Abstract
The measurement of Pavlovian forms of fear extinction offers a relatively simple behavioral preparation that is nonetheless tractable, from a translational perspective, as an approach to study mechanisms of exposure therapy and biological underpinnings of anxiety and trauma-related disorders such as post-traumatic stress disorder (PTSD). Deficient fear extinction is considered a robust clinical endophenotype for these disorders and, as such, has particular significance in the current “age of RDoC (research domain criteria).” Various rodent models of impaired extinction have thus been generated with the objective of approximating this clinical, relapse prone aberrant extinction learning. These models have helped to reveal neurobiological correlates of extinction circuitry failure, gene variants, and other mechanisms underlying deficient fear extinction. In addition, they are increasingly serving as tools to investigate ways to therapeutically overcome poor extinction to support long-term retention of extinction memory and thus protection against various forms of fear relapse; modeled in the laboratory by measuring spontaneous recovery, reinstatement and renewal of fear. In the current article, we review models of impaired extinction built around (1) experimentally induced brain region and neural circuit disruptions (2) spontaneously-arising and laboratory-induced genetic modifications, or (3) exposure to environmental insults, including stress, drugs of abuse, and unhealthy diet. Collectively, these models have been instrumental in advancing in our understanding of extinction failure and underlying susceptibilities at the neural, genetic, molecular, and neurochemical levels; generating renewed interest in developing novel, targeted and effective therapeutic treatments for anxiety and trauma-related disorders.
Keywords: Threat conditioning, Deficient fear inhibition, Anxiety drug development, Sex differences, Fear extinction, Cognitive behavioral therapy, Medial prefrontal cortex, Amygdala
Canst thou not minister to a mind diseased,
Pluck from the memory a rooted sorrow,
Raze out the written troubles of the brain…
Shakespeare, Macbeth
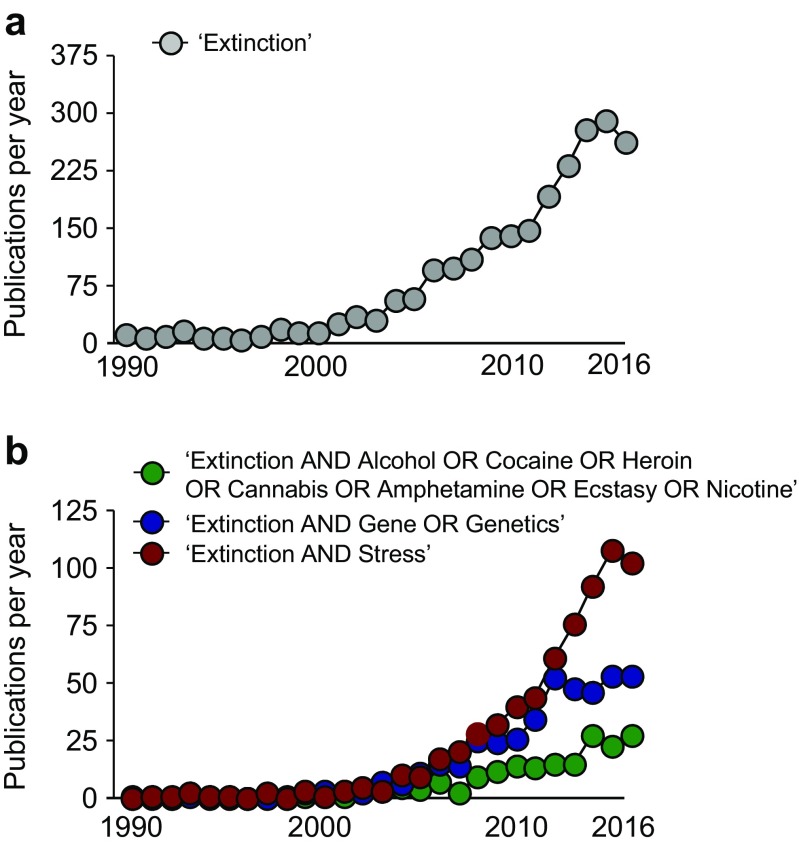
Fear extinction: from Pavlov to the present
It is almost 100 years since I.P. Pavlov (1849–1936) described extinction as a phenomenon whereby repeated non-reinforced presentation of a conditioned stimulus (CS) led to the reduction in the magnitude of the conditioned response(s) (CR) (Pavlov 1927). In the case of fear extinction, the CS is typically a previously neutral stimulus that, through conditioning, has come to be associated with an aversive outcome, such that its occurrence alone is capable of eliciting some form(s) of fear/anxiety/defensive CR. The CR, and the degree of its diminution in amplitude and frequency under extinction, can be objectively measured and quantified in the laboratory in human (e.g., galvanic skin response, startle) and rodent (e.g., startle, freezing) subjects and has even been documented in invertebrates (Eisenhardt 2014). In part because of its conceptual appeal as an (ostensibly) straightforward psychological phenomenon and the relative ease of measurement across species in the laboratory, fear extinction has become an increasingly popular behavioral assay in clinical and preclinical settings alike (Flores et al. 2018; Hariri and Holmes 2015). Pavlov would no doubt be astonished at the number of research publications that now in some way make use of fear extinction (Fig. 1).
Fig. 1.
The growing popularity of rodent models of impaired fear extinction. A PubMed search was performed for the years 1990–2016 (inclusive), using the search term “Extinction” (a) or a combination of the terms “Extinction AND Alcohol OR Cocaine OR Heroin OR Cannabis OR Amphetamine OR Ecstasy OR Nicotine,” “Extinction AND Gene OR Genetics,” or “Extinction AND Stress” (b)
In addition to being relatively easy to compare readouts of fear extinction between humans and rodents, given the similarity of laboratory testing procedures, there are a number of other factors that give extinction translational appeal. First, as summarized below, many of the brain regions that have been connected in some way to effective or deficient fear extinction, respectively, are common across humans and rodents—lending credence to the idea that findings at the neural level in one species are informative to the other (Milad and Quirk 2012). Second, fear extinction has repeatedly been found to be impaired in various psychiatric conditions associated with trauma, notably PTSD, but also phobias, panic disorder, and obsessive-compulsive disorder (Lissek et al. 2005; Milad et al. 2008; Milad et al. 2009; Rauch et al. 2006; Rosen and Schulkin 1998; Wicking et al. 2016; Zuj et al. 2016). Indeed, poor fear extinction efficacy is linked to the persistence and treatment resistance of symptoms in PTSD (King et al. 2018b; Sijbrandij et al. 2013). Deficient fear extinction therefore represents a robust clinical endophenotype for these disorders and, as such, has particular significance in the current “age of RDoC” (Anderzhanova et al. 2017; Lonsdorf and Richter 2017). Third, extinction in rodents is impaired by known factors in the etiology of trauma-related conditions—we discuss some of these factors in greater detail below. Fourth, the extinction of unwanted responses to reminders of (a) prior trauma(s) is a core process underlying exposure therapy for PTSD and other anxiety disorders. Indeed, individual differences in fear extinction in humans are predictive of the degree of fear reductions produced by exposure therapy (Ball et al. 2017; Waters and Pine 2016) and enhanced extinction recall positively predicts cognitive behavioral therapy (CBT) outcome in, for example, social anxiety disorder (Ball et al. 2017; Berry et al. 2009; Forcadell et al. 2017).
The importance of models of impaired extinction
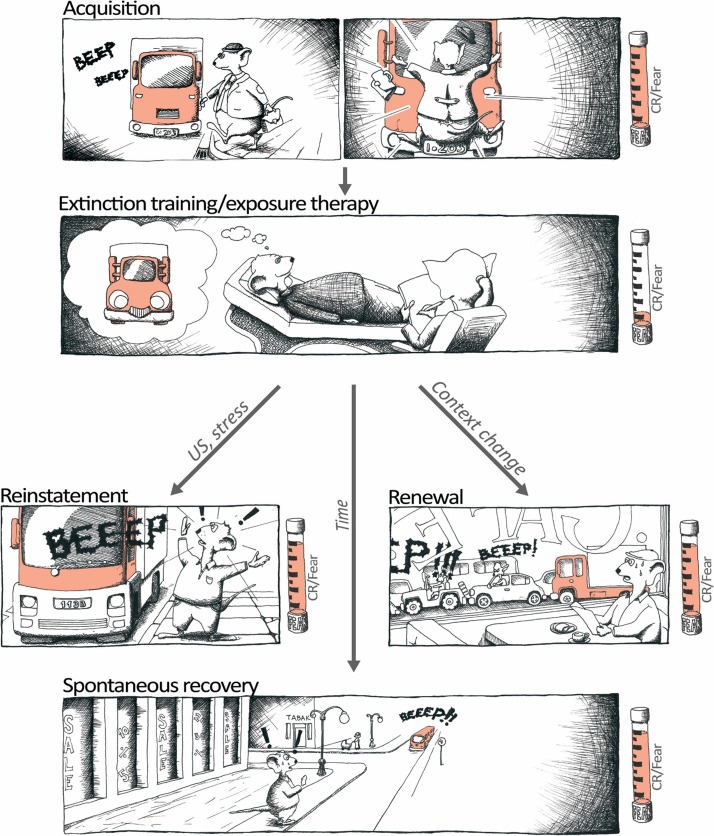
The various facets of fear extinction support the face, construct and predictive validity of this measure as a behavior and higher-order neural process of relevance to both the pathophysiology and treatment of PTSD and other emotional disorders. There is a pressing need for such translationally relevant experimental paradigms because emotional disorders are at globally pandemic proportions (Craske et al. 2017) and resistance to current treatments remains a major constraint to recovery (Sippel et al. 2018). While exposure therapy can be successful in alleviating anxiety, fear extinction is an inherently fragile form of inhibitory memory that is prone to reinstatement (in the face of stressors), spontaneous recovery (with the passage of time) and renewal of fear (in non-extinction contexts) (Bouton 2014; King et al. 2018b; Vervliet and Raes 2013) (Fig. 2). These examples of fear relapse are observed in individuals having undergone exposure therapy and follow-up assessments. It has therefore been proposed that failure to build fear inhibitory associations can explain the high rates of fear relapse in anxiety disorder patients (Craske et al. 2014). The risk of relapse thus remains a major limitation of current therapies and advocates for the importance of models that capture not just the extinction process per se, but a scenario more closely approximating to the clinical, relapse-prone, clinical picture of impaired extinction.
Fig. 2.
Relapse of extinguished fear poses an important challenge in behavioral, extinction-based therapies. This cartoon depicts three of the principal ways relapse can occur and which can be modeled in the laboratory both in animals and humans by return of fear paradigms. Reinstatement: the return of fear following exposure to the original US or stressors. Renewal: the return of fear following exposure to the original trauma-associated context or to contexts that otherwise differ from the therapy-context. Spontaneous recovery: the return of fear simply with the passage of time since therapy. CR conditioned response; US, unconditioned stimulus
Much has already been written on the topic of extinction. In the current article, our goal is not to attempt a summary of the vast literature pertaining to fear extinction. Rather, we aim to highlight some of the work that has been directed at studying and developing rodent models of impaired fear extinction. This is because as already noted, by recapitulating the deficient extinction present in anxiety and trauma-related disorders, these models arguably have the greatest potential to reveal insight into important aspects of the pathophysiology of these disorders. Furthermore, a better understanding of the mechanisms of impaired extinction and the associated limitations of current therapeutic strategies forms a solid platform for designing new approaches to more effective therapeutics (Bukalo et al. 2014; Graham et al. 2011; Singewald et al. 2015).
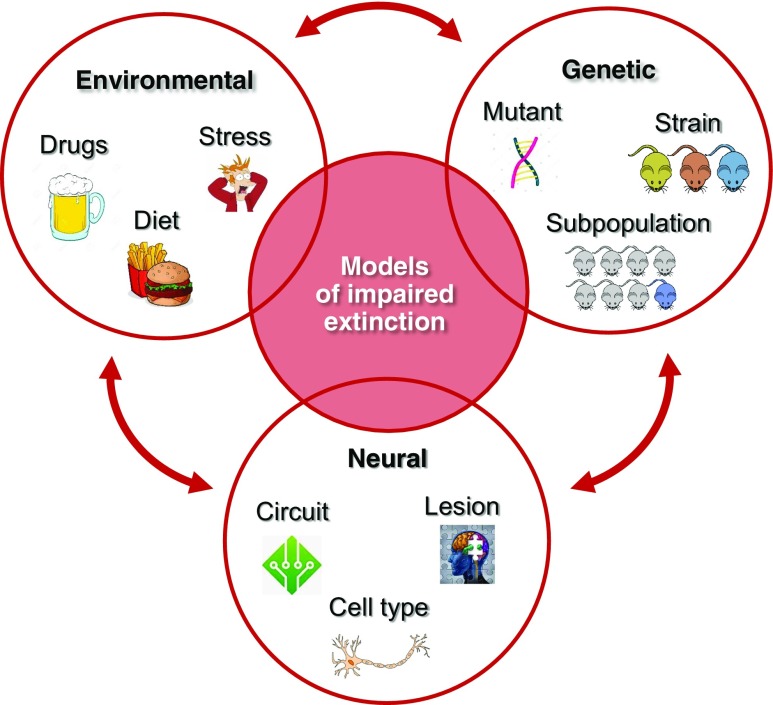
We place models into somewhat arbitrary subcategories based on how the impairment in fear extinction was produced: by disruptions to neural function, via genetic engineering or spontaneous variations, or from other factors including environmental insults such as drug, bad diet, or stress exposure (Fig. 3). A “model” in this context is a subject exhibiting an impairment in extinction as a result of one (or more) of these factors, and is distinguished from the use of fear extinction as a test or assay (Cryan and Holmes 2005). We have not included models of impaired extinction of avoidance behavior and refer the reader to excellent recent review of this emerging literature (Rodriguez-Romaguera and Quirk 2017). We acknowledge from the outset that the scope of the article is far from exhaustive and does not cover a great deal of important research, particularly with regard to pharmacologically induced deficits in extinction already covered in earlier reviews (Giustino and Maren 2018; Singewald et al. 2015).
Fig. 3.
Some of the main classes of models of impaired extinction
Nonetheless, relevant examples for each category are shown in Table 1, together with observed evidence of corresponding extinction-circuit abnormalities. In these examples and elsewhere, we dissociate impairments (i.e., delayed and/or no/insufficient reductions in conditioned responding) occurring either within extinction-training, from deficits in extinction memory retrieval manifest at recent (e.g., 1 day) or more remote (e.g., 1 week) timepoints after training. While the importance of within-session extinction for longer-term reduction in fear responding is debated (Plendl and Wotjak 2010), there is evidence to suggest that the rate of within-session extinction determines vulnerability to fear relapse (King et al. 2018b). In addition, at least some degree of within-session extinctions appears to be important for pharmacological boosting of extinction (Smits et al. 2013) (for further discussion, see Singewald et al. 2015).
Table 1.
Representative examples of rodent models of impaired fear extinction. Effects on extinction training, retrieval (typically assessed 1 day after training) and fear relapse (assessed via spontaneous recovery, renewal, or reinstatement). Abbreviations: I = impaired, N = not impaired, n.d. = not determined, ↑ high freezing in fear relapse paradigm, - not changed. FC = fear conditioning, BDNF = brain-derived neurotrophic factor, BLA = basolateral nucleus of the amygdala, CeL = centrolateral nucleus of the amygdala, CeM = centromedial nucleus of the amygdala, dmPFC = dorsomedial prefrontal cortex, IFN-α = interferon alpha, LPS = lipopolysaccharide, SR = spontaneous recovery, vmPFC = ventromedial prefrontal cortex, 5-HTT = serotonin transporter
| Model subcategory | Extinction training | Extinction retrieval | Fear relapse | Extinction circuitry dysfunction | Reference |
|---|---|---|---|---|---|
| Region and neural circuit disruptions | |||||
| BLA inactivation | (N) | I | n.d. | (Sierra-Mercado et al. 2011 | |
| vmPFC inactivation | I | I | n.d. | (Sierra-Mercado et al. 2011 | |
| vHPC inactivation | (N) | I | n.d. | (Sierra-Mercado et al. 2011) | |
| CeL cell-specific disruption | N | I | n.d. | (Gafford et al. 2012) | |
| Genetic factors | |||||
| 5-HTT deletion | I | n.d. | n.d. | vmPFC/BLA dendritic dysmorphology, vmPFC hypoactivity | (Wellman et al. 2007) |
| BDNF mutation | I | n.d. | n.d. | vmPFC hypoactivity | (Soliman et al. 2010) |
| S1 inbred strain | I | I | ↑ | vmPFC/BLA hypoactivity, dmPFC/CeM hyperactivity | (Hefner et al. 2008; Sartori et al. 2016) |
| S1 (weak conditioning) | N | I | (Whittle et al. 2013) | ||
| Selection for trait anxiety | I | I | ↑. | vmPFC hypoactivity, dmPFC hyperactivity | (Muigg et al. 2008; Yen et al. 2012) |
| Subpopulation stratification | I | I | ↑ | vmPFC/BLA dendritic dysmorphology | (Laricchiuta et al. 2016) |
| Exposure to environmental insults, developmental factors | |||||
| Acute stress | I | I | n.d. | vmPFC/BLA dendritic dysmorphology | (Maroun et al. 2013) |
| Single prolonged stress | N | I | ↑ | vmPFC hypoactivity, BLA/vHPC hyperactivity/connectivity | (Knox et al. 2012; Knox et al. 2018) |
| Acute stress and behavioral stratification | I | I | ↑ | vmPFC hypoactivity, BLA hyperactivity/gene expression | (Sillivan et al. 2017) |
| Subchronic or chronic stress | N | I | n.d. | vmPFC dendritic dysmorphology | (Izquierdo et al. 2006; Miracle et al. 2006) |
| Chronic ethanol | N | I | ↑ | vmPFC hypoactivity, dmPFC dendritic dysmorphology | (Holmes et al. 2012) |
| High fat/sugar diet | I(trend) | I | n.d. | Fewer vmPFC parvalbumin cells, increased vmPFC FosB/ΔFosB | (Baker and Reichelt 2016) |
| Immune activation (IFN-α) | I | n.d. | n.d. | BLA microglia, astrocyte activation | (Bi et al. 2016) |
| (LPS) | I | I | n.d. | (Quinones et al. 2016) | |
| Adolescence | N | I | n.d. | (McCallum et al. 2010) | |
| I | I | - | vmPFC hypoactivity | (Hefner and Holmes 2007; Pattwell et al. 2013) | |
Toward a neurotopography of extinction: system and circuit models of impaired extinction
Altering the activity of specific brain regions is a classical approach to mapping the key structures necessary for the acquisition, consolidation, or retrieval of extinction. Traditional methods such local lesioning, interregional disconnection, electrical stimulation, and pharmacological (e.g., GABA receptor agonist) inactivation, have been supplemented by newer optogenetic and chemogenetic approaches that allow for access over specific neural populations and pathways with better spatial and/or temporal precision. From these studies, it is clear that the learning of and the memory for extinction is distributed in a network fashion across brain areas including the prefrontal cortex (PFC), amygdala and hippocampus, but also a range of additional structures such as periaqueductal gray (PAG), bed nucleus of the stria terminalis (BNST), VTA, striatum, and others.
The broad strokes of the principal findings to date are as follows: Using a range of techniques, including temporary inactivations, immediate-early gene analyses, single-unit recordings, and optogenetics, activity in the dorsomedial PFC (dmPFC) positively associates with high fear/poor extinction, via reciprocal connections to pro-fear subpopulations of projections neurons in the basal amygdala (BA) (Burgos-Robles et al. 2009; Courtin et al. 2014; Dejean et al. 2016; Fitzgerald et al. 2014; Karalis et al. 2016; Senn et al. 2014; Whittle et al. 2010). Conversely, the ventromedial PFC (vmPFC) and its projections to the BA exerts a pro-extinction effect (Bloodgood et al. 2018; Bukalo et al. 2015; Sierra-Mercado et al. 2006). In turn, ventral hippocampus (vHPC) inputs to the central amygdala (CeA) (Xu et al. 2016) and vmPFC (Marek et al. 2018) are recruited to gate the flow of information underlying contextual fear and context-induced fear renewal after extinction, respectively.
The well-studied vHPC-mPFC-BA system subserving extinction is itself supported by other structures that are being revealed by recent work. These include the ventrolateral periaqueductal gray (vlPAG), which when inhibited impairs extinction (and fear learning) (Arico et al. 2017; Tovote et al. 2015), the BNST, inhibition of which prevents stress-induced fear renewal (Goode et al. 2015) and the lateral part of the central amygdala (CeL), wherein different populations of cells are predicted to promote or oppose the expression of extinction via inputs from the paraventricular nucleus of the thalamus (PVT) (Do-Monte et al. 2015; Haubensak et al. 2010; Knobloch et al. 2012; Li et al. 2013; Penzo et al. 2015). Thus, functional deficits at any of these multiple nodes within the highly integrated “extinction network” potentially contribute to extinction deficits (Knox et al. 2018) (reviewed in Holmes and Singewald 2013) and enhanced propensity for fear relapse (Marek et al. 2018) in psychiatric disorders due to irregularities in communication across the network. A recurring observation across a diverse set of models (Table 1) links functional deficiencies in certain nodes in the “extinction circuit;” in particular, emphasizing loss of function in the vmPFC (infralimbic cortex) and BLA and CeL subregions of the amygdala, and a corresponding over-engagement of the dmPFC (prelimbic cortex) CeM amygdala nucleus. For some examples of disruptions in fear extinction caused by experimental manipulations of these nodes (see Table 1).
The notion of network disruptions underlying poor extinction is also already finding support from human functional imaging studies, though the low spatial resolution of these tools does not afford the same level of subregional changes revealed by the rodent studies (Fenster et al. 2018; Fullana et al. 2018; Sevenster et al. 2018). For instance, high resting dmPFC metabolism correlates with low vmPFC and hippocampal activation during extinction recall and this, in turn, associates with PTSD severity scores (Marin et al. 2016). Moreover, hippocampal-vmPFC co-activation in healthy subjects correlates with superior extinction recall (Kalisch et al. 2006; Milad et al. 2007; Rabinak et al. 2013), while stronger hippocampal–dmPFC connectivity is associated with greater fear renewal (Hermann et al. 2017). An important goal for future human and rodent studies is now to further parse precisely how these finely balanced dynamic interregional interactions breakdown during impaired extinction (Lesting et al. 2011; Muigg et al. 2008).
It is (not) all in the genes: genetic models of impaired extinction
The fact that there is such high heritability estimates of PTSD and anxiety disorders (Pitman et al. 2012; Stein et al. 2002), suggests there is a genetic component to the risk of developing a clinical disorder after encountering trauma(s) (Almli et al. 2014). The most common (“reverse genetics”) approach to identifying genetic factors associated with impaired extinction has been to examine the behavioral consequences of engineering functional changes (e.g., knockout, knockin, overexpression) in specific genes encoding for molecules including Reelin, Pet-1, GAD67, Plaur, Dynorphin, GRP, Trk B, Stathmin, and others (Bukalo et al. 2014). Of those models based on well-known human polymorphisms, candidate genes associated with allele-specific variation in extinction (Lonsdorf and Kalisch 2011), include the BDNF Val66Met (see Felmingham et al. 2018 for evidence of a link between BDNF alleles and impaired fear extinction learning in PTSD) and COMT Val158Met polymorphisms (Table 1). Other examples are FKBP5 and the serotonin transporter, 5-HTTLPR, which interacts with stress to influence risk for PTSD (Caspi et al. 2010).
To date there have been fewer examples of models that are based on a ‘forward-genetics’ approach that use a rat or mouse strain exhibiting impaired extinction as a basis for elucidating underlying biological and genetic correlates (Holmes and Singewald 2013; McGuire et al. 2013). However, our laboratories have taken such an approach in examining a profound extinction deficit in a common inbred mouse strain, 129S1/SvImJ (S1), that was detected from a mouse inbred strain panel survey (Camp et al. 2009; Camp et al. 2012; Flores et al. 2014; Hefner et al. 2008; Temme et al. 2014). This inability to extinguish fear is seen across cued and contextual fear paradigms when contrasted with the profiles of normal extinguishing (e.g., C57BL/6 J) mouse strains. Interestingly, however, under “weak” (low shock) fear conditioning, short-term extinction acquisition is evident in S1 mice but the extinction memory still fails to consolidate and express over the long-term (Whittle et al. 2013).
The deficit in S1 mice does not extend to appetitively motivated instrumental extinction (Hefner et al. 2008), but there is deficient safety learning and overgeneralization of fear to ambiguous contexts and cues in these mice (Camp et al. 2012; Temme et al. 2014). Notably, deficient safety learning and fear overgeneralization are also characteristics of anxiety and trauma-related disorders (Duits et al. 2015; Lissek et al. 2014; Lissek et al. 2005). In another clinical parallel, S1 mice have lower heart rate variability (HRV) and depressed HRV during extinction training (Camp et al. 2012); resembling the reduced HRV seen in anxiety patients (Chalmers et al. 2014) and the slow recovery of HRV after trauma recall in PTSD patients (Arditi-Babchuk et al. 2009).
At the neural level, ex vivo immediate-early gene analysis (Hefner et al. 2008) and in vivo neuronal recordings (Fitzgerald et al. 2014) has revealed evidence of hyper-excitability in the dmPFC and medial nucleus of the CeA (CeM) and hypoactivity in the vmPFC and BA of S1 mice (Table 1), consistent with the respective pro-fear and pro-extinction roles of these regions. Speaking to the translational relevance of these observations, they align well with functional magnetic resonance imaging studies of patients with PTSD that reported a hypoactivation of the vmPFC and exaggerated amygdala reactivity during extinction recall (Garfinkel et al. 2014; Milad et al. 2009; Phelps et al. 2004). The generation of an effective extinction memory in these structures requires the expression and translation of relevant plasticity and learning-associated genes (Orsini and Maren 2012; Singewald et al. 2015).
The mechanisms by which the expression of genes are fine-tuned to, in turn, shape extinction is an emerging area that has also led to a focus on microRNAs (miRNAs) (Murphy and Singewald 2018)—a class of short, single-stranded non-coding RNAs (Smith and Kenny 2017). A pioneering study on this subject showed that extinction training increased the microRNA, miR-128b, to cause expression of a set of genes which are associated with synaptic plasticity. When miR-128b was experimentally increased in the IL of the B6 mouse strain, it was found to promote fear extinction (Lin et al. 2011). In an extinction-deficient mouse model, microarray approaches revealed that miR-144-3p exhibited increased amygdalar expression following successful extinction training. Viral enhancement of miR-144-3p expression in the BA rescued impaired fear extinction in S1 mice leading to reduced conditioned responses during both training and extinction retrieval. Furthermore, miR-144-3p overexpression protected against the return of fear in extinction-intact B6 mice, suggesting that miR-144-3p plays a critical role in extinction learning and long-lasting fear alleviation via interaction with its target genes Pten, Notch1, and Spred1, and their noted plasticity-associated downstream signaling cascades (Murphy et al. 2017).
Clearly, we remain in the earliest stages of defining how extinction efficacy is influenced not only by inherited gene variation, but also the ever-increasing range of mechanisms that are engaged to lay down extinction memories by controlling gene-expression. This is certainly an exciting area to watch going forward.
Stress, drugs, and bad diet: environmental insult models of impaired extinction
We now turn to models of impairments in extinction produced by various environmental insults and certain other factors (Table 1). Given clinical evidence that a history of exposure to stress is a major risk factor for anxiety and trauma-related disorders, there have been multiple efforts to model stress-induced extinction deficits in rodents and identify mechanisms to prevent or reverse these (Chauveau et al. 2012) This literature has been recently reviewed (Deslauriers et al. 2018; Maren and Holmes 2015; Stockhorst and Antov 2015), but we would like to emphasize a number of the key findings here. One notable point is that the literatures on the neural and genetic correlates of impaired extinction increasingly align with emerging evidence linking stress and extinction. As an example, the aforementioned contrasting extinction phenotype of the S1 and B6 strains was exploited by a quantitative genetic approach to uncover a genomic region associated with extinction located on chromosome 3, and a novel candidate gene (peptidylprolyl isomerase D, Ppid) encoded within this genomic region (Gunduz-Cinar et al. 2018).
In turn, Ppid is a member of the tetratricopeptide repeat protein family, which includes FKBP5, and is involved in the regulation of steroid hormone receptors (Zannas and Binder 2014). Moreover, Ppid alters extinction in a manner requiring the glucocorticoid receptor (GR), suggesting this gene affects extinction by modulating a key stress-regulating system (Gunduz-Cinar et al. 2018). This latter finding is notable given an increasingly compelling translational evidence implicating glucocorticoids in trauma-related conditions and fear extinction (Maren and Holmes 2015) and S1 mice have abnormal HPA-axis responses to stress (Camp et al. 2012). For example, at least a subpopulation of PTSD patients show increased sensitivity of the negative-feedback system of the HPA-axis and lower cortisol levels (Yehuda 2002), while (systemic or intra-BLA) administration of GR agonists promotes extinction in rodents (Flores et al. 2018) and in humans with PTSD or other anxiety disorders (de Quervain et al. 2011; Michopoulos et al. 2017; Soravia et al. 2014).
Another major take home message in this section is that the effects of stress on extinction are dependent not only on the type and chronicity of the stressors, but also on the age, sex, and prior experience of the subject. For example, extinction efficacy varies dramatically across development and adolescence through into adulthood, both in rodents and in humans (Baker et al. 2016; Pattwell et al. 2012) (Table 1). Concerning stressor-type, to date, it seems that immobilization stress and single prolonged stress produce particularly robust deficits in fear extinction (Deslauriers et al. 2018). In an illustrative example of the often reported nuances in this field, stressing adolescent rats, through a combination of predator order and elevated platform exposure, impaired extinction into adulthood but, for reasons that remain unclear, did so only in males and not females (Ter Horst et al. 2012; Toledo-Rodriguez et al. 2012). This extends clear evidence of sex differences in fear extinction (Baran et al. 2009; Fenton et al. 2016; Hunter 2018; Matsuda et al. 2015; Shansky 2015; Shvil et al. 2014).
Adding to the complexity of this area, not only are there varying responses to stress between sexes, but there is also individual variation within a population of the same sex. For example, following exposure to a footshock-based stress-enhanced fear learning procedure, male (but not female) (C57BL/6 J) mice could be split into extinction-resilient and susceptible subgroups, that were in turn associated with specific patterns of corticoamygdala activity (Table 1) and gene expression (Sillivan et al. 2017). These data advocate for the greater consideration of subpopulation differences in stress-related models of impaired extinction, both to better approximate the marked individual differences in risk for stress disorders in humans and predict the efficacy of drugs and other therapeutic interventions (King et al. 2018a).
There are interesting overlaps between the effects of exposure to stress and drugs of abuse, another risk factor for anxiety disorders and PTSD, on extinction. For example, chronic cannabis use is associated with impaired extinction in humans (Papini et al. 2017) as is chronic ethanol exposure in rodents. Socially isolating rats during adolescence has been shown to increase ethanol drinking and impair fear extinction (Skelly et al. 2015), while chronic exposure to vaporized ethanol impairs extinction retrieval in mice, in association with dendritic dysmorphology and blunted NMDA receptor-mediated neuronal transmission in the dmPFC (Holmes et al. 2012). Along similar lines, 2 weeks of ethanol consumption in a liquid diet rendered rats extinction resistant (Bertotto et al. 2006), while a shorter regimen of intraperitoneally administered ethanol produced an increase in fear during extinction acquisition and increased neuronal activation (i.e., c-Fos expression) in the dmPFC, BA, CeA, and PVT (Quinones-Laracuente et al. 2015). However, while stress and ethanol exposure may produce similar effects on extinction, there is no clear cut relationship between differences in the propensity to drink ethanol across mouse strains and the capacity for extinction (Crabbe et al. 2016).
Unlike most other abused drugs, alcohol is consumed like a food and is a source of calorific intake. The degree to which this contribute to the deleterious physiological effects of chronic drinking is debated but may be relevant here given recent evidence that abnormal diet can affect fear extinction. Rats fed a high-fat/high-sugar diet over the course of 6 weeks developed poor extinction (Table 1) and altered certain makers of infralimbic cortex function (Baker and Reichelt 2016). One possibility is that such effects are driven by the neuroinflammatory responses that are associated with a high-fat diet (Valdearcos et al. 2014). Giving credence to this hypothesis are reports that immune activation (via lipopolysaccharide administration) disrupts fear extinction (Quinones et al. 2016), as does intra-BLA infusion of interferon-α; in a manner preventable by administration of a microglial activation inhibitor (minocycline) (Bi et al. 2016).
We wish to highlight these latter findings not to overstate the potential importance of poor diet as a risk factor for trauma-related conditions, but rather to underscore the expanding range of environmental insults found to disrupt fear extinction. A challenge for future work will be to model the real-world combination of dietary factors, exposure to drugs and life stressors faced by most at-risk individuals, and to use the rodent models to decipher how these interact and potentially synergize to affect clinical outcomes.
Outlook: using models of impaired extinction to discover novel therapeutic strategies
The value of rodent models of impaired extinction is ultimately gauged by their utility as a platform for the identification of novel mechanisms for therapeutically normalizing extinction. While there are examples of targeting circuit abnormalities via deep brain stimulation in these models (Rodriguez-Romaguera and Quirk 2017; Whittle et al. 2013), much of this work has focused on pharmacological approaches, reflecting the continued importance of developing novel drugs for anxiety, and trauma-related disorders (Bukalo et al. 2014; Graham and Richardson 2011; Singewald et al. 2015). Encouragingly, certain models in mouse strains (e.g., S1 strain (Gunduz-Cinar et al. 2013; Gunduz et al. 2015; Hefner et al. 2008; Sartori et al. 2016; Whittle et al. 2010; Whittle et al. 2016; Whittle et al. 2013) and rats, e.g., ethanol-exposed (Bertotto et al. 2006), stressed (Matsumoto et al. 2013), and adolescents (Ganella et al. 2017; McCallum et al. 2010), have demonstrated that deficient extinction is effectively rescued by pharmacological manipulations of various transmitter systems including serotonergic, glutamatergic, dopaminergic, noradrenergic, endocannabinoid signaling. Along these lines, there is the exciting potential for enhancing disturbed neuroplasticity in extinction-related circuits via epigenetic mechanisms such as histone acetylation (Whittle et al. 2016; Whittle et al. 2013) or altering the expression of specific microRNAs, such as miR144 (Murphy et al. 2017) to produce long-term fear reductions in extinction-impaired subjects.
Once a promising pharmacological target is identified, a critical question is how it should be clinically administered to maximize its therapeutic potential and mitigate risk of failure in clinical trials. In this regard, the administration of a single drug concomitant to fear extinction in extinction-deficient individuals does often not suffice to support the extinction memory-augmenting mechanism to an extent that prevents temporal, spatial, or stress-dependent fear relapse (Singewald et al. 2015). Using extinction-deficient mice, our group was able to show for the first time that only the administration of neuropeptide S (NPS) before and the NMDA receptor partial agonist d-cycloserine (DCS) after successful extinction training, but not administration of NPS alone results in formation of a robust extinction memory, which withstands various types of fear relapse (Sartori et al. 2016).
Supporting the utility of this dual pharmacotherapeutic concept, it was demonstrated that fear relapses in extinction-deficient mice can also be reduced by combined administration of L-DOPA and the HDAC-inhibitor MS-275, concomitant to extinction training (Whittle et al. 2016). This speaks to the potential importance of dual or multiple pharmacotherapeutic adjuncts to extinction in these cases. These should be critical considerations in drug development when designing preclinical experiments to evaluate translational potential in extinction-impaired rodent models. Moreover, at present no drug that can pass the blood brain barrier has a pharmacodynamic profile that combines the advantages of promoting memory and reducing anxiety, without also being sedating. This is not to say it is unfeasible and has already been achieved by neuropeptide S or fibroblast growth factor-2 targeting drugs, (Graham and Richardson 2011; Sartori et al. 2016) and endocannabinoid-targeting approaches (Micale et al. 2013; Patel et al. 2017), to give just a few examples. Although the pharmacological augmentation of exposure-based therapies has not yet entered broad clinical use, it represents an exciting idea with the clear potential for improving clinical outcome.
Beyond pharmacological approaches, less conventional approaches have to date been less studied in extinction-deficient models, but are certainly worthy of investigation. One interesting modification to changing the way extinction memories are formed simply involves training in multiple contexts (de Jong et al. 2018). This could potentially mitigate against the context dependency of extinction memories (Bukalo and Holmes 2018; Maren et al. 2013) and the high rate of fear relapse after CBT (Boschen 2009). Preliminary clinical work has shown that performing exposure therapy in multiple contexts reduces, for instance, the reoccurrence of fear of spiders (Vansteenwegen et al. 2007). As more extinction trials/longer CSs are typically needed to achieve reductions in fear in extinction-impaired individuals, behavioral manipulations that could potentially shorten these procedures are of particular interest. Reactivation of the original fear memory prior to or during extinction training has been proposed to render fear memories plastic and receptive to extinction (Monfils et al. 2009; Schiller et al. 2010) (but see Luyten and Beckers 2017) and has been successfully used to attenuate remote fear memories, which are known to be resilient against extinction-mediated attenuation (Khalaf et al. 2018). Along similar lines, there are neurally based strategies for reversing plastic changes underlying fear memory to enable extinction, including the targeting of perineuronal nets around parvalbumin-positive interneurons in the BA (Gogolla et al. 2009; Gunduz-Cinar et al. 2018).
A final point to underscore is that eventual success of novel treatments will be bolstered by grounding them in a solid understanding of how they act at the neural level. The field can draw upon the great advances that have been made in delineating the neural circuitry of fear extinction, as discussed above (Hariri and Holmes 2015). In the ideal scenario, extinction rescuing effects in an impaired model can be aligned with the normalization of disturbed neurobiological markers, including abnormal patterns of brain activation within key brain substrates for extinction (for an example, see Whittle et al. 2010). This notion of therapeutic circuit modulation is supported by clinical observations that successful exposure-based CBT is associated with the reversal of dACC and amygdala hyper-reactivity (Ball et al. 2017; Goossens et al. 2007; Straube et al. 2006) and improved extinction recall is associated with increased vmPFC activity (Ball et al. 2017; Lonsdorf et al. 2014; Milad et al. 2007). Though still preliminary, these convergent neural and behavioral data, from both the laboratory and clinic, help position models of impaired fear extinction as a vital component of future research aimed at developing effective new therapeutic approaches to alleviating the suffering of patients with trauma-related conditions.
Acknowledgements
We are very grateful to Dr. Maria Kharitonova for supporting the literature search and to Zeljko Stevic for drawing the cartoon.
Funding information
Open access funding provided by Austrian Science Fund (FWF). NS is supported by the FWF (Austrian Science Fund, I2433-B26, DK W-1206 and SFB F4410). AH is supported by the NIAAA Intramural Research Program.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
This article belongs to a Special Issue on Psychopharmacology of Extinction
References
- Almli LM, Fani N, Smith AK, Ressler KJ. Genetic approaches to understanding post-traumatic stress disorder. Int J Neuropsychopharmacol. 2014;17:355–370. doi: 10.1017/S1461145713001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderzhanova E, Kirmeier T, Wotjak CT. Animal models in psychiatric research: the RDoC system as a new framework for endophenotype-oriented translational neuroscience. Neurobiol Stress. 2017;7:47–56. doi: 10.1016/j.ynstr.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arditi-Babchuk H, Feldman R, Gilboa-Schechtman E. Parasympathetic reactivity to recalled traumatic and pleasant events in trauma-exposed individuals. J Trauma Stress. 2009;22:254–257. doi: 10.1002/jts.20417. [DOI] [PubMed] [Google Scholar]
- Arico C, Bagley EE, Carrive P, Assareh N, McNally GP. Effects of chemogenetic excitation or inhibition of the ventrolateral periaqueductal gray on the acquisition and extinction of Pavlovian fear conditioning. Neurobiol Learn Mem. 2017;144:186–197. doi: 10.1016/j.nlm.2017.07.006. [DOI] [PubMed] [Google Scholar]
- Baker KD, Reichelt AC. Impaired fear extinction retention and increased anxiety-like behaviours induced by limited daily access to a high-fat/high-sugar diet in male rats: implications for diet-induced prefrontal cortex dysregulation. Neurobiol Learn Mem. 2016;136:127–138. doi: 10.1016/j.nlm.2016.10.002. [DOI] [PubMed] [Google Scholar]
- Baker KD, Bisby MA, Richardson R. Impaired fear extinction in adolescent rodents: Behavioural and neural analyses. Neurosci Biobehav Rev. 2016;70:59–73. doi: 10.1016/j.neubiorev.2016.05.019. [DOI] [PubMed] [Google Scholar]
- Ball TM, Knapp SE, Paulus MP, Stein MB. Brain activation during fear extinction predicts exposure success. Depress Anxiety. 2017;34:257–266. doi: 10.1002/da.22583. [DOI] [PubMed] [Google Scholar]
- Baran SE, Armstrong CE, Niren DC, Hanna JJ, Conrad CD. Chronic stress and sex differences on the recall of fear conditioning and extinction. Neurobiol Learn Mem. 2009;91:323–332. doi: 10.1016/j.nlm.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry AC, Rosenfield D, Smits JA. Extinction retention predicts improvement in social anxiety symptoms following exposure therapy. Depress Anxiety. 2009;26:22–27. doi: 10.1002/da.20511. [DOI] [PubMed] [Google Scholar]
- Bertotto ME, Bustos SG, Molina VA, Martijena ID. Influence of ethanol withdrawal on fear memory: effect of D-cycloserine. Neuroscience. 2006;142:979–990. doi: 10.1016/j.neuroscience.2006.07.013. [DOI] [PubMed] [Google Scholar]
- Bi Q, Shi L, Yang P, Wang J, Qin L. Minocycline attenuates interferon-alpha-induced impairments in rat fear extinction. J Neuroinflammation. 2016;13:172. doi: 10.1186/s12974-016-0638-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloodgood DW, Sugam JA, Holmes A, Kash TL. Fear extinction requires infralimbic cortex projections to the basolateral amygdala. Transl Psychiatry. 2018;8:60. doi: 10.1038/s41398-018-0106-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boschen S. Hybrid regimes of knowledge? Challenges for constructing scientific evidence in the context of the GMO-debate. Environ Sci Pollut Res Int. 2009;16:508–520. doi: 10.1007/s11356-009-0164-y. [DOI] [PubMed] [Google Scholar]
- Bouton ME. Why behavior change is difficult to sustain. Prev Med. 2014;68:29–36. doi: 10.1016/j.ypmed.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukalo O, Holmes A. Everything in its right place: a prefrontal-midbrain circuit for contextual fear discrimination. Neuron. 2018;97:732–733. doi: 10.1016/j.neuron.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukalo O, Pinard CR, Holmes A. Mechanisms to medicines: elucidating neural and molecular substrates of fear extinction to identify novel treatments for anxiety disorders. Br J Pharmacol. 2014;171:4690–4718. doi: 10.1111/bph.12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukalo O, Pinard C, Silverstein S, Brehm C, Hartley N, Whittle N, Colacicco G, Busch E, Patel S, Singewald N, Holmes A. Prefrontal inputs to the amygdala instruct fear extinction memory formation. Sci Adv. 2015;1:e1500251. doi: 10.1126/sciadv.1500251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgos-Robles A, Vidal-Gonzalez I, Quirk GJ. Sustained conditioned responses in prelimbic prefrontal neurons are correlated with fear expression and extinction failure. J Neurosci. 2009;29:8474–8482. doi: 10.1523/JNEUROSCI.0378-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camp M, Norcross M, Whittle N, Feyder M, D’Hanis W, Yilmazer-Hanke D, Singewald N, Holmes A. Impaired Pavlovian fear extinction is a common phenotype across genetic lineages of the 129 inbred mouse strain. Genes Brain Behav. 2009;8:744–752. doi: 10.1111/j.1601-183X.2009.00519.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camp MC, Macpherson KP, Lederle L, Graybeal C, Gaburro S, Debrouse LM, Ihne JL, Bravo JA, O'Connor RM, Ciocchi S, Wellman CL, Luthi A, Cryan JF, Singewald N, Holmes A. Genetic strain differences in learned fear inhibition associated with variation in neuroendocrine, autonomic, and amygdala dendritic phenotypes. Neuropsychopharmacology. 2012;37:1534–1547. doi: 10.1038/npp.2011.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Hariri AR, Holmes A, Uher R, Moffitt TE. Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am J Psychiatry. 2010;167:509–527. doi: 10.1176/appi.ajp.2010.09101452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psychiatry. 2014;5:80. doi: 10.3389/fpsyt.2014.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauveau F, Lange MD, Jungling K, Lesting J, Seidenbecher T, Pape HC. Prevention of stress-impaired fear extinction through neuropeptide S action in the lateral amygdala. Neuropsychopharmacology. 2012;37:1588–1599. doi: 10.1038/npp.2012.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtin J, Chaudun F, Rozeske RR, Karalis N, Gonzalez-Campo C, Wurtz H, Abdi A, Baufreton J, Bienvenu TC, Herry C. Prefrontal parvalbumin interneurons shape neuronal activity to drive fear expression. Nature. 2014;505:92–96. doi: 10.1038/nature12755. [DOI] [PubMed] [Google Scholar]
- Crabbe JC, Schlumbohm JP, Hack W, Barkley-Levenson AM, Metten P, Lattal KM. Fear conditioning in mouse lines genetically selected for binge-like ethanol drinking. Alcohol. 2016;52:25–32. doi: 10.1016/j.alcohol.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Treanor M, Conway CC, Zbozinek T, Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behav Res Ther. 2014;58:10–23. doi: 10.1016/j.brat.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Stein MB, Eley TC, Milad MR, Holmes A, Rapee RM, Wittchen HU. Anxiety disorders. Nat Rev Dis primers. 2017;3:17024. doi: 10.1038/nrdp.2017.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cryan JF, Holmes A. The ascent of mouse: advances in modelling human depression and anxiety. Nat Rev Drug Discov. 2005;4:775–790. doi: 10.1038/nrd1825. [DOI] [PubMed] [Google Scholar]
- de Jong R, Lommen MJJ, de Jong PJ, Nauta MH (2018) Using multiple contexts and retrieval cues in exposure-based therapy to prevent relapse in anxiety disorders. Cogn Behav Pract (in press)
- de Quervain DJ, Bentz D, Michael T, Bolt OC, Wiederhold BK, Margraf J, Wilhelm FH. Glucocorticoids enhance extinction-based psychotherapy. Proc Natl Acad Sci U S A. 2011;108:6621–6625. doi: 10.1073/pnas.1018214108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dejean C, Courtin J, Karalis N, Chaudun F, Wurtz H, Bienvenu TC, Herry C. Prefrontal neuronal assemblies temporally control fear behaviour. Nature. 2016;535:420–424. doi: 10.1038/nature18630. [DOI] [PubMed] [Google Scholar]
- Deslauriers J, Toth M, Der-Avakian A, Risbrough VB. Current status of animal models of posttraumatic stress disorder: behavioral and biological phenotypes, and future challenges in improving translation. Biol Psychiatry. 2018;83:895–907. doi: 10.1016/j.biopsych.2017.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do-Monte FH, Quinones-Laracuente K, Quirk GJ. A temporal shift in the circuits mediating retrieval of fear memory. Nature. 2015;519:460–463. doi: 10.1038/nature14030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duits P, Cath DC, Lissek S, Hox JJ, Hamm AO, Engelhard IM, van den Hout MA, Baas JM. Updated meta-analysis of classical fear conditioning in the anxiety disorders. Depress Anxiety. 2015;32:239–253. doi: 10.1002/da.22353. [DOI] [PubMed] [Google Scholar]
- Eisenhardt D. Molecular mechanisms underlying formation of long-term reward memories and extinction memories in the honeybee (Apis mellifera) Learn Mem. 2014;21:534–542. doi: 10.1101/lm.033118.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felmingham KL, Zuj DV, Hsu KCM, Nicholson E, Palmer MA, Stuart K, Vickers JC, Malhi GS, Bryant RA. The BDNF Val66Met polymorphism moderates the relationship between posttraumatic stress disorder and fear extinction learning. Psychoneuroendocrinology. 2018;91:142–148. doi: 10.1016/j.psyneuen.2018.03.002. [DOI] [PubMed] [Google Scholar]
- Fenster RJ, Lebois LAM, Ressler KJ, Suh J. Brain circuit dysfunction in post-traumatic stress disorder: from mouse to man. Nat Rev Neurosci. 2018;19:535–551. doi: 10.1038/s41583-018-0039-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenton GE, Halliday DM, Mason R, Bredy TW, Stevenson CW. Sex differences in learned fear expression and extinction involve altered gamma oscillations in medial prefrontal cortex. Neurobiol Learn Mem. 2016;135:66–72. doi: 10.1016/j.nlm.2016.06.019. [DOI] [PubMed] [Google Scholar]
- Fitzgerald PJ, Whittle N, Flynn SM, Graybeal C, Pinard CR, Gunduz-Cinar O, Kravitz AV, Singewald N, Holmes A. Prefrontal single-unit firing associated with deficient extinction in mice. Neurobiol Learn Mem. 2014;113:69–81. doi: 10.1016/j.nlm.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores A, Valls-Comamala V, Costa G, Saravia R, Maldonado R, Berrendero F. The hypocretin/orexin system mediates the extinction of fear memories. Neuropsychopharmacology. 2014;39:2732–2741. doi: 10.1038/npp.2014.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores A, Fullana MA, Soriano-Mas C, Andero R (2018) Lost in translation: how to upgrade fear memory research. Mol Psychiatry (in press) [DOI] [PubMed]
- Forcadell E, Torrents-Rodas D, Vervliet B, Leiva D, Tortella-Feliu M, Fullana MA. Does fear extinction in the laboratory predict outcomes of exposure therapy? A treatment analog study. Int J Psychophysiol. 2017;121:63–71. doi: 10.1016/j.ijpsycho.2017.09.001. [DOI] [PubMed] [Google Scholar]
- Fullana MA, Albajes-Eizagirre A, Soriano-Mas C, Vervliet B, Cardoner N, Benet O, Radua J, Harrison BJ. Fear extinction in the human brain: a meta-analysis of fMRI studies in healthy participants. Neurosci Biobehav Rev. 2018;88:16–25. doi: 10.1016/j.neubiorev.2018.03.002. [DOI] [PubMed] [Google Scholar]
- Gafford GM, Guo JD, Flandreau EI, Hazra R, Rainnie DG, Ressler KJ. Cell-type specific deletion of GABA(a)alpha1 in corticotropin-releasing factor-containing neurons enhances anxiety and disrupts fear extinction. Proc Natl Acad Sci U S A. 2012;109:16330–16335. doi: 10.1073/pnas.1119261109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganella DE, Drummond KD, Ganella EP, Whittle S, Kim JH. Extinction of conditioned fear in adolescents and adults: a human fMRI study. Front Hum Neurosci. 2017;11:647. doi: 10.3389/fnhum.2017.00647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfinkel SN, Abelson JL, King AP, Sripada RK, Wang X, Gaines LM, Liberzon I. Impaired contextual modulation of memories in PTSD: an fMRI and psychophysiological study of extinction retention and fear renewal. J Neurosci. 2014;34:13435–13443. doi: 10.1523/JNEUROSCI.4287-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giustino TF, Maren S. Noradrenergic modulation of fear conditioning and extinction. Front Behav Neurosci. 2018;12:43. doi: 10.3389/fnbeh.2018.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gogolla N, Caroni P, Luthi A, Herry C. Perineuronal nets protect fear memories from erasure. Science. 2009;325:1258–1261. doi: 10.1126/science.1174146. [DOI] [PubMed] [Google Scholar]
- Goode TD, Kim JJ, Maren S (2015) Reversible inactivation of the bed nucleus of the Stria terminalis prevents reinstatement but not renewal of extinguished fear. eNeuro 2 [DOI] [PMC free article] [PubMed]
- Goossens L, Sunaert S, Peeters R, Griez EJ, Schruers KR. Amygdala hyperfunction in phobic fear normalizes after exposure. Biol Psychiatry. 2007;62:1119–1125. doi: 10.1016/j.biopsych.2007.04.024. [DOI] [PubMed] [Google Scholar]
- Graham BM, Richardson R. Fibroblast growth factor-2 alters the nature of extinction. Learn Mem. 2011;18:80–84. doi: 10.1101/lm.2006511. [DOI] [PubMed] [Google Scholar]
- Graham BM, Langton JM, Richardson R. Pharmacological enhancement of fear reduction: preclinical models. Br J Pharmacol. 2011;164:1230–1247. doi: 10.1111/j.1476-5381.2010.01175.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunduz-Cinar O, Hill MN, McEwen BS, Holmes A. Amygdala FAAH and anandamide: mediating protection and recovery from stress. Trends Pharmacol Sci. 2013;34:637–644. doi: 10.1016/j.tips.2013.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunduz-Cinar O, Flynn S, Kaugars K, Ramikie TS, Cinar R, Kunos G, Patel S, Holmes A. Fluoxetine facilitates fear extinction through amygdala endocannabinoids. Neuropsychopharmacology. 2016;41(6):1598–609. doi: 10.1038/npp.2015.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunduz-Cinar O, Brockway E, Lederle L, Wilcox T, Halladay LR, Ding Y, Oh H, Busch EF, Kaugars K, Flynn S, Limoges A, Bukalo O, MacPherson KP, Masneuf S, Pinard C, Sibille E, Chesler EJ, Holmes A (2018) Identification of a novel gene regulating amygdala-mediated fear extinction. Mol Psychiatry (in press) [DOI] [PMC free article] [PubMed]
- Hariri AR, Holmes A. Finding translation in stress research. Nat Neurosci. 2015;18:1347–1352. doi: 10.1038/nn.4111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haubensak W, Kunwar PS, Cai H, Ciocchi S, Wall NR, Ponnusamy R, Biag J, Dong HW, Deisseroth K, Callaway EM, Fanselow MS, Luthi A, Anderson DJ. Genetic dissection of an amygdala microcircuit that gates conditioned fear. Nature. 2010;468:270–276. doi: 10.1038/nature09553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hefner K, Holmes A. Ontogeny of fear-, anxiety- and depression-related behavior across adolescence in C57BL/6J mice. Behav Brain Res. 2007;176:210–215. doi: 10.1016/j.bbr.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hefner K, Whittle N, Juhasz J, Norcross M, Karlsson RM, Saksida LM, Bussey TJ, Singewald N, Holmes A. Impaired fear extinction learning and cortico-amygdala circuit abnormalities in a common genetic mouse strain. J Neurosci. 2008;28:8074–8085. doi: 10.1523/JNEUROSCI.4904-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermann A, Stark R, Blecker CR, Milad MR, Merz CJ. Brain structural connectivity and context-dependent extinction memory. Hippocampus. 2017;27:883–889. doi: 10.1002/hipo.22738. [DOI] [PubMed] [Google Scholar]
- Holmes A, Singewald N. Individual differences in recovery from traumatic fear. Trends Neurosci. 2013;36:23–31. doi: 10.1016/j.tins.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes A, Fitzgerald PJ, Macpherson KP, Debrouse L, Colacicco G, Flynn SM, Masneuf S, Pleil KE, Li C, Marcinkiewcz CA, Kash TL, Gunduz-Cinar O, Camp M. Chronic alcohol remodels prefrontal neurons and disrupts NMDAR-mediated fear extinction encoding. Nat Neurosci. 2012;15:1359–1361. doi: 10.1038/nn.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter AS. REM deprivation but not sleep fragmentation produces a sex-specific impairment in extinction. Physiol Behav. 2018;196:84–94. doi: 10.1016/j.physbeh.2018.08.008. [DOI] [PubMed] [Google Scholar]
- Izquierdo A, Wellman CL, Holmes A. Brief uncontrollable stress causes dendritic retraction in infralimbic cortex and resistance to fear extinction in mice. J Neurosci. 2006;26:5733–5738. doi: 10.1523/JNEUROSCI.0474-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalisch R, Korenfeld E, Stephan KE, Weiskopf N, Seymour B, Dolan RJ. Context-dependent human extinction memory is mediated by a ventromedial prefrontal and hippocampal network. J Neurosci. 2006;26:9503–9511. doi: 10.1523/JNEUROSCI.2021-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karalis N, Dejean C, Chaudun F, Khoder S, Rozeske RR, Wurtz H, Bagur S, Benchenane K, Sirota A, Courtin J, Herry C. 4-Hz oscillations synchronize prefrontal-amygdala circuits during fear behavior. Nat Neurosci. 2016;19:605–612. doi: 10.1038/nn.4251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalaf O, Resch S, Dixsaut L, Gorden V, Glauser L, Graff J. Reactivation of recall-induced neurons contributes to remote fear memory attenuation. Science. 2018;360:1239–1242. doi: 10.1126/science.aas9875. [DOI] [PubMed] [Google Scholar]
- King G, Graham BM, Richardson R. Effects of d-cycloserine on individual differences in relapse of fear. Prog Neuro-Psychopharmacol Biol Psychiatry. 2018;84:115–121. doi: 10.1016/j.pnpbp.2018.02.005. [DOI] [PubMed] [Google Scholar]
- King G, Graham BM, Richardson R. Individual differences in fear relapse. Behav Res Ther. 2018;100:37–43. doi: 10.1016/j.brat.2017.11.003. [DOI] [PubMed] [Google Scholar]
- Knobloch HS, Charlet A, Hoffmann LC, Eliava M, Khrulev S, Cetin AH, Osten P, Schwarz MK, Seeburg PH, Stoop R, Grinevich V. Evoked axonal oxytocin release in the central amygdala attenuates fear response. Neuron. 2012;73:553–566. doi: 10.1016/j.neuron.2011.11.030. [DOI] [PubMed] [Google Scholar]
- Knox D, George SA, Fitzpatrick CJ, Rabinak CA, Maren S, Liberzon I. Single prolonged stress disrupts retention of extinguished fear in rats. Learn Mem. 2012;19:43–49. doi: 10.1101/lm.024356.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knox D, Stanfield BR, Staib JM, David NP, DePietro T, Chamness M, Schneider EK, Keller SM, Lawless C. Using c-Jun to identify fear extinction learning-specific patterns of neural activity that are affected by single prolonged stress. Behav Brain Res. 2018;341:189–197. doi: 10.1016/j.bbr.2017.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laricchiuta D, Saba L, De Bartolo P, Caioli S, Zona C, Petrosini L. Maintenance of aversive memories shown by fear extinction-impaired phenotypes is associated with increased activity in the amygdaloid-prefrontal circuit. Sci Rep. 2016;6:21205. doi: 10.1038/srep21205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesting J, Narayanan RT, Kluge C, Sangha S, Seidenbecher T, Pape HC. Patterns of coupled theta activity in amygdala-hippocampal-prefrontal cortical circuits during fear extinction. PLoS One. 2011;6:e21714. doi: 10.1371/journal.pone.0021714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H, Penzo MA, Taniguchi H, Kopec CD, Huang ZJ, Li B. Experience-dependent modification of a central amygdala fear circuit. Nat Neurosci. 2013;16:332–339. doi: 10.1038/nn.3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Q, Wei W, Coelho CM, Li X, Baker-Andresen D, Dudley K, Ratnu VS, Boskovic Z, Kobor MS, Sun YE, Bredy TW. The brain-specific microRNA miR-128b regulates the formation of fear-extinction memory. Nat Neurosci. 2011;14:1115–1117. doi: 10.1038/nn.2891. [DOI] [PubMed] [Google Scholar]
- Lissek S, Powers AS, McClure EB, Phelps EA, Woldehawariat G, Grillon C, Pine DS. Classical fear conditioning in the anxiety disorders: a meta-analysis. Behav Res Ther. 2005;43:1391–1424. doi: 10.1016/j.brat.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Lissek S, Kaczkurkin AN, Rabin S, Geraci M, Pine DS, Grillon C. Generalized anxiety disorder is associated with overgeneralization of classically conditioned fear. Biol Psychiatry. 2014;75:909–915. doi: 10.1016/j.biopsych.2013.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonsdorf TB, Kalisch R. A review on experimental and clinical genetic associations studies on fear conditioning, extinction and cognitive-behavioral treatment. Transl Psychiatry. 2011;1:e41. doi: 10.1038/tp.2011.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonsdorf TB, Richter J. Challenges of fear conditioning research in the age of RDoC. Z Psychol. 2017;225:189–199. [Google Scholar]
- Lonsdorf TB, Haaker J, Kalisch R. Long-term expression of human contextual fear and extinction memories involves amygdala, hippocampus and ventromedial prefrontal cortex: a reinstatement study in two independent samples. Soc Cogn Affect Neurosci. 2014;9:1973–1983. doi: 10.1093/scan/nsu018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luyten L, Beckers T. A preregistered, direct replication attempt of the retrieval-extinction effect in cued fear conditioning in rats. Neurobiol Learn Mem. 2017;144:208–215. doi: 10.1016/j.nlm.2017.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marek R, Jin J, Goode TD, Giustino TF, Wang Q, Acca GM, Holehonnur R, Ploski JE, Fitzgerald PJ, Lynagh T, Lynch JW, Maren S, Sah P. Hippocampus-driven feed-forward inhibition of the prefrontal cortex mediates relapse of extinguished fear. Nat Neurosci. 2018;21:384–392. doi: 10.1038/s41593-018-0073-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maren S, Holmes A. Stress and fear extinction. Neuropsychopharmacology. 2016;41(1):58–79. doi: 10.1038/npp.2015.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maren S, Phan KL, Liberzon I. The contextual brain: implications for fear conditioning, extinction and psychopathology. Nat Rev Neurosci. 2013;14:417–428. doi: 10.1038/nrn3492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin MF, Song H, VanElzakker MB, Staples-Bradley LK, Linnman C, Pace-Schott EF, Lasko NB, Shin LM, Milad MR. Association of Resting Metabolism in the fear neural network with extinction recall activations and clinical measures in trauma-exposed individuals. Am J Psychiatry. 2016;173:930–938. doi: 10.1176/appi.ajp.2015.14111460. [DOI] [PubMed] [Google Scholar]
- Maroun M, Ioannides PJ, Bergman KL, Kavushansky A, Holmes A, Wellman CL. Fear extinction deficits following acute stress associate with increased spine density and dendritic retraction in basolateral amygdala neurons. Eur J Neurosci. 2013;38:2611–2620. doi: 10.1111/ejn.12259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuda S, Matsuzawa D, Ishii D, Tomizawa H, Sutoh C, Shimizu E. Sex differences in fear extinction and involvements of extracellular signal-regulated kinase (ERK) Neurobiol Learn Mem. 2015;123:117–124. doi: 10.1016/j.nlm.2015.05.009. [DOI] [PubMed] [Google Scholar]
- Matsumoto Y, Morinobu S, Yamamoto S, Matsumoto T, Takei S, Fujita Y, Yamawaki S. Vorinostat ameliorates impaired fear extinction possibly via the hippocampal NMDA-CaMKII pathway in an animal model of posttraumatic stress disorder. Psychopharmacology. 2013;229:51–62. doi: 10.1007/s00213-013-3078-9. [DOI] [PubMed] [Google Scholar]
- McCallum J, Kim JH, Richardson R. Impaired extinction retention in adolescent rats: effects of D-cycloserine. Neuropsychopharmacology. 2010;35:2134–2142. doi: 10.1038/npp.2010.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire JL, Bergstrom HC, Parker CC, Le T, Morgan M, Tang H, Selwyn RG, Silva AC, Choi K, Ursano RJ, Palmer AA, Johnson LR. Traits of fear resistance and susceptibility in an advanced intercross line. Eur J Neurosci. 2013;38:3314–3324. doi: 10.1111/ejn.12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micale V, Di Marzo V, Sulcova A, Wotjak CT, Drago F. Endocannabinoid system and mood disorders: priming a target for new therapies. Pharmacol Ther. 2013;138:18–37. doi: 10.1016/j.pharmthera.2012.12.002. [DOI] [PubMed] [Google Scholar]
- Michopoulos V, Norrholm SD, Stevens JS, Glover EM, Rothbaum BO, Gillespie CF, Schwartz AC, Ressler KJ, Jovanovic T. Dexamethasone facilitates fear extinction and safety discrimination in PTSD: a placebo-controlled, double-blind study. Psychoneuroendocrinology. 2017;83:65–71. doi: 10.1016/j.psyneuen.2017.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milad MR, Quirk GJ. Fear extinction as a model for translational neuroscience: ten years of progress. Annu Rev Psychol. 2012;63:129–151. doi: 10.1146/annurev.psych.121208.131631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milad MR, Wright CI, Orr SP, Pitman RK, Quirk GJ, Rauch SL. Recall of fear extinction in humans activates the ventromedial prefrontal cortex and hippocampus in concert. Biol Psychiatry. 2007;62:446–454. doi: 10.1016/j.biopsych.2006.10.011. [DOI] [PubMed] [Google Scholar]
- Milad MR, Orr SP, Lasko NB, Chang Y, Rauch SL, Pitman RK. Presence and acquired origin of reduced recall for fear extinction in PTSD: results of a twin study. J Psychiatr Res. 2008;42:515–520. doi: 10.1016/j.jpsychires.2008.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milad MR, Pitman RK, Ellis CB, Gold AL, Shin LM, Lasko NB, Zeidan MA, Handwerger K, Orr SP, Rauch SL. Neurobiological basis of failure to recall extinction memory in posttraumatic stress disorder. Biol Psychiatry. 2009;66:1075–1082. doi: 10.1016/j.biopsych.2009.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miracle AD, Brace MF, Huyck KD, Singler SA, Wellman CL. Chronic stress impairs recall of extinction of conditioned fear. Neurobiol Learn Mem. 2006;85:213–218. doi: 10.1016/j.nlm.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Monfils MH, Cowansage KK, Klann E, LeDoux JE. Extinction-reconsolidation boundaries: key to persistent attenuation of fear memories. Science. 2009;324:951–955. doi: 10.1126/science.1167975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muigg P, Hetzenauer A, Hauer G, Hauschild M, Gaburro S, Frank E, Landgraf R, Singewald N. Impaired extinction of learned fear in rats selectively bred for high anxiety--evidence of altered neuronal processing in prefrontal-amygdala pathways. Eur J Neurosci. 2008;28:2299–2309. doi: 10.1111/j.1460-9568.2008.06511.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy CP, Singewald N. Potential of microRNAs as novel targets in the alleviation of pathological fear. Genes Brain Behav. 2018;17:e12427. doi: 10.1111/gbb.12427. [DOI] [PubMed] [Google Scholar]
- Murphy CP, Li X, Maurer V, Oberhauser M, Gstir R, Wearick-Silva LE, Viola TW, Schafferer S, Grassi-Oliveira R, Whittle N, Huttenhofer A, Bredy TW, Singewald N. MicroRNA-mediated rescue of fear extinction memory by miR-144-3p in extinction-impaired mice. Biol Psychiatry. 2017;81:979–989. doi: 10.1016/j.biopsych.2016.12.021. [DOI] [PubMed] [Google Scholar]
- Orsini CA, Maren S. Neural and cellular mechanisms of fear and extinction memory formation. Neurosci Biobehav Rev. 2012;36:1773–1802. doi: 10.1016/j.neubiorev.2011.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papini S, Ruglass LM, Lopez-Castro T, Powers MB, Smits JA, Hien DA. Chronic cannabis use is associated with impaired fear extinction in humans. J Abnorm Psychol. 2017;126:117–124. doi: 10.1037/abn0000224. [DOI] [PubMed] [Google Scholar]
- Patel S, Hill MN, Cheer JF, Wotjak CT, Holmes A. The endocannabinoid system as a target for novel anxiolytic drugs. Neurosci Biobehav Rev. 2017;76:56–66. doi: 10.1016/j.neubiorev.2016.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattwell SS, Duhoux S, Hartley CA, Johnson DC, Jing D, Elliott MD, Ruberry EJ, Powers A, Mehta N, Yang RR, Soliman F, Glatt CE, Casey BJ, Ninan I, Lee FS. Altered fear learning across development in both mouse and human. Proc Natl Acad Sci U S A. 2012;109:16318–16323. doi: 10.1073/pnas.1206834109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattwell SS, Lee FS, Casey BJ. Fear learning and memory across adolescent development: hormones and behavior special issue: puberty and adolescence. Horm Behav. 2013;64:380–389. doi: 10.1016/j.yhbeh.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlov IP. Conditioned reflexes. London: Oxford University Press; 1927. [Google Scholar]
- Penzo MA, Robert V, Tucciarone J, De Bundel D, Wang M, Van Aelst L, Darvas M, Parada LF, Palmiter RD, He M, Huang ZJ, Li B. The paraventricular thalamus controls a central amygdala fear circuit. Nature. 2015;519:455–459. doi: 10.1038/nature13978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelps EA, Delgado MR, Nearing KI, LeDoux JE. Extinction learning in humans: role of the amygdala and vmPFC. Neuron. 2004;43:897–905. doi: 10.1016/j.neuron.2004.08.042. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Rasmusson AM, Koenen KC, Shin LM, Orr SP, Gilbertson MW, Milad MR, Liberzon I. Biological studies of post-traumatic stress disorder. Nat Rev Neurosci. 2012;13:769–787. doi: 10.1038/nrn3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinones MM, Maldonado L, Velazquez B, Porter JT. Candesartan ameliorates impaired fear extinction induced by innate immune activation. Brain Behav Immun. 2016;52:169–177. doi: 10.1016/j.bbi.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinones-Laracuente K, Hernandez-Rodriguez MY, Bravo-Rivera C, Melendez RI, Quirk GJ. The effect of repeated exposure to ethanol on pre-existing fear memories in rats. Psychopharmacology. 2015;232:3615–3622. doi: 10.1007/s00213-015-4016-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinak CA, Angstadt M, Lyons M, Mori S, Milad MR, Liberzon I, Luan Phan K. Cannabinoid modulation of prefrontal-limbic activation during fear extinction learning and recall in humans. Neurobiol Learn Mem. 2014;113:125–34. doi: 10.1016/j.nlm.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research--past, present, and future. Biol Psychiatry. 2006;60:376–382. doi: 10.1016/j.biopsych.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Romaguera J, Quirk GJ (2017) Extinction of conditioned fear and avoidance: relevance for OCD. In: Pittenger C (ed) Obsessive compulsive disorder: phenomenology, pathophysiology, and treatment. Oxford University Press
- Rosen JB, Schulkin J. From normal fear to pathological anxiety. Psychol Rev. 1998;105:325–350. doi: 10.1037/0033-295x.105.2.325. [DOI] [PubMed] [Google Scholar]
- Sartori SB, Maurer V, Murphy C, Schmuckermair C, Muigg P, Neumann ID, Whittle N, Singewald N (2016) Combined neuropeptide S and D-cycloserine augmentation prevents the return of fear in extinction-impaired rodents: advantage of dual versus single drug approaches. Int J Neuropsychopharmacol 19(6). pii: pyv128 [DOI] [PMC free article] [PubMed]
- Schiller D, Monfils MH, Raio CM, Johnson DC, Ledoux JE, Phelps EA. Preventing the return of fear in humans using reconsolidation update mechanisms. Nature. 2010;463:49–53. doi: 10.1038/nature08637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senn V, Wolff SB, Herry C, Grenier F, Ehrlich I, Grundemann J, Fadok JP, Muller C, Letzkus JJ, Luthi A. Long-range connectivity defines behavioral specificity of amygdala neurons. Neuron. 2014;81:428–437. doi: 10.1016/j.neuron.2013.11.006. [DOI] [PubMed] [Google Scholar]
- Sevenster D, Visser RM, D'Hooge R. A translational perspective on neural circuits of fear extinction: current promises and challenges. Neurobiol Learn Mem. 2018;155:113–126. doi: 10.1016/j.nlm.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shansky RM. Sex differences in PTSD resilience and susceptibility: challenges for animal models of fear learning. Neurobiol Stress. 2015;1:60–65. doi: 10.1016/j.ynstr.2014.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shvil E, Sullivan GM, Schafer S, Markowitz JC, Campeas M, Wager TD, Milad MR, Neria Y. Sex differences in extinction recall in posttraumatic stress disorder: a pilot fMRI study. Neurobiol Learn Mem. 2014;113:101–108. doi: 10.1016/j.nlm.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sierra-Mercado D, Jr, Corcoran KA, Lebron-Milad K, Quirk GJ. Inactivation of the ventromedial prefrontal cortex reduces expression of conditioned fear and impairs subsequent recall of extinction. Eur J Neurosci. 2006;24:1751–1758. doi: 10.1111/j.1460-9568.2006.05014.x. [DOI] [PubMed] [Google Scholar]
- Sierra-Mercado D, Padilla-Coreano N, Quirk GJ. Dissociable roles of prelimbic and infralimbic cortices, ventral hippocampus, and basolateral amygdala in the expression and extinction of conditioned fear. Neuropsychopharmacology. 2011;36:529–538. doi: 10.1038/npp.2010.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sijbrandij M, Engelhard IM, Lommen MJ, Leer A, Baas JM. Impaired fear inhibition learning predicts the persistence of symptoms of posttraumatic stress disorder (PTSD) J Psychiatr Res. 2013;47:1991–1997. doi: 10.1016/j.jpsychires.2013.09.008. [DOI] [PubMed] [Google Scholar]
- Sillivan SE, Joseph NF, Jamieson S, King ML, Chevere-Torres I, Fuentes I, Shumyatsky GP, Brantley AF, Rumbaugh G, Miller CA. Susceptibility and resilience to posttraumatic stress disorder-like behaviors in inbred mice. Biol Psychiatry. 2017;82:924–933. doi: 10.1016/j.biopsych.2017.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singewald N, Schmuckermair C, Whittle N, Holmes A, Ressler KJ. Pharmacology of cognitive enhancers for exposure-based therapy of fear, anxiety and trauma-related disorders. Pharmacol Ther. 2015;149:150–190. doi: 10.1016/j.pharmthera.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sippel LM, Holtzheimer PE, Friedman MJ, Schnurr PP. Defining treatment-resistant posttraumatic stress disorder: a framework for future research. Biol Psychiatry. 2018;84:e37–e41. doi: 10.1016/j.biopsych.2018.03.011. [DOI] [PubMed] [Google Scholar]
- Skelly MJ, Chappell AE, Carter E, Weiner JL. Adolescent social isolation increases anxiety-like behavior and ethanol intake and impairs fear extinction in adulthood: possible role of disrupted noradrenergic signaling. Neuropharmacology. 2015;97:149–159. doi: 10.1016/j.neuropharm.2015.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ACW, Kenny PJ. MicroRNAs regulate synaptic plasticity underlying drug addiction. Genes Brain Behav. 2018;17(3):e12424. doi: 10.1111/gbb.12424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JA, Rosenfield D, Otto MW, Powers MB, Hofmann SG, Telch MJ, Pollack MH, Tart CD. D-cycloserine enhancement of fear extinction is specific to successful exposure sessions: evidence from the treatment of height phobia. Biol Psychiatry. 2013;73:1054–1058. doi: 10.1016/j.biopsych.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soliman F, Glatt CE, Bath KG, Levita L, Jones RM, Pattwell SS, Jing D, Tottenham N, Amso D, Somerville LH, Voss HU, Glover G, Ballon DJ, Liston C, Teslovich T, Van Kempen T, Lee FS, Casey BJ. A genetic variant BDNF polymorphism alters extinction learning in both mouse and human. Science. 2010;327:863–866. doi: 10.1126/science.1181886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soravia LM, Heinrichs M, Winzeler L, Fisler M, Schmitt W, Horn H, Dierks T, Strik W, Hofmann SG, de Quervain DJ. Glucocorticoids enhance in vivo exposure-based therapy of spider phobia. Depress Anxiety. 2014;31:429–435. doi: 10.1002/da.22219. [DOI] [PubMed] [Google Scholar]
- Stein MB, Jang KL, Taylor S, Vernon PA, Livesley WJ. Genetic and environmental influences on trauma exposure and posttraumatic stress disorder symptoms: a twin study. Am J Psychiatry. 2002;159:1675–1681. doi: 10.1176/appi.ajp.159.10.1675. [DOI] [PubMed] [Google Scholar]
- Stockhorst U, Antov MI. Modulation of fear extinction by stress, stress hormones and estradiol: a review. Front Behav Neurosci. 2015;9:359. doi: 10.3389/fnbeh.2015.00359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straube T, Glauer M, Dilger S, Mentzel HJ, Miltner WH. Effects of cognitive-behavioral therapy on brain activation in specific phobia. Neuroimage. 2006;29:125–135. doi: 10.1016/j.neuroimage.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Temme SJ, Bell RZ, Pahumi R, Murphy GG. Comparison of inbred mouse substrains reveals segregation of maladaptive fear phenotypes. Front Behav Neurosci. 2014;8:282. doi: 10.3389/fnbeh.2014.00282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ter Horst JP, Carobrez AP, van der Mark MH, de Kloet ER, Oitzl MS. Sex differences in fear memory and extinction of mice with forebrain-specific disruption of the mineralocorticoid receptor. Eur J Neurosci. 2012;36:3096–3102. doi: 10.1111/j.1460-9568.2012.08237.x. [DOI] [PubMed] [Google Scholar]
- Toledo-Rodriguez M, Pitiot A, Paus T, Sandi C. Stress during puberty boosts metabolic activation associated with fear-extinction learning in hippocampus, basal amygdala and cingulate cortex. Neurobiol Learn Mem. 2012;98:93–101. doi: 10.1016/j.nlm.2012.05.006. [DOI] [PubMed] [Google Scholar]
- Tovote P, Fadok JP, Luthi A. Neuronal circuits for fear and anxiety. Nat Rev Neurosci. 2015;16:317–331. doi: 10.1038/nrn3945. [DOI] [PubMed] [Google Scholar]
- Valdearcos M, Robblee MM, Benjamin DI, Nomura DK, Xu AW, Koliwad SK. Microglia dictate the impact of saturated fat consumption on hypothalamic inflammation and neuronal function. Cell Rep. 2014;9:2124–2138. doi: 10.1016/j.celrep.2014.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vansteenwegen D, Vervliet B, Iberico C, Baeyens F, Van den Bergh O, Hermans D. The repeated confrontation with videotapes of spiders in multiple contexts attenuates renewal of fear in spider-anxious students. Behav Res Ther. 2007;45:1169–1179. doi: 10.1016/j.brat.2006.08.023. [DOI] [PubMed] [Google Scholar]
- Vervliet B, Raes F. Criteria of validity in experimental psychopathology: application to models of anxiety and depression. Psychol Med. 2013;43:2241–2244. doi: 10.1017/S0033291712002267. [DOI] [PubMed] [Google Scholar]
- Waters AM, Pine DS. Evaluating differences in Pavlovian fear acquisition and extinction as predictors of outcome from cognitive behavioural therapy for anxious children. J Child Psychol Psychiatry. 2016;57:869–876. doi: 10.1111/jcpp.12522. [DOI] [PubMed] [Google Scholar]
- Wellman CL, Izquierdo A, Garret JE, Martin KP, Carroll J, Millstein R, Lesch KP, Murphy DL, Holmes A. Impaired stress-coping and fear extinction and abnormal corticolimbic morphology in serotonin transporter knock-out mice. J Neurosci. 2007;27:684–691. doi: 10.1523/JNEUROSCI.4595-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle N, Hauschild M, Lubec G, Holmes A, Singewald N. Rescue of impaired fear extinction and normalization of cortico-amygdala circuit dysfunction in a genetic mouse model by dietary zinc restriction. J Neurosci. 2010;30:13586–13596. doi: 10.1523/JNEUROSCI.0849-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle N, Schmuckermair C, Gunduz-Cinar O, Hauschild M, Ferraguti F, Holmes A, Singewald N. Deep brain stimulation, histone deacetylase inhibitors and glutamatergic drugs rescue resistance to fear extinction in a genetic mouse model. Neuropharmacology. 2013;64:414–423. doi: 10.1016/j.neuropharm.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle N, Maurer V, Murphy C, Rainer J, Bindreither D, Hauschild M, Scharinger A, Oberhauser M, Keil T, Brehm C, Valovka T, Striessnig J, Singewald N. Enhancing dopaminergic signaling and histone acetylation promotes long-term rescue of deficient fear extinction. Transl Psychiatry. 2016;6:e974. doi: 10.1038/tp.2016.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wicking M, Steiger F, Nees F, Diener SJ, Grimm O, Ruttorf M, Schad LR, Winkelmann T, Wirtz G, Flor H. Deficient fear extinction memory in posttraumatic stress disorder. Neurobiol Learn Mem. 2016;136:116–126. doi: 10.1016/j.nlm.2016.09.016. [DOI] [PubMed] [Google Scholar]
- Xu C, Krabbe S, Grundemann J, Botta P, Fadok JP, Osakada F, Saur D, Grewe BF, Schnitzer MJ, Callaway EM, Luthi A. Distinct hippocampal pathways mediate dissociable roles of context in memory retrieval. Cell. 2016;167:961–972 e16. doi: 10.1016/j.cell.2016.09.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R. Current status of cortisol findings in post-traumatic stress disorder. Psychiatr Clin N Am. 2002;25:341–368. doi: 10.1016/s0193-953x(02)00002-3. [DOI] [PubMed] [Google Scholar]
- Yen YC, Mauch CP, Dahlhoff M, Micale V, Bunck M, Sartori SB, Singewald N, Landgraf R, Wotjak CT. Increased levels of conditioned fear and avoidance behavior coincide with changes in phosphorylation of the protein kinase B (AKT) within the amygdala in a mouse model of extremes in trait anxiety. Neurobiol Learn Mem. 2012;98:56–65. doi: 10.1016/j.nlm.2012.04.009. [DOI] [PubMed] [Google Scholar]
- Zannas AS, Binder EB. Gene-environment interactions at the FKBP5 locus: sensitive periods, mechanisms and pleiotropism. Genes Brain Behav. 2014;13:25–37. doi: 10.1111/gbb.12104. [DOI] [PubMed] [Google Scholar]
- Zuj DV, Palmer MA, Lommen MJ, Felmingham KL. The centrality of fear extinction in linking risk factors to PTSD: a narrative review. Neurosci Biobehav Rev. 2016;69:15–35. doi: 10.1016/j.neubiorev.2016.07.014. [DOI] [PubMed] [Google Scholar]