Abstract
Metabolic syndrome (MetS) has been postulated to increase the risk for type 2 diabetes, cardiovascular disease and cancer. Adipose tissue (AT) plays an important role in metabolic homeostasis, and AT dysfunction has an active role in metabolic diseases. MetS is closely related to lifestyle and environmental factors. Epigenetics has emerged as an interesting landscape to evaluate the possible interconnection between AT and metabolic disease, since it can be modulated by environmental factors and metabolic status. The aim of this study was to determine whether MetS has an impact on the global DNA methylation pattern and the DNA methylation of several genes related to adipogenesis (PPARG, PPARA), lipid metabolism (RXRA, SREBF2, SREBF1, SCD, LPL, LXRb), and inflammation (LRP1 C3, LEP and TNF) in visceral adipose tissue. LPL and TNF DNA methylation values were significantly different in the control-case comparisons, with higher and lower methylation respectively in the MetS group. Negative correlations were found between global DNA methylation (measured by LINE-1 methylation levels) and the metabolic deterioration and glucose levels. There were associations among variables of MetS, BMI, and HOMA-IR with DNA methylation at several CpG positions for the studied genes. In particular, there was a strong positive association between serum triglyceride levels (TG) with PPARA and LPL methylation levels. TNF methylation was negatively associated with the metabolic worsening and could be an important factor in preventing MetS occurrence according to logistic regression analysis. Therefore, global DNA methylation and methylation at specific genes related to adipogenesis, lipid metabolism and inflammation are related to the etiology of MetS and might explain in part some of the features associated to metabolic disorders.
Keywords: epigenetics, DNA methylation, adipose tissue, metabolic syndrome
1. Introduction
Metabolic syndrome (MetS) is a cluster of metabolic alterations which altogether increase the risk of suffering diabetes, cardiovascular disease and cancer [1,2]. These metabolic risk factors include high glucose, TG, and blood pressure, low HDL cholesterol (HDL-c) and greater waist circumference [1]. Genetic and lifestyle factors have been shown to be important for the development and etiology of MetS [3].
DNA methylation is one of the epigenetic mechanisms present in the cell. It consists of the addition of a methyl group to the carbon 5 of a cytosine pyrimidine ring next to a guanidine nucleotide, which is commonly called a CpG residue. CpG islands (CpGi) are regions composed of a high incidence of repetitions in CpG di-nucleotides inside the genome. These CpGi are usually located in or near gene promoters and are usually hypo-methylated, while gene bodies and other intergenic regions are usually hypermethylated [4]. This hypomethylation at CpG promoter regions assures that the transcription starts at the beginning of the gene, avoiding truncated transcripts [5,6].
On the other hand, environmental and lifestyle factors are related to epigenetics and the DNA methylation status, as well as the development of metabolic disorders [7,8]. Thus, DNA methylation and other epigenetic mechanisms could be a regulatory landscape that could explain (at least in part) the etiology of MetS. In this regard, some studies have found an association between DNA methylation and MetS or metabolic variables related to MetS [3,9,10].
Adipose tissue (AT), traditionally considered a mere energy storage depot, has been recently proposed as a central player in metabolism and its function is usually dysregulated in metabolic disorders and cancer [11,12]. A lot of recently published literature shows that deregulation of genes important in metabolism and adipose tissue biology can affect adipose tissue function and in turn the whole metabolic state [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. Moreover, epigenetic deregulation has also been related to adipose tissue dysfunction, which can lead to metabolic disorders. In fact, our group has previously demonstrated that methylation levels of the LPL promoter are higher in the AT of MetS subjects, and these methylation levels are related to triglyceride withdrawal [3]. In agreement with our findings, it has been shown that dietary fatty acids can alter DNA methylation in AT [32].
Nevertheless, little is known about the association between MetS, global DNA methylation and the methylation status of genes related to the development of MetS in AT. Thus, the aim of this study was to analyze the overall DNA methylation state of visceral adipose tissue (VAT), as well as the DNA methylation at the promoter regions of specific genes related to adipogenesis (PPARG, PPARA), lipid metabolism (RXRA, SREBF2, SREBF1, SCD, LPL, LXRb), and inflammation (LRP1 C3, LEP, and TNF) in subjects with and without MetS.
2. Material and Methods
2.1. Study Population
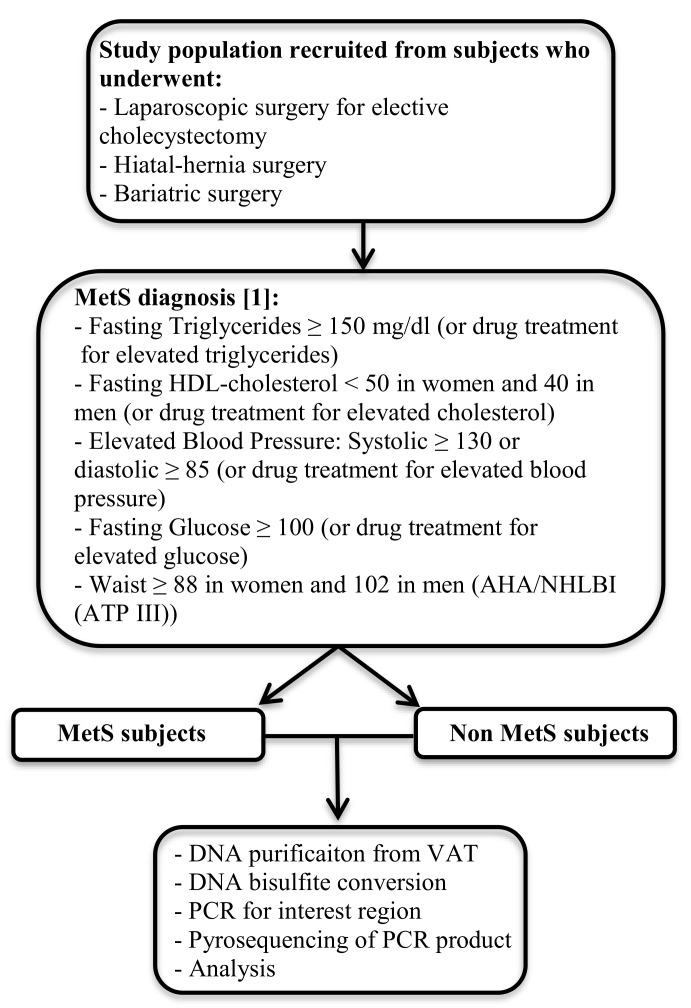
This case-control study was performed in 55 patients without metabolic syndrome (Non MetS) and 53 patients with MetS recruited between January 2012 and December 2014 from the Endocrinology and Nutrition Department at Virgen de la Victoria Hospital (Malaga, Spain). MetS and Non MetS study subjects were recruited from patients that had undergone laparoscopic surgery for elective cholecystectomy, hiatal-hernia, or bariatric surgery. MetS patients were included if they met three or more of the updated parameters for the diagnosis of MetS according to Alberti’s Harmonization definition [1] and Non-MetS patients were selected if they had fewer than three MetS parameters (Figure 1). With respect to the drug treatment for blood pressure, lipids, and glucoses in MetS patients, 32% were treated with blood pressure lowering drugs, 11% with lipid lowering drugs and 3% with glucose lowering drugs, while in the case of the Non MetS population only 5% were treated with blood pressure lowering drugs.
Figure 1.
Diagram presenting the workflow of the study to measure global and specific DNA methylation levels.
Exclusion criteria in both study groups included the presence of cardiovascular disease, arthritis, acute inflammatory disease, infectious disease, or renal disease.
Study procedures included a comprehensive physical examination and blood analysis. Smoking habits and alcohol consumption were measured using a standardized questionnaire.
The study was conducted in accordance with the guidelines laid down in the Declaration of Helsinki. All participants gave their written informed consent and the study was reviewed and approved by the Ethics and Research Committee of Virgen de la Victoria Hospital.
2.2. Laboratory Measurements
Serum glucose, cholesterol, triglycerides (TG) and HDL cholesterol (HDL-c) were measured in a Dimension auto analyzer (Dade Behring Inc., Deerfield, IL, USA) by enzymatic methods (Randox Laboratories Ltd., Crumlin, UK). The LDL cholesterol (LDL-c) was calculated from the Friedewald equation. Insulin was quantified by radioimmunoassay (BioSource International, Camarillo, CA, USA). Serum leptin and adiponectin levels were analyzed by enzyme immunoassay (ELISA) kits (respectively: DSL, Webster, FL, USA; and DRG Diagnostics GmbH, Marburg, Germany). The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated from fasting insulin and glucose with the following equation: HOMA-IR = fasting insulin (μIU/mL) × fasting glucose (mmol/L)/22.5 [33].
2.3. Visceral Adipose Tissue DNA Isolation and Pyrosequencing
VAT was obtained during laparoscopic surgery for elective cholecystectomy, hiatal-hernia or bariatric surgery. Biopsy samples were washed in physiological saline and were immediately frozen in liquid nitrogen. Biopsy samples were maintained at −80 °C until analysis.
The PyroMark® Q96 ID Pyrosequencing System (Qiagen, Seoul, South Korea) was used to determine the methylation status of the study genes. The following pre-made assays (Qiagen, Valencia, CA, USA) were used: PPARA (PM00082635) (Figure S1), RXRA (PM00144431) (Figure S2), LXRb (PM00190260) (Figure S3), SREBF1 (PM00178087) (Figure S4), SREBF2 (PM00082516) (Figure S5), SCD (PM00042196) (Figure S6), LPL (PM00037401) (Figure S7), LRP1 (PM00051835) (Figure S8), C3 (PM00189399) (Figure S9), and LEP (PM00129724) (Figure S10). For the analysis of LINE-1 a tested assay which included 6 CpG sites was used [34]. We developed the assay for TNF and PPARG using the MethPrimer software [35]. 5 CpG sites were analyzed for TNF (Figure S11) while 5 CpG (Figure S12) sites were analyzed for PPARG as well using the following primer sets: TNF, Forward: GGAAAGGATATTATGAGTATTGAAAGTATG, Reverse: ACACTCACCTCTTCCCTCTAA, Sequencing primer: ATTATGAGTATTGAAAGTATGAT; PPARG: Forward: AAGAGGATTAGGTTTAGAATAGTATGT, Reverse: AATAAACAATAACCTTTTCTTTTCCTAC, Sequencing primer: AAGAGGGGTTTTAAGT. DNA methylation analyses were performed using bisulfite-treated DNA followed by a highly quantitative analysis based on PCR-pyrosequencing. The bisulfite conversion was done with 2 µg genomic DNA isolated from VAT using Qiazol (Qiagen, Valencia, CA, USA) and 0.1 µM citrate ethanol solutions. Then, the PCR was performed in 25 µL total volume, with a final primer concentration of 0.2 M. One of the primers was biotinylated in order to purify the final PCR product using sepharose beads. The biotinylated PCR amplifications were purified using the pyrosequencing Vacuum Prep-Tool (Qiagen, Valencia, CA, USA). Finally, 15 µL of the PCR products were pyrosequenced using the PyroMark Q96 ID Pyrosequencing System (Qiagen, Seoul, South Korea), and 0.4 µM sequencing primer.
The methylation level was expressed as the percentage methylated cytosine over the sum of methylated and unmethylated cytosines. Non-CpG cytosine residues were used as built-in controls to verify bisulfite conversion. The values were expressed as the mean for all the sites. We also included unmethylated and methylated DNA as controls in each run (New England Biolabs, Ipswich, MA, USA). Inter-assay precision (%CV) was <2.5%, intra-assay (%CV) was <1.0%.
2.4. Statistical Analysis
Comparisons of the anthropometric and biochemical characteristics as well as the DNA methylation levels between the study groups were made with a non-parametric test (Mann–Whitney U test). A variable named “MetS index” formed by the number of MetS components present in each subject, which ranged from 0 to 5, was defined. The Pearson’s correlation coefficients were calculated to evaluate the association between LINE-1 methylation and the anthropometric and biochemical variables. The Spearman’s correlation coefficients were calculated to evaluate the association between the specific-site methylation levels and the anthropometric and biochemical variables. Multiple linear regression analyses were performed to evaluate the contribution of diverse CpG DNA methylation variables to the changes in the levels of triglycerides (TG). We performed a linear regression analysis with TG as the dependent variable and with the CpG sites which were significant in the correlation study as independent variables, controlling for age and gender. Moreover, we tested through logistic regression what CpG dinucleotide could be a risk factor for MetS. This model was corrected for age and gender. Values were considered to be statistically significant when p < 0.05. The correlation and mean differences between groups analyzed were performed with SPSS (Version 15.0 for Windows; SPSS Iberica, Madrid, Spain).
3. Results
3.1. Patient Characterization and Global Methylation
MetS patients showed a clear metabolic deterioration, with higher body mass index (BMI), waist circumference, glucose, insulin, HOMA-IR, TG, total cholesterol, LDL-c, apolipoprotein B (ApoB), systolic blood pressure (SBP), diastolic blood pressure (DBP) and leptin; and lower levels of HDL-c and adiponectin compared to the Non-MetS group (Table 1).
Table 1.
Biochemical and anthropometric parameters in non-metabolic syndrome subjects (Non MetS) and metabolic syndrome subjects (MetS).
| Non MetS (n = 55) | MetS (n = 53) | |
|---|---|---|
| Age (years) | 48.4 ± 13.9 | 52.7 ± 14.6 |
| Male/female (%) | 52/48 | 44/56 |
| BMI (Kg/m2) ** | 29.8 ± 7.9 | 36.4 ± 10.9 |
| WC (cm) ** | 97.6 ± 14.8 | 112.6 ± 22.4 |
| Glucose (mg/dL) ** | 94.3 ± 11.6 | 118.4 ± 29.5 |
| Insulin (pmol/L) ** | 9.8 ± 7.4 | 16.2 ± 11.4 |
| HOMA-IR ** | 2.3 ± 1.9 | 4.7 ± 3.4 |
| TG (mg/dL) ** | 101.6 ± 38.1 | 164.2 ± 65.1 |
| Cholesterol (mg/dL) ** | 194.0 ± 32.5 | 214.5 ± 41.3 |
| HDL-c (mg/dL) ** | 55.0 ± 11.0 | 48.5 ± 14.2 |
| LDL-c (Friedwald) * | 119.0 ± 31.8 | 135.1 ± 30.2 |
| ApoA1 (mg/dL) | 171.6 ± 21.8 | 160.5 ± 29.5 |
| ApoB (mg/dL) ** | 91.9 ± 22.3 | 108.7 ± 22.3 |
| SBP (mm Hg) ** | 123.5 ± 17.8 | 139.8 ± 19.5 |
| DBP (mm Hg) ** | 76.1 ± 11.2 | 82.7 ± 10.3 |
| GOT (mg/dL) | 20.0 ± 13.1 | 19.3 ± 8.7 |
| GPT (mg/dL) | 40.3 ± 23.9 | 44.6 ± 21.5 |
| GGT (mg/dL) | 57.4 ± 203.4 | 42.1 ± 27.9 |
| Uric acid (mg/dL) ** | 4.6 ± 1.2 | 5.6 ± 1.2 |
| Leptin (ng/mL) ** | 18.9 ± 23.8 | 38.1 ± 30.5 |
| Adiponectin (μg/mL) * | 11.2 ± 5.3 | 8.2 ± 4.1 |
Body mass index (BMI), waist circumference (WC), homeostatic model assessment of insulin resistance (HOMA-IR), baseline triglycerides (TG), high-density lipoprotein cholesterol (HDL-c), low density lipoprotein cholesterol (LDL-c), apolipoprotein A1 (ApoA1), Apolipoprotein B (ApoB), systolic blood pressure (SBP), diastolic blood pressure (DBP), glutamate-oxaloacetate transaminase (GOT), glutamate-pyruvate transaminase (GPT), gamma glutamyl transpeptidase (GGT). * p < 0.05 and ** p < 0.01 considered statistically significant according to a Student’s T-test and chi-squared test for gender.
In order to assess the global DNA methylation profile, DNA methylation at LINE-1 sequence was studied. Specifically, 6 CpG sites were included and pyrosequenced. The results showed no differences of global DNA methylation at any of the CpGs included between the study groups (Table 2).
Table 2.
DNA methylation level for each CpG position at LINE-1 pyrosequenced in both Non MetS and MetS groups. Values are given as the mean ± SE.
| Non MetS | MetS | |
|---|---|---|
| LINE-1 P1 (%) | 74.15 ± 0.39 | 74.37 ± 0.34 |
| LINE-1 P2 (%) | 65.84 ± 0.20 | 65.75 ± 0.33 |
| LINE-1 P3 (%) | 55.21 ± 0.29 | 55.29 ± 0.29 |
| LINE-1 P4 (%) | 61.37 ± 0.33 | 61.48 ± 0.24 |
| LINE-1 P5 (%) | 65.02 ± 0.17 | 65.24 ± 0.21 |
| LINE-1 P6 (%) | 65.05 ± 0.48 | 64.71 ± 0.23 |
Non metabolic syndrome group (Non MetS); metabolic syndrome group (MetS); long interspersed element 1 (LINE-1).
We also performed a correlation analysis to determine the possible relationship between the global DNA methylation and the variables related to MetS (Table 3). We found a negative correlation between LINE-1 P2 and the MetS index. Furthermore, there were negative correlations between glucose levels and LINE-1 P1, P2 and P5.
Table 3.
Pearson’s correlation between LINE-1 CpG positions (P1, P2, P3, P4, P5, P6) and the anthropometric and biochemical variables related to MetS. * p < 0.05 and ** p < 0.01 were considered statistically significant.
| MetS Index | BMI | Waist | Glucose | Tg | HDL-c | LDL-c | SBP | DBP | HOMA-IR | |
|---|---|---|---|---|---|---|---|---|---|---|
| LINE-1 P1 | −0.167 | 0.057 | −0.031 | −0.246 * | −0.088 | 0.113 | 0.082 | 0.162 | 0.02 | −0.114 |
| LINE-1 P2 | −0.233 * | 0.025 | −0.068 | −0.334 ** | −0.208 | 0.074 | 0.028 | 0.171 | 0.010 | −0.199 |
| LINE-1 P3 | −0.136 | 0.018 | −0.011 | −0.168 | −0.072 | −0.115 | 0.093 | 0.220 | 0.155 | −0.101 |
| LINE-1 P4 | −0.068 | 0.042 | 0.012 | −0.158 | 0.039 | −0.112 | 0.077 | 0.168 | 0.010 | −0.041 |
| LINE-1 P5 | −0.137 | 0.093 | −0.037 | −0.238 * | 0.016 | −0.139 | 0.05 | 0.136 | 0.100 | −0.088 |
| LINE-1 P6 | −0.19 | −0.055 | −0.05 | −0.137 | −0.166 | 0.028 | 0.052 | 0.066 | 0.016 | −0.126 |
Number of metabolic syndrome variables present in the subject of study (MetS index); body mass index (BMI); triglycerides (TG); high-density lipoprotein cholesterol (HDL-c); low-density lipoprotein cholesterol (LDL-c); systolic blood pressure (SBP); diastolic blood pressure (DBP); homeostatic model assessment of insulin resistance (HOMA-IR); long interspersed element 1 DNA methylation at positions 1 to 6 (LINE-1 P1–P6). * and ** mean p < 0.05 and p < 0.01 respectively according to Pearson’s correlation.
3.2. Gene Specific DNA Methylation in MetS versus Non MetS
3.2.1. Adipogenic and Lipid Metabolism Factors
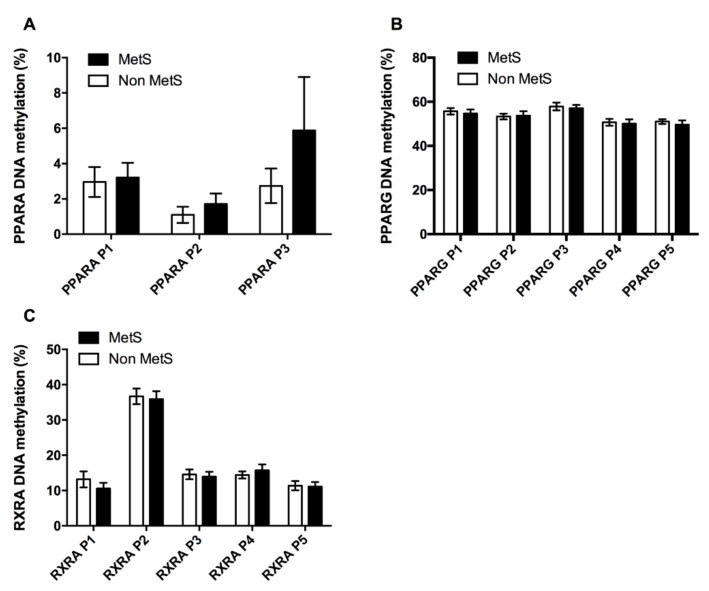
We studied genes related to adipose tissue development, such as PPARA, PPARG, and their heterodimer partner RXRA. As depicted in Figure 2, there were no differences in the methylation levels at any of the CpG sites analyzed for PPARA, PPARG or RXRA. Nevertheless, a tendency was observed for higher levels of DNA methylation in PPARA for MetS subjects than in Non MetS.
Figure 2.
Adipogenic factors DNA methylation. DNA methylation profile across the CpG analyzed at the promoters of the adipogenic factors PPARA (A), PPARG (B), and the PPARs partner RXRA (C) in both, Non MetS and MetS groups. Values are given as the mean ± SE. Peroxisome proliferator-activated receptor alpha (PPARA); Peroxisome proliferator-activated receptor gamma (PPARG); Retinoid X receptor alpha (RXRA).
In addition, we found a positive correlation between PPARA P2 with the MetS index, TG levels and HOMA-IR. PPARG P1 correlated positively with BMI, while PPARG P1 and P3 were negatively associated to DBP. In the case of the PPAR’s partner RXRA, we found a negative correlation between RXRA P1 and BMI and waist circumference.
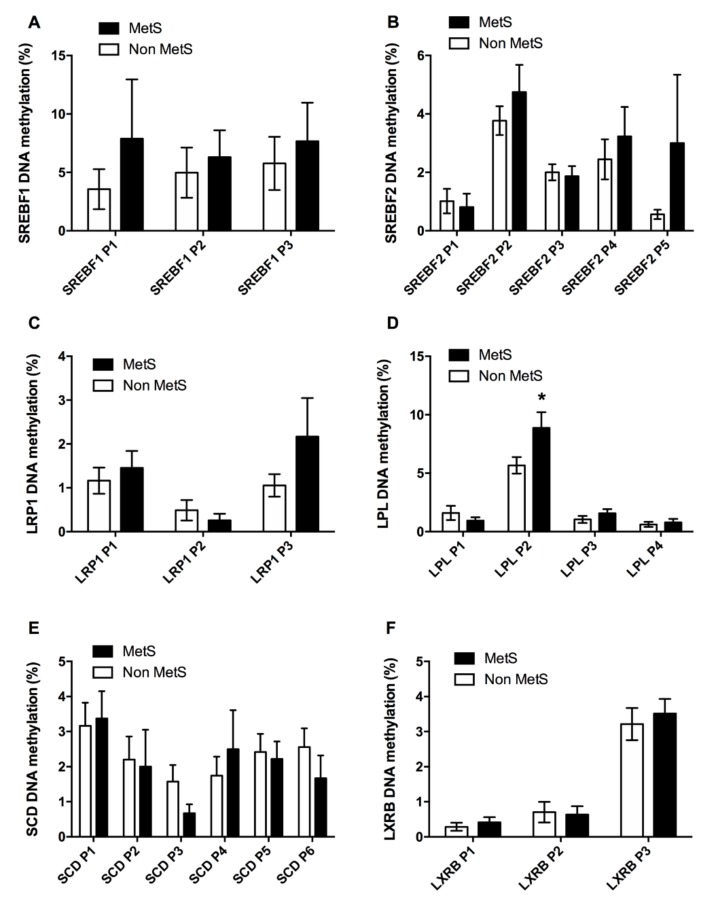
A set of CpG sites inside gene promoters related only to lipid metabolism was also pyrosequenced. No differences were found at any of the CpGs analyzed for SREBF1, SREBF2 or LRP1 (Figure 3A–C). In the case of LPL, we found an increase in the DNA methylation levels for the CpG sites located at position 2 (LPL P2) (Figure 3D). We did not find different levels of DNA methylation at any of the CpG studied for the SCD or LXRB genes (Figure 3E,F).
Figure 3.
Lipid metabolism DNA methylation. The figure shows the DNA methylation in Non MetS and MetS groups at each CpG for several factors related to lipid metabolism as SREBF1 (A), SREBF2 (B), LRP1 (C), LPL (D), SCD (E), and LXRB (F). Values are given as the mean ± SE. Sterol regulatory element binding transcription factor 1 (SREBF1); Sterol regulatory element binding transcription factor 2 (SREBF2); low density lipoprotein receptor-related protein 1 (LRP1); lipoprotein lipase (LPL); Stearoyl-CoA desaturase (SCD); liver X receptor beta (LXRB). * means p < 0.05 according to a Student’s T-test.
For these genes, we observed that the MetS index correlated negatively with SCD P6, while SCD P3 was negatively associated to BMI. Positive associations existed between TG levels and LPL P3, and between HDL-c and LRP1 P2. Furthermore, there was a negative association between the cholesterol regulator SREBF2 and DBP, specifically with SREBF2 P2.
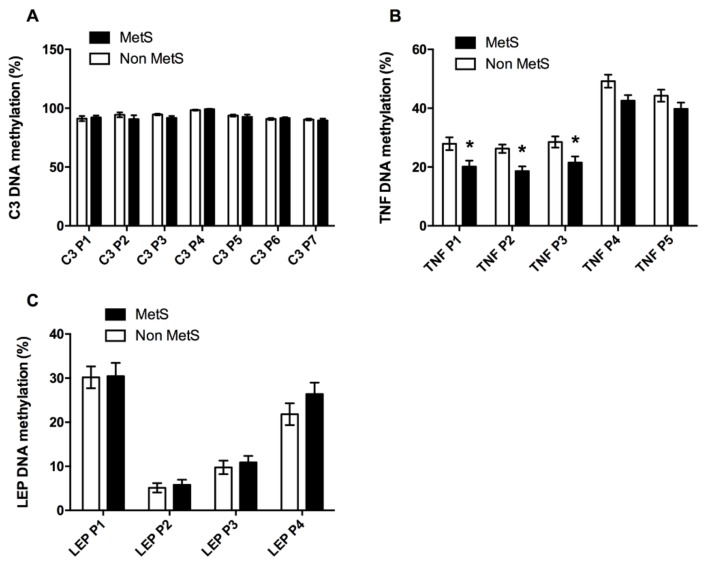
3.2.2. Inflammation Factors
Given the relationship between adipose tissue and inflammation in MetS, we analyzed some factors involved in this process. We analyzed 7 CpG sites inside the C3 gene promoter, but we did not find different DNA methylation levels between the Non MetS and the MetS subjects (Figure 4A). We also studied 5 CpG sites for the tumor necrosis factor (TNF). In this case, MetS subjects presented lower DNA methylation levels at 3 out of the 5 CpG sites that were analyzed, specifically at positions 1, 2 and 3 (TNF P1–P3) (Figure 4B). The third factor we studied was leptin (LEP), for which we analyzed 4 CpG sites at the leptin sequence, which did not present significant differences between Non MetS and MetS subjects (Figure 4C).
Figure 4.
Inflammatory promoters DNA methylation. Comparisons between the Non MetS and the MetS group for DNA methylation at different CpG from genes implied in inflammatory processes as C3 (A), TNF (B) and LEP (C). Values are given as the mean ± SE. Complement factor 3 (C3); tumor necrosis factor (TNF); leptin (LEP). * means p < 0.05 according to a Student’s T-test.
On the other hand, a negative relationship was found between the MetS index and the DNA methylation levels of TNF P2, TNF P3, TNF P4, and TNF P5 (Table 4). Glucose correlated negatively with the DNA methylation of TNF P4 (Table 4). For triglyceride levels, there were negative correlations found with TNF P2 and P5. Inversely to TG, HDL-c correlated positively with TNF P1, P2, P5 (Table 4).
Table 4.
Correlation analyses between anthropometric and biochemical variables associated to MetS with some of the DNA methylation at the CpG islands (CpGi) analyzed. Only CpG that presented any significant association are represented.
| MetS Index | BMI | Waist | Glucose | Tg | HDL-c | LDL-c | SBP | DBP | HOMA-IR | |
|---|---|---|---|---|---|---|---|---|---|---|
| PPARA P2 | 0.276 * | 0.076 | 0.165 | 0.166 | 0.392 ** | 0.061 | 0.08 | 0.066 | −0.025 | 0.229 * |
| PPARG P1 | −0.072 | 0.306 * | 0.169 | −0.224 | −0.194 | 0.015 | −0.197 | −0.2 | −0.293 * | −0.058 |
| PPARG P3 | −0.078 | 0.138 | 0.174 | 0.03 | −0.139 | 0.021 | −0.218 | 0.037 | −0.283 * | 0.112 |
| RXRA P1 | −0.102 | −0.298 ** | −0.229 * | −0.052 | 0.025 | −0.095 | 0.127 | −0.066 | −0.225 | −0.032 |
| SREBF2 P2 | 0.056 | 0.006 | 0.144 | 0.112 | 0.136 | −0.032 | 0.189 | −0.224 | −0.262 * | 0.121 |
| LRP1 P2 | 0.09 | −0.065 | −0.048 | 0.114 | −0.215 | 0.373 * | −0.055 | 0.192 | 0.180 | 0.251 |
| LPL P3 | 0.135 | 0.029 | 0.089 | 0.128 | 0.245 * | −0.102 | 0.085 | 0.126 | −0.111 | 0.149 |
| SCD P3 | −0.056 | −0.340 * | −0.283 | −0.096 | −0.018 | 0.108 | 0.22 | 0.087 | −0.117 | −0.03 |
| SCD P6 | −0.325 * | −0.116 | −0.17 | −0.141 | −0.134 | 0.121 | 0.102 | −0.275 | −0.232 | −0.172 |
| TNF P1 | −0.212 | 0.132 | 0.046 | −0.034 | −0.188 | 0.283 * | −0.02 | −0.010 | −0.115 | 0.029 |
| TNF P2 | −0.420 ** | 0.054 | −0.061 | −0.192 | −0.273 * | 0.304 * | −0.195 | −0.188 | −0.217 | −0.196 |
| TNF P3 | −0.320 * | 0.151 | −0.021 | −0.094 | −0.155 | 0.222 | −0.109 | −0.237 | −0.242 | −0.03 |
| TNF P4 | −0.330 * | −0.006 | −0.096 | −0.278 * | −0.203 | 0.098 | −0.295 * | −0.245 | −0.305 * | −0.133 |
| TNF P5 | −0.281 * | 0.132 | −0.100 | −0.153 | −0.281 * | 0.380 ** | −0.132 | −0.097 | −0.008 | −0.074 |
| LEP P1 | 0.088 | 0.081 | −0.159 | 0.061 | −0.071 | 0.015 | 0.229 * | 0.264 * | 0.230 * | 0.028 |
Number of metabolic syndrome variables present in the subject of study (MetS index); body mass index (BMI); Triglycerides (TG); high-density lipoprotein cholesterol (HDL-c); low-density lipoprotein cholesterol (LDL-c); systolic blood pressure (SBP); diastolic blood pressure (DBP); homeostatic model assessment of insulin resistance (HOMA-IR); peroxisome proliferator-activated receptor alpha DNA methylation at position 2 (PPARA P2); retinoid X receptor alpha methylation at position 1 (RXRA P1); leptin DNA methylation at position 1 (LEP P1); sterol regulatory element binding transcription factor DNA methylation at position 2 (SREBF2 P2); Stearoyl-CoA desaturase DNA methylation at positions 3 and 6 (SCD P3 and P6); Tumor necrosis factor DNA methylation at positions P1 to P5 (TNF P1–P5); peroxisome proliferator-activated receptor gamma DNA methylation at positions 1and 2 (PPARG P1 and P2); Lipoprotein lipase DNA methylation at position 3 (LPL P3); Low-density lipoprotein receptor-related protein 1 DNA methylation at position 2 (LRP1 P2). * and ** means p < 0.05 and p < 0.01 respectively.
There was also a negative correlation between TNF P4 and LDL-c and DBP. Furthermore, there were positive and significant correlations between LEP P1 and LDL-c, SBP and DBP (Table 4).
3.2.3. Regression Analyses
To study the strength of the association observed in the correlation analyses we performed lineal regression analyses. We observed that the DNA methylation levels of PPARA P2 and LPL P3 could explain TG levels (Table 5), a regression that was corrected for age, gender, and BMI.
Table 5.
Lineal regression analysis with fasting triglycerides as dependent variable and PPARA P2, LPL P3, and TNF P2 as independent variables and corrected for age, gender and BMI.
| Fasting triglycerides (R = 0.566; R2 = 0.320) | |||
|---|---|---|---|
| β | P | CI 95% | |
| Age | 0.111 | 0.425 | −0.582–1.358 |
| Gender | −0.268 | 0.047 | −48.377–(−0.312) |
| BMI | −0.101 | 0.446 | −1.825–0.816 |
| PPARA P2 | 0.332 | 0.012 | 1.32–10.012 |
| LPL P3 | 0.264 | 0.046 | 0.099–10.72 |
| TNF P2 | −0.117 | 0.347 | −1.867–0.669 |
Body mass index (BMI); peroxisome proliferator-activated receptor alpha DNA methylation at position 2 (PPARA P2); lipoprotein lipase DNA methylation at position 3 (LPL P3); tumor necrosis factor DNA methylation at position 2 (TNF P2).
Furthermore, we performed a logistic regression analysis (harmonized by step method) to determine what factors could predict the risk of having MetS. We observed that TNF P2 remained as a protective variable, with a reduction of 23% in the probability of having MetS per unit of DNA methylation increase (Table 6).
Table 6.
Logistic regression analysis: risk of MetS. The regression was conducted using a step method to look for the most harmonized model. Variables that showed a significant association with the MetS index at the correlation analyses, such as Age, gender, PPARA P2, SCD P6, and TNF P2 to P5, were introduced as independent variables and a harmonized model in which gender, PPARA P2, and TNF P2 were maintained was generated.
| Non Mets/MetS (R2 = 0.506–0.686) | |||
|---|---|---|---|
| OR | p | CI 95% | |
| Gender | 5.813 | 0.094 | 0.739–45.699 |
| PPARA P2 | 1.630 | 0.246 | 0.714–3.719 |
| TNF P2 | 0.791 | 0.008 | 0.664–0.942 |
Non metabolic syndrome group (Non MetS); Metabolic syndrome group (MetS); Peroxisome proliferator-activated receptor alpha DNA methylation at position 2 (PPARA P2); Tumor necrosis factor DNA methylation at position 2 (TNF P2).
4. Discussion
Epigenetic marks can be changed under developmental processes, nutritional conditions, exercise or metabolic status [36,37,38], highlighting the importance of epigenetics to fully understand the etiology of metabolic diseases. Altogether, our results show a general stability in the DNA methylation of the adipose tissue of our patients for the studied marks. The global methylation (LINE 1) remained stable between the study groups. However, some differences at specific genes were observed between groups. LPL and TNF genes were found to be especially affected, in line with our previous work where a difference in DNA methylation at the LPL promoter was described between subjects with and without MetS [3]. Even though the groups did not show great differences, the whole population showed interesting relationships with MetS components, something that may be indicative of the importance of the DNA methylation in metabolic disturbances.
Epigenetic marks, and concretely DNA methylation, are receiving increased attention to explain the etiology of metabolic diseases. LINE-1 DNA methylation levels have been proposed as a measurement of the global DNA methylation of an individual [39]. We observed a negative relationship between the LINE-1 DNA methylation levels and the MetS index and serum glucose levels. This supports previous data where a negative association was found between LINE-1 methylation and the worsening of MetS, and especially the glucose levels in obese patients [9]. Furthermore, it has been shown that lower LINE-1 methylation in blood cells is related to an improvement in impaired glucose metabolism after a physical activity intervention in subjects with glucose metabolism disorders [40]. Thus, our study expands this inverse relationship between LINE-1 methylation and the worsening of MetS and glucose metabolism to a population with a different range of BMI and metabolic disorders.
Examining the master genes of metabolism and adipogenesis, PPARA is a factor that stimulates β-oxidation and that is the pharmacological target of a group of TG-lowering drugs called fibrates [41,42]. DNA methylation changes in PPARA have been related with metabolic worsening in rats [41]. We found a positive correlation between the PPARA DNA methylation level and the MetS index, TG levels and HOMA-IR, in line with previous results [41,42]. PPARG is the other nuclear hormone receptor superfamily member we studied. PPARG DNA methylation levels showed a negative association with DBP and, more interestingly, a positive correlation with BMI. It is known that PPARG mRNA levels are negatively associated with BMI, and that obese people have lower expression levels of this gene, which has been associated with adipose tissue dysfunction [43]. PPARG down-regulation leads to impaired capacity of adipose tissue to accumulate lipids, which in turn provokes ectopic lipid accumulation, insulin resistance and other obesity-associated comorbidities [44]. Thus, this association observed between PPARG methylation and BMI is in accordance with previous studies [43,44]. Interestingly, a previous study has shown an increase in PPARG methylation and a decrease of PPARG mRNA associated with this DNA methylation increase in db/db and diet-induced obesity mice [45], which is in line with our results. Moreover, PPARG methylation deregulation has been described in the context of colorectal cancer, hepatitis B and liver inflammation and fibrosis associated with hepatitis B [46,47,48].
Both, PPARA and PPARG receptors carry out their actions by a heterodimer formed with their partner RXRA [49]. We observed a negative correlation between adipose tissue RXRA methylation and the BMI and waist circumference. Contrary to this result, but in a non-metabolic tissue, RXRA hypermethylation in the umbilical cord has been associated with higher adiposity later in childhood, a methylation status dependent on maternal nutrition [50].
Dysfunctional lipid metabolism is characteristic of metabolic diseases. Obesity has been traditionally correlated to low levels of HDL-c [51]. LRP1 is a factor involved in lipid homeostasis and it has been shown to be overexpressed in adipose tissue in obesity and to control intracellular cholesterol storage and fatty acid synthesis [52,53]. We found a positive association between LRP1 DNA methylation and HDL-c. Moreover, MetS patients exhibited higher levels of LPL methylation. LPL methylation levels together with PPARA methylation levels were capable of explaining fasting TG levels. This was in line with a previous study carried out by our group, where this LPL methylation not only explained fasting TG levels but also postprandial TG [3]. In addition, we found a negative relationship between SCD DNA methylation and BMI and the MetS index. SCD is a key enzyme in the conversion of polyunsaturated fatty acids (PUFAS) to monounsaturated fatty acids (MUFAS), and it has been shown to be overexpressed in adipose tissue in obesity and metabolic disorders. The absence of SCD has been related with an improvement of metabolic syndrome features in mice [54]. Furthermore, a decrease in SCD DNA methylation has been associated with weight loss in both a dietary intervention study and after bariatric surgery [55,56].
Adipose tissue inflammation, which can be the response of adipose tissue to overnutrition, is well documented in obesity and metabolic disorders. This inflammation can trigger a deterioration of the adipose tissue and in turn the metabolic state, which as a consequence reinforces the inflammatory process [57]. In this sense, we noted lower levels of TNF DNA methylation in MetS subjects compared to Non MetS subjects. We also found negative correlations between TNF methylation levels and the MetS index, BMI, TG, glucose, LDL-c and DBP, and a positive association with HDL-c. Thus, TNF methylation seems to be an epigenetic mark highly affected by MetS parameters, and is a risk factor for MetS according to our data. In line with our results, lower levels of adipose tissue TNF methylation have been described in diabetic subjects [58]. Besides, TNF methylation together with LEP DNA methylation in adipose tissue is capable of predicting responsiveness to a low-calorie diet [59]. Adipose tissue TNF is almost entirely produced by the macrophage fraction [60], and it is a gene highly expressed in M1 phenotype macrophages [61]. Moreover, in obesity and adipose tissue dysfunction there is a higher macrophage infiltration, and a polarization from the M2 phenotype to the pro-inflammatory M1 phenotype [60,62], a process that is epigenetically regulated [61,63,64,65]. Therefore, the lower levels of TNF methylation in MetS could be a sign of the macrophage cellularity in the tissue.
Lastly, LEP, a hormone secreted by adipose tissue known for exerting satiety, has been associated with pro-inflammatory processes as well [66]. LEP has been observed to stimulate a blood pressure rise in a process involving the sympathetic nervous system and kidney Na+ reabsorption. Leptin-resistance associated with obesity might, though, be prompting the related blood pressure increase [67,68]. We observed a positive relationship between LEP methylation and blood pressure, which at first would not agree with previous results unless due to a compensatory mechanism trying to re-establish lower leptin levels. Moreover, it is known that leptin can regulate cholesterol ester (CE) metabolism by activating the Hormone-sensitive Lipase (HSL) in macrophages, an enzyme that carries out the breakdown of CE, therefore protecting against atherosclerosis [69]. A positive association has also been shown between LEP methylation and LDL-c, both in blood cells and subcutaneous adipose tissue, in morbid obese subjects, whereas no association was found in visceral adipose tissue [70]. Our study showed a positive correlation between LEP DNA methylation in visceral adipose tissue and LDL-c in the whole study population.
This study has as limitations the number of factors studied and its cross-sectional nature that does not allow us to infer causality, and that the duration of MetS was not measured. Nevertheless, as strengths it provides an exploratory insight for the epigenetic state for some important factors involved in human adipose tissue function and that we found to be related to MetS and metabolic worsening.
5. Conclusions
In conclusion, we provide data supporting the idea that global DNA methylation and methylation at specific genes related to adipogenesis, lipid metabolism and inflammation in VAT are related to the etiology of MetS. We show that LINE-1 was positively associated with glucose. LPL and PPARA DNA methylation were strongly associated with TG levels, while TNF DNA methylation was associated with TG, glucose, HDL-c and blood pressure and SCD was negatively associated with MetS worsening. Finally, TNF DNA methylation could be an important factor in preventing MetS occurrence according to logistic regression analysis. Our study shows the importance of better understanding the epigenetic regulation of adipose tissue in order to widen the possible role of this tissue in the etiology of the MetS, which could lead to new therapeutic epigenetic strategies.
Acknowledgments
The research group belongs to the “Centros de Investigación en Red” [CIBER, CB06/03/0018] of the “Instituto de Salud Carlos III”. Daniel Castellano-Castillo was supported by a grant “FPU” (FPU13/04211), Isabel Moreno-Indias was supported by a ‘‘Miguel Servet Type I’’ contract from the Instituto de Salud Carlos III (CP16/00163), Jose Carlos Fernandez-Garcia from a grant (B-0033-2014) from Servicio Andaluz de Salud. María Isabel Queipo-Ortuño is a recipient of a “Miguel Servet Type II” program (CPI13/00003) co-funded by the Fondo Europeo de Desarrollo Regional - FEDER Madrid Spain and also belong to the regional “Nicolas Monardes” research program of the Consejería de Salud (C-0030-2018), Junta de Andalucía, Spain. Fernando Cardona acknowledges support from the Nicolas Monardes (C-0032-2016) from Consejería de Salud, co-funded by the Fondo Europeo de Desarrollo Regional—FEDER Madrid Spain. Bruno Ramos-Molina was recipient of a Sara Borrell postdoctoral fellowship, ISCIII, Spain (CD16/0003). This work was supported in part by a grant from the Instituto de Salud Carlos III co-founded by Fondo Europeo de Desarrollo Regional—FEDER, PI08/1655, PI11/02518, PI14/00082, Madrid Spain.
Abbreviations
| MetS | Metabolic syndrome |
| Non MetS | Non metabolic syndrome |
| CpGi | CpG island |
| VAT | Visceral adipose tissue |
| TG | Triglycerides |
| HOMA-IR | homeostasis model assessment of insulin resistance |
| BMI | Body mass index |
| LDL-c | LDL cholesterol |
| HDL-c | HDL cholesterol |
| SBP | Systolic blood pressure |
| DBP | Diastolic blood pressure |
| PUFAS | Monounsaturated fatty acids |
| PPARG | Peroxisome Proliferator Activated Receptor Gamma |
| PPARA | Peroxisome Proliferator Activated Receptor Alpha |
| RXRA | Retinoid X receptor alpha |
| SREBF1 | Sterol regulatory element-binding transcription factor 1 |
| SREBF2 | Sterol regulatory element-binding transcription factor 2 |
| SCD | Stearoyl-CoA desaturase |
| LXRB | Liver X receptor beta |
| LRP1 | Low density lipoprotein receptor-related protein 1 |
| C3 | Complement component 3 |
| TNF | Tumoral necrosis factor |
| LEP | Leptin |
Supplementary Materials
The following are available online at http://www.mdpi.com/2077-0383/8/1/87/s1, Figure S1: Genomic region overview of the promoter of PPARA gene; Figure S2: Genomic region overview of the promoter of RXRA gene; Figure S3: Genomic region overview of the promoter of LXRB gene; Figure S4: Genomic region overview of the promoter of SREBF1 gene; Figure S5: Genomic region overview of the promoter of SREBF2 gene; Figure S6: Genomic region overview of the promoter of SCD gene; Figure S7: Genomic region overview of the promoter of LPL gene; Figure S8: Genomic region overview of the promoter of LRP1 gene; Figure S9: Genomic region overview of the promoter of C3 gene; Figure S10: Genomic region overview of the promoter of LEP gene; Figure S11: Genomic region overview of the promoter of TNF gene; Figure S12: Genomic region overview of the promoter of PPARG gene.
Author Contributions
Conceptualization: F.C.; Funding acquisition: F.C.; Investigation: F.C.; Writing—original draft: D.C.-C.; Methodology: D.C.-C., J.A.-T., B.R.-M. and L.O.-W.; Data curation: I.M.-I., B.R.-M. and M.I.Q.-O.; Resources: M.I.Q.-O.; Formal analysis: I.M.-I. and D.C.-C.; Writing—review and editing: I.M.-I., L.S.-A., S.M., M.I.Q.-O. and F.C.; Visualization: D.C.-C.; Validation: F.T.; Supervision: M.I.Q.-O. and F.C.; The corresponding author and all of the authors have read and approved the final submitted manuscript and they participated in writhing and reviewing manuscript.
Funding
The authors have no financial or other contractual agreements.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Alberti K.G.M.M., Eckel R.H., Grundy S.M., Zimmet P.Z., Cleeman J.I., Donato K.A., Fruchart J.-C., James W.P.T., Loria C.M., Smith S.C. Harmonizing the Metabolic Syndrome: A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/circulationaha.109.192644. [DOI] [PubMed] [Google Scholar]
- 2.Uzunlulu M., Telci Caklili O., Oguz A. Association between Metabolic Syndrome and Cancer. Ann. Nutr. Metab. 2016;178:173–179. doi: 10.1159/000443743. [DOI] [PubMed] [Google Scholar]
- 3.Castellano-Castillo D., Moreno-Indias I., Fernandez-Garcia J.C., Alcaide-Torres J., Moreno-Santos I., Ocana L., Gluckman E., Tinahones F., Queipo-Ortuno M.I., Cardona F. Adipose Tissue LPL Methylation Is Associated with Triglyceride Concentrations in the Metabolic Syndrome. Clin. Chem. 2017 doi: 10.1373/clinchem.2017.277921. [DOI] [PubMed] [Google Scholar]
- 4.Suzuki M.M., Bird A. DNA Methylation Landscapes: Provocative Insights from Epigenomics. Nat. Rev. Genet. 2008;9:465–476. doi: 10.1038/nrg2341. [DOI] [PubMed] [Google Scholar]
- 5.Deaton A., Bird A. CpG Islands and the Regulation of Transcription. Genes Dev. 2011;25:1010–1022. doi: 10.1101/gad.2037511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones P.A. Functions of DNA Methylation: Islands, Start Sites, Gene Bodies and Beyond. Nat. Rev. Genet. 2012;13:484–492. doi: 10.1038/nrg3230. [DOI] [PubMed] [Google Scholar]
- 7.He Z., Zhang R., Jiang F., Hou W., Hu C. Role of Genetic and Environmental Factors in DNA Methylation of Lipid Metabolism. Genes Dis. 2018;5:9–15. doi: 10.1016/j.gendis.2017.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alegría-Torres J.A., Baccarelli A., Bollati V. Epigenetics and Lifestyle. Epigenomics. 2011;3:267–277. doi: 10.2217/epi.11.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turcot V., Tchernof A., Deshaies Y., Pérusse L., Bélisle A., Marceau S., Biron S., Lescelleur O., Biertho L., Vohl M.-C. LINE-1 Methylation in Visceral Adipose Tissue of Severely Obese Individuals Is Associated with Metabolic Syndrome Status and Related Phenotypes. Clin. Epigenet. 2012;4:10. doi: 10.1186/1868-7083-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ali O., Cerjak D., Kent J.W., James R., Blangero J., Carless M.A., Zhang Y. Methylation of SOCS3 Is Inversely Associated with Metabolic Syndrome in an Epigenome-Wide Association Study of Obesity. Epigenetics. 2016;11:699–707. doi: 10.1080/15592294.2016.1216284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hajer G.R., Van Haeften T.W., Visseren F.L.J. Adipose Tissue Dysfunction in Obesity, Diabetes, and Vascular Diseases. Eur. Heart J. 2008;29:2959–2971. doi: 10.1093/eurheartj/ehn387. [DOI] [PubMed] [Google Scholar]
- 12.Van Kruijsdijk R.C.M., van der Wall E., Visseren F.L.J. Obesity and Cancer: The Role of Dysfunctional Adipose Tissue. Cancer Epidemiol. Biomark. Prev. 2009;18:2569–2578. doi: 10.1158/1055-9965.EPI-09-0372. [DOI] [PubMed] [Google Scholar]
- 13.Clemente-Postigo M., Queipo-Ortuño M.I., Fernandez-Garcia D., Gomez-Huelgas R., Tinahones F.J., Cardona F. Adipose Tissue Gene Expression of Factors Related to Lipid Processing in Obesity. PLoS ONE. 2011;6:e24783. doi: 10.1371/journal.pone.0024783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang Z.G., de Boer I.H., Mackey R.H., Jensen M.K., Lai M., Robson S.C., Tracy R., Kuller L.H., Mukamal K.J. Associations of Insulin Resistance, Inflammation and Liver Synthetic Function with Very Low-density Lipoprotein: The Cardiovascular Health Study. Metabolism. 2015;65:92–99. doi: 10.1016/j.metabol.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mao H., Lockyer P., Li L., Ballantyne C.M., Patterson C., Xie L., Pi X. Endothelial LRP1 Regulates Metabolic Responses by Acting as a Co-Activator of PPARγ 3. Nat. Commun. 2017;8:14960. doi: 10.1038/ncomms14960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Au D.T., Strickland D.K., Muratoglu S.C. The LDL Receptor-Related Protein 1: At the Crossroads of Lipoprotein Metabolism and Insulin Signaling. J. Diabetes Res. 2017;2017 doi: 10.1155/2017/8356537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goto T., Lee J.-Y., Teraminami A., Kim Y.-I., Hirai S., Uemura T., Inoue H., Takahashi N., Kawada T. Activation of Peroxisome Proliferator-Activated Receptor-Alpha Stimulates Both Differentiation and Fatty Acid Oxidation in Adipocytes. J. Lipid Res. 2011;52:873–884. doi: 10.1194/jlr.M011320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cawthorn W.P., Scheller E.L., MacDougald O.A. Adipose Tissue Stem Cells Meet Preadipocyte Commitment: Going Back to the Future. J. Lipid Res. 2012;53:227–246. doi: 10.1194/jlr.R021089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sarantopoulos C.N., Banyard D.A., Ziegler M.E., Sun B., Shaterian A., Widgerow A.D. Elucidating the Preadipocyte and Its Role in Adipocyte Formation: A Comprehensive Review. Stem Cell Rev. Rep. 2018;14:27–42. doi: 10.1007/s12015-017-9774-9. [DOI] [PubMed] [Google Scholar]
- 20.Landa V., Zidek V., Mlejnek P., Simakova M., Silhavy J., Trnovska J., Kazdova L., Pravenec M. Sterol Regulatory Element Binding Protein 2 Overexpression Is Associated with Reduced Adipogenesis and Ectopic Fat Accumulation in Transgenic Spontaneously Hypertensive Rats. Physiol. Res. 2014;63:587–590. doi: 10.33549/physiolres.932751. [DOI] [PubMed] [Google Scholar]
- 21.Madison B.B. Srebp2: A Master Regulator of Sterol and Fatty Acid Synthesis. J. Lipid Res. 2016;57:333–335. doi: 10.1194/jlr.C066712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yew Tan C., Virtue S., Murfitt S., Robert L.D., Phua Y.H., Dale M., Griffin J.L., Tinahones F., Scherer P.E., Vidal-Puig A. Adipose Tissue Fatty Acid Chain Length and Mono-Unsaturation Increases with Obesity and Insulin Resistance. Sci. Rep. 2015;5:18366. doi: 10.1038/srep18366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ntambi J.M., Miyazaki M., Dobrzyn A. Regulation of Stearoyl-CoA Desaturase Expression. Lipids. 2004;39:1061–1065. doi: 10.1007/s11745-004-1331-2. [DOI] [PubMed] [Google Scholar]
- 24.Hoang M.H., Jia Y., Mok B., Jun H.J., Hwang K.Y., Lee S.J. Kaempferol Ameliorates Symptoms of Metabolic Syndrome by Regulating Activities of Liver X Receptor-β. J. Nutr. Biochem. 2015;26:868–875. doi: 10.1016/j.jnutbio.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Faulds M.H., Zhao C., Dahlman-Wright K. Molecular Biology and Functional Genomics of Liver X Receptors (LXR) in Relationship to Metabolic Diseases. Curr. Opin. Pharmacol. 2010;10:692–697. doi: 10.1016/j.coph.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 26.Paz-Filho G., Mastronardi C.A., Licinio J. Leptin Treatment: Facts and Expectations. Metabolism. 2015;64:146–156. doi: 10.1016/j.metabol.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 27.La Cava A. Leptin in Inflammation and Autoimmunity. Cytokine. 2017;98:51–58. doi: 10.1016/j.cyto.2016.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barbu A., Hamad O.A., Lind L., Ekdahl K.N., Nilsson B. The Role of Complement Factor C3 in Lipid Metabolism. Mol. Immunol. 2015;67:101–107. doi: 10.1016/j.molimm.2015.02.027. [DOI] [PubMed] [Google Scholar]
- 29.Castellano-Castillo D., Moreno-Indias I., Fernandez-Garcia J.C., Clemente-Postigo M., Castro-Cabezas M., Tinahones F.J., Queipo-Ortuño M.I., Cardona F. Complement Factor C3 Methylation and MRNA Expression Is Associated to BMI and Insulin Resistance in Obesity. Genes. 2018;9:410. doi: 10.3390/genes9080410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palacios-Ortega S., Varela-Guruceaga M., Algarabel M., Milagro F.I., Martínez J.A., De Miguel C. Effect of TNF-Alpha on Caveolin-1 Expression and Insulin Signaling during Adipocyte Differentiation and in Mature Adipocytes. Cell. Physiol. Biochem. 2015;36:1499–1516. doi: 10.1159/000430314. [DOI] [PubMed] [Google Scholar]
- 31.Srikanthan K., Feyh A., Visweshwar H., Shapiro J.I., Sodhi K. Systematic Review of Metabolic Syndrome Biomarkers: A Panel for Early Detection, Management, and Risk Stratification in the West Virginian Population. Int. J. Med. Sci. 2016;13:25–38. doi: 10.7150/ijms.13800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Perfilyev A., Dahlman I., Gillberg L., Rosqvist F., Iggman D., Volkov P., Nilsson E., Risérus U., Ling C. Impact of Polyunsaturated and Saturated Fat Overfeeding on the DNA-Methylation Pattern in Human Adipose Tissue: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2017;105:991–1000. doi: 10.3945/ajcn.116.143164. [DOI] [PubMed] [Google Scholar]
- 33.Matthews D.R., Hosker J.P., Rudenski A.S., Naylor B.A., Treacher D.F., Turner R.C. Homeostasis Model Assessment: Insulin Resistance and Beta-Cell Function from Fasting Plasma Glucose and Insulin Concentrations in Man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 34.Daskalos A., Nikolaidis G., Xinarianos G., Savvari P., Cassidy A., Zakopoulou R., Kotsinas A., Gorgoulis V., Field J.K., Liloglou T. Hypomethylation of Retrotransposable Elements Correlates with Genomic Instability in Non-Small Cell Lung Cancer. Int. J. Cancer. 2009;124:81–87. doi: 10.1002/ijc.23849. [DOI] [PubMed] [Google Scholar]
- 35.Li L.-C., Dahiya R. MethPrimer: Designing Primers for Methylation PCRs. Bioinformatics. 2002;18:1427–1431. doi: 10.1093/bioinformatics/18.11.1427. [DOI] [PubMed] [Google Scholar]
- 36.Panzeri I., Pospisilik J.A. Epigenetic Control of Variation and Stochasticity in Metabolic Disease. Mol. Metab. 2018;14:26. doi: 10.1016/j.molmet.2018.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davegårdh C., García-Calzón S., Bacos K., Ling C. DNA Methylation in the Pathogenesis of Type 2 Diabetes in Humans. Mol. Metab. 2018;14:12–25. doi: 10.1016/j.molmet.2018.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Donkin I., Barrès R. Sperm Epigenetics and Influence of Environmental Factors. Mol. Metab. 2018;14:1–11. doi: 10.1016/j.molmet.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang A.S. A Simple Method for Estimating Global DNA Methylation Using Bisulfite PCR of Repetitive DNA Elements. Nucleic Acids Res. 2004;32:e38. doi: 10.1093/nar/gnh032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martín-Núñez G.M., Rubio-Martín E., Cabrera-Mulero R., Rojo-Martínez G., Olveira G., Valdés S., Soriguer F., Castaño L., Morcillo S. Type 2 Diabetes Mellitus in Relation to Global LINE-1 DNA Methylation in Peripheral Blood: A Cohort Study. Epigenetics. 2014;9:1322–1328. doi: 10.4161/15592294.2014.969617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ohashi K., Munetsuna E., Yamada H., Ando Y., Yamazaki M., Taromaru N., Nagura A., Ishikawa H., Suzuki K., Teradaira R., et al. High Fructose Consumption Induces DNA Methylation at PPARα and CPT1A Promoter Regions in the Rat Liver. Biochem. Biophys. Res. Commun. 2015;468:185–189. doi: 10.1016/j.bbrc.2015.10.134. [DOI] [PubMed] [Google Scholar]
- 42.Shiomi Y., Yamauchi T., Iwabu M., Okada-Iwabu M., Nakayama R., Orikawa Y., Yoshioka Y., Tanaka K., Ueki K., Kadowaki T. A Novel Peroxisome Proliferator-Activated Receptor (PPAR)α Agonist and PPARy Antagonist, Z-551, Ameliorates High-Fat Diet-Induced Obesity and Metabolic Disorders in Mice. J. Biol. Chem. 2015;290:14567–14581. doi: 10.1074/jbc.M114.622191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Walczak R., Tontonoz P. PPARadigms and PPARadoxes: Expanding Roles for PPARγ in the Control of Lipid Metabolism. J. Lipid Res. 2002;43:177–186. [PubMed] [Google Scholar]
- 44.Soriguer F., Morcillo S., Cardona F., Rojo-martı G. Pro12Ala Polymorphism of the PPARG2 Gene Is Associated with Type 2 Diabetes Mellitus and Peripheral Insulin Sensitivity in a Population with a High Intake of Oleic Acid. J. Nutr. 2006;136:2325–2330. doi: 10.1093/jn/136.9.2325. [DOI] [PubMed] [Google Scholar]
- 45.Fujiki K., Kano F., Shiota K., Murata M. Expression of the Peroxisome Proliferator Activated Receptor Gamma Gene Is Repressed by DNA Methylation in Visceral Adipose Tissue of Mouse Models of Diabetes. BMC Biol. 2009;7:38. doi: 10.1186/1741-7007-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao Z.-H., Fan Y.-C., Zhao Q., Dou C.-Y., Ji X.-F., Zhao J., Gao S., Li X.-Y., Wang K. Promoter Methylation Status and Expression of Ppar-γ Gene Are Associated with Prognosis of Acute-on-Chronic Hepatitis B Liver Failure. Clin. Epigenet. 2015;7:115. doi: 10.1186/s13148-015-0149-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sabatino L., Fucci A., Pancione M., Colantuoni V. PPARG Epigenetic Deregulation and Its Role in Colorectal Tumorigenesis. PPAR Res. 2012;2012:687492. doi: 10.1155/2012/687492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhao Q., Fan Y.C., Zhao J., Gao S., Zhao Z.H., Wang K. DNA Methylation Patterns of Peroxisome Proliferator-Activated Receptor Gamma Gene Associated with Liver Fibrosis and Inflammation in Chronic Hepatitis B. J. Viral Hepat. 2013;20:430–437. doi: 10.1111/jvh.12048. [DOI] [PubMed] [Google Scholar]
- 49.Wells R.A., Chan L.S.A. Cross-Talk between PPARs and the Partners of RXR: A Molecular Perspective. PPAR Res. 2009;2009 doi: 10.1155/2009/925309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Godfrey K.M., Sheppard A., Gluckman P.D., Lillycrop K.A., Burdge G.C., Mclean C., Rodford J., Slater-jefferies J.L., Garratt E., Crozier S.R., et al. Epigenetic Gene Promoter Methylation at Birth Is Associated with Child’s Later Adiposity. Diabetes. 2011;60:1528–1534. doi: 10.2337/db10-0979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rashid S., GENEST J. Effect of Obesity on High-Density Lipoprotein Metabolism. Obesity. 2007;15:2875–2888. doi: 10.1038/oby.2007.342. [DOI] [PubMed] [Google Scholar]
- 52.Masson O., Chavey C., Dray C., Meulle A., Daviaud D., Quilliot D., Muller C., Valet P., Liaudet-Coopman E. LRP1 Receptor Controls Adipogenesis and Is Up-Regulated in Human and Mouse Obese Adipose Tissue. PLoS ONE. 2009;4:e7422. doi: 10.1371/journal.pone.0007422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Terrand J., Bruban V., Zhou L., Gong W., El Asmar Z., May P., Zurhove K., Haffner P., Philippe C., Woldt E., et al. LRP1 Controls Intracellular Cholesterol Storage and Fatty Acid Synthesis through Modulation of Wnt Signaling. J. Biol. Chem. 2009;284:381–388. doi: 10.1074/jbc.M806538200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Macdonald M.L.E., Singaraja R.R., Bissada N., Ruddle P., Karasinska J.M., Gibson W.T., Fievet C., Vance J.E., Staels B., Hayden M.R. Absence of Stearoyl-CoA Desaturase-1 Ameliorates Features of the Metabolic Syndrome in LDLR-Deficient Mice. J. Lipid Res. 2016;49:217–229. doi: 10.1194/jlr.M700478-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Martín-Núñez G.M., Cabrera-Mulero R., Rubio-Martín E., Rojo-Martínez G., Olveira G., Valdés S., Soriguer F., Castaño L., Morcillo S. Methylation Levels of the SCD1 Gene Promoter and LINE-1 Repeat Region Are Associated with Weight Change: An Intervention Study. Mol. Nutr. Food Res. 2014;58:1528–1536. doi: 10.1002/mnfr.201400079. [DOI] [PubMed] [Google Scholar]
- 56.Morcillo S., Martín-Núñez G.M., García-Serrano S., Gutierrez-Repiso C., Rodriguez-Pacheco F., Valdes S., Gonzalo M., Rojo-Martinez G., Moreno-Ruiz F.J., Rodriguez-Cañete A., et al. Changes in SCD Gene DNA Methylation after Bariatric Surgery in Morbidly Obese Patients Are Associated with Free Fatty Acids. Sci. Rep. 2017;7:46292. doi: 10.1038/srep46292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Reilly S.M., Saltiel A.R. Adapting to Obesity with Adipose Tissue Inflammation. Nat. Rev. Endocrinol. 2017;13:633–643. doi: 10.1038/nrendo.2017.90. [DOI] [PubMed] [Google Scholar]
- 58.Zhang J., Wang C., Ha X., Li W., Xu P., Gu Y., Wang T., Wang Y., Xie J. DNA Methylation of Tumor Necrosis Factor-α, Monocyte Chemoattractant Protein-1, and Adiponectin Genes in Visceral Adipose Tissue Is Related to Type 2 Diabetes in the Xinjiang Uygur Population. J. Diabetes. 2017;9:699–706. doi: 10.1111/1753-0407.12478. [DOI] [PubMed] [Google Scholar]
- 59.Cordero P., Campion J., Milagro F.I., Goyenechea E., Steemburgo T., Javierre B.M., Martinez J.A. Leptin and TNF-Alpha Promoter Methylation Levels Measured by MSP Could Predict the Response to a Low-Calorie Diet. J. Physiol. Biochem. 2011;67:463–470. doi: 10.1007/s13105-011-0084-4. [DOI] [PubMed] [Google Scholar]
- 60.Moreno-indias I., Oliva-olivera W., Omiste A., Castellano-castillo D., Lhamyani S., Camargo A., Tinahones F.J. Adipose Tissue Infiltration in Normal-Weight Subjects and Its Impact on Metabolic Function. Transl. Res. 2016;172:6.e3–17.e3. doi: 10.1016/j.trsl.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 61.Wang X., Cao Q., Yu L., Shi H., Xue B., Shi H. Epigenetic Regulation of Macrophage Polarization and Inflammation by DNA Methylation in Obesity. JCI Insight. 2016;1:e87748. doi: 10.1172/jci.insight.87748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cawthorn W.P., Sethi J.K. TNF-α and Adipocyte Biology. FEBS Lett. 2008;582:117–131. doi: 10.1016/j.febslet.2007.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yang X., Wang X., Liu D., Yu L., Xue B., Shi H. Epigenetic Regulation of Macrophage Polarization by DNA Methyltransferase 3b. Mol. Endocrinol. 2014;28:565–574. doi: 10.1210/me.2013-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhou D., Yang K., Chen L., Zhang W., Xu Z., Zuo J., Jiang H., Luan J. Promising Landscape for Regulating Macrophage Polarization: Epigenetic Viewpoint. Oncotarget. 2015;8:57693–57706. doi: 10.18632/oncotarget.17027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Baardman J., Licht I., de Winther M.P., Van den B.J. Metabolic–Epigenetic Crosstalk in Macrophage Activation. Epigenomics. 2015;7:1155–1164. doi: 10.2217/epi.15.71. [DOI] [PubMed] [Google Scholar]
- 66.Iikuni N., Lam Q.L.K., Lu L., Matarese G., La Cava A. Leptin and Inflammation. Curr. Immunol. Rev. 2008;4:70–79. doi: 10.2174/157339508784325046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Beltowski J. Role of Leptin in Blood Pressure Regulation and Arterial Hypertension. J. Hypertens. 2006;24:789–801. doi: 10.1097/01.hjh.0000222743.06584.66. [DOI] [PubMed] [Google Scholar]
- 68.Simonds S.E., Pryor J.T., Ravussin E., Greenway F.L., Dileone R., Allen A.M., Bassi J., Elmquist J.K., Keogh J.M., Henning E., et al. Leptin Mediates the Increase in Blood Pressure Associated with Obesity. Cell. 2014;159:1404–1416. doi: 10.1016/j.cell.2014.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.O’Rourke L., Yeaman S.J., Shepherd P.R. Insulin and Leptin Acutely Regulate Cholesterol Ester Metabolism in Macrophages by Novel Signaling Pathways. Diabetes. 2001;50:955–961. doi: 10.2337/diabetes.50.5.955. [DOI] [PubMed] [Google Scholar]
- 70.Houde A.A., Légaré C., Biron S., Lescelleur O., Biertho L., Marceau S., Tchernof A., Vohl M.C., Hivert M.F., Bouchard L. Leptin and Adiponectin DNA Methylation Levels in Adipose Tissues and Blood Cells Are Associated with BMI, Waist Girth and LDL-Cholesterol Levels in Severely Obese Men and Women. BMC Med. Genet. 2015;16:29. doi: 10.1186/s12881-015-0174-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.