Abstract
Dog bites are a significant public health issue. There is no comprehensive study of dog bite demographics. It was the purpose of this study to perform such an analysis across the US. The National Electronic Injury Surveillance System All Injury Program data for the years 2005 through 2013 was accessed; dog bite injuries were extracted and analyzed. Statistical analyses were performed with SUDAAN 11.0.01™ software to account for the weighted, stratified nature of the data. Incidence values were calculated using population data from the US Census Bureau. A P < 0.05 was considered significant. There was an average 337,103 ED visits each year for dog bites. The average age was 28.9 years; 52.6% were male and 47.4% female. The bites were located on the upper extremity in 47.3%, head/neck in 26.8%, lower extremity in 21.5%, and trunk in 4.4%. Younger patients had more bites involving the head/neck, while older patients the upper extremity. More occurred in the summer and on weekends and 80.2% occurred at home. Hospital admission occurred in 1.7%. Logistic regression analysis demonstrated that the odds of admission was solely dependent upon the age group. The OR for admission was 11.03 [4.68, 26.01] for those >85 years of age, 4.88 [2.89, 8.24] 75–84 years, and 2.79 [1.77, 4.39] those ≤4 years of age, with the 10–14 year age group the reference group. The average annual incidence was 1.1 per 1,000, and was slightly higher in males (1.18 vs 1.02 per 1,000). The estimated cost was at least 400 million US$ per year. Potential prevention strategies are educational programs directed at both children and parents/caretakers outlining the responsibilities of owning a dog. This information can be disseminated in health care facilities, radio/TV/Internet venues, and dog kennels/shelters.
Keyword: Epidemiology
1. Introduction
In 2018 48% of the US population owned a dog [1], and in the United Kingdom 26% of the population owned a dog [2]. These numbers reflect the feeling that a dog is man's best friend: “The one absolutely unselfish friend that man can have . . . is his dog” [3]. Nevertheless, human dog bite injuries from “man's best friend” are a significant public health issue [4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18] and are in the top 15 causes of non-fatal injuries [19]. Dog bites often occur in younger children [11, 12, 13, 16, 20, 21, 22], although some have noted a predominance in other age groups [5, 8, 10]. Children, especially younger ones, typically sustain bites to the head and neck [13, 14, 15, 16, 23, 24], while the extremities are often more involved in older children [15]. There is no in depth study of human dog bites encompassing the entire United States for all age groups, especially adults, studying anatomic location of injury, gender, race, month/weekday of injury, and other demographic variables. It was the purpose of this study to perform such an analysis using a national data base which can hopefully assist in further development of prevention programs.
2. Materials and methods
2.1. Data source
The data for this study comes from the National Electronic Injury Surveillance System (NEISS) All Injury Program (AIP). The NEISS is a dataset managed by the US Consumer Product Safety Commission (USCPSC) which collects emergency department (ED) injury data from ∼100 hospitals in the United States and its territories that have an ED. It was initially directed at injuries resulting from consumer products. However, not all injuries are from consumer products; thus the USCPSC selected ∼65 of these hospitals to obtain data for all injuries, regardless of the association with consumer products. This has been designated as the All Injury Program (AIP). This data is in the public domain and housed by the Inter-University Consortium for Political and Social Research (ICPSR) and can be downloaded from their website. Use of this publicly available de-identified data was considered exempt by our local Institutional Review Board.
The data base includes hospital size (strata), date of ED visit, gender/race/age of the injured patient, diagnosis, disposition from the ED, incident locale, and body part injured. The hospital strata are comprised of 5 hospital categories; 4 are based on size (the total number of ED visits reported by the hospital, which are small [0–16,830], medium [16,831–21,850], large [28,151–41,130], and very large [>41,130]), and one consisting of children's hospitals of all sizes. With appropriate statistical techniques, an estimated number of injuries is then calculated from this weighted, stratified data.
The NEISS-AIP data for the years 2005 through 2013 was used. These years were chosen because 2013 was the last available year at the time the study was performed beginning in early 2018, and data before 2005 was coded differently for many variables, making it difficult to combine the years before 2005 with those afterwards. Injuries due to dog bites were identified by the NEISS AIP codes PCAUSE_C = 16 and/or ICAUSE_C = 16. Race was classified according to Eveleth and Tanner [25] as White, Black, Amerindian (Hispanic and Native American), Asian, Indo-Mediterranean (Middle Eastern and Indian subcontinent), and Polynesian. Due to the small numbers of Polynesian and Indo-Mediterranean peoples in the data set, race/ethnicity is only reported for the White, Black, Amerindian and Asian groups.
2.2. Statistical analysis
Statistical analyses were performed with SUDAAN 11.0.01™ software (RTI International, Research Triangle Park, North Carolina, 2013) which accounts for the weighted, stratified nature of the data. The estimated value and 95% confidence limits [lower, upper] are calculated across the entire population encompassed by the data set. Analyses between groups of continuous data were performed with the t-test (2 groups) or ANOVA (3 or more groups). Differences between groups of categorical data were analyzed by the χ2 test. Multivariate logistic regression was used to determine predictors of dog bites for various parameters, giving an odds ratio (OR), 95% confidence limits and associated P values. Incidence values were calculated using population data from the US Census Bureau for each year 2005–2013. For all statistical analyses, P < 0.05 was considered to be significant. It must be remembered that with a large data set such as this that there may be many statistical differences but which are not clinically meaningful.
3. Results
The actual number of ED visits for injuries over the nine year period was 4,664,468 giving a nationwide estimate of 275,014,511 ED visits. Dog bite injuries accounted for 51,486 of the actual 4.6 million ED injury visits, or an estimated 3,033,931 [2,832,649, 3,245,171] million ED visits (1.1%). This equates to an estimated 337,103 dog bite visits per year to US EDs. To put this 1.1% into perspective, the top 20 reasons for ED visits for injuries were determined (Table 1). Dog bites were the 13th most common injury, and exceeded those occurring on motorcycles (14th), to pedestrians (15th) and firearm gunshot injuries (16th).
Table 1.
The top 20 injuries seen in USA EDs from 2005 through 2013 using the NEISS AIP data.
| Injury | n | N | L 95% CL | U 95% CL | % |
|---|---|---|---|---|---|
| Fall | 1,154,655 | 68,739,406 | 65,480,955 | 72,108,805 | 25.0 |
| Struck by/against an object | 1,085,883 | 62,228,114 | 59,678,149 | 64,848,422 | 22.6 |
| Overexertion | 471,199 | 30,485,345 | 28,298,993 | 32,809,231 | 11.1 |
| Motor vehicle occupant | 431,154 | 23,992,846 | 20,818,598 | 27,611,457 | 8.7 |
| Cut/pierced | 364,231 | 23,173,426 | 21,891,155 | 24,503,793 | 8.4 |
| Unspecified | 332,793 | 18,226,592 | 15,950,842 | 20,818,598 | 6.6 |
| Other bite/sting | 174,168 | 10,499,289 | 9,598,006 | 11,468,105 | 3.8 |
| Poisoning | 158,996 | 9,421,120 | 7,947,919 | 11,138,088 | 3.4 |
| Other transport injury | 83,952 | 5,423,411 | 4,895,258 | 5,995,316 | 2.0 |
| Foreign body | 95,913 | 5,403,619 | 5,115,270 | 5,720,302 | 2.0 |
| Pedal cyclist | 81,649 | 4,537,927 | 3,960,209 | 5,170,273 | 1.7 |
| Fire/burn | 67,582 | 3,977,581 | 3,822,702 | 4,125,218 | 1.4 |
| Dog bite | 51,486 | 3,033,931 | 2,832,649 | 3,245,171 | 1.1 |
| Motorcyclist | 35,857 | 2,298,615 | 1,815,096 | 2,915,154 | 0.8 |
| Pedestrian | 36,914 | 1,763,852 | 1,347,571 | 2,310,122 | 0.6 |
| Firearm gunshot | 16,846 | 669,514 | 412,522 | 1,072,557 | 0.2 |
| Inhalation/suffocation | 8,605 | 450,939 | 385,020 | 522,528 | 0.2 |
| Natural/environmental | 8,096 | 444,119 | 330,017 | 577,530 | 0.2 |
| BB/pellet gunshot | 2,950 | 161,012 | 137,507 | 192,510 | 0.1 |
| Drowning/near drowning | 1,192 | 58,064 | 27,501 | 82,504 | 0.0 |
n = actual number, N = estimated number, L 95% CL is the lower 95% confidence limit of the estimate, U 95% CL is the upper 95% confidence limit of the estimate.
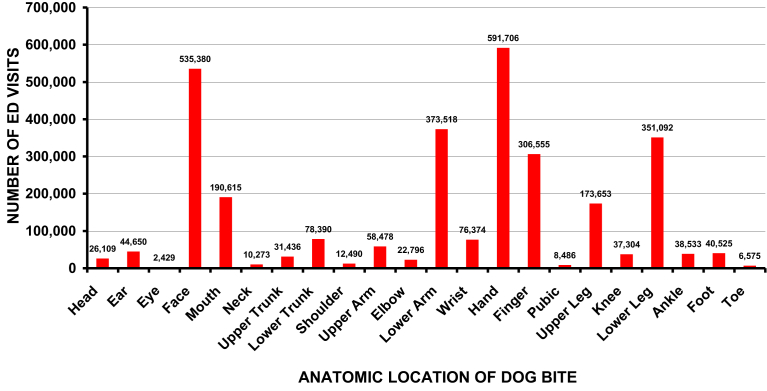
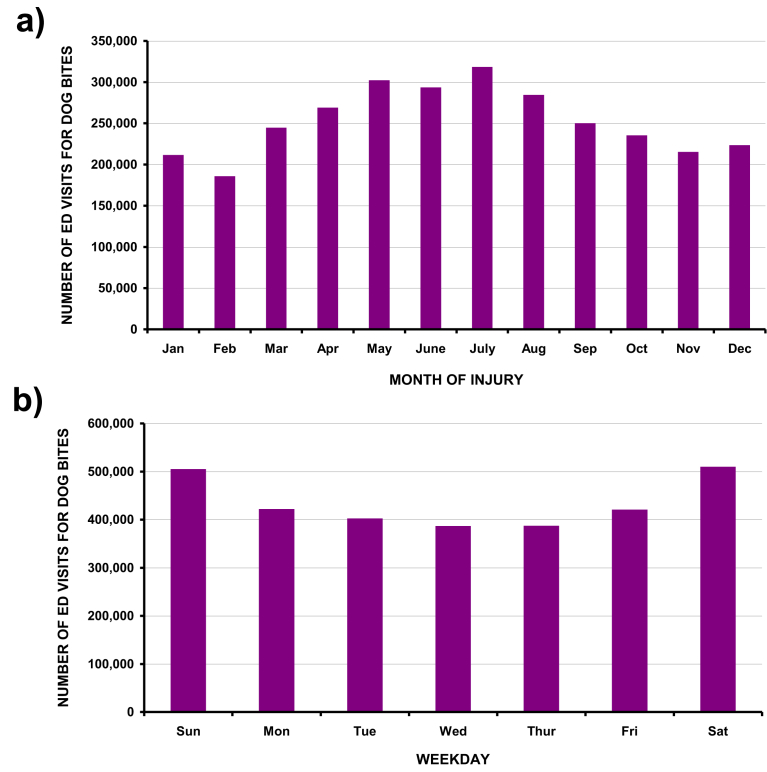
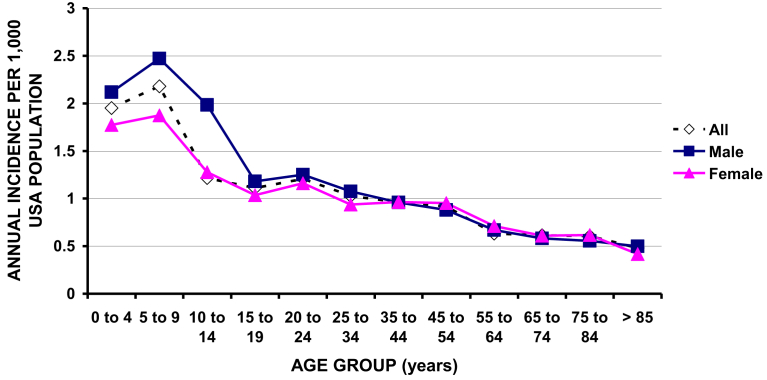
The average age of those with dog bites was 28.9 [28.0, 29.8] years and median age 24 [23.6, 26.2] years. The dog bite was unintentional in 98.8% [98.1, 99.2], due to legal intervention in 1.1% [0.7, 1.8], and an assault in 0.2% [0.1, 0.3]. The gender was male in 52.6% [51.5, 53.7] and female in 47.4% [46.3, 48.5]; the race was 71.6% [62.5, 81.0] White, 13.3% [9.3, 18.7] Black, 11.5% [6.3, 20.2] Amerindian, and 2.4% [1.0, 5.3] Asian. The bite occurred in the upper extremity in 47.3% [46.0, 48.7], head/neck in 26.8% [25.2, 28.5], lower extremity in 21.5% [19.9, 23.1], lower trunk in 2.9% [2.6, 3.2], and upper trunk in 1.5% [1.3, 1.6]. Detailed anatomic locations are shown in Fig. 1. The majority (80.2% [77.7, 82.4]) of the bites occurred at home, 7.1% [5.9, 9.2] on the street, 2.5% [2.0, 3.2] at schools or sporting places, and the remaining 10% [7.7, 12.1] at other locations. The patients were treated and released from the ED in 98.3% [97.8, 98.7] and hospitalized in 1.7% [1.3, 2.2]. Bites were more common in the summer and on weekends (Fig. 2). The overall annual incidence of dog bite injures seen in US EDs was 1.1 per 1,000 US population. There were significant differences by age and gender (Fig. 3), with males having a slightly higher incidence (1.18 vs 1.02 per 1,000). The peak incidence was 2.18 per 1,000 in the 5–9 year age group and the lowest 0.47 per 1,000 in those ≥85 years old. Detailed results are shown in Table 2. From here forward, only the estimated values are given, with the 95% confidence limits in the tables.
Fig. 1.
Anatomic location of the estimated 3.03 million non-fatal dog bites.
Fig. 2.
Temporal variation of dog bites. a. By month. b. By weekday.
Fig. 3.
Incidence of dog bite visits to US EDs in 1,000 per US population: differences by age and gender.
Table 2.
Demographic variables of the dog bite injuries over 9 years.
| n | N | L 95% CL | U 95% CL | % | |
|---|---|---|---|---|---|
| Average age (yrs) | 28.9 | 28 | 29.8 | ||
| Median age (yrs) | 24.3 | 23.6 | 26.2 | ||
| Age group (yrs) | |||||
| 0 to 4 | 7,379 | 352,370 | 322,198 | 384,999 | 11.6 |
| 5 to 9 | 8,020 | 393,264 | 371,043 | 416,551 | 13 |
| 10 to 14 | 6,138 | 306,753 | 286,095 | 328,872 | 10.1 |
| 15 to 19 | 3,769 | 217,612 | 200,843 | 235,732 | 7.2 |
| 20 to 24 | 3,647 | 235,112 | 219,046 | 252,115 | 7.7 |
| 25 to 34 | 5,912 | 377,188 | 356,177 | 398,955 | 12.4 |
| 35 to 44 | 5,343 | 361,431 | 343,131 | 380,448 | 11.9 |
| 45 to 54 | 5,298 | 363,934 | 338,884 | 390,763 | 12 |
| 55 to 64 | 3,192 | 219,792 | 202,360 | 238,766 | 7.2 |
| 65 to 74 | 1,592 | 115,155 | 103,759 | 128,030 | 3.8 |
| 75 to 84 | 915 | 69,867 | 60,981 | 80,094 | 2.3 |
| >85 | 278 | 21,398 | 18,203 | 25,181 | 0.7 |
| Sex | |||||
| Male | 27,686 | 1,595,929 | 1,562,982 | 1,628,814 | 52.6 |
| Female | 23,795 | 1,437,810 | 1,404,925 | 1,470,757 | 47.4 |
| Race | |||||
| White | 25,412 | 1,725,572 | 1,506,841 | 1,951,858 | 71.6 |
| Black | 7,884 | 321,477 | 283,364 | 567,335 | 13.3 |
| Amerindian | 5,468 | 278,162 | 191,438 | 612,540 | 11.5 |
| Asian | 946 | 57,193 | 31,552 | 161,402 | 2.4 |
| Anatomic location of injury | |||||
| Head/neck | 15,483 | 809,455 | 760,779 | 860,103 | 26.8 |
| Upper trunk | 807 | 43,926 | 39,744 | 49,149 | 1.5 |
| Lower trunk | 1,535 | 86,876 | 79,184 | 96,477 | 2.9 |
| Arm/hand | 22,382 | 1,429,428 | 1,396,494 | 1,476,588 | 47.3 |
| Leg/foot | 10,900 | 647,863 | 602,528 | 701,736 | 21.5 |
| Other | 25 | 1,597 | 910 | 2,730 | 0.1 |
| Detailed anatomic locations | |||||
| Head | 528 | 26,109 | 21,133 | 32,001 | 0.9 |
| Ear | 827 | 44,650 | 40,654 | 49,452 | 1.5 |
| Eye | 41 | 2,429 | 1,517 | 3,641 | 0.1 |
| Face | 10,361 | 535,380 | 500,590 | 577,650 | 17.7 |
| Mouth | 3,520 | 190,615 | 177,785 | 206,304 | 6.3 |
| Neck | 206 | 10,273 | 8,495 | 12,742 | 0.3 |
| Upper trunk | 576 | 31,436 | 27,608 | 36,103 | 1 |
| Lower trunk | 1,379 | 78,390 | 71,296 | 87,072 | 2.6 |
| Shoulder | 231 | 12,490 | 10,315 | 15,169 | 0.4 |
| Upper arm | 945 | 58,478 | 52,486 | 65,835 | 1.9 |
| Elbow | 353 | 22,796 | 19,417 | 27,002 | 0.8 |
| Lower arm | 5,874 | 373,518 | 356,481 | 395,314 | 12.4 |
| Wrist | 1,171 | 76,374 | 70,386 | 83,735 | 2.5 |
| Hand | 9,196 | 591,706 | 566,728 | 623,462 | 19.6 |
| Finger | 4,843 | 306,555 | 294,893 | 321,894 | 10.2 |
| Pubic | 156 | 8,486 | 6,675 | 11,225 | 0.3 |
| upper leg | 2,994 | 173,653 | 160,189 | 189,921 | 5.8 |
| Knee | 645 | 37,304 | 31,856 | 43,991 | 1.2 |
| Lower leg | 5,794 | 351,092 | 323,411 | 384,696 | 11.6 |
| Ankle | 647 | 38,533 | 33,373 | 44,901 | 1.3 |
| Foot | 705 | 40,525 | 345,862 | 47,632 | 1.3 |
| Toe | 115 | 6,575 | 4,854 | 9,102 | 0.2 |
| 25–50% body | 4 | 276 | 0 | 910 | 0 |
| All body | 20 | 1,296 | 607 | 2,427 | 0 |
| Internal | 1 | 25 | 0 | 303 | 0 |
| Diagnosis | |||||
| Contusion/abrasion | 3,422 | 184,953 | 150,208 | 226,827 | 6.1 |
| Fracture | 417 | 23,540 | 19,382 | 28,467 | 0.8 |
| Laceration | 18,349 | 955,588 | 836,440 | 1,087,038 | 31.6 |
| Puncture | 15,877 | 840,057 | 681,409 | 1,023,023 | 27.7 |
| Other | 13,318 | 1,024,258 | 761,807 | 1,328,231 | 33.8 |
| Incident locale | |||||
| Home/Apt/mobile | 28,281 | 1,719,945 | 1,666,554 | 1,768,689 | 80.2 |
| School/sports | 955 | 53,501 | 42,270 | 67,804 | 2.5 |
| Street | 2,634 | 151,846 | 125,523 | 198,261 | 7.1 |
| Other property | 3,564 | 210,475 | 167,364 | 263,061 | 9.8 |
| Farm | 45 | 3,619 | 2,575 | 5,364 | 0.2 |
| Disposition from ED | |||||
| Treated/released | 49,333 | 2,937,229 | 2,922,113 | 2,949,006 | 98.3 |
| Admitted | 1,360 | 50,922 | 39,145 | 66,038 | 1.7 |
| Stratum (Hospital size) | |||||
| Small | 6,332 | 763,029 | 589,493 | 967,217 | 25.1 |
| Medium | 7,331 | 909,989 | 682,016 | 1,175,931 | 30 |
| Large | 9,136 | 817,104 | 599,494 | 1,078,543 | 26.9 |
| Very large | 20,808 | 474,939 | 354,660 | 626,496 | 15.7 |
| Children's | 7,879 | 68,869 | 46,722 | 101,028 | 2.3 |
| Year | |||||
| 2005 | 5,530 | 321,980 | 296,415 | 349,205 | 10.6 |
| 2006 | 5,064 | 310,892 | 282,459 | 341,924 | 10.2 |
| 2007 | 5,350 | 312,561 | 285,493 | 341,924 | 10.3 |
| 2008 | 5,656 | 333,256 | 311,281 | 356,487 | 11 |
| 2009 | 5,932 | 337,483 | 323,417 | 352,239 | 11.1 |
| 2010 | 5,891 | 346,943 | 330,698 | 363,768 | 11.4 |
| 2011 | 6,051 | 360,362 | 339,193 | 382,579 | 11.9 |
| 2012 | 6,157 | 363,456 | 335,249 | 393,804 | 12 |
| 2013 | 5,855 | 346,997 | 323,720 | 371,657 | 11.4 |
| Month | |||||
| Jan | 3,609 | 211,386 | 193,565 | 230,882 | 7 |
| Feb | 3,170 | 185,831 | 175,058 | 197,206 | 6.1 |
| Mar | 4,231 | 244,772 | 234,523 | 255,457 | 8.1 |
| Apr | 4,624 | 269,031 | 256,974 | 281,549 | 8.9 |
| May | 5,209 | 302,343 | 285,493 | 320,080 | 10 |
| June | 5,201 | 293,715 | 279,122 | 308,854 | 9.7 |
| July | 5,380 | 318,355 | 307,641 | 329,182 | 10.5 |
| Aug | 4,798 | 284,510 | 274,874 | 294,595 | 9.4 |
| Sep | 4,128 | 250,045 | 239,984 | 260,615 | 8.2 |
| Oct | 3,893 | 235,245 | 222,994 | 248,176 | 7.8 |
| Nov | 3,549 | 215,274 | 206,307 | 224,511 | 7.1 |
| Dec | 3,694 | 223,424 | 213,892 | 233,309 | 7.4 |
| Day | |||||
| Sun | 8,692 | 504,930 | 490,890 | 519,106 | 16.6 |
| Mon | 7,217 | 421,953 | 410,491 | 433,549 | 13.9 |
| Tue | 6,763 | 402,448 | 392,287 | 412,918 | 13.3 |
| Wed | 6,558 | 386,790 | 375,904 | 398,052 | 12.7 |
| Thur | 6,642 | 386,991 | 371,960 | 402,603 | 12.8 |
| Fri | 7,009 | 421,032 | 409,581 | 432,639 | 13.9 |
| Sat | 8,605 | 509,786 | 494,227 | 525,780 | 16.8 |
n = actual number, N = estimated number, U 95% CL is upper 95% confidence limit of the estimate, L 95% CL is the lower 95% confidence limit of the estimate.
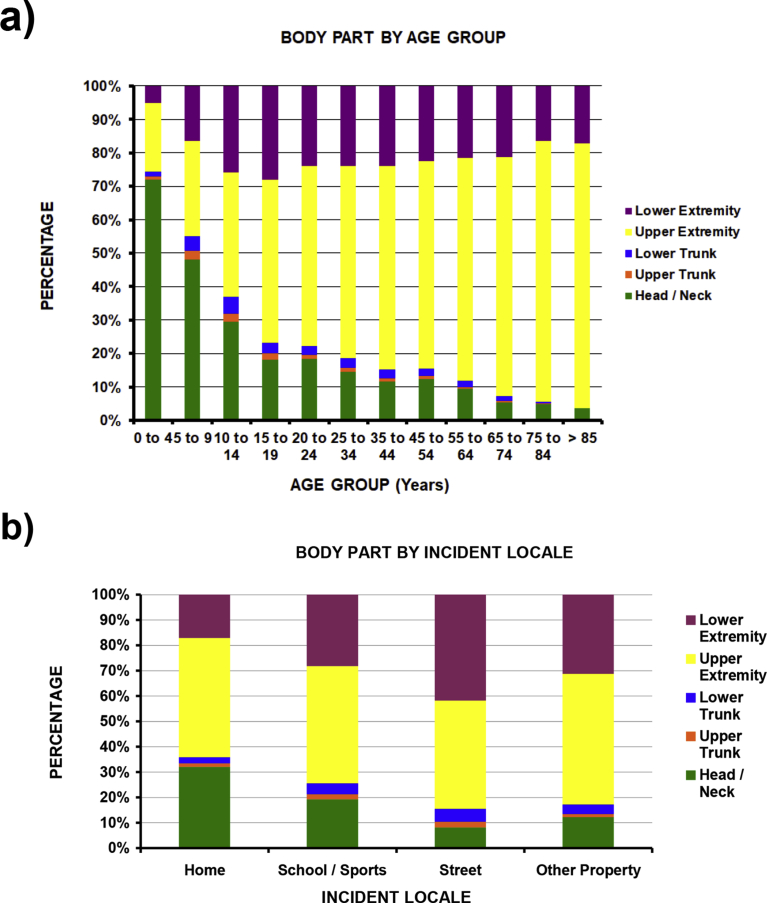
3.1. Analyses by anatomic area of injury
There were notable differences by age and incident locale (P < 10−4). Younger patients had more bites involving the head/neck, while older patients the upper extremity (Fig. 4a). The average age for those with head/neck bites was 15.3, upper trunk 20.7, lower trunk 24.0, upper extremity 36.0, and lower extremity 31.5 years. Lower extremity bites more commonly occurred on the street (41.8%) compared to other locations (17.1%–30.9%) (P < 10−4) (Fig. 4b). Detailed results are shown in Supplemental Table 1.
Fig. 4.
Differences in dog bites by anatomic location of injury (all P < 10−4). a. By age. b. By incident locale.
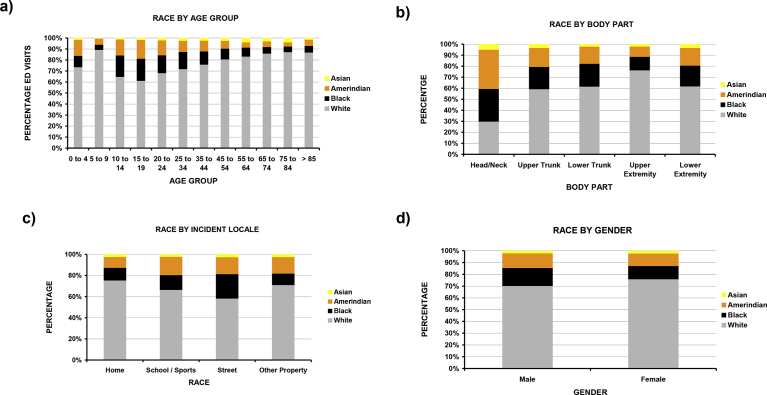
3.2. Analyses by race
There were differences by race for age, incident locale, and anatomic location of the bite (Fig. 5). Although all age groups demonstrated a White predominance (71.6% White, 24.9% Black/Amerindian), Amerindians and Blacks comprised a larger proportion of those 10–34 years of age (31.6%–27.3%) (P < 10−4) (Fig. 5a), bites to the trunk (P < 10−4) (3.6% Whites, 6.4% Black/Amerindian) (Fig. 5b), and those occurring on the street (P = 0.017) (60% White, 14.3% Black/Amerindian) (Fig. 5c). White patients were 75.7% female and 70.0% male (P < 10−4) (Fig. 5d). Detailed results are shown in Supplemental Table 2.
Fig. 5.
Differences in dog bites by race (all P < 10−4). a. By age group. b. By anatomic location of injury. c. By incident locale. d. By gender.
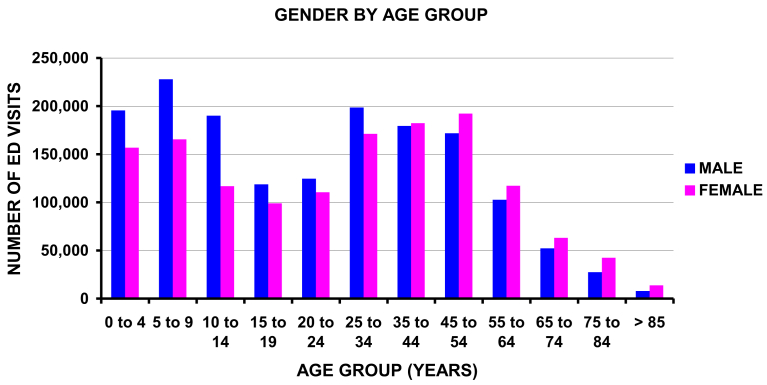
3.3. Analyses by gender
The most striking differences were by age. The average age for males was 26.9 years and for females 31.1 years (P < 10−4), with males having a higher proportion in those <35 years old and females in those ≥45 years old (Fig. 6). Detailed results are shown in Supplemental Table 3.
Fig. 6.
Number of ED visits for dog bites by gender and age group (P < 10−4).
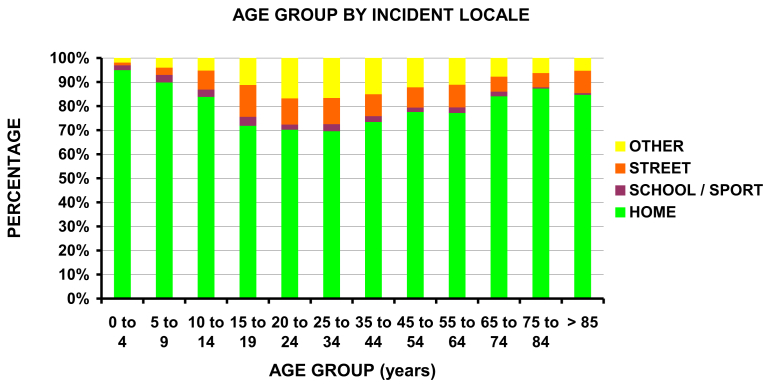
3.4. Analyses by incident locale
In addition to the above findings, there was a significant difference by age group (Fig. 7). For those <10 years of age the bite nearly always occurred in the home (P < 10−4).
Fig. 7.
Differences in incident locale by age group (P < 10−4).
3.5. Outcome predictors from multivariate logistic regression analysis
The most common bite locations were the head/neck, upper, and lower extremity. A hospital admission was used as a surrogate for a serious injury. Multivariate logistic regression was used to determine predictors of the following outcomes: a hospital admission, and bite to the head/neck, upper, and lower extremities. The variables entered into the model were gender, race, age group, and incident locale.
The only predictor (Table 3) for hospital admission was the age group. The OR for admission was greater for the older and younger patients, and lowest for those 10–14 years of age. The OR for those >85 years of age was 11.03 [4.68, 26.01], 75–84 years 4.88 [2.89, 8.24], and those ≤4 years of age 2.79 [1.77, 4.39] with the 10–14 year age group the reference group. Predictors of a bite to the head/neck, upper extremity, and lower extremity were all dependent upon the age group, race, and incident locale. A bite to the head neck was most common in those ≤4 years of age (OR 100.2 [43.2, 232.4]) and decreased with increasing age, with the reference group those >85 years of age. Such bites most commonly occurred in the home (OR 3.13 [2.74, 3.58] with the street the reference group. They were more likely in Whites (OR 2.06 [1.69, 2.50]) with Blacks the reference group. By contrast, a bite to the upper extremity was most likely in the oldest group >85 years of age (OR 15.49 [9.17, 26.15] with the reference group those ≤4 years of age. Upper extremity bites occurred most commonly at home (OR 1.54 [1.30, 1.81]) with the street the reference group. They were also more likely in Whites (OR 1.36 [1.12, 1.66]) with Asians the reference group. A bite to the lower extremity was most common in those 10-14 years (OR 5.82 [4.49, 7.56]) and 15-19 years (OR 5.69 [4.17, 7.77]) of age with the reference group those ≤4 years of age. They were most likely to occur on the street (OR 2.48 [2.22, 2.77]) with home being the reference group, and in Amerindians (OR 2.06 [1.43, 2.96]) and Asians (OR 2.07 [1.78, 2.38] with Whites the reference group.
Table 3.
Multivariate logistic regression analyses predicting a hospital admission, and a dog bite to the head/neck, upper extremity, or lower extremity over 9 years.
| Head/neck bite |
Upper extremity bite |
Lower extremity bite |
Hospital admission |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | L 95% CL | U 95% CL | p value | OR | L 95% CL | U 95% CL | p value | OR | L 95% CL | U 95% CL | p value | OR | L 95% CL | U 95% CL | p value | |
| Age group (yrs) | ||||||||||||||||
| 0 to 4 | 100.2 | 43.21 | 232.43 | <10−4 | R | - | - | - | R | - | - | - | 2.79 | 1.77 | 4.39 | <10−4 |
| 5 to 9 | 36.29 | 17.46 | 75.42 | <10−4 | 1.67 | 1.4 | 1.99 | <10−4 | 3.34 | 2.64 | 4.21 | <10−4 | 1.56 | 1 | 2.44 | 0.052 |
| 10 to 14 | 16.12 | 7.94 | 32.75 | <10−4 | 2.7 | 2.17 | 3.35 | <10−4 | 5.82 | 4.49 | 7.56 | <10−4 | R | - | - | - |
| 15 to 19 | 9.67 | 4.77 | 19.62 | <10−4 | 4.51 | 3.62 | 5.61 | <10−4 | 5.69 | 4.17 | 7.77 | <10−4 | 1.54 | 0.81 | 2.91 | 0.19 |
| 20 to 24 | 10.06 | 5.21 | 19.43 | <10−4 | 5.41 | 4.25 | 6.89 | <10−4 | 4.62 | 3.6 | 5.93 | <10−4 | 1.33 | 0.8 | 2.24 | 0.27 |
| 25 to 34 | 7.25 | 3.64 | 14.45 | <10−4 | 6.41 | 5.18 | 7.93 | <10−4 | 4.71 | 3.69 | 6.03 | <10−4 | 1.6 | 1.1 | 2.31 | 0.014 |
| 35 to 44 | 5.12 | 2.8 | 9.21 | <10−4 | 7.7 | 5.84 | 10.15 | <10−4 | 4.84 | 3.74 | 6.24 | <10−4 | 2.04 | 1.22 | 3.43 | 0.008 |
| 45 to 54 | 5.25 | 2.63 | 10.48 | <10−4 | 7.68 | 5.75 | 10.25 | <10−4 | 4.83 | 3.86 | 6.03 | <10−4 | 2.72 | 1.55 | 4.76 | 0.0007 |
| 55 to 64 | 3.99 | 2.06 | 7.74 | 0.0001 | 9.27 | 6.85 | 12.54 | <10−4 | 4.75 | 3.84 | 5.88 | <10−4 | 3.66 | 2.3 | 5.83 | <10−4 |
| 65 to 74 | 1.92 | 1.06 | 3.49 | 0.033 | 11.11 | 8.8 | 14.04 | <10−4 | 5.15 | 3.77 | 7.03 | <10−4 | 3 | 1.79 | 5.05 | 0.0001 |
| 75 to 84 | 1.89 | 1.1 | 3.24 | 0.022 | 15.02 | 10.69 | 21.09 | <10−4 | 3.68 | 2.7 | 5.03 | <10−4 | 4.88 | 2.89 | 8.24 | <10−4 |
| >85 | R | - | - | - | 15.49 | 9.17 | 26.15 | <10−4 | 4.67 | 2.98 | 7.32 | <10−4 | 11.03 | 4.68 | 26.01 | <10−4 |
| Incident locale | ||||||||||||||||
| Home | 3.13 | 2.74 | 3.58 | <10−4 | 1.54 | 1.3 | 1.81 | <10−4 | R | - | - | - | ||||
| Street | R | - | - | - | R | - | - | 2.48 | 2.22 | 2.77 | <10−4 | |||||
| Other property | 1.54 | 1.2 | 1.98 | 0.001 | 1.33 | 1.15 | 1.54 | 0.00002 | 1.78 | 1.56 | 2.04 | <10−4 | ||||
| Race | ||||||||||||||||
| White | 2.06 | 1.69 | 2.5 | <10−4 | 1.36 | 1.12 | 1.66 | 0.003 | R | - | - | - | ||||
| Black | R | - | - | - | 1.3 | 1.08 | 1.57 | 0.006 | 1.72 | 1.48 | 1.98 | <10−4 | ||||
| Amerindian | 1.25 | 0.96 | 1.62 | 0.092 | 1.07 | 0.8 | 1.43 | 0.65 | 2.06 | 1.43 | 2.96 | 0.0002 | ||||
| Asian | 1.23 | 0.92 | 1.64 | 0.16 | R | - | - | 2.07 | 1.78 | 2.38 | <10−4 | |||||
OR = odds ratio, L95% CL = lower 95% confidence limit of the OR, U95% CL = upper 95% confidence limit of the OR, R = reference group.
4. Discussion
This is the first study to the author's knowledge to analyze the demographics of non-fatal human dog bite ED visits across the entire US for all age groups, geographic locations (ie. both rural and urban), and ED disposition (released/admitted). It likely portrays the most representative national analysis of dog bite injuries, which is the major strength of this study. There are certain limitations as well. First, the NEISS only identifies individuals who sought care in an ED. It does not include those who might have been treated in urgent care centers, physician offices, or those persons who did not seek medical care. Thus the overall number of injuries in this study is likely lower than the true number. Another potential limitation is the accuracy of the NEISS data. However two studies have demonstrated over 90% accuracy [26, 27]. Other limitations are lack of detailed data. The severity of the injury, aside from either the patient being treated and released or admitted, is unknown. As the vast majority of the patients were released from the ED, injury severity is likely minor overall. Another area lacking information is the diagnosis, and was given as “other” in 33.8% of the cases. This likely represents the injury being a dog bite, as that is a valid NEISS data base code as a cause of injury. However, this can not be confirmed.
In this study the average annual incidence of dog bites seen in US EDs was 1.1 per 1,000. This is similar to the 1.05 per 1,000 in North Carolina [20], 1.3 per 1,000 in the US [13], 1.71 per 1,000 in Milwaukee [28], and 0.8 per 1,000 in Los Angles [10]. It is greater than the 0.4 per 1,000 [11] in New York City and less than the 2.35 per 1,000 in Bay County, Florida [8]. However the Florida study used ED visits as well as data from animal control agencies, schools, and county health departments which obviously increases the numbers. In Baltimore, Maryland, when using hospital and police records, the annual incidence was 6.42 per 1,000 [29]. A detailed Internet survey of dog owners in The Netherlands [5] found an ED visit incidence of 0.7 per 1,000 while the self reported incidence was 8.3 per 1,000. This much higher incidence, similar to the 6.43 in Baltimore, was due to the fact that 62% sought no treatment, 29% were treated by their personal physician, and only 8.3% were treated in the ED. Under reporting of dog bites has also been noted in Pennsylvania children, with up to 45% having been bitten during childhood [30]. These studies [5, 29] suggest that ED visits for dog bites account for only ∼8% of all dog bites. Another study suggested that 17% of dog bites were reported [31]. It must be remembered, however, that these unreported cases, which likely constitute the majority of dog bite incidents, as well as those that did not seek medical attention, were likely very minor in severity. They were most likely treated at home with simple cleansing and a dressing. In fact, what the individuals in these questionnaire studies considered a dog bite is not known. Even in those that presented to the ED for medical care in this study, only 1.7% were admitted to the hospital. Finally, many may visit the ED not for the severity of the injury but for other concerns, such as infection, concern for rabies, etc.
There are several notable findings in this study. The first is the rapid change in anatomic location of the bite by age (Fig. 4a). Several authors [14, 21, 32, 33] have noted that children are more likely to sustain bites to the head and neck, while adults are more likely to sustain bites to the extremities. However, a breakdown of anatomic location by detailed age groups has not been described until now. The rapid drop in the percentage of bites to the head/neck with a corresponding increase in upper extremity bites is likely due to the size and motor ability of the patient. Children are shorter than adults which places their head/neck at the same level as the dog's mouth; for adults, the dog's mouth is at the level of the lower extremity, or the hand if reaching toward the dog [34]. Children, especially younger ones, are not as agile or fast, and thus when encountered with a dog beginning to bite, likely can not defend themselves as quickly due their inability to rapidly raise their upper extremity and/or run away as means of defense. Thus the dog could easily bite their head/face/neck due to anatomic proximity.
Using hospital admission as a proxy for severity, logistic regression demonstrated analysis that the OR for admission was the age group. The OR for admission was greater for the older and younger patients, and lowest for those 10–14 years of age. It is likely that the very young, having more bites to the head/neck, might require general anesthesia for repair, thus resulting in a higher admission. Similarly, the elderly typically have more medical comorbidities, and thus were likely admitted more frequently for aggressive medical care (eg intravenous antibiotics, monitoring of systemic diseases [diabetes, cardiac, peripheral vascular disease]). These are however suppositions, as the data is not adequately detailed to prove these postulates.
The financial burden of dog bites is large. According to the Health Care Cost Institute, the average price of an ED visit in the US in 2016 was $1917.20, the average cost of a surgical admission was $41,701.60, and the average cost of a medical admission was $18,464.62 [35, 36]. Assuming that the costs for those admitted with dog bites in this study was the average of the surgical and medical groups ($30,083.11), then the overall expenditure in 2016 US$ for these nine years was $7.163 billion ($5.631 billion for those treated and released from the ED and $1.532 billion for those admitted to the hospital), or an annual $795 million in the US alone. This is likely an inflated estimate as the average ED cost is likely skewed by more expensive cases. In 2006–2008, the median ED charge for an open wound of an extremity (likely similar to a dog bite) was $979 [37]. This equates to $1,146 in 2016 dollars (CPI Inflation Calculator, Bureau of Labor Statistics https://data.bls.gov/cgi-bin/cpicalc.pl). Using this value, then the ED cost for those treated and release is $3.366 billion over 9 years, or $374 million annually. It must be remembered that these cost estimates do not include those that were treated in non ED venues, costs of subsequent follow-up care, and medications (eg. antibiotics).
More needs to be done to prevent dog bite injuries [38] for both the patient and society. According to the American Veterinary Medical Association [18], dogs bite for a variety of reasons, “but most commonly as a reaction to something. If the dog finds itself in a stressful situation, it may bite to defend itself or its territory. Dogs can bite because they are scared or have been startled. They can bite because they feel threatened. They can bite to protect something that is valuable to them, like their puppies, their food or a toy. Dogs might bite because they aren't feeling well. They could be sick or sore due to injury or illness and might want to be left alone. Dogs also might nip and bite during play. Even though nipping during play might be fun for the dog, it can be dangerous for people. It's a good idea to avoid wrestling or playing tug-of-war with your dog. These types of activities can make your dog overly excited, which may lead to a nip or a bite.” Understanding these reasons is the first step in prevention [18]. The various avenues suggested to prevent dog bites are socialization, responsible pet ownership, education, avoiding risky situations, and paying attention to the dog's body language.
In this study, 35% of the injuries occurred in those <14 years old, with the vast majority occurring at home (Fig. 7). Directing education to this age group is thus important. Education can occur in schools and/or the Internet [30, 39, 40]. One opportune time is just before school finishes for the summer break, as there were more bites in the summer. Education should also be directed to the parents/care takers. This could occur in many ways: pamphlets in medical offices (human and veterinary) and emergency departments [41, 42]; radio, television, and Internet public service announcements; and prospective dog owners visiting animal shelters, kennels, breeders, etc. The manner of education has been previously outlined and consists of denoting the responsibilities of owning a dog [17, 31], appropriate handling of the dog [5]; and potential dangers of the dog [28], as well as the American Veterinary Medical Association guidelines [18]. Simply ensuring that young children are not in the presence of a dog (Fig. 3) without supervision would be a very simple way to minimize these injuries.
5. Conclusion
Non-fatal human dog bites account for 1.1% of ED injury visits in the US with an average annual incidence of 1.1 per 1000; 98.8% were unintentional and 80.2% occurred at home. The average age of those was 28.9 years with a slight male predominance (52.6%), especially in those <35 years of age. The bite was located in the upper extremity in 47.3%, head/neck in 26.8%, lower extremity in 21.5%, and trunk in 4.4%. Hospital admission was rare 1.7%, and there was a higher occurrence in the summer and on weekends. Potential prevention strategies are educational programs directed at both those children able to comprehend the information as well as all parents/caretakers outlining the responsibilities of owning a dog along with appropriate handling and potential dangers of a dog. Information can also be disseminated in health care facilities, radio/TV/Internet venues, and dog kennels/shelters. One of the easiest prevention methods is to ensure that young children are never the unsupervised presence of a dog. Dog bite injuries represent a significant financial burden to society with a conservative estimate of an annual 400 million US$ in the USA alone.
Declarations
Author contribution statement
Randall T. Loder: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This work was supported in part by the Garceau Professorship Fund and the Rapp Pediatric Orthopaedic Research Fund, Riley Children's Foundation.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
This study was supported in part by the Garceau Professorship Fund and the Rapp Pediatric Orthopaedic Research Fund, Riley Children's Foundation.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
References
- 1.Springer J. American Pet Products Association; Greenwich, CT: 2018. The 2017–2018 APPA National Pet Owners Survey.https://americanpetproducts.org/Uploads/MemServices/GPE2017_NPOS_Seminar.pdf [Google Scholar]
- 2.Statista.com . 2018. Estimated Pet Population in the United Kingdom.https://www.statista.com/statistics/308229/estimated-pet-population-in-the-united-kingdom-uk [Google Scholar]
- 3.Vest G.G. The History PlaceTM. Great Speeches Collection. 1855. Tribute to the dog. [Google Scholar]
- 4.Palacio J., León M., García-Belenguer S. Aspectos epidemiológicos de las moreduras caninas (Epidemiological apsects of dog bites) Gac. Sanit. 2005;19:50–58. doi: 10.1157/13071818. [DOI] [PubMed] [Google Scholar]
- 5.Cornelissen J.M.R., Hopster H. Dog bites in The Netherlands: a study of victims, injuries, circumstances and aggressors to support evaluation of breed specific legislation. Vet. J. 2010;186:292–298. doi: 10.1016/j.tvjl.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Morgan M., Palmer J. Dog bites. BMJ. 2007;334:413–417. doi: 10.1136/bmj.39105.659919.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patronek G.J., Slavinski S.A. Animal bites. J. Am. Vet. Med. Assoc. 2009;234:336–345. doi: 10.2460/javma.234.3.336. [DOI] [PubMed] [Google Scholar]
- 8.Matthias J., Templin M., Jordan M.M., Stanek D. Cause, setting and ownership analysis of dog bites in Bay County, Florida from 2009 to 2010. Zoonoses Pub. Health. 2015;62:38–43. doi: 10.1111/zph.12115. [DOI] [PubMed] [Google Scholar]
- 9.Rhea S., Weber D.J., Poole C., Cairns C. Risk factors for hospitalization after dog bite injury: a case-cohort study of emergency department visits. Acad. Emerg. Med. 2014;21:196–203. doi: 10.1111/acem.12312. [DOI] [PubMed] [Google Scholar]
- 10.Lyu C., Jewell M.P., Piron J., Enhert K., Beeler E., Swanson A. Burden of bites by dogs and other animals in Los Angeles county, California, 2009–2011. Public Health Rep. 2016;13:800–808. doi: 10.1177/0033354916675148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bregman B., Slavinksi S. Using emergency department data to conduct dog and animal bite surveillance in New York City, 2003–2006. Public Health Rep. 2012;127:195–201. doi: 10.1177/003335491212700208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patrick G.R., O'Rourke K.M. Dog and cat bites: epidemiologic analyses suggest different prevention strategies. Public Health Rep. 1998;113:252–257. [PMC free article] [PubMed] [Google Scholar]
- 13.Weiss H.B., Friedman D.I., Coben J.H. Incidence of dog bite injuries treated in emergency departments. JAMA. 1998;279:51–53. doi: 10.1001/jama.279.1.51. [DOI] [PubMed] [Google Scholar]
- 14.Gandhi R.R., Liebman M.A., Stafford B.L., Stafford P.W. Dog bite injuries in children: a preliminary survey. Am. Surg. 1999;65:863–864. [PubMed] [Google Scholar]
- 15.Kaye A.E., Belz J.M., Kirschner R.E. Pediatric dog bite injuries: a 5-year review of the experience at the Children's Hospital of Philadelphia. Plast. Reconstr. Surg. 2009;124:551–558. doi: 10.1097/PRS.0b013e3181addad9. [DOI] [PubMed] [Google Scholar]
- 16.Ellis R., Ellis C. Dog and cat bites. Am. Fam. Phys. 2014;90:239–243. [PubMed] [Google Scholar]
- 17.Voelker R. Dog bites recognized as a public health problem. JAMA. 1997;277:278–279. doi: 10.1001/jama.277.4.278. [DOI] [PubMed] [Google Scholar]
- 18.American Veterinary Medical Association . 2019. Dog Bite Prevention.www.avma.org/public/Pages/Dog-Bite-Prevention.aspx?mode [Google Scholar]
- 19.Nilson F., Damsager J., Lauritsen J., Bonander C. The effect of breed-specific legislation on hospital treated dog bites in Odense, Denmark – a time series intervention study. PLoS One. 2018;13(1–8):e0208393. doi: 10.1371/journal.pone.0208393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rhea S.K., Weber D.J., Poole C., Waller A.E., Ising A.I., Williams C. Use of statewide emergency department surveillance data to assess incidence of animal bite injuries among humans in North Carolina. J. Am. Vet. Med. Assoc. 2014;244:597–603. doi: 10.2460/javma.244.5.597. [DOI] [PubMed] [Google Scholar]
- 21.Golinko M.S., Arslanian B., Williams J.K. Characteristics of 1616 consecutive dog bite injuries at a single institution. Clin. Pediatr. 2016;2016:1–10. doi: 10.1177/0009922816657153. [DOI] [PubMed] [Google Scholar]
- 22.Gersham K.A., Sacks J.J., Wright J.C. Which dogs bite? A case-control study of risk factors. Pediatrics. 1994;93:913–917. [PubMed] [Google Scholar]
- 23.Ting J.W.C., Yue B.Y.T., Tang H.H.F., Rizzitelli A., Shayan R., Ralola F. Emergency department presentations with mammalian bite injuries: risk factors for admission and surgery. Med. J. Austral. 2016;204:114. doi: 10.5694/mja15.00653. [DOI] [PubMed] [Google Scholar]
- 24.Rosado B., García-Belenguer S., León M., Palacio J. A comprehensive study of dog bites in Spain, 1995–2004. Vet. J. 2009;179:383–391. doi: 10.1016/j.tvjl.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 25.Eveleth P.B., Tanner J.M. second ed. University Press; Cambridge: 1990. Worldwide Variation in Human Growth. [Google Scholar]
- 26.Annest J.L., Mercy J.A., Gibson D.R., Ryan G.W. National estimates of nonfatal firearm-related injuries. Beyond the tip of the iceberg. JAMA. 1995;273:1749–1754. [PubMed] [Google Scholar]
- 27.Hopkins R.S. Consumer product-related injuries in Athens, Ohio, 1980–1985: assessment of emergency room-based surveillance. Am. J. Prev. Med. 1989;5:104–112. [PubMed] [Google Scholar]
- 28.Ndon J.A., Jach G.J., Wehrenberg W.B. Incidence of dog bites in Milwaukee, wis. Wis. Med. J. 1996;95:237–241. [PubMed] [Google Scholar]
- 29.Berzon D.R. The animal bite epidemic in Baltimore, Maryland: review and update. Am. J. Pub. Health. 1978;68:593–595. doi: 10.2105/ajph.68.6.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beck A.M., Jones B.A. Unreported dog bites in children. Public Health Rep. 1985;100:315–321. [PMC free article] [PubMed] [Google Scholar]
- 31.Sacks J.J., Kresnow M-j, Houston B. Dog bites: how big a problem? Inj. Prev. 1996;2:52–54. doi: 10.1136/ip.2.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Speirs J., Showery J., Abdou M., Pieral-Cruz M.A., Abdelgawd A.A. Dog bites to the upper extremity in children. J. Paediatr. Child Health. 2015;51:1172–1174. doi: 10.1111/jpc.12948. [DOI] [PubMed] [Google Scholar]
- 33.Reisner I.R., Nance M.L., Zeller J.S., Houseknecht E.M., Kassam-Adams N., Wiebe D.J. Behavioural characteristics associated with dog bites to children presenting to an urban trauma centre. Inj. Prev. 2011;17:348–353. doi: 10.1136/ip.2010.029868. [DOI] [PubMed] [Google Scholar]
- 34.Overall K.L., Love M. Dog bites to humans-demography, epidemiology, injury, and risk. JAVMA. 2001;218:1923–1934. doi: 10.2460/javma.2001.218.1923. [DOI] [PubMed] [Google Scholar]
- 35.Health Care Cost Institute . Health Care Cost Institute; 2018. 2016-HCCUR-Appendix-Tables-1.23.18-c.http://www.healthcostinstitute.org/report/2016-health-care-cost-utilization-report/ [Google Scholar]
- 36.Frost A., Hargraves J., Rodriguez S., Brennan N. Health Care Cost Institute; 2018. 2016 Health Care Cost and Utilization Report. [Google Scholar]
- 37.Caldwell N., Srebotnjak T., Wang T., Hsia R. “How much will I get charged for this?” Patient charges for top ten diagnoses in the emergency department. PLoS One. 2013;8(1–6) doi: 10.1371/journal.pone.0055491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.American Veterinary Medical Association A community approach to dog bite prevention. JAVMA. 2001;218:1732–1749. doi: 10.2460/javma.2001.218.1732. [DOI] [PubMed] [Google Scholar]
- 39.Schwebel D.C., McClure L.A., Severson J. Evaluating a website to teach children safety with dogs. Inj. Prev. 2015;21(1–6):e2. doi: 10.1136/injuryprev-2014-041286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lakestani N., Donaldson M.L. Dog bite prevention: effect of a short educational intervention for preschool children. PLoS One. 2015;10(1–14):e0134319. doi: 10.1371/journal.pone.0134319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shields W.C., McDonald E.M., Stepnitz R., McKenzie L.T., Gielen A.C. Dog bites: an opportunity for parent education in the pediatric emergency department. Ped. Emerg. Care. 2012;28:966–970. doi: 10.1097/PEC.0b013e31826c6c13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mannion C.J., Greenberg D. Dog bites – are vets missing an educational opportunity? Vet. Rec. 2016;178:535–536. doi: 10.1136/vr.i2541. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.