Abstract
Studies on the prevalence of hypertension in Vietnam have reported various estimates. There is no up-to-date assessment of the evidence on the magnitude of hypertension in Vietnam. Search engines for scientific and gray literature were used to identify relevant records for eligibility screening and quality assessment. Data from selected articles were extracted using standardized spreadsheets. Statistical analysis included estimating pooled prevalence and odds ratio, heterogeneity evaluation, meta-regression, and subgroup analysis, in addition to sensitivity analysis and publication bias evaluation. The pooled prevalence of measured hypertension in Vietnam was 21.1% (95% confidence interval = 18.5-23.7) based on 10 studies, and 18.4% (95% confidence interval = 15.2-21.8) based on 3 national surveys. Lower pooled prevalence was estimated for hypertension awareness (9.3%) and hypertension treatment (4.7%). The pooled prevalence of measured hypertension is significantly higher among men. The pooled prevalence of measured hypertension and hypertension awareness and treatment were significantly lower in rural settings. There is a need to strengthen efforts for primary and secondary prevention and disease management to reduce morbidity and mortality, especially in rural residence settings.
Keywords: prevalence, hypertension, Vietnam, meta-analysis, systematic review, awareness
Introduction
Rationale
Noncommunicable diseases caused 72.3% of global deaths in 2016, with cardiovascular diseases (CVDs) representing the highest proportion of these deaths.1 Primary hypertension (HTN) is one of the CVDs that is caused by different physiological and behavioral risk factors such as harmful use of alcohol, high body mass index, lead exposure, tobacco use, and a high-salt diet. Concurrently, high blood pressure (HBP) as a physiological risk factor contributes to a high burden of other noncommunicable diseases, for example, strokes and chronic kidney diseases.2,3 While the burden of HTN is increasing globally,1,4 low- and middle-income countries (LMICs) are enduring a higher burden due to their demographic, socioeconomic, urban, and/or epidemiological transitions.5
Primary prevention for HTN/HBP is possible by managing its risk factors; besides, HBP/HTN can be considered a modifiable risk factor since its management and control are secondary prevention measures for associated complications.6 Management of HBP/HTN includes promoting and supporting behavioral changes toward a more healthy living, in addition to treating and controlling through pharmacological interventions.7 In LMICs, management and control efforts are more complicated due to their weak health systems and limited resources.6,8 Vietnam established its national HTN program in 2008.9 Since then, studies on the prevalence of HTN, including few national samples, have been published and varied in their estimates. In 2012, a time trends analysis for blood pressure was performed using a dataset compiled by multiple cross-sectional studies; the analysis showed a significant increase of HTN prevalence of 0.9% per year between 2001 and 2009.10 There is no up-to-date assessment of the evidence on the magnitude of HTN in Vietnam. Consolidating available data in the literature into a national estimate of the prevalence of HTN is crucial to provide information for future policy regarding population need, management, and control of HTN in Vietnam.
Objectives
This article aims to perform a systematic review and a meta-analysis of the prevalence of HTN in Vietnam and its associated risk factors reported as relevant to the Vietnamese population, in addition to the prevalence of HTN awareness and treatment.
Methods
The reporting of this review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.11
Eligibility Criteria
Eligibility criteria for inclusion were community-based (ie, population-based) studies to detect hypertensive subjects among adult population (≥18 years) living in Vietnam. Study design could be cross-sectional or cohort. Exclusion criteria were the following: the population was refugees and migrants living outside Vietnam in addition to war veterans who are not Vietnamese; records that were abstracts, conference posters, reviews, and meta-analysis; articles reporting duplicated data; and studies that were facility-based or did not use random sampling.
Information Sources and Search Strategy
The following databases were searched: PubMed, EMBASE, CINAHL, and Web of Science (performed on October 13, 2017), in addition to gray literature (eg, governmental and international documents) through Google and relevant websites. The search terms incorporated a combination of keywords and index terms related to HTN (eg, CVDs, HTN, HBP) and the outcome (eg, prevalence, burden, morbidity, health need). Detailed tables on the search terms used are provided in Appendix 1 (all appendixes are available online). Furthermore, the reference lists of retrieved full-text records were searched to identify additional relevant records. The search strategy focused on records published in English; however, we reviewed relevant Vietnamese websites and documents to look for information on national surveys that might be only available in Vietnamese and not published in English.
Selection Process
One researcher (LM) screened the title and abstract using the Rayyan application.12 Then, full-texts were retrieved for selected records and assessed again for their eligibility. Finally, quality assessment was performed during data extraction to make a final decision on record’s inclusion in the meta-analysis.
Data Extraction
The data extraction was done using standardized spreadsheets. Since one researcher (LM) was available to perform the data extraction, it was conducted twice within 1 month to compare the results between 2 separate time points.13 The information extracted included (1) study characteristics: author, publication year, objective, project related to the study (if applicable), data collection year, location, sampling technique, sample size and response rate, HTN definition used, and type of statistical analysis and adjustment variables; (2) participants characteristics: age group targeted, mean age, proportions of women, and residence setting; and finally (3) outcome(s) of interest: number of hypertensive subjects in total and by risk factors categories, in addition to number of those aware of their HTN condition and/or treated.
Quality Assessment
Studies were assessed based on a checklist of 5 criteria covering both study and reporting qualities14; these criteria were also applicable for assessing the risk of bias at study level. The checklist included (1) appropriate sampling strategy, (2) response rate >80.0%, (3) clear procedures for blood pressure measurement including use of World Health Organization’s guidelines of STEPwise approach to surveillance of noncommunicable diseases15 to develop study protocol or providing detailed information on type of blood pressure measurement device and number of readings taken to measure the outcome, (4) definition of HTN used is measured HTN at ≥140/90 mm Hg levels, and (5) at least one quality assurance method such as training of data collectors, pretesting, and supervision. High-quality studies (with a complete score of 5) were included for meta-analysis.
Operationalization of Summary Measures
Summary measures included the following: first, the prevalence of HTN; second, the prevalence of HTN awareness; third, the prevalence of HTN treatment; and fourth, factors associated with HTN and sex, expressed as a crude odds ratio (OR).
Statistical Analysis
The pooled prevalence was weighted by inverse variance method, with the use of Freeman-Tukey double arcsine transformation to stabilize the proportions calculated for each study. The pooled OR for the association between HTN and reported risk factors was calculated using Mantel-Haenszel method. Due to the expected heterogeneity among studies, DerSimonian-Laird random-effects model was used to compute the effect estimates; however, the forest plots included results of the fixed-effect model as well. Assessment of heterogeneity comprised calculating τ2 statistic and I2 statistic. Tau-squared statistic provides an estimate of the between-study variance, in which a value of >1.0 suggests the presence of substantial statistical heterogeneity. I-squared statistic provides an estimate of the percentage of the variability in effect estimate that is due to heterogeneity rather than sampling error or chance differences where values of 25.0%, 50.0%, and 75.0% are interpreted as low, medium, and high heterogeneity, respectively.
The potential modifying effects of 7 study-level variables on the pooled prevalence of HTN were assessed using univariate mixed-effects meta-regression analyses and subgroup analysis. The included variables were data collection year, study publication year, use of STEPS protocols, type of used measurement device, proportion of women, youngest age group targeted, sample’s mean age, and residence settings. For subgroup differences, Cochran’s Q test (χ2) was performed, where significant P < .10 suggests evidence of heterogeneity.
Sensitivity analyses were performed by removing studies with the smallest sample sizes and outlier results. Finally, publication bias to assess the risk of bias across studies was conducted by evaluating funnel plot asymmetry using Egger’s linear regression test and Begg’s rank correlation test, as significant P value suggests the presence of statistical publication bias.
The results reported the pooled estimates with their 95% confidence interval (CI). CI for pooled prevalence was calculated using an “exact” binomial interval (ie, Clopper-Pearson interval). Significance was set at P < .05. The analysis was conducted using “meta” and “metafor” packages of R software.16,17
Results
Study Selection
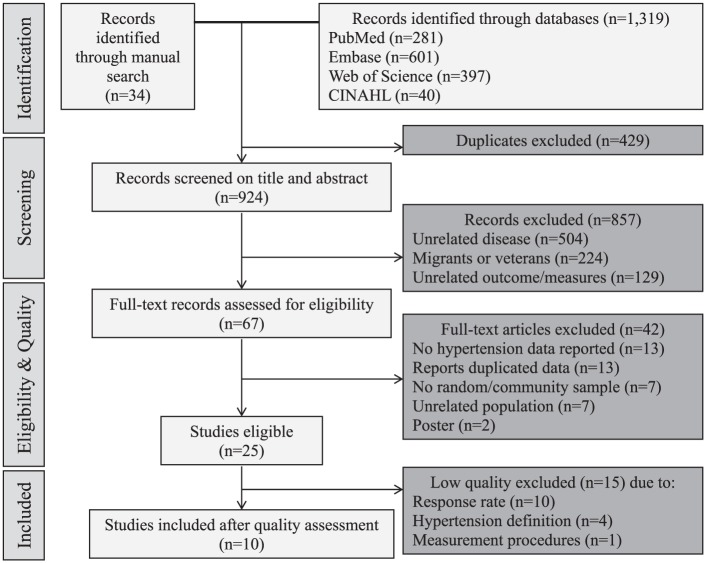
There were 1319 records identified from the database search and 34 from the manual search (Figure 1). Of these, 429 were duplicates, and 857 were excluded based on “title and abstract” screening. After full-text assessment of the remaining 67 articles, 25 studies were found to be eligible.18-42
Figure 1.
Flow chart of records retrieved, screened and included in the systematic review and meta-analysis
Quality Assessment
Of the 25 eligible studies, 15 studies (60.0%) did not meet all 5 quality criteria.18,19,21,23,26,29,34-42 Excluded studies comprise 70.9% of overall participants because 2 national surveys had low response rate.18,19 Ten studies, with a population of 44 941 subjects, were included in this meta-analysis.20,20,22,24,25,27,28,30-33 Detailed tables on the quality assessment are available in Appendix 2.
Study Characteristics
An overview of the included articles is available in Table 1. All studies are population-based observational cross-sectional design. Seven studies focused on HTN as a primary outcome,20,20,27,28,30-33 while the rest focused on other related diseases or risk factors and had HTN as a secondary outcome. There were 3 national studies that comprised 66.6% of total subjects27,31,32; the rest were conducted in 4 regions: North East (n = 2; 13.6% of total subjects), Red River Delta (n = 2; 8.9% of total subjects), North Central and Central Coastal Areas (n = 2; 5.8% of total subjects), and South East (n = 1; 5.0% of total subjects). Three studies had an equal proportion of females and males in their samples, while the rest had higher proportions for females. Three studies reported age categories only; the mean age reported from 10 studies was 48.1 ± 4.6. For further analysis regarding residence settings, the studies were classified using the following criteria: rural settings if they covered >75.0% rural residents (n = 5); urban settings if they covered ≤30.0% rural residents (n = 2); and mixed rural/urban settings (n = 3) where the proportion of rural residents ranged between 50.8% and 65.9%. Results of meta-analysis are shown in Table 2.
Table 1.
Study Characteristics.
| # | First Author, Year (Project) | Data Collection Year | Study Focus | Province, Region | Population | Sampling Technique | Use of STEPS Protocols | Sample Size, n | Response Rate, % | Women, % | Mean Age, n | Rural Residents, % | Residence Setting |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Minh, 2006 (FilaBavi HDSS) | 2002 | Hypertension | Hanoi, Red River Delta | 25-64 years | Random selection from database | Yes | 1996 | 99.8 | 50.0 | NR | 100.0 | Rural |
| 2 | Hoang, 2007 (FilaBavi HDSS) | 2005 | Risk factors of chronic diseases | Hanoi, Red River Delta | 25-64 years | Random selection from database | Yes | 1984 | 99.2 | 50.3 | NR | 100.0 | Rural |
| 3 | Ta, 2010 | NR | Type 2 diabetes mellitus | HCMC, South East | 30-70 years | Random sample, with PPS | NR | 2330 | 90.0 | 69.1 | 50.0 | 0.0 | Urban |
| 4 | Fitzpatrick, 2012 | 2010 | Risk factors and symptoms of stroke | Da Nang, North Central, and Central Coastal Areas | ≥35 years | Multistage clustered sampling | Yes | 1621 | 94.5 | 56.1 | 52.0 | 30.4 | Urban |
| 5 | Son, 2012 (NESH, STEPS survey) | 2002-2008 | Hypertension | National, 8 provinces | ≥25 years | Multistage stratified samplinga | Yes | 9823 | 93.0 | 60.8 | 42.7 | 50.8 | Mixed |
| 6 | Ha, 2013 | 2011 | Hypertension | Thai Nguyen, North East | ≥25 years | Multistage stratified clustered, with PPSa | NR | 2348 | 81.5 | 56.3 | 45.0 | 82.8 | Rural |
| 7 | Nguyen, 2014 | 2012 | Hypertension | Thai Nguyen, North East | 35-64 years | Random sample in 4 communes | NR | 3779 | 86.5 | 56.7 | 47.4 | 100.0 | Rural |
| 8 | Do, 2015 (NAOS) | 2005 | Hypertension | National, 8 provinces | 25-64 years | Multistage stratified clustered, with PPSa,b,c | Yes | 17 199 | 97.0 | 50.7 | 44.2 | 76.4 | Rural |
| 9 | Ministry of Health, 2016 | 2015 | Hypertension | National, 63 provinces | 18-69 years | Multistage stratified clustered, with PPSb,c | Yes | 2590 | 79.8 | 57.0 | NR | 55.2 | Mixed |
| 10 | Hien, 2018 | 2015 | Hypertension | Thua Thien Hue, North Central, and Central Coastal Areas | 40-64 years | Multistage clustered sampling | Yes | 969 | 80.8 | 56.1 | 55.5 | 65.9 | Mixed |
Abbreviations: STEPS, STEPwise approach to surveillance of noncommunicable diseases; FilaBavi HDSS, Health and Demographic Surveillance System at Ba Vi District, part of INDEPTH Network; NR, not reported; PPS, probability proportional to size; NESH, National Epidemiological Survey on Hypertension and Its Risk Factors; NAOS, National Adult Overweight Survey.
Stratified by geographical regions.
Stratified by age and sex strata.
Stratified by urban/rural settings.
Residence settings that are either totally rural or urban are indicated in bold.
Table 2.
Results of Meta-Analysis (Forest Plots Are Available in Appendices).
| Prevalence of Measured Hypertension |
Prevalence of Hypertension Awareness |
Prevalence of Hypertension Treatment |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| k | Pooled | 95% CI | τ2 | I 2 | P * | k | Pooled | 95% CI | τ2 | I 2 | P * | k | Pooled | 95% CI | τ2 | I 2 | P * | ||||
| Studies included in meta-analysis | 10 | 21.1 | 18.5 | 23.7 | 0.0026 | 97.6 | 6 | 9.3 | 5.3 | 14.3 | 0.0094 | 99.4 | 7 | 4.7 | 2.6 | 7.3 | 0.0056 | 99.0 | |||
| Studies with national samples | 3 | 18.4 | 15.2 | 21.8 | 0.0014 | 97.9 | 2 | 8.4 | 3.0 | 16.3 | 0.0075 | 99.7 | 3 | 4.8 | 1.9 | 9.0 | 0.0052 | 99.4 | |||
| Subgroup analyses | |||||||||||||||||||||
| Sex | |||||||||||||||||||||
| Men | 9 | 26.4 | 23.1 | 29.9 | 0.0033 | 95.9 | <.01 | 5 | 10.3 | 5.8 | 15.9 | 0.0088 | 98.7 | .73 | 5 | 5.1 | 2.7 | 8.2 | 0.0050 | 97.8 | .95 |
| Women | 9 | 16.6 | 13.4 | 20.0 | 0.0044 | 97.6 | 5 | 8.9 | 3.9 | 15.7 | 0.0138 | 99.3 | 5 | 5.0 | 2.0 | 9.1 | 0.0085 | 98.9 | |||
| Mean age category | |||||||||||||||||||||
| <45 years | 2 | 20.0 | 16.4 | 23.9 | 0.0011 | 98.2 | <.01 | 2 | 8.4 | 3.0 | 16.3 | 0.0075 | 99.7 | <.01 | 2 | 4.7 | 1.1 | 10.6 | 0.0068 | 99.7 | <.01 |
| 45-48 years | 2 | 20.4 | 19.4 | 21.4 | 0 | 0.0 | 1 | 7.4 | 6.4 | 8.5 | — | — | 1 | 3.1 | 2.4 | 3.8 | — | — | |||
| 50-56 years | 3 | 28.3 | 27.1 | 29.6 | <0.0001 | 0.9 | 1 | 30.1 | 27.3 | 33.1 | — | — | 1 | 14.9 | 12.7 | 17.2 | — | — | |||
| NR | 3 | 15.6 | 12.7 | 18.7 | 0.0013 | 91.9 | 2 | 4.3 | 1.1 | 9.4 | 0.0053 | 97.7 | 3 | 3.0 | 0.9 | 6.2 | 0.0047 | 97.7 | |||
| Residence setting | |||||||||||||||||||||
| Mixed rural/urban | 3 | 21.9 | 15.7 | 28.9 | 0.0049 | 98.3 | <.01 | 2 | 20.4 | 6.0 | 40.4 | 0.0252 | 99.4 | .04 | 3 | 8.7 | 5.3 | 12.7 | 0.0033 | 97.5 | <.01 |
| Rural | 5 | 18.1 | 16.1 | 20.3 | 0.0009 | 93.1 | 4 | 5.3 | 3.6 | 7.2 | 0.0016 | 95.6 | 4 | 2.4 | 1.5 | 3.6 | 0.0010 | 93.4 | |||
| Urban | 2 | 27.9 | 26.6 | 29.4 | 0 | 0.0 | 0 | — | —- | — | — | — | 0 | — | — | — | — | — | |||
Abbreviations: k, number of studies included in the meta-analysis of the pooled estimate; CI, confidence interval; τ2, a statistic provides an estimate of the between-study variance, in which a value of >1.0 suggests the presence of substantial statistical heterogeneity; I2, a statistic provides an estimate of the percentage of the variability in effect estimate that is due to heterogeneity rather than sampling error or chance differences where values of 25.0%, 50.0%, and 75.0% are interpreted as low, medium, and high heterogeneity, respectively; NR, not reported.
Test for subgroup differences, that is, Cochran’s Q test (χ2) where significant P < .10 suggests evidence of heterogeneity.
Significant p values are indicated in bold.
Measured Hypertension
Forest plots are available in Appendix 3. The pooled prevalence of measured HTN for the 10 studies is 21.1% (95% CI = 18.5-23.7; τ2 = 0.0026; I2 = 98%). The pooled prevalence of measured HTN for the 3 national studies is 18.4% (95% CI = 15.2-21.8; τ2 = 0.0014; I2 = 98%).
The results of the univariate meta-regression analyses showed that 3 factors significantly influenced the HTN prevalence and explained proportions of total between-study variance (ie, R2 statistic); these were proportions of women (QM = 7.8, degrees of freedom [df] = 1, P < .01, R2 = 31.8%), mean age (QM = 38.3, df = 3, P < .001, R2 = 67.1%), and residence setting (QM = 10.2, df = 2, P < .01, R2 = 29.5%).
Nine studies reported on the number of hypertensive subjects disaggregated by sex. The pooled prevalence of HTN among men is 26.4% (95% CI = 23.1-29.9; τ2 = 0.0033; I2 = 96%), which is higher than the overall prevalence. However, the pooled prevalence of HTN among women was lower, equaling 16.6% (95% CI = 13.4-20.0; τ2 = 0.0044; I2 = 98%).
The pooled prevalence of HTN among studies with a mean age ranging between 50 and 56 years is higher than the overall prevalence, equaling 28.3% (95% CI = 27.1-29.6; τ2 < 0.0001; I2 = 1%). With regard to residence settings, higher prevalence of HTN was found among studies undertaken in urban settings (27.9; 95% CI = 26.6-29.4; I2 = 0%) compared with mixed rural/urban settings (21.9%; 95% CI = 15.7-28.9; I2 = 98%) then rural settings (18.1%; 95% CI = 16.1-20.3; I2 = 93%).
Awareness of Hypertension
Forest plots are available in Appendix 4. Only 6 studies reported on the proportion of those aware of their HTN condition. The pooled prevalence of HTN awareness was 9.3% (95% CI = 5.3-14.3; τ2 = 0.0094; I2 = 99%).
Awareness was significantly associated with age and residence. A significant higher proportion of HTN awareness was reported among studies with oldest age group and those conducted in mixed rural/urban settings (49.0%; 95% CI = 43.6-54.4; τ2 = 0.002; I2 = 89%) compared with rural settings (27.5%; 95% CI = 21.7-33.6; τ2 = 0.0041; I2 = 92%).
Treatment of Hypertension
Forest plots are available in Appendix 5. Only 7 studies reported on the proportion of those treated for their HTN condition. The pooled prevalence of HTN treatment was 4.7% (95% CI = 2.6-7.3; τ2 = 0.0056; I2 = 99%). Similar to prevalence of HTN awareness, a significant higher proportion of HTN treatment was reported among studies with oldest age group and those conducted in mixed rural/urban settings (8.7%; 95% CI = 5.3-12.7; τ2 = 0.0033; I2 = 98%) compared with rural settings (2.4%; 95% CI = 1.5-3.6; τ2 = 0.0010; I2 = 93%).
Factors Associated With the Pooled Prevalence and Sex
Data are available in Appendix 6. Men has substantially higher odds than women for measured HTN (OR = 1.8; 95% CI = 1.6-2.1), HTN awareness (OR = 1.8; 95% CI = 1.5-2.1), and HTN treatment (OR = 1.8; 95% CI = 1.6-2.1). When stratified by categories for mean age and residence settings, only 2 subgroup analyses are significant. The association between male sex and measured HTN was higher for one study with mean age category 45 to 48 years (OR = 2.3; 95% CI = 2.0-2.7; τ2 = 0.0205; I2 = 76%), while the association between male sex and HTN awareness was higher for studies conducted in rural settings (OR = 1.9; 95% CI = 1.8-2.1; τ2 = 0.00216; I2 = 80%) compared with mixed rural/urban settings (OR = 1.5; 95% CI = 1.3-1.7).
Heterogeneity, Sensitivity Analyses, and Publication Bias
The included studies in the analyses of the pooled estimates showed a high heterogeneity. As a result of the regression analyses, the heterogeneity decreased when stratifying by sex, mean age category, and residence settings. To further identify specific sources of heterogeneity, more analysis for the prevalence of HTN excluded studies based on their smaller sample size or outlier results. The pooled prevalence calculated after the removal of 5 studies remained within ±10% of the original estimate. No evidence of publication bias was found based on the funnel plot asymmetry tests for all 3 summary measures (funnel plots are available in Appendix 7).
Discussion
To the best of our knowledge, this is the most comprehensive systematic review and meta-analysis on HTN prevalence in Vietnam. The pooled estimate for the prevalence of measured HTN in Vietnam, based on 10 studies published between 2005 and 2018, is 21.1%. However, the pooled estimate for the 3 studies with national surveys was lower (18.4%). These national samples can be more representative and reliable since they cover 66.6% of the total surveyed population included in this meta-analysis. A meta-analysis on the prevalence of HTN in LMICs (2001-2015) found an overall prevalence of 32.3% (29.4-35.3) and 35.5% (32.2-39.4) in East Asia and Pacific, respectively, based on 33 articles from China (n = 22), Vietnam (n = 5, all included in our analysis), Malaysia (n = 4), Thailand (n = 1), and Federated States of Micronesia (n = 1).5 Another meta-analysis for the prevalence of HTN in Chinese cities (2002-2010) had an estimate of 21.5% (19.4% to 23.6%).43 Our estimate for the prevalence of HTN in Vietnam appears to be lower than estimates reported in other countries of East Asia and Pacific. One explanation may be the observed differences in conducting surveys and measurement procedures, which have either changed over time or have not followed one specific guideline. Additionally, while most studies used digital measurement devices, only 2 with one of the national studies have used mercury sphygmomanometer. However, the pooled prevalence was not significantly associated with the use of digital or mercury measurement device.
Residence settings have significantly influenced the pooled prevalence of measured HTN and HTN awareness and treatment. There was a higher prevalence of measured HTN in urban and mixed rural/urban compared with separate rural settings; this is similar to findings from the meta-analysis of LMICs5 and the time trends analysis of Vietnam.10 Furthermore, the proportion of hypertensive subjects who are aware of their condition was significantly higher among mixed rural/urban compared with rural settings. The time trends analysis found an increased prevalence of HTN awareness in both rural and urban areas between 2001 and 2009; however, the change in HTN awareness in urban areas and HTN control in rural areas had slower progress.10 Our results regarding the lower awareness of HTN in rural settings may reflect a limited detection of HTN in the rural areas of the country compared with urban areas.
As expected, the odds of measured HTN among men was higher than the odds of HTN among women. This sex difference was also affected by residence settings with higher odds of HTN among men living in rural settings, while the overall prevalence for both sexes is higher in urban settings. This is an unusual pattern that was also reported in the individual studies. Further research may focus on explaining this sex difference in the prevalence of HTN in Vietnam.
The quality assessment has excluded 2 national surveys18,19 due to a low response rate. The data collection date for these 2 surveys was 2002 and 2009-2010, respectively. In addition, both studies had good sample sizes (n = 77 758 and n = 14 706, respectively). The 2 studies reported a lower overall prevalence of HTN; however, both studies showed a higher prevalence among men compared with women. Furthermore, the latest study19 explored regional differences in the prevalence of HTN with the highest prevalence in West Highland (Dak Lak province) and Mekong River Delta (Can Tho province) and the lowest prevalence in Red River Delta (Ha Noi) and North Central (Hue). Our analysis could not look at regional differences because half the included studies are from 2 regions and the national ones did not report their data by region.
Strengths and Limitations
We reported results from only high-quality studies, and there was no evidence of publication bias. We also reported results for both random and fixed models, which showed similar results in pooled estimates; however, they differed in the 95% CIs. Heterogeneity among studies was high; its causes include differences in sample characteristics and standardization of blood pressure measurement procedures including devices and number of readings. Although we tried to lower the heterogeneity by conducting meta-regression and subgroup analysis, we were limited to the factors that could be included, especially with only 7 studies with a primary focus on HTN. For example, the age range was different in included studies; when stratifying by age groups, we had a smaller number of studies. Few studies reported on the awareness, treatment, and control of HTN. There was enough number of studies to perform an analysis on HTN awareness and treatment; a smaller number of studies reported estimates for control of HTN. The studies covered different parts of the country for both rural and urban populations. However, representation is questionable since some regions were only covered by the national surveys, with no individual studies conducted there.
Conclusion
Hypertension is a significant public health problem in Vietnam. Almost 1 in 5 people may have HTN. Awareness and treatment were much lower in rural areas. There is a need to strengthen primary and secondary prevention measures in addition to management activities to reduce morbidity and mortality of HTN, especially in rural areas.
Supplemental Material
Supplemental material, Appendix_1_Search_Strategy for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental Material
Supplemental material, Appendix_2_Quality_Assessment_Final for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental Material
Supplemental material, Appendix_3_Forest_Plot_Measured_HTN for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental Material
Supplemental material, Appendix_4_Forest_Plot_HTN_Awareness for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental Material
Supplemental material, Appendix_5_Forest_Plot_HTN_Treatment for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental Material
Supplemental material, Appendix_6_OR_HTN_Sex for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental Material
Supplemental material, Appendix_7_Funnel_Plots for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Acknowledgments
The authors would like to thank Ralph de Vries, Vrije Universiteit Library, for his assistance and guidance in refining the search strategy and modifying it to fit the parameters of the various databases. The authors would also like to thank Onaedo Ilozumba and Mealnie Bannister-Tyrrell for their comments on an earlier version of this article.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Erasmus Mundus Joint Doctorate Fellowship, Specific Grant Agreement 2014-0681, which Lana Meiqari is a beneficiary of, supported this review. The funding agency had no role in study design, analysis, or preparation of the article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD: Lana Meiqari  https://orcid.org/0000-0001-9348-4830
https://orcid.org/0000-0001-9348-4830
References
- 1. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151-1210. doi: 10.1016/S0140-6736(17)32152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1345-1422. doi: 10.1016/S0140-6736(17)32366-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1260-1344. doi: 10.1016/S0140-6736(17)32130-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211-1259. doi: 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sarki AM, Nduka CU, Stranges S, Kandala NB, Uthman OA. Prevalence of hypertension in low- and middle-income countries: a systematic review and meta-analysis. Medicine (Baltimore). 2015;94:e1959. doi: 10.1097/MD.0000000000001959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis. Geneva, Switzerland: World Health Organization; 2013. http://www.who.int/cardiovascular_diseases/publications/global_brief_hypertension/en/. [Google Scholar]
- 7. World Health Organization. Prevention of Cardiovascular Disease. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 8. World Health Organization. Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings. Geneva, Switzerland: World Health Organization; 2010. http://www.who.int/nmh/publications/essential_ncd_interventions_lr_settings.pdf. [Google Scholar]
- 9. Vietnam Ministry of Health; Health Partnership Group. Joint Annual Health Review 2014: Strengthening Prevention and Control of Non-Communicable Diseases. Hanoi, Vietnam: Vietnam Ministry of Health; Health Partnership Group; 2014. [Google Scholar]
- 10. Nguyen QN, Pham ST, Nguyen VL, et al. Time trends in blood pressure, body mass index and smoking in the Vietnamese Population: a meta-analysis from multiple cross-sectional surveys. PLoS One. 2012;7:e42825. doi: 10.1371/journal.pone.0042825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bown MJ, Sutton AJ. Quality control in systematic reviews and meta-analyses. Eur J Vasc Endovasc Surg. 2010;40:669-677. doi: 10.1016/j.ejvs.2010.07.011 [DOI] [PubMed] [Google Scholar]
- 14. Dreier M. Quality assessment in meta-analysis. In: Doi SAR, Williams GM, eds. Methods of Clinical Epidemiology. Springer Series on Epidemiology and Public Health. Berlin, Germany: Springer; 2013:213-228. [Google Scholar]
- 15. World Health Organization. WHO STEPS Surveillance Manual: The WHO STEPwise Approach to Chronic Disease Risk Factor Surveillance. Geneva, Switzerland: World Health Organization; 2017. http://www.who.int/ncds/surveillance/steps/manual/en/. [Google Scholar]
- 16. Schwarzer G. meta: an R package for meta-analysis. R News. 2007;7:40-45. [Google Scholar]
- 17. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1-48. doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 18. Nguyen TT, Adair LS, Suchindran CM, He K, Popkin BM. The association between body mass index and hypertension is different between East and Southeast Asians. Am J Clin Nutr. 2009;89:1905-1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bui TV, Blizzard CL, Luong KN, et al. National survey of risk factors for non-communicable disease in Vietnam: prevalence estimates and an assessment of their validity. BMC Public Health. 2016;16:498. doi: 10.1186/s12889-016-3160-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Minh HV, Byass P, Chuc NT, Wall S. Gender differences in prevalence and socioeconomic determinants of hypertension: findings from the WHO STEPs survey in a rural community of Vietnam. J Hum Hypertens. 2006;20:109-115. doi: 10.1038/sj.jhh.1001942 [DOI] [PubMed] [Google Scholar]
- 21. Cuong TQ, Dibley MJ, Bowe S, Hanh TTM, Loan TTH. Obesity in adults: an emerging problem in urban areas of Ho Chi Minh City, Vietnam. Eur J Clin Nutr. 2007;61:673-681. doi: 10.1038/sj.ejcn.1602563 [DOI] [PubMed] [Google Scholar]
- 22. Hoang VM, Byass P, Dao LH, Nguyen TK, Wall S. Risk factors for chronic disease among rural Vietnamese adults and the association of these factors with sociodemographic variables: findings from the WHO STEPS survey in rural Vietnam, 2005. Prev Chronic Dis. 2007;4:A22. [PMC free article] [PubMed] [Google Scholar]
- 23. Trinh OT, Nguyen ND, Phongsavan P, Dibley MJ, Bauman AE. Prevalence and risk factors with overweight and obesity among Vietnamese adults: Caucasian and Asian cut-offs. Asia Pac J Clin Nutr. 2009;18:226-233. [PubMed] [Google Scholar]
- 24. Ta MT, Nguyen KT, Nguyen ND, Campbell LV, Nguyen TV. Identification of undiagnosed type 2 diabetes by systolic blood pressure and waist-to-hip ratio. Diabetologia. 2010;53:2139-2146. doi: 10.1007/s00125-010-1841-6 [DOI] [PubMed] [Google Scholar]
- 25. Fitzpatrick AL, Ngo QV, Ly KA, et al. Symptoms and risk factors for stroke in a community-based observational sample in Viet Nam. J Epidemiol Glob Health. 2012;2:155-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nguyen QN, Pham ST, Do LD, et al. Cardiovascular disease risk factor patterns and their implications for intervention strategies in Vietnam. Int J Hypertens. 2012;2012:560397. doi: 10.1155/2012/560397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Son PT, Quang NN, Viet NL, et al. Prevalence, awareness, treatment and control of hypertension in Vietnam-results from a national survey. J Hum Hypertens. 2012;26:268-280. doi: 10.1038/jhh.2011.18 [DOI] [PubMed] [Google Scholar]
- 28. Ha DA, Goldberg RJ, Allison JJ, Chu H, Nguyen HL. Prevalence, awareness, treatment, and control of high blood pressure: a population-based survey in Thai Nguyen, Vietnam. PLoS One. 2013;8:e66792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Binh TQ, Phuong PT, Nhung BT, Tung do D. Metabolic syndrome among a middle-aged population in the Red River Delta region of Vietnam. BMC Endocr Disord. 2014;14:77. doi: 10.1186/1472-6823-14-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nguyen TPL, Schuiling-Veninga CCM, Nguyen TBY, Hang VTT, Wright EP, Postma MJ. Models to predict the burden of cardiovascular disease risk in a rural mountainous region of Vietnam. Value Health Reg Issues. 2014;3:87-93. [DOI] [PubMed] [Google Scholar]
- 31. Do HT, Geleijnse JM, Le MB, Kok FJ, Feskens EJ. National prevalence and associated risk factors of hypertension and prehypertension among Vietnamese adults. Am J Hypertens. 2015;28:89-97. doi: 10.1093/ajh/hpu092 [DOI] [PubMed] [Google Scholar]
- 32. Ministry of Health. National Survey on the Risk Factors of Non-Communicable Diseases (STEPS) Viet Nam, 2015. Hanoi, Vietnam: Ministry of Health; 2016. [Google Scholar]
- 33. Hien HA, Tam NM, Tam V, Derese AJ, Devroey D. Prevalence, awareness, treatment, and control of hypertension and its risk factors in (Central) Vietnam. Int J Hypertens. 2018;2018:6326984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hanh TTM, Komatsu T, Hung NT, et al. Nutritional status of middle-aged Vietnamese in Ho Chi Minh City. J Am Coll Nutr. 2001;20:616-622. [DOI] [PubMed] [Google Scholar]
- 35. Hanh TTM, Komatsu T, Hung NTK, et al. Blood pressure, serum cholesterol concentration and their related factors in urban and rural elderly of Ho Chi Minh City. J Nutr Sci Vitaminol (Tokyo). 2001;47:147-155. [DOI] [PubMed] [Google Scholar]
- 36. Son LND, Kusama K, Hung NT, et al. Prevalence and risk factors for diabetes in Ho Chi Minh City, Vietnam. Diabet Med. 2004;21:371-376. doi: 10.1111/j.1464-5491.2004.01159.x [DOI] [PubMed] [Google Scholar]
- 37. Tesfaye F, Nawi NG, Van Minh H, et al. Association between body mass index and blood pressure across three populations in Africa and Asia. J Hum Hypertens. 2007;21:28-37. doi: 10.1038/sj.jhh.1002104 [DOI] [PubMed] [Google Scholar]
- 38. Van Minh H, Soonthornthada K, Ng N, et al. Blood pressure in adult rural INDEPTH population in Asia. Glob Health Action. 2009;2:60-67. doi: 10.3402/gha.v2i0.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pham LH, Au TB, Blizzard L, et al. Prevalence of risk factors for non-communicable diseases in the Mekong Delta, Vietnam: results from a STEPS survey. BMC Public Health. 2009;9:291. doi: 10.1186/1471-2458-9-291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Do HTP, Santos JA, Trieu K, et al. Effectiveness of a Communication for Behavioral Impact (COMBI) intervention to reduce salt intake in a Vietnamese Province based on estimations from spot urine samples. J Clin Hypertens (Greenwich). 2016;18:1135-1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Miyakawa M, Shimizu T, Van Dat N, et al. Prevalence, perception and factors associated with diabetes mellitus among the adult population in central Vietnam: a population-based, cross-sectional seroepidemiological survey. BMC Public Health. 2017;17:298. doi: 10.1186/s12889-017-4208-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bui Van N, Pham Van Q, Vo Hoang L, et al. Prevalence and risk factors of hypertension in two communes in the Vietnam Northern Mountainous, 2017. Biomed Res Int. 2018;2018:7814195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ma YQ, Mei WH, Yin P, Yang XH, Rastegar SK, Yan JD. Prevalence of hypertension in Chinese cities: a meta-analysis of published studies. PLoS One. 2013;8:e58302. doi: 10.1371/journal.pone.0058302 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendix_1_Search_Strategy for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental material, Appendix_2_Quality_Assessment_Final for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental material, Appendix_3_Forest_Plot_Measured_HTN for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental material, Appendix_4_Forest_Plot_HTN_Awareness for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental material, Appendix_5_Forest_Plot_HTN_Treatment for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental material, Appendix_6_OR_HTN_Sex for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health
Supplemental material, Appendix_7_Funnel_Plots for Prevalence of Hypertension in Vietnam: A Systematic Review and Meta-Analysis by Lana Meiqari, Dirk Essink, Pamela Wright and Fedde Scheele in Asia Pacific Journal of Public Health