Abstract
Background
Exercise training is commonly recommended for individuals with fibromyalgia. This review is one of a series of reviews about exercise training for people with fibromyalgia that will replace the "Exercise for treating fibromyalgia syndrome" review first published in 2002.
Objectives
• To evaluate the benefits and harms of aerobic exercise training for adults with fibromyalgia
• To assess the following specific comparisons ० Aerobic versus control conditions (eg, treatment as usual, wait list control, physical activity as usual) ० Aerobic versus aerobic interventions (eg, running vs brisk walking) ० Aerobic versus non‐exercise interventions (eg, medications, education) We did not assess specific comparisons involving aerobic exercise versus other exercise interventions (eg, resistance exercise, aquatic exercise, flexibility exercise, mixed exercise). Other systematic reviews have examined or will examine these comparisons (Bidonde 2014; Busch 2013).
Search methods
We searched the Cochrane Library, MEDLINE, Embase, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Physiotherapy Evidence Database (PEDro), Thesis and Dissertation Abstracts, the Allied and Complementary Medicine Database (AMED), the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP), and the ClinicalTrials.gov registry up to June 2016, unrestricted by language, and we reviewed the reference lists of retrieved trials to identify potentially relevant trials.
Selection criteria
We included randomized controlled trials (RCTs) in adults with a diagnosis of fibromyalgia that compared aerobic training interventions (dynamic physical activity that increases breathing and heart rate to submaximal levels for a prolonged period) versus no exercise or another intervention. Major outcomes were health‐related quality of life (HRQL), pain intensity, stiffness, fatigue, physical function, withdrawals, and adverse events.
Data collection and analysis
Two review authors independently selected trials for inclusion, extracted data, performed a risk of bias assessment, and assessed the quality of the body of evidence for major outcomes using the GRADE approach. We used a 15% threshold for calculation of clinically relevant differences between groups.
Main results
We included 13 RCTs (839 people). Studies were at risk of selection, performance, and detection bias (owing to lack of blinding for self‐reported outcomes) and had low risk of attrition and reporting bias. We prioritized the findings when aerobic exercise was compared with no exercise control and present them fully here.
Eight trials (with 456 participants) provided low‐quality evidence for pain intensity, fatigue, stiffness, and physical function; and moderate‐quality evidence for withdrawals and HRQL at completion of the intervention (6 to 24 weeks). With the exception of withdrawals and adverse events, major outcome measures were self‐reported and were expressed on a 0 to 100 scale (lower values are best, negative mean differences (MDs)/standardized mean differences (SMDs) indicate improvement). Effects for aerobic exercise versus control were as follows: HRQL: mean 56.08; five studies; N = 372; MD ‐7.89, 95% CI ‐13.23 to ‐2.55; absolute improvement of 8% (3% to 13%) and relative improvement of 15% (5% to 24%); pain intensity: mean 65.31; six studies; N = 351; MD ‐11.06, 95% CI ‐18.34 to ‐3.77; absolute improvement of 11% (95% CI 4% to 18%) and relative improvement of 18% (7% to 30%); stiffness: mean 69; one study; N = 143; MD ‐7.96, 95% CI ‐14.95 to ‐0.97; absolute difference in improvement of 8% (1% to 15%) and relative change in improvement of 11.4% (21.4% to 1.4%); physical function: mean 38.32; three studies; N = 246; MD ‐10.16, 95% CI ‐15.39 to ‐4.94; absolute change in improvement of 10% (15% to 5%) and relative change in improvement of 21.9% (33% to 11%); and fatigue: mean 68; three studies; N = 286; MD ‐6.48, 95% CI ‐14.33 to 1.38; absolute change in improvement of 6% (12% improvement to 0.3% worse) and relative change in improvement of 8% (16% improvement to 0.4% worse). Pooled analysis resulted in a risk ratio (RR) of moderate quality for withdrawals (17 per 100 and 20 per 100 in control and intervention groups, respectively; eight studies; N = 456; RR 1.25, 95%CI 0.89 to 1.77; absolute change of 5% more withdrawals with exercise (3% fewer to 12% more).
Three trials provided low‐quality evidence on long‐term effects (24 to 208 weeks post intervention) and reported that benefits for pain and function persisted but did not for HRQL or fatigue. Withdrawals were similar, and investigators did not assess stiffness and adverse events.
We are uncertain about the effects of one aerobic intervention versus another, as the evidence was of low to very low quality and was derived from single trials only, precluding meta‐analyses. Similarly, we are uncertain of the effects of aerobic exercise over active controls (ie, education, three studies; stress management training, one study; medication, one study) owing to evidence of low to very low quality provided by single trials. Most studies did not measure adverse events; thus we are uncertain about the risk of adverse events associated with aerobic exercise.
Authors' conclusions
When compared with control, moderate‐quality evidence indicates that aerobic exercise probably improves HRQL and all‐cause withdrawal, and low‐quality evidence suggests that aerobic exercise may slightly decrease pain intensity, may slightly improve physical function, and may lead to little difference in fatigue and stiffness. Three of the reported outcomes reached clinical significance (HRQL, physical function, and pain). Long‐term effects of aerobic exercise may include little or no difference in pain, physical function, and all‐cause withdrawal, and we are uncertain about long‐term effects on remaining outcomes. We downgraded the evidence owing to the small number of included trials and participants across trials, and because of issues related to unclear and high risks of bias (performance, selection, and detection biases). Aerobic exercise appears to be well tolerated (similar withdrawal rates across groups), although evidence on adverse events is scarce, so we are uncertain about its safety.
Plain language summary
Aerobic exercise for adults with fibromyalgia
This review summarizes the effects of aerobic exercise for adults with fibromyalgia.
What are aerobic exercises?
Aerobic exercises, such as walking and swimming, cause harder breathing and faster heart beating than occur at rest. Benefits of doing aerobic exercise include strengthening the heart and improving circulation, lowering blood pressure, and helping to control blood sugar and weight.
What problems does fibromyalgia cause?
People with fibromyalgia have chronic bodily pain and often have increased fatigue (feeling tired), stiffness, depression, and problems sleeping.
Study characteristics
We searched for studies until June 2016, and found 13 studies (839 individuals). Most studies (61.5%) included only female participants. Average age of participants was 41 years (minimum 32 to maximum 56 years). According to the inclusion/exclusion criteria, most participants were not doing exercises before starting the study.
Aerobic interventions were compared with controls (wait list, treatment as usual, daily activities as usual) over six to 24 weeks. On average, exercise sessions were provided two to three times per week for 35 minutes each session. Exercises involved walking, cycling, running, and doing low‐impact aerobics and aquacise. Participants exercised at different intensities, starting light and increasing as the study progressed. All programs were supervised.
Key results at the end of treatment
The findings of aerobic exercise compared with no exercise control were prioritised and are presented fully here. Moderate‐quality evidence revealed that aerobic exercise improved HRQL, and low‐quality evidence showed improvement in physical function and decreased pain, fatigue, and stiffness compared with control. Similar numbers of people dropped out of the aerobic interventions group and the comparison group. Minor adverse events were reported, but reporting was inconsistent in these studies.
Four studies explored long‐term effects at 24 to 208 weeks after the intervention ended. They reported benefits for pain and physical function among exercisers and noted no other effects.
Best estimates of what happened in people with fibromyalgia when they did aerobic exercise compared with when they received control interventions
Each outcome below was measured on a scale from 0 to 100, on which lower scores were better.
HRQL after 12 to 24 weeks: People who exercised were 7% better (or 7 points, ranging from 3 to 13 points) and rated their HRQL as 48 points versus 56 points in the control group.
Pain after 6 to 24 weeks: People who exercised were 11% better (or 11 points, ranging from 4 to 18 points) and rated their pain as 56 points versus 65 points in the control group.
Fatigue after 14 to 24 weeks: Those who exercised were 6% better (or 6 points, ranging from 12 better to 0.3 worse) and rated their fatigue as 63 points versus 68 points in the control group.
Stiffness after 16 weeks: Those who exercised were 8% better (or 8 points, ranging from 1 to 15) and rated their stiffness as 61 points versus 69 points in the control group.
Physical function after 8 to 24 weeks: The aerobic exercise group was 10% better (or 10 points, ranging from 15 to 5) and participants rated their physical function as 37 points versus 46 points in the control group.
Other results:
Withdrawal from treatment
A total of 20 out of 100 people dropped out of the aerobic group compared with 17 out of 100 from the control group (3% more, ranging from 3% fewer to 12% more) for any reason.
Adverse events
We do not have precise information about adverse events associated with aerobic exercise. Some reports describe increased pain or fatigue, and one of the 496 participants doing aerobic exercise experienced a foot bone (metatarsal) stress fracture. This may have happened by chance.
Quality of the evidence
Evidence shows that aerobic exercise may improve HRQL, pain, stiffness, and physical function, and probably leads to similar numbers of people dropping out from each group. Aerobic exercise does not seem to improve fatigue. The quality of the evidence was considered to be low or moderate because of the small numbers of people included in the studies, some issues involving study design, and low certainty of results.
Summary of findings
Summary of findings for the main comparison. Aerobic exercise training compared with control for fibromyalgia.
| Aerobic exercise training compared with control for fibromyalgia | ||||||
|
Patient or population: individuals with fibromyalgia
Settings: group and supervised
Intervention: aerobic exercise training
Comparison: control comparison (treatment as usual, wait list control, continuation of daily activities including physical activity) Outcome: measured at the end of the intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Aerobic exercise training | |||||
| Health‐related quality of life FIQ Total. Scale from 0 to 100 (0 is best) Follow‐up: 12‐24 weeksa | Mean health‐related quality of life ranged across control groups from 54 to 63.7 units | Mean health‐related quality of life in the intervention groups was 7.89 lower (13.23 to 2.55 lower) | 372 (5 studies) |
⊕⊕⊕⊝ moderateb | Absolute change 8% (3% to 13%) better Relative changec 15% (5% to 24%) better NNTB 6 (4 to 16)d |
|
|
Pain intensity
Visual analogue scale Scale from 0 to 100 mm (0 is best) Follow‐up: 6‐24 weekse |
Mean pain intensity ranged across control groups from 56 to 80.5 mm | Mean pain intensity in the intervention groups was 11.06 lower (18.34 to 3.77 lower) | 351 (6 studies) | ⊕⊕⊝⊝ lowb,f | Absolute change 11% (4% to 18%) better Relative changec 18% (7% to 30%) better NNTB 4 (2 to 15)d |
|
|
Fatigue
Visual analogue scale Scale from 0 to 100 mm (0 is best) Follow‐up: 14‐24 weeksg |
Mean fatigue ranged across control groups from 62.3 to 72 mm | Mean fatigue in the intervention groups was 6.06 lower (‐12.41 lower to 0.30 higher) |
246 (3 studies) | ⊕⊕⊝⊝ lowb,h | Absolute difference 6% improvement (12% improvement to 0.3% worse) Relative changec 8% improvement (16% improved to 0.4% worse) NNTB n/a |
|
|
Stiffness
FIQ Scale from 0 to 100 mm (lower scores mean less stiffness) Follow‐up: 16 weeks |
Mean stiffness in control groups was 69 mm | Mean stiffness in the intervention groups was 7.96 lower (14.95 to 0.97 lower) | 143 (1 study) | ⊕⊕⊝⊝ lowb,i | Absolute difference 8% (1% to 15%) improvement Relative changec 11% improvement (1% to 21% improved) NNTB 6 (3 to 218)d |
|
| Physical function FIQ and SF‐36 converted, 0 to 100 scale (0 is best) Follow‐up: 8‐24 weeksj | Mean physical function ranged across control groups from 6 to 22 units | Mean physical function in the intervention groups was 10.16 lower (15.39 to 4.94 lower) |
246 (3 studies) | ⊕⊕⊝⊝ lowb,h | Absolute change 10% (95% CI 15 to 5) improvement Relative changec 21.9% (95% CI 33.2 to 10.7) improvement NNTB 5 (3 to 13)d |
|
| Withdrawals All‐cause attrition Follow‐up: 6‐24 weeks | 17 per 100 | 20 per 100 (14 to 25) |
RR 1.25 (0.89 to 1.77) |
456 (8 studies) | ⊕⊕⊕⊝ moderateb | Absolute change: 5% more withdrawals with exercise (3% fewer to 12% more) Relative change 25% more (11% fewer to 77% more) NNTH n/a |
|
Adverse events Descriptive information |
"the present study findings confirm earlier studies that have shown aerobic exercise to reduce tender point tenderness, increase work capacity without adverse side effects..." (Wigers 1996; pages 83‐84). The following statements show some minor adverse events following aerobic exercise training: "...unable to exercise after an injury" (Sanudo 2010; pages 1840), but it is unclear whether the injury was related to intervention participation: "One participant assigned to the short bout exercise withdrew after developing a metatarsal stress fracture" (Schachter 2003; page 347) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; NNTB: number needed to treat for an additional beneficial outcome; NNTH: number needed to treat for an additional harmful outcome; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
aStudy author (intervention length in weeks): King 2002 (12), Schachter 2003 and Kayo 2011 (16), Gowans 2001 (23), Sanudo 2010 (24) bDowngraded because of lack of blinding (performance and detection bias) cRelative change calculation as per Cochrane Musculoskeletal Review Group procedures: mean difference (MD)/pooled control group baseline means dNumber needed to treat for an additional beneficial outcome (NNTB): NNTB for continuous outcomes calculated using the Wells calculator (from the CMSG Editorial office; http://musculoskeletal.cochrane.org/) for statistically significant outcomes only. Mean and standard deviation (SD) for the control group at baseline taken from Schachter 2003 (health‐related quality of life 55 (1.3), pain 61 (1.97), stifness 7 (1.9), and physical function 38 (1.86) eStudy author (intervention length in weeks): Sencan 2004 (6), Wigers 1996 (14), Kayo 2011 and Schachter 2003 (16), Mengshoel 1992 (20), Sanudo 2010 (24) fDowngraded for imprecision, wide confidence intervals, issues related to selective reporting (ie, Mengshoel 1992 and/or Kayo 2011) gStudy author (intervention length in weeks): Wigers 1996 (14), Kayo 2011 and Schachter 2003 (16), Sanudo 2010 (24) hDowngraded for imprecision iOne study
jStudy author (intervention length in weeks): Wigers 1996 (14), Kayo 2011 and Schachter 2003 (16), Sanudo 2010 (24)
Background
Description of the condition
Fibromyalgia is a chronic condition characterized by widespread muscular pain and soft tissue tenderness (Mease 2005; Wolfe 2010; Schmidt‐Wilcke 2011). Fibromyalgia is often associated with other somatic complaints, disability, sleep disturbances, anxiety, cognitive dysfunction, depressive episodes, and physical deconditioning. These symptoms significantly affect quality of life and result in both physical and psychosocial disabilities with important implications for family, employment, and independence (Mease 2005). Several abnormalities in brain and neural function in patients with fibromyalgia appear to have a genetic basis (Arnold 2013; Staud 2002).
Canadian statistics reflect the self‐reported prevalence of fibromyalgia at 1.1% across all ages, with female diagnoses outnumbering male diagnoses (1.83% female to 0.33% male; McNalley 2006). Prevalence rates among European countries (France, Italy, Portugal, Spain) are estimated to range between 1.4% (France) and 3.7% (Italy), and fibromyalgia diagnoses are twice as common among females (Branco 2010). Nakamura and colleagues found the rate in Japan to be 2.1% (Nakamura 2014); this is higher than the fibromyalgia prevalence in China of about 0.05% (Zeng 2008). The American College of Rheumatology (ACR) has prepared new diagnostic criteria for fibromyalgia (Wolfe 2010; Wolfe 2011). Use of these new diagnostic criteria may change prevalence rates in North America. In Olmsted County, Minnesota, in the USA, prevalence with age‐ and sex‐adjusted criteria was estimated at 6.4% (Vincent 2013). In Germany, use of the new criteria revealed a prevalence rate of 2.1%, with a higher rate among females (2.4%) than males (1.8%; Wolfe 2013).
Fibromyalgia research reveals high levels of health care utilization and high costs associated with medical visits, drug prescriptions, and diagnostic testing (Hauser 2010; Kelley 2011). Individuals with fibromyalgia are often seen by health care professionals for concomitant medical issues (somatic comorbidity associated with fibromyalgia) and related pharmacological treatment. Several Cochrane systematic reviews and a Cochrane overview on the use of medications for treatment of fibromyalgia have yielded tier‐2 evidence of moderate pain relief with pregabalin (an antiepileptic; Wiffen 2013), amitriptyline (a tricyclic antidepressant; Moore 2012), milnacipran (a serotonin–norepinephrine reuptake inhibitor; Derry 2012), and monoamine oxidase inhibitors (Tort 2012). These Cochrane reviews have informed recent clinical practice guidelines (Macfarlane 2016). Systematic reviews of non‐pharmacological treatments have provided low‐quality evidence of the effectiveness of exercise (Bidonde 2014; Bidonde 2014a; Busch 2008), cognitive‐behavioral therapy (Bernardy 2013), and acupuncture (Deare 2013) in the management of fibromyalgia. Ablin 2013 noted that "recent evidence‐based interdisciplinary guidelines concur on the importance of treatments tailored to the individual patient and further emphasize the necessity of self management strategies which include exercise and psychological techniques."
People with fibromyalgia are often intolerant of physical activity and tend to have a sedentary lifestyle that increases risks of additional morbidity (Park 2007; Raftery 2009). Exercise is an important part of fibromyalgia management (Goldenberg 2004; Hauser 2010a; Rooks 2008) because individuals with fibromyalgia are often deconditioned by low cardiovascular fitness (Turk 2002), muscle strength, and muscle endurance (Bennett 1989; Bennett 1998). Whether physical deconditioning plays a role in the causal pathway of fibromyalgia is not clear, but several studies have demonstrated that individuals with fibromyalgia can perform different types of exercise (Bidonde 2014; Busch 2013; Carville 2008; Hauser 2010). Regular exercise is an important factor in countering age‐related loss of muscle, bone mass, and functional independence for the general population; therefore, individuals with fibromyalgia may improve their overall health and moderate risks associated with other chronic conditions by following an exercise program (Rooks 2008). Answers to questions regarding the best type of exercise, appropriate intensity, and delivery options for exercise interventions are still needed. This review on aerobic exercise training provides information that will guide clinicians and patients with fibromyalgia in designing the most effective aerobic exercise training interventions. Definitions for some of the terms utilized in this review can be found in the "Glossary of terms" (Table 2).
1. Glossary of terms.
| Term | Definition |
| Agonist‐antagonist muscle contraction | Agonist muscles and antagonist muscles refer to muscles that cause or inhibit movement. Agonist muscles cause movement to occur through their own contraction, and antagonist muscles oppose a specific movement, for example, biceps (agonist) and triceps (antagonist) muscles |
| Amitriptyline | A widely use tricyclic antidepressant medication; it is used to treat several mental illnesses/disorders such as major depression, anxiety, psychosis, bipolar disorder, etc. Other uses include prevention of neuropathic pain such as fibromyalgia |
| Biomarker | In medicine, "biomarker" is a term that is often used to refer to measurable characteristics that reflect the severity or presence of some disease state. It is often an indicator of a particular disease state or some other psychological state of an organism |
| Cardiorespiratory fitness | The ability of the circulatory and respiratory systems to supply oxygen to muscles during sustained physical activity |
| Cognitive‐behavioral therapy | A form of therapy in which the goal is to diminish symptoms by correcting distorted thinking based on negative self‐perceptions and expectations |
| Concomitant | Existing or concurring with something else |
| Detraining | Losing physical and health effects gained during exercise training by stopping exercise |
| Exercise | Physical activity that is planned, structured, and repetitive, and [that] has as a final or intermediate objective of improvement or maintenance of physical fitness (Garber 2011) |
| Exercise training | Program that is designed to meet individual health and physical fitness goals; a single exercise session should include warm‐up, stretching, conditioning, and cool‐down components. The rate of progression depends on the individual's health status and exercise tolerance |
| Genetic | Considered a field of biology, genetics is the study of genes within living organisms; pertaining or according to genetics |
| Heart rate reserve (HRR) | Difference between resting heart rate (HRrest) and maximum heart rate (HRmax). Heart rate reserve is used to determine exercise heart rates |
| Hormones | Any of various internally secreted compounds, such as insulin or thyroxine, formed in endocrine glands that affect the functions of specifically receptive organs or tissues when transported to them by body fluids |
| Inflammatory | Pathology of or caused by inflammation; biological response of body tissues to harmful stimuli such as irritants, damaged cells, or pathogens |
| Maximal aerobic performance | Maximum rate of oxygen consumption as measured during incremental exercise |
| Maximum heart rate (HRmax) | The highest number of beats per minute your heart can reach during maximum physical exertion. This rate is individual and depends on hereditary factors and age |
| Microtrauma | Trauma to muscle cells |
| Milnacipran | A serotonin‐norepinephrine reuptake inhibitor |
| Min × d−1 | Minutes per day |
| Monoamine oxidase inhibitors | An oxidoreductase inhibitor of a single amino group neurotransmitter |
| Muscle strength | A physical test of the amount of force a muscle can generate |
| Neurotransmitters | Any of several chemical substances, such as epinephrine or acetylcholine, that transmit nerve impulses across a synapse to a postsynaptic element, such as another nerve, muscle, or gland |
| Non‐pharmacological | Treatment that does not include medication |
| OMERACT | OMERACT (Outcome Measures in Rheumatology) is an independent initiative of international health professionals interested in outcome measures in rheumatology. Over the past 20 years, OMERACT has served a critical role in the development and validation of clinical and radiographic outcome measures in rheumatoid arthritis, osteoarthritis, psoriatic arthritis, fibromyalgia, and other rheumatic diseases (www.omeract.org). OMERACT is linked to the Cochrane Collaboration Musculoskeletal Review Group, where outcomes endorsed by OMERACT are recommended for use in Cochrane Systematic Reviews |
| Pathophysiology | The physiology of abnormal or diseased organisms or their parts |
| Perceived exertion | Amount of effort that is perceived by someone, usually rated on a scale of 6 to 20 or 1 to 10 |
| Physical activity | Any bodily movement produced by skeletal muscles that results in energy expenditure above resting (basal) levels. Physical activity broadly encompasses exercise, sports, and physical activities done as part of daily living, occupation, leisure, and active transportation (Garber 2011) |
| Physical fitness | Ability to carry out daily tasks with vigor and alertness, without undue fatigue and with ample energy to enjoy (leisure) pursuits and to meet unforeseen emergencies. Physical fitness is operationalized as "[a set of] measurable health and skill‐related attributes" |
| Physical function | The capacity of an individual to carry out physical activities of daily living. Physical function reflects motor function and control, physical fitness, and habitual physical activity and is an independent predictor of functional independence, disability, and morbidity |
| Physiology | Branch of biology dealing with the functions and activities of living organisms and their parts, including all physical and chemical processes |
| Predicted maximum heart rate (HRmax‐p) | HRmax‐p is a score equivalent to maximum heart rate (HRmax). HRmax‐p may provide a way to define training intensities as percentages of maximum heart rate and to follow maximum heart rate changes due to training without an exhaustive maximal stress test |
| Pregabalin | An antiepileptic medication |
| Prevalence | Rate of occurrence of a condition, usually expressed on a per‐year basis |
| Skewness | Not every distribution of data is symmetrical ‐ sets of data that are not symmetrical are said to be "asymmetrical." The measure of how asymmetrical a distribution can be is called "skewness" |
| Sleep disturbance | A score derived from a questionnaire that measures sleep quantity and quality. The Medical Outcomes Survey Sleep Scale measures 6 dimensions of sleep (initiation, staying asleep, quantity, adequacy, drowsiness, shortness of breath, snoring) |
| Somatic comorbidities | Conditions of the body related to a disease |
| Symptoms | Patients' perceptions of an "abnormal" physical, emotional, or cognitive state |
| Tenderness | Pain evoked by tactile pressure |
Description of the intervention
For this review, we focused on studies that examined aerobic exercise training in the management of fibromyalgia. According to the American College of Sports Medicine (ACSM) guidelines for exercise testing and prescription, "aerobic exercise (also called cardiorespiratory or endurance exercise) represents a broad range of physical activities such as walking, jogging, cycling, and dancing performed at submaximal intensities that can be sustained from minutes to hours, depending in part on the fitness level of the individual and the intensity of the exercise. Aerobic exercise training represents organized regimens of physical activity that are repeated over time" (ACSM 2013). We also included two studies of leisure time physical activity ‐ a less structured intervention, in which participants were advised to perform moderate‐intensity aerobic activity on their own. Moderate and vigorous programs of aerobic exercise training and leisure time physical activity have been shown to improve physical fitness, lower risk of all‐cause and cardiovascular disease mortality and morbidity (Garber 2011), and achieve other health benefits (ACSM 2013, pages 7‐10).
The ACSM position paper on quantity and quality of exercise for developing fitness in apparently healthy adults provides well‐recognized and widely accepted guidelines for aerobic and other types of exercise training (Garber 2011). In its position paper, the ACSM recommends that for aerobic exercise, most adults should engage in moderate‐intensity cardiorespiratory exercise training using large muscle groups and rhythmical activities for 30 minutes or longer per day on five or more days per week for a total of 150 minutes or longer; or vigorous‐intensity cardiorespiratory exercise training for 20 minutes or longer per day on three or more days per week for a total of 75 minutes or longer per week; or a combination of moderate‐ and vigorous‐intensity exercise performed to achieve a total energy expenditure of 500 to 1000 metabolic equivalent (MET) minutes per week.
The ACSM position paper (Garber 2011) and subsequent publications (ACSM 2013) have described aerobic exercise training based on the FITT‐VP principle of exercise prescription: frequency (F), intensity (I), time or duration (T), type or mode (T), total volume (V), and progression (P), with increased training volume, as explained below.
F ‐ Exercise frequency refers to the number of times per week that a person exercises.
I ‐ Exercise intensity can be described in terms of heart rate, oxygen consumption (VO2), perceived exertion, or METs. No studies have compared all methods of exercise intensity at the same time, and these methods are not necessarily completely equivalent to each other (ACSM 2013). Exercise intensity is most accurately determined from data measured during tests of maximal aerobic performance. Such tests have not been commonly employed in fibromyalgia and exercise research. Although the calculation is subject to greater error, intensity is more commonly determined from predictive equations (ACSM 2013). Many studies included in this review used predictive heart rate calculations to determine the intensity of the exercise training intervention and described training intensity as a percentage of participants’ predicted maximal heart rate. The specific range of values used to classify exercise intensity as moderate or vigorous has changed over time, guided by research over the past 40 years (ACSM 2013). We have included in this review a table that shows the current classification of aerobic exercise intensities as described by Garber 2011 (Table 3).
2. Classification of exercise intensity (Garber, 2011).
| Intensity | %VO2 reserve/% HR reserve | % HRmax | Perceived exertion scale (RPE) 6 to 20 |
| Very light | < 37 | < 57 | RPE < 9 |
| Light | 37 to 45 | 57 to 63 | RPE 9 (very light) to 11 (fairly light) |
| Moderate | 46 to 63 | 64 to 76 | RPE 12 (fairly light) to 13 (somewhat hard) |
| Vigorous | 64 to 90 | 77 to 95 | RRE 14 (somewhat hard to 17 (very hard) |
| Near maximal to maximal | ≥ 91 | ≥ 96 | RPE ≥ 18 (very hard) |
HR: heart rate; RPE: rating of perceived exertion; VO2: oxygen consumption
T ‐ Time (duration) of exercise refers to the length of an exercise session.
T ‐ Exercise type (mode) refers to the actual activity done for aerobic exercise.
V ‐ Total volume of exercise refers to the product of frequency, intensity, and time (FIT) of aerobic exercise.
P ‐ The recommended rate of progression depends on the participant’s health status, physical fitness, training responses, and exercise program goals. Progression may consist of raising any of frequency, intensity, time, or type of exercise. The ACSM recommends increasing time of aerobic exercise first, then increasing training volume through changes in frequency, intensity, or time.
How the intervention might work
The pathophysiology of fibromyalgia includes changes in brain and neural structure and function, muscular physiology, hormonal factors, neurotransmitters, neuroendocrine transmitters, inflammatory markers, and genetic influences, resulting in augmented experiences and lowered inhibition of pain and other sensations (Jahan 2012; Marcus 2011;Schmidt‐Wilcke 2011). Muscle abnormalities that may result in weakness, fatigue, and muscle pain for individuals with fibromyalgia include reductions in type II fibers, abnormal muscle metabolism, excessive agonist–antagonist co‐contraction, lowered levels of adenosine triphosphate, and damage to nerve fibers (Park 2000;Schmidt‐Wilcke 2011). Mood disorders and psychiatric comorbidities, which also are associated with fibromyalgia, are linked to disturbed stress adaptation responses due to hypothalamic‐pituitary axis abnormalities and interactions among biological, psychological, and behavioral mechanisms (Jahan 2012; Schmidt‐Wilcke 2011).
Effective treatment and management strategies for fibromyalgia consist of non‐pharmacological therapies such as exercise (Nuesch 2013; Schmidt‐Wilcke 2011). Exercise, primarily aerobic exercise, is known to enhance feelings of “energy” and improve quality of life and cognitive function (Garber 2011). Regular exercise can also improve experiences of anxiety, depression, and pain, and can improve sleep quality (Busch 2011;Klaperski 2014; Moylan 2013; Yang 2012). Aerobic exercise alters neurotransmitters, neuromodulators, brain chemistry, and hypothalamic‐pituitary function (Barclay 2014; Klaperski 2014; Lopresti 2013; Moylan 2013; Puetz 2006). These elements are involved in brain function, and their improvement through exercise can lead to improved feelings of energy, improved mood, and reduced stress, anxiety, and depression (Klaperski 2014; Moylan 2013; Puetz 2006). With aerobic exercise, the hypothalamus releases increased levels of neurotransmitters including endorphins (Barclay 2014; Lopresti 2013; Scheef 2012). This increase in endorphin release results in decreased pain sensation and improved mood states and sleep quality (Scheef 2012; Yang 2012). Exercise may contribute to pain reduction by improving the physiological response to muscle microtrauma through increased resilience, repair, and resultant adaptation (McLoughlin 2011). Aerobic exercise also leads to reduced inflammation and oxidative stress in the body, which results in reduced anxiety and stress responses (Klaperski 2014; Moylan 2013). Overall, aerobic exercise can contribute to improved physiology, which can attenuate the alterations associated with fibromyalgia.
Why it is important to do this review
This is an update of a previously published Cochrane review on exercise for treating fibromyalgia (Busch 2002; Busch 2007). Review authors specifically evaluated the benefits of aerobic exercise training. Aerobic exercise has been recognized as beneficial for overall health and prevention/management of chronic conditions for more than 50 years (Bouchard 2012; Garber 2011). Increasing evidence has shown the benefits of aerobic exercise as a treatment for chronic conditions, including fibromyalgia (Nunan 2013). Aerobic exercise is the most easily accessible and most commonly recognized form of exercise, making it a reasonable recommendation and treatment strategy (Eyler 2003). However, current evidence showing the benefits of aerobic exercise for individuals with fibromyalgia is limited. A growing body of literature suggests that a review of these benefits is needed to accurately assess aerobic exercise effectiveness for improving the health of individuals with fibromyalgia. To provide indicators of the safety of aerobic exercise among patients with fibromyalgia, this review investigated adverse events and evaluated attrition rates and adherence to training protocols. New trials added to this update have served to strengthen the quality of the evidence.
Objectives
To evaluate the benefits and harms of aerobic exercise training for adults with fibromyalgia
-
To assess the following specific comparisons
Aerobic versus control conditions (eg, treatment as usual, wait list control, physical activity as usual)
Aerobic versus aerobic interventions (eg, running vs brisk walking)
Aerobic versus non‐exercise interventions (eg, medications, education)
We did not assess specific comparisons involving aerobic exercise versus other exercise interventions (eg, resistance exercise, aquatic exercise, flexibility exercise, mixed exercise). Other systematic reviews have examined or will examine these comparisons (Bidonde 2014; Busch 2013).
Methods
Criteria for considering studies for this review
Types of studies
We included trials described as randomized, even when methods of generating the random sequence were unclear or were not reported, or when the method of allocating participants was likely to be quasi‐random (ie, by alternation, date of birth, or a similar pseudo‐randomized method).
Types of participants
We included in the review studies that examined adults with fibromyalgia (≥ 18 years of age). We selected studies that used published criteria for the diagnosis (or classification) of fibromyalgia. Until recently, American College of Rheumatology (ACR) 1990 criteria have been used as the standard for classifying individuals as having fibromyalgia (Wolfe 1990). By this method, individuals are classified as having fibromyalgia when they have experienced widespread pain lasting longer than three months with at least 11 active tender points. Tender points are noted at 18 designated locations on the body and are defined as active if pain can be elicited by applying 4 kilogram tactile pressure.
A preliminary diagnostic tool, ACR 2010 (Wolfe 2010), which does not rely upon a physical tender point examination, is now available both as a clinician‐administered questionnaire and as a survey questionnaire (Wolfe 2011). This measure includes the Widespread Pain Index (19 areas representing anterior and posterior axis and limbs), in addition to a Symptom Severity Scale that contains items related to secondary symptoms such as fatigue, sleep disturbances, cognition, and somatic complaints. Scores on both measures are used to determine whether a person qualifies for a “case definition” of fibromyalgia. This tool has been found to correctly classify 88% of cases that meet ACR 1990 criteria, and it allows ongoing monitoring of symptom change among people with a current or previous fibromyalgia diagnosis (Wolfe 2010). Although measures focusing on tender point counts have been widely applied in clinical and research settings, the methods described by Wolfe 2010 and Wolfe 2011 promise to classify people with fibromyalgia more efficiently, while allowing improved monitoring of disease status over time.
Although some differences between published fibromyalgia diagnostic/classification criteria are known, for the purposes of this review, we considered all criteria to be acceptable and comparable.
Types of interventions
We examined trials that studied aerobic exercise training interventions (eg, cycling, walking) regardless of frequency, duration, or intensity. We defined aerobic exercise training as dynamic physical activity performed by using large muscle groups and rhythmical movements that increase heart rate and breathing rate above resting levels to submaximal levels for a prolonged period (Donatelle 2015).
In this review, we present data on interventions using the FITT‐VP method and express exercise intensity using both published percentages of maximum heart rate (HRmax) or heart rate reserve (HRR) and corresponding ACSM literal descriptors.
Comparator interventions included control (eg, treatment at usual, placebo, wait list control), other aerobic‐only exercise interventions (eg, low‐intensity walking), and non‐exercise interventions (eg, education, self‐management interventions).
Types of outcome measures
We designated seven outcomes as major outcomes ‐ heath‐related quality of life, pain intensity, fatigue, stiffness, physical function, number of participants who withdrew or dropped out, and adverse events ‐ and three as minor outcomes ‐ maximum cardiorespiratory function, submaximal cardiorespiratory function, and greater than 30% improvement in pain. In selecting these outcomes, we considered the consensus statement of Choy and associates (Choy 2009) regarding a core set of outcome measures for clinical trials in fibromyalgia, as well as anticipated effects of aerobic exercise training on physical fitness. We extracted data for the selected outcomes for any time points measured but included baseline, post‐treatment, and follow‐up data in this review. Review criteria required each included study to report measurement of one or more outcomes for at least one of these time periods.
Major outcomes
When an included study used more than one instrument to measure a particular outcome, we applied the following preferred hierarchy in choosing the outcome for analysis.
Health‐related quality of life (HRQL) ‐ This outcome consists of multidimensional indices used to measure general health status or health‐related quality of life, or both (Choy 2009). When included studies used more than one instrument to measure health‐related quality of life, we preferentially extracted data from the Fibromyalgia Impact Questionnaire (FIQ Total; Burckhardt 1991), followed by the Short Form Questionnaire (ie, SF‐36 Total or SF‐12 Total; Busija 2011; Ware 1993), and the EuroQol Group Quality of Life Questionnaire (EQ‐5D) (Wolfe 1997).
Pain intensity ‐ The International Association for the Study of Pain defined pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” (Merskey 1994). For the purposes of this review, we focused on a single aspect of the pain experience – pain intensity. When a single study reported more than one measure of pain intensity, we preferentially extracted measures of average pain intensity (as opposed to worst, least, or current pain) assessed by visual analogue scale (VAS), FIQ Pain, FIQ‐Translated, or McGill Pain VAS followed by the Numerical Pain Rating Scale. For studies that did not report unidimensional measures of pain intensity, we extracted composite measures that included pain intensity and interference (SF‐36 or Rand 36 Bodily Pain Scale) or pain intensity and suffering from pain (Mulitdimensional Pain Inventory ‐ Pain Severity Scale).
Fatigue ‐ Individuals with fibromyalgia and clinicians alike recognize fatigue as an important symptom of fibromyalgia (Choy 2009). Fatigue can be measured in a global manner, whereby an individual rates fatigue on a single‐item scale or using a multidimensional tool that breaks the experience of fatigue down into two or more dimensions, such as general fatigue, physical fatigue, mental fatigue, reduced motivation, reduced activity, and degree of interference with activities of daily living (Boomershine 2012). We accepted both unidimensional and multidimensional measures for this outcome. When included studies used more than one instrument to measure fatigue, we preferentially extracted data from the fatigue VAS (FIQ/FIQ‐Translated Fatigue, or single‐item fatigue VAS), followed by the SF‐36 or the Rand 36 Vitality Subscale, the Chalder Fatigue Scale (Total), the Fatigue Severity Scale, and the Multidimensional Fatigue Inventory.
Stiffness ‐ In focus groups conducted by Arnold 2008, individuals with fibromyalgia "... remarked that their muscles were constantly tense. Participants alternately described feeling as if their muscles were ‘lead jelly’ or ‘lead Jell‐O', and this resulted in a general inability to move with ease and a feeling of stiffness." A measure of stiffness commonly encountered in this literature is the FIQ Stiffness Subscale.
Physical function ‐ This outcome focuses on the basic actions and complex activities considered “essential for maintaining independence, and those considered discretionary that are not required for independent living, but may have an impact on quality of life” (Painter 1999). Cardiorespiratory fitness, neuromuscular attributes (eg, muscular strength, endurance, power), and muscle and joint flexibility are important determinants of physical function; therefore, this outcome is highly relevant as an outcome of exercise interventions. When more than one measure of physical function was available within a study, we preferentially extracted data from the FIQ Physical Impairment Scale (Burckhardt 1991), followed by the Health Assessment Questionnaire (HAQ) Disability Scale, the SF‐36 or the Rand 36 Physical Function Scale,the Sickness Impact Profile – Physical Disability Scale (Bergner 1981), and the Multidimensional Pain Inventory Household Chores Scale (Huskisson 1976; Huskisson 1983).
Adverse events ‐ We extracted the proportion of participants who experienced adverse events during the intervention (ie, injuries, exacerbations of pain, and/or other fibromyalgia symptoms); if this information was not available, we described the nature of the adverse events in a narrative report.
Withdrawals ‐ We recorded the proportion or number of participants who withdrew or dropped out of the study for any reason.
Minor outcomes
We present here a rationale and preference listing of minor outcomes. Among the three outcomes designated as minor outcomes, we included two fitness variables that potentially could be improved by aerobic exercise training.
Maximal cardiorespiratory function (CR max) ‐ Cardiorespiratory function is the ability of the heart, lungs, and circulatory system to efficiently supply oxygen and nutrients to working muscles. Rhythmical, aerobic‐type exercises involving large muscle groups are recommended for improving cardiovascular fitness. Maximal oxygen uptake (VO2max) is accepted as the best criterion for measuring cardiorespiratory fitness. Maximal oxygen uptake is the product of maximal cardiac output (L blood × min‐1) and the arterial‐venous oxygen difference (mL O2/L blood). Disadvantages of maximal tests include that they require the participant to exercise to the point of volitional fatigue and often require medical supervision and access to the emergency equipment. For this reason, maximal exercise testing is not always feasible in research, health, and fitness settings. For this review, we preferentially extracted data from maximal or symptom‐limited treadmill or cycle ergometer tests in units of mL/kg/min, energy expended, peak workload, or test duration. We also accepted data from exercise tests that yielded predicted maximum oxygen uptake.
Submaximal cardiorespiratory function (CR submax) ‐ Two major categories of submaximal tests are available: predictive and performance tests. Predictive tests are submaximal tests that are used to predict maximal aerobic capacity (Noonan 2000). Performance tests involve measuring responses to standardized physical activities that are typically encountered in everyday life. For this review, we preferentially extracted data on work completed at a specified exercise heart rate (eg, PWC170 test ‐ estimates physical work capacity at 170 beats per minute), followed by distance walked in six minutes (meters), the two‐minute walk test (meters), walking time for a set distance (seconds), an anaerobic threshold test, and timed walking distance (eg, Quarter Mile Walk Test).
Improvement in pain greater than 30% ‐ A 30% reduction is considered a benchmark for a moderately important change in pain intensity and is recommended by an Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) for interpreting clinical trial efficacy (Dworkin 2008). When available, we extracted data on proportions of participants who met this criterion for intervention efficacy.
Search methods for identification of studies
The team Information Specialist conducted a comprehensive search of nine databases for physical activity interventions for adults with fibromyalgia. We screened citations found by electronic and manual searches and classified them by type of exercise training. This comprehensive search revealed physical activity intervention studies that included a subset of aerobic training interventions.
Electronic searches
We searched the following databases from database inception to June 2016 using current methods outlined in Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011). We applied no language restrictions. We have provided full search strategies for each database in the appendices, as indicated in the list.
MEDLINE (OVID) 1946 to June 2016 (Appendix 1).
Embase (OVID), Embase Classic+Embase 1947 to June 2016 (Appendix 2).
-
Cochrane Library (Wiley) to the present (http://www.thecochranelibrary.com/view/0/index.html) (Appendix 3):
Cochrane Database of Systematic Reviews (Cochrane Reviews);
Database of Abstracts of Reviews of Effects (DARE);
Cochrane Central Register of Controlled Trials (CENTRAL);
Health Technology Assessment Database (HTA); and
NHS Economic Evaluation Database (EED).
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (Ebsco) 1982 to June 2016 (Appendix 4).
Physiotherapy Evidence Database (PEDro) (www.pedro.org.au/) accessed to June 2016 (Appendix 5).
Dissertation Abstracts (ProQuest) accessed to June 2016 (Appendix 6).
Current Controlled Trials accessed to October 25, 2013 (discontinued) (Appendix 7).
Clinicaltrials.gov accessed from June 2014 to June 2016 (Appendix 7).
World Health Organization (WHO) International Clinical Trials Registry Platform (www.who.int/ictrp/) accessed to June 2016 (Appendix 8).
Allied and Complementary Medicine (AMED) (OVID) 1985 to June 2016 (Appendix 9).
Searching other resources
Two review authors independently reviewed reference lists from key journals, identified articles and reviews of all types of treatment for fibromyalgia, scrutinized all promising or potential references, and added appropriate titles to the search output.
Data collection and analysis
Review authors
Review authors were members of the Cochrane Musculoskeletal Group (CMSG) ‐ Exercise for Fibromyalgia Team (see Acknowledgments). The authors of this review were trained in data extraction using a standardized orientation program. Review authors worked independently and in pairs with at least one physical therapist in each pair to extract data. The team met regularly to discuss progress, to clarify procedures, to make decisions regarding inclusion or exclusion and classification of outcome variables, and to work collaboratively in the production of this review.
Selection of studies
Two review authors used a set of predetermined criteria to independently examine the titles and abstracts of studies generated by the searches (see Appendix 10). We retrieved full‐text publications for all abstracts of potential interest. We had all non‐English reports translated. Two review authors then independently examined the full‐text reports to determine whether studies met selection criteria (see Appendix 10). Review authors resolved disagreements and questions regarding interpretation of inclusion criteria through discussion with partners or by involvement of a third review team member if needed.
Data extraction and management
We used electronic data extraction forms developed and refined in our previous reviews to facilitate independent data extraction and consensus (Busch 2008). Pairs of review authors independently extracted data. We resolved disagreements by involving a third review author (AJB). Two review authors (AJB and JB) transferred data into Review Manager (RevMan 2014) software. We double‐checked that data were entered correctly by comparing data presented in the software against study reports. We noted in the Characteristics of included studies table whether outcome data were obtained directly from randomized controlled trial (RCT) authors or were transformed or estimated from a graph. If both unadjusted and adjusted values were reported for the same outcome, we extracted adjusted values. If data were analysed using an intention‐to‐treat (ITT) sample and another sample (eg, per‐protocol, as‐treated), we extracted ITT data.
We extracted the following data from the included studies.
Methods: study design, total duration of study and follow‐up (if applicable), and date of study.
Participants: N, mean age, age range, gender ratio, disease duration, diagnostic criteria, and inclusion and exclusion criteria.
-
Interventions, comparisons, concomitant treatments, recording:
for all interventions with an exercise component: intervention duration, frequency, duration of exercise sessions, intensity, progression model, mode, and congruence with ACSM guidelines (Appendix 11); and
for interventions with a non‐exercise component: frequency, duration, and main characteristics.
Outcomes: major and minor outcomes as indicated above. Additional outcomes assessed (recorded in the Characteristics of included studies section under "Outcomes Other"), means and standard deviations for tests at baseline and post intervention, and follow‐up for continuous outcomes. If post‐test data were not available, we extracted means and standard deviations of change scores.
Characteristics of trial design as outlined in the Assessment of risk of bias in included studies section.
Notes: funding for trial, language of the article, records of trial author contacts, and notable declarations of interest.
Assessment of risk of bias in included studies
Two review authors independently evaluated the risk of bias of each included study using a customized form based on the Cochrane "Risk of bias" tool (Higgins 2011a). The risk of bias tool addresses seven specific domains: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective outcome reporting (including publication bias), and other sources of bias. For "other" sources of bias, we considered sources such as baseline inequities despite randomization. We rated each criterion as introducing low, high, or unclear risk of bias according to information provided in the studies and sometimes through study author responses. We classified studies as having low risk of bias if all key domains had low risk of bias and no serious flaws. We assigned unclear risk when absence or ambiguity of information blocked assessors' ability to determine the potential for bias. In such cases, we revised assessments when study authors responded to our requests for more information. We resolved disagreements between review author pairs through consensus meetings or by involvement of a third review team member if needed.
Measures of treatment effect
For continuous data, we used group post‐test means and standard deviations to calculate effect sizes with RevMan 2014 software. We expressed effect sizes preferentially as mean differences (MDs) and 95% confidence intervals (95% CIs), but when different scales were used to measure the same outcome, we calculated standardized mean differences (SMDs) with corresponding 95% CIs instead. We analyzed dichotomous data as risk ratios (RRs) and 95% confidence intervals. We used RevMan 2014 software to generate forest plots to display study results.
In the comments column of Table 1, we provided the absolute percent difference and the number needed to treat for an additional beneficial outcome (NNTB) or for an additional harmful outcome (NNTH). We provided the NNTB or NNTH only when the outcome showed a statistically significant difference. We calculated the NNTB for continuous measures using the Wells calculator (available at the CMSG Editorial Office). For dichotomous outcomes, such as adverse events, we calculated the NNTH from the control group event rate and the relative risk using the Visual Rx NNT calculator (Cates 2008).
In accordance with the Philadelphia Panel (Philadelphia Panel 2001), we assumed a minimal clinically important difference (MCID) of 15 points on a 100‐point continuous pain scale, and a relative difference of 15% on all functional scales, as clinically relevant. We used the MCID in calculating NNTB for continuous outcomes. For dichotomous outcomes, we calculated the absolute risk difference using the risk difference statistic available in RevMan 2014, and expressed the result as a percentage. For continuous outcomes, we calculated the absolute benefit as improvement in the intervention group minus improvement in the control group, expressed in original units.
We calculated the relative per cent change for dichotomous data as the risk ratio ‐ 1, and expressed this as a percentage. For continuous outcomes, we calculated the relative difference in changes from baseline as the absolute benefit divided by the baseline mean of the control group, expressed as a percentage.
Unit of analysis issues
Although many randomized controlled trials (RCTs) include only two parallel arms (ie, groups), some consist of three or four parallel arms; thus a single randomized trial can yield several relevant comparisons. This review examined any relevant comparisons that allowed evaluation of effects of aerobic exercise training interventions on people with fibromyalgia. For example, a three‐arm trial comparing aerobic versus drug treatment versus sham could appear in two separate analyses: aerobic versus sham and aerobic versus drug treatment. When a control group was used as a comparator twice in the same analysis, we halved the sample size of the control group (Deeks 2011).
Dealing with missing data
When numerical data were missing, we contacted the study author to request additional data required for analysis. We used open‐ended questions to request the information needed to assess risk of bias and/or treatment effects. When numerical data were available only in graphical form, we used Engauge version 5.1 (Mitchell 2012) to extrapolate means and standard deviations by digitalizing data points on the graphs provided.
For dichotomous outcomes (eg, number of withdrawals), we calculated the withdrawal rate by using the number of participants randomized in the group as the denominator. For continuous outcomes (eg, post‐test pain score), we calculated the MD or the SMD using the number of individuals analysed at that time point. When the number of individuals analysed was not presented for each time point, we used the number of individuals randomized to each group at baseline. When means were not reported, we accepted medians. When post‐test standard deviations were unavailable, we used standard deviations of pretest scores as estimates. When variance was expressed using statistics other than standard deviation (eg, standard error, confidence interval, P value), we computed standard deviations using the methods recommended in Chapter 7 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). When we could not derive missing standard deviations using the methods described above, we imputed them from other studies included in the meta‐analysis.
Assessment of heterogeneity
We assessed clinical and methodological diversity in terms of participants, interventions, outcomes, and study characteristics for the included studies to determine whether a meta‐analysis was appropriate. We did this by reviewing data obtained from data extraction tables. We assessed statistical heterogeneity through visual inspection of the forest plot to look for obvious differences in results between studies, and through use of I² and Chi² statistical tests. As recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011), we interpreted an I² value from 0% to 40% as might "not be important"; from 30% to 60% as may represent "moderate" heterogeneity; from 50% to 90% as may represent "substantial" heterogeneity; and from 75% to 100% as representing "considerable" heterogeneity. We interpreted the Chi² test with a P value ≤ 0.10 as indicating statistical heterogeneity.
When we removed a trial from the analysis, we noted changes in both heterogeneity and effect size. Because I² involves overlapping categories (eg, 0% to 40%, 30% to 60%) or "ambiguous" zones, we explored statistical heterogeneity thoroughly when noted (eg, I² between 50% and 60%). Given that values between 50% and 60% fall into an "ambiguous" zone, if we could find no apparent causes of heterogeneity, we kept the trial in the analysis and documented our decision.
Assessment of reporting biases
We planned to draw contour‐enhanced funnel plots (Sterne 2011) for each meta‐analysis to assess publication reporting bias if a large enough sample of studies (ie, more than 10 studies) was available/included in the meta‐analysis. As the statistical conditions were not met, we did not perform these analyses.
If the RCT protocol was available, we compared outcomes in the RCT protocol versus outcomes in the published report. For studies published after July 1, 2005, we screened the Clinical Trials Register at the International Clinical Trials Registry Platform of the World Health Organisation (http://apps.who.int/trialssearch) and at ClinicalTrials.gov (http://clinicaltrials.gov) to look for the RCT protocol.
We compared the fixed‐effect estimate against the random‐effects model to assess the possible presence of small sample bias (ie, by which the intervention effect is more beneficial in smaller studies) in the published literature. In the presence of small sample bias, the random‐effects estimate of the intervention is more beneficial than the fixed‐effect estimate (Sterne 2011).
Data synthesis
When two or more studies reported the same outcome and when interventions were deemed homogeneous enough, we pooled the data (meta‐analysis) using RevMan 2014. Before pooling data, we ensured the directionality of the data that permitted pooling; we arithmetically reversed selected scales as needed so higher values consistently had the same meaning. We ensured that scaling factors were consistent to permit calculation of MD (eg, 10‐cm scales expressed in mm to match 100‐mm scales). We presented results grouped by common comparator, for example, aerobics versus control, aerobics versus no exercise, aerobics versus aerobic intervention. We included all studies for adverse events and withdrawals.
"Summary of findings" table
We used GradePro (version 3.6; Schünemann 2011a) to prepare the "Summary of findings" table for major outcomes for aerobic exercise training versus no exercise control, at the end of the intervention. In the "Summary of findings" table, we integrated analysis of quality of evidence and magnitude of effect of the interventions. We downgraded the overall rating of quality of evidence for the study (outcome by outcome) by at least one grade (using GRADE) if the study had high or unclear risk of bias in at least one domain.
We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of the body of evidence at one of four levels.
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: Research shows substantial uncertainty about the estimate.
We assigned GRADE quality ratings separately for the seven major outcomes. Because of the comprehensive nature of the outcome variable of health‐related quality of life, we gave it primacy over all other variables in the "Summary of findings" table and in the "Plain language summary."
Subgroup analysis and investigation of heterogeneity
We planned two subgroup analyses on two major outcomes (HRQL and pain intensity) for the aerobics versus control comparison.
To explore the relative effects of age: Subgroups for age were younger (≤ 45 years of age) and older (> 45 years of age). Forty‐five is proposed as the cut‐off because of changes in hormone levels and lifestyle (physical activity participation) that occur with aging (Shephard 1998).
To explore subgroups for exercise volume (frequency × duration × intensity) based upon American College of Sports Medicine (ACSM) criteria (meets ACSM criteria/does not meet ACSM criteria) according to ACSM 2013 9th Guidelines.
Sensitivity analysis
We planned to conduct a sensitivity analysis to assess how results of the meta‐analysis might be affected by selection, attrition (> 20%), and detection biases for post‐treatment pain intensity and HRQL outcomes in the main comparison.
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies; and Characteristics of studies awaiting classification.
Results of the search
The search resulted in a total of 3684 records, which included 3646 journal records and 38 trial registry records. After we had removed 942 duplicates, 2742 records remained. We excluded 2529 records on citation and abstract screening. We assessed 213 full‐text articles and 20 protocols/trial registry records for eligibility and excluded 77 full‐text articles and seven protocols/trial registry records. We included 16 full‐text publications (13 primary studies, three companion papers) and three RCT protocols examining aerobic exercise training. On the most recent update to the search, we found five additional full‐text articles (three of which had trial registry records) that are awaiting full assessment. See Figure 1 for details.
1.
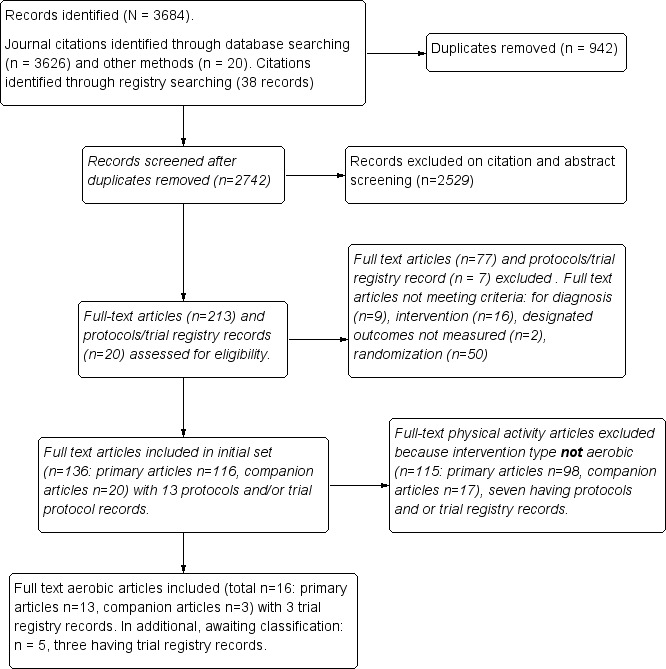
Study flow diagram.
Included studies
We considered for this review 16 full‐text reports and three registry records describing 13 unique aerobic exercise training studies and meeting our selection criteria. We used the three registry records (hereafter, RCT protocols) to assess the quality of studies (Fontaine 2010; Kayo 2011; Mannerkorpi 2010). We included the following 13 distinct RCTs for analysis: Fontaine 2007; Fontaine 2010; Gowans 2001; Kayo 2011; King 2002; Mannerkorpi 2010; Mengshoel 1992; Nichols 1994; Ramsay 2000; Sanudo 2010; Schachter 2003; Sencan 2004; and Wigers 1996. Although we found 16 separate article publications, we included only 13 studies. One publication (Fontaine 2011) reported additional variables from the Fontaine 2010 primary study; therefore, we included the two and counted them as one study for analysis (hereafter identified as Fontaine 2010). Similarly, Gowans 2002 reported additional variables from the primary article for Gowans 2001, and we counted these as one study for analysis (hereafter identified as Gowans 2001). One publication by Mengshoel published in 1993 reported additional variables from the Mengshoel 1992 primary study; therefore, we included the two and counted them as one study for analysis (hereafter identified as Mengshoel 1992). The average length of treatment was 15 weeks (minimum of six and maximum of 24 weeks); follow‐up data post intervention were available for seven trials (Fontaine 2010; Kayo 2011; King 2002; Mannerkorpi 2010; Ramsay 2000; Sencan 2004; Wigers 1996) and ranged from 24 to 208 weeks. All studies used a randomized clinical trial with a parallel group study design. In the recent update to the search, we identified five additional full‐text articles (with three registry records) that are awaiting assessment (Bjersing 2012; Duruturk 2015; Espí‐López 2016; Mendonca 2016; Sanudo 2015).
Studies were published between 1992 and 2011 and were conducted across eight countries, including Canada (3), United States (3), Brazil (1), Spain (1), Norway (2), Sweden (1), United Kingdom (1), and Turkey (1). All studies were written in English. We contacted six study authors (Fontaine 2007; Fontaine 2010; Kayo 2011; Mannerkorpi 2010; Sanudo 2010; Schachter 2003) using open‐ended questions to request information needed to assess risk of bias, the exercise intervention, and/or the treatment effect. We received responses from five study authors and have presented in Table 4 outcome measures extracted for all included studies.
3. Outcome measures used in included studies.
| Outcome | Name of Instrument or index/subscale |
| Health‐related quality of life | FIQ Total (0‐100) |
| Pain intensity/interference | Current pain (VAS), FIQ pain (VAS), SF‐36 bodily pain (interference) |
| Fatigue | VAS (0‐100), FIQ fatigue (0‐100), SF‐36 vitality (0‐100), Fatigue Severity Scale (9‐63), Multidimensional Fatigue Inventory (4‐20) |
| Stiffness | FIQ stiffness |
| Physical function | SF‐36 physical functioning (0‐100), FIQ physical function (0‐100), Sickness Impact Profile (0‐68), Health Assessment Questionnaire (HAQ) |
| Maximal cardiorespiratory function | Oxygen uptake (VO2max), maximum work capacity (w) |
| Submaximal cardiorespiratory function | 6‐minute walk test (distance in meters), Astrand submaximal cycle ergometer test (heart rate at a steady state workload) |
| Adverse events | Not a standardized instrument or index/narrative information |
FIQ: Fibromyalgia Impact Questionnaire; HAQ: Health Assessment Questionnaire; SF‐36: Short Form 36; VAS: visual analogue scale; VO2max: maximal oxygen uptake
Six studies reported findings on multiple treatment arms (Kayo 2011; King 2002; Sanudo 2010; Schachter 2003; Sencan 2004; Wigers 1996); we included in the analysis arms comparing an aerobic exercise training group versus another aerobic exercise training group or versus a non‐exercise intervention. Information on which arms were included in the analyses can be found in the Characteristics of included studies section.
Participants
This review included 839 participants, of whom 750 were female. Nine studies included female participants only, three included participants of both genders, and one study (Ramsay 2000) did not specify the gender of participants. The average duration of disease or symptoms since diagnosis ranged from 5 to 11.5 years; three studies did not report this information (Ramsay 2000; Sanudo 2010; Schachter 2003). Average age of participants was 41 years (minimum to maximum, 32 to 56 years); one study (Ramsay 2000) did not report participants' age.
Fibromyalgia diagnosis was based on ACR 1990 (Wolfe 1990) criteria in all studies but one (Wigers 1996), in which participants had to fulfill the diagnostic criteria of Smythe 1979 and Yunus 1981. Retrospective investigation confirmed that 58 of the 60 participants in this study also fulfilled ACR 1990 criteria (Wolfe 1990).
Inclusion criteria for these trials included age (eg, 18 to 65, 30 to 55); a diagnosis of fibromyalgia; interest in exercising or willingness to comply with the exercise protocol; sedentary for six months before the trial; permission to exercise from family doctor; acceptance of randomization results; signed informed consent for study participation; stable on medications for at least three months before the start of the study; patient at the institution where the study took place or resident of the city where the study was conducted; discontinuation of medications for fibromyalgia four weeks before the start of the study; at least four years of schooling; involvement in medico‐legal cases (patients were not excluded); ability to manage a bicycle test at 50 watts or more; interest in exercising outdoors; and normal laboratory test results.
Exclusion criteria for trials consisted of presence of an acute or chronic medical condition or disease (eg, cancer; cardiovascular or respiratory disease; metabolic, musculoskeletal, and neurological conditions) interfering with moderate‐intensity aerobic exercise; inflammatory diseases (eg, systemic lupus erythematous, rheumatoid arthritis); other pain disorders; intention to seek professional help for depression or anxiety during the study period or intent to change medications that might affect mood; need for an assistive device to ambulate; enrollment in or intention to begin an aerobic exercise program or ongoing planned physical activity including exercise or participation in any regular aerobic exercise program within the six months before the study or meeting the US Surgeon 1996 recommendation for physical activity for the previous six months (not engaging in moderate physical activity for the previous six months for 30 minutes on five days per week or vigorous physical activity three times per week for 10 minutes each time during the previous month); unstable pharmacological treatment in the first month before study entry; and not speaking Swedish.
Interventions
We have provided a detailed description of trial interventions, including FITT‐VP parameters, in the Characteristics of included studies section and in Table 5. Fontaine 2007; Fontaine 2010; Kayo 2011; and Schachter 2003 met ACSM guidelines for healthy adults. Gowans 2001 met ACSM criteria for individuals who are sedentary/have no habitual activity/are extremely deconditioned. We have provided a summary of congruence with ACSM guidelines in Table 6.
4. FITT parameters.
| Author, year, intervention | Frequency, times per week – length in weeks | Intensity/ACSM intensity classification | Time/Duration/Session, minutes | Type/Mode | |
| Aerobic vs control | |||||
| Gowans 2001 | 3 times/wk | 23 weeks | 60%‐75% age‐adjusted HRmax ACSM: low to moderate | 30' | Supervised water walking/running progressing to land walking/running |
| Kayo 2011 | 3 times/wk | 16 weeks | 40%‐50% HRR at week 1 to 60%‐70% HRR by week 16 ACSM: moderate at week 1 to vigorous by week 16 | ˜ 60' | Supervised indoor or outdoor walking |
| King 2002 | 3 times/wk | 12 weeks | 60%‐75% predicted HRmax ACSM: light to moderate | Starting duration 10 to 15' progressing to 20 to 40' | Supervised walking, aquacise (deep and shallow water), or low‐impact aerobics |
| Mengshoel 1992 | 2 times/wk | 20 weeks | 120‐150 beats per minute ACSM: moderate to vigorous |
60' | Supervised low‐impact aerobic dance program |
| Nichols 1994 | 3 times/wk | 8 weeks | 60%‐70% predicted HRmax/age ACSM: light to moderate |
Unclear | Supervised fast‐paced walking on an indoor track |
| Sanudo 2010 | 2 times/wk | 24 weeks | 60%‐65% HRmax (steady state aerobics) and 75%‐80% HRmax (interval training) ACSM: light to moderate and moderate to vigorous |
45‐60’ | Supervised aerobics including continuous walking with arm movements and jogging; interval training including aerobic dance and jogging |
| Schachter 2003 Short bout | 3 to 5 times/wk | 16 weeks | 40%‐50% HRR at week 1, 60%‐70% HRR by week 10 ACSM: moderate at week 1, vigorous by week 10 |
2/d, 5' at week 1 to 15' at week 9 | Home program of low‐impact aerobics to videotaped instructor and music, rhythmical movements of lower body muscles. Supervision at 0, 4, 8, and 12 weeks |
|
Schachter 2003 Long bout |
3 to 5 times/wk | 16 weeks | 40%‐50% HRR at week 1, 60%‐70% HRR by week 10 ACSM: moderate at week 1; vigorous by week 10 |
10' at week 1 to 30' at week 9 | Home program of low‐impact aerobics to videotaped instructor and music, rhythmical movements of lower body muscles. Supervision at 0, 4, 8, and 12 weeks |
| Sencan 2004 Aerobic exercise | 3 times/wk | 6 weeks | Not specified | 40’ | Cycle ergometry. Supervision unclear |
| Wigers 1996 | 3 times/wk | 14 weeks | Tempo gradually increased up to, and decreased down from, 4 periods of 60%‐70% HRmax ACSM: light to moderate |
45’ | Supervised movement to music and games |
| Aerobic vs aerobic2 | |||||
| Mannerkorpi 2010 AE: Nordic walking | 2 times/wk | 15 weeks | 10’ at RPE 9‐11 2' intervals of RPE 13‐15, alternated with 2' at RPE 10 to 11 ACSM: 10’ light, 2’ intervals moderate to vigorous alternated with 2’ light. |
20’ | Supervised walking in parks and forests with flat areas and small hills |
|
Mannerkorpi 2010 AE2: low‐intensity walking |
1 time/wk | 15 weeks | RPE 9 to 11 ACSM: light | 20’ | Supervised walking in parks and forests with flat areas and small hills |
|
Ramsay 2000. AE: exercise class |
1 time/wk | 12 weeks | Not specified | 60’ | Supervised graded circuit exercises consisting of step‐ups, sitting to standing, skipping, jogging on the spot, alternate side bends, circling arms with increasing weights, plus encouragement to continue and increase exercises at home |
|
Ramsay 2000 AE2: single class |
1 session | 12 weeks | Not specified | 60’ | Demonstration of aerobic exercises, stretching and relaxation technique, plus written advice on aerobic exercises plus stretching and relaxation |
| Schachter 2003: AE: short bout | 3 to 5/wk | 16 weeks | 40%‐50% HRR at week 1, 60%‐70% HRR by week 10 ACSM: moderate at week 1, vigorous by weeks 10‐16 | 2/d 5' up to 15' | Home program of low‐impact aerobics to videotaped instructor and music, rhythmical movements of lower body muscles. Supervision at 0, 4, 8, and 12 weeks |
|
Schachter 2003 AE2: long bout |
3 to 5/wk | 16 weeks | 40%‐50% HRR at week 1, 60%‐70% HRR by week 10 ACSM: moderate at week 1, vigorous by weeks 10‐16 |
10' up to 30' | Home program of low‐impact aerobics to videotaped instructor and music, rhythmical movements of lower body muscles. Supervision at 0, 4, 8, and 12 weeks |
| Aerobic vs other (education or stress management training) | |||||
| Fontaine 2007 | Group session every 2 weeks AE: 5‐7 times/wk | 12 weeks | Moderate intensity ACSM: moderate Review authors used appropriate references to help translate "moderate" into action |
10’ and increase daily 5’/wk to at least 30’ | Brisk walking and other modes of aerobic activity (+ group session/supervision) |
| Fontaine 2010 | 5‐7 times/wk | 12 weeks | Moderate (breathing heavily but able to keep a conversation) + 15’ of above usual level ACSM: moderate Review authors used appropriate references to help translate "moderate" into action |
60’ | Walking (the most common form of LPA) and other forms (eg, garden/mowing the lawn); household activity (eg, vacuuming); and sports activity (eg, cycling, swimming, field hockey) (+ group sessions/supervision) |
| King 2002 | 3 times/wk | 12 weeks | 60%‐75% predicted HRmax ACSM: light to moderate |
Starting duration 10 to 15' progressing to 20 to 40' | Supervised walking, aquacise (deep and shallow water), or low‐impact aerobics |
| Sencan 2004 | 3 times/wk | 6 weeks | Not specified | 40’ | Cycle ergometry. Supervision unclear |
| Wigers 1996 | 3 times/wk | 14 weeks | Tempo gradually increased up to, and decreased down from, 4 periods at 60%‐70% HRmax ACSM: light to moderate | 45’ | Supervised movement to music and games |
ACSM: American College of Sports Medicine; AE: aerobic exercise; FITT: frequency, intensity, time, and type of training; HRmax: maximum heart rate; HRR: heart rate reserve; RPE: rating of perceived exertion
5. Congruence with ACSM aerobic criteria for healthy adults.
| Met ACSM criteria | Did not meet ACSM criteria | Not enough information to judge |
| Fontaine 2007; Fontaine 2010; Kayo 2011; Schachter 2003 met ACSM guidelines for healthy adults. Gowans 2001 met ACSM criteria for individuals who are sedentary/have no habitual activity/are extremely deconditioned | King 2002: based on frequency and duration (only 3/wk, light to moderate); Mannerkorpi 2010: based on frequency and duration (only twice or once a week with 20' session duration); Mengshoel 1992: based on frequency of 2 times/wk; Nichols 1994: based on frequency and duration (only twice a week); Ramsay 2000: based on frequency (only once a week); Sanudo 2010: based on frequency (only twice a week) for aerobics; Wigers 1996: intensity too low, duration too short (only 18‐20’ at HR 60%‐70%) | Sencan 2004 |
ACSM: American College of Sports Medicine; HR: heart rate
Aerobic versus control conditions (treatment as usual, wait list control, daily activities including physical activity as usual): Exercise frequency was three times per week in most studies. In Mengshoel 1992 and Sanudo 2010, exercise frequency was two times per week for 20 and 24 weeks, respectively. Duration varied from six weeks (Sencan 2004) to 24 weeks (Sanudo 2010). Investigators expressed intensity five different ways: percentage age‐adjusted heart rate (Gowans 2001), target heart rate (Mengshoel 1992), percentage maximum heart rate (HRmax; Sanudo 2010), predicted maximum heart rate (King 2002; Nichols 1994), and percentage heart rate reserve (HRR; Kayo 2011; Schachter 2003). One study (Sencan 2004) did not specify duration, and another study (Wigers 1996) provided a description involving tempo. Average intervention time was 35 minutes (minimum‐maximum: 20 to 60). The predominant mode of activity was walking (indoor or outdoor), in some cases accompanied by upper body movements or with progression to running; other modes included aerobic exercise on a stationary bicycle, low‐impact aerobics to music, rhythmical movements of lower body muscles, aquacise, and music and games. All interventions were supervised regularly or at specified times (Schachter 2003). We were unable to determine if the intervention was supervised in one study (Sencan 2004).
Aerobic versus aerobic: Investigators performed three sets of comparisons: Nordic walking versus low‐intensity walking (Mannerkorpi 2010); once‐per‐week exercise versus single exercise session and home program (Ramsay 2000); and one long versus two short bouts of aerobic exercise (Schachter 2003). Exercise frequency varied from one time per week to three times per week. One study (Ramsay 2000) did not specify intensity; another (Schachter 2003) expressed intensity in HRR; and another study (Mannerkorpi 2010) provided a rating of perceived exertion (RPE). Among the studies that reported intensity, intensity started light and increased to moderate or vigorous. Average duration of the intervention was 30 minutes. The mode involved supervised (Nordic or low‐intensity) walking in parks and forests with flat areas and small hills, low‐impact aerobics to music, rhythmical movements of lower body muscles, an unspecified home program, cardiovascular fitness classes plus stretching and relaxation, and written advice on aerobic exercises plus stretching and relaxation. Interventions were supervised in five of the six comparisons, and were self‐supervised in another (Ramsay 2000).
Aerobic versus other: We found three distinct sets of comparisons: aerobic exercise versus education (Fontaine 2007; Fontaine 2010; King 2002); aerobic exercise versus stress management training (Wigers 1996); and aerobic exercise versus medication (eg, paroxetine; Sencan 2004). Two trials reported frequency of exercise as five to seven times per week, and the other three reported exercise three times per week. Intensity was set at "moderate" (breathing heavily but able to keep a conversation), was reported as 60% to 75% predicted heart rate or with a tempo gradually increased up to, and decreased down from, four periods of high‐intensity training at 60% to 70% HRmax, and was not specified in one study (Sencan 2004). Average duration was 30 minutes. The aerobic mode involved walking (the most common form of leisure time physical activity) and other forms of movement; and sports activity (eg, cycling, swimming, field hockey), aquacise, low‐impact aerobics, and movement to music and games.
Excluded studies
We excluded 2529 records on citation and abstract screening, as they did not meet the inclusion criteria for this review (see Figure 1). We examined 213 full‐text articles and 20 RCT protocols, and we excluded 77 full‐text articles and seven RCT protocols. We excluded full‐text articles because they did not meet the selection criteria related to diagnosis of fibromyalgia (n = 9); intervention (n = 16); designated outcomes not measured (n = 2); or randomization (n = 50). The remaining 136 full‐text articles represented RCTs examining effects of physical activity interventions for fibromyalgia. We screened 115 additional articles to rule them out because the physical activity intervention did not have an aerobics‐only intervention; or the study was reviewed or was designated to be reviewed in another Cochrane Review in this series.
Risk of bias in included studies
We have provided results of the "Risk of bias" assessment for the 13 included studies in the Characteristics of included studies section and in Figure 2 and Figure 3. "Risk of bias" assessments were based on primary article data supplemented by study author responses.
2.
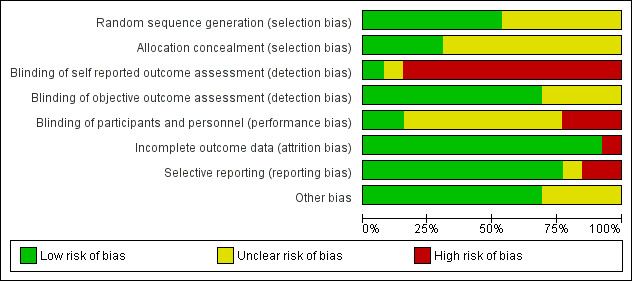
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
3.
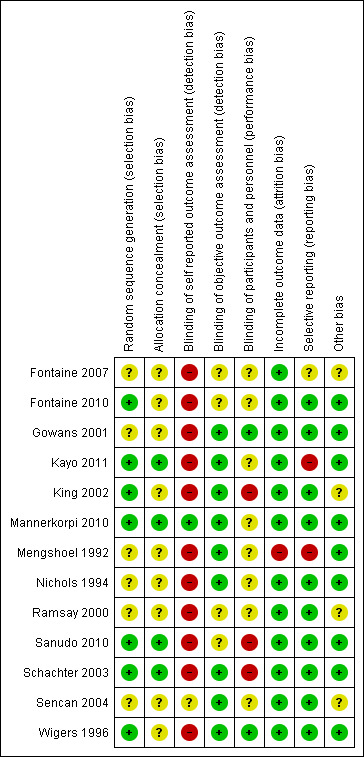
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Allocation
Seven of the 13 studies used an acceptable method of random sequence generation (computer‐generated sequence, coin toss, drawing of cards or lots), and we rated them as low risk (Fontaine 2010; Kayo 2011; King 2002; Mannerkorpi 2010; Sanudo 2010; Schachter 2003; Wigers 1996). Six studies used allocation methods that were unclear (Fontaine 2007; Gowans 2001; Mengshoel 1992; Nichols 1994; Ramsay 2000; Sencan 2004).
We rated four studies as low risk because they utilized acceptable methods to conceal the allocation sequence, such as central allocation by telephone, Web‐based or pharmacy‐controlled randomization, or sequentially numbered opaque sealed envelopes (Kayo 2011; Mannerkorpi 2010; Sanudo 2010; Schachter 2003). We rated as presenting unclear risk nine studies that did not present sufficient information to allow definitive judgment (Fontaine 2007; Fontaine 2010; Gowans 2001; King 2002; Mengshoel 1992; Nichols 1994; Ramsay 2000; Sencan 2004; Wigers 1996).
Blinding
In exercise studies, blinding of participants and care providers from treatment allocation is very rare.
Performance bias
Among the included studies, we rated blinding of participants and personnel (performance bias) as low risk for two studies (Gowans 2001; Wigers 1996), unclear risk for eight studies (Fontaine 2007; Fontaine 2010; Mannerkorpi 2010; Mengshoel 1992; Nichols 1994; Ramsay 2000; Sanudo 2010; Sencan 2004), and high risk for three studies (King 2002; Sanudo 2010; Schachter 2003).
Detection bias
For detection bias, we separated assessment of blinded assessors for subjective and objective outcomes. Not all trials used a combination of both kinds of outcomes. While completing the "Risk of bias" tool, we were unable to insert "not applicable" or to leave the section blank (indicating that the outcome was not measured). We then chose "low risk" and inserted the comment "not applicable/this outcome was not measured." For self‐reported outcomes (subjective), we rated 11 studies as high risk (Fontaine 2007; Fontaine 2010; Gowans 2001; Kayo 2011; King 2002; Mengshoel 1992; Nichols 1994; Ramsay 2000; Sanudo 2010; Schachter 2003; Wigers 1996); one study as low risk, as both interventions were considered equal (Mannerkorpi 2010); and one study using a placebo control as unclear risk (Sencan 2004), as we could not determine whether participants were aware of the intervention. For objective reported outcomes, nine studies blinded outcome assessors to participant group assignment, and we rated these studies as low risk (Gowans 2001; Kayo 2011; King 2002; Mannerkorpi 2010; Mengshoel 1992; Nichols 1994; Schachter 2003; Sencan 2004; Wigers 1996). We rated four studies as unclear risk (Fontaine 2007Fontaine 2010; Ramsay 2000; Sanudo 2010).
Incomplete outcome data
Twelve studies reported complete outcome data. Gowans 2001; Kayo 2011; Ramsay 2000; Sanudo 2010; Schachter 2003; and Wigers 1996 analyzed data using ITT. King 2002 reported post‐test data and analyzed them using ITT; at follow‐up, investigators provided only complete data with no analysis. Missing outcome data were balanced in numbers across intervention groups, with similar reasons for missing data reported across groups in Fontaine 2007; Mannerkorpi 2010; and Nichols 1994. Missing outcome data were balanced in numbers across intervention groups, and reasons for missing outcome data were unlikely to be related to true outcomes in Fontaine 2010. Sencan 2004 reported no missing data at post‐test. Mengshoel 1992 provided incomplete income data, and we rated this study as high risk.
Selective reporting
A priori RCTs protocols were available for three of the reviewed studies (Fontaine 2010, ClinicalTrials.gov NCT00383084; Kayo 2011, ClinicalTrials.gov ID NCT00498264; Mannerkorpi 2010, ClinicalTrials.gov ID NCT00643006). We rated 10 of the 13 studies as having low risk of selective reporting bias. These included two studies with an a priori RCT protocol (Fontaine 2010; Mannerkorpi 2010). In eight published reports, although RCT protocols were not available, it was clear that published reports included all expected outcomes (Gowans 2001; King 2002; Nichols 1994; Ramsay 2000; Sanudo 2010; Schachter 2003; Sencan 2004; Wigers 1996). We rated one study as having high risk of selective reporting. Kayo 2011 did not provide in the article outcome data for some key variables such as tender points, SF‐36 physical functioning, SF‐36 vitality, and SF‐36 mental health that would be expected. We rated two out of 13 studies as having unclear risk (Fontaine 2007; Mengshoel 1992). Overall, we rated risk of selective reporting bias as low (77%; Figure 2).
Other potential sources of bias
Overall, we rated risk due to other sources of bias as low (70%; Figure 2). We rated four studies as having unclear risk because information was insufficient for assessment of whether an important risk of bias existed (Fontaine 2007; King 2002; Ramsay 2000; Sencan 2004).
Poor adherence is another potential source of bias in exercise studies. None of the included studies reported detailed results of systematic data collection and analysis of participant adherence to exercise performance in a way that would allow the review authors to understand the volume of exercise training actually performed by participants.
Effects of interventions
See: Table 1
See Table 1 for the main comparison ‐ aerobic exercise training compared with control conditions (treatment as usual, wait list control, daily activities including physical activity as usual). We have grouped results related to effects of interventions from the meta‐analysis to correspond to comparisons and objectives of the review. See below.
Aerobics versus control at the end of the intervention
Major outcomes
Five studies provided data for health‐related quality of life (Gowans 2001; Kayo 2011; King 2002; Sanudo 2010; Schachter 2003), six studies for pain intensity (Gowans 2001; Mengshoel 1992; Sanudo 2010; Schachter 2003; Sencan 2004; Wigers 1996), four for fatigue (Kayo 2011; Sanudo 2010; Schachter 2003; Wigers 1996) and physical function (Kayo 2011; Nichols 1994; Sanudo 2010; Schachter 2003), and one for the major outcome of stiffness (Schachter 2003). For this comparison, one study (Schachter 2003) included two aerobic exercise arms; the arms were aggregated for analyses and were compared with control conditions.
HRQL (self‐reported, FIQ Total, lower scores mean better health, negative numbers mean improvement)
Researchers in five studies (Gowans 2001; Kayo 2011; King 2002; Sanudo 2010; Schachter 2003) provided evidence of effect post intervention for aerobic exercise training compared with control (N = 372; mean difference (MD) ‐7.89, 95% confidence interval (CI) ‐13.23 to ‐2.55; Analysis 1.1). Absolute change was 8% (3% to 13%) and relative improvement with exercise was 15% (95% CI 5% to 24%); the number needed to treat for an additional beneficial outcome (NNTB) was 6 (4 to 16).
1.1. Analysis.
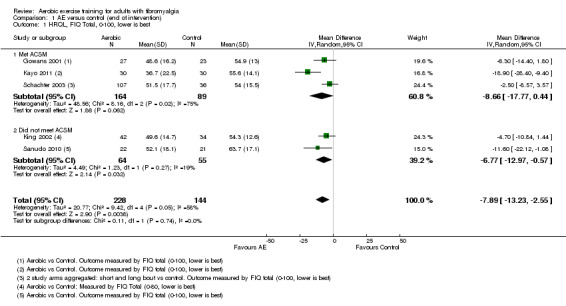
Comparison 1 AE versus control (end of intervention), Outcome 1 HRQL, FIQ Total, 0‐100, lower is best.
Pain intensity (self‐reported, 0 to 100 VAS scale, lower scores mean less pain, negative numbers mean improvement)
Data from six studies (Kayo 2011; Mengshoel 1992; Sanudo 2010; Schachter 2003; Sencan 2004; Wigers 1996) revealed a difference between aerobic exercise training and control favoring aerobic training post intervention (N = 351; MD ‐11.06, 95% CI ‐18.34 to ‐3.77; Analysis 1.3). Absolute change was 11% (4% to 18%) and relative change was 18% (95% CI 7% to 30%); the NNTB was 4 (2 to 15).
1.3. Analysis.
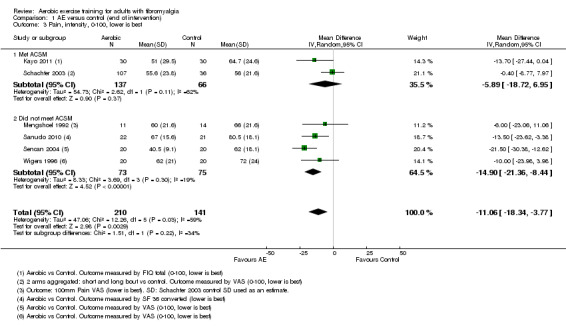
Comparison 1 AE versus control (end of intervention), Outcome 3 Pain, intensity, 0‐100, lower is best.
Fatigue (self‐reported, 0 to 100 scale, lower scores mean less fatigue, negative numbers mean improvement)
Data on fatigue were available for five studies (Kayo 2011; Mengshoel 1992; Sanudo 2010; Schachter 2003; Wigers 1996). Data on fatigue provided by Mengshoel 1992 were available only in ordinal format and were not included in the meta‐analysis; Mengshoel 1992 found no difference in fatigue between aerobic exercise and control when performing non‐parametric analysis. The meta‐analysis presented evidence of no statistically significant effect for aerobic exercise training compared with control post intervention (N = 286; MD ‐6.06, 95% CI ‐12.41 to 0.30; Analysis 1.6). Absolute difference was 6% improvement (12% improvement to 0.3% worse). Relative change was 8% (95% CI 16% improvement to 0.4%worse); the NNTB was not applicable.
1.6. Analysis.
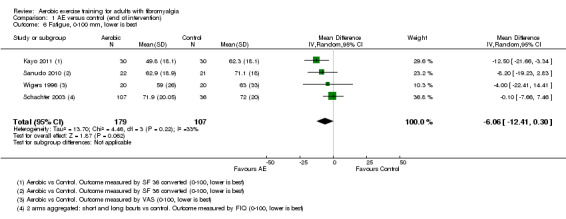
Comparison 1 AE versus control (end of intervention), Outcome 6 Fatigue, 0‐100 mm, lower is best.
Stiffness (self‐reported, 0 to 100 FIQ scale, lower scores mean less stiffness, negative numbers mean improvement)
Only one study provided data on stiffness (Schachter 2003), showing evidence of an effect of aerobic exercise training (two arms) compared with control post intervention (N = 143; MD ‐7.96, 95% CI ‐14.95 to ‐0.97; Analysis 1.7). Absolute difference shows 8% (1% to 15%) improvement. Relative change was 11% (95% CI 1% to 21%); the NNTB was 6 (3 to 218).
1.7. Analysis.
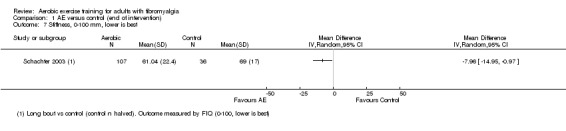
Comparison 1 AE versus control (end of intervention), Outcome 7 Stiffness, 0‐100 mm, lower is best.
Physical function (self‐reported, 0 to 100 FIQ impairment scale, lower scores means fewer limitations, negative numbers mean improvement)
Four trials assessed physical function as an outcome (Kayo 2011; Nichols 1994; Sanudo 2010; Schachter 2003). Assessment of statistical heterogeneity among trials indicated I2 = 69% (ie, from 50% to 90% as may represent "substantial" heterogeneity). After we performed a sensitivity analysis and removed Nichols 1994, I2 was decreased to 0%. Evidence showed an effect of aerobic exercise training compared with control post intervention (N = 246; MD ‐10.16, 95% CI ‐15.39 to ‐4.94; Analysis 1.8). Absolute change was 10% (15% to 5%) improvement. Relative change was 21.9% (95% CI ‐33.2% to 10.7%); the NNTB was 5 (3 to 13).
1.8. Analysis.
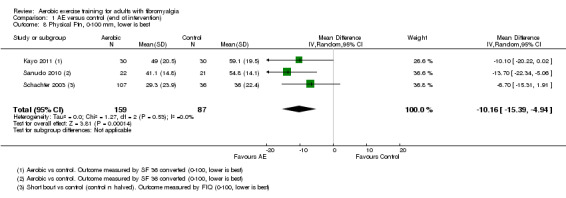
Comparison 1 AE versus control (end of intervention), Outcome 8 Physical Ftn, 0‐100 mm, lower is best.
Adverse events
Most studies did not measure adverse events, and other studies reported them incompletely; thus we are uncertain of the estimate.
The following statements show some of the adverse events that occurred after aerobic exercise training.
"...unable to exercise after an injury" (Sanudo 2010; page 1840), but it is unclear whether the injury was related to participation in the intervention.
"One participant assigned to the short bout exercise withdrew after developing a metatarsal stress fracture" (Schachter 2003; page 347).
One study author surmised that aerobic exercise is safe for individuals with fibromyalgia, as follows: "the present study findings confirm earlier studies that have shown aerobic exercise to reduce tender point tenderness, increase work capacity without adverse side effects..." (Wigers 1996; page 83 to 84).
All‐cause withdrawal rates for aerobic exercise training groups (n1/N1) versus control groups (n2/N2) were 12/27 versus 8/24 (Gowans 2001); 5/30 versus 5/30 (Kayo 2011); 4/46 versus 5/39 (King 2002); 7/18 versus 3/17 (Mengshoel 1992); 2/12 versus 3/12 (Nichols 1994); 4/22 versus 1/21 (Sanudo 2010); 21/56 versus 5/18 (Schachter 2003); 15/51 versus 5/18 (Schachter 2003); 0/20 and 0/20 (Sencan 2004) (not included in the analysis); and 4/20 versus 3/20 (Wigers 1996). We found no significant difference in all‐cause withdrawal between aerobic exercise and control groups (risk ratio (RR) 1.25, 95% CI 0.89 to 1.77; Analysis 1.9). Reasons for participant withdrawals are footnoted in the meta‐analysis (Analysis 1.9).
1.9. Analysis.
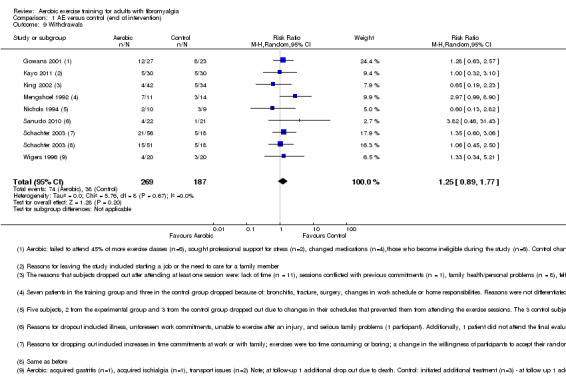
Comparison 1 AE versus control (end of intervention), Outcome 9 Withdrawals.
Minor outcomes
Four studies (Gowans 2001; King 2002; Mengshoel 1992; Sanudo 2010) evaluated effects of aerobic training on the minor outcome of submaximal cardiorespiratory function. Two studies (Schachter 2003; Wigers 1996) evaluated maximal cardiorespiratory function.
CR max (oxygen uptake)
Two arms of the same study presented data on this outcome (Schachter 2003). Results showed no differences between groups in cardiorespiratory function post intervention (N = 143; MD 1.60, 95% CI ‐0.06 to 3.26; Analysis 1.10).
1.10. Analysis.
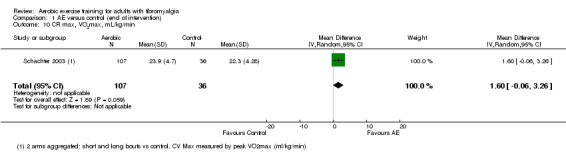
Comparison 1 AE versus control (end of intervention), Outcome 10 CR max, VO2max, mL/kg/min.
CR submax (six‐minute walk test (m))
We found a statistically significant difference in submaximal cardiorespiratory function favoring the aerobic exercise training intervention post intervention (N = 169; MD 55.58 metres, 95% CI 27.20 to 83.96; Analysis 1.11)..
1.11. Analysis.
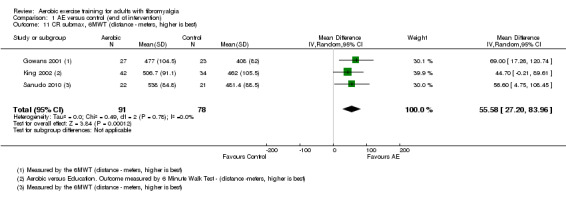
Comparison 1 AE versus control (end of intervention), Outcome 11 CR submax, 6MWT (distance ‐ meters, higher is best).
We did not include Mengshoel 1992 in the meta‐analysis; unlike the other three studies that measured CR submax, Mengshoel 1992 used an Astrand steady state cycle ergometry test to obtain heart rate (HR) at steady state and did not provide standard deviation (SD) values. Mengshoel 1992 found no difference in CR submax between aerobic exercise and control groups using non‐parametric analysis.
Improvement in pain greater than 30%
No studies reported data on this outcome.
Clincal significance
Two major outcomes met the threshold for clinically relevant differences (15%) in this comparison as follows: pain intensity (15%) and physical function (22%).
Aerobics versus control, subgroup analyses
We planned to carry out a subgroup analysis of the relative effects of age (≤ 45 years of age and > 45 years of age); we did not do this because of the proximity of mean age to the set cut‐off of 45 years. This proximity would have prevented us from seeing meaningful differences.
Subgroup analysis investigating effects of the intervention for studies meeting ACSM criteria for HRQL versus studies not meeting ACSM criteria for HRQL and pain intensity (Analysis 1.1; Analysis 1.3) showed no statistically significant differences (P > 0.05). We report these analyses as follows.
HRQL: studies that met ACSM (MD ‐8.66, 95% CI ‐17.77 to 0.44); those that did not meet ACSM (MD ‐6.77, 95% CI ‐12.97 to ‐0.57); test for subgroup differences: Chi² = 0.11, df = 1 (P = 0.74).
Pain intensity: studies that met ACSM (MD ‐5.89, 95% CI ‐18.79 to 6.95); those that did not meet ACSM (MD ‐14.90, 95% ‐21.36 to ‐8.44); test for subgroup differences: Chi² = 1.51, df = 1 (P = 0.22).
Aerobics versus control, sensitivity analyses
We explored effects of selection biases for HRQL and pain intensity outcomes and attrition biases for pain intensity. We did not find attrition rates greater than 20% for HRQL; therefore, we did not conduct this sensitivity analysis as planned. Results of sensitivity analysis for HRQL (selection bias) showed no major impact on the direction and magnitude of estimates when we removed studies with high or unclear risk from the meta‐analyses. We have presented results in Table 7 and Analysis 1.2. Results of sensitivity analysis for pain intensity (selection bias) changed the effect size to a non‐significant result; this can potentially be interpreted as the influence of primary studies with high or unclear risks of bias on the direction and magnitude of estimates. We have presented these results in Table 7 and in Analysis 1.4 and Analysis 1.5. Pain intensity attrition bias sensitivity analysis effect estimates remained the same. However, these analyses must be interpreted with caution, as the number of studies included is small, and the analyses are exploratory in nature. It is possible that a risk may exist, but presently we do not know how much it might affects study results.
6. Sensitivity analyses: aerobics versus control.
| Outcome |
All studies MD (95% CI), number of studies (participants), I2 |
Low risk of selection bias MD (95% CI), number of studies (participants), I2 |
Low risk of attrition bias MD (95% CI), number of studies (participants), I2 |
Detection bias |
| HRQL | ‐7.89 (‐13.23 to ‐2.55), 5 studies (372), I2= 58% | ‐10.47 (‐20.79 to ‐0.15), 3 studies (246), I2 = 77% | > 20% was not present ‐ this sensitivity analysis was not conducted | Sensitivity analysis not conducted |
| Pain | ‐11.06 (‐18.34 to ‐3.77), 6 studies (351), I2= 59% | ‐8.38 (‐17.88 to 1.12), 3 studies (246), I2 = 59% | ‐11.71 (‐19.93 to ‐3.50), 5 studies (326), I2 = 66% | Sensitivity analysis not conducted |
CI: confidence interval; HRQL: health‐related quality of life; MD: mean difference
1.2. Analysis.
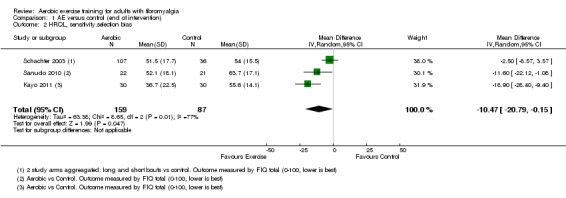
Comparison 1 AE versus control (end of intervention), Outcome 2 HRQL, sensitivity.selection bias.
1.4. Analysis.
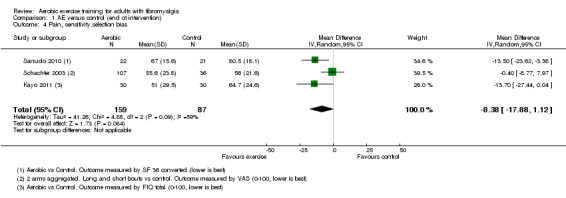
Comparison 1 AE versus control (end of intervention), Outcome 4 Pain, sensitivity.selection bias.
1.5. Analysis.
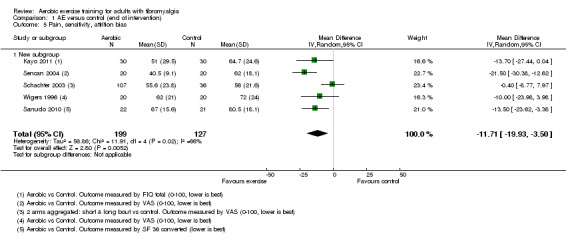
Comparison 1 AE versus control (end of intervention), Outcome 5 Pain, sensitivity, attrition bias.
We did not conduct sensitivity analysis for HRQL and pain intensity for detection bias as all of these outcomes were evaluated with self‐report instruments; therefore we deemed risk of bias to be high.
Aerobics versus control, long‐term effects
Four studies examined long‐term effects: Wigers 1996 (follow‐up at four years after the end of the 14‐week intervention), King 2002 (follow‐up at 24 weeks, 12 weeks after the end of the 16‐week intervention), Sencan 2004 (follow‐up at 26 weeks, 20 weeks after the end of the six‐week intervention), and Kayo 2011 (follow‐up at 28 weeks, 12 weeks after the end of the 16‐week intervention).
Major outcomes
HRQL (self‐reported, 0 to 100 FIQ Total scale, lower scores mean better health, negative numbers mean improvement)
Two studies examined the long‐term effects of aerobic exercise on HRQL: Kayo 2011 found a statistically significant effect favoring aerobic exercise (N = 60; MD ‐19.16, 95% CI ‐29.7 to ‐8.62; Analysis 2.1), whereas King 2002 found no statistically significant difference (MD ‐4.00, 95% CI ‐11.86 to 3.86).
2.1. Analysis.
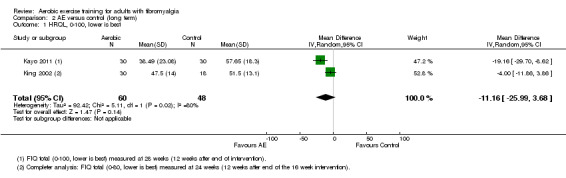
Comparison 2 AE versus control (long term), Outcome 1 HRQL, 0‐100, lower is best.
Pain intensity (self‐reported, 0 to 100 mm VAS scale, lower scores mean less pain, negative numbers mean improvement)
Three studies examined long‐term effects of aerobic exercise on pain intensity (Kayo 2011; Sencan 2004; Wigers 1996) and found a statistically significant effect for the aerobic intervention at post‐test follow‐up (N = 134; MD ‐10.56, 95% CI ‐20.00 to ‐1.12; Analysis 2.2).
2.2. Analysis.

Comparison 2 AE versus control (long term), Outcome 2 Pain intensity, 0‐100, lower is best.
Fatigue (self‐reported, 0 to 100 mm VAS scale, lower scores mean less fatigue, negative numbers mean improvement)
Two studies examined the long‐term effects of aerobic exercise on fatigue (Kayo 2011; Wigers 1996). Kayo 2011 found a statistically significant effect favoring aerobic exercise (N = 60; MD ‐14.00, 95% CI ‐24.34 to ‐3.81; Analysis 2.3), whereas Wigers 1996 found no significant differences (N = 40; MD 5.00, 95% CI ‐12.69 to 22.69).
2.3. Analysis.
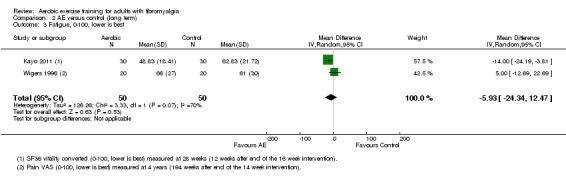
Comparison 2 AE versus control (long term), Outcome 3 Fatigue, 0‐100, lower is best.
Physical function (self‐reported, 0 to 100 FIQ impairment scale, lower scores mean fewer limitations, negative numbers mean improvement)
One study examined the long‐term effects of aerobic exercise on physical function (Kayo 2011) and found a statistically significant effect favoring aerobic exercise (N = 60; MD ‐11.33, 95% CI ‐22.11 to ‐0.55; Analysis 2.4).
2.4. Analysis.
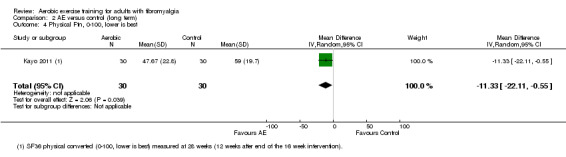
Comparison 2 AE versus control (long term), Outcome 4 Physical Ftn, 0‐100, lower is best.
All‐cause withdrawal
Three studies provided sufficient data for evaluation of differences in all‐cause withdrawal: Kayo 2011; King 2002; and Wigers 1996. We excluded Sencan 2004 from the analysis because the sample size of the control group at follow‐up was not provided. By follow‐up, 22 of 70 had withdrawn from the aerobics groups compared with 25 of 70 in the control groups. Researchers found no significant differences in the proportion of participants who had withdrawn at follow‐up (N = 140; RR 0.75, 95% CI 0.47 to 1.22; Analysis 2.5).
2.5. Analysis.
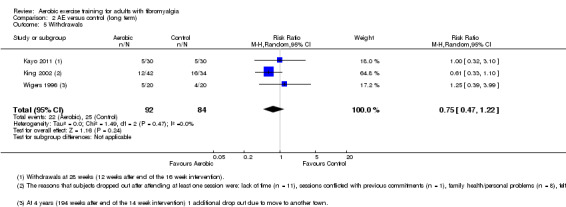
Comparison 2 AE versus control (long term), Outcome 5 Withdrawals.
Stiffness and adverse events
No studies reported data on these outcomes.
Minor outcomes
CR max (work capacity (w))
One study examined the long‐term effects of aerobic exercise on CR max (Wigers 1996) and found no evidence of an effect at four years (208 weeks) between aerobic and control groups (Analysis 2.6).
2.6. Analysis.
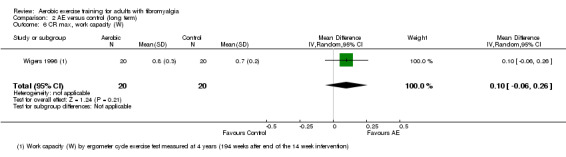
Comparison 2 AE versus control (long term), Outcome 6 CR max, work capacity (W).
CR submax (six‐minute walk test (m))
One study examined the long‐term effects of aerobic exercise on CR submax (King 2002) and found no evidence of an effect at two years (24 weeks) between aerobic and control groups (Analysis 2.7).
2.7. Analysis.
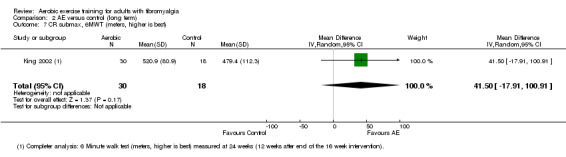
Comparison 2 AE versus control (long term), Outcome 7 CR submax, 6MWT (meters, higher is best).
Improvement in pain greater than 30%
No studies reported data on this outcome.
Aerobics versus aerobics at the end of the intervention
We did not pool studies, as these interventions (ie, population and mode) were not considered comparable across trials. Three studies provided data for this comparison: Mannerkorpi 2010 compared Nordic walking versus low‐intensity aerobic training; Ramsay 2000 compared supervised versus unsupervised aerobic exercise; and Schachter 2003 compared two short bouts versus one long bout of aerobic exercise per day. Results from these studies show the effect sizes found for each of the reported outcomes. Unless otherwise indicated, researchers measured HRQL, pain, fatigue, stiffness, and physical function on a 0 to 100 scale; lower scores are best, and negative numbers mean improvement.
Mannerkorpi 2010, which compared 15‐week Nordic walking (n = 28) versus low‐intensity aerobic training (n = 27), found evidence of no effect on HRQL (FIQ Total, scale 0 to 100; N = 55; MD ‐7.30, 95% CI ‐18.90 to 4.30; Analysis 3.1), pain intensity (100‐mm VAS; N = 57; MD ‐4.70, 95% CI ‐17.42 to 8.02; Analysis 3.2), fatigue (Multidimensional Fatigue Inventory, scale 4 to 20; N = 55; MD ‐0.33, 95% CI ‐0.87 to 0.20; Analysis 3.3), physical function (FIQ impairment scale, scale 0 to 100; MD ‐6.00, 95% CI ‐18.77 to 6.77; Analysis 3.5 ), all‐cause withdrawals (RR 1.21, 95% CI 0.36 to 4.13; Analysis 3.6), and CR submax (six‐minute walk test in meters; N = 55; MD 28.80, 95% CI ‐3.89 to 61.49). Regarding adverse effects, Mannerkorpi 2010 observed that "a temporary increase of pain was reported by several patients at exercise sessions, not only participants in the Nordic walking group but also participants in the low intensity walking group"; however, one participant in the Nordic walking group had increased pain and dropped out, and "only one patient interrupted the exercise program due to adverse effects of exercise. She had chronic trochanteritis, which deteriorated after a few exercise sessions" (page 8 of 10).
3.1. Analysis.
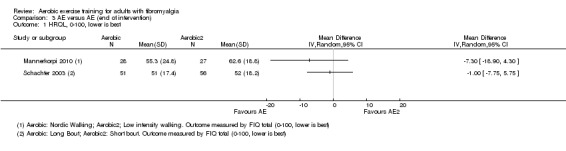
Comparison 3 AE versus AE (end of intervention), Outcome 1 HRQL, 0‐100, lower is best.
3.2. Analysis.
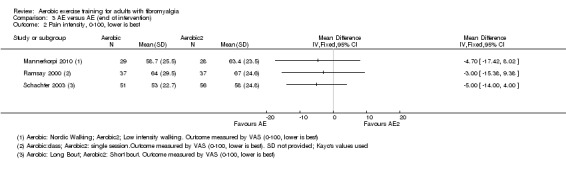
Comparison 3 AE versus AE (end of intervention), Outcome 2 Pain intensity, 0‐100, lower is best.
3.3. Analysis.
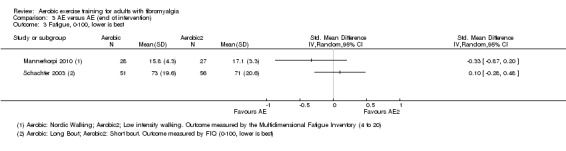
Comparison 3 AE versus AE (end of intervention), Outcome 3 Fatigue, 0‐100, lower is best.
3.5. Analysis.
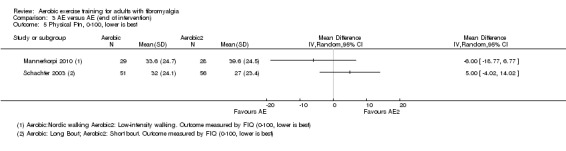
Comparison 3 AE versus AE (end of intervention), Outcome 5 Physical Ftn, 0‐100, lower is best.
3.6. Analysis.
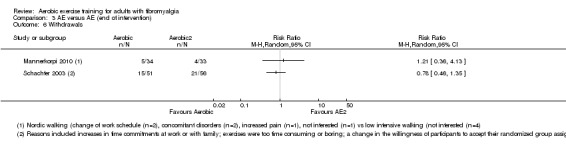
Comparison 3 AE versus AE (end of intervention), Outcome 6 Withdrawals.
Ramsay 2000 compared participants undertaking supervised aerobic exercise (N = 37) versus participants attending a single exercise class with instructions to continue with a home program (N = 37). At 12 weeks, Ramsay 2000 found evidence of no effect on pain intensity (100‐mm VAS; N = 74; MD ‐3.00, 95% CI ‐15.38 to 9.38; Analysis 3.2). Ramsay 2000 did not clearly specify drop‐outs from the study; therefore, we were not able to pool the data. Ramsay 2000 reported no adverse events but measured physical function with a modified HAQ and presented data in medians and 25th and 75th percentiles. The HAQ is a 20‐item instrument with total scores ranging from 0 to 3 (with high scores denoting poorer function). Because no other trial in this review used the HAQ, we were not able to impute standard deviations for this trial. Using non‐parametric tests, Ramsay 2000 found no significant differences in HAQ scores between the two groups.
Schachter 2003, which compared 16‐week programs of one long bout per day (N = 51) versus two short bouts per day (N = 56) of low‐impact aerobics intensity, found no statistically significant between‐group differences in HRQL (FIQ Total, scale 0 to 100; N = 107; MD ‐1.00, 95% CI ‐7.75 to 5.75; Analysis 3.1), pain intensity (100‐mm VAS; N = 107; MD ‐5.00, 95% CI ‐14.00 to 4.00; Analysis 3.2), fatigue (FIQ fatigue, scale 0 to 100; N = 107; MD 0.10, 95% CI ‐0.28 to 0.48; Analysis 3.3), stiffness (FIQ stiffness, scale 0 to 100; N = 107; MD ‐2.00, 95% CI ‐10.53 to 6.53; Analysis 3.4), physical function (FIQ impairment scale, scale 0 to 100; N = 107; MD 5.00, 95% CI ‐4.02 to 14.02; Analysis 3.5), all‐cause withdrawals (N = 107; RR 0.78, 95% CI 0.46 to 1.35; Analysis 3.6), or CR max (VO2max, mL/kg; N = 107; MD 0.70, 95% CI ‐1.23 to 2.63; Analysis 3.7). Regarding adverse events, Schachter noted: "One participant assigned to the short bout exercise withdrew after developing a metatarsal stress fracture" (page 347).
3.4. Analysis.
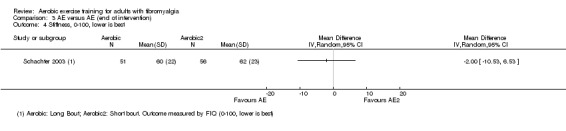
Comparison 3 AE versus AE (end of intervention), Outcome 4 Stiffness, 0‐100, lower is best.
3.7. Analysis.
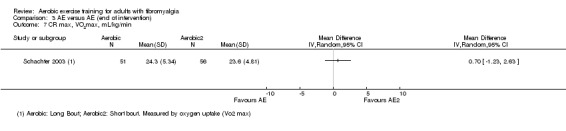
Comparison 3 AE versus AE (end of intervention), Outcome 7 CR max, VO2max, mL/kg/min.
No studies comparing two aerobic interventions provided data on Improvement in pain greater than 30%.
Aerobics versus other non‐exercise interventions at the end of the intervention
We did not pool studies, as we did not consider interventions and comparators comparable across trials. Five studies (six publications) provided data for this comparison (Fontaine 2007; Fontaine 2010; King 2002; Sencan 2004; Wigers 1996). Fontaine 2007; Fontaine 2010; and King 2002 compared aerobic exercise versus education, Wigers 1996 compared aerobic exercise versus stress management training, and Sencan 2004 compared aerobic exercise versus medication (ie, paroxetine). Our analyses show effect size on major and minor outcome variables for each of the included studies. Unless otherwise indicated, investigators measured HRQL, pain, and fatigue on a 0 to 100 scale, lower scores are best, and negative numbers mean improvement.
Fontaine 2007, which compared a 12‐week program of aerobic exercise (called "leisure time physical activity"; n = 22) versus education (n = 26), found evidence of no effect on HRQL (FIQ Total, scale 0 to 100; N = 33; MD ‐8.90, 95% CI ‐24.07 to 6.2; Analysis 4.1), fatigue (Fatigue Severity Scale; N = 32; SMD ‐0.14, 95% CI ‐0.84 to 0.56; Analysis 4.3), all‐cause withdrawal (N = 48; RR 1.03, 95% CI ‐0.45 to 2.40), and CR submax (six‐minute walk test, meters; N = 33; MD ‐4.30, 95% CI ‐99.14 to 90.54; Analysis 4.6). This study found statistically significant results for pain intensity (100‐mm VAS; N = 32; MD ‐15.00, 95% CI ‐29.95 to ‐0.05; Analysis 4.2) and reported no adverse events (ie, injuries, exacerbations, or other) for either group.
4.1. Analysis.
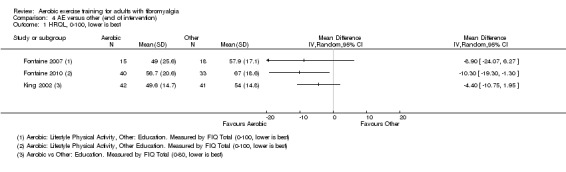
Comparison 4 AE versus other (end of intervention), Outcome 1 HRQL, 0‐100, lower is best.
4.3. Analysis.
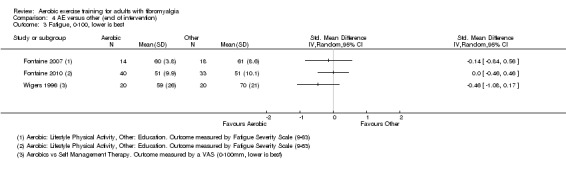
Comparison 4 AE versus other (end of intervention), Outcome 3 Fatigue, 0‐100, lower is best.
4.6. Analysis.
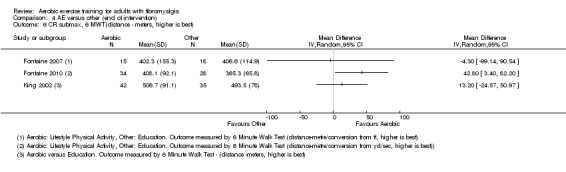
Comparison 4 AE versus other (end of intervention), Outcome 6 CR submax, 6 MWT(distance ‐ meters, higher is best).
4.2. Analysis.

Comparison 4 AE versus other (end of intervention), Outcome 2 Pain intensity, 0‐100, lower is best.
Fontaine 2010, which compared a 12‐week aerobics program (leisure time physical activity) (n = 43) versus education (n = 33), found statistically significant differences post intervention in HRQL (FIQ Total, scale 0 to 100; N = 73; MD ‐10.30, 95% CI ‐19.30 to ‐1.30; Analysis 4.1), pain intensity (100‐mm VAS; N = 73; MD ‐16.10, 95% CI ‐27.33 to ‐4.87; Analysis 4.2), and CR submax (six‐minute walk test, meters; N = 73; MD 42.80, 95% CI 3.40 to 82.20; Analysis 4.5); this study did not report between‐group differences post intervention in fatigue (Fatigue Severity Scale; N = 73; SMD 0.00, 95% CI ‐0.46 to 0.46; Analysis 4.3) or all‐cause withdrawal (N = 73; RR 0.99, 95% CI ‐0.33 to 3.00; Analysis 4.4). Neither group reported adverse events (ie, injuries, exacerbations, or other).
4.5. Analysis.
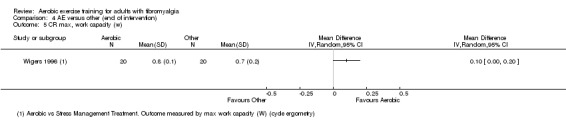
Comparison 4 AE versus other (end of intervention), Outcome 5 CR max, work capacity (w).
4.4. Analysis.
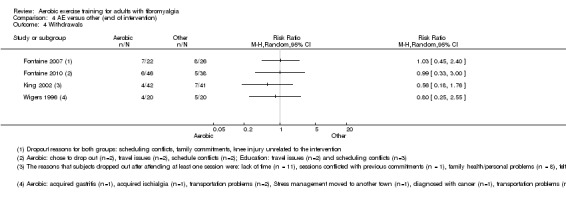
Comparison 4 AE versus other (end of intervention), Outcome 4 Withdrawals.
King 2002 compared a 12‐week aerobic intervention (n = 42) versus education (n = 41) and found evidence of no effects on HRQL (FIQ Total, scale 0 to 80; MD ‐4.40, 95% CI ‐10.75 to 1.95), all‐cause withdrawal (RR ‐0.56, 95% CI ‐0.18 to 1.76), or CR submax (six‐minute walk test, meters; MD 13.20, 95% CI ‐24.57 to 50.97). With regard to adverse events, study authors surmise, "No complications or adverse effects were observed during the study period among patients who completed the treatment protocols" (page 3 of 8).
Wigers 1996 compared a 14‐week aerobics program (n = 16) versus stress management training (n = 17) and noted no between‐group differences in pain intensity (100‐mm VAS; N = 40; MD ‐2.00, 95% CI ‐14.41 to 10.41; Analysis 4.2), fatigue (100‐mm VAS; N = 40; SMD ‐0.46, 95% CI ‐1.08 to 0.17; Analysis 4.3), or all‐cause withdrawal (N = 40; RR ‐0.80, 95% CI ‐0.25 to 2.55; Analysis 4.4) and reported no adverse events (ie, injuries, exacerbations, or other) for either group. Data on CR max post intervention show a statistically significant difference in favor of aerobic exercise training versus stress management therapy (measured by work capacity, watts; N = 40; MD 0.10, 95% CI 0.00 to 0.20; Analysis 4.5).
Sencan 2004 compared six weeks of aerobic exercise (ie, cycling; n = 20) versus medication (ie, paroxetine; n = 20) and found no evidence of effects on pain intensity (N = 40; MD 5.00, 95% CI ‐2.14 to 12.14; Analysis 4.2). Investigators reported no adverse events (ie, injuries, exacerbations, or other) for either group.
Stiffness, physical function, and improvement in pain greater than 30%
No studies reported data on these outcomes.
Discussion
This review is one of a series of reviews examining effects of physical activity interventions for individuals with fibromyalgia; this review focused on aerobic exercise training.
Summary of main results
Thirteen unique studies involving 839 people met our inclusion criteria. Nine studies compared aerobic exercise versus control, three compared one aerobic intervention versus another aerobic intervention, and five compared aerobic exercise versus a non‐exercise intervention.
Aerobics versus control studies: IThe eight trials that compared aerobic exercise training versus control included a total of 456 participants. Investigators reported statistically significant improvement at the end of the intervention (with two outcomes reaching clinical significance) and provided evidence of low to moderate quality favoring aerobic exercise training for health‐related quality of life (HRQL), pain intensity, stiffness, and physical function. Results showed no statistically significant differences in the number of participants who withdrew from exercise groups and control groups, and fatigue and other adverse events were difficult to evaluate because they were not reported in a systematic or standardized manner. A small quantiity of data revealed that those who participated in aerobic interventions had less pain and better physical function at long‐term follow‐up when compared with those in control groups; however, long‐term follow‐up revealed no differences in HRQL.
Aerobics versus aerobics studies: Three studies involving 248 people compared two forms of aerobic exercise. Owing to differences between interventions and comparators, we did not pool the data. One study compared Nordic walking versus low‐intensity walking, another compared aerobic exercise done in two short bouts versus one long bout per day, and a final study compared effects of a once‐per‐week exercise class versus a single exercise session and home program. Results showed no significant differences in major or minor outcomes between any of the interventions provided in these studies.
Aerobics versus other non‐exercise intervention studies: Four studies compared aerobic exercise versus self‐management training and education interventions, and one study compared aerobic exercise versus medication (paroxetine). Owing to differences between interventions and comparators, we did not pool the data. Results showed statistically significant differences favoring the aerobics program for HRQL (one of three trials) and pain intensity (two of four studies). Researchers noted no differences in fatigue nor in all‐cause withdrawals. No studies provided data on stiffness and physical function. Information on the number and quality of adverse events was scarce.
Overall completeness and applicability of evidence
Although additional studies with greater numbers of participants would increase our confidence in these results, and despite the issues mentioned above, it appears that aerobic exercise training can be effective in improving our major fibromyalgia outcomes of health‐related quality of life, pain intensity, stiffness, and physical function. Evidence on long‐term effects (24 to 208 weeks post intervention) shows that benefits for pain and function persisted, but benefits for HRQL or fatigue did not. Withdrawals were similar, and stiffness and adverse events were not measured. It is important to note that aerobic exercise training does not seem to be linked with greater withdrawal from programs. Indeed, results lead us to believe that this is an acceptable intervention for individuals with fibromyalgia. Aerobic exercise is a type of exercise that can be performed without the need for elaborate equipment or facilities; it is therefore an accessible form of exercise for individuals with fibromyalgia. Our limited evidence appears to support aerobic exercise training as part of the management of fibromyalgia. Although the body of literature has grown over the past decade, studies remain insufficient for subgroup analyses or evaluation of dose‐response relationships.
We evaluated exercise interventions against well‐accepted guidelines for improving cardiorespiratory fitness and health that outline frequency, intensity, time, type, and volume, as well as progression of aerobic exercise training (Garber 2011). Only four of 13 studies included interventions that were congruent with American College of Sports Medicine (ACSM) guidelines (Table 6). Interventions that fell short of the guidelines included exercise intensities and frequencies below recommendations and total accumulated durations less than the minimum 150 minutes per week for programs of moderate intensity. Few studies in the subgroup analyses (Analysis 1.1; Analysis 1.3) indicate that the effect of the intervention in studies not meeting ACSM guidelines is similar to effects on HRQL and pain intensity. Further, it does appear that aerobic exercise training programs providing lower training volumes than those recommended by ACSM can improve fibromyalgia symptoms. Nonetheless, ACSM guidelines may serve as a useful guide for individuals with fibromyalgia and for health care providers, as they provide ideas for starting, progressing, and maintaining aerobic exercise training programs associated with cardiorespiratory fitness and other health‐related benefits (eg, lower all‐cause mortality, lower risk of cardiovascular disease mortality and morbidity) (ACSM 2013; Garber 2011).
Included studies were published in Canada, United States, Brazil, Spain, Norway, Sweden, United Kingdom, and Turkey. These may represent only some of the total published papers on aerobic exercise and fibromyalgia. Most interventions reflected supervised group training, hence we do not know what home programs or individualized supervision would do to our quality of evidence levels. Most of our studies included only female participants. Additional studies that focus on interventions for males will indicate whether aerobic exercise training interventions have similar effects for men and women. Therefore, our findings are not easily generalized beyond a middle‐aged, largely Caucasian, female population.
Within the context of current practice, many programs targeting individuals with fibromyalgia are already implementing aerobic exercise training, such as walking or moving to music. Expensive or challenging equipment is not required for aerobic exercise training to be incorporated into practice, yet evidence shows a paucity of research examining these types of interventions.
Quality of the evidence
We extracted the evidence presented in this review from trials published in academic journals, from trial registries, and from information requested of trial authors. Using the GRADE system in rating our evidence for major outcomes, we found evidence of low to moderate quality for benefits in HRQL, pain intensity, fatigue, stiffness, and physical function with aerobic exercise training versus control at the end of treatment. We downgraded this evidence because of potential limitations related to imprecision (ie, total cumulative sample size lower than 400, wide confidence intervals), data based on results of one study, and limitations related to risk of bias. Sample sizes of aerobic exercise intervention groups among the 13 studies ranged from 10 to 56 participants. Although most of the individual studies were underpowered, aerobic exercise training versus control group meta‐analyses were sufficient to reveal differences for most variables. Reporting of adverse events was limited owing to inconsistency and lack of information among these studies, although it remains unclear whether injuries occurred, as the reporting is not explicit. Our analysis identified moderate‐quality evidence showing that withdrawal rates did not differ between aerobic exercise training and controls.
We rated the quality of evidence as low for long‐term benefits of aerobic exercise for pain intensity and all‐cause withdrawal owing to risk of bias (lack of allocation concealment, blinding) and imprecision (wide confidence intervals, small number of participants), and we further downgraded the level to very low for HRQL, fatigue, and physical function owing to considerable heterogeneity in study results, Investigators did not measure stiffness and adverse events (see Table 8).
7. Quality of evidence ‐ GRADE assessment: long‐term effects of AE versus control comparison.
| Quality assessment | Number of participants | Quality | Importance | |||||||
| Number of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other comments | AE only | Control | ||
| HRQL (follow‐up 12 weeks after end of intervention; assessed with 0‐100 scale, lower is best) | ||||||||||
| 2 | Randomized trials | Seriousa | Seriousb | Not serious | Seriousc | 60 | 48 | ⊕⊝⊝⊝ very low | CRITICAL | |
| Pain intensity (follow‐up 12 weeks after end of intervention to 4 years; assessed with 0‐100 scale, lower is best) | ||||||||||
| 3 | Randomized trials | Seriousa | Not serious | Not serious | Seriousc | 64 | 70 | ⊕⊕⊝⊝ low | CRITICAL | |
| Fatigue (follow‐up from 12 weeks after end of intervention to 4 years; assessed with 0‐100 scale, lower is best) | ||||||||||
| 2 | Randomized trials | Seriousa | Seriousb | Not serious | Seriousc | 50 | 50 | ⊕⊝⊝⊝ very low | IMPORTANT | |
| Stiffness: not measured | ||||||||||
| Physical function (follow‐up at 12 weeks after end of intervention; assessed with 0‐100 scale, lower is best) | ||||||||||
| 1 | Randomized trials | Seriousd | Not serious | Not serious | Seriousc | One study | 30 | 30 | ⊕⊝⊝⊝ very low | IMPORTANT |
| All‐cause withdrawal (follow‐up from 12 weeks after end of intervention to 4 years) | ||||||||||
| 3 | Randomized trials | Seriousa | Not serious | Not serious | Seriousc | 22/92 (23.9%) | 25/84 (29.8%) | ⊕⊕⊝⊝ low | IMPORTANT | |
| Adverse events: not reported | ||||||||||
aIssues with allocation, detection, performance, selective reporting, and other biases
bConsiderable heterogeneity in results (I2 = 80%)
cNumber of participants lower than 400 rule of thumb, wide confidence interval
dIssues related to detection bias, performance bias, and selective reporting
AE: aerobic exercise; HRQL: health‐related quality of life
In comparisons of an aerobic intervention versus another, we found evidence of low to very low quality for benefits in HRQL, pain intensity, fatigue, stiffness, physical function, and all‐cause withdrawal. We downgraded the quality of evidence owing to issues with risk of bias (detection, performance, and other risks of bias), imprecision (wide confidence intervals and small numbers of participants), and heterogeneity of interventions (see Table 9).
8. Quality of evidence ‐ GRADE assessment: AE intervention versus another AE intervention.
| Quality assessment | Number of participants | Quality | Importance | |||||||
| Number of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | AE intervention | AE control | ||
| HRQL, 0‐100, lower is best | ||||||||||
| 2 | Randomized trial | Seriousa | Not serious | Not serious | Seriousb | Studies not pooled | 79 | 83 | ⊕⊕⊝⊝ low | CRITICAL |
| Pain intensity, 0‐100, lower is best | ||||||||||
| 3 | Randomized trial | Seriousb | Not serious | Not serious | Seriousc | Studies not pooled | 117 | 121 | ⊕⊕⊝⊝ low | CRITICAL |
| Fatigue, 0‐100, lower is best | ||||||||||
| 2 | Randomized trial | Seriousa | Not serious | Not serious | Seriousb | Studies not pooled | 79 | 83 | ⊕⊕⊝⊝ low | IMPORTANT |
| Stiffness, 0‐100, lower is best | ||||||||||
| 1 | Randomized trial | Seriousa | Not serious | Not serious | Seriousb | One study | 51 | 56 | ⊕⊝⊝⊝ very low | IMPORTANT |
| Physical function, 0‐100, lower is best | ||||||||||
| 2 | Randomized trial | Seriousa | Seriousd | Not serious | Seriousb | 80 | 84 | ⊕⊝⊝⊝ very low | IMPORTANT | |
| All‐cause withdrawals | ||||||||||
| 2 | Randomized trial | Seriousa | Not serious | Not serious | Seriousb | 20/85 (23.5%) | 25/89 (28.1%) | ⊕⊕⊝⊝ low | IMPORTANT | |
| Adverse events: not reported | ||||||||||
aIssues of detection and performance bias
bIssues related to selection, detection, performance, and other risk of bias
cWide confidence intervals, number of participants less than 400 rule of thumb
dInterventions not similar across studies
AE: aerobic exercise; HRQL: health‐related quality of life
In comparisons of an aerobic intervention versus a non‐exercise (other) intervention, the quality of the evidence ranged from low to very low. We downgraded the quality of the evidence because of issues related to risk of bias, very low numbers of trial participants and wide confidence intervals, and inconsistency across comparators (see Table 10).
9. Quality of evidence ‐ GRADE assessment AE intervention versus other (non‐exercise intervention).
| Quality assessment | Number of participants | Quality | Importance | |||||||
| Number of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | AE | Other | ||
| HRQL, 0‐100, lower is best (AE and lifestyle vs education or SMP) | ||||||||||
| 3 | Randomized trial | Seriousa | Not serious | Not serious | Seriousb | 97 | 92 | ⊕⊕⊝⊝ low | CRITICAL | |
| Pain intensity, 0‐100, lower is best (AE only vs education or SMP and AE only vs medication) | ||||||||||
| 4 | Randomized trial | Seriousa | Seriousc | Not serious | Seriousb | 94 | 91 | ⊕⊝⊝⊝ very low | CRITICAL | |
| Fatigue, 0‐100, lower is best (AE and lifestyle vs education or SMP) | ||||||||||
| 3 | Randomized trial | Seriousa | Not serious | Not serious | Seriousb | 74 | 71 | ⊕⊕⊝⊝ low | IMPORTANT | |
| Withdrawals | ||||||||||
| 4 | Randomized trial | Seriousa | Not serious | Not serious | Seriousb | 21/130 (16.2%) | 25/125 (20.0%) | ⊕⊕⊝⊝ low | IMPORTANT | |
| Stiffness and physical function: not measured | ||||||||||
| Adverse events: reported for 1 study: King 2002: "No complications or adverse effects were observed during the study period among patients who completed the treatment protocols" (page 3 of 8) | ||||||||||
AE: aerobic; HRQL: health‐related quality of life; SMP: self‐management program
aIssues related to risk of bias
bLow number of participants (less than 400 rule of thumb) and wide confidence intervals
cComparator not similar across studies
AE: aerobic exercise; HRQL: health‐related quality of life; SMP: self‐management program
However, the robustness of study results remains questionable until we are certain whether participants in these trials were aware of their allocated group (ie, whether they were aware of the intervention to which they were assigned). Until we are certain of this, study results presented may tend to be overestimated. This is particularly true for self‐reported outcomes such as HRQL, pain intensity, fatigue, stiffness, and physical function. Therefore, evidence must be interpreted with caution.
Potential biases in the review process
Despite efforts to reduce the impact of publication bias on this review, the possibility remains that some studies (with positive or negative findings) may not have been identified by the search.
Contacting study authors for additional information enhanced the accuracy of the information reported in most cases, but this may have introduced a "response bias" into the risk of bias assessment.
We had to impute some values for missing data (such as standard deviations).
The small number of trials included in some analyses further reduced the robustness of these findings.
Other bias may have been introduced by limitations such as incomplete description of exercise protocols and inadequate documentation of adherence to exercise prescriptions.
In our review process, we attempted to control for biases in the following ways.
We applied no language restrictions.
We updated searches periodically and utilized multiple databases.
We complemented our searches with handsearching.
We contacted primary authors for clarification and additional information when indicated, although we did not always receive a response. We asked our questions in an open‐ended fashion, so as to avoid leading questions or answers.
By searching clinical trial registries (eg, clinicaltrials.gov), we enhanced the opportunity to identify unpublished trials and selective reporting of outcomes. Publication bias may lead to overestimation of a treatment effect by up to 12%.
Our multidisciplinary team represented a range of expertise (ie, in library science, systematic reviews and methods, critical appraisal, clinical rheumatology, exercise physiology, physiotherapy, kinesiology, and knowledge translation).
We used a standardized procedure to determine selection and inclusion of studies in the review, and review authors were trained in data extraction.
Two members of our multidisciplinary team also presented the perspective of consumers (ie, one team member had fibromyalgia, and another team member had another rheumatic disease).
We used intention‐to‐treat data preferentially.
Agreements and disagreements with other studies or reviews
Over the past 10 years, several reviews have assessed physical activity interventions for fibromyalgia. In light of their relevance to aerobic exercise, we have chosen to comment on five recent publications: Brosseau 2008 (a clinical practice guideline), Garcia‐Hermoso 2014 (a systematic review), Hauser 2010 (a systematic review), Thomas 2010 (a practical review), and Nuesch 2013 (a network meta‐analysis).
Brosseau 2008 provided clinical practice guidelines for aerobic fitness exercises in the management of fibromyalgia and presented evidence on 13 randomized controlled trials (RCTs; we included only four in this review) and three controlled clinical trials evaluating aerobic exercise for fibromyalgia. Brosseau 2008 reviewed trials of aquatics‐based aerobic exercise as well as interventions including mixed types of exercise such as components of muscle strengthening. We excluded these aquatic and mixed interventions from our present review. Brosseau 2008 assessed methodological quality using the Jadad scale and identified six of 16 trials as having high quality and remaining trials as showing low quality. In contrast, we used the Cochrane "Risk of bias" tool to assess methodological quality. In our review, we identified five studies with high risk of performance bias or reporting bias, and we noted low or unclear risks of bias in remaining categories of all studies. Brosseau 2008 identified inconclusive effects of aerobic exercise training alone on symptoms of fibromyalgia including pain and depression. Conversely, Brosseau 2008 identified aerobic exercise training as improving endurance, which in turn greatly improves physical function, even when only low to moderate exercise intensity is achieved. Brosseau 2008 identified challenges in interpreting results due to a diversity of outcome measures and instruments across primary studies. These challenges combined with the diversity of exercise types included in the Brosseau 2008 review prevented pooled analysis. Conversely, in our review, we were able to conduct pooled analyses identifying benefits of aerobic exercise training for health‐related quality of life, pain intensity, fatigue, stiffness, physical function, and submaximal cardiorespiratory function. Overall, both reviews support aerobic exercise training for the management of fibromyalgia.
Hauser 2010 was a systematic review and meta‐analysis that evaluated the efficacy of aerobic exercise in fibromyalgia. Review authors identified 28 RCTs comparing aerobic exercise versus a control, and seven RCTs comparing different types of aerobic exercise. In contrast to our review, these review authors included studies combining aerobics with other physical activities such as muscle strengthening and aquatic‐specific exercise training programs. We included in our review eight studies identified by Hauser 2010. Attrition rates identified by Hauser 2010 for combined aerobic and control groups were higher, at 67%, versus our 27.3% overall withdrawal rate. Further, Hauser 2010 identified that aerobic exercise training groups had lower rates of intervention program completion when compared with control intervention groups (78% vs 83%). Both reviews identified statistically significant reductions in pain intensity post aerobic exercise training, with effect sizes of standardized mean difference (SMD) ‐0.29 (95% confidence interval (CI) ‐0.46 to ‐0.13), specifically among land‐based aerobic exercise groups (Hauser 2010), whereas we have reported a mean difference (MD) of ‐10.39 on a 100‐point scale (SMD ‐0.48, small effect calculated for comparison). Both reviews identified significant reductions in fatigue and health‐related quality of life. Hauser 2010 found that aerobic exercise training programs improved physical fitness, with improvements similar to those noted in our review for submaximal cardiorespiratory function. Hauser 2010 identified a need for standardized outcome measures and standardized reporting of adverse events in future research. This important finding is congruent with our results, showing inconsistent and unspecified reporting of adverse events of exercise for this population.
Thomas 2010 was a practical review that evaluated aerobic exercise for fibromyalgia. This review included 19 primary articles evaluating land‐ or aquatic‐based exercise and comparing aerobic‐only exercise training versus non‐aerobic exercise training. Thomas 2010 identified nine RCTs of land‐based exercise groups compared with non‐exercise groups. We included five of these primary articles in our review. We excluded from our review the additional four primary articles identified in Thomas 2010 because they include strength training in addition to aerobic exercise in the training program. In contrast to our review, Thomas 2010 did not pool results from studies to identify overall benefits and risks of aerobic exercise, but review authors identified mixed outcomes , with some studies reporting significant improvements in pain, physical function, and aerobic capacity, and others reporting no differences. Thomas 2010 identified statistically significant improvements in pain with aerobic‐ and land‐based exercise among one of three primary articles, and lack of improvement in fatigue in another article. By contrast, we identified statistically significant effects on pain and fatigue in our review, although these improvements may not be clinically significant. Three of four primary articles in the Thomas 2010 review found that physical function significantly improved, similar to statistically significant improvements in physical function identified in our review. Three of four primary articles identified by Thomas 2010 evaluated significant improvements in maximal cardiorespiratory function (CR max) or submaximal cardiorespiratory function (CR submax) with aerobic‐ and land‐based exercise. In our review, we identified significant improvements in CR submax. Thomas 2010 identified a need for standard outcome measure reporting, adequately sized research investigations, and reporting of adherence in future studies. Similarly, we determined that future investigations should report adverse events associated with aerobic exercise.
Garcia‐Hermoso 2014 was a systematic review of 13 primary studies published to August 2013 evaluating the effectiveness and structure of exercise programs designed to improve functional capacity in patients with fibromyalgia. This review included four primary studies of aerobic exercise, two of which we included in the current review. We excluded from the current review two additional studies identified by Garcia‐Hermoso 2014 review authors ‐ one because trial used a single group design, and the second because we judged the belly dance intervention to represent mixed exercise (aerobic and resistance training, rather than strictly aerobic training). Both reviews evaluated randomized controlled interventions of aerobic exercise training compared with a control. In contrast to our review, Garcia‐Hermoso 2014 assessed the quality of methods by applying Physiotherapy Evidence Database (PEDro) criteria, rather than the Cochrane "Risk of bias" tool, as was used in our investigation. Our review identified greater diversity of aerobic training program details, with training program length ranging from 6 to 24 weeks, frequency from one to five times per week, duration from 5 to 60 minutes per session, and intensity from light to vigorous, compared with program length of 12 to 24 weeks, frequency of 0.5 to 2 times per week, duration of 45 to 60 minutes per session, and HRmax intensity of 75% to 80% (one study), as identified by Garcia‐Hermoso 2014. Our findings regarding CR submax are generally consistent with those of Garcia‐Hermoso 2014. Authors of the Garcia‐Hermoso 2014 review identified a large effect size for benefits of aerobic exercise training in improving CR submax (SMD 0.85, 95% CI 0.57 to 1.12), but we identified an effect estimate of MD 62.81 m on the six‐minute walk test, with 95% CI of 26.19 to 99.44 (moderate; SMD 0.58, 95% CI 0.27 to 0.89, calculated for comparison). Similar to our review, Garcia‐Hermoso 2014 noted that adverse events are not well reported by most investigators.
Nuesch 2013 conducted a network meta‐analysis (NMA) evaluating pharmacological and non‐pharmacological interventions for adults with fibromyalgia. NMA is a method used to assess the comparative effectiveness of experimental treatments among similar populations that have not been compared directly in a randomized clinical trial. Unlike the meta‐analysis conducted for this review, which summarized the results of trials that evaluated similar interventions, NMA compares results from two or more studies that have one treatment in common. Nuesch included 33 trials of aerobic exercise as one of the non‐pharmacological interventions evaluated. Both reviews found that aerobic exercise training improved pain intensity, although analysis limited to groups of 50 or more patients within the Nuesch 2013 review reduced the degree of identified improvements. Both reviews found that aerobic exercise was associated with improvements in health‐related quality of life. In contrast to the Nuesch 2013 review, we identified significant reductions in fatigue with aerobic exercise for fibromyalgia. Neither our review nor Nuesch 2013 could identify clinically relevant differences of pain intensity or fatigue outcome measures. Consistent with our findings, Nuesch 2013 identified a need for large‐scale studies of high methodological quality to compare interventions of aerobic exercise for this population.
Authors' conclusions
Implications for practice.
During past decades, a growing body of research, including several RCTs, umbrella and systematic reviews, and meta‐analyses, has shown that exercise and physical activity are important in the treatment of individuals with a diagnois of fibromyalgia, as they contribute to the individual's daily life by reducing pain and improving function. Nevertheless, despite growth in the literature, trial sample sizes remain small, and effect sizes are also small, often not reaching clinically meaningful levels.
Accordingly, the findings of this review indicate that aerobic exercise interventions probably improve HRQL and all‐cause withdrawal, and may slightly decrease pain intensity and stiffness, while slightly improving physical function and cardiorespiratory function, among adults with fibromyalgia. These findings support our current knowledge and understanding of the role of aerobics‐only exercise training in the management of fibromyalgia. Although only two major outcomes reached the clinically meaningful 15% improvement level, aerobic exercises seem to be well tolerated and may be integrated into the treatment of adults with fibromyalgia.
Variation in intervention modes was wide and the number of trials was insufficient for calculating effects of different modes on outcomes. Review authors noted poor reporting about the presence or absence of adverse events; however, similar drop‐out rates in treatment and control groups indicate that the risk of adverse events for people receiving aerobic exercise training was low. This review suggests that individuals with fibromyalgia may perform a simple and accessible activity such as walking without exacerbating pain and other symptoms.
Heterogeneity among exercise protocols and inconsistencies in reporting of exercise parameters and outcomes make interpretation of results challenging. Consequently, it is unclear which aerobic exercise protocols (intensity, duration, frequency, mode) will yield optimal results for adults with fibromyalgia. At the same time, the heterogeneity of exercise protocols leads us to speculate that benefits of aerobic exercise training may be achieved through a variety of combinations of intensity, duration, frequency, and mode. In general terms, most interventions in this review were supervised, frequency was three times per week, average duration was 35 minutes, intensity progressed from light to vigorous, and interventions were provided for 15 weeks.
Some data suggest that long‐term improvements in pain intensity and physical function outcomes occur at six months and at four years. Information on participant activities during this period was not available, so we cannot be sure whether the "intervention" alone produced positive outcomes. Indeed, individuals may have adopted a physically active lifestyle (ie, walking 30') at completion of the intervention, and this might have allowed them to maintain the benefits gained.
Emphasis on simple and easy aerobic training interventions such as walking seems acceptable and is well tolerated in this review. It makes sense to encourage promotion of walking ‐ an activity easily accessible and potentially cost free.
Evidence is insufficient to reveal the effectiveness of one aerobic exercise intervention compared with another, or of an aerobic exercise intervention compared with education, stress management training, or medication, for adults with fibromyalgia.
Implications for research.
This review presents several implications for further research. We have used the EPICOT approach to describe implications for future researchers (Brachaniec 2009).
Evidence
We found evidence of low to moderate quality for outcomes of the main comparison group in this review. Although major outcomes were statistically significant, only three of them reached the minimal clinically important difference of 15 points (HRQL, physical function, and pain). Confidence intervals (or precision of results) were likely affected, but smaller sample sizes were included for some outcomes (ie, stiffness, CR max, and CR submax). The small number of studies, clinical heterogeneity, and few participants limited the potential for meta‐analyses on effects of aerobic exercise training compared with other aerobic interventions or other non‐exercise interventions. To determine recommendations on aerobic exercise training for adults with fibromyalgia, researchers should focus on conducting robust (well‐designed and carefully reported) RCTs.
The recent trend toward publication of RCT protocols allowed improved evaluation of selective reporting bias. Accumulation of additional studies with a registered or published RCT protocol will permit better evaluation of publication bias and improved transparency in the overall process. In accordance with the findings of this review, trials should take into account the need to accurately report on randomization procedures and allocation concealment processes.
Some methodological issues pertaining to the body of literature played a role in the current grading of evidence. A common limitation of exercise trials involves blinding of participants and personnel; another limitation is the typical use of participant‐reported outcome measures in this body of literature. Methodological robustness of trials and detailed reporting practices at all steps taken to avoid or minimize bias may contribute to our understanding and evaluation of the quality of evidence in the future.
Population
As fibromyalgia predominantly affects females, it was not surprising to find that more than half of the studies included middle‐aged female participants only. Although this approach provides great advantage in reducing clinical heterogeneity, it limits the generalization of review findings to males with fibromyalgia. Consideration of gender, socioeconomic status, and ethnicity would provide advantages for generalizing findings across geographical areas.
The population should be described and the common binding characteristic of members should be clearly specified in future trials, to avoid misleading readers to believe that this is a sample of the general population rather than a specific subgroup. Little is known about which subgroups benefit more (or less) from aerobic exercise interventions. For instance, we need more specific information on factors such as age, severity of disease, pain level at baseline, and level of physical activity. Furthermore, studies identifying individuals who respond well to exercise (responders) and those who do not respond (non‐responders) are scarce in the current body of literature. Studies show variability in mode of intervention delivery, with some interventions supervised and others performed at home or supervised sporadically.
Information on the lifestyle or physical activity of individuals before, during, or after exercise intervention is insufficient. Information on the baseline level of participation in physical activity was scarce. Inclusion and exclusion criteria provided some evidence that these individuals were sedentary (ie, did not participated in a planned exercise program for six months before the start of the trial). The total number of hours the individual is actively moving may contribute to the presence or absence of conditioning and symptoms. This information will help us understand the long‐term benefits of the intervention. Also, as discussed in the topic presented above, "gap area" refers to time spent engaging in sedentary behavior (eg, sitting, watching television).
Intervention
In comparing findings from this review with current knowledge presented in other reviews, we found evidence to show that future research must document the FITT‐VP (frequency (F), intensity (I), time or duration (T), type or mode (T), total volume (V), and progression (P), with increased training volume) characteristics of exercise interventions more clearly;,this will help us understand and compare the true effects of particular exercise training protocols.
In addition, exercise adherence, another important contributor to the efficacy of exercise, needs further examination. Future studies should document exercise adherence to further our understanding of the dose‐response relationship between exercise and fibromyalgia symptoms.
Provided we can identify a sufficient number of RCTs in the future, further reviews should have a narrower focus to ensure that effective elements of the specific components of aerobic exercise training can be identified.
To increase the robustness of our conclusions on effects of the intervention, information on blinding of participants to their group assignment and/or study hypothesis is of utmost importance. We encourage researchers to report this information in future trials.
Walking was the most popular intervention examined in this review. The effectiveness of this basic form of aerobic exercise training warrants research attention.
Comparators
Studies used a combination of treatment as usual, placebo, attention only, different aerobic exercise training programs, or other interventions for comparison. Using or finding a placebo control group for this area of research is unlikely, and only one study in this review (with three arms) used a placebo control (Sencan 2004).
Comparing an aerobic training intervention versus another meaningful alternative or aerobic training intervention is a common scenario. Multiple modes of aerobic exercise training are available for individuals with fibromyalgia. However, differences in aerobic training modes compared in this review prevented us from taking a methodological standpoint to meta‐analyse the evidence. Similarly, varying levels of aerobic training interventions compared with other non‐exercise interventions resulted in inability to pool the interventions. Evidence would be strengthened by more studies examining each category.
Outcomes
Few studies have described adverse events experienced by participants. In fact, adverse events often were not identified as outcomes but were described in a side note. This information is critical for evaluating the safety and feasibility of interventions in clinical practice and should be reported in a standardized and systematic way. Studies must directly address adverse events, including the number noted (or absence thereof), and should provide a specific description of each adverse event.
Different instruments measuring the same outcome present a methodological challenge for combining them in a meta‐analysis. A wide range of outcome measures reported between trials made the combination and further interpretation of study results challenging. Investigators could facilitate future systematic reviews by paying attention to responsiveness to the instrument selected and its relationship to other outcome measures commonly utilized in this area of research.
Although we found evidence of post‐treatment effects of exercise training, few trials have focused on long‐term effects.
Trials tended to focus more on fibromyalgia symptoms and less on cardiorespiratory outcomes. This finding is similar to that of our previous review, for which the major interest consisted of helping to relieve symptoms associated with the condition. As our knowledge of the benefits of exercise training for symptoms increases, trials can start to focus on general health or cardiorespiratory responses to this type of activity.
In accordance with Cochrane methods and IMMPACT recommendations, we included a 30% reduction in pain intensity for interpreting clinical trial efficacy (Dworkin 2008); no study measured this outcome. As this outcome was incorporated, in keeping with a Cochrane recommendation, researchers may wish to focus on it in the future.
Time
This review presents data identified up to June 2016; updates will be required as new evidence emerges. This review should be updated in three to five years.
What's new
| Date | Event | Description |
|---|---|---|
| 10 April 2017 | New search has been performed | This review is one of a series of reviews about exercise training for adults with fibromyalgia that will replace the "Exercise for treating fibromyalgia syndrome" review first published in 2002 |
History
Review first published: Issue 6, 2017
| Date | Event | Description |
|---|---|---|
| 17 August 2007 | Amended | We made substantive amendments. See differences between protocol and review |
Acknowledgements
We would like to acknowledge the following.
Exercise for Fibromyalgia Cochrane Review Team.
Mary Brachaniec, Janet Gunderson, and Anne Lyddiatt (consumer members of the Exercise for Fibromyalgia Cochrane Review Team) ‐ special thanks for contributing to team discussions, reviewing outcome measures, and drafting and reviewing the plain language summary.
Christoper Ross, Tanis Kershaw, Joell Harris, and Saf Malleck for providing administrative support for the review team.
Beliz Acan, Patricia Mancini, Julia Bidonde, and Nora Chavarria for assisting with translation from Turkish, Portuguese, Spanish, and German studies, which permitted screening inclusion and data extraction (only some studies used in this review).
Dr Kristin Musselman ‐ thanks for her contributions and thoughtful comments after reviewing the final manuscript.
Jan Odgaard‐Jensen for providing statistical support.
Appendices
Appendix 1. MEDLINE (OVID) search strategy
1. Fibromyalgia/
2. fibromyalgi$.tw.
3. fibrositis.tw.
4. or/1‐3
5. exp Exercise/
6. Physical Exertion/
7. Physical Fitness/
8. exp Physical Endurance/
9. exp Sports/
10. Pliability/
11. exertion$.tw.
12. exercis$.tw.
13. sport$.tw.
14. ((physical or motion) adj5 (fitness or therapy or therapies)).tw.
15. (physical$ adj2 endur$).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
16. manipulat$.tw.
17. (skate$ or skating).tw.
18. jog$.tw.
19. swim$.tw.
20. bicycl$.tw.
21. (cycle$ or cycling).tw.
22. walk$.tw.
23. (row or rows or rowing).tw.
24. weight train$.tw.
25. muscle strength$.tw.
26. exp Yoga/
27. yoga.tw.
28. exp Tai Ji/
29. tai chi.tw.
30. ai chi.tw.
31. exp Vibration/
32. vibration.tw.
33. pilates.tw.
34. or/5‐33
35. 4 and 34
Appendix 2. Embase (OVID) search strategy
1. FIBROMYALGIA/
2. fibromyalgi$.tw.
3. fibrositis.tw.
4. or/1‐3
5. exp exercise/
6. fitness/
7. exercise tolerance/
8. exp sport/
9. pliability/
10. exertion$.tw.
11. exercis$.tw.
12. sport$.tw.
13. ((physical or motion) adj5 (fitness or therapy or therapies)).tw.
14. (physical$ adj2 endur$).tw.
15. manipulat$.tw.
16. (skate$ or skating).tw.
17. jog$.tw.
18. swim$.tw.
19. bicycl$.tw.
20. (cycle$ or cycling).tw.
21. walk$.tw.
22. (row or rows or rowing).tw.
23. weight train$.tw.
24. muscle strength$.tw.
25. or/5‐24
26. 4 and 25
27. (random$ or placebo$).ti,ab.
28. ((single$ or double$ or triple$ or treble$) and (blind$ or mask$)).ti,ab.
29. controlled clinical trial$.ti,ab.
30. RETRACTED ARTICLE/
31. or/27‐30
32. (animal$ not human$).sh,hw.
33. 31 not 32
34. 26 and 33
Appendix 3. Cochrane Library (Wiley) search strategy
#1 MeSH descriptor: [Exercise] explode all trees
#2 MeSH descriptor: [Exercise Therapy] explode all trees
#3 MeSH descriptor: [Physical Therapy Modalities] explode all trees
#4 exercise:ti,ab
#5 MeSH descriptor: [Physical Fitness] explode all trees
#6 MeSH descriptor: [Exercise Tolerance] explode all trees
#7 MeSH descriptor: [Sports] explode all trees
#8 MeSH descriptor: [Pliability] explode all trees
#9 MeSH descriptor: [Physical Exertion] explode all trees
#10 MeSH descriptor: [Motion] explode all trees
#11 MeSH descriptor: [Physical Endurance] explode all trees
#12 swim:ti,ab
#13 skate:ti,ab
#14 jog:ti,ab
#15 bike:ti,ab
#16 cycle:ti,ab
#17 walk:ti,ab
#18 row:ti,ab
#19 weight train:ti,ab
#20 muscle strength:ti,ab
#21 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20
#22 MeSH descriptor: [Fibromyalgia] explode all trees
#23 fibromyalgia:ti,ab
#24 #22 or #23
#25 #21 and #24
Appendix 4. CINAHL (EBSCOhost) search strategy
S01 (MH "Fibromyalgia")
S02 TI fibromyalgia or AB fibromyalgia
S03 TI fibrositis or AB fibrositis
S04 (MH "Exercise+")
S05 (MH "Exertion+")
S06 (MH "Physical Fitness")
S07 (MH "Exercise Test+")
S08 (MH "Sports+")
S09 (MH "Pliability")
S10 (MH "Physical Endurance+")
S11 TI exertion* or AB exertion*
S12 TI exercis* or AB exercis*
S13 TI sport* or AB sport*
S14 TI physical N5 fitness or TI physical N5 therapy or TI physical N5 therapies or AB physical N5 fitness or AB physical N5 therapy or AB physical N5 therapies
S15 TI motion N5 fitness or TI motion N5 therapy or TI motion N5 therapies or AB motion N5 fitness or AB motion N5 therapy or AB motion N5 therapies
S16 TI physical* N2 endur* or AB physical* N2 endur*
S17 ( skate* or skating ) or AB ( skate* or skating )
S18 TI jog* or AB jog*
S19 TI swim* or AB swim*
S20 TI bicycl* or AB bicycl*
S21 TI ( (cycle* or cycling) ) or AB ( (cycle* or cycling) )
S22 TI walk* or AB walk*
S23 TI (row or rows or rowing ) or AB ( row or rows or rowing )
S24 TI weight train* or AB weight train*
S25 TI muscle strength* or AB muscle strength*
S26 TI manipulat* or AB manipulat*
S27 MH "Yoga") OR (MH "Yoga Pose")
S28 TX yoga
S29 TX tai chi
S30 (MM "Tai Chi")
S31 TX tai ji
S32 TX pilates
S33 (MH "Pilates") OR "pilates"
S34 (MH "Vibration")
S35 TX vibration
S36 S1 OR S2 OR S3
S37 S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35
S38
S36 AND S37
Appendix 5. PEDro Physiotherapy Evidence Database (http://www.pedro.org.au/) search strategy
fibromyalg* AND fitness training
fibromyalg* AND strength training
fibrositis
Appendix 6. Dissertation Abstracts (ProQuest) search strategy
Terms searched fibromyalg* or fibrositis (in citation or abstract)
Appendix 7. Current Controlled Trials (http://www.controlled‐trials.com/) or ClinicalTrials.gov search strategy
Terms searched fibromyalg* or fibrositis
Appendix 8. WHO International Clinical Trials Registry Platform (http://www.who.int/ictrp/en/) search strategy
Terms searched fibromyalg* or fibrositis in Condition
Appendix 9. AMED (OVID) Allied and Complementary Medicine search strategy
1. Fibromyalgia/
2. fibromyalgi$.tw.
3. fibrositis.tw.
4. or/1‐3
5. exp exercise/
6. physical fitness/
7. exp physical endurance/
8. exp sports/
9. Pliability/
10. exertion$.tw.
11. exercis$.tw.
12. sport$.tw.
13. ((physical or motion) adj5 (fitness or therapy or therapies)).tw.
14. (physical$ adj2 endur$).tw.
15. manipulat$.tw.
16. (skate$ or skating).tw.
17. jog$.tw.
18. swim$.tw.
19. bicycl$.tw.
20. (cycle$ or cycling).tw.
21. walk$.tw.
22. (row or rows or rowing).tw.
23. weight train$.tw.
24. muscle strength$.tw.
25. exp pilates/
26. exp yoga/
27. Tai chi/
28. tai ji.tw.
29. yoga.tw.
30. (hatha or kundalini or ashtanga or bikram).tw.
31. pilates.tw.
32. exp exercise therapy/
33. or/5‐32
34. 4 and 33
Appendix 10. Selection criteria
Level One screen:
Based solely on the title of the report:
1. Does the study deal exclusively with fibromyalgia? No ‐ exclude, Yes or uncertain ‐ go to step two
2. Does it include exercise? No ‐ exclude, Yes or uncertain ‐ go to step three
3. Does the study deal exclusively with adults? No ‐ exclude, Yes or uncertain ‐ go to step four
4. Is it an RCT? No ‐ exclude, Yes or uncertain ‐ include
Level Two screen
Based solely on the abstract of the report:
1. Does the study deal exclusively with fibromyalgia? No ‐ exclude, Yes or uncertain ‐ go to step two
2. Does it include exercise? No ‐ exclude, Yes or uncertain ‐ go to step three
3. Does the study deal exclusively with adults? No ‐ exclude, Yes or uncertain ‐ go to step four
4. Is it an RCT? No ‐ exclude, Yes or uncertain ‐ include
Level Three screen
Based on the full text of the report:
1. Does the study deal exclusively with fibromyalgia? No ‐ exclude, Yes ‐ go to step two, Uncertain ‐ add to list of questions for study author and proceed to step two
2. Is the diagnosis of fibromyalgia based on published criteria? No ‐ exclude, Yes ‐ go to step three, Uncertain ‐ add to list of questions for study author and proceed to step 3
3. Does the study deal exclusively with adults? No ‐ exclude, Yes ‐ go to step 4, Uncertain ‐ add to list of questions for study author and proceed to step 4
4. Is it an RCT? (the study uses terms such as ”random,“ ”randomized,“ ”RCT,“ or ”randomization“ to describe the study design or assignment of subjects to groups) No ‐ exclude, Yes ‐ go to step 5, Uncertain ‐ add to list of questions for study author and proceed to step 5
5. Does it include exercise (the study involves at least one intervention that includes exercise)? No ‐ exclude, Yes ‐ go to step 6, Uncertain ‐ add to list of questions for study author and proceed to step 6
6. Are between‐group data provided for the outcomes? No (the study contains ONLY fibromyalgia, or results are reported such that effects on fibromyalgia cannot be isolated ‐ exclude, Yes ‐ include the study, Yes but uncertain about one or more of steps 1 to 5 ‐ reserve judgment until study authors are contacted
Level Four screen(classification of the study using team’s intervention listing)
1. Classification of design
2. Number of interventions
3. Type of comparisons:
Head‐to‐head comparison?
Exercise to control?
Composite to control?
4. Control group
Classify type of control
3. Exercise
Enter types of exercise interventions used in the study
Complete naming of the intervention groups
Appendix 11. 2011 ACSM position stand: guidance for prescribing exercise
The following recommendations are from Garber 2011.
Recommendations for cardiorespiratory fitness
Moderate‐intensity cardiorespiratory exercise training for ≥ 30 minutes/d on ≥ 5 days per week for a total of ≥ 150 minutes per week, vigorous‐intensity cardiorespiratory exercise training for ≥ 20 minutes/d on ≥ 3 days per week ( ≥ 75 minutes/wk), or a combination of moderate‐ and vigorous‐intensity exercise to achieve a total energy expenditure ≥ 500 to 1000 METs min/wk
Recommendations for muscular fitness
On two to three days per week, adults should also perform resistance exercises for each of the major muscle groups, and neuromotor exercise involving balance, agility, and co‐ordination
Two to four sets of resistance exercises per muscle group are recommended, but even a single set of exercises may significantly improve muscle strength and size
Rest interval between sets if more than one set is performed: two to three minutes
Resistance equivalent of 60% to 80% of one repetition max (1RM) effort. For novices, 60% to 70% of 1RM is recommended, for experienced exercises ≥ 80% may be appropriate
The selected resistance should permit the completion of 8 to 12 repetitions per set or the number needed to induce muscle fatigue but not exhaustion
For people who wish to focus on improving muscular endurance, lower intensity (< 50% of 1RM) can be used with 15 to 25 repetitions in no more than 2 sets
Recommendations for flexibility
A series of flexibility exercises for each major muscle‐tendon group with a total of 60 seconds per exercise on ≥ 2 days per week is recommended. A series of exercises targeting the major muscle‐tendon units of the shoulder girdle, chest, neck, trunk, lower back, hips, posterior and anterior legs, and ankles are recommended. For most individuals, this routine can be completed within 10 minutes
Stretches should be held for 1 to 30 seconds at the point of tightness or slight discomfort. Older persons may realize greater improvements in range of motion with longer stretching durations (30 to 60 seconds). A 20% to 75% maximum contraction held for three to six seconds followed by a 10‐ to 30‐second assisted stretch is recommended for PNF techniques
Repeating each flexibility exercise two to four times is effective
Appendix 12. Busch 2002 search strategy
| Process | Particulars |
| Databases used | MEDLINE (1966‐12/2000), CINAHL (1982‐12/2000), HealthSTAR (1990‐12/2000), Sports Discus (1975‐12/2000), Embase (1974 to 12/2000), the Cochrane Controlled Trials Register (2000, Issue 4) |
| Adjunctive search methods | Reference lists from identified articles, meta‐analyses, and reviews of all types of treatment for fibromyalgia were reviewed independently by two review authors and all promising references were scrutinized. We searched without language restriction and translated all non‐English studies that were initially identified as possibly meeting the inclusion criteria |
| Search strategy used for MEDLINE | Search strategy on SilverPlatter v3.0 for Windows |
| 1 "Fibromyalgia"/ all subheadings 2 fibromyalgia 3 fibrositis 4 fibromyalgia or fibrositis 5 #1 or #4 6 explode "Exertion"/all subheadings 7 "Physical‐Fitness"/all subheadings 8 explode "Physical‐Therapy"/all subheadings 9 "Exercise‐Test"/all subheadings 10 "Exercise‐Tolerance"/all subheadings 11 explode "Sports"/all subheadings 12 "Pliability"/all subheadings 13 #6 or #7 or #8 or #9 or #10 or #11 or #12 14 exertion* 15 exercis* 16 physical 17 motion 18 fitness 19 therapy 20 therapies 21 (physical or motion) near (fitness or therapy or therapies) 22 physical 23 endurance 24 physical near endurance 25 manipulation* 26 skating 27 running 28 jogging 29 swimming 30 bicycling 31 cycling 32 walking 33 rowing 34 weight 35 training 36 muscle 37 strengthening 38 skating or running or jogging or swimming or bicycling or cycling or walking or rowing or weight training or muscle strengthening 39 #13 or #14 or #15 or #21 or #24 or #25 or #38 40 #5 and #39 41 explode "Research‐Design"/all subheadings 42 explode "Clinical‐Trials"/all subheadings 43 #41 or #42 44 #40 and #43 45 PT = "CLINICAL‐TRIAL" 46 #40 and (PT = "CLINICAL‐TRIAL") 47 #44 or #46 |
Data and analyses
Comparison 1. AE versus control (end of intervention).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HRQL, FIQ Total, 0‐100, lower is best | 5 | 372 | Mean Difference (IV, Random, 95% CI) | ‐7.89 [‐13.23, ‐2.55] |
| 1.1 Met ACSM | 3 | 253 | Mean Difference (IV, Random, 95% CI) | ‐8.66 [‐17.77, 0.44] |
| 1.2 Did not meet ACSM | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐6.77 [‐12.97, ‐0.57] |
| 2 HRQL, sensitivity.selection bias | 3 | 246 | Mean Difference (IV, Random, 95% CI) | ‐10.47 [‐20.79, ‐0.15] |
| 3 Pain, intensity, 0‐100, lower is best | 6 | 351 | Mean Difference (IV, Random, 95% CI) | ‐11.06 [‐18.34, ‐3.77] |
| 3.1 Met ACSM | 2 | 203 | Mean Difference (IV, Random, 95% CI) | ‐5.89 [‐18.72, 6.95] |
| 3.2 Did not meet ACSM | 4 | 148 | Mean Difference (IV, Random, 95% CI) | ‐14.90 [‐21.36, ‐8.44] |
| 4 Pain, sensitivity.selection bias | 3 | 246 | Mean Difference (IV, Random, 95% CI) | ‐8.38 [‐17.88, 1.12] |
| 5 Pain, sensitivity, attrition bias | 5 | 326 | Mean Difference (IV, Random, 95% CI) | ‐11.71 [‐19.93, ‐3.50] |
| 5.1 New subgroup | 5 | 326 | Mean Difference (IV, Random, 95% CI) | ‐11.71 [‐19.93, ‐3.50] |
| 6 Fatigue, 0‐100 mm, lower is best | 4 | 286 | Mean Difference (IV, Random, 95% CI) | ‐6.06 [‐12.41, 0.30] |
| 7 Stiffness, 0‐100 mm, lower is best | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8 Physical Ftn, 0‐100 mm, lower is best | 3 | 246 | Mean Difference (IV, Random, 95% CI) | ‐10.16 [‐15.39, ‐4.94] |
| 9 Withdrawals | 8 | 456 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.89, 1.77] |
| 10 CR max, VO2max, mL/kg/min | 1 | 143 | Mean Difference (IV, Random, 95% CI) | 1.60 [‐0.06, 3.26] |
| 11 CR submax, 6MWT (distance ‐ meters, higher is best) | 3 | 169 | Mean Difference (IV, Random, 95% CI) | 55.58 [27.20, 83.96] |
Comparison 2. AE versus control (long term).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HRQL, 0‐100, lower is best | 2 | 108 | Mean Difference (IV, Random, 95% CI) | ‐11.16 [‐25.99, 3.68] |
| 2 Pain intensity, 0‐100, lower is best | 3 | 134 | Mean Difference (IV, Random, 95% CI) | ‐10.56 [‐18.00, ‐1.12] |
| 3 Fatigue, 0‐100, lower is best | 2 | 100 | Mean Difference (IV, Random, 95% CI) | ‐5.93 [‐24.34, 12.47] |
| 4 Physical Ftn, 0‐100, lower is best | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐11.33 [‐22.11, ‐0.55] |
| 5 Withdrawals | 3 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.47, 1.22] |
| 6 CR max, work capacity (W) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.06, 0.26] |
| 7 CR submax, 6MWT (meters, higher is best) | 1 | 48 | Mean Difference (IV, Random, 95% CI) | 41.5 [‐17.91, 100.91] |
Comparison 3. AE versus AE (end of intervention).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HRQL, 0‐100, lower is best | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Pain intensity, 0‐100, lower is best | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Fatigue, 0‐100, lower is best | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Stiffness, 0‐100, lower is best | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Physical Ftn, 0‐100, lower is best | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Withdrawals | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 CR max, VO2max, mL/kg/min | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8 CR submax, 6MWT (distance ‐ meters, higher is best) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
3.8. Analysis.

Comparison 3 AE versus AE (end of intervention), Outcome 8 CR submax, 6MWT (distance ‐ meters, higher is best).
Comparison 4. AE versus other (end of intervention).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HRQL, 0‐100, lower is best | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Pain intensity, 0‐100, lower is best | 4 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 AE only vs education or SMP | 3 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 AE only vs medication | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Fatigue, 0‐100, lower is best | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Withdrawals | 4 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 CR max, work capacity (w) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 CR submax, 6 MWT(distance ‐ meters, higher is best) | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Fontaine 2007.
| Methods | 2 groups: lifestyle physical activity (AE); education (control) Length: 12 weeks; follow‐up: none Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: 46:2 Age (years (SD)): 48 (10); 52 (8) Inclusion: men and women 18 years of age or older, diagnosis of fibromyalgia (ACR 1990), sedentary for 6 months before enrolment, stable on medication regimen for ≥ 3 months before enrollment Exclusion: acute or chronic condition (eg, cancer, coronary artery disease), inflammatory disease, or other pain disorders; intending to seek professional treatment for anxiety or depression during the study period; unwilling to participate in a physical activity program, assistive device required to ambulate Duration of illness (years (SD)): 7(5); 7(4) |
|
| Interventions |
Lifestyle physical activity (n = 22): Frequency: 5‐7/wk; Duration: 10' and increased daily duration 5'/wk; once participants accumulated at least 30', they were encouraged but were not prescribed longer durations;Intensity: moderate; Mode: "brisk walking was primary mode, although other forms were also recommended" (page 4). Non‐exercise component: "90' group session every 2 weeks for 12 weeks, group sessions based on a cognitive‐behavioral physical activity promotion program" (page 4) Education (n = 26): education on fibromyalgia symptoms, diagnosis, and treatment for 3 months. Frequency: 1/mo; Duration: 90' |
|
| Outcomes | Health‐related quality of life (FIQ Total), pain (VAS), fatigue (FSS), CR submax (6‐minute walk test) Others: tenderness (tender point count), patient‐rated global (self‐perceived) change Measurements taken at 0 and 12 weeks |
|
| Adherence to exercise protocols | Monitoring methods: logs to track mode; adherence criteria: none stated; adherence: attendance rate 71% | |
| Congruence with ACSM guidelines for aerobic training | Yes | |
| Notes | Country: United States Language: English Study author contacted: yes, study author confirmed that participants from the 2 studies (Fontaine 2007 and Fontaine 2010) were different Funding source/declaration of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information on the method used to generate the allocation sequence to permit judgment of risk |
| Allocation concealment (selection bias) | Unclear risk | No description of the method used for allocation concealment |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: health‐related quality of life (FIQ Total), pain intensity (VAS), fatigue (FSS) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Unclear risk | CR submax (6‐minute walk test): no information on blinding of assessors |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information on blinding of participants and personnel to permit judgment of risk |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were balanced in numbers across intervention groups, with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgment of risk |
| Other bias | Unclear risk | Insufficient information to assess whether an important risk of bias existed |
Fontaine 2010.
| Methods | 2 groups: lifestyle physical activity (AE); education (control) Length: 12 weeks; follow‐up: 26 weeks and 52 weeks Study design: randomized clinical trial with parallel group |
|
| Participants | Female:Male: 73:0 Age (years (SD)): 46.4 (11.6); 49 (10.2) Inclusion: diagnosis of fibromyalgia (ACR 1990), patient at Johns Hopkins Arthritis Center, affiliated Johns Hopkins Rheumatology clinics Exclusion: meeting US Surgeon General’s 1996 recommendation for physical activity for previous 6 months (ie, not engaging in moderate‐intensity physical activity for 30 minutes on 5 days per week or in vigorous physical activity 3 times per week for 20 minutes each time during the previous month), acute or chronic medical condition that could preclude active participation (cancer, coronary artery disease), intent to change medications that might affect mood, intent to seek professional treatment for anxiety or depression during the study period, not unwilling to make the required time commitment Duration of illness (years (SD)): 5.9 (5.1); 9.6 (6.8) |
|
| Interventions |
Lifestyle physical activity (n = 43): Increase moderate‐intensity physical activity by helping participants find ways to accumulate short bouts of physical activity throughout the day. Frequency: 5‐7 times/wk; Duration: 60';Intensity: moderate; Mode: walking (the most common form of LPA) and other forms (eg, gardening/mowing the lawn) of household activity (eg,vacuuming); and sports activity (eg, cycling, swimming, field hockey) Education (n = 33): Provide education and control for effects of being enrolled in a clinical trial and receiving increased attention and social support; Frequency: 1/mo; Duration: 90‐120'; Intensity: not applicable; Mode: education, question and answer, and social support |
|
| Outcomes | Health‐related quality of life (FIQ Total), pain (VAS for pain), fatigue (Fatigue Severity Scale ‐ FSS), CR submax (6‐minute walk test) Others: depression (Center for Epidemiological Studies Depression Scale ‐ CES‐D), tenderness (tender point count), physical activity level (pedometer); perceived improvement ("Since the start of the study, how much change has there been in your fibromyalgia?") Measurements taken at 0 and 12 weeks |
|
| Adherence to exercise protocols | Monitoring methods: intensity monitored by pedometer once a week and diaries used to track mode; adherence criteria: not specified; adherence: unknown | |
| Congruence with ACSM guidelines for aerobic training | Yes | |
| Notes | Country: United States Language: English Study author contacted: yes, study author confirmed that participants from the 2 studies (Fontaine 2007 and Fontaine 2010) were different Funding source/declaration of interest: Work was supported by NIH/NIAMS (National Institutes of Health/National Institute of Arthritis and Musculoskeletal Skin Diseases) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Particiants were randomized via a coin flip at a 1:1 allocation ratio to each of the two groups" (page 5) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit evaluation of risk |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: health‐related quality of life (FIQ Total), pain intensity (VAS for pain), fatigue (Fatigue Severity Scale ‐ FSS) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Unclear risk | CR submax (6‐minute walk test): no information on blinding assessors |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information on blinding of participants and personnel to permit judgment of risk |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for missing outcome data unlikely to be related to true outcomes; missing outcome data were balanced in numbers across intervention groups |
| Selective reporting (reporting bias) | Low risk | Study protocol is available (clinicaltrials.gov NCT00383084) and all of the study's prespecified outcomes of interest in the review have been reported in the prespecified way |
| Other bias | Low risk | Study appears to be free of other sources of bias |
Gowans 2001.
| Methods | 2 groups: exercise (AE); control Length: 23 weeks; follow‐up: none Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: 44:6 Age (years (SD)): 44.6 (8.7); 49.8 (7.3) Inclusion: diagnosis of fibromyalgia (ACR 1990), willingness to comply with experimental protocol Exclusion: diagnosis of high blood pressure or symptomatic cardiac disease, other serious systemic diseases (eg, cancer, diabetes), intention of changing medications for anxiety or depression or seeking professional treatment for anxiety or depression during the study period, enrolled in or intended to begin an aerobic exercise program Duration of illness (years (SD)): symptoms: 9.6 (8.6); 8.4 (7.6); diagnosis: 2.8 (2.6); 4.2 (4.4) | |
| Interventions |
Exercise (n = 27): Classes for the first 6 weeks were conducted in a warm therapeutic pool; starting at 7 weeks, participants progressed to 2 walking classes in a gym and 1 pool class. Frequency: 3 hospital‐based classes/wk; Duration: 30' (5' stretching first, 20' aerobic, 5' stretching after);Intensity: low to moderate (60% to 75% age‐adjusted HRmax); Mode: water (warm) walking/running progressing to land walking/running Control (n = 23): "continue ad libitum activity" (page 520) |
|
| Outcomes | Health‐related quality of life (FIQ Total), CR submax (6‐minute walk test) Other: depression (Beck Depression Index cognitive/affective), anxiety (state anxiety inventory), self‐efficacy (ASES), tenderness (tender point count), muscle function (isokinetic knee extension strength at 60 degrees) Measurements taken at 0 and 23 weeks |
|
| Adherence to exercise protocols | Monitoring methods: HR and attendance were monitored; adherence criteria for efficacy analysis: must attend > 45% of exercise classes; adherence: mean attendance at exercise classes 67% (range 46%–84%) | |
| Congruence with ACSM guidelines for aerobic training | No for healthy adults, based on duration (only 20 minutes per session); met ACSM criteria for individuals who are sedentary/have no habitual activity/are extremely deconditioned | |
| Notes | Country: Canada
Language: English Study author contacted: no Funding sources/declaration of interest: Work was supported by a grant from the Toronto Hospital Auxiliary Women's Health Project on Women and Arthritis (page 528) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were stratified by sex and randomly assigned to..." (page 520) |
| Allocation concealment (selection bias) | Unclear risk | No description of the method used for allocation concealment |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instrument: health‐related quality of life (FIQ Total) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Low risk | CR submax (6‐minute walk test): "Their distance was recorded to the nearest meter by an assessor blinded to subjects’ group assignments" (page 520) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants in the intervention group had no contact with those in the control group; control group did not meet |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were analyzed by ITT |
| Selective reporting (reporting bias) | Low risk | Published reports include all expected outcomes |
| Other bias | Low risk | Study appears to be free of other sources of bias |
Kayo 2011.
| Methods | 3 groups: walking program (AE); strengthening exercise; control Length: 16 weeks; follow‐up: 28 weeks Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: 90:0 Age (years (SD)): 47.7 (5.3); 46.7 (6.3); 46.1 (6.4) Inclusion: women 30‐55 years of age who agreed to participate in an exercise program 3/wk for 16 weeks and to discontinue medications for fibromyalgia 4 weeks before the start of the study; individuals who had at least 4 years of schooling Exclusion: women with contraindications to exercise based on clinical rheumatological examination, those involved in cases of medical litigation Duration of illness (years (SD)): 4.0 (3.1); 4.7 (5.7); 5.4 (3.5) |
|
| Interventions |
Walking program (n = 30): 48 sessions in total. Frequency: 3/wk; Duration: ˜ 60' (warm‐up with 5‐10' stretching, conditioning stimulus, cool‐down 5'); Intensity: moderate at week 1 to vigorous by week 16 (40%‐50% to 60%‐70% heart rate reserve by week 16); Mode: supervised indoor or outdoor walking monitored by a heart rate monitor Resistance exercise training (n = 30): 48 sessions in total. Frequency: 3/wk; Duration: ˜ 60'; Intensity: high intensity (4 on 10‐point Borg scale), exercise load and intensity increased every 2 weeks (reps ‐ weeks 1 + 2: 3 sets of 10 reps with rest intervals of 1' between sets, weeks 3‐16; load ‐ weeks 1‐4, no load, weeks 5‐16, load included). The training load was individually and systematically adjusted every time the participant performed more than 15 repetitions successfully; Mode: supervised exercise protocol consisting of 11 free active exercises for upper and lower limbs and trunk muscles, with free weights and body weight performed in the standing, sitting, and lying positions Control group (n = 30): control conditions not specified, except study authors stated that participants in all 3 groups were asked to discontinue tricyclic antidepressants but were allowed to use acetaminophen (paracetamol) for pain Co‐interventions: Exercise was administered in this study as a single modality; the timing of restarting medication was monitored *For this review: only walking program and control group were considered |
|
| Outcomes | Health‐related quality of life (FIQ Total), pain (VAS), fatigue (SF‐36 Vitality Scale), physical function (SF‐36 Physical Function Scale) Other: tenderness (tender point count), mental health (SF‐36 mental health) as provided by study author on request Measurements taken at 0, 8, 16, and 28 weeks |
|
| Adherence to exercise protocols | Monitoring methods: HR monitored; adherence criteria: drop‐outs were those who missed more than 20% of sessions or 3 consecutive sessions; adherence: attendance rate 80% | |
| Congruence with ACSM guidelines for aerobic training | Yes | |
| Notes | Country: Brazil Language: English Study author contacted: yes, study authors provided data on outcomes (fatigue and physical function) Funding source/declaration of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The allocation sequence was based on a random number list (GraphPad Statmate version 1.0), which was organized by an investigator (MSP)" (online page 2) |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes were used |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: health‐related quality of life (FIQ Total), pain intensity (VAS), fatigue (SF‐36 ‐ Vitality Scale), physical function (SF‐36 Physical Function Scale) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Low risk | "All patients were clinically examined by the same rheumatologist (CSM), who was blinded to group assignment throughout the study" (pages 2‐8) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Unclear blinding of participants and personnel delivering the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were analyzed by ITT |
| Selective reporting (reporting bias) | High risk | Outcome data for important variables (eg, tender points, SF‐36 Physical Functioning, SF‐36 Vitality, SF‐36 Mental Health) were not provided in the published report, but study authors provided these on request. RCT protocol is available (ClinicalTrials.gov ID NCT00498264) |
| Other bias | Low risk | No other serious sources of bias is evident |
King 2002.
| Methods | 4 groups: exercise only (AE); education only; education and exercise; control (wait list) Length: 12 weeks; follow‐up: 24 weeks Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: 170:0 Age (years (SD)): 45.2 (9.4); 44.9 (10); 47.4 (9); 47.3 (7.3) Inclusion: diagnosis of fibromyalgia (ACR 1990), women 18 to 65 years of age, willing to meet 3 weeks × 12 weeks, persons involved in medico‐legal cases were not excluded Exclusion: conditions precluding ability to exercise (severe cardiac arrhythmia, dizziness, severe shortness of breath), inflammatory arthritis, systemic lupus erythematosus, rheumatoid arthritis Duration of illness (years (SD)): 7.8; 10.9; 8.9; 9.6 |
|
| Interventions |
Exercise only (AE) (n = 42): Frequency: 3/wk; Duration: starting duration 10' to 15' progressing to 20' to 40', Intensity: light to moderate (60%‐75% predicted HRmax/age); Mode: walking, aquacise (deep and shallow water), or low‐impact aerobics Education only (n = 41): based upon principles of self‐management. Frequency: 1/wk; Duration: 1 1/2 to 2 hour educational session provided by a multidisciplinary team. Topics focused on potential causes of fibromyalgia, principles of self‐management (goal setting, maximizing energy for household chores or personal activities, pain or fatigue coping strategies, benefits of exercise, evaluating alternative therapies, and barriers to behavior change) Exercise + Education (n = 35): exercise same as for exercise only, and education same as for education only. Frequency: 3/wk (2 exercise sessions/wk and 1 combined educational and exercise session per week) Wait list control (n = 34): a page of written instructions for basic stretches and 5 items related to general coping strategies provided on entry to the study For a, b, c, and d: Participants were instructed not to change their present treatment (ie, medications) for the duration of the study *For this review: only exercise only, education only, and wait list control groups were considered |
|
| Outcomes | Health‐related quality of life (FIQ Total), CR submax (6‐minute walk test) Other: pain (Chronic Pain Self‐Efficacy Scale), function (Chronic Pain Self‐Efficacy Scale), coping with symptoms (Chronic Pain Self‐Efficacy Scale), tenderness (tender point count), and total survey site score Measurements taken at 0, 12, and 24 weeks |
|
| Adherence to exercise protocols | Monitoring methods: HR and logbooks; adherence criteria: missed 3 consecutive sessions or 12 of the 36 total; adherence: attendance 75% (21%) | |
| Congruence with ACSM guidelines for aerobic training | No, based on frequency and duration (only 3/wk, light to moderate) | |
| Notes | Country: Canada Language: English Stud author contacted: no Funding sources: Work was supported by grants from the Medical Services Incorporated Foundation and from the Health Services Research and Innovation Fund, Alberta Health, administered by Alberta Heritage Foundation for Medical Research |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random assignment of subjects to groups was done in blocks of 4 to 16. A list was prepared prior to start of study using a table of random numbers and subject ID number (order of admission to study" (page 2621) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information on allocation concealment to permit judgment of risk |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: health‐related quality of life (FIQ Total) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Low risk | CR submax (6‐minute walk test): "Baseline testing occurred before randomization" and "both assessors were blinded to the subject’s group randomization on subsequent visits" (page 2621) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded (pages 2623 and 2626). It is unlikely that care providers were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were analyzed by ITT for post‐intervention status; follow‐up data were reported and analyzed with completer data |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but it is clear that the published report includes all expected outcomes |
| Other bias | Unclear risk | Insufficient information for assessment of whether an important risk of bias exists |
Mannerkorpi 2010.
| Methods | 2 groups: Nordic walking (AE); low intensive walking (AE) Length: 15 weeks; follow‐up: 26 weeks Study design: randomized clinical trial with parallel group |
|
| Participants | Female:Male: 67:0 Age (years (SD)): 48.0 (7.8); 50.0 (7.6) Inclusion: diagnosis of fibromyalgia (ACR 1990), ability to manage a bicycle test at 50 watts or more, interest in exercising outdoors Exclusion: did not speak or read Swedish, presence of other severe somatic or psychiatric disease, ongoing planned physical therapy ‐ including exercise, inability to accept times for planned exercise sessions Duration of illness (years (SD)): 11 (5.4); 12 (5.3) |
|
| Interventions |
Nordic walking (n = 34): supervised moderate‐ to high‐intensity aerobic exercise. Frequency: 2/wk; Duration: 20'; Intensity: 10' light (RPE 9‐11), 2' interval moderate to vigorous (RPE 13‐15) alternated with 2' light (RPE 10 to 11); Mode: walking in parks and forests with flat areas and small hills Low intensive walking (n = 33): supervised low‐intensity aerobic exercise. Frequency: 1/wk; Duration: 20'; Intensity: light (RPE 9 to 11); Mode: walking in parks and forests with flat areas and small hills |
|
| Outcomes | Health‐related quality of life (FIQ Total), pain (FIQ), fatigue (FIQ), physical function (FIQ), CR submax (6‐minute walk test, ergometer test) Others: fatigue (multidimensional fatigue inventory) Measurements taken at 0, 15, and 26 weeks |
|
| Adherence to exercise protocols | Monitoring methods: participant monitored; adherence criteria: not specified; adherence: median attendance was 62% and 50%, respectively, in a and b | |
| Congruence with ACSM guidelines for aerobic training | No, based on frequency and duration (only twice or once a week with 20' session duration) | |
| Notes | Country: Sweden Language: English Study author contacted: yes, study author provided information on post‐test data Funding source/declaration of interest: Work was supported by Swedish Research Council, the Health and Medical Care Executive Board of Västra Götaland Region, the Swedish Rheumatism Association, the Rheumatic Pain Society in Göteborg/RiG, and the LUA/ALF at Sahlgrenska University Hospital |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was prepared by a statistician using a random number generator |
| Allocation concealment (selection bias) | Low risk | "Randomization was conducted by using concealed envelopes prepared by a statistician" (page 2) |
| Blinding of self reported outcome assessment (detection bias) All outcomes | Low risk | Self‐report instruments: health‐related quality of life (FIQ Total), pain intensity (FIQ), fatigue (FIQ), physical function (FIQ). Active comparison group of similar conditions |
| Blinding of objective outcome assessment (detection bias) All outcomes | Low risk | CR submax (6‐minute walk test, ergometer test). Communication from study authors indicates that all assessors were blinded for all post test measures."..where single‐blinded examiners did not know the group to which patient would be randomized" (page 2‐10) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information on blinding of participants and personnel to permit judgment of risk |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were balanced in numbers across intervention groups with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Low risk | Study protocol is available (ClinicalTrials.gov ID NCT00498264) and all of the study's prespecified outcomes of interest in the review have been reported in the prespecified way |
| Other bias | Low risk | Study appears to be free of other sources of bias |
Mengshoel 1992.
| Methods | 2 groups: low‐impact aerobic dance; control Length: 20 weeks; follow‐up: none Study design: randomized clinical trial with parallel groups (age) |
|
| Participants | Female:Male: 25:0 Age (years (min to max)): 33.5 (21 to 42); 34 (25 to 38) Inclusion: females with fibromyalgia according to 1990 ACR, normal lab test (haemoglobin, liver enzymes, serum creatinine, ESR, ANA, latex, and thyroxine) Exclusion: none stated Duration of illness (years (min to max)): 8.5 (3 to 20), 8 (3 to 23) |
|
| Interventions |
Low‐impact aerobic dance (n = 11): Frequency: 2/wk; Duration: 60'; Intensity: moderate to vigorous (HR 120 to 150 bpm); Mode: modified low‐impact aerobic dance; exercise for upper extremities performed at intervals between periods of rest; exercises modified to prevent pain, fatigue, and static muscle work Control (n = 14): instructed to not change their habits regarding physical activities |
|
| Outcomes | Pain intensity over past 7 days (VAS ‐ 100 mm), fatigue (VAS ‐ 100 mm) ‐ baseline data only, CR submax (Astrand test, RPE) Other: muscle endurance (grip strength at 1st and 20th rep, duration of shoulder hold in seconds, duration in minutes for stair climbing at a constant velocity), sleep (VAS ‐ 100 mm), pain coping (Vanderbilt Pain Management Inventory), fatigue during exercise (Borg's Rating Scale) Measurements taken at 0, 10, and 20 weeks |
|
| Adherence to exercise protocols | Monitoring methods: HR controlled periodically by pulse watch recorder; adherence criteria: not specified; adherence: attendance not specified | |
| Congruence with ACSM guidelines for aerobic training | Exercise protocol did not meet the frequency requirement; only 2 times/wk | |
| Notes | Country: Norway Language: English Study author contact: no Funding sources: Financial support was received from the Norwegian Fund for Postgraduate Training in Physiotherapy, the Olga Immerslund Legacy for Rheumatological Research, the Grethe Harbitz Legacy and Hafslund‐Nycomed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to permit judgment of ‘Yes’ or ‘No’ |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgment of ‘Yes’ or ‘No’ |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: pain intensity over past 7 days (VAS ‐ 100 mm), fatigue (VAS ‐ 100 mm) ‐ baseline data only |
| Blinding of objective outcome assessment (detection bias) All outcomes | Low risk | Measure: CR submax (Astrand test). "The testing was undertaken by a physical therapist who was blinded to the patients' classification. At the time of re‐test neither the patients nor the physiotherapist had access to the results of the baseline tests" (page 346) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information on blinding of participants and personnel to permit judgment of risk |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing outcome data likely led to an imbalance in results across groups |
| Selective reporting (reporting bias) | High risk | Insufficient information to permit judgment |
| Other bias | Low risk | Study appears to be free of other sources of bias |
Nichols 1994.
| Methods | 2 groups: aerobic exercise (AE); control (daily activities not involving physical activity) Length: 8 weeks; follow‐up: none Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: 17:2 Age (years (SD)): 47.8 (11.1); 50.8 (11.8) Inclusion: diagnosis of fibromyalgia (ACR 1990) Exclusion: history of heart disease, lung disease, uncontrolled hypertension, or orthopedic disorders that would preclude aerobic activity; participation in any regular aerobic exercise program within 6 months before the study Duration of illness (years (SD)): > 10; > 10 except for person who had 4 (years) |
|
| Interventions |
Aerobic exercise (n = 10): "Each session included a warm up and cool down regimen of stretching exercises, 1 warm up and cool down lap of slow paced walking" (page 329). Frequency: 3/wk; Duration: unclear; Intensity: light to moderate (60%‐70% predicted HRmax/age); Mode: fast‐paced walking on an indoor track Control Group (n = 9): daily activities as usual not involving physical activity |
|
| Outcomes | Physical function (Sickness Impact Profile) Other: mental health (Sickness Impact Profile), pain (McGill Pain Questionnaire, Brief Symptom Inventory) Measurements taken at 0 and 8 weeks |
|
| Adherence to exercise protocols | Monitoring methods: HR and cadence monitored at midsession; Adherence criteria: not stated; adherence: all participants were able to achieve 60% to 70% of HRmax | |
| Congruence with ACSM guidelines for aerobic training | No, based on frequency and duration (only twice a week) | |
| Notes | Country: United States Language: English Study author contacted: no Funding sources: none stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information on the method used to generate the allocation sequence to permit judgment of risk (page 329) |
| Allocation concealment (selection bias) | Unclear risk | No description of the method used for allocation concealment |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: physical function (Sickness Impact Profile) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Low risk | Not applicable: Objective outcomes were not assessed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Conflicting information regarding whether participants in the exercise and control groups interacted (pages 329 and 331) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were balanced in numbers across exercise and control groups with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but the published report includes all expected outcomes |
| Other bias | Low risk | Study appears to be free of other sources of bias |
Ramsay 2000.
| Methods | 2 groups: exercise class (AE); single session Length: 12 weeks; follow‐up: 24 weeks and 48 weeks Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: not specified Age (years (SD)): not specified for either group Inclusion: diagnosis of fibromyalgia (ACR 1990) Exclusion: unstable pharmacological treatment in the first month before entry to the study Duration of illness (years (SD)): not specified for either group |
|
| Interventions |
Exercise class (n = 37): Frequency: 1/wk; Duration: 60' and home program: not specified;Intensity: not specified; Mode: graded circuit exercises consisting of step‐ups, sitting to standing, skipping, jogging on the spot, alternate side bends, circling arms with increasing weights, plus encouragement to continue and increase exercises at home Single session (n = 37): demonstration of aerobic exercises, stretching and relaxation technique, plus home program; Frequency: 1 session; Duration: 60'; home program: not specified; Intensity: not specified; Mode: written advice on aerobic exercises plus stretching and relaxation |
|
| Outcomes | Pain intensity (VAS), physical function (HAQ) Other: tenderness (tender point count), depression (Hospital Anxiety and Depression questionnaire), anxiety (Hospital Anxiety and Depression questionnaire), sleep (number of nights per week with difficulty; average number of hours slept/night over past week) Measurements taken at 0, 12, 24, and 48 weeks |
|
| Adherence to exercise protocols | Monitoring methods: attendance; adherence criteria: not specified; adherence: carrying out 72%, 50% of home exercise sessions over the 12 weeks (median values) | |
| Congruence with ACSM guidelines for aerobic training | No, based on frequency (only once a week) | |
| Notes | Country: United Kingdom Language: English Study author contacted: no Funding source/declaration of interest: Work was supported by The Scottish Office Department of Health |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information on the method used to generate the allocation sequence to permit judgment of risk |
| Allocation concealment (selection bias) | Unclear risk | No description of the method used for allocation concealment to permit judgment of risk |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: pain intensity (VAS), physical function (HAQ) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Unclear risk | Information on abstract and title indicates 'observer‐blinded' ‐ unclear who is the observer |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information on blinding of participants and personnel to permit judgment of risk |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were analyzed using ITT |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but it is clear that the published report includes all expected outcomes |
| Other bias | Unclear risk | Insufficient information for assessment of whether an important risk of bias exists |
Sanudo 2010.
| Methods | 3 groups: aerobic exercise (AE); mixed exercise (aerobic + resistance + flexibility); control Length: 24 weeks; follow‐up: none Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: 64:0 Age (years (SE)): 55.9 (1.6); 55.9 (1.7); 56.6 (1.9) Inclusion: women with diagnosis of fibromyalgia (ACR 1990) Exclusion: presence of inflammatory rheumatic disease and severe psychiatric illness, respiratory or cardiovascular disease that prevented physical exertion, women with fibromyalgia receiving psychological or physical therapy to avoid possible interactions with the present trial Duration of illness (years (SD)): not specified for either group |
|
| Interventions |
Aerobic exercise (n = 22): supervised aerobic exercise intervention. Frequency: 2/wk; Duration: 45‐60' (10' warm‐up and 5‐10' cool‐down, 15‐20' of steady state AE, 15' interval training); Intensity: light to moderate (steady state aerobic 60%‐65% of HRmax) and moderate to vigorous (interval training 75%‐80% HRmax); Mode: Warm‐up included slow walks, easy movements of progressive intensity, steady state AE included continuous walking with arm movements and jogging, interval training included aerobic dance and jogging, cool‐down included slow walks, easy movements, relaxation training Mixed exercise (aerobics, resistance, flexibility) (n = 21): combined supervised aerobic exercise and resistance exercise. Frequency: 2/wk; Duration: AE and RT same duration, which included 10' warm‐up, 10‐15' AE, 15‐20' RT, 10' FX;Intensity: AE 65%‐75% HRmax, RT weights 1‐3 kg; Mode: RT 1 set of 8‐10 reps for 8 different muscle groups with a load of 1‐3 kg, FX 1 set of 3 reps of 8‐9 different exercises, maintaining stretch position for 30 seconds, RT and FX exercises focused on main areas of pain in patients with fibromyalgia (deltoids, biceps, neck (trapezius), hops (gluteus, quadriceps), back/chest/torso (latissimus dorsi, pectoralis major, abdominals)) Control group (n = 21): received medical treatment for fibromyalgia and continued normal daily activities, which did not include structured exercise *For this review: only aerobic exercise and control group were considered |
|
| Outcomes | Health‐related quality of life (FIQ Total), pain (SF‐36), fatigue (SF‐36), physical function (SF‐36), CR submax (6‐minute walk test) Other: muscle strength (grip strength), depression (Beck Depression Inventory) Measurements taken at 0 and 24 weeks |
|
| Adherence to exercise protocols | Monitoring methods: HR monitoring but unreported results and attendance; adherence criteria: not stated; adherence: attendance rate in 89% and in 86% | |
| Congruence with ACSM guidelines for aerobic training | No, based on frequency (only twice a week) for aerobics | |
| Notes | Country: Spain Language: English Study author contacted: yes, study author confirmed that data from 2 studies (J Rehabil Med 2011), although similar, were from 2 different groups of people Funding sources: none stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random number generator was used |
| Allocation concealment (selection bias) | Low risk | Randomization by member not involved in recruitment or assessment of patients; randomization list kept at a separate location in a locked filing cabinet (page 1839) |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: health‐related quality of life (FIQ Total), pain (SF‐36), fatigue (SF‐36), physical function (SF‐36) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Unclear risk | CR submax (6‐minute walk test). No information provided on blinding |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Insufficient information on blinding of participants and personnel to permit judgment of risk |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were analyzed by intention‐to‐treat |
| Selective reporting (reporting bias) | Low risk | Study protocol is available and all of the study's prespecified outcomes of interest in the review have been reported in the prespecified way |
| Other bias | Low risk | Study appears to be free of other sources of bias |
Schachter 2003.
| Methods | 3 groups: long bout (AE); short bout (AE); control Length: 16 weeks; follow‐up: none Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: 143:0 Age (years (SD)): 41.3 (8.7); 41.9 (8.6); 42.5 (6.7) Inclusion: diagnosis of fibromyalgia (ACR 1990), sedentary women, 20 to 55 years of age, willing to provide informed consent and be randomly assigned to treatment or control, permission from physician for participation Exclusion: more than 2 coronary artery disease risk factors outlined in 1995 ACSM, known cardiorespiratory or metabolic musculoskeletal or neurological conditions that could interfere with performance of moderate‐intensity exercise Duration of illness (years (SD)): not specified for either group Baseline mean and SD (health‐related quality of life 55 (1.3), pain 61 (1.97), stiffness 7 (1.9), and physical function 38 (1.86) |
|
| Interventions |
Long bout aerobic exercise (n = 51): long bout of AE with rhythmical movements designed to use all major muscle groups of the lower extremities performed to music. Frequency: 3 up to 5/wk; Duration: 10' up to 30'; Intensity: moderate on week 1 (40%‐50% HRR), vigorous by week 10 (65%‐75% HRR) (modulated through changes in music tempo); Mode: home program of low‐impact aerobics to videotaped instructor and music, rhythmical movements of lower body muscles Short bout aerobic exercise (n = 56): short bout of AE with rhythmical movements designed to use all major muscle groups of the lower extremities performed to music. Frequency: 3 up to 5/wk; Duration: 2/d 5' up to 15'; Intensity: moderate on week 1 (40%‐50% HRR), vigorous by week 10 (65%‐75% HRR) (modulated through changes in music tempo); Mode: home program of low‐impact aerobics to videotaped instructor and music, rhythmical movements of lower body muscles Control (n = 36): Participants were asked to refrain from starting any new regular physical activity or exercise programs or other non‐pharmacological interventions *For this review: All group interventions were considered |
|
| Outcomes | Health‐related quality of life (FIQ Total), pain (VAS), fatigue (FIQ), stiffness (FIQ), physical function (FIQ impairment), CR max (peak VO2) Other: tenderness (mean myalgic score), clinician global rating (physician rating of global severity), depression (FIQ), anxiety (FIQ), self‐efficacy (chronic pain self‐efficacy scale), sleep (FIQ) Measurements taken at 0, 8, and 16 weeks |
|
| Adherence to exercise protocols | Monitoring methods: HR monitoring but unreported results; adherence criteria: exercise adherence calculated in four 4‐week phases by dividing the sum of the minutes of exercise performed within a phase (as recorded in the participant’s exercise log) by the minimum number of minutes of exercise recommended for that period. Participants met the minimum recommended when they completed ≥ 11 of the 12 recommended sessions in ≥ 22 of the 24 recommended sessions for SBE in over 4 weeks; adherence in 46%, 40%, 42%, and 22% as compared with 68%, 74%, 54%, and 41% in those exercising at or above the minimum level across the 4 phases | |
| Congruence with ACSM guidelines for aerobic training | Yes | |
| Notes | Country: Canada Language: English Study author contacted: yes, study author provided additional information on outcome measures, risk of bias, and study procedures Funding source/declaration of interest: Work was supported by Saskatchewan Health Services Utilization and Research Commission, Canada |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number sequence was prepared by a person not connected with the study |
| Allocation concealment (selection bias) | Low risk | Assignments were placed in opaque envelopes |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: health‐related quality of life (FIQ Total), pain intensity (VAS), fatigue (FIQ), stiffness (FIQ), physical function (FIQ Impairment) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Low risk | CR max (peak VO2). "One rheumatologist who was masked to group assignment conducted all tender point examinations and evaluated fibromyalgia severity of all participants before starting and after completing the study" (page 345) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded to the hypothesis and may have had contact with care providers who worked with other groups, although care providers for group meetings were trained and supervised regarding discussion of only specific topics with each group |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were analyzed by intention‐to‐treat |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but published report includes all expected outcomes |
| Other bias | Low risk | Study appears to be free of other sources of bias |
Sencan 2004.
| Methods | 3 groups: aerobic exercise; paroxetine; placebo transcutaneous electrical stimulation (TENS) Length: 6 weeks; follow‐up at 26 weeks Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: 60:0 Age (years (SD)): 35.4 (9.6); 32.7 (9.4); 35.6 (7.9) Inclusion: diagnosis of fibromyalgia (ACR 1990), no other pharmacological treatment, other comorbid disease Exclusion: tumoral, infectious, metabolic, cardiovascular, or endocrine disease; drug dependency Duration of illness (years (SD)): 4.7; 6.5; 5.1 |
|
| Interventions |
Aerobic exercise (n = 20): aerobic exercise on stationary bicycle. Frequency: 3/wk; Duration: 40 minutes; not specified; Intensity: not specified; Mode: bicycle ergometer Paroxetine (n = 20): undertaken 20 mg/d paroxetine. Frequency: 1/d, home exercise for 6 months' follow‐up (followed by telephone calls at 2 and 4 months); Duration: not specified; Intensity: not specified Placebo TENS (n = 20): given placebo TENS. Frequency: 3/wk; Duration: 20 minutes; Intensity: not specified; Mode: electrodes applied on the 2 most painful tender points (no current) *For this review: All interventions were considered |
|
| Outcomes | Pain intensity (VAS) Other: tenderness (pressure algometry), depression (Beck Depression Inventory) Measurements taken at 0, 6, and 26 weeks |
|
| Adherence to exercise protocols | Monitoring methods: not specified; adherence criteria: not specified; adherence: unknown | |
| Congruence with ACSM guidelines for aerobic training | Not enough information to judge | |
| Notes | Country: Turkey Language: English Study author contacted: no Funding source/declaration of interest: none stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information on the method used to generate the allocation sequence to permit judgment of risk |
| Allocation concealment (selection bias) | Unclear risk | No description of the method used for allocation concealment to permit judgment of risk |
| Blinding of self reported outcome assessment (detection bias) All outcomes | Unclear risk | Self‐report instruments: pain intensity (VAS). Although this study includes a placebo control, it was not specified whether participants were aware of the assigned intervention |
| Blinding of objective outcome assessment (detection bias) All outcomes | Low risk | Not applicable: Objective outcomes were not measured |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information on blinding of participants and personnel to permit judgment of risk |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data at post‐test |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but it is clear that the published report includes all expected outcomes |
| Other bias | Unclear risk | Insufficient information to assess whether an important risk of bias exists |
Wigers 1996.
| Methods | 3 groups: aerobic exercises (AE); stress management; control Length: 14 weeks; follow‐up: 4 years Study design: randomized clinical trial with parallel groups |
|
| Participants | Female:Male: 55:5 Age (years (SD)): 43 (9); 44 (12); 46 (9) Inclusion: diagnosis of fibromyalgia (ACR 1990; Smythe 1979 + Yunus criteria 1981) Exclusion: none Duration of illness (years (SD)): 9 (5); 11 (10); 11 (9) |
|
| Interventions |
Aerobic exercise (n = 20): total duration (over 40 sessions) of aerobic exercise, focusing on the whole body and aimed at minimizing eccentric muscle strain, was 30 hours of active treatment. Frequency: 3/wk; Duration: 45' (23' music session comprising warming up and 2 peaks of high‐intensity training, each 3‐4', 15' aerobic games representing 2 high‐intensity periods 5‐6' with 4' calming down in between); Intensity: light to moderate (60%‐70% HRmax); Mode: movement to music and games Stress management training (n = 20): 2 treatment groups of 10, with each totalling 20 sessions and 30 hours of active treatment; Frequency: 2/wk first 6 weeks, 1/wk remaining 8 weeks; Duration: 90' Control (n = 20): continued treatments being used at baseline For this review: All interventions were considered |
|
| Outcomes | Pain (VAS), fatigue (VAS), CR max (ratio of max voluntary effort) Other: tenderness (tender point count), global rating (self‐perceived change numerical rating scale), sleep (VAS), depression (VAS) Measurements taken at 0, 7 weeks (mid‐test), 14 weeks (post‐test), and 4 years |
|
| Adherence to exercise protocols | Monitoring methods: self‐monitored HR guidelines given to participants and attendance; adherence criteria: not stated; adherence: attendance rate 70%, 68% | |
| Congruence with ACSM guidelines for aerobic training | No, intensity too low, duration too short (only 18‐20’ at HR 60%‐70%) | |
| Notes | Country: Norway Language: English Study author contacted: no Funding source/declaration of interest: Work was supported by The Research Council of Norway and The Norwegian Fibromyalgia Association |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After baseline registration the patients were randomized [by drawing lots] into an AE group, a SMT group or a TAU group" (page 78) |
| Allocation concealment (selection bias) | Unclear risk | No details on allocation concealment were provided |
| Blinding of self reported outcome assessment (detection bias) All outcomes | High risk | Self‐report instruments: pain intensity (VAS), fatigue (VAS) |
| Blinding of objective outcome assessment (detection bias) All outcomes | Low risk | CR max (ratio of max voluntary effort). "Neither patients nor investigators had access to previous recordings on any test occasion" (page 78) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Patients were instructed not to reveal their group membership before treatment specific questions were asked at the very end of completion test. Neither patients nor investigators had access to previous recordings on any test occasion" (page 78) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were analyzed by ITT |
| Selective reporting (reporting bias) | Low risk | Study protocol is not available but it is clear that the published reports include all expected outcomes |
| Other bias | Low risk | Study appears to be free of other sources of bias |
ACR: American College of Rheumatology; AE: aerobic exercise; ANA: antinuclear antibody; CR submax: submaximal cardiorespiratory function; ESR: erythrocyte sedimentation rate; FIQ: Fibromyalgia Impact Questionnaire; FSS: Fatigue Severity Scale; FX: Flexibility; HR: heart rate; HRmax: maximum hear rate; HRR: heart rate reserve; ITT: intention to treat; LPA: lifestyle physical activity; RPE: rating of perceived exertion; RT: resistance exercise training; SBE: short bout exercise; SD: standard deviation; SF‐36: Short Form 36; VAS: visual aalogue scale; VO2: oxygen consumption
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adsuar 2012 | Physical activity intervention did not meet requirements for aerobic training (companion) |
| Ahlgren 2001 | Diagnosis ‐ trapezius myalgia |
| Alentorn‐Geli 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Alentorn‐Geli 2009 | Lacks required outcomes |
| Altan 2004 | Physical activity intervention did not meet requirements for aerobic training |
| Altan 2009 | Physical activity intervention did not meet requirements for aerobic training |
| Amanollahi 2013 | Physical activity intervention did not meet requirements for aerobic training |
| Andrade 2016 | Not an RCT |
| Ang 2007 | Randomization does not allow analysis of the effects of exercise |
| Aquino 2013 | Exercise requirements were not met |
| Arcos‐Carmona 2011 | Physical activity intervention did not meet requirements for aerobic training |
| Assis 2006 | Physical activity intervention did not meet requirements for aerobic training |
| Astin 2003 | Physical activity intervention did not meet requirements for aerobic training |
| Bailey 1999 | Not an RCT ( one ‐group design) |
| Bakker 1995 | Designated outcomes were not measured |
| Baniak 2015 | Study does not include exercise |
| Baptista 2012 | Physical activity intervention did not meet requirements for aerobic training |
| Bardal 2015 | Not an RCT |
| Bircan 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Bojner‐Horwitz 2006 | Physical activity intervention did not meet requirements for aerobic training |
| Bote 2013 | Not an RCT |
| Bressan 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Buckelew 1998 | Physical activity intervention did not meet requirements for aerobic training |
| Calandre 2010 | Physical activity intervention did not meet requirements for aerobic training |
| Carbonell‐Baeza 2011 | RCT protocol ( physical activity intervention did not meet requirements for aerobic training ) |
| Carbonell‐Baeza 2012 | RCT protocol (physical activity intervention did not meet requirements for aerobic training ) |
| Carson 2010 | Physical activity intervention did not meet requirements for aerobic training |
| Carson 2012 | Physical activity intervention did not meet requirements for aerobic training |
| Casanueva‐Fernandez 2012 | Exercise requirements were not met |
| Castel 2013 | Physical activity intervention did not meet requirements for aerobic training |
| Castel 2015 | Physical activity intervention did not meet requirements for aerobic training |
| Castro‐Sanchez 2011 | Exercise requirements were not met |
| Cedraschi 2004 | Physical activity intervention did not meet requirements for aerobic training |
| Clarke‐Jenssen 2014 | Physical activity intervention did not meet requirements for aerobic training |
| Cocke 2015 | Physical activity intervention did not meet requirements for aerobic training |
| Da Costa 2005 | Physical activity intervention did not meet requirements for aerobic training |
| da Silva 2007 | Physical activity intervention did not meet requirements for aerobic training |
| da Silva 2015 | RCT protocol (physical activity intervention did not meet requirements for aerobic training ) |
| Dal 2011 | Not an RCT |
| Dawson 2003 | Not an RCT ( one ‐group before‐after design) |
| De Andrade 2008 | Physical activity intervention did not meet requirements for aerobic training |
| de Araujo Farias 2013 | Physical activity intervention did not meet requirements for aerobic training |
| de Melo Vitorino 2006 | Physical activity intervention did not meet requirements for aerobic training |
| Delgado 2011 | RCT protocol (physical activity intervention did not meet requirements for aerobic training ) |
| Demir‐Gocmen 2013 | Physical activity intervention did not meet requirements for aerobic training |
| Ekici 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Etnier 2009 | Physical activity intervention did not meet requirements for aerobic training |
| Evcik 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Field 2003 | Physical activity intervention did not meet requirements for aerobic training |
| Fioravanti 2015 | Study does not include exercise |
| Gandhi 2000 | Not an RCT |
| Garcia‐Martinez 2011 | Physical activity intervention did not meet requirements for aerobic training |
| Gavi 2014 | Physical activity intervention did not meet requirements for aerobic training |
| Geel 2002 | Not an RCT |
| Genc 2002 | Physical activity intervention did not meet requirements for aerobic training |
| Genc 2015 | Physical activity intervention did not meet requirements for aerobic training |
| Giannotti 2014 | Physical activity intervention did not meet requirements for aerobic training |
| Gomes da Silva 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Gonzalez 2015 | Not an RCT |
| Gowans 1999 | Physical activity intervention did not meet requirements for aerobic training |
| Gowans 2002 | Focused on measurement issues of selected variables already reported in an included study; new variables did not include standard deviations |
| Gowans 2004 | Between ‐group data for exercise intervention not available |
| Guarino 2001 | Diagnosis did not meet requirements (Gulf War syndrome) |
| Gusi 2006 | Physical activity intervention did not meet requirements for aerobic training |
| Gusi 2008 | Physical activity intervention did not meet requirements for aerobic training (companion) |
| Gusi 2010 | Physical activity intervention did not meet requirements for aerobic training |
| Gusi Fuertes 2016 | RCT protocol (physical activity intervention did not meet requirements for aerobic training ) |
| Hakkinen 2001 | Physical activity intervention did not meet requirements for aerobic training |
| Hakkinen 2002 | Physical activity intervention did not meet requirements for aerobic training |
| Hammond 2006 | Physical activity intervention did not meet requirements for aerobic training |
| Han 1998 | Not a randomized study (geographical control) |
| Hecker 2011 | Physical activity intervention did not meet requirements for aerobic training |
| Hoeger Bement 2011 | Not an RCT |
| Hoeger Bement 2014 | Not an RCT |
| Hooten 2012 | Physical activity intervention did not meet requirements for aerobic training |
| Hsieh 2010 | Not an RCT |
| Huijnen 2016 | Not an RCT |
| Hunt 2000 | Diagnosis of FMS was not clear, even when the study author was contacted to clarify the diagnostic criteria used |
| Huyser 1997 | Not an RCT |
| Ide 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Ismael 2014 | Physical activity intervention did not meet requirements for aerobic training |
| Jentoft 2001 | Physical activity intervention did not meet requirements for aerobic training |
| Jones 2002 | Physical activity intervention did not meet requirements for aerobic training |
| Jones 2007 | Physical activity intervention did not meet requirements for aerobic training |
| Jones 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Jones 2009 | Not an RCT; a topical review |
| Jones 2011 | Not an RCT |
| Jones 2012 | Physical activity intervention did not meet requirements for aerobic training |
| Joshi 2009 | Physical activity intervention did not meet requirements for aerobic training |
| Kadetoff 2010 | Not an RCT |
| Kaleth 2013 | Randomization does not allow analysis of the effects of exercise |
| Kaleth 2016 | Randomization does not allow analysis of the effects of exercise |
| Karolinska Institutet 2015 | Study does not include exercise |
| Karper 2001 | Not a randomized trial (program evaluation) |
| Keel 1998 | Physical activity intervention did not meet requirements for aerobic training |
| Kendall 2000 | Study did not meet exercise criteria ( body awareness) |
| Kesiktas 2011 | Not an RCT |
| Khalsa 2009 | Not an RCT |
| Kibar 2015 | Physical activity intervention did not meet requirements for aerobic training |
| Kingsley 2005 | Diagnosis of FMS made by physician or rheumatologist, but when contacted, study authors did not verify the use of published criteria (eg, ACR 1990 classification) |
| Kingsley 2010 | Not an RCT |
| Klug 1989 | Not an RCT |
| Kroenke 2013 | Diagnosis; no data |
| Kurt 2016 | Physical activity intervention did not meet requirements for aerobic training |
| Lange 2011 | Not an RCT |
| Larsson 2013 | Physical activity intervention did not meet requirements for aerobic training |
| Latorre 2013 | Not an RCT |
| Latorre 2015 | Physical activity intervention did not meet requirements for aerobic training |
| Lemstra 2005 | Physical activity intervention did not meet requirements for aerobic training |
| Letieri 2013 | Physical activity intervention did not meet requirements for aerobic training |
| Liu 2012 | Physical activity intervention did not meet requirements for aerobic training |
| Lopez‐Pousa 2015 | Study does not include exercise |
| Lorig 2008 | Exercise requirements were not met |
| Lynch 2012 | Physical activity intervention did not meet requirements for aerobic training |
| López‐Rodríguez 2012 | Physical activity intervention did not meet requirements for aerobic training |
| Mannerkorpi 2000 | Physical activity intervention did not meet requirements for aerobic training |
| Mannerkorpi 2002 | Physical activity intervention did not meet requirements for aerobic training |
| Mannerkorpi 2009 | Physical activity intervention did not meet requirements for aerobic training |
| Martin 1996 | Physical activity intervention did not meet requirements for aerobic training |
| Martin 2014 | Physical activity intervention did not meet requirements for aerobic training |
| Martin‐Nogueras 2012 | Physical activity intervention did not meet requirements for aerobic training |
| Mason 1998 | Not a randomized trial ( participants enrolled for multimodal treatment compared with those who were unable to participate for insurance reasons) |
| Matsumoto 2011 | Data for FM were not isolated |
| Matsutani 2007 | Physical activity intervention did not meet requirements for aerobic training |
| Matsutani 2012 | Physical activity intervention did not meet requirements for aerobic training |
| McCain 1986 | Physical activity intervention did not meet requirements for aerobic training (companion) |
| McCain 1988 | Physical activity intervention did not meet requirements for aerobic training |
| Meiworm 2000 | Not a randomized trial ( participant s self ‐selected their groups) |
| Meyer 2000 | Between ‐group data for exercise intervention are not available |
| Mobily 2001 | Not an RCT ( case study) |
| Munguia‐Izquierdo 2007 | Physical activity intervention did not meet requirements for aerobic training |
| Munguia‐Izquierdo 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Mutlu 2013 | Physical activity intervention did not meet requirements for aerobic training (data for outcomes are not available) |
| Newcomb 2011 | Exercise requirements were not met |
| Nielen 2000 | Not a randomized trial (cross‐sectional case control study of fitness) |
| Nijs 2004 | Not an RCT |
| Norregaard 1997 | Physical activity intervention did not meet requirements for aerobic training |
| Offenbacher 2000 | Not an RCT ( narrative review) |
| Olivares 2011 | Physical activity intervention did not meet requirements for aerobic training (companion) |
| Oncel 1994 | Insufficient description of exercise (one group received "medical therapy and exercise"; no further information about the exercise intervention was given) |
| Palekar 2014 | Physical activity intervention did not meet requirements for aerobic training |
| Paolucci 2016 | Physical activity intervention did not meet requirements for aerobic training |
| Pastor 2014 | RCT protocol (physical activity intervention did not meet requirements for aerobic training ) |
| Perez‐ de la Cruz 2015 | Study does not allow analysis of fibromyalgia only |
| Peters 2002 | Diagnosis does not meet requirements (persistent unexplained symptoms) |
| Pfeiffer 2003 | Not an RCT (one ‐group before‐after design) |
| Piso 2001 | Not a randomized trial ‐ Our translator reported: "The authors wrote only how they recruited nine of the patients. They wrote nothing about if and how the patients were allocated to the two groups." We were unsuccessful on several attempts to contact study authors for clarification |
| Richards 2002 | Physical activity intervention did not meet requirements for aerobic training |
| Rivera 2004 | Physical activity intervention did not meet requirements for aerobic training |
| Rooks 2002 | Not an RCT (one‐group design) |
| Rooks 2007 | Physical activity intervention did not meet requirements for aerobic training |
| Salek 2005 | Not an RCT |
| Santana 2010 | Diagnosis does not meet requirements |
| Sa¤udo 2010 | Physical activity intervention did not meet requirements for aerobic training |
| Sañudo 2010 | Diagnosis does not meet requirements |
| Sañudo 2010a | Physical activity intervention did not meet requirements for aerobic training |
| Sañudo 2010b | Physical activity intervention did not meet requirements for aerobic training |
| Sañudo 2011 | Physical activity intervention did not meet requirements for aerobic training |
| Sañudo 2012 | Physical activity intervention did not meet requirements for aerobic training |
| Sañudo 2012a | Physical activity intervention did not meet requirements for aerobic training |
| Sañudo 2013 | Physical activity intervention did not meet requirements for aerobic training |
| Schmidt 2011 | Physical activity intervention did not meet requirements for aerobic training |
| Sigl‐Erkel 2011 | Not an RCT |
| Srikuea 2013 | Exercise requirements were not met |
| Steiner 2015 | Not a physical activity RCT; analysis does not isolate the effects of exercise |
| Suman 2009 | Not an RCT |
| Thieme 2003 | Did not meet exercise criteria (passive PT with light movement in water ‐ active exercise was too small a component and was not described or quantified sufficiently) |
| Thijssen 1992 | Not an RCT |
| Tiidus 1997 | One ‐group repeated ‐measures design |
| Tomas‐Carus 2007a | Physical activity intervention did not meet requirements for aerobic training |
| Tomas‐Carus 2007b | Physical activity intervention did not meet requirements for aerobic training |
| Tomas‐Carus 2007c | Physical activity intervention did not meet requirements for aerobic training |
| Tomas‐Carus 2007d | Physical activity intervention did not meet requirements for aerobic training |
| Tomas‐Carus 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Tomas‐Carus 2009 | Physical activity intervention did not meet requirements for aerobic training |
| Torres 2015 | Study does not include exercise |
| Uhlemann 2007 | Not an RCT |
| Valencia 2009 | Physical activity intervention did not meet requirements for aerobic training |
| Valim 2003 | Physical activity intervention did not meet requirements for aerobic training |
| Valim 2013 | Physical activity intervention did not meet requirements for aerobic training (companion) |
| Valkeinen 2004 | Physical activity intervention did not meet requirements for aerobic training |
| Valkeinen 2005 | Physical activity intervention did not meet requirements for aerobic training |
| Valkeinen 2008 | Physical activity intervention did not meet requirements for aerobic training |
| van Eijk‐Hustings 2013 | Physical activity intervention did not meet requirements for aerobic training |
| van Koulil 2010 | Physical activity intervention did not meet requirements for aerobic training |
| VanRavenstein 2014 | Not an RCT |
| vanSanten 2002 | Physical activity intervention did not meet requirements for aerobic training |
| vanSanten 2002a | Physical activity intervention did not meet requirements for aerobic training |
| Verstappen 1997 | Physical activity intervention did not meet requirements for aerobic training |
| Vlaeyen1996 | Mode of exercise was insufficientl described. "Each session ended with a physical exercise such as swimming or bicycling, excluding systematic physical or fitness training" |
| Wang 2010 | Physical activity intervention did not meet requirements for aerobic training |
| Wang 2015 | RCT protocol (physical activity intervention did not meet requirements for aerobic training ) |
| Westfall 1999 | Diagnosis does not meet requirements |
| Williams 2010 | Exercise requirements were not met |
| Worrel 2001 | Not an RCT ( one‐group design) |
| Yuruk 2008 | Physical activity intervention did not meet requirements for aerobic training |
| Zijlstra 2005 | Not an RCT |
FM: fibromyalgia; FMS: fibromyalgia syndrome; PT: physical therapy; RCT: randomized controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Bjersing 2012.
| Methods | 2 groups: moderate‐ to high‐intensity Nordic walking (NW) program; supervised low‐intensity walking (LIW) program Length: 15 weeks; follow‐up 30 weeks Study design: randomized clinical trial with parallel groups |
| Participants | Female:Male: 49:0 Age (pooled mean, range): 52 (48 to 56) years Inclusion: women with FM, 20 to 60 years of age, with interest in exercising outdoors twice a week for 15 weeks, participating in blood test at baseline and after the exercise period. To ensure that people would manage planned aerobic exercise, a bicycle test at 50 watts was included in the inclusion criteria. All included patients managed to perform the test. They were also invited to participate in an examination of cerebrospinal fluid, which, however, was not a criterion of inclusion. FM was defined by ACR 1990 criteria [1]: a history of long‐lasting generalized pain, and pain in at least 11 of 18 tender points examined by manual palpation Exclusion: patients not speaking or reading Swedish, other severe somatic or psychiatric disease, ongoing or planned physical therapy, including exercise, inability to accept times for planned exercise sessions Duration of illness (years (SD)): not assessed |
| Interventions |
Nordic walking (n = 26): Intensity: moderate to high, twice a week for 40 to 45 minutes Supervised low‐intensity walking (LIW) (n = 23) |
| Outcomes | Serum levels of free IGF‐1, pain (rating on a 0 to 100‐mm scale), pain threshold, and CR Sumax (6‐minute walk test) were examined. as well as CSF, neuropeptides, matrix metalloproteinase 3 (MMP‐3), and inflammatory cytokines Measurements at baseline (0), 15 and 30 weeks |
| Notes | Country: Sweden Language: English Study author contacted: not yet Funding source/declaration of interest: not assessed Trial registration: ClinicalTrials.govNCT00643006 |
Duruturk 2015.
| Methods | 2 groups: aerobic exercise (AE); balance exercise training Length: 6 weeks Study design: randomized clinical trial with parallel groups |
| Participants | Female:Male: 33:0 Age (years (SD)): 48.1 (7.4); 54.0 (6.6) Inclusion: medical practitioner’s referral for the study, willing to participate in an exercise group, an established diagnosis of fibromyalgia according to ACR 1990 diagnostic criteria, older than 18 years or age Exclusion: cardiovascular, pulmonary, orthopedic, or other systemic diseases that could limit exercise and balance testing and training; pregnancy, schizoaffective disorder, dementia, major depression or drug use that could interfere with balance control Duration of illness (years (SD)): proxy used "pain duration'"(months(SD)): 69.7 (54.0); 66.4 (108.5) |
| Interventions |
Aerobic exercise (n = 17 started, 14 completed and analyzed): supervised treadmill exercise sessions. Each session included 5 minutes of warm‐up and cool‐down periods (slow walking on the treadmill with no incline). Participants performed the exercise at 60%–75% of their maximal heart rate (calculated as 220 ‐ the age of the participant). Exercise intensity was also adjusted on the basis of participants' Modified Borg Scale‐rated perceived exertion. Intensity was increased if the Borg rate was < 4 and was decreased if the Borg rate was > 7. During exercise, heart rate, blood pressure, and electrocardiographic measurements were obtained at 5‐minute intervals Balance exercise training (n = 16 started, 12 completed and analyzed): The balance training intervention was performed in the same laboratory using the TIBS (Tetrax Sunlight Medical Ltd, 56 Miryam St, Ramat Gan, Israel). Frequency: 3 sessions/wk of 20–30 minutes of BE for 6 weeks. During balance training, a computer‐based system allowed 4 different kinds of postural biofeedback exercises (catch, speedball, sky ball, and gotcha) to be carried out. These exercises involved changing participants’ center of gravity while they followed a visual object, caught a fast‐moving object, or escaped from the object |
| Outcomes | Myalgic score, pain intensity (VAS), HRQL (FIQ), exercise testing (exercise duration, Borg scale, resting blood pressures (RBP), and maximal heart rate), Timed Up‐Go (TUG) and TIBS measurements Measurements taken at 0 and 6 weeks |
| Notes | Country: Berlin Language: English Study author contacted: not yet Funding source/declaration of interest: not assessed yet Trial registration: not assessed yet |
Espí‐López 2016.
| Methods | 3 groups: aerobic exercise training with music (n = 13); aerobic exercise at any rhythm (n = 13); control (n = 9) Length: 8 weeks Study design: randomized clinical trial with parallel groups |
| Participants | Female:Male: 33:2 Age (years (SD)): 53.4 (10.7), 53.1 (15.7), 57.1 (7.1) Inclusion: 30 to 80 years of age, diagnosis of fibromyalgia according to ACR 2010 Exclusion: deafness or limited hearing, vestibular disorders that compromise balance, very low vision or blindness, psychotic disorder, cognitive disabilities, decompensation or changes in medications Duration of illness (years (SD)): not assessed |
| Interventions | Each session consisted of 60 minutes Low‐impact aerobic exercise with music therapy (n = 13): Intervention was aimed at improving functionality; the session was divided into warm‐up (15 minutes) consisting of free range of motion exercises of upper and lower limbs and spine, and coordination‐based exercises of hands and feet, plus active stretching exercises of major muscles of arm, leg, and trunk. The main phase exercise component included 3 types of exercises/games, group dynamics, and aerobics (30 minutes), and cool‐down consisted of stretching for 15 minutes (major muscles of arm, leg, and trunk). Exercises were carried out to the rhythm of melodic music, adapted to the tastes of participants and the way the exercise was performed Therapeutic aerobic exercise at any rhythm (n = 13): Intervention was similar to low‐impact aerobic exercise with music therapy but was not performed to the rhythm of chosen melodic music Control group (n = 9): no intervention |
| Outcomes | Pain (Faces pain scale), depression (BDI), HRQL (FIQ), balance (Berg Balance Scale) Measurements at baseline and at 8 weeks |
| Notes | Country: Spain Language: English Stud author contacted: not yet Funding: not assessed yet Trial registration: not assessed yet |
Mendonca 2016.
| Methods | 3 groups: aerobic exercise training and active transcranial direct current stimulation (tDCS) intervention; aerobic exercise and placebo tDCS; placebo AE and tDCS Length: 8 weeks; follow‐up conducted 1 month (T3) and 2 months (T4) after the end of the intervention period Study design: randomized clinical trial with parallel groups |
| Participants | Female:Male: 44:1 Age (years (SD)): 44.5 (14), 48 (11.8), 49.9 (10.6) Inclusion: completed high school and age between 18 and 65 years Exclusion: on medication for pain control for less than 2 months; had been treated for depression for less than 2 months; had epilepsy, psychiatric disorder, or any recent episode of neurological disorder, such as idiopathic syncope; pregnant and infant‐aged; had metallic implants in the brain; using illicit drugs; had been undergoing some type of physical treatment for less than 2 months Duration of illness (years (SD)): proxy ‐ pain duration (months (SD)): 140.6 (72.2); 149.3 (111.1); 125.6 (100.2) |
| Interventions | Participants were divided into 3 intervention groups: tDCS/AE, which received active intervention of aerobic exercise training and active tDCS intervention; AE, which received active intervention of aerobic exercise and placebo tDCS; and tDCS, which received placebo AE and active intervention for tDCS |
| Outcomes | Intensity of pain, level of anxiety, quality of life, mood, pressure pain threshold, and cortical plasticity, as indexed by transcranial magnetic stimulation. All variables were measured 1 week before the beginning of the intervention (baseline), after the intervention period (T2), and during periods of follow‐up conducted 1 month (T3) and 2 months (T4) after the end of the intervention period |
| Notes | Country: Brazil Language: English Study author contacted: not yet Funding source/declaration of interest: not assessed yet Trial registry: not assessed yet |
Sanudo 2015.
| Methods | 2 groups: aerobic exercise (AE); usual care control Length: 24 weeks Study design: randomized clinical trial with parallel groups |
| Participants | Female:Male: 28:0 Age (years (SE)): 58 (2); 55 (2) Inclusion: diagnosis of fibromyalgia according to ACR guidelines Exclusion: pulmonary, cardiovascular, severe psychiatric, or inflammatory rheumatic disease. In addition, those who attended to psychological or physical therapy, or received exercise training, over the past year Duration of illness (years (SD)): not assessed |
| Interventions |
Aerobic exercise (n = 16): 2 aerobic exercise sessions per week of 45–60 minutes' duration including 15–20 minutes of steady state aerobic exercise at 60% to 65% of predicted maximum heart rate (HRmax) and 15 minutes of interval training at 75%‐80% HRmax (6 repetitions of 1.5 minutes, with 1 minute interpolated rest intervals) Usual care (n = 12) |
| Outcomes | Cardiac autonomic modulation (power spectral analysis of HRV). Symptom severity (pain VAS), sleep disturbance, stiffness, anxiety, and depression |
| Notes | Country: Spain Language: English Study author contacted: not yet Funding: University of Seville provided support for this study |
ACR: American College of Rheumatology; AE: aerobic exercise; ASES: Arthritis self‐efficacy scale; BDI: Beck Depression Inventory; BE: bout of exercise; CSF: cerebrospinal fluid; FIQ: Fibromyalgia Impact Questionnaire; FM: fibromyalgia; HRmax: maximum heart rate; HRQL: health‐related quality of life; HRV: heart rate variability; IGF‐1: insulin growth factor‐1; LIW: low‐intensity walking; MMP‐3: matrix metalloproteinase 3; NW: Nordic walking; RBP: resting blood pressure; SD: standard deviation; tDCS: transcranial direct current stimulation; TIBS: Tetraks interactive balance system; TUG: Timed Up‐Go; VAS: visual analogue scale
Differences between protocol and review
We prepared no new protocol for this review. This review presents a major update of previous reviews completed in 2002 and 2007 on exercise for fibromyalgia. Although this is an update, review team members ran the search from inception of the databases, screened studies, and extracted data from all included studies. Given growth in the literature, we have split this review into several reviews (ie, resistance, aquatic, mixed, aerobic, flexibility, and whole body vibration). Differences between the 2007 review and this update include the following.
Further refinement of the definition of what constitutes an aerobic exercise training intervention as required to provide clear criteria on the types of interventions that would and would not meet criteria for inclusion in this review.
Revisions to search terms, databases, and registries (see Appendix 12).
Changes in membership of the review team (new review authors and two consumers added).
Use of the "Risk of bias" tool (Higgins 2011a) instead of van Tulder 2003 and Jadad 1996 to assess quality of the evidence.
Outcomes presented to facilitate standardization of outcomes between reviews on fibromyalgia within Cochrane.
Adverse events and withdrawals for groups added to major outcomes to reflect other important potential harmful outcomes of aerobic exercise interventions.
Revisions to Cochrane methods described in version 5.1.0 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c), including addition of the Plain Language Summary, the "Summary of findings" table, and GRADEpro to judge evidence certainty.
Use of electronic data screening (Covidence) extraction methods (Google Docs) as opposed to paper‐based methods used in earlier versions of the review.
Subgroup analyses (including participant and intervention characteristics).
Post hoc sensitivity analysis.
Compliance with MECIR standards.
Contributions of authors
Initials correspond to review authors as they are listed under the review title.
JB: has been responsible for leading the aerobic exercise training review team, participating in discussion regarding review design and methods, screening studies for eligibility for inclusion in the review, supporting data extraction, performing methodological and statistical analysis, drafting and reviewing the manuscript. Read and approved the final manuscript.
AJB: has been responsible for co‐ordinating the Fibromyalgia and Exercise Team, designing and reviewing the review protocol, performing the literature search, assessing eligibility of studies, supporting data extraction, performing methodological and statistical analysis, drafting and reviewing the manuscript. Read and approved the final manuscript.
CLS: has been responsible for designing and reviewing the review protocol, screening studies for eligibility, supportingdata extraction, providing expert opinion on exercise physiology, supporting interpretation of study findings, assessing risk of bias, writing and reviewing the manuscript. Read and approved the final manuscript.
SMG: extracted data, wrote and reviewed drafts of the manuscript, contributed to creation of the Characteristics of included studies section. Read and approved the final manuscript.
TJO: collaborated with data extraction, provided content expertise on exercise physiology, supported interpretation of study findings, and contributed to writing and reviewing of drafts. Read and approved the final manuscript.
SYK: supported data extraction, contributed to creation of the Characteristics of included studies section, wrote and reviewed drafts and approved the final draft of the manuscript. Read and approved the final manuscript.
CB: performed literature searches; participated in discussion regarding methods; worked on plain language summary, flow chart, searches to support background and discussion sections of the manuscript; assisted with writing and reviewing of the manuscript. Read and approved the final manuscript.
HJAF: collaborated on data extraction, provided content expertise on exercise physiology, supported interpretation of study findings, and contributed to writing and reviewing of drafts. Read and approved the final manuscript.
Sources of support
Internal sources
School of Physical Therapy, University of Saskatchewan, Canada.
College of Medicine, University of Saskatchewan, Canada.
External sources
No sources of support supplied
Declarations of interest
We confirm that any present or past affiliations or other involvement in any organization or entity with an interest in the protocol that might lead me/us to have a real or perceived conflict of interest is listed below.
Julia Bidonde: none known.
Angela J Busch*: none known.
Candice L Schachter*: none known.
Tom J Overend: none known.
Soo Y Kim: none known.
Suelen M Góes: none known.
Catherine Boden: none known.
Heather JA Foulds: none known.
*To avoid conflict of interest, review authors (AJB, CLS) did not assess the RCT that they had authored (Schachter 2003) .
New
References
References to studies included in this review
Fontaine 2007 {published and unpublished data}
- Fontaine KR, Haas S. Effects of lifestyle physical activity on health status, pain, and function in adults with fibromyalgia syndrome. Journal of Musculoskeletal Pain 2007;15(1):3‐9. [Google Scholar]
Fontaine 2010 {published and unpublished data}
- Fontaine KR, Conn L, Clauw DJ. Effects of lifestyle physical activity in adults with fibromyalgia: results at follow‐up. Journal of Clinical Rheumatology 2011;17(2):64‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontaine KR, Conn L, Clauw DJ. Effects of lifestyle physical activity on perceived symptoms and physical function in adults with fibromyalgia: results of a randomized trial. Arthritis Research Therapy 2010;12(2):R55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gowans 2001 {published data only}
- Gowans SE, deHueck A, Voss S, Silaj A, Abbey SE. Six‐month and one‐year follow up of 23 weeks of aerobic exercise for individuals with fibromyalgia. Arthritis Care & Research 2004;51(6):890‐8. [DOI] [PubMed] [Google Scholar]
- Gowans SE, deHueck A, Voss S, Silaj A, Abbey SE, Reynolds WJ. Effect of a randomized, controlled trial of exercise on mood and physical function in individuals with fibromyalgia. Arthritis Care & Research 2001;45(6):519‐29. [DOI] [PubMed] [Google Scholar]
Kayo 2011 {published data only}
- Kayo AH, Peccin MS, Sanches CM, Trevisani VF. Effectiveness of physical activity in reducing pain in patients with fibromyalgia: a blinded randomized clinical trial. Rheumatology International 2011;32(8):2285‐92. [DOI] [PubMed] [Google Scholar]
King 2002 {published data only}
- King SJ, Wessel J, Bhambhani Y, Sholter D, Maksymowych W. The effects of exercise and education, individually or combined, in women with fibromyalgia. Journal of Rheumatology 2002;29(12):2620‐7. [PubMed] [Google Scholar]
Mannerkorpi 2010 {published and unpublished data}
- Mannerkorpi K, Nordeman L, Cider A, Jonsson G. Does moderate‐to‐high intensity Nordic walking improve functional capacity and pain in fibromyalgia? A prospective randomized controlled trial. Arthritis Research & Therapy 2010;12(5):R189. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mengshoel 1992 {published data only}
- Mengshoel AM, Forre O. Physical fitness training in patients with fibromyalgia. Musculoskeletal Pain 1993;1(4):267‐72. [Google Scholar]
- Mengshoel AM, Komnaes HB, Forre O. The effects of 20 weeks of physical fitness training in female patients with fibromyalgia. Clinical & Experimental Rheumatology 1992;10(4):345‐9. [PubMed] [Google Scholar]
Nichols 1994 {published data only}
- Nichols DS, Glenn TM. Effects of aerobic exercise on pain perception, affect, and level of disability in individuals with fibromyalgia. Physical Therapy 1994;74:327‐32. [DOI] [PubMed] [Google Scholar]
Ramsay 2000 {published data only}
- Ramsay C, Moreland J, Ho M, Joyce S, Walker S, Pullar T. An observer‐blinded comparison of supervised and unsupervised aerobic exercise regimens in fibromyalgia. Rheumatology (Oxford) 2000;39(5):501‐5. [DOI] [PubMed] [Google Scholar]
Sanudo 2010 {published data only}
- Sanudo B, Galiano D, Carrasco L, Blagojevic M, Hoyo M, Saxton J. Aerobic exercise versus combined exercise therapy in women with fibromyalgia syndrome: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2010;91(12):1838‐43. [DOI] [PubMed] [Google Scholar]
Schachter 2003 {published data only}
- Schachter CL, Busch AJ, Peloso P, Sheppard MS. The effects of short vs long bouts of aerobic exercise in sedentary women with fibromyalgia: a randomized controlled trial. Physical Therapy 2003;83(4):340‐58. [PubMed] [Google Scholar]
Sencan 2004 {published data only}
- Sencan S, Ak S, Karan A, Muslumanoglu L, Ozcan E, Berker E. A study to compare the therapeutic efficacy of aerobic exercise and paroxetine in fibromyalgia syndrome. Journal of Back & Musculoskeletal Rehabilitation 2004;17(2):57‐61. [Google Scholar]
Wigers 1996 {published data only}
- Finset A, Wigers SH, Gotestam KG. Depressed mood impedes pain treatment response in patients with fibromyalgia. Journal of Rheumatology 2004;31(5):976‐80. [PubMed] [Google Scholar]
- Wigers SH, Stiles TC, Vogel PA. Effects of aerobic exercise versus stress management treatment in fibromyalgia. A 4.5 year prospective study. Scandinavian Journal of Rheumatology 1996;25(2):77‐86. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adsuar 2012 {published data only}
- Adsuar JC, Pozo‐Cruz B, Parraca JA, Olivares PR, Gusi N. Whole body vibration improves the single‐leg stance static balance in women with fibromyalgia: a randomized controlled trial. Journal of Sports Medicine & Physical Fitness 2012;52(1):85‐91. [PubMed] [Google Scholar]
Ahlgren 2001 {published data only}
- Ahlgren C, Waling K, Kadi F, Djupsjobacka M, Thornell L, Sundelin G. Effects on physical performance and pain from three dynamic training programs for women with work‐related trapezius myalgia. Journal of Rehabilitation Medicine 2001;33(4):162‐9. [PubMed] [Google Scholar]
Alentorn‐Geli 2008 {published data only}
- Alentorn‐Geli E, Padilla J, Moras G, Lazaro Haro C, Fernandez‐Sola J. Six weeks of whole‐body vibration exercise improves pain and fatigue in women with fibromyalgia. Journal of Alternative & Complementary Medicine 2008;14(8):975‐81. [DOI] [PubMed] [Google Scholar]
Alentorn‐Geli 2009 {published data only}
- Alentorn‐Geli E, Moras G, Padilla J, Fernandez Sola J, Bennett RM, Lazaro Haro C, et al. Effect of acute and chronic whole‐body vibration exercise on serum insulin‐like growth factor‐1 levels in women with fibromyalgia. Journal of Alternative & Complementary Medicine 2009;15(5):573‐8. [DOI] [PubMed] [Google Scholar]
Altan 2004 {published data only}
- Altan L, Bingol U, Aykac M, Koc Z, Yurtkuran M. Investigation of the effects of pool‐based exercise on fibromyalgia syndrome. Rheumatology International 2004;24(5):272‐7. [DOI] [PubMed] [Google Scholar]
Altan 2009 {published data only}
- Altan L, Korkmaz N, Bingol U, Gunay B. Effect of Pilates training on people with fibromyalgia syndrome: a pilot study. Archives of Physical Medicine and Rehabilitation 2009;90(12):1983‐8. [DOI] [PubMed] [Google Scholar]
Amanollahi 2013 {published data only}
- Amanollahi A, Naghizadeh J, Khatibi A, Hollisaz MT, Shamseddini AR, Saburi A. Comparison of impacts of friction massage, stretching exercises and analgesics on pain relief in primary fibromyalgia syndrome: a randomized clinical trial. Tehran University Medical Journal 2013;70(10):616‐22. [Google Scholar]
Andrade 2016 {published data only}
Ang 2007 {published data only}
- Ang D, Kesavalu R, Lydon JR, Lane KA, Bigatti S. Exercise‐based motivational interviewing for female patients with fibromyalgia: a case series. Clinical Rheumatology 2007;26(11):1843‐9. [DOI] [PubMed] [Google Scholar]
Aquino 2013 {published data only}
- Aquino JK. Effect of group empowerment drumming on cognitive performance and mood in women with fibromyalgia. Califronia State University, Fullerton (Dissertation). California State University, Fullerton, 2013:118.
Arcos‐Carmona 2011 {published data only}
- Arcos‐Carmona IM, Castro‐Sanchez AM, Mataran‐Penarrocha GA, Gutierrez‐Rubio AB, Ramos‐Gonzalez E, Moreno‐Lorenzo C. Effects of aerobic exercise program and relaxation techniques on anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia: a randomized controlled trial [Effectos de un programa de ejercicios aerobicos y tecnicas de relajacion sobre el estado de ansiedad, calidad del sueno, depresion y calidad de vida en pacientes con fibromialgia: ensayo clinico aleatorizado]. Medicina Clinica 2011;137(9):398‐401. [DOI] [PubMed] [Google Scholar]
Assis 2006 {published data only}
- Assis MR, Duardo Silva L, Martins Barros Alves A, Pessanha AP, Valim V, Feldman D, et al. A randomized controlled trial of deep water running: clinical effectiveness of aquatic exercise to treat fibromyalgia. Arthritis & Rheumatism 2006;55(1):57‐65. [DOI] [PubMed] [Google Scholar]
Astin 2003 {published data only}
- Astin JA, Berman BM, Bausel B, Lee WL, Hochberg M, Forys KL. The efficacy of mindfulness meditation plus Qigong movement therapy in the treatment of fibromyalgia: a randomized controlled trial. Journal of Rheumatology 2003;30(10):2257‐62. [PubMed] [Google Scholar]
Bailey 1999 {published data only}
- Bailey A, Starr L, Alderson M, Moreland J. A comparative evaluation of a fibromyalgia rehabilitation program. Arthritis Care & Research 1999;12(5):336‐40. [DOI] [PubMed] [Google Scholar]
Bakker 1995 {published data only}
- Bakker C, Rutten M, Santen‐Hoeufft M, Bolwijn P, Doorslaer E, Linden S. Patient utilities in fibromyalgia and the association with other outcome measures. Journal of Rheumatology 1995;22:1536‐43. [PubMed] [Google Scholar]
Baniak 2015 {published data only}
Baptista 2012 {published data only}
- Baptista AS, Villela AL, Jones A, Natour J. Effectiveness of dance in patients with fibromyalgia: a randomized, single‐blind, controlled study. Clinical and Experimental Rheumatology 2012;30(6 Suppl 74):18‐23. [PubMed] [Google Scholar]
Bardal 2015 {published data only}
Bircan 2008 {published data only}
- Bircan C, Karasel SA, Akgun B, El O, Alper S. Effects of muscle strengthening versus aerobic exercise program in fibromyalgia. Rheumatology International 2008;28(6):527‐32. [DOI] [PubMed] [Google Scholar]
Bojner‐Horwitz 2006 {published data only}
- Bojner Horwitz E, Kowalski J, Theorell T, Anderberg UM. Dance/movement therapy in fibromyalgia patients: changes in self‐figure drawings and their relation to verbal self‐rating scales. Arts in Psychotherapy 2006;33(1):11‐25. [Google Scholar]
Bote 2013 {published data only}
- Bote ME, Garcia JJ, Hinchado MD, Otega E. Fibromyalgia: anti‐inflammatory and stress responses after acute moderate exercise. PLoS ONE 2013;e74524:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bressan 2008 {published data only}
- Bressan LR, Matsutani LA, Assumpcao A, Marques AP, Cabral CMN. Effects of muscle stretching and physical conditioning as physical therapy treatment for patients with fibromyalgia [Portuguese]. Revista Brasileira de Fisioterapia/Brazilian Journal of Physical Therapy 2008;12(2):88‐93. [Google Scholar]
Buckelew 1998 {published data only}
- Buckelew SP, Conway R, Parker J, Deuser WE, Read J, Witty TE, et al. Biofeedback/relaxation training and exercise interventions for fibromyalgia: a prospective trial. Arthritis & Rheumatism 1998;11(3):196‐209. [DOI] [PubMed] [Google Scholar]
Calandre 2010 {published data only}
- Calandre EP, Rodriguez‐Claro ML, Rico‐Villademoros F, Vilchez JS, Hidalgo J, Delgado‐Rodriguez A. Effects of pool‐based exercise in fibromyalgia symptomatology and sleep quality: a prospective randomized comparison between stretching and Tai Chi. Clinical and Experimental Rheumatology 2009;27(5 Suppl 56):S21‐8. [PubMed] [Google Scholar]
Carbonell‐Baeza 2011 {published data only}
- Carbonell‐Baeza A, Aparicio VA, Ortega FB, Cuevas AM, Alvarez IC, Ruiz JR, et al. Does a 3‐month multidisciplinary intervention improve pain, body composition and physical fitness in women with fibromyalgia?. British Journal of Sports Medicine 2011;45(15):1189‐95. [DOI] [PubMed] [Google Scholar]
Carbonell‐Baeza 2012 {published data only}
- Carbonell‐Baeza A, Ruiz JR, Ortega FB, Munguia‐Izquierdo D, Alvarez‐Gallardo IC, Segura‐Jimenez V, et al. Land‐ and water‐based exercise intervention in women with fibromyalgia: the al‐Andalus physical activity randomised controlled trial. BMC Musculoskeletal Disordder 2012;13(18):doi: 10.1186/1471‐2474‐13‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carson 2010 {published data only}
- Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD. A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain 2010;151(2):530‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carson 2012 {published data only}
- Carson JW, Carson KM, Jones KD, Mist SD, Bennett RM. Follow‐up of Yoga of Awareness for fibromyalgia: results at 3 months and replication in the wait‐list group. Clinical Journal of Pain 2012;28(9):804‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Casanueva‐Fernandez 2012 {published data only}
- Casanueva‐Fernandez B, Llorca J, Rubio JBI, Rodero‐Fernandez B, Gonzalez‐Gay MA. Efficacy of a multidisciplinary treatment program in patients with severe fibromyalgia. Rheumatology International 2012;32(8):2497‐502. [DOI] [PubMed] [Google Scholar]
Castel 2013 {published data only}
- Castel A, Fontova R, Montull S, Perinan R, Poveda MJ, Miralles I, et al. Efficacy of a multidisciplinary fibromyalgia treatment adapted for women with low educational levels: a randomized controlled trial [with consumer summary]. Arthritis Care & Research 2013;65(3):421‐31. [DOI] [PubMed] [Google Scholar]
Castel 2015 {published data only}
- Castel A, Castro S, Fontova R, Poveda MJ, Cascon‐Pereira R, Montull S, et al. Body mass index and response to a multidisciplinary treatment of fibromyalgia. Rheumatology International 2015;35(2):303‐14. [DOI] [PubMed] [Google Scholar]
Castro‐Sanchez 2011 {published data only}
- Castro‐Sanchez AM, Mataran‐Penarrocha GA, Arroyo‐Morales M, Saavedra‐Hernandez M, Fernandez‐Sola C, Moreno‐Lorenzo C. Effects of myofascial release techniques on pain, physical function, and postural stability in patients with fibromyalgia: a randomized controlled trial. Clinical Rehabilitation 2011;25(9):800‐13. [DOI] [PubMed] [Google Scholar]
Cedraschi 2004 {published data only}
- Cedraschi C, Desmeules J, Rapiti E, Baumgartner E, Cohen P, Finckh A, et al. Fibromyalgia: a randomised, controlled trial of a treatment programme based on self management. Annals of the Rheumatic Diseases 2004;63(3):290‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clarke‐Jenssen 2014 {published data only}
- Clarke‐Jenssen AC, Mengshoel AM, Staalesen SY, Forseth KO. Effect of a fybromyalgia rehabilitation programme in warm versus cold climate: a randomized controlled study. Journal of Rehabilitation Medicine (Stiftelsen Rehabiliteringsinformation) 2014;46(7):676‐83. [DOI] [PubMed] [Google Scholar]
Cocke 2015 {published data only}
- Cocke M. Altered Recovery Process after Fatiguing Exercise and Potential Benefits of Qigong in Patients. Lawrence, KS: University of Kansas (Dissertation),. University of Kansas, 2015; Vol. http://hdl.handle.net/1808/19381:96.
Da Costa 2005 {published data only}
- Costa D, Abrahamowicz M, Lowensteyn I, Bernatsky S, Dritsa M, Fitzcharles MA, et al. A randomized clinical trial of an individualized home‐based exercise programme for women with fibromyalgia. Rheumatology 2005;44(11):1422‐7. [DOI] [PubMed] [Google Scholar]
Dal 2011 {published data only}
- Dal U, Cimen OB, Incel NA, Adim M, Dag F, Erdogan AT, et al. Fibromyalgia syndrome patients optimize the oxygen cost of walking by preferring a lower walking speed. Journal of Musculoskeletal Pain 2011;19(4):212‐7. [Google Scholar]
da Silva 2007 {published data only}
- Silva GD, Lorenzi‐Filho G, Lage LV. Effects of yoga and the addition of Tui Na in patients with fibromyalgia. Journal of Alternative & Complementary Medicine 2007;13(10):1107‐13. [DOI] [PubMed] [Google Scholar]
da Silva 2015 {published data only}
- Silva MM, Albertini R, Leal‐Junior EC, Tarso Camillo de Carvalho, Silva JA Jr, Bussadori SK, et al. Effects of exercise training and photobiomodulation therapy (EXTRAPHOTO) on pain in women with fibromyalgia and temporomandibular disorder: study protocol for a randomized controlled trial. Trials 2015;16:252. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dawson 2003 {published data only}
- Dawson KA, Tiidus PM, Pierrynowski M, Crawford JP, Trotter J. Evaluation of a community‐based exercise program for diminishing symptoms of fibromyalgia . Physiotherapy Canada 2003;55:17‐22. [Google Scholar]
De Andrade 2008 {published data only}
- Andrade SC, Carvalho RFP, Soares AS, Abreu Freitas RP, Maderios Guerra LM, Vilar MJ. Thalassotherapy for fibromyalgia: a randomized controlled trial comparing aquatic exercises in sea water and water pool. Rheumatology International 2008;29:147‐52. [DOI: 10.1007/s00296-008-0644-2] [DOI] [PubMed] [Google Scholar]
de Araujo Farias 2013 {published data only}
- Araujo Farias D, Abrahao AA, Rossato M, Bezerra Ede S. Effects of two different training methods in women with fibromyalgia syndrome. Research in Sports Medicine 2013;21(3):280‐5. [DOI] [PubMed] [Google Scholar]
Delgado 2011 {published data only}
- Delgado M. Land‐ and water‐based exercise intervention in women with fibromyalgia: the al‐Andalus physical activity randomised control trial. ClinicalTrials.gov; ID: NCT01490281, 2011. [ClinicalTrials.gov ID: NCT01490281]
de Melo Vitorino 2006 {published data only}
- Vitorino DF, Carvalho LB, do Prado GF. Hydrotherapy and conventional physiotherapy improve total sleep time and quality of life of fibromyalgia patients: randomized clinical trial. Sleep Medicine 2006;7:293‐6. [DOI: 10.1016/j.sleep.2005.09.002] [DOI] [PubMed] [Google Scholar]
Demir‐Gocmen 2013 {published data only}
- Demir‐Gocmen D, Altan L, Korkmaz N, Arabaci R. Effect of supervised exercise program including balance exercises on the balance status and clinical signs in patients with fibromyalgia. Rheumatology International 2013;33(3):743‐50. [DOI] [PubMed] [Google Scholar]
Ekici 2008 {published data only}
- Ekici G, Yakut E, Akbayrak T. Effects of pilates exercises and connective tissue manipulation on pain and depression in females with fibromyalgia: a randomized controlled trial [Turkish]. Fizyoterapi Rehabilitasyon 2008;19(2):47‐54. [Google Scholar]
Etnier 2009 {published data only}
- Etnier JL, Karper WB, Gapin JI, Barella LA, Chang YK, Murphy KJ. Exercise, fibromyalgia, and fibrofog: a pilot study. Journal of Physical Activity & Health 2009;6(2):239‐46. [DOI] [PubMed] [Google Scholar]
Evcik 2008 {published data only}
- Evcik D, Yugit I, Pusak H, Kavuncu V. Effectiveness of aquatic therapy in the treatment of fibromyalgia syndrome: a randomized controlled open study. Rheumatology International 2008;28(9):885‐90. [DOI: 10.1007/s00296-008-0538-3] [DOI] [PubMed] [Google Scholar]
Field 2003 {published data only}
- Field T, Delage J, Hernandez Reif M. Movement and massage therapy reduce fibromyalgia pain. Journal of Bodywork and Movement Therapies 2003;7(1):49‐52. [Google Scholar]
Fioravanti 2015 {published data only}
- Fioravanti A. Efficacy and tolerability of balneotherapy with mineral water named "Debole of Vetriolo" in fibromyalgia syndrome (VET). ClinicalTrials.gov; Vol. ID: NCT02548065, 2015.
Gandhi 2000 {published data only}
- Gandhi N. Effect of an exercise program on quality of life of women with fibromyalgia. Effect of an Exercise Program on Quality of Life of Women With Fibromyalgia. Eugene, OR: Microform Publications, University of Oregon, 2000. [Google Scholar]
Garcia‐Martinez 2011 {published data only}
- Garcia‐Martinez AM, Paz JA, Marquez S. Effects of an exercise programme on self‐esteem, self‐concept and quality of life in women with fibromyalgia: a randomized controlled trial. Rheumatology International 2011;32(7):1869‐76. [DOI] [PubMed] [Google Scholar]
Gavi 2014 {published data only}
- Gavi MB, Vassalo DV, Amaral FT, Macedo DC, Gava PL, Dantas EM, et al. Strengthening exercises improve symptoms and quality of life but do not change autonomic modulation in fibromyalgia: a randomized clinical trial. PLoS One 2014;9(3):e90767. [DOI] [PMC free article] [PubMed] [Google Scholar]
Geel 2002 {published data only}
- Geel SE, Robergs RA. The effect of graded resistance exercise on fibromyalgia symptoms and muscle bioenergetics: a pilot study. Arthritis & Rheumatism 2002;47(1):82‐6. [DOI] [PubMed] [Google Scholar]
Genc 2002 {published data only}
- Genc A, Sagiroglu E. Comparison of two different exercise programs in fibromyalgia treatment [Turkish]. Fizyoterapi Rehabilitasyon 2002;13(2):90‐5. [Google Scholar]
Genc 2015 {published data only}
- Genc A, Tur BS, Aytur YK, Oztuna D, Erdogan MF. Does aerobic exercise affect the hypothalamic‐pituitary‐adrenal hormonal response in patients with fibromyalgia syndrome?. Journal of Physical Therapy Science 2015;27(7):2225‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Giannotti 2014 {published data only}
- Giannotti E, Koutsikos K, Pigatto M, Rampudda ME, Doria A, Masiero S. Medium‐/long‐term effects of a specific exercise protocol combined with patient education on spine mobility, chronic fatigue, pain, aerobic fitness and level of disability in fibromyalgia. Biomed Research International 2014;2014:474029. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gomes da Silva 2008 {published data only}
- Silva G, Fernandes T, Yuri SE, Aparecida MC, Silva PFH, Targino PG. Comparison of transcutaneous electrical nerve stimulation and hydrotherapy effects on pain, flexibility and quality of life in patients with fibromyalgia. Fisioterapia e Pesquisa 2008;15:118‐24. [Google Scholar]
Gonzalez 2015 {published data only}
Gowans 1999 {published data only}
- Gowans SE, deHueck A, Voss S, Richardson M. A randomized, controlled trial of exercise and education for individuals with fibromyalgia. Arthritis Care & Research 1999;12(2):120‐8. [DOI] [PubMed] [Google Scholar]
Gowans 2002 {published data only}
- Gowans SE, deHueck A, Abbey SE. Measuring exercise‐induced mood changes in fibromyalgia: a comparison of several measures. Arthritis & Rheumatism 2002;47:603‐9. [DOI] [PubMed] [Google Scholar]
Gowans 2004 {published data only}
- Gowans SE, deHueck A, Voss S, Silaj A, Abbey SE. Six‐month and one‐year followup of 23 weeks of aerobic exercise for individuals with fibromyalgia. Arthritis Care & Research 2004;51(6):890‐8. [DOI] [PubMed] [Google Scholar]
Guarino 2001 {published data only}
- Guarino P, Peduzzi P, Donta ST, et al. A multicenter two by two factorial trial of cognitive behavioral therapy and aerobic exercise for Gulf War veterans' illnesses: design of a Veterans Affairs Cooperative Study (CSP #470). Controlled Clinical Trials 2001;22:310‐32. [DOI] [PubMed] [Google Scholar]
Gusi 2006 {published data only}
- Gusi N, Tomas‐Carus P, Hakkinen A, Hakkinen K, Ortega‐Alonso A. Exercise in waist‐high warm water decreases pain and improves health‐related quality of life and strength in the lower extremities in women with fibromyalgia. Arthritis & Rheumatism 2006;55(1):66‐73. [DOI] [PubMed] [Google Scholar]
Gusi 2008 {published data only}
- Gusi N, Tomas‐Carus P. Cost‐utility of an 8‐month aquatic training for women with fibromyalgia: a randomized controlled trial. Arthritis Research & Therapy 2008;10(1):R24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gusi 2010 {published data only}
- Gusi N, Parraca JA, Olivares PR, Leal A, Adsuar JC. Tilt vibratory exercise and the dynamic balance in fibromyalgia: a randomized controlled trial. Arthritis Care & Research 2010;62(8):1072‐8. [DOI] [PubMed] [Google Scholar]
Gusi Fuertes 2016 {published data only}
- Gusi Fuertes N. Effects of a virtual reality‐based physical exercise in fibromyalgia patients. A randomized controlled trial. Australian New Zealand Clinical Trials Registry Vol. ACTRN12615000836538, 2016.
Hakkinen 2001 {published data only}
- Hakkinen A, Hakkinen K, Hannonen P, Alen M. Strength training induced adaptations in neuromuscular function of premenopausal women with fibromyalgia: comparison with healthy women. Annals of the Rheumatic Diseases 2001;60(1):21‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hakkinen 2002 {published data only}
- Hakkinen K, Pakarinen A, Hannonen P, Hakkinen A, Airaksinen O, Valkeinen H, et al. Effects of strength training on muscle strength, cross‐sectional area, maximal electromyographic activity, and serum hormones in premenopausal women with fibromyalgia. Journal of Rheumatology 2002;29(6):1287‐95. [PubMed] [Google Scholar]
Hammond 2006 {published data only}
- Hammond A, Freeman K. Community patient education and exercise for people with fibromyalgia: a parallel group randomized controlled trial. Clinical Rehabilitation 2006;20(10):835‐46. [DOI] [PubMed] [Google Scholar]
Han 1998 {published data only}
- Han SS. Effects of a self‐help program including stretching exercise on symptom reduction in patients with fibromyalgia. Taehan Kanho 1998;37:78‐80. [PubMed] [Google Scholar]
Hecker 2011 {published data only}
- Hecker CD, Melo C, Silva Tomazoni S, Brandao Lopes Martins RA, Pinto Leal EC. Analysis of effects of kinesiotherapy and hydrokinesiotherapy on the quality of life of patients with fibromyalgia ‐ a randomized clinical trial [Analise dos efeitos da cinesioterapia e da hidrocinesioterapia sobre a qualidade de vida de pacientes com fibromialgia ‐ um ensaio clinico randomizado]. Fisioterapia em Movimento 2011;24(1):57‐64. [Google Scholar]
Hoeger Bement 2011 {published data only}
Hoeger Bement 2014 {published data only}
- Hoeger Bement MK, Weyer AD, Yoon T, Hunter SK. Corticomotor excitability during a noxious stimulus before and after exercise in women with fibromyalgia. Journal of Clinical Neurophysiology 2014;31(1):94‐8. [DOI] [PubMed] [Google Scholar]
Hooten 2012 {published data only}
- Hooten WM, Qu W, Townsend CO, Judd JW. Effects of strength vs aerobic exercise on pain severity in adults with fibromyalgia: a randomized equivalence trial. Pain 2012;153(4):915‐23. [DOI] [PubMed] [Google Scholar]
Hsieh 2010 {published data only}
- Hsieh L‐F, Chien H‐L, Chuang C‐C, Bai C‐H. Aerobic capacity is reduced in Chinese women with primary fibromyalgia syndrome. Journal of Musculoskeletal Pain 2010;18(3):216‐25. [Google Scholar]
Huijnen 2016 {published data only}
Hunt 2000 {published data only}
- Hunt J, Bogg J. An evaluation of the impact of a fibromyalgia self‐management programme on patient morbidity and coping. Advancing in Physiotherapy 2000;2(4):168‐75. [Google Scholar]
Huyser 1997 {published data only}
- Huyser B, Buckelew SP, Hewett JE, Johnson JC. Factors affecting adherence to rehabilitation interventions for individuals with fibromyalgia. Rehabilitation Psychology 1997;42:75‐91. [Google Scholar]
Ide 2008 {published data only}
- Ide MR, Laurindo LMM, Rodrigues‐Junior AL, Tanaka C. Effect of aquatic respiratory exercise‐based program in patients with fibromyalgia. APLAR Journal of Rheumatology 2008;11(2):131‐40. [Google Scholar]
Ismael 2014 {published data only}
- Ismael Martins MR, Gritti CC, Dos Santos Junior R, Araujo MCL, Dias LC, D'All Aglio Foss MH, et al. Randomized controlled trial of a therapeutic intervention group in patients with fibromyalgia syndrome. Revista Brasileira de Reumatologia 2014;54:179‐84. [PubMed] [Google Scholar]
Jentoft 2001 {published data only}
- Jentoft ES, Kvalvik AG, Mengshoel AM. Effects of pool‐based and land‐based aerobic exercise on women with fibromyalgia/chronic widespread muscle pain. Arthritis & Rheumatism 2001;45:42‐7. [DOI] [PubMed] [Google Scholar]
Jones 2002 {published data only}
- Jones KD, Burckhardt CS, Clark SR, Bennett RM, Potempa KM. A randomized controlled trial of muscle strengthening versus flexibility training in fibromyalgia. Journal of Rheumatology 2002;29(5):1041‐8. [PubMed] [Google Scholar]
Jones 2007 {published data only}
- Jones KD, Deodhar AA, Burckhardt CS, Perrin NA, Hanson GC, Bennett RM. A combination of 6 months of treatment with pyridostigmine and triweekly exercise fails to improve insulin‐like growth factor‐I levels in fibromyalgia, despite improvement in the acute growth hormone response to exercise. Journal of Rheumatology 2007;34(5):1103‐11. [PubMed] [Google Scholar]
Jones 2008 {published data only}
- Jones KD, Burckhardt CS, Deodhar AA, Perrin NA, Hanson GC, Bennett RM. A six‐month randomized controlled trial of exercise and pyridostigmine in the treatment of fibromyalgia. Arthritis & Rheumatism 2008;58(2):612‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2009 {published data only}
- Jones KD, Liptan GL. Exercise interventions in fibromyalgia: clinical applications from the evidence. Rheumatic Disease Clinics North America 2009;35(2):373‐91. [DOI] [PubMed] [Google Scholar]
Jones 2011 {published data only}
- Jones KD. Nordic walking in fibromyalgia: a means of promoting fitness that is easy for busy clinicians to recommend. Arthritis Research & Therapy 2011;13(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2012 {published data only}
- Jones K, Sherman C, Mist S, Carson J, Bennett R, Li F. A randomized controlled trial of 8‐form Tai Chi improves symptoms and functional mobility in fibromyalgia patients. BMC Complementary and Alternative Medicine 2012;12:1205‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Joshi 2009 {published data only}
- Joshi MN, Joshi R, Jain AP. Effect of amitriptyline vs. physiotherapy in management of fibromyalgia syndrome: what predicts a clinical benefit?. Journal of Postgraduate Medicine 2009;55(3):185‐9. [DOI] [PubMed] [Google Scholar]
Kadetoff 2010 {published data only}
- Kadetoff D, Kosek E. Evidence of reduced sympatho‐adrenal and hypothalamic‐pituitary activity during static muscular work in patients with fibromyalgia. Journal of Rehabilitation Medicine 2010;42(8):765‐72. [DOI] [PubMed] [Google Scholar]
Kaleth 2013 {published data only}
- Kaleth AS, Saha CK, Jensen MP, Slaven JE, Ang DC. Effect of moderate to vigorous physical activity on long‐term clinical outcomes and pain severity in fibromyalgia. Arthritis Care & Research 2013;65(8):1211‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaleth 2016 {published data only}
- Kaleth AS, Slaven JE, Ang DC. Does increasing steps per day predict improvement in physical function and pain interference in adults with fibromyalgia?. Arthritis Care & Research 2016; Vol. 66, issue 12:1887‐94. [DOI] [PMC free article] [PubMed]
Karolinska Institutet 2015 {published data only}
- Karolinska Institutet. Internet‐based exposure‐based therapy for fibromyalgia: a randomized controlled trial. ClinicalTrials.gov; Vol. ID NCT02638636, 2015.
Karper 2001 {published data only}
- Karper WB, Hopewell R, Hodge M. Exercise program effects on women with fibromyalgia syndrome. Clinical Nurse Specialist 2001;15:67‐75. [DOI] [PubMed] [Google Scholar]
Keel 1998 {published data only}
- Keel PJ, Bodoky C, Gerhard U, Muller W. Comparison of integrated group therapy and group relaxation training for fibromyalgia. Clinical Journal of Pain 1998;14(3):232‐8. [DOI] [PubMed] [Google Scholar]
Kendall 2000 {published data only}
- Kendall SA, Brolin MK, Soren B, Gerdle B, Henriksson KG. A pilot study of body awareness programs in the treatment of fibromyalgia syndrome. Arthritis Care & Research 2000;13:304‐11. [DOI] [PubMed] [Google Scholar]
Kesiktas 2011 {published data only}
Khalsa 2009 {published data only}
- Khalsa KPS. Bodywork for fibromyalgia: alternative therapies soothe the pain. Massage & Bodywork 2009, (May/June):80‐9. [Google Scholar]
Kibar 2015 {published data only}
- Kibar S, Yildiz HE, Ay S, Evcik D, Ergin ES. New approach in fibromyalgia exercise program: a preliminary study regarding the effectiveness of balance training. Archives of Physical Medicine and Rehabilitation 2015;96(9):1576‐82. [DOI] [PubMed] [Google Scholar]
Kingsley 2005 {published data only}
- Kingsley JD, Panton LB, Toole T, Sirithienthad P, Mathis R, McMillan V. The effects of a 12‐week strength‐training program on strength and functionality in women with fibromyalgia. Archives of Physical Medicine and Rehabilitation 2005;86(9):1713‐21. [DOI] [PubMed] [Google Scholar]
Kingsley 2010 {published data only}
- Kingsley JD, McMillan V, Figueroa A. The effects of 12 weeks of resistance exercise training on disease severity and autonomic modulation at rest and after acute leg resistance exercise in women with fibromyalgia. Archives of Physical Medicine and Rehabilitation 2010;91(10):1551‐7. [DOI] [PubMed] [Google Scholar]
Klug 1989 {published data only}
- Klug GA, McAuley E, Clark S. Factors influencing the development and maintenance of aerobic fitness: lessons applicable to the fibrositis syndrome. Journal of Rheumatology 1989;19 Suppl:30‐9. [PubMed] [Google Scholar]
Kroenke 2013 {published data only}
- Kroenke Kurt. Telephone‐based cognitive‐behavioural therapy and a structured exercise programme are effective for chronic widespread pain (fibromyalgia). Evidence Based Medicine 2013;18(1):23‐4. [DOI] [PubMed] [Google Scholar]
Kurt 2016 {published data only}
- Kurt EE, Kocak FA, Erdem HR, Tuncay F, Kelez F. Which non‐pharmacological treatment is more effective on clinical parameters in patients with fibromyalgia: balneotherapy or aerobic exercise?. Archives of Rheumatology 2016; Vol. 31, issue 2:162‐9. [DOI] [PMC free article] [PubMed]
Lange 2011 {published data only}
Larsson 2013 {published data only}
- Larsson A, Palstam A, Lofgren M, Ernberg M, Bjersing J, Bileviciute‐Ljungar I, et al. Resistance exercise improves muscle strength, health status and pain intensity in fibromyalgia ‐ a randomized controlled trial. Arthritis Research & Therapy 2015;17:161. [DOI] [PMC free article] [PubMed] [Google Scholar]
Latorre 2013 {published data only}
- Latorre PA, Santos MA, Heredia‐Jimenez JM, Delgado‐Fernandez M, Soto VM, Manas A, et al. Effect of a 24‐week physical training programme (in water and on land) on pain, functional capacity, body composition and quality of life in women with fibromyalgia. Clinical and Experimental Rheumatology 2013;31(6 Suppl 79):S72‐80. [PubMed] [Google Scholar]
Latorre 2015 {published data only}
- Latorre Roman PA, Santos E Campos MA, Garcia‐Pinillos F. Effects of functional training on pain, leg strength, and balance in women with fibromyalgia. Modern Rheumatology 2015;25(6):943‐7. [DOI] [PubMed] [Google Scholar]
Lemstra 2005 {published data only}
- Lemstra M, Olszynski WP. The effectiveness of multidisciplinary rehabilitation in the treatment of fibromyalgia: a randomized controlled trial. Clinical Journal of Pain 2005;21(2):166‐74. [DOI] [PubMed] [Google Scholar]
Letieri 2013 {published data only}
- Letieri RV, Furtado GE, Letieri M, Goes SM, Pinheiro CJ, Veronez SO, et al. Pain, quality of life, self perception of health and depression in patients with fibromyalgia, submitted to hydrocinesiotherapy [Dor, qualidade de vida, autopercepção de saúde e depressão de pacientes com fibromialgia, tratados com hidrocinesioterapia]. Revista Brasileira de Reumatologia 2013;53(6):494‐500. [DOI] [PubMed] [Google Scholar]
Liu 2012 {published data only}
- Liu W, Zahner L, Cornell M, Le T, Ratner J, Wang Y, et al. Benefit of Qigong exercise in patients with fibromyalgia: a pilot study. International Journal of Neuroscience 2012;122(11):657‐64. [DOI] [PubMed] [Google Scholar]
Lopez‐Pousa 2015 {published data only}
- Lopez‐Pousa S, Bassets PG, Monserrat‐Vila S, Gracia BM, Hidalgo CJ, Garre‐Olmo J. Sense of well‐being in patients with fibromyalgia: aerobic exercise program in a mature forest‐A pilot study. Evidence Based Complementary and Alternative Medicine 2015;2015:614783. [DOI] [PMC free article] [PubMed] [Google Scholar]
López‐Rodríguez 2012 {published data only}
- López‐Rodríguez MM, Castro‐Sánchez AM, Fernández‐Martínez M, Matarán‐Peñarrocha GA, Rodríguez‐Ferrer ME. Comparison between aquatic‐biodanza and stretching for improving quality of life and pain in patients with fibromyalgia. Atencion Primaria 2012;44(11):641‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lorig 2008 {published data only}
- Lorig KR, Ritter PL, Laurent DD, Plant K, Lorig KR, Ritter PL. The internet‐based arthritis self‐management program: a one‐year randomized trial for patients with arthritis or fibromyalgia. Arthritis & Rheumatism 2008;59(7):1009‐17. [DOI] [PubMed] [Google Scholar]
Lynch 2012 {published data only}
- Lynch M, Sawynok J, Hiew C, Marcon D. A randomized controlled trial of qigong for fibromyalgia. Arthritis Research & Therapy 2012;14(4):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mannerkorpi 2000 {published data only}
- Mannerkorpi K, Nyberg B, Ahlmen M, Ekdahl C. Pool exercise combined with an education program for patients with fibromyalgia syndrome. A prospective, randomized study. Journal of Rheumatology 2000;27(10):2473‐81. [PubMed] [Google Scholar]
Mannerkorpi 2002 {published data only}
- Mannerkorpi K, Ahlmen M, Ekdahl C. Six‐ and 24‐month follow‐up of pool exercise therapy and education for patients with fibromyalgia. Scandinavian Journal of Rheumatology 2002;31(5):306‐10. [DOI] [PubMed] [Google Scholar]
Mannerkorpi 2009 {published data only}
- Mannerkorpi K, Nodeman L, Eericsson A, Arndorw M, GAUSG. Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomized controlled trial and subgroup analysis. Journal of Rehabilitation Medicine 2009;41:751‐60. [DOI] [PubMed] [Google Scholar]
Martin 1996 {published data only}
- Martin L, Nutting A, MacIntosh BR, Edworthy SM, Butterwick D, Cook J. An exercise program in the treatment of fibromyalgia. Journal of Rheumatology 1996;23(6):1050‐3. [PubMed] [Google Scholar]
Martin 2014 {published data only}
- Martin J, Torre F, Padierna A, Aguirre U, Gonzalez N, Matellanes B, et al. Impact of interdisciplinary treatment on physical and psychosocial parameters in patients with fibromyalgia: results of a randomised trial. International Journal of Clinical Practice 2014;68:618‐27. [DOI] [PubMed] [Google Scholar]
Martin‐Nogueras 2012 {published data only}
- Martin‐Nogueras AM, Calvo‐Arenillas JI. Efficacy of physiotherapy treatment on pain and quality of life in patients with fibromyalgia [Spanish]. Rehabilitacion 2012;46(3):199‐206. [Google Scholar]
Mason 1998 {published data only}
- Mason LW, Goolkasian P, McCain GA. Evaluation of multimodal treatment program for fibromyalgia. Journal of Behavioral Medicine 1998;21(2):163‐78. [DOI] [PubMed] [Google Scholar]
Matsumoto 2011 {published data only}
- Matsumoto S, Shimodozono M, Etoh S, Miyata R, Kawahira K. Effects of thermal therapy combining sauna therapy and underwater exercise in patients with fibromyalgia. Complementary Therapies in Clinical Practice 2011;17(3):162‐6. [DOI] [PubMed] [Google Scholar]
Matsutani 2007 {published data only}
- Matsutani LA, Marques AP, Ferreira EA, Assumpcao A, Lage LV, Casarotto RA, et al. Effectiveness of muscle stretching exercises with and without laser therapy at tender points for patients with fibromyalgia. Clinical and Experimental Rheumatology 2007;25(3):410‐5. [PubMed] [Google Scholar]
Matsutani 2012 {published data only}
- Matsutani LA, Assumpcao A, Marques AP. Stretching and aerobic exercises in the treatment of fibromyalgia: pilot study [Portuguese]. Fisioterapia em Movimento 2012;25(2):411‐8. [Google Scholar]
McCain 1986 {published data only}
- McCain GA. Role of physical fitness training in the fibrositis/fibromyalgia syndrome. American Journal of Medicine 1986;81(3A):73‐7. [DOI] [PubMed] [Google Scholar]
McCain 1988 {published data only}
- McCain GA, Bell DA, Mai FM, Halliday PD. A controlled study of the effects of a supervised cardiovascular fitness training program on the manifestations of primary fibromyalgia. Arthritis & Rheumatism 1988;31(9):1135‐41. [DOI] [PubMed] [Google Scholar]
Meiworm 2000 {published data only}
- Meiworm L, Jakob E, Walker UA, Peter HH, Keul J. Patients with fibromyalgia benefit from aerobic endurance exercise. Clinical Rheumatology 2000;19(4):253‐7. [DOI] [PubMed] [Google Scholar]
Meyer 2000 {published data only}
- Meyer BB, Lemley KJ. Utilizing exercise to affect the symptomology of fibromyalgia: a pilot study. Medicine and Science in Sports and Exercise 2000;32(10):1691‐97. [DOI] [PubMed] [Google Scholar]
Mobily 2001 {published data only}
- Mobily KE, Verburg MD. Aquatic therapy in community‐based therapeutic recreation: pain management in a case of fibromyalgia. Therapeutic Recreation Journal 2001;35:57‐69. [Google Scholar]
Munguia‐Izquierdo 2007 {published data only}
- Munguia‐Izquierdo D, Legaz‐Arrese A. Exercise in warm water decreases pain and improves cognitive function in middle‐aged women with fibromyalgia. Clinical and Experimental Rheumatology 2007;25(6):823‐30. [PubMed] [Google Scholar]
Munguia‐Izquierdo 2008 {published data only}
- Munguia‐Izquierdo D, Legaz‐Arrese A. Assessment of the effects of aquatic therapy on global symptomatology in patients with fibromyalgia syndrome: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2008;89:2250‐7. [DOI] [PubMed] [Google Scholar]
Mutlu 2013 {published data only}
- Mutlu B, Paker N, Bugdayci D, Tekdos D, Kesiktas N. Efficacy of supervised exercise combined with transcutaneous electrical nerve stimulation in women with fibromyalgia: a prospective controlled study. Rheumatology International 2013;33(3):649‐655. [DOI] [PubMed] [Google Scholar]
Newcomb 2011 {published data only}
- Newcomb LW, Koltyn KF, Morgan WP, Cook DB. Influence of preferred versus prescribed exercise on pain in fibromyalgia. Medicine and Science in Sports and Exercise 2011;43(6):1106‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nielen 2000 {published data only}
- Nielens H, Boisset V, Masquelier E. Fitness and perceived exertion in patients with fibromyalgia syndrome. Clinical Journal of Pain 2000;16(3):209‐13. [DOI] [PubMed] [Google Scholar]
Nijs 2004 {published data only}
- Nijs J, Parijs M. Long‐term effectiveness of pool exercise therapy and education in patients with fibromyalgia. Journal of Chronic Fatigue Syndrome 2004;12(3):73‐9. [Google Scholar]
Norregaard 1997 {published data only}
- Norregaard J, Lykkegaard JJ, Mehlsen J, Danneskiold Samsoe B. Exercise training in treatment of fibromyalgia. Journal of Musculoskeletal Pain 1997;5(1):71‐9. [Google Scholar]
Offenbacher 2000 {published data only}
- Offenbacher M, Stucki G. Physical therapy in the treatment of fibromyalgia. Scandinavian Journal of Rheumatology 2000;Suppl 29:78. [DOI] [PubMed] [Google Scholar]
Olivares 2011 {published data only}
- Olivares PR, Gusi N, Parraca JA, Adsuar JC, Pozo‐Cruz B. Tilting whole body vibration improves quality of life in women with fibromyalgia: a randomized controlled trial. Journal of Alternative and Complementary Medicine 2011;17(8):723‐8. [DOI] [PubMed] [Google Scholar]
Oncel 1994 {published data only}
- Oncel A, Eskiyurt N, Leylabadi M. The results obtained by different therapeutic measures in the treatment of generalized fibromyalgia syndrome. Tip Fakultesi Mecmuasi 1994;57(4):45‐9. [Google Scholar]
Palekar 2014 {published data only}
- Palekar TJ, Basu S. Comparative study of pilates exercise verses yogasana in the treatment of fibromyalgia syndrome: a pilot study. International Journal of Pharma and Bio Sciences 2014;5:B410‐20. [Google Scholar]
Paolucci 2016 {published data only}
- Paolucci T, Baldari C, Franco M, Didona D, Reis V, Vetrano M, et al. A new rehabilitation tool in fibromyalgia: the effects of perceptive rehabilitation on pain and function in a clinical randomized controlled trial. Evidence Based Complementary and Alternative Medicine 2016;2016:7574589. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pastor 2014 {published data only}
- Pastor MA, Lopez‐Roig S, Leido A, Penacoba C, Velasco L, Schweiger‐Gallo I, et al. Combining motivational and volitional strategies to promote unsupervised walking in patients with fibromyalgia: study protocol for a randomized controlled trial. Trials 2014; Vol. 120:1‐15. [DOI] [PMC free article] [PubMed]
Perez‐ de la Cruz 2015 {published data only}
- Perez‐ de la Cruz S, Lambeck J. [Effects of a programme of aquatic Ai Chi exercise in patients with fibromyalgia. A pilot study]. Revista de Neurologia 2015; Vol. 60, issue 2:59‐65. [PubMed]
Peters 2002 {published data only}
- Peters S, Stanley I, Rose M, Kaney S, Salmon P. A randomized controlled trial of group aerobic exercise in primary care patients with persistent, unexplained physical symptoms. Family Practice 2002;19:665‐74. [DOI] [PubMed] [Google Scholar]
Pfeiffer 2003 {published data only}
- Pfeiffer AT. Effects of a 1.5‐day multidisciplinary outpatient treatment program for fibromyalgia: a pilot study. American Journal of Physical Medicine & Rehabilitation 2003;82:196‐201. [DOI] [PubMed] [Google Scholar]
Piso 2001 {published data only}
- Piso U, Kuther G, Gutenbrunner C, Gehrke A. Analgesic effects of sauna in fibromyalgia. [German]. Physikalische Medizin Rehabilitationsmedizin Kurortmedizin 2001;11(3):94‐9. [Google Scholar]
Richards 2002 {published data only}
- Richards SC, Scott DL. Prescribed exercise in people with fibromyalgia: parallel group randomised controlled trial. BMJ 2002;325(7357):185. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rivera 2004 {published data only}
- Rivera RJ, Moratalla JC, Valdepenas MF, Garcia Velayos Y, Oses Puche JJ, Ruiz Zubero J, et al. Long‐term efficacy of therapy in patients with fibromyalgia: a physical exercise‐based program and a cognitive‐behavioral approach. Arthritis & Rheumatism 2004;51(2):184‐92. [DOI] [PubMed] [Google Scholar]
Rooks 2002 {published data only}
- Rooks DS, Silverman CB, Kantrowitz FG. The effects of progressive strength training and aerobic exercise on muscle strength and cardiovascular fitness in women with fibromyalgia: a pilot study. Arthritis & Rheumatism 2002;47:22‐8. [DOI] [PubMed] [Google Scholar]
Rooks 2007 {published data only}
- Rooks DS, Gautam S, Romeling M, Cross ML, Stratigakis D, Evans B, et al. Group exercise, education, and combination self‐management in women with fibromyalgia: a randomized trial. Archives of Internal Medicine 2007;167(20):2192‐200. [DOI] [PubMed] [Google Scholar]
Sa¤udo 2010 {published data only}
- Saudo CB, Galiano OD, Carrasco PL, Saxton J. Autonomous nervous system response and quality of life on women with fibromyalgia after a long‐term intervention with physical exercise. [Spanish]. Rehabilitacion 2010;44(3):244‐9. [Google Scholar]
Salek 2005 {published data only}
- Salek AK, Khan MM, Ahmed SM, Rashid MI, Emran MA, Mamun MA. Effect of aerobic exercise on patients with primary fibromyalgia syndrome. Mymensingh Medical Journal 2005;14(2):141‐4. [PubMed] [Google Scholar]
Santana 2010 {published data only}
- Santana JS, Almeida AP, Brandão PM. [The effect of Ai Chi method in fibromyalgic patients] [Os efeitos do método Ai Chi em pacientes portadoras da síndrome fibromiálgica]. Ciencia & Saude Coletiva 2010;15 Suppl(1):1433‐8. [DOI] [PubMed] [Google Scholar]
Sañudo 2010 {published data only}
- Sañudo CB, Galiano OD, Carrasco PL, Saxton J. Autonomous nervous system response and quality of life on women with fibromyalgia after a long‐term intervention with physical exercise. [Spanish]. Rehabilitacion 2010;44(3):244‐9. [Google Scholar]
Sañudo 2010a {published data only}
- Sanudo B, Hoyo M, Carrasco L, McVeigh JG, Corral J, Cabeza R, et al. The effect of 6‐week exercise programme and whole body vibration on strength and quality of life in women with fibromyalgia: a randomised study. Clinical and Experimental Rheumatology 2010;28(6 Suppl 63):S40‐5. [PubMed] [Google Scholar]
Sañudo 2010b {published data only}
- Sanudo B, Galiano D, Carrasco L, Blagojevic M, Hoyo M, Saxton J. Aerobic exercise versus combined exercise therapy in women with fibromyalgia syndrome: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2010;91(12):1838‐43. [DOI] [PubMed] [Google Scholar]
Sañudo 2011 {published data only}
- Sanudo B, Galiano D, Carrasco L, Hoyo M, McVeigh JG. Effects of a prolonged exercise program on key health outcomes in women with fibromyalgia: a randomized controlled trial. Journal of Rehabilitation Medicine 2011;43(6):521‐6. [DOI] [PubMed] [Google Scholar]
Sañudo 2012 {published data only}
- Sañudo B, Hoyo M, Carrasco L, Rodriguez‐Blanco C, Oliva‐Pascual‐Vaca A, McVeigh JG. Effect of whole‐body vibration exercise on balance in women with fibromyalgia syndrome: a randomized controlled trial. Journal of Alternative and Complementary Medicine 2012;18(2):158‐64. [DOI] [PubMed] [Google Scholar]
Sañudo 2012a {published data only}
- Sanudo B, Carrasco L, Hoyo M, McVeigh JG. Effects of exercise training and detraining in patients with fibromyalgia syndrome: a 3‐yr longitudinal study. American Journal of Physical Medicine and Rehabilitation 2012;91(7):561‐73. [DOI] [PubMed] [Google Scholar]
Sañudo 2013 {published data only}
- Sanudo B, Carrasco L, Hoyo M, Oliva‐Pascual‐Vaca A, Rodriguez‐Blanco C. Changes in body balance and functional performance following whole‐body vibration training in patients with fibromyalgia syndrome: a randomized controlled trial. Journal of Rehabilitation Medicine 2013;45(7):678‐84. [DOI] [PubMed] [Google Scholar]
Schmidt 2011 {published data only}
- Schmidt S, Grossman P, Schwarzer B, Jena S, Naumann J, Walach H. Treating fibromyalgia with mindfulness‐based stress reduction: results from a 3‐armed randomized controlled trial. Pain 2011;152(2):1838‐43. [DOI] [PubMed] [Google Scholar]
Sigl‐Erkel 2011 {published data only}
- Sigl‐Erkel T. A randomized trial of tai chi for fibromyalgia. [German] Studienbesprechung zu tai chi (taiji) bei fibromyalgie. Chinesische Medizin 2011;26(2):112‐6. [Google Scholar]
Srikuea 2013 {published data only}
- Srikuea R, Symons TB, Long DE, Lee JD, Shang Y, Chomentowski PJ, et al. Association of fibromyalgia with altered skeletal muscle characteristics which may contribute to postexertional fatigue in postmenopausal women. Arthritis & Rheumatism 2013;65(2):519‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steiner 2015 {published data only}
Suman 2009 {published data only}
- Suman AL, Biagi B, Biasi G, Carli G, Gradi M, Prati E, et al. One‐year efficacy of a 3‐week intensive multidisciplinary non‐pharmacological treatment program for fibromyalgia patients. Clinical & Experimental Rheumatology 2009;27(1):7‐14. [PubMed] [Google Scholar]
Thieme 2003 {published data only}
- Thieme K, Gronica‐Ihle E, Flor H. Operant behavioral treatment of fibromyalgia: a controlled study. Arthritis Care & Research 2003;49:314‐20. [DOI] [PubMed] [Google Scholar]
Thijssen 1992 {published data only}
- Thijssen Ej, Klerk E. Evaluation of a swimming program for patients with fibromyalgia [Evaluatie van een zwemprogramma voor patienten met fibromyalgie]. Ned Tijdschr Fysiother 1992;102(3):71‐5. [Google Scholar]
Tiidus 1997 {published data only}
- Tiidus PM. Manual massage and recovery of muscle function following exercise: a literature review. Journal of Orthopaedic & Sports Physical Therapy 1997;25(2):107‐12. [DOI] [PubMed] [Google Scholar]
Tomas‐Carus 2007a {published data only}
- Tomas‐Carus P. Aquatic training and detraining on fitness and quality of life in FM. Medicine and Science in Sports and Exercise 2007;39(7):1044‐50. [DOI] [PubMed] [Google Scholar]
Tomas‐Carus 2007b {published data only}
- Tomas‐Carus P. The fibromyalgia treatment with physical exercise in warm water reduces the impact of disease [El tratamiento para la fibromialgia con ejercicio fisico en agua caliente reduce el impacto de la enfermedad en la salud fisica y mental de mujeres afectadas]. Reumatologia Clinica 2007;3(1):33‐7. [DOI] [PubMed] [Google Scholar]
Tomas‐Carus 2007c {published data only}
- Tomas‐Carus P. Effects of aquatic training and subsequent detraining on the perception and intensity of pain and number of sensitive points in women with fibromyalgia [Efectos del entrenamiento acuatico y posterior desentrenamiento sobre la percepcion e intensidad del dolor y numero de puntos sensibles de mujeres con fibromialgia]. Apunts Medicina de l'Esport 2007;154(42):76‐81. [Google Scholar]
Tomas‐Carus 2007d {published data only}
- Tomas‐Carus P, Raimundo A, Timon R, Gusi N. Exercise in warm water decreases pain but not the number of tender points in women with fibromyalgia: a randomized controlled trial [El ejercicio fisico en agua caliente reduce el dolor pero no el numero de puntos sensibles de mujeres con fibromialgia: un ensayo clinico randomizado]. Seleccion 2007;16(2):98‐102. [Google Scholar]
Tomas‐Carus 2008 {published data only}
- Tomas‐Carus P, Gusi N, Hakkinen A, Hakkinen K, Leal A, Ortega‐Alonso A. Eight months of physical training in warm water improves physical and mental health in women with fibromyalgia: a randomized controlled trial. Journal of Rehabilitation Medicine 2008;40(4):248‐52. [DOI] [PubMed] [Google Scholar]
Tomas‐Carus 2009 {published data only}
- Tomas‐Carus P, Gusi N, Hakkinen A, Hakkinen K, Raimundo A, Ortega‐Alonso A. Improvements of muscle strength predicted benefits in HRQOL and postural balance in women in fibromyalgia: an 8‐month randomized controlled trial. Rheumatology 2009;48:1147‐51. [DOI] [PubMed] [Google Scholar]
Torres 2015 {published data only}
- Torres JR, Martos IC, Sanchez IT, Rubio AO, Pelegrina AD, Valenza MC. Results of an active neurodynamic mobilization program in patients with fibromyalgia syndrome: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2015;96(10):1771‐8. [DOI] [PubMed] [Google Scholar]
Uhlemann 2007 {published data only}
- Uhlemann C, Strobel I, Muller‐Ladner U, Lange U. Prospective clinical trial about physical activity in fibromyalgia. [German]. Aktuelle Rheumatologie 2007;32(1):27‐33. [Google Scholar]
Valencia 2009 {published data only}
- Valencia M, Alonso B, Alvarez MJ, Barrientos MJ, Ayan C, Sanchez VM. Effects of 2 physiotherapy programs on pain perception, muscular flexibility, and illness impact in women with fibromyalgia: a pilot study. Journal of Manipulative and Physiological Therapeutics 2009;32(1):84‐92. [DOI] [PubMed] [Google Scholar]
Valim 2003 {published data only}
- Valim V, Oliveira L, Suda A, Silva L, Assis M, Barros Neto T, et al. Aerobic fitness effects in fibromyalgia. Journal of Rheumatology 2003;30(5):1060‐9. [PubMed] [Google Scholar]
Valim 2013 {published data only}
- Valim V, Natour J, Xiao Y, Pereira AF, Lopes BB, Pollak DF, et al. Effects of physical exercise on serum levels of serotonin and its metabolite in fibromyalgia: a randomized pilot study. Revista Brasileira de Reumatologia 2013;53(6):538‐41. [DOI] [PubMed] [Google Scholar]
Valkeinen 2004 {published data only}
- Valkeinen H, Alen M, Hannonen P, Hakkinen A, Airaksinen O, Hakkinen K. Changes in knee extension and flexion force, EMG and functional capacity during strength training in older females with fibromyalgia and healthy controls. Rheumatology 2004;43(2):225‐8. [DOI] [PubMed] [Google Scholar]
Valkeinen 2005 {published data only}
- Valkeinen H, Hakkinen K, Pakarinen A, Hannonen P, Hakkinen A, Airaksinen O, et al. Muscle hypertrophy, strength development, and serum hormones during strength training in elderly women with fibromyalgia. Scandinavian Journal of Rheumatology 2005;34(4):309‐14. [DOI] [PubMed] [Google Scholar]
Valkeinen 2008 {published data only}
- Valkeinen H, Alen M, Hakkinen A, Hannonen P, Kukkonen‐Harjula K, Hakkinen K. Effects of concurrent strength and endurance training on physical fitness and symptoms in postmenopausal women with fibromyalgia: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2008;89(9):1660‐6. [DOI] [PubMed] [Google Scholar]
van Eijk‐Hustings 2013 {published data only}
- Eijk‐Hustings Y, Kroese M, Tan F, Boonen A, Bessems‐Beks M, Landewe R. Challenges in demonstrating the effectiveness of multidisciplinary treatment on quality of life, participation and health care utilisation in patients with fibromyalgia: a randomised controlled trial. Clinical Rheumatology 2013;32(2):199‐209. [DOI] [PubMed] [Google Scholar]
van Koulil 2010 {published data only}
- Koulil S, Lankveld W, Kraaimaat FW, Helmond T, Vedder A, Hoorn H, et al. Tailored cognitive‐behavioral therapy and exercise training for high‐risk patients with fibromyalgia. Arthritis Care & Research 2010;62(10):1377‐85. [DOI] [PubMed] [Google Scholar]
VanRavenstein 2014 {published data only}
- VanRavenstein KA. Physical Activity in Women With Fibromyalgia. Charleston, SC: Medical University of South Carolina (Dissertation),. Medical University of South Carolina, 2014; Vol. PhD:120.
vanSanten 2002 {published data only}
- vanSanten M, Bolwijn P, Landewe R, Verstappen F, Bakker C, Hidding A, et al. High or low intensity aerobic fitness training in fibromyalgia: does it matter?. Journal of Rheumatology 2002;29(3):582‐7. [PubMed] [Google Scholar]
vanSanten 2002a {published data only}
- vanSanten M, Bolwijn P, Verstappen F, Bakker C, Hidding A, Houben H, et al. A randomized clinical trial comparing fitness and biofeedback training versus basic treatment in patients with fibromyalgia. Journal of Rheumatology 2002;29(3):575‐81. [PubMed] [Google Scholar]
Verstappen 1997 {published data only}
- Verstappen FTJ, Santen‐Hoeuftt HMS, Bolwijn PH, Linden S, Kuipers H. Effects of a group activity program for fibromyalgia patients on physical fitness and well being. Journal of Musculoskeletal Pain 1997;5(4):17‐28. [Google Scholar]
Vlaeyen1996 {published data only}
- Vlaeyen JW, Teeken‐Gruben NJ, Goossens ME, Rutten‐van Molken MP, Pelt RA, Eek H, et al. Cognitive‐educational treatment of fibromyalgia: a randomized clinical trial. I. Clinical effects. Journal of Rheumatology 1996;23(7):1237‐45. [PubMed] [Google Scholar]
Wang 2010 {published data only}
- Wang C, Schmid CH, Rones R, Kalish R, Yinh J, Goldenberg DL, et al. A randomized trial of tai chi for fibromyalgia. New England Journal of Medicine 2010;363(8):743‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2015 {published data only}
- Wang C, McAlindon T, Fielding RA, Harvey WF, Driban JB, Price LL, et al. A novel comparative effectiveness study of Tai Chi versus aerobic exercise for fibromyalgia: study protocol for a randomized controlled trial. Trials 2015; Vol. 16, issue 1. [DOI] [PMC free article] [PubMed]
Westfall 1999 {published data only}
- Westfall JK. The Effects of a Water Exercise Program on the Manifestations of Fibromyalgia. Thesis/Dissertation, M.S. Slippery Rock, PA: Slippery Rock University,. Eugene, Or. : Microform Publications, University of Oregon. 1999. http://kinpubs.uoregon.edu/, 1999.
Williams 2010 {published data only}
- Williams DA, Kuper D, Segar M, Mohan N, Sheth M, Clauw DJ. Internet‐enhanced management of fibromyalgia: a randomized controlled trial. Pain 2010; Vol. 151, issue 3:694‐702. [DOI] [PMC free article] [PubMed]
Worrel 2001 {published data only}
- Worrel LM, Krahn LE, Sletten CD, Pond GR. Treating fibromyalgia with a brief interdisciplinary program: initial outcomes and predictors of response. Mayo Clinic Proceedings 2001;76(4):384‐90. [DOI] [PubMed] [Google Scholar]
Yuruk 2008 {published data only}
- Yuruk OB, Gultekin Z. Comparison of two different exercise programs in women with fibromyalgia syndrome [Turkish]. Fizyoterapi Rehabilitasyon 2008;19(1):15‐23. [Google Scholar]
Zijlstra 2005 {published data only}
- Zijlstra TR, Laar MA, Bernelot Moens HJ, Taal E, Zakraoui L, Rasker JJ. Spa treatment for primary fibromyalgia syndrome: a combination of thalassotherapy, exercise and patient education improves symptoms and quality of life. Rheumatology 2005;44:539‐46. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Bjersing 2012 {published data only}
- Bjersing JL, Dehlin M, Erlandsson M, Bokarewa MI, Mannerkorpi K. Changes in pain and insulin‐like growth factor 1 in fibromyalgia during exercise: the involvement of cerebrospinal inflammatory factors and neuropeptides. Arthritis Research & Therapy 2012;14(4):R162. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duruturk 2015 {published data only}
- Duruturk N, Tuzun EH, Culhaoglu B. Is balance exercise training as effective as aerobic exercise training in fibromyalgia syndrome?. Rheumatology International 2015;35(5):845‐54. [DOI] [PubMed] [Google Scholar]
Espí‐López 2016 {published data only}
- Espí‐López GV, Inglés M, Ruescas‐Niculau M‐A, Moreno‐Segura N. Effect of low‐impact aerobic exercise combined with music therapy on patients with fibromyalgia. A pilot study. Complementary Therapies in Medicine 2016;28:1‐7. [DOI] [PubMed] [Google Scholar]
Mendonca 2016 {published data only}
- Mendonca ME, Simis M, Grecco LC, Battistella LR, Baptista AF, Fregni F. Transcranial direct current simulation combined with aerobic exercise to optimize analgesic responses in fibromyalgia: a randomized placebo‐controlled clinical trial. Frontiers in Human Neurosciences 2016;10:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sanudo 2015 {published data only}
- Sanudo B, Carrasco L, Hoyo M, Figueroa A, Saxton JM. Vagal modulation and symptomatology following a 6‐month aerobic exercise program for women with fibromyalgia. Clinical and Experimental Rheumatology 2015;33(1 Suppl 88):41‐5. [PubMed] [Google Scholar]
Additional references
Ablin 2013
- Ablin JN, Buskila D, Amital H, Fitzcharles M, Shir Y, Henningsen P. A paradigm change for treatment strategies for fibromyalgia syndrome reflected by recommendations of recent evidence‐based interdisciplinary guidelines developed independently in three countries. Arthritis & Rheumatism 2013;65(Suppl 10):839. [Google Scholar]
ACSM 2013
- American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription Ninth Edition. 9th Edition. Baltimore, MD: Lippincott Williams & Wilkins, 2013. [DOI] [PubMed] [Google Scholar]
Arnold 2008
- Arnold LM, Crofford LJ, Mease PJ, Burgess SM, Palmer SC, Abetz L, et al. Patient perspectives on the impact of fibromyalgia. Patient Education and Counseling 2008;73(1):114‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arnold 2013
- Arnold LM, Fan J, Russell IJ, Yunus MB, Khan MA, Kushner I, et al. The fibromyalgia family study: a genome‐wide linkage scan study. Arthritis & Rheumatism 2013;65(4):1122‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barclay 2014
- Barclay T, Richards S, Schoffstall J, Magnuson C, McPhee C, Price J, et al. A pilot study on the effects of exercise on depression symptoms using levels of neurotransmitters and EEG as markers. European Journal of Psychology and Educational Studies 2014;1(1):30‐5. [Google Scholar]
Bennett 1989
- Bennett RM, Clark SR, Goldberg L, Nelson D, Bonafede RP, Porter J, et al. Aerobic fitness in patients with fibrositis. A controlled study of respiratory gas exchange and 133xenon clearance from exercising muscle. Arthritis & Rheumatism 1989;32(4):454‐60. [DOI] [PubMed] [Google Scholar]
Bennett 1998
- Bennett RM, Clark SC, Walczyk J. A randomized, double‐blind, placebo‐controlled study of growth hormone in the treatment of fibromyalgia. American Journal of Medicine 1998;104(3):227‐31. [DOI] [PubMed] [Google Scholar]
Bergner 1981
- Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Medical Care 1981;19(8):787‐805. [DOI] [PubMed] [Google Scholar]
Bernardy 2013
- Bernardy K, Klose P, Busch AJ, Choy EH, Häuser W. Cognitive behavioural therapies for fibromyalgia. Cochrane Database of Systematic Reviews 2013, Issue 9. [DOI: 10.1002/14651858.CD009796.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bidonde 2014
- Bidonde J, Busch AJ, Webber SC, Schachter CL, Danyliw A, Overend TJ, et al. Aquatic exercise training for fibromyalgia. Cochrane Database of Systematic Reviews 2014, Issue 10. [DOI: 10.1002/14651858.CD011336] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bidonde 2014a
- Bidonde J, Busch AJ, Bath B, Milosavljevic S. Exercise for adults with fibromyalgia: an umbrella systematic review with synthesis of best evidence. Current Rheumatology Reviews 2014;10(1):45‐79. [DOI] [PubMed] [Google Scholar]
Boomershine 2012
- Boomershine CS. A comprehensive evaluation of standardized assessment tools in the diagnosis of fibromyalgia and in the assessment of fibromyalgia severity. Pain Research and Treatment 2012;2012:653714. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bouchard 2012
- Bouchard C, Blair S, Haskell W. History and current status of the study of physical activity and health.Why study physical activity and health?. Tocco AN, Zavala MJ, editors. 2nd Edition. Vol. Chapter 1, Windsor, ON: Human Kinetics, 2012. [Google Scholar]
Brachaniec 2009
- Brachaniec M, DePaul V, Elliott M, Moor L, Sherwin P. Partnership in action: an innovative knowledge translation approach to improve outcomes for persons with fibromyalgia (Editorial). Physiotherapy Canada 2009;61(3):123‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Branco 2010
- Branco JC, Bannwarth B, Failde I, Abello Carbonell J, Blotman F, Spaeth M, et al. Prevalence of FM: a survey in five European countries. Seminars in Arthritis and Rheumatism 2010;39(6):448‐53. [DOI] [PubMed] [Google Scholar]
Brosseau 2008
- Brosseau L, Wells GA, Tugwell P, Egan M, Wilson KG, Dubouloz CJ, et al. Ottawa panel evidence‐based clinical practice guidelines for aerobic fitness exercises in the management of fibromyalgia: part 1. Physical Therapy 2008;88(7):857‐71. [DOI] [PubMed] [Google Scholar]
Burckhardt 1991
- Burckhardt CS, Clark SR, Bennett RM. The Fibromyalgia Impact Questionnaire: development and validation. Journal of Rheumatology 1991;18(5):728‐33. [PubMed] [Google Scholar]
Busch 2011
- Busch AJ, Webber SC, Brachaniec M, Bidonde J, Bello‐Haas VD, Danyliw AD, et al. Exercise therapy for fibromyalgia. Current Pain and Headache Reports 2011;15(5):358‐67. [DOI: 10.1007/s11916-011-0214-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Busch 2013
- Busch AJ, Webber SC, Richards RS, Bidonde J, Schachter CL, Schafer LA, et al. Resistance exercise training for fibromyalgia. Cochrane Database of Systematic Reviews 2013, Issue 12. [DOI: 10.1002/14651858.CD010884] [DOI] [PMC free article] [PubMed] [Google Scholar]
Busija 2011
- Busija L, Pausenberger E, Haines TP, Haymes S, Buchbinder R, Osborne RH. Adult measures of general health and health‐related quality of life: Medical Outcomes Study Short Form 36‐Item (SF‐36) and Short Form 12‐Item (SF‐12) Health Surveys, Nottingham Health Profile (NHP), Sickness Impact Profile (SIP), Medical Outcomes Study Short Form 6D (SF‐6D), Health Utilities Index Mark 3 (HUI3), Quality of Well‐Being Scale (QWB), and Assessment of Quality of Life (AQoL). Arthritis Care & Research 2011;63 Suppl 11:S383‐412. [DOI] [PubMed] [Google Scholar]
Carville 2008
- Carville SF, Arendt‐Nielsen S, Bliddal H, Blotman F, Branco JC, Buskila D, et al. EULAR evidence‐based recommendations for the management of fibromyalgia syndrome. Annals of the Rheumatic Diseases 2008;67(4):536‐41. [DOI] [PubMed] [Google Scholar]
Cates 2008 [Computer program]
- Cates C. Visual Rx, Version 3. Dr. Chris Cates' EBM Web Site, 2008.
Choy 2009
- Choy EH, Mease PJ. Key symptom domains to be assessed in fibromyalgia (outcome measures in rheumatoid arthritis clinical trials). Rheumatic Disease Clinics of North America 2009;35(2):329‐37. [DOI] [PubMed] [Google Scholar]
Deare 2013
- Deare JC, Zheng Z, Xue CCL, Liu JP, Shang J, Scott SW, et al. Acupuncture for treating fibromyalgia. Cochrane Database of Systematic Reviews 2013, Issue 5. [DOI: 10.1002/14651858.CD007070.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. The Cochrane Collaboration [updated March 2011]. [Google Scholar]
Derry 2012
- Derry S, Gill D, Phillips T, Moore RA. Milnacipran for neuropathic pain and fibromyalgia in adults. Cochrane Database of Systematic Reviews 2012, Issue 3. [DOI: 10.1002/14651858.CD008244.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Donatelle 2015
- Donatelle RJ, Kolen‐Thompson AM. Chapter 4. Engaging in physical activity for health, fitness, and performance. Health: The Basics. 6th Edition. Toronto, ON: Pearson Canada Inc, 2015. [Google Scholar]
Dworkin 2008
- Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. Journal of Pain 2008;9(2):105‐21. [DOI] [PubMed] [Google Scholar]
Eyler 2003
- Eyler AA, Brownson RC, Bacak SJ, Housemann RA. The epidemiology of walking for physical activity in the United States. Medicine & Science in Sports & Exercise 2003;35(9):1529‐36. [DOI] [PubMed] [Google Scholar]
Fontaine 2011
- Fontaine KR, Conn L, Clauw DJ. Effects of lifestyle physical activity in adults with fibromyalgia: results at follow‐up. Journal of Clinical Rheumatology 2011;17(2):64‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Garber 2011
- Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Medicine & Science in Sports Exercise 2011;43(7):1334‐59. [DOI] [PubMed] [Google Scholar]
Garcia‐Hermoso 2014
- Garcia‐Hermoso A, Saavedra JM, Escalante Y. Effects of exercise on functional aerobic capacity in adults with fibromyalgia syndrome: a systematic review of randomized controlled trials. Journal of Back and Musculoskeletal Rehabilitation 2014;28(4):609‐19. [DOI] [PubMed] [Google Scholar]
Goldenberg 2004
- Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA 2004;292(19):2388‐95. [DOI] [PubMed] [Google Scholar]
Hauser 2010
- Hauser W, Klose P, Langhorst J, Moradi B, Steinbach M, Schiltenwolf M, et al. Efficacy of different types of aerobic exercise in fibromyalgia syndrome: a systematic review and meta‐analysis of randomised controlled trials. Arthritis Research & Therapy 2010;12(3):R79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hauser 2010a
- Hauser W, Thieme K, Turk DC. Guidelines on the management of fibromyalgia syndrome ‐ a systematic review. European Journal of Pain 2010;14(1):5‐10. [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC, editors. Chapter 8. Assessing risk of bias in included studies. Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. www.cochrane‐handbook.org. The Cochrane Collaboration, 2011. [Google Scholar]
Higgins 2011b
- Higgins JPT, Deeks JJ, editors. Chapter 7. Selecting studies and collecting data. Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. www.cochrane‐handbook.org. The Cochrane Collaboration, 2011. [Google Scholar]
Higgins 2011c
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. 5.1.0. Available from www.cochrane‐handbook.org: The Cochrane Collaboration, 2011. [Google Scholar]
Huskisson 1976
- Huskisson EC, Jones J, Scott PJ. Application of visual‐analogue scales to the measurement of functional capacity. Rheumatology and Rehabilitation 1976;15(3):185‐7. [DOI] [PubMed] [Google Scholar]
Huskisson 1983
- Huskisson EC, Sturrock RD, Tugwell P. Measurement of patient outcome. British Journal of Rheumatology 1983;22:86‐9. [DOI] [PubMed] [Google Scholar]
Jadad 1996
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Control Clinical Trials 1996;17(1):1‐12. [DOI] [PubMed] [Google Scholar]
Jahan 2012
- Jahan F, Nanji K, Qidwai W, Qasim R. Fibromyalgia syndrome: an overview of pathophysiology, diagnosis and management. Oman Medical Journal 2012;27(3):192‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kelley 2011
- Kelley GA, Kelley KS, Jones DL. Efficacy and effectiveness of exercise on tender points in adults with fibromyalgia: a meta‐analysis of randomized controlled trials. Arthritis 2011;2011:1‐10. [DOI: 10.1155/2011/125485] [DOI] [PMC free article] [PubMed] [Google Scholar]
Klaperski 2014
- Klaperski S, Dawans B, Heinrichs M, Fuchs R. Effects of a 12‐week endurance training program on the physiological response to psychosocial stress in men: a randomized controlled trial. Journal of Behavioral Medicine 2014;37(6):1118‐33. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6. Searching for studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Lopresti 2013
- Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise. Journal of Affective Disorders 2013;148(1):12‐27. [DOI] [PubMed] [Google Scholar]
Macfarlane 2016
- Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Flub E, et al. EULAR revised recommendations for the management of fibromyalgia. Annals of the Rheumatic Diseases 2016;0:1‐11. [DOI: ] [DOI] [PubMed] [Google Scholar]
Marcus 2011
- Marcus DA, Deodhar A. Non‐medication treatments. Fibromyalgia. New York, NY: Springer Science + Business Media, 2011:159‐74. [Google Scholar]
McLoughlin 2011
- McLoughlin MJ, Stegner AJ, Cook DB. The relationship between physical activity and brain responses to pain in fibromyalgia. Journal of Pain 2011;12(6):640‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
McNalley 2006
- McNalley JD, Matheson DA, Bakowshy VS. The epidemiology of self‐reported fibromyalgia in Canada. Chronic Diseases in Canada 2006;27(1):9‐16. [PubMed] [Google Scholar]
Mease 2005
- Mease P. Fibromyalgia syndrome: review of clinical presentation, pathogenesis, outcome measures, and treatment. [erratum appears in J Rheumatol Suppl. 2005 Oct;32(10):2063]. Journal of Rheumatology. Supplement 2005;75:6‐21. [PubMed] [Google Scholar]
Merskey 1994
- Merskey H, Bogduk N. Classifications of Chronic Pain: Descriptions and Definitions of Chronic Pain Syndromes and Definitions of Pain Terms. Seattle, WA: IASP, 1994. [Google Scholar]
Mitchell 2012 [Computer program]
- Mitchell M. Engauge Digitizer ‐ Digitizing Software. Version 5.1. https://markummitchell.github.io/engauge‐digitizer/, 2012. [digitizer.sourceforge.net]
Moore 2012
- Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for neuropathic pain and fibromyalgia in adults. Cochrane Database of Systematic Reviews 2012;Issue 12:Art. No.: CD008242. DOI: 10.1002/14651858.CD008242.pub2. [DOI] [PubMed] [Google Scholar]
Moylan 2013
- Moylan S, Eyre HA, Maes M, Baune BT, Jacka FN, Berk M. Exercising the worry away: how inflammation, oxidative and nitrogen stress mediates the beneficial effect of physical activity on anxiety disorder symptoms and behaviours. Neuroscience & Biobehavioral Reviews 2013;37(4):573‐84. [DOI] [PubMed] [Google Scholar]
Nakamura 2014
- Nakamura I, Nishioka K, Usui C, Osada K, Ichibayashi H, Ishida M, et al. An epidemiologic internet survey of fibromyalgia and chronic pain in Japan. Arthritis Care & Research 2014;66(7):1093‐101. [DOI] [PubMed] [Google Scholar]
Noonan 2000
- Noonan V, Dean E. Submaximal exercise testing: clinical application and interpretation. Physical Therapy 2000;80(8):782‐807. [PubMed] [Google Scholar]
Nuesch 2013
- Nuesch E, Hauser W, Bernardy K, Barth J, Juni P. Comparative efficacy of pharmacological and non‐pharmacological interventions in fibromyalgia syndrome: network meta‐analysis. Annals of the Rheumatic Disease 2013;72(6):955‐62. [DOI] [PubMed] [Google Scholar]
Nunan 2013
- Nunan D, Mahtani KR, Roberts N, Heneghan C. Physical activity for the prevention and treatment of major chronic disease: an overview of systematic reviews. Systematic Reviews 2013;2(56):doi:10. 1186/2046‐4053‐2‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Painter 1999
- Painter P, Stewart AL, Carey S. Physical functioning: definitions, measurement, and expectations. Advances in Renal Replacement Therapy 1999;6(2):110‐23. [DOI] [PubMed] [Google Scholar]
Park 2000
- Park JH, Niermann KJ, Olsen N. Evidence for metabolic abnormalities in the muscles of patients with fibromyalgia. Current Rheumatology Reports 2000;2(2):131‐40. [DOI] [PubMed] [Google Scholar]
Park 2007
- Park J, Knudson S. Medically unexplained physical symptoms. Health Reports 2007;18(1):43‐7. [PubMed] [Google Scholar]
Philadelphia Panel 2001
- Philadelphia Panel 2001. Philadelphia Panel evidence‐based clinical practice guidelines on selected rehabilitation interventions for knee pain. Physical Therapy 2001;81(10):1675‐700. [PubMed] [Google Scholar]
Puetz 2006
- Puetz TW. Physical activity and feelings of energy and fatigue: epidemiological evidence. Sports Medicine 2006;36(9):767‐80. [DOI] [PubMed] [Google Scholar]
Raftery 2009
- Raftery G, Bridges M, Heslop P, Walker DJ. Are fibromyalgia patients as inactive as they say they are?. Clinical Rheumatology 2009;28(6):711‐4. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The NCC. Review Manager (RevMan). Version 5.3. Copenhaugen: The Cochrane Collaboration, 2014.
Rooks 2008
- Rooks DS. Talking to patients with fibromyalgia about physical activity and exercise. Current Opinion in Rheumatology 2008;20(2):208‐12. [DOI] [PubMed] [Google Scholar]
Scheef 2012
- Scheef L, Jankowski J, Daamen M, Weyer G, Klingenberg M, Renner J, et al. An fMRI study on the acute effects of exercise on pain processing in trained athletes. Pain 2012;153(8):1702‐14. [DOI] [PubMed] [Google Scholar]
Schmidt‐Wilcke 2011
- Schmidt‐Wilcke T, Clauw DJ. Fibromyalgia: from pathophysiology to therapy. Nature Reviews. Rheumatology 2011;7(9):518‐27. [DOI] [PubMed] [Google Scholar]
Schünemann 2011a
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Presenting results and 'Summary of findings' tables. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Smythe 1979
- Smythe HA. Non‐articular rheumatism and psychogenic musculoskeletal syndromes. In: McCarty DJ editor(s). Arthritis and Allied Conditions. Philadelphia: Lea and Febiger, 1979:881‐91. [Google Scholar]
Staud 2002
- Staud R. Evidence of involvement of central neural mechanisms in generating fibromyalgia pain. Current Rheumatology Reports 2002;4(4):299‐305. [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D, editors. Chapter 10. Addressing reporting biases. Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. Vol. www.cochrane‐handbook.org, The Cochrane Collaboration, 2011:297‐333. [OTHER] [Google Scholar]
Thomas 2010
- Thomas EN, Blotman F. Aerobic exercise in fibromyalgia: a practical review. Rheumatology International 2010;30(9):1143‐50. [DOI] [PubMed] [Google Scholar]
Tort 2012
- Tort S, Urrútia G, Nishishinya MB, Walitt B. Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD009807] [DOI] [PubMed] [Google Scholar]
Turk 2002
- Turk DC. Suffering and dysfunction in fibromyalgia syndrome. Journal of Musculoskeletal Pain 2002;10(1‐2):85‐96. [Google Scholar]
van Tulder 2003
- Tulder MW, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 2003;28(12):1290‐9. [DOI] [PubMed] [Google Scholar]
Vincent 2013
- Vincent A, Lahr BD, Wolfe F, Clauw DJ, Whipple MO, Oh TH, et al. Prevalence of fibromyalgia: a population‐based study in Olmsted County, Minnesota, utilizing the Rochester Epidemiology Project. Arthritis Care & Research 2013;65(5):786‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Visual Rx [Computer program]
- Dr. Christopher Cates EBM website. URL: http://www.nntonline.net. Visual Rx. Version 3. Dr. Christopher Cates EBM website. URL: http://www.nntonline.net, 2008.
Ware 1993
- Ware JE, Snow KK, Kosinski M, Gandek B, New E. SF‐36 Health Survey: Manual and Interpretation Guide. New York: The Health Institute, New England Medical Center, 1993. [Google Scholar]
Wiffen 2013
- Wiffen PJ, Derry S, Moore RA, Aldington D, Cole P, Rice ASC, et al. Antiepileptic drugs for neuropathic pain and fibromyalgia ‐ an overview of Cochrane reviews. Cochrane Database of Systematic Reviews 2013, Issue 11. [DOI: 10.1002/14651858.CD010567.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wolfe 1990
- Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis & Rheumatism 1990;33(2):160‐72. [DOI] [PubMed] [Google Scholar]
Wolfe 1997
- Wolfe F, Anderson J, Harkness D, Bennett RM, Caro XJ, Goldenberg DL, et al. Work and disability status of persons with fibromyalgia. Journal of Rheumatology 1997;24(6):1171‐8. [PubMed] [Google Scholar]
Wolfe 2010
- Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care & Research 2010;62(5):600‐10. [DOI] [PubMed] [Google Scholar]
Wolfe 2011
- Wolfe F, Hassett AL, Katz RS, Michaud K, Walitt B. Do we need core sets of fibromyalgia domains? The assessment of fibromyalgia (and other rheumatic disorders) in clinical practice. Journal of Rheumatology 2011;38(6):1104‐12. [DOI] [PubMed] [Google Scholar]
Wolfe 2013
- Wolfe F, Brahler E, Hinz A, Hauser W. Fibromyalgia prevalence, somatic symptom reporting, and the dimensionality of polysymptomatic distress: results from a survey of the general population. Arthritis Care & Research 2013;65(5):777‐85. [DOI] [PubMed] [Google Scholar]
Yang 2012
- Yang PY, Ho KH, Chen HC, Chien MY. Exercise training improves sleep quality in middle‐aged and older adults with sleep problems: a systematic review. Journal of Physiotherapy 2012;58(3):157‐63. [DOI: 10.1016/S1836-9553(12)70106-6] [DOI] [PubMed] [Google Scholar]
Yunus 1981
- Yunus M, Masi AT, Calabro JJ, Miller KA, Feigenbaum SL. Primary fibromyalgia (fibrositis): clinical study of 50 patients with matched normal controls. Seminars in Arthritis and Rheumatism 1981;11:151‐71. [DOI] [PubMed] [Google Scholar]
Zeng 2008
- Zeng QY, Chen R, Darmawan J, Xiao ZY, Chen SB, Wigley R, et al. Rheumatic diseases in China. Arthritis Research & Therapy 2008;10(1):1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Busch 2001
- Busch AJ, Schachter CL, Peloso PM. Fibromyalgia and exercise training: a systematic review of randomized clinical trials. Physical Therapy Review 2001;6:287‐306. [Google Scholar]
Busch 2002
- Busch AJ, Schachter CL, Peloso P, Bombardier C. Exercise for treating fibromyalgia syndrome. Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD003786.pub2] [DOI] [PubMed] [Google Scholar]
Busch 2007
- Busch AJ, Barber KAR, Overend TJ, Peloso PMJ, Schachter CL. Exercise for treating fibromyalgia syndrome. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD003786.pub2] [DOI] [PubMed] [Google Scholar]
Busch 2008
- Busch AJ, Schachter CL, Overend TJ, Peloso PM, Barber KA. Exercise for fibromyalgia: a systematic review. Journal of Rheumatology 2008;35(6):1130‐44. [PubMed] [Google Scholar]


