Abstract
Background: Ageing is associated with sleep pattern changes and body composition changes, which are related to several diseases. Purpose: This study aimed to analyse the association between sleep quality and an extensive set of body composition parameters (waist-hip ratio, body mass index, bone mineral content, bone mineral density, lean mass, lean mass index, fat mass, fat mass percentage, fat mass index, visceral adipose tissue) and sleep quality in sedentary middle-aged adults. We also aimed to evaluate whether the possible associations accord between subjective and objective measurements of sleep quality. Methods: 74 (39 women) middle-aged sedentary adults (40–65 years old) participated in the present study. The sleep quality was assessed using the Pittsburgh sleep quality index (PSQI) scale and accelerometers. A PSQI global score more than 5 indicates poor sleep quality. Weight, height, waist and hip circumferences were measured, and body mass index and waist-hip ratio were also calculated. Body composition was assessed with a dual-energy X-ray absorptiometry scanner. Results: The PSQI global score was negatively associated with bone mineral content, bone mineral density, lean mass, lean mass index and positively associated with fat mass percentage. No association was found between accelerometer parameters and body composition variables. Conclusion: We showed that a subjective poor sleep quality was negatively associated with bone mineral content (BMC), bone mineral density (BMD), lean mass and lean mass index (LMI) whereas was positively associated with fat mass percentage in middle-aged adults. We also observed that these associations did not accord with objective sleep quality measurements.
Keywords: sleep quality, body composition, body mass index, bone mineral density, lean mass, fat mass
1. Introduction
Age-related changes in body composition, characterized by a decrease in bone mineral density and muscle mass and an increment of fat mass, is a concern in the aged society [1]. Sarcopenia, obesity and osteopenia/osteoporosis are three frequent chronic diseases in the older population but these conditions are progressive and initiate at a younger age [2,3]. These body composition changes are related to a decrease in the quality of life and an increase of mortality risk [4], producing a significant burden on individual wellness and public health [3].
Another significant concern associated with ageing is sleep pattern changes [5], including a decrease in the quantity and quality of sleep [5]. It has been estimated that approximately 50% of older adults complain about difficulty initiating or maintaining sleep [6]. A poor sleep quality could increase inflammation, decrease melatonin production and disrupt the circadian rhythms [7], which are involved in several diseases related to the ageing process, such as, coronary heart disease [8], type 2 diabetes [9], obesity [10], depression [11], and consequently an increased risk of mortality [6].
Certain studies have proposed a relationship between sleep quality and bone mineral density [12], muscle mass [13] and fat mass [14]. A poor sleep quality deregulates the catabolic/anabolic cycle increasing the risk of osteoporosis [15], induces high insulin resistance increasing the risk of sarcopenia [16], and produces metabolic and endocrine alterations increasing the risk of obesity [17]. However, these studies used subjective questionnaires to assess sleep quality. Although these questionnaires have been previously validated, there are no studies that evaluate the association between sleep quality measured by accelerometry with body composition parameters.
This study aimed to analyse the association between sleep quality (measured using subjective and objective methods) with an extensive set of body composition parameters (waist-hip ratio, body mass index, bone mineral content, bone mineral density, lean mass, lean mass index, fat mass, fat mass percentage, fat mass index, visceral adipose tissue) in sedentary middle-aged adults. We also aimed to evaluate whether these associations were similar considering sleep quality measured by subjective versus objective methods. We hypothesized that participants with poor sleep quality would have low bone mineral density, low lean mass and high fat mass levels. Additionally, we hypothesized that these associations would be similar in subjective and objective methods.
2. Materials and Methods
2.1. Participants
A total of 74 (39 women) middle-aged sedentary adults (40–65 years old) took part in the present study. The participants were enrolled in the FIT-AGEING study [18], an exercise-based randomized controlled trial (clinicaltrial.gov: ID: NCT03334357). All participants reported to be non-physically active (<20 min of moderate-intensity physical activity on 3 days/week), with stable weight (weight changes <5 kg) over the last 5 months, free of disease, and not taking any medication. The study was approved by the Ethics Committee on Human Research at the University of Granada and Servicio Andaluz de Salud (CEI-Granada) (0838-N-2017) (25 September 2017). The study protocols and experimental design were applied in accordance with the last revised ethical guidelines of the Declaration of Helsinki. All participants signed an informed consent. All variables were assessed at the baseline of the FIT-AGEING study [18].
2.2. Sleep Quality Assessment
The sleep quality of the participants was assessed by the Pittsburgh sleep quality index (PSQI) scale, a 19-item scale that provides 7 component scores (ranges 0–3) [19]. It consists of 7 elements: (i) subjective sleep quality (very good to very bad), (ii) sleep latency (≤15 min to >60 min), (iii) sleep duration (≥7 h to <5 h), (iv) sleep efficiency (≥85% to <65% hours sleep/hours in bed), (v) sleep disturbances (not during the past month to ≥ 3 times per week), (vi) use of sleeping medications (none to ≥ 3 times a week), and (vii) daytime dysfunction (not a problem to a very big problem); with a total global score ranging from 0 to 21 [19]. A PSQI global score more than 5 was considered as poor sleep quality [19].
Objective characteristics of sleep-wake patterns were measured with a wrist-worn accelerometer (ActiSleep, ActiGraph, Pensacola, FL, USA) for 7 consecutive days (24 h/day) [18]. The participants received detailed information on how to wear the accelerometer and were asked to remove it only during water activities. They also recorded the times they went to bed each night, woke up each morning and removed the device every day. Data were processed using the ActiLife v. 6.13.3 software (ActiGraph, Pensacola, FL, USA). The accelerometers were initialized to store raw accelerations at a sampling frequency of 100 Hz [20]. The following variables were analyzed: Total sleep time (minutes slept between bedtime and wake time), sleep efficiency (percentage of time asleep while in bed) and wake after sleep onset (minutes awake between sleep onset and wake time). Wake after sleep onset referred to periods of wakefulness occurring after defined sleep onset, and it was a measurement of wakefulness, reflecting sleep fragmentation [21].
2.3. Anthropometric and Body Composition Assessment
Body weight and height measurements were performed without shoes and with light clothing, using a pre-validated scale and stadiometer (model 799, Electronic Column Scale, Hamburg, Germany) and the body mass index (BMI) was calculated (weight/height2) [22].
We measured (in triplicate) waist circumference (WC) at the midpoint between the lowest rib cage and the top of the iliac crest and hip circumference (HC) around the widest portion of the buttocks with a non-elastic tape (Seca 200, MWS Ltd., Scalesmart, Leicester, UK) to the nearest 0.1 cm. Waist-hip ratio (WHiR) was calculated by dividing waist measurement by hip measurement.
A dual-energy X-ray absorptiometry scanner (Discovery Wi, Hologic, Inc., Bedford, MA, USA) was used to measure body composition following the manufacturer’s recommendations. The whole-body scan was considered to obtain all body composition parameters (bone mineral content, lean mass, fat mass and visceral adipose tissue). We conducted the quality controls, the positioning of the participants, and the analyses of the results following the manufacturer’s recommendations. An automatic delineation of the anatomic regions was performed by the software APEX 4.0.2. We acquired spine phantom quality control scans on each study day. Bone mineral density (BMD) was calculated as bone mineral content (BMC) in g divided by the total bone surface in cm2. Lean mass index (LMI) was calculated as lean mass in kg divided by height in m2. Similarly, we calculated the fat mass index (FMI) as fat mass in kg divided by height in m2. Fat mass was also expressed as weight percentage.
2.4. Statistical Analysis
The sample size and power calculations were made based on the data of a pilot study [18]. The Shapiro–Wilk test, visual check of histograms, Q-Q and box plots were used to verify the distribution of all variables. The descriptive parameters were reported as mean and standard deviation.
We conducted simple linear regression models to examine the association of sleep quality (PSQI global score, total sleep time, sleep efficiency and wake after sleep onset) with body composition parameters (BMI, WHiR, BMC, BMD, lean mass, LMI, fat mass, fat mass percentage, FMI, and visceral adipose tissue).
We also conducted multiple linear regression models to test these associations after adjusting by sex, and age.
All analyses were conducted using the Statistical Package for Social Sciences (SPSS, v. 25.0, IBM SPSS Statistics, IBM Corporation) and the level of significance was set at <0.05. Graphical presentations were prepared using GraphPad Prism 5 (GraphPad Software, San Diego, CA, USA).
3. Results
The characteristics of the study sample are shown in Table 1.
Table 1.
Descriptive parameters.
| All (n = 74) | Men (n = 35) | Women (n = 39) | |
|---|---|---|---|
| Age (years) | 53.7 ± 5.1 | 54.4 ± 5.3 | 53.0 ± 5.0 |
| Body composition parameters | |||
| Body mass index (kg/m2) | 26.7 ± 3.8 | 28.3 ± 3.6 | 25.3 ± 3.3 |
| Waist-Hip ratio | 0.91 ± 0.08 | 0.97 ± 0.07 | 0.86 ± 0.06 |
| Bone mineral content (g) | 2258.1 ± 453.5 | 2633.6 ± 301.2 | 1921.1 ± 259.8 |
| Bone mineral density (g/cm2) | 1.10 ± 0.10 | 1.16 ± 0.08 | 1.05 ± 0.09 |
| Lean mass (kg) | 43.5 ± 11.7 | 53.9 ± 6.5 | 34.1 ± 5.8 |
| Lean mass index (kg/m2) | 15.2 ± 2.9 | 17.5 ± 2.0 | 13.2 ± 1.8 |
| Fat mass (kg) | 30.0 ± 8.4 | 30.9 ± 9.8 | 29.2 ± 7.1 |
| Fat mass (%) | 39.9 ± 9.1 | 34.7 ± 8.0 | 44.5 ± 7.4 |
| Fat mass index (kg/m2) | 10.7 ± 3.1 | 10.0 ± 3.2 | 11.4 ± 2.9 |
| Sleep quality parameters | |||
| PSQI global score | 5.6 ± 3.5 | 4.8 ± 3.1 | 6.3 ± 3.6 |
| Total sleep time (min) | 359.9 ± 48.8 | 337.9 ± 46.3 | 380.1 ± 42.4 |
| Sleep efficiency (%) | 85.0 ± 6.3 | 84.9 ± 7.5 | 86.1 ± 4.7 |
| Wake after sleep onset (min) | 63.9 ± 27.4 | 65.8 ± 32.4 | 62.2 ± 22.2 |
Values are expressed as mean ± standard deviation. Abbreviations: PSQI—Pittsburgh sleep quality index.
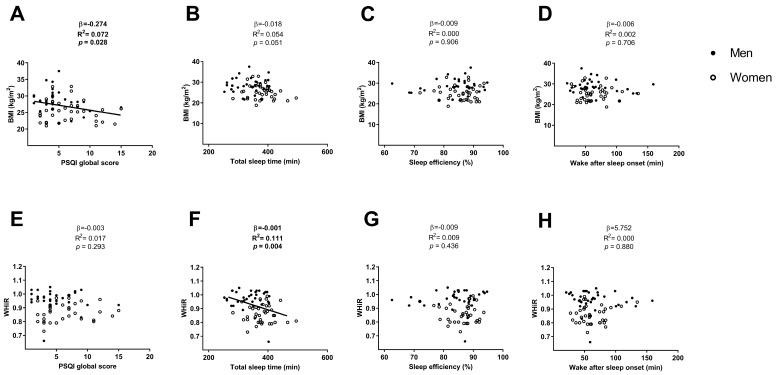
The PSQI global score was negatively associated with the BMI (β = −0.274, R2 = 0.072, p = 0.028; Figure 1A), which disappeared after including sex, and both sex and age in the model (all p > 0.05; Table 2). The PSQI global score was not associated with the WHiR (β = −0.003, R2 = 0.017, p = 0.293; Figure 1E) neither after including sex, age, and both sex and age in the model (all p > 0.05; Table 2).
Figure 1.
Linear regression graphs between the PSQI global score, total sleep time, sleep efficiency and wake after sleep onset with BMI (Panels A, B, C, and D, respectively) and with WHiR (Panels E, F, G, and H, respectively). β—non-standardised linear regression coefficient; R2—Coefficient of determination; p value. Abbreviations: PSQI—Pittsburgh sleep quality index, BMI—body mass index, WHiR—waist-hip ratio.
Table 2.
Association of PSQI global score with body composition parameters.
| All (n = 74) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||||
| Body Composition Parameters | β | R2 | p | β | R2 | p | β | R2 | p |
| Body mass index (kg/m2) | −0.188 | 0.204 | 0.112 | −0.241 | 0.094 | 0.057 | −0.144 | 0.127 | 0.279 |
| Waist-Hip ratio | −5.498 | 0.345 | 0.982 | −0.004 | 0.050 | 0.178 | −1.030 | 0.111 | 0.867 |
| Bone mineral content (g) | −20.624 | 0.634 | 0.045 | −42.544 | 0.107 | 0.009 | −0.002 | 0.144 | 0.121 |
| Bone mineral density (g/cm2) | −0.010 | 0.419 | 0.001 | −0.013 | 0.197 | <0.001 | −14.293 | 0.230 | 0.003 |
| Lean mass (kg) | −0.466 | 0.725 | 0.044 | −1.001 | 0.115 | 0.016 | −8.629 | 0.129 | 0.259 |
| Lean mass index (kg/m2) | −0.238 | 0.640 | <0.001 | −0.332 | 0.228 | 0.001 | −0.724 | 0.219 | 0.004 |
| Fat mass (kg) | 0.331 | 0.026 | 0.255 | 0.274 | 0.014 | 0.346 | 5.945 | 0.129 | 0.256 |
| Fat mass (%) | 0.511 | 0.353 | 0.058 | 0.765 | 0.106 | 0.016 | 0.083 | 0.140 | 0.150 |
| Fat mass index (kg/m2) | 0.072 | 0.068 | 0.506 | 0.116 | 0.018 | 0.297 | 0.077 | 0.115 | 0.588 |
| Visceral adipose tissue (g) | 6.407 | 0.188 | 0.591 | −5.293 | 0.006 | 0.687 | 0.001 | 0.115 | 0.583 |
The analyses were controlled for: Sex (Model 1); age (Model 2); both sex and age (Model 3). β—unstandardized regression coefficient; R2, and p value were obtained from the multiple linear regression analyses. Abbreviations: PSQI—Pittsburgh sleep quality index; bold values are values that are significant (p < 0.05).
No association was found between total sleep time and BMI (β = −0.018, R2 = 0.054, p = 0.051; Figure 1B), neither including sex or both sex and age in the model (all p > 0.05; Table 3) and was negatively associated when we included age (β = −0.019, R2 = 0.083, p = 0.040; Table 3) in the model. Total sleep time was negatively associated with WHiR (β=−0.001, R2 = 0.111, p = 0.004; Figure 1F), which disappeared after including sex or both sex and age in the model (all p > 0.05; Table 3) and remained after including age in the model (β = −0.001, R2 = 0.126, p = 0.006; Table 3).
Table 3.
Association of sleep time with body composition parameters.
| All (n = 74) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||||
| Body Composition Parameters | β | R2 | p | β | R2 | p | β | R2 | p |
| Body mass index (kg/m2) | −0.005 | 0.182 | 0.622 | −0.019 | 0.083 | 0.040 | −0.876 | 0.192 | 0.587 |
| Waist-Hip ratio | 0.000 | 0.391 | 0.455 | −0.001 | 0.126 | 0.006 | −58.250 | 0.195 | 0.467 |
| Bone mineral content (g) | −0.441 | 0.639 | 0.565 | −3.664 | 0.152 | 0.001 | −0.012 | 0.193 | 0.532 |
| Bone mineral density (g/cm2) | 0.000 | 0.352 | 0.120 | −0.001 | 0.159 | 0.001 | −102.173 | 0.219 | 0.110 |
| Lean mass (kg) | −0.004 | 0.734 | 0.825 | −0.096 | 0.186 | 0.001 | 0.000 | 0.190 | 0.718 |
| Lean mass index (kg/m2) | −0.003 | 0.563 | 0.544 | −0.023 | 0.237 | <0.001 | −2.916 | 0.198 | 0.393 |
| Fat mass (kg) | 0.007 | 0.019 | 0.775 | −0.003 | 0.010 | 0.870 | 0.000 | 0.190 | 0.765 |
| Fat mass (%) | 0.006 | 0.275 | 0.774 | 0.049 | 0.109 | 0.022 | 0.261 | 0.190 | 0.724 |
| Fat mass index (kg/m2) | −7.391 | 0.039 | 0.993 | 0.006 | 0.016 | 0.451 | 0.020 | 0.189 | 0.991 |
| Visceral adipose tissue (g) | −0.576 | 0.221 | 0.548 | −2.049 | 0.073 | 0.033 | −0.009 | 0.193 | 0.555 |
The analyses were controlled for: Sex (Model 1); age (Model 2); both sex and age (Model 3). β—unstandardized regression coefficient; R2, and p value were obtained from the multiple linear regression analyses. Bold values are values that are significant (p < 0.05).
No association was found between sleep efficiency and the wake after sleep onset with BMI and WHiR (all p > 0.05; Figure 1C,D, respectively for BMI and Figure 1G,H, respectively for WHiR), neither after including sex age or both sex and age in the model (all p > 0.05; Table 4 and Table 5).
Table 4.
Association of sleep efficiency with body composition parameters.
| All (n = 74) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||||
| Body Composition Parameters | β | R2 | p | β | R2 | p | β | R2 | p |
| Body mass index (kg/m2) | 3.686 | 0.183 | 0.584 | −1.190 | 0.024 | 0.869 | 0.120 | 0.035 | 0.598 |
| Waist-Hip ratio | 0.020 | 0.386 | 0.879 | −0.122 | 0.028 | 0.460 | 1.861 | 0.031 | 0.869 |
| Bone mineral content (g) | 71.598 | 0.637 | 0.896 | −960.826 | 0.019 | 0.279 | 0.000 | 0.031 | 0.918 |
| Bone mineral density (g/cm2) | −0.101 | 0.332 | 0.545 | −0.266 | 0.031 | 0.180 | −5.737 | 0.036 | 0.527 |
| Lean mass (kg) | −2.926 | 0.734 | 0.807 | −32.049 | 0.057 | 0.152 | −0.053 | 0.033 | 0.716 |
| Lean mass index (kg/m2) | −2.532 | 0.564 | 0.502 | −8.966 | 0.123 | 0.092 | −0.435 | 0.043 | 0.365 |
| Fat mass (kg) | 23.375 | 0.047 | 0.150 | 20.077 | 0.032 | 0.212 | 0.132 | 0.061 | 0.148 |
| Fat mass (%) | 15.583 | 0.286 | 0.298 | 29.174 | 0.079 | 0.044 | 0.116 | 0.049 | 0.261 |
| Fat mass index (kg/m2) | 6.054 | 0.053 | 0.313 | 7.752 | 0.032 | 0.196 | 0.254 | 0.046 | 0.306 |
| Visceral adipose tissue (g) | 148.816 | 0.217 | 0.827 | −342.253 | 0.011 | 0.651 | 0.000 | 0.031 | 0.824 |
The analyses were controlled for: Sex (Model 1); age (Model 2); both sex and age (Model 3). β—unstandardized regression coefficient; R2, and p value were obtained from the multiple linear regression analyses. Bold values are values that are significant (p < 0.05).
Table 5.
Association of wake after sleep onset with body composition parameters.
| All (n = 74) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||||
| Body Composition Parameters | β | R2 | p | β | R2 | p | β | R2 | p |
| Body mass index (kg/m2) | −0.010 | 0.184 | 0.502 | −0.006 | 0.025 | 0.739 | −0.634 | 0.011 | 0.528 |
| Waist-Hip ratio | −7.338 | 0.386 | 0.807 | 4.170 | 0.020 | 0.912 | −13.219 | 0.006 | 0.791 |
| Bone mineral content (g) | −0.414 | 0.637 | 0.737 | 0.509 | 0.003 | 0.803 | −0.004 | 0.007 | 0.771 |
| Bone mineral density (g/cm2) | 0.000 | 0.329 | 0.745 | 0.000 | 0.010 | 0.546 | 14.698 | 0.007 | 0.714 |
| Lean mass (kg) | 0.004 | 0.734 | 0.897 | 0.031 | 0.034 | 0.551 | 0.186 | 0.007 | 0.772 |
| Lean mass index (kg/m2) | 0.005 | 0.563 | 0.580 | 0.011 | 0.096 | 0.365 | 1.764 | 0.016 | 0.406 |
| Fat mass (kg) | −0.055 | 0.049 | 0.136 | −0.053 | 0.040 | 0.151 | −0.604 | 0.039 | 0.132 |
| Fat mass (%) | −0.034 | 0.285 | 0.321 | −0.047 | 0.023 | 0.224 | −0.506 | 0.023 | 0.269 |
| Fat mass index (kg/m2) | −0.014 | 0.054 | 0.307 | −0.016 | 0.027 | 0.253 | −1.152 | 0.022 | 0.294 |
| Visceral adipose tissue (g) | −0.510 | 0.218 | 0.741 | −0.107 | 0.008 | 0.951 | −0.003 | 0.007 | 0.735 |
The analyses were controlled for: Sex (Model 1); age (Model 2); both sex and age (Model 3). β—unstandardized regression coefficient; R2, and p value were obtained from the multiple linear regression analyses.
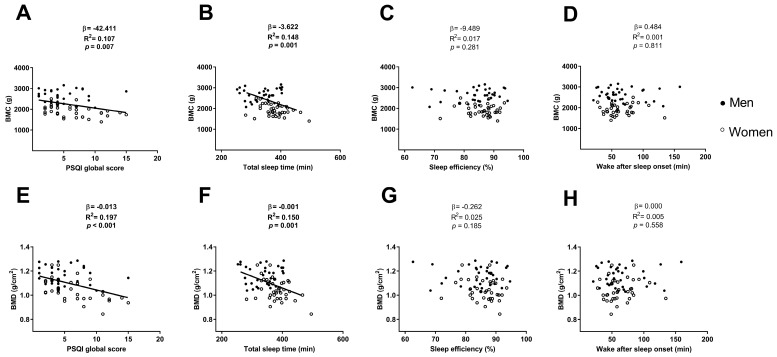
The PSQI global score was negatively associated with the BMC and the BMD (β = −42.411, R2 = 0.107, p = 0.007; Figure 2A; β = −0.013, R2 = 0.197, p < 0.001; Figure 2E respectively), which remained after including sex (β = −20.624, R2 = 0.634, p = 0.045; β = −0.010, R2 = 0.419, p = 0.001 respectively; Table 2) and age (β = −42.544, R2 = 0.107, p = 0.009; β = −0.013, R2 = 0.197, p < 0.001 respectively; Table 2) in the model. However, when we included both sex and age in the model, the association between the PSQI global score and BMC disappeared (p > 0.05; Table 2), and remained with BMD (β = −14.293, R2 = 0.230, p = 0.003; Table 2).
Figure 2.
Linear regression graphs between PSQI global score, total sleep time, sleep efficiency and wake after sleep onset with BMC (Panels A, B, C, and D, respectively) and with BMD (Panels E, F, G, and H, respectively). β—non-standardised linear regression coefficient; R2—Coefficient of determination; p value. Abbreviations: PSQI—Pittsburgh sleep quality index, BMC—bone mineral content, BMD—bone mineral density.
The total sleep time was negatively associated with the BMC and the BMD (β = −3.622, R2 = 0.148, p = 0.001; Figure 2B; β = −0.001, R2 = 0.150, p = 0.001; Figure 2F respectively), which disappeared after including sex in the model or both sex and age in the model (all p > 0.05; Table 3) and remained after including age in the model (β = −3.664, R2 = 0.152, p = 0.001; β = −0.001; R2 = 0.159, p = 0.001 respectively; Table 3).
No association was found between the sleep efficiency and the wake after sleep onset with the BMC and the BMD (all p > 0.05; Figure 2C,D, respectively for BMC and Figure 2G,H, respectively for BMD), neither after including sex, age or both sex and age in the model (all p > 0.05; Table 5).
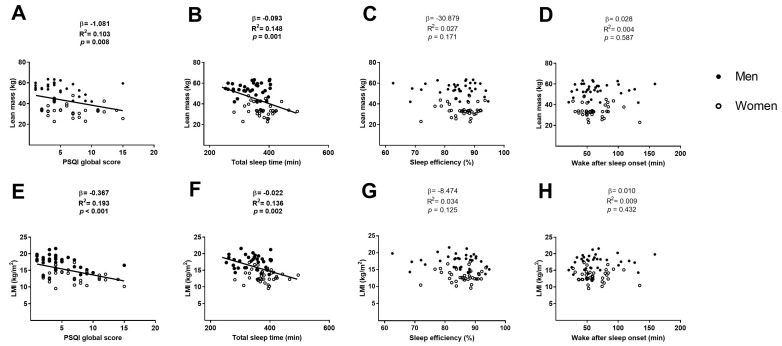
The PSQI global score was negatively associated with the lean mass and the LMI (β = −1.081, R2 = 0.103, p = 0.008; Figure 3A; β = −0.367, R2 = 0.193, p < 0.001; Figure 3E respectively), which remained after including sex (β = −0.466, R2 = 0.725, p = 0.044; β = −0.238, R2 = 0.640, p < 0.001 respectively; Table 2) and age (β = −1.001, R2 = 0.115, p = 0.016; β = −0.332, R2 = 0.228, p = 0.001 respectively; Table 2) in the model. However, when we included both sex and age in the model, the association between the PSQI global score and lean mass disappeared (p > 0.05; Table 2), and remained with LMI (β = −0.724, R2 = 0.219, p = 0.004; Table 2).
Figure 3.
Linear regression graphs between PSQI global score, total sleep time, sleep efficiency and wake after sleep onset with lean mass (Panels A, B, C, and D, respectively) and with LMI (Panels E, F, G, and H, respectively). β—non-standardised linear regression coefficient; R2—Coefficient of determination; p value. Abbreviations: PSQI—Pittsburgh sleep quality index, LMI—lean mass index.
No association was found between the sleep efficiency and the wake after sleep onset with the lean mass and the LMI (all p > 0.05; Figure 3C,D respectively for lean mass Figure 3G,H respectively for LMI), neither when we included sex, age or both sex and age in the model (all p > 0.05; Table 4 and Table 5).
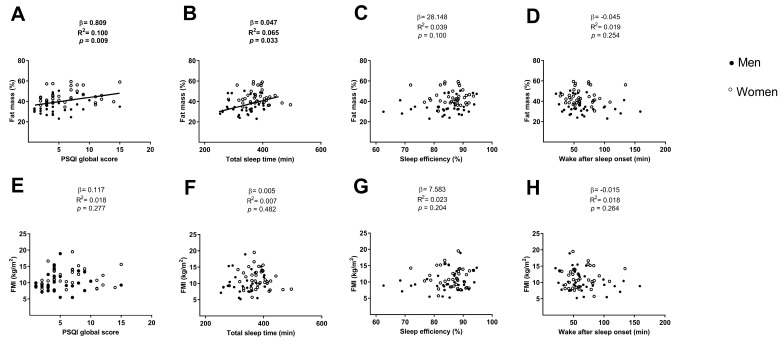
The PSQI global score and the total sleep time were positively associated with the fat mass percentage (β = 0.809, R2 = 0.100, p = 0.009; Figure 4A; β = 0.047, R2 = 0.065, p = 0.033; Figure 4B, respectively), which disappeared after including sex or both sex and age in the model (all p > 0.05; Table 2 and Table 3) and remained after including age in the model (β = 0.765, R2 = 0.106, p = 0.016; Table 2; β = 0.049, R2 = 0.109, p = 0.022; Table 3 respectively).
Figure 4.
Linear regression graphs between PSQI global score, total sleep time, sleep efficiency and wake after sleep onset with fat mass percentage (Panels A, B, C, and D, respectively) and with FMI (Panels E, F, G, and H, respectively). β—non-standardised linear regression coefficient; R2—Coefficient of determination; p value. Abbreviations: PSQI–Pittsburgh sleep quality index, FMI—fat mass index.
No association was found between the PSQI global score and the total sleep with the FMI (all p > 0.05; Figure 4E,F, respectively), neither after including sex, age or both sex and age in the model (all p > 0.05; Table 2 and Table 3, respectively).
No association was found between the sleep efficiency and the wake after sleep onset with the fat mass percentage and the FMI (all p > 0.05; Figure 4C,D respectively for fat mass percentage and Figure 4G and 4H respectively for FMI), neither when we included sex, age or both sex and age in the model (all p > 0.05; Table 4 and Table 5).
4. Discussion
The present study showed that a poor subjective sleep quality was negatively associated with BMC, BMD, lean mass and LMI, and positively associated with the fat mass percentage in middle-aged adults. However, no association was found between objective sleep quality and any body composition variable, neither when we accounted for sex and age.
Osteoporosis is a prevalent age-related disease characterized by low bone mass and microarchitectural deterioration of bone tissue [15], and a poor sleep quality could be a risk factor for osteoporosis and osteopenia in middle-aged adults [23]. A poor sleep quality could have different physiological effects that negatively influence the BMD: (i) Alteration of circadian rhythms that disrupt bone microstructure [24]; (ii) an elevation of pro-inflammatory cytokines [25], which are linked to osteoporosis [26]; (iii) an abnormal melatonin secretion [27], since low melatonin levels are related to bone disease and abnormality [28]; (iv) an elevation of cortisol [25], since cortisol hypersecretion decreases bone cell growth and decreases BMD [29]; (v) decreased levels of leptin [25], which adequate levels have been positively correlated with BMD [30]. All aforementioned mechanisms could negatively influence BMD increasing the risk of developing osteoporosis. Our results agree with others studies that demonstrated that poor sleep quality could be associated with low BMD in middle-aged women [12], in young men [31], and older adults [32].
Sarcopenia is the continuous and progressive age-related decline in skeletal muscle mass [16]. A poor quality of sleep has been demonstrated to be a risk factor for age-related sarcopenia [16]. There are several mechanisms that could explain the negative influence of poor sleep quality on lean mass: (i) An increment in the secretion of the catabolic hormone cortisol [33], which is known to stimulate degradation and inhibit synthesis of muscle proteins [34]; (ii) a disruption of the physiological rhythm of the anabolic hormone testosterone; (iii) an alteration of the secretion peak of the anabolic hormone growth hormone [25]; (iv) a decrease in insulin growth factor 1 (IGF-1) concentration [35], which has a key role in the stimulation of muscle protein synthesis [36]; (v) an increment of pro-inflammatory cytokines [25], which are related to muscle atrophy [36]; and (vi) an increase on insulin resistance [37], which may limit the muscle protein synthesis [38]. In relation to lean mass, our results agreed with those obtained by a cross-sectional study that included 1,196 elderly participants [13].
Obesity is characterized by an excessive accumulation of adiposity, which is highly prevalent during the ageing process [39]. A poor sleep quality increases inflammation [25], which is significantly elevated in obesity [40]. Additionally, poor sleep quality alters circadian rhythms increasing fatness through different mechanisms (i.e., dietary habits disruption, hormonal disruption, etc.) [41]. A poor sleep quality can disturb melatonin secretion [27], which has demonstrated to be the key mediator for the optimization of energy balance and body weight regulation [42], with a direct relationship with fatness and obesity [42]. Poor sleep quality is associated with low leptin and high ghrelin, which are likely to increase appetite, and consequently the risk of obesity [25]. It has been reported that low sleep quality decreases adiponectin levels [43], which is inversely correlated with adiposity [44]. Healthy individuals with poor sleep quality are more insulin resistant [37], which is associated with an increment in adiposity [45]. A poor sleep quality through all aforementioned mechanisms could increase adiposity, and consequently, increase the risk of developing obesity. In line with our results, previous studies reported a relationship between poor sleep quality and higher fat mass in middle-aged adults [46], young adolescents [47] and college students [14].
The lack of association between sleep parameters and body composition parameters when sex or age were accounted for, could be explain by: (i) The sex differences in sleep and sleep disorders between women and men [48], which could be based on differences in physiological conditions between sexes like menstrual cycles, male and female hormones [49] and differences in circadian rhythms [50] and (ii) the age-related sleep changes, and the common sleep disturbances that arise with advancing age [6].
Interestingly, we observed different results when the association between sleep quality and body composition was performed considering subjective sleep quality measured by a PSQI questionnaire versus objective sleep quality measured with an accelerometer. A previous study in youth observed that the PSQI and the accelerometer may measure different attributes of sleep, reporting the inadequate capacity of an accelerometry to detect wakefulness, thus lying in bed awake but motionless is likely to be coded as sleep [51]. Due to this limitation, using both complementary assessment methods (objective and subjective) to obtain detailed information beyond the limited data derived from body movements, is recommended [52].
This study has some limitations that have to be considered: Firstly, we cannot clarify by this cross-sectional study whether sleep quality contributes to maintenance adequate body composition variables (i.e., high BMD, low fat mass, and high lean mass), or whether the body composition status has a positive influence on sleep quality. Longitudinal studies are needed to clarify the direction of the association. Secondly, our study only included middle-aged sedentary adults, thus we cannot extrapolate our results to older, younger, and/or physically active individuals. Thirdly, the sample size of this study was relatively small. Finally, the lack of blood parameters mentioned above, does not allow for confirmation that the relationship is due to the proposed physiological mechanisms. Despite the aforementioned limitations, we measured sleep quality subjectively and objectively, which was indeed the strength of this study, since prior similar studies did not objectively measure sleep quality [12,13,14,31,32,46].
5. Conclusions
In conclusion, our study showed that a subjective poor sleep quality was negatively associated with BMC, BMD, lean mass and LMI whereas was positively associated with fat mass percentage in middle-aged adults. Interestingly, we observed different results when the association between sleep quality and body composition was performed considering subjective sleep quality measured by a PSQI questionnaire versus objective sleep quality measured with an accelerometer. Nevertheless, further studies are needed to confirm the observed association in individuals with similar and different characteristics since the sample size of this study was relatively small. Longitudinal studies are also required to establish the causal association between body composition variables and sleep quality.
Author Contributions
Conceptualization, M.J.C.; data curation, L.J.-F.; formal analysis, L.J.-F. and F.J.A.-G.; investigation, L.J.-F., F.J.A.-G., A.D.-l.-O. and M.D.-M.; methodology, F.J.A.-G.; project administration, Á.G. and M.J.C.; supervision, Angel Gutierrez; writing—original draft, Lucas Jurado-Fasoli; writing—review and editing, Francisco J.A.-G. and M.J.C.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Kohara K. Sarcopenic obesity in aging population: Current status and future directions for research. Endocrine. 2014;45:15–25. doi: 10.1007/s12020-013-9992-0. [DOI] [PubMed] [Google Scholar]
- 2.Prado C.M., Purcell S.A., Alish C., Pereira S.L., Deutz N.E., Heyland D.K., Goodpaster B.H., Tappenden K.A., Heymsfield S.B. Implications of low muscle mass across the continuum of care: a narrative review. Ann. Med. 2018:1–19. doi: 10.1080/07853890.2018.1511918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirschfeld H.P., Kinsella R., Duque G. Osteosarcopenia: Where bone, muscle, and fat collide. Osteoporos. Int. 2017;28:2781–2790. doi: 10.1007/s00198-017-4151-8. [DOI] [PubMed] [Google Scholar]
- 4.Hamer M., O’Donovan G. Sarcopenic obesity, weight loss, and mortality: The English Longitudinal Study of Ageing. Am. J. Clin. Nutr. 2017;106:125–129. doi: 10.3945/ajcn.117.152488. [DOI] [PubMed] [Google Scholar]
- 5.Gadie A., Shafto M., Leng Y., Kievit R.A. How are age-related differences in sleep quality associated with health outcomes ? An epidemiological investigation in a UK cohort of 2406 adults. BMJ Open. 2017;7:e014920. doi: 10.1136/bmjopen-2016-014920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crowley K. Sleep and sleep disorders in older adults. Neuropsychol. Rev. 2011;21:41–53. doi: 10.1007/s11065-010-9154-6. [DOI] [PubMed] [Google Scholar]
- 7.Medic G., Wille M., Hemels M.E. Short- and long-term health consequences of sleep disruption. Nat. Sci. Sleep. 2017;9:151–161. doi: 10.2147/NSS.S134864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lao X.Q., Liu X., Deng H., Chan T., Ho K.F., Wang F., Vermeulen R., Tam T., Wong M.C., Tse L.A., et al. Sleep quality, sleep duration, and the risk of coronary heart disease: A prospective cohort study with 60, 586 adults. J. Clin. Sleep Med. 2018;14:109–117. doi: 10.5664/jcsm.6894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lou P., Chen P., Zhang L., Zhang P., Yu J., Zhang N. Relation of sleep quality and sleep duration to type 2 diabetes: A population-based cross-sectional survey. BMJ. 2012;2:e000956. doi: 10.1136/bmjopen-2012-000956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nedeltcheva A.V., Scheer F.A. Metabolic effects of sleep disruption, links to obesity and diabetes. Curr. Opin. Endocrinol. Diabetes Obes. 2014;21:293–298. doi: 10.1097/MED.0000000000000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leary K.O., Bylsma L.M., Rottenberg J., Leary K.O., Bylsma L.M., Why J.R. Why might poor sleep quality lead to depression? A role for emotion regulation regulation. Cogn. Emot. 2016;31:1698–1706. doi: 10.1080/02699931.2016.1247035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albayrak I., Aydogmus M., Ozerbil O.M., Levendoglu F. The association between bone mineral density, quality of life, quality of sleep and fatigue. Acta Clin. Belg. 2016;71:92–98. doi: 10.1179/2295333715Y.0000000061. [DOI] [PubMed] [Google Scholar]
- 13.Buchmann N., Spira D., Norman K., Demuth I., Eckardt R., Steinhagen-Thiessen E. Sleep, muscle mass and muscle function in older people: a cross-sectional analysis based on data from the Berlin Aging Study II (BASE-II) Dtsch. Arztebl. Int. 2016;113:253–260. doi: 10.3238/arztebl.2016.0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karschin J., Breusing N., Bosy-Westphal A., Kahlh J. Relationship between actigraphy-assessed sleep quality and fat mass in college students. Obesity. 2016;24:335–341. doi: 10.1002/oby.21326. [DOI] [PubMed] [Google Scholar]
- 15.Sasaki N., Fujiwara S., Yamashita H., Ozono R., Teramen K., Kihara Y. Impact of sleep on osteoporosis: Sleep quality is associated with bone stiffness index. Sleep Med. 2016;25:73–77. doi: 10.1016/j.sleep.2016.06.029. [DOI] [PubMed] [Google Scholar]
- 16.Piovezan R.D., Abucham J., dos Santos R.V.T., Mello M.T., Tufik S., Poyares D. The impact of sleep on age-related sarcopenia: Possible connections and clinical implications. Ageing Res. Rev. 2015;23:210–220. doi: 10.1016/j.arr.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Beccuti G., Pannain S. Sleep and obesity. Curr. Opin. Clin. Nutr. Metab. Care. 2011;14:402–412. doi: 10.1097/MCO.0b013e3283479109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amaro-Gahete F.J., Jurado-Fasoli L., Espuch-Oliver A., Robles-Gonzalez L., Navarro-Lomas G., de Haro T., Femia P., Castillo M.J., Gutierrez A. Exercise training as S-Klotho protein stimulator in sedentary healthy adults: Rationale, design, and methodology. Contemp. Clin. Trials Commun. 2018;11:10–19. doi: 10.1016/j.conctc.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buysse D.J., Reynolds C.F., Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 20.Migueles J.H., Ulf C.C., Nystro C.D. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: A systematic review and practical considerations. Sport. Med. 2017;47:1821–1845. doi: 10.1007/s40279-017-0716-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shrivastava D., Jung S., Saadat M., Sirohi R., Crewson K. How to interpret the results of a sleep study. J. Community Hosp. Intern. Med. Perspect. 2014;4:24983. doi: 10.3402/jchimp.v4.24983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.OMS | Obesidad y Sobrepeso WHO 2016. [(accessed on 16 November 2018)]; Available online: http://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight.
- 23.Lucassen E.A., de Mutsert R., le Cessie S., Appelman-Dijkstra N.M., Rosendaal F.R., van Heemst D., den Heijer M., Biermasz N.R., NEO Study Group Poor sleep quality and later sleep timing are risk factors for osteopenia and sarcopenia in middle-aged men and women: The NEO study. PLoS ONE. 2017;12:e0176685. doi: 10.1371/journal.pone.0176685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lucassen E.A., Coomans C.P., van Putten M., de Kreij S.R., van Genugten J.H., Sutorius R.P., de Rooij K.E., van der Velde M., Verhoeve S.L., Smit J.W., Löwik C.W. Environmental 24-hr cycles are essential for health. Curr. Biol. 2016;26:1843–1853. doi: 10.1016/j.cub.2016.05.038. [DOI] [PubMed] [Google Scholar]
- 25.Banks S., Dinges D.F. Behavioral and physiological consequences of sleep restriction. J. Clin. Sleep Med. 2007;3:519–528. [PMC free article] [PubMed] [Google Scholar]
- 26.Lacativa P.G.S., Farias M.L.F.D. Osteoporosis and inflammation. Arq. Bras. Endocrinol. Metab. 2010;54:123–132. doi: 10.1590/S0004-27302010000200007. [DOI] [PubMed] [Google Scholar]
- 27.Claustrat B., Brun J., Chazot G. The basic physiology and pathophysiology of melatonin. Sleep Med. Rev. 2005;9:11–24. doi: 10.1016/j.smrv.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 28.Liu J., Huang F., He H. Melatonin effects on hard tissues: Bone and tooth. Int. J. Mol. Sci. 2013;14:10063–10074. doi: 10.3390/ijms140510063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chiodini I., Scillitani A. Role of cortisol hypersecretion in the pathogenesis of osteoporosis. Recenti Prog. Med. 2008;99:309–313. [PubMed] [Google Scholar]
- 30.Upadhyay J., Farr O.M., Mantzoros C.S. The role of leptin in regulating bone metabolism. Metabolism. 2016;64:105–113. doi: 10.1016/j.metabol.2014.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zakhem E., El R.H., Zunquin G., Jacob C., Moussa E., Theunynck D. Sleep quality is a determinant of hip bone mineral density in a group of young Lebanese men. J. Med. Liban. 2014;62:213–216. [PubMed] [Google Scholar]
- 32.Saint Martin M., Labeix P., Garet M., Thierry T., Barthélémy J.C., Collet P., Sforza E. Does subjective sleep affect bone mineral density in older people with minimal health disorders? The PROOF cohort. J. Clin. Sleep Med. 2016;12:1461–1469. doi: 10.5664/jcsm.6266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goodin B.R., Smith M.T., Quinn N.B., King C.D., McGuire L. Poor sleep quality and exaggerated salivary cortisol reactivity to the cold pressor task predict greater acute pain severity in a non-clinical sample. Biol. Psychol. 2012;91:36–41. doi: 10.1016/j.biopsycho.2012.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peeters G.M.E.E., Van Schoor N.M., Van Rossum E.F.C., Visser M., Lips P.T.A.M. The relationship between cortisol, muscle mass and muscle strength in older persons and the role of genetic variations in the glucocorticoid receptor. Clin. Endocrinol. (Oxf.) 2008;69:673–682. doi: 10.1111/j.1365-2265.2008.03212.x. [DOI] [PubMed] [Google Scholar]
- 35.Rusch H.L., Guardado P., Baxter T., Mysliwiec V., Gill J.M. Improved sleep quality is associated with reductions in depression and PTSD arousal symptoms and increases in IGF-1 concentrations. J. Clin. Sleep Med. 2015;11:615–623. doi: 10.5664/jcsm.4770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sandri M. Signaling in muscle atrophy and hypertrophy. Physiology. 2008;23:160–170. doi: 10.1152/physiol.00041.2007. [DOI] [PubMed] [Google Scholar]
- 37.Pyykkönen A.J., Isomaa B., Pesonen A.K., Eriksson J.G., Groop L., Tuomi T., Räikkönen K. Subjective sleep complaints are associated with insulin resistance in individuals without diabetes. Diabetes Care. 2012;35:2271–2278. doi: 10.2337/dc12-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gordon B.S., Kelleher A.R., Kimball S.R. Regulation of muscle protein synthesis and the effects of catabolic states. Int. J. Biochem. Cell Biol. 2013;45:2147–2157. doi: 10.1016/j.biocel.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Woo J. Obesity in older persons. Curr. Opin. Clin. Nutr. Metab. Care. 2015;18:5–10. doi: 10.1097/MCO.0000000000000113. [DOI] [PubMed] [Google Scholar]
- 40.Monteiro R., Azevedo I. Chronic inflammation in obesity and the metabolic syndrome. Mediat. Inflamm. 2010;2010:289645. doi: 10.1155/2010/289645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Potter G.D., Skene D.J., Arendt J., Cade J.E., Grant P.J., Hardie L.J. Circadian rhythm and sleep disruption: Causes, metabolic consequences, and countermeasures. Endocr. Rev. 2016;37:584–608. doi: 10.1210/er.2016-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cipolla-Neto J., Amaral F.G., Afeche S.C., Tan D.X., Reiter R.J. Melatonin, energy metabolism, and obesity: A review. J. Pineal. Res. 2014;56:371–381. doi: 10.1111/jpi.12137. [DOI] [PubMed] [Google Scholar]
- 43.Simpson N.S., Banks S., Arroyo S., Dinges D.F. Effects of sleep restriction on adiponectin levels in healthy men and women. Physiol. Behav. 2010;101:693–698. doi: 10.1016/j.physbeh.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goropashnaya A.V., Herron J., Sexton M., Havel P.J., Stanhope K.L., Plaetke R., Mohatt G.V., Boyer B.B. Relationships between plasma adiponectin and body fat distribution, insulin sensitivity, and plasma lipoproteins in Alaskan Yup’ik eskimos: The CANHR study. Metabolism. 2009;58:22–29. doi: 10.1016/j.metabol.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Patel P., Abate N. Body fat distribution and insulin resistance. Nutrients. 2013;5:2019–2027. doi: 10.3390/nu5062019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rahe C., Czira M.E., Teismann H., Berger K. Associations between poor sleep quality and different measures of obesity. Sleep Med. 2015;16:1225–1228. doi: 10.1016/j.sleep.2015.05.023. [DOI] [PubMed] [Google Scholar]
- 47.Ferranti R., Marventano S., Castellano S., Giogianni G., Nolfo F., Rametta S., Matalone M., Mistretta A. Sleep quality and duration is related with diet and obesity in young adolescent living in Sicily, Southern Italy. Sleep Sci. 2016;9:117–122. doi: 10.1016/j.slsci.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mallampalli M.P., Carter C.L. Exploring sex and gender differences in sleep health: A society for women’s health research report. J. Womens Health (Larchmt) 2014;23:553–562. doi: 10.1089/jwh.2014.4816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krishnan V., Collop N.A. Gender differences in sleep disorders. Curr. Opin. Pulm. Med. 2006;12:383–389. doi: 10.1097/01.mcp.0000245705.69440.6a. [DOI] [PubMed] [Google Scholar]
- 50.Santhi N., Lazar A.S., Mccabe P.J., Lo J.C., Groeger J.A., Dijk D.J. Sex differences in the circadian regulation of sleep and waking cognition in humans. Proc. Natl. Acad. Sci. USA. 2016;113:E2730–E2739. doi: 10.1073/pnas.1521637113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Berger I., Obeid J., Timmons B.W., DeMatteo C. Exploring accelerometer versus self-report sleep assessment in youth with concussion. Glob. Pediatr. Health. 2017;4:1–7. doi: 10.1177/2333794X17745973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sadeh A. The role and validity of actigraphy in sleep medicine: An update. Sleep Med. Rev. 2011;15:259–267. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]