Abstract
Purpose:
Early mobilization in the intensive care unit (ICU) can improve patient outcomes but has perceived barriers to implementation. As part of an ongoing structured quality improvement project to increase mobilization of medical ICU patients by nurses and clinical technicians, we adapted the existing, validated Patient Mobilization Attitudes & Beliefs Survey (PMABS) for the ICU setting and evaluated its performance characteristics and results.
Materials and Methods:
The 26-item PMABS adapted for the ICU (PMABS-ICU) was administered as an online survey to 163 nurses, clinical technicians, respiratory therapists, attending and fellow physicians, nurse practitioners, and physician assistants in one medical ICU. We evaluated the overall and subscale (knowledge, attitude, and behavior) scores and compared these scores by respondent characteristics (clinical role and years of work experience).
Results:
The survey response rate was 96% (155/163). The survey demonstrated acceptable discriminant validity and acceptable internal consistency for the overall scale (Cronbach α: 0.82, 95% confidence interval: 0.76-0.85), with weaker internal consistency for all subscales (Cronbach α: 0.62-0.69). Across all respondent groups, the overall barrier score (range: 1-100) was relatively low, with attending physicians perceiving the lowest barriers (median [interquartile range]: 30 [28-34]) and nurses perceiving the highest (37 [31-40]). Within the first 10 years of work experience, greater experience was associated with a lower overall barrier score (−0.8 for each additional year; P = 0.02).
Conclusions:
In our medical ICU, across 6 different clinical roles, there were relatively low perceived barriers to patient mobility, with greater work experience over the first 10 years being associated with lower perceived barriers. As part of a structured quality improvement project, the PMABS-ICU may be valuable in assisting to identify specific perceived barriers for consideration in designing mobility interventions for the ICU setting.
Keywords: early mobility, rehabilitation, barriers, quality improvement, survey, multiprofessional
Introduction
Survivors of critical illness frequently experience muscle weakness and impaired physical functioning.1–5 Rehabilitation and mobilization of critically ill patients is often provided by physical and occupational therapists. Notably, mobility interventions performed by nurses also can improve patient outcomes, particularly when initiated within the first few days after intensive care unit (ICU) admission.6–11 We are currently engaged in an ongoing multiprofessional project to increase patient mobilization by nurses and clinical technicians in our medical intensive care unit (MICU), using a structured quality improvement (QI) framework.12 A key part of this QI framework is identifying initial barriers to the proposed intervention prior to designing any QI intervention.13,14 A preexisting survey was created and validated to identify barriers to mobilization of patients in the general ward setting, but no evaluation has been conducted of its psychometric performance in the ICU setting.15 Although ICU guidelines encourage early mobilization, no validated tool exists to empirically evaluate barriers to patient mobility for purposes of designing QI interventions.16,17 In administering an adaptation of this mobility barriers survey to a multiprofessional group of ICU staff, we aimed to (1) evaluate the psychometric performance of this survey in the ICU setting, (2) identify baseline barriers to patient mobility in the ICU for subsequent comparison, and (3) custom design interventions for the QI project that target local barriers.
Material and Methods
Survey Population
All nurses, clinical technicians, respiratory therapists, attending and fellow physicians, nurse practitioners (NPs), and physician assistants (PAs) working in the 24-bed MICU at Johns Hopkins Hospital in January 2017 were invited to participate in the survey. Johns Hopkins Hospital is a quaternary care academic teaching hospital in Baltimore, Maryland. The staff-patient ratios for clinical technicians (1:4), nurses (1:2), respiratory therapists (1:12), attending physicians (1:12), fellow physicians (1:12), and NPs/PAs (1:6) have some variability based on MICU census, patient severity of illness, and patient needs. Typically, 2 to 3 physical therapists from the long-established critical care physical medicine and rehabilitation program provide dedicated coverage to the MICU 7 days per week, mobilizing patients alone or with the assistance of nurses, clinical technicians, and respiratory therapists when available or necessary. Physical and occupational therapists were not included in our survey population as our ongoing QI project was focused on enhancing mobilization by nurses and clinical technicians.
Survey
The preexisting, 26-item Patient Mobilization Attitudes & Beliefs Survey (PMABS, freely available at https://www.johnshopkinssolutions.com/solution/amp/amp-hospital/), validated in a ward setting,15 was adapted for the ICU (PMABS-ICU, freely available at https://www.johnshopkinssolutions.com/solution/amp/activity-mobility-promotion-amp-icu/). The PMABS-ICU was administered via a web-based platform (Qualtrics®). Adaptations to the survey wording were minor and included changing “three times daily” to “once daily” in 2 items (Supplemental Table S1) to reflect a more feasible minimum frequency of nurse-led mobilization for ICU patients. Response options used a 5-point Likert scale (0 = not applicable; 1 = strongly disagree; 2 = disagree; 3 = neutral; 4 = agree; 5 = strongly agree). We also asked the respondents to specify the following: clinical role, years of work experience with hospitalized patients, and a free-text question for any additional comments on issues regarding patient mobility not already covered in the survey. As per instructions for the original validated survey, scores were calculated for the overall barriers scale and 3 subscales (ie, knowledge, attitude, and behavior), with each ranging from 0 to 100, with higher scores indicating greater barriers to mobility. Barrier items answered as “not applicable” were not included in the scores.
Statistical Analysis
To aid in comparability, psychometric evaluation of the PMABS-ICU was performed in a similar manner to the original PMABS.15 The response rates and median years of experience were calculated and reported by clinical role. Free-text comments were categorized and tabulated. Cronbach a was calculated to evaluate the internal consistency of the overall scale and subscales, with a value ≥.70 considered acceptable. Correlations of the individual survey items with the overall scale and with the subscales were evaluated using Pearson correlation, with acceptability defined as correlation coefficients >0.40 for most items. Discriminant validity was considered acceptable if the correlation coefficient of most items was higher for the assigned subscale versus the other 2 subscales. Principal factor analysis with 3 factors was performed using an oblique promax rotation to evaluate attribution of survey items to the 3 hypothesized subscales, with loading values ≥0.40 considered positive.
The distribution of the overall and subscale scores was examined for all respondents and stratified by clinical role and median years of experience, with differences evaluated by the Kruskal-Wallis test; Dwass, Steel, Critchlow-Fligner test; and unpaired t tests, as appropriate. A multivariable linear regression model was used to evaluate the independent associations of clinical role and years of work experience with barriers scores. Scatterplots and LOWESS curves were used to visualize the association of clinical role and years of experience with overall and subscale scores. On the basis of this evaluation, a spline term was included in the linear regression model with one knot at 10 years of experience, along with 3 categories of clinical role. A second model was fit with the addition of an interaction term between years of experience and clinical role. All analyses were conducted using SAS version 9.4 (2013, Cary, North Carolina) and figures prepared using STATA® version 14.2 (2015, College Station, Texas).
Results
The survey was distributed to 163 individuals with 155 respondents (96% response rate; Table 1). The only missing data were years of experience for 2 (1%) respondents. The “not applicable” response option was chosen infrequently (Supplemental Table S2).
Table 1.
Characteristics of Survey Participants by Clinical Role.
| Characteristics | Clinical Technician | Nurse | Respiratory Therapist | Attending | Fellow | NP/PA |
|---|---|---|---|---|---|---|
| Invited, n | 7 | 93 | 14 | 13 | 28 | 7 |
| Responded, n | 7 | 86 | 14 | 13 | 28 | 7 |
| Response rate, % | 100% | 92% | 100% | 100% | 100% | 100% |
| Years of experience, median (IQR) | 2 (1-2) | 5 (2-10) | 14 (8-17) | 16 (15-20) | 6 (4-7) | 6 (3-11) |
| n (%) below 10 years | 7 (100%) | 66 (77%) | 6 (43%) | 1 (8%) | 25 (89%) | 5 (72%) |
Abbreviations: IQR, interquartile range; NP, nurse practitioner; PA, physician assistant.
Psychometric Performance
A minority of respondents (29/155, 19%) had any response to the free-text question regarding additional comments on issues regarding patient mobility not already covered in the survey. These free-text responses were categorized into 12 themes (Supplemental Table S3). Only 2 themes (related to sedation and restraints, 4 comments, 3% of responses) were raised that were not already evaluated by an existing survey item.
Cronbach α for the overall barriers scale was acceptable at 0.82 (95% confidence interval [CI]: 0.76-0.85) and was slightly below the 0.70 threshold for the 3 subscales (Table 2). We found acceptable item-scale correlations of >0.40 for the overall barriers scale (50% of items) as well as the subscales (85% of items). Discriminant validity was acceptable with 96% of items correlating most strongly with the assigned subscale. Factor analysis demonstrated that 12 items were categorized correctly (46%) with no cross-loading (ie, no loading of the item onto a second factor), with 5 items (19%; 2 knowledge subscale, 3 behavior subscale) not loading to any factor. In subgroup analyses of nursing versus nonnursing clinical roles, we found no significant difference in the factor analysis finding, suggesting that clinical role did not explain the observed results.
Table 2.
Internal Consistency and Interscale Correlation Measuresa for the Patient Mobilization Attitudes & Beliefs Survey for the ICU (PMABS-ICU).
| Scale | Knowledge Subscale | Attitude Subscale | Behavior Subscale | Overall Scale |
|---|---|---|---|---|
| Knowledge subscale | 0.62 (0.49-0.72) | |||
| Attitude subscale | 0.29 (0.12-0.44) | 0.69 (0.61-0.76) | ||
| Behavior subscale | 0.33 (0.16-0.47) | 0.66 (0.55-0.74) | 0.66 (0.55-0.74) | |
| Overall scale | 0.53 (0.40-0.64) | 0.87 (0.82-0.90) | 0.91 (0.87-0.93) | 0.82 (0.76-0.85) |
Abbreviation: ICU, intensive care unit.
Internal consistency for the 3 subscales and the overall scale was evaluated using Cronbach α (95% confidence interval), as displayed in bold on the main diagonal of the table. Other values in the table (not in bold) represent correlations between the subscales, evaluated using the Pearson correlation statistic (95% confidence interval).
Baseline Barriers to Patient Mobility
The mean (standard deviation, SD) overall barriers score was 34.6 (7.2). Nurses reported the highest overall barrier score and attitude and behavior subscale scores; these scores were only significantly higher in comparison to attending and/or fellow physicians (Table 3). Average scores for all barrier items are available by clinical role in Supplemental Table S4. In a comparison of scores for all respondents below versus above the median years of experience (6 years), those with less experience had higher barriers based on the overall score (35.7 [8.8] vs 32.5 [6.7]; P = 0.01) and 2 of the 3 subscale scores: attitude (37.8 [10.6] vs 33.5 [8.9]; P = 0.01) and behavior (36.9 [9.5] vs 33.3 [7.7]; P = 0.01).
Table 3.
Overall and Subscale Scoresa, by Clinical Role, for the Patient Mobilization Attitudes & Beliefs Survey for the ICU (PMABS-ICU).
| Scale | Clinical Technician n = 7 | Nurse n = 86 | Respiratory Therapist n = 14 | Attending n = 13 | Fellow n = 28 | NP/PA n=7 |
|---|---|---|---|---|---|---|
| Knowledge subscale | 20 (15-25) | 25 (20-30) | 25 (15-30) | 30 (27-40) | 30 (23-35) | 35 (5-50) |
| Attitude subscale | 33 (29-44) | 38 (29-44)b | 36 (31-40) | 30 (23-36) | 33 (28-36) | 36 (31-49) |
| Behavior subscale | 34 (25-37) | 39 (32-43)b,c | 33 (30-39) | 28 (26-31) | 32 (25-39) | 35 (28-46) |
| Overall scale | 32 (25-37) | 37 (31-40)c | 32 (31-37) | 30 (28-34) | 31 (26-37) | 36 (29-39) |
Abbreviations: ICU, intensive care unit; NP, nurse practitioner; PA, physician assistant.
All data are reported as median (interquartile range) for scaled scores (range: 0-100), with a higher score indicating greater perceived barriers to mobility.
P value for unpaired t test comparison with fellow physicians <.05.
P value for unpaired t test comparison with attending physicians <.05.
Bold values indicates summary of the table.
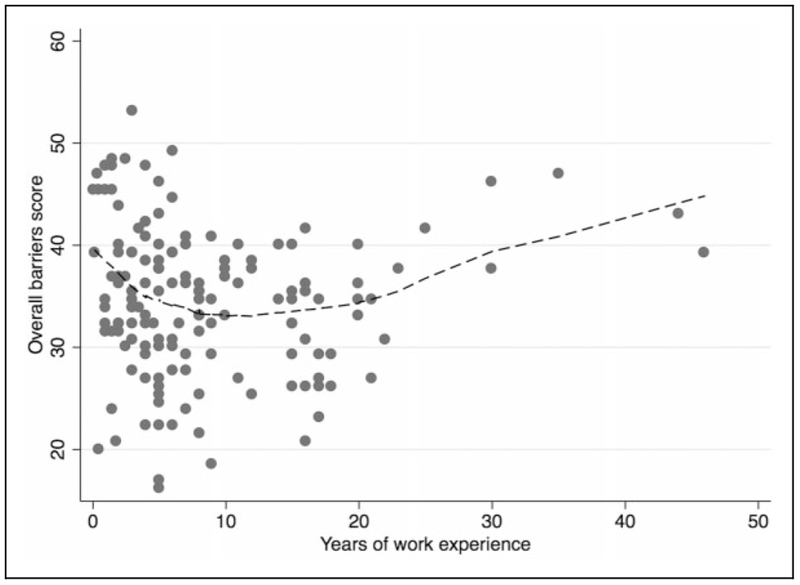
The relationship between years of work experience with hospitalized patients and the overall barrier score is shown in Figure 1. Accounting for clinical role, regression analysis demonstrated that each additional year of experience, up to 10 years, was associated with a significantly lower score for the overall barriers and for each subscale (Table 4). Each year of work experience beyond 10 years had no association with the overall score or 2 of the subscale scores (Table 4). The multivariable regression analyses also demonstrated that nurses and clinical technicians (vs the physician/NP/PA reference group) had significantly higher mean scores for the overall score and for the attitude and behavior subscale scores and significantly lower knowledge subscale scores (Table 4). There was no significant statistical interaction between years of experience and clinical role.
Figure 1.
Scatterplot of years of work experience versus overall score for Patient Mobilization Attitudes & Beliefs Survey for the Intensive Care Unit (PMABS-ICU) for all survey respondents. Dotted line represents a smoothed average (using a LOWESS function) of the relationship between years of work experience with hospitalized patients and overall scaled score for the PMABS-ICU.
Table 4.
Multivariable Linear Regression Results for Overall and Subscale Scores of the Patient Mobilization Attitudes & Beliefs Survey for the ICU (PMABS-ICU), by Clinical Role and Years of Experience.a
| Knowledge |
Attitudes |
Behaviors |
Overall |
|||||
|---|---|---|---|---|---|---|---|---|
| Variables | β | P Value | β | P Value | β | P Value | β | P Value |
| Attending, fellow, NP/PA | [reference] | |||||||
| Nurse, clinical technician | −4.7 | .031 | 3.7 | .040 | 5.2 | <.001 | 3.1 | .026 |
| Respiratory therapist | −2.9 | .426 | 4.6 | .119 | 3.5 | .167 | 2.9 | .206 |
| Experience up to 10 years, per year | −0.8 | .020 | −0.9 | .002 | −0.7 | .008 | −0.8 | <.001 |
| Experience beyond 10 years, per year | 0.4 | .030 | 0.3 | .107 | 0.2 | .231 | 0.2 | .057 |
Abbreviations: ICU, intensive care unit; NP, nurse practitioner; PA, physician assistant.
The β represents the coefficient from the regression model, with numbers in bold denoting P < .05 using a multivariable linear regression model with a spline term for years of work experience with hospitalized patients (with a “knot” at 10 years, based on visual inspection of data, see Figure 1). To prevent overfitting the regression model, 6 clinical roles were collapsed to 3 categories: (1) attending physician, fellow physician, and NP/PA; (2) nurse and clinical technician; and (3) respiratory therapist, based on the anticipated similarity of perceived barriers due to related job roles.
Interventions to Target Barriers
Based on these survey results, our multiprofessional QI group designed several interventions intended to address the identified baseline barriers. First, education about patient mobility was included in nursing staff meetings and physician education sessions. Second, to better understand the barriers and opportunities for patient mobilization within nursing and technician workflow, a physical therapist directly observed nurses and a nurse technician engaged in their regular clinical care, with detailed empirical data collection and analyses of their activities, as described in detail elsewhere.14 Third, training sessions were held with existing nurses and clinical technicians regarding safe techniques for patient mobilization and implemented into orientation for new staff. Fourth, discussion and documentation of a daily goal for nurse-based patient mobility, using the Johns Hopkins Highest Level of Mobility scale,18 was implemented as part of daily work flow, with daily documentation of the actual mobility achieved by the nurse or technician.
Discussion
This project, reporting on the results of adapting and administering a previously validated, inpatient mobility barriers survey in the ICU setting, had a 96% response rate and demonstrated relatively low baseline perceived barriers as well as acceptable internal consistency and discriminant validity in a large, multiprofessional group of 155 MICU clinicians. Nurses reported the highest overall barriers and highest attitude and behavior barriers, but relatively lower knowledge barriers. Across all clinical roles and all survey scales, over the first 10 years of work experience, greater experience was associated with lower barrier scores. Interventions were designed to target barriers identified from this survey for the ongoing QI project.
We adapted the PMABS for the ICU via minor changes in the wording of survey items. The original PMABS was validated in a sample of medicine floor nurses and occupational and physical therapists.15 Here, the PMABS-ICU was administered to 6 different clinical roles relevant to our ongoing QI project. Psychometric analysis of the PMABS-ICU demonstrated adequate internal consistency of the overall barriers scale (α = 0.82, 95% CI: 0.76-0.85), similar to the original survey (α = 0.87, 95% CI: 0.83-0.90). Internal consistency of the subscales scores was lower for the PMABS-ICU versus original survey (ie, 0.62-0.69 vs 0.75-0.82), possibly due to the difference in clinical setting or greater heterogeneity in the clinical roles surveyed.
The objective of our multiprofessional QI project is to increase the mobilization of MICU patients by nurses and clinical technicians, to complement the existing physical therapy (PT)-led early rehabilitation program.19 As this objective most directly impacts nursing workflow, it is not surprising that nurses (vs other roles) had higher attitude and behavior perceived barriers in our survey administered in the planning stages of our QI project. We found greater attitude and behavior barriers, relative to knowledge barriers, in all clinical roles except for attending physicians and NP/PAs. Group discussions, in-depth interviews, and observation of work flow, as reported in prior ICU QI papers,14,20 can assist with further understanding these identified barriers and with informing approaches to overcome them as outlined elsewhere.21,22
Notably, there were lower barrier scores with each additional year of work experience during the first 10 years. Prior research in general medicine nurses and rehabilitation technicians has reported similar findings,15 which could indicate increasing comfort with patient mobility as experience and confidence in patient care increase.
There are few published reports of similar surveys for comparison purposes. In Canada, the Mobility Survey Questionnaire was designed to assess ICU physician and physiotherapist knowledge, barriers, and practice of rehabilitation using 30 items in 3 domains (barriers/facilitators, knowledge, and clinical practice).23 Compared to the PMABS-ICU, the Mobility Survey Questionnaire is more focused on beliefs and practices regarding mobility. Also, the Mobility Survey Questionnaire was administered in a narrower group of clinical roles than the PMABS-ICU, limiting comparability of results between these 2 surveys. Among ICU physicians, the only clinician group common to both surveys, results were similar regarding lack of equipment being a barrier. Specifically, 56% of the Canadian respondents reporting this barrier compared to a mean response of 3.9 (a score of 4 = “agree”) in PMABS-ICU item 7 among attending physician respondents.23
There are potential limitations to our survey project. First, the internal consistency of the subscales was lower in our multiprofessional MICU sample compared to the original survey in sample of general medical floor nurses and physical and occupational therapists. The factor analysis suggests that the survey subscales do not delineate the barrier subscales (knowledge, attitudes, and behaviors) as clearly in the MICU sample versus the original sample. This finding may be due to unmeasured differences between the respondents or differences between the general medicine ward versus ICU settings. We did not collect detailed demographic data on our respondents, and it is possible that such unmeasured factors as age and gender may have accounted for some of these differences. Second, our respondents demonstrated relatively low knowledge barriers to mobility, unlike other studies. Therefore, our results may not generalize to centers without a preexisting early mobility program. However, the starting point of any QI project is a unit-specific evaluation of barriers, which emphasizes the importance of using a tool, such as the PMABS-ICU, to understand local barriers. Third, the small size of some of our clinical role groups may have limited our ability to discern statistically significant differences between roles.
In conclusion, a survey administered to a multiprofessional group of MICU staff demonstrated relatively low perceived barriers to patient mobility across clinical roles. Within the first decade of work experience, greater experience was associated with lower perceived barriers to patient mobility. As part of a structured QI project, the PMABS-ICU may be a valuable tool to assist in identifying specific perceived barriers for consideration when designing mobility interventions for the ICU setting.
Supplementary Material
Acknowledgments
The authors would like to thank all of the survey respondents and the entire Johns Hopkins MICU staff for their participation in this ongoing quality improvement project.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dale M. Needham is a principal investigator on a NIH-funded, multicentered randomized trial (R01HL132887) evaluating nutrition and exercise in acute respiratory failure and, related to this trial, is currently in receipt of an unrestricted research grant and donated amino acid product from Baxter Healthcare Corporation and an equipment loan from Reck Medical Devices.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Financial support was provided by the National Heart Lung Blood Institute for Dr Goodson [T32HL007534] and Dr Parker [K23HL138206]. The funding bodies had no role in the design, implementation, or output of this study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Pfoh ER, Wozniak AW, Colantuoni E, et al. Physical declines occurring after hospital discharge in ARDS survivors: a 5-year longitudinal study. Intensive Care Med. 2016; 42(10):1557–1566. doi: 10.1007/s00134-016-4530-1 [DOI] [PubMed] [Google Scholar]
- 2.Herridge MS, Tansey CM, Matte A, et al. Canadian Critical Care Trials Group. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–1304. doi: 10.1056/NEJMoa1011802 [DOI] [PubMed] [Google Scholar]
- 3.Dinglas VD, Aronson Friedman L, Colantuoni E, et al. Muscle weakness and 5-year survival in acute respiratory distress syndrome survivors. Crit Care Med. 2017;45(3):446–453. doi: 10.1097/CCM.0000000000002208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fan E, Dowdy DW, Colantuoni E, et al. Physical complications in acute lung injury survivors: a two-year longitudinal prospective study. Crit Care Med. 2014;42(4):849–859. doi: 10.1097/CCM.0000000000000040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Needham DM,Wozniak AW, Hough CL, et al. National Institutes of Health NHLBI ARDS Network. Risk factors for physical impairment after acute lung injury in a national, multicenter study. Am J Respir Crit Care Med. 2014;189(10):1214–1224. doi: 10.1164/rccm.201401-0158OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schaller SJ, Anstey M, Blobner M, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016;388(10052):1377–1388. doi: 10.1016/S0140-6736(16)31637-3 [DOI] [PubMed] [Google Scholar]
- 7.Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017;43(2):171–183. doi: 10.1007/s00134-016-4612-0 [DOI] [PubMed] [Google Scholar]
- 8.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009; 373(9678):1874–1882. doi: 10.1016/S0140-6736(09)60658-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hodgson CL, Bailey M, Bellomo R, et al. Trial of Early Activity and Mobilization Study Investigators. A binational multicenter pilot feasibility randomized controlled trial of early goal-directed mobilization in ICU. Crit Care Med. 2016;44(6): 1145–1152. doi: 10.1097/CCM.0000000000001643 [DOI] [PubMed] [Google Scholar]
- 10.Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238–2243. doi: 10.1097/CCM.0b013e318180b90e [DOI] [PubMed] [Google Scholar]
- 11.Goodson CM, Tipping C, Mantheiy EC, et al. Physical rehabilitation in the ICU: understanding the evidence. ICU Manag Pract. 2017;17(3):152–154. [Google Scholar]
- 12.Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ. 2008;337:a1714. doi: 10.1136/bmj.a1714 [DOI] [PubMed] [Google Scholar]
- 13.Colquhoun HL, Squires JE, Kolehmainen N, Fraser C, Grimshaw JM. Methods for designing interventions to change healthcare professionals’ behaviour: a systematic review. Implement Sci. 2017;12(1):30. doi: 10.1186/s13012-017-0560-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Young DL, Seltzer J, Glover M, et al. Identifying barriers to nurse-facilitated patient mobility in the intensive care unit. Am J Crit Care. 2018;27(3):186–193. doi: 10.4037/ajcc2018368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoyer EH, Brotman DJ, Chan KS, Needham DM. Barriers to early mobility of hospitalized general medicine patients: survey development and results. Am J Phys Med Rehabil. 2015;94(4): 304–312. doi: 10.1097/PHM.0000000000000185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Girard TD, Alhazzani W, Kress JP, et al. ATS/CHEST Ad Hoc Committee on Liberation from Mechanical Ventilation in Adults. An Official American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: liberation from mechanical ventilation in critically ill adults. Rehabilitation protocols, ventilator liberation protocols, and cuff leak tests. Am J Respir Crit Care Med. 2016. doi: 10.1164/rccm.201610-2075ST [DOI] [PubMed] [Google Scholar]
- 17.Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825. doi: 10.1097/CCM.0000000000003299 [DOI] [PubMed] [Google Scholar]
- 18.Hoyer EH, Young DL, Klein LM, et al. Toward a common language for measuring patient mobility in the hospital: reliability and construct validity of interprofessional mobility measures. Phys Ther. 2018;98(2):133–142. doi: 10.1093/ptj/pzx110 [DOI] [PubMed] [Google Scholar]
- 19.Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010; 91(4):536–542. doi: 10.1016/j.apmr.2010.01.002 [DOI] [PubMed] [Google Scholar]
- 20.Eakin MN, Ugbah L, Arnautovic T, Parker AM, Needham DM. Implementing and sustaining an early rehabilitation program in a medical intensive care unit: a qualitative analysis. J Crit Care. 2015;30(4):698–704. doi: 10.1016/j.jcrc.2015.03.019 [DOI] [PubMed] [Google Scholar]
- 21.Dubb R, Nydahl P, Hermes C, et al. Barriers and strategies for early mobilization of patients in intensive care units. Ann Am Thorac Soc. 2016;13(5):724–730. doi: 10.1513/AnnalsATS.201509-586CME [DOI] [PubMed] [Google Scholar]
- 22.Parry SM, Knight LD, Connolly B, et al. Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intensive Care Med. 2017;43(4):531–542. doi: 10.1007/s00134-017-4685-4 [DOI] [PubMed] [Google Scholar]
- 23.Koo KK, Choong K, Cook DJ, et al. Canadian Critical Care Trials Group. Early mobilization of critically ill adults: a survey of knowledge, perceptions and practices of Canadian physicians and physiotherapists. CMAJ Open. 2016;4(3):E448–E454. doi: 10.9778/cmajo.20160021 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.