Abstract
Objectives
To evaluate the comparative effectiveness and safety of intravitreal bevacizumab, ranibizumab and aflibercept for patients with choroidal neovascular age-related macular degeneration (cn-AMD), diabetic macular oedema (DMO), macular oedema due to retinal vein occlusion (RVO-MO) and myopic choroidal neovascularisation (m-CNV).
Design
Systematic review and random-effects meta-analysis.
Methods
Multiple databases were searched from inception to 17 August 2017. Eligible head-to-head randomised controlled trials (RCTs) comparing the (anti-VEGF) drugs in adult patients aged ≥18 years with the retinal conditions of interest. Two reviewers independently screened studies, extracted data and assessed risk of bias.
Results
19 RCTs involving 7459 patients with cn-AMD (n=12), DMO (n=3), RVO-MO (n=2) and m-CNV (n=2) were included. Vision gain was not significantly different in patients with cn-AMD, DMO, RVO-MO and m-CNV treated with bevacizumab versus ranibizumab. Similarly, vision gain was not significantly different between cn-AMD patients treated with aflibercept versus ranibizumab. Patients with DMO treated with aflibercept experienced significantly higher vision gain at 12 months than patients receiving ranibizumab or bevacizumab; however, this difference was not significant at 24 months. Rates of systemic serious harms were similar across anti-VEGF agents. Posthoc analyses revealed that an as-needed treatment regimen (6–9 injections per year) was associated with a mortality increase of 1.8% (risk ratio: 2.0 [1.2 to 3.5], 2 RCTs, 1795 patients) compared with monthly treatment in cn-AMD patients.
Conclusions
Intravitreal bevacizumab was a reasonable alternative to ranibizumab and aflibercept in patients with cn-AMD, DMO, RVO-MO and m-CNV. The only exception was for patients with DME and low visual acuity (<69 early treatment diabetic retinopathy study [ETDRS] letters), where treatment with aflibercept was associated with significantly higher vision gain (≥15 ETDRS letters) than bevacizumab or ranibizumab at 12 months; but the significant effects were not maintained at 24 months. The choice of anti-VEGF drugs may depend on the specific retinal condition, baseline visual acuity and treatment regimen.
PROSPERO registration number
CRD42015022041.
Keywords: ranibizumab, bevacizumab, aflibercept, anti-vascular endothelial growth factor, age-related macular degeneration, diabetic macular edema, retinal vein occlusion, myopic choroidal neovascularization
Strengths and limitations of this study.
We consolidated the evidence for treatment choice of all common retinal conditions, allowing the interpretation of the strength of the evidence of benefits and harms of the anti-VEGF drugs across conditions.
We summarised information regarding treatment regimens (eg, three initial monthly intravitreal injections and as-needed monthly retreatment, treat and extend), as-needed retreatment criteria and the reconstitution of bevacizumab, and examined the influence of the choice of treatment regimens on the benefits and harms of the anti vascular endothelial growth factor (anti-VEGF) drugs for specific retinal conditions.
We limited our review to English studies, and found that very few randomised controlled trials evaluated the anti-VEGF drugs in patients with macular oedema due to retinal vein occlusion and myopic choroidal neovasculari sation.
Our sensitivity and subgroup analyses were not specified a-priori and should be interpreted with caution.
Background
Retinal conditions due to neovascular abnormality are common in older adults. Choroidal neovascular age-related macular degeneration (cn-AMD) is the leading cause of irreversible blindness in individuals aged 50 years or older in high-income countries.1 2 If left untreated, potentially irreversible visual impairment can also be caused by diabetic macular oedema (DMO) and macular oedema due to retinal vein occlusion (RVO-MO).3–5 Choroidal neovascularisation secondary to pathologic myopia (myopic CNV) is another major cause of blindness and visual impairment worldwide.6 7 Together, these retinal diseases cause substantial reduction in quality of life, and are a significant burden on healthcare systems.8
Ranibizumab, off-label use of repackaged bevacizumab, and aflibercept are widely used antivascular endothelial growth factor (anti-VEGF) drugs for intravitreal treatment of retinal conditions. Multiple systematic reviews have evaluated the comparative effectiveness of anti-VEGF drugs in patients with cn-AMD, DMO, RVO-MO and m-CNV9–12; but given the publication of new trials in patients with RVO-MO13 and DMO,14 and long-term follow-up data for patients with cn-AMD,15 an update is necessary. We aimed to conduct a systematic review to evaluate the comparative effectiveness and safety of bevacizumab, ranibizumab and aflibercept for patients with cn-AMD, DMO, RVO-MO and m-CNV.
Methods
A systematic review regarding the comparative efficacy and safety of the anti-VEGF drugs was planned in response to a query from the Canadian Drug Safety and Effectiveness Network, for which a preliminary report was prepared to inform listing recommendations.16 17 The report included a meta-analysis of pairwise comparisons of the anti-VEGF drugs for individual retinal conditions, as well as a network meta-analysis to evaluate the anti-VEGF drugs in cn-AMD patients. This paper summarises results of the meta-analysis; a separate paper is underway for the network meta-analysis results.
The current review was conducted using the Cochrane Handbook for Systematic Reviews and reported using the Preferred Reporting Items for Systematic Review and Meta-Analysis statement18 (additional file 1). The methods are outlined briefly below, as they are described in greater detail in additional file 2: Appendix 1 and a related therapeutic review report.17
bmjopen-2018-022031supp001.pdf (31.2KB, pdf)
bmjopen-2018-022031supp002.pdf (1.1MB, pdf)
Data sources and searches
MEDLINE, Embase and Cochrane Central Register of Controlled Trials were searched. Studies, which are not widely available or commercially published (ie, grey literature), were identified using an established approach.19 Additional studies were identified by searching reference lists of included studies, and email correspondence with expert clinicians and anti-VEGF drug manufacturers.
An information specialist developed the search strategy, which was peer reviewed by another information specialist using the Peer Review of Electronic Search Strategies (PRESS) statement.20 The MEDLINE strategy can be found in additional file 2: Appendix 1. The search was conducted on 27 May 2015 and updated on 17 August 2017.
Study selection and outcome definitions
Eligible studies were randomised controlled trials (RCTs) that directly compared intravitreal bevacizumab, ranibizumab and/or aflibercept for the treatment of patients (aged ≥18 years) with cn-AMD, DMO, RVO-MO or m-CNV. We excluded RCTs comparing anti-VEGF drugs with other comparators, such as photodynamic therapy, intravitreal corticosteroids and grid laser photocoagulation (additional file 2: Appendix 1). Due to time and resource constraints, we only included studies published in English.
Eligible RCTs reported one of the following benefits and harms outcomes: vision gain, defined as a gain in best-corrected visual acuity (BCVA) letter score of ≥15 on the early treatment diabetic retinopathy study (ETDRS) chart21; vision loss, defined as a loss in BCVA letter score of ≥15; mean change in BCVA from baseline; legal blindness (BCVA of 20/200 or worse measured on a standard Snellen chart, or worse than 20/100 visual acuity measured on ETDRS chart); vision-related function according to the 25-item National Eye Institute Visual Function Questionnaire (NEI-VFQ-25)22; serious adverse events; all-cause mortality; arterial thromboembolic events (TEs); venous TEs; bacterial endophthalmitis and retinal detachment.
All titles/abstracts and potentially relevant full-text articles were screened by two reviewers, independently. Discrepancies were discussed and if necessary, resolved with input from a third reviewer. When multiple reports of the same trial were identified, the main report was included and the others were treated as companion reports.23
Data extraction and quality assessment
Data extraction forms were developed with input from three clinicians, pilot-tested and refined twice. Data extraction was conducted by two reviewers, independently. Discrepancies were discussed and if necessary, resolved with input from a third reviewer. A similar approach was followed for quality assessment using the Cochrane risk-of-bias tool for RCTs.24
Patient and public involvement
There was no patient or public involvement in the conduct of this study.
Synthesis of study results
Study results were synthesised with respect to benefits and harms of treatment, treatment regimen (eg, monthly and as-needed regimens) and trends in BCVA improvement over time. With respect to visual acuity improvement, meta-analyses were conducted with studies reporting BCVA letter score as measured on the ETDRS chart. For studies reporting visual acuity in logMAR and decimal values, the values were converted to approximate ETDRS letter scores,25 with approximate SD.26 Pairwise comparisons of drugs were assessed at the longest treatment duration, allowing for the inclusion of trials in the meta-analysis that reported outcome data at different time points. Subgroup analyses were conducted at 12 and 24 months, as these were the most frequently reported time points. A posthoc analysis was conducted to compare different treatment regimens across the drugs. For DMO patients, treatment effect estimates were obtained for all patients as well as subgroups based on baseline BCVA, which were prespecified in the Diabetic Retinopathy Clinical Research Network (DRCR.net) trial.27 The meta-analysis was conducted using a random-effects model, as we assumed treatment effects varied across trials. A sensitivity analysis was conducted by restricting results to trials determined to be at low risk of selection bias. Between-study heterogeneity was assessed using the I² statistic, with values above 75% indicating substantial heterogeneity.28
Results
Literature search
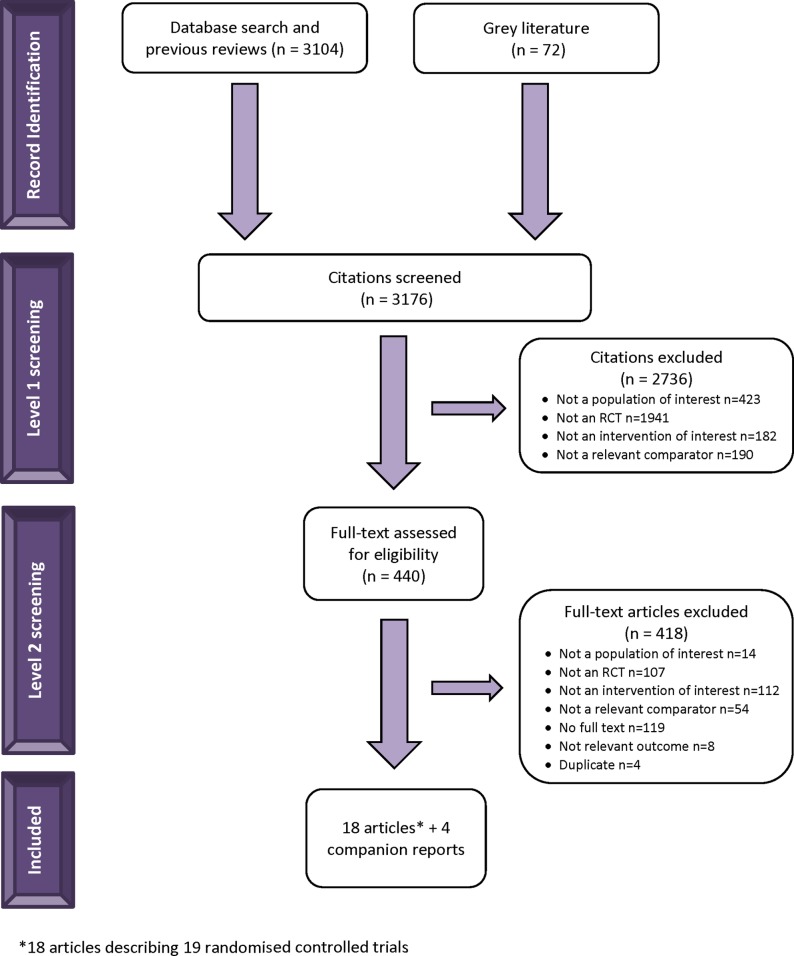
After screening 3176 titles/abstracts and 440 full-text articles, 19 head-to-head RCTs of the anti-VEGF drugs were included, with 7459 patients, including 12 RCTs for cn-AMD, 3 RCTs for DMO, 2 RCTs for RVO-MO and 2 RCTs for m-CNV (figure 1, additional file 2: Appendix 1).27 29–42 Given our inclusion criteria, we excluded RCTs that compared anti-VEGF drugs with placebo or laser photocoagulation.43–49
Figure 1.
Study flow. RCT, randomised controlled trial.
Study and patient characteristics
Studies were completed between 2010 and 2017 with an average sample size of 393 patients per trial (range: 28, 1240) (table 1, additional file 2: Appendices 2 and 3). The mean age ranged from approximately 60–80 years, and females accounted for 5%–76% of the patients. The average follow-up duration was 13 months (range: 6–24 months). RCTs were conducted in Europe (n=8), North America (n=5), Asia (n=4), Africa (n=1) and across multiple continents (n=1); most were multicentre RCTs (n=13), in addition to six single-centre RCTs.
Table 1.
Summary study characteristics
| Study characteristic | Total no of trials included (n=19)* (%) | No of studies with cn-AMD (n=12) (%) | No of studies with DMO (n=3) (%) | No of studies with RVO-MO (n=2) (%) | No of studies with m-CNV (n=2) (%) |
| Year of publication | |||||
| 2010–2011 | 5 (26.32) | 4 (33.33) | 0 (0) | 0 (0) | 1 (50) |
| 2012–2013 | 6 (31.58) | 5 (41.67) | 0 (0) | 0 (0) | 1 (50) |
| 2014–2015 | 5 (26.32) | 2 (16.67) | 2 (66.67) | 1 (50) | 0 (0) |
| 2016 | 3 (15.79) | 1 (8.33) | 1 (33.33) | 1 (50) | 0 (0) |
| Geographic region | |||||
| Europe | 8 (42.11) | 6 (50) | 0 (0) | 0 (0) | 2 (100) |
| North America | 5 (26.32) | 3 (25) | 1 (33.33) | 1 (50) | 0 (0) |
| Asia | 4 (21.05) | 2 (16.67) | 1 (33.33) | 1 (50) | 0 (0) |
| Africa | 1 (5.26) | 0 (0) | 1 (33.33) | 0 (0) | 0 (0) |
| Multicontinent | 1 (5.26) | 1 (8.33) | 0 (0) | 0 (0) | 0 (0) |
| Setting | |||||
| Single-centre | 6 (31.58) | 2 (16.67) | 1 (33.33) | 1 (50) | 2 (100) |
| Multicentre | 12 (63.16) | 10 (83.33) | 1 (33.33) | 1 (50) | 0 (0) |
| NR | 1 (5.26) | 0 (0) | 1 (33.33) | 0 (0) | 0 (0) |
| Follow-up duration | |||||
| 6–12 months | 14 (73.68) | 9 (75) | 2 (66.67) | 2 (100) | 1 (50) |
| 13–19 months | 4 (21.05) | 2 (16.67) | 1 (33.33) | 0 (0) | 1 (50) |
| ≥20 months | 1 (5.26) | 1 (8.33) | 0 (0) | 0 (0) | 0 (0) |
*Total number of randomised controlled trials, n=19, from 18 publications.
cn-AMD, choroidal neovascular age-related macular degeneration; DMO, diabetic macular oedema; m-CNV, myopic choroidal neovascularisation; NR, not reported; RVO-MO, macular oedema due to retinal vein occlusion.
Risk of bias assessment
Random sequence generation and allocation concealment were unclear for 12/19 (63.2%) and 9/19 (47.4%) of the included RCTs, respectively, suggesting the potential for selection bias (additional file 2: Appendices 4 and 5). The RCTs were at low risk of bias with respect to blinding of participants and trial personnel 18/19 (94.7%), blinding of outcome assessment 18/19 (94.7%), incomplete outcome data 13/19 (68.4%) and selective reporting 13/19 (68.4%). Two of the 19 RCTs (10.5%) were industry funded.38
Patients with cn-AMD
Comparative effectiveness of bevacizumab and ranibizumab
Results from 10 RCTs (3302 patients) showed that approximately 22% of patients attained vision gain of ≥15 BCVA letter scores with treatment, and patients treated with bevacizumab were as likely to attain vision gain as those treated with ranibizumab (risk ratio [RR]: 1.05 [95% CI, 0.93 to 1.19], table 2, additional file 2: Appendices 6–7). Over an average treatment duration of 16 months, approximately 94% of patients maintained their vision, with no statistical difference between patients treated with bevacizumab or ranibizumab (RR of vision loss: 0.91 [95% CI, 0.70 to 1.19]). Patients treated with bevacizumab or ranibizumab gained an average of seven letters in terms of mean BCVA with no statistical difference between the drugs (mean difference (MD) 0.03 letters [95% CI, −1.02 to 1.08]). Approximately 2%–4% patients treated with bevacizumab or ranibizumab became legally blind (RR: 2.04 [95% CI, 0.32 to 12.50], 3 trials, 1823 patients). Overall, the results were consistent across the 10 trials and did not change with the sensitivity analyses restricted to trials determined to be at low risk of selection bias and with different follow-up lengths (additional file 2: Appendices 6, 8–9).
Table 2.
Comparative effectiveness results
| Condition | Treatment vs comparator | Outcome* | No of RCTs (no of patients) |
Baseline ETDRS letters†~Snellen equivalent | Treatment effect Mean (range)† |
Comparator effect Mean (range)† |
Risk ratio or mean difference
estimate (95% CI) |
I2‡ (%) |
| cn-AMD | Bevacizumab vs ranibizumab | Vision gain | 9 (3245) | 57 (35 to 61)~20/80 | 22% (12 to 33) | 23% (14 to 29) | 0.95 (0.84 to 1.07) | 0 |
| Vision loss | 10 (3302) | 60 (35 to 61)~20/63 | 6% (0 to 11) | 7% (4 to 14) | 0.91 (0.7 to 1.19) | 4 | ||
| BCVA change | 8 (3064) | 56 (35 to 61)~20/80 | 7.2 (4.1 to 15.2) | 5.9 (0.6 to 11.4) | −0.03 (−1.08 to 1.02) | 0 | ||
| Aflibercept vs ranibizumab | Vision gain | 2 (1815) | 54 (53 to 55)~20/80 | 32% (30 to 34) | 32% (31 to 34) | 0.99 (0.81 to 1.22) | 52 | |
| Vision loss | 2 (1815) | 54 (53 to 55)~20/80 | 5% (5 to 5) | 6% (5 to 6) | 0.90 (0.60 to 1.350) | 0 | ||
| BCVA change | 2 (1793) | 54 (53 to 55)~20/80 | 8.8 (8.3 to 9.4) | 8.8 (8.1 to 9.4) | −0.05 (−2.5 to 2.4) | 66 | ||
| DMO | Bevacizumab vs ranibizumab | Vision gain | 1 (376) | 65~20/50 | 35% | 37% | 0.94 (0.72 to 1.23) | NA |
| Vision loss | 1 (376) | 65~20/50 | 3% | 2% | 0.48 (0.12 to 1.91) | NA | ||
| BCVA change | 2 (456) | 59 (54 to 65)~20/63 | 10.3 (10.0 to 10.5) | 12.1 (11.9 to 12.3) | −2.0 (−3.9 to 0.1) | 0 | ||
| Bevacizumab vs aflibercept | Vision gain | 1 (386) | 65~20/50 | 35% | 39% | 1.06 (0.80 to 1.38) | NA | |
| Vision loss | 1 (376) | 65~20/50 | 2% | 3% | 2.08 (0.52 to 8.33) | NA | ||
| BCVA change | 1 (386) | 65~20/50 | 10.0 (SD: 11.8) | 12.8 (SD: 12.4) | −2.7 (−5.2 to 0.3) | NA | ||
| Aflibercept vs ranibizumab |
Vision gain | 1 (392) | 65~20/50 | 39% | 37% | 1.06 (0.73 to 1.22) | NA | |
| Vision loss | 1 (392) | 65~20/50 | 2% | 2% | 0.63 (0.15 to 2.61) | NA | ||
| BCVA change | 2 (462) | 56 (47 to 65)~20/80 | 16.2 (12.8 to 19.6) | 14.0 (12.3 to 15.7) | 1.4 (-1.6 to 4.3) | 27 | ||
| RVO-MO | Bevacizumab vs ranibizumab | Vision gain | 1 (74) | 56~20/80 | 59% | 59% | 1.00 (0.68 to 1.45) | NA |
| BCVA change | 1 (77) | 56~20/80 | 15.6 | 18.1 | −2.5 (−8.0 to 5.0) | NA | ||
| Bevacizumab vs aflibercept | Vision gain | 1 (358) | 50~20/100 | 65% | 61% | 1.06 (0.91 to 1.25) | NA | |
| BCVA change | 1 (348) | 50~20/100 | 18.6 | 18.9 | 1.5 (−1.2 to 4.2) | NA | ||
| m-CNV | Bevacizumab vs ranibizumab | Vision gain | 1 (32) | 30~20/250 | 62% | 56% | 1.11 (0.63 to 1.96) | NA |
| Vision loss | 1 (32) | 30~20/250 | 0% | 0% | 0% | NA | ||
| BCVA change | 2 (80) | 42 (30 to 55)~20/160 | 12.2 (8.5 to 15.9) | 13.4 (9.5 to 17.3) | −1.3 (−6.5 to 4.0) | 0 |
*In terms of outcomes, vision gain was defined as a gain in BCVA of ≥15 EDTRS letters, vision loss of ≥15 EDTRS letters and visual acuity was expressed using ETDRS letters (with conversion, if necessary). The main analysis was conducted with outcomes at the longest follow-up duration for each RCT.
†Mean (range) were derived across control groups of the included RCTs.
‡I2 <75 was interpreted as low evidence of substantial variation across included RCTs.
BCVA, best-corrected visual acuity; cn-AMD, choroidal neovascular age-related macular degeneration; DMO, diabetic macular oedema; ETDRS, early treatment diabetic retinopathy study; m-CNV, myopic choroidal neovascularisation; NA, not applicable; RCT, randomised controlled trials; RVO-MO, macular oedema due to retinal vein occlusion.
Comparative effectiveness of aflibercept and ranibizumab
Results from two RCTs (1815 patients; table 2, and additional file 2: Appendix 6) showed that approximately 32% of patients attained vision gain with treatment, and patients treated with aflibercept were as likely to attain vision gain as patients treated with ranibizumab (RR: 0.99 [95% CI, 0.81 to 1.22]). Over an average assessment and treatment duration of 12 months, approximately 95% of patients maintained their vision, and aflibercept patients were as likely to maintain vision as ranibizumab patients (RR of vision loss: 0.90 [95% CI, 0.60 to 1.35]). With respect to mean BCVA, patients gained on average nine letters (MD: −0.05 [95% CI, −2.5 to 2.4]). Compared with baseline, patients gained some visual-related function, with an average of 5 points on the NEI-VFQ-25 questionnaire (MD: 2.2 [95% CI, −0.6 to 5.1]).
Comparative effectiveness of bevacizumab and aflibercept
There were no RCTs that directly compared bevacizumab and aflibercept (table 2, and additional file 2: Appendix 6). Regarding BCVA change, the MD between bevacizumab and ranibizumab was −0.03 (95% CI, −1.08 to 1.02), whereas the MD between aflibercept and ranibizumab was −0.05 (95% CI, −2.5 to 2.4), suggesting a MD between bevacizumab and aflibercept of 0.02 (95% CI, −2.60 to 2.64).50 For vision gain, the corresponding RR estimate was 0.95 (95% CI, 0.84 to 1.07) for bevacizumab versus ranibizumab and 0.99 (95% CI, 0.81 to 1.22) for bevacizumab versus ranibizumab, suggesting a RR estimate of 0.96 (95% CI, 0.75 to 1.22) between bevacizumab and aflibercept.
Treatment regimens
Additional file 2: Appendix 10 provides detailed information regarding the treatment regimens in the included trials, the as-needed retreatment criteria and the reconstitution of bevacizumab for intravitreal injections. The treatment regimens varied widely, and are summarised in table 3 along with the mean number of injections per year for each treatment regimen. The number of reported treatment regimens varied by condition (cn-AMD [n=6], DMO [n=3], RVO-MO [n=2] and m-CNV [n=1]). In cn-AMD patients, the two most commonly reported regimens for bevacizumab and ranibizumab included monthly injections (~11 injections/year) and 3 monthly injections followed by as-needed treatment (~6 injections/year). Aflibercept was most commonly administered using a monthly regimen (~11 injections/year).
Table 3.
Summary of treatment regimens
| Condition | Treatment regimen | No of RCTs | Mean monthly injections per year (range)* |
| cn-AMD | Monthly treatment with ranibizumab | 5 | 11.3 (10.9–11.7) |
| Monthly treatment with bevacizumab | 3 | 11.5 (11.0–11.9) | |
| Treat and extend with ranibizumab | 1 | 8.0 | |
| Treat and extend with bevacizumab | 1 | 8.9 | |
| 3 initial monthly treatments and as-needed treatment (every month) with ranibizumab | 6 | 5.7 (4.4–7.1) | |
| 3 initial monthly treatments and as-needed treatment (every month) with bevacizumab | 5 | 6.3 (4.6–7.9) | |
| 3 initial monthly treatments and as-needed treatment (every 3 months) with ranibizumab | 1 | 8.5 | |
| 3 initial monthly treatments and as-needed treatment (every 3 months) with bevacizumab | 1 | 8.7 | |
| As-needed monthly treatment with ranibizumab | 1 | 6.9 | |
| As-needed monthly treatment with bevacizumab | 1 | 7.7 | |
| Monthly treatment with aflibercept | 2 | 11.4† | |
| 3 initial monthly treatment and as-needed treatment (every 2 months) with aflibercept | 2 | 6.9† | |
| DMO | 3 initial monthly treatments and as-needed treatment (every month) with ranibizumab | 1 | 6.0 |
| 3 initial monthly treatments and as-needed treatment (every month) with aflibercept | 1 | 5.6 | |
| 3 initial monthly treatments and as-needed treatment (every month for 3 months) and as-needed treatment (every month) with ranibizumab | 1 | 6.5 | |
| 3 initial monthly treatments and as-needed treatment (every month for 3 months) and as-needed treatment (every month) with bevacizumab | 1 | 5.1 | |
| As-needed treatment till stable visual acuity (up to 6 months) and as-needed treatment (every month) with ranibizumab | 1 | 10‡ | |
| As-needed treatment till stable visual acuity (up to 6 months) and as-needed treatment (every month) with bevacizumab | 1 | 10‡ | |
| As-needed treatment till stable visual acuity (up to 6 months) and as-needed treatment (every month) with aflibercept | 1 | 9‡ | |
| RVO-MO | 1 initial monthly treatment and as-needed treatment (every month) with ranibizumab | 1 | 6.4 |
| 1 initial monthly treatment and as-needed treatment (every month) with bevacizumab | 1 | 6.0 | |
| Monthly treatment with aflibercept | 1 | 11.6 | |
| Monthly treatment with bevacizumab | 1 | 11.5 | |
| m-CNV | 1 initial monthly treatment and as-needed treatment (every month) with ranibizumab | 2 | 2.4 (1.7–3.1) |
| 1 initial monthly treatment and as-needed treatment (every month) with bevacizumab | 2 | 3.1 (1.9–4.3) |
*Mean and ranges were derived from trial-specific means. Cases, in which a single RCT reported on a regimen, do not have an associated range.
†Value was reported once for both trials in Heier et al. 38
‡Reported median values (Wells et al).27
cn-AMD, choroidal neovascular age-related macular degeneration; DMO, diabetic macular oedema; m-CNV, myopic choroidal neovascularisation; RCT, randomised controlled trial; RVO-MO, macular oedema due to retinal vein occlusion.
Results of our posthoc analysis comparing as-needed versus monthly treatment in cn-AMD patients are summarised in table 4. The as-needed treatment regimen with ranibizumab or bevacizumab was less effective than the monthly regimen in improving mean BCVA (MD: −1.9 letters [95% CI, −3.3 to −0.5 letters], 2 RCTs, 1622 patients) and vision gain (RR: 0.73 [95% CI, 0.55 to 0.95]). When the regimens were assessed for non-inferiority at 1 year with an inferiority margin of five points, monthly bevacizumab was equivalent to monthly ranibizumab (MD: −0.5 [95% CI, −3.9 to 2.9]), as-needed bevacizumab was equivalent to as-needed ranibizumab (MD: −0.8 [95% CI, −4.1 to 2.5]), as-needed ranibizumab was equivalent to monthly ranibizumab (MD: −1.7 [95% CI, −4.7 to 1.3]) but monthly bevacizumab was not equivalent to as-needed bevacizumab (MD: −2.1 [95% CI, −5.7 to 1.6]).51Compared with the monthly regimen, the as-needed regimen was associated with a significant increase in mortality of 1.8% (95% CI, 0.1% to 3.4%, meta-analysis of mortality data reported in 2 RCTs, 1795 patients, with a RR of 2.0, 95% CI, 1.2 to 3.5).35 51
Table 4.
Comparison of monthly versus as needed anti-VEGF treatment regimens in cn-AMD patients
| Comparison | Outcome | No of RCTs*, no of patients |
Baseline ETDRS letters† and Snellen equivalent | As-needed regimen Mean (range)† |
Monthly regimen Mean (range)† | Risk ratio or mean difference
estimate (95% CI) |
I2‡ (%) |
| As-needed Rx vs monthly Rx | Vision gain | 2/1622 | 62 (61 to 63)~20/63 | 20.8% (15.1 to 26.4) | 28.9% (25.1 to 32.8) | 0.73 (0.55 to 0.95) | 0 |
| BCVA change | 2/1622 | 62 (61 to 63)~20/63 | 4.9 (3.5 to 6.4) | 6.9 (5.5 to 8.3) | −1.9 (-0.5 to 3.3) | 0 | |
| Mortality | 2/1795 | NA | 4.6% (2.6 to 6.6) | 2.3% (1.4 to 3.3) | 2.00 (1.15 to 3.45) | 12 |
*CATT and IVAN trials (Martin et al; Chakravarthy et al).35 51
†Mean (range) were derived across control groups of the included RCTs.
‡I2 <75 was interpreted as low evidence of substantial variation across included RCTs. For each treatment regimen, patients were randomised to be treated with bevacizumab or ranibizumab.
anti-VEGF, antivascular endothelial growth factor; BCVA, best-corrected visual acuity; CATT, Comparison of AMD Treatments Trials; cn-AMD, choroidal neovascular age-related macular degeneration; ETDRS, early treatment diabetic retinopathy study; IVAN, Inhibit VEGF in Age-related choroidal Neovascularisation; RCTs, randomised controlled trials.
Harms
Over an average of 14 months (range: 12–24 months), mortality was reported in 4% and 3% of patients treated with bevacizumab or ranibizumab, respectively (RR: 1.14 [95% CI, 0.72 to 1.79], 6 RCTs, 2941 patients, additional file 2:Appendix 6). Serious adverse events were reported in 19% and 18% of patients treated with bevacizumab or ranibizumab, respectively (RR: 1.09 [95% CI, 0.93 to 1.27], 5 RCTs, 3026 patients). Arterial TEs were reported in 4% and 3%of patients treated with bevacizumab or ranibizumab, respectively (RR: 0.86 [95% CI, 0.51 to 1.47], 4 RCTs, 2033 patients). Venous TEs, bacterial endophthalmitis and retinal detachment were reported in <1% of patients treated with either drug. In the trials evaluating aflibercept and ranibizumab, arterial TEs were reported in 2% of patients treated with aflibercept or ranibizumab (RR: 0.96 [95% CI, 0.45 to 2.04], 2 RCTs, 1818 patients), and venous TEs were reported in <1% of patients treated with either drug. Data on other harms were not available.
Patients with DMO
Comparative effectiveness of ranibizumab, bevacizumab and aflibercept
Results from DRCR.net trial (620 patients) showed that over 2 years of treatment, patients were as likely to attain vision gain with ranibizumab (37%), bevacizumab (35%) or aflibercept (39%)—bevacizumab versus ranibizumab, RR: 0.94 [95% CI, 0.72 to 1.23]; aflibercept versus bevacizumab, RR: 1.06 [95% CI, 0.80 to 1.38] and aflibercept versus ranibizumab, RR: 1.06 [95% CI, 0.82 to 1.37] (table 2). Over 2 years of treatment, approximately 98% of patients maintained their vision with all three drugs. Besides the DRCR.net RCT, two small single-centred RCTs reported BCVA data, one comparing aflibercept with ranibizumab,14 and another comparing bevacizumab and ranibizumab.31 Patients’ mean BCVA improved by approximately 13 letters with aflibercept, 10 letters with bevacizumab and 12 letters with ranibizumab (aflibercept vs ranibizumab: MD: 1.4 [95% CI, −1.6 to 4.3]; bevacizumab vs aflibercept: MD: −2.7 [95% CI, −5.2 to −0.3] and bevacizumab vs ranibizumab: MD: −2.0 [95% CI, −3.9 to −0.1], table 2).
The DRCR.net trial reported results stratified by baseline visual acuity at 12 and 24 months (additional file 2: Appendix 11). In patients with high baseline visual acuity (BCVA ≥69 letters), approximately 16% of patients treated with bevacizumab, 15% of patients treated with ranibizumab and 18% of patients treated with aflibercept attained vision gain at 12 months (RR of bevacizumab vs aflibercept: 0.91 [95% CI, 0.50 to 1.65]; RR of aflibercept vs ranibizumab: 1.18 [95% CI, 0.64 to 2.17]). Vision gain at 24 months was 17% with bevacizumab, 19% with ranibizumab and 20% with aflibercept (RR of bevacizumab vs aflibercept: 0.84 [95% CI, 0.47 to 1.52]; RR of aflibercept vs ranibizumab: 1.10 [95% CI, 0.63 to 1.92]). In patients with low baseline visual acuity (BCVA <69 letters), approximately 41% of patients treated with bevacizumab, 50% of patients treated with ranibizumab and 67% of patients treated with aflibercept attained vision gain at 12 months (RR of bevacizumab vs aflibercept: 0.62 [95% CI, 0.47 to 0.81]; RR of aflibercept vs ranibizumab: 1.35 [95% CI, 1.06 to 1.72]). At 24 months, vision gain was 52% with bevacizumab, 55% with ranibizumab and 58% with aflibercept (RR of bevacizumab vs aflibercept: 0.90 [95% CI, 0.69 to 1.16]; RR of aflibercept vs ranibizumab: 1.05 [95% CI, 0.82 to 1.35]).
Treatment regimen
With respect to treatment regimen, the DRCR.net trial treated patients initially with monthly injections until stable visual acuity within 6 months, followed by as-needed treatment (additional file 2: Appendix 10).27 The median number of injections administered over a 1-year period was 10 in the bevacizumab group, 9 in the aflibercept group and 10 in the ranibizumab group (table 3).27 In the second year, the median number of injections was: 6, 5 and 6 in the bevacizumab, aflibercept and ranibizumab groups, respectively.52 Two smaller trials both started treatment with 3 monthly intravitreal injections, followed by monthly retreatment with persistence of macular oedema, thickening of central macular or worsening of visual acuity (table 3 and additional file 2: Appendix 10).14 31
Harms
After 24 months of treatment in the DRCR.net trial,27 mortality was reported in approximately 6% of bevacizumab patients, 2% of aflibercept patients and 5% of ranibizumab patients (additional file 2: Appendix 6). Serious adverse events were reported in 21% of bevacizumab patients, 27% of aflibercept patients and 25% of ranibizumab patients. Arterial TEs were reported in 4%, 3% and 5%, of patients treated with bevacizumab, aflibercept and ranibizumab, respectively. Bacterial endophthalmitis and retinal detachments were reported in <1% of patients treated with any of the drugs.
Patients with RVO-MO
Comparative effectiveness of ranibizumab, bevacizumab and aflibercept
Results from one randomised, double-blind, controlled and non-inferiority trial conducted in India (including 77 patients with ME due to branch RVO) showed that approximately 59% of patients attained vision gain with bevacizumab and ranibizumab treatment, and no statistical difference was observed between the drugs (RR: 1.0 [95% CI, 0.68 to 1.45]; table 2 and additional file 2: Appendix 8).32 With respect to mean BCVA, patients treated with either drug gained an average of 16 letters (MD −2.5 [95% CI, −8.0 to 5.0]).
Results from the Study of Comparative Treatments for Retinal Vein Occlusion 2 (SCORE2) randomised non-inferiority trial conducted in 66 centres in the USA(348 patients with ME due to central RVO) showed that approximately 61% of patients treated with bevacizumab or aflibercept attained vision gain, with no statistical difference between the drugs (RR: 1.06 [95% CI, 0.91 to 1.25]; table 2).13 With respect to mean BCVA, patients treated with either drug gained an average of 19 letters (MD 1.52 [95% CI, −1.2 to 4.2)).
Treatment regimens
In the SCORE2 trial, patients were treated with monthly intravitreal injections for 6 months, with a mean number of 5.8 injections in patients treated with bevacizumab or aflibercept (table 3 and additional file 2: Appendix 11).13 In the other trial, patients were treated with one initial intravitreal injection and then as-needed monthly retreatment over 6 months, with a mean number of 3 injections in patients treated with bevacizumab or ranibizumab.13 32
Harms
Serious adverse events were reported in 3% of bevacizumab patients and 5% of ranibizumab patients (RR: 0.5 [95% CI, 0.05 to 5.26], 1 RCT, 74 patients; additional file 2: Appendix 8).32 Serious adverse events were reported in 8% of the patients treated with bevacizumab or aflibercept over 6 months (RR: 0.99 [95% CI, 0.49 to 2.00], 1 RCT, 362 patients).13
Patients with m-CNV
Comparative effectiveness of ranibizumab and bevacizumab
Two small RCTs both conducted in Italy evaluated ranibizumab and bevacizumab for patients with m-CNV. Results from one RCT (32 patients) showed that 62% of patients treated with bevacizumab and 56% of patients treated with ranibizumab attained vision gain (RR: 1.11 [95% CI, 0.63 to 1.96], 1 RCT; table 2 and additional file 2: Appendix 11).30 The other RCT (55 patients) only report BCVA results.29 With respect to mean BCVA, patients treated with bevacizumab gained 12 letters and patients treated with ranibizumab gained 13 letters (MD: −1.3 [95% CI, −6.5 to 4.0], 2 RCTs, 80 patients).29 30 The included trials did not report data on harms.
Treatment regimens
Both trials evaluated ranibizumab and bevacizumab with patients receiving 1 monthly intravitreal injection and as-needed monthly retreatment for 18 and 6 months, respectively, with a mean number of 3.1 injections per year in patients treated with bevacizumab and 2.4 injections in patients treated with ranibizumab (table 3 and additional file 2: Appendix 6).29 30
Discussion
This systematic review synthesised results from 19 RCTs to evaluate the comparative effectiveness and safety of intravitreal bevacizumab, ranibizumab and aflibercept for patients with cn-AMD, DMO, RVO-MO and m-CNV. Intravitreal bevacizumab was as effective as ranibizumab in patients with cn-AMD, DMO, RVO-MO and m-CNV for the outcomes examined. Ranibizumab was as effective as aflibercept in patients with cn-AMD.
In patients with DMO that were treated for 2 years, vision gain was equally likely to be attained with aflibercept, ranibizumab or aflibercept. In the first year of treatment, however, patients treated with aflibercept were more likely to attain vision gain than patients treated with ranibizumab or bevacizumab—differential effects that were observed mainly in patients with initial BCVA <69 letter scores (equivalent to 20/50 or worse) but not observed in patients with initial BCVA ≥69 letter scores (equivalent to 20/40 or better) based on the results from the subgroup analyses. Rates of systemic serious harms were similarly low among the anti-VEGF drugs, across the retinal conditions. None of the included RCTs were designed with sufficient statistical power to detect significant differences between the treatments with respect to the incidence of harms. In our posthoc analysis, cn-AMD patients and compared with monthly treatment, an as-needed treatment regimen (ie, 6–9 monthly injections per year) was significantly associated with a small loss in visual acuity, but a significant increase in mortality risk of 1.8% (RR: 2.0 [95% CI, 1.2 to 3.5]).
Results from the Comparison of AMD Treatments Trials (CATT) and Inhibit VEGF in Age-related choroidal Neovascularisation (IVAN) trials showed that relative to monthly treatment, patients with cn-AMD receiving as-needed treatment experienced a significant increase in risk of mortality. Whether there are any biological explanations for the increased risk of mortality associated with fewer monthly injections is unclear and this finding may have been attributable to chance. As such, further research should be conducted to verify this result. In DMO, RVO-MO and m-CNV trials, patients tended to receive fewer monthly injections per year (table 3). None of the trials in DMO, RVO-MO and m-CNV patients evaluated a monthly treatment regimen, and therefore the safety risk between as-needed and monthly regimens could not be evaluated. This requires further study.
Additional file 2: Appendix 12 displays the mean change in BCVA over time in patients treated with bevacizumab or ranibizumab. For all of the retinal conditions, patients showed improvement in mean BCVA by 3–6 months with initial monthly injections, and maintained a plateau to 24 months in the treatment of cn-AMD patients (average improvement of 6 letters), DMO patients (eight letters), RVO-MO patients (16 letters) and m-CNV patients (11 letters). Comparative outcomes beyond 6 months in patients with RVO-MO and m-CNV were lacking and as such, long-term comparative data of anti-VEGF drugs in these patients are needed.
Our findings are consistent with findings from previous systematic reviews. A meta-analysis of six head-to-head trials concluded that bevacizumab and ranibizumab had equivalent efficacy with respect to visual acuity in cn-AMD patients.11 A meta-analysis of five RCTs suggested no differences in effectiveness between ranibizumab and bevacizumab in DMO patients.53 Other reviews in patients with RVO-MO and m-CNV came to similar conclusions.9 10 54 55 Although findings were consistent with those in these recent reviews, our review serves as an update (with the inclusion of data up to 2017) while also examining the additional factor of treatment regimen.
There are several limitations worth noting. First, none of our sensitivity and subgroup analyses were specified a-priori and as such, these results should be interpreted with caution. This also pertains to our posthoc analysis on treatment regimen. Second, we limited our review to English studies due to time and resources constraints. We believe, however, that the impact of the restrictions is small since our findings are consistent with previous systematic reviews that included RCTs reported in all languages, evaluating the same anti-VEGF drugs for specific retinal conditions,11 53 56 and results were consistent across studies, so the impact of including additional studies reported in other languages, if any, would be insignificant. We only identified a few RCTs evaluating the anti-VEGF drugs in patients with DMO, RVO-MO and m-CNV. We did not include ziv-aflibercept (a low-cost anti-VEGF alternative to aflibercept and bevacizumab57), the old anti-VEGF pegaptanib, or the newest anti-VEGF brolucizumab. Although the rates of reported adverse events were similar across the anti-VEGF drugs, the assessment of harms using comparative trial data is limited. We excluded RCTs which randomised eyes (instead of patients) since the reported analyses failed to adjust for the correlation between the outcomes of eyes from the same individuals.58 Similarly, we also excluded one quasi-randomised trial,59 because we focused on randomised studies.
Conclusions
Intravitreal bevacizumab was a reasonable alternative to ranibizumab and aflibercept in patients with cn-AMD, DMO, RVO-MO and m-CNV. The only exception was for patients with DMO and low visual acuity (<69 ETDRS letters, 20/50 or worse), where treatment with aflibercept was associated with significantly higher vision gain (≥15 ETDRS letters) than bevacizumab or ranibizumab at 12 months; but the significant effects were not maintained at 24 months. The choice of anti-VEGF drug may depend on specific retinal conditions, baseline visual acuity and treatment regimen.
Supplementary Material
Acknowledgments
We thank Becky Skidmore for drafting our search strategies, Kelly Farrah for peer reviewing the search strategies (PRESS) and Alissa Epworth for deduplicating search results and obtaining full-text articles. We thank Meghan Kenny for helping screen studies for inclusion and performing quality appraisal and Jaimie Adams for helping screen studies for inclusion. We would also like to thank Michel Boucher, Sarah Berglas, Hongbo Yuan and Sarah Jennings for their valuable contribution, insights, and for facilitating the production and dissemination of the synthesised evidence. In addition, we would like to thank the clinical experts and stakeholders who provided feedback on the previous therapeutic review report. Finally, we thank Susan Le, Inthuja Selvaratnam, Katrina Chiu and Krystle Amog for preparing tables and formatting the manuscript for submission.
Footnotes
Contributors: BP screened titles, abstracts and full-text articles; abstracted and cleaned data, conducted quality assessment and drafted the manuscript. SMT led the coordination of the systematic review; drafted the protocol; screened titles, abstracts and full-text articles; abstracted and cleaned data; conducted quality assessment; and helped draft and revise the manuscript. TL screened titles, abstracts and full-text articles; abstracted and cleaned data; conducted quality assessment; helped conduct meta-analysis and reviewed the manuscript. EL screened titles, abstracts and full-text articles; abstracted and cleaned data; conducted quality assessment and reviewed the manuscript. JH conducted the analysis and interpretation of data; and reviewed the manuscript. TR helped with conceptualising the research design, drafting and revising the protocol, interpretation of data and reviewed the manuscript. GJ helped draft and revise the protocol; screened titles, abstracts and full-text articles; abstracted data; conducted quality assessment; helped interpret the data and reviewed the manuscript. AA screened titles, abstracts and full-text articles; abstracted and cleaned data; conducted quality assessment and reviewed the manuscript. JPS screened titles, abstracts and full-text articles; abstracted and cleaned data; conducted quality assessment and reviewed the manuscript. AS screened titles, abstracts and full-text articles; abstracted and cleaned data, conducted quality assessment and reviewed the manuscript. RW screened titles, abstracts and full-text articles; abstracted and cleaned data, conducted quality assessment and reviewed the manuscript. RB abstracted and cleaned data, conducted quality assessment and reviewed the manuscript. EM screened titles, abstracts and full-text articles; abstracted and cleaned data; and reviewed the manuscript. SES helped with conceptualising the research and design; interpretation of data and reviewed the manuscript. ACT conceptualised the research and design; drafted the protocol; obtained funding; assisted with data acquisition and interpretation; and drafted and revised the manuscript. ACT and BP had full access to all the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: This work was supported by the Canadian Institutes of Health Research/Drug Safety and Effectiveness Network (CIHR/DSEN). SES is funded by a Tier 1 Canada Research Chair in Knowledge Translation. ACT is funded by a Tier 2 Canada Research Chair in Knowledge Synthesis. The therapeutic review was commissioned by the Canadian Agency for Drugs and Technology in Health (CADTH) and funded by a grant from the Canadian Institutes of Health Research Drug Safety and Effectiveness Network. The funders had no role in design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript and decision to submit the manuscript for publication.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data sets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Presented at: The data from the original therapeutic review were presented by ACT and SMT to the Canadian Drug Expert Committee in Ottawa, Ontario, on 17 November 2015.
Patient consent for publication: Not required.
References
- 1. Bourne RR, Jonas JB, Flaxman SR, et al. Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe: 1990-2010. Br J Ophthalmol 2014;98:629–38. 10.1136/bjophthalmol-2013-304033 [DOI] [PubMed] [Google Scholar]
- 2. Congdon N, O’Colmain B, Klaver CC, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol 2004;122:477–85. 10.1001/archopht.122.4.477 [DOI] [PubMed] [Google Scholar]
- 3. Campochiaro PA. Anti-vascular endothelial growth factor treatment for retinal vein occlusions. Ophthalmologica 2012;227(Suppl 1):30–5. 10.1159/000337157 [DOI] [PubMed] [Google Scholar]
- 4. Ehlers JP, Fekrat S. Retinal vein occlusion: beyond the acute event. Surv Ophthalmol 2011;56:281–99. 10.1016/j.survophthal.2010.11.006 [DOI] [PubMed] [Google Scholar]
- 5. Ford JA, Elders A, Shyangdan D, et al. The relative clinical effectiveness of ranibizumab and bevacizumab in diabetic macular oedema: an indirect comparison in a systematic review. BMJ 2012;345:e5182 10.1136/bmj.e5182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Silva R. Myopic maculopathy: a review. Ophthalmologica 2012;228:197–213. 10.1159/000339893 [DOI] [PubMed] [Google Scholar]
- 7. Wong TY, Ferreira A, Hughes R, et al. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am J Ophthalmol 2014;157:9–25. 10.1016/j.ajo.2013.08.010 [DOI] [PubMed] [Google Scholar]
- 8. Taylor DJ, Hobby AE, Binns AM, et al. How does age-related macular degeneration affect real-world visual ability and quality of life? A systematic review. BMJ Open 2016;6:e011504 10.1136/bmjopen-2016-011504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhu Y, Zhang T, Xu G, et al. Anti-vascular endothelial growth factor for choroidal neovascularisation in people with pathological myopia. Cochrane Database Syst Rev 2016;12:CD011160 10.1002/14651858.CD011160.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Braithwaite T, Nanji AA, Lindsley K, et al. Anti-vascular endothelial growth factor for macular oedema secondary to central retinal vein occlusion. Cochrane Database Syst Rev 2014:CD007325 10.1002/14651858.CD007325.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Solomon SD, Lindsley KB, Krzystolik MG, et al. Intravitreal Bevacizumab Versus Ranibizumab for Treatment of Neovascular Age-Related Macular Degeneration: Findings from a Cochrane Systematic Review. Ophthalmology 2016;123:70–7. 10.1016/j.ophtha.2015.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Virgili G, Parravano M, Evans JR, et al. Anti-vascular endothelial growth factor for diabetic macular oedema: a network meta-analysis. Cochrane Database Syst Rev 2017;6:Cd007419 10.1002/14651858.CD007419.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Scott IU, VanVeldhuisen PC, Ip MS, et al. Effect of Bevacizumab vs Aflibercept on Visual Acuity Among Patients With Macular Edema Due to Central Retinal Vein Occlusion: The SCORE2 Randomized Clinical Trial. JAMA 2017;317:2072–87. 10.1001/jama.2017.4568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fouda SM, Bahgat AM. Intravitreal aflibercept versus intravitreal ranibizumab for the treatment of diabetic macular edema. Clin Ophthalmol 2017;11:567–71. 10.2147/OPTH.S131381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Maguire MG, Martin DF, Ying GS, et al. Five-Year Outcomes with Anti-Vascular Endothelial Growth Factor Treatment of Neovascular Age-Related Macular Degeneration: The Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology 2016;123:1751–61. 10.1016/j.ophtha.2016.03.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tricco A, Straus S, Thomas S, et al. Comparative efficacy and safety of three different anti-vascular endothelial growth factor (VEGF) drugs for retinal conditions: a systematic review PROSPERO: International prospective register of systematic reviews. 2015. http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42015022041 (accessed October 18. 2017).
- 17. Thomas SM, Pham B, Lee T, et al. Anti–vascular endothelial growth factor drugs for the treatment of retinal conditions. Ottawa: CADTH, 2016. [Google Scholar]
- 18. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 19. CADTH. Grey Matters: a practical tool for searching health-related grey literature. Ottawa: CADTH, 2015. [Google Scholar]
- 20. Sampson M, McGowan J, Cogo E, et al. An evidence-based practice guideline for the peer review of electronic search strategies. J Clin Epidemiol 2009;62:944–52. 10.1016/j.jclinepi.2008.10.012 [DOI] [PubMed] [Google Scholar]
- 21. Falkenstein IA, Cochran DE, Azen SP, et al. Comparison of visual acuity in macular degeneration patients measured with snellen and early treatment diabetic retinopathy study charts. Ophthalmology 2008;115:319–23. 10.1016/j.ophtha.2007.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mangione CM, Lee PP, Pitts J, et al. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Arch Ophthalmol 1998;116:1496–504. [DOI] [PubMed] [Google Scholar]
- 23. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1–34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 24. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gregori NZ, Feuer W, Rosenfeld PJ. Novel method for analyzing snellen visual acuity measurements. Retina 2010;30:1046–50. 10.1097/IAE.0b013e3181d87e04 [DOI] [PubMed] [Google Scholar]
- 26. Greene WH. Econometric Analysis. 5th edn New York, NY: Pearson, 2003:913. [Google Scholar]
- 27. Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med 2015;372:1193–203. 10.1056/NEJMoa1414264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Higgins J, Green S, Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0: The Cochrane Collaboration, 2011. [Google Scholar]
- 29. Iacono P, Parodi MB, Papayannis A, et al. Intravitreal ranibizumab versus bevacizumab for treatment of myopic choroidal neovascularization. Retina 2012;32:1539–46. 10.1097/IAE.0b013e31826956b7 [DOI] [PubMed] [Google Scholar]
- 30. Gharbiya M, Giustolisi R, Allievi F, et al. Choroidal neovascularization in pathologic myopia: intravitreal ranibizumab versus bevacizumab--a randomized controlled trial. Am J Ophthalmol 2010;149:458–64. 10.1016/j.ajo.2009.10.010 [DOI] [PubMed] [Google Scholar]
- 31. Ekinci M, Ceylan E, Çakıcı Özgür, et al. Treatment of macular edema in diabetic retinopathy: comparison of the efficacy of intravitreal bevacizumab and ranibizumab injections. Expert Rev Ophthalmol 2014;9:139–43. 10.1586/17469899.2014.900439 [DOI] [Google Scholar]
- 32. Narayanan R, Panchal B, Das T, et al. A randomised, double-masked, controlled study of the efficacy and safety of intravitreal bevacizumab versus ranibizumab in the treatment of macular oedema due to branch retinal vein occlusion: MARVEL Report No. 1. Br J Ophthalmol 2015;99:954–9. 10.1136/bjophthalmol-2014-306543 [DOI] [PubMed] [Google Scholar]
- 33. Berg K, Pedersen TR, Sandvik L, et al. Comparison of ranibizumab and bevacizumab for neovascular age-related macular degeneration according to LUCAS treat-and-extend protocol. Ophthalmology 2015;122:146–52. 10.1016/j.ophtha.2014.07.041 [DOI] [PubMed] [Google Scholar]
- 34. Scholler A, Richter-Mueksch S, Weingessel B, et al. Differences of frequency in administration of ranibizumab and bevacizumab in patients with neovascular AMD. Wien Klin Wochenschr 2014;126(11-12):355–9. 10.1007/s00508-014-0539-z [DOI] [PubMed] [Google Scholar]
- 35. Chakravarthy U, Harding SP, Rogers CA, et al. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet 2013;382:1258–67. 10.1016/S0140-6736(13)61501-9 [DOI] [PubMed] [Google Scholar]
- 36. Kodjikian L, Souied EH, Mimoun G, et al. Ranibizumab versus Bevacizumab for Neovascular Age-related Macular Degeneration: Results from the GEFAL Noninferiority Randomized Trial. Ophthalmology 2013;120:2300–9. 10.1016/j.ophtha.2013.06.020 [DOI] [PubMed] [Google Scholar]
- 37. Krebs I, Schmetterer L, Boltz A, et al. A randomised double-masked trial comparing the visual outcome after treatment with ranibizumab or bevacizumab in patients with neovascular age-related macular degeneration. Br J Ophthalmol 2013;97:266–71. 10.1136/bjophthalmol-2012-302391 [DOI] [PubMed] [Google Scholar]
- 38. Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 2012;119:2537–48. 10.1016/j.ophtha.2012.09.006 [DOI] [PubMed] [Google Scholar]
- 39. Biswas P, Sengupta S, Choudhary R, et al. Comparative role of intravitreal ranibizumab versus bevacizumab in choroidal neovascular membrane in age-related macular degeneration. Indian J Ophthalmol 2011;59:191–6. 10.4103/0301-4738.81023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Biswas P, Sengupta S, Choudhary R, et al. Comparing ranibizumab with bevacizumab. Ophthalmology 2011;118:600–600.e2. 10.1016/j.ophtha.2010.10.027 [DOI] [PubMed] [Google Scholar]
- 41. The CATT Research Group. Ranibizumab and Bevacizumab for Neovascular Age-Related Macular Degeneration. N Engl J Med Overseas Ed 2011;364:1897–908. 10.1056/NEJMoa1102673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Subramanian ML, Abedi G, Ness S, et al. Bevacizumab vs ranibizumab for age-related macular degeneration: 1-year outcomes of a prospective, double-masked randomised clinical trial. Eye 2010;24:1708–15. 10.1038/eye.2010.147 [DOI] [PubMed] [Google Scholar]
- 43. Nguyen QD, Brown DM, Marcus DM, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012;119:789–801. 10.1016/j.ophtha.2011.12.039 [DOI] [PubMed] [Google Scholar]
- 44. Heier JS, Korobelnik JF, Brown DM, et al. Intravitreal Aflibercept for Diabetic Macular Edema: 148-Week Results from the VISTA and VIVID Studies. Ophthalmology 2016;123:2376–85. 10.1016/j.ophtha.2016.07.032 [DOI] [PubMed] [Google Scholar]
- 45. Elman MJ, Aiello LP, Beck RW, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 2010;117:1064–77. 10.1016/j.ophtha.2010.02.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Brown DM, Campochiaro PA, Singh RP, et al. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology 2010;117:1124–33. 10.1016/j.ophtha.2010.02.022 [DOI] [PubMed] [Google Scholar]
- 47. Campochiaro PA, Brown DM, Pearson A, et al. Sustained delivery fluocinolone acetonide vitreous inserts provide benefit for at least 3 years in patients with diabetic macular edema. Ophthalmology 2012;119:2125–32. 10.1016/j.ophtha.2012.04.030 [DOI] [PubMed] [Google Scholar]
- 48. Boyer D, Heier J, Brown DM, et al. Vascular endothelial growth factor Trap-Eye for macular edema secondary to central retinal vein occlusion: six-month results of the phase 3 COPERNICUS study. Ophthalmology 2012;119:1024–32. 10.1016/j.ophtha.2012.01.042 [DOI] [PubMed] [Google Scholar]
- 49. Holz FG, Roider J, Ogura Y, et al. VEGF Trap-Eye for macular oedema secondary to central retinal vein occlusion: 6-month results of the phase III GALILEO study. Br J Ophthalmol 2013;97:278–84. 10.1136/bjophthalmol-2012-301504 [DOI] [PubMed] [Google Scholar]
- 50. Bucher HC, Guyatt GH, Griffith LE, et al. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol 1997;50:683–91. 10.1016/S0895-4356(97)00049-8 [DOI] [PubMed] [Google Scholar]
- 51. Martin DF, Maguire MG, Ying GS, et al. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med 2011;364:1897–908. 10.1056/NEJMoa1102673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, Bevacizumab, or Ranibizumab for Diabetic Macular Edema: Two-Year Results from a Comparative Effectiveness Randomized Clinical Trial. Ophthalmology 2016;123 10.1016/j.ophtha.2016.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ford JA, Lois N, Royle P, et al. Current treatments in diabetic macular oedema: systematic review and meta-analysis. BMJ Open 2013;3:e002269 10.1136/bmjopen-2012-002269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ford JA, Clar C, Lois N, et al. Treatments for macular oedema following central retinal vein occlusion: systematic review. BMJ Open 2014;4:e004120 10.1136/bmjopen-2013-004120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mitry D, Bunce C, Charteris D. Anti-vascular endothelial growth factor for macular oedema secondary to branch retinal vein occlusion. Cochrane Database Syst Rev 2013;1:CD009510 10.1002/14651858.CD009510.pub2 [DOI] [PubMed] [Google Scholar]
- 56. Solomon SD, Lindsley K, Vedula SS, et al. Anti-vascular endothelial growth factor for neovascular age-related macular degeneration. Cochrane Database Syst Rev 2014:Cd005139 10.1002/14651858.CD005139.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Singh SR, Dogra A, Stewart M, et al. Intravitreal Ziv-Aflibercept: Clinical Effects and Economic Impact. Asia Pac J Ophthalmol 2017;6 10.22608/APO.2017263 [DOI] [PubMed] [Google Scholar]
- 58. Pece A, Milani P, Monteleone C, et al. A randomized trial of intravitreal bevacizumab vs. ranibizumab for myopic CNV. Graefes Arch Clin Exp Ophthalmol 2015;253:1867–72. 10.1007/s00417-014-2886-x [DOI] [PubMed] [Google Scholar]
- 59. Russo V, Barone A, Conte E, et al. Bevacizumab compared with macular laser grid photocoagulation for cystoid macular edema in branch retinal vein occlusion. Retina 2009;29:511–5. 10.1097/IAE.0b013e318195ca65 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-022031supp001.pdf (31.2KB, pdf)
bmjopen-2018-022031supp002.pdf (1.1MB, pdf)