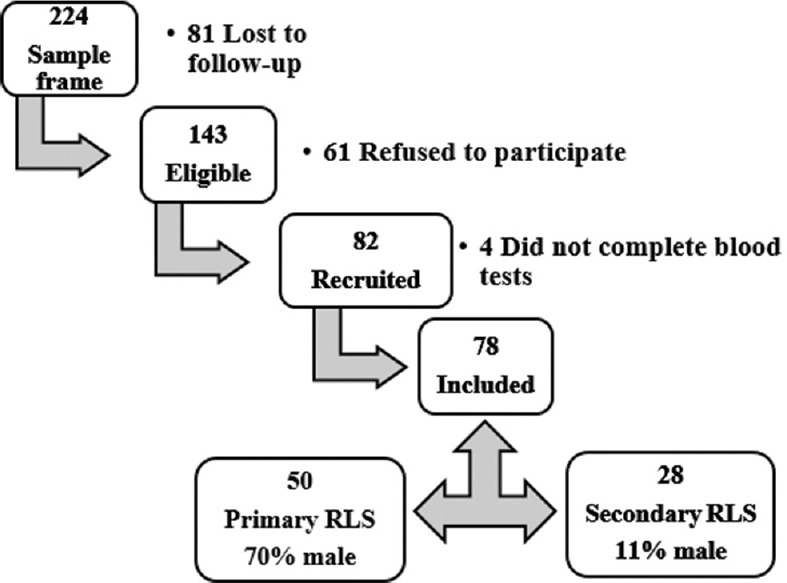
Descriptive flowchart of the restless legs syndrome cases
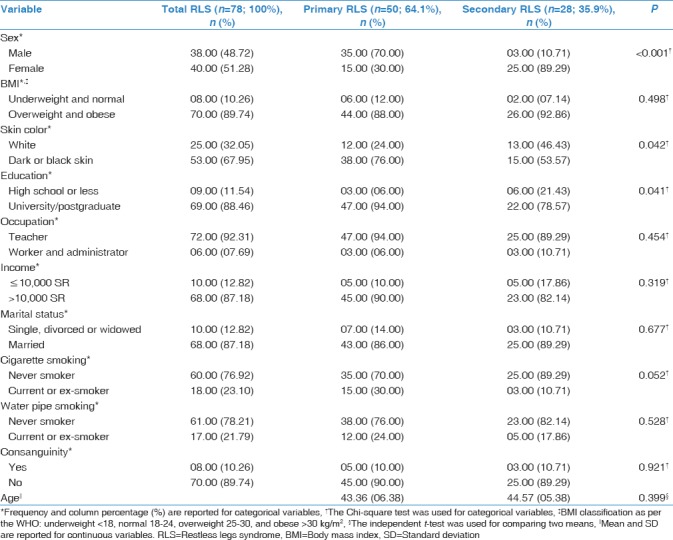
No significant differences were found between the primary and secondary cases in terms of mean age, BMI, water pipe smoking, consanguinity, occupation, income, or marital status. A significant difference in gender was noted. Most of the primary cases were males (35, 70%), and the secondary cases mainly consisted of females (25, 89.3%) (P < 0.001). The difference in skin color was also significant; more dark- and black-skinned participants were in the primary RLS group (38, 76%) than in the secondary group (15, 53.6%) (P = 0.042). University and postgraduate participants were represented more in the primary RLS group (47, 94%) than in the secondary group (22, 78.5%) (P = 0.041). History of cigarette smoking was not significantly different between the two groups (P = 0.052). However, more current and ex-smokers were noted in the primary RLS group (15, 30%) than in the secondary group (3.0, 10.7%) [Table 1].
Table 1.
Demographic characteristics of the restless legs syndrome cases
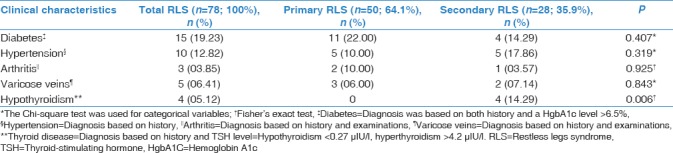
Based on the participants' medical history, there was no significant difference between the two groups regarding the incidence of diabetes, hypertension, arthritis, or varicose veins. However, four cases of hypothyroidism were present in the secondary RLS group, while no cases were found in the primary RLS group (P = 0.006). Table 2 presents the clinical characteristics of the RLS cases.
Table 2.
Comparison of clinical characteristics between the primary and secondary restless legs syndrome cases
The results of the univariate regression demonstrated that RLS was significantly associated with male gender (odds ratio [OR] =19.44, P < 0.001, 95% CI [5.1–74.4]) and dark/black skin color (OR = 2.74, 95% CI [1–7.35], P = 0.045). Multivariate regression confirmed the association of male gender with primary RLS after controlling for all other variables (OR = 14.53, 95% CI [2.9–75], P = 0.001).
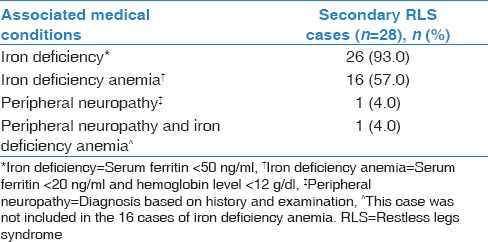
Among the secondary cases, iron deficiency defined as serum ferritin <50 ng/ml, iron deficiency anemia defined as serum ferritin <20 ng/ml, and hemoglobin level <12 g/dl were the two most common comorbid conditions associated with secondary RLS cases in our population. In addition, there were 2(4%) cases of peripheral neuropathy diagnosed based on history and physical examination. Table 3 lists the comorbid conditions in the secondary RLS cases in the study.
Table 3.
Comorbid conditions causing secondary restless legs syndrome in our study population
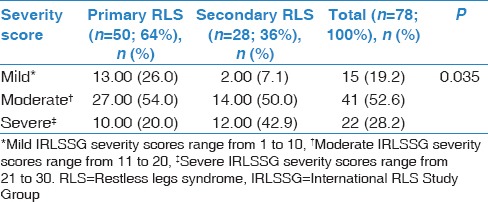
The mean symptom severity score was significantly different between the primary (15.42± [5.81]) and secondary groups (18.75± [5.43]) (P = 0.0153). Analysis of the severity score categories revealed milder symptoms in the primary RLS patients than in the secondary patients, 26% versus 7.1%, while 42.9% of secondary cases were severe compared to only 20% in the primary group. This difference was statistically significant [P = 0.035, Table 4].
Table 4.
Comparison of the mean severity score according to the International Restless Legs Syndrome Study Group criteria between primary and secondary restless legs syndrome cases
Fifteen (19.23%) patients with RLS had an Epworth score ≥9, including 10 (20%) primary and 5 (17.86%) secondary cases. No significant difference was observed in daytime sleepiness between the primary and the secondary RLS groups (P = 0.818).
Discussion
In this study, the numbers and percentages of primary RLS cases were approximately 2-fold greater than those of secondary RLS cases. Primary RLS patients were mostly male. In contrast, most secondary RLS patients were female. Male gender and racial background (represented by skin color) were the major risk factors for primary RLS. In contrast, the majority of secondary RLS cases were related to iron deficiency. No significant difference was observed in age, BMI, or other comorbidities between the two groups.
The primary and secondary RLS groups had similar mean ages (approximately 44 years). In general, epidemiological studies have reported that RLS may begin at any age, but most individuals suffering from RLS are over the age of 40 years.[28,29,30] The age of onset in relation to etiology has been examined in only two studies. Both studies reported a similar age of onset for idiopathic RLS of approximately 33–35 years.[31,32] However, the age of onset for secondary RLS was 47.4 ± 5.3 years in the second study.[32]
A significant gender distribution difference between primary and secondary RLS patients was observed. Most of the primary patients were male, in contrast to the secondary patients, who were mostly female. In addition, multivariate logistic regression confirmed the strong association between male gender and primary RLS, even after adjusting for all other demographic factors and comorbidities. Most studies on sex differences in relation to RLS were conducted on RLS cases in general. To our knowledge, the literature lacks any report on sex differences in relation to RLS case classifications. North American and European studies have reported approximately twice the prevalence of RLS in females compared to males,[33,34,35] whereas Asian and Middle Eastern countries have reported either an increased prevalence in males or no gender differences.[36,37,38] This diversity in the reported results may indicate that other genetic or environmental factors could potentially explain this gender difference. Indeed, some studies have reported that the different genders have different risk factors, according to subgroup analysis. Iron deficiency anemia and gastritis were the most frequent causes of RLS among females, whereas genetics, hypertension, and related neurological diseases were the main risk factors for RLS among men.[39,40,41] Our study findings support the above statement, as we found an increased prevalence of primary RLS cases in males, which is presumably related to genetic factors, based on our finding of a significant difference in skin color (ethnic background) between the primary and secondary RLS cases. Furthermore, we reported an almost exclusive prevalence of secondary RLS in females, which is related mainly to iron deficiency.
The significant difference observed between primary and secondary RLS cases in terms of racial background, as represented by skin color, showed that more RLS cases with dark and black skin color were represented in the primary group than in the secondary group. Unfortunately, previous studies on the association of race and ethnic background with RLS are rare. Three studies found contradictory results. One study reported no difference in RLS prevalence between Caucasian and African-Americans,[42] whereas two other studies confirmed differences in prevalence among different ethnic groups.[25,43]
We also identified a difference between the two groups in terms of smoking habits. The percentage of smokers was greater in the primary group than in the secondary group, but this difference did not reach statistical significance (P = 0.052). This finding is consistent with previously reported data, which have indicated that smoking is an independent risk factor for RLS.[24,44]
Clinically, no difference was observed between groups in terms of the following medical disorders: diabetes, hypertension, arthritis, and varicose veins. This is an interesting finding that supports previous reports regarding the true association between these diseases and secondary RLS. Studies strongly support that rather than the disease itself, the altered metabolic factors associated with these disorders, such as iron deficiency, anemia, uremia, peripheral neuropathy, and obesity, are the triggers for RLS in genetically susceptible patients.[45,46,47] This finding may explain why some patients with these disorders develop RLS, whereas the majority of patients do not, and may also explain why no difference between the primary and secondary cases was reported in this study.
Iron deficiency and related anemia was the most frequent cause of secondary RLS in our study. Secondary RLS patients were mainly female. The pathophysiology of RLS is not well understood, but a low serum iron level is considered the primary pathological factor related to its development.[14,48,49] Serum iron levels are lower in females than in males. Furthermore, the brain iron level is lower in adult females than in males,[50] which may explain the increased prevalence of secondary RLS in females with iron deficiency in our study. Clinically, a dose–response relationship was noted between iron level and RLS symptom severity, with improvement of symptoms after iron supplementation.[51] On the other hand, only two cases were found with peripheral neuropathy, which is a known cause for RLS.[45] Moreover, although all 4 patients with hypothyroidism in the study population were in the secondary RLS group, thyroid disorders are not well known as being associated with RLS.[45,52]
Regarding disease severity, our study demonstrated a significant increase in symptom severity in secondary cases compared to primary cases, and as most of the secondary patients had lower serum iron levels than primary patients, this increase may be related to their iron deficiency status.
Finally, only a fifth of the study population had excessive daytime sleepiness as measured by the Epworth scale, including 20% of the primary group and 18% of the secondary group. Fulda and Wetter[53] reported a similar percentage of daytime sleepiness in untreated primary RLS patients in a meta-analysis of all studies utilizing the Epworth scale. The percentage of daytime sleepiness among secondary RLS patients varies in the literature depending on underlying conditions, but the studies seem to agree on a lesser percentage in secondary cases than in primary RLS cases.[54,55] More studies are needed on this subject.
Conclusions
To the best of our knowledge, this is the first study to compare the demographic determinants, risk factors, and comorbidities of both primary and secondary RLS in the same setting. Male gender and ethnic background play a role in the pathogenesis of primary RLS, whereas iron deficiency may be the main risk factor for secondary RLS, especially in female patients. Future large-cohort studies comparing primary to secondary RLS cases are needed to confirm these observations.
Financial support and sponsorship
This study was funded by King Abdulaziz City for Science and Technology, Riyadh, Kingdom of Saudi Arabia; Grant Number: A-L-12-0867 and the Sleep Medicine and Research Center, King Abdulaziz University Hospital, Jeddah, Kingdom of Saudi Arabia.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to express our gratitude to Dr. Mohamed Hamed for collecting blood samples and to Mrs. Walaa Abuzahra for coordinating the data collection process and arranging the procedures.
References
- 1.Coccagna G, Vetrugno R, Lombardi C, Provini F. Restless legs syndrome: An historical note. Sleep Med. 2004;5:279–83. doi: 10.1016/j.sleep.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Ekbom KA. Restless legs: A clinical study. Acta Med Scand. 1945;158:1–123. [Google Scholar]
- 3.Walters AS. Toward a better definition of the restless legs syndrome. The international restless legs syndrome study group. Mov Disord. 1995;10:634–42. doi: 10.1002/mds.870100517. [DOI] [PubMed] [Google Scholar]
- 4.Sevim S, Dogu O, Kaleagasi H, Aral M, Metin O, Camdeviren H, et al. Correlation of anxiety and depression symptoms in patients with restless legs syndrome: A population based survey. J Neurol Neurosurg Psychiatry. 2004;75:226–30. [PMC free article] [PubMed] [Google Scholar]
- 5.Fulda S, Beitinger ME, Reppermund S, Winkelmann J, Wetter TC. Short-term attention and verbal fluency is decreased in restless legs syndrome patients. Mov Disord. 2010;25:2641–8. doi: 10.1002/mds.23353. [DOI] [PubMed] [Google Scholar]
- 6.Walters AS, Rye DB. Review of the relationship of restless legs syndrome and periodic limb movements in sleep to hypertension, heart disease, and stroke. Sleep. 2009;32:589–97. doi: 10.1093/sleep/32.5.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allen RP, Earley CJ. Restless legs syndrome: A review of clinical and pathophysiologic features. J Clin Neurophysiol. 2001;18:128–47. doi: 10.1097/00004691-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Xiong L, Montplaisir J, Desautels A, Barhdadi A, Turecki G, Levchenko A, et al. Family study of restless legs syndrome in Quebec, Canada: Clinical characterization of 671 familial cases. Arch Neurol. 2010;67:617–22. doi: 10.1001/archneurol.2010.67. [DOI] [PubMed] [Google Scholar]
- 9.Allen RP, La Buda MC, Becker P, Earley CJ. Family history study of the restless legs syndrome. Sleep Med. 2002;3(Suppl):S3–7. doi: 10.1016/s1389-9457(02)00140-5. [DOI] [PubMed] [Google Scholar]
- 10.Cesnik E, Casetta I, Turri M, Govoni V, Granieri E, Strambi LF, et al. Transient RLS during pregnancy is a risk factor for the chronic idiopathic form. Neurology. 2010;75:2117–20. doi: 10.1212/WNL.0b013e318200d779. [DOI] [PubMed] [Google Scholar]
- 11.Hattan E, Chalk C, Postuma RB. Is there a higher risk of restless legs syndrome in peripheral neuropathy? Neurology. 2009;72:955–60. doi: 10.1212/01.wnl.0000336341.72621.db. [DOI] [PubMed] [Google Scholar]
- 12.Takaki J, Nishi T, Nangaku M, Shimoyama H, Inada T, Matsuyama N, et al. Clinical and psychological aspects of restless legs syndrome in uremic patients on hemodialysis. Am J Kidney Dis. 2003;41:833–9. doi: 10.1016/s0272-6386(03)00031-3. [DOI] [PubMed] [Google Scholar]
- 13.Neau JP, Marion P, Mathis S, Julian A, Godeneche G, Larrieu D, et al. Restless legs syndrome and pregnancy: Follow-up of pregnant women before and after delivery. Eur Neurol. 2010;64:361–6. doi: 10.1159/000322124. [DOI] [PubMed] [Google Scholar]
- 14.O'Keeffe ST, Gavin K, Lavan JN. Iron status and restless legs syndrome in the elderly. Age Ageing. 1994;23:200–3. doi: 10.1093/ageing/23.3.200. [DOI] [PubMed] [Google Scholar]
- 15.O'Keeffe ST. Iron deficiency with normal ferritin levels in restless legs syndrome. Sleep Med. 2005;6:281–2. doi: 10.1016/j.sleep.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Wali SO, Abaalkhail B. Prevalence of restless legs syndrome and associated risk factors among middle-aged Saudi population. Ann Thorac Med. 2015;10:193–8. doi: 10.4103/1817-1737.160839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wali SO, Alkhouli AF. Restless legs syndrome among Saudi end-stage renal disease patients on hemodialysis. Saudi Med J. 2015;36:204–10. doi: 10.15537/smj.2015.2.10036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Jahdali HH, Al-Qadhi WA, Khogeer HA, Al-Hejaili FF, Al-Ghamdi SM, Al Sayyari AA, et al. Restless legs syndrome in patients on dialysis. Saudi J Kidney Dis Transpl. 2009;20:378–85. [PubMed] [Google Scholar]
- 19.Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, et al. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: Updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria – History, rationale, description, and significance. Sleep Med. 2014;15:860–73. doi: 10.1016/j.sleep.2014.03.025. [DOI] [PubMed] [Google Scholar]
- 20.Walters AS, LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP, et al. Validation of the international restless legs syndrome study group rating scale for restless legs syndrome. Sleep Med. 2003;4:121–32. doi: 10.1016/s1389-9457(02)00258-7. [DOI] [PubMed] [Google Scholar]
- 21.Abetz L, Arbuckle R, Allen RP, Garcia-Borreguero D, Hening W, Walters AS, et al. The reliability, validity and responsiveness of the international restless legs syndrome study group rating scale and subscales in a clinical-trial setting. Sleep Med. 2006;7:340–9. doi: 10.1016/j.sleep.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 22.Allen RP, Kushida CA, Atkinson MJ. RLS QoL Consortium. Factor analysis of the International Restless Legs Syndrome Study Group's scale for restless legs severity. Sleep Med. 2003;4:133–5. doi: 10.1016/s1389-9457(02)00193-4. [DOI] [PubMed] [Google Scholar]
- 23.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 24.Batool-Anwar S, Li Y, De Vito K, Malhotra A, Winkelman J, Gao X, et al. Lifestyle factors and risk of restless legs syndrome: Prospective cohort study. J Clin Sleep Med. 2016;12:187–94. doi: 10.5664/jcsm.5482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gao X, Schwarzschild MA, Wang H, Ascherio A. Obesity and restless legs syndrome in men and women. Neurology. 2009;72:1255–61. doi: 10.1212/01.wnl.0000345673.35676.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. [Last accessed 2017 Nov 17]. Available from: https://www.stats.gov.sa/sites/default/files/household_expenditure_and_income_survey_2013.pdf .
- 27.World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 28.Taşdemir M, Erdoǧan H, Börü UT, Dilaver E, Kumaş A. Epidemiology of restless legs syndrome in Turkish adults on the western black sea coast of Turkey: A door-to-door study in a rural area. Sleep Med. 2010;11:82–6. doi: 10.1016/j.sleep.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 29.Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res. 2002;53:547–54. doi: 10.1016/s0022-3999(02)00443-9. [DOI] [PubMed] [Google Scholar]
- 30.Rothdach AJ, Trenkwalder C, Haberstock J, Keil U, Berger K. Prevalence and risk factors of RLS in an elderly population: The MEMO study. Memory and morbidity in Augsburg elderly. Neurology. 2000;54:1064–8. doi: 10.1212/wnl.54.5.1064. [DOI] [PubMed] [Google Scholar]
- 31.Vogl FD, Pichler I, Adel S, Pinggera GK, Bracco S, De Grandi A, et al. Restless legs syndrome: Epidemiological and clinicogenetic study in a South Tyrolean population isolate. Mov Disord. 2006;21:1189–95. doi: 10.1002/mds.20922. [DOI] [PubMed] [Google Scholar]
- 32.Park YM, Lee HJ, Kang SG, Choi HS, Choi JE, Cho JH, et al. Prevalence of idiopathic and secondary restless legs syndrome in Korean women. Gen Hosp Psychiatry. 2010;32:164–8. doi: 10.1016/j.genhosppsych.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 33.Allen RP, Walters AS, Montplaisir J, Hening W, Myers A, Bell TJ, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165:1286–92. doi: 10.1001/archinte.165.11.1286. [DOI] [PubMed] [Google Scholar]
- 34.Tison F, Crochard A, Léger D, Bouée S, Lainey E, El Hasnaoui A, et al. Epidemiology of restless legs syndrome in French adults: A nationwide survey: The INSTANT study. Neurology. 2005;65:239–46. doi: 10.1212/01.wnl.0000168910.48309.4a. [DOI] [PubMed] [Google Scholar]
- 35.Bjorvatn B, Leissner L, Ulfberg J, Gyring J, Karlsborg M, Regeur L, et al. Prevalence, severity and risk factors of restless legs syndrome in the general adult population in two Scandinavian countries. Sleep Med. 2005;6:307–12. doi: 10.1016/j.sleep.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 36.BaHammam A, Al-shahrani K, Al-zahrani S, Al-shammari A, Al-amri N, Sharif M, et al. The prevalence of restless legs syndrome in adult Saudis attending primary health care. Gen Hosp Psychiatry. 2011;33:102–6. doi: 10.1016/j.genhosppsych.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 37.Rangarajan S, Rangarajan S, D'Souza GA. Restless legs syndrome in an Indian urban population. Sleep Med. 2007;9:88–93. doi: 10.1016/j.sleep.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 38.Chen NH, Chuang LP, Yang CT, Kushida CA, Hsu SC, Wang PC, et al. The prevalence of restless legs syndrome in Taiwanese adults. Psychiatry Clin Neurosci. 2010;64:170–8. doi: 10.1111/j.1440-1819.2010.02067.x. [DOI] [PubMed] [Google Scholar]
- 39.Berger K, Luedemann J, Trenkwalder C, John U, Kessler C. Sex and the risk of restless legs syndrome in the general population. Arch Intern Med. 2004;164:196–202. doi: 10.1001/archinte.164.2.196. [DOI] [PubMed] [Google Scholar]
- 40.Shi Y, Yu H, Ding D, Yu P, Wu D, Hong Z, et al. Prevalence and risk factors of restless legs syndrome among Chinese adults in a rural community of Shanghai in China. PLoS One. 2015;10:e0121215. doi: 10.1371/journal.pone.0121215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Erer S, Karli N, Zarifoglu M, Ozcakir A, Yildiz D. The prevalence and clinical features of restless legs syndrome: A door to door population study in Orhangazi, Bursa in Turkey. Neurol India. 2009;57:729–33. doi: 10.4103/0028-3886.59467. [DOI] [PubMed] [Google Scholar]
- 42.Lee HB, Hening WA, Allen RP, Earley CJ, Eaton WW, Lyketsos CG, et al. Race and restless legs syndrome symptoms in an adult community sample in east Baltimore. Sleep Med. 2006;7:642–5. doi: 10.1016/j.sleep.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 43.Castillo PR, Kaplan J, Lin SC, Fredrickson PA, Mahowald MW. Prevalence of restless legs syndrome among native South Americans residing in coastal and mountainous areas. Mayo Clin Proc. 2006;81:1345–7. doi: 10.4065/81.10.1345. [DOI] [PubMed] [Google Scholar]
- 44.Fereshtehnejad SM, Rahmani A, Shafieesabet M, Soori M, Delbari A, Motamed MR, et al. Prevalence and associated comorbidities of restless legs syndrome (RLS): Data from a large population-based door-to-door survey on 19176 adults in Tehran, Iran. PLoS One. 2017;12:e0172593. doi: 10.1371/journal.pone.0172593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Trenkwalder C, Allen R, Högl B, Paulus W, Winkelmann J. Restless legs syndrome associated with major diseases: A systematic review and new concept. Neurology. 2016;86:1336–43. doi: 10.1212/WNL.0000000000002542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Innes KE, Selfe TK, Agarwal P. Restless legs syndrome and conditions associated with metabolic dysregulation, sympathoadrenal dysfunction, and cardiovascular disease risk: A systematic review. Sleep Med Rev. 2012;16:309–39. doi: 10.1016/j.smrv.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 47.Szentkirályi A, Völzke H, Hoffmann W, Happe S, Berger K. A time sequence analysis of the relationship between cardiovascular risk factors, vascular diseases and restless legs syndrome in the general population. J Sleep Res. 2013;22:434–42. doi: 10.1111/jsr.12040. [DOI] [PubMed] [Google Scholar]
- 48.Rangarajan S, D'Souza GA. Restless legs syndrome in Indian patients having iron deficiency anemia in a tertiary care hospital. Sleep Med. 2007;8:247–51. doi: 10.1016/j.sleep.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 49.Earley CJ, Connor JR, Beard JL, Malecki EA, Epstein DK, Allen RP, et al. Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology. 2000;54:1698–700. doi: 10.1212/wnl.54.8.1698. [DOI] [PubMed] [Google Scholar]
- 50.Bartzokis G, Tishler TA, Lu PH, Villablanca P, Altshuler LL, Carter M, et al. Brain ferritin iron may influence age- and gender-related risks of neurodegeneration. Neurobiol Aging. 2007;28:414–23. doi: 10.1016/j.neurobiolaging.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 51.Davis BJ, Rajput A, Rajput ML, Aul EA, Eichhorn GR. A randomized, double-blind placebo-controlled trial of iron in restless legs syndrome. Eur Neurol. 2000;43:70–5. doi: 10.1159/000008138. [DOI] [PubMed] [Google Scholar]
- 52.Tan EK, Ho SC, Eng P, Loh LM, Koh L, Lum SY, et al. Restless legs symptoms in thyroid disorders. Parkinsonism Relat Disord. 2004;10:149–51. doi: 10.1016/j.parkreldis.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 53.Fulda S, Wetter TC. Is daytime sleepiness a neglected problem in patients with restless legs syndrome? Mov Disord. 2007;22(Suppl 18):S409–13. doi: 10.1002/mds.21511. [DOI] [PubMed] [Google Scholar]
- 54.Yildiz D, Kahvecioǧlu S, Buyukkoyuncu N, Kilic AK, Yildiz A, Gul CB, et al. Restless-legs syndrome and insomnia in hemodialysis patients. Ren Fail. 2016;38:194–7. doi: 10.3109/0886022X.2015.1111118. [DOI] [PubMed] [Google Scholar]
- 55.Moreira NC, Damasceno RS, Medeiros CA, Bruin PF, Teixeira CA, Horta WG, et al. Restless leg syndrome, sleep quality and fatigue in multiple sclerosis patients. Braz J Med Biol Res. 2008;41:932–7. doi: 10.1590/s0100-879x2008001000017. [DOI] [PubMed] [Google Scholar]


