Abstract
CONTEXT:
Despite their important influence on child health, it is assumed that fathers are less likely than mothers to participate in pediatric obesity treatment and prevention research.
OBJECTIVE:
This review investigated the involvement of fathers in obesity treatment and prevention programs targeting children and adolescents (0–18 years).
DATA SOURCES:
A systematic review of English, peer-reviewed articles across 7 databases. Retrieved records included at least 1 search term from 2 groups: “participants” (eg, child*, parent*) and “outcomes": (eg, obes*, diet*).
STUDY SELECTION:
Randomized controlled trials (RCTs) assessing behavioral interventions to prevent or treat obesity in pediatric samples were eligible. Parents must have “actively participated” in the study.
DATA EXTRACTION:
Two authors independently extracted data using a predefined template.
RESULTS:
The search retrieved 213 eligible RCTs. Of the RCTs that limited participation to 1 parent only (n = 80), fathers represented only 6% of parents. In RCTs in which participation was open to both parents (n = 133), 92% did not report objective data on father involvement. No study characteristics moderated the level of father involvement, with fathers underrepresented across all study types. Only 4 studies (2%) suggested that a lack of fathers was a possible limitation. Two studies (1%) reported explicit attempts to increase father involvement.
LIMITATIONS:
The review was limited to RCTs published in English peer-reviewed journals over a 10-year period.
CONCLUSIONS:
Existing pediatric obesity treatment or prevention programs with parent involvement have not engaged fathers. Innovative strategies are needed to make participation more accessible and engaging for fathers.
Obesity is associated with numerous physical and psychological health consequences for children.1–3 Escalating childhood obesity rates remain a global public health concern.4 Poor lifestyle behaviors have greatly contributed to this issue, with few children and adolescents meeting diet and physical activity recommendations internationally.5–7 Childhood obesity also tracks throughout life.8 Compared with healthy-weight peers, overweight children are 4 times more likely to become obese adolescents,9 and overweight/obese adolescents are 5 to 7 times more likely to become overweight/obese adults.10,11 Although a plethora of studies have examined the efficacy of pediatric obesity treatment and prevention interventions, progress has been modest.12,13 Identifying innovative strategies to improve health outcomes for children and adolescents remains an international research priority.
Parents have a profound influence on their children’s weight status and lifestyle behaviors through their own behaviors, parenting practices, and role in shaping the food and physical activity environment at home.14–16 As such, identifying the most effective ways to engage parents in pediatric obesity treatment and prevention has become an important area of research. Although there is some evidence for the efficacy of family-based approaches,17,18 the optimal nature of parental involvement remains unclear.13,19 In particular, researchers have called for greater and more meaningful involvement of fathers,20–22 who are assumed to participate less often than mothers in research studies.
In general, most parenting interventions to date have targeted mothers because of the historical nature of mothers as the primary socialization agent.23,24 As such, the potential underrepresentation of fathers in childhood obesity treatment and prevention research would align with a general trend observed in other fields of research including pediatric psychology treatment,25 developmental psychopathology,26 and general parenting research.27,28 However, this paradigm has become outdated as a growing body of research has revealed that fathers have a profound and independent influence on their children’s health and development.29,30 Moreover, fathers appear to have a particularly important influence on key behaviors such as their children’s physical activity31–33 and dietary habits,34–36 which are intrinsically linked to child weight status. A longitudinal study of 3285 families identified that children with an obese father, but a healthy-weight mother, were 15 times more likely to be obese than children with healthy-weight parents.37 In contrast, having an obese mother but a healthy-weight father did not increase the risk of childhood obesity.37
These findings suggest that failing to include fathers in childhood obesity treatment and prevention efforts may have considerable consequences for intervention efficacy. Indeed, scholars have argued that implementing parenting programs without meaningful father engagement is akin to poor practice, leads to wasted resources, provides incomplete evaluation, and may undermine the duty of care that researchers and practitioners have to optimize child well-being.28 This practice also places disproportionate responsibility on mothers who already spend more hours on household and child-rearing tasks, even when they work outside the home.38 In response, the American Academy of Pediatrics recently published a clinical report highlighting the need to encourage and support father involvement in pediatric care through all stages of child development.39
Although it is generally accepted that mothers are much more likely than fathers to participate in childhood obesity prevention and treatment research,20–22 this problem has never been systematically investigated. As such, the scope of the imbalance remains unclear, and little is currently known about how best to engage fathers in future interventions.40 To address this evidence gap and encourage an informed discourse about the role of fathers in future studies, this review was conducted to investigate the following 4 research questions:
What is the involvement of fathers in pediatric obesity treatment and prevention programs when participation is limited to 1 parent per family?
What is the involvement of fathers when both parents can participate?
Are fathers more or less likely to participate in studies with certain characteristics (eg, diet versus exercise; obesity prevention versus treatment)?
How many studies explicitly attempted to increase the recruitment of fathers or identified a lack of fathers as a possible study limitation?
Methods
The conduct and reporting of this review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.41
Eligibility Criteria
Eligibility criteria were as follows:
Study was a randomized controlled trial (RCT).
Study explicitly targeted and reported outcomes for adiposity, physical activity, diet, and/or sedentary behavior in children aged 0 to 18 years.
Study promoted behavior change rather than solely examining the effect of weight loss or a prescribed diet or physical activity regimen on clinical biomarkers. Drug trials were not eligible.
At least 1 intervention arm included an “interactive” parent component (eg, family counseling sessions, parent-child home tasks, parent information nights). Studies in which parents were “passively” involved (eg, received newsletters or text messages) were not eligible. For the purposes of this review, the definition of parents also included primary caregivers (eg, stepparents).
Children were not a specifically targeted group with special medical conditions other than overweight/obesity (eg, mental illness, malnourishment).
Study was published in a peer-reviewed, English journal from January 2004 to January 2014.
Information Sources and Search
Studies were identified by searching the following 7 electronic databases with a standardized protocol: MEDLINE, Embase, PsycINFO, Cumulative Index to Nursing and Allied Health Literature (CINAHL), SCOPUS, ERIC, and SPORTDiscus. Search terms were divided into 2 groups: (1) “participants” (eg, child*, parent*, father*) and (2) “outcomes” (eg, obes*, diet). To maximize the sensitivity of the search, the Boolean phrase “AND” was used between groups, and the Boolean phrase “OR” was used within groups. Where possible, the following limits were applied: “English,” “human,” “RCT,” “peer reviewed.” For a summary of the search syntax, see Supplemental Table 3.
Study Selection
After duplicates were removed, 2 authors screened all retrieved citations based on title and abstract in a standardized, nonblinded manner. Full text articles were retrieved for remaining records, including those in which the abstract did not contain conclusive eligibility information. After this, 2 authors independently screened each article by using an “include,” “exclude,” or “unsure” approach. Disagreements were resolved through discussion, and full consensus was achieved. To ensure each included study represented an independent RCT, 1 author (M.D.Y.) reviewed all included studies for unique distinguishing characteristics (eg, number of children, number of parents, year conducted), particularly in relation to other studies conducted by the same investigator.
Development of Coding Criteria
The data extraction template was adapted from a manual used in a previous systematic review of male engagement in weight loss RCTs.42 After adapting and developing items to suit the current review objectives, the template was pilot tested by the study authors with a random selection of eligible articles. The authors then met to clarify ambiguous items. This process was repeated several times to improve agreement before the final template was set.
Data Extraction
For each article, 2 of 6 authors independently extracted the required data (A.B.L., M.L.W., A.M., N.E., E.M.M., A.T.B.). Each possible combination of coders received an equal share of articles. An additional author (M.D.Y.) resolved discrepancies with reference to the instruction manual and original article. Krippendorff’s α (k-α) was calculated to indicate interrater agreement, which is recommended for studies using ≥3 coders.43
Total Number of Parents
Where the data were available, coders recorded the total number of parents who were randomized into the study (k-α = .79).
Father Involvement
Where reported, the representation of fathers as a proportion of the total number of parents was also recorded (k-α = .79).
Study Aim
Coders recorded whether the study tested interventions for obesity treatment or prevention. If a study recruited overweight and obese children only, it was deemed to be obesity treatment. Studies without this eligibility criterion were classed as obesity prevention (k-α = .86).
Child Age Group
Studies were grouped based on the reported age range of the children: newborn/infant (0–1 year), toddler (2–4 years), child (5–9 years), preadolescent (10–12 years), and adolescent (13–18 years). If the child age range spanned 2 adjacent categories, the mean age of the sample was used for categorization. If the age range spanned >2 groups, the study was not categorized (k-α = .97).
Targeted Behaviors
Studies were classified into 3 groups based on the targeted behavior/s: (1) physical activity (including sedentary behavior), (2) diet, or (3) both physical activity and diet (k-α = .83).
Intervention Format
The primary “setting” and “delivery mode” of the parental intervention components were recorded. The categories for intervention setting were (1) school/community, (2) university/clinic, and (3) home. The categories for intervention mode were (1) face-to-face; multiple families, (2) face-to-face; 1 family, (3) face-to-face; multiple + single (ie, a mix of individual and group based sessions) and (4) distance (eg, phone consultations, online). k-α was slightly lower for these variables (setting: .65, mode: .64) due to inconsistent reporting across studies. However, because all discrepancies were resolved with a consistent approach by a single reviewer, these variables were deemed acceptable for inclusion in the analysis.
Additional Comments on Father Involvement
Coders recorded any references to explicit strategies used by the researchers to increase the involvement of fathers in the intervention. The coders also noted if the authors reported that a lack of fathers was a study limitation. Interrater reliability was not calculated for these qualitative items.
Data Analysis
Analyses were conducted by using SPSS version 22.0 (SPSS, Chicago, IL). Means for quantitative variables and percentages for categorical variables were calculated. Independent samples t tests and analyses of variance investigated whether any study factors were associated with father involvement. Because the RCT design precludes participants from choosing a particular intervention arm, studies that tested multiple interventions that differed on a particular characteristic (eg, physical activity versus diet) were removed from that particular analysis. Studies that explicitly excluded mothers or fathers from participation were not included.
Results
The search provided a total of 18 583 unique citations. After screening titles, 8765 abstracts were reviewed and the full texts of 803 articles were retrieved for further investigation (Fig 1). Initial interrater agreement for article inclusion was 83%, and discrepancies were discussed until consensus was reached. Overall, 212 articles reporting the results of 213 RCTs were deemed eligible for inclusion (see Supplemental Table 4 for a complete list of included studies).
FIGURE 1.
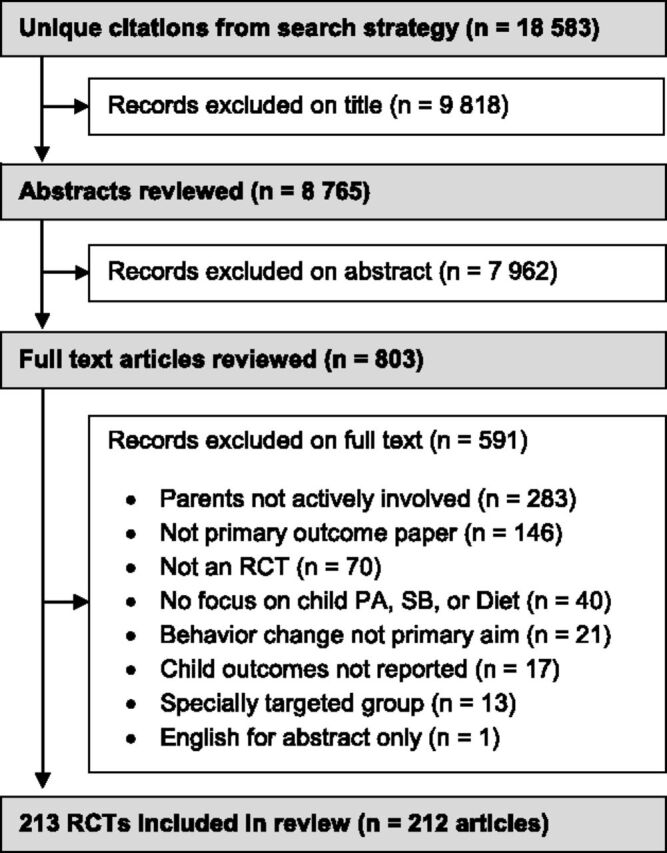
PRISMA flow diagram of article inclusion and exclusion. PA, physical activity; SB, sedentary behavior.
As seen in Table 1, most included studies were conducted in the United States (47%). A similar number of studies tested interventions aimed at obesity prevention (51%) and treatment (49%). The number of published RCTs steadily increased over time, from 15 (7%) in 2004–2005 to 73 (34%) in 2012–2013. Nineteen studies explicitly recruited mothers only (9%), and 1 recruited fathers only (0.5%). The most commonly targeted age group was “child” (5–9 years; 35%), and studies were more likely to target both physical activity and diet in combination (62%) rather than alone. The interactive parent components of the interventions were most often held in the school/community setting (27%), and the most common mode of delivery was face-to-face (multiple families) (43%). Of the 56 582 children that participated in the studies, 46% were boys, and 50% were girls (4% not reported).
TABLE 1.
Characteristics of Included Studies
| Characteristic | Studies, n | Study, % |
|---|---|---|
| Country | ||
| United States | 100 | 47 |
| Australia | 22 | 10 |
| United Kingdom | 13 | 6 |
| Othera | 78 | 37 |
| Year | ||
| 2012–2013 | 73 | 34 |
| 2010–2011 | 62 | 29 |
| 2008–2009 | 38 | 18 |
| 2006–2007 | 25 | 12 |
| 2004–2005 | 15 | 7 |
| Child age | ||
| Newborn/infant (0–1 y) | 12 | 6 |
| Toddler (2–4 y) | 26 | 12 |
| Child (5–9 y) | 75 | 35 |
| Preadolescent (10–12 y) | 42 | 20 |
| Adolescent (13–18 y) | 30 | 14 |
| Uncategorizedb | 28 | 13 |
| Parent type | ||
| Mothers only | 19 | 9 |
| Fathers only | 1 | 0 |
| Mothers and/or fathers | 193 | 91 |
| Targeted behavior(s) | ||
| Physical activity + diet | 133 | 62 |
| Diet only | 33 | 15 |
| Physical activity only | 26 | 12 |
| Uncategorizedc | 21 | 10 |
| Primary setting | ||
| Clinic/university | 56 | 26 |
| School/community | 58 | 27 |
| Home | 51 | 24 |
| Uncategorizedc | 19 | 9 |
| Not reported | 29 | 14 |
| Primary delivery mode | ||
| Face-to-face (multiple families) | 91 | 43 |
| Face-to-face (single family) | 38 | 18 |
| Face-to-face (single + multiple) | 12 | 6 |
| Distance (eg, phone, online) | 32 | 15 |
| Uncategorizedc | 36 | 17 |
| Not reported | 4 | 2 |
| Aim | ||
| Obesity prevention | 109 | 51 |
| Obesity treatment | 104 | 49 |
Israel (n = 7), Germany (n = 7), Iran (n = 6), Canada (n = 6), Mexico (n = 5), Norway (n = 4), Netherlands (n = 4), China (n = 4), Brazil (n = 4), Belgium (n = 4), Sweden (n = 3), New Zealand (n = 3), Finland (n = 3), Turkey (n = 2), Switzerland (n = 2), Portugal (n = 2), Italy (n = 2), Iceland (n = 2), Greece (n = 2), Spain (n = 1), Singapore (n = 1), Malaysia (n = 1), India (n = 1), France (n = 1), Chile (n = 1).
Child age range spanned multiple categories.
Study included >1 intervention arm that differed on this characteristic (eg, diet only versus physical activity only).
Research Question 1: What Is the Involvement of Fathers in Pediatric Obesity Treatment and Prevention Programs When Participation Is Limited to 1 Parent per Family?
Eighty RCTs tested interventions where participation was limited to 1 parent per family (eg, parent-child dyad studies). As seen in Table 2, the breakdown of participating parents by sex was initially available for 83% of these RCTs (n = 66), although this increased to 89% (n = 71) after the corresponding authors of 5 RCTs provided additional data on request. Of the available data, mothers represented the nominated parent/caregiver in 93% of families (n = 12 604), fathers in 6% of families (n = 871), and another family member (eg, stepparent, grandparent) in 1% of families (n = 84). The modal proportion of fathers per RCT was 0%.
TABLE 2.
Father Involvement in Child and Adolescent Obesity Treatment and Prevention RCTs
| One Parent per Familya (n = 80) | Open Parent Participationb (n = 133) | All studies (n = 213) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| RCTs providing objective father engagement data | ||||||
| Yes | 71 | 89 | 11 | 8 | 82 | 38 |
| No | 9 | 11 | 122 | 92 | 131 | 62 |
| Parental distribution (when reported) | ||||||
| Fathers | 871 | 6 | 622 | 32 | 1493 | 10 |
| Mothers | 12 604 | 93 | 1 277 | 65 | 13 881 | 89 |
| Other (eg, stepparent) | 84 | 1 | 73 | 4 | 157 | 1 |
| RCTs reporting specific attempts to engage fathers | ||||||
| Yes | 1 | 2 | 1 | 1 | 2 | 1 |
| No | 60 | 98 | 132 | 99 | 192 | 99 |
| N/Ac | 19 | — | 0 | — | 19 | — |
| RCTs noting lack of fathers as possible limitation | ||||||
| Yes | 3 | 4 | 1 | 1 | 4 | 2 |
| No | 76 | 96 | 127 | 99 | 203 | 98 |
| N/Ad | 1 | — | 5 | — | 6 | — |
Only 1 parent per family participated in the “active” parent component of intervention (eg, parent-child dyad programs).
Parent component of intervention open to ≥1 parents (eg, family sessions).
Study explicitly excluded fathers (not included in percentages).
Study included >40% fathers (not included in percentages).
Research Question 2: What Is the Involvement of Fathers When Both Parents Can Participate?
Overall, 133 RCTs tested interventions in which participation in the parental component was open to both parents (eg, family counseling, parent information night). These studies were much less likely to report father involvement; only 11 (8%) provided quantitative data. Where reported, fathers represented 32% of parents at baseline, although none of the studies indicated whether treatment attendance throughout the program varied by parent sex. Six additional studies (5%) explicitly stated that parent participation was predominantly limited to the mother but did not provide quantitative data.
Because the majority of these studies did not describe the nature of father involvement, the corresponding authors were also e-mailed for additional insights. If the authors had not collected any data on the issue, they were asked to estimate the proportion of participating fathers. Of the 122 authors e-mailed, 22 replied with estimates of father involvement ranging from 0% to 10% (n = 15), 10% to 20% (n = 3), 20% to 30% (n = 2), and 40% to 50% (n = 2). For the purposes of this review, these estimates were not considered objective engagement data and are included to provide additional insight only.
Research Question 3: Are Fathers More or Less Likely to Participate in Studies With Certain Characteristics?
The moderator analyses investigated whether fathers were more or less likely to participate in trials with different characteristics. Although 82 RCTs reported the breakdown of parent participation by sex, studies were only included if they allowed participation from both mothers and/or fathers. As such, 20 studies that explicitly excluded fathers (n = 19) or mothers (n = 1) were not included in the analysis. Five studies that recruited mothers only but did not explicitly exclude fathers from enrolling were included. As summarized in the following sections, father involvement was not significantly associated with any of the examined characteristics.
Intervention Aim
The proportion of fathers did not vary between studies testing interventions designed for obesity treatment (17%) or obesity prevention (13%; t60 = −1.0, P = .31).
Year
Father involvement did not vary significantly over time (F2,59 = 0.9, P = .43). To account for the escalating publication rate, studies were analyzed in 3 groups of approximately equal size. Fathers represented 19%, 14%, and 14% of participants in studies published from 2004 to 2008, 2009 to 2011, and 2012 to 2013, respectively.
USA Versus International
No association was detected between father participation in studies conducted in or outside the United States. US trials had a smaller mean proportion of fathers than international trials (13% vs 20%), but the difference was not significant (t24 = –1.5, P = .13).
Child Age Group
Child age did not have a significant influence on father involvement (F2,52 = 1.7, P = .20). However, all newborn/infant studies explicitly recruited mothers only so could not be included. Overall, toddler studies had the lowest proportion of fathers (10%), followed by preadolescent/adolescent studies (15%) and child studies (18%). The preadolescent and adolescent categories were merged as only 4 adolescent studies were eligible for the analysis.
Targeted Behavior(s)
Diet only studies had the lowest representation of fathers (9%), compared with those targeting physical activity only (17%) or physical activity plus diet (17%), although this difference was not significant (F3,58 = 1.8, P = .15).
Setting
Father participation did not vary by setting. The greatest participation of fathers (17%) was observed when the primary setting of the parental intervention component was in the school or community, compared with 12% in universities/clinics and 12% at home. However, the difference between settings was not significant (F2,43 = 0.9, P = .42).
Delivery Mode
No association was detected between father participation across the different delivery modes (F3,47 = 0.4, P = .74). Father participation was greatest when the parental intervention components were delivered in a group setting with other families (17%) or in a mix of group and individual family sessions (18%), compared with individual family sessions (12%) or distance-based delivery (eg, online; 15%).
Research Question 4: How Many Studies Explicitly Attempted to Increase the Recruitment of Fathers or Identified a Lack of Fathers as a Possible Study Limitation?
Across the 213 RCTs, 2 studies (1%) explicitly reported using strategies to specifically recruit or engage fathers. One of these was the only published RCT to target fathers and children exclusively.44 The second was a preschool nutrition intervention that included 1 module in which fathers cooked with their children.45 Only 4 studies (2%) suggested that a lack of father involvement was a possible study limitation or important area to address in future research.
Discussion
This was the first systematic review to quantify the involvement of fathers in pediatric obesity treatment and prevention programs with parental involvement. In studies that recruited only 1 parent per family, participation could be verified for only 871 fathers (6%), compared with 12 604 mothers (93%). In studies in which both parents could participate, 92% did not provide objective data on fathers, with most studies reporting only general “parent” involvement. No characteristics moderated the level of father involvement, with fathers underrepresented across all study types. Despite this, only 2% of studies suggested that a lack of fathers was a possible study limitation, and only 1% reported the use of explicit strategies to increase father involvement.
This review has confirmed that most obesity treatment or prevention programs for children have not engaged fathers. Because of the relative scarcity of father-focused studies in obesity-related literature, the reasons for this lack of father involvement are not well understood. In a review that considered published evidence, practitioner insights, and father focus groups, Bayley and colleagues suggested that key barriers to participation in general parenting programs included competing work commitments, reduced awareness of programs, and a general discomfort participating in mother-dominated groups.27 In general, fathers have also been reported to take a passive role in the management of their child’s weight and may be less likely than mothers to perceive their child’s weight as a problem.46
To the extent that fathers may not be as concerned about their child’s weight, researchers may need to make concerted efforts to recruit them in future studies. Despite the important role of socioculturally targeted recruitment,47 existing programs may not have appealed directly to fathers. Indeed, only 1% of studies in this review reported the use of specific strategies to increase father involvement. This is particularly important because fathers often assume the term “parent” is interchangeable with “mother” when viewing advertising material for parenting programs.27 Notably, explicitly targeting men has shown promise as a recruitment strategy in the adult obesity literature,48 where men also represent a minority of participants.42
The lack of fathers in pediatric obesity prevention and treatment programs creates a number of conceptual and practical limitations for the field. Although it is plausible that mother-focused interventions could indirectly affect fathers’ behavior, a recent obesity prevention intervention identified that targeting mothers exclusively did not generate any flow-on benefits for father obesity risk behaviors, suggesting more direct targeting is required.49 This is particularly important given that parenting practices from mothers and fathers may differentially affect child behavior.22,50 Reduced father participation also affects data collection and study evaluation. Research shows that 2 parents from the same household can provide different accounts of child behavior,50 with fathers providing more accurate estimates in some instances.51
Perhaps most important, evidence has highlighted the critical and independent role of fathers on their children’s physical activity and dietary behaviors. Compared with mothers, fathers are more likely to initiate and facilitate co–physical activity at home,33 spend a greater proportion of their time playing with their children,52 and engage in a type of play that is more physical, stimulating, and unpredictable.53 Indeed, the emotional bond between fathers and their children has been referred to as an “activation relationship” that develops primarily through physical play.54 Although not statistically significant, it is notable that studies targeting physical activity included almost twice the representation of fathers (17%) in this review, compared with those targeting diet only (9%). However, preliminary evidence suggests that fathers also play a key role in shaping their children’s dietary behavior. For example, strong associations have been observed between fathers and child intake of fruit and energy-dense, nutrient-poor foods,35,36 even after controlling for maternal diet.35 Furthermore, fathers’ use of fast-food restaurants and perceptions of dinner as an important family ritual have been linked to child fast-food consumption.34
This review did not identify any factors that were associated with greater participation of fathers. However, it should be noted that the moderator analysis may have been affected by the insufficient variation between studies, with fathers greatly underrepresented in almost all studies with reported data. Although the proportion of participating fathers appeared larger in studies when both parents could participate (32%), this estimate may have been inflated because only 8% of these studies provided data and none described whether session attendance varied between mothers and fathers during the intervention.
Of note, the rate of father participation in the research studies did not appear to markedly improve over time. This was an interesting finding given fathers are now more engaged with their children than ever before.39 Indeed, the average number of hours per week fathers spend on child care has tripled in the past 50 years.38 There was also a paucity of fathers in obesity prevention studies targeting newborns, infants, and toddlers. Indeed, of the 19 studies that explicitly excluded fathers, 15 targeted children from these age groups (79%). Given that physical activity and dietary behaviors can be established at a very young age55 and that fathers are critical for encouraging breastfeeding initiation and duration,56–58 early-life interventions would likely benefit from a more meaningful engagement of fathers.
Of concern, little evidence exists to suggest that the underrepresentation of fathers is considered an important evidence-gap or research priority within the field. Of the 213 RCTs in this review, only 4 (2%) explicitly reported that a lack of fathers was a limitation of the study. The silence on this issue is also evident in many recent reviews of family- and parent-based interventions targeting pediatric obesity prevention59–62 and treatment,63–65 which have failed to highlight the absence of fathers as an important area to address in future research. Notably, in a recent scientific summary of important research gaps relating to specifically parent-based interventions for childhood obesity treatment, the American Heart Association identified the need to increase the involvement of grandparents, siblings, and cousins in future efforts, but the issue of father involvement was not addressed.66 To meaningfully improve the involvement of fathers in future interventions, the issue must become a much more prominent consideration on the scientific agenda through explicit acknowledgment as well as intervention design considerations.
Currently, little research exists to illuminate which strategies are most important for recruiting fathers into behavioral pediatric interventions. Best practice insights from the broader literature on parenting interventions include using targeted advertising appealing to “fathers” rather than “parents”67 and providing flexibility in the location and timing of the program (eg, afternoon/evening rather than work hours).68 Importantly, programs should also be socioculturally relevant, targeting core values and preferences of fathers.47 Fathers report appreciating programs that allow them to spend quality time with their children, provide practical parenting tips, include opportunities for interaction with other fathers, recognize the unique contributions of fathers, provide opportunities for co–physical activity, and are delivered by credible facilitators.47,69
The search retrieved only 1 study that specifically targeted fathers. The Healthy Dads, Healthy Kids RCT from Australia was designed to treat overweight and obesity in fathers and prevent obesity in their children.44 Compared with a control group, the program significantly improved weight status, physical activity, and diet for both fathers and children,44,70 providing strong evidence for the utility of socioculturally relevant programs for fathers.
This review applied a comprehensive search strategy to 7 databases by using search term combinations that maximized sensitivity. For the 213 included RCTs, all data were extracted by at least 2 independent reviewers, and the conduct and reporting of the review adhered to the PRISMA guidelines. This review also had some limitations. Given the immense number of published studies, the review was limited to English-language RCTs published in peer-reviewed journals over a 10-year period. Consequently, the findings of this review may not be generalizable to non-English-speaking cultures. In addition, the review was unable to examine the moderating influence of family ethnicity on father involvement because of the insufficient reporting of this variable.
Conclusions
This systematic review highlighted several conceptual and methodological gaps in the literature stemming from the relative absence of fathers in pediatric obesity treatment and prevention studies that included parent involvement. Targeted recruitment strategies are required to increase the participation and engagement of fathers in future research. Studies that examine the differential impact of including fathers and mothers together, fathers only, and mothers only will also provide valuable insights into factors that may influence intervention efficacy. To advance the field, a much greater understanding of the role and presence of fathers in obesity treatment and prevention trials is required. To achieve this, researchers should strive to report more comprehensive data to highlight the involvement and engagement of fathers in their studies.
Supplementary Material
Glossary
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
randomized controlled trial
Footnotes
Dr Morgan conceptualized the review, developed the search criteria, determined manuscript eligibility, drafted the initial manuscript, and contributed to manuscript revisions; Dr Young conceptualized the review, developed the search criteria, determined manuscript eligibility, assisted in data extraction, conducted the statistical analysis, drafted the initial manuscript, and contributed to manuscript revisions; Dr Lloyd conceptualized the review, developed the search criteria, determined manuscript eligibility, assisted in data extraction, and contributed to manuscript revisions; Drs Wang, Eather, Miller, Murtagh, and Barnes determined manuscript eligibility, assisted in data extraction, and contributed to manuscript revisions; Dr Pagoto served as a senior advisor, assisted with the data extraction instrument design, and contributed to manuscript revisions; and all authors approved the final manuscript as submitted.
FUNDING: No external funding.
References
- 1.Harriger JA, Thompson JK. Psychological consequences of obesity: weight bias and body image in overweight and obese youth. Int Rev Psychiatry. 2012;24(3):247–253 [DOI] [PubMed] [Google Scholar]
- 2.Pulgarón ER. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clin Ther. 2013;35(1):A18–A32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harrist AW, Swindle TM, Hubbs-Tait L, Topham GL, Shriver LH, Page MC. The social and emotional lives of overweight, obese, and severely obese children. Child Dev. 2016;87(5):1564–1580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U; Lancet Physical Activity Series Working Group . Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257 [DOI] [PubMed] [Google Scholar]
- 6.Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. J Nutr. 2010;140(10):1832–1838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Australian Bureau of Statistics . National Health Survey: First Results, 2014–2015 (4364.0.55.001). Canberra, Australia: ABS; 2015 [Google Scholar]
- 8.Wright CM, Parker L, Lamont D, Craft AW. Implications of childhood obesity for adult health: findings from Thousand Families cohort study. BMJ. 2001;323(7324):1280–1284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(17):1660–1661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herman KM, Craig CL, Gauvin L, Katzmarzyk PT. Tracking of obesity and physical activity from childhood to adulthood: the Physical Activity Longitudinal Study. Int J Pediatr Obes. 2009;4(4):281–288 [DOI] [PubMed] [Google Scholar]
- 11.Hulens M, Beunen G, Claessens AL, et al. Trends in BMI among Belgian children, adolescents and adults from 1969 to 1996. Int J Obes Relat Metab Disord. 2001;25(3):395–399 [DOI] [PubMed] [Google Scholar]
- 12.Spruijt-Metz D. Etiology, treatment and prevention of obesity in childhood and adolescence: a decade in review. J Res Adolesc. 2011;21(1):129–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;(12):CD001871. [DOI] [PubMed] [Google Scholar]
- 14.Edwardson CL, Gorely T. Parental influences on different types and intensities of physical activity in youth: a systematic review. Psychol Sport Exerc. 2010;11:522–535 [Google Scholar]
- 15.Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr. 2005;24(2):83–92 [DOI] [PubMed] [Google Scholar]
- 16.Jalali MS, Sharafi-Avarzaman Z, Rahmandad H, Ammerman AS. Social influence in childhood obesity interventions: a systematic review. Obesity Rev. 2016;17(9):820–832 [DOI] [PubMed] [Google Scholar]
- 17.Sung-Chan P, Sung YW, Zhao X, Brownson RC. Family-based models for childhood-obesity intervention: a systematic review of randomized controlled trials. Obes Rev. 2013;14(4):265–278 [DOI] [PubMed] [Google Scholar]
- 18.Yavuz HM, van Ijzendoorn MH, Mesman J, van der Veek S. Interventions aimed at reducing obesity in early childhood: a meta-analysis of programs that involve parents. J Child Psychol Psychiatry. 2015;56(6):677–692 [DOI] [PubMed] [Google Scholar]
- 19.Gerards SMPL, Sleddens EFC, Dagnelie PC, de Vries NK, Kremers SPJ. Interventions addressing general parenting to prevent or treat childhood obesity. Int J Pediatr Obes. 2011;6(2-2):e28–e45 [DOI] [PubMed] [Google Scholar]
- 20.Sleddens EFC, Gerards SMPL, Thijs C, de Vries NK, Kremers SPJ. General parenting, childhood overweight and obesity-inducing behaviors: a review. Int J Pediatr Obes. 2011;6(2–2):e12–e27 [DOI] [PubMed] [Google Scholar]
- 21.Rodenburg G, Oenema A, Kremers SPJ, van de Mheen D. Clustering of diet- and activity-related parenting practices: cross-sectional findings of the INPACT study. Int J Behav Nutr Phys Act. 2013;10(36):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patrick H, Hennessy E, McSpadden K, Oh A. Parenting styles and practices in children’s obesogenic behaviors: scientific gaps and future research directions. Child Obes. 2013;9(suppl):S73–S86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lundahl BW, Tollefson D, Risser H, Lovejoy MC. A meta-analysis of father involvement in parent training. Res Soc Work Pract. 2008;18(2):97–106 [Google Scholar]
- 24.Lamb ME. The Role of the Father in Child Development. 4th ed. New York, NY: Wiley; 2004 [Google Scholar]
- 25.Phares V, Lopez E, Fields S, Kamboukos D, Duhig AM. Are fathers involved in pediatric psychology research and treatment? J Pediatr Psychol. 2005;30(8):631–643 [DOI] [PubMed] [Google Scholar]
- 26.Phares V, Fields S, Kamboukos D, Lopez E. Still looking for Poppa. Am Psychol. 2005;60(7):735–736 [DOI] [PubMed] [Google Scholar]
- 27.Bayley J, Wallace LM, Choudhry K. Fathers and parenting programmes: barriers and best practice. Community Pract. 2009;82(4):28–31 [PubMed] [Google Scholar]
- 28.Panter-Brick C, Burgess A, Eggerman M, McAllister F, Pruett K, Leckman JF. Practitioner review: engaging fathers—recommendations for a game change in parenting interventions based on a systematic review of the global evidence. J Child Psychol Psychiatry. 2014;55(11):1187–1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sarkadi A, Kristiansson R, Oberklaid F, Bremberg S. Fathers’ involvement and children’s developmental outcomes: a systematic review of longitudinal studies. Acta Paediatr. 2008;97(2):153–158 [DOI] [PubMed] [Google Scholar]
- 30.Allen S, Daly K. The Effects of Father Involvement: An Updated Research Summary of the Evidence Inventory. Guelph, Canada: University of Guelph; 2007 [Google Scholar]
- 31.Lloyd AB, Lubans DR, Plotnikoff RC, Morgan PJ. Paternal lifestyle-related parenting practices mediate changes in children’s dietary and physical activity behaviors: findings from the Healthy Dads, Healthy Kids community randomized controlled trial. J Phys Act Health. 2015;12(9):1327–1335 [DOI] [PubMed] [Google Scholar]
- 32.Lubans DR, Morgan PJ, Collins CE, Okely AD, Burrows T, Callister R. Mediators of weight loss in the “Healthy Dads, Healthy Kids” pilot study for overweight fathers. Int J Behav Nutr Phys Act. 2012;9(45):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zahra J, Sebire SJ, Jago R. “He’s probably more Mr. sport than me”—a qualitative exploration of mothers’ perceptions of fathers’ role in their children’s physical activity. BMC Pediatr. 2015;15:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McIntosh A, Kubena KS, Tolle G, et al. Determinants of children’s use of and time spent in fast-food and full-service restaurants. J Nutr Educ Behav. 2011;43(3):142–149 [DOI] [PubMed] [Google Scholar]
- 35.Walsh AD, Cameron AJ, Hesketh KD, Crawford D, Campbell KJ. Associations between dietary intakes of first-time fathers and their 20-month-old children are moderated by fathers’ BMI, education and age. Br J Nutr. 2015;114(6):988–994 [DOI] [PubMed] [Google Scholar]
- 36.Hall L, Collins CE, Morgan PJ, Burrows TL, Lubans DR, Callister R. Children’s intake of fruit and selected energy-dense nutrient-poor foods is associated with fathers’ intake. J Am Diet Assoc. 2011;111(7):1039–1044 [DOI] [PubMed] [Google Scholar]
- 37.Freeman E, Fletcher R, Collins CE, Morgan PJ, Burrows T, Callister R. Preventing and treating childhood obesity: time to target fathers. Int J Obes. 2012;36(1):12–15 [DOI] [PubMed] [Google Scholar]
- 38.Pew Research Center . Modern Parenthood: Roles of Moms and Dads Converge as They Balance Work and Family. Washington, DC: Pew Research Centre; 2013 [Google Scholar]
- 39.Yogman M, Garfield CF; Committee on Psychosocial Aspects of Child and Family Health, American Academy of Pediatrics . Fathers’ roles in the care and development of their children: the role of pediatricians. Pediatrics. 2016;138(1):e20161128. [DOI] [PubMed] [Google Scholar]
- 40.McLean N, Griffin S, Toney K, Hardeman W. Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. Int J Obes Relat Metab Disord. 2003;27(9):987–1005 [DOI] [PubMed] [Google Scholar]
- 41.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269, W64 [DOI] [PubMed] [Google Scholar]
- 42.Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity (Silver Spring). 2012;20(6):1234–1239 [DOI] [PubMed] [Google Scholar]
- 43.Hayes A, Krippendorff K. Answering the call for a standard reliability measure for coding data. Commun Methods Meas. 2007;1:77–89 [Google Scholar]
- 44.Morgan PJ, Lubans DR, Callister R, et al. The “Healthy Dads, Healthy Kids” randomized controlled trial: efficacy of a healthy lifestyle program for overweight fathers and their children. Int J Obes. 2011;35(3):436–447 [DOI] [PubMed] [Google Scholar]
- 45.De Bock F, Breitenstein L, Fischer JE. Positive impact of a pre-school-based nutritional intervention on children’s fruit and vegetable intake: results of a cluster-randomized trial. Public Health Nutr. 2012;15(3):466–475 [DOI] [PubMed] [Google Scholar]
- 46.Anti E, Laurent JS, Tompkins C. The health care provider’s experience with fathers of overweight and obese children: a qualitative analysis. J Pediatr Health Care. 2016;30(2):99–107 [DOI] [PubMed] [Google Scholar]
- 47.Morgan PJ, Young MD, Smith JJ, Lubans DR. Targeted health behavior interventions promoting physical activity: a conceptual model. Exerc Sport Sci Rev. 2016;44(2):71–80 [DOI] [PubMed] [Google Scholar]
- 48.Young MD, Morgan PJ, Plotnikoff RC, Callister R, Collins CE. Effectiveness of male-only weight loss and weight loss maintenance interventions: a systematic review with meta-analysis. Obes Rev. 2012;13(5):393–408 [DOI] [PubMed] [Google Scholar]
- 49.Walsh AD, Lioret S, Cameron AJ, et al. The effect of an early childhood obesity intervention on father’s obesity risk behaviors: the Melbourne InFANT Program. Int J Behav Nutr Phys Act. 2014;11:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lloyd AB, Lubans DR, Plotnikoff RC, Collins CE, Morgan PJ. Maternal and paternal parenting practices and their influence on children’s adiposity, screen-time, diet and physical activity. Appetite. 2014;79(1):149–157 [DOI] [PubMed] [Google Scholar]
- 51.Burrows TL, Truby H, Morgan PJ, Callister R, Davies PS, Collins CE. A comparison and validation of child versus parent reporting of children’s energy intake using food frequency questionnaires versus food records: who’s an accurate reporter? Clin Nutr. 2013;32(4):613–618 [DOI] [PubMed] [Google Scholar]
- 52.Craig L. Does father care mean fathers share? A comparison of how mothers and fathers in intact families spend time with children. Gend Soc. 2006;20(2):259–281 [Google Scholar]
- 53.Paquette D. Theorizing the father-child relationship:mechanisms and developmental outcomes. Hum Dev. 2004;47(4):193–219 [Google Scholar]
- 54.Paquette D, Dumont C. Is father-child rough-and-tumble play associated with attachment or activation relationships? Early Child Dev Care. 2013;183(6):760–773 [Google Scholar]
- 55.Campbell KJ, Hesketh KD. Strategies which aim to positively impact on weight, physical activity, diet and sedentary behaviours in children from zero to five years. A systematic review of the literature. Obes Rev. 2007;8(4):327–338 [DOI] [PubMed] [Google Scholar]
- 56.Hauck YL. Factors influencing mothers’ decision to breastfeed in public. Breastfeed Rev. 2004;12(1):15–23 [PubMed] [Google Scholar]
- 57.Scott JA, Binns CW, Oddy WH, Graham KI. Predictors of breastfeeding duration: evidence from a cohort study. Pediatrics. 2006;117(4). Available at: www.pediatrics.org/cgi/content/full/117/4/e646 [DOI] [PubMed] [Google Scholar]
- 58.Scott JA, Binns CW, Graham KI, Oddy WH. Temporal changes in the determinants of breastfeeding initiation. Birth. 2006;33(1):37–45 [DOI] [PubMed] [Google Scholar]
- 59.Brown HE, Atkin AJ, Panter J, Wong G, Chinapaw MJ, van Sluijs EM. Family-based interventions to increase physical activity in children: a systematic review, meta-analysis and realist synthesis. Obes Rev. 2016;17(4):345–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hingle MD, O’Connor TM, Dave JM, Baranowski T. Parental involvement in interventions to improve child dietary intake: a systematic review. Prev Med. 2010;51(2):103–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Marsh S, Foley LS, Wilks DC, Maddison R. Family-based interventions for reducing sedentary time in youth: a systematic review of randomized controlled trials. Obes Rev. 2014;15(2):117–133 [DOI] [PubMed] [Google Scholar]
- 62.van Sluijs EMF, Kriemler S, McMinn AM. The effect of community and family interventions on young people’s physical activity levels: a review of reviews and updated systematic review. Br J Sports Med. 2011;45(11):914–922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Appelhans BM, Moss OA, Cerwinske LA. Systematic review of paediatric weight management interventions delivered in the home setting. Obes Rev. 2016;17(10):977–988 [DOI] [PubMed] [Google Scholar]
- 64.Janicke DM, Steele RG, Gayes LA, et al. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. J Pediatr Psychol. 2014;39(8):809–825 [DOI] [PubMed] [Google Scholar]
- 65.Loveman E, Al-Khudairy L, Johnson RE, et al. Parent-only interventions for childhood overweight or obesity in children aged 5 to 11 years. Cochrane Database Syst Rev. 2015;12(12):CD012008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Faith MS, Van Horn L, Appel LJ, et al. ; American Heart Association Nutrition and Obesity Committees of the Council on Nutrition; Physical Activity and Metabolism; Council on Clinical Cardiology; Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention, and Council on the Kidney in Cardiovascular Disease . Evaluating parents and adult caregivers as “agents of change” for treating obese children: evidence for parent behavior change strategies and research gaps: a scientific statement from the American Heart Association. Circulation. 2012;125(9):1186–1207 [DOI] [PubMed] [Google Scholar]
- 67.Burgess A. Engaging Fathers in Their Children’s Learning: Tips for Practitioners. Abergavenny, United Kingdom: Fatherhood Institute; 2006 [Google Scholar]
- 68.Centre for Urban and Communtiy Research . Project and Literature Review on Fatherhood for North Leyton Sure Start. London, England: Goldsmiths, University of London; 2004 [Google Scholar]
- 69.Phares V, Fields S, Binitie I. Getting fathers involved in child-related therapy. Cognit Behav Pract. 2006;13(1):42–52 [Google Scholar]
- 70.Morgan PJ, Collins CE, Plotnikoff RC, et al. The “Healthy Dads, Healthy Kids” community randomized controlled trial: a community-based healthy lifestyle program for fathers and their children. Prev Med. 2014;61:90–99 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


