Abstract
Background
Communication and language development are areas of particular weakness for young children with Down syndrome. Caregivers' interaction with children influences language development, so many early interventions involve training parents how best to respond to their children and provide appropriate language stimulation. Thus, these interventions are mediated through parents, who in turn are trained and coached in the implementation of interventions by clinicians. As the interventions involve a considerable commitment from clinicians and families, we undertook this review to synthesise the evidence of their effectiveness.
Objectives
To assess the effects of parent‐mediated interventions for improving communication and language development in young children with Down syndrome. Other outcomes are parental behaviour and responsivity, parental stress and satisfaction, and children's non‐verbal means of communicating, socialisation and behaviour.
Search methods
In January 2018 we searched CENTRAL, MEDLINE, Embase and 14 other databases. We also searched three trials registers, checked the reference lists of relevant reports identified by the electronic searches, searched the websites of professional organizations, and contacted their staff and other researchers working in the field to identify other relevant published, unpublished and ongoing studies.
Selection criteria
We included randomised controlled trials (RCTs) and quasi‐RCTs that compared parent‐mediated interventions designed to improve communication and language versus teaching/treatment as usual (TAU) or no treatment or delayed (wait‐listed) treatment, in children with Down syndrome aged between birth and six years. We included studies delivering the parent‐mediated intervention in conjunction with a clinician‐mediated intervention, as long as the intervention group was the only group to receive the former and both groups received the latter.
Data collection and analysis
We used standard Cochrane methodological procedures for data collection and analysis.
Main results
We included three studies involving 45 children aged between 29 months and six years with Down syndrome. Two studies compared parent‐mediated interventions versus TAU; the third compared a parent‐mediated plus clinician‐mediated intervention versus a clinician‐mediated intervention alone. Treatment duration varied from 12 weeks to six months. One study provided nine group sessions and four individualised home‐based sessions over a 13‐week period. Another study provided weekly, individual clinic‐based or home‐based sessions lasting 1.5 to 2 hours, over a six‐month period. The third study provided one 2‐ to 3‐hour group session followed by bi‐weekly, individual clinic‐based sessions plus once‐weekly home‐based sessions for 12 weeks. Because of the different study designs and outcome measures used, we were unable to conduct a meta‐analysis.
We judged all three studies to be at high risk of bias in relation to blinding of participants (not possible due to the nature of the intervention) and blinding of outcome assessors, and at an unclear risk of bias for allocation concealment. We judged one study to be at unclear risk of selection bias, as authors did not report the methods used to generate the random sequence; at high risk of reporting bias, as they did not report on one assessed outcome; and at high risk of detection bias, as the control group had a cointervention and only parents in the intervention group were made aware of the target words for their children. The sample sizes of each included study were very small, meaning that they are unlikely to be representative of the target population.
The findings from the three included studies were inconsistent. Two studies found no differences in expressive or receptive language abilities between the groups, whether measured by direct assessment or parent reports. However, they did find that children in the intervention group could use more targeted vocabulary items or utterances with language targets in certain contexts postintervention, compared to those in the control group; this was not maintained 12 months later. The third study found gains for the intervention group on total‐language measures immediately postintervention.
One study did not find any differences in parental stress scores between the groups at any time point up to 12 months postintervention. All three studies noted differences in most measures of how the parents talked to and interacted with their children postintervention, and in one study most strategies were maintained in the intervention group at 12 months postintervention. No study reported evidence of language attrition following the intervention in either group, while one study found positive outcomes on children's socialisation skills in the intervention group. One study looked at adherence to the treatment through attendance data, finding that mothers in the intervention group attended seven out of nine group sessions and were present for four home visits. No study measured parental use of the strategies outside of the intervention sessions.
A grant from the Hospital for Sick Children Foundation (Toronto, Ontario, Canada) funded one study. Another received partial funding from the National Institute of Child Health and Human Development and the Department of Education in the USA. The remaining study did not specify any funding sources.
In light of the serious limitations in methodology, and the small number of studies included, we considered the overall quality of the evidence, as assessed by GRADE, to be very low. This means that we have very little confidence in the results, and further research is very likely to have an important impact on our confidence in the estimate of treatment effect.
Authors' conclusions
There is currently insufficient evidence to determine the effects of parent‐mediated interventions for improving the language and communication of children with Down syndrome. We found only three small studies of very low quality. This review highlights the need for well‐designed studies, including RCTs, to evaluate the effectiveness of parent‐mediated interventions. Trials should use valid, reliable and similar measures of language development, and they should include measures of secondary outcomes more distal to the intervention, such as family well‐being. Treatment fidelity, in particular parental dosage of the intervention outside of prescribed sessions, also needs to be documented.
Plain language summary
Parent‐mediated interventions to promote communication and language development in young children with Down syndrome
Review question
Do parent‐mediated interventions improve communication and language development in young children with Down syndrome?
Background
Language development is an area of particular weakness for young children with Down syndrome. Caregivers' interaction with children influences language development, so sometimes clinicians coach parents so they can stimulate their children's language and communication skills.
Study characteristics
The evidence is current to January 2018.
We found three studies involving 45 children aged between 29 months and six years. Two studies were randomised controlled trials: experiments in which children were allocated to treatment (i.e. parent‐mediated) and control (treatment as usual or clinician‐mediated, or both) groups using a random method such as a computer‐generated list of random numbers. The other study reported that randomisation took place but did not specify how this was done.
Two studies compared parent‐mediated intervention to treatment as usual. One of these lasted for 13 weeks, and parents in the intervention group received nine, weekly group sessions and four individual sessions in the home. The total intervention time was approximately 26.5 hours. A second study lasted for six months, and parents received weekly, 1.5‐ to 2‐hour clinic or home‐based, individualised, parent‐child sessions. The total intervention time was approximately 48 hours. A third study compared a parent‐ and clinician‐mediated intervention to a clinician‐only‐mediated intervention. In this study the parents in the intervention group took part in a two‐ to three‐hour interactive workshop plus three individualised sessions (two clinic‐based and one home‐based) every week for 12 weeks. The control group received the same individualised sessions, but a clinician delivered them (i.e. there was no parental involvement). The total intervention time was approximately 19 hours.
A grant from the Hospital for Sick Children Foundation (Toronto, Ontario, Canada) funded one study. Another received partial funding from the National Institute of Child Health and Human Development and the Department of Education in the USA. The remaining study did not specify any funding sources.
Key results
Two of the three studies found no differences in children's language ability after parent training. However, these same two studies found that children in the intervention group used more words that had been specifically targeted, postintervention; this was not maintained 12 months later. The study that gave parents the largest amount of intervention reported gains on general measures of overall language ability for children in the intervention group. One study did not find any changes in levels of parental stress immediately or up to 12 months postintervention in either group. All three studies noted changes in how parents talked to and interacted with their children immediately postintervention, and most strategies were retained by the intervention group 12 months later. One study reported increases in the socialisation skills of children who received the intervention. No study reported language attrition in either group postintervention.
Quality of the evidence
We rated the quality of the evidence in this review as very low, as only three studies fulfilled the criteria for inclusion, and all had small sizes and serious methodological limitations. There is currently insufficient evidence to determine the effect of parent‐mediated interventions for improving the communication and language development in young children with Down syndrome.
Summary of findings
Background
Description of the condition
Down syndrome, caused by extra genetic material on chromosome 21, is the most common genetic cause of intellectual disability. The condition can be detected through prenatal screening and testing, or shortly after birth through clinical observations that are confirmed through genetic testing. The World Health Organization (WHO) estimates the incidence of Down syndrome to be between 1 per 1000 to 1100 live births worldwide. Rising maternal age over recent years has led to an increase in the syndrome, although this is somewhat offset by prenatal screening and terminations, leading to wide variations in incidence across countries (Loane 2013). For example, Ireland (where abortion has historically been tightly restricted) had an incidence of approximately 23 per 10,000 of live births between 1990 and 2009, which was much higher than other European countries, including the UK (10 per 10,000), France (7 per 10,000) and Germany (8 per 10,000) (Loane 2013), and twice as high as that reported in the USA (11.8 per 10,000; Shin 2009). Shin 2009 also reported a higher incidence in Hispanic individuals compared to non‐Hispanic whites and African Americans. Three types of chromosomal anomalies lead to Down syndrome. The most common is trisomy 21 (present in 95% of cases), followed by translocation (4%) and mosaicism (1%), the latter having better outcomes for language and cognitive abilities (Roizen 2007). Down syndrome is associated with a number of medical, physical and developmental difficulties, including motor and intellectual problems, although language is considered to be the area that is most impaired, with the greatest effect on independent living (Abbeduto 2007).
The intellect of children with Down syndrome varies widely, although most fall in the moderate range of intellectual disability (Roizen 2007). A meta‐analysis of speech and language skills in children with Down syndrome found similar variability and individual differences, though most had an impairment when compared to typically developing children of the same non‐verbal mental age (Nӕss 2011). One exception was vocabulary comprehension, which was in line with the children's non‐verbal mental age. Young children with Down syndrome are often reported to progress through stages and sequences of language and early communication development in a similar way to younger, typically developing children (Chapman 1997), albeit at a slower pace. This progress leads to an overall profile of delayed early language development (Polišenská 2014), with some differences (Ypsilanti 2008). The general profile of language difficulties in children with Down syndrome is poorer expressive language compared to language comprehension, particularly in the area of vocabulary, while for grammar, studies have reported both receptive and expressive difficulties (Laws 2004; Miller 1999). Phonology, syntax and particular aspects of pragmatic language development also present specific challenges for individuals with Down syndrome (Martin 2009). The heterogeneity of language development in this population has been well documented: while most children are delayed in the onset of their first words (Roizen 2007), others have found that some children start using words at a similar age to typically developing children (Chapman 1997). However, the gap in language attainment between children with Down syndrome and their typically developing peers, even those of the same non‐verbal mental age, tends to widen with increasing age. More importantly, research has uncovered disproportionate delays in the expressive language abilities of children with Down syndrome compared to those expected from their overall level of cognitive functioning, and relative to other groups of children with intellectual disability matched for chronological age, mental age and intelligence (Roberts 2008; Warren 2008; Yodor 2004; Yodor 2014). A significant contributor to speech and language impairment in this population is the high rate of hearing loss (Laws 2014), particularly fluctuating conductive hearing loss from frequent middle ear infections, which has been observed to affect 93% of one‐year olds, with 68% still affected at five years (Barr 2011). Deficits in auditory (phonological) short‐term memory have also been linked to language difficulties in this population (Chapman 2001; Laws 2003), as have early difficulties with joint attention (Zampini 2015). Their language difficulties are compounded by deficits in speech sound production and intelligibility (Kent 2013). Some studies have reported a plateau in linguistic attainment in adolescents, particularly for expressive language, morphosyntax (Laws 2004), and narrative production (Chapman 1998), while others have shown that they can continue to make gains in their language development into adulthood (Abbeduto 2007; Chapman 2001). Areas of relative strength for children with Down syndrome are in socialisation and non‐verbal communication through the use of gestures (Chapman 1997). Moreover, they can have a preference for gestures over verbal communication early in development, and research has found a positive relationship between gesture use and later expressive language (Te Kaat‐van den Os 2015).
Description of the intervention
There is strong consensus that children develop within the context of their family and that parents are best placed to support this development. Therefore, where children are at risk for developmental delay, training parents on how to promote early language development effectively is essential (Barton 2013). This intervention is particularly important for young children with Down syndrome, as there tends to be less interaction between parents and children with Down syndrome than typically developing children as young as five months of age (Slonims 2006). One important aspect of parent‐child interaction is responsivity. For example, Mahoney 1985a found that children with Down syndrome had higher scores on the mental domain of the Bayley Scales of Infant Development (BSID; Bayley 1969) if their mothers used a more responsive interaction style when playing with them, compared to children who had mothers who used a more directive or teaching style of interaction. A follow‐up study demonstrated that maternal responsivity was associated with increased use of words, imitation, and non‐verbal communication in the children when compared to those with mothers who used a didactic or inattentive style of interaction (Mahoney 1988). Optimal parental response is also a predictor of later productive language in studies of children with intellectual disabilities (Yodor 2004).
Caregivers can also influence their child's language development through the quality and quantity of their linguistic input and interactions. For example, Huttenlocher 2010 reported that the diversity of language input that children receive predicts their language growth, while more recent research has signalled the importance of children's active involvement in conversational exchanges with their caregivers (Romeo 2018). The language learning environment is also heavily influenced by parental socioeconomic status (Hart 1995; Hoff 2006). For young children with Down syndrome, research has shown that the vocabulary directed to them can be simpler, in terms of composition and variability, and that they receive a lower proportion of imitations from their mothers when compared to typically developing peers (Zampini 2011). It is important to realise that the effect on this interaction is bi‐directional, as the interactional characteristics of children with Down syndrome such as passivity and low requesting behaviours are also linked to differences in parental input with implications for their language learning experiences (Mundy 1995).
For the reasons outlined above, a large part of speech and language intervention for young children with Down syndrome involves training parents and caregivers about the importance of responsivity, quality and quantity of their language input and interaction to maximise cognitive, social and communication development. The intervention is known variously as '(interactive) focused stimulation', 'responsivity education/teaching' 'naturalistic teaching' or 'milieu teaching', but regardless of the label, the aim is similar: training caregivers to recognise and respond to verbal and non‐verbal communication and interaction in their children in order to encourage an increase in these behaviours (Warren 2008). One example is the Hanen Parent Program 'It Takes Two to Talkʼ (Girolametto 2006), which educates parents about the importance of child‐oriented behaviours to promote joint attention and reciprocal interaction and helps them to apply language facilitation strategies in natural, everyday interactions. Enhanced milieu teaching (EMT) is another version of this intervention, which combines elements of responsivity education with behavioural strategies and milieu teaching through modelling and appropriate environmental arrangements to reinforce children's communicative responses to adult prompts and teach targeted language goals (Hancock 2007). Other versions of the programme combine parent responsivity training with direct clinician‐mediated intervention (for example Fey 2006), but the focus of this review will be on parent‐mediated interventions to determine the effects outside of the intervention delivered by a clinician. In addition, although other programmes may encourage parents to explicitly teach their children manual signs or key‐word reading, this review will focus on interventions that target interactive language learning through daily activities and play.
Parent‐mediated interventions can take place in group classroom sessions where caregivers learn about communication strategies and then are regularly videotaped interacting with their child by the clinician in order to provide feedback and reinforcement of goals for the individual parent‐child dyad (Girolametto 2006). Alternatively, the intervention can be delivered on an individual basis, where a clinician and parent work together to devise goals for both the parent and child, and the clinician coaches the parent through discussion, role play, live modelling and video‐feedback on how to implement strategies to achieve these goals. Therefore, the outcomes of the intervention are measured primarily in terms of changes in the child's interaction, communication and language skills, but also through changes in caregiver behaviour and responsivity, as this is a key factor in the success of the programmes.
As language is acquired in everyday interactions between children and their caregivers, and as parents and caregivers spend the most time interacting and communicating with their children, this intervention is considered to be ecologically valid and family‐centred. Furthermore, best practice guidelines for speech and language therapy in preschool children with Down syndrome highlight the importance of early intervention and of parents being aware of, and trained in, effective strategies for promoting language and communication (Buckley 2002).
How the intervention might work
Parent‐mediated interventions come from naturalistic observations of the bi‐directional nature of adult‐child interactions, whereby an increase in non‐verbal or verbal communication from the child changes how the adult responds (known as contingent responses), which, in turn, helps to support further communication development in the child (Warren 2008). This means that both the child and those in their communicative environment change over time and affect each other in a reciprocal fashion. However, the interventions presume that more tailored, focused and intensive caregiver input is required in children with language delay, who have difficulty picking up on parental cues, and because both caregivers and children interact and respond differently when compared to typically developing children and their parents. The interventions aim to help adults become aware of the child's communication and interaction and their role in facilitating this development by altering their responses to their child. This should help children increase their frequency of intentional communication through joint attention and verbal or non‐verbal communication, or both (for example, pointing and gestures), thereby preparing children to use early language skills more efficiently (Warren 2008). Furthermore, the approaches aim to make caregivers aware of the quality and quantity of their own linguistic input to the children and to modify it according to the child's ability, which helps the child to understand and eventually use language themselves (Girolametto 1996). The overall aims of parent‐mediated interventions, therefore, are as follows.
To foster and increase adult‐child interaction and joint attention through child‐centred activities.
To promote the frequency and complexity of adult responsivity to non‐verbal and verbal communication.
To facilitate appropriate language modelling and prompting from adults that helps the child to understand and produce language.
The model of parent‐mediated interventions is 'triadic' (Roberts 2011), with an experienced clinician training parents to use specific interaction‐ and language‐promoting strategies with their children. This means that there are many aspects that can influence the overall effectiveness of the intervention, including how the intervention is delivered and by whom, parental implementation of the strategies, and the child's ability to benefit from the same. For example, an early study noted that maternal style of interaction and level of education before treatment affected the outcome (Yoder 1998). Other factors that might influence the outcome include the caregiver's relationship with the clinician, their willingness to implement the intervention, their socioeconomic status and levels of stress. How the intervention is delivered (for example, group or individually), the intensity of delivery, as well as the training and experience of the clinician delivering the intervention may also have an effect (Laudahl 2006). For the children, previous research has noted that baseline language and cognitive skills can influence a child's response to this type of intervention (Siller 2013); and similarly, the child's general health, hearing status, personality and behaviour could be important mediators of treatment gains. We attempted to extract this information from the studies, where provided, in order to understand the complex factors that make this intervention work.
Why it is important to do this review
Experts in the field of Down syndrome argue that "speech and language therapy is the most important part of intervention services for children with Down syndrome if we wish to promote their cognitive … and social development" (Buckley 2002, p 70). To date, however, there has been no systematic review of any speech and language intervention in children with Down syndrome. Changes in healthcare services for young children have moved towards providing for the needs of the whole family through initiatives such as individualised family service plans (IFSPs), which outline the support required by the whole family. As parents are best placed to facilitate their child's main language because they are able to maximise communication opportunities in everyday situations (Girolametto 2006), early intervention services are now embedded in the home and mediated through parents and caregivers (Kaiser 2011). The aim of this early intervention is to enhance family patterns of interaction within a transactional model of development that can change the child's actual and potential outcomes at an early and malleable stage of development. Sameroff 2000 (p 142) says that a child's development is "a product of the continuous dynamic interactions between the child and the experience provided by his or her family and social context". Thus, interventions that enhance those interactions with very young children are appropriate and well placed to support the most positive outcomes. However, the evidence base for these interventions has not yet been established for this group. Furthermore, the various therapist, parent, child and therapy factors (for example, mode of delivery, dosage etc.) that influence the success of the intervention are not yet known. Roberts 2011 carried out a meta‐analysis into the effectiveness of parent‐implemented language interventions, but this review was not limited to randomised controlled trials (RCTs) and included children with any type of language impairment. Cochrane Reviews on speech and language interventions exist, or are undergoing updates, for other identifiable groups of children with language difficulties such as those with primary speech and language delay or disorder as well as children with non‐progressive motor disorders (Law 2017; Pennington 2018). In addition, there are systematic reviews of parent‐mediated interventions for children with autism spectrum disorders (ASD; Oono 2013) and attention deficit hyperactivity disorder (ADHD; Zwi 2011), but, as yet, there are no reviews of parent‐mediated interventions for children with Down syndrome. Finally, as parent‐mediated interventions involve a considerable commitment from families and clinicians and are considered to be 'indirect', parents may become more stressed by having to be directly responsible for their children's intervention when they are already dealing with the additional demands of having a child with a disability (Brinker 1994). If early parent‐mediated interventions are to continue, we need to gather the evidence for the effects on the child's language and other communication skills and identify the specific factors that are likely to make them more successful. We anticipate that the findings from this review will help inform clinicians, parents and educators about best practice in early intervention for children with Down syndrome.
Objectives
To assess the effects of parent‐mediated interventions for improving communication and language development in young children with Down syndrome. Other outcomes are parental behaviour and responsivity, parental stress and satisfaction, and children's non‐verbal means of communicating, socialisation and behaviour.
Methods
Criteria for considering studies for this review
Types of studies
RCTs and quasi‐RCTs (studies where participants are allocated to treatments by, for example, date of birth, location or alternate allocation). We did not include cross‐over designs, as these are not considered appropriate for interventions with lasting consequences.
Types of participants
Primary caregivers of children with Down syndrome aged between birth and six years, irrespective of the severity or type of Down syndrome. All children had to be monolingual but could have spoken any language.
The term 'caregiver' includes grandparents and other caregivers who take on the 'parent' role for the purposes of the intervention.
We included studies of children with Down syndrome as part of a group of children with intellectual disabilities provided we could obtain the separate results for the group with Down syndrome.
Types of interventions
All parent‐mediated interventions designed to improve communication and language in children with Down syndrome from birth to six years of age. The intervention involved coaching, supervision and support from a clinician, and took place either on an individual or group basis. Specifically, we made comparisons between the parent‐mediated interventions and the following.
General stimulation conditions or teaching/treatment as usual (TAU).
Interventions that used clinician‐mediated interventions.
Controlled conditions that involved no treatment or delayed (wait‐listed) treatment.
We included studies in which the parent‐mediated intervention was delivered in conjunction with another intervention, such as a clinician‐mediated intervention, as long as the latter was given to both intervention and control groups, and the parent‐mediated intervention was provided only to those in the intervention group.
Types of outcome measures
Primary outcomes
Expressive and receptive language skills measured through scores from standardised tests, criterion referenced tests, parent reports, experimental tasks, and language samples/conversations (for example, the Reynell Developmental Language Scales (RDLS; Edwards 1997). The scores from language samples included: mean length of utterance (MLU), measured in words or morphemes; number of different words (NDW) in a sample; or total number of words (TNW), which could be used to calculate type‐token ratios (TTRs).
We also measured possible adverse effects of intervention such as an increase in parental stress as assessed by, for example, the Parenting Stress Index (PSI; Abidin 1995).
Secondary outcomes
Secondary outcomes included changes in parental behaviours/responsivity captured through videotaped interactions or observations and measured by a validated scale (for example, the Maternal Behaviour Rating Scale (MBRS; Mahoney 1999a), as well as parental satisfaction with the intervention measured by questionnaires and interviews. We also measured child‐related changes in non‐verbal communication (for example, pointing/gestures, use of signs) and socialisation (for example, requesting/commenting) assessed through naturalistic observations or videotaped interactions and validated checklists such as the MacArthur‐Bates Communicative Development Inventories (CDIs; Fenson 2007).
We considered possible secondary adverse effects of the intervention such as an increase in negative behaviour in the child (measured by the Maladaptive Behaviour Index (MBI) subscale of the Vineland Adaptive Behavior Scales (VABS; Sparrow 2005) or other validated scales) or language attrition (indicated by a reduction in scores from baseline language tests). We also measured the adherence to treatment, such as any non‐attendance or non‐completion of home practice by the parents, measured and reported by the study authors, plus any reasons for the same.
We measured the effects of the interventions at the following time points: immediately (within 1 month postintervention), short to medium term (1 to 12 months postintervention), and long term (one to two years postintervention).
We used all primary outcomes and four secondary outcomes (changes in parental behaviours/responsivity, socialisation, language attrition and adherence to treatment) to populate the 'Summary of findings' tables.
Search methods for identification of studies
Electronic searches
The Information Specialist of Cochrane Developmental, Psyhcological and Learning Problems, and one review author (COT) ran the searches in March 2016 and updated them in January 2018. We searched the following databases and trial registers to identify relevant trials.
Cochrane Central Register of Controlled Trials (CENTRAL; 2016 Issue 2), in the Cochrane Library, which includes the Cochrane Developmental, Psychosocial and Learning Problems Specialised Register.
MEDLINE Ovid (1946 to January week 2 2018).
MEDLINE In‐Process & Other Non‐indexed Citations OVID (searched 22 January 2018).
MEDLINE Epub Ahead of Print OVID (searched 22 January 2018).
Embase Ovid (1980 to 2018 week 4).
ERIC EBSCOhost (1966 to 22 January 2019).
PsycINFO Ovid (1806 to January week 2 2018).
CINAHL Plus EBSCOhost (Cumulative Index to Nursing and Allied Health Literature; 1937 to 22 January 2018).
Science Citation Index Web of Science (SCI; 1970 to 22 January 2018).
Social Sciences Citation Index Web of Science (SSCI; 1970 to 22 January 2018).
Cochrane Database of Systematic Reviews (CDSR; 2018, Issue 6), part of the Cochrane Library.
Database of Abstracts of Reviews of Effects (DARE; 2015, Issue 2; final issue), part of the Cochrane Library.
Academic Search Complete EBSCOhost (searched 22 January 2018).
ProQuest Dissertations and Theses UK & Ireland (1990 to 22 January 2018).
ProQuest Dissertations and Theses A&I (1970 to 22 January 2018).
LILACS (Latin American and Caribbean Health Science Information database; lilacs.bvsalud.org/en; searched 22 January 2018).
SpeechBITE (speechbite.com; searched 22 January 2018).
UK Clinical Trials Gateway (www.ukctg.nihr.ac.uk; searched 22 January 2018. Replaced UKCRN Portfolio Database searched 21 March 2016 ).
Clinical Trials.gov (clinicaltrials.gov; searched 22 January 2018).
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; apps.who.int/trialsearch/default.aspx, searched 22 January 2018).
We did not apply any restrictions on date, language or publication status. We planned to seek translations when necessary; however, all included studies were written in English, so translation was unnecessary. We report the search strategies used for each database in Appendix 1.
Searching other resources
We handsearched the reference lists of relevant journal papers, book chapters, and systematic reviews identified by the Electronic searches. We approached relevant professional organisations, such as Down Syndrome Education International (dseinternational.org), searched the website of the Hanen Centre (hanen.org), and emailed colleagues and researchers to identify other possible published and unpublished studies such as technical or research reports, conference abstracts and dissertations, or ongoing trials. We also searched WhatWorks (thecommunicationtrust.org.uk/whatworks), an online resource, which summarises research on intervention for speech, language and communication, based on the Better Communication Research Programme in the UK.
Data collection and analysis
Selection of studies
We managed all references generated from the search strategy using the reference management programme, EndNote X7.
We removed duplicates, and then the first two review authors (COT and AL) independently conducted an initial screening of titles and abstracts, eliminating any records that were obviously irrelevant to the review and identifying relevant studies based on our inclusion/exclusion criteria (Criteria for considering studies for this review). In cases where an abstract contained insufficient information to judge whether or not a study met the inclusion criteria, we retrieved the full text to independently examine adherence to our eligibility criteria. We resolved disagreements over inclusion by consulting a third review author (FG) for arbitration. We linked together multiple reports of the same study.
We report the outcome of the search strategy in the Results section below and in a PRISMA diagram (Moher 2009).
Data extraction and management
We developed and piloted a data extraction form based on the inclusion/exclusion criteria (for example, only RCTs or quasi‐RCTs, no single case studies) before carrying out full data extraction. Review authors (COT and AL) then independently extracted information from each paper on the following.
Participants: number; age (of caregivers and children); gender (of caregivers and children); caregiver status (parent/other); inclusion and exclusion criteria; child's intelligence quotient (IQ); socioeconomic status (for example, maternal education/income); hearing status; health status (of caregivers and children); comorbid conditions (for example, autism); and attendance at preschool or other therapy/educational settings.
Methods: baseline language and communication assessment(s); outcome measure(s) used and assessment results (for example, number of reported words or standardised scores); secondary outcomes, including any measures of caregiver behaviour/responsivity or stress through validated scales; and child measures of changes in non‐verbal communication and socialisation. We also recorded the timing of the outcome measurement.
Interventions: mode of delivery (for example, group or individual; clinic or classroom based; and whether video feedback was used); frequency and number of the intervention sessions; duration of the intervention sessions; date and location; qualifications and experience of clinician; and whether adherence was evaluated.
Training fidelity: we recorded the presence or absence of features of training fidelity based on implementation fidelity and intervention fidelity described in Barton 2013 and the categories proposed by Lieberman‐Betz 2015. We also recorded any sources of funding for the study.
Assessment of risk of bias in included studies
Two review authors (COT and AL), working independently, rated the risk of bias in each included study using Cochrane's tool for assessing risk of bias, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We reached final judgement of risk of bias by consensus. The assessment consisted of two parts. The first consisted of a succinct description, which included verbatim quotations from the study reports or from correspondence with the trial author(s), or a comment from the review author about the procedures used to avoid bias, or both. The second part was an assessment of the risk of bias by assigning a rating of the likely risk of bias for the adequacy of the following domains: sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective outcome reporting; other potential sources of bias. The detailed methods for judging 'Risk of bias' are in Table 3.
1. Assessment of risk of bias in included studies.
| Sequence generation | We outlined the methods used to generate the allocation sequence in sufficient detail, to assess whether it should have produced comparable groups, using quotations wherever possible. We added a comment, such as 'probably done' or 'probably not done', to supplement any ambiguous quotation. We assigned each included study to one of the following categories.
|
| Allocation concealment | We described the methods used to conceal the allocation sequence in sufficient detail to determine whether intervention allocation could have been foreseen in advance of, or during, recruitment and assigned the included studies to one of the following criteria.
|
| Blinding of participants and personnel | As this review is addressing parent‐mediated interventions, it was not possible (or highly unlikely) that participants who received the intervention (the caregivers) and the personnel who deliver the intervention (that is, the clinicians) will have been blinded to the type of intervention received. Nonetheless, we described the methods used, if any, to blind study participants and personnel from knowledge of which intervention was received for each included study. We assessed the risk of bias that resulted from any lack of blinding on a case‐by‐case basis, using the categories listed below.
|
| Blinding of outcome assessment | For each included study, we described the methods used, if any, to blind outcome assessor(s) from knowledge of which intervention a participant received. Assessment was made for each main outcome (for example, outcome measures at 6 and 12 months postintervention). We graded this domain as follows.
|
| Incomplete outcome data | We described the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. We reported the numbers in each intervention group (compared with total randomised participants); the reason(s) for attrition/exclusion, where provided; and any re‐inclusions in analyses performed by the review authors. We graded this domain as follows.
|
| Selective outcome reporting | We assessed the possibility of selective outcome reporting by the study authors by checking whether any of the stated outcomes were not reported at the end of the study. We assessed this by checking the trial protocol, if available from a trial registry or from the study authors, and by looking for potential inconsistencies of reporting in the final study paper, such as inconsistencies between the Methods and Results sections. We assigned each included study to one of the following categories.
|
| Other potential sources of bias | We described any additional problems that may have put a study at risk of bias. We graded this domain as follows.
|
Measures of treatment effect
We did not carry out quantitative analyses of the data, as the included studies used different intervention methods, outcome measures or both (see the 'Interventions' and 'Outcomes' subsections in the Results section below). As a result, we present the individual results of studies.
Table 4 presents the methods from our protocol that we had planned to use but did not (O'Toole 2016).
2. Methods planned in the protocol but not used in this review.
| Issue | Method |
| Primary Outcomes | We will consider both the level and rate of language development (as indicated by the change in scores) but will analyse these separately. |
| Measurement of treatment effect |
Binary and categorical data Binary or dichotomous data (for example, vocabulary improvement versus no change) may occur. Categorical data may also be presented where ordinal measurement scales are used. We will analyse these data by calculating the odds ratio and presenting it with a 95% confidence interval. |
|
Continuous data Most data from the expected outcome measures are likely to be continuous data such as standardised language test results, mean length of utterance (in words or morphemes), number of different words, and total number of words as derived from spontaneous language samples. Similarly, secondary outcomes (for example, changes in parental and child interactional behaviours) are also likely to be continuous data. Where possible, we will extract the numbers of participants, means and standard deviations in the intervention and control groups. We will use change‐from‐baseline scores (change scores) and postintervention only scores if the required means and standard deviations are available, as we expect to find only a small number of RCTs, thus making comparability at baseline problematic. We will analyse change scores and postintervention scores separately. However, if all studies measure outcomes using a uniform measurement scale, we will combine the different types of analyses using the (unstandardised) mean difference (or the 'difference in means') method in Review Manager 5 (RevMan 2014), as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011). Where studies measure the same outcome using different methods, we will use the standardised mean difference to combine studies and present it with 95% confidence intervals as a summary statistic. We will use Hedge's g to calculate the effect size since it is more appropriate for studies with small samples, as is expected in this review (Hedges 1985). Given the nature of child language assessment, it is likely that studies will use different methods of administration (for example, parental questionnaires versus direct assessment) and measure different aspects of language (comprehension versus expression). Therefore, we may need to conduct separate analyses for these outcomes. | |
| Unit of analysis issues |
Cluster‐randomised trials It is possible that we will include cluster‐randomised trials in this review (for example, groups of children attending different clinics or preschools). In this case, appropriate statistical approaches should be used; for example, using a 2‐sample t‐test to compare the means of the cluster in the intervention group at cluster level, or a mixed‐effects linear regression approach at individual level (Donner 2000). We will contact the study author(s) if it is unclear that appropriate adjustments have been made (Donner 2000). If individual level data cannot be secured, we will control the data for the clustering effects using the procedures described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).This will either be by extracting the number of clusters (or groups) randomised to each intervention group or the average (mean) size of each cluster; by extracting the outcome data ignoring the cluster design for the total number of individuals (for example, means and standard deviations); or by extracting an estimate of the intracluster correlation coefficient (ICC). We will obtain an appropriate ICC by using external estimates obtained from similar studies, and if this cannot be achieved we will explore the impact of the inclusion of data from cluster‐randomised trials by imputing a set of ICCs (for example, high (0.1), moderate (0.01), and small (0.001) ICC). We will calculate the inflated standard errors that account for clustering by multiplying the standard errors of the effect estimate by the square root of the design effect as outlined in Higgins 2011b (Chapter 16.3.6). We will combine the results with those from individually randomised trials for meta‐analysis using the generic inverse variance method in Review Manager 5 (RevMan 2014), providing that clinical heterogeneity between the studies is small (Donner 2000; Higgins 2011b). |
|
Multi‐arm studies For studies that compare more than 2 intervention groups, we intend to combine results across eligible intervention groups (that is, parent‐mediated interventions) to form a single intervention group and use pair‐wise comparisons to compare these with all eligible control groups combined to form a single control group. We will give detailed descriptions of the intervention groups and the nature of each study in the 'Notes' and 'Interventions' sections of the 'Characteristics of included studies' tables. | |
| Dealing with missing data | We will contact the authors of the included studies, where necessary, and ask them to supply any missing data or relevant unreported information. We will describe the missing data and the reasons, numbers and characteristics of dropouts/attrition for each included study in the 'Risk of bias' tables beneath the 'Characteristics of included studies' tables. We will consult the Cochrane Handbook for Systematic Reviews of Interventions for options for dealing with missing data (Higgins 2011b). If the data appear to be missing at random, we will analyse the available data only. If data are not missing at random, we will impute the missing data with replacement values and treat these as if they were observed. For missing continuous data, we will impute the missing data either by using last observation carried forward or mean scores. For dichotomous data, we will perform a sensitivity analysis based on best and worst case scenarios to assess how sensitive results are to changes in the missing data (Gamble 2005). A best case scenario is where all participants with missing outcomes in the intervention group had good outcomes, and those in the control group had poor outcomes; a worst case scenario is the reverse. We will address the potential impact of missing data on the findings of the review in the Discussion section. |
| Assessment of heterogeneity | We will assess statistical heterogeneity by using the Chi2 test for heterogeneity, through visual inspection of forest plots, and by using the I2 statistic (Higgins 2002; Higgins 2003). As the Chi2 test has low power in a meta‐analysis of a small sample of studies, we will use the recommended P value of 0.10 (rather than the typical value of 0.05) to determine statistical significance (Deeks 2011). In addition to a test of statistical heterogeneity, we will use the I2 statistic to detect inconsistencies across studies. We will use the formula and guidelines for interpreting the outcomes outlined in Deeks 2011 (section 9.5.2), which includes taking the magnitude and direction of effects into account as well as the strength of evidence for statistical heterogeneity (for example, a CI for I2). Should we identify any unexpected variability in these areas we will discuss it in full. |
| Assessment of reporting bias | We will draw funnel plots (estimated differences in intervention effect sizes against their standard error) if we find sufficient studies (N = 10). An asymmetric appearance of the funnel plot might indicate a relationship between effect size and study size, which would suggest the possibility of either reporting bias or poor methodological quality in small studies leading to inflated effects. If we identify funnel plot asymmetry, and there are at least 10 studies included in the meta‐analysis, we will consult a statistician for assistance in implementing statistical tests for funnel plot asymmetry in line with recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Sterne 2011). Should a relationship between trial and effect size emerge, we will examine the clinical diversity of the studies (for example, sample size or use of blinded outcome measures). |
| Data synthesis | We will carry out a meta‐analysis using Review Manager 5 (RevMan 2014), if there are sufficient data and where the interventions are similar in terms of the characteristics of the participants, the ways in which parent‐mediated interventions are delivered, the frequency and duration of interventions, and the outcome measures used. We will apply both fixed‐effect and random‐effects models and compare the results to assess the impact of statistical heterogeneity. We will present the results from the random‐effects model only, unless contraindicated (for example, if there are large differences between the results from fixed‐effect and random‐effects meta‐analyses or if there is funnel plot asymmetry). In the case of serious funnel plot asymmetry, we will present both fixed‐effect and random‐effects analyses, under the assumption that asymmetry suggests that neither model is appropriate. If the same outcome is presented as dichotomous data in some studies and as continuous data in other studies, we will convert odds ratios for the dichotomous data to standardised mean differences if it can be assumed that the underlying continuous measurements follow a normal or logistic distribution. Otherwise, we will conduct separate analyses. |
| Subgroup analysis and investigation of heterogeneity | If we identify sufficiently homogenous studies, we will conduct subgroup analyses to assess the impact of the following.
|
| Sensitivity analysis | We will conduct a sensitivity analysis to examine the impact of study quality on the robustness of the conclusions drawn. This will be based on our assessment of the risk of bias concerning the quality of factors such as randomisation, blinding of outcome assessment, and completeness of data. We will include in the analysis studies that we categorise as low or unclear risk of bias for these factors. |
RCT: randomised controlled trial.
Assessment of heterogeneity
We assessed clinical heterogeneity by considering the variability in the participants (for example, socioeconomic status, age of parents and children, health status and linguistic abilities of the children), trial factors (for example, duration and intensity of the interventions, randomised concealment), and outcomes (for example, parent report versus direct assessment) studied.
Data synthesis
We did not conduct quantitative analyses of the data due to heterogeneity amongst the included studies. Thus, we present the individual results of studies in successive sections.
'Summary of findings' table
We assessed the overall quality of the body of evidence using the GRADE approach (Guyatt 2008). The GRADE Working Group outlines five factors that may decrease the quality of a body of evidence. These are: limitations in the design and implementation of available studies (high risk of bias), inconsistency (unexplained heterogeneity), indirectness (population, intervention, comparison and outcome), imprecision of results, and high probability of publication bias. Two review authors (COT and AL) assessed the quality of the body of evidence for each outcome against these criteria and assigned each one a judgement of high, moderate, low, or very low quality. There were no disagreements between the review authors. We reported this information in Table 1, comparing parent‐mediated intervention versus treatment as usual, and Table 2, comparing parent‐ and clinician‐mediated intervention to clinician‐mediated intervention alone, which we constructed using GRADE profiler (GRADEproGDT 2015). We included all primary and secondary outcomes in our assessment of quality, and outcomes ranged from immediately after the intervention to 12 months postintervention.
Summary of findings for the main comparison. Parent‐mediated intervention versus treatment as usual for communication and language development in young children with Down syndrome.
| Parent‐mediated intervention versus treatment as usual for communication and language development in young children with Down syndrome | |||
|
Patient or population: children with Down syndrome aged between birth and six years Setting: home, clinic, or both; interventions delivered through group or one‐to‐one sessions Intervention: parent‐mediated intervention Comparison: treatment as usual | |||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) |
|
Expressive language (number of (different) target words) Assessed with: parent reports, language sample, experimental task Follow‐up: 3 weeks |
1 study found that the intervention did not increase the children's overall vocabulary size on a standardised parent report. However, parents in the study reported that the intervention group used almost 5 more targeted words than the control group (P < 0.05), postintervention. Children who received treatment also used almost 2 more target words in free‐play interaction with their mothers than those in the control (P < 0.05), although no differences were noted in the production of these target words in a semi‐structured experimental task | 12 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c,d |
|
Receptive language (total language; standard scores) Assessed with: direct assessment; parent reports Follow‐up: 2 months |
1 study found that children in the intervention group made a 50% increase in their 'language' scores (P < 0.01) using direct assessment, and a 47% increase in their 'language‐cognitive' scores (P < 0.01) using parent reports, compared to just 12% and 3% increases respectively in the control group | 15 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,d |
| Parental stress | Not measured | ||
|
Changes in parental behaviour/responsivity Assessed with: observational rating scales (not specified); Maternal Behaviour Rating Scale (Likert scale scored 1‐5; higher scores indicate increased use of coded behaviour); self‐reports Follow‐up: range 3 weeks to 2 months |
1 study found that mothers in the intervention group used almost 3 more target labels (P < 0.05), almost 7 more focused stimulation of target labels (P < 0.001) and maintained a more stable rate of talk (P < 0.05) compared to those in the control group. However, the mothers did not use more complex language than those in the control group postintervention. Qualitative information found that mothers also reported changes in the way they communicated with their children after the intervention, which was confirmed through checklists completed by clinicians following home visits | 27 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,d |
| 1 study found that mothers in the intervention group made a 67% increase (P < 0.001) in their 'responsiveness' ratings and a 56% increase (P < 0.001) in their ratings on 'affect', compared to the control group increases of 13% and 6%, respectively. The intervention group also reduced their ratings on 'achievement/directiveness' by 27% (P < 0.01), compared to a 3% reduction in the control group, postintervention | |||
|
Socialisation
Assessed with: direct assessment; parent reports; Child Behaviour Rating Scale (Likert scale scored 1‐5; higher scores indicate increased use of coded behaviour) Follow‐up: 2 months |
1 study found that children in the intervention group increased their social development quotient scores on direct assessment by 50% (P < 0.01) and on parent reports by 44% (P < 0.01), compared to 13% and 3% increases, respectively, in the control group. A rating scale also found that the intervention group increased their ratings in attention by 54% (P < 0.001) and initiation by 57% (P < 0.001), compared to 11% and 7% in the control group, respectively | 15 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,d |
|
Language attrition Assessed with: parent reports; direct assessment; language samples; experimental task Follow‐up: range 3 weeks to 2 months |
No studies reported evidence of language attrition in the intervention or control group at postintervention | 27 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,d |
|
Adherence to treatment Assessed with: consumer questionnaire; observation checklists (not specified) Follow‐up: 3 weeks |
1 study found that mothers in the intervention group attended at least 7/9 training sessions and all 4 home visits | 12 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c,d |
| CI: confidence interval; RCT: randomised controlled trial. | |||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||
aDowngraded by two levels as the sample size was not justified and was small, and the analysis involved a narrative synthesis and so estimates are not available. bDowngraded by one level as it is not possible to measure inconsistency from a single study. cDowngraded by one level as the control group had a cointervention in one study. dDowngraded by two levels as the risk of bias was judged to be high or unclear risk for most factors.
Summary of findings 2. Parent‐ and clinician‐mediated intervention versus clinician‐mediated intervention alone for language development in young children with Down syndrome.
| Parent‐ and clinician‐mediated intervention versus clinician‐mediated intervention alone for communication and language development in young children with Down syndrome | |||
|
Patient or population: children with Down syndrome aged between birth and six years Setting: home, clinic, or both; interventions delivered through group or one‐to‐one sessions Intervention: parent‐ and clinician‐mediated intervention Comparison: clinician‐only‐mediated intervention | |||
| Outcomes | Impact | № of participants (studies) | Certainty of the evidence (GRADE) |
|
Expressive language (number of words; standard scores; MLUw; NDW; IPSyn; frequency of unique targets; % target talk) Assessed with: parent reports; direct assessment; language sample analysis; experimental task Follow‐up: range 1 day to 12 months |
1 study found no child language differences between the groups based on parent‐report or norm‐referenced measures immediately, 6 months or 12 months postintervention. Similarly, there were no differences in child language measures based on trained experimental tasks, apart from the number of utterances with child language targets, which was ranked more than twice as high for the intervention group (P = 0.006) immediately postintervention and almost twice as high for the intervention group (P = 0.043) at 6 months postintervention,compared to the control group. This difference was not maintained 12 months postintervention. No differences were noted in the untrained activities at any time point postintervention. | 18 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
|
Receptive language (total language; standard scores) Assessed with: direct assessment Follow‐up: range 1 day to 12 months |
1 study found no child language differences between the groups for any norm‐referenced measures for any time point postintervention | 18 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
|
Parental stress (total stress scores)
Assessed with: Parenting Stress Index Follow‐up: range 1 day to 12 months |
1 study did not find any differences between total parental stress scores at any time point postintervention | 18 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
|
Changes in parental behaviour/responsivity Assessed with: Milieu Teaching Project KidTalk Code Rating Scale (scored on a scale of 0‐100%; higher scores indicate increased use of target strategies as a % of potential episodes) Follow‐up: range 1 day to 12 months |
1 study found that parents in the intervention group were ranked, on average, twice as high on a measure of 'responsive interaction' immediately (P = 0.006, P = 0.005), 6 months (P = 0.006, P = 0.002) and 12 months (P = 0.001, P = 0.030) postintervention in trained and untrained activities, respectively. They were also ranked, on average, twice as high on the number of 'expansions' used at all time points on trained and untrained activities postintervention compared to the control group. With the exception of 12 months postintervention in trained activities, parents had a higher ranking on 'percentage of language modelling' at all time points in trained and untrained activities. The intervention group were ranked almost twice as high on their use of 'milieu teaching prompts' immediately postintervention in untrained activities (P = 0.021) and 6 months postintervention in trained (P = 0.020) and untrained (P = 0.005) activities compared to the control group. This was not maintained 12 months postintervention in trained or untrained activities. | 18 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Socialisation | Not measured | ||
|
Language attrition Assessed with: parent reports; direct assessment; language sample; experimental task Follow‐up: range 1 day to 12 months |
1 study did not find evidence of language attrition in the intervention or control group postintervention | 18 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b,c |
| Adherence to treatment | Not measured | ||
| CI: confidence interval; IPSyn: Index of Productivity Syntax; MLUw: mean length of utterance in words; NDW: number of different words; RCT: randomised controlled trial; TNW: total number of words | |||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||
aDowngraded by one level as we judged the risk of bias to be high or unclear for some factors. bDowngraded by one level as it is not possible to measure inconsistency from a single study. cDowngraded by two levels as the sample size was small and the analysis involved a narrative synthesis and so estimates were not available.
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies tables.
Results of the search
The searches yielded a total of 8604 records (8599 from searching of databases and 5 additional records from searching secondary sources). After removing duplicates, two review authors (COT and AL) independently screened the titles and abstracts of 5408 records and found 63 that were potentially relevant. We retrieved and assessed the full‐text reports for eligibility and contacted the authors of 11 studies to request further detail and clarification. We received responses from the authors of nine studies, either to confirm that they excluded children with Down syndrome from their study (Gibbard 1992; Gibbard 1994; Gibbard 2004; Leung 2016; Mahoney 1985b), or that they no longer had access to the data to extract the results for the children with Down syndrome separately (Girolametto 1988; Heifetz 1977; Innocenti 1993; Tannock 1992). COT and AL disagreed over the inclusion of two studies and consulted a third review author (FG) for arbitration. Following this process, we determined that three studies met the inclusion criteria. We also contacted the authors of these studies with requests for clarification and further data. One responded to say that they no longer had access to the data (Girolametto 1998) and another shared the data set for the children with Down syndrome only (Kaiser 2013). We received no response from the author of the third study. See Figure 1 for a breakdown of the search results.
1.
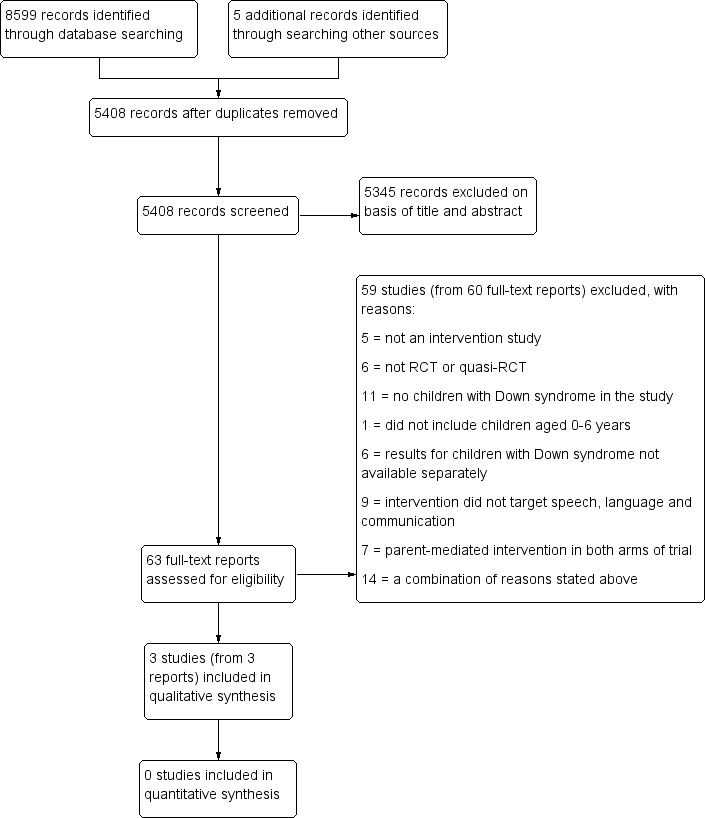
Study flow diagram.
Included studies
This review includes three included studies, all of which were published in peer‐reviewed journals (Girolametto 1998;Karaaslan 2013a; Kaiser 2013). Kaiser 2013 published the results for their entire group of preschool children with intellectual disabilities, but following a request from the review team, provided an SPSS file with the data for the 18 children with Down syndrome separately. COT undertook secondary analysis of this data, thus the results presented for Kaiser 2013 in this review are for the children with Down syndrome only.
Location and setting of studies
Girolametto 1998 took place in Toronto, Canada; Karaaslan 2013a in Turkey; and Kaiser 2013 in Tennessee, USA. All studies used a combination of clinic and home‐based interventions. As the aim of the intervention is to increase and improve parental responsivity and language input in naturalistic settings, all studies encouraged parents to apply techniques opportunistically.
Participants
The studies included between 12 and 18 children with Down syndrome with ages ranging from 29 months to six years. Girolametto 1998 and Kaiser 2013 reported that the children's IQ ranged from 53‐103, that the children used at least 10 single words or signs, that most children had hearing that was within normal limits, and that English was the only language in the home. Karaaslan 2013a did not report this detail. None of the studies reported whether the children had any comorbid conditions such as autism. The participating parents were all mothers, apart from one father in the Kaiser 2013 study, and they ranged in age from 29 to 51 years. All studies reported that the families were 'middle class' and 'intact' or with married parents. About half of the parents in the Girolametto 1998 and Kaiser 2013 studies were reported to be homemakers, with the other half being employed on at least a part‐time basis. Karaaslan 2013a did not report on maternal occupation.
Interventions
Although the theoretical basis of the interventions was similar, their content and mode of delivery differed.
Girolametto 1998 used the Hanen Parent Program (Manolson 1992), based on an interactive model of language intervention, teaching parents to model language at their child's level during naturally occurring situations. The programme was modified to a focused stimulation approach whereby each mother in the intervention group chose 10 words from a list of 20 target words that they thought their child would be most motivated to learn. These words were thought to be understood but not spoken by the children, developmentally appropriate, functional and began with a phoneme the child used, as reported by parents. Once the child used a word three times spontaneously in three different contexts (as determined from parent diaries), the word was replaced by another word from those remaining on the list. Mothers also learned how to set up routines to allow for modelling of the target words and how to use signs as they spoke with their children. The programme included group sessions to teach techniques through discussions, videotaped examples or role play. In addition, mothers received individual home visits with videotaping to give them feedback and coaching on their use of the techniques with their children. An experienced speech‐language pathologist who was certified by the Hanen Centre to administer the programme delivered the intervention. Children in the intervention group did not participate in any other therapy during the parent programme.
Karaaslan 2013a used responsive teaching (RT), which trains parents to increase their responsivity while modelling behaviours and communications matched to the child's level of functioning. The intervention consisted of individual, parent‐child sessions that were conducted at either a centre‐based facility or in families' homes. The procedures used were based on those recommended in the RT manual whereby the trainer first explains why the behaviour is linked to the child's development, then describes and demonstrates strategies for parents to use, before coaching them and providing feedback as they interact with their child. The intervention was provided by a professional with a doctoral degree in special education who had received five months of training on RT in the USA and was a certified RT provider. Children in both groups continued to receive early intervention services at their local special education rehabilitation centres twice a week during the intervention. This consisted of one hour of group special education or two hours of individual special education support, or both, per week. During group instruction, children were taught social and adaptive living skills, typically through the use of picture exchange communication system and applied behavioural analysis. Individual sessions consisted of one‐to‐one instruction related to the outcomes listed on the child's individualised education programme. Parents could observe but did not participate actively in this intervention.
Kaiser 2013 used enhanced milieu teaching (EMT), a hybrid naturalistic teaching procedure that uses a child's interests and initiations as opportunities for adults to model and prompt language use in everyday contexts. It includes the use of environmental arrangements, responsive interaction, specific language modelling and expansions, and milieu teaching prompts to increase the frequency and complexity of language. It is argued to be more structured than focused stimulation, with increased use of models and prompts (DeVeney 2016). The intervention also involved selecting words to target for each child based on their performance on the languages tests and samples competed prior to the intervention. The study compared the communication outcomes for children who received EMT provided by a parent and a therapist (intervention condition) to those of children who received EMT from a therapist only (control condition). The therapists and parent‐trainers had at least a bachelor's degree related to child development or special education and were trained to criterion on the intervention procedures prior to working with children. In the intervention condition, parents first participated in a workshop that included individualised information about language development, behaviour, play, environmental arrangements and routines that are foundational to the EMT intervention. They received written information on each topic, with individualised information on their child's language development. Following this, parents received clinic‐ and home‐based treatment sessions. In the clinic‐based sessions, one therapist intervened with the child, and the other trained the parent. The sessions consisted of parent training on a specific EMT strategy, which was then implemented with the child by the therapist while the parent observed with the parent trainer. Then, the parent implemented the strategy, with coaching, support and feedback provided by the parent trainer. The home sessions involved similar support and feedback from the parent trainer on the parent's use of EMT strategies. Most of the children in the intervention group (6/8) continued to receive regular community‐based speech‐language therapy during the intervention, as well as other special education services. Because the nature of the intervention in this study was different to Girolametto 1998 and Karaaslan 2013a, in that the intervention condition involved both parent and therapist‐mediated intervention, we presented the results from Kaiser 2013 separately.
Control condition
Girolametto 1998 and Karaaslan 2013a used a TAU control condition, and Kaiser 2013 used a therapist‐only control condition in addition to TAU. In the Girolametto 1998 study, families in the control group were all enrolled in preschool programmes, so they continued to receive language intervention services during the intervention phase. Four of the six children received monthly consultations from a speech‐language pathologist who provided parents with language stimulation ideas. One child was enrolled in a specialised treatment centre that employed a speech‐language pathologist who consulted with teachers and families. The exact nature of the consultation and advice received by parents and the children in the control group was otherwise not described. In addition, unlike those in the intervention group, parents in the control group were not aware of the 20 target words used as outcome measures of the intervention, which, as outlined in the Risk of bias in included studies section, has implications for how the outcomes were measured. Children in Karaaslan 2013a received the same two‐day per week early intervention services as those described for the intervention group (see 'Interventions' section directly above). The control group in the Kaiser 2013 study received the same EMT intervention sessions, although only delivered by a clinician. In the clinic‐based sessions, two therapists used EMT strategies within child‐preferred play activities identified by the parent, but the parent did not watch these sessions. In addition, one therapist implemented EMT in the child's home, and it is unknown whether parents used similar materials in these routines outside the intervention sessions. The therapists in the control group chose the child's target words and focused on them in the intervention sessions. Furthermore, similar to those in the intervention condition, most of the children in the control arm of this study (6/10) received regular community‐based speech‐language therapy during the intervention, as well as other special education services.
Duration and frequency of treatment
The duration and intensity of the interventions varied greatly. Girolametto 1998 had nine weekly, 2.5‐hour group training sessions and four individual home visits (duration unspecified). Karaaslan 2013a involved weekly, individual parent‐child sessions lasting between 1.5 and 2 hours over six months. They did not specify how many sessions took place in total, although it was probably between 24 and 26. Finally, Kaiser 2013 had one 2‐ to 3‐hour individual workshop, followed by 24 twice‐weekly individual sessions of 30 minutes each and 12 home sessions of 20 minutes each. The same dosage was used for children in the control group, albeit without the initial workshop or parental involvement in the intervention. As all studies were unclear on some aspect of the timing of the intervention, it is not possible to be exact about the total time involved in each study. However, an approximation would be a total of 26.5 hours for Girolametto 1998 (9 × 2.5 hours + 4 × 1‐hour home sessions); 48 hours for Karaaslan 2013a (24 × 2‐hour sessions), and 19 hours for Kaiser 2013 (1 × 3‐hour workshop + 24 × 30‐minute clinic sessions + 12 × 20‐minute home sessions). Using the Warren 2007 classification of intervention intensity, it seems that families in the Kaiser 2013 study had a higher dosing frequency of three times per week over a 12‐week period, but those in the Karaaslan 2013a study had a higher total intervention duration of six months (albeit at a lower dose frequency of once per week), resulting in almost twice the amount of cumulative intervention intensity of their intervention compared to the other two studies.
Training fidelity
Training fidelity in parent‐mediated intervention is complex and involves measuring what Barton 2013 terms 'implementation fidelity', or the training and support given by clinicians, as well as 'intervention fidelity', relating to parental use of the intervention strategies. Furthermore, Lieberman‐Betz 2015 recommends that four subcomponents of treatment fidelity need to be considered for both clinicians and parents: dosage (amount of intervention provided); adherence (whether prescribed elements were delivered accurately); quality (how well the strategies were delivered); and participant responsiveness (how both parents and children responded to the intervention). All of the studies in this review addressed at least some aspects of implementation fidelity. For example, all three studies provide information on the dosage of the intervention offered to parents by the practitioner (outlined under 'Duration and frequency of treatment' directly above), but only Girolametto 1998 reported the actual attendance data at these sessions. In that study, all mothers in the intervention group attended at least seven of the nine training sessions and all four home visits. Although Kaiser 2013 documented that one parent apiece dropped out from the intervention and control conditions between the beginning of the pretest assessments and the beginning of the interventions, it was not clear whether the participants attended all 36 sessions over the 12 weeks.
Karaaslan 2013a looked at implementation adherence by evaluating the degree to which the interventionist adhered to both the RT curriculum content and intervention procedures. An independent coder rated 10% of all sessions by using a 24‐item responsive teaching (RT) intervention session guide, judging treatment integrity to be 100% for all sessions. Kaiser 2013 addressed adherence by first training clinicians to criterion on the intervention procedures prior to working with the children, and secondly by videotaping 20% of the sessions, which they subsequently transcribed and coded using the Milieu Teaching Project Kidtalk Code for the four main EMT strategies (Vijay 2004). The overall fidelity of therapist delivery of EMT was calculated by dividing the percentage of use of each of the four EMT strategies by the criterion level to yield a percentage of fidelity. Therapist use of EMT strategies was 100% for both the control and intervention condition. For the parent training, three components (pre‐teaching, coaching and feedback) were evaluated using a checklist for 20% of clinic and home sessions, and overall fidelity was calculated by summing scores for each of the individual components. Fidelity was above 80% for home and 76% for clinic feedback. It was unclear in both Karaaslan 2013a and Kaiser 2013 who was involved in measuring this fidelity, and Girolametto 1998 did not document implementation adherence. None of the studies looked at implementation quality. Finally, all three studies measured participant responsiveness for parents by measuring their interactive behaviours before and after the intervention. We considered these results to be Secondary outcomes of this review and discuss them under 'Outcome measures' directly below.
In terms of intervention fidelity, no study measured dosage at the parent level; that is, how often parents used strategies with their children outside of the intervention sessions. This makes it very hard to evaluate the efficacy of the intervention, as the assumed benefit is that parents have many opportunities to implement the strategies with their children at home (Lieberman‐Betz 2015). Neither Karaaslan 2013a nor Kaiser 2013 measured parental adherence to the intervention. Girolametto 1998 addressed adherence by having the clinician complete a checklist following each home visit, which confirmed that the mothers used target words and demonstrated focused labelling during the second, third and fourth home visits. None of the studies reported on the quality of intervention fidelity. Finally, all three studies measured participant responsiveness for children by recording changes in the children's language or socialisation in response to the intervention, as outlined under 'Outcome measures' directly below.
Outcome measures
The three studies used a wide variety of methods to measure the outcomes, and it was not always clear which linguistic construct (such as expressive or receptive language) the assessment was targeting. For this reason, we did not combine the measures in a meta‐analysis but summarised the data narratively, provided they used similar methods or assessed similar constructs, in the Effects of interventions section. Girolametto 1998 used a parent‐report tool (Mervis's adaptation of the communicative development inventory (CDI; Fenson 1993), which combines all sections of the 'Words and Gestures and Words and Sentences' checklist; a direct assessment (using the receptive scale of the sequenced inventory of communication development (SICD); Hedrick 1984); free play situations between the mother and child; and experimental probes targeting the child's use of 20 individualised, target vocabulary items over two sessions within three weeks postintervention. Each session took approximately 90 minutes. All of the outcomes were reported in median scores and ranges, and the results from the SICD were not reported in the paper. When we contacted the authors, they told us that the data had been destroyed, which meant that we could not combine the results with scores from other studies in a meta‐analysis. This study did not measure the primary outcome related to parental stress but did measure some relevant secondary outcomes. The first was changes in maternal interactional behaviours, measured by maternal use of language‐modelling techniques based on a 15‐minute sample of videotaped interaction. From this sample, they calculated rate of talk (number of utterances/min), complexity of language input (mean length of utterances in morphemes (MLUm) and type token ratio (TTR)) and use of labels (number of focused target words). Changes in maternal behaviours were also collected from a consumer questionnaire completed by the mothers following the programme, and confirmed through therapist observations over the home visits. It was not clear if all assessors were blind to the group assignment.
Karaaslan 2013a used two broad, standardised measures of child development. The first was the Turkish version of the Denver Developmental Screening Test II (Denver II), which includes 116 items that assess four domains of developmental functioning: 'personal‐social', 'language', 'fine motor', and 'gross motor' development (Anlar 1996). For the most part, a certified examiner observed the child to assess this outcome, although parents provided information on items that could not be observed. Study authors provided no further detail on whether the 'language' domain referred to expressive or receptive language, so we assumed that it refers to total language abilities. The second assessment was the Ankara Developmental Screening Inventory (ADSI), a parent‐report tool used to assess four domains of 'cognitive‐language', 'fine motor', 'gross motor', and 'social/emotional' functioning (Savaşir 1994). Again, no further detail was available on what skills the investigators assessed under the 'cognitive‐language' domain, so we assumed that it too referred to total language abilities. In addition, the secondary outcome of parental behaviour was measured using the Turkish translation of the Maternal Behaviour Rating Scale (MBRS), a five‐point Likert rating scale that assesses characteristics of mothers' interactive style in terms of 'responsiveness', 'affect' and 'achievement/directiveness' (Mahoney 1999a), measured from a transcription of a 15‐minute video of the mothers and children playing with a set of developmentally appropriate toys. Investigators also used the Turkish translation of the Child Behaviour Ratings Scale (CBRS) to rate children's interactional behaviours from the video (conceptualised under 'socialisation' in Table 1) (Mahoney 1999b). This scale assesses children's engagement in social interaction across 'attention' and 'initiation'. Two raters who were blinded to group assignment coded video recordings of the mother‐child interaction separately for the MBRS and CBRS. Most of these outcomes, as well as those from Girolametto 1998, are summarised in Table 1.
Kaiser 2013 used a number of directly administered assessments, parent reports and observational measures from spontaneous language samples and experimental procedures to measure the children's language at the end of the intervention. These assessments were carried at three time points: immediately postintervention; six months postintervention and 12 months postintervention. The direct assessments included the Preschool Language Scale‐4 (PLS‐4; Zimmerman 2002), the Expressive Vocabulary Test (EVT; Williams 1997), and the Peabody Picture Vocabulary Test‐III of receptive vocabulary (PPVT‐III; Dunn 1997). Crude and standardised mean scores as well as standard deviations were available for all of these tests, which were undertaken by clinicians who were not involved in the child's intervention but not blind to the intervention condition. The parent‐report measure was the MacArthur Communication Development Inventory: Words and Sentences (MCDI:WS; Fenson 1993), which measured total number of words produced by the child (expressive vocabulary). In addition, standardised language samples were collected during a 20‐minute play interaction with a responsive adult who did not prompt the child. A number of linguistic measures were derived from these samples using the Systematic Analysis of Language Transcripts (SALT; Miller 1992). These were number of different words (NDW), MLU in words (MLUw) and the Index of Productivity of Syntax (IPSyn; Scarborough 1990), which is a measure of syntactic and semantic development. Finally, children and parents in both conditions were videotaped interacting in two 5‐minute play activities at home, one in which the intervention group had received training and one in which they had not (i.e. untrained activity). This was transcribed using SALT and coded using the Milieu Teaching Project KidTalk Code rating scale by a familiar member of staff who was not the child's therapist or parent's trainer (Vijay 2004). Child‐coded variables included the number of child vocabulary targets produced and the percentage of child utterances that contained any of the child language targets in trained and untrained activities. MLUw and NDW were also calculated from these activities. Parents moreover completed the Parenting Stress Index (Abidin 1995), and the scores were summarised into the parent domain, which relates to potential sources of stress for parent‐child relationships across seven domains: competence, isolation, attachment, health, role restriction, depression and spouse. For secondary outcomes, Kaiser 2013 measured changes in parental behaviours based on their use of four EMT strategies on the Milieu Teaching Project Kidtalk Code rating scale from observations of the parents and children interacting in both trained and untrained activities. These strategies were 'responsive interaction' (% of child utterances to which the adult responded); 'language modelling' (% of adult utterances that contained one of the child language targets); 'expansions' (% of child's utterances to which the adult expanded the child's utterance by repeating the child's words and then adding one or more words); and 'milieu teaching prompts' (% of prompting episodes that were delivered in response to a child request, following a system of least to most support, and giving the child the desired action or object at the end of the prompt sequence). The observational methods were transcribed and coded by students who were blind to the intervention condition. Most of these outcomes are summarised in Table 2.
Funding
A grant from the Hospital for Sick Children Foundation (Toronto, Ontario, Canada) funded Girolametto 1998. Kaiser 2013 received partial funding from the National Institute of Child Health and Human Development (grant HD45745) and the Department of Education (grant H325D070075) in the USA. Karaaslan 2013a did not specify any funding sources.
Excluded studies
We excluded 59 studies (from 60 reports) for various reasons, which we summarise below.
Five studies were review articles describing what is involved in similar parent‐mediated interventions (Buschmann 2010; Estes 1984; Hopman 1989), mental health treatment for adults (McNally 2008), or similar interventions for children with developmental delay (Te Kaat‐van den Os 2017).
Six studies were not RCTs or quasi‐RCTs (Barna 1980; Bauer 2014; Bauer 2015; Bidder 1975; Pelchat 1999; Wright 2017).
Eleven studies did not include participants with Down syndrome in the study (Bagner 2016; Barnett 1988; Baxendale 2003; Gibbard 1992; Gibbard 1994; Haney 1993; Leung 2016; Mahoney 1985b; Moxley‐Haegert 1983; Pratt 2015; Roberts 2015).
One study did not include children aged between birth and six years (Hornby 1984).
Six studies did not provide the results for children with Down syndrome separately from the rest of the participants (Boyce 1993; Girolametto 1988; Heifetz 1977; Innocenti 1993; Karaaslan 2013b; Tannock 1992). We attempted to make contact with all authors (see Discussion), and four responded to say that the data were no longer available (Girolametto 1988; Heifetz 1977; Innocenti 1993; Tannock 1992).
In nine studies the intervention did not target communication and language but focused on problematic behaviour (Allin 1988; Bagner 2007; Hassiotis 2017; Roberts 2006; Roux 2013; Shapiro 2014; Sofronoff 2011); self‐help skills (Kashima 1988); or family functioning and use of support networks (Coutinho 2003).
Seven studies had parent‐mediated interventions in both arms of the trial (Aparicio 2003; Cologon 2017; NCT02158390; Russell 2004; Seifer 1991; Warren 2008; Woynaroski 2014).
-
Fourteen studies were excluded for a combination of the aforementioned reasons.
Adamson 2010 did not state whether children with Down syndrome were included, compared three types of parent‐mediated interventions, and only measured the outcome in terms of joint attention and not language or communication.
Allen 1980 was not an RCT and did not measure communication or language.
Baker 1980 and Baker 1984 had parent‐mediated interventions in both arms of the trial and did not target communication and language development.
Bennett 1983 was not an RCT, the children did not have Down syndrome, and they did not measure language and communication.
Campbell 1978 was not an RCT, had parent‐mediated interventions in both treatment conditions, and it was unclear whether children with Down syndrome were involved.
Del Giudice 2006 used a behavioural intervention (not naturalistic teaching as in this review) and did not provide results for communication and language separately.
Gibbard 2004 was not an RCT and did not include children with Down syndrome.
Hudson 1982 did not provide results for children with Down syndrome separately, used a behavioural intervention, and did not measure communication and language.
Hwang 2013 included only one child with Down syndrome in the study and had a parent‐mediated intervention in both arms.
Mahoney 1998 was a summary of four intervention studies that were either not RCTs, did not include children with Down syndrome, or had a parent‐mediated intervention in both arms.
McIntyre 2008 did not include children with Down syndrome, and the intervention focused on problem behaviours;
Niccols 2000 was not an RCT, and the intervention did not target language or communication; and
Schoenbrodt 2016 was not an RCT and did not include children with Down syndrome.
Further details about reasons for exclusion are in the Characteristics of excluded studies tables.
Risk of bias in included studies
Review authors assessed the risk of bias across a number of domains, the details of which can be found in the 'Risk of bias' tables beneath the Characteristics of included studies tables. The results are also presented as percentages in the 'Risk of bias' graph (Figure 2) and summarised in the 'Risk of bias' summary (Figure 3).
2.
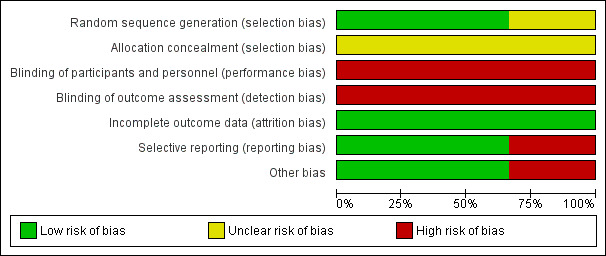
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
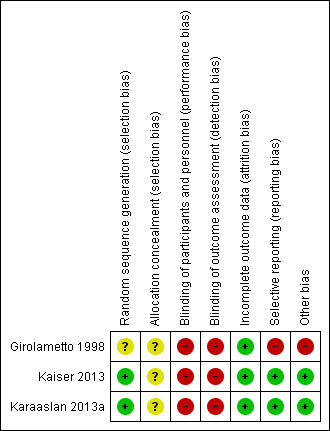
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Girolametto 1998 reported random assignment to intervention and control groups but did not indicate the randomisation method. When we contacted the study authors they could not remember the details on randomisation and did not indicate if the allocation was concealed. Therefore, we judged this study to be at unclear risk of selection bias.
Kaiser 2013 and Karaaslan 2013a reported the use of computerised randomisation for assigning participants to the intervention and control groups, so we rated both studies to be at low risk of bias for random sequence generation. Neither study, however, indicated if the allocation was concealed, so we judged both studies to be at unclear risk of bias for this domain.
Blinding
Due to the nature of the intervention, parents and clinicians were aware of who received the intervention, and no study reported any methods to blind the study participants and personnel, as it was not possible. Therefore, we judged all studies to be at high risk of performance bias.
Although blinding of outcome assessors was possible, we rated all three studies to be at high risk of detection bias for the following reasons. Girolametto 1998 used parent report as one outcome measure, and parents were not blind to the intervention. For the other outcomes it was not specified if the assessor was blind to group assignment. In Karaaslan 2013a, even though the coding of the videos was conducted by raters who were blind to the group assignment, the other assessments used to measure the outcome were fully (ADSI) or partially (Denver II) completed by parents who were not blind to the intervention. Kaiser 2013 used parent reports and stated that the administration and scoring of norm‐referenced assessments was completed by staff members who were not blind to the intervention, even though the observational methods were transcribed by assessors who were. For all other outcome measures used in the Kaiser 2013 study, it was not clear if the assessors were blind to the intervention.
Incomplete outcome data
We considered all three included studies to have addressed missing data and attrition in ways judged to be at low risk of attrition bias. There seemed to be no missing data for Girolametto 1998 or Karaaslan 2013a. Kaiser 2013 reported that attrition was moderate at each phase of the study and that there were no differences in any parent or child characteristics between families who did not complete the study and those who did. For the children with Down syndrome, one child from each condition dropped out between the beginning of the pre‐test assessments and the beginning of the intervention. All of those who took part completed all of the assessments, apart from the MCDI, immediately postintervention, and over 90% were available for at least some of the assessments at 6 and 12 months postintervention.
Selective reporting
Kaiser 2013 and Karaaslan 2013a appeared to be free of selective reporting, so we judged both studies to be at low risk of reporting bias.
Girolametto 1998 reported that they administered the receptive scale of the SICD at postintervention but did not report these outcomes, so we judged this study to be at high risk of reporting bias.
Other potential sources of bias
We considered Karaaslan 2013a and Kaiser 2013 to have no other potential sources of bias. For example, both the intervention and control groups continued to receive their regular speech and language therapy intervention, and there were no significant differences in baseline characteristics between the participants.
In Girolametto 1998, only the control group continued to receive their regular speech and language therapy input, and it was unclear how much parental involvement took place. Furthermore, parents in the intervention group chose target words to focus on during the intervention and then received training on how to target these words, but the control group was not aware of any target words. Due to both of these factors, we rated this study to be at high risk of other bias.
Effects of interventions
The review identified two different comparisons. Girolametto 1998 and Karaaslan 2013a compared parent‐mediated intervention to treatment as usual (TAU), and Kaiser 2013 compared parent‐mediated plus clinician‐mediated intervention with clinician‐only‐mediated intervention. We present the results of these comparisons separately.
All three studies measured the primary outcome of expressive and receptive language skills, albeit through different means. Only Kaiser 2013 measured parental stress. In terms of our secondary outcomes, all three studies measured changes in parental behaviour/responsivity from videotaped parent‐child interactions of free play, although using different observational rating scales. Girolametto 1998 also used a self‐report consumer questionnaire and clinician observation of parent use of target words and focused labelling to measure this outcome postintervention. Karaaslan 2013a measured changes in child socialisation through direct assessment, parent reports and videotaped mother‐child play interactions. All three studies measured language attrition by observing any reduction in language scores from baseline. Finally, Girolametto 1998 measured adherence to treatment through attendance data. No study measured parental satisfaction with the intervention, child‐related changes in nonverbal communication, or negative behaviours in children.
We did not carry out a meta‐analysis on the primary outcomes of Girolametto 1998 and Karaaslan 2013a, as the studies presented results in a way that did not permit meta‐analysis (i.e. median scores and ranges), used different types of assessments (parent reports versus direct assessment versus language sample/experimental tasks), or measured different aspects of language (for example, expressive, receptive or total language). We also did not carry out a meta‐analysis on the secondary outcomes, as the observational scales used to measure rate changes in parental behaviour were different. Therefore, we present the effects of the intervention in this review as a narrative analysis only.
Exact P values were available for only one study: Kaiser 2013.
Parent‐mediated intervention versus treatment as usual
Primary outcomes
Expressive and receptive language skills
Girolametto 1998 used a modified version of the CDI parent report measure and did not find differences between the groups in reported number of words signed/spoken from Mann‐Whitney U tests. They did find that children in the intervention group used almost twice as many target words according to their parents postintervention compared to those in the control group and that this difference was statistically significant (using Mann‐Whitney U comparisons, P < 0.05). However, this comparison was confounded by the fact that parents in the control group were not made aware of their children's target words, which makes it difficult to separate out the effects of parent training received by the intervention group from just knowing which words to target.
Girolametto 1998 also reported that children in the intervention group used significantly more of their target words (five more signed or spoken words, or both) during a free‐play interaction between the mother and child, compared to those in the control group, based on Mann‐Whitney U results (P < 0.05). However, there was no difference in the use of targeted words based on a semi‐structured experimental probe. We rated the quality of the evidence for this outcome as very low (Table 1).
Karaaslan 2013a used a parent‐report measure (ASDI Developmental Quotient) and, based on ANOVA (analysis of variance) results, reported a significant time‐by‐treatment interaction for the 'language‐cognitive' quotient (P < 0.01), with a large effect size (Hedge's g = −1.14). Children in the RT group showed a 46% improvement on the 'language‐cognitive' quotient compared to a 3% improvement achieved by children in the control group. The trialists also used the 'language' quotient of the Denver II and reported a significant effect of time and time‐by‐treatment effect, with a medium effect size (P < 0.05, Hedge's g = 0.42). Children in the RT group showed a 50% improvement on their 'language' quotient scores compared to the 12% improvement achieved by children in the control group. We rated the quality of the evidence for this outcome as very low (see Table 1).
Secondary outcomes
Changes in parental behaviour/responsivity
Both Girolametto 1998 and Karaaslan 2013a addressed changes in parental behaviours/responsivity pre‐ and postintervention, albeit using different measurements. Girolametto 1998 rated mothers' behaviours from a transcription of videotaped mother‐child interaction and reported a significant difference between the two groups at postintervention for 'talkativeness' (rate of utterances per minute) and 'labelling' (number of target words and focused stimulation of target words), based on Mann Whitney U tests (P < 0.05). Mothers in the intervention group used three more target labels and seven more focused stimulations of these labels compared to mothers in the control group. As before, the validity of this comparison is questionable, as the mothers in the control group were not aware of the vocabulary targets. This study also reported that mothers in the intervention group maintained a stable rate of talk, whereas mothers in the control group reduced their rate slightly from pre‐ to postintervention. There were no differences between the two groups of mothers, however, for measures of linguistic complexity (MLUm and TTR). The trialists also used a consumer questionnaire to ask whether mothers in the intervention group thought they had changed in the way in which they communicate with their child as a result of taking part in the programme. All parents indicated that they did, and they listed the child‐centred, interaction‐promoting and language modelling strategies that they found useful. Mothers also responded affirmatively when asked if they found themselves thinking about using the target words during their everyday interactions with their child. Furthermore, the clinician completed checklists following each home visit, and confirmed that the mothers used target words and demonstrated focused labelling during the second, third and fourth home visits. Authors provided no quantitative measures for these outcomes, nor did they assess similar measures from the control group.
Karaaslan 2013a reported that mothers in the intervention group made greater interactive changes than those in the control group, according to their ratings on the MBRS (Mahoney 1999a), which were significant for 'responsiveness' (P < 0.001), 'affect' (P < 0.001) and 'achievement/directiveness' (P < 0.01), as indicated by univariate ANOVA analyses. Mothers in the intervention group increased their responsiveness by 67%, compared to 13% in the control group, and increased their affect by 56%, compared to 6% in the control group. Futhermore, the mothers in the intervention group reduced their ratings on achievement/directiveness by 27%, compared to 3% in the control group.
Child‐related changes in socialisation
Karaaslan 2013a reported that children in the intervention group made significantly greater improvements in social development on the CBRS, ASDI and Denver II measures of socialisation, as indicated by MANOVA (multivariate analysis of variance; P < 0.01). The observational methods from transcriptions of videotaped mother‐child play also found that the children in the intervention group made significantly greater increases in their 'interactive engagement' (attention and initiation) on the CBRS, as indicated by univariate ANOVA (P < 0.001). Again, we assessed the quality of the evidence for this outcome very low (Table 1).
Language attrition
Neither Girolametto 1998 nor Karaaslan 2013a reported significant reductions either in crude or standardised scores on direct assessments, or on any of the parent report, language samples or experimental tasks for the intervention or control groups. We rated the quality of the evidence for this outcome as very low (Table 1).
Adherence to treatment
Only one study, Girolametto 1998, looked at adherence to treatment, measuring this through attendance data, where they reported that all mothers in the intervention group attended at least seven out of nine training sessions and all four home visits. No study reported adherence measures for the treatment that parents gave at home outside of the prescribed intervention sessions. Again, we rated the quality of the evidence for this outcome as very low (Table 1).
Parent‐ and clinician‐mediated intervention versus clinician‐mediated intervention alone
Primary outcomes
Expressive and receptive language skills
Kaiser 2013 showed no differences between the groups immediately, 6 months or 12 months postintervention, based on our secondary analysis of parent reports of expressive vocabulary using Mann‐Whitney U tests. There were no significant differences between the groups as regards their scores on the EVT, PPVT‐III, or 'expressive communication' subscale and 'auditory comprehension' section of the PLS‐4, at any time point. There were no differences in the NDWs used, MLUw or on the IPSyn at any time point postintervention either. Finally, analysis of language samples from trained and untrained activities using the Milieu Teaching Project KidTalk Code showed that the intervention group had a significantly higher percentage of child utterances that contained the child's language targets immediately (P = 0.006) and 6 months postintervention (P = 0.043), but not 12 months postintervention. The same measures were taken from an untrained activity, and no differences were apparent between the groups on any aspect. There were no differences between the intervention and control groups on the number of unique targets produced, MLUw or NDW. We rated the quality of the evidence for this outcome as very low (Table 2).
Parental stress
Kaiser 2013 measured parental stress using the Parenting Stress Index (Abidin 1995). We conducted a secondary analysis of the scores at time points immediately, 6 and 12 months postintervention and found no differences in total stress scores between the intervention and control groups.
Secondary outcomes
Changes in parental behaviour/responsivity
Kaiser 2013 used transcriptions from videotapes of parent‐child interactions in trained and untrained activities to rate changes in parental behaviour using the Milieu Teaching Project Kidtalk Code. Following training, parents in the intervention group used significantly more EMT strategies than parents in the control group, as indicated by our secondary analysis of the data using Mann‐Whitney U scores. For example, for 'responsive interaction' (percentage of child utterances to which the adult responded) and 'language expansion' (percentage of child utterances to which the adult expanded the child's utterances by repeating the child's word and then adding one or more words), they found significant differences between the groups (measured by Mann Whitney U scores) immediately (P = 0.006, P = 0.005), 6 months (P = 0.001; P = 0.030) and 12 months (P = 0.001; P = 0.030) postintervention in trained and untrained activities, respectively. Similarly, parents in the intervention group used a significantly higher percentage of 'language modelling' (percentage of adult utterances that contained one of the child's language targets) immediately and six months postintervention, in trained and untrained activities. They also used more 'milieu teaching prompts' (percentage of prompting episodes that were delivered in response to a child's request) immediately and six months postintervention (Mann Whitney U scores: P = 0.021, P = 0.020), but not 12 months postintervention, in trained activities, and 6 months postintervention in only untrained activities (Mann‐Whitney U score: P = 0.005). We rated the quality of the evidence for this outcome as very low (Table 2).
Language attrition
Kaiser 2013 found no significant reductions, either in raw or standard scores on direct assessments, or on any of the parent reports, language samples or experimental tasks for the intervention or control groups. We rated the quality of the evidence for this outcome as very low (see Table 2).
Discussion
Summary of main results
Our search yielded several intervention studies that investigated parent‐mediated interventions for children with Down syndrome, but it is a serious limitation of this review that only three studies involving 45 children met our inclusion criteria. We contacted the authors of five studies that we could have included had the data for children with Down syndrome been available separately to the rest of the group, but the authors of three studies responded to say that the data had been destroyed or were no longer available (Girolametto 1988; Innocenti 1993; Tannock 1992), while the authors of the other two did not respond to our requests (Boyce 1993; Karaaslan 2013b). In addition, we were unable to conduct a meta‐analysis of the data from those studies included in the review, since each used different outcome measures and did not present their results in a sufficiently transparent manner. For example, Girolametto 1998 only presented their results as median scores and ranges, and as they had destroyed their data, we could not obtain the means and standard deviations needed to conduct a meta analysis; they also used different modes of delivery for the intervention and control groups. Furthermore, the results from the three included studies were inconsistent. Girolametto 1998 and Kaiser 2013 found no differences in results from direct assessment or parent reports of expressive or receptive language abilities, while Karaaslan 2013a reported gains for the intervention group on similar total‐language measures. Girolametto 1998 found that children in the intervention group used five more target labels, according to parent reports, and three more target labels, based on observations of free‐play interaction, than children in the control group; however, this was not evident in an experimental probe eliciting production of these targets. Furthermore, as the control group was not aware of any vocabulary targets, the significance of this finding should not be overestimated. A secondary analysis of the data from the group of children with Down syndrome in the Kaiser 2013 study found gains in the children's use of utterances with language targets compared to the control group immediately and 6 months postintervention, but not 12 months postintervention. Gains in targeted vocabulary, moreover, were not present in this study on measures of language taken from the same parent‐child interaction on trained or untrained activities, or from free play interaction with a responsive adult who did not prompt the child. Only Kaiser looked at parental stress and did not find any differences between the groups at time points immediately, 6 or 12 months postintervention.
A more consistent finding was noted for the effects of the intervention on changes in parental behaviour/responsivity. All three studies found differences in most measures of how parents talked and interacted with their children postintervention, although not all strategies were maintained in the longer term (12 months postintervention). It would be worth investigating how these changes are maintained in the long term and how much, if any, they affect the children's language and communication. Only Karaaslan 2013a looked at changes in the child's socialisation, and although they found positive outcomes (e.g. higher quotient scores on social development assessments), larger studies would need to replicate this outcome. No study found evidence of language attrition following the intervention, and only one study looked at adherence to the treatment by reporting on parental attendance, although no study measured parental use of the strategies outside of the intervention sessions.
Overall, this narrative review is inconclusive as to whether children with Down syndrome make gains in language and communication skills following parent‐mediated interventions.
Overall completeness and applicability of evidence
The overall applicability of evidence is limited and incomplete. The children in Girolametto 1998 and Kaiser 2013 were described as having at least 10 single words and a mean IQ of approximately 70, which is relatively high for children with Down syndrome (Roizen 2007). Both studies took place in North America, and the children were from English‐speaking homes. Children in Karaaslan 2013a were in Turkey, and so presumably speaking Turkish although the nature of their language exposure was not clear. Their baseline language scores were presented in terms of 'developmental ages' and were, on average, about 18 months, which could have been relatively similar to that of the other studies (i.e. single‐word stage). No study described or reported any comorbid conditions for the children. In addition, it was mostly mothers (apart from one father in Kaiser 2013) who were involved in the intervention, and most were married, well educated and middle class, and over half of them were homemakers (as reported by Girolametto 1998 and Kaiser 2013). It is unclear whether the evidence could be generalised to children with lower or higher language or intellectual ability, bilingual families or those from other cultural groups. It is also unclear whether the evidence would apply to fathers, single‐parent families, parents in full‐time work or those from working‐class backgrounds.
All of the studies involved at least some one‐to‐one home sessions, although the mode of delivery differed. Girolametto 1998 used mostly group‐based training sessions, with four individual video‐feedback sessions in the home, while Kaiser 2013 and Karaaslan 2013a involved almost exclusively individual sessions with live modelling and coaching. Each study used interventions of different durations and intensities, and none collected information on how often the parents implemented the intervention in their daily contact with the child, making it difficult to quantify the amount of intervention received, and how this might influence the outcomes. Karaaslan 2013a had the largest dosage (approximately 48 hours) and seemed to show the greatest effect on children's language, but the outcomes were only measured immediately postintervention, and other studies would need to replicate this finding.
Quality of the evidence
We noted several limitations in the methodology of the three included studies (Girolametto 1998; Karaaslan 2013a; Kaiser 2013). In all studies, the sample sizes were very small, and none of the studies attempted to calculate the sample size required to achieve adequate power before recruiting participants. We considered all studies to be at high risk of bias in relation to allocation concealment, blinding of participants and blinding of outcome assessment. We also considered Girolametto 1998 to be at high risk of both selective reporting bias, as authors did not report on one assessed outcome, and detection bias, as only the intervention group was aware of the children's vocabulary targets that were used to measure the outcome. In Kaiser 2013 and Karaaslan 2013a, both intervention and control groups continued to receive speech and language therapy or early intervention services, or a combination of both, making it difficult to judge the effectiveness of the parent‐mediated interventions in isolation.
We assessed the overall quality of evidence for those important outcomes included in Table 1 and Table 2 using the GRADE approach (Guyatt 2008). In light of the serious methodological limitations, and the fact that we were unable to combine the results in a meta‐analysis, we judged the overall quality of the evidence provided by the included studies to be very low. Our reasons for downgrading the quality of the evidence were: the small sample sizes; the lack of precision of the estimated effects, since we were unable to conduct a meta‐analysis; the ratings of high or unclear risk of bias for most domains on the Cochrane 'Risk of bias' tool (Higgins 2011a); and a cointervention in the control group of Girolametto 1998. This indicates that we have very little confidence in the outcomes and that further research is very likely to have an important impact on our confidence in the estimate of treatment effect (Guyatt 2008)
Potential biases in the review process
To identify all relevant studies, we conducted comprehensive searches, contacted colleagues and researchers for grey literature, and checked the reference lists of related reports. We searched five additional, relevant electronic databases that were not listed in our protocol (O'Toole 2016), as recommended by the Information Specialist of the Cochrane Developmental, Psychosocial and Learning Problems Editorial Team. Where insufficient information was available in the report, we contacted the study authors directly, requesting them to supply the missing information. We think it unlikely that we omitted an important trial.
Despite our best efforts, not all study authors responded to our requests for further information on their studies, meaning that we could not include them in the review (Boyce 1993; Karaaslan 2013b), or we had to reach judgements about their risks of bias without further information (Karaaslan 2013a). Girolametto 1998 had destroyed the data from their study, so we could not access these data to extract mean scores and standard deviations, nor could we include their data from two other eligible studies that they had conducted (Girolametto 1988;Tannock 1992), as separate data for the children with Down syndrome were not available in the published report. Furthermore, we were unable to conduct a meta‐analysis since the individual studies varied considerably in their study design, tools used for measuring outcomes, and definitions of control and intervention conditions. This means that the conclusions of this review are based only on a narrative synthesis of the included studies.
We adhered to our published protocol as far as possible through the review process (O'Toole 2016). Our only deviation was that we did not use the categories of 'intervention integrity', as proposed by Dane 1988, during data extraction (see Differences between protocol and review). Instead, we looked at treatment fidelity in terms of implementation fidelity and intervention fidelity with the categories recommended by Lieberman‐Betz 2015, as these were more appropriate for parent‐mediated interventions.
Although COT received a fellowship to complete the review, no other review author received any direct funding for conducting this review, and no review author has a conflict of interest.
Agreements and disagreements with other studies or reviews
Findings from this review are largely in line with those reported in previous reviews of parent‐mediated interventions targeting language and communication. Of most relevance is Oono 2013, which included 17 RCTs involving 919 children with autism spectrum disorder. Like this review, it did not find statistical evidence of gains in most aspects of language and communication assessed, apart from parent reports of an improvement in language comprehension. Nor did review authors find that parents changed the way they interacted and spoke with their children, or that the severity of children's autism characteristics was reduced. A review by Pennington 2018 on parent‐mediated interventions for children with non‐progressive motor disorders, such as cerebral palsy, also reported that mothers in the intervention groups became more responsive. We, however, were unable to evaluate the effects of training on children's language development due to missing data, and we found no reports for changes in the children's communication skills. Law 2003, in a review of speech and language interventions for children with primary speech and language disorder, also examined parent‐mediated interventions. Although only three studies were relevant to the review, they too found non‐significant effect sizes for all language outcomes when comparing the intervention to non‐treatment control groups on standardised measures of language development. Roberts 2011 carried out a meta‐analysis of parent‐implemented language interventions but included studies that used a wide range of experimental designs (for example, pre‐post comparison and non‐RCTs) and looked at children with language impairment with and without intellectual disability. They found that the intervention did improve receptive and expressive language and vocabulary, expressive morphosyntax and rate of communication when compared to a control group, and that the parents improved their responsiveness and use of language models. Their results also indicated that the type of outcome measure (direct assessment, parent report, etc.) did not affect the magnitude of the effect. However, they also noted that gains in expressive vocabulary were significantly lower for children with intellectual disability than those without, and that children with intellectual disability "may require more intensive and longer term language intervention to ensure improvements in their functional and social communication measured across context and over time" (Kaiser 2011, p 308). Finally, Te Kaat‐van den Os 2017 conducted a systematic review of parent‐mediated intervention for all children with developmental disabilities but included interventions that were delivered in conjunction with clinician‐mediated interventions. The found similar, positive effects for parental responsiveness and the frequency of child communication acts but not for expressive vocabulary development.
Authors' conclusions
Implications for practice.
As this review identified only three small‐scale studies, generally of very low quality, parents and clinicians need to be aware that there is currently insufficient evidence to determine the effects of parent‐mediated interventions to improve the language and communication of children with Down syndrome. This does not mean that we have found evidence that the interventions are ineffective, but rather that we have yet to find evidence that there is an effect on the children's language and communication. The implications for practice are that service providers need to pay attention to how they promote and recommend these interventions, using clinical expertise, family preferences and best practice guidelines to inform their intervention decisions (DeVeney 2016).
One factor that is important to consider when interpreting this evidence is that most of the studies were of a relatively low dose (one session per week, or over a three‐month period), and given the significant difficulty that children with Down syndrome have in developing expressive vocabulary, a more intensive intervention over a longer period may be required (see Yodor 2014). The only study to report gains in language development had the highest cumulative intervention intensity (48 hours), as it was completed over a total intervention duration of six months. Threrefore, children with Down syndrome may need a longer period of intervention in order to benefit from the changes in interactions with their parents, although further research would need to investigate this empirically. Another issue to consider when implementing this intervention is that two studies found that only individually targeted vocabulary goals showed improvement postintervention. This suggests that individualised vocabulary and language targets should be included in the intervention, as opposed to more generalised language instruction, particularly since parents may need guidance on selecting developmentally appropriate target vocabulary for their child as well as training on how to teach these. Girolametto 1993 has suggested that the Hanen Parent Program could be optimised through a stronger emphasis on individualisation, with more one‐on‐one sessions to make it immediately relevant to the specific skills of the children and the parents involved (Pennington 2009).
Finally, most of the theoretical basis and evidence to date for this intervention comes from mainstream, middle‐class, Western cultures and includes parents (usually mothers) who are generally highly motivated to help their children's language development. Roberts 2014 discussed the importance of considering the impact of cultural beliefs and practices on parenting behaviour in order to best involve family members in the intervention process. This includes how parents direct, play and interact with their children and objects; who should be included in the intervention process; and how consideration of language goals should be based on what is important to the family.
Implications for research.
This review highlights the need for well‐designed studies, that are rigorous in delivery, to evaluate the effectiveness of parent‐mediated intervention for promoting communication and language development in young children with Down syndrome. Ideally, this would be achieved through further RCTs that adhere to the CONSORT standards of reporting trials (Schulz 2010), including a description of the mediators and moderators of the interventions, such as:
a description of the fidelity of intervention;
the children's age, sex, age of siblings, language and cognitive functioning;
the parents' age, sex, educational history, employment, cultural background/ethnicity, responsibilities in terms of work and other caring roles, previous training on how to communicate with and enhance language and communication with children, attitudes to an indirect intervention, and present communication and interaction style with their child; and
the clinicians' education, training, experience and expertise in delivering this type of intervention, and relationship or familiarity with the participants.
A major improvement needed in future research design relates to the issue of treatment fidelity. The premise behind the cascading model of parent‐mediated intervention is that parents implement the effective training, coaching and support that they receive from clinicians with a high level of accuracy, consistency and frequency, thereby resulting in improvements in the child's outcomes (Barton 2013; Roberts 2014). Lieberman‐Betz 2015 acknowledges that the tools to measure these factors lack reliability and validity. Nonetheless, it is particularly important to measure dosage at the parental level, to determine how much training is being implemented at home. Many other reviews have noted a lack of systematic reporting on parental implementation of strategies at home (Roberts 2011), which could be overcome through technological advances in collecting data on parental language input, such as the Language Environment Analysis (LENA) system for measuring language environments (Suskind 2015). In addition, the intervention should be described well enough so that clinician implementation can be evaluated, and the length, frequency and duration of training sessions clearly documented, so that total training hours can be calculated. Other studies have found that children with Down syndrome benefit from a higher dosing frequency of clinician‐mediated milieu teaching (five 1‐hour sessions per week versus one 1‐hour session per week for a total of nine months), but this was mediated by the observation that only children who displayed functional play with objects at the start of the intervention benefited, and the effects of the interventions were strongly influenced by the intellectual capacity of the children (Fey 2013; Yodor 2014). The current review indicates that a higher total intervention duration (of at least six months) may also be required before changes in the children's language are apparent, although replication of this finding is necessary. Only well‐designed RCTs can determine the best treatment intensity required to produce a desirable effect, so it is important that future studies document dosage clearly and recognise that it is a complex construct to measure in this type of intervention. Future studies should consider Warren 2007's framework for documenting and measuring treatment intensity, whereby 'dose' relates to the length of the session, how many teaching episodes occur in that session and how they are distributed; 'dose form' relates to the type of activity used for the teaching episode; and 'dose frequency' relates to the frequency per day, week, or month with which the intervention is delivered. These factors result in a cumulative total intervention duration, which can then be used to measure the overall dosage.
Another consideration for future studies is to clearly describe the training procedures used so that we can consider which aspects result in changes in both children and parents. For example, Roberts 2014 used an individualised Teach‐Model‐Coach‐Review method, whereas other interventions tend to involve videotaping the parent and using that to give feedback on how they are implementing the strategies. Roberts 2011 noted that most of the studies in their review lacked detail on the procedures used in the training, making it difficult to link specific training practices (modelling, feedback or role play, etc.) with high‐fidelity parental implementation of the intervention (Barton 2013).
Given the challenges of balancing the needs of the families and children in terms of therapeutic services, with the requirements for good research design as acknowledged by Oono 2013, not to mention the very large sample size that would be required to evaluate all of the moderators of the interventions, a number of alternative study designs and feasibility studies may need to be considered before embarking on future RCTs. In addition, recent evidence from similar interventions for children with autism show that language gains are greater for children when the clinician and parent deliver the intervention together (Hampton 2016). Their reasoning for this is that parents benefit from modelling, which results in better fidelity of intervention and thus a higher dosage outside of the clinical environment, and that the children benefit from a consistent language teaching strategy across communication partners. Therefore, a study that compares a parent‐mediated intervention to a parent‐ plus clinician‐mediated intervention may be considered more ethically appropriate and be useful for answering these questions. Future studies could expand this model to include a wait‐list control group. With further clarity on these issues, we may then be able to address the characteristics of families who do and do not respond to the intervention.
Finally, valid, reliable and, where possible, similar outcome measures should be used, and there should be appropriate and complete reporting of the results using mean scores and standard deviations to enable some form of meta‐analysis. The outcome measures should be clearly described in terms of which aspect of language is being assessed, (for example, vocabulary or grammar), whether the measure represents scores for expressive, receptive or total language, and the nature of these scores (i.e. t scores, z scores, raw scores). Parent‐report measures have an inherent bias when measuring the outcomes of a parent‐mediated intervention, as parents are not blind to group assignment, so this could result in a Hawthorne effect or response bias toward the intervention. In addition, as the intervention may have impacts beyond the changes in the child's language and communication, investigators should also consider secondary outcomes that are more distal to the intervention, such as social validity in terms of parental satisfaction, family well‐being, child nonverbal/socialisation skills, behaviour and parental knowledge about language development in Down syndrome. Oono 2013 also suggests including an estimate of the costs of the interventions, which is particularly important if a higher dosage is required to produce language gains, as well as any adverse effects, such as parental stress, as they have important implications for translating research into practice. Studies should follow up families, ideally at 6‐ or 12‐monthly intervals throughout childhood, so that we can determine the longer term benefits for the children's language development.
Acknowledgements
We would like to thank Dr Joanne Duffield, Professor Geraldine Macdonald and Editors from the Cochrane Developmental, Psychosocial and Learning Problems Editorial Team for their support and guidance in developing the protocol (O'Toole 2016) and throughout the review process. We would also like to thank Mrs Margaret Anderson, Queen's University, Belfast (UK), for her advice on the search strategies and work in conducting most of the electronic searches, as well as the anonymous reviewers and the statistician for their useful comments on previous drafts of the protocol and review. We would also like to thank colleagues in the field for providing information, articles and support for this review, particularly Ann Kaiser and Megan Roberts from Vanderbilt Univiersity (US) for sharing their data with us. Finally, we would like to thank the Health Research Board for the Fellowship awarded to Ciara O'Toole to facilitate completion of this review.
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library
Searched up to 22 January 2018 (300 records)
#1[mh "Down syndrome"] #2(down* next syndrome) #3"Downs disease" #4"trisomy 21" #5"chromosome 21" #6(mongol or mongols or mongoloid or mongolism) #7[mh "Intellectual Disability"] #8[mh " Developmental disabilities"] #9((intellectual* or learning) near/3 (disabilit* or disabl*)) #10(developmental* near/3 (delay* or disabilit* or disabl*)) #11mental* next retard* #12{or #1‐#11} #13[mh Child] #14[mh infant] #15(child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*) #16{or #13‐#15} #17#12 and #16 #18[mh "Parent‐Child Relations"] #19[mh Parenting] #20[mh Parents] #21[mh Caregivers] #22{or #18‐#21} #23[mh Education] #24[mh teaching] #25[mh "Early intervention (Education)"] #26early next intervent* #27[mh "Education of Intellectually Disabled"] #28[mh "education, special"] #29[mh "language therapy"] #30[mh "speech therapy"] #31(speech* or languag* or communicat* or sign* or nonverbal* or non‐verbal* or cue*) #32[mh "Sign language"] #33[mh "Manual Communication"] #34[mh "Nonverbal communication"] #35{or #23‐#34} #36#22 and #35 #37((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)) #38((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (interact* or inter‐act* or involv* or mediat* or respon*)) #39focus*ed next stimulation #40naturalistic near/2 teaching #41(milieu near/2 teaching) #42responsiv* near/2 education #43responsiv* near/2 teaching #44Hanen* 17 #45{or #37‐#44} #46#36 or #45 #47#17 and #46 in Trials [Note: Final search line 2016] #48#17 and #46 in Trials Publication Year from 2016 to 2018 [Note: Final search line 2018]
MEDLINE Ovid
Searched up to 22 January 2018 (968 records)
1 Down Syndrome/ 2 (down$ adj syndrome).tw. 3 Downs disease.tw. 4 trisomy 21.tw. 5 chromosome 21.tw. 6 (mongol or mongols or mongoloid or mongolism).tw. 7 Intellectual Disability/ 8 Developmental disabilities/ 9 ((intellectual$ or learning) adj3 (disabilit$ or disabl$)).tw. 10 (developmental$ adj3 (delay$ or disabilit$ or disabl$)).tw. 11 mental$ retard$.tw. 12 or/1‐11 13 exp child/ 14 (child$ or infant$ or babies or baby or toddler$ or girl$ or boy$ or pre‐school$ or preschool$ or nurser$ or kindergarten$ or kinder‐garten$).tw. 15 or/13‐14 16 12 and 15 17 exp Parent‐Child Relations/ 18 Parenting/ 19 exp Parents/ 20 Caregivers/ 21 or/17‐20 22 education/ 23 teaching/ 24 "Early intervention (Education)"/ 25 early intervent$.tw. 26 Education of Intellectually Disabled/ 27 education, special/ 28 language therapy/ 29 speech therapy/ 30 (speech$ or languag$ or communicat$ or sign$ or nonverbal$ or non‐verbal$ or cue$).tw. 31 Sign language/ 32 Manual Communication/ 33 Nonverbal communication/ 34 or/22‐33 35 21 and 34 36 exp Parents/ed [Education] 37 Caregivers/ed [Education] 38 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (coach$ or educat$ or intervention$ or learn$ or program$ or teach$ or train$)).tw. 39 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (interact$ or inter‐act$ or involv$ or mediat$ or respon$)).tw. 40 or/36‐39 41 focus?ed stimulation.tw. 42 (naturalistic adj2 teaching).tw. 43 (milieu adj2 teaching).tw. 44 (responsiv$ adj2 education).tw. 45 (responsiv$ adj2 teaching).tw. 46 Hanen$.tw. 47 or/41‐46 48 35 or 40 or 47 49 16 and 48 50 randomized controlled trial.pt. 51 controlled clinical trial.pt. 52 randomi#ed.ab. 53 placebo$.ab. 54 drug therapy.fs. 55 randomly.ab. 56 trial.ab. 57 groups.ab. 58 or/50‐57 59 exp animals/ not humans.sh. 60 58 not 59 61 49 and 60 [Note:Final search line 2016 ] 62 remove duplicates from 61 63 limit 62 to ed=20160301‐20180111 [Note:Final search line 2018 ]
MEDLINE In‐Process & Other Non‐indexed Citations OVID
Searched up to 22 January 2018 (208 records)
1 (down$ adj syndrome).tw,kf. 2 Downs disease.tw,kf. 3 trisomy 21.tw,kf. 4 chromosome 21.tw,kf. 5 (mongol or mongols or mongoloid or mongolism).tw,kf. 6 ((intellectual$ or learning) adj3 (disabilit$ or disabl$)).tw,kf. 7 (developmental$ adj3 (delay$ or disabilit$ or disabl$)).tw,kf. 8 mental$ retard$.tw,kf. 9 or/1‐8 10 (child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*).tw,kf. 11 9 and 10 12 ((speech$ or languag$ or communicat$ or sign$ or nonverbal$ or non‐verbal$ or cue$) and (parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$)).tw,kf. 13 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (coach$ or educat$ or intervention$ or learn$ or program$ or teach$ or train$)).tw,kf. 14 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (interact$ or inter‐act$ or involv$ or mediat$ or respon$)).tw,kf. 15 focus?ed stimulation.tw,kf. 16 (naturalistic adj2 teaching).tw,kf. 17 (milieu adj2 teaching).tw,kf. 18 (responsiv$ adj2 education).tw,kf. 19 (responsiv$ adj2 teaching).tw,kf. 20 Hanen$.tw,kf. 21 or/12‐20 22 11 and 21 23 (random$ or control$ or group$ or cluster$ or placebo$ or trial$ or assign$ or prospectiv$ or meta‐analysis or systematic review or longitudinal$).tw,kf. 24 22 and 23
MEDLINE Epub Ahead of Print OVID
Searched up to 22 January 2018 (95 records)
1 (down$ adj syndrome).tw,kf. 2 Downs disease.tw,kf. 3 trisomy 21.tw,kf. 4 chromosome 21.tw,kf. 5 (mongol or mongols or mongoloid or mongolism).tw,kf. 6 ((intellectual$ or learning) adj3 (disabilit$ or disabl$)).tw,kf. 7 (developmental$ adj3 (delay$ or disabilit$ or disabl$)).tw,kf. 8 mental$ retard$.tw,kf. 9 or/1‐8 10 (child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*).tw,kf. 11 9 and 10 12 ((speech$ or languag$ or communicat$ or sign$ or nonverbal$ or non‐verbal$ or cue$) and (parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$)).tw,kf. 13 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (coach$ or educat$ or intervention$ or learn$ or program$ or teach$ or train$)).tw,kf. 14 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (interact$ or inter‐act$ or involv$ or mediat$ or respon$)).tw,kf. 15 focus?ed stimulation.tw,kf. 16 (naturalistic adj2 teaching).tw,kf. 17 (milieu adj2 teaching).tw,kf. 18 (responsiv$ adj2 education).tw,kf. 19 (responsiv$ adj2 teaching).tw,kf. 20 Hanen$.tw,kf. 21 or/12‐20 22 11 and 21 23 (random$ or control$ or group$ or cluster$ or placebo$ or trial$ or assign$ or prospectiv$ or meta‐analysis or systematic review or longitudinal$).tw,kf. 24 22 and 23
Embase Ovid
Searched up to 22 January 2018 (831 records)
1 Down syndrome/ 2 (down$ adj syndrome).tw. 3 Downs disease.tw. 4 trisomy 21.tw. 5 chromosome 21.tw. 6 (mongol or mongols or mongoloid or mongolism).tw. 7 intellectual impairment/ 8 developmental disorder/ 9 ((intellectual$ or learning) adj3 (disabilit$ or disabl$)).tw. 10 (developmental$ adj3 (delay$ or disabilit$ or disabl$)).tw. 11 mental$ retard$.tw. 12 or/1‐11 13 exp child/ 14 (child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*).tw. 15 or/13‐14 16 12 and 15 17 exp parent/ 18 exp child parent relation/ 19 caregiver/ 20 or/17‐19 21 education/ 22 education program/ 23 teaching/ 24 early intervention/ 25 early intervent$.tw. 26 "education of intellectually disabled"/ 27 special education/ 28 speech therapy/ 29 exp nonverbal communication/ 30 (speech$ or languag$ or communicat$ or sign$ or nonverbal$ or non‐verbal$ or cue$).tw. 31 or/21‐30 32 20 and 31 33 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (coach$ or educat$ or intervention$ or learn$ or program$ or teach$ or train$)).tw. 34 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (interact$ or inter‐act$ or involv$ or mediat$ or respon$)).tw. (19861) 35 or/33‐34 36 focus?ed stimulation.tw. 37 (naturalistic adj2 teaching).tw. 38 (milieu adj2 teaching).tw. 39 (responsiv$ adj2 education).tw. 40 (responsiv$ adj2 teaching).tw. 41 Hanen$.tw. 42 or/36‐41 43 32 or 35 or 42 44 12 and 43 45 Randomized controlled trial/ 46 controlled clinical trial/ 47 Single blind procedure/ 48 Double blind procedure/ 49 triple blind procedure/ 50 Crossover procedure/ 51 (crossover or cross‐over).tw. 52 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 53 Placebo/ 54 placebo.tw. 55 prospective.tw. 56 factorial$.tw. 57 random$.tw. 58 assign$.ab. 59 allocat$.tw. 60 volunteer$.ab. 61 or/45‐60 62 44 and 61 Note: Final search line 2016 63 limit 62 to yr="2016 ‐Current" [Note: Final search line 2018]
ERIC EBSCOhost (Education Resources Information Center)
Searched up to 23 January 2018 (997 records)
S1 DE "Down Syndrome" S2 DE "Developmental Disabilities" S3 DE "Mental Retardation" S4 (down* syndrome) S5 Downs disease S6 trisomy 21 S7 chromosome 21 S8 (mongol or mongols or mongoloid or mongolism) S9 ((intellectual* or learning) N3 (disabilit* or disabl*)) S10 (developmental* N3 (delay* or disabilit* or disabl*)) S11 mental* retard* S12 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 S13 DE "Children" OR DE "Young Children" OR DE "Infants" OR DE "Toddlers" S14 TI(child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*) OR AB(child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*) S15 S13 OR S14 S16 S12 AND S15 S17 DE "Child Caregivers" OR DE "Parent Role" OR DE "Fathers" OR DE "Mothers" OR DE "Parent Child Relationship" OR DE "Parent Participation" OR DE "Parents" S18 DE "Education" S19 DE "Teaching Methods" OR DE "Teaching (1966 1980)" S20 DE "Early Intervention" S21 DE "Special Education" S22 DE "Speech Education (1966 1980)" OR DE "Speech Improvement" OR DE "Speech Therapy" OR DE "Speech Instruction" OR DE "Speech Language Pathology" S23 TI(speech* or languag* or communicat* or sign* or nonverbal* or non‐verbal* or cue*)OR AB(speech* or languag* or communicat* or sign* or nonverbal* or non‐verbal* or cue*) S24 (DE "Sign Language" OR DE "Manual Communication") S25 (DE "Nonverbal Communication") OR (DE "Augmentative and Alternative Communication") S26 S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 S27 S17 AND S26 S28 DE "Parents as Teachers" S29 DE "Parent Education" S30 AB((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)) OR AB((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (interact* or inter‐act* or involv* or mediat* or respon*)) OR TI((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)) OR TI((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (interact* or inter‐act* or involv* or mediat* or respon*)) S31 S28 OR S29 OR S30 S32 S27 OR S31 S33 focus#ed stimulation S34 (naturalistic N2 teaching) S35 (milieu N2 teaching) S36 (responsiv* N2 education) S37 (responsiv* N2 teaching) S38 Hanen* S39 S33 OR S34 OR S35 OR S36 OR S37 OR S38 S40 S32 OR S39 S41 S16 AND S40 S42 DE "Meta Analysis" OR DE "Evaluation Research" OR DE "Control Groups" OR DE "Experimental Groups" OR DE "Longitudinal Studies" OR DE "Followup Studies" OR DE "Program Effectiveness" OR DE "Program Evaluation" S43 (random* or trial* or PROSPECTIVE* OR longitudinal or BLIND* or CONTROL* or assign* or allocat*) S44 S42 OR S43 S45 S41 AND S44 [Note: Final search line 2016] S46 Limiters ‐ Date Published: 20160101‐20181231 S47 S45 AND S46 [Note: Final search line 2018]
PsycINFO Ovid
Searched up to 23 January 2018 (731 records)
1 down's syndrome/ 2 (down$ adj syndrome).tw. 3 Downs disease.tw. 4 trisomy 21.tw. 5 chromosome 21.tw. 6 (mongol or mongols or mongoloid or mongolism).tw. 7 intellectual development disorder/ 8 developmental disabilities/ 9 ((intellectual$ or learning) adj3 (disabilit$ or disabl$)).tw. 10 (developmental$ adj3 (delay$ or disabilit$ or disabl$)).tw. 11 mental$ retard$.tw. 12 or/1‐11 13 (childhood birth 12 yrs or infancy 2 23 mo or neonatal birth 1 mo or preschool age 2 5 yrs or school age 6 12 yrs).ag. 14 (child$ or infant$ or babies or baby or toddler$ or girl$ or boy$ or pre‐school$ or preschool$ or nurser$ or kindergarten$ or kinder‐garten$).tw. 15 13 or 14 16 12 and 15 17 parenting/ 18 exp parent child relations/ 19 parental involvement/ 20 parent child communication/ 21 parental role/ 22 exp parents/ 23 caregivers/ 24 or/17‐23 25 education/ 26 teaching/ 27 teaching methods/ 28 early intervention/ 29 early intervent$.tw. 30 Special Education/ 31 speech therapy/ 32 language therapy/ 33 manual communication/ 34 nonverbal communication/ 35 sign language/ 36 (speech$ or languag$ or communicat$ or sign$ or nonverbal$ or non‐verbal$ or cue$).tw. 37 or/25‐36 38 24 and 37 39 parent training/ 40 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (coach$ or educat$ or intervention$ or learn$ or program$ or teach$ or trai$)).tw. 41 ((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$) adj3 (interact$ or inter‐act$ or involv$ or mediat$ or respon$)).tw. 42 focus?ed stimulation.tw. 43 (naturalistic adj2 teaching).tw. 44 (milieu adj2 teaching).tw. 45 (responsiv$ adj2 education).tw. 46 (responsiv$ adj2 teaching).tw. 47 Hanen$.tw. 48 or/39‐47 49 38 or 48 50 16 and 49 51 clinical trials/ 52 random$.tw. 53 (allocat$ or assign$).tw. 54 ((clinic$ or control$) adj trial$).tw. 55 ((control$ or experiment$ or intervention$) adj3 group$).tw. 56 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 57 (crossover$ or "cross over$").tw. 58 random sampling/ 59 Experiment Controls/ 60 Placebo/ 61 placebo$.tw. 62 exp program evaluation/ 63 treatment effectiveness evaluation/ 64 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw. 65 or/51‐64 66 50 and 65
CINAHL Plus EBSCOhost (Cumulative Index to Nursing and Allied Health Literature)
Searched up to 23 January 2018 (504 records)
S1 (MH "Down Syndrome") S2 down* syndrome S3 Downs disease S4 trisomy 21 S5 chromosome 21 S6 (mongol or mongols or mongoloid or mongolism) S7 (MH "Intellectual Disability") S8 ((intellectual* or learning) N3 (disabilit* or disabl*)) S9 (MH "Developmental Disabilities") S10 (developmental* N3 (delay* or disabilit* or disabl*)) S11 mental* retard* S12 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 S13 (MH "Infant+") OR (MH "Child+") S14 (child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*) S15 S13 OR S14 S16 S12 AND S15 S17 (MH "Parent‐Child Relations+") S18 (MH "Parenting") S19 (MH "Parents+") S20 (MH "Caregivers") S21 S17 OR S18 OR S19 OR S20 S22 (MH "Education") S23 (MH "Teaching") OR (MH "Teaching Methods") S24 (MH "Early Intervention+") S25 early intervent* S26 (MH "Education, Special") S27 (MH "Speech Therapy") S28 (MH "Language Therapy") S29 (MH "Nonverbal Communication+") S30 (speech* or languag* or communicat* or sign* or nonverbal* or non‐verbal* or cue*) S31 S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 S32 S21 AND S31 S33 (parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)) S34 ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (interact* or inter‐act* or involv* or mediat* or respon*) S35 S33 OR S34 S36 S32 OR S35 S37 focus#ed stimulation S38 (naturalistic N2 teaching) S39 (milieu N2 teaching) S40 (responsiv* N2 education) S41 (responsiv* N2 teaching) S42 Hanen* S43 S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 S44 S16 AND S43 S45 (MH "Clinical Trials+") S46 MH random assignment S47(MH "Meta Analysis") S48 (MH "Crossover Design") S49 (MH "Quantitative Studies") S50 PT randomized controlled trial S51 PT Clinical trial S52 (clinical trial*) or (control* N2 trial*) S53 ("follow‐up study" or "follow‐up research") S54 (prospectiv* study or prospectiv* research) S55 (evaluat* N2 study or evaluat* N2 research) S56 (MH "Program Evaluation") S57 (MH "Treatment Outcomes") S58 TI(single N2 mask* or single N2 blind*) OR AB(single N2 mask* or single N2 blind*) S59 TI((doubl* N2 mask*) or (doubl* N2 blind*)) OR AB((doubl* N2 mask*) or (doubl* N2 blind*)) S60 TI ((tripl* N2 mask*) or (tripl* N2 blind*)) or ((trebl* N2 mask*) or (trebl* N2 blind*)) OR AB((tripl* N2 mask*) or (tripl* N2 blind*)) or ((trebl* N2 mask*) or (trebl* N2 blind*) S61 random* N2 assign* OR random* N2 allocat* S62 S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 S63 S44 AND S62 [Note: Final search line 2016] S64 EM 20160301‐ S65 S63 AND S64 [Note: Final search line 2018]
Science Citation Index Web of Science
Searched up to 23 January 2018 (1024 records)
# 19#18 AND #17 Indexes=SCI‐EXPANDED Timespan=All years # 18TS=(random* or assign* or allocat* or group* or trial* or control* ) Indexes=SCI‐EXPANDED Timespan=All years # 17#16 OR #14 Indexes=SCI‐EXPANDED Timespan=All years # 16#15 AND #5 Indexes=SCI‐EXPANDED Timespan=All years # 15TS= ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/10 (speech* or languag* or communicat* or sign* or nonverbal* or non‐verbal* or cue*)) Indexes=SCI‐EXPANDED Timespan=All years # 14#13 AND #5 Indexes=SCI‐EXPANDED Timespan=All years # 13#12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 Indexes=SCI‐EXPANDED Timespan=All years # 12TS=(responsiv* near/2 teaching) Indexes=SCI‐EXPANDED Timespan=All years # 11TS=(responsiv* near/2 education) Indexes=SCI‐EXPANDED Timespan=All years # 10TS=(milieu near/2 teaching) Indexes=SCI‐EXPANDED Timespan=All years # 9TS=(naturalistic near/2 teaching) Indexes=SCI‐EXPANDED Timespan=All years # 8TS=("focus* stimulation") Indexes=SCI‐EXPANDED Timespan=All years # 7TS= ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)) Indexes=SCI‐EXPANDED Timespan=All years 6TS= ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (interact* or inter‐act* or involv* or mediat* or respon*)) Indexes=SCI‐EXPANDED Timespan=All years # 5#4 AND #3 Indexes=SCI‐EXPANDED Timespan=All years # 4TS=(child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*) Indexes=SCI‐EXPANDED Timespan=All years # 3#2 OR #1 Indexes=SCI‐EXPANDED Timespan=All years # 2TS=((intellectual* or learning) near/1 (disabled or disabilit* or impair*)) OR TS=(developmental* near/1 (delay* or disabilit* or disabl*)) or TS= ("mental* retard*" OR mongol* or "trisomy 21" or "chromosome 21") Indexes=SCI‐EXPANDED Timespan=All years # 1TS=("down* syndrome" or "downs disease") Indexes=SCI‐EXPANDED Timespan=All years
Social Sciences Citation Index Web of Science
Searched up to 23 January 2018 (1583 records)
# 19#18 AND #17 Indexes=SSCI Timespan=All years # 18TS=(random* or assign* or allocat* or group* or trial* or control* ) Indexes=SSCI Timespan=All years # 17#16 OR #14 Indexes=SSCI Timespan=All years # 16#15 AND #5 Indexes=SSCI Timespan=All years # 15TS= ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/10 (speech* or languag* or communicat* or sign* or nonverbal* or non‐verbal* or cue*)) Indexes=SSCI Timespan=All years # 14#13 AND #5 Indexes=SSCI Timespan=All years # 13#12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 Indexes=SSCI Timespan=All years # 12TS=(responsiv* near/2 teaching) Indexes=SSCI Timespan=All years # 11TS=(responsiv* near/2 education) Indexes=SSCI Timespan=All years # 10TS=(milieu near/2 teaching) Indexes=SSCI Timespan=All years # 9TS=(naturalistic near/2 teaching) Indexes=SSCI Timespan=All years # 8TS=("focus* stimulation") Indexes=SSCI Timespan=All years # 7TS= ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)) Indexes=SSCI Timespan=All years # 6TS= ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (interact* or inter‐act* or involv* or mediat* or respon*)) Indexes=SSCI Timespan=All years # 5#4 AND #3 Indexes=SSCI Timespan=All years # 4TS=(child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*) Indexes=SSCI Timespan=All years # 3#2 OR #1 Indexes=SSCI Timespan=All years # 2TS=((intellectual* or learning) near/1 (disabled or disabilit* or impair*)) OR TS=(developmental* near/1 (delay* or disabilit* or disabl*)) or TS= ("mental* retard*" OR mongol* or "trisomy 21" or "chromosome 21") Indexes=SSCI Timespan=All years # 1TS=("down* syndrome" or "downs disease") Indexes=SSCI Timespan=All years
Cochrane Database of Systematic Reviews (CDSR), part of the Cochrane Library
Searched up to 22 January 2018 (25 records)
#1[mh "Down syndrome"] #2(down* next syndrome):ti,ab,kw #3"Downs disease":ti,ab,kw #4"trisomy 21":ti,ab,kw 59 #5"chromosome 21":ti,ab,kw #6(mongol or mongols or mongoloid or mongolism):ti,ab,kw #7[mh "Intellectual Disability"] #8[mh " Developmental disabilities"] #9((intellectual* or learning) near/3 (disabilit* or disabl*)):ti,ab,kw #10(developmental* near/3 (delay* or disabilit* or disabl*)):ti,ab,kw #11mental* next retard*:ti,ab,kw #12{or #1‐#11} #13[mh Child] #14[mh infant] #15(child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*):ti,ab,kw #16{or #13‐#15} #17#12 and #16 #18[mh "Parent‐Child Relations"] #19[mh Parenting] #20[mh Parents] #21[mh Caregivers] #22{or #18‐#21} #23[mh Education] #24[mh teaching] #25[mh "Early intervention (Education)"] #26(early next intervent*):ti,ab,kw #27[mh "Education of Intellectually Disabled"] #28[mh "education, special"] #29[mh "language therapy"] #30[mh "speech therapy"] #31(speech* or languag* or communicat* or sign* or nonverbal* or non‐verbal* or cue*):ti,ab,kw #32[mh "Sign language"] #33[mh "Manual Communication"] #34[mh "Nonverbal communication"] #35{or #23‐#34} #36#22 and #35 #37((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)):ti,ab,kw #38((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (interact* or inter‐act* or involv* or mediat* or respon*)) 2360 #39focus*ed next stimulation #40(naturalistic near/2 teaching):ti,ab,kw #41(milieu near/2 teaching):ti,ab,kw #42(responsiv* near/2 education):ti,ab,kw #43(responsiv* near/2 teaching):ti,ab,kw #44(Hanen*):ti,ab,kw #45{or #37‐#44} #46#36 or #45 #47#17 and #46 in Cochrane Reviews (Reviews and Protocols) [Note: Final search line 2016] #48#17 AND ##46 in Cochrane Reviews (Reviews and Protocols) added to Cochrane Library March 2016 ‐ Jan 2018 [Note: Final search line 2018]
Database of Abstracts of Reviews of Effects (DARE), part of the Cochrane Library
Searched up to 18 March 2016 (9 records). This was the final issue of DARE to be updated.
#1[mh "Down syndrome"] #2(down* next syndrome):ti,ab,kw #3"Downs disease":ti,ab,kw #4"trisomy 21":ti,ab,kw 59 #5"chromosome 21":ti,ab,kw #6(mongol or mongols or mongoloid or mongolism):ti,ab,kw #7[mh "Intellectual Disability"] #8[mh " Developmental disabilities"] #9((intellectual* or learning) near/3 (disabilit* or disabl*)):ti,ab,kw #10(developmental* near/3 (delay* or disabilit* or disabl*)):ti,ab,kw #11mental* next retard*:ti,ab,kw #12{or #1‐#11} #13[mh Child] #14[mh infant] #15(child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*):ti,ab,kw #16{or #13‐#15} #17#12 and #16 #18[mh "Parent‐Child Relations"] #19[mh Parenting] #20[mh Parents] #21[mh Caregivers] #22{or #18‐#21} #23[mh Education] #24[mh teaching] #25[mh "Early intervention (Education)"] #26(early next intervent*):ti,ab,kw #27[mh "Education of Intellectually Disabled"] #28[mh "education, special"] #29[mh "language therapy"] #30[mh "speech therapy"] #31(speech* or languag* or communicat* or sign* or nonverbal* or non‐verbal* or cue*):ti,ab,kw #32[mh "Sign language"] #33[mh "Manual Communication"] #34[mh "Nonverbal communication"] #35{or #23‐#34} #36#22 and #35 #37((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)):ti,ab,kw #38((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) near/3 (interact* or inter‐act* or involv* or mediat* or respon*)) 2360 #39focus*ed next stimulation #40(naturalistic near/2 teaching):ti,ab,kw #41(milieu near/2 teaching):ti,ab,kw #42(responsiv* near/2 education):ti,ab,kw #43(responsiv* near/2 teaching):ti,ab,kw #44(Hanen*):ti,ab,kw #45{or #37‐#44} #46#36 or #45 #47#17 and #46 in Other Reviews
Academic Search Complete EBSCOhost
Searched up to 22 January 2018 (2317 records)
1.DE "DOWN syndrome" 2.TI (down* N1 syndrome) or AB (down* N1 syndrome) 3.TI Downs disease or AB Downs disease 4.TI trisomy 21 or AB trisomy 21 5.TI chromosome 21 or AB chromosome 21 6.TI (mongol or mongols or mongoloid or mongolism) or AB (mongol or mongols or mongoloid or mongolism) 7.Intellectual Disability 8.DE "DEVELOPMENTAL disabilities" 9.TI ((intellectual* or learning) N3 (disabilit* or disable*)) or AB ((intellectual* or learning) N3 (disabilit* or disable*)) 10.TI (developmental* N3 (delay* or disabilit* or disabl*)) or AB (developmental* N3 (delay* or disabilit* or disabl*)) 11.TI mental* retard* or AB mental* retard* 12.S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 13.TI child or AB child 14.TI ((child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*)) OR AB ((child* or infant* or babies or baby or toddler* or girl* or boy* or pre‐school* or preschool* or nurser* or kindergarten* or kinder‐garten*)) 15.S13 or S14 16.S12 and S15 17.DE "PARENT‐child caregiver relations" 18.DE "PARENTING" 19.DE "PARENTS" 20.DE "CAREGIVERS" 21.S17 or S18 or S19 or S20 22.DE "EDUCATION" 23.DE "TEACHING" 24.DE "EARLY Intervention (Education)" 25.TI early intervent* or AB early intervent* 26.DE "PEOPLE with disabilities ‐‐Education" 27.DE "SPECIAL education" 28.language therapy 29.DE "SPEECH therapy" 30.TI (speech* or language* or communicat* or sign* or nonverbal* or non‐verbal* or cue*) or AB (speech* or language* or communicat* or sign* or nonverbal* or non‐verbal* or cue*) 31.DE "SIGN language" 32.Manual Communication 33.DE "NONVERBAL communication" 34.S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 35.S21 and S34 36.DE "PARENTS –Education" 37.DE "CAREGIVER education" 38.TI ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)) or AB ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (coach* or educat* or intervention* or learn* or program* or teach* or train*)) 39.TI ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (interact* or interact* or involve* or mediat* or respon*)) or AB ((parent* or maternal* or mother* or father* or paternal* or carer* or caregiver* or care‐giver*) N3 (interact* or interact* or involve* or mediat* or respon*)) 40.S36 or S37 or S38 or S39 41.TI focus?ed stimulation or AB focus?ed stimulation 42.TI (naturalistic N2 teaching) or AB (naturalistic N2 teaching) 43.TI (milieu N2 teaching) or AB (milieu N2 teaching) 44.TI (responsiv* N2 education) or AB (responsiv* N2 education) 45.TI (responsiv* N2 teaching) or AB (responsiv* N2 teaching) 46.TI Hanen*or AB Hanen* 47.S41 or S42 or S43 or S44 or S45 48.S35 or S40 or S47 49.S16 and S48 50.random assignment 51.DE "CLINICAL trials" 52.DE "META‐analysis" 53.randomis* or randomiz* 54.(random* N3 allocat*) or (random* N3 assign*) 55.(clinic* N3 trial*) or (control* N3 trial*) 56.(singl* N3 mask*) or (singl* N3 blind*) 57.(doubl* N3 mask*) or (doubl* N3 blind*) 58.(trebl* N3 mask*) or (trebl* N3 blind*) 59.(tripl* N3 mask*) or (tripl* N3 blind*) 60.DE "CROSSOVER trials" 61.crossover* or "cross‐over*" 62.placebo* 63.T1 (evalut* study or evalut* research) or AB (evaluat* study or evaluat* research) or T1 (effective* study or effective* research) or AB (effective* study or effective* research) or T1 (prospectiv* study or prospectiv* research) or AB (prospectiv* study or prospectiv* research) 774,229or T1 (follow‐up study) or follow‐up research) or AB (follow‐up study or follow‐up research) 64.S50 or S51 or S52 or S53 or S54 or S55 or S56 or S57 or S58 or S59 or S60 or S61 or S62 or S63 65.65. S49 and S64
ProQuest Dissertations and Theses UK & Ireland (1990 to 22 January 2018)
Searched up to 22 January 2018 (286 records)
TI,AB((Down* NEAR/1 syndrom* OR Mental* NEAR/1 retard*) OR ((Intellectual* OR Learning OR Developmental*) NEAR/1 ( Disabilit* or disabl* or handicap*))) AND ((speech OR language OR communicat* OR signs OR signing OR nonverbal* OR non‐verbal* OR cue*) OR ((parent* OR mother* OR father* OR carer*) NEAR/5 ( teach* OR interact* OR mediat* OR nonverbal* OR non‐verbal* OR cue*)) OR (Naturalistic OR Milieu OR Responsiv* OR "focus*ed stimulation" OR HANEN))
ProQuest Dissertations and Theses A&I (1970 to 22 January 2018)
Searched up to 22 January 2018 (433 records)
TI,AB((Down* NEAR/1 syndrom*)) AND ((parent* OR carer*) NEAR/5 (teach* OR interact* OR mediat*) OR (Naturalistic OR Milieu OR Responsiv* OR "focus*ed stimulation" OR HANEN))
LILACS (Latin American and Caribbean Health Science Information database; lilacs.bvsalud.org/en)
Searched up to 22 January 2018 (0 records)
(tw:((downs$ syndrome or downs disease) AND (child$ or infant$ or babies or baby or toddler$ or girl$ or boy$ or pre‐school$ or preschool$ or nurser$ or kindergarten$ or kinder‐garten$))) AND (tw:((parent$ or maternal$ or mother$ or father$ or paternal$ or carer$ or caregiver$ or care‐giver$ ) )) AND limited to RCTs
SpeechBITE (speechbite.com)
Searched up to 22 January 2018 (78 records)
"Down syndrome" OR "Parent or caregiver" filtered by publication types = RCTs
UKCRN Portfolio Database
Searched 21 March 2016 [9 records]
Search strings used in research Summary Field ( With "All" selected)
down syndrome speech down syndrome communication down syndrome language down syndrome parents down syndrome mediated down syndrome naturalistic down syndrome milieu Hanen (
UK Clinical Trials Gateway (www.ukctg.nihr.ac.uk)
Searched 24 January 2018 (6 records)
down* syndrome AND speech
down* syndrome AND language
down* syndrome AND communication
intellectual disability AND speech
intellectual disability AND language
intellectual disability AND communication
developmental disability AND speech
developmental disability AND language
developmental disability AND communication
developmental delay AND speech
developmental delay AND communication
developmental delay AND language
down* syndrome AND parent* AND communication
down* syndrome AND parent* AND language
down* syndrome AND parent* AND speech
Clinical Trials.gov (clinicaltrials.gov)
Searched up to 24 January 2018 (79 records)
Conditions: down syndrome
Interventions: parents OR carers OR caregivers or naturalistic OR milieu OR focused OR responsive OR mediated OR interaction OR involvement OR speech OR language OR communication OR sign OR nonverbal OR cue
AND
Age group: child (birth‐17)
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; apps.who.int/trialsearch/default.aspx)
Searched 24 January 2016 (23 records)
Advanced search
Condition: down syndrome
Intervention: parents OR carers OR caregivers or naturalistic OR milieu OR focused OR responsive OR mediated OR interaction OR involvement OR speech OR language OR communication OR sign OR nonverbal OR cue
Synonyms automatically searched: CHROMOSOME 21 TRISOMY, DOWN'S SYNDROME, DOWNS SYNDROME, G TRISOMY, MONGOLISM, SYNDROME DOWN'S, SYNDROME, DOWN, SYNDROME, DOWN'S, TRISOMY 21, TRISOMY 21 SYNDROME, down syndrome: ‐ communicative ‐ communication ‐ naturalistic ‐ involved ‐ involvement ‐ interactive ‐ interaction ‐ responsive ‐ ^caregiver ‐ care giver ‐ care givers ‐ caregiver ‐ caregivers ‐ nonverbal ‐ biopharma brand of benfluorex hydrochloride ‐ mediator ‐ mediator brand of benfluorex hydrochloride ‐ mediator trade name of benfluorex hydrochloride ‐ mediated ‐ linguistics ‐ language ‐ parent ‐ parental ‐ parents ‐ focal ‐ focus ‐ focused ‐ phonetics ‐ speech ‐ milieu ‐ carers ‐ physical findings ‐ sign ‐ stimulus ‐ cue
The Hanen Centre (hanen.org)
Last searched 22 January 2018 'Research Summaries' (4 records)
'WhatWorks' (thecommunicationtrust.org.uk/whatworks)
Last searched 22 January 2018 (15 records)
Area of Need: speech Language Communcation
Age Range: preschool
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Girolametto 1998.
| Methods | Design: quasi‐RCT | |
| Participants |
Location: Toronto, Canada Setting: participants were drawn from early intervention services Child participants Sample size: 12 children (intervention: 6, control: 6) with Down syndrome Mean age: intervention: 39.2 months (range 29‐44 months), control: 37.2 months (range 32‐41 months) IQ: intervention: 59‐93, control: 65‐103 Inclusion criteria: children communicated using at least 10 single words or signs with no word combinations, had a confirmed diagnosis of trisomy 21, and English was the only language of the home Comorbid conditions: 3 children (intervention: 1, control: 2) had mild hearing losses but did not use hearing aids. Most children had hearing that was within normal limits as assessed by a paediatric audiologist. Number of children per family: 2.7 (average), with 1 singleton in each group Parent participants Sample size: 12 mothers Mean age: 32 years (range 23‐34 years), across both groups Education: all mothers had completed at least high school, with 10 completing additional postsecondary education Marital status: all families described as being 'intact' Occupation: 7 mothers were homemakers, and the remainder were employed outside the house on at least a part‐time basis Socioeconomic status: middle class |
|
| Interventions | The 12 participants were randomly assigned to 1 of 2 groups.
|
|
| Outcomes | The measures listed below were used to measure the outcomes over 2 × 90‐minute sessions within 3 weeks following the intervention.
There was no report on adherence to the intervention by the clinician, although this was measured for the parent. Parental dosage (intervention fidelity) was not reported. |
|
| Notes |
Study start and end dates: not reported Funding source: grant from the Hospital for Sick Children Foundation, Toronto, Ontario, Canada Conflict of interest: none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no indication of how randomisation was carried out |
| Allocation concealment (selection bias) | Unclear risk | Comment: did not report if this was conducted |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: parent‐report measures were used and parents were not blind to group allocation. In addition, they did not report if the raters of the observational assessments were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: seemed to be no missing outcome data |
| Selective reporting (reporting bias) | High risk | Comment: the receptive scale of the SICD was completed after the intervention but was not reported. |
| Other bias | High risk | Comment: control group continued to receive their regular speech and language therapy input, and it was unclear how much parents were involved, but the intervention group did not. Target words were chosen for both groups to be measured after the intervention, but only the intervention group were made aware of these targets. |
Kaiser 2013.
| Methods | Design: RCT | |
| Participants |
Location: Tenessesse, USA Setting: 'clinic' location not specified, home sessions in participants' homes Child participants Sample size: 77 children with intellectual disability, 18 of whom had Down syndrome (intervention: 8, control: 10) Mean age: not reported (range 30‐54 months) IQ: intervention: mean 67 (SD 8.35), control: mean 68.5 (SD 7.65) Inclusion criteria
Comorbid conditions: none reported Number of children per family: not reported Parent participants Sample size: 18 parents (1 father (in the intervention group), 17 mothers) Mean age: intervention: 42.3 years, control: 39.8 years, range 30‐50 years across both groups Education: 3 parents had a master's degree, 8 a a bachelor's degree, 1 up to 3‐years of college, 2 up to 2‐years of college, 3 a high‐school level education, and 1 did not specify. Marital status: not reported Occupation: 9 participants were homemakers, with 8 (including the 1 father) being employed on a part‐ or full‐time basis, and 1 person did not specify Socioeconomic status: not reported, but see 'education' and 'occupation' directly above |
|
| Interventions | The 18 participants were randomly assigned to 1 of 2 groups:
Most children in the intervention and control groups continued to receive regular community‐based speech‐language therapy during the study, as well as other special education services. |
|
| Outcomes | The measures listed below were used to measure the outcomes immediately postintervention, 6 months postintervention and 1 month postintervention.
The study measured adherence to the intervention by the clinician, although parental dosage (intervention fidelity) was not reported. |
|
| Notes |
Study start and end dates: not reported Funding source: this study was supported, in part, by the National Institute of Child Health and Human Development (grant HD45745) and by the Department of Education (grant H325D070075). Conflicts of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: children were randomly assigned to 1 of 2 experimental conditions using an automated, randomisation computer programme after the child qualified for the study. |
| Allocation concealment (selection bias) | Unclear risk | Comment: did not report if this was conducted |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: administration and scoring of norm‐referenced assessments were completed by staff members who were not blind to the experimental condition. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: although there were missing data, the reasons were unlikely to be related to the true outcome, and they were balanced across groups. |
| Selective reporting (reporting bias) | Low risk | Comment: reported all pre‐specified outcomes |
| Other bias | Low risk | Comment: appears to be free of other sources of bias |
Karaaslan 2013a.
| Methods | Design: RCT | |
| Participants |
Location: Turkey Setting: participants were drawn from 2 special education rehabilitation centres Child participants Sample size: 15 children (intervention: 7, control: 8) with Down syndrome Mean age: intervention: 55.1 months, control: 44.1 months, range 2‐6 months across both groups IQ: the overall IQs of the children were not clear. Inclusion criteria: children had to be under 6 years of age, with a diagnosis of Down syndrome, and their mothers must not have been previously involved in a parenting intervention Comorbid conditions: not reported Number of children per family: not reported Parent participants Sample size: 15 mothers Mean age: intervention: 42.4 years, control: 42.4 years Education(mean level): intervention: 8.9 years, control: 9.6 years Marital status: all married Occupation: not reported Socioeconomic status: not reported but see 'education level' above |
|
| Interventions | The 15 participants were randomly assigned to 1 of 2 groups.
|
|
| Outcomes | The measures listed below were used to measure the outcomes, 2 months following the intervention.
The study measured adherence to the intervention by the clinician, although parental dosage (intervention fidelity) was not reported. |
|
| Notes |
Study start and end dates: not reported Funding source: not reported Conflicts of interest: not reported, although the 2nd author was one of the authors of the intervention programme |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: children were randomly assigned to the treatment or control group using a computer‐generated list of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Comment: did not report if this was conducted |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: 2 of the assessments used were totally or partially based on parent report, and parents were not blind to the group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: seemed to be no missing outcome data |
| Selective reporting (reporting bias) | Low risk | Comment: reported all pre‐specified outcomes |
| Other bias | Low risk | Comment: appears to be free of other sources of bias |
EMT: enhanced milieu teaching; IPSyn: Index of Productivity of Syntax; MLU: mean length of utterances; NDW: number of different words; RCT: randomised controlled trial; SICD: sequenced inventory of communication development.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adamson 2010 | Unclear whether children with Down syndrome were included, compared 3 types of parent‐mediated intervention, and outcomes were only measured in terms of joint attention and not language or communication |
| Allen 1980 | Not an RCT and did not measure language or communication skills |
| Allin 1988 | Targeted problematic behaviour and not language or communication |
| Aparicio 2003 | Parent‐mediated intervention in both arms of the trial |
| Bagner 2007 | Targeted problematic behaviour and not language or communication |
| Bagner 2016 | Did not include children with Down syndrome |
| Baker 1980 | Parent‐mediated intervention in both arms of the trial and did not target language or communication |
| Baker 1984 | Parent‐mediated intervention in both arms of the trial and did not target language or communication |
| Barna 1980 | Not an RCT |
| Barnett 1988 | Did not include children with Down syndrome |
| Bauer 2014 | Not an RCT |
| Bauer 2015 | Not an RCT |
| Baxendale 2003 | Did not include children with Down syndrome |
| Bennett 1983 | Not an RCT, did not include children with Down syndrome, and did not measure language or communication |
| Bidder 1975 | Not an RCT |
| Boyce 1993 | Results for children with Down syndrome were not reported separately, and study authors did not reply to our attempts to contact them |
| Buschmann 2010 | Not an intervention study |
| Campbell 1978 | Not an RCT, unclear whether children with Down syndrome were included, parent‐mediated intervention in both arms of the trial |
| Cologon 2017 | Parent‐mediated intervention in both arms of the trial |
| Coutinho 2003 | Targeted family functioning and use of support networks and not language or communication |
| Del Giudice 2006 | The intervention was behavioural in its approach and did not provide results for language and communication separately |
| Estes 1984 | Not an intervention study |
| Gibbard 1992 | Did not include children with Down syndrome |
| Gibbard 1994 | Did not include children with Down syndrome |
| Gibbard 2004 | Not an RCT and did not include children with Down syndrome |
| Girolametto 1988 | Results for children with Down syndrome were not reported separately |
| Haney 1993 | Did not include children with Down syndrome |
| Hassiotis 2017 | Did not measure speech, language or communication |
| Heifetz 1977 | The intervention targeted self‐help and not language or communication |
| Hopman 1989 | Not an intervention study |
| Hornby 1984 | Children were not aged 0‐6 years |
| Hudson 1982 | Results for children with Down syndrome were not reported separately, intervention was behavioural, and did not measure language or communication |
| Hwang 2013 | Included only one child with Down syndrome and parent‐mediated interventions in both arms of the trial |
| Innocenti 1993 | Results for children with Down syndrome were not reported separately, and study authors did not reply to our attempts to contact them |
| Karaaslan 2013b | Results for children with Down syndrome were not reported separately and study authors did not reply to our attempts to contact them |
| Kashima 1988 | The intervention targeted self‐help skills and not language or communication |
| Leung 2016 | Did not include children with Down syndrome |
| Mahoney 1985b | Did not include children with Down syndrome |
| Mahoney 1998 | Not an intervention study or RTC and parent mediated intervention in both arms of the trial |
| McIntyre 2008 | Did not include children with Down syndrome, and the intervention targeted problematic behaviour and not language or communication |
| McNally 2008 | Not an intervention study |
| Moxley‐Haegert 1983 | Did not include children with Down syndrome |
| NCT02158390 | Parent‐mediated intervention in both arms of the trial |
| Niccols 2000 | Not an RCT, and the intervention did not target language or communication |
| Pelchat 1999 | Not an RCT |
| Pratt 2015 | Did not include children with Down syndrome |
| Roberts 2006 | Targeted problematic behaviour and not language or communication |
| Roberts 2015 | Did not include children with Down syndrome |
| Roux 2013 | Targeted problematic behaviour and not language or communication |
| Russell 2004 | Parent‐mediated intervention in both arms of the trial |
| Schoenbrodt 2016 | Not an RCT and did not include children with Down syndrome |
| Seifer 1991 | Parent‐mediated intervention in both arms of the trial |
| Shapiro 2014 | Targeted problematic behaviour and not language or communication |
| Sofronoff 2011 | Targeted problematic behaviour and not language or communication |
| Tannock 1992 | Results for children with Down syndrome were not reported separately as the data had been destroyed |
| Te Kaat‐van den Os 2017 | Not an RCT but a systematic review |
| Warren 2008 | The intervention had parent‐mediated intervention in both arms of the trial |
| Woynaroski 2014 | Parent‐mediated interventions in both arms of the trial |
| Wright 2017 | Not an RCT |
RCT: randomised controlled trial.
Differences between protocol and review
-
Review authors
Paul Conway did not contribute to the review and hence was removed from the author line.
-
We have re‐written parts of the Background section with more up‐to‐date references on the condition and intervention.
-
We planned to include all of our secondary outcomes in the 'Summary of findings' table (O'Toole 2016), but instead we included only seven in compliance with MECIR Standards.
-
We searched two additional MEDLINE segments, which are updated daily and which became available to us after the protocol was published: MEDLINE in‐Process and Non‐Indexed Citations; and MEDLINE Epub Ahead of Print.
By the time of the top‐up search, UKCRN Portfolio Database had been replaced by UK Clinical Trials Gateway.
-
Data extraction and management
We did not use the categories of Intervention integrity as proposed by Dane 1988, but instead looked at treatment fidelity in terms of implementation fidelity and intervention fidelity with the categories recommended by Lieberman‐Betz 2015, as these were more appropriate for parent‐mediated intervention.
Contributions of authors
COT, AL, and FG planned the review. COT wrote the protocol and developed the search strategy, with advice from AL, FG and AvB. NH provided feedback on the accessibility of the information to services users. COT has overall responsibility for the review.
Sources of support
Internal sources
-
University College Cork, Ireland.
Salary for Alice Lee
-
University of Canterbury, New Zealand.
Salary for Anne van Bysterveldt
-
Down syndrome Ireland, Ireland.
Salary for Nicola Hart
External sources
-
Health Research Board, Ireland.
Cochrane Fellowship awarded to Ciara O'Toole
Declarations of interest
Ciara O'Toole (COT) received a Health Research Board Cochrane Fellowship Grant to assist in completing this work. The fellowship was received in January 2015, lasted for two years and paid for teaching cover, training support and related travel expenses. COT's institution received a grant from Foras Na Gaeilge for a project looking at early language acquisition of Irish. COT receives royalties as Co‐Author of the Language Development and Language Impairment: A Problem‐Based Introduction, which she confirms does not cover the interventions being investigated in this review.
Alice Lee (AL) is currently a Principal Investigator on a research project (2016 to 2018) funded by the Health Research Board, Ireland. AL was involved as a Co‐Investigator on a research project (2010 to 2012) funded by the National Institutes of Health, USA. AL received support through the programme, ERASMUS Staff Mobility – training for higher education institution staff at enterprises and at higher education institutions, European Commission, in 2012, for research‐related activities. None of these financial activities are related to the present systematic review.
Fiona Gibbon (FG) was paid an honorarium from the University of Hong Kong in 2013 for her advice on a research strategy for a Research Assessment Exercise, and received a fee from Newcastle University in 2014 for being an external participant on an Internal Subject Review. FG's institution received funding from the Health Research Board for a Health Research Award in 2012 to 2015 and 2016 to 2018. FG receives royalties as Co‐Editor of the Handbook of Phonetic Sciences, which she confirms does not cover the interventions being investigated in this review. FG has shares in various companies, which she confirms do not have a real or potential vested interest in the findings of this review.
Anne van Bysterveldt (AvB) received fees for clinical supervision of a staff member from Christchurch District Health Board. AvB holds an unpaid adjunct position at the Champion Centre, a multi‐disciplinary early intervention centre for preschool children with complex developmental disabilities. AvB's current position at the University of Canterbury involves the development and delivery of courses in the field of speech and language therapy.
Nicola J Hart (NH) is a national Speech and Language Advisor for Down Syndrome Ireland, a charity that provides training, support and advocacy for people with Down syndrome and their families. NH leads a small multidisciplinary team of advisors who provide information and advice about issues that arise across the lifespan, from early intervention to old age, in people with Down syndrome.
New
References
References to studies included in this review
Girolametto 1998 {published data only (unpublished sought but not used)}
- Girolametto L. Access to data for children with Down syndrome [personal communication]. Email to: C O'Toole 21 August 2017.
- Girolametto L, Weitzman E, Clements‐Baartman J. Vocabulary intervention for children with Down syndrome: parent training using focused stimulation. Infant‐Toddler Intervention: the Transdisciplinary Journal 1998;8(2):109‐25. [ERIC Number: EJ568724] [Google Scholar]
Kaiser 2013 {published and unpublished data}
- Kaiser A. Request for data for children with Down syndrome [personal communication]. Email to: C O'Toole 7 July 2016.
- Kaiser AP, Roberts MY. Parent‐implemented enhanced milieu teaching with preschool children who have intellectual disabilities. Journal of Speech, Language, and Hearing Research 2013;56(1):295‐309. [DOI: 10.1044/1092-4388(2012/11-0231); NIHMSID: NIHMS489833; PMCID: PMC3740334; PUBMED: 22744141] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts A. Location of the study [personal communication]. Email to: C O'Toole 27 September 2018.
Karaaslan 2013a {published data only}
- Karaaslan O, Mahoney G. Effectiveness of responsive teaching with children with Down syndrome. Intellectual and Developmental Disabilities 2013;51(6):458‐69. [DOI: 10.1352/1934-9556-51.6.458; PUBMED: 24447017] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adamson 2010 {published data only}
- Adamson L B, Romski M, Bakeman R, Sevcik RA. Augmented language intervention and the emergence of symbol‐infused joint engagement. Journal of Speech, Language, and Hearing Research 2010;53(6):1769‐73. [DOI: 10.1044/1092-4388(2010/09-0208); PMC4428337; PUBMED: 20705741] [DOI] [PMC free article] [PubMed] [Google Scholar]
Allen 1980 {published data only}
- Allen DA. Relationship‐focused intervention with high‐risk infants: first year findings. 88th Annual Meeting of the American Psychological Association; 1980 Sept 1‐5; Montreal, Quebec (CA). Washington (DC): American Psychological Association, 1980.
Allin 1988 {published data only}
- Allin RB Jr. Intensive home‐based treatment interventions with mentally retarded/emotionally disturbed individuals and their families. In: Stark JA, Menolascino FJ, Albarelli MH, Gray VC editor(s). Mental Retardation and Mental Health: Classification, Diagnosis, Treatment, Services. New York (NY): Springer Verlag, 1988:265‐80. [DOI: 10.1007/978-1-4612-3758-7_24] [DOI] [Google Scholar]
Aparicio 2003 {published data only}
- Aparicio MTS, Balana JM. Social early stimulation of trisomy‐21 babies. Early Child Development and Care 2003;173(5):557‐61. [DOI: 10.1080/0300443032000088221] [DOI] [Google Scholar]
Bagner 2007 {published data only}
- Bagner DM, Eyberg SM. Parent‐child interaction therapy for disruptive behavior in children with mental retardation: a randomised controlled trial. Journal of Clinical Child and Adolescent Psychology 2007;36(3):418‐29. [DOI: 10.1080/15374410701448448; PUBMED: 17658985] [DOI] [PubMed] [Google Scholar]
Bagner 2016 {published data only}
- Bagner DM, Garcia D, Hill R. Direct and indirect effects of behavioral parent training on infant language production. Behavior Therapy 2016;47(2):184‐97. [DOI: 10.1016/j.beth.2015.11.001] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 1980 {published data only}
- Baker BL, Heifetz LJ, Murphy DM. Behavioral training for parents of mentally retarded children: one‐year follow‐up. American Journal of Mental Deficiency 1980;85(1):31‐8. [PUBMED: 7446567] [PubMed] [Google Scholar]
Baker 1984 {published data only}
- Baker BL, Brightman RP. Training parents of retarded children: program‐specific outcomes. Journal of Behavior Therapy and Experimental Psychiatry 1984;15(3):255‐60. [DOI: 10.1016/0005-7916(84)90034-X] [DOI] [PubMed] [Google Scholar]
Barna 1980 {published data only}
- Barna S, Bidder RT, Gray OP, Clements J, Gardner S. The progress of developmentally delayed pre‐school children in a home‐training scheme. Child: Care, Health and Development 1980;6(3):157‐64. [DOI: 10.1111/j.1365-2214.1980.tb00807.x] [DOI] [PubMed] [Google Scholar]
Barnett 1988 {published data only}
- Barnett WS, Escobar CM, Ravsten MT. Parent and clinic early intervention for children with language handicaps: a cost‐effectiveness analysis. Journal of Early Intervention 1988;12(4):290‐8. [DOI: 10.1177/1053811518801200401] [DOI] [Google Scholar]
Bauer 2014 {published data only}
- Bauer SM, Jones EA, KM Feeley. Teaching responses to questions to young children with Down syndrome. Behavioral Interventions 2014;29:36‐49. [DOI: 10.1002/bin.1368] [DOI] [Google Scholar]
Bauer 2015 {published data only}
- Bauer SM, EA Jones. Requesting and verbal imitation intervention for infants with Down syndrome: generalization, intelligibility, and problem solving. Journal of Developmental and Physical Disabilities 2015;27(1):37‐66. [DOI: 10.1007/s10882-014-9400-6] [DOI] [Google Scholar]
Baxendale 2003 {published data only}
- Baxendale J, Hesketh A. Comparison of the effectiveness of the Hanen Parent Programme and traditional clinic therapy. International Journal of Language and Communication Disorders 2003;38(4):397‐415. [DOI: 10.1080/1368282031000121651; PUBMED: 14578050] [DOI] [PubMed] [Google Scholar]
Bennett 1983 {published data only}
- Bennett T, Algozzine R, Handicapped Children's Early Education Program (US). Effects of Family‐oriented Intervention with Young Handicapped Children on Indicators of Parental Stress. Washington (DC): Special Education Programs; Handicapped Children's Early Education Program, 1983. [Google Scholar]
- Bennett T, Algozzine R, Special Education Programs (US), Handicapped Children's Early Education Program (US). Effects of Family‐oriented Intervention on Home Environment Variables with Young Handicapped children. Washington (DC): Special Education Programs; Handicaped Children's Early Education Program, 1986. [Google Scholar]
Bidder 1975 {published data only}
- Bidder RT, Bryant G, Gray OP. Benefits to Down's syndrome children through training their mothers. Archives of Disease in Childhood 1975;50(5):383‐6. [PMCID: PMC1544420; PUBMED: 127552] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boyce 1993 {published data only (unpublished sought but not used)}
- Boyce GC, White KR, Kerr B. The effectiveness of adding a parent involvement component to an existing center‐based program for children with disabilities and their families. Early Education and Development 1993;4(4):327‐45. [DOI: 10.1207/s15566935eed0404_8] [DOI] [Google Scholar]
Buschmann 2010 {published data only}
- Buschmann A, Jooss B. Communication training and language initiation for children with global developmental delay [Kommunikationsförderung und sprachanbahnung bei kindern mit globaler entwicklungsstörung]. Frühförderung interdisziplinär [Early Intervention Interdisciplinary] 2010;2:51‐61. [DOI: 10.2378/fi2010.art06d] [DOI] [Google Scholar]
Campbell 1978 {published data only}
- Campbell AA. A Comparison of the Effect of Two Types of Treatment Involving Professionals and Parents on the Developmental Progress of Preschool Developmentally Delayed Children [PhD thesis]. Memphis (TN): Memphis State University, 1978. [Google Scholar]
Cologon 2017 {published data only}
- Cologon K, Wicks L, Salvador A. Supporting caregivers in developing responsive communication partnerships with their children: extending a caregiver‐led interactive language program. Child Language Teaching and Therapy 2017;33(2):157‐69. [DOI: 10.1177/026565901665] [DOI] [Google Scholar]
Coutinho 2003 {published data only}
- Coutinho MTB. Parental training: family impact assessment [Formação Parental: avaliação do impacto na família]. Psicologia [Psychology] 2003;17(1):227‐44. [DOI: 10.17575/rpsicol.v17i1.446] [DOI] [Google Scholar]
Del Giudice 2006 {published data only}
- Giudice E, Titomanlio L, Brogna G, Bonaccorso A, Romano A, Mansi G, et al. Early intervention for children with Down syndrome in southern Italy: the role of parent‐implemented developmental training. Infants and Young Children 2006;19(1):50‐8. [DOI: 10.1097/00001163-200601000-00006] [DOI] [Google Scholar]
Estes 1984 {published data only}
- Estes MV. A Model Treatment Plan for Children with Down Syndrome from Birth to Thirty‐Six Months [PhD thesis]. Chicago (IL): Chicago School of Professional Psychology, 1984. [Google Scholar]
Gibbard 1992 {published data only}
- Gibbard DJ. An Evaluation of Parental‐Based Intervention with Pre‐School Language‐Delayed Children [PhD thesis]. Portsmouth (UK): University of Portsmouth, 1992. [DOI] [PubMed] [Google Scholar]
- Gibbard DJ. Inclusion of children with Down syndrome [personal communication]. Email to: C O'Toole 4 May 2016.
Gibbard 1994 {published data only}
- Gibbard DJ. Inclusion of children with Down syndrome [personal communication]. Email to: C O'Toole 4 May 2016.
- Gibbard DJ. Parental‐based intervention with pre‐school language‐delayed children. European Journal of Disorders of Communication 1994;29(2):131‐50. [PUBMED: 7865920] [DOI] [PubMed] [Google Scholar]
Gibbard 2004 {published data only}
- Gibbard DJ. Inclusion of children with Down syndrome [personal communication]. Email to: C O'Toole 4 May 2016.
- Gibbard DJ, Coglan L, MacDonald J. Cost‐effectiveness analysis of current practice and parent intervention for children under three years presenting with expressive language delay. International Journal of Language and Communication Disorders 2004;39(2):229‐44. [DOI: 10.1080/13682820310001618839; PUBMED: 15204453] [DOI] [PubMed] [Google Scholar]
Girolametto 1988 {published data only (unpublished sought but not used)}
- Girolametto LE. Access to data for children with Down syndrome [personal communication]. Email to: C O'Toole 21 August 2017.
- Girolametto LE. Improving the social‐conversational skills of developmentally delayed children: an intervention study. Journal of Speech and Hearing Disorders 1988;53(2):156‐67. [PUBMED: 2452300] [DOI] [PubMed] [Google Scholar]
Haney 1993 {published data only}
- Haney M, Klein MD. Impact of a program to facilitate mother‐infant communication in high‐risk families of high‐risk infants. Communication Disorders Quarterly 1993;15(1):15‐21. [DOI: 10.1177/152574019301500104] [DOI] [Google Scholar]
Hassiotis 2017 {published data only}
- Hassiotis A. Evidence for parent interventions in young children with intellectual developmental disabilities: application in the EPICC‐ID randomised controlled trial. Journal of Mental Health Research in Intellectual Disabilities 2017;10(Suppl 1):205. [Accession number: WOS:000408778700279] [Google Scholar]
Heifetz 1977 {published data only}
- Heifetz LJ. Access to data for children with Down syndrome [personal communication]. Email to: C O'Toole 22 June 2016.
- Heifetz LJ. Behavioral training for parents of retarded children: alternative formats based on instructional manuals. American Journal of Mental Deficiency 1977;82(2):194‐203. [PUBMED: 907011] [PubMed] [Google Scholar]
Hopman 1989 {published data only}
- Silvern SB, Hopman WM. Reviews of research: interactional approaches to parent training. Childhood Education 1989;65(3):167‐71. [DOI: 10.1080/00094056.1989.10522425] [DOI] [Google Scholar]
Hornby 1984 {published data only}
- Hornby G, Singh NN. Behavioural group training with parents of mentally retarded children. Journal of Mental Deficiency Research 1984;28(Pt 1):43‐52. [PUBMED: 6716455] [DOI] [PubMed] [Google Scholar]
Hudson 1982 {published data only}
- Hudson AM. Training parents of developmentally handicapped children: a component analysis. Behavior Therapy 1982;13(3):325‐33. [DOI: 10.1016/S0005-7894(82)80041-5] [DOI] [Google Scholar]
Hwang 2013 {published data only}
- Hwang AW, Chao M‐Y, Liu S‐W. A randomized controlled trial of routines‐based early intervention for children with or at risk for developmental delay. Research in Developmental Disabilities 2013;34(10):3112‐23. [DOI: 10.1016/j.ridd.2013.06.037; PUBMED: 23886756] [DOI] [PubMed] [Google Scholar]
Innocenti 1993 {published data only (unpublished sought but not used)}
- Innocenti MS. Access to data for children with Down syndrome [personal communication]. Email to: C O'Toole 21 June 2016.
- Innocenti MS, Hollinger PD, Escobar CM, White KR. The cost‐effectiveness of adding one type of parent involvement to an early intervention program. Early Education and Development 1993;4(4):306‐26. [DOI: 10.1207/s15566935eed0404_7] [DOI] [Google Scholar]
Karaaslan 2013b {published data only (unpublished sought but not used)}
- Karaaslan O, Diken IH, Mahoney G. A randomized control study of responsive teaching with young Turkish children and their mothers. Topics in Early Childhood Special Education 2013;33(1):18‐27. [DOI: 10.1177/0271121411429749] [DOI] [Google Scholar]
Kashima 1988 {published data only}
- Kashima KJ, Baker BL, Landen SJ. Media‐based versus professionally led training for parents of mentally retarded children. American Journal on Mental Retardation 1988;93(2):209‐17. [psycnet.apa.org/record/1989‐27126‐001] [PubMed] [Google Scholar]
Leung 2016 {published data only (unpublished sought but not used)}
- Leung C. Inclusion of children with Down syndrome [personal communication]. Email to: C O'Toole 30 January 2018.
- Leung C, Chan S, Lam T, Yau S, Tsang S. The effect of parent education program for preschool children with developmental disabilities: a randomized controlled trial. Research in Developmental Disabilities 2016;56:18‐28. [DOI: 10.1016/j.ridd.2016.05.015; PUBMED: 27258925] [DOI] [PubMed] [Google Scholar]
Mahoney 1985b {published data only}
- Mahoney WJ. Inclusion of children with Down syndrome [personal communication]. Email to: C O'Toole 21 June 2016.
- Mahoney WJ, Feldman W, Roche D, Kuzell N. A randomised controlled trial of a course for parents of children with learning disabilities: indirect beneficial effects. Developmental Medicine and Child Neurology 1984;26(2):114. [DOI: 10.1111/j.1469-8749.1984.tb04438.x] [DOI] [Google Scholar]
Mahoney 1998 {published data only}
- Mahoney G, Boyce G, Fewell RR, Spiker D, Wheeden CA. The relationship of parent‐child interaction to the effectiveness of early intervention services for at‐risk children and children with disabilities. Topics in Early Childhood Special Education 1998;18(1):5‐17. [DOI: 10.1177/027112149801800104] [DOI] [Google Scholar]
McIntyre 2008 {published data only}
- McIntyre LL. Parent training for young children with developmental disabilities: randomized controlled trial. American Journal of Mental Retardation 2008;113(5):356‐68. [DOI: 10.1352/2008.113:356-368; PMC2784887; PUBMED: 18702556] [DOI] [PMC free article] [PubMed] [Google Scholar]
McNally 2008 {published data only}
- McNally S. Evaluating intensive interaction. Learning Disability Practice 2008;11(9):25. [DOI: 10.7748/ldp.11.9.25.s26] [DOI] [Google Scholar]
Moxley‐Haegert 1983 {published data only}
- Moxley‐Haegert L, Serbin LA. Developmental education for parents of delayed infants: effects on parental motivation and children's development. Child Development 1983;54(5):1324‐31. [PUBMED: 6194944] [PubMed] [Google Scholar]
NCT02158390 {published data only}
- NCT02158390. Phenotypic specific communication intervention for children with Down syndrome. clinicaltrials.gov/ct2/show/NCT02158390 (first received 6 June 2014).
Niccols 2000 {published data only}
- Niccols A, Mohamed S. Parent training in groups: pilot study with parents of infants with developmental delay. Journal of Early Intervention 2000;23(2):133‐43. [DOI: 10.1177/105381510002300207] [DOI] [Google Scholar]
Pelchat 1999 {published data only}
- Pelchat D, Bisson J, Ricard N, Perreault M, Bouchard JM. Longitudinal effects of an early family intervention programme on the adaptation of parents of children with a disability. International Journal of Nursing Studies 1999;36(6):465‐77. [PUBMED: 10576117] [DOI] [PubMed] [Google Scholar]
Pratt 2015 {published data only}
- Pratt AS, Justice LM, Perez A, Duran LK. Impacts of parent‐implemented early‐literacy intervention for Spanish‐speaking children with language impairment. International Journal of Language and Communication Disorders 2015;50(5):569‐79. [DOI: 10.1111/1460-6984.12140; PUBMED: 26176703] [DOI] [PubMed] [Google Scholar]
Roberts 2006 {published data only}
- Roberts C, Mazzucchelli T, Studman L, Sanders MR. Behavioral family intervention for children with developmental disabilities and behavioral problems. Journal of Clinical Child and Adolescent Psychology 2006;35(2):180‐93. [DOI: 10.1207/s15374424jccp3502_2; PUBMED: 16597214] [DOI] [PubMed] [Google Scholar]
Roberts 2015 {published data only}
- Roberts MY, Kaiser AP. Early intervention for toddlers with language delays: a randomized controlled trial. Pediatrics 2015;135(4):686‐93. [DOI: 10.1542/peds.2014-2134; PUBMED: 25733749] [DOI] [PMC free article] [PubMed] [Google Scholar]
Roux 2013 {published data only}
- Roux G, Sofronoff K, Sanders M. A randomized controlled trial of group Stepping Stones Triple P: a mixed‐disability trial. Family Process 2013;52(3):411‐24. [DOI: 10.1111/famp.12016; PUBMED: 24033239] [DOI] [PubMed] [Google Scholar]
Russell 2004 {published data only}
- Russell PSS, John JK, Lakshmanan J, Russell S, Lakshmidevi KM. Family intervention and acquisition of adaptive behaviour among intellectually disabled children. Journal of Learning Disabilities 2004;8(4):383‐95. [DOI: ] [Google Scholar]
Schoenbrodt 2016 {published data only}
- Schoenbrodt L, Kumin L, Dautzenberg D, Lynds J. Training parents to enhance narrative language skills in their children with intellectual disability [Formación parental para mejorar las técnicas del lenguaje narrativo de sus hijos con discapacidad intelectual]. International Medical Review on Down Syndrome [Revista Médica Internacional sobre el Síndrome de Down] 2016;20(3):31‐8. [DOI: 10.1016/j.sdeng.2016.09.001] [DOI] [Google Scholar]
Seifer 1991 {published data only}
- Seifer R, Clarke GN, Sameroff AJ. Positive effects of interaction coaching on infants with developmental disabilities and their mothers. American Journal on Mental Retardation 1991;96(1):1‐11. [psycnet.apa.org/record/1991‐34041‐001] [PubMed] [Google Scholar]
Shapiro 2014 {published data only}
- Shapiro CJ, Kilburn J, Hardin JW. Prevention of behavior problems in a selected population: Stepping Stones Triple P for parents of young children with disabilities. Research in Developmental Disabilities 2014;35(11):2958‐75. [DOI: 10.1016/j.ridd.2014.07.036; PUBMED: 25124695] [DOI] [PubMed] [Google Scholar]
Sofronoff 2011 {published data only}
- Sofronoff K, Jahnel D, Sanders M. Stepping Stones Triple P seminars for parents of a child with a disability: a randomized controlled trial. Research in Developmental Disabilities 2011;32(6):2253‐62. [DOI: 10.1016/j.ridd.2011.07.046; PUBMED: 21871779] [DOI] [PubMed] [Google Scholar]
Tannock 1992 {published data only (unpublished sought but not used)}
- Tannock R. Access to data for children with Down syndrome [personal communication]. Email to: C O'Toole 6 July 2016.
- Tannock R, Girolametto L, Siegel LS. Language intervention with children who have developmental delays: effects of an interactive approach. American Journal of Mental Retardation 1992;97(2):145‐60. [PUBMED: 1384566] [PubMed] [Google Scholar]
Te Kaat‐van den Os 2017 {published data only}
- Kaat‐van den Os DJA, Jongmans MJ, Volman MJM, Lauteslager PEM. Parent‐implemented language interventions for children with a developmental delay: a systematic review. Journal of Policy and Practice in Intellectual Disability 2017;14(2):129‐37. [DOI: 10.1111/jppi.12181] [DOI] [Google Scholar]
Warren 2008 {published data only}
- Warren SF, Fey ME, Finestack LH, Brady NC, Bredin‐Oja SL, Fleming KK. A randomized trial of longitudinal effects of low‐intensity responsivity education/prelinguistic milieu teaching. Journal of Speech, Language, and Hearing Research 2008;51(2):451‐70. [DOI: 10.1044/1092-4388(2008/033); PUBMED: 18367689] [DOI] [PubMed] [Google Scholar]
Woynaroski 2014 {published data only}
- Woynaroski T, Yoder PJ, Fey ME, Warren SF. A transactional model of spoken vocabulary variation in toddlers with intellectual disabilities. Journal of Speech, Language, and Hearing Research 2014;57(5):1754‐63. [DOI: 10.1044/2014_JSHLR-L-13-0252; PMC4192117; PUBMED: 24802090] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wright 2017 {published data only}
- Wright CA, Kaiser AP. Teaching parents Enhanced Milieu Teaching with words and signs using the Teach‐Model‐Coach‐Review Model. Topics in Early Childhood Special Education 2017;36(4):192‐204. [DOI: 10.1177/0271121415621027] [DOI] [Google Scholar]
Additional references
Abbeduto 2007
- Abbeduto L, Warren SF, Conners FA. Language development in Down syndrome: from the prelinguistic period to the acquisition of literacy. Mental Retardation and Developmental Disabilities Research Reviews 2007;13(3):247‐61. [DOI: 10.1002/mrdd.20158; PUBMED: 17910087] [DOI] [PubMed] [Google Scholar]
Abidin 1995
- Abidin RR. Parenting Stress Index. 3rd Edition. Odessa (FL): Psychological Assessment Resources, 1995. [Google Scholar]
Anlar 1996
- Anlar B, Yalaz K. Denver II Gelişimsel Tarama Testi Türk C̡ocuklarina Uyarlamasti ve Standardizasyonu El Kitabi [Turkish Manual for Denver II]. Ankara (TR): Meteksan Matbasi, 1996. [Google Scholar]
Barr 2011
- Barr E, Dungworth J, Hunter K, McFarlane M, Kubba H. The prevalence of ear, nose and throat disorders in preschool children with Down's syndrome in Glasgow. Scottish Medical Journal 2011;56(2):98‐103. [DOI: 10.1258/smj.2011.011036; PUBMED: 21670137] [DOI] [PubMed] [Google Scholar]
Barton 2013
- Barton EE, Fetting A. Parent‐implemented interventions for young children with disabilities: a review of fidelity features. Journal of Early Intervention 2013;35(2):194‐210. [DOI: 10.1177/1053815113504625] [DOI] [Google Scholar]
Bayley 1969
- Bayley N. Bayley Scales of Infant Development. New York (NY): Psychological Corporation, 1969. [Google Scholar]
Brinker 1994
- Brinker RP, Seifer R, Sameroff AJ. Relations among maternal stress, cognitive development and early intervention in middle‐ and low‐SES infants with developmental disabilities. American Journal on Mental Retardation 1994;98(4):463‐80. [PUBMED: 8148123] [PubMed] [Google Scholar]
Buckley 2002
- Buckley S, Prèvost P. Speech and language therapy for children with Down syndrome. Down Syndrome News and Update 2002;2(2):70‐6. [DOI: 10.3104/practice.171] [DOI] [Google Scholar]
Chapman 1997
- Chapman RS. Language development in children and adolescents with Down syndrome. Mental Retardation and Developmental Disabilities Research Reviews 1997;3(4):307‐12. [DOI: 10.1002/(SICI)1098-2779(1997)3:4%3C307::AID-MRDD5%3E3.0.CO;2-K] [DOI] [Google Scholar]
Chapman 1998
- Chapman RS, Seung H‐K, Schwartz SE, Kay‐Raining Bird E. Language skills of children and adolescents with Down syndrome: II. Production deficits. Journal of Speech, Language, and Hearing Research 1998;41(4):861‐73. [DOI: 10.1044/jslhr.4104.861] [DOI] [PubMed] [Google Scholar]
Chapman 2001
- Chapman RS, Hesketh LJ. Language, cognition, and short‐term memory in individuals with Down syndrome. Down Syndrome Research and Practice 2001;7(1):1‐7. [DOI: 10.3104/reviews.108; PUBMED: 11706807] [DOI] [PubMed] [Google Scholar]
Dane 1988
- Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control?. Clinical Psychology Review 1988;18(1):23‐45. [PUBMED: 9455622] [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG, editor(s). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Intervention Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
DeVeney 2016
- DeVeney SL, Hagaman JL. Comparison of parent‐implement and clinician‐directed intervention for toddlers identified as late talkers: a literature review. EBP Briefs 2016;10(6):1‐9. [800.627.7271; www.asha.org/articlesummary.aspx?id=8589969886] [Google Scholar]
Donner 2000
- Donner A, Klar N. Design and Analysis of Cluster Randomisation Trials in Health Research. London (UK): Arnold, 2000. [Google Scholar]
Dunn 1997
- Dunn LM, Dunn DM. Peabody Picture Vocabulary Test‐III: Manual. Circle Pines (MN): AGS, 1997. [Google Scholar]
Edwards 1997
- Edwards S, Fletcher P, Garman M, Hughes A, Letts C, Sinka I. Reynell Developmental Language Scales III. London (UK): GL Assessments, 1997. [Google Scholar]
EndNote X7 [Computer program]
- Thomas Reuters. EndNote. Version X7. Thomas Reuters, 2015.
Fenson 1993
- Fenson L, Dale PS, Reznick JS, Thal D, Bates E, Hartung JP, et al. The MacArthur Communicative Development Inventories: User's Guide and Technical Manual. San Diego (CA): Singular Publishing Group, 1993. [Google Scholar]
Fenson 2007
- Fenson L, Marchman VA, Thal DJ, Dale PS, Reznick JS, Bates E. MacArthur‐Bates Communicative Development Inventories (CDI): User's guide and Technical Manual. 2nd Edition. Baltimore (MD): Brookes Publishing Co, 2007. [Google Scholar]
Fey 2006
- Fey ME, Warren SF, Brady N, Finestack LH, Bredin‐Oja SL, Fairchild M, et al. Early effects of responsivity education/prelinguistic milieu teaching for children with developmental delays and their parents. Journal of Speech, Language, and Hearing Research 2006;49(3):525‐47. [DOI: 10.1044/1092-4388(2006/039)] [DOI] [PubMed] [Google Scholar]
Fey 2013
- Fey ME, Yoder PJ, Waren SF, Bredin‐Oja SL. Is more better? Milieu communication teaching in toddlers with intellectual disabilities. Journal of Speech, Language, and Hearing Research 2013;56(2):679‐93. [DOI: 10.1044/1092-4388(2012/12-0061); PMC3733661; PUBMED: 23275404] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gamble 2005
- Gamble C, Hollis S. Uncertainty method improved on best‐worst case analysis in a binary meta‐analysis. Journal of Clinical Epidemiology 2005;58(6):579‐88. [DOI: 10.1016/j.jclinepi.2004.09.013; PUBMED: 15878471] [DOI] [PubMed] [Google Scholar]
Girolametto 1993
- Girolametto L, Tannock R, Siegel L. Consumer‐orientated evaluation of interactive language intervention. American Journal of Speech‐Language Pathology 1993;2(3):41‐51. [DOI: ] [Google Scholar]
Girolametto 1996
- Girolametto L, Pearce PS, Weitzman E. Interactive focused stimulation for toddlers with expressive vocabulary delays. Journal of Speech and Hearing Research 1996;39(6):1274‐83. [PUBMED: 8959612] [DOI] [PubMed] [Google Scholar]
Girolametto 2006
- Girolametto L, Weitzman E. It Takes Two To Talk ‐‐ the Hanen Program for parents: early language intervention through caregiver training. In: McCauley RJ, Fey ME editor(s). Treatment of Language Disorders in Children. Baltimore (MD): Brookes Publishing Co, 2006:77‐103. [Google Scholar]
GRADEproGDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed 30 April 2018. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. British Medical Journal 2008;336(7650):924‐6. [DOI: 10.1136/bmj.39489.470347.AD; PMC2335261; PUBMED: 18436948] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hampton 2016
- Hampton LH, Kaiser AP. Intervention effects on spoken‐language outcomes for children with autism: a systematic review and meta analysis. Journal of Intellectual Disability Research 2016;60(5):444‐63. [DOI: 10.1111/jir.12283; PUBMED: 27120988] [DOI] [PubMed] [Google Scholar]
Hancock 2007
- Hancock TB, Kaiser AP. Enhanced milieu teaching. In: McCauley RJ, Fey ME editor(s). Treatment of Language Disorders in Children. Baltimore (MD): Paul H Brooks, 2007:203‐36. [Google Scholar]
Hart 1995
- Hart B, Risley TR. Meaningful Differences in the Everyday Experience of Young American Children. Baltimore (MD): Brookes Publishing Co, 1995. [Google Scholar]
Hedges 1985
- Hedges LV, Olkin I. Statistical Methods of Meta‐Anlaysis. London (UK): Academic Press, 1985. [Google Scholar]
Hedrick 1984
- Hedrick DL, Prather EM, Tobin AR. Sequenced Inventory of Communication Development: Instruction Manual. Seattle (WA): University of Washington Press, 1984. [Google Scholar]
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21(11):1539‐58. [10.1002/sim.1186; 12111919] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistencies in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI: 10.1136/bmj.327.7414.557; PMC192859; PUBMED: 12958120] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Intervention Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG. Chapter 16: Special topics in statistics. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Intervention Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
Hoff 2006
- Hoff E. How social contexts support and shape language development. Developmental Review 2006;26(1):55‐88. [DOI: 10.1016/j.dr.2005.11.002] [DOI] [Google Scholar]
Huttenlocher 2010
- Huttenlocher J, Waterfall H, Vasilyeva M, Vevea J, Hedges LV. Sources of variability in children's language growth. Cognitive Psychology 2010;61(4):343‐65. [DOI: 10.1016/j.cogpsych.2010.08.002; PMC2981670; PUBMED: 20832781] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaiser 2011
- Kaiser AP, Roberts MY. Advances in early communication and language intervention. Journal of Early Intervention 2011;33(4):298‐309. [DOI: 10.1177/1053815111429968] [DOI] [Google Scholar]
Kent 2013
- Kent RD, Vorperian HK. Speech impairment in Down syndrome: a review. Journal of Speech, Language and Hearing Research 2013;56(1):178‐210. [DOI: 10.1044/1092-4388(2012/12-0148); PMC3584188; PUBMED: 23275397] [DOI] [PMC free article] [PubMed] [Google Scholar]
Laudahl 2006
- Laudahl B, Risser HJ, Lovejoy MC. A meta‐analysis of parent training: moderators and follow‐up effects. Clinical Psychology Review 2006;26(1):86‐104. [DOI: 10.1016/j.cpr.2005.07.004; PUBMED: 16280191] [DOI] [PubMed] [Google Scholar]
Law 2003
- Law J, Garrett Z, Nye C. Speech and language therapy interventions for children with primary speech and language delay or disorder. Cochrane Database of Systematic Reviews 2003, Issue 3. [DOI: 10.1002/14651858.CD004110] [DOI] [PMC free article] [PubMed] [Google Scholar]
Law 2017
- Law, J, Dennis, JA, Charlton, JJV. Speech and language therapy interventions for children with primary speech and/or language disorders. Cochrane Database of Systematic Reviews 2017, Issue 1. [DOI: 10.1002/14651858.CD012490] [DOI] [PMC free article] [PubMed] [Google Scholar]
Laws 2003
- Laws G, Bishop DMV. A comparison of language abilities in adolescents with Down syndrome and children with specific language impairment. Journal of Speech, Language, and Hearing Research 2003;46(6):1324‐39. [PUBMED: 14700358] [DOI] [PubMed] [Google Scholar]
Laws 2004
- Laws G, Bishop DMV. Verbal deficits in Down's syndrome and specific language impairment: a comparison. International Journal of Language and Communication Disorders 2004;39(4):423‐51. [PUBMED: 15691074] [DOI] [PubMed] [Google Scholar]
Laws 2014
- Laws G, Hall AJ. Early hearing loss and language abilities in children with Down syndrome. International Journal of Language and Communication Disorders 2014;49(3):333‐42. [DOI: 10.1111/1460-6984.12077; PUBMED: 24655309] [DOI] [PubMed] [Google Scholar]
Lieberman‐Betz 2015
- Lieberman‐Betz RG. A systematic review of fidelity of implementation in parent‐mediated early communication intervention. Topics in Early Childhood Special Education 2014;35(1):15‐27. [DOI: 10.1177/071121414557282] [DOI] [Google Scholar]
Loane 2013
- Loane M, Morris JK, Addor M‐C, Arriola L, Budd J, Doray B, et al. Twenty‐year trends in the prevalence of Down syndrome and other trisomies in Europe: impact of maternal age and prenatal screening. European Journal of Human Genetics 2013;21(1):27‐33. [DOI: 10.1038/ejhg.2012.94; PMC3522199; PUBMED: 22713804] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mahoney 1985a
- Mahoney GJ, Finger I, Powell A. Relationship of maternal behavioral style to the developmental of organically impaired mentally retarded infants. American Journal of Mental Deficiency 1985;90(3):296‐302. [PUBMED: 4083310] [PubMed] [Google Scholar]
Mahoney 1988
- Mahoney GJ. Communication patterns between mothers and mentally retarded infants. First Language 1988;8(23):157‐71. [DOI: 10.1177/014272378800802305] [DOI] [Google Scholar]
Mahoney 1999a
- Mahoney GJ. Maternal Behaviour Rating Scale. Tallmadge (OH): Family Child Learning Center, 1999. [Google Scholar]
Mahoney 1999b
- Mahoney G, Wheedan CA. The effect of teacher style on interactive engagement of preschool‐aged children with special learning needs. Early Childhood Research Quarterly 1999;14(1):51‐68. [DOI: ] [Google Scholar]
Manolson 1992
- Manolson A. It Takes Two To Talk: A Parent's Guide to Helping Children Communicate. Toronto (CA): Hanen Centre, 1992. [Google Scholar]
Martin 2009
- Martin GE, Klusek J, Estigarribia B, Roberts JE. Language characteristics of individuals with Down syndrome. Topics in Language Disorders 2009;29(2):112‐32. [DOI: 10.1097/TLD.0b013e3181a71fe1; NIHMSID: NIHMS100466; PMC2860304; PUBMED: 20428477] [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 1992
- Miller JF, Chapman RS. Systematic Analysis of Language Transcripts. Madison (WI): University of Wisconsin‐Madison, 1992. [Google Scholar]
Miller 1999
- Miller JF. Profiles of language development in children with Down syndrome. In: Miller JF, Leddy M, Leavitt LA editor(s). Improving the Communication of People with Down Syndrome. Baltimore (MD): Brookes Publishing Co, 1999:11‐39. [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLOS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097; PMC2707599; PUBMED: 19621072] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mundy 1995
- Mundy P, Kasari C, Sigman M, Ruskin E. Nonverbal communication and early language acquisition in children with Down syndrome and in normally developing children. Journal of Speech, Language, and Hearing Research 1995;38(1):157‐67. [DOI: 10.1044/jshr.3801.157; PUBMED: 7537345] [DOI] [PubMed] [Google Scholar]
Nӕss 2011
- Nӕss KA, Lyster SA, Hulme C, Melby‐Lervåg M. Language and verbal short‐term memory skills in children with Down syndrome: a meta‐analytic review. Research in Developmental Disabilities 2011;32(6):2225‐34. [DOI: 10.1016/j.ridd.2011.05.014; PUBMED: 21628091] [DOI] [PubMed] [Google Scholar]
Oono 2013
- Oono IP, Honey EJ, McConachie H. Parent‐mediated early intervention for young children with autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews 2013, Issue 4. [DOI: 10.1002/14651858.CD009774.pub2] [DOI] [PubMed] [Google Scholar]
Pennington 2009
- Pennington L, Noble E. Acceptability and usefulness of the group interaction training programme It Takes Two to Talk to parents of pre‐school children with motor disorders. Child: Care, Health and Development 2009;36(2):285‐296. [DOI: 10.1111/j.1365-2214.2009.01054.x; PUBMED: 20047598] [DOI] [PubMed] [Google Scholar]
Pennington 2018
- Pennington L, Akor WA, Laws K, Goldbart J. Parent‐mediated communication interventions for improving the communication skills of preschool children with non‐progressive motor disorders. Cochrane Database of Systematic Reviews 2018, Issue 7. [DOI: 10.1002/14651858.CD012507.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Polišenská 2014
- Polišenská K, Kapalková S. Language profiles in children with Down syndrome and children with language impairment: implications for early intervention. Research in Developmental Disabilities 2014;35(2):373‐82. [DOI: ; PUBMED: 24334226] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Roberts 2008
- Roberts JE, Chapman RS, Martin GE, Moskowitz L. Language of preschool and school‐age children with Down syndrome and fragile X syndrome. In: Roberts JE, Chapman RS, Warren SF editor(s). Speech & Language Development & Intervention in Down Syndrome and Fragile X Syndrome. Baltimore (MD): Brookes Publishing Co, 2008:77‐115. [Google Scholar]
Roberts 2011
- Roberts MY, Kaiser AP. The effectiveness of parent‐implemented language interventions: a meta‐analysis. American Journal of Speech‐Language Pathology 2011;20(3):180‐99. [DOI: 10.1044/1058-0360(2011/10-0055); PUBMED: 21478280] [DOI] [PubMed] [Google Scholar]
Roberts 2014
- Roberts MY, Kaiser AP, Wolfe CE, Bryant JD, Spidaleri AM. Effects of the Teach‐Model‐Coach‐Review instructional approach on caregiver use of language support strategies and children's expressive language skills. Journal of Speech, Language, and Hearing Research 2014;57(5):1851‐69. [DOI: 10.1044/2014_JSHLR-L0-13-0113] [DOI] [PubMed] [Google Scholar]
Roizen 2007
- Roizen N. Down syndrome. In: Batshaw ML, Pellegrino L, Roizen NJ editor(s). Children with Disabilities. 6th Edition. Baltimore (MD): Brookes Publishing Co, 2007:263‐74. [Google Scholar]
Romeo 2018
- Romeo RR, Leonard JA, Robinson ST, West MR, Mackey, AP, Rowe ML, et al. Beyond the 30‐million‐word gap: children's conversational exposure is associated with language‐related brain function. Psychological Science 2018;29(5):700‐10. [DOI: 10.1177/0956797617742725; PMC5945324; PUBMED: 29442613] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sameroff 2000
- Sameroff AJ, Fiese BH. Transactional regulation: the developmental ecology of early intervention. In: Shonkoff P, Meisels SJ editor(s). Handbook of Early Intervention. 2nd Edition. Cambridge (UK): Cambridge University Press, 2000:135‐59. [Google Scholar]
Savaşir 1994
- Savaşir I, Sezgin N, Erol N. Ankara Gelişim Tarama Envanteri‐AGTE [Ankara Developmental Screening Inventory]. 3rd Edition. Ankara (TR): Turkish Psychology Association, 1994. [Google Scholar]
Scarborough 1990
- Scarborough HS. Index of productive syntax. Applied Psycholinguistics 1990;11(1):1‐22. [DOI: 10.1017/S0142716400008262] [DOI] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Annals of Internal Medicine 2010;152(11):726‐32. [DOI: 10.7326/0003-4819-152-11-201006010-00232; PUBMED: 20335313] [DOI] [PubMed] [Google Scholar]
Shin 2009
- Shin M, Besser LM, Kucik JE, Lu C, Siffel C, Correa A. Prevalence of Down syndrome among children and adolescents in 10 regions of the United States. Pediatrics 2009;124(6):1565‐71. [DOI: 10.1542/peds.2009-0745; PUBMED: 19948627] [DOI] [PubMed] [Google Scholar]
Siller 2013
- Siller M, Hutman T, Sigman M. A parent‐mediated intervention to increase responsive parental behaviors and child communication in children with ASD: a randomised clinical trial. Journal of Autism and Developmental Disorders 2013;43(3):540‐55. [DOI: 10.1007/s10803-012-1584-y; PMC3511916; PUBMED: 22825926] [DOI] [PMC free article] [PubMed] [Google Scholar]
Slonims 2006
- Slonims V, McCohachie H. Analysis of mother‐infant interaction in infants with Down syndrome and typically developing infants. American Journal of Mental Retardation 2006;111(4):273‐89. [DOI: 10.1352/0895-8017(2006)111[273:AOMIII]2.0.CO;2; PUBMED: 16792429] [DOI] [PubMed] [Google Scholar]
Sparrow 2005
- Sparrow SS, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales. 2nd Edition. Boston (MA): Pearson, 2005. [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D, editor(s). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Intervention Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
Suskind 2015
- Suskind DL, Leffel KR, Graf E, Hernandez MW, Gunderson EA, Sapolich SG, et al. A parent‐directed language intervention for children of low socioeconomic status: a randomized controlled pilot study. Journal of Child Language 2016;43(2):366‐406. [DOI: 10.1017/S0305000915000033; PUBMED: 26041013] [DOI] [PMC free article] [PubMed] [Google Scholar]
Te Kaat‐van den Os 2015
- Kaat‐van den Os DJ, Jongmans MJ, Volman JM, Lauteslager PE. Do gestures pave the way? A systematic review of the transitional role of gesture during the acquisition of early lexical and syntactic milestones in young children with Down syndrome. Child Language Teaching and Therapy 2015;31(1):71‐84. [DOI: 10.1177/0265659014537842] [DOI] [Google Scholar]
Vijay 2004
- Vijay P, Windsor K, Hancock T, Kaiser A. Milieu Teaching Project KidTalk Code: Manual and Coding Protocol. Nashville (TN): Vanderbilt University, 2004. [Google Scholar]
Warren 2007
- Warren SF, Fey ME, Yodor PJ. Differential treatment intensity research: a missing link to creating optimally effective communication interventions. Mental Retardation and Developmental Disabilities Research Reviews 2007;13(1):70‐7. [DOI: 10.1002/mrdd.20139; PUBMED: 17326112] [DOI] [PubMed] [Google Scholar]
Williams 1997
- Williams KT. Expressive Vocabulary Test. Circle Pines (MN): AGS, 1997. [Google Scholar]
Yoder 1998
- Yoder PJ, Warren SF. Maternal responsivity predicts the prelinguistic communication that facilitates generalized intentional communication. Journal of Speech, Language, and Hearing Research 1998;41(5):1207‐19. [DOI: 10.1044/jshlr.4105.1207; PUBMED: 9771641] [DOI] [PubMed] [Google Scholar]
Yodor 2004
- Yodor PJ, Warren SF. Early predictors of language in children with and without Down syndrome. American Journal of Mental Retardation 2004;109(4):285‐300. [DOI: 10.1352/0895-8017(2004)109%3C285:EPOLIC%3E2.0.CO;2; PUBMED: 15176918] [DOI] [PubMed] [Google Scholar]
Yodor 2014
- Yoder P, Woynaroski T, Fey M, Warren S. Effects of dose frequency of early communication intervention in young children with and without Down syndrome. American Journal on Intellectual and Developmental Disabilities 2014;119(1):17‐32. [DOI: 10.1352/1944-7558-119.1.17; PMC4059517; PUBMED: 24450319] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ypsilanti 2008
- Ypsilanti A, Grouios G. Linguistic profiles of individuals with Down syndrome: comparing the linguistic performance of three developmental disorders. Child Neuropsychology 2008;14(2):148‐70. [DOI: 10.1080/09297040701632209; PUBMED: 18306077] [DOI] [PubMed] [Google Scholar]
Zampini 2011
- Zampini L, Fasolo M, D'Odorico L. Characteristics of maternal input to children with Down syndrome: a comparison with vocabulary size and chronological age‐matched groups. First Language 2011;32(3):324‐42. [DOI: 10.1177/0142723711410780] [DOI] [Google Scholar]
Zampini 2015
Zimmerman 2002
- Zimmerman I, Steiner V, Pond R. Preschool Language Scale. 4th Edition. San Antonio (TX): Psychological Corporation, 2002. [Google Scholar]
Zwi 2011
- Zwi M, Jones H, Thorgaard C, York A, Dennis JA. Parent training interventions for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD003018.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
O'Toole 2016
- O'Toole C, Lee AS‐Y, Gibbon FE, Bysterveldt AK, Hart NJ. Parent‐mediated interventions to promote communication and language development in children with Down syndrome aged between birth and six years. Cochrane Database of Systematic Reviews 2016, Issue 2. [DOI: 10.1002/14651858.CD012089] [DOI] [PMC free article] [PubMed] [Google Scholar]


