Abstract
The advent of the online electronic health record patient portal has provided an efficient and practical means for patients to become more involved in their health care. In this report, we analyze how demographic variables such as age, gender, race, and geographic location affect patient portal activation and usage at the University of Iowa Hospitals and Clinics, the sole academic medical center in the state of Iowa, a predominantly rural state. Our primary end points were activation of the patient portal (MyChart, Epic, Inc) and access of outpatient laboratory and radiology results, among the most commonly accessed and popular features of the patient portal. We thus analyzed data from 536 378 patients to determine rates of patient portal activation and data from 219 671 patient encounters to determine the frequency at which patients access their online diagnostic test results. Higher rates of patient portal activation and usage were associated with female gender, Caucasians/non-underrepresented minorities, geographic location in closer proximity to the medical center (Iowa City and neighboring cities/suburbs), and nonelderly adults. For underrepresented minority and rural patients, opportunities for improvement exist for both activation and more robust use of online patient portal accounts. Overall, these data highlight existing disparities with online patient portal usage and provide a base on which further studies and interventions can help to improve utilization of these systems.
Keywords: health information technology, electronic health records, patient portals, personal health information, computers/utilization
Introduction
Electronic health records (EHRs) are common in industrialized countries and provide a way to store patient health information in a secure, efficient, and easily accessible manner.1,2 Online EHR portals (hereafter referred to as “patient portals”) are a tool for increasing patient engagement and high-value care.3 In the United States, EHR and patient portal use has become more prevalent in recent years in part due to the enactment of the HITECH (Health Information Technology for Economic and Clinical Health) Act, a program that seeks to improve the quality of health care in the United States by encouraging patient engagement in their health care through the concept of meaningful use.4-7 Financial incentives and penalties introduced by this program have led to EHR implementation in over 86% of US physician practices.6-9
Previous studies have shown that patients have a positive perception of participating in care via patient portals.10,11 Use of patient portals has been associated with improved care, decreased cost, and better patient–physician communication.12-17 Accessing of pathology results and radiology reports, in addition to other activities such as e-mail messaging or medication refills, are among the most popular features used within patient portals.18,19 Literature has also revealed that patient portal usage patterns differ depending on patient demographics. Patients who actively use patient portals tend to be Caucasian, younger, female, English speaking, and have fewer medical problems than nonusers.19-23 Underreported in the literature are findings describing patient portal usage patterns by race and patient geographic location (eg, rural vs urban; in a previous study, we examined broad trends in release and patient access of diagnostic test results).22 That study showed that outpatient test results were reviewed in the patient portal at much higher rates than inpatient or emergency department test results but did not examine race and patient geographic location as variables.
In this study, we analyzed patient portal activation and usage at the University of Iowa Hospitals and Clinics (UIHC). University of Iowa Hospitals and Clinics is the only academic medical center in the state of Iowa, a predominantly rural state. In addition to patient portal account activation, we focused on online access of outpatient laboratory and radiology results, a popular patient portal feature available to all UIHC patients.
Materials and Methods
Setting
University of Iowa Hospitals and Clinics is a 761-bed tertiary/quaternary care medical center that includes outpatient services, pediatric and adult inpatient units, multiple intensive care units, and an emergency department with level I trauma capability. University of Iowa Hospitals and Clinics draws in significant referrals, both in state and out of state (predominantly neighboring states such as Illinois), and is located in a predominantly rural state with few urban areas. University of Iowa Hospitals and Clinics implemented the Epic EHR in 2009 and adopted the associated patient portal (MyChart) in 2010.22,24 To set up a MyChart account, patients are typically provided with paperwork (often as part of after visit summary documents) with an activation code at clinical encounters that they can then use to activate their portal account. Since June 2016, patients can additionally request an activation code online to sign up for MyChart. Parents can activate and manage the MyChart accounts of their children 11 years and younger with full functionality. Parents have restricted proxy access (eg, limited functionality such as immunization records) of childrens’ portal accounts from ages 12 to 17 and lose proxy access completely when children reach the age of 18. There are policies allowing for proxy access for caretakers and legal guardians of adult dependent patients. Once the MyChart account is active, patients can schedule appointments, fill out medical history surveys, view test results, renew prescriptions, access visit summaries, and communicate with the health-care team.
Patients
The present study had institutional review board approval as a retrospective study with waiver of informed consent (protocol #201710835). A total of 536 378 patients who had medical care at UIHC facilities (outpatient clinics, emergency department, inpatient units) were included in the analysis of overall MyChart activation rates. Patient data were organized based on age, gender, race, distance from UIHC, and city size (metropolitan, micropolitan, or rural). Distance from UIHC and city size utilized the zip code of the patient’s primary address within the EHR. Metropolitan areas were defined as counties associated with cities that have a population of >50 000. The metropolitan areas in Iowa include Iowa City, Des Moines, Cedar Rapids, Waterloo, Sioux City, and their surrounding counties. Micropolitan areas are defined as cities with populations of 10 000 to 50 000; there are 17 micropolitan areas in the state of Iowa—Boone, Burlington, Carroll, Clinton, Fairfield, Fort Dodge, Fort Madison-Keokuk, Marshalltown, Mason City, Muscatine, Newton, Oskaloosa, Ottumwa, Pella, Spencer, Spirit Lake, and Storm Lake. Rural areas are defined as having less than 10 000 people in the town and surrounding area. Geographically, most of the state of Iowa falls into this rural category.25 The results from the geographic data analysis are presented in aggregate by type of area (metropolitan, micropolitan, and rural) and distance from UIHC main campus (<10 miles, 10-50 miles, 51-100 miles, >100 miles).
Patient encounters were also organized based on self-indicated patient race as recorded in the EHR. This was divided into 8 categories—white, African American, Hispanic/Latino, Asian, Native Hawaiian/Pacific Islander, American Indian/Alaska native, Multiracial, and unknown. Most patients in the retrospective cohort described below that had outpatient diagnostic tests performed indicated white (n = 77 789) as their race, followed by African American (n = 3803) and Asian (n = 2814).
There were 91 207 unique patients and 219 671 total outpatient diagnostic test encounters included in the analysis of result viewing rates. Outpatient diagnostic test results were chosen, since access of those results was a popular feature for UIHC MyChart. In contrast, in a previous study, we found that patient access of inpatient and emergency department results is generally very low (<10%) across age and gender breakdowns, making it difficult to compare across patient subgroups.22 The analysis on outpatient diagnostic tests only looked at diagnostic testing that originated from UIHC clinics in the Iowa City and surrounding region (Coralville, North Liberty, Riverside, Muscatine). Inpatient and emergency department results were not included in the analysis for the present study.
The MyChart system at UIHC allows patient access to pathology results and radiology reports.22 Authorized health-care providers who have ordered these tests have the option to manually release the results to MyChart, at which time the results cross immediately to the patient portal. Manual release is typically done by the ordering provider when reviewing laboratory results in the Epic InBasket by clicking a button labeled “Reviewed/Release to MyChart.” This workflow is common for outpatient providers. For results not manually released by the provider, diagnostic test results autorelease according to a specific schedule. Most chemistry and hematology tests will autorelease at 03:00 am on a business day following a full business day delay (eg, assuming no intervening holidays, a result finalized on Monday will autorelease on Wednesday or a result finalized on Friday will autorelease on Tuesday). Anatomic pathology and radiologic imaging reports autorelease following a delay of 4 full business days (meaning that autorelease occurs in approximately a week with intervening weekend days). Autorelease of microbiology results is either 1 or 4 business day delay, with sexually transmitted disease (eg, chlamydia and gonorrhea polymerase chain reaction [PCR]) testing typically being 4 business day delay. Human immunodeficiency virus screening and confirmatory results do not release to the patient portal.
Measures
This study involved 2 primary measures. The first primary outcome involved analyzing overall patient portal activation rates at UIHC. Patients considered “active” with respect to patient portals were those that registered their account online with their provided activation code. We did not distinguish between patient and proxy activation or access. Activation rates were then studied based on the previously described demographic variables.
The second category studied involved analysis of viewing patterns of outpatient diagnostic test results within MyChart. We included a selected group of pathology and radiology tests from the following 5 categories: Chemistry, Hematology, Imaging, Microbiology, and Anatomic Pathology. A breakdown of the specific tests are as follows: Chemistry (arterial blood gas, basic metabolic panel, hemoglobin A1c, lactic acid, lipid panel, thyroid-stimulating hormone, and 25-hydroxy vitamin D), Hematology (complete blood count, partial thromboplastin time, prothrombin time/international normalized ratio), Imaging (chest X-ray, computed tomography [CT] scan of brain, CT scan of chest), Microbiology (Chlamydia trachomatis PCR, Neisseria gonorrhoeae PCR, urine culture), and Anatomic Pathology (gynecologic and nongynecologic cytology, dermatopathology, surgical pathology). Diagnostic test results were studied based on the same demographic variables as the activation rates.
Data Source
Epic Reporting Workbench (RWB) was used to retrieve patient demographics, MyChart status, pathology results, and radiology reports covering dates from October 1, 2016, to October 1, 2017, using methods previously described.22,26,27 For the diagnostic test results, RWB captured whether patient had an active MyChart account and whether he/she (or a proxy) accessed outpatient diagnostic results. The RWB report included age, gender, MyChart status, zip code, patient location at order (inpatient, outpatient, or emergency department), and diagnostic test order. Zip codes were used to determine county of residency, state, city size, and distance from UIHC. Patients with an invalid or absent zip code (n = 199, 0.04% of total cohort) were not included in data analysis for geographic location.
Statistical Analysis
Analyses were performed using SPSS (PASW Statistics 18, Chicago, Illinois). To compare across groups, we used analysis of variance (for continuous variables) and χ2 tests (for categorical variables).
Results
Patient Portal Activation Rates: Influence of Age, Gender, Race, and Geographic Location
Overall, female patients were found to have a higher rate of patient portal account activation than their male counterparts (Figure 1A). Activation rate across all female patients was 39.9%, while males had an overall activation rate of 31.9%. When broken down by age, females had higher activation rates across nearly all age groups. The largest difference was in the 31- to 40-year-old age-group—females at 43.2% and males at 29.6% activation. Males and females were nearly equal in activation rates for children (less than 18 years) and for patients 71 years or older. The highest overall rates of activation (greater than 60%) were in children 11 years and younger, an age range where patient portal access would be solely by proxy access by parents or guardians.
Figure 1.
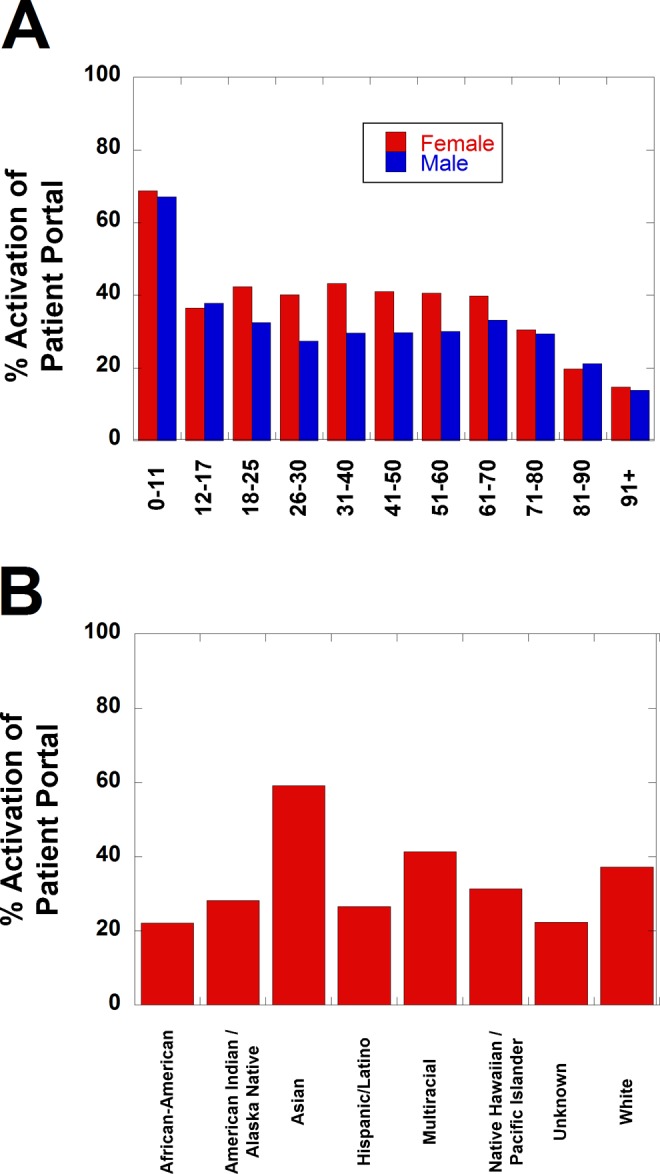
Patient portal activation rates by UIHC patients. A, Activation rates sorted by gender and subdivided into age distributions. Activation rates in patients 11 years and younger were significantly greater than other ages, while activation rates in patients 81 years and older were significantly lower than other ages (P < .001 for both groups, χ2 without Yates’ correction). Females showed significantly greater activation rates in all age distributions shown except 0 to 17 years and 81 years and older (P < .001). B, Activation rates sorted by self-declared patient race. Compared to the white population (the largest component of UIHC patients), African American, American Indian/Alaska Native, and Hispanic/Latino patients had significantly lower activation rates, while Asian patients had significantly higher rates (P < .001, χ2 without Yates’ correction). UIHC indicates University of Iowa Hospitals and Clinics.
Patient portal activation rates also varied considerably among different racial groups (Figure 1B). Asian patients had the highest account activation rates at 59.1%. African American patients had the lowest rate of portal activation at only 22%. White patients, which make up the majority of the patient population in Iowa, had an intermediate activation rate of 37.2%. Multiracial patients had slightly higher activation rates than white patients.
Geographic location of patient’s home address also had a significant impact on patient portal activation rates (Figure 2). Users living within 10 miles of UIHC had the highest activation rates overall at 51.4%, 15.1% higher than the overall patient portal activation rate of 36.3% (Figure 2A). Activation rates steadily declined the further patients live from UIHC. Patients living in metropolitan areas (40.5% activation) had higher activation rates than patients living in micropolitan and rural areas (Figure 2B). Patients living in micropolitan areas had very similar activation rates to those living in rural areas (29.6% and 30.9%, respectively). Low activation rates were seen throughout the western and southernmost parts of Iowa. These regions of the state are notably devoid of any metropolitan areas.
Figure 2.
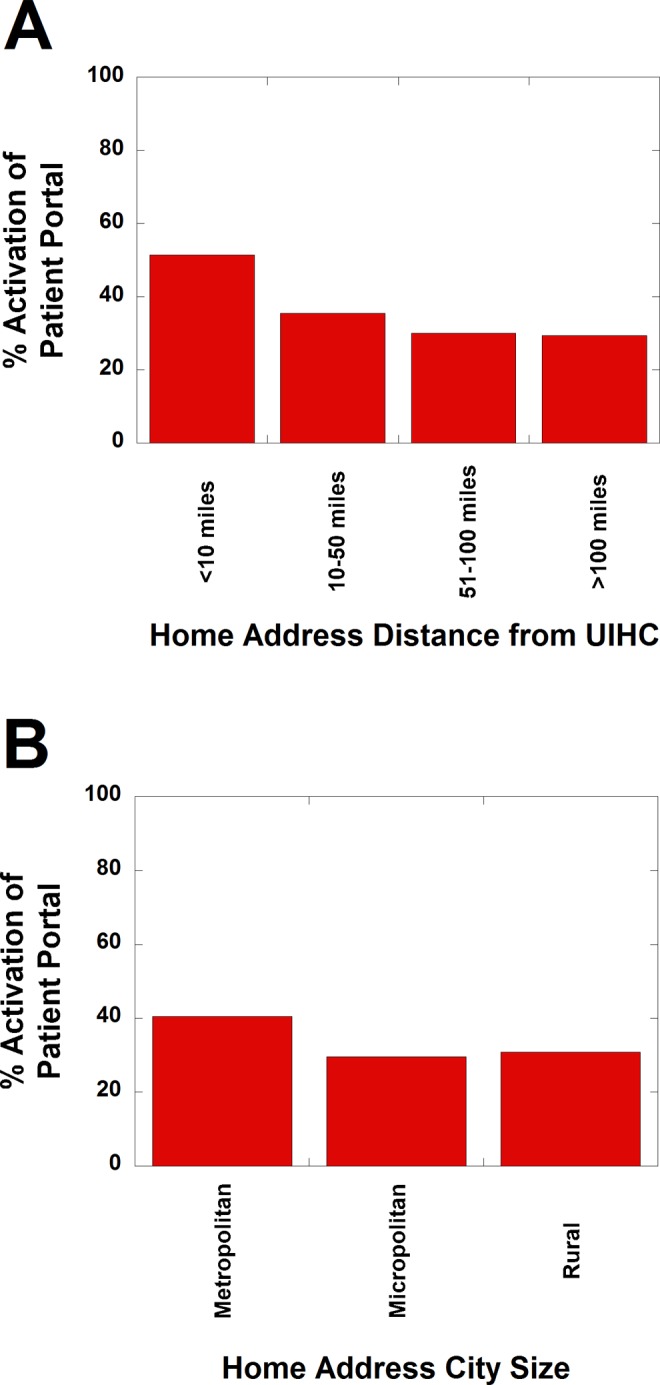
Patient portal activation rates by UIHC patients sorted by home address geographic location. A, Activation rates sorted by distance of patient’s home address from UIHC. Patients within 10 miles of UIHC have significantly higher activation rates than those farther away (P < .001, χ2 without Yates’ correction). B, Activation rates sorted by whether patient’s home address in metropolitan, micropolitan, or rural location. Patients in metropolitan regions have significantly higher activation rates than those in micropolitan or rural locations (P < .001, χ2 without Yates’ correction). UIHC indicates University of Iowa Hospitals and Clinics.
Utilization of the Patient Portal: Patient Access of Outpatient Diagnostic Test Results
Accessing of outpatient diagnostic test results requires both an active patient portal account and then the patient or proxy accessing the results once available in the patient portal. Overall, 39.5% of all outpatient diagnostic test results were viewed in the patient portal, and 44.4% of outpatients viewed at least 1 diagnostic test result. Figure 3A shows viewing of outpatient test results (divided into Anatomic Pathology, Chemistry, Hematology, Microbiology, and Radiologic imaging), showing both view rates among only those with active patient portal accounts (red bars; excluding those with inactive portal accounts) and overall view rates that also include results associated with patients with inactive patient portal accounts (blue bars). Outpatients with an active patient portal account viewed 69.3% of their test results overall regardless of demographics. The most commonly viewed test category among outpatients was Microbiology at 71.1%. Chemistry, Pathology, and Imaging tests were all viewed in the 60% to 70% range. The least viewed test category is Hematology, at 58.3%.
Figure 3.
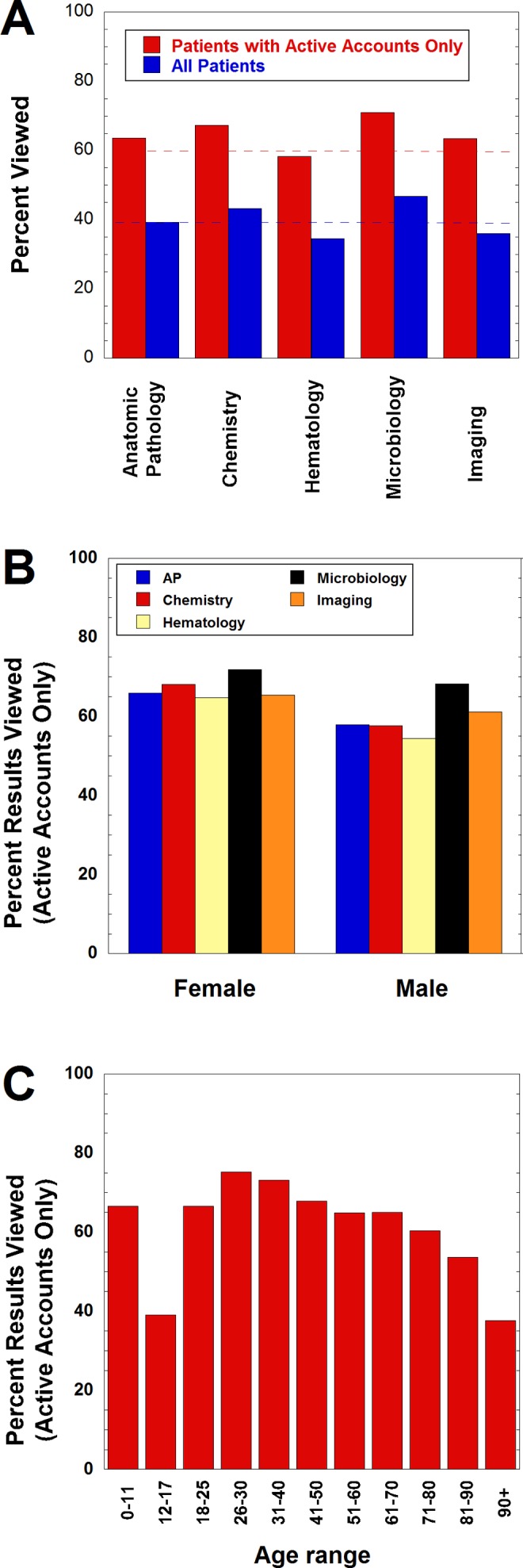
View rates of outpatient diagnostic tests sorted into Anatomic Pathology, Chemistry, Hematology, Microbiology, and Radiologic Imaging. A, Overall view rates of outpatient diagnostic tests showing view rates among only those with an active patient portal account (red bars; patients with inactive portal accounts excluded) and total including those without an active account (blue bars). The upper dashed line shows the overall average view rates of all tests for those with an active account. The lower dashed line shows the overall average view rate (including those with inactive portal accounts). B, View rates of outpatient diagnostic tests subdivided by gender and showing view rates among only those with an active patient portal account (patients with inactive portal accounts excluded). C, View rates of outpatient diagnostic tests among only those with an active patient portal account subdivided by age distribution (patients with inactive portal accounts excluded). Patients aged 12 to 17 years and 81 years and older had significantly lower view rates than other ages (P < .001).
Although females overall viewed outpatient diagnostic test results at rates higher than males, the difference between the 2 genders was less pronounced when looking at only those patients with active portal accounts (Figure 3B; contrast with activation data in Figure 1A). The most common test category viewed by females was Microbiology (71.8%), followed closely by Chemistry (71.4%). Microbiology was also the most commonly viewed category among males (68.2%), followed by Chemistry and Radiology, both at 61.1%. The largest difference among viewing patterns was among the Chemistry and Hematology categories; females viewed these labs 10% more frequently than males in both. The smallest gap was in the Microbiology category; females viewed microbiology results at only 3.6% more than their male counterparts.
Among those with active patient portal accounts, adults 26 to 40 years old showed the highest view rates of viewing outpatient diagnostic test results (Figure 3C). Above age 40, viewing patterns stay consistent until age 70, at which point they gradually start to taper downward. Young children (ages 0-11) had viewing rates comparable to the adult age groups. The one age category that was far less likely to view their test results is the 12- to 17-year-old age-group, with less than 40% of results viewed even among those with active patient portal accounts.
In regard to race, differences in outpatient test result viewing among those with active patient portal accounts (Figure 4A, red bars; patients with inactive portal accounts excluded) were less pronounced than the differences discussed earlier in patient portal activation rates (Figure 1B). In all categories, view rates exceeded 50% provided the patient had an active portal account. Asian outpatients were the most likely to view their test results at 76.2%; African Americans were the least likely at 53.8%. Figure 4A (blue bars) shows outpatient test view rates that includes both active and inactive patient portal users. The inclusion of inactive patient portal users drops overall view rates for African American and Hispanic patients to less than 30% and widens the differences between the races. Only the Asian population at UIHC (a group with the highest rate of active patient portal accounts; Figure 1B) exceeds 50% in overall viewing of outpatient test results even when inactive portal users are included.
Figure 4.
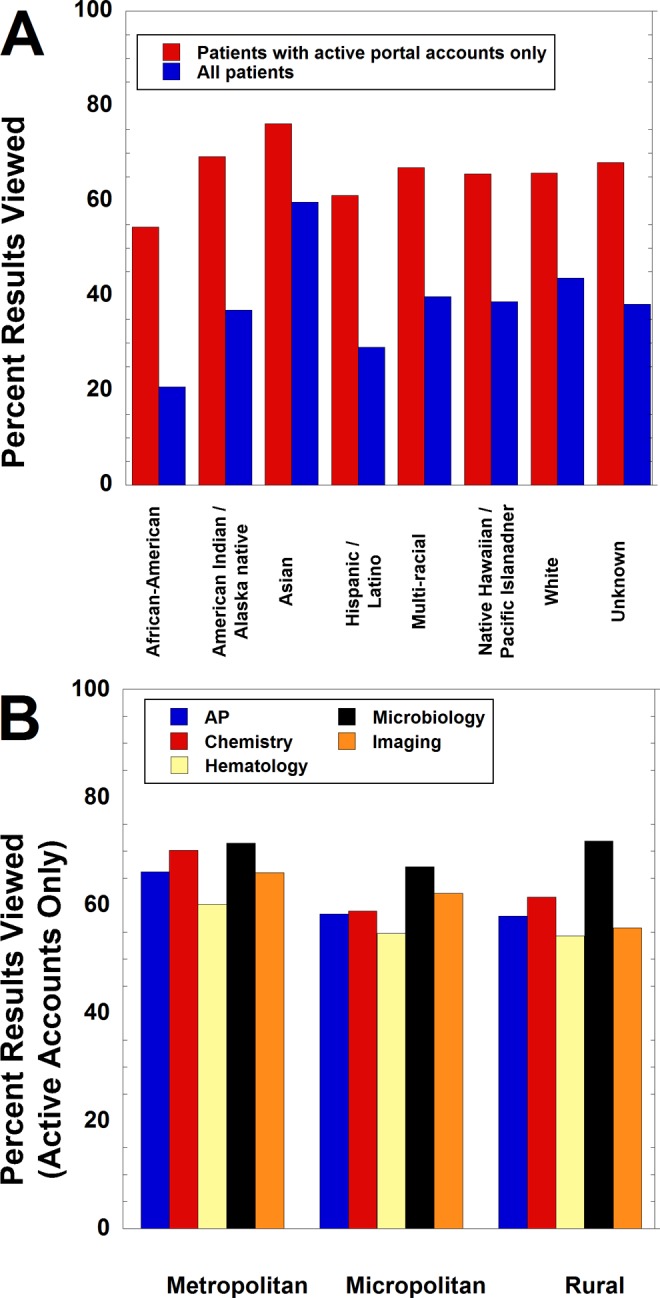
View rates of outpatient diagnostic tests sorted into race and geographic location of home address. A, View rates of outpatient diagnostic tests subdivided by self-declared patient race and showing view rates among those with an active patient portal account (red bars; patients with inactive portal accounts excluded) and total including those without an active account (blue bars). In both groups, compared to the white population (the largest component of UIHC patients), African American, American Indian/Alaska Native, and Hispanic/Latino patients had significantly lower view rates, while Asian patients had significantly higher rates (P < .001, χ2 without Yates’ correction). B, View rates of outpatient diagnostic tests subdivided by whether patient’s home address in metropolitan, micropolitan, or rural location and showing view rates among only those with an active patient portal account (patients with inactive portal accounts excluded). UIHC indicates University of Iowa Hospitals and Clinics.
Figure 4B shows outpatient test result view rates among those with active patient portal accounts subdivided by location of patient’s home address. Although users in metropolitan areas had slightly higher view rates than those in micropolitan or rural areas, this was less pronounced than the differences in patient portal activation rates discussed above (Figure 2C).
Figure 5 shows view rates of specific outpatient diagnostic tests among those with active patient portal accounts. Tests with higher view rates than the average for patient with active portal accounts include CT scans of the brain, thyroid-stimulating hormone with reflex to free thyroxine (T4), lipid panel, hemoglobin A1C, Pap test, chlamydia PCR, N gonorrhoeae PCR, and urine cultures. Interestingly, lactic acid and arterial blood gas analyses had very low view rates (<20%).
Figure 5.
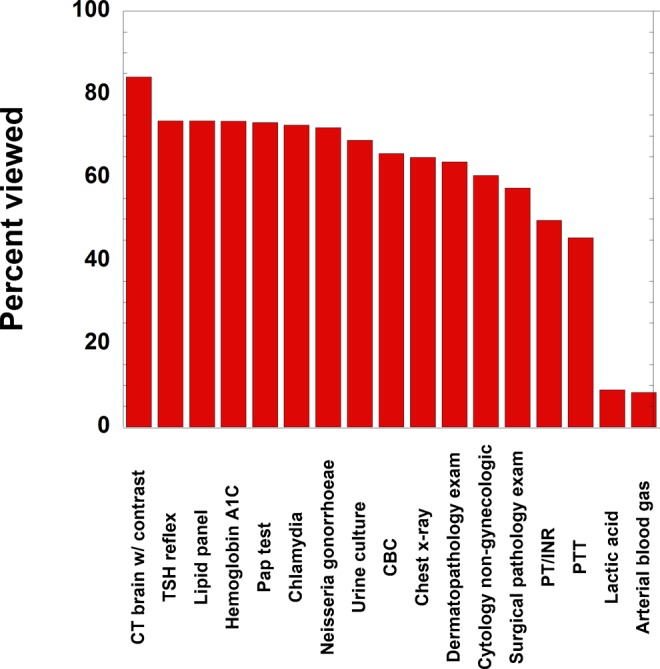
View rates of selected outpatient diagnostic tests. The tests on the left side of the plot are those that are higher than the overall average view rate. The right side of the plot has some tests with lower than average view rates.
Discussion
Previous studies have demonstrated that patients who actively use patient portals are more likely to be Caucasian, younger, female, English speaking, and have fewer medical problems than nonusers.19-23 Our findings also show that females were more likely than males to activate their patient portals across all but 2 age categories, with the largest differences existing between adults ages 18 to 70. Only among the 12- to 17-year-old and 71+ year groups did males have nearly equal or even slightly higher portal activation rates than females. Females were also more likely than males to view their outpatient diagnostic test results, although the percentage gaps were smaller overall with respect to diagnostic test viewing when looking at those with active patient portal accounts. One possible explanation for the higher activation rates among males in the 12- to 17- and 81- to 90-year-old age groups would be that these accounts may be activated by proxy users (ie, parents for children or caretakers of adult dependents) or with the assistance of partners, other relatives, or others. The literature on patient portal activation rates via proxy users and caretakers is limited, but one study has shown that low-income and elderly patients are more likely to access their online health portals if they have in-person assistance,28 and that patients who have better health literacy and higher self-reported ability to use the Internet are also more likely to use their online portals.29,30 The finding that females tend to participate in care via an online health portal more than males is consistent with some previously described literature,19,23 but other studies found no significant difference in portal use based on gender.30,31
Our data show that patients 71 years and older are less likely to utilize their patient health portals, which is also consistent with previously described literature.20,32 Portal activation and diagnostic test viewing rates remain relatively stable from 18 to 70 years old. Above 70 years old, there is decline in activation rates. This suggests that some older adults may encounter difficulties in activating their accounts, but once active, they tend to use them. One plausible explanation for this may be that online health portals select for older individuals who are more technologically literate, and therefore, those who are able to activate their accounts are also able to use them. It is also possible that the elderly population with active patient portal accounts are more likely to have help from a spouse, child, or some other caretaker. The existing literature contains sparse data on the extent to which relatives or other people help elderly patients with patient portal use. This is not something that our own institution has collected survey data on, although it is a future goal to probe these questions. The data in the present study do not contain information on the educational status of patients.
Trends among children and teenagers in our data set are somewhat variable. Children 11 years and older have the highest portal activation of all categories (much higher than adults) and also outpatient diagnostic test viewing rates comparable to adult age groups. Older children 12 to 17 years old have activation rates similar to the adult population, but their viewing of outpatient diagnostic test results is much lower. A probable explanation for some teenage patients is that parents may be activating these accounts through proxy access when the children were younger. Either way, teenagers are less likely than other age categories to utilize their active health portal accounts. It is unknown whether this is due to lack of health literacy, lack of interest, or both. It has been shown that many adolescents have problems with overall literacy—statistics from the The Nation’s Report Card show that only 36% of US fourth grade students and 34% of eight grade students read at or above a “proficient” level, but studies have not been conducted that measure adolescent health-care literacy specifically.33
Our study reinforces others studies that show patient portal activation and utilization are lowest among underrepresented minorities.34-36 In a previous study, we showed that patient portal access of diagnostic test data were much higher in outpatient versus inpatient or emergency department encounters.22 However, the present data show that subgroups are utilizing the functionality of accessing the patient portal for outpatient diagnostic tests results at lower rates, driven in large part by lower patient portal account activation rates. Interestingly, once patient portal accounts are activated, utilization of the portal in accessing outpatient tests results was much less divergent between races. This suggests that once minority patients with low activation rates (African American, Hispanic/Latino) activate their accounts, they are using the account functions with rates closer to that of the high-activation groups (Asian, Caucasian). Therefore, there may be some barrier to activation among minority groups that is preventing these groups from activating their accounts, but once active, they are engaged in using the patient portal. Previous studies have shown that patients with English-language barriers, patients with low incomes, and patients with lower education levels are less likely to utilize health-care portals,34-36 which could in part account for the low usage among these groups. It has even been reported that African Americans and Hispanics are less likely to be offered access to patient health portals compared to patients of other racial demographics.37 Other potential barriers to activation could be a lack of provided information, lack of health literacy, difference in socioeconomic status, and/or poor access to broadband Internet. However, although usage rates are higher among minorities once they activate their accounts, a gap still does exist among diagnostic test result viewing percentages based on patient race. So, it is a possibility that minority patients also encounter barriers to using their activated accounts for a more complex function such as accessing diagnostic test results.
Patients who live in metropolitan areas and patients who live in closer proximity to UIHC were more likely to both activate and use their patient portal accounts. Higher health portal account use seems to be related to distance within a 50-mile radius around the hospital. Patients living further than 50 miles from UIHC seem to have universally lower use rates, regardless of how far beyond the 50 miles they live. One possible explanation for this trend is that patients living within 50 miles of the hospital may be more likely to be regular patients at UIHC, and patients may be more motivated to use the health portal at their regular hospital. Additional factors may be differences in socioeconomic and educational status. Patients living further than 50 miles from UIHC may be more likely to be those who are attending appointments for one-time referrals and may therefore be less motivated to participate in the UIHC patient portal. Lack of reliable access to broadband Internet may also be a factor in rural areas.30,38,39 Research on the relationship between geographic location and patient portal use is limited and requires further investigation.
In a previous study, we showed that patient access of inpatient diagnostic test results via the patient portal was much lower than outpatient test results.22 One possible explanation for this finding is that inpatients may be less likely to have a regular primary care provider than their outpatient counterparts, and it has been previously described that patients without regular primary care are less likely to engage in an online health portal.35 Other explanations may be that inpatients may be less likely to receive routine medical care from UIHC and might have primary physicians who are outside the UIHC system—these patients may be engaging in non-UIHC patient portals. It is also possible that they are not engaging in an outside portal at all, but do not utilize the UIHC portal because their inpatient hospitalization at UIHC is a limited occurrence and setting up a patient portal would not provide much benefit to them once they leave. There are many possible explanations to this, but the question requires further study. The data in this study can guide marketing and other efforts to enhance activation and utilization of the patient portal across demographic groups, as is ongoing at our institution.
Conclusions
Overall activation rates within the UIHC patient portal were highest among women, patients of Asian, multiracial, and white ethnicity, young to middle-aged adults, patients who live in close proximity to Johnson county (where UIHC is located), and patients who live in other more populated areas in Iowa. Some of the groups with the lowest activation rates include African American patients, Hispanic/Latino patients, and teenagers. Our data suggest that activation of the patient portal account is a significant barrier in differences between subgroups of patients. Once patients have active accounts, they are more likely to use their patient portal, at least as it pertains to outpatient diagnostic test results. More research should be done to determine how to minimize these discrepancies in patient portal usage and increase access to underserved populations.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Matthew D. Krasowski, MD, PhD  http://orcid.org/0000-0003-0856-8402
http://orcid.org/0000-0003-0856-8402
References
- 1. Adler-Milstein J, Everson J, Lee SY. Sequencing of EHR adoption among US hospitals and the impact of meaningful use. J Am Med Inform Assoc. 2014;21:984–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Evans RS. Electronic health records: then, now, and in the future. Yearb Med Inform. 2016;20:S48–S61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pillemer F, Price RA, Paone S, et al. Direct release of test results to patients increases patient engagement and utilization of care. Plos One. 2016;11:e0154743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Agency for Healthcare Research and Quality. Guide to Patient and Family Engagement. 2014. https://www.ahrq.gov/research/findings/final-reports/ptfamilyscan/ptfamily1.html. Accessed July 24, 2018.
- 5. Kern LM, Edwards A, Kaushal R, Investigators H. The meaningful use of electronic health records and health care utilization. Am J Med Qual. 2016;31:301–307. [DOI] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. Meaningful Use. 2017. https://www.cdc.gov/ehrmeaningfuluse/introduction.html. Accessed July 24, 2018.
- 7. United States Department of Health and Human Services. HITECH Act Enforcement Interim Final Rule. 2017. https://www.hhs.gov/hipaa/for-professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.html. Accessed July 24, 2018.
- 8. Adler-Milstein J, DesRoches CM, Kralovec P, et al. Electronic health record adoption in US hospitals: progress continues, but challenges persist. Health Aff (Millwood). 2015;34:2174–2180. [DOI] [PubMed] [Google Scholar]
- 9. Centers for Disease Control and Prevention. Electronic Medical Records/Electronic Health Records (EMRs/EHRs). 2017. https://www.cdc.gov/nchs/fastats/electronic-medical-records.htm. Acccessed July 24, 2018.
- 10. Hassol A, Walker JM, Kidder D, et al. Patient experiences and attitudes about access to a patient electronic health care record and linked web messaging. J Am Med Inform Assoc. 2004;11:505–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sorondo B, Allen A, Bayleran J, et al. Using a patient portal to transmit patient reported health information into the electronic record: workflow implications and user experience. EGEMS (Wash DC). 2016;4:1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ammenwerth E, Schnell-Inderst P, Hoerbst A. The impact of electronic patient portals on patient care: a systematic review of controlled trials. J Med Internet Res. 2012;14:e162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Campanella P, Lovato E, Marone C, et al. The impact of electronic health records on healthcare quality: a systematic review and meta-analysis. Eur J Public Health. 2016;26:60–64. [DOI] [PubMed] [Google Scholar]
- 14. Herrin J, da Graca B, Nicewander D, et al. The effectiveness of implementing an electronic health record on diabetes care and outcomes. Health Serv Res. 2012;47:1522–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reed M, Huang J, Graetz I, et al. Outpatient electronic health records and the clinical care and outcomes of patients with diabetes mellitus. Ann Intern Med. 2012;157:482–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Reicher JJ, Reicher MA. Implementation of certified EHR, patient portal, and “direct” messaging technology in a radiology environment enhances communication of radiology results to both referring physicians and patients. J Digit Imaging. 2016;29:337–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sorondo B, Allen A, Fathima S, Bayleran J, Sabbagh I. Patient portal as a tool for enhancing patient experience and improving quality of care in primary care practices. EGEMS (Wash DC). 2016;4:1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Griffin A, Skinner A, Thornhill J, Weinberger M. Patient portals: who uses them? What features do they use? And do they reduce hospital readmissions? Appl Clin Inform. 2016;7:489–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Weingart SN, Rind D, Tofias Z, Sands DZ. Who uses the patient internet portal? The PatientSite Experience. J Am Med Inform Assoc. 2006;13:91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med. 2011;26:1112–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gordon NP, Hornbrook MC. Differences in access to and preferences for using patient portals and other ehealth technologies based on race, ethnicity, and age: a database and survey study of seniors in a large health plan. J Med Internet Res. 2016;18:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Krasowski MD, Grieme CV, Cassady B, et al. Variation in results release and patient portal access to diagnostic test results at an academic medical center. J Pathol Inform. 2017;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wallace LS, Angier H, Huguet N, et al. Patterns of electronic portal use among vulnerable patients in a nationwide practice-based research network: from the OCHIN practice-based research network (PBRN). J Am Board Fam Med. 2016;29:592–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Krasowski MD, Wilford JD, Howard W, et al. Implementation of epic beaker clinical pathology at an academic medical center. J Pathol Inform. 2016;7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. United States Office of Management and Budget. Share Data Center. Metropolitan, Micropolitan, and Combined Statistical Areas. 2018. www.iowadatacenter.org/aboutdata/statisticalareas. Accessed July 24, 2018.
- 26. Grieme CV, Voss DR, Davis SR, Krasowski MD. Impact of endogenous and exogenous interferences on clinical chemistry parameters measured on blood gas analyzers. Clin Lab. 2017;63:561–568. [DOI] [PubMed] [Google Scholar]
- 27. Krasowski MD, Chudzik D, Dolezal A, et al. Promoting improved utilization of laboratory testing through changes in an electronic medical record: experience at an academic medical center. BMC Med Inform Decis Mak. 2015;15:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kim EH, Stolyar A, Lober WB, et al. Challenges to using an electronic personal health record by a low-income elderly population. J Med Internet Res. 2009;11:e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Diviani N, van den Putte B, Giani S, van Weert JC. Low health literacy and evaluation of online health information: a systematic review of the literature. J Med Internet Res. 2015;17:e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Woods SS, Forsberg CW, Schwartz EC, et al. The association of patient factors, digital access, and online behavior on sustained patient portal use: a prospective cohort of enrolled users. J Med Internet Res. 2017;19:e345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Miller H, Vandenbosch B, Ivanov D, Black P. Determinants of personal health record use: a large population study at Cleveland Clinic. J Healthc Inf Manag. 2007;21:44–48. [PubMed] [Google Scholar]
- 32. Jhamb M, Cavanaugh KL, Bian A, et al. Disparities in electronic health record patient portal use in nephrology clinics. Clin J Am Soc Nephrol. 2015;10:2013–2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. The Nation’s Report Card. Mathematics & Reading Assessments. 2015. https://www.nationsreportcard.gov/reading_math_2015/#reading?%20grade=4. Accessed July 24, 2018.
- 34. Ancker JS, Hafeez B, Kaushal R. Socioeconomic disparities in adoption of personal health records over time. Am J Manag Care. 2016;22:539–540. [PMC free article] [PubMed] [Google Scholar]
- 35. Mook PJ, Trickey AW, Krakowski KE, et al. Exploration of portal activation by patients in a healthcare system. Comput Inform Nurs. 2018;36:18–26. [DOI] [PubMed] [Google Scholar]
- 36. Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18:318–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Peacock S, Reddy A, Leveille SG, et al. Patient portals and personal health information online: perception, access, and use by US adults. J Am Med Inform Assoc. 2017;24:e173–e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Luque AE, van Keken A, Winters P, Keefer MC, Sanders M, Fiscella K. Barriers and facilitators of online patient portals to personal health records among persons living with HIV: formative research. JMIR Res Protoc. 2013;2:e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Perzynski AT, Roach MJ, Shick S, et al. Patient portals and broadband internet inequality. J Am Med Inform Assoc. 2017;24:927–932. [DOI] [PMC free article] [PubMed] [Google Scholar]


