Summary
Background
Young people require specific attention when it comes to suicide prevention, however efforts need to be based on robust evidence.
Methods
We conducted a systematic review and meta-analysis of all studies examining the impact of interventions that were specifically designed to reduce suicide-related behavior in young people.
Findings
Ninety-nine studies were identified, of which 52 were conducted in clinical settings, 31 in educational or workplace settings, and 15 in community settings. Around half were randomized controlled trials. Large scale interventions delivered in both clinical and educational settings appear to reduce self-harm and suicidal ideation post-intervention, and to a lesser extent at follow-up. In community settings, multi-faceted, place-based approaches seem to have an impact. Study quality was limited.
Interpretation
Overall whilst the number and range of studies is encouraging, gaps exist. Few studies were conducted in low-middle income countries or with demographic populations known to be at increased risk. Similarly, there was a lack of studies conducted in primary care, universities and workplaces. However, we identified that specific youth suicide-prevention interventions can reduce self-harm and suicidal ideation; these types of intervention need testing in high-quality studies.
Keywords: Suicide prevention, Self-harm, Young people, Systematic review, Meta-analysis
Highlights
-
•
This is the first systematic review and meta-analysis to synthesize the full spectrum of youth suicide prevention approaches.
-
•
Findings suggest that interventions designed to reduce suicide risk in young people can be effective.
-
•
Interventions delivered in clinical, educational and community settings appear to reduce self-harm and/or suicidal ideation.
-
•
The quantity and range of studies identified is encouraging, suggesting increased attention and investment in this area.
Research in Context
Evidence Before This Study
Prior to this study systematic reviews in suicide prevention have been limited by either only including RCTs, or by concentrating on particular settings (e.g., schools) or intervention type (e.g., gatekeeper training), and as such do not cover the full spectrum of approaches. The more comprehensive systematic reviews do not focus specifically on youth.
Added Value of This Study
This is the first systematic review and meta-analysis to synthesize the full spectrum of suicide prevention approaches in young people. It identified a large number of studies conducted across clinical, educational/workplace and community settings. Studies also tested the full spectrum of interventions including universal means restriction and educational interventions, selective interventions such as training programs, indicated interventions such as cognitive or dialectical behavior therapy, and multimodal interventions that combined education with either screening or gatekeeper training. The meta-analysis found that interventions delivered in both clinical and educational settings appear to have an impact on suicide-related outcomes at post-intervention and follow-up. In community settings, multi-faceted, place-based approaches seem to have an impact on rates of suicide and self-harm. Overall, study quality was limited.
Implications of All the Available Evidence
The review identified that specific youth suicide-prevention interventions can reduce both self-harm and suicidal ideation in clinical, school and community settings, challenging the nihilism that often pervades in suicide prevention. Indeed, the number and range of studies identified by this review is encouraging and reflects increasing investment and best practice internationally when it comes to youth suicide prevention. However, there was an absence of studies conducted in low-middle income countries where large numbers of suicides occur, or with specific populations known to be at elevated risk of suicide, such as indigenous or same-sex attracted young people. Similarly, few studies were conducted in primary care, workplace or university settings, and very few utilized digital platforms. Additionally, many studies simply tested interventions that had previously been designed for adults as opposed to young people specifically. Together these findings suggest that important opportunities for youth suicide prevention are currently being missed. These gaps now need to be addressed by researchers, research funders, and by policy makers if we are to successfully address the rising rates of suicide among young people worldwide.
Alt-text: Unlabelled Box
1. Introduction
Suicide is the second-leading cause of death among young people and rates appear to be increasing [1]. Suicidal thoughts and behaviors (defined as suicide attempt or self-harm with clear or unclear suicidal intent) are more common than suicide [2] and predict future suicide and suicide attempts [3], with the period following a first suicide attempt associated with highest risk [4]. Presenting to hospital with self-harm significantly predicts subsequent suicide in youth [5]; with the period immediately following discharge from psychiatric inpatient treatment associated with highest risk for suicide [6]. The period following hospital discharge therefore provides a crucial opportunity for intervention. Suicidal ideation is a necessary precursor to suicide attempt and as such also requires intervention. Although suicidal ideation is arguably a distinct concept from suicidal behavior, for ease of reading it is included under the term “suicide-related behavior” throughout this review unless otherwise specified.
The majority of OECD countries have a national suicide prevention strategy and many identify young people as requiring specific attention [7], [8], [9]. In accordance with international best practice, most strategies recommend a comprehensive approach to suicide prevention spanning universal approaches (i.e., delivered to the whole population), selective approaches (i.e., delivered to groups or communities believed to be at higher risk of suicide) and indicated approaches (i.e., delivered to individuals displaying suicide-related behaviors). Strategies also recommend interventions operate across a range of settings, including clinical, educational, workplace and community settings [1]. More recently, strategies have called for interventions to be delivered in digital, as well as face-to-face, settings [10], [11].
Strategies must encompass evidence-based interventions if they are to reduce suicide [1]. Generating such evidence in suicide prevention, however, is complex [12]. Statistically, suicide is a relatively rare event, therefore it is often unfeasible to obtain sample sizes necessary to demonstrate the impact of interventions on this outcome. Moreover, many interventions do not lend themselves to being tested using randomized controlled trials (RCTs), typically considered the gold-standard [13]. As such, researchers assess changes in other more prevalent outcomes, including self-harm and suicidal ideation, using alternative study designs. Therefore, when synthesizing the evidence regarding what works in youth suicide prevention, alternative study designs warrant consideration.
Whilst previous reviews have synthesized this evidence, many only include RCTs [14]. Additionally, many concentrate on particular settings (e.g., schools) [15], or types of intervention (e.g., gatekeeper training programs) [16], and as such do not cover the full spectrum of approaches. Finally, systematic reviews that include a range of study designs and intervention types do not focus specifically on youth [17], [18]. Hence, a comprehensive review of the literature on youth suicide prevention interventions spanning the range of settings, study designs and intervention types, is required to better understand what works in youth suicide prevention. This will help policy makers, clinicians, service providers and commissioners determine the focus of future suicide prevention efforts.
We conducted a systematic review and, where possible, meta-analysis, of all studies examining the impact of interventions that were specifically designed to reduce suicide-related behavior in young people. Overcoming the limitations of previous reviews, we placed no restriction on study setting, intervention approach, or study design.
2. Methods
The methodology was informed by the Cochrane Collaboration [19] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20].
2.1. Study Selection and Classification
2.1.1. Inclusion Criteria
Studies of any design were eligible for inclusion in this review, provided they: [1] evaluated the impact of an intervention specifically designed to reduce suicide-related behavior; [2] assessed a suicide-related outcome, including suicide, suicide attempt, self-harm (defined as intentional self-injury and/or self-poisoning where suicidal intent was either not specified or was unclear), suicidal ideation, suicide risk, and/or reasons for living; [3] targeted young people aged 12–25 and/or if data on young people (mean age between 12·0 and 25·0) was specifically reported; [4] were published in a peer-reviewed journal or identified via the reference lists of included articles; and [5] were written in English.
2.1.2. Exclusion Criteria
Studies were excluded from the review if: [1] they were not implemented with the expressed and primary purpose of preventing or reducing suicide-related behavior. Under this criterion, studies of indicated interventions were excluded if they did not recruit participants based on present or recent suicidal ideation or behavior. Additionally, studies of means restriction approaches were included only if the intervention was implemented, wholly or partially, to prevent suicide. As such, studies of firearm regulations implemented with the expressed and primary purpose of preventing homicide were excluded under this criterion. Studies were also excluded if they: [2] did not measure and report on a suicide-related outcome (as defined above); this included studies that exclusively measured non-suicidal self-injury, as this is generally considered to be a separate phenomenon; [3] did not target young people, or if data relating to outcomes for young people could not be disaggregated from that adults; [4] employed a non-experimental design; [5] were not published in a peer-reviewed journal; [6] were not available in English; or [7] did not contain any unique relevant data over and above the first included study.
2.2. Search Strategy
We searched Medline, PsycINFO, and EMBASE from January 1 1990 to September 21, 2017. Keywords relevant to suicide-related behavior, intervention type and youth were combined using standard Boolean operators (see Appendix). Key words were developed by consensus among the author group and in consultation with a librarian. In addition, we hand-searched the reference lists of all previous reviews retrieved via the search.
In the first instance study titles and abstracts were screened by five of the review authors (EB, JR, SH, NS, KW). Due to the large number of studies retrieved two review authors independently screened 10% of the total number of records retrieved. Cohen's Kappa [21] was 0·748 and Prevalence-Adjusted and Bias-Adjusted Kappa (PABAK [22]) was 0·978, indicating excellent agreement regarding inclusion and exclusion of studies. Discrepancies were resolved by discussion. In the second stage of screening, full texts of potentially relevant studies were screened for inclusion by four authors (EB, JR, SH, NS). Full text double-screening was not undertaken, but review authors met regularly to resolve any queries.
2.3. Data Extraction and Classification
Data were extracted independently by seven authors (JR, EB, SH, NS, KW, DC, AM) using a pilot tested pro forma. The following information was extracted: (i) author(s) and publication date; (ii) country; (iii) study design; (iv) setting from which participants were recruited; (v) study sample or population characteristics; (vi) intervention description; (vii) details of control or comparison group (classified as treatment as usual (TAU), enhanced TAU and placebo), and; (viii) outcome data on suicide deaths, suicide attempt, suicidal ideation, suicide-related behavior, and/or self-harm at the point of post-intervention and (where appropriate) longest follow-up (note that follow-up periods varied). Where studies used more than one measure for an outcome, data from the measure that was most commonly used across all included studies were used, as has been done previously [23]. Two authors (SH and KW) undertook double data entry of all outcome data.
Studies were classified according to the following taxonomy. In the first instance studies were classified according to the setting from which the participants were recruited (i.e. clinical, education or workplace, and community). If participants were recruited from multiple settings, the study was classified according to the setting from which participants were primarily recruited. Studies were then classified by study design (i.e. RCTs and non-RCTs) and then by intervention approach (i.e. universal, selective, indicated). Some studies combined a number of different intervention approaches. In these cases studies were classified as ‘multi-modal’ when the intervention comprised a number of different components implemented together (e.g. psycho-education AND screening), and ‘multiple’ when studies tested the impact of different interventions that were implemented separately (e.g. psycho-education program in location A and gatekeeper training in location B). They were then classified according to intervention type (e.g. means restriction, educational, therapeutic). For the therapeutic interventions, the therapeutic modality itself was also specified. For example, within this category there were a number of studies that tested cognitive behavioral therapy (CBT), dialectical behavioral therapy (DBT) and so on.
2.4. Study Quality
An assessment of study quality was conducted. For all RCTs, this was assessed based on the Cochrane Collaboration Risk of Bias Tool [19]. In the majority of trials, as is often the case [24], blinding of participants and therapists was not possible. Each trial was therefore assessed with regard to random sequence generation, allocation concealment, ascertainment of self-harm, outcome assessor blinding, whether analyses were conducted according to the intention-to-treat (ITT) principle, and rates of attrition. For the latter criterion, an attrition rate of 15% or less on the primary outcome at the longest follow-up point indicated low risk of bias.
Non-RCTs were assessed in two ways. For those conducted in clinical, educational, or workplace settings (where a range of study designs were employed) we used a set of criteria based on resources from the Cochrane Effective Practice and Organization of Care (EPOC) group [25]. We assessed whether or not: [1] the study was adequately powered; [2] outcome assessors were blinded to treatment allocation (for studies where outcomes were measured via interview); [3] the attrition rate was below 15%; and [4] the authors used statistical testing to measure change.
Studies in community settings employed either an ecological or interrupted time series design. Here two criteria were used to assess quality: whether or not data were collected at multiple time points before and after the intervention [26], and whether or not the intervention itself was likely to affect data collection. “Multiple time points” was defined as at least twice before or after implementation of the intervention. The intervention was considered not to affect data collection if sources and methods of data collection were the same before and after the intervention, or if data were collected from official sources (e.g. coronial records).
2.5. Data Synthesis
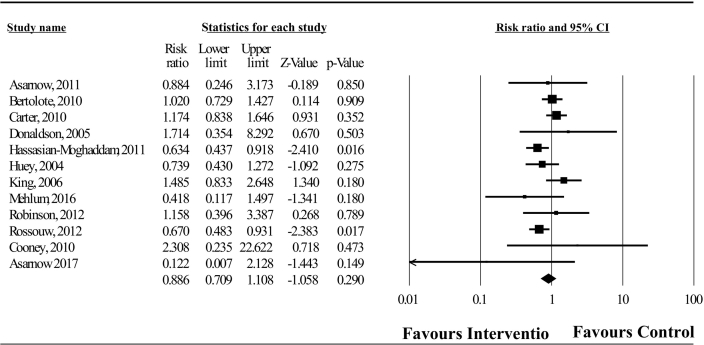
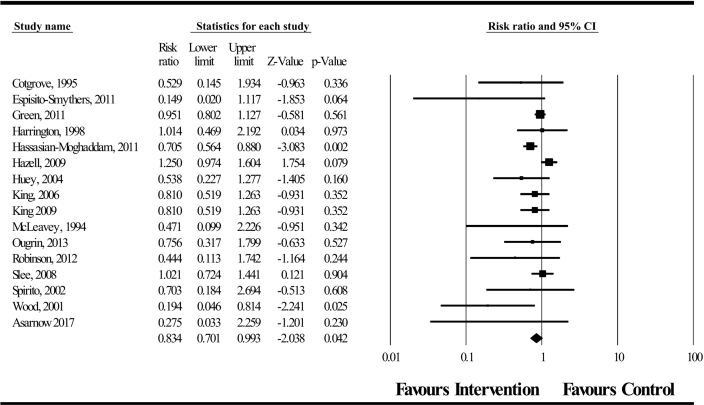
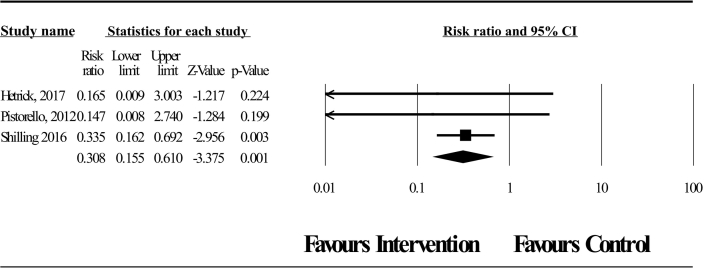
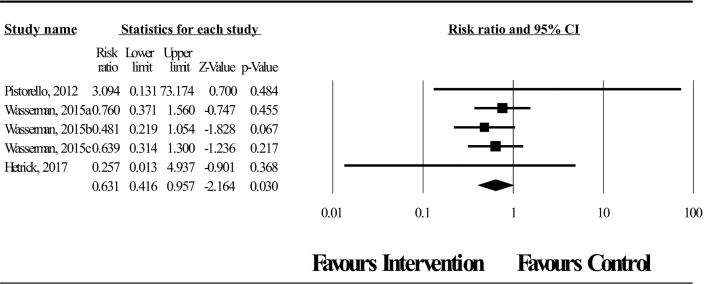
Meta-analysis was only conducted for RCTs. We analyzed data separately according to study setting. Because self-harm can encompass suicide attempts, is a key predictor of future suicide [27], and is more prevalent and more commonly assessed than suicide, self-harm (measured dichotomously) was our primary outcome and all dichotomous self-harm and suicide attempt data were combined. Additional outcomes were self-harm measured continuously, suicide and suicidal ideation (measured dichotomously and continuously). Where studies had more than one intervention arm, we included those arms that provided relevant data and split the control group to avoid double counting [28].
For dichotomous data, we pooled data between studies using the relative risk with 95% confidence interval. For continuous outcomes, given the range of different tools used, means and standard deviations were pooled using the standardized mean difference (SMD) using the Hedges' adjusted g with a 95% confidence interval. SMD effect sizes of 0·2 were considered small, 0·5 were considered medium, and ≥ 0·8 were considered large [29]. Measurement scales were standardized so that higher scores were indicative of greater levels of suicidal ideation. For both continuously- and dichotomously-measured outcomes, pooled effect size estimates were calculated using the DerSimonian-Laird random effects model [30] implemented using Comprehensive Meta-Analysis 2·2·064 software [31].
Between-study heterogeneity was measured using the I2 statistic. I2 values of 25%, 50% and 75% or larger are indicative of small, moderate and high heterogeneity, respectively [32].
2.5.1. Subgroup Analysis
For the primary outcome we undertook three subgroup analyses to investigate whether the intervention approach, intervention type and, for those interventions coded as psychotherapy, the therapeutic modality modified the pooled effect sizes.
First, intervention approach was coded as universal, selective or indicated. Second, type of intervention was categorized as psychotherapy, brief contact, or educational. Psychotherapy interventions were established psychotherapeutic approaches belonging to a particularly theoretical or philosophical school. Brief contact interventions were defined as those interventions that either: [1] focused on maintaining contact or facilitating re-engagement with services via a minimal amount of supportive contact, including provision of an emergency or crisis card as defined by Milner et al. [33]; or [2] interventions delivered within a very brief period, such as screening and referral or provision of one-off assessment and supportive therapy. Educational interventions delivered psycho-education about suicide-related behaviors, mental illness associated with these behaviors, signs and symptoms to look out for and advice on how to respond. Finally, trials coded as psychotherapy were further categorized by modality as either: CBT; DBT; mentalisation therapy; problem solving; motivational interviewing; supportive therapy; family therapy; interpersonal psychotherapy; combined (where several modes of psychotherapy were combined); or other (where the intervention did not clearly fit any category of named therapeutic approach).
2.5.2. Sensitivity Analysis
The robustness of results of the meta-analysis was checked for the primary outcome by conducting sensitivity analyses. RCTs judged as high or unclear risk of bias for allocation concealment, and RCTs where more than 15% of participants were lost to follow-up or where no data were reported, were excluded from this analysis.
For studies in which no data amenable to meta-analysis were reported, a narrative synthesis of results was conducted.
3. Results
3.1. Search Results
In total, 34,463 articles were retrieved via database searching and an additional four via the reference lists of included articles. Following initial screening, 572 full-text articles were retrieved, of which 105 met our inclusion criteria. Six were secondary publications that were included as they reported novel data [34], [35], [36], [37], [38], [39]. The review therefore includes findings from 105 articles corresponding to 99 unique studies (see Fig. 1).
Fig. 1.
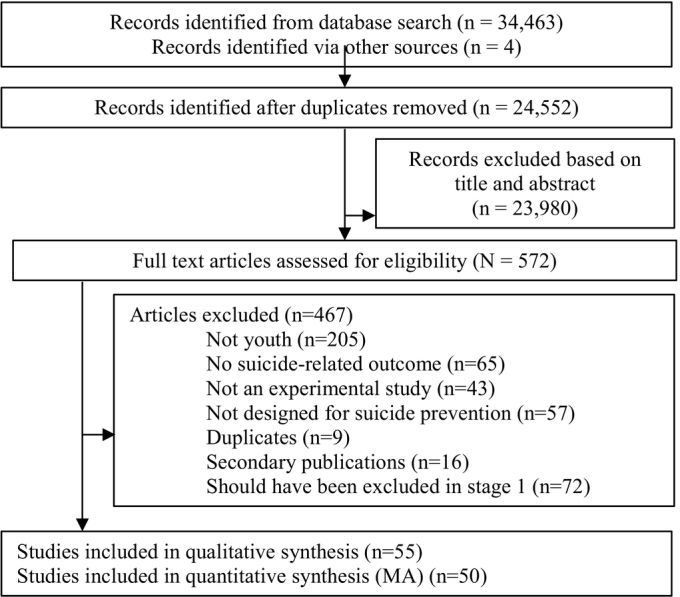
PRISMA flow diagram.
3.2. Overall Description of Included Studies
Half (52·5%) of included studies were conducted in clinical settings (Table 1, Table 2), 31 (31·3%) in educational or workplace settings (Table 3, Table 4), and 16 (16·2%) in community settings (Table 5, Table 6). Most studies tested indicated interventions (k = 66; 66·7%), followed by universal (k = 17; 17·2%), multimodal (k = 11; 11·1%), and selective (k = 2; 2·0%) interventions. Three studies (3·0%) evaluated multiple interventions. Forty-eight studies (48·5%) were RCTs. This included 33 (63·5%) of the studies conducted in clinical settings and 15 (48·4%) of those conducted in educational or workplace settings. None of the community-based studies were RCTs.
Table 1.
Randomized controlled trials conducted in clinical settings (N = 33).
| Study; country | Target population | Participants | Intervention description | Comparison condition | Risk of bias | Suicide related outcome(s) assessed; longest follow-up |
|---|---|---|---|---|---|---|
| Alavi et al. (2013) [41] Iran |
Inclusion: Young people admitted to hospital for a SA Exclusion: SH w/o intent; no current SI; inability to participate in psychotherapy; diagnosed with bipolar, psychosis, pervasive developmental or substance use disorders Recruited from: Hospital/ED |
Whole sample N = 30 Mean age: 16.1 (SD: 1.4; Range: 12–18 Gender: 10% male Treatment group N = 15 Mean age: 16.1 (SD: 1.6) Gender: 6.7% male Control group N = 15 Mean age: 16.0 (SD: 1.2) Gender: 13.3% male |
Individual cognitive behavioral therapy plus TAU Length: 12 sessions over 3 months Developed by: Stanley et al. (2009)a Delivered by: NR |
TAU: routine psychiatric intervention and follow up; pharmacotherapy if needed. | Random sequence generation method: Alternate allocation Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Was ITT analysis undertaken: NR |
SI (continuous): Beck Scale for Suicidal Ideation (BSSI) Longest follow-up: Post-intervention only |
| Asarnow et al. (2011) [65] USA |
Inclusion: Young people who presented to ED with SA or SI Exclusion: Acute psychosis or other symptoms that impede consenting and/or assessment process Recruited from: Hospital/ED |
Whole sample N = 181 Mean age: 14.7 (SD: 2.0; Range: 10–18) Gender: 30.9% male Treatment group N = 89 Mean age: 14.8 (SD: 2.1) Gender: 33.7% male Control group N = 92 Mean age: 14.6 (SD: 1.9) Gender: 28.3% male |
Brief contact intervention Compliance enhancement measures mixed with family therapy plus TAU Length: 1 month Developed by: Based on Rotheram-Borus et al. (1996)b and adapted by authors Delivered by: MH professionals |
Enhanced TAU: usual ED care, with staff education on linking to treatment, reducing access to means, risks of substance use. | Random sequence generation method: Computer generated algorithm Allocation concealment method: Independent researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate for SH at post-intervention: Yes (11.6%) Was ITT analysis undertaken: Yes |
SI (dichotomous): DISC-IV, an clinician administered diagnostic interview SA (dichotomous): DISC-IV, an clinician administered diagnostic interview and Harkavy Asnis Scale (HASS) Longest follow-up: Post-intervention only |
| Asarnow et al. (2017) [42] USA |
Inclusion: i) Young people who had presented after engaging in SH (SA or NSSI included) within the last three months; ii). history of repetitive SH (≥ 3 lifetime episodes) Exclusion: symptoms interfering with participation in assessments or intervention (psychosis, substance use) and inability to speak English Recruited from: Hospital/ED and MH outpatient |
Whole sample N = 42 Mean age: 14.62 (SD: 1.83) Gender: 11.9% male Treatment group N = 20 Mean age: 14.35 (SD: 1.81) Gender: 10.0% male Control group N = 22 Mean age: 14.86 (SD: 1.86) Gender: 13.6% male |
SAFETY program Combined intervention consisting of CBT and DBT informed family intervention that included formulation driven CBT, DBT and family centered interventions. Each family had two therapists: one for the young person and one for the parents and there were joint family sessions as well as separated sessions. Length: 12 sessions over 3 months Developed by: study authors Delivered by: MH professionals |
Enhanced TAU: in-clinic parent education on risk of repetition, accessing treatment; 3 + phone-calls monitoring safety, encouraging treatment attendance. | Random sequence generation method: Computerized randomization program Allocation concealment method: Enrolment and assessment staff masked to randomization status Ascertainment of DSH repetition: Self-report Outcome assessor blinding: Yes Less than 15% drop-out rate: No (23.8% for self-reported outcomes) Was ITT analysis undertaken: Yes |
SA (dichotomous): used a slight modification of the clinician administered Columbia Suicide Severity Rating Scale (C-SSRS) Longest follow-up: 12 months post-baseline |
| Bertolote et al. (2010) [66]; Fleischmann et al. (2008) [34] Multi-national |
Inclusion: Young people who presented to ED following SH/self-poisoning Exclusion: ‘any clinical condition(s) that would disallow interview’ Recruited from: Hospital/ED |
Whole sample N = 1867 Mean age: NR (Median = 23.0) Gender: 41.8% male Treatment group N = 922 Mean age: NR Gender: 40% male Control group N = 945 Mean age: NR Gender: 43.3% male |
Brief contact intervention 1 1-hour information session plus 9 phone calls or visits. Length: Up to 10 contacts over 18 months Developed by: study authors (based on existing BIC methods) Delivered by: doctor, nurse or psychologist |
TAU: varied between sites, primarily acute injury management with or without mental health referral. | Random sequence generation method: Random numbers table Allocation concealment method: Offsite researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: NR Less than 15% drop-out rate: Yes (11.0%) Was ITT analysis undertaken: NR |
SA (dichotomous): European Parasuicide Study Interview Schedule (EPSIS) of the WHO/EURO Multicenter Study on Suicidal Behavior Longest follow-up: Post-intervention only |
| Byford et al. (1999) [43] UK |
Inclusion: Diagnosis of SH (self-poisoning) Exclusion: Overdose was accidental; psychiatric condition which would preclude engagement with therapy; social situation precluded engagement with family therapy Recruited from: MH outpatient |
Whole sample N = 162 Age/gender: NR Treatment group N = 85 Age/gender: NR Control group N = 77 Age/gender: NR |
Individual family therapy plus TAU Length: 1 ½ hour assessment plus 1 h of therapy Developed by: study authors Delivered by: MH professionals |
TAU: routine assessment and psychiatric care in outpatient clinic. | Random sequence generation method: Shuffled cards Allocation concealment method: Sealed envelope Ascertainment of SH repetition: interview Outcome assessor blinding: Yes Less than 15% drop-out rate: Yes (8.0%) Was ITT analysis undertaken: NR |
SI (continuous): Suicidal Ideation Questionnaire (SIQ) Longest follow-up: Post-intervention only |
| Carter et al. (2010) [44] Australia |
Inclusion: Females referred for treatment following self-poisoning, meeting criteria for borderline personality disorder, with at least three self-reported episodes of self-harm over the preceding year. Exclusion: Males, those engaging in self-injury without self-poisoning Recruited from: MH outpatient |
Whole sample N = 70 Mean age: 24.5 (SD: 6.1; Range: 18–65) Gender: 0% male Treatment group N = 37 Mean age: 24.5 (SD: 6.1) Control group N = 33 Mean age: 24.7 (SD: 6.2) |
Dialectical behavior therapy Individual and group therapy, with telephone coaching. Length: number of sessions not specified, delivered over six months Developed by: based on Linehan et al. (1991)c Delivered by: MH professionals |
TAU + Waitlist: 6 month period of unspecified TAU while waitlisted. | Random sequence generation method: Shuffled envelopes Allocation concealment method: Sealed, opaque envelopes Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: Yes (0.0%) Was ITT analysis undertaken: Mixed methods |
SH (continuous): Linehan's Lifetime Parasuicide Count–2; Parasuicide History Interview SH (dichotomous): Linehan's Lifetime Parasuicide Count–2; Parasuicide History Interview Longest follow-up: Post-intervention only |
| Cooney et al. (2010) [45] New Zealand |
Inclusion: History of at least one SA or one episode of SH in past three months Exclusion: i) Intellectual disability; ii) Psychosis Recruited from: MH outpatient |
Whole sample N = 29 Mean age: 15.9 (SD: 1.0; Range: 14–18) Gender: 24.1% male Treatment group N = 14 Mean age: 16.2 (SD: 0.98) Gender: 28.6% male Control group N = 15 Mean age: 15.7 (SD: 1.1) Gender: 20% male |
Individual plus group dialectical behavioral therapy Length: weekly sessions for approximately 26 weeks Developed by: based on Linehan (1993)d & Miller et al. (2007)e Delivered by: MH professional |
TAU: type and duration varied: CBT, motivational interviewing, supportive counseling, family therapy; medication and case management as needed. | Random sequence generation method: Computer generated algorithm Allocation concealment method: Sealed, opaque envelopes Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: Yes (0.0%) Was ITT analysis undertaken: Mixed methods |
SI (continuous): BSSI SA (dichotomous): Linehan's Suicide Attempt-Self-Injury Interview (SASII) Longest follow-up: Post-intervention only |
| Cotgrove et al. (1995) [67] UK |
Inclusion: Admitted to hospital following SA/SH Exclusion: Records of the original SA were missing, or were there insufficient follow-up data (p. 572) Recruited from: Hospital/ED |
Whole sample N = 105 Mean age: 14.9 (SD: NR; Range: 12.2–16.7) Gender: 15.2% male Treatment group N = 4 Age/gender: NR Control group N = 58 Age/gender: NR |
Brief contact intervention Emergency card allowing readmission to hospital on request. Length: NA Developed by: based on Morgan et al. (1993)f Delivered by: NA |
TAU: standard follow-up care per ED site. | Random sequence generation method: Open random numbers table Allocation concealment method: Use of an open random numbers table suggests allocation could not have been concealed Ascertainment of SH repetition: Hospital and clinical notes Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Was ITT analysis undertaken: NR |
SA (dichotomous): information collected from clinic and hospital records, and contacting general practitioners and other health professionals involved with young person Longest follow-up: 12 months post-baseline |
| Diamond et al. (2010) [46]g USA |
Inclusion: i) Scored > 31 on the SIQ-JR (Reynolds, 1987)h; ii) score remained elevated 2 days later following a second screen. Exclusion: i) Current psychosis; ii) mental retardation/history of borderline intellectual functioning Recruited from: Hospital/ED and primary care practices (75.0% were recruited from primary care and 25.0% from hospitals/EDs) |
Whole sample N = 66 Mean age: 15.2 (SD: 1.62; Range 12–17) Gender: 16.7% male Treatment group N = 35 Mean age: 15.1 (SD: 1.41) Gender: 8.6% male Control group N = 31 Mean age: 15.3 (SD; 1.83) Gender: 25.8% male |
Individual family therapy plus TAU Length: Up to 15 sessions delivered over a 3-month period Developed by: study authors Delivered by: trained PhD or Masters level therapists |
Enhanced TAU: safety monitoring and facilitated referrals for treatment (incl. Individual, group, or family therapy, or case management). | Random sequence generation method: Adaptive randomization Allocation concealment method: Independent researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: No Less than 15% drop-out rate: Yes (0.0%) Was ITT analysis undertaken: Yes |
SI (continuous): SIQ-Junior (SIQ-JR) SI (dichotomous): SIQ-JR Longest follow-up: 3 months post-intervention |
| Donaldson et al. (2005) [47] USA |
Inclusion: Presented to general pediatric child psychiatric hospital after SA. Exclusion: Current psychosis Recruited from: Hospital/ED |
Whole sample N = 39 Mean age: 15.0 (SD: 1.7; Range: 12–17) Gender: 18% male Treatment group: N = NR Age/gender: NR Control group: N = NR Age/gender: NR |
Individual skills-based therapyi by trained therapists Length: 12 sessions delivered over 6 months Developed by: Study authors Delivered by: Trained therapists |
Enhanced TAU: Supportive Relationship Treatment (SRT). | Random sequence generation method: Random numbers table Allocation concealment method: NR Ascertainment of SH repetition: Interview Outcome assessor blinding: NR Less than 15% drop-out rate: No (20.5%) Was ITT analysis undertaken: No |
SI (continuous): SIQ SA (dichotomous): Structured adolescent follow-up interviews Longest follow-up: 6 months post-baseline |
| Esposito-Smythers et al. (2011) [48] USA |
Inclusion: SA in past 3 months or scored > 41 on the SIQ (Reynolds, 1987) Exclusion: Verbal IQ score < 70; ii) Psychosis; iv) Bipolar disorder; iv) Dependent on substances other than alcohol or cannabis Recruited from: MH outpatient |
Whole sample N = 40 Mean age: 15.7 (SD: 1.19; Range: 13–17) Gender: 33.3% male Treatment group N = 20 Mean age: 15.8 (SD: 0.98) Gender: 31.6% male Control group N = 20 Mean age: 15.7 (SD: 1.41) Gender: 35.3% male |
Individual cognitive behavioral therapy Length: 24 sessions delivered over 12 months Developed by: based on Donaldson et al. (2005) and Esposito Smythers et al. (2006) and adapted by study authors Delivered by: Trained therapists |
Enhanced TAU: treatment schedule and approach determined by community providers. Diagnostic evaluation report provided. Study psychiatrist assisted with medication management. Access to information and resources. | Random sequence generation method: Computer generated adaptive randomization Allocation concealment method: Unclear Ascertainment of SH repetition: Interview Outcome assessor blinding: Assessors could guess allocation due to offhand comments made by participants during interviews Less than 15% drop-out rate: No (25.0%) Was ITT analysis undertaken: Yes |
SI (continuous): SIQ SA (dichotomous): Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS) – clinician administered diagnostic interview. Longest follow-up: 6 months post-intervention |
| Green et al. (2011) [49] UK |
Inclusion: Presented to child and adolescent services with at least two episodes of SH in the past 12 months Exclusion: i) Severe low weight anorexia nervosa; ii) psychosis; iii) learning disability Recruited from: MH outpatient |
Whole sample N = 366 Mean age: NR (Range: 12–16) Gender: 11.5% male Treatment group N = 183 Mean age: NR Gender: 11.5% male Control group N = 183 Mean age: NR Gender: 11.5% male |
Group cognitive behavioral therapy Length: 6 sessions during the acute phase & as many sessions needed during the maintenance phase Developed by: based on Wood et al. (2001) Delivered by: Trained therapists |
TAU: routine care provided by local child & adolescent mental health services according to clinical judgment, excluding group interventions. | Random sequence generation method: Computer generated minimization algorithm Allocation concealment method: Independent, off-site researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: Yes (4.0%) Was ITT analysis undertaken: No |
SI (continuous): SIQ-JR SI (dichotomous): SIQ-JR SH (dichotomous): SIQ-JR Longest follow-up: 12 months post-baseline |
| Harrington et al. (1998) [50]j UK |
Inclusion: Presented to hospital with self-poisoning Exclusion: i) Other SH (e.g. cutting); ii) Severe suicidality; iii) clinician determined risk of contraindication for family treatment, e.g. psychosis, currently receiving psychiatric treatment, parent/child had a learning difficulty Recruited from: MH outpatient |
Whole sample N = 162 Mean age: 14.5 (SD: 1.15; Range: 10–16) Gender: 10.5% male Treatment group N = 85 Mean age: 14.4 (SD: 1.2) Gender: 10.6% male Control group N = 77 Mean age: 14.6 (SD: 1.1) Gender: 10.6% male |
Five sessions of family therapy plus TAU Length: NR Developed by: study authors Delivered by: 2 experienced masters'-level child psychiatric social workers |
TAU: routine psychiatric aftercare including diverse range of interventions, but no home-based family interventions. | Random sequence generation method: Shuffled envelopes Allocation concealment method: Sealed, opaque envelopes Ascertainment of SH repetition: Interview Outcome assessor blinding: Attempted but not always possible Less than 15% drop-out rate: Yes (8.0%) Was ITT analysis undertaken: No |
SI (continuous): SIQ SI (dichotomous): SIQ Suicide: NR Longest follow-up: 12 months post-baseline |
| Hassanian-Moghaddam et al. (2011) [68] Iran |
Inclusion: Presented to hospital with self-poisoning Exclusion: Psychosis Recruited from: Hospital/ED |
Whole sample N = 2133 Mean age: 24.1 (SD: 8.11; Range: NR) Gender: 33.7% male Treatment group N = 1043 Mean age: 24.7 (SD: 7.97) Gender: 33.3% male Control group N = 1070 Mean age: 24.1 (SD: 8.25) Gender: 34% male |
Brief contact intervention (Postcards from Persia) plus TAU. Length: 8 postcards mailed over 12 months Developed by: based on Carter et al. (2005)k Delivered by: NA |
TAU: follow-up care for self-poisoning in Tehran is “poor”, contact is mainly hospital- or office-based. | Random sequence generation method: Block randomization using a random numbers table Allocation concealment method: Allocation was concealed, but information on the method used was not provided Ascertainment of SH repetition: Interview Outcome assessor blinding: No Less than 15% drop-out rate: Yes (8.1%) Was ITT analysis undertaken: No |
SI (continuous): follow-up interview SI (dichotomous): follow-up interview SH (continuous): follow-up interview SH (dichotomous): follow-up interview SA (continuous): follow-up interview SA (dichotomous): follow-up interview Suicide: mortality records Longest follow-up: 12 months post-baseline |
| Hazell et al. (2009) [51] Australia |
Inclusion: Presented to hospital with > 2 episodes of SH Exclusion: i) Acute psychosis; ii) intellectual disability Recruited from: MH outpatient |
Whole sample N = 72 Mean age: 14.5 (SD: 1.1; Range 12–16) Gender: 9.7% male Treatment group N = 35 Mean age: 14.6 (SD: 1.1) Gender: 8.6% male Control group N = 37 Mean age: 14.4 (SD: 1.2) Gender: 10.8% male |
Group based cognitive behavioral therapy (Moving on from self-harm) plus TAU Length: 6 sessions over 12 months Developed by: study authors Delivered by: MH professionals |
TAU: routine care varied but generally included individual/family counseling, medication assessment, and care-coordination. | Random sequence generation method: Block randomization using a computer generated random numbers table Allocation concealment method: Independent, offsite researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: Yes (0.0%) Was ITT analysis undertaken: Mixed methods |
SI (continuous): SIQ SH (dichotomous): Linehan's Parasuicide History Interview Longest follow-up: 12 months post-baseline |
| Huey et al. (2004) [52] USA |
Inclusion: Presented to hospital with SA/SI Exclusion: Autism spectrum disorder Recruited from: Hospital/ED |
Whole sample N = 156 Mean age: 12.9 (SD: 2.1; Range 10–17) Gender: 35% male Treatment group N = Unclear Age/gender: NR Control group N = Unclear Age/gender: NR |
Multi-systematic family therapy Length: Unclear Developed by: Henggeler et al. (2002)l Delivered by: MH professionals |
Active placebo: hospitalization at youth inpatient psychiatric unit. | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of SH repetition: Interview Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Was ITT analysis undertaken: NR |
SI (dichotomous): Youth Risk Behavior Survey (YRBS) SA (dichotomous): Child Behavior Checklist (CBCL) Longest follow-up: 12 months post-intervention |
| Husain et al. (2014) [53] Pakistan |
Inclusion: Admitted to hospital following SH Exclusion: i) dementia; ii) substance misuse; iii) organic mental disorder; iv) delirium; v) alcohol and/or drug dependence; vi) schizophrenia; vii) bipolar disorder; viii) intellectual disability Recruited from: Hospital/ED |
Whole sample N = 221 Mean age: 23.1 (SD: 5.5; Range: 16–64) Gender: 31.2% male Treatment group N = 108 Mean age: 23.2 (SD: 5.8) Gender: 29.6% male Control group N = 113 Mean age: 23.1 (SD: 5.3) Gender: 32.7% |
Individual cognitive behavioral therapy (Life After Self-harm) plus TAU Length: 6 sessions over 3 months Developed by: based on Schmidt & Davidson (2004)m and adapted by study authors Delivered by: masters-level psychologists |
TAU: standard routine care provided by local services. | Random sequence generation method: Computer generated random numbers table Allocation concealment method: Independent, offsite researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: Yes (3.6% by the 6-month follow-up period; could not calculate for final follow-up) Was ITT analysis undertaken: Yes |
SI (continuous): BSSI Suicide: Not stated Longest follow-up: 6 months post-baseline |
| King et al. (2006) [54] USA |
Inclusion: i) SA or severe SI in past 3 months ii) Score of 20 or 30 on the Self-Harm subscale of the Child and Adolescent Functional Assessment Scale (Hodges, 1989)n Exclusion: i) Severe intellectual disability; ii) Psychosis Recruited from: Hospital/ED |
Whole sample N = 289 Mean age: 15.3 (SD: 1.5; Range: 12–17) Gender: 31.8% male Treatment group N = 151 Mean age: 15.4 (SD: 1.5) Gender: 31.1% male Control group N = 138 Mean age: 15.2 (SD: 1.4) Gender: 32.6% male |
Supportive intervention Youth nominated support team Version 1 plus TAU One-off brief psycho-education intervention for support team plus up to 9 contacts per week between adolescent and support team Length: 1.5 to 2 h Developed by: study authors Delivered by: MH professional |
TAU: varied, included psychotherapy, medication, alcohol/drug treatment, partial hospitalization, and community services. | Random sequence generation method: Random numbers table Allocation concealment method: Independent researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: No Less than 15% drop-out rate: Yes (18.3%) Was ITT analysis undertaken: Yes |
SI (continuous): SIQ-JR SI (dichotomous): SIQ-JR SA (dichotomous): Not stated Longest follow-up: 6 months post-baseline |
| King et al. (2009) [55] USA |
Inclusion: SA or severe SI in past 4 weeks Exclusion: NR Recruited from: Hospital/ED |
Whole sample N = 448 Mean age: 15.6 (SD: 1.31; Range: 13–17) Gender: 28.8% male Treatment group N = 223 Mean age: 15.6 (SD: 1.24) Gender: NR Control group N = 225 Mean age: 15.6 (SD: 1.37) Gender: NR |
Supportive intervention Youth nominated support team Version 2 plus TAU One-off, individual or group-based (as preferred) psycho-education session plus weekly telephone contacts. For adolescents: weekly sessions by telephone or face-to-face as preferred with support team. Length: 1 h Developed by: study authors Delivered by: MH professional |
TAU: as above. | Random sequence generation method: Block randomization using a computer generated sequence Allocation concealment method: Independent researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate for: No (23.0%) Was ITT analysis undertaken: Mixed methods |
Suicide: Not stated SA (dichotomous): Clinician administered diagnostic interview DISC-IV Mood Disorders module Longest follow-up: 12 months post-baseline |
| King et al. (2015) [56] USA |
Inclusion: Presented to ED with SI, a recent SA or positive screens for both depression plus alcohol/drug abuse Exclusion: Required referral for inpatient psychiatric hospitalization Recruited from: Hospital/ED |
Whole sample N = 49 Mean age: 17.7 (SD: 1.7; Range: 14–19) Gender: 40% male Treatment group N = 27 Age/gender: NR Control group N = 22 Age/gender: NR |
Individual motivational interview plus TAU Length: 35–45 min Developed by: study authors (based on standard motivational interviewing protocols) Delivered by: trained therapists |
Enhanced TAU: adolescents given a crisis card and written information about depression, suicide, firearm safety, and services. | Random sequence generation method: Shuffled envelopes Allocation concealment method: NR Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: Yes (6.1%) Was ITT analysis undertaken: Yes |
SI (continuous): SIQ-JR Longest follow-up: 2 months post-baseline |
| McLeavey et al. (1994) [57] Republic of Ireland |
Inclusion: Presented to ED with self-poisoning Exclusion: i) Required psychiatric inpatient/day-hospital admission; ii) Psychosis; iii) Intellectual disability; iv) organic cognitive impairment Recruited from: Hospital/ED |
Whole sample N = 39 Mean age: 24.4 (SD: 7.0; Range 15–45) Gender: 25.6% male Treatment group N = 19 Mean age: 23.6 (SD: 5.9) Gender: 21% male Control group N = 20 Mean age: 25.3 (SD: 8.1) Gender: 30% male |
Individual Interpersonal Problem-Solving Skills Training Length: Five weekly one-hour sessions for 5 weeks (with 1 additional session if necessary) Developed by: study authors Delivered by: MH professionals |
Active placebo: brief problem-oriented approach, did not involve skills training. | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of SH repetition: GP questionnaire and hospital records Outcome assessor blinding: NA Less than 15% drop-out rate: No (15.4%) Was ITT analysis undertaken: Not described |
SH (dichotomous): ED readmission Suicide: Hospital records Longest follow-up: 12 months post-intervention |
| Mehlum et al. (2016) [58]o Norway |
Inclusion: Referred to child & adolescent psychiatric outpatient clinic with a history of > 2 episodes of self-harm; 1 within the past 16 weeks Exclusion: i) Bipolar disorder (except bipolar II); ii) Schizophrenia; iii) Affective disorder; iv) Psychosis NOS; v) Intellectual disability; vi) Asperger's syndrome Recruited from: MH outpatient & Hospital/ED |
Whole sample N = 77 Mean age: 15.6 (SD: 1.6; Range: 12–18) Gender: 11.7% male Treatment group N = 39 Mean age: 15.9 (SD: 1.4) Gender: 12.8% male Control group N = 38 Mean age: 15.3 (SD: 1.6) Gender: 20.5% male |
Individual and group Dialectical Behavior Therapy Length: 19 weeks – One 1-hour weekly session of individual therapy; one 2-hour weekly session of multifamily skills training; plus family therapy & telephone coaching as needed. Developed by: Miller et al. (2007) Delivered by: MH professionals |
Enhanced TAU: standard care enhanced for the purpose of the trial by requiring that therapists agree to provide at least 1 weekly treatment session per patient. | Random sequence generation method: Block randomization using a computer generated sequence Allocation concealment method: Independent researcher Ascertainment of SH repetition: Interview supplemented with hospital records Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (2.6% by the one-year follow-up period) Was ITT analysis undertaken: Yes |
SI (continuous): SIQ-JR SH (continuous): ED readmission and self-report SH (dichotomous): ED readmission and self-report Suicide: Mortality records Longest follow-up: 12 months post-intervention |
| Ougrin et al. (2011) [69]; (2013) [39] UK |
Inclusion: Referred to ED following SH Exclusion: i) Psychosis; ii) Intoxication; iii) Learning disability; iv) Required inpatient admission Recruited from: Hospital/ED |
Whole sample N = 70 Mean age: 15.5 (SD: 1.3; Range: 12–18) Gender: 20% male Treatment group N = 35 Mean age: 15.6 (SD: 1.5) Gender: 20% male Control group N = 35 Mean age: 15.5 (SD: 1.2) Gender: 20% male |
Brief contact intervention Comprised psychosocial history & risk assessment plus brief intervention Length: 1 h plus 30 min Developed by: study authors Delivered by: MH professionals |
TAU: standard psychosocial history and risk assessment, report sent to relevant community team | Random sequence generation method: Block randomization using a computer generated sequence Allocation concealment method: Independent researcher Ascertainment of SH repetition: Interview supplemented with clinical records Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (1.4% by the two-year follow-up period) Was ITT analysis undertaken: Yes |
SH (dichotomous): ED readmission Longest follow-up: 24 months post-baseline |
| Pineda & Dadds, (2013) [59] Australia |
Inclusion: Presented to ED with either SI, SA or SH within the 2 months prior to presentation Exclusion: 1) Overdose of recreational drugs; ii) Intellectual disability Recruited from: ED |
Whole sample N = 48 Mean age: 15.1 (SD: 1.2; Range: 12–17) Gender: 25% male Treatment group N = 24 Mean age: 15.0 (SD: 1.31) Gender: 27.3% male Control group N = 24 Mean age: 15.28 (SD: 1.18) Gender: 22.2% male |
Strengths-based family education program plus TAU: Resourceful Adolescent Parent Program (RAP-P) Length: Four 2-hour sessions delivered in a single family format either once a week or once every two weeks. A total of five, 2-hour sessions were provided over up to 2.5 months. Developed by: based on Shochet et al. (1997)p and adapted by study authors Delivered by: primary author |
TAU: routine care (included any intervention deemed necessary by the treating team other than RAP-P). | Random sequence generation method: Random numbers table Allocation concealment method: Independent researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: No (16.7%) Was ITT analysis undertaken: Yes |
SI (continuous): ASQ-R Longest follow-up: 6 months post-baseline |
| Power et al. (2003) [60] Australia |
Inclusion: Referred to a specialist first episode psychosis clinic with SI or SA Exclusion: NR Recruited from: MH outpatient |
Whole sample N = 56 Age/gender: NR Treatment group N = 31 Age/gender: NR Control group N = 25 Age/gender: NR |
Individual cognitive oriented therapy (Lifespan) plus TAU Length: Eight to ten sessions over 10 weeks. Developed by: study authors Delivered by: MH professionals |
TAU: standard clinical care. | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of SH repetition: Clinical records Outcome assessor blinding: NA Less than 15% drop-out rate: No (37.5%) Was ITT analysis undertaken: NR |
Suicide: Not stated Longest follow-up: Post-intervention only |
| Robinson et al. (2012) [70] Australia |
Inclusion: Referred but not accepted to a specialist outpatient adolescent MH service with a history of SI, SA or SH Exclusion: i) Intellectual disability; ii) Known organic cause for presentation Recruited from: MH outpatient |
Whole sample N = 164 Mean age: 18.6 (SD: NR; Range: 15–24) Gender: 35.4% male Treatment group N = 81 Mean age: NR Gender: 39.5% male Control group N = 83 Mean age: NR Gender: 31.3% male |
Brief contact intervention plus TAU – monthly postcards Length: Twelve postcards over 12 months Developed by: study authors (based on existing BIC methods) Delivered by: NA |
TAU: treatment or support already being received; e.g., from school counselor, GP, psychologist. | Random sequence generation method: Block randomization using a computer generated sequence Allocation concealment method: Independent researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: No (52.7%) Was ITT analysis undertaken: No. However, sensitivity analyses were undertaken which suggested that ITT results with data imputed for all missing observations not materially different to per protocol analysis |
SI (continuous): BSSI SI (dichotomous): BSSI SH (dichotomous): Suicide Behavior Questionnaire-14 item version (SBQ-14) SA (dichotomous): SBQ-14 Longest follow-up: 6 months post-intervention |
| Rossouw & Fonagy, (2012) [61] UK |
Inclusion: Presented to ED or referred to community MH services with SH Exclusion: i) Presentation the result of excessive use of recreational drugs; ii) Psychosis; iii) Severe learning disability; iv) Developmental disorder; v) Eating disorder; vi) Dependence on alcohol/drugs Recruited from: Hospital/ED and MH outpatient |
Whole sample N = 80 Mean age: 14.7 (SD: 1.25; Range: 12–17) Gender: 15% male Treatment group N = 40 Mean age: 15.4 (SD: 1.3) Gender: 17.5% male Control group N = 40 Mean age: 14.8 (SD: 1.2) Gender: 12.5% male |
Mentalization therapy: comprised weekly individual sessions plus monthly family therapy. Length: 1 year Developed by: study authors Delivered by: MH professionals. |
TAU: routine care provided by community-based adolescent mental health services. Mainly individual therapeutic intervention, combined individual and family therapy, or psychiatric review. | Random sequence generation method: Minimization algorithm Allocation concealment method: Independent, offsite researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: Yes (11.2%) Was ITT analysis undertaken: Yes |
Suicide: Not stated SH (continuous): Risk-Taking and Self-Harm Inventory (RTSHI) SH (dichotomous): RTSHI Longest follow-up: Post-intervention only |
| Rudd et al. (1996) [40]q USA |
Inclusion: Referred to outpatient mental health clinics, an inpatient service or an ED with SA, SI Exclusion: i) Substance abuse/dependence ii) Psychosis/thought disorder; iii) Personality disorder Recruited from: Hospital/ED and MH outpatient NB: Setting comprised 1y medical center |
Whole sample N = 264 Mean age: 22.2 (SD: 2.3; Range: NR) Gender: 82.2% male Treatment group N = 143 Mean age: NR Gender: 77.6% male Control group N = 121 Mean age: NR Gender: 87.6% male |
Group-based problem-solving and social competence training Length: 9 h a day for two weeks Developed by: study authors Delivered by: MH professionals |
TAU: combination of inpatient and outpatient care. | Random sequence generation method: Sequential randomization Allocation concealment method: NR Ascertainment of SH repetition: Interview Outcome assessor blinding: NR Less than 15% drop-out rate: No (73.1% by the 12 month follow-up period) Was ITT analysis undertaken: Unclear |
SI (continuous): Modified Scale for Suicidal Ideation (MSSI)r Longest follow-up: Post-intervention only |
| Slee et al. (2008) [62]s The Netherlands |
Inclusion: Presented to an outpatient MH service with recent SH Exclusion: Psychiatric disorder requiring inpatient treatment Recruited from: MH outpatient |
Whole sample N = 82 Mean age: 24.6 (SD: 5.4; Range: 15–35) Gender: 6.1% male Treatment group N = 40 Mean age: 23.9 (SD: 6.4) Gender: 2.5% male Control group N = 42 Mean age: 25.4 (SD: 4.5) Gender: 9.5% male |
12 out-patient, individual cognitive behavioral therapy sessions plus TAU Length: weekly sessions for up to 5.5 months Developed by: NR (but based on standard CBT protocol) Delivered by: MH professionals |
TAU: participants' choice, three forms: psychotropic medication, psychotherapy and psychiatric hospitalizations | Random sequence generation method: Computer generated random numbers table Allocation concealment method: Independent, offsite researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: NR. Less than 15% drop-out rate: No (21.0%) Was ITT analysis undertaken: Mixed methods |
SH (continuous): Structured clinical interview SH (dichotomous): Structured clinical interview Longest follow-up: 9 months post-baseline |
| Spirito et al. (2002) [71] USA |
Inclusion: Presented to an ED/pediatric hospital with SA Exclusion: NR Recruited from: Hospital/ED |
Whole sample N = 63 Mean age: 15.0 (1.4; Range: 12–18) Gender: 9.5% male Treatment group N = 29 Mean age: NR Gender: 13.8% male Control group N = 34 Mean age: NR Gender: 5.9% male |
Brief contact intervention Individual compliance enhancement intervention plus TAU Length: one hour Developed by: study authors Delivered by: post-doctoral psychology fellows |
TAU: standard disposition planning. | Random sequence generation method: Random numbers table Allocation concealment method: NR Ascertainment of SH repetition: Interview Outcome assessor blinding: NR Less than 15% drop-out rate: No (17.1%) Was ITT analysis undertaken: No |
SH (dichotomous): Structured interview Suicide: Not stated Longest follow-up: 3 months post-baseline |
| Spirito et al. (2015) [72] USA |
Inclusion: Resided in a specific catchment plus current or past ‘suicidality’ Exclusion: NR Recruited from: MH outpatient and Hospital/ED |
Whole sample N = 24 Mean age: 14.3 (SD: 1.7; Range: 11–17) Gender: 16.7% male Treatment group N = 16 Mean age: 14.7 (SD: 1.8) Gender: 12.5% male Control group N = 8 Mean age: 14.0 (SD: 1.7) Gender: 25% male |
Parent-Adolescent-cognitive behavioral therapy Individual CBT (for the parents plus adolescents) and family sessions Length: 12 sessions over 12 weeks Developed by: based on protocols used in prior clinical trials with depressed Adolescents. Delivered by: masters and PhD level clinicians |
Active placebo: adolescent-only CBT. | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of DSH repetition: Interview Outcome assessor blinding: NR Less than 15% drop-out rate: Unclear Was ITT analysis undertaken: Yes |
SI (continuous): BSSI-A Longest follow-up: 12 months post-baseline Not included in MA2 |
| Wharff et al. (2017) [63] USA |
Inclusion: i) presentation to ED with “suicidality” or suicide attempt; ii) presence of consenting parent or legal guardian Exclusion: i) not fluent in English; ii) Not medically stable, including intoxication; iii) cognitive ‘limitations’ preventing completion of research instruments; iv) active psychosis; v) required physical or medical restraint in ED Recruited from: Hospital/ED |
Whole sample N = 142 Mean age: 15.5 (SD: 1.4) Gender: 28% male Treatment group N = 68 Mean age: 15.4 (SD: 1.3) Gender: 26% male Control group N = 71 Mean age: 15.6 (SD: 1.5) Gender: 30% male |
Family Based Crisis Intervention (based on cognitive behavioral therapy) plus TAU; an emergency crisis intervention Length: 60 to 90-min Developed by: study authors Delivered by: master's level psychiatric social workers |
TAU: standard psychiatric Evaluation and clinical/discharge recommendations. |
Random sequence generation method: NR Allocation concealment method: NR Ascertainment of DSH repetition: NA Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (19.0%) Was ITT analysis undertaken: No |
SI (continuous): Reasons for Living Inventory for Adolescents (RFL-A)t Longest follow-up: 1 month post-intervention |
| Wood et al. (2001) [64] UK |
Inclusion: i) Referred to child & adolescent MH service following SH; ii) Engaged in SH on at least one other occasion during the past year Exclusion: i) ‘Too suicidal’ for ambulatory care; ii) psychosis; iii) learning ‘problems’ Recruited from: MH outpatient |
Whole sample N = 63 Mean age: 14.3 (SD: 1.6; Range: 12–16) Gender: 22.2% male Treatment group N = 32 Mean age: 14.2 (SD: 1.1) Gender: 21.9% male Control group N = 31 Mean age: 14.3 (SD: 2.1) Gender: 25.8% male |
Combined group-based psychotherapy plus TAU. Comprised aspects of cognitive behavioral therapy, dialectical behavioral therapy and psychodynamic psychotherapy. Length: “until the young person feels ready to leave” (p. 1247). Developed by: study authors Delivered by: MH professionals |
TAU: variety of interventions delivered by community psychiatric nurses & psychologists. Included family sessions, nonspecific counseling. Psychotropic medication (where indicated). | Random sequence generation method: Random numbers table Allocation concealment method: Independent, offsite researcher Ascertainment of SH repetition: Interview Outcome assessor blinding: Yes Less than 15% drop-out rate: Yes (3.1%) Was ITT analysis undertaken: Yes |
SH (continuous): ED readmission (assessed via interview) SH (dichotomous): ED readmission Suicide: Not stated Longest follow-up: 7 months post-randomization |
Notes: ED = Emergency Department; ITT = intention-to-treat; IQR = Interquartile Range; MA = meta-analysis; MH = mental health; NR = not reported; TAU = treatment as usual; SA = suicide attempt; SD = standard deviation; SH = self-harm; SI = suicidal ideation; SRB = suicide-related behavior.
Stanley B, et al. Cognitive behavioral therapy for suicide prevention (CBTSP): treatment model, feasibility and acceptability. J Am Acad Child Adolesc Psychiatry 2009; 48 [10]:1005–13.
Rotheram-Borus MJ, et al. Enhancing treatment adherence with aspecialized emergency room program for adolescent suicide attempters. J Am Acad Child Adolesc Psychiatry 1996; 35:654–663.
Linehan MM, et al. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry 1991; 48:1060–1064.
Linehan MM. Skills training manual for treating borderline personality disorder. New York: Guilford Press, 1993.
Miller, AL, et al. Dialectical behavior therapy with suicidal adolescents. New York: Guilford Press, 2007.
Morgan HG et al. Secondary prevention of non-fatal deliberate self-harm. The green card study. BJP 1993; 163: 111–112.
Excluded secondary publications: Diamond G, et al. Sexual trauma history does not moderate treatment outcome in Attachment-Based Family Therapy (ABFT) for adolescents with suicide ideation. J Fam Psychol 2012; 26(4): 595-605; Shpigel MS, et al. Changes in parenting behaviors, attachment, depressive symptoms, and suicidal ideation in attachment-based family therapy for depressive and suicidal adolescents. J Marital Fam Ther 2012; 38(Suppl 1): 271-83.
Reynolds WM. Suicidal Ideation Questionnaire: Professional Manual. Psychological Assessment Resources Inc., 1987.
Classified as CBT in the meta-analysis.
Excluded secondary publication: Harrington R, et al. Deliberate self-poisoning in adolescence: why does a brief family intervention work in some cases and not others? J Adolesc 2000; 23(1): 13–20.
Carter GL, et al. Postcards from the EDge project: randomised controlled trial of an intervention using postcards to reduce repetition of hospital treated deliberate self poisoning. BMJ 2005; 331: 805–7.
Henggeler S, et al. Serious Emotional Disturbance in Children and Adolescents: Multisystemic Therapy. New York: Guilford Press, 2002.
Schmidt U, Davidson KM. Life After Self-Harm: A Guide to the Future. Routledge, 2004.
Hodges K. Child and Adolescent Functional Assessment Scale. Ypsilanti: Eastern Michigan University, 1989.
Excluded secondary publication: Mehlum L, et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. J Am Acad Child Adolesc Psychiatry 2014; 53(10): 1082–91.
Shochet I, et al. Resourceful Adolescent Parent Program: group leader's manual. Brisbane, Australia: Griffith University, 1997.
Excluded secondary publication: Wingate LR, et al. (Comparison of compensation and capitalization models when treating suicidality in young adults. J Consult Clin Psychol, 2005. 73(4): 756–62.
Miller I, et al. (1986). The modified scale for suicidal ideation: Reliability and validity. J Consult Clin Psychol, 54, 724–725.
Excluded secondary publications: Slee N, et al. Emotion regulation as mediator of treatment outcome in therapy for deliberate self-harm. Clin Psychol Psychother 2008; 15(4): 205–16.; Spinhoven P, et al. Childhood sexual abuse differentially predicts outcome of cognitive-behavioral therapy for deliberate self-harm. J Nerv Ment Dis 2009; 197(6): 455–7.
Osman A, et al. The Reasons for Living Inventory for Adolescents (RFL-A): development and psychometric properties. J Clin Psychol 1998; 54: 1063–1078.
Table 2.
Study characteristics: Non-randomized controlled trials conducted in clinical settings (N = 19).
| Study; country | Study design; level of evidence | Target population | Participants | Intervention description | Comparison condition | Risk of bias | Suicide related outcome(s) assessed; Longest follow-up | Results | Interpretation |
|---|---|---|---|---|---|---|---|---|---|
| Asarnow et al. (2015) [73] USA |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: SA in past 3 months; stable living situation Exclusion: No contact information available for follow-up; psychosis; substance abuse/dependence; not English-speaking; no family to participate Recruited from: Hospital/ED |
N = 35 Mean age: 14.89 (SD: 1.6; Range: 11–18) Gender: 14% male |
Suicide-specific family-based cognitive behavioral therapy comprising psycho-education plus individual therapy. The Safe Alternatives for Teens & Youths program (SAFETY Program) Length: Up to 20 sessions over 12 weeks, incl: 1 × family session then individual (16 x youth-only & parent-only), then up to 16 × family sessions Developed by: Henggeler (2002) Delivered by: a MH professional |
NA | Adequately powered: NR Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (11.4%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: Harkavy-Asnis Suicide Survey, passive suicidal ideation subscale. SA: Harkavy-Asnis Suicide Survey, suicide attempt subscale. SRB: Harkavy-Asnis Suicide Survey, active suicidal behavior and ideation subscale. Longest follow-up: 6 months post-intervention |
SI: Pre-test Mean (SD): 12.69 (9.79) Post-test Mean (SD): 9.19 (10.14) SA: Pre-test Mean (SD): 0.89 (1.86) Post-test Mean (SD): 0.13 (0.34) SRB: Pre-test Mean (SD): 3.71 (4.42) Post-test Mean (SD): 1.81 (2.69) |
There was evidence of a significant reduction in SI (t-test = 2.56, p = 0.016, Cohen's d = 0.39), SA (t-test = 2.42, p = 0.019), and SRB (t-test = 2.63, p = 0.013) between baseline and three-month follow-up. Four young people either re-attempted suicide and/or re-engaged in NSSI during the treatment period (significance test not reported). |
| Brent et al. (2009) [91] USA |
Study design: Non-randomized, experimental trial Level of evidence: III-2 |
Inclusion: Had major unipolar mood disorder & SA in past 90 days; living with a parent or guardian who could participate in treatment Exclusion: Substance dependence, bipolar disorder, psychosis, or developmental disorder Recruited from: Unclear |
Whole sample N = 124 Mean age: 15.8 (SD: 1.5; Range: 12–18) Gender: 22.6% male Treatment group (1) N = 18 Age/gender: NR Treatment group (2) N = 93 Age/gender: NR Control group N = NR Age/gender: NR |
Suicide-specific individual cognitive behavioral therapy with some elements of dialectical behavior therapy. Length: between 12 and 16 weekly sessions. Developed by: Study authors Delivered by: Unclear |
Medication management or combined medication & CBT | Adequately powered: No Outcome assessor blinding: Yes Less than 15% drop-out rate: No (33.1%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SA: Columbia Classification Algorithm of Suicide Assessment SRB: Columbia Classification Algorithm of Suicide Assessment. Suicide: not described. Longest follow-up: Post-intervention only |
SA: NR SRB: NR Suicide: NR |
There was evidence of an increase in SRB between baseline and six-month follow-up in the combination (i.e., psycho- and pharmacotherapy group) compared to either condition alone (22/93 vs. 2/31; Fisher's exact test p = < 0.04). There was one completed suicide after the six-month follow-up, however, it is unclear to which treatment group this young person had been allocated. |
| Courtney & Flament, (2015) [74] Canada |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: BPD features with SI OR SH in past 4 months Exclusion: psychosis; developmental disorder Recruited from: MH outpatient |
N = 61 Mean age: 16.5 (SD: 0.8; Range: 15–18) Gender: 7% male |
Dialectical behavior therapy adapted for adolescents in tertiary care. A-DBT-A Length: 1 x weekly group-based and 1 × weekly individual sessions over 14-weeks (session duration not stated). Developed by: Based on Miller et al. (2006) but adapted by the study authors Delivered by: a MH professional |
NA | Adequately powered: NR Outcome assessor blinding: NA Less than 15% drop-out rate: No (49.2%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: Suicidal Ideation Questionnaire (SIQ). SRB: Medical/clinical records. Suicide: NR Longest follow-up: Post-intervention only |
SI: Pre-test Median (IQR): 131.0 (92.0 to 144.0). Post-test Median (IQR): 77.0 (48.5 to 121.0). SRB: NR Suicide: NR |
There was evidence of a significant reduction in SI (t-test = 4.96, p < 0.001, Cohen's d = 0.89) between baseline and the 15-week post-intervention assessment. There was also evidence of a significant reduction in the proportion of young people engaging in SRB over this period (36/42 vs. 16/42, McNemar test p < 0.001). There were no reports of completed suicides. |
| Cwik et al. (2016) [82] USA |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: Apaches with SA in past 90 days Exclusion: none Recruited from: Community suicide surveillance system |
N = 13 Mean age: 14.3 (SD: 2.2) Gender: 8% male |
New Hope, a brief psycho-education intervention for American Indian adolescents Length: 1–2 visits (2–4 h total). Developed by: Study authors Delivered by: Community Mental Health Workers |
NA | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: No (15.4%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: SIQ Longest follow-up: 3 months Post-intervention |
SI: N (%) scoring above clinical cut-off: Pre-test: 7/11 (64%) Post-test: 1/10 (10%) |
The number of participants who scored above the clinical cut-off for the SIQ seemed to decrease over the follow-up period. |
| Diamond et al. (2013) [83]a USA |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: LGB discharged from hospital with SI (admitted for SI or SA) Exclusion: Psychosis or ID Recruited from: Hospital/ED |
N = 10 Mean age: 15.1 (SD: 1.37; Range: 14–18) Gender: 20% male |
Attachment-based family therapy adapted for use with suicidal LGB youth. ABFT-LGB Length: 12 x weekly sessions (range = 8–16). Sessions lasted for 60-min & sessions 3–5 were for parents only. Developed by: Study authors Delivered by: a MH professional |
NA | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: SIQ-Junior (SIQ-JR) Longest follow-up: Post-intervention only |
SI: Pre-test Mean (SD): 51.00 (13.00) Post-test Mean (SD): 6.88 (7.34) |
There was evidence of a significant reduction in SI between baseline and the 3-month post-intervention assessment (F-test = 18.78, p = 0.001, Cohen's d = 0.21). |
| Duarte-Velez et al. (2016) [75] Puerto Rico |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: Admitted to ED with SI or SA, hospitalized, stabilized and referred to outpatient; legal guardian. Exclusion: Psychosis; developmental disorder; ID; already receiving psychotherapy; involvement in a legal procedure that would require psychological care mandated by the judicial system Recruited from: Hospital/ED |
N = 11 Mean age: 15.36 (SD-NR; Range: 13–17) Gender: 45% male |
Cognitive behavioral therapy adapted for Puerto Rican adolescents with suicidal behavior. Length: Weekly individual sessions lasting for 1 h & delivered over 6 months. Plus 60–120 min family sessions & follow-up bi-weekly as necessary. Phone calls & case management as needed. Developed by: Study authors Delivered by: a MH professional |
NA | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: No (27.3%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: SIQ-JR Longest follow-up: Post-intervention |
SI: Pre-test Mean (SD): 27.20 (NR) Post-test Mean (SD): 16.00 (NR) |
There was evidence of a reduction in SI between baseline and the six month post-intervention assessment (significance test not reported). |
| Esposito-Smythers et al. (2006) [76] USA |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: Admitted to inpatient unit for SI/SA with co-occurring alcohol abuse/dependence Exclusion: ID, DSM-IV dependence on substances other than alcohol or cannabis. Recruited from: Hospital/ED |
N = 6 Mean age: 15 (SD: 1; Range: 14–16) Gender: 17% male |
Integrated cognitive behavioral therapy for adolescents with co-occurring alcohol use disorder and suicidality. Length: Acute phase: Weekly sessions lasting 1 h & delivered over 6 months (plus maintenance & booster phases). Developed by: Study authors, incorporating modifications of Monti's (2002)b coping skills training package for youth with co-occurring alcohol use disorder Delivered by: a MH professional |
NA | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: No (16.7%) Use of statistical testing to measure change from pre-test to post-test: No |
SI: SIQ SRB: NR Longest follow-up: 12 months post-intervention |
SI: Pre-test Mean (SD): 80.80 (NR) Post-test Mean (SD): 32.80 (NR) |
There was evidence of a reduction in SI between baseline and the 12 month post-intervention assessment (significance test not reported). Two young people re-engaged in SRB during this period (significance test not reported). |
| Geddes et al. (2013) [77] Australia |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: At least 3 BPD features & SI/SH in past 12 months Exclusion: Primary diagnosis of psychosis or substance abuse; ID Recruited from: MH Outpatient |
N = 6 Mean age: 15.1 (SD-NR; Range 14–15) Gender: 0% male |
Dialectical behavior therapy modified for adolescents: Life Surfing Length: 1–2 weekly sessions lasting for 1 h & delivered over 26 weeks. Plus a weekly 2 h family skills group delivered over an 18-week period. Developed by: Based on Swales (2000)c but adapted by the study authors. Delivered by: NR |
NA | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: No (16.7% by the three-month follow-up period) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: NR SBR: Self-Harm/Suicidal Thoughts Questionnaire: Parent and Adolescent Versions. SA: NR Longest follow-up: 12 months post-baseline |
SA: NR SRB: NR |
There was evidence of a reduction in the proportion of young people reporting SI between baseline and the 18-week post-intervention assessment (significance test not reported). By the 18-week post-intervention assessment, 5 of the 6 young people had had no further episodes of SRB, whilst the sixth reported a 50% reduction in SRB frequency (significance tests not provided). By the 12 month follow-up period, no young person had a further episode of SA (significance test not reported). |
| Gutstein & Rudd (1990) [78] USA |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: Referred to a guidance center following a near-lethal SA/persistent suicide threats (severe risk) Exclusion: NA Recruited from: Hospital/Ed, MH outpatient & community |
N = 47 Mean age: 14.4 (SD-NR; Range: 7–19) Gender: 47% male |
A suicide-specific intensive group crisis intervention: Systemic Crisis Intervention Program Length: Two × 4-hour group meetings over a 2–6 week period. Developed by: Study authors Delivered by: NR |
NA | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Use of statistical testing to measure change from pre-test to post-test: No |
SA: Parental report Longest follow-up: Post-intervention only |
SA: NR | There was evidence of a reduction in the proportion of young people engaging in SA between baseline and the 18 month follow-up assessment (significance test not reported). |
| James et al. (2011) [79] UK |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: Living in ‘out of home care’ & engaged in SH for > 6 months Exclusion: diagnosis of schizophrenia, bipolar disorder, autism spectrum disorder; Moderate–severe mental impairment Recruited from: MH outpatient service |
N = 25 Mean age: 15.5 SD: 1.5; Range: 13–17 Gender: 12% male |
Dialectical behavior therapy comprising a skills training group, individual therapy, telephone support, support for schools/carers & outreach. Length: 1-hour individual sessions plus 2-hour group sessions delivered weekly over 12 months. Developed by: Based on Linehan (1993) and Rathus and Miller (2002)d but adapted by the study authors. Delivered by: a MH professional |
NA | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: No (28.0%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SRB: Clinical interview Longest follow-up: Post-intervention only |
SRB: NR | There was evidence of a reduction in the proportion of young people engaging in SRB between baseline and the 12 week post-intervention period (14/18 young people had ceased engaging in SRB altogether) (significance tests not provided). There was also evidence of a reduction in the frequency of these SRB episodes over this period (significance tests not provided). |
| James et al. (2015) [80] UK |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: SH in past 12 months Exclusion: NR Recruited from: MH outpatient & community |
N = 154 Mean age: 14.9 (SD: 1.3; Range: 12–18) Gender: 14.8% male |
Dialectical behavior therapy for adolescents Length: Three-hour group sessions delivered twice weekly, plus weekly individual or family sessions, 30–60 min in duration. Delivered over 16 weeks. Developed by: Based on Miller (2006) Delivered by: MH professional |
NA | Adequately powered: NR Outcome assessor blinding: NA Less than 15% drop-out rate: No (30.3%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SRB: Youth Outcome Questionnaire, Self-Report, version 2.0, item 21 Longest follow-up: Post-intervention only |
SRB: Pre-test Mean (SD): 2.06 (1.68). Post-test Mean (SD): 0.65 (0.98). |
There was evidence of a significant reduction in SRB between baseline and the 16-week post-intervention assessment (F-test = 68.83, p < 0.001, η2 = 0.42). |
| Katz et al. (2004) [84] Canada |
Study design: Non-randomized, experimental trial Level of evidence: III-2 |
Inclusion: Admitted to Inpatient unit for SA or SI Exclusion: ID, severe learning disability, psychosis, bipolar disorder Recruited from: Hospital/ED |
Whole sample N = 62 Mean age: 15.4 (Range: 14–17) Gender: 16.1% male Treatment group N = 31 Age/gender: NR Control group N = 31 Age/gender: NR |
Individual & group dialectical behavior therapy Length: 10 daily group sessions plus 4 individual sessions delivered over 2 weeks Developed by: Based on Miller (1997)e but adapted by the study authors Delivered by: MH professional |
TAU: daily psychodynamic psychotherapy group, weekly individual therapy, and psychodynamically-oriented milieu. | Adequately powered: Study authors provide power calculations, however, study unlikely to be adequately powered for SRB. Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (10.0%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: SIQ-JR Suicide: NR Longest follow-up: 1 year post-intervention |
SI: Post-intervention Intervention mean (SD): 40.90 (24.73) Control mean (SD): 37.97 (24.56) 12 months: Intervention mean (SD): 18.15 (12.52) Control mean (SD): 19.25 (17.89) Suicide: NR |
There was no evidence of a reduction in SI between the intervention and control groups at post-intervention (40.90 ± 24.73 vs. 37.97 ± 24.56) and at the 12 month follow-up assessment (18.15 ± 12.52 vs. 19.35 ± 17.89). There were no completed suicides in either group by the 12 month follow-up assessment (significance test not reported). |
| King et al. (2003) [81] Australia |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: Called helpline and reported SI Exclusion: None Recruited from: Telephone helpline |
N = 101 Age: NR Gender: Unclear |
Kids helpline Single crisis phone call Length: Mean duration 40 min; range 10–120 min Developed by: Charitable organization Delivered by: trained volunteers |
NA | Adequately powered: NR Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: Idiosyncratic, binary-coded instrument adapted from items from the Mini International Neuropsychiatric Interview. Longest follow-up: Post-intervention only |
SI: Pre-test Mean (SD): 6.30 (2.22). Post-test Mean (SD): 3.01 (2.43). |
There was evidence of a significant reduction in SI from the beginning to the end of the call (average call duration 40 min) (t-test = 12.66, p < 0.005, η2 = 0.62). |
| Law et al. (2016) [85] Hong Kong |
Study design: Non-randomized, experimental trial Level of evidence: III-2 |
Inclusion: Admitted to the ED with SH Exclusion: any DSM IV-TR Axis II disorder; psychosis; bipolar disorder Recruited from: Hospital/ED |
Whole sample N = 78 Mean age: NR Range: 18–34 Gender: NR Treatment group N = 40 Mean age: 24.7 (SD: 5.4) Gender: 18.4% male Control group N = 38 Mean age: 26.0 (SD: 6.2) Gender: 11.1% male |
Brief contact intervention: Volunteer mentorship Length: ≥ 2 contacts per month over 9 months. Developed by: Study authors Delivered by: trained volunteers supervised by psychiatrists, psychologists, and social workers |
TAU (not described) | Adequately powered: Study authors provide power calculations, however, study unlikely to be adequately powered for SRB Outcome assessor blinding: NA Less than 15% drop-out rate: No (67.6%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: SIQ SRB: Hospital records Longest follow-up: Post-intervention only |
SI: Post-intervention: Intervention mean (SD): 20.70 (3.00) Control mean (SD): 15.60 (6.50) SRB: NR |
There was no evidence of a significant reduction in SI between the intervention and control groups at post-intervention (20.70 ± 3.00 vs. 15.60 ± 6.50, β = 2.31, SE = 2.52, p > 0.05).There was also no evidence of a reduction in SRB between the intervention and control groups by this time point (4/38 vs. 4/36) (significance test not provided). |
| Oldershaw et al. (2012) [86] UK |
Study design: Retrospective cohort study Level of evidence: III-2 |
Inclusion: Reported history of SH Exclusion: ID; serious head injury; used medication with sedatory side effects; primary diagnosis not depression or SH. Recruited from: MH outpatient, schools & personal contacts |
Whole sample N = 33 Mean age: NR (SD: NR; Range: 12–18) Gender: NR Treatment group N = 24 Age: NR Gender: 4.2% male Control N = 9 Age: NR Gender: 22.2% male |
Standalone, formulation based, and modularized cognitive behavioral therapy with core and optional modules, depending on clinical need. Length: 12 sessions Developed by: Study authors Delivered by: MH professional |
No treatment: Participants either declined or did not pursue treatment | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SRB: Idiosyncratic, binary-coded instrument Longest follow-up: 5 months post-baseline |
SRB: NR | There was evidence of a significant reduction in the proportion of participants engaging in SRB between the intervention and control groups at post-intervention (14/24 vs. 3/9). There was also evidence of a significant reduction in the frequency of SRB by this time point (Z = − 3.20, p < 0.001). |
| Perera Ramani & Kathriarachchi, (2011) [87] Sri Lanka |
Study design: Non-randomized, experimental trial Level of evidence: III-2 |
Inclusion: Admitted to hospital for SA; categorized as medium- and low-intent Exclusion: Diagnosed with major psychiatric disorder Recruited from: Hospital/ED |
Whole sample N = 124 Mean age: NR (SD: NR; Range: 15–24) Gender: Unclear Treatment group N = 62 Age/Gender: NR Control group N = 62 Age/Gender: NR |
Individual problem solving therapy Length: 4 sessions delivered over 1 month Developed by: Based on Palmer (1995)f Delivered by: MH professional |
TAU: routine care (referral to a medical officer, psychiatric referral, referrals to other agencies). | Adequately powered: No Outcome assessor blinding: NR Less than 15% drop-out rate: No (18.5%) Use of statistical testing to measure change from pre-test to post-test: No |
SA: NR Longest follow-up: 6 months post-baseline |
SA: NR | There was a reduction in the proportion of participants engaging in SA between the intervention and control groups at post-intervention (0/55 vs. 2/46) (significance test not reported). |
| Rathus & Miller, (2002) [88] USA |
Study design: Non-randomized, experimental trial Level of evidence: III-2 |
Inclusion: SA or SI in past 4 months AND Borderline Personality Disorder features Exclusion: NR Recruited from: MH outpatient |
Whole sample N = 111 Age: NR Gender: 21.6% male Treatment group N = 29 Mean age: 16.1 (SD: 1.2; Range: NR) Gender: 7% male Control group N = 82 Mean age: 15.0 (SD: 1.7; Range: NR) Gender: 27% male |
Dialectical behavior therapy adapted for adolescents. Length: Two sessions per week for 12 weeks Developed by: Based on Linehan (1993) but adapted for adolescents by study authors Delivered by: MH professional |
Active placebo: Short term psychodynamic or supportive approach aimed at resolving acute problems. | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: Beck Scale for Suicidal Ideation (BSSI) SA: Self-report Longest follow-up: 3 months post-intervention |
SI: Pre-test Mean (SD): 9.80 (5.30) Post-test Mean (SD): 3.80 (4.60) SA: NR |
There was a significant reduction in SI between baseline and the 12-week post-intervention assessment (t-test = 2.65, p = 0.26). There was also evidence of a reduction in SA between the intervention and control groups by the 12-week post-intervention assessment (1/29 vs. 7/82). |
| Rotheram-Borus et al. (1996) [89]; (2000) [35] USA |
Study design: Historical controlled study Level of evidence: III-3 |
Inclusion: Presented to ED with SA & hospitalized for < 1 week Exclusion: Low IQ, no parent or family Recruited from: Hospital/ED |
Whole sample N = 140 Mean age: 15.0 (SD: NR; Range: 12–18) Gender: 0% male Treatment group N = 65 Mean age: 15.0 (SD: 1.4) Control group N = 75 Mean age: 15.3 (SD: 1.6) |
Specialized Emergency Room Program: Comprised 1 family psychotherapy session plus psycho-education video. Length: Session = NR; video = 20 min Developed by: Study authors Delivered by: MH professional |
TAU: evaluation to determine if hospitalization required & referral to outpatient therapy. | Adequately powered: Likely to be adequately powered for SI. Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: Harkavy-Asnis Suicide Survey, passive suicidal ideation subscale SA: Self- and parental-report in conjunction with hospital records Longest follow-up: 18 months post-suicide attempt |
SI: Post-intervention: Intervention mean (SD): 1.40 (2.38) Control mean (SD): 2.10 (2.86) SA: 18-month follow-up: Tx – 6/65 participants reattempted; Control – 11/75 participants reattempted |
There was evidence of a significant reduction in SI between the intervention and control groups by the post-intervention assessment (p < 0.001). There was also evidence of a reduction in SA between the intervention and control groups by the 18 month follow-up assessment (significance test not reported). |
| Wharff et al. (2012) [90] USA |
Study design: Historical controlled study Level of evidence: III-3 |
Inclusion: Presented to the ED with SRB Exclusion: not living with family; presented to ED without a family member; intoxicated/sedated at time of presentation; psychosis or developmental delay; presented during overnight shift or on weekend Recruited from: Hospital/ED |
Whole sample N = 250 Mean age: NR (SD: NR; Range: 13–18) Gender: 29% male Treatment group N = 100 Mean age: 15.6 (SD: 1.5) Gender: 24% male Control group N = 150 Age: NR Gender: 26% male |
One session of family based crisis intervention Developed by: Study authors Length: NR Delivered by: MH professional |
TAU: retrospective comparison group who presented to the same ER prior to implementation of FBCI. | Adequately powered: No Outcome assessor blinding: Unclear Less than 15% drop-out rate: No (44.6%) Use of statistical testing to measure change from pre-test to post-test: No |
SRB: NR SA: NR Suicide: NR Longest follow-up: 3 months post-intervention |
SRB: NR SA: NR Suicide: NR |
There were no episodes of SA or completed suicide in either the intervention or control group by the three month follow-up period. Two participants (unclear if allocated to intervention or control groups) were hospitalized for SRB by the three month follow-up assessment. |
Notes: ED = Emergency Department; ID = Intellectual Disability; ITT = intention-to-treat; IQR = Interquartile Range; MH = mental health; NR = not reported; TAU = treatment as usual; SA = suicide attempt; SD = standard deviation; SH = self-harm; SI = suicidal ideation; SRB = suicide-related behavior.
Corrected version of the same paper published in 2012.
Monti PM, et al. Treating Alcohol Dependence: A Coping Skills Training Guide. 2nd ed. New York, NY: Guilford Press; 2002.
Swales M, et al. Linehan's Dialectical Behaviour Therapy (DBT) for borderline personality disorder: overview and adaptation. J Ment Health 2000; 9(1): 7–23.
Rathus J, Miller A. Dialectic behavior therapy adapted for suicidal adolescents. Suicide Life Threat Behav 2002; 32: 146–157.
Miller AL, et al. Dialectical behavior therapy adapted for suicidal adolescents. J Pract Psychiatry Behav Health 1997; 3:78–86.
Palmer S, Dryden W. Counseling for Stress Problems. New Delhi: Sage Publications, 1995.
Table 3.
Study characteristics: Randomized controlled trials conducted in educational or workplace settings (N = 15).
| Study; country | Target population | Participants | Intervention description | Comparison condition | Risk of bias | Suicide related outcome(s) assessed; longest follow-up |
|---|---|---|---|---|---|---|
| Universal interventions | ||||||
| Guille et al. (2015) [113] USA |
Inclusion: Medical students beginning their internship in July 2009 or July 2011 at one of two participating university hospitals Exclusion: NR Recruited from: Universities (N = 2) |
Whole sample N = 199 Mean age: 25.2 (SD: 8.1; Range: NR) Gender: 50.7% male Treatment group N = 100 Mean age: 24.9 (SD: 8.7) Gender: 49% male Control group N = 99 Mean age: 25.4 (SD: 7.4) Gender: 51.6% male |
Individual access to MoodGym: online Cognitive Behavioral Therapy. Module 1: Understanding the interplay between thoughts, emotions & behavior. Modules 2–3: Cognitive restructuring. Module 4: Problem-solving. Length: Four 30-min modules Developed by: National Institute for Mental Health Research at The Australian National University Delivered by: Self-directed |
Active placebo: Email once a week for 4 weeks with information about depression, suicide & where to seek treatment. | Random sequence generation method: NR Allocation concealment method: Independent researcher Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Was ITT analysis undertaken: Yes |
SI (dichotomous): Item 9 of the Patient Health Questionnaire-9 (PHQ-9) Longest follow-up: 12 months post-intervention |
| Orbach & Bar-Joseph, (1993) [92] Israel |
Inclusion: High school juniors from six schools Exclusion: None Recruited from: Secondary schools (N = 6) |
Whole sample N = 393 Mean age: NR Gender: 45% male Treatment group N = 215 Age/gender: NR Control group N = 178 Age/gender: NR |
Weekly group psycho-education workshops: 1) Depression & happiness 2) The individual & their family 3) Helplessness 4) Coping with failure 5) Coping & problem solving 6) Coping with suicidal urges 7) Summary Length: Seven 2-hour workshops Developed by: based on Ross (1997)a and adapted by study authors. Delivered by: NR |
TAU: social issues discussion class | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Was ITT analysis undertaken: Mixed methods |
SI (continuous): Israeli Index of Potential Suicide (IIPS) Longest follow-up: Post-intervention only |
| Till et al. (2017) [119] Austria |
Inclusion: medical, psychology and communication studies undergraduate students Exclusion: None Recruited from: University (N = 1) |
Whole sample N = 161 Mean age: 24.5 (SD 5.8) Gender: 32.9% male Treatment group N = 121 Mean age: 24.3 (SD NR) Gender: 33.9% male Control group N = 40 Mean age: 25.0 (SD 6.8) Gender: 30% male |
Psychoeducation plus support Three German-language websites on suicide-related education and prevention. Two of the three websites also offered email counseling by peers. Length: NA Developed by: mental health organizations Delivered by: Self-directed |
A website unrelated to suicide or mental health | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of DSH repetition: NA Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Was ITT analysis undertaken: Yes |
SI (continuous): Reasons for Living Inventory (RFLI) Longest follow-up: Post-intervention only |
| Indicated interventions | ||||||
| Eggert et al. (2002)b[95], USA |
Inclusion: Students who screened positive for SRB Exclusion: None Recruited from: Secondary schools (N = 7) |
Whole sample N = 341 Mean age (SD): NR (Range: 14–19) Gender: 48% male Treatment group 1 (C-CAST) N = 103 Mean age: 16.02 (SD: 1.14) Gender: 40.77% male Treatment group 2 (C-Care) N = 117 Mean age: 15.71 (SD: 1.21) Gender: 52.14% male Control group N = 121 Mean age: 15.62 (SD: 1.26) Gender: 50.83 male |
Supportive intervention comprising:
Delivered by: 1) Trained research staff e.g. practice nurses & social workers; 2) Teachers, counselors or nurses |
TAU: a brief assessment interview and social connections intervention with parents and school personnel. | Random sequence generation method: Block randomization using a predetermined sequence Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out: No (20.5%) Was ITT analysis undertaken: No |
SRB: High School Questionnaire: Profile of Experiences (HSQ) Longest follow-up: 9 months post-baseline Not included in MA |
| Fitzpatrick et al. (2005) [115] USA |
Inclusion: Students who screened positive for SI Exclusion: students who were judged to represent an immediate threat of danger to themselves or others Recruited from: University (N = 1) |
Whole sample N = 110 Mean age: 19.02 (SD: 1.21; Range: 18–24) Gender: 45% male Treatment group: NR Control group: NR |
A one-off suicide-specific problem solving intervention. Included a video, narrated Power-Point presentation & a case study. Included identifying problems and cognitive, behavioral & affective reactions. It encouraged participants to elicit their problems and apply the skills learned in the video to their personal problems. Length: 40 mins Developed by: based on D'Zurilla and Nezu (1999)c Delivered by: NR |
Active placebo: Video about health issues e.g. diet, exercise, and sleep. | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: No (31.8%) Was ITT analysis undertaken: No |
SI (continuous): Beck Scale for Suicidal Ideation (BSSI) Longest follow-up: 1 month post-baseline |
| Hetrick et al. (2017) [123] Australia |
Inclusion: Presented to school counselor with SI Exclusion: Intellectual disability; psychotic symptoms; inability to speak English Recruited from: Secondary schools (N = 18) |
Whole sample N = 50 Mean age: 14.7 (SD: 1.4) Gender: 18% male Treatment group N = 26 Mean age: 14.8 (SD: 1.6) Gender: 19.3% male Control group N = 24 Mean age: 14.5 (SD: 1.3) Gender: 16.7% male |
Online cognitive behavioral therapy (Reframe IT) Length: Eight self-directed modules over 10 weeks Developed by: study authors Delivered by: self-directed, in the presence of school well-being staff |
TAU: contact with school wellbeing staff plus any outside mental health service provision normally available. | Random sequence generation method: Online randomization program, stratified by school Allocation concealment method: The online program did not allow knowledge of treatment next to be allocated before the participant details were entered into the computer Ascertainment of SH repetition: Interview Outcome assessor blinding: NA Less than 15% drop-out: No (28.6%) Was ITT analysis undertaken: Yes |
SI (continuous): SIQ SA: a specifically designed questionnaire that asked participant whether they had attempted suicide since their last assessment, and if so, how many times Longest follow-up: 3 months post-intervention |
| Hill & Pettit, (2016) [122]d USA |
Inclusion: Endorsed a perceived burdensomeness score of 17 or greater on the Interpersonal Needs Questionnaire Perceived Burdensomeness subscale (Van Orden et al., 2012)e Exclusion: Current psychosocial treatment or use of psychoactive medications, unless on a stable dose for > 8 weeks Recruited from: Schools (N = NR) & public gathering places |
Whole sample N = 80 Mean age: 16.9 (SD: 1.7; Range: 13–19) Gender: 31.2% male Treatment group N = 40 Age/gender: NR Control group N = 40 Age/gender: NR |
Online cognitive behavioral therapy (LEAP: Learn, Explore, Assess you options, Plan) Length: Two modules delivered over two weeks Developed by: study authors Delivered by: self-directed |
Placebo: e-mail containing psychoeducational information about mental health & suicide, and resources for mental health treatment and suicide/crisis counseling. |
Random sequence generation method: Sequentially numbered envelopes Allocation concealment method: Sealed, opaque envelopes Ascertainment of SH repetition: Self-report questionnaire. Outcome assessor blinding: NA Less than 15% drop-out: Yes (13.8%) Was ITT analysis undertaken: Yes |
SI (continuous): BSSI Longest follow-up: 2 months post-baseline |
| Hooven et al. (2012) [96] USA |
Inclusion: Students who met criteria for suicide risk status Exclusion: None Recruited from: Secondary schools (N = 20) |
Whole sample N = 615 Mean age: 16.0 (SD: NR; Range: 14–19) Gender: 40% male Treatment group C-CARE N = 153 Age/gender: NR P-CARE N = 155 Age/gender: NR Combined N = 164 Age/gender: NR Control group N = 143 Age/gender: NR |
Combined intervention comprising:
Developed by: study authors Delivered by: unclear |
Placebo: brief screening interview. | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate at post-intervention: Unclear Was ITT analysis undertaken: Unclear |
SRB: High School Questionnaire: Profile of Experiences (HSQ) Longest follow-up: 15 months post-baseline Not included in MA |
| Kovac & Range, (2002) [114] USA |
Inclusion: Students who screened positive for SRB Exclusion: None Recruited from: University (N = 1) |
Whole sample N = 121 Mean age: 23.12 (SD: 5.44; Range: 18–42) Gender: 27.3% male Treatment group N = NR Age/gender: NR Control group N = NR Age/gender: NR |
A writing interventionf to examine whether writing with ‘cognitive change’ reduced suicide risk when compared to writing just about suicidal experience and compared to controls. Group 1: Wrote about being suicidal & were instructed to think about their thoughts and feelings at the time. Group 2: Wrote about being suicidal but were asked to provide details about the event. Group 3: Control. Length: four 20-min sessions delivered once a day for 4 days Developed by: study authors Delivered by: Unclear |
Placebo: Wrote in detail about their bedroom | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: No (19.1%) Was ITT analysis undertaken: No |
SI (continuous): SIQ Longest follow-up: 6 weeks post-intervention |
| Pistorello et al. (2012) [116] USA |
Inclusion: Students seeking treatment from a University mental health service for SI, SA, or NSSI Exclusion: psychosis, need for inpatient care, or prior DBT treatment Recruited from: University (N = 1) |
Whole sample N = 63 Mean age: 20.9 (SD: 1.92) Gender: 19% male Treatment group N = 31 Mean age: 20.4 (SD: 1.6) Gender: 22.6% male Control group N = 32 Mean age: 21.3 (SD: 2.1) Gender: 15.6% male |
A combination of individual and group dialectical behavioral therapy. Delivered by: Length: Comprised one 50-min individual psychotherapy session plus a 90-min group skills training session per week, over a 12-month period. Developed by: based on Linehan, (1993)g Delivered by: MH professionals |
Enhanced TAU: included weekly individual & group therapy, weekly group supervision for therapists, & between-session consultation and family. Interventions as needed. | Random sequence generation method: Computer generated adaptive randomization Allocation concealment method: NR Ascertainment of SH repetition: Interview Outcome assessor blinding: NA Less than 15% drop-out rate at post-intervention: No (22.2%) Was ITT analysis undertaken: Yes. All participants with missing data were coded as unimproved. |
SI (continuous): Suicidal Behaviors Questionnaire (SBQ-23) SA: SBQ-32 Longest follow-up: 18 months post-baseline |
|
Robinson W et al. (2016) [97] USA |
Inclusion: Students who screened positive for SRB Exclusion: None Recruited from: Secondary schools (N = 4) |
Whole sample N = 330 Mean age: NR Range: 14–17 + Gender: 40% male Treatment group: NR Control group: NR |
Group coping with stress course: 1) Identifying feelings of stress 2) Reducing negative cognitions & increasing positive thoughts 3) Identifying risk factors for stress 4) Enhancing competencies for managing stress 5) Planning for stress. Length: Fifteen 45-min sessions Developed by: based on Robinson & Case (2003)h and adapted by study authors Delivered by: MH professional |
TAU: one-to-one sessions on stress management. | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.6%) Was ITT analysis undertaken: NR |
SI (categorical): Four suicidality screening items (not included in MA) Longest follow-up: Post-intervention only Not included in MA |
| Tang et al. (2009) [98] Taiwan |
Inclusion: Students with moderate–severe depression, SI, SA, moderate–severe anxiety, or significant hopelessness in previous 2 weeks. Exclusion: acute psychotic symptoms, act out lethal suicidal behaviors, lack proper care for suicide risk by their family, drug abuse, or serious medication condition Recruited from: Secondary schools (N = 1) |
Whole sample N = 73 Mean age: NR (Range: 14–18) Treatment group N = 35 Mean age: 15.26 (SD: 1.7) Gender: 34% male Control group N = 38 Mean age: 15.24 (SD: 1.65) Gender: 34% male |
Interpersonal psychotherapy Length: Two sessions per week for 6 weeks Developed by: based on Mufson et al. (2004)i and adapted by study authors Delivered by: School counselor & intern counseling psychotherapists |
TAU: psycho-education and individual supportive counseling once or twice a week. | Random sequence generation method: NR Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Was ITT analysis undertaken: Yes |
SI (continuous): BSSI Longest follow-up: Post-intervention only |
| Multi-modal interventions | ||||||
| Schilling et al. (2014) [100] USA |
Inclusion: Middle school students Exclusion: None Recruited from: Middle schools (N = 8) |
Whole sample N = 470 Age: NR Gender: 47.4% male Treatment group: NR Control group: NR |
Suicide-specific psycho-education (plus screening). Signs of Suicide (SOS). Video & discussion guide depicting signs of suicidality & depression and recommended ways to respond. Also included screening to identify students at risk. Length: Video = 17 min Developed by: Screening for Mental Health Inc. Delivered by: Teachers |
Attended class as usual & received the program after the study period | Random sequence generation method: Cluster simple randomization. However, 2 schools allocated to control crossed over into the intervention Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Was ITT analysis undertaken: No |
SRB: Centers for Disease Control and Prevention's (CDC) Youth Risk Behavior Survey (YRBS) Longest follow-up: 3-months post-intervention Not included in MA |
| Schilling et al. (2016) [99] USA |
Inclusion: ninth-grade students Exclusion: None Recruited from: Secondary schools (N = 16) |
Whole sample N = 1272 Mean age: NR (Range14–15) Gender: 58.3% male Treatment group N = 719 Age: NR Gender: 55.8% Control N = 553 Age: NR Gender: 61.6% male |
Suicide-specific psycho-education (plus screening). Signs of Suicide (SOS). As above. |
Waitlist control | Random sequence generation method: Cluster simple randomization. Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Was ITT analysis undertaken: No |
SI (dichotomous): CDC YRBS Longest follow-up: Post-intervention only |
| Multiple interventions | ||||||
| Wasserman et al. (2015) [101] Multi-site: 10 European countries |
Inclusion: all students in participating classrooms Exclusion: None (although students who reported suicide attempts ever, or severe suicidal ideation in the past 2 weeks before the baseline assessment, and those with missing data regarding these two variables were excluded from the final analysis) Recruited from: Secondary schools (N = 168) |
Whole sample N = 11,110 Mean age: 14.8 (SD:0·82 Range: 14–16) Gender: NR Treatment group 1 N = 2692 Mean age: 14.8 (SD: 0.82) Gender: 37% male Treatment group 2 N = 2721 Mean age: 14.8 (SD: 0.85) Gender: 40% male Treatment group 3 N = 2764 Mean age: 14.8 (SD: 0.8) Gender: 42% male Control group N = 2933 Mean age: 14.78 (SD: 0.89) Gender: 44% male |
Psycho-educational (universal) component Youth Aware of Mental Health Programme (YAM), a universal intervention that aims to raise awareness of risk & protective factors associated with suicide, including knowledge of depression/anxiety and to enhance skills to manage stress, adverse life events & suicidal behaviors Length: 3 h role play session plus 2 × 1 h lectures Developed by: study authors Gatekeeper training (selective) component Question, Persuade, and Refer (QPR), a gatekeeper training module targeting teachers and other school personnel. Length: NR Developed by: Tompkins et al. (2010)j Screening (selective) component Screening by health professionals (ProfScreen) with referral of at-risk pupils. Length: NA Developed by: study authors Delivered by: Trained instructors |
Active placebo: The control group was exposed to the same 6 educational posters as the YAM group. These included information about local health-care providers. | Random sequence generation method: Cluster stratified randomization using a random numbers table Allocation concealment method: NR Ascertainment of SH repetition: Self-report Outcome assessor blinding: NA Less than 15% drop-out rate: No (26.3%) Was ITT analysis undertaken: No |
SI (dichotomous): single item from five item Paykel Hierarchical Suicidal Ladder SA (dichotomous): single item from five item Paykel Hierarchical Suicidal Ladder Longest follow-up:12 months (not specified if post-test or post-intervention) |
Notes: ED = Emergency Department; ITT = intention-to-treat; IQR = Interquartile Range; MA = meta-analysis; MH = mental health; NA = not applicable; NR = not reported; TAU = treatment as usual; SA = suicide attempt; SD = standard deviation; SH = self-harm; SI = suicidal ideation; SRB = suicide-related behavior.
Ross CP. School and suicide: Education for life and death. In RFW Diekstra & K Hawton (Eds.), Suicide in adolescence. Dordrecht: Martinus Nijhoff, 1987.
Excluded secondary publication: Randell BP et al. Immediate post-intervention effects of two brief youth suicide prevention interventions. Suicide Life Threat Behav 2001; 31(1): 41–61.
D'Zurilla TJ, Nezu AM. Development and preliminary evaluation of the Social Problem-Solving Inventory. Psychol Asses 1990; 2: 156–163.
Note: This study recruited participants from both schools and the community.
Van Orden KA, et al. Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol Assess 2012; 24:197–215.
Classified as BCI in the meta-analysis
Linehan MM. Skills training manual for treating borderline personality disorder. New York: Guilford Press, 1993.
Robinson WL, Case MH. Leader manual for the Down with Drama course. Unpublished Manual. DePaul University; Chicago: Illinois: 1995.
Mufson L, et al. Effectiveness research: Transporting interpersonal psychotherapy for depressed adolescents (IPT-A) from the lab to school-based health clinics. J Consult Clin Psychol 2004; 7: 251–261.
Tompkins TL, et al. Does a gatekeeper suicide prevention program work in a school setting? Evaluating training outcome and moderators of effectiveness. Suicide Life Threat Behav 2010; 40: 506–15.
Table 4.
Study characteristics: Non-randomized controlled trials conducted in educational or workplace settings (N = 16).
| Study; country | Study design; level of evidence | Target population | Participants | Intervention description | Comparison condition | Risk of bias | Suicide related outcome(s) assessed; Longest follow-up | Results | Interpretation |
|---|---|---|---|---|---|---|---|---|---|
| Universal interventions | |||||||||
| Bailey et al. (2017) [110] Australia |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: year 11 and 12 students at participating schools Exclusion: None Recruited from: Secondary schools (N = 3) |
Whole sample: N = 129 Mean age: 16.7 (range 16–18) Gender: 53.5% male |
Educational safeTALK Length: One 3-hour session Developed by: LivingWorks Delivered by: Trained instructors |
NA | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: No (25.9%) Use of statistical testing to measure change at from pre-test to post-test: Yes |
SI: Single item asking participants to indicate whether or not they were experiencing current suicidal thoughts. Longest follow-up: 1 month post-intervention |
SI: NR | In comparison with Time 1 (the reference category), individuals at Time 2 had 0.53 times the odds of experiencing suicidal thoughts (95% CI = 0.20–1.36), and at Time 3 had 0.30 times the odds (95% CI = 0.10–0.91). |
| King et al. (2011) [102] USA |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: Students at participating schools Exclusion: None Recruited from: Secondary schools (N participating = NR, but the program was implemented in 24 schools). |
Whole sample: N = 1030 Mean age: 14.1 (SD: 0.79; range 14–18) Gender: 43.9% male |
Educational Surviving the Teens® Suicide Prevention and Depression Awareness Program. Length: Four 50-min sessions Developed by: Study authors Delivered by: MH professionals |
NA | Adequately powered: No power calculations provided. However, likely to be adequately powered for SI but not SA. Outcome assessor blinding: NA Less than 15% drop-out rate: No (59.6%) Use of statistical testing to measure change at from pre-test to post-test: Yes |
SI: Single item asking participants to indicate whether or not they were currently seriously considering attempting suicide Longest follow-up: 3 months post-intervention |
SI: Post-test Yes = 2.9% (n = 26) Follow-up Yes = 1.5% (n = 6) |
There was no significant change in the number of students seriously considering suicide at post-intervention from pre-intervention (χ2 = 0.837, p = 0.360). At 3-month follow-up, students were significantly less likely than at pre-test to be currently considering suicide (p = 0.035). |
| LaFromboise & Howard-Pitney, (1994) [93] USA |
Study design: Non-randomized experimental trial Level of evidence: III-2 |
Inclusion: Students attending a Zuni secondary school Exclusion: None Recruited from: Secondary school (N = 1) |
Whole sample: N = 83 Mean age: 15.6 SD/Range: NR Gender: 41% male Treatment group: NR Control group: NR |
Educational The Zuni Life Skills Development Curriculum. Units included: information about suicide; suicide intervention skills; communication skills; coping with oppression; anger & stress management and goal setting. Length: Six units delivered across 28 lessons Developed by: Study authors Delivered by: Teachers |
NR | Intervention developer: Study authors Adequately powered: Unclear Outcome assessor blinding: NA Less than 15% drop-out rate: No (25.3%) Use of statistical testing to measure change at from pre-test to post-test: Yes |
SI: Suicide Ideation subscale of the Suicide Probability Scale (SPS) Longest follow-up: Post-intervention only |
SI: Intervention mean (SD): 13.4 (NR) Control mean (SD): 16.8 (NR) |
No between-group statistical analysis completed. |
| LaFramboise & Howard-Pitney, (1995) [94] USA |
Study design: Non-randomized experimental trial Level of evidence: III-2 |
Inclusion: Freshman and junior students taking language arts classes at a Zuni secondary school Exclusion: None Recruited from: Secondary school (N = 1) |
Whole sample: N = 128 Mean age: 15.9 (Range: 14–19) Gender: 36% male Treatment group: N = 69 Age/gender: NR Control group: N = 59 Age/gender: NR |
Educational The Zuni Life Skills Development Curriculum. Units: building self-esteem; identifying emotions & stress; communication & problem-solving skills; recognizing & eliminating self-destructive behavior; suicide information; suicide intervention training; goal setting Length: Seven units delivered 3 times a week over approx. 30 weeks Developed by: Study authors Delivered by: Teachers |
No intervention | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: No (23.4%) Use of statistical testing to measure change at from pre-test to post-test: Yes |
SRB: SPS Longest follow-up: 8 months post-baseline |
SRB: Intervention mean (SD): 54.3 (SD: 11.6) Control mean (SD): 58.9 (SD: 13.0) |
The treatment group was less suicidal after taking part in the curriculum than the control group, t[61] = 1.45, p < 0.07. |
| Vieland et al. (1991) [103] USA |
Study design: Non-randomized experimental trial Level of evidence: III-2 |
Inclusion: Ninth grade students from participating schools Exclusion: Schools excluded if they had ever received a suicide prevention program Recruited from: Secondary schools (N = 4) |
Whole sample: N = 381 Mean age: 15.8 Gender: NR Treatment group: N = 174 Mean age: 15.8 (SD: 0.64) Gender: 45% male Control group: N = 207 Mean age: 15.8 (SD: 0.59) Gender: 51% male |
Educational In-class presentation. Emphasized support networks in alleviating stress, confronting one's peers, and community resources. Length: 1.5 h Developed by: Unclear Delivered by: Teachers |
No intervention | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Use of statistical testing to measure change at from pre-test to post-test: No |
SA: Single item asking participants to indicate whether or not they had made a first suicide attempt Longest follow-up: 18 months post-baseline |
SA: Intervention: Yes = 2.5% Control: Yes = 2.7% |
There was no evidence that the program had an effect on suicide attempt rates. |
| Selective interventions | |||||||||
| Hazell & Lewin (1993) [104] Australia |
Study design: Post-test case series Level of evidence: IV |
Inclusion: Students who had been exposed to the suicide of a peer Exclusion: None Recruited from: Secondary schools (N = 2) |
Whole sample: N = 126 Mean age/gender: NR Treatment group: N = 63 Age/gender: NR Control group: N = 63 Age/gender: NR |
Therapeutic One session of group counseling provided at school within 7 days of a student suicide. Following the session, school staff were debriefed & arrangements made to follow-up high risk students. Length: 90 min Developed by: Study authors Delivered by: MH professionals |
Unclear | Adequately powered: NR Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Use of statistical testing to measure change at from pre-test to post-test: Yes |
SA: Hospitalization for SA assessed using Youth Self Report (YSR) version of the Child Behavior Checklist (CBCL) SH: Incidence of current suicidal behavior - YSR CBCL SI: % of group currently experiencing suicidal ideation – YSR CBCL Longest follow-up: Post-intervention only |
SA: Intervention: 1.6% Control: 0.0% SH: Intervention: 21.0% Control: 19.0% SI: Intervention: 14.5% Control group: 19.0% |
There were no differences between groups on SA, SH or SI as assessed by Pearson X2 |
| McDaniel et al. (1990) [121] USA |
Study design: Interrupted time series with a control group Level of evidence: III-2 |
Inclusion: US Navy instructors Exclusion: None Recruited from: Navy training command (N = 1) |
NR | Training sessions for instructors in US Navy training command. Focused on how instructors can identify signs of distress and risk in their students, how to intervene and how to get help. Length: 3 × 1 h Developed by: Unclear Delivered by: MH professionals |
“Operational command” - less than 10 miles away from training command and about the same size but no training. | Adequately powered: NR Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Use of statistical testing to measure change at from pre-test to post-test: Yes |
SA: Average monthly rate of SA (obtained from official sources) Longest follow-up: NA |
SA: Post-test Intervention rate: 9.4 Control rate: 1.8 |
There was a declining trend in the suicide attempt rate in the intervention group. At post-test, the average monthly suicide attempt rate was significantly higher in the intervention group, p < 0.001. |
| Indicated interventions | |||||||||
| Biddle et al. (2014) [105] USA |
Study design: Post-test case series Level of evidence: IV |
Inclusion: Students demonstrating SRB Exclusion: NA Recruited from: Secondary schools (N = 619) |
N = 18,445 Mean age: NR (Range: 13–21) Gender: NR |
Therapeutic Student Assistance Program (SAP): Identify individual student problems & recommend interventions. Participants are students referred to the SAP who accessed the recommended services. Length: NA Developed by: Commonwealth Student Assistance Program Interagency Committee, Pennsylvania. Delivered by: Trained school staff |
No intervention | Adequately powered: Yes Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Use of statistical testing to measure change at from pre-test to post-test: Unclear |
Suicide: Number of suicides and suicide rate per 100,000 students Longest follow-up: NA |
Suicide: Post-test Intervention N (rate): 9 (65.2) Control N (rate): 6 (129.25) |
The difference in suicide rates was not statistically significant. |
| Eggert et al. (1995) [106]; (1999)a[36], USA |
Study design: Post-test case series Level of evidence: IV |
Inclusion: Students reporting: SA; SI; moderate-serious depression; specific levels of alcohol or other drug use, polyuse, or drug use control problems Exclusion: None Recruited from: Secondary schools (N = 5) |
Whole sample: N = 105 Mean age/gender: NR PGC I group: N = 36 Mean age: 16.19 (SD: 0.92) Gender: 41.7% male PGC II group N = 34 Mean age: 15.82 (SD: 1.11) Gender: 37.1% male Control: N = 35 Mean age: 15.57 (SD: 1.01) Gender: 45.7% male |
Psycho-education Personal growth classes (PGCs): Incorporated [1] group work; [2] weekly monitoring of activities targeting changes in mood management, school performance and attendance, and drug involvement; and [3] life skills training in self-esteem enhancement, decision making, personal control (skills training in anger, depression, and stress management), and interpersonal communication. Length: (PGC I): One semester - 5 months or 90 class days; (PGC-II): Two semesters − 10 months or 180 class days. Developed by: Study authors Delivered by: Trained school staff |
Enhanced TAU: Assessed for suicide ‘potential’. | Adequately powered: NR Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Use of statistical testing to measure change at from pre-test to post-test: Yes |
SRB: The Brief Suicide Risk Behavior Scale; A 5-item scale measuring the frequency of suicide thoughts, direct and indirect suicide threats, and suicide attempts Longest follow-up: 10 months post-intervention |
SRB: Post-test PGC1 mean (SD): 0.27 (0.55) PGC2 mean (SD): 0.66 (0.85) Control mean (SD): 0.55 (0.65) Follow-up PGC1 mean (SD): 0.56 (0.93) PGC2 mean (SD): 0.66 (0.79) Control mean (SD): 0.23 (0.37) |
There was no significant difference in suicide risk behaviors between the groups. There was a significant decline in suicide risk behaviors for all three groups (F Linear [1], [102] = 104.14, p < 0.001) revealed a significant decline for all three groups. |
| Joffe (2008) [118] USA |
Study design: Interrupted time series with a control group Level of evidence: III-2 |
Inclusion: Students with a SA or suicide ‘threat’ Exclusion: NA Recruited from: University (N = 1) |
Student population Treatment location: 1980–1983: 139,384 1984–1990: 249,812 Control location: 1980–1983: 1,244,469 1984–1990: 1,807,968 |
Policy Implementation of a policy requiring any student who made a suicide threat or attempt to receive 4 individual sessions of professional assessment, the first which occurred within a week of the incident. Length: NR Developed by: Counseling Center, University of Illinois Delivered by: MH professionals |
Data collected from 11 other universities | Adequately powered: NR Outcome assessor blinding: NA Less than 15% drop-out rate: Not Reported Use of statistical testing to measure change at from pre-test to post-test: Yes |
Suicide: Deaths by suicide per 100,000 enrolled students per year Longest follow-up: NA |
Suicide: Post-test Intervention rate: 2.0 Control rate: 8.68 |
The treatment group had a 74.7% reduction in the suicide rate, compared to an increasing suicide rate in the comparison group, z score = 5.90, p < 0.05 |
| Lerner & Clum (1990) [117] USA |
Study design: Non-randomized, experimental trial Level of evidence: III-2 |
Inclusion: Students with SI Exclusion: Psychosis, substance abuse Recruited from: University (N = 1) |
Whole sample N = 18 Mean age: 19.17 (SD: 1.38; Range: 18–24) Gender: 22% male Treatment group N = 9 Mean age: 18.78 (SD: 0.83; Range: NR) Gender: 11% male Control group N = 9 Mean age: 19.56 (SD: 1.74) Gender: 33% male |
Therapeutic group problem solving therapy Length: 10 sessions over 5–7 weeks Developed by: Based on D'Zurilla and Goldfried (1971)b Delivered by: MH professional |
Active placebo: empathetic listening, sharing experiences with the group. | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: Yes (0.0%) Use of statistical testing to measure change at from pre-test to post-test: Yes |
SI: Modified Scale for Suicidal Ideation (MSSI) Longest follow-up: 3 months post-intervention |
SI: Post-test Intervention mean (SD): 5.8 (7.0) Control mean (SD): 5.3 (9.2) 3-month follow-up Intervention mean (SD): 4.7 (3.4) Control mean (SD): 10.6 (8.8) |
There was no significant difference in suicidal ideation between the groups at both time points (T2: F value < 1; T3: F value = 1.87) |
| Robinson J et al. (2016)c[112], Australia |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: Students who presented to the school counselor with SI in the past month Exclusion: ID, psychosis, inability to speak English Recruited from: Secondary schools (N = 11) |
Whole sample: N = 32 Mean age: 15.6 (Range: 14–17) Gender: 12.5% male |
Therapeutic Reframe-IT. Individual online suicide-specific CBT: eight 20-min modules incorporating standard CBT approaches commonly used with young people. Length: eight 20-min modules Developed by: Study authors Delivered by: self-directed |
NA | Adequately powered: No Outcome assessor blinding: NA Less than 15% drop-out rate: No (38.2%) Use of statistical testing to measure change at from pre-test to post-test: Yes |
SI: Suicidal Ideation Questionnaire (SIQ) Longest follow-up: Post-intervention only |
SI: Pre-test Mean (SD): 3.2 (1.6) Post-test Mean (SD): 1.5 (1.3) |
There was a statistically significant decrease in SI from per to post-test, with a moderate effect size, t = 6.2; p < 0.0005 |
| Multi-modal interventions | |||||||||
| Aseltine et al. (2007)d[107], USA |
Study design: Pseudo-RCT Level of evidence: III-1 |
Inclusion: Students at participating schools Exclusion: None Recruited from: Secondary schools (N = 9) |
Whole sample N = 4133 Mean age/range: NR Gender: 50.0% male Treatment group: 2039 Control group: 2094 |
Psycho-education & screening Signs of Suicide (SOS). Universal educational component: Video & discussion guide depicting signs of suicidality & depression and recommended ways to respond. Selective component: Screening to identify students at risk. Length: Video = 17 min Developed by: Screening for Mental Health Inc. Delivered by: NR |
Attended class as usual & received the program after the study period | Adequately powered: No power calculations provided. However, likely to be adequately powered for SI but not SA. Outcome assessor blinding: NA Less than 15% drop-out rate: Unclear Use of statistical testing to measure change at from pre-test to post-test: No |
SA: Item from the Youth Risk Behavior Survey (YRBS): During the past 3 months did you actually attempt suicide? SI: Item from the YRBS: During the past 3 months did you ever seriously consider attempting suicide? Longest follow-up: 3 months post-intervention |
SA: Post-test % answered “Yes” Intervention: 3.0% Control: 4.6% SI: Post-test % answered “Yes” Intervention: 10.1% Control: 11.5% |
Participants in the treatment group were 40% less likely to report a SA in the past 3 months compared with participants in the control group, beta = − 0.47 (SE 0.16), p = 0.0075 (OR = 47%) There was no significant effect of the SOS program on SI, beta = − 0.53 (SE = 1.01), p > 0.05 |
| Shelef et al. (2016) [120] Israel |
Study design: Interrupted time series with a control group Level of evidence: III-2 |
Inclusion: Active duty mandatory service military personnel who served between 1992 and 2012 Exclusion: subsection of the population that did not represent the regular mandatory service soldiers Recruited from: Israeli Defense Force |
Whole sample: N = 1,171,359 Mean age: 19.0 (Range: 17–24) Gender: 53.4% male Treatment group: N = 405,252 Mean age: 19.0 Gender: 55.2% male Control group: N = 766,107 Mean age: 19.0 Gender: 15.4% male |
Multiple Israeli Defense Force Suicide Prevention Program. Includes: means restriction, improved screening & management of suicidal soldiers, psycho-education and gatekeeper training. Length: NA Developed by: Based on Knox et al. (2003)e Delivered by: NR |
Cohort inducted into the IDF prior to the implementation of the intervention (1992–2005) | Adequately powered: Yes Outcome assessor blinding: NA Less than 15% drop-out rate: NR Use of statistical testing to measure change at from pre-test to post-test: Yes |
Suicide: Total number of suicides & average number per year Longest follow-up: NA |
Suicide: Pre-intervention (2006–2012): N = 344; 24.6 per year Post-intervention (1992–2005): N = 89; 12.7 per year |
Trend analysis showed lower suicide rates in the cohort after intervention, Hazard ratio = 0.48 (95%CI: 0.37–0.60) |
| Silverstone et al. (2015) [108]; (2017) [37] Canada |
Study design: Pre-test/post-test case series Level of evidence: IV |
Inclusion: All secondary school students, plus targeted intervention for students with SI (with or without SA) Exclusion: None Recruited from: Secondary schools (N = 5) |
N = 3244 Mean age: NR (Range: 10–19) Gender: 51.7% male |
Therapeutic & screening Empowering a Multi-modal Pathway Toward Healthy Youth (EMPATHY): Universal CBT for all students in years 7 and 8; screening for all students; rapid intervention, guided online CBT for those identified as being at-risk. Length: Universal CBT = 8–16 sessions; online CBT = NR Developed by: Study authors Delivered by: MH professionals |
NA | Adequately powered: Yes Outcome assessor blinding: NA Less than 15% drop-out rate: No (24.2%) Use of statistical testing to measure change at from pre-test to post-test: Yes |
SI: N at “High risk” (“thought you were better off dead” more than half the days in past 2 weeks) or “medium risk” (“thought you were better off dead” several days in past 2 weeks) of suicide Longest follow-up: 15 months post-baseline |
SI: 12-week follow-up High risk N = 30 Medium risk N = 19 Actively suicidal N = 49 15-month follow-up High risk N = 16 Medium risk N = 21 Actively suicidal N = 37 |
Less students were at “high” or “medium” risk of suicide at follow-up compared to baseline (significance testing not reported). At 15-month follow-up, significantly less people were “actively suicidal” (high or medium risk) than at baseline, p < 0.001 |
| Zenere & Lazarus, (1997) [109] USA |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Inclusion: All public secondary school students in Miami, Florida Exclusion: NA Recruited from: Secondary schools (N = 300) |
NR | Multiple Suicide Prevention and School Crisis Management Program: Comprising psycho-education, postvention, school-based crisis teams, staff training, crisis hotline. Length: NA Developed by: Dade County Public Schools Department, Florida. Delivered by: MH professionals & teachers. |
Cohort of students at beginning of implementation of the SPSCMP (1989–1990) | Adequately powered: No power calculations provided. However, likely to be adequately powered for SI but not SA. Outcome assessor blinding: NA Less than 15% drop-out rate: NR Use of statistical testing to measure change at from pre-test to post-test: No |
SI: Number of suicidal ideations, obtained via hotline reports SA: number and rate of suicide attempts, obtained via hotline reports Longest follow-up: NA |
SI: Pre-test (1989–1990) N = 641 Post-test (1993–1994) N = 640 SA: Pre-test N = 243; 87/100,000 Post-test N = 95; 31/100,000 |
The number of suicidal ideations among students fluctuated during the data collection period, initially showing a decrease in activity before returning to previous levels. The rate of suicide attempts decreased |
Notes: ED = Emergency Department; ID = Intellectual Disability; ITT = intention-to-treat; IQR = Interquartile Range; MH = mental health; NA = not applicable; NR = not reported; TAU = treatment as usual; SA = suicide attempt; SD = standard deviation; SH = self-harm; SI = suicidal ideation; SRB = suicide-related behavior.
1999 is a correction; excluded secondary publication: Thompson EA, et al. Mediating effects of an indicated prevention program for reducing youth depression and suicide risk behaviors. Suicide Life Threat Behav 2000; 30(3): 252–71.
D'Zurilla T, Goldfried M. Problem solving and behavior modification. J Abnorm Psychol 1971; 78: 107–126.
Excluded secondary publications: Robinson J, et al. The safety and acceptability of delivering an online intervention to secondary students at risk of suicide: findings from a pilot study. Early Interv Psychiatry 2015; 9(6): 498–506.; Hetrick S, et al. Does cognitive behavioural therapy have a role in improving problem solving and coping in adolescents with suicidal ideation? Cognitive Behaviour Therapist 2014; 7.
Excluded secondary publication: Aseltine RH, DeMartino R, An Outcome Evaluation of the SOS Suicide Prevention Program. American Journal of Public Health 2004; 94(3): 446–451.
Knox KL, et al. Risk of suicide and related adverse outcomes after exposure to a suicide prevention programme in the US Air Force: cohort study. BMJ 2003; 327(7428):1376.
Table 5.
Interrupted time series and ecological studies in community settings (N = 15).
| Study; country | Study design; level of evidence | Target region/population; comparison | Intervention description | Time period | Risk of bias | Outcome/data source | Rates per 100,000 | Interpretation |
|---|---|---|---|---|---|---|---|---|
| Universal: means restriction | ||||||||
| Beautrais et al. (2006) [125] New Zealand |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: NA Comparison: None |
Firearms legislation introduced in 1992 mandating license to own a firearm. | 1985–1992: pre-legislation; 1993–1996: implementation; 1997–2002: post-implementation. |
Were data collected at multiple time points?a Yes Was the intervention likely to affect data collection? No: Data collection from official mortality data at a national level |
Suicide: Mean annual age-specific suicide rates by all methods and by firearm for persons aged 15–24 years, obtained through New Zealand Health Information Service (NZHIS) |
Suicide: All: Unclear Firearm: Unclear |
There was a 66% decrease in the mean annual rate of firearm-related suicide (B = − 1.09; SE = 0.24; p < 0.001). There was a decrease in the fraction of all suicides accounted for by firearm-related suicides (p < 0.0001). There was no significant decrease in overall rates of suicide (b = 0.08; SE = 0.10; p = 0.39). |
| Caron (2004) [126] Canada |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: Northern Quebec Comparison: None |
Firearms legislation introduced in 1992 mandating firearm owners to safely store their firearms. | 1986–1991: pre-legislation; 1992–1996: post-legislation |
Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? No: Data collection from official mortality dataset |
Suicide: Age-specific suicide rates by all methods and by firearm for under 25 age group obtained through the Quebec Coroner's office. | Suicide: All: NR Firearm: NR |
There was a 38% decrease in firearm suicides (significance = NR). There was a 69% increase in the overall suicide rate (X2 = 22.09, df = 1, p < 0.001). |
| Cheung and Dewa (2005) [128] Canada |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: NA Comparison: none |
Restrictive firearms regulations - Bill C-17 enacted in 1991. | 1979: pre-implementation 1999: post-implementation |
Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? No: data collection from official mortality dataset. |
Suicide: Age-specific suicide rates for youth between 15 and 19 years by firearm, overdose, hanging, and total, and percentage of suicides by each particular method, obtained from data collected by the Coroner's office. | Suicide: All: Unclear Firearm: 1979: Unclear 1999: 3.0 Overdose: 1979: 1.2 1999: 0.2 Hanging: 1979: 2.6 1999: 7.8 |
The findings suggest a substantial decrease in firearm-related suicides but no decrease in the overall suicide rate (significance = NR). |
| Leenaars & Lester (1997) [131] Canada |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: NA Comparison: None |
Gun control legislation introduced in 1977 (Bill C-51). | 1969–1976: pre-legislation 1978–1985: post-legislation |
Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? No: data collection from official sources. |
Suicide: Suicides rates by firearm and by all methods, and percentage of total suicide rate by firearm, in persons aged 15–24, obtained from Statistics Canada and supplemented by personal communications. | Suicide: All: Pre-legislation: 12.57 Post-legislation: 16.11 Firearm: Pre-legislation: 5.89 Post-legislation: 7.12 |
There was a significant increase in the mean firearm suicide rate and mean total suicide rate from pre-legislation to post-legislation (p < 0.05). There was no statistically significant change in the percentage of all suicides that were by firearm. |
| Lubin et al. (2010) [132] Israel |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: Defense Force personnel Comparison: None |
Rule prohibiting soldiers from taking home service weapons on the weekend. | T1: 2003–2005 T2: 2007–2008 |
Were data collected at multiple time points? No Was the intervention likely to affect data collection? No: Israeli Defense Force suicide data. |
Suicide: Average number of suicide deaths per year; firearm suicides on weekends; firearm suicides on weekdays in soldiers aged 18–21: data source not specified. | Suicide: All: NR Firearm suicides on weekends: NR Firearm suicides on weekdays: NR |
Following policy change, suicide rates decreased significantly by 40% (t = 3.35, p = 0.04). Most of this decrease was due to decrease in suicide using firearms over the weekend (t = 17.44, p < 0.001). There was no significant change in rates of suicide on weekdays |
| Niederkrotenthaler et al. (2009) [135] Austria |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: NA Comparison: None |
1997 revision of firearm laws to harmonize with EU regulations | T period 1–1986-1987 T period 2 - 1987–2006 |
Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? No: National mortality data. |
Suicide: Suicide rates by firearm and all methods in 10–19 year-olds, obtained from Statistics Austria. | Suicide: All: NR Firearm: Unclear |
There was a temporary increase in firearm suicides, followed by a continuous decrease (adjusted − 0.20 95% CI − 0.33 to − 0.07; p = 0.003). On the whole, firearm suicide rates after the firearm legislation reform were significantly lower than before the reform. The adjusted model showed no changes in total suicide rates associated with the reform (adjusted 0.017 95%CI 0.04–0.074; p = 0.533). |
| Wheeler et al. (2009) [137] Multi-national (23 Countries of 35 with available suicide data from the WHO's Mortality Stratum A). |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: NA Comparison: None |
“Regulatory action” to restrict use of SSRIs | Pre-intervention: 1990–2003 Post-intervention: 2004–2006 |
Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? No: National mortality data & Hospital admissions data. |
Suicide: Suicide rates in 10–14 and 15–19 year-olds, obtained from WHO mortality database. | Suicide: NR | There was no evidence for an overall effect on the incidence of suicide of regulatory action regarding SSRIs for 15–19 year-olds (p = 0.95) or 10–14 year-olds (p = 0.97). |
| Wheeler et al. (2008)b[136], UK |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: Young people treated with SSRIs Comparison: None |
Restriction of SSRIs | Suicide deaths Period 1–1993-2003 Period 2–2003-2005 Self-harm Period 1 1999–2003 Period 2–2003-2005 |
Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? No: National mortality data & Hospital admissions data. |
Suicide: Mortality rates due to intentional self-harm or undetermined intent in 12–17 year-olds, obtained from Office for National Statistics. SA/SH: Hospital admissions per year due to intentional self-harm or undetermined intent in 12–17 year olds, obtained from the Department of Health Hospital Episode Statistics |
Suicide: Unclear Admissions for SA/SH: Males 1999: ~ 120 2005: ~ 120 Females 1999: 367 2005: 525 |
There was no statistical evidence of changes in trends in suicide rates between 1993 and 2005. The rate of hospital admissions remained relatively stable in males and steadily increased in females. |
| Multi-modal | ||||||||
| Ahmadi & Ytterstad (2007) [124] Iran |
Study design: Interrupted time series with a control group Level of evidence: III-2 |
Target region/population: Young women and low SES in 2 cities Comparison: Sarpolzahab hospital (reference group) |
Multi-modal: mix of passive and active strategies (not described). Key feature was psycho-education via videos | Pre-intervention - 1999–2000 Intervention - 2000–2003 |
Were data collected at multiple time points? No Was the intervention likely to affect data collection? Yes: Possible that those involved in data collection were not blinded to the intervention (suicide attempts). |
SH: N (%) of total self-inflected burn cases who was admitted in Gilangharb and Sarpolzahab hospitals during the baseline year to the study, during the study period, and the last year of the study period in persons aged 0–20 years. | SH: NR | No statistical analyses were performed on rates of self-immolation in youth. |
| Center for Disease Control (1998) [127] USA |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: Western Athabaskan tribe in rural New Mexico, USA Comparison: None |
Multi-modal: gatekeeper training, outreach to families, immediate response and follow up for reported at-risk youth, community psychoeducation, and screening in services. | 1988–1989: pre-implementation; 1990–1999: post-implementation |
Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? It is possible that those involved in data collection were not blinded to the intervention (suicide attempts). This was a not a problem with suicide deaths as this was obtained from official sources. |
SRB: Rates of suicide acts for persons aged 15–19 (included completions and attempts) obtained via a surveillance form. | SRB: 1988–1989: 59.8 1990–1991: 8.9 1992–1993: 9.2 1994–1995: 17.6 1996–1999: 10.9 |
Although rates varied after implementation of the program, they remained substantially lower than before the program was initiated. |
| Cwik et al. (2016) [129] USA |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: Apache Indians Comparison: None |
Multi-modal: implemented in 2006, included psychoeducation for students, gatekeeper training, and indicated interventions for suicidal young people. | 2001–2006: pre-implementation 2007–2012: post-implementation |
Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? Yes: it is possible that those involved in data collection were not blinded to the intervention (suicide attempts). |
Suicide: Suicide rates for persons aged 10–24 years, obtained via The Celebrating Life surveillance system (established by tribal resolution in 2001). | Suicide: Pre-test: 10–14 years: 17.1 15–19 years: 23.6 20–24 years: 151.9 Post-test: 10–14 years: 23.6 15–19 years: 101.9 20–24 years: 96.0 |
The suicide rate increased by 38% in 10–14 year-olds, and decreased by 5.5% in 15–19 year-olds and 36.8% in 20–24 year-olds. |
| Hacker et al. (2008) [130] USA |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: Somerville, MA, USA Comparison: Massachusetts |
Multi-modal: implemented between 2003 and 2005, included local trauma response network, community wide vigil, school based counseling, hospital beds made available, outreach to suicide survivors to offer services, youth leadership programs, media reporting guidelines, community-wide education. | 1994–2003: pre-intervention period. 2003–2005: Intervention period. 2005 onwards: post-intervention. |
Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? No: data collection from official sources. |
Suicide: Data on suicide rates for 10–24 year-olds obtained via death certificate data (examined from 2001 to 2007, and then from 1994 for comparison), mortality data from Massachusetts Department of Public Health for (1994–2005). SA/SH: Data on suicide attempts for 10–24 year-olds obtained via self-inflicted injury data from Massachusetts Department of Public Health for (1994–2005), hospital discharge data (1996–2006), 911 dispatch call data (2004 onwards), teen health survey conducted in Somerville High School. SI: Teen health survey |
Suicide: 1994–1999: Somerville: 6.04 2000–2005: Somerville: 9.77 Massachusetts: 4.27 SA/SH: 2005 Somerville: 47.3 Massachusetts: 73.7 2006 Somerville: 53.2 Massachusetts: 74.8 |
Overall the data indicates a decrease in the rate of suicide and suicide attempts (significance = NR). |
| May et al. (2005) [134] USA |
Study design: Interrupted time series without a control group Level of evidence: III-3 |
Target region/population: Western Athabaskan Tribal Nation. New Mexico, USA Comparison: None |
Multi-modal: Surveillance, screening/clinical interventions with extensive outreach in multiple settings, school-based prevention programs, community education for adults and youths, training of ‘natural helpers. | Baseline - 1988–1989; then two yearly numbers and yearly averages until 2002 | Were data collected at multiple time points? Yes Was the intervention likely to affect data collection? Unclear: program providers also main data collectors for non-fatal behaviors, participants may avoid reporting. |
SRB: Number of self-harm incidents (attempts and gestures combined) in 11 to 24 year-olds obtained from staff case conference notes and Indian Health Service records. | SRB: NR | There was a significant decline in the number of combined gestures and attempts in 19–24 year-olds (coeff = − 765, p = 0.001) and 11 to 18 year-olds (coeff = − 0.517, p = 0.048). |
| Multiple interventions | ||||||||
| Garraza et al. (2015) [139]; Walrath et al. (2015) [38] USA |
Study design: Ecological Level of evidence: III-2 |
Target region/population: 466 counties, USA Comparison: 1161 counties not exposed to suicide prevention efforts |
Multiple: Activities funded by the Garrett Lee Smith (GLS) Memorial Suicide Prevention Program, implemented between 2006 and 2009. Includes gatekeeper training, psychoeducation programs, screening, improved community partnerships and linkages to service, postvention programs, and crisis hotlines. | At least 1 NSDUH respondent between 2008 and 2011, suicide mortality between 2007 and 2010 |
Were data collected at multiple time points? No Was the intervention likely to affect data collection? No: Data collection from official sources. |
SA: Suicide attempt rates for each county following the implementation of the GLS program for the population that was approximately 16 to 23 years of age during implementation, obtained via self-report from the NSDUH between 2008 and 2011 Suicide: Suicide rates for persons aged 10–24 years between 2007 and 2010, obtained from the National Vital Statistics System. |
SA: NR Suicide: NR |
Suicide attempts: Counties implementing GLS program activities had significantly lower suicide attempt rates among youths 16 to 23 years of age in the year following implementation of the GLS program than did similar counties that did not implement GLS program activities (4.9 fewer attempts per 1000 youths [95%CI, 1.8–8.0 fewer attempts per 1000 youths]; p = 0.003). There was no evidence of longer-term differences in suicide attempt rates. Suicide deaths: Counties implementing GLS training had significantly lower suicide rates among the population aged 10–24 years in the year after GLS training than similar counties that did not implement GLS training (1.33 fewer deaths per 100,000; p = 0.02). No evidence of an effect beyond one year after training implementation. |
| Matsubayashi & Ueda (2011) [133] Multi-national |
Study design: interrupted time series with a control group Level of evidence: III-2 |
Target region/population: 21 OECD nations Comparison: 10 OECD countries without a national suicide prevention program |
Multiple: National prevention programs - specific interventions not specified or analyzed. | 1980–2004 One time period, statistical models include date of implementation of suicide prevention program - varies for each country |
Were data collected at multiple time points? No Was the intervention likely to affect data collection? No: National mortality data. |
Suicide: Suicide rates in under 25 year-olds, obtained via the WHO mortality database | Suicide: 20.901 (mean total rate) |
Suicide rates: Suicide prevention programs have a negative impact on the suicide rate (Males: − 1.33, SE 0.5; p < 0.05; Females − 0.276 SE.08, p < 0.05) |
Notes: NSDUH = National Survey on Drug Use and Health; NA = not applicable; NR = not reported; OECD = Organization for Economic Co-operation and Development; WHO = World Health Organization; SA = suicide attempt; SE = standard error; SES = socio-economic status; SH = self-harm; SI = suicidal ideation; SRB = suicide-related behavior.
Defined as at least twice before or at least twice after implementation of the intervention.
Note: it is likely that this study is a subset of the date included in Wheeler et al (2009).
Table 6.
Non-randomized experimental trials in community settings (N = 1).
| Study; country | Study design; level of evidence | Target population | Participants | Intervention description | Comparison condition | Risk of bias | Suicide related outcome(s) assessed; Longest follow-up | Results | Interpretation |
|---|---|---|---|---|---|---|---|---|---|
| Allen et al. (2017) USA [138] |
Study design: Non-randomized experimental trial Level of evidence: III-2 |
Inclusion: Young people living in Yup'ik communities Exclusion: None Recruited from: Yup'ik communities in southwest Alaska |
Whole sample N = 124 Mean age: NR Gender: NR Treatment group N = 128 Mean age (SD): 14.24(1.72) Gender: 43% male Control group N = 74 Mean age (SD): 14.62(1.82) Gender: 73% male |
Qungasvik: A cultural intervention based in a local, Indigenous theory of personal and community change. Modules are individual, family, or community level. Length: one or more 1–3 h sessions. Developed by: study authors Delivered by: different cultural experts. |
Community 2 – exposed to less-intensive intervention. | Intervention developer: Rasmus et al. (2014)a Adequately powered: NR Was SH a pre-determined outcome: No Outcome assessor blinding: NR Less than 15% drop-out rate for DSH at post-intervention: Unclear Use of statistical testing to measure change from pre-test to post-test: Yes |
SI: “A Way to Live a Very Good, Beautiful Life”—Reasons for Life (RL): a cultural adaptation and strengths-based extension of the Brief Reasons for Living Inventory for Adolescents. Longest follow-up: post-intervention |
SI: Post-intervention: Intervention mean (SD): 22.42 (4.99) Control mean (SD): 62.98 (17.49) |
The treatment group showed a greater reduction in SI (indicated by increased scores on the RL) than the control group (d = 0.28, p < 0.05), |
Notes: NR = not reported; SD = standard deviation; SI = suicidal ideation.
Rasmus SM, et al. Creating Qungasvik (a Yup'ik intervention “toolbox”): Case examples from a community-developed and culturally-driven intervention. Am J Community Psychol 2014; 54: 140–152.
The majority of studies were conducted in the United States of America (k = 49; 49·5%), followed by the United Kingdom (k = 12; 12·1%) and Australia (k = 11; 11·1%). Some were conducted across multiple countries and only two (2·0%) were conducted in low-middle income countries. The number of studies more than doubled in the period of 2005–2017 compared to 1990–2004.
3.3. Studies Conducted in Clinical Settings
Fifty-two of the included studies were conducted in clinical settings and all tested indicated interventions delivered to young people with a history of self-harm or attempted suicide resulting in presentation to hospital-based or mental health services. Outcomes therefore refer to repeated self-harm in these studies. Thirty-three were RCTs. Forty (76.9%) had a mean participant age of 18 years or younger, eight studies (15.4%) had a mean age over 18, and in four studies (7.7%) the mean age could not be determined.
3.3.1. Randomized Controlled Trials
3.3.1.1. Study Description
Participants were recruited from emergency departments, inpatient units and community mental health services/outpatient clinics. One study was set in a military hospital [40]. Studies examined the impact of a range of interventions, including individual and group cognitive behavioral therapy (CBT), dialectical behavioral therapy (DBT), family therapy, and brief contact interventions. Control conditions included TAU, e.g. routine care, enhanced TAU, e.g. safety monitoring and facilitated referrals, and active placebo e.g. problem oriented support but without a specific skills-based training component. Twenty-four (72·7%) of the studies in this category included participants with a mean age of 18 or younger. Please see Table 1.
3.3.1.2. Study Efficacy
Thirty-two of the 33 clinical RCTs reported data amenable to meta-analysis. Twenty-five were psychological interventions [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64] and seven were brief contact interventions [65], [66], [67], [68], [69], [70], [71]. The results of the meta-analysis, classified according to outcome assessed, are reported below. The primary outcome (self-harm) is reported first, followed by suicidal ideation; suicide is reported last as it was least frequently assessed.
3.3.1.2.1. Self-harm Measured Dichotomously
Compared to controls, there was no evidence of any intervention effect on self-harm at post-intervention (k = 12, RR = 0·889, 95% CI 0·71 to 1·11, I2 = 37·1%) (Fig. 2). At follow-up there was some evidence of a reduction in the proportion of people who had received an intervention who went on to have a repeat self-harm episode (k = 16, RR = 0·83, 95% CI 0·70 to 0·99, I2 = 40·9%) (Fig. 3).
Fig. 2.
Random effects risk ratio and 95% confidence interval (CI) for clinical interventions at the post-intervention assessment.
Fig. 3.
Random effects risk ratio and 95% confidence interval (CI) for clinical interventions at the longest follow-up assessment.
3.3.1.2.2. Sensitivity Analysis
There was no material change to the outcome at post-intervention when studies at high risk of bias for allocation concealment were removed. At follow-up, when studies at high risk of bias were removed, the effect was no longer significant.
3.3.1.2.3. Subgroup Analysis
There was no evidence that the type of intervention modified the size of the treatment effect post-intervention (p = 0·67) or at follow-up (p = 0·09); nor was there any evidence that therapy modality modified the size of the treatment effect post-intervention (p = 0·13), or at follow-up (p = 0·08).
3.3.1.2.4. Self-harm Measured Continuousl
Compared to controls, there was little evidence, with high heterogeneity (I2 = 94·4%), that the intervention resulted in a reduction in the mean number of self-harm episodes at post-intervention (k = 5, SMD = − 0·66, 95% CI − 1·45 to 0·13), and there was limited evidence of this at follow-up (k = 4, SMD = − 0·23, 95% CI − 0·49 to 0·03, I2 = 38·9).
3.3.1.2.5. Suicidal Ideation Measured Dichotomously
Compared to controls, there was no evidence of any effect of intervention on the proportion of people who experienced suicidal ideation post-intervention (k = 7, RR = 0·89, 95% CI 0·68 to 1·16, I2 = 83·0%) or at follow-up (k = 5; RR = 0·84, 95% CI 0·64 to 1·09, I2 = 74·8%). Heterogeneity was high.
3.3.1.2.6. Suicidal Ideation Measured Continuously
Compared to controls, there was strong evidence of a small effect of the intervention on suicidal ideation post-intervention (k = 15, SMD = − 0·28, 95% CI − 0·48 to − 0·08, I2 = 76·3%). The effect was smaller at follow-up (k = 11, SMD = − 0·18, 95% CI − 0·34 to − 0·02, I2 = 41·1%).
One RCT in this category was not included in the meta-analysis. This investigated the impact of Parent-Adolescent CBT [72]; authors reported reduced suicidal ideation in both groups during active and maintenance treatment and at follow-up.
3.3.1.3. Study Quality
The majority of these studies used random sequence generation [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [53], [54], [55], [56], [58], [59], [61], [62], [64], [65], [66], [67], [68], [69], [70], [71] (k = 28; 84·8%) and 21 (60·6%) used adequate allocation concealment strategies [42], [43], [44], [45], [46], [49], [50], [51], [53], [54], [55], [58], [59], [61], [62], [64], [65], [66], [67], [69], [70]. Of the 25 studies that assessed outcomes via interview, 13 (52·0%) reported assessor blinding [43], [44], [45], [49], [51], [53], [55], [56], [59], [61], [64], [65], [70]. Thirteen studies reported conducting intention-to-treat (ITT) analysis [42], [46], [48], [53], [54], [56], [58], [59], [61], [64], [65], [69], [72]. One study did not use ITT, but conducted a sensitivity analysis to assess the robustness of the findings [70]. Nineteen (57·6%) reported less than 15% drop out and were classed as low risk for the purpose of meta-analysis [41], [43], [44], [45], [46], [49], [50], [51], [53], [54], [56], [58], [61], [63], [64], [65], [66], [67], [68], [69].
3.3.2. Other Study Designs
3.3.2.1. Study Description
All nineteen studies in this category tested indicated therapeutic interventions. The majority employed a pre-test/post-case series study design (k = 11; 57·9%) [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83]. Sixteen (84·2%) recruited participants from community mental health services or hospitals, including inpatient and emergency department settings [73], [74], [75], [76], [77], [78], [79], [80], [83], [84], [85], [86], [87], [88], [89], [90], [91]. Interventions included DBT, CBT, and brief contact interventions. Sixteen (84.2%) of the studies in this category had a mean age of 18 or younger. Please see Table 2.
3.3.2.2. Study Efficacy
Two of the five studies testing a CBT-based intervention reported reductions in suicide-related behaviour [73], [86], and three reported reductions in suicidal ideation [73], [75], [76]. Five of the six studies testing DBT reported reductions in suicide-related behaviour [74], [77], [79], [80], [88], and four reported reductions in suicidal ideation [74], [77], [84], [88]. Two of the three studies testing family-based interventions reported reductions in suicidal ideation [83], [89], and one reported a reduction in suicide attempts [89]. One study reported a reduction in the proportion of young people reporting a suicide attempt following exposure to a crisis intervention program [78], and one reported reduced suicidal ideation following telephone counseling [81]. One study tested a brief contact intervention and reported no between-group differences [85]. A study of a problem solving intervention reported a reduction in the proportion of participants reporting suicide attempts in the treatment group compared to controls [87]. Finally, a study testing an intervention for American Indians reported reductions in suicidal ideation over time [82]. Significance testing was not always conducted or reported for studies in this category.
3.3.2.3. Study Quality
Only seven studies had dropout rates of less than 15% [73], [78], [81], [83], [84], [86], [89]. All but one [89] were either under-powered or the adequacy of the sample size could not be determined. Eight studies used a comparison group [84], [85], [86], [87], [88], [89], [90], [91]. Three assessed outcomes using interview-rated measures [87], [90], [91], and only one reported that outcome assessors were blinded to treatment allocation [91]. Fifteen studies (78·9%) conducted statistical testing to measure change from baseline [73], [74], [75], [77], [79], [80], [81], [82], [83], [84], [85], [86], [88], [89], [91].
3.4. Studies Conducted in Educational and Workplace Settings
Thirty-one studies recruited participants from educational or workplace settings; of these 21 (67·7%) were conducted in schools [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107], [108], [109], [110], [111], [112], seven (22·6%) in universities [113], [114], [115], [116], [117], [118], [119], two (6·5%) in military-based workplace settings [120], [121], and one (3·2%) from both schools and public places in the community [122]. Twenty-one (67·7%) had a mean participant age of 18 years or younger, eight studies (25.8%) had a mean age over 18, and in two studies (6·5%) the mean age could not be determined. Fifteen (48.4%) were RCTs.
3.4.1. Randomized Controlled Trials
3.4.1.1. Study Description
Three of the RCTs tested universal interventions [92], [113], [119], nine tested indicated interventions [95], [96], [97], [98], [114], [115], [116], [122], [123], and three tested multi-modal or multiple interventions [99], [100], [101]. Studies were either educational or therapeutic in nature, and four tested an internet-based intervention [113], [119], [122], [123]. One large cluster-RCT tested three distinct interventions (workshops for students; gatekeeper training; and screening) [101]. Two multimodal studies combined a universal educational component with screening. Examples of control conditions in these studies included TAU e.g. an interview with a school counselor, enhanced TAU, e.g. weekly therapy, and placebo e.g. a video about unrelated health issues. Ten studies (66·7%) in this category included participants with a mean age of 18 or under. See Table 3.
3.4.1.2. Study Efficacy
Eleven RCTs reported data amenable to meta-analysis [92], [98], [99], [101], [113], [114], [115], [116], [119], [122], [123]. Together there were 13 individual intervention arms because one study tested three interventions (one brief contact intervention and two universal educational interventions) [101]. Two intervention arms were brief contact interventions, five were universal educational interventions, and six were psychological interventions. As above findings are presented according to the outcome assessed, with the primary outcome (self-harm) reported first, followed by suicidal ideation. No studies reported suicide as an outcome.
3.4.1.2.1. Self-harm Measured Dichotomously
Compared to control, there was evidence of an intervention effect on self-harm at post-intervention (k = 3, RR = 0·31, 95% CI 0·15 to 0·61, I2 = 0%) (Fig. 4) and at follow-up (k = 3, RR = 0·63, 95% CI 0·42 to 0·96, I2 = 0%) (Fig. 5).
Fig. 4.
Random effects risk ratio and 95% confidence interval (CI) for educational interventions at the post-intervention assessment.
Fig. 5.
Random effects risk ratio and 95% confidence interval (CI) for educational interventions at the longest follow-up assessment.
3.4.1.2.2. Sensitivity and Subgroup Analysis
As there were only three studies in this category these analyses were not possible.
3.4.1.2.3. Self-harm Measured Continuously
Compared to control, there was one study that reported continuous data post-intervention [115] with little evidence of an effect (k = 1, SMD = − 0·16, 95% CI − 0·61 to 0·30). No studies reported follow-up data for this outcome.
3.4.1.2.4. Suicidal Ideation Measured Dichotomously
Compared to control, there was little evidence of an effect at post-intervention (k = 1, RR = 0·76, 95% CI 0·50 to 1·16) or follow-up (k = 2 (4 intervention arms), RR = 0·72, 95% CI 0·51 to 1·03, I2 = 0%).
3.4.1.2.5. Suicidal Ideation Measured Continuously
Compared to control, there was strong evidence of an effect of the intervention on suicidal ideation at post-intervention (k = 7, SMD = − 0·41, 95% CI − 0·57 to − 0·24, I2 = 15·2%). By follow-up, the effect was no longer significant (k = 5, SMD = − 0·21, 95% CI − 0·52 to 0·1, I2 = 46·9%).
Four RCTs were not included in the meta-analysis. One tested a supportive intervention and found decreases in ‘suicide risk behaviors’ in treatment and control groups, but no between-group differences [95]. One examined a parent-specific intervention and found reductions over time in both groups, with greater reductions in the treatment group [96]. A group ‘coping with stress course’ tested with African-American adolescents was associated with a relative risk reduction in suicide in the intervention group compared to controls [97]. Finally, a multimodal intervention combining psycho-education and screening was associated with reduced suicidal ideation and behavior in intervention participants compared to controls [100].
3.4.1.3. Study Quality
Seven studies (46·7%) reported using random sequence generation techniques [95], [99], [100], [101], [116], [122], [123] and only three (20·0%) reported adequate concealment of treatment allocation [113], [122], [123]. None of the studies in this category assessed primary outcomes using interviews, so outcome assessor blinding is not applicable. Six (40·0%) studies used ITT analysis [98], [113], [116], [119], [122], [123]. One third (k = 5) had dropout rates of less than 15% [92], [97], [98], [113], [122].
3.4.2. Other Study Designs
3.4.2.1. Study Description
Of these 16 studies, four were non-randomized experimental trials [93], [94], [103], [107], [117], four were pre-test/post-test case series studies [102], [108], [110], [112], three were post-test case series studies [104], [105], [106], and four employed an interrupted time series design [109], [118], [120], [121]. The majority were conducted in school settings (k = 12; 75·0%), with two each (12·5%) conducted in university [117], [118] and military settings [120], [121]. Five studies tested universal educational programs [93], [94], [102], [103], [110], two evaluated selective interventions [104], [121], five evaluated indicated interventions [105], [106], [112], [117], [118] and four evaluated multimodal interventions [93], [94], [102], [103], [107], [108], [109], [110], [120]. Two studies evaluated online interventions [108], [112]. Eleven studies (68.8%) in this category had a mean participant age of 18 or under. See Table 4.
3.4.2.2. Study Efficacy
Of the five studies testing universal interventions, one reported a reduction in suicide-related behavior post-intervention [94], one reported a reduction in suicidal ideation post-intervention and at follow-up [110], and one reported a reduction at follow-up only [102]. Two studies tested selective interventions: one showed no effect of a counseling session delivered to school students bereaved by suicide [104] and the second reported a reduction in suicide attempts associated with a training intervention delivered to U.S. naval instructors [121].
Two of the five studies testing indicated interventions assessed suicide rates as the outcome of interest. The first found no impact of a therapeutic program among secondary school students [105]. The second examined the impact of a university suicide prevention policy and reported a reduction among the intervention group compared to increases among controls [118]. Of the remaining three studies of indicated interventions, only one therapeutic-based intervention was associated with a reduction in suicidal ideation from pre- to post-test [112].
Four studies tested a multimodal intervention. One was conducted in a workplace setting and reported lower suicide rates at post-intervention [120]. Two studies reported decreases in suicide attempts [107], [109]. The final study examined the impact of a combined therapeutic and screening intervention and reported reductions in suicidal ideation at post-intervention and follow-up [108].
3.4.2.3. Study Quality
Only one study [117] reported an attrition rate of less than 15%. Three studies were adequately powered [105], [108], [120], and in another three, although no power calculations were provided, the sample size was sufficient to examine changes in suicidal ideation but not self-harm [102], [107], [109]. The majority of studies (k = 12; 75·0%) used statistical testing to measure change from pre- to post-test [93], [94], [102], [104], [106], [108], [110], [112], [117], [118], [120], [121].
3.5. Studies Conducted in Community Settings
3.5.1. Study Description
Fourteen studies in this category (87·5%) were interrupted time series studies [124], [125], [126], [127], [128], [129], [130], [131], [132], [133], [134], [135], [136], [137]; two (14·3%) utilized a control group [124], [133]. One study was a non-randomized experimental trial [138] and one was an ecological study [139]. None of the community-based studies were RCTs. Eight (50·0%) evaluated means restriction approaches, five (31·3%) tested multimodal interventions [124], [127], [129], [130], [134] and two (12·5%) evaluated multiple interventions [133], [139]. One non-randomized experimental trial [138] examined the impact of a cultural intervention among indigenous young people in Alaska.
3.5.2. Study Efficacy
Five of the six studies examining the impact of policies designed to restrict access to firearms reported decreases in the firearm suicide rate among young people [125], [126], [128], [132], [135], and one reported an increase [131]. Only one reported a decrease in the overall youth suicide rate [132].
Two studies examined the impact of regulatory action to restrict use of antidepressants and found no evidence of an effect on suicide rates [136], [137]. One of these studies also examined the impact of such regulatory action on rates of hospital admissions for self-harm and reported decreases in females only [136].
Three of the five studies evaluating multimodal interventions reported generally positive impacts on rates of suicide and/or suicide-related behaviour [127], [130], [134]. One study found the suicide rate decreased by 5·5% in 15–19 year-olds but increased by 38% in 10–14 year-olds [129]. Finally, one study evaluated the impact of an intervention targeting self-immolation in women; the authors reported a reduction in the number and percentage of self-immolation cases but did not report statistical significance [124].
One study evaluated multiple interventions delivered across different counties in the U.S. The interventions were associated with lower rates of suicide attempt [139] and suicide [38] but there was no evidence of a longer-term effect. Finally, a study evaluating the impact of government-initiated national suicide prevention programs across multiple nations reported decreases in suicide rates [133].
3.5.3. Study Quality
In 11 studies (73·3%), data were collected at multiple time points [125], [126], [127], [128], [129], [130], [131], [134], [135], [136], [137] and in 11 studies the intervention was deemed unlikely to impact data collection for the primary outcome of interest [125], [126], [128], [130], [131], [132], [133], [135], [136], [137], [139].
4. Discussion
This review examined 99 individual studies of interventions designed to reduce suicide-related behaviors among young people. Samples were diverse, although few studies were conducted in low-to-middle income countries. Studies were conducted across a range of settings and tested a variety of intervention approaches, reflecting the spread of suicide prevention activity as recommended by current policy [7], [1]. Less than half the studies were RCTs, which is unsurprising as the lack of RCTs in suicide prevention has been highlighted previously [24], [140]. Although not all intervention approaches, or intervention types, lend themselves to being tested this way, there remains a clear need for high-quality intervention studies in this field. In the majority of studies the mean age of participants was 18 or under (68.7%). In the clinical studies this was more prominent than in those conducted in educational settings (76.9% compared to 67.7%), suggesting that the findings from the clinical trials may be most applicable to young people aged 18 and under.
The number of intervention studies in youth suicide prevention has doubled in recent years, which is encouraging. However, many studies tested interventions originally designed for adults with little, or no, adaption for young people [24]. This may partially account for the high rates of attrition in many of the studies reviewed. Adolescence and young adulthood are developmental periods requiring specific attention [141], [142]. As such interventions that account for developmental stage and are both acceptable to, and ideally co-designed with, young people are necessary.
The meta-analysis showed little evidence that interventions reduced repetition of self-harm at post-intervention in clinical settings. Whilst there was some evidence for reduced repetition of self-harm at follow-up, this effect disappeared after removing low-quality studies; as such these findings should be interpreted with caution. There may be a small effect on frequency of self-harm measured continuously. It is possible that these effects are being driven by the large trial by Hassanian-Moghaddam and colleagues that tested a brief contact intervention in Iran [68]. This finding is in contrast to a review by Ougrin and colleagues, which found evidence of benefit for clinical interventions in reducing the proportion of adolescents re-engaging in repeat self-harm [143]. This variation in findings may be explained by the settings in which the studies were conducted, or may be attributable to methodological differences such as the more specific inclusion criteria employed by the current review and/or differences in reporting of results (i.e., use of relative vs absolute effect size). There was also strong evidence of a small effect on suicidal ideation at post-intervention, and to a lesser extent at follow-up, again possibly being driven by the large Hassanian-Moghaddam trial [ 68].
There is less evidence for interventions delivered in educational or workplace settings given that fewer methodologically-rigorous studies have been conducted. Of note are the large studies conducted by Wasserman and colleagues [101] and Schilling and colleagues [99]. The educational components of the interventions tested in these studies appeared to reduce self-harm at post-intervention and at follow-up [99], [100], [101], although there were too few studies to conduct meaningful sub-group analyses. There was also an effect on suicidal ideation at post-intervention, but not follow-up. Overall these results indicate that school-based psycho-educational interventions that are coupled with screening have the potential to be effective, however the robustness of findings is hampered by study quality.
To some extent the overall limited effects detected may reflect a lack of statistical power, either due to small sample sizes at baseline or high attrition rates. Many studies (in particular those of indicated interventions) were underpowered and did not find statistically significant improvements despite the direction of effect being positive. This was particularly true for studies examining self-harm given the large sample sizes required to detect an effect [144]. It may also be that suicidal ideation and self-harm are different constructs, and whilst it is largely accepted that they exist along a continuum [145], specific processes may facilitate the transition from suicidal ideation to suicide attempt [146]. It may therefore be the case that existing interventions more effectively target suicidal ideation than self-harm, and that interventions with stronger theoretical underpinnings are required to reduce self-harm and suicide. Further work delineating the modifiable risk and protective factors associated with repeated self-harm is therefore required [147].
Evidence regarding the efficacy of interventions in community settings was mixed. The studies that examined the impact of multimodal interventions generally reported reductions in rates of suicide and/or self-harm, although study quality was variable. These findings are encouraging given the emphasis in many countries on place-based responses to suicide prevention [148], [149]. The interventions tested typically comprised universal educational programs, gatekeeper training, screening, and treatment responses where appropriate, and appeared to positively impact young people. These intervention types should be included in future place-based approaches and subject to rigorous testing.
Means restriction, such as reducing access to known jumping sites, has long been considered an effective suicide prevention intervention [17], [18]. Our review identified few studies examining the effects of means restriction on young people, and those that did focused on firearm restriction. These were generally associated with decreases in rates of firearm suicide, but no reduction in overall youth suicides. An explanation may be that firearm suicides are relatively uncommon among youth in the countries studied. For example, three studies were conducted in Canada where the most common method of youth suicide is hanging [150]. It stands to reason that restricting access to a particular method will only reduce overall suicide rates if it is a method commonly used by the population.
Despite the spread of studies across intervention types and settings, gaps existed. For example, General Practitioners (GPs) are often a first port of call for young people yet there were no studies in primary care settings. GPs and have identified the need for training in youth suicide prevention [151]; as such primary care settings may provide an opportunity for intervention early in the suicidal trajectory that is currently being missed. Additionally, few studies were conducted in universities or workplaces compared to schools. Given that suicide rates are highest post-school age [152], tertiary education facilities and workplaces are key settings for future suicide prevention efforts and greater evidence is required [142], [153]. Moreover, only six studies tested online interventions; all were in educational settings. There is increasing evidence supporting the efficacy of online interventions in the treatment of depression and anxiety [154], as well as evidence supporting their acceptability with young people at risk of suicide and potential to reduce risk [155]. All the studies of online interventions were CBT-based and most appeared to show promise, raising the question of why online interventions are not being trialed in clinical settings. This is an important avenue for youth suicide prevention yet to be capitalized on.
Finally, there are some groups who are underrepresented in this research. Only three studies [93], [94], [138] tested interventions among indigenous young people, despite this group being at elevated risk in many countries [156]. Similarly, same-sex-attracted and gender diverse young people are at elevated risk of suicide [157], yet only one study specifically targeted same-sex attracted youth [83]. Whilst this may be partially due to methodological challenges [156], [158], generating evidence regarding effective suicide prevention approaches for these populations must be a priority. Related to this, females were over-represented in the studies reviewed. This is unsurprising given the higher rates of both self-harm and help-seeking among females compared to males [159], [160], however there is a lack of knowledge regarding effective interventions for young men, whose rates of suicide are three times those of females [1].
A strength of this review is the inclusion criteria used. These were both broad (e.g., no restrictions on intervention approach or study design) and specific (i.e., studies tested interventions that were specifically designed for suicide prevention and reported suicide-related outcome data). Whilst some potentially effective interventions may have been excluded (e.g., those designed to treat or prevent depression), this review is well-placed to provide guidance regarding what does and does not impact suicide-related outcomes in young people. Despite this, some limitations must be addressed.
Firstly, the broad scope of the review, together with time and resource constraints, required us to make a number of pragmatic methodological decisions. For example, we adopted a pragmatic approach to assessing study quality, as applying standard Risk of Bias criteria to the non-RCTs would result in a low quality rating for all studies. Although we acknowledge the high risk of bias associated with non-randomized study designs, ethical and methodological barriers often prevent suicide prevention researchers from conducting RCTs. To accommodate this, the quality of non-RCTs was assessed using a tool appropriate to that design. Overall, however, study quality was limited. Indeed, many RCTs were not reported according to the Consort statement [161] and many were underpowered. Whilst this is not uncommon in suicide prevention research [144], priority needs to be given to well-designed, sufficiently powered studies. Additionally, for pragmatic reasons we did not include analysis of publication bias in our analysis of study quality. Other minor methodological limitations relate to our decisions not to prospectively register the review and not to contact key authors in the field. Although these steps are encouraged, they are not a requirement of compliance with the PRISMA statement and were not anticipated to impact the results; therefore due to time and resource constraints they were not a part of the present review.
A third limitation relates to the quality of the studies included in the meta-analysis, the results of which should be treated with caution. Additionally, on several occasions different studies contributed data to the post-intervention and follow-up outcomes. We therefore cannot be certain that changes at follow-up are in fact the result of a true reduction in the treatment effect over time. There was also heterogeneity in the control conditions and in the outcome measures used between studies, limiting our ability to be confident that studies measured the same constructs. For example, methods to assess self-harm included self-report instruments, hospital data and clinician-rated interviews. It was also often unclear if measures had been validated among young people. Researchers have previously called for the use of well-validated and standardized measures in adult suicide research, and we argue the same is required in studies with youth [162].
Finally, we acknowledge that a number of relevant studies have been published since the search was conducted. For example, a 2018 RCT trial found no benefit of systemic family therapy compared to treatment as usual in reducing subsequent hospital presentations for young people who self-harm [163]. Another RCT found DBT was more effective in reducing repeat suicide attempts in adolescents, compared to individual and group supportive therapy [164]. Although these studies both meet criteria for inclusion in the current review they were published after our search was conducted.
5. Conclusion
This review identified a large number of studies testing a broad range of interventions across multiple settings. We found that some interventions for example, brief contact interventions in clinical settings, and psychoeducation combined with screening in school settings can reduce the frequency of self-harm and suicidal ideation, although it is likely the size of these studies that is driving the effects. Large-scale multimodal interventions also show promise. Despite these promising findings there remains a paucity of high-quality youth suicide prevention intervention studies. Whilst not all interventions lend themselves to testing via RCTs, other robust study designs can and should be employed. Additionally, many studies, particularly those in clinical and community settings, tend to test interventions originally designed for adults. By focusing suicide prevention efforts on generic, as opposed to youth-specific, interventions, we are likely missing crucial opportunities for intervention, such as delivery via online platforms. Future research should adapt known effective interventions for young people, and for delivery online. A focus on university and workplace settings is also warranted.
Although young people have repeatedly been identified by suicide prevention policy as a group requiring specific attention, their suicide rates are rising. To reverse this trend, we need more large-scale methodologically-rigorous studies that develop and test new approaches. These approaches should be acceptable to all young people and capitalize on the ways in which young people interact with the health system, supports, and services.
The following is the supplementary data related to this article.
Search terms.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eclinm.2018.10.004.
Acknowledgments
Acknowledgments
Funding from the Future Global Generations Fund and the William Buckland Foundation supported several of the research assistants (including EB and NS). JR is supported by a NHMRC Career Development Fellowship. SH is supported by an Auckland Medical Research Foundation Douglas Goodfellow Repatriation Fellowship. AM is supported by the Victorian Health and Medical Research Fellowship. KW is supported by a post-doctoral fellowship awarded by the American Foundation for Suicide Prevention.
The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Outstanding Questions
-
•
Despite the encouraging findings, key questions remain as to exactly which components of interventions, in particular those delivered in clinical settings, are most effective when it comes to reducing suicide risk among young people.
-
•
There is also a pressing need for large-scale high quality trials in clinical, educational and community settings. This includes in primary care, tertiary education and online settings, which are currently largely negelected.
-
•
Questions also remain as to what interventions are most likely to be effective in sub-sections of the population, including among indigenous young people, those who live in low to middle income countries, and those who identify as same sex attracted and/or gender diverse.
Author Contributions
Jo Robinson obtained funds for the study. She oversaw the design and conduct of the review, including data extraction, analysis and interpretation. She wrote the manuscript. She also played a leading role in the design of the search strategy.
Eleanor Bailey was responsible for conducting the literature search and coordinating the screening and data extraction phases. She also assisted with designing the search strategy, screening, data extraction, interpretation of results and preparation of the manuscript.
Katrina Witt assisted with screening and data extraction, and was responsible for conducting and interpreting the meta-analysis together with Sarah Hetrick.
Nina Stefanac assisted with screening, data extraction and preparation of the manuscript.
Allison Milner assisted with screening and data extraction.
Dianne Currier assisted with screening and data extraction.
Jane Pirkis provided methodological and conceptual advice. She also contributed to writing the manuscript.
Patrick Condron assisted with the development of the search strategy.
Sarah Hetrick assisted with the development of the search, assisted with screening and data extraction, was responsible for conducting and interpreting the meta-analysis together with Katrina Witt, and provided general oversight to the study.
References
- 1.World Health Organization . World Health Organization; Switzerland: 2014. Preventing suicide: a global imperative. [Google Scholar]
- 2.Hawton K., Zahl D., Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182(6):537–542. doi: 10.1192/bjp.182.6.537. [DOI] [PubMed] [Google Scholar]
- 3.Geulayov G., Kapur N., Turnbull P. Epidemiology and trends in non-fatal self-harm in three centres in England, 2000–2012: findings from the Multicentre Study of Self-harm in England. BMJ Open. 2016:6(4). doi: 10.1136/bmjopen-2015-010538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nock M., Green J., Hwang I. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the national comorbidity survey replication adolescent supplement. JAMA Psychiat. 2013;70(3):300–310. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawton K., Harriss L. Deliberate self-harm in young people: characteristics and subsequent mortality in a 20-year cohort of patients presenting to hospital. J Clin Psychiatry. 2007;68:1574–1583. [PubMed] [Google Scholar]
- 6.Hunt I.M., Kapur N., Webb R. Suicide in recently discharged psychiatric patients: a case-control study. Psychol Med. 2009;39(3):443–449. doi: 10.1017/S0033291708003644. [DOI] [PubMed] [Google Scholar]
- 7.Commonwealth Government Department of Health and Aging . Author; Canberra, Australia: 2007. Living is for everyone (LiFE) framework. [Google Scholar]
- 8.New Zealand Government . Author; New Zealand: 2013. New Zealand suicide prevention action plan 2013–2016. [Google Scholar]
- 9.U.S. Department of Health and Human Services . Office of the Surgeon General and National Action Alliance for Suicide Prevention; Washington, D.C.: 2012. National Strategy for Suicide Prevention: goals and objectives for action. [PubMed] [Google Scholar]
- 10.Patton G.C., Sawyer S.M., Santelli J.S. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–2478. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Mental Health Commission . Sydney, Australia; Author: 2017. The 2017 report on mental health and suicide prevention. [Google Scholar]
- 12.Hawton K., Pirkis J. Suicide is a complex problem that requires a range of prevention initiatives and methods of evaluation. Br J Psychiatry. 2017;210(6):381. doi: 10.1192/bjp.bp.116.197459. [DOI] [PubMed] [Google Scholar]
- 13.Goldney R. Suicide prevention: a pragmatic review of recent studies. Crisis. 2005;26:128–140. doi: 10.1027/0227-5910.26.3.128. [DOI] [PubMed] [Google Scholar]
- 14.Calear A., Christensen H., Freeman A. A systematic review of psychosocial suicide prevention interventions for youth. Eur Child Adolesc Psychiatry. 2016;25:467–482. doi: 10.1007/s00787-015-0783-4. [DOI] [PubMed] [Google Scholar]
- 15.Robinson J., Cox G., Malone A. A systematic review of school based interventions aimed at preventing, treating, and responding to, suicide-related behaviour in young people. Crisis. 2012;28:1–19. doi: 10.1027/0227-5910/a000168. [DOI] [PubMed] [Google Scholar]
- 16.Isaac M., Elias B., Katz L. Gatekeeper training as a preventative intervention for suicide: a systematic review. Can J Psychiatr. 2009;54(4):260–268. doi: 10.1177/070674370905400407. [DOI] [PubMed] [Google Scholar]
- 17.Mann J., Apter A., Bertolote J. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 18.Zalsman G., Hawton K., Wasserman D. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry. 2017;3:646–659. doi: 10.1016/S2215-0366(16)30030-X. [DOI] [PubMed] [Google Scholar]
- 19.Higgins J., Altman D., Sterne J. Assessing risk of bias in included studies. In: Higgins J., editor. Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration; 2011. [Google Scholar]
- 20.Moher D., Liberati A., Tetzlaff J., Altman D. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009;6(6) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 22.Mak H., Yau K., Chan B. Prevalence-adjusted bias-adjusted kappa values as additional indicators to measure observer agreement. Radiology. 2004;232:302–303. doi: 10.1148/radiol.2321031974. [DOI] [PubMed] [Google Scholar]
- 23.Robinson J., Hetrick S., Martin C. Preventing suicide in young people: systematic review. Aust N Z J Psychiatry. 2011;45(1):3–26. doi: 10.3109/00048674.2010.511147. [DOI] [PubMed] [Google Scholar]
- 24.Hawton K., Witt K.G., Taylor Salisbury T.L. Interventions for self-harm in children and adolescents. Cochrane Database Syst Rev. 2015;12 doi: 10.1002/14651858.CD012013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Norwegian Knowledge Centre for the Health Services . 2015. Effective Practice and Organisation of Care (EPOC). EPOC Resources for review authors Oslo. [Google Scholar]
- 26.Cochrane Effective Practice and Organisation of Care (EPOC) Suggested risk of bias criteria for EPOC reviews. 2017. http://epoc.cochrane.org/resources/epoc-resources-review-authors
- 27.Hawton K., Bergen H., Cooper J. Suicide following self-harm: Findings from the Multicentre Study of self-harm in England, 2000–2012. J Affect Disord. 2015;175:147–151. doi: 10.1016/j.jad.2014.12.062. [DOI] [PubMed] [Google Scholar]
- 28.Rücker G., Cates C.J., Schwarzer G. Methods for including information from multi-arm trials in pairwise meta-analysis. Res Synth Methods. 2017;8(4):392–403. doi: 10.1002/jrsm.1259. [DOI] [PubMed] [Google Scholar]
- 29.Pace N.L. Research methods for meta-analyses. Clinical Anaesthesiology. 2011;25(4):523–533. doi: 10.1016/j.bpa.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Dersimonian R., Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(177–88) doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 31.Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H.R. Biostat, Inc.; Englewood, NJ: 2011. Comprehensive meta-analysis. 2.2.064 ed. [Google Scholar]
- 32.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Br Med J. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Milner A., Carter G., Pirkis J., Robinson J., Spittal M. Letters, green cards, telephone calls, and postcards: a systematic and meta-analytic review of brief contact interventions for reducing self-harm, suicide attempts, and suicide. Br J Psychiatry. 2015;206:184–190. doi: 10.1192/bjp.bp.114.147819. [DOI] [PubMed] [Google Scholar]
- 34.Fleischmann A., Bertolote J.M., Wasserman D. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bull World Health Organ. 2008;86(9):703–709. doi: 10.2471/BLT.07.046995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rotheram-Borus M.J., Piacentini J., Cantwell C., Belin T.R., Song J. The 18-month impact of an emergency room intervention for adolescent female suicide attempters. J Consult Clin Psychol. 2000;68(6):1081–1093. doi: 10.1037//0022-006x.68.6.1081. [DOI] [PubMed] [Google Scholar]
- 36.Eggert L., Thompson E., Herting J., Nicholas L. Reducing suicide potential among high-risk youth: tests of a school-based prevention program. Erratum. Suicide Life Threat Behav. 1999:29(96). [PubMed] [Google Scholar]
- 37.Silverstone P.H., Bercov M., Suen V.Y.M. Long-term results from the Empowering a Multimodal Pathway Toward Healthy Youth Program, a multimodal school-based approach, show marked reductions in suicidality, depression, and anxiety in 6227 students in grades 6–12 (aged 11–18) Front Psychiatry. 2017;8:81. doi: 10.3389/fpsyt.2017.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walrath C., Garraza L.G., Reid H., Goldston D.B., McKeon R. Impact of the Garrett Lee Smith youth suicide prevention program on suicide mortality. Am J Public Health. 2015;105(5):986–993. doi: 10.2105/AJPH.2014.302496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ougrin D., Boege I., Stahl D., Banarsee R., Taylor E. Randomised controlled trial of therapeutic assessment versus usual assessment in adolescents with self-harm: 2-year follow-up. Arch Dis Child. 2013;98(10):772–776. doi: 10.1136/archdischild-2012-303200. [DOI] [PubMed] [Google Scholar]
- 40.Rudd M.D., Rajab M.H., Orman D.T., Joiner T., Stulman D.A., Dixon W. Effectiveness of an outpatient intervention targeting suicidal young adults: preliminary results. J Consult Clin Psychol. 1996;64(1):179–190. doi: 10.1037//0022-006x.64.1.179. [DOI] [PubMed] [Google Scholar]
- 41.Alavi A., Sharifi B., Ghanizadeh A., Dehbozorgi G. Effectiveness of cognitive-behavioral therapy in decreasing suicidal ideation and hopelessness of the adolescents with previous suicidal attempts. Iran J Pediatr. 2013;23(4):467–472. [PMC free article] [PubMed] [Google Scholar]
- 42.Asarnow J.R., Hughes J.L., Babeva K.N., Sugar C.A. Cognitive-behavioral family treatment for suicide attempt prevention: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2017;56(6):506–514. doi: 10.1016/j.jaac.2017.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Byford S., Harrington R., Torgerson D. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. Br J Psychiatry. 1999;174:56–62. doi: 10.1192/bjp.174.1.56. [DOI] [PubMed] [Google Scholar]
- 44.Carter G.L., Willcox C.H., Lewin T.J., Conrad A.M., Bendit N. Hunter DBT project: randomized controlled trial of dialectical behaviour therapy in women with borderline personality disorder. Aust N Z J Psychiatry. 2010;44(2):162–173. doi: 10.3109/00048670903393621. [DOI] [PubMed] [Google Scholar]
- 45.Cooney E., Davis K., Thompson P., Wharewera-Mika J., Stewart J. Te Pou o Te Whakaaro Nui; Auckland, New Zealand: 2010. Feasibility of evaluating DBT for self-harming adolescents: A small randomised controlled trial. [Google Scholar]
- 46.Diamond G.S., Wintersteen M.B., Brown G.K. Attachment-based family therapy for adolescents with suicidal ideation: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2010;49(2):122–131. doi: 10.1097/00004583-201002000-00006. [DOI] [PubMed] [Google Scholar]
- 47.Donaldson D., Spirito A., Esposito-Smythers C. Treatment for adolescents following a suicide attempt: results of a pilot trial. J Am Acad Child Adolesc Psychiatry. 2005;44(2):113–120. doi: 10.1097/00004583-200502000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Esposito-Smythers C., Spirito A., Kahler C.W., Hunt J., Monti P. Treatment of co-occurring substance abuse and suicidality among adolescents: a randomized trial. J Consult Clin Psychol. 2011;79(6):728–739. doi: 10.1037/a0026074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Green J.M., Wood A.J., Kerfoot M.J. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ. 2011;342:d682. doi: 10.1136/bmj.d682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harrington R., Kerfoot M., Dyer E. Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves. J Am Acad Child Adolesc Psychiatry. 1998;37(5):512–518. [PubMed] [Google Scholar]
- 51.Hazell P.L., Martin G., McGill K. Group therapy for repeated deliberate self-harm in adolescents: failure of replication of a randomized trial. J Am Acad Child Adolesc Psychiatry. 2009;48(6):662–670. doi: 10.1097/CHI.0b013e3181aOacec. [DOI] [PubMed] [Google Scholar]
- 52.Huey S.J., Jr., Henggeler S.W., Rowland M.D. Multisystemic therapy effects on attempted suicide by youths presenting psychiatric emergencies. J Am Acad Child Adolesc Psychiatry. 2004;43(2):183–190. doi: 10.1097/00004583-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 53.Husain N., Afsar S., Ara J. Brief psychological intervention after self-harm: randomised controlled trial from Pakistan. Br J Psychiatry. 2014;204(6):462–470. doi: 10.1192/bjp.bp.113.138370. [DOI] [PubMed] [Google Scholar]
- 54.King C.A., Kramer A., Preuss L., Kerr D.C., Weisse L., Venkataraman S. Youth-Nominated Support Team for Suicidal Adolescents (version 1): a randomized controlled trial. J Consult Clin Psychol. 2006;74(1):199–206. doi: 10.1037/0022-006X.74.1.199. [DOI] [PubMed] [Google Scholar]
- 55.King C.A., Klaus N., Kramer A., Venkataraman S., Quinlan P., Gillespie B. The Youth-Nominated Support Team-Version II for suicidal adolescents: a randomized controlled intervention trial. J Consult Clin Psychol. 2009;77(5):880–893. doi: 10.1037/a0016552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.King C.A., Gipson P.Y., Horwitz A.G., Opperman K.J. Teen Options for Change (TOC): an intervention for adolescent emergency patients who screen positive for suicide risk. Psychiatr Serv. 2015;66(1):97–100. doi: 10.1176/appi.ps.201300347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McLeavey B.C., Daly R.J., Ludgate J.W., Murray C.M. Interpersonal problem-solving skills training in the treatment of self-poisoning patients. Suicide Life Threat Behav. 1994;24(4):382–394. [PubMed] [Google Scholar]
- 58.Mehlum L., Ramberg M., Tormoen A.J. Dialectical behavior therapy compared with enhanced usual care for adolescents with repeated suicidal and self-harming behavior: outcomes over a one-year follow-up. J Am Acad Child Adolesc Psychiatry. 2016;55(4):295–300. doi: 10.1016/j.jaac.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 59.Pineda J., Dadds M.R. Family intervention for adolescents with suicidal behavior: a randomized controlled trial and mediation analysis. J Am Acad Child Adolesc Psychiatry. 2013;52(8):851–862. doi: 10.1016/j.jaac.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 60.Power P.J., Bell R.J., Mills R. Suicide prevention in first episode psychosis: the development of a randomised controlled trial of cognitive therapy for acutely suicidal patients with early psychosis. Aust N Z J Psychiatry. 2003;37(4):414–420. doi: 10.1046/j.1440-1614.2003.01209.x. [DOI] [PubMed] [Google Scholar]
- 61.Rossouw T.I., Fonagy P. Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2012;51(12) doi: 10.1016/j.jaac.2012.09.018. [1304–13.e3] [DOI] [PubMed] [Google Scholar]
- 62.Slee N., Garnefski N., van der Leeden R., Arensman E., Spinhoven P. Cognitive-behavioural intervention for self-harm: randomised controlled trial. Br J Psychiatry. 2008;192(3):202–211. doi: 10.1192/bjp.bp.107.037564. [DOI] [PubMed] [Google Scholar]
- 63.Wharff E.A., Ginnis K.B., Ross A.M., White E.M., White M.T., Forbes P.W. Family-based crisis intervention with suicidal adolescents: a randomized clinical trial. Pediatr Emerg Care. 2017 doi: 10.1097/PEC.0000000000001076. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 64.Wood A., Trainor G., Rothwell J., Moore A., Harrington R. Randomized trial of group therapy for repeated deliberate self-harm in adolescents. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1246–1253. doi: 10.1097/00004583-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 65.Asarnow J.R., Baraff L.J., Berk M. An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatr Serv. 2011;62(11):1303–1309. doi: 10.1176/appi.ps.62.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bertolote J.M., Fleischmann A., De Leo D. Repetition of suicide attempts: data from emergency care settings in five culturally different low- and middle-income countries participating in the WHO SUPRE-MISS study. Crisis. 2010;31(4):194–201. doi: 10.1027/0027-5910/a000052. [DOI] [PubMed] [Google Scholar]
- 67.Cotgrove A., Zirinsky L., Black D., Weston D. Secondary prevention of attempted suicide in adolescence. J Adolesc. 1995;18(5):569–577. [Google Scholar]
- 68.Hassanian-Moghaddam H., Sarjami S., Kolahi A.A., Carter G.L. Postcards in Persia: randomised controlled trial to reduce suicidal behaviours 12 months after hospital-treated self-poisoning. Br J Psychiatry. 2011;198(4):309–316. doi: 10.1192/bjp.bp.109.067199. [DOI] [PubMed] [Google Scholar]
- 69.Ougrin D., Zundel T., Banarsee R., Bottle A., Taylor E. Trial of Therapeutic Assessment in London: randomised controlled trial of Therapeutic Assessment versus standard psychosocial assessment in adolescents presenting with self-harm. Arch Dis Child. 2011;96(2):148–153. doi: 10.1136/adc.2010.188755. [DOI] [PubMed] [Google Scholar]
- 70.Robinson J., Yuen H., Gook S. Can receipt of a regular postcard reduce suicide-related behaviour in young help seekers? A randomized controlled trial. Early Interv Psychiatry. 2012;6(2):145–152. doi: 10.1111/j.1751-7893.2011.00334.x. [DOI] [PubMed] [Google Scholar]
- 71.Spirito A., Boergers J., Donaldson D., Bishop D., Lewander W. An intervention trial to improve adherence to community treatment by adolescents after a suicide attempt. J Am Acad Child Adolesc Psychiatry. 2002;41(4):435–442. doi: 10.1097/00004583-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 72.Spirito A., Wolff J.C., Seaboyer L.M. Concurrent treatment for adolescent and parent depressed mood and suicidality: feasibility, acceptability, and preliminary findings. J Child Adolesc Psychopharmacol. 2015;25(2):131–139. doi: 10.1089/cap.2013.0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Asarnow J.R., Berk M., Hughes J.L., Anderson N.L. The SAFETY Program: a treatment-development trial of a cognitive-behavioral family treatment for adolescent suicide attempters. J Clin Child Adolesc Psychol. 2015;44(1):194–203. doi: 10.1080/15374416.2014.940624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Courtney D.B., Flament M.F. Adapted dialectical behavior therapy for adolescents with self-injurious thoughts and behaviors. J Nerv Ment Dis. 2015;203(7):537–544. doi: 10.1097/NMD.0000000000000324. [DOI] [PubMed] [Google Scholar]
- 75.Duarte-Velez Y., Torres-Davila P., Spirito A., Polanco N., Bernal G. Development of a treatment protocol for Puerto Rican adolescents with suicidal behaviors. Psychotherapy. 2016;53(1):45–56. doi: 10.1037/pst0000044. [DOI] [PubMed] [Google Scholar]
- 76.Esposito-Smythers C., Spirito A., Uth R., Lachance H. Cognitive behavioral treatment for suicidal alcohol abusing adolescents: development and pilot testing. Am J Addict. 2006;15(Suppl. 1):126–130. doi: 10.1080/10550490601003631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Geddes K., Dziurawiec S., Lee C.W. Dialectical behaviour therapy for the treatment of emotion dysregulation and trauma symptoms in self-injurious and suicidal adolescent females: a pilot programme within a community-based child and adolescent mental health service. Psychiatry J. 2013;2013:10. doi: 10.1155/2013/145219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gutstein S.E., Rudd M.D. An outpatient treatment alternative for suicidal youth. J Adolesc. 1990;13(3):265–277. doi: 10.1016/0140-1971(90)90018-3. [DOI] [PubMed] [Google Scholar]
- 79.James A.C., Winmill L., Anderson C., Alfoadari K. A preliminary study of an extension of a community dialectic behaviour therapy (DBT) programme to adolescents in the looked after care system. Child Adolesc Mental Health. 2011;16(1):9–13. doi: 10.1111/j.1475-3588.2010.00571.x. [DOI] [PubMed] [Google Scholar]
- 80.James S., Freeman K.R., Mayo D. Does insurance matter? Implementing dialectical behavior therapy with two groups of youth engaged in deliberate self-harm. Admin Pol Ment Health. 2015;42(4):449–461. doi: 10.1007/s10488-014-0588-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.King R., Nurcombe B., Bickman L., Hides L., Reid W. Telephone counselling for adolescent suicide prevention: changes in suicidality and mental state from beginning to end of a counselling session. Suicide Life Threat Behav. 2003;33(4):400–411. doi: 10.1521/suli.33.4.400.25235. [DOI] [PubMed] [Google Scholar]
- 82.Cwik M.F., Tingey L., Lee A. Development and piloting of a brief intervention for suicidal American Indian adolescents. Am Indian Alsk Native Ment Health Res. 2016;23(1):105–124. doi: 10.5820/aian.2301.2016.105. [DOI] [PubMed] [Google Scholar]
- 83.Diamond G.M., Diamond G.S., Levy S., Closs C., Ladipo T., Siqueland L. Attachment-based family therapy for suicidal lesbian, gay, and bisexual adolescents: a treatment development study and open trial with preliminary findings. Psychol Sex Orientat Gend Divers. 2013;1(S):91–100. doi: 10.1037/a0026247. [DOI] [PubMed] [Google Scholar]
- 84.Katz L.Y., Cox B.J., Gunasekara S., Miller A.L. Feasibility of dialectical behavior therapy for suicidal adolescent inpatients. J Am Acad Child Adolesc Psychiatry. 2004;43(3):276–282. doi: 10.1097/00004583-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 85.Law Y.W., Yip P.S., Lai C.C. A pilot study on the efficacy of volunteer mentorship for young adults with self-harm behaviors using a quasi-experimental design. Crisis. 2016;37(6):415–426. doi: 10.1027/0227-5910/a000393. [DOI] [PubMed] [Google Scholar]
- 86.Oldershaw A., Simic M., Grima E. The effect of cognitive behavior therapy on decision making in adolescents who self-harm: a pilot study. Suicide Life Threat Behav. 2012;42(3):255–265. doi: 10.1111/j.1943-278X.2012.0087.x. [DOI] [PubMed] [Google Scholar]
- 87.Perera E.A., Kathriarachchi S.T. Problem-solving counseling as a therapeutic tool on youth suicidal behavior in the suburban population in Sri Lanka. Indian J Psychiatry. 2011;53(1):30–35. doi: 10.4103/0019-5545.75558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rathus J.H., Miller A.L. Dialectical behavior therapy adapted for suicidal adolescents. Suicide Life Threat Behav. 2002;32(2):146–157. doi: 10.1521/suli.32.2.146.24399. [DOI] [PubMed] [Google Scholar]
- 89.Rotheram-Borus M.J., Piacentini J., Van Rossem R. Enhancing treatment adherence with a specialized emergency room program for adolescent suicide attempters. J Am Acad Child Adolesc Psychiatry. 1996;35(5):654–663. doi: 10.1097/00004583-199605000-00021. [DOI] [PubMed] [Google Scholar]
- 90.Wharff E.A., Ginnis K.M., Ross A.M. Family-based crisis intervention with suicidal adolescents in the emergency room: a pilot study. Soc Work. 2012;57(2):133–143. doi: 10.1093/sw/sws017. [DOI] [PubMed] [Google Scholar]
- 91.Brent D.A., Greenhill L.L., Compton S. The Treatment of Adolescent Suicide Attempters study (TASA): predictors of suicidal events in an open treatment trial. J Am Acad Child Adolesc Psychiatry. 2009;48(10):987–996. doi: 10.1097/CHI.0b013e3181b5dbe4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Orbach I., Bar-Joseph H. The impact of a suicide prevention program for adolescents on suicidal tendencies, hopelessness, ego identity, and coping. Suicide Life Threat Behav. 1993;23(2):120–129. [PubMed] [Google Scholar]
- 93.Lafromboise T., Howard-Pitney B. The Zuni Life Skills Development Curriculum: a collaborative approach to curriculum development. Am Indian Alsk Native Ment Health Res Monogr Ser. 1994;4:98–121. doi: 10.5820/aian.mono04.1994.98. [DOI] [PubMed] [Google Scholar]
- 94.Lafromboise T., Howard-Pitney B. The Zuni Life Skills Development Curriculum: description and evaluation of a suicide prevention program. J Couns Psychol. 1995;42(4):479–486. [Google Scholar]
- 95.Eggert L.L., Thompson E.A., Randell B.P., Pike K.C. Preliminary effects of brief school-based prevention approaches for reducing youth suicide-risk behaviors, depression, and drug involvement. J Child Adolesc Psychiatr Nurs. 2002;15(2):48–64. doi: 10.1111/j.1744-6171.2002.tb00326.x. [DOI] [PubMed] [Google Scholar]
- 96.Hooven C., Walsh E., Pike K.C., Herting J.R. Promoting CARE: including parents in youth suicide prevention. Fam Community Health. 2012;35(3):225–235. doi: 10.1097/FCH.0b013e318250bcf9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Robinson W.L., Case M.H., Whipple C.R. Culturally grounded stress reduction and suicide prevention for African American adolescents. Pract Innov (Wash DC) 2016;1(2):117–128. doi: 10.1037/pri0000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tang T.C., Jou S.H., Ko C.H., Huang S.Y., Yen C.F. Randomized study of school-based intensive interpersonal psychotherapy for depressed adolescents with suicidal risk and parasuicide behaviors. Psychiatry Clin Neurosci. 2009;63(4):463–470. doi: 10.1111/j.1440-1819.2009.01991.x. [DOI] [PubMed] [Google Scholar]
- 99.Schilling E.A., Aseltine R.H., Jr., James A. The SOS Suicide Prevention Program: further evidence of efficacy and effectiveness. Prev Sci. 2016;17(2):157–166. doi: 10.1007/s11121-015-0594-3. [DOI] [PubMed] [Google Scholar]
- 100.Schilling E.A., Lawless M., Buchanan L., Aseltine R.H., Jr. “Signs of Suicide” shows promise as a middle school suicide prevention program. Suicide Life Threat Behav. 2014;44(6):653–667. doi: 10.1111/sltb.12097. [DOI] [PubMed] [Google Scholar]
- 101.Wasserman D., Hoven C.W., Wasserman C. School-based suicide prevention programmes: the SEYLE cluster-randomised, controlled trial. Lancet. 2015;385(9977):1536–1544. doi: 10.1016/S0140-6736(14)61213-7. [DOI] [PubMed] [Google Scholar]
- 102.King K.A., Strunk C.M., Sorter M.T. Preliminary effectiveness of surviving the teens suicide prevention and depression awareness program on adolescents' suicidality and self-efficacy in performing help-seeking behaviors. J Sch Health. 2011;81(9):581–590. doi: 10.1111/j.1746-1561.2011.00630.x. [DOI] [PubMed] [Google Scholar]
- 103.Vieland V., Whittle B., Garland A., Hicks R., Shaffer D. The impact of curriculum-based suicide prevention programs for teenagers: an 18-month follow-up. J Am Acad Child Adolesc Psychiatry. 1991;30(5):811–815. [PubMed] [Google Scholar]
- 104.Hazell P., Lewin T. An evaluation of postvention following adolescent suicide. Suicide Life Threat Behav. 1993;23(2):101–109. [PubMed] [Google Scholar]
- 105.Biddle V.S., Kern J., 3rd, Brent D.A., Thurkettle M.A., Puskar K.R., Sekula L.K. Student assistance program outcomes for students at risk for suicide. J Sch Nurs. 2014;30(3):173–186. doi: 10.1177/1059840514525968. [DOI] [PubMed] [Google Scholar]
- 106.Eggert L.L., Thompson E.A., Herting J.R., Nicholas L.J. Reducing suicide potential among high-risk youth: tests of a school-based prevention program. Suicide Life Threat Behav. 1995;25(2):276–296. [PubMed] [Google Scholar]
- 107.Aseltine R.H., Jr., James A., Schilling E.A., Glanovsky J. Evaluating the SOS suicide prevention program: a replication and extension. BMC Public Health. 2007;7:161. doi: 10.1186/1471-2458-7-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Silverstone P.H., Bercov M., Suen V.Y.M. Initial findings from a novel school-based program, EMPATHY, which may help reduce depression and suicidality in youth. PLoS One. 2015;10(5) doi: 10.1371/journal.pone.0125527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zenere F.J., 3rd, Lazarus P.J. The decline of youth suicidal behavior in an urban, multicultural public school system following the introduction of a suicide prevention and intervention program. Suicide Life Threat Behav. 1997;27(4):387–402. [PubMed] [Google Scholar]
- 110.Bailey E., Spittal M.J., Pirkis J., Gould M., Robinson J. Universal suicide prevention in young people: an evaluation of the safeTALK program in Australian high schools. Crisis. 2017;38(5):300–308. doi: 10.1027/0227-5910/a000465. [DOI] [PubMed] [Google Scholar]
- 111.Hetrick S., Yuen H.P., Cox G. Does cognitive behavioural therapy have a role in improving problem solving and coping in adolescents with suicidal ideation? Cogn Behav Ther. 2014;7 [Google Scholar]
- 112.Robinson J., Hetrick S., Cox G. Can an internet-based intervention reduce suicidal ideation, depression and hopelessness among secondary school students: results from a pilot study. Early Interv Psychiatry. 2016;10(1):28–35. doi: 10.1111/eip.12137. [DOI] [PubMed] [Google Scholar]
- 113.Guille C., Zhao Z., Krystal J., Nichols B., Brady K., Sen S. Web-based cognitive behavioral therapy intervention for the prevention of suicidal ideation in medical interns: a randomized clinical trial. JAMA Psychiat. 2015;72(12):1192–1198. doi: 10.1001/jamapsychiatry.2015.1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kovac S.H., Range L.M. Does writing about suicidal thoughts and feelings reduce them? Suicide Life Threat Behav. 2002;32(4):428–440. doi: 10.1521/suli.32.4.428.22335. [DOI] [PubMed] [Google Scholar]
- 115.Fitzpatrick K.K., Witte T.K., Schmidt N.B. Randomized controlled trial of a brief problem-orientation intervention for suicidal ideation. Behav Ther. 2005;36(4):323–333. [Google Scholar]
- 116.Pistorello J., Fruzzetti A.E., Maclane C., Gallop R., Iverson K.M. Dialectical behavior therapy (DBT) applied to college students: a randomized clinical trial. J Consult Clin Psychol. 2012;80(6):982–994. doi: 10.1037/a0029096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lerner M.S., Clum G.A. Treatment of suicide ideators: a problem-solving approach. Behav Ther. 1990;21(4):403–411. [Google Scholar]
- 118.Joffe P. An empirically supported program to prevent suicide in a college student population. Suicide Life Threat Behav. 2008;38(1):87–103. doi: 10.1521/suli.2008.38.1.87. [DOI] [PubMed] [Google Scholar]
- 119.Till B., Tran U.S., Voracek M., Niederkrotenthaler T. Beneficial and harmful effects of educative suicide prevention websites: randomised controlled trial exploring Papageno v. Werther effects. Br J Psychiatry. 2017;211(2):109–115. doi: 10.1192/bjp.bp.115.177394. [DOI] [PubMed] [Google Scholar]
- 120.Shelef L., Tatsa-Laur L., Derazne E., Mann J.J., Fruchter E. An effective suicide prevention program in the Israeli Defense Forces: a cohort study. Eur Psychiatry. 2016;31:37–43. doi: 10.1016/j.eurpsy.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 121.McDaniel W.W., Rock M., Grigg J.R. Suicide prevention at a United States Navy training command. Mil Med. 1990;155(4):173–175. [PubMed] [Google Scholar]
- 122.Hill R.M., Pettit J.W. Pilot randomized controlled trial of LEAP: a selective preventive intervention to reduce adolescents' perceived burdensomeness. J Clin Child Adolesc Psychol. 2016:1–12. doi: 10.1080/15374416.2016.1188705. [DOI] [PubMed] [Google Scholar]
- 123.Hetrick S.E., Yuen H.P., Bailey E. Internet-based cognitive behavioural therapy for young people with suicide-related behaviour (Reframe-IT): a randomised controlled trial. Evid Based Ment Health. 2017;20(3):76–82. doi: 10.1136/eb-2017-102719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ahmadi A., Ytterstad B. Prevention of self-immolation by community-based intervention. Burns. 2007;33(8):1032–1040. doi: 10.1016/j.burns.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 125.Beautrais A.L., Fergusson D.M., Horwood L.J. Firearms legislation and reductions in firearm-related suicide deaths in New Zealand. Aust N Z J Psychiatry. 2006;40(3):253–259. doi: 10.1080/j.1440-1614.2006.01782.x. [DOI] [PubMed] [Google Scholar]
- 126.Caron J. Gun control and suicide: possible impact of Canadian legislation to ensure safe storage of firearms. Arch Suicide Res. 2004;8(4):361–374. doi: 10.1080/13811110490476752. [DOI] [PubMed] [Google Scholar]
- 127.Center for Disease Control Suicide prevention evaluation in a Western Athabaskan American Indian Tribe-New Mexico, 1988–1997. MMWR Morb Mortal Wkly Rep. 1998;47(13):257–261. [PubMed] [Google Scholar]
- 128.Cheung A.H., Dewa C.S. Current trends in youth suicide and firearms regulations. Can J Public Health. 2005;96(2):131–135. doi: 10.1007/BF03403676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cwik M.F., Tingey L., Maschino A. Decreases in suicide deaths and attempts linked to the White Mountain apache suicide surveillance and prevention system, 2001–2012. Am J Public Health. 2016;106(12):2183–2189. doi: 10.2105/AJPH.2016.303453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hacker K., Collins J., Gross-Young L., Almeida S., Burke N. Coping with youth suicide and overdose: one community's efforts to investigate, intervene, and prevent suicide contagion. Crisis. 2008;29(2):86–95. doi: 10.1027/0227-5910.29.2.86. [DOI] [PubMed] [Google Scholar]
- 131.Leenaars A.A., Lester D. The impact of gun control on suicide and homicide across the life span. Can J Behav Sci. 1997;29(1):1–6. [Google Scholar]
- 132.Lubin G., Werbeloff N., Halperin D., Shmushkevitch M., Weiser M., Knobler H.Y. Decrease in suicide rates after a change of policy reducing access to firearms in adolescents: a naturalistic epidemiological study. Suicide Life Threat Behav. 2010;40(5):421–424. doi: 10.1521/suli.2010.40.5.421. [DOI] [PubMed] [Google Scholar]
- 133.Matsubayashi T., Ueda M. The effect of national suicide prevention programs on suicide rates in 21 OECD nations. Soc Sci Med. 2011;73(9):1395–1400. doi: 10.1016/j.socscimed.2011.08.022. [DOI] [PubMed] [Google Scholar]
- 134.May P.A., Serna P., Hurt L., Debruyn L.M. Outcome evaluation of a public health approach to suicide prevention in an American Indian tribal nation. Am J Public Health. 2005;95(7):1238–1244. doi: 10.2105/AJPH.2004.040410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Niederkrotenthaler T., Till B., Herberth A. Can media effects counteract legislation reforms? The case of adolescent firearm suicides in the wake of the Austrian firearm legislation. J Adolesc Health. 2009;44(1):90–93. doi: 10.1016/j.jadohealth.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 136.Wheeler B.W., Gunnell D., Metcalfe C., Stephens P., Martin R.M. The population impact on incidence of suicide and non-fatal self harm of regulatory action against the use of selective serotonin reuptake inhibitors in under 18s in the United Kingdom: ecological study. BMJ. 2008;336(7643):542–545. doi: 10.1136/bmj.39462.375613.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wheeler B.W., Metcalfe C., Martin R.M., Gunnell D. International impacts of regulatory action to limit antidepressant prescribing on rates of suicide in young people. Pharmacoepidemiol Drug Saf. 2009;18(7):579–588. doi: 10.1002/pds.1753. [DOI] [PubMed] [Google Scholar]
- 138.Allen J., Rasmus S.M., Fok C.C.T., Charles B., Henry D. Multi-level cultural intervention for the prevention of suicide and alcohol use risk with Alaska Native youth: a nonrandomized comparison of treatment intensity. Prev Sci. 2017 doi: 10.1007/s11121-017-0798-9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Garraza L., Walrath C., Goldston D.B., Reid H., McKeon R. Effect of the garrett lee smith memorial suicide prevention program on suicide attempts among youths. JAMA Psychiat. 2015;72(11):1143–1149. doi: 10.1001/jamapsychiatry.2015.1933. [DOI] [PubMed] [Google Scholar]
- 140.Robinson J., Pirkis J. Research priorities in suicide prevention: an examination of Australian-based research 2007–11. Aust Health Rev. 2014;38(1):18–24. doi: 10.1071/AH13058. [DOI] [PubMed] [Google Scholar]
- 141.Dahl R., Allen N., Ballonoff Suleimna A. Importance of investing in adolescence from a developmental science perspective. Nature. 2018;554:441–450. doi: 10.1038/nature25770. [DOI] [PubMed] [Google Scholar]
- 142.Robinson J., Bailey E., Browne V., Cox G., Hooper C. The National Centre of Excellence in Youth Mental Health; Melbourne: Orygen: 2016. Raising the Bar for youth suicide prevention. [Google Scholar]
- 143.Ougrin D., Tranah T., Stahl D., Moran P., Asarnow J.R. Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2015;54(2) doi: 10.1016/j.jaac.2014.10.009. [97–107.e2] [DOI] [PubMed] [Google Scholar]
- 144.Arensman E., Townsend E., Hawton K. Psychosocial and pharmacological treatment of patients following deliberate self-harm: the methodological issues involved in evaluating effectiveness. Suicide Life Threat Behav. 2001;31(2) doi: 10.1521/suli.31.2.169.21516. [DOI] [PubMed] [Google Scholar]
- 145.Sveticic J., De Leo D. The hypothesis of a continuum in suicidality: a discussion on its validity and practical implications. Ment Illn. 2012;2 doi: 10.4081/mi.2012.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.O'Connor R.C. Towards an integrated motivational–volitional model of suicidal behaviour. In: O'Connor R.C., Platt S., Gordon J., editors. Handbook of suicide prevention: research, policy and practice. Chichester, UK; John Wiley & Sons, Ltd.: 2011. [Google Scholar]
- 147.Witt K., Milner A., Spittal M. Population attributable risk of factors associated with the repetition of self-harm behaviour in young people presenting to clinical services: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry. 2018 doi: 10.1007/s00787-018-1111-6. [ePub ahead of print] [DOI] [PubMed] [Google Scholar]
- 148.Krysinska K., Batterham P., Tye M. Best strategies for reducing the suicide rate in Australia. Aust N Z J Psychiatry. 2016;50(2):115–118. doi: 10.1177/0004867415620024. [DOI] [PubMed] [Google Scholar]
- 149.Hegerl U., Rummel-Kluge C., Varnik A., Arensman E., Koburger N. Alliances against depression – a community based approach to target depression and to prevent suicidal behaviour. Neurosci Biobehav Rev. 2013;37:2404–2409. doi: 10.1016/j.neubiorev.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 150.Statistics Canada . 2017. Suicide rates: An overview. [Google Scholar]
- 151.Michail M., Tait L., Churchill D. General practitioners' clinical expertise in managing suicidal young people: implications for continued education. Prim Health Care Res Dev. 2017;18:419–428. doi: 10.1017/S1463423617000299. [DOI] [PubMed] [Google Scholar]
- 152.Australian Bureau of Statistics . Commonwealth of Australia; Canberra: 2015. 3303.0 Causes of Death, Australia; p. 2016. [Google Scholar]
- 153.Milner A., Page K., Spencer-Thomas S., Lamotagne A.D. Workplace suicide prevention: a systematic review of published and unpublished activities. Health Promot Int. 2015;30(1):29–37. doi: 10.1093/heapro/dau085. [DOI] [PubMed] [Google Scholar]
- 154.Välimäki M., Anttila K., Anttila M., Lahti M. Web-based interventions supporting adolescents and young people with depressive symptoms: systematic review and meta-analysis. JMIR Mhealth And Uhealth. 2017;5(12) doi: 10.2196/mhealth.8624. [e180-e] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Witt K.G., Spittal M.J., Carter G. Effectiveness of online and mobile telephone applications (‘apps’) for the self-management of suicidal ideation and self-harm: a systematic review and meta-analysis. BMC Psychiatry. 2017;17(1):297. doi: 10.1186/s12888-017-1458-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Clifford A.C., Doran C.M., Tsey K. A systematic review of suicide prevention interventions targeting indigenous peoples in Australia, United States, Canada and New Zealand. BMC Public Health. 2013;13(1):463. doi: 10.1186/1471-2458-13-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Turban J.L.E.D. Research review: gender identity in youth: treatment paradigms and controversies. J Child Psychol Psychiatry. 2017 doi: 10.1111/jcpp.12833. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 158.Silenzio V.M.B., Duberstein P.R., Tang W., Lu N., Tu X., Homan C.M. Connecting the invisible dots: reaching lesbian, gay, and bisexual adolescents and young adults at risk for suicide through online social networks. Soc Sci Med. 2009;69(3):469–474. doi: 10.1016/j.socscimed.2009.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wendt D., Shafer K. Gender and attitudes about mental health help seeking: results from National Data. Health Soc Work. 2016;41(1) [e20–e8] [Google Scholar]
- 160.Morgan C., Webb R.T., Carr M.J. Incidence, clinical management, and mortality risk following self harm among children and adolescents: cohort study in primary care. BMJ. 2017;359 doi: 10.1136/bmj.j4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Schulz K.F., Altman D.G., Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340 doi: 10.4103/0976-500X.72352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Batterham P., Ftanou M., Pirkis J. A systematic review and evaluation of measures for suicidal ideation and behaviors in population-based research. Psychol Assess. 2015;27(2):501–512. doi: 10.1037/pas0000053. [DOI] [PubMed] [Google Scholar]
- 163.Cottrell D.J., Wright-Hughes A., Collinson M. Effectiveness of systemic family therapy versus treatment as usual for young people after self-harm: a pragmatic, phase 3, multicentre, randomised controlled trial. The Lancet Psychiatry. 2018;5(3):203–216. doi: 10.1016/S2215-0366(18)30058-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.McCauley E., Berk M.S., Asarnow J.R. Efficacy of dialectical behavior therapy for adolescents at high risk for suicide: a randomized clinical trial. JAMA Psychiat. 2018;75(8):777–785. doi: 10.1001/jamapsychiatry.2018.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search terms.