Abstract
Rationale: Navajo children living on the reservation have high rates of asthma prevalence and severity. Environmental influences may contribute to asthma on the Navajo Nation and are inadequately understood.
Objectives: We performed a comprehensive, integrative literature review to determine the environmental factors that may contribute to increased asthma prevalence and severity among Navajo children living on the reservation.
Methods: A systematic search was conducted in four databases regarding the environmental risk factors for asthma in Navajo children living on the reservation. Relevant studies between 1990 and 2017 were examined. Nonexperimental literature was also integrated into the review to describe the environmental injustices that have historically, disproportionately, and systematically affected the Navajo people, thus contributing to respiratory disparities among Navajo children.
Results: Eight studies met inclusion criteria for systematic review; however, limited research regarding environmental risk factors specific to asthma and Navajo children living on the reservation was identified. Our integrative review indicated both indoor and outdoor environmental risk factors commonly found on the Navajo reservation appear to be important determinants of asthma.
Conclusions: Future research should examine indoor and outdoor air pollution from wood-burning stoves and cook stoves, coal combustion, tobacco and traditional ceremonial smoke, diesel exhaust exposure from long bus rides, indoor allergens, ambient pollutants, and regional dusts. Comprehensive mitigation efforts created in partnership with the Navajo Nation are necessary to address less-recognized risk factors as well as the common risk factors known to contribute to increased childhood asthma prevalence and severity.
Keywords: Navajo, American Indian, Native American, asthma
Despite perceptions to the contrary, asthma rates are not lower in rural as compared with urban populations, and exposure to indoor and outdoor pollution not typical in urban environments may increase pediatric asthma prevalence and severity (1, 2). Approximately 13.0% of American Indian/Alaska Native children have asthma, as compared with 8.6% of children in the U.S. general population (3). Asthma morbidity also appears to be higher among American Indian/Alaska Native children, with 67.3% reporting an asthma attack in the past 12 months, as compared with 60.7% of the U.S. general population (3). In 2013, the Navajo Nation Epidemiology Center surveyed the Chinle Agency and found that 14.2% of respondents reported ever having been told by a health professional they had asthma, and 11.0% of respondents reported having a current asthma diagnosis (4). Health disparities for American Indian/Alaska Native children with asthma living on the reservation include poverty, limited access to specialty care, and environmental challenges, which include high levels of indoor and outdoor air pollution.
The Navajo reservation is located in the southwestern United States and spans a geographic area of more than 27,000 square miles (5). The reservation is positioned across six counties and three states and consists of multiple U.S. census blocks, which presents numerous challenges with epidemiological data collection and analysis (6). Tribal-specific data composed by the U.S. government are limited, and most data collected by the Navajo Nation are not publicly available to researchers. The Navajo Nation is the most populous of all Indian Nations, with more than 250,000 individuals; approximately 44% of the Navajo population are children younger than 19 years of age (n = 117,769) (5, 7). The southwest Indian Health Services region, which includes the Navajo Nation, reports the highest rates for asthma hospitalizations among the six Indian Health Services regions (10.0 per 10,000 population; range, 1.8–10.1 per 10,000 population) (8).
The physical environment on the Navajo reservation may disproportionately expose children to risk factors for increased childhood asthma prevalence and severity. Indoor use of wood-burning stoves is suspected to be common; otherwise, information about potential asthma-relevant environmental determinants remains sparse. In this review, we sought to integrate the known literature on indoor and outdoor air quality specific to the Navajo reservation and highlight the issues that impact these risks, while acknowledging the historic impact of environmental injustices that may influence increased pediatric asthma prevalence and severity among Navajo children living on the reservation.
Methods
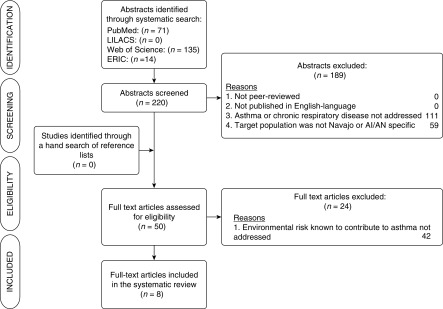
A protocol adapted from PRISMA (Preferred Reporting Items for Systemic Reviews and Meta-Analyses) guidelines (see Table E1 in the online supplement) was developed to systematically guide the abstract selection process. A comprehensive search was conducted in four databases (Table 1). Abstracts yielded by the search were scanned by both the primary author (A.A.L.) and senior author (L.B.G.). We selected articles for full review if they met the following inclusion criteria: 1) a peer-reviewed study, 2) published in the English-language, 3) the target population was the Navajo Nation or American Indian/Alaska Native (AI/AN), 4) content was specific to asthma or chronic respiratory illnesses, and 5) research addressed an indoor or outdoor environmental risk factor of asthma or respiratory disease. The primary reason articles were excluded from full review was that the content did not address an environmental risk factor of childhood asthma on the Navajo Nation or in an AI/AN population. A hand search was also conducted by reviewing the reference lists of articles as well as consultation with experts in the field. Figure 1 illustrates the abstract and full-text selection process of articles included in this review. The last search was completed on November 1, 2017. Where no peer-reviewed literature was found, we briefly discussed potential indoor and outdoor environmental risk factors as suggested by the non-AI/AN– and non-Navajo–specific literature.
Table 1.
Databases and full electronic search strategy for systematic search
| Database | No. of References | Full Electronic Search Strategy |
|---|---|---|
| PubMed (1966–present) | 71 | (“asthma”[Mesh:NoExp] or asthma[ti] or “respiratory illness”) AND (“indians, north american”[Mesh] OR “native americans”[tiab] OR “southwest”[tiab] OR “navajo”[tiab] OR “Navaho”[tiab] OR “dine”[tiab] OR “dineh”[tiab]) |
| Latin American and Caribbean Health Sciences database (LILACS) (1980–present) | 0 | American Native Continental Ancestry Group AND Asthma OR Respiratory Illness |
| Web of Science (1900–present) | 135 | TOPIC: (asthma OR respiratory illness) AND TOPIC: (native american OR native americans OR american indians OR navaho OR navajo OR dine OR dineh OR southwest) |
| Education Resources Information Center (ERIC) (1965–1998) | 14 | (navajo OR navaho OR diné OR dineh) AND (diesel OR bus OR buses OR busing OR pollution OR emissions OR asthma) |
Definition of abbreviations: ERIC = Education Resources Information Center; LILACS = Latin American and Caribbean Health Sciences database.
Figure 1.
Flow chart of systematic integrative review process. AI/AN = American Indian/Alaska Native; ERIC = Education Resources Information Center; LILACS = Latin American and Caribbean Health Sciences database.
Results
Out of 220 screened abstracts, only 8 articles met our inclusion criteria for review. Four articles were specific to the Navajo population, and four included all AI/AN (Table 2). Table 3 summarizes the environmental exposures (i.e., indoor and outdoor) suspected of affecting asthma development, severity, and exacerbation among children.
Table 2.
Peer-reviewed studies meeting inclusion criteria examining environmental risks and adverse respiratory outcomes in Navajo and American Indian/Alaska Native children
| Author(s) | Publication Date | Location | Methods | Environmental Concept | Specific to Navajo | Specific to AI/AN | Findings |
|---|---|---|---|---|---|---|---|
| Morris and colleagues (17) | 1990 | Conducted at the U.S. Public Health Service hospital clinic in Tuba City, AZ | Case–control study (n = 58); age- and sex-matched pairs ranging from ages 2 wk to 24 mo; cases = Navajo children with a diagnosis of bronchiolitis or pneumonia; control subjects = Navajo children who presented to the outpatient clinic for well-child care with no acute infectious disease | Wood stoves | X | Wood-burning stove use (OR, 4.2; 95% CI, 1.69–12.91) and respiratory illness exposure (OR, 3.7; 95% CI, 1.58–11.30) were associated with higher risk of lower respiratory tract infections | |
| Robin and colleagues (18) | 1996 | Conducted at the U.S. Public Health Service Indian Hospital in Fort Defiance, AZ | Case–control study (n = 45); age- and sex-matched pairs ranging from ages 1 to 24 mo; cases = Navajo children hospitalized with an acute lower respiratory illness; control subjects = Navajo children who had a health record at the same hospital and had never been hospitalized for an acute lower respiratory illness | Wood stoves; cook stoves | X | Increased risk of ALRI for children living in households that cooked with any wood (OR, 5.0; 95% CI, 0.6–42.8), had indoor air concentrations of respirable particles ≥ 65 μg/m3 (i.e., 90th percentile) (OR, 7.0; 95% CI, 0.9–56.9), and where the primary caretaker was other than the mother (OR, 9; 95% CI, 1.1–71.4) | |
| Bunnell and colleagues (16) | 2010 | Conducted on the Navajo reservation in the Shiprock, NM area | Household exposure risk analysis (n = 137), analysis of hospital records (n = 133,759 records over a 6-yr period); (n = 12 air samples from 2 field sites); assessment of fine particulate matter concentrations (n = 20 indoor samples) | Wood stoves; coal combustion; outdoor air pollution | X | 25% of stoves were not designed to burn coal; residents in the Shiprock area appear to be at greater risk for respiratory disease than nearby communities (annual asthma prevalence in Shiprock, NM = 16.762%); respiratory disease burden was increased in the winter compared with the summer, yet power plant emissions were greater in the summer than in the winter | |
| Ward and colleagues (20) | 2011 | Conducted on the Nez Perce Reservation in northern Idaho | Pre- and postassessment of a wood-stove changeout program for new, EPA-certified wood stoves in homes (n = 16); indoor air quality samples were analyzed from each home | Wood stoves | X | The wood stove changeout/exchange program resulted in 10 homes that had improved indoor air quality (reduction in PM2.5), 5 homes demonstrated unimproved or worsened PM2.5 values, and 1 home was lost to follow-up. 52% reduction in indoor PM2.5, and maximum spike values were reduced by 60% | |
| Noonan and colleagues (21) | 2012 | Conducted in Libby, MT | Pre- and postassessment wood-burning stove replacement program for EPA-certified wood burning stoves; n = 1,100; health impacts were measured using surveys from parents of school-aged children. Changes in air quality over 6 yr were measured using compliance air monitoring data from the Montana Department of Environmental Quality (n = 1 site) | Wood stoves; outdoor air pollution | X | Ambient PM2.5 was 27.6% lower in the winters after wood stove changeout; 27.6% reduced odds of reported wheeze for a 5-μg/m3 decrease in average winter PM2.5; lower ambient PM2.5 was associated with reduced odds for reported respiratory infections, including cold (25.4%), bronchitis (54.6%), influenza (52.3%), and throat infection (45.1%) | |
| Ward and colleagues (22) | 2015 | Conducted in 2 locations: Fairbanks, AK and rural western Montana | Three-armed randomized placebo-controlled trial with 2 household-level interventions: wood stove changeouts and air filtration units (n = 98 homes) | Wood stoves | X | No significant reductions in PM2.5 were observed in homes receiving the wood stove changeout. The air filtration strategy demonstrated a 69% reduction in indoor PM2.5 concentrations and 75% reduction in the particle count concentration | |
| Champion and colleagues (19) | 2017 | Conducted at the University of Colorado Emissions Standardization and Testing facility | Experimental design that used a standardized protocol to conduct controlled emission testing of 4 materials commonly burned in Navajo home stoves on the Navajo reservation: ponderosa pine, Utah juniper, Black Mesa (grade C) bituminous coal, and Fruitland (grades B & C) bituminous coal | Wood stoves; coal combustion | X | Coal produced much higher emissions as compared to wood, but the Black Mesa variety produced the highest mEF and eEF for PM2.5, organic carbon, and carbon monoxide. However, ponderosa pine had lower mEF PM2.5 (1.7 g/kg; SD, 0.7) than Utah juniper (3.1 g/kg; SD, 0.5), with approximately 50% lower PM2.5 emissions during the preburn phase. Ponderosa pine was recommended for wood stove use over Utah juniper or coal | |
| Reece and colleagues (29) | 1996 | Conducted at IHS Clinics | 545 randomly selected charts were reviewed from 22 IHS clinics for documentation of smoking history in patients | Tobacco smoke exposure | X | X | 73% of records did not document tobacco use status in patients; 9% documented a nonuser, and 18% documented a current user. Documentation varied by the area, ranging from no documentation in the Albuquerque, Navajo, and Phoenix areas to 51% in the Oklahoma area. |
Definition of abbreviations: AI/AN = American Indian/Alaska Native; ALRI = acute lower respiratory tract illness; CI = confidence interval; eEF = energy emission factors; EPA = U.S. Environmental Protection Agency; IHS = Indian Health Services; mEF = mass emission factors; OR = odds ratio; PM2.5 = particulate matter less than or equal to 2.5 μm in aerodynamic diameter; SD = standard deviation.
Table 3.
Environmental exposures suspected of affecting asthma development and severity/exacerbation in children on the Navajo reservation
| Indoor Exposures | Outdoor Exposures |
|---|---|
| Heating & cooking sources |
|
| Wood-burning stoves |
|
| Coal-burning stoves |
|
| Other material–burning stoves |
|
| Open fires | |
| Gas stoves: NO2* |
|
| Personal smoking |
|
| Commercial tobacco* | |
| Mountain tobacco | |
| Ceremonial | |
| Marijuana | |
| Allergens | |
| Dog/cat dander* | |
| Domestic birds* | |
| Cow and horse* | |
| Rodents* | |
| Other animals | |
| Cockroach* | |
| Other insects besides cockroach | |
| House dust mite* | |
| Fungi* | |
| Endotoxin* | |
| Dampness, mold* |
Definition of abbreviations: NOx = oxides of nitrogen; PM = particulate matter; SOx = oxides of sulfur.
Strong evidence that this exposure affects asthma development and/or severity/exacerbations.
Indoor Air Quality/Exposures
There is ample literature investigating the connection between indoor air pollution and poor respiratory health. Particulate matter (PM) less than or equal to 2.5 μm in aerodynamic diameter (PM2.5) and PM less than or equal to 10 μm in aerodynamic diameter (PM10) are associated with asthma severity and morbidity and acute lower respiratory infection (9, 10). Indoor pollution poses a great risk to children because of their increased respiratory rate, developing immune systems, and narrower airways (11).
Wood-burning stoves
Approximately 49% of homes lack electricity on the Navajo reservation, and 89% of Navajo families rely on biomass combustion as an economic and primary source of heat (6, 12). Prior research indicated that children residing in rural locations without access to clean fuels have higher mortality rates than children residing in rural locations with cleaner fuels (13), and exposure to indoor combustion sources increases the risk of asthma and asthma severity in children (14). Toxic pollutants including PM, carbon monoxide, oxides of nitrogen, and volatile organic carbons are present in wood smoke (15). In addition, wood-burning stoves are sometimes used to burn alternative materials for heat, which may increase the health-damaging effects of indoor air pollution. A survey conducted by Bunnell and colleagues found that 77% of Navajo homes (n = 137) used an indoor woodstove for heating, and 25% of homes burned coal in woodstoves not designed for higher combustion temperatures. Ninety-one percent of these stoves had visible cracks, fissures, holes, or insufficient ventilation, and 26% of these stoves were more than 10 years old (16).
Yet, there is limited research specific to Navajo children regarding indoor wood stoves and their impact on asthma, despite the large proportion of reservation families that rely on biomass combustion for domestic heat. Our systematic search revealed two studies specific to Navajo children that discussed woodstoves, indoor biomass combustion, and respiratory infections. Morris and colleagues investigated wood-burning stoves and lower respiratory tract infections in Navajo children 24 months of age or younger (17). Fifty-eight children with diagnosed pneumonia or bronchiolitis were matched with a control child of identical sex and age. Parents were interviewed about environmental exposures inside the home. The authors concluded that wood-burning stoves were independently associated with a higher risk of respiratory infections (odds ratio [OR], 4.2; P < 0.001) (17). Robin and colleagues subsequently examined acute lower respiratory tract illness in Navajo children (18). Children with acute lower respiratory tract illness were matched with control subjects who had a health record at the same hospital and had never been hospitalized for acute lower respiratory tract illness (n = 45). Findings suggested that wood-burning stoves were associated with an increased risk of acute lower respiratory tract illness (OR, 5.0; 95% confidence interval [CI], 0.6–42.8), but differences were not statistically significant (18).
Because wood stoves are commonly used on the Navajo reservation, investigating the efficacy and effectiveness of Environmental Protection Agency (EPA)-certified woodstoves is necessary. Recently, Champion and colleagues compared the emission factors (EF) of EPA-certified stoves using four of the most common solid fuel sources used by Navajo families (19). Ponderosa pine, Utah juniper, Black Mesa (grade C) bituminous coal, and Fruitland (grades B and C) bituminous coal were tested (19). Controlled emission testing was conducted to determine mass emission factors and energy emission factors. Coal produced much higher emissions than wood, but the Black Mesa variety produced the highest mass emission factors and energy emission factors for PM2.5, organic carbon, and carbon monoxide (19). However, ponderosa pine had the lowest mass emission factors and energy emission factors, with 50% lower PM2.5 emissions than Utah juniper during the preburn phase, and was recommended over Utah juniper or coal by the research team for wood stove use (19). These findings suggest that newer, EPA-certified stoves in combination with fuel sources such as Utah juniper may reduce exposure to harmful indoor pollutants that contribute to asthma development.
This review did not identify any studies that were specific to the Navajo reservation and the implementation of woodstove exchange programs; however, such programs have been evaluated in other AI/AN populations. Ward and colleagues evaluated the effectiveness of a wood stove exchange program on the Nez Perce Reservation (20). Indoor air samples (n = 16) were collected in homes at baseline and after intervention, and homeowners were asked to complete activity and wood-burning stove logs. After crude rates were compared, the data indicated a 36% reduction in mean indoor PM2.5 when older stoves were replaced with newer EPA-certified wood stoves. However, 10 homes demonstrated improved air quality and 6 homes demonstrated reduced air quality after intervention (20). The authors explained that reduced air quality in these six homes most likely resulted from poor burning practices, such as drying wood on top of the stove, burning wet wood in the stove, or burning incense, thus outlining the importance of incorporating culturally appropriate education with stove exchange programs (20).
Noonan and colleagues also examined the impact of a community-wide woodstove replacement program in 1,110 homes near Libby, Montana (21). Ambient air quality and parent-reported childhood respiratory symptoms were prospectively measured. The woodstove exchange program resulted in a 27% reduction in outdoor ambient PM2.5 during the winter months and a reduced odds of parent-reported wheeze in children (OR, 0.73; 95% CI, 0.55–0.97) (21). A third study conducted by Ward and colleagues used a three-armed randomized, placebo-controlled trial to examine the effectiveness of household-level interventions for improving indoor air quality (22). Ninety-eight homes with wood-burning stoves were randomized into one of three treatment groups: 1) wood stove replacement, 2) active air filtration unit, or 3) placebo air filtration unit. Indoor PM2.5 was prospectively measure over two consecutive winters. Findings suggested that the air filtration strategy demonstrated the greatest reduction in PM2.5 (69% reduction) inside homes (22).
Indoor cooking
Although no research specific to the Navajo reservation was identified that investigated exposure to domestic pollution from cook stoves, given the limited availability of electricity on the Navajo reservation, it is suspected that many Navajo families rely on indoor wood stoves and open fires for cooking, especially during the winter. A meta-analysis of 25 studies found a significant association between indoor biomass exposure and acute respiratory infection in children (OR, 3.53; 95% CI, 1.94–6.43) (23), suggesting that indoor cook stoves disproportionately expose women and children to harmful pollutants because of their traditional roles of cooking in the home (23). In many cultures, infants and toddlers are exposed to harmful levels of air pollution when they are strapped to their mother’s back during meal preparation (23, 24). The adverse health impacts of biomass smoke exposure have been well established but remain inadequately understood in the United States. Sood and colleagues demonstrated exposure to wood smoke was linked with gene promoter methylation and synergistically increased the risk of reduced lung function in cigarette smokers among a sample of women in New Mexico (25).
Tobacco smoke
Children exposed to secondhand smoke are at an increased risk for respiratory symptoms, impaired lung function, and lower respiratory illness, and cigarette smoke has been established as a leading risk factor of lung disease and increased asthma severity (26). Among AI/AN adults 18 years or older, commercial tobacco use was 38.9%, as compared with 16.8% of the general U.S. population (27, 28), which indicates a higher risk for tobacco smoke exposure among AI/AN children. The Navajo Nation Youth Risk Behavior Survey indicated that 11.4% of Navajo students in sixth, seventh, and eighth grades reported smoking cigarettes on 1 or more of the past 30 days, and 16.4% of students had smoked cigarettes or cigars in the past 30 days (n = 9,152 students) (4). Our review included the work of Reece, which indicated that clinical documentation of tobacco use in Navajo area IHS clinics was 0% (29). Recently, Nez-Henderson and colleagues found that male sex and younger age were associated with higher odds of cigarette smoking in a sample of southwestern American Indian tribal members (30). These recent data suggest that cigarette smoking may be on the rise among Navajo youth, but more research is necessary.
Indoor allergens
Allergic asthma is common among children, and exposure to indoor allergens (e.g., dust mite, cockroach, fungi, rodents, cats, dogs) may provoke asthma exacerbation (31, 32). Coexposures, such as endotoxin’s role in allergic asthma and atopy, may also increase childhood asthma prevalence and severity (33). Padhi and colleagues found a significant association between biomass burning and increased indoor endotoxin levels (34), and the synergistic relationship between endotoxin and diesel exhaust has been associated with increased frequency of wheeze in children (35). Although the Navajo reservation is a semiarid region and dust-mite and fungal exposures are believed to be low, there is little research to support this notion. We found no literature regarding indoor exposures among Navajo or AI/AN children but propose this is an important area for future investigation.
Outdoor Exposures
Exposure to toxic air pollutants has been associated with increased incidence and severity of asthma, emergency department use, hospital admissions, and use of asthma medications (36). Since the 1960s, the Navajo reservation has experienced high levels of pollution from coal-fired energy production, mining operations, and blowing dust storms.
Coal-fired power plants
The long-range transport of fine particles found in coal-fired sulfur emissions has been associated with asthma morbidity, increased lower respiratory symptoms, and decreased peak flow (37). Only one study met our review criteria: Bunnell and colleagues completed a multicomponent study comparing the outdoor air quality to the indoor air quality in Navajo homes (n = 20) (16). The study was conducted near Shiprock, New Mexico where there were two coal-fired power plants nearby; however, industrial activities and motor vehicle use were limited. During the winter months, atmospheric thermal inversions often trapped air pollution low to the ground (16). Bunnell and colleagues demonstrated that the average indoor ambient PM2.5 concentration was much greater than the average outdoor ambient PM2.5 concentration (36.0 μg/m3 and 9.95 μg/m3, respectively), and 9 of the 20 homes had levels far exceeding the EPA guidelines (16). When examining hospital admission and outpatient visit records (n = 133,759), the respiratory disease burden was much higher in the winter months than the summer months (16). Interestingly, the power plant emissions were much higher in the summer months, as a result of increased energy demands in the Southwestern United States, which was inversely correlated with the respiratory burden (16, 38). Bunnell and colleagues determined that coal burning inside Navajo homes was a primary risk factor for respiratory disease burden (16).
Diesel exhaust
Diesel exhaust has been associated with increased asthma and allergy symptoms, increased asthma exacerbation, and decreased lung function and has been implicated as a causative agent in lung cancer and respiratory disease (39). Approximately 50 to 94% of diesel particulate matter is classified as fine or ultrafine particulate matter. Diesel particulate matter is highly respirable, coats a large surface area of the lungs, and can easily reach the lower respiratory tract in children (39). Past studies have indicated that diesel particulate matter and PM2.5 concentrations within the school bus microenvironment consistently exceed federal air quality standards and do not sufficiently protect children’s health (40, 41). Among urban children living near roadways, diesel “soot” fraction PM2.5 significantly contributed to PM exposure and was associated with pollution-related asthma exacerbation (42). Children with longer bus commutes are exposed to increased concentrations of diesel particulate matter, black carbon, and oxides of nitrogen (41, 43).
We found no literature examining diesel exposure among Navajo or AI/AN children; however, exposure to diesel exhaust and harmful pollutants remains a valid concern in Navajo communities. Many Navajo children travel long distances to school, and more than 83% of roads on the Navajo reservation remain unpaved (44). The Chinle Unified School District transports 4,200 students, and 60% of the roads in this district remain unpaved (45). Navajo children in Blanding, Utah spend 4.5 hours per day on the bus, and Monument Valley High School students spend more than 6 hours per day on the bus (46). Also concerning is the disproportionately high bus failure rate on the Navajo and Apache reservations, which range from 40% to 88%, compared with the statewide average of 21% (45). Chinle Unified School District had a 41% fail rate (45), and many failed inspections cited major exhaust leaks entering the school bus cabin (47).
Mining and dust
Exposure to metals (e.g., copper) has been associated with asthma symptoms and increased risk of asthma in school children (48). Heavy metals, such as iron, nickel, cadmium, and chromium, are associated with increased wheezing symptoms, and higher blood chromium levels have been associated with increased coughing episodes (49, 50). Chronic exposure to arsenic in drinking water has also been associated with respiratory complications (51). Historical uranium mining has also been a concern, as blowing dust from more than 1,200 abandoned uranium mines has been implicated in adverse health effects, which may include respiratory health (52). A recent study determined that dust storms in the United States are most prevalent in Arizona and southern California (53). Dust is an important consideration on the Navajo reservation, because overgrazed land and severe drought have promoted desertification and increased the frequency of desert dust storms and wildfires. Currently, mobile sand dunes cover over 30% of the Navajo reservation (54). Therefore, dust and desertification are unique environmental determinants that may influence respiratory disease in this population.
Discussion
In this review, we systematically searched for peer-reviewed articles but were unable to find a large body of evidence regarding pediatric asthma on the Navajo reservation. Therefore, we integrated literature regarding the environmental exposures (both indoor and outdoor) known to enhance the risk of asthma on the Navajo reservation. Among the environmental risks discussed in this review, the most abundant peer-reviewed literature specific to the Navajo reservation and respiratory illnesses was conducted on indoor air pollution, with an emphasis on exposure to wood-burning stoves and coal combustion. Although exchanging older stoves for newer stoves is one possible solution, the high cost of such interventions may not be feasible for this population. Using more practical and low-cost interventions for families with lower socioeconomic status is important. Community-based participatory research approaches that focus on promoting best burning practices (i.e., ensuring wood is aged and properly seasoned; burning woods that produce less smoke, burn slower, and provide more heat energy) are necessary. Traditional cooking methods (especially if commonly used within the indoor microenvironment) remain a potential area for intervention, considering the large number of Navajo homes that lack access to electricity.
Diesel exhaust exposure on the school bus is an important future direction for interventions. Exposure to diesel exhaust has deleterious effects on children’s health, and protective measures include using newer and more efficient buses for the longest bus routes, limiting school bus idling to reduce exposure, and paving frequently used sections of dusty roads or other road infrastructure improvements.
We also sought literature on other known indoor asthma triggers, such as animal and pest allergens, mold, pollens, endotoxin and tobacco smoke exposure, and ceremonial smoke exposure, but no peer-reviewed literature specific to the Navajo reservation was available. Gaps in current research investigating indoor environmental allergens remain an important future direction for researchers, especially as they relate to increased asthma prevalence on the Navajo reservation. Quantifying ceremonial tobacco smoke and cigarette smoke exposure among the Navajo is important, but challenges exist with acquiring this information. Therefore, partnerships with the Navajo Nation and community-based participatory research methods are essential to obtaining accurate information while practicing cultural humility among this population.
Although our integrative review found a scarcity of published literature regarding the environmental factors influencing pediatric asthma in Navajo children, there is some evidence to suggest environmental risks may contribute to the disparate burden of asthma in children on the Navajo reservation. Some of these environmental risks, such as the common use of indoor heat and cook stoves, locale-specific indoor and outdoor allergens and fungi, various forms of personal smoke exposure, and diesel exhaust, are well known and are modifiable. Other potential risk factors such as dust storms, dust from contaminated soil, and coal-fired power plants are less recognized, yet may present additional insidious risks. The lack of published research affects our ability to adequately understand the causes of asthma disparities and plan future interventions.
The historic mistreatment, trauma, environmental injustices, and contraventions against American Indian/Alaska Native people by the U.S. government have led to a general mistrust of research. Some researchers have perpetuated this mistrust by publishing research that used culturally insensitive methods, was not collaborative with local partners, and fundamentally failed to understand the problems and resources of the Tribe. Furthermore, these publications often stigmatized and stereotyped American Indian/Alaska Native people. American Indians and Alaska Natives have experienced poor health outcomes for more than 500 years, and political and economic influences have continually affected the response (55). Such disparities are often viewed as markers of social injustice that clearly parallel disparities in wealth and power (55). Therefore, the Navajo Nation has been a leader in the movement by tribes to assert sovereignty in research conducted on the Navajo Nation, who mandate by law a specific process for conducting research on the reservation.
Future priorities to address children’s asthma, therefore, should be built through sustainable collaboration, including: addressing indoor air pollution from wood-burning stoves and coal combustion, diesel exhaust exposure from long bus rides, and understanding the burden of indoor allergens such as animal dander, dust, molds, pollens, and other known triggers of asthma exacerbation. Such future research could inform policy regarding effective ways to improve asthma disparities and be broadly applied to other Tribal reservations and rural populations with similar environmental risk factors. These indoor and outdoor pollutant exposures require further, careful investigation to fully describe and understand their impact on pediatric asthma for the Navajo Nation’s children. Ultimately, this information can direct comprehensive interventions to improve outcomes for children with asthma.
Supplementary Material
Acknowledgments
Acknowledgment
This manuscript was officially approved by the Navajo Nation Human Research Review Board (NNHRRB) on March 22, 2017 and given the number NNP-17.550. The authors thank the NNHRRB and Beverly Becenti-Pigman for their thoughtful review of the manuscript. They also thank Mari Stoddard, Health Promotion Sciences (HPS) librarian (retired) at the University of Arizona Mel and Enid Zuckerman College of Public Health, for assistance with our systematic, integrative search methodology, the University of Arizona Native American Training and Research Center for assistance during the search process, and Peter Nez of the Navajo Nation for his exceptional efforts with ensuring the Navajo perspective and cultural humility were practiced during our inquiry.
Footnotes
Supported by the National Institutes of Health, National Heart, Lung, and Blood Institute grant U34 HL130762 and by the Arizona Area Health Education Centers (AHEC) Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of Arizona AHEC.
Author Contributions: A.A.L. is the guarantor. All authors contributed to the conception and design of the work, and all authors read, provided feedback, and approved the final manuscript.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Valet RS, Gebretsadik T, Carroll KN, Wu P, Dupont WD, Mitchel EF, et al. High asthma prevalence and increased morbidity among rural children in a Medicaid cohort. Ann Allergy Astma Immunol. 2011;106:467–473. doi: 10.1016/j.anai.2011.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hendryx M, Gurka M, Ahern M, Putman H. Childhood asthma in rural-urban areas. 2012. [accessed 2017 Nov 20]. Available from: https://www.ruralhealthresearch.org/mirror/4/489/2011_asthma_final_report.pdf.
- 3.Brim SN, Rudd RA, Funk RH, Callahan DB. Asthma prevalence among US children in underrepresented minority populations: American Indian/Alaska Native, Chinese, Filipino, and Asian Indian. Pediatrics. 2008;122:e217–e222. doi: 10.1542/peds.2007-3825. [DOI] [PubMed] [Google Scholar]
- 4.Navajo Epidemiology Center. Navajo Nation Youth Risk Behavior Survey 2011 Report. 2011 [accessed 2016 Dec 11]. Available from: http://www.nec.navajo-nsn.gov/Portals/0/Reports/2011%20NYRBS%20MS%20Report%20-%20Final.pdf.
- 5.Navaho Nation. Welcome to the Navajo Nation Government. 2011 [accessed 2017 Sep 20]. Available from: http://www.navajo-nsn.gov/history.htm.
- 6.Navajo Epidemiology Center. Navajo Population Profile 2010 US Census. Window Rock, AZ: Navajo Department of Health; 2010. [Google Scholar]
- 7.U.S. Census Bureau. American Indian and Alaska Native: census 2000 data for 539 tribes. 2015 [accessed 2016 Nov 7]. Available from: http://www.census.gov/aian/census_2000/census_2000_data_for_539_tribes.html.
- 8.Mehal JM, Holman RC, Steiner CA, Bartholomew ML, Singleton RJ. Epidemiology of asthma hospitalizations among American Indian and Alaska Native people and the general United States population. Chest. 2014;146:624–632. doi: 10.1378/chest.14-0183. [DOI] [PubMed] [Google Scholar]
- 9.Delfino RJ, Staimer N, Tjoa T, Gillen DL, Schauer JJ, Shafer MM. Airway inflammation and oxidative potential of air pollutant particles in a pediatric asthma panel. J Expo Sci Environ Epidemiol. 2013;23:466–473. doi: 10.1038/jes.2013.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin M, Chen Y, Burnett RT, Villeneuve PJ, Krewski D. The influence of ambient coarse particulate matter on asthma hospitalization in children: case-crossover and time-series analyses. Environ Health Perspect. 2002;110:575–581. doi: 10.1289/ehp.02110575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Etzel RA. Indoor and outdoor air pollution: tobacco smoke, moulds and diseases in infants and children. Int J Hyg Environ Health. 2007;210:611–616. doi: 10.1016/j.ijheh.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Navajo Housing Authority. Spatial distribution of Navajo Housing Authority survey data. [Revised 2017 Nov 20; accessed 2016 Nov 7]. Available from: http://www.navajohousingauthority.org/
- 13.Smith KR, Mehta S. The burden of disease from indoor air pollution in developing countries: comparison of estimates. Int J Hyg Environ Health. 2003;206:279–289. doi: 10.1078/1438-4639-00224. [DOI] [PubMed] [Google Scholar]
- 14.Belanger K, Triche EW. Indoor combustion and asthma. Immunol Allergy Clin North Am. 2008;28:507–519, vii. doi: 10.1016/j.iac.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naeher LP, Brauer M, Lipsett M, Zelikoff JT, Simpson CD, Koenig JQ, et al. Woodsmoke health effects: a review. Inhal Toxicol. 2007;19:67–106. doi: 10.1080/08958370600985875. [DOI] [PubMed] [Google Scholar]
- 16.Bunnell JE, Garcia LV, Furst JM, Lerch H, Olea RA, Suitt SE, et al. Navajo coal combustion and respiratory health near Shiprock, New Mexico. J Environ Public Health. 2010;2010:260525. doi: 10.1155/2010/260525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morris K, Morgenlander M, Coulehan JL, Gahagen S, Arena VC. Wood-burning stoves and lower respiratory tract infection in American Indian children. Am J Dis Child. 1990;144:105–108. doi: 10.1001/archpedi.1990.02150250117047. [DOI] [PubMed] [Google Scholar]
- 18.Robin LF, Less PS, Winget M, Steinhoff M, Moulton LH, Santosham M, et al. Wood-burning stoves and lower respiratory illnesses in Navajo children. Pediatr Infect Dis J. 1996;15:859–865. doi: 10.1097/00006454-199610000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Champion WM, Connors L, Montoya LD. Emission factors of fine particulate matter, organic and elemental carbon, carbon monoxide, and carbon dioxide for four solid fuels commonly used in residential heating by the U.S. Navajo Nation. J Air Waste Manag Assoc. 2017;67:1020–1035. doi: 10.1080/10962247.2017.1334717. [DOI] [PubMed] [Google Scholar]
- 20.Ward T, Boulafentis J, Simpson J, Hester C, Moliga T, Warden K, et al. Lessons learned from a woodstove changeout on the Nez Perce Reservation. Sci Total Environ. 2011;409:664–670. doi: 10.1016/j.scitotenv.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 21.Noonan CW, Ward TJ, Navidi W, Sheppard L. A rural community intervention targeting biomass combustion sources: effects on air quality and reporting of children’s respiratory outcomes. Occup Environ Med. 2012;69:354–360. doi: 10.1136/oemed-2011-100394. [DOI] [PubMed] [Google Scholar]
- 22.Ward TJ, Semmens EO, Weiler E, Harrar S, Noonan CW. Efficacy of interventions targeting household air pollution from residential wood stoves. J Expo Sci Environ Epidemiol. 2015;27:1–8. doi: 10.1038/jes.2015.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Po JY, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. 2011;66:232–239. doi: 10.1136/thx.2010.147884. [DOI] [PubMed] [Google Scholar]
- 24.Naeher LP, Leaderer BP, Smith KR. Particulate matter and carbon monoxide in highland Guatemala: indoor and outdoor levels from traditional and improved wood stoves and gas stoves. Indoor Air. 2000;10:200–205. doi: 10.1034/j.1600-0668.2000.010003200.x. [DOI] [PubMed] [Google Scholar]
- 25.Sood A, Petersen H, Blanchette CM, Meek P, Picchi MA, Belinsky SA, et al. Wood smoke exposure and gene promoter methylation are associated with increased risk for COPD in smokers. Am J Respir Crit Care Med. 2010;182:1098–1104. doi: 10.1164/rccm.201002-0222OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Centers for Disease Control and Prevention. The health consequences of involuntary exposure to tobacco smoke. Rockville, MD: Department of Health and Human Services; 2006. [Google Scholar]
- 27.Martell B, Garrett B, Caraballo R. Disparities in adult cigarette smoking — United States, 2002–2005 and 2010–2013. Atlanta, GA: U.S. Centers for Disease Control and Prevention; 2016. [DOI] [PubMed] [Google Scholar]
- 28.Jamal A, Homa D, O’Connor E, Babb SD, Caraballo RS, Singh T, et al. Current cigarette smoking among adults–United States, 2005–2014. Atlanta, GA: U.S. Centers for Disease Control and Prevention; 2015. [DOI] [PubMed] [Google Scholar]
- 29.Reece DH. Clinical annotation of tobacco use in patient charts at Indian Health Service clinics and hospitals. J Community Health. 1996;21:389–396. doi: 10.1007/BF01702790. [DOI] [PubMed] [Google Scholar]
- 30.Nez Henderson P, Jacobsen C, Beals J AI-SUPERPFP Team. Correlates of cigarette smoking among selected Southwest and Northern plains tribal groups: the AI-SUPERPFP Study. Am J Public Health. 2005;95:867–872. doi: 10.2105/AJPH.2004.050096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Academy of Allergy Asthma & Immunology. Allergic asthma. 2016 [accessed 2016 Oct 16]. Available from: http://www.aaaai.org/conditions-and-treatments/conditions-a-to-z-search/allergic-asthma.
- 32.Crain EF, Walter M, O’Connor GT, Mitchell H, Gruchalla RS, Kattan M, et al. Home and allergic characteristics of children with asthma in seven U.S. urban communities and design of an environmental intervention: the Inner-City Asthma Study. Environ Health Perspect. 2002;110:939–945. doi: 10.1289/ehp.02110939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Michel O, Kips J, Duchateau J, Vertongen F, Robert L, Collet H, et al. Severity of asthma is related to endotoxin in house dust. Am J Respir Crit Care Med. 1996;154:1641–1646. doi: 10.1164/ajrccm.154.6.8970348. [DOI] [PubMed] [Google Scholar]
- 34.Padhi BK, Adhikari A, Satapathy P, Patra AK, Chandel D, Panigrahi P. Predictors and respiratory depositions of airborne endotoxin in homes using biomass fuels and LPG gas for cooking. J Expo Sci Environ Epidemiol. 2017;27:112–117. doi: 10.1038/jes.2016.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ryan PH, Bernstein DI, Lockey J, Reponen T, Levin L, Grinshpun S, et al. Exposure to traffic-related particles and endotoxin during infancy is associated with wheezing at age 3 years. Am J Respir Crit Care Med. 2009;180:1068–1075. doi: 10.1164/rccm.200808-1307OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ostro B, Roth L, Malig B, Marty M. The effects of fine particle components on respiratory hospital admissions in children. Environ Health Perspect. 2009;117:475–480. doi: 10.1289/ehp.11848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schwartz J, Neas LM. Fine particles are more strongly associated than coarse particles with acute respiratory health effects in schoolchildren. Epidemiology. 2000;11:6–10. doi: 10.1097/00001648-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Navajo Generating Station. About. 2017 [accessed 2017 Nov 20]. Available from: https://www.ngspower.com/
- 39.U.S. Environmental Protection Agency. Health assessment document for diesel engine exhaust. Washington, DC: National Center for Environmental Assessment Office of Research and Development; 2002. [Google Scholar]
- 40.U.S. Environmental Protection Agency. History of children’s environmental health protection at EPA. 2016 [accessed 2016 Jul 22]. Available from: https://www.epa.gov/children/history-childrens-environmental-health-protection-epa.
- 41.Wargo J. Children’s exposure to diesel exhaust on school buses. New Haven, CT: Yale University; 2002. [Google Scholar]
- 42.Spira-Cohen A, Chen LC, Kendall M, Sheesley R, Thurston GD. Personal exposures to traffic-related particle pollution among children with asthma in the South Bronx, NY. J Expo Sci Environ Epidemiol. 2010;20:446–456. doi: 10.1038/jes.2009.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sabin LD, Behrentz E, Winer AM, Jeong S, Fitz DR, Pankratz DV, et al. Characterizing the range of children’s air pollutant exposure during school bus commutes. J Expo Anal Environ Epidemiol. 2005;15:377–387. doi: 10.1038/sj.jea.7500414. [DOI] [PubMed] [Google Scholar]
- 44.Chaco P. Roads and transportation on the Navajo Nation. 2012 [accessed 2016 Sep 8]. Available from: https://www.whitehouse.gov/blog/2012/02/15/roads-and-transportation-navajo-nation.
- 45.Cano R. Rural Arizona school district: ‘Buses weren’t made to run on these roads’. 2016 [accessed 2016 Dec 12]. Available from: http://www.azcentral.com/story/news/local/arizona-investigations/2016/09/14/chinle-arizona-school-district-bus-safety/87558372/
- 46.Zars B. Long rides, tough hides: enduring long school bus rides. Randolph, VT: Rural Challenge Policy Program; 1998. [Google Scholar]
- 47.McGlade C, Cano R. How safe are your children’s buses. 2016 [accessed 2016 Dec 11]. Available from: http://www.azcentral.com/pages/interactives/arizona-school-bus-inspections-data/
- 48.Gehring U, Beelen R, Eeftens M, Hoek G, de Hoogh K, de Jongste JC, et al. Particulate matter composition and respiratory health: the PIAMA Birth Cohort study. Epidemiology. 2015;26:300–309. doi: 10.1097/EDE.0000000000000264. [DOI] [PubMed] [Google Scholar]
- 49.Zeng X, Xu X, Zheng X, Reponen T, Chen A, Huo X. Heavy metals in PM2.5 and in blood, and children’s respiratory symptoms and asthma from an e-waste recycling area. Environ Pollut. 2016;210:346–353. doi: 10.1016/j.envpol.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 50.Dunea D, Iordache S, Liu HY, Bøhler T, Pohoata A, Radulescu C. Quantifying the impact of PM2.5 and associated heavy metals on respiratory health of children near metallurgical facilities. Environ Sci Pollut Res Int. 2016;23:15395–15406. doi: 10.1007/s11356-016-6734-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Islam LN, Nabi AH, Rahman MM, Zahid MS. Association of respiratory complications and elevated serum immunoglobulins with drinking water arsenic toxicity in human. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2007;42:1807–1814. doi: 10.1080/10934520701566777. [DOI] [PubMed] [Google Scholar]
- 52.Dawson SE, Madsen GE. Psychosocial and health impacts of uranium mining and milling on Navajo lands. Health Phys. 2011;101:618–625. doi: 10.1097/HP.0b013e3182243a7a. [DOI] [PubMed] [Google Scholar]
- 53.Crooks JL, Cascio WE, Percy MS, Reyes J, Neas LM, Hilborn ED. The association between dust storms and daily non-accidental mortality in the United States, 1993-2005. Environ Health Perspect. 2016;124:1735–1743. doi: 10.1289/EHP216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morales L.Navajo Nation witnesses changing landscape: growing sand dunes [transcript] Morning EditionNational Public Radio.May 282015 [Google Scholar]
- 55.Jones DS. The persistence of American Indian health disparities. Am J Public Health. 2006;96:2122–2134. doi: 10.2105/AJPH.2004.054262. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.