Abstract
Background: Long-term trends mask critical recent dynamics in the prevalence of under- and overweight.
Objective: The objective of this study was to compare annualized prevalence rates of both under- and overweight among nonpregnant women aged 19–49 y during the periods covering 1) the 1990s–the early 2000s and 2) the early 2000s–the late 2000s or early 2010s, by rural–urban residence.
Methods: Data are from nationally representative surveys (29 Demographic and Health Surveys and 4 national surveys). Standardized protocols were used to measure weight and height. Underweight was defined as body mass index (BMI) < 18.5 kg/m2 and overweight as BMI ≥ 25 kg/m2.
Results: From the 1990s to the early 2000s, most countries were making progress on decreasing the prevalence of underweight, especially in rural areas. Although many countries continued to make progress more recently, several countries in Sub-Saharan Africa that previously had a decreasing prevalence of underweight now have an increasing prevalence of underweight. For example, in rural areas of Senegal, the prevalence of underweight decreased 0.23% annually between 1992 and 2005, then increased 1.60% annually between 2005 and 2010. Meanwhile, the prevalence of overweight is increasing in nearly all countries, and in approximately half of all countries, the rate of increase is greater in rural areas than in urban areas. Although underweight persists as more prevalent than overweight in rural areas of many East Asian, South Asian, and Sub-Saharan African countries, the ratio of underweight to overweight in many countries has decreased over time, indicating that this trend is reversing.
Conclusions: Select countries in Sub-Saharan Africa may be more susceptible to food crises and should be targets for intervention. At the same time, global health efforts need to focus on preventing overweight, particularly in rural areas, which are quickly catching up to their urban counterparts.
Keywords: underweight, overweight, dual burden, rural health, developing countries
Introduction
Scientific evidence consistently supports urbanization as a key underlying factor in the rise in prevalence of overweight in low- and middle-income countries (LMIC)5, whereas underweight has traditionally affected mainly rural areas (1–5). However, areas officially designated as “rural” are not immune to the effects of urbanization (6–9), nor are “urban” areas free of the burden of underweight (10, 11). Widespread access to cheap, energy-dense foods and motorized transportation in conjunction with rapid expansion of global mass media have led to more urbanized ways of life in areas classically designated as “rural” (6–9). Indeed, an analysis of the World Health Survey (2002–2003) found similar effects of urbanization on the prevalence of under- and overweight in urban and rural areas (5). Furthermore, the vulnerability of the urban poor to health risks such as underweight is increasingly recognized by researchers and international organizations, including the UN (12). Analysis of recent data is needed to identify populations susceptible to increasing burdens of under- and overweight in order to develop appropriate interventions and policies.
Women are a critically important population subgroup for targeting given evidence that prepregnancy BMI is a strong predictor of neonatal and childhood health outcomes (13). For example, maternal underweight is associated with an increased risk of having small-for-gestational-age and low-birth-weight infants (14, 15) and maternal overweight is associated with increased risk of congenital defects in infants (16). Improving maternal health was 1 of 8 UN Millennium Development Goals and will likely be a key component of the post-2015 development agenda. Updated data on maternal under- and overweight in LMIC are needed to inform the direction of this agenda.
Previous studies of trends in body composition among adults in LMIC focused only on overweight (17–19), included a single country (20, 21), used both measured and self-reported weight and height data (17), calculated only a single annualized prevalence rate spanning several decades (22), and did not evaluate separate trends in rural vs. urban regions within countries (18–20), which is essential, because national-level estimates mask important subnational variations.
This study is unique in examining annualized prevalence rates of both under- and overweight among nonpregnant women aged 19–49 y during the periods covering 1) the 1990s–the early 2000s and 2) the early 2000s–the late 2000s or early 2010s, by rural–urban residence, and then the changes in prevalence between these 2 periods.
Methods
Data sources.
Most data (surveys from 29 countries) are from the Demographic and Health Surveys (DHSs), a series of nationally representative surveys typically conducted every 5 y (23). Details of sampling methodology for the DHSs are described elsewhere (24). Additional data are from the Indonesian Family Life Surveys (representative of 83% of the Indonesian population) (25), the China Health and Nutrition Surveys (representative of 56% of the Chinese population) (26), the Brazilian national surveys (nationally representative) (27), and the Mexican Health and Nutrition Surveys (nationally representative) (28–30).
Study population and sample size.
All analyses were restricted to nonpregnant women aged 19–49 y (except for the 1989 and 2003 surveys in Brazil, for which pregnancy status was not available). Thirty-three countries had data from at least 3 surveys and were therefore included in this analysis. For countries with more than 3 surveys, the oldest survey and 2 most recent surveys were included in this analysis. The mean rural sample size was 3670 and the mean urban sample size was 3333; the overall rural sample size was 363,320 and the overall urban sample size was 329,933.
Measures.
All surveys used standardized protocols to measure weight and height (31). BMI was calculated as weight in kilograms divided by height in meters squared. Underweight and overweight were defined according to the WHO's recommendation: underweight, BMI < 18.5 kg/m2, and overweight, BMI ≥ 25 kg/m2 (32).
Rural–urban residence was defined by each country's national statistical office at the time of each survey. “Urban” areas included large cities (capitals and cities with over 1 million population), small cities (population over 50,000), and towns (other urban areas) (33). “Rural” areas were assumed to be countryside (33). Data on gross domestic product per capita (GDPPC) are from the 2010 World Bank Development Indicators (34). Results presented in the figures are sorted by GDPPC.
Statistical analysis.
All statistical analyses were conducted using Stata, version 13 (StataCorp). We calculated the prevalence of underweight and overweight at 3 time points for all countries (rural areas, Supplemental Table 1, and urban areas, Supplemental Table 2). Standard errors and 95% CIs were calculated using the Taylor series linearization variance estimator in Stata, which accounts for the complex sampling method. As a sensitivity analysis to explore the effects of demographic shifts in age distribution over time, data were age-standardized to the 2010 world population (35) (rural areas, Supplemental Table 1, and urban areas, Supplemental Table 2). Results presented in the text and figures are unstandardized unless otherwise indicated. To compare past and recent trends in the prevalence of under- and overweight, we calculated 2 annualized prevalence rates for each country: 1) earliest (1990s) to middle (early 2000s) survey and 2) middle (early 2000s) to latest (late 2000s or early 2010s) survey. We then calculated the difference between these 2 annualized prevalence rates. The relative prevalence of under- vs. overweight was calculated by dividing the prevalence of these measures at each of the 3 time points. All analyses were stratified by rural–urban residence (33).
Results
Earlier trends in the prevalence of underweight.
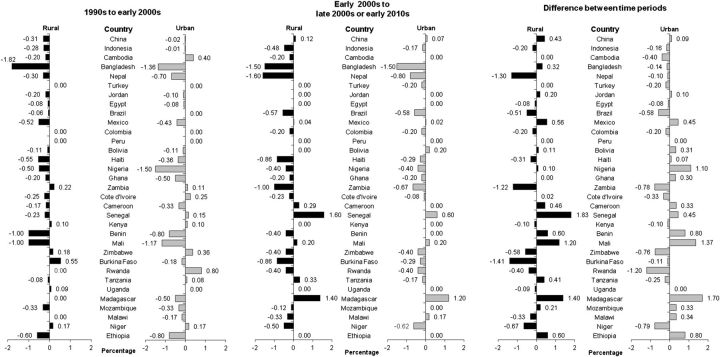
The annualized change in the prevalence of underweight for both the earlier and later time periods, across all countries and sorted by region and GDPPC within region, is presented in Figure 1. From the 1990s to the early 2000s, underweight was decreasing to a greater extent in rural areas than in urban areas in all countries outside of Sub-Saharan Africa except Nepal, where the prevalence was decreasing by 0.30% annually in rural areas and by 0.70% annually in urban areas. In Sub-Saharan Africa, there was much greater variability. For example, 6 countries (Nigeria, Ghana, Cameroon, Mali, Madagascar, and Ethiopia) had greater decreases in the prevalence of underweight in urban areas than did rural areas, and 4 countries (Zambia, Kenya, Zimbabwe, and Niger) had increases in the prevalence of underweight in both rural and urban areas.
FIGURE 1.
National annualized change in the prevalence of underweight among nonpregnant women aged 19–49 y by rural–urban residence, sorted by region and 2010 per capita gross domestic product within region. Underweight was defined according to the WHO's recommendation as BMI < 18.5 kg/m2.
Later trends in the prevalence of underweight.
More recently (early 2000s to late 2000s or early 2010s), the prevalence of underweight continued to decrease or remained unchanged in most (79% of countries) rural and urban areas (Figure 1). However, 3 countries stood out as having large increases in underweight relative to the earlier time period: Senegal, Madagascar, and Mali, although the large increase in urban areas in Mali was somewhat attenuated in age-standardized analyses. For example, in Madagascar, the prevalence of underweight was previously not increasing in rural areas and decreasing by 0.50% annually in urban areas, but during the more recent time period, it was increasing by 1.40% and 1.20% annually in rural and urban areas, respectively. Rural areas in China, Mexico, Cameroon, and Tanzania, and urban areas in Bolivia and Malawi, also experienced this “flip,” whereby an underweight prevalence that was decreasing in earlier time periods was increasing in more recent time periods. There were also some important improvements to note. For example, in Zambia and Zimbabwe, where the prevalence of underweight was previously increasing in both rural and urban areas, the prevalence of underweight has been decreasing more recently. In rural areas of Niger, there were also improvements in the prevalence of underweight, which was previously increasing but decreased during the more recent time period. However, of note, in urban areas of Niger, unstandardized results indicated that underweight was increasingly slightly in the earlier time period (0.17% annually), whereas age-standardized results indicated that underweight was decreasing slightly (−0.23% annually); in the more recent time period, both unstandardized and age-standardized results indicated that underweight was decreasing in this population.
Earlier trends in the prevalence of overweight.
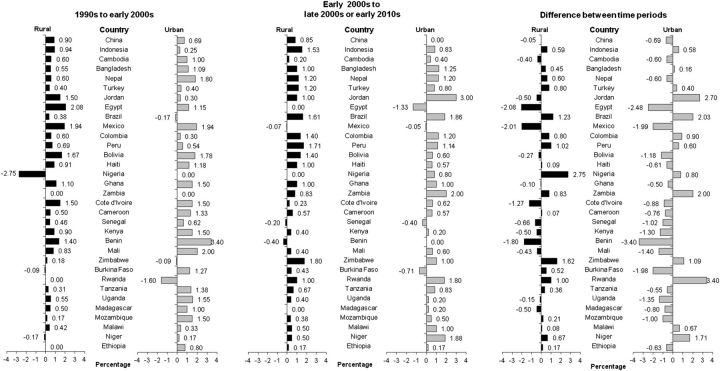
The annualized change in the prevalence of overweight for both the earlier and later time periods, across all countries and sorted by region and GDPPC within region, is presented in Figure 2. The prevalence of overweight was increasing in most countries (82% in rural areas; 85% in urban areas) during the period covering the 1990s to the early 2000s. The major exceptions were Nigeria, where the prevalence was decreasing by 2.75% annually in rural areas, and Rwanda, where the prevalence was decreasing by 1.60% annually in urban areas. The prevalence of overweight in many rural areas was already catching up to urban areas during this earlier time period; indeed, in 27% of countries, the prevalence of overweight in rural areas was increasing at a rate greater than that in urban areas. However, there was a clear distinction between Sub-Saharan Africa and all other regions: overweight was not increasing as much in rural areas and remained much lower than urban areas in most Sub-Saharan African countries in contrast to countries in other parts of the world.
FIGURE 2.
National annualized change in the prevalence of overweight among nonpregnant women aged 19–49 y by rural–urban residence, sorted by region and 2010 per capita gross domestic product within region. Overweight was defined according to the WHO's recommendation as BMI ≥ 25 kg/m2.
Later trends in the prevalence of overweight.
More recently (early 2000s to late 2000s or early 2010s), the prevalence of overweight continued to increase in most countries (85% in both rural and urban areas) (Figure 2). Indeed, several countries with a previously decreasing or unchanged prevalence of overweight witnessed large increases in the prevalence of overweight during the later time period. For example, in urban Rwanda, the annual change in the prevalence of overweight went from −1.60% to +1.80%; in urban Zambia it went from 0% to +2.00%; and in urban Brazil it went from −0.17% to +1.86%. Two key exceptions to this trend were Mexico and Benin. In Mexico, overweight was previously increasing by nearly 2% annually, but is now decreasing slightly in both rural and urban areas. Results from age-standardization were similar, but did not indicate a decreasing prevalence but, rather, a substantially smaller increase (e.g., in rural areas, from +1.94% to −0.07% in unstandardized analyses and from +1.74% to +0.18% in age-standardized analyses). In Benin, overweight was increasing by 1.40% and 3.40% annually in rural and urban areas, respectively, but is now decreasing by 0.40% annually in rural areas and unchanged in urban areas.
Similar to the earlier time period, during the more recent time period (early 2000s to late 2000s or early 2010s), the prevalence of overweight in rural areas was increasing at a rate greater than that in urban areas in 33% of countries (Figure 2). Furthermore, there was again a clear distinction between Sub-Saharan Africa and all other regions: rural areas were not catching up to urban areas in as many Sub-Saharan African countries as countries in other parts of the world (21% in Sub-Saharan Africa vs. 50% in all other regions combined).
Relative prevalence of under- vs. overweight.
In Latin America and the Caribbean, the prevalence of overweight was substantially higher than the prevalence of underweight in both rural and urban areas for all survey years except 1994 in rural Haiti (Supplemental Table 1). For example, in 2010, the prevalence of over- and underweight in rural Colombia was 53.66% and 3.21%, respectively. Furthermore, later surveys tended to have ratios of underweight to overweight closer to zero than did earlier surveys, indicating that the prevalence of overweight is increasingly surpassing that of underweight in this region. Similarly, in Turkey, Jordan, and Egypt, the prevalence of overweight exceeded that of underweight across all survey years.
This phenomenon of a greater burden of overweight than underweight was also observed in the more recent surveys from urban areas in East Asia and the Pacific, South Asia, and Sub-Saharan Africa. In most rural areas in these regions, however, the prevalence of underweight continues to exceed that of overweight. For example, in 2011, the prevalence of under- and overweight in rural Bangladesh was 26.88% and 12.79%, respectively (Supplemental Table 1). In Sub-Saharan Africa, rural areas of 6 countries (Senegal, Mali, Burkina Faso, Madagascar, Niger, and Ethiopia) had similar situations with the most recent prevalence of underweight exceeding that of overweight. For example, in 2011, the prevalence of under- and overweight in rural Ethiopia was 25.25% and 3.13%, respectively (Supplemental Table 1). Of note, 3 Sub-Saharan African countries with the lowest GDPPC (Madagascar, Niger, and Ethiopia) fell into this group.
There is some evidence to suggest that the prevalence of overweight in some rural areas of East Asia and the Pacific and South Asia is approaching that of underweight, as indicated by the decreasing ratios of underweight to overweight in these regions over time. For example, the ratio in Bangladesh went from 16.83 in 1993 to 2.10 in 2011. There was much more heterogeneity in this ratio over time in Sub-Saharan Africa, with an increasing trend observed in some countries over time (e.g., Niger) and a decreasing trend observed in other countries (e.g., Cote d'Ivoire and Mali).
Discussion
During the period spanning the 1990s to the early 2000s, the majority of countries included in this analysis were making progress on decreasing the prevalence of underweight, especially in rural areas. Although many countries continued to make progress more recently, several countries in Sub-Saharan Africa that previously had a decreasing prevalence of underweight now have an increasing prevalence of underweight. Meanwhile, the prevalence of overweight is increasing in nearly all countries, and in approximately half of all countries, the rate of increase is greater in rural areas than in urban areas.
As early as 1992–2000, there was evidence suggesting that the burden of overweight was exceeding that of underweight in LMIC, particularly those with higher per capita gross national incomes (3). Here we document that this trend is not only continuing, but also expanding to include both urban and rural areas, particularly in Asia, as well as Latin America and the Caribbean. We suspect that the factors underlying these shifts in disease burden relate to concurrent changes in the food value chain of LMIC, whereby transnational retail sectors have expanded rapidly and the purchasing of consumer packaged foods and beverages has increased (36). However, the research community has not yet quantified changes in the food system spanning agriculture to retail in LMIC or the resulting health effects. This will be a critical next step in understanding and preventing the burden of malnutrition in these countries.
We found a set of Sub-Saharan African countries with increasing underweight and varying shifts in overweight status. The prevalence of underweight in Senegal, which was decreasing during the earlier time period (1992–2005), is now on the rise in both rural and urban areas (2005–2010). This shift in progress on alleviating underweight in this population could be the result of rises in the cost of food following the 2007–2008 food crisis and a poor harvest in 2007. For example, in July 2008, the price of rice in Senegal was more than double the price in July 2007 (37). Similarly, in Mali (2001–2006) and Madagascar (2003–2008), the prevalence of underweight increased in the later time period in both rural and urban areas. However, unlike in Senegal, where the prevalence of overweight concurrently decreased, in Mali and Madagascar, the prevalence of overweight remained constant or increased in the later time period, particularly in urban areas. Other studies reported that recessions (both national and global) may result in increases in underweight and decreases in overweight, particularly in low-income countries (38, 39). The results presented here should inform population monitoring and intervention targeting strategies in Sub-Saharan Africa aimed at food security in the face of food crises. Furthermore, future research should involve positive deviance analyses to understand why some countries are more resilient to food crises than others.
Zambia (1992–2001 vs. 2001–2007), Zimbabwe (1994–2005 vs. 2005–2010), and Niger (1992–1998 vs. 1998–2006) managed to turn around an increasing prevalence of underweight, and most recently are decreasing their prevalence of underweight. This is an especially important observation for Niger, because although the prevalence of underweight is decreasing, it remains quite high at 17.32% in rural areas. Continued monitoring of these countries—particularly Niger, for which more recent data are not available—and evaluation of potential policies that may have protected these countries from rising food prices is needed (40).
The prevalence of overweight in Mexico was previously increasing dramatically: nearly 2% annually between 1988 and 2006 in both rural and urban areas. However, more recently (2006–2012), the prevalence of overweight has been decreasing slightly in nonpregnant adult women. This result is consistent with a recent review of overweight in Mexico that reported a drop in the rate of increase in overweight among Mexican women aged 20–49 y (20). This decrease could be the result of national initiatives beginning in 2006 with the design of a national obesity prevention policy, and including the development of national recommendations on beverage intake in 2008, the signing of the National Agreement for Health and Nutrition in 2010, and initiatives to ban sodas and regulate unhealthy foods in schools. A similar slowing of the rate of increase in overweight was observed in Benin, where the prevalence of overweight was increasing by 3.40% annually between 1996–2001, but was unchanged between 2001–2006, a period before the global recession during which Benin's growth in real output averaged 4% (41). This result is surprising given recent documentation of the nutrition transition in urban areas of Benin (42–44) and warrants further investigation.
There are several challenges of this analysis worth noting. Rural and urban residence was defined by each country; thus, definitions vary between countries (45). Furthermore, although dichotomization of this variable improves interpretability of the results, we recognize that urbanicity is a continuum. Researchers comparing the DHS rural-urban classification scheme to the Global Rural-Urban Mapping Project, which is based on satellite imagery of nighttime lights, showed that some areas classified as “rural” in the DHSs may in fact be periurban when using household electrification as a marker of urbanicity (46). Updated, uniform definitions of rural-urban residence in the DHSs and other large demographic surveys are warranted (47). Nonetheless, use of country-specific classifications of rural-urban residence renders results more readily translatable into targeted national policies to prevent under- and overweight.
Additional challenges of this analysis include the fact that 3 countries (Cambodia, Ethiopia, and Rwanda) did not have data available in the 1990s. Their earliest surveys with available data were conducted in 2000 and, therefore, the trends in under- and overweight prevalence in these countries are slightly more recent than those reported for other countries. Furthermore, we calculated annualized rates of change, which should not be interpreted as actual rates of increase or decrease in the prevalence of under- or overweight over time, because these changes might have occurred in a nonlinear fashion. Finally, the DHSs only collect data on women in the household. As data become available, sex differences will be an important area to explore. Meanwhile, the results presented here are of particular importance because women of childbearing age are a critical point of intervention, with prepregnancy BMI being a strong predictor of child health outcomes (13, 15, 48).
To our knowledge, this is the first study to document changes in the trends of under- and overweight prevalence in nationally representative surveys of nonpregnant adult women from 33 LMIC. Results suggest that select countries in Sub-Saharan Africa may be more susceptible to food crises, and should be points of policy intervention to avoid future adverse outcomes. At the same time, global health efforts must focus on preventing overweight, particularly in rural areas, which are quickly catching up to their urban counterparts.
Supplementary Material
Acknowledgments
We thank Dr. Phil Bardsley and Ms. Amanda Lyerley for programming and statistical analysis support and Mr. Tom Swasey for graphics support. MMS and BMP conceived the project; LMJ wrote the original manuscript, had primary responsibility for the final content, developed the overall research plan, and was responsible for study oversight. All authors were involved in research design, contributed substantially to manuscript revisions, and read and approved the final version of the paper.
Abbreviations
- DHS
Demographic and Health Survey
- GDPPC
gross domestic product per capita
- LMIC
low- and middle-income countries
References
- 1. Jaacks LM, Gordon-Larsen P, Mayer-Davis EJ, Adair LS, Popkin B. Longitudinal trends in adult BMI and overweight from 1991 to 2009 in China: the China Health and Nutrition Survey. Int J Epidemiol 2013;42:828–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Martorell R, Khan LK, Hughes ML, Grummer-Strawn LM. Obesity in women from developing countries. Eur J Clin Nutr 2000;54:247–52. [DOI] [PubMed] [Google Scholar]
- 3. Mendez MA, Monteiro CA, Popkin BM. Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr 2005;81:714–21. [DOI] [PubMed] [Google Scholar]
- 4. Neuman M, Kawachi I, Gortmaker S, Subramanian SV. Urban-rural differences in BMI in low- and middle-income countries: the role of socioeconomic status. Am J Clin Nutr 2013;97:428–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nandi A, Sweet E, Kawachi I, Heymann J, Galea S. Associations between macrolevel economic factors and weight distributions in low- and middle-income countries: a multilevel analysis of 200,000 adults in 40 countries. Am J Public Health 2014;104:e162–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Popkin BM. Technology, transport, globalization and the nutrition transition food policy. Food Policy 2006;31:554–69. [Google Scholar]
- 7. Keding GB, Msuya JM, Maass BL, Krawinkel MB. Dietary patterns and nutritional health of women: the nutrition transition in rural Tanzania. Food Nutr Bull 2011;32:218–26. [DOI] [PubMed] [Google Scholar]
- 8. Lipoeto NI, Geok Lin K, Angeles-Agdeppa I. Food consumption patterns and nutrition transition in South-East Asia. Public Health Nutr 2013;16:1637–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale. Soc Sci Med 2010;71:1436–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Haddad L, Ruel MT, Garrett JL. Are urban poverty and undernutrition growing? Some newly assembled evidence. World Dev 1999;27:1891–904. [Google Scholar]
- 11. Harpham T. Urban health in developing countries: what do we know and where do we go? Health Place 2009;15:107–16. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization Centre for Health Development and United Nations Human Settlements ProgrammeHidden cities: unmasking and overcoming health inequities in urban settings. Geneva: World Health Organization Centre for Health Development; 2010. [Google Scholar]
- 13. Papachatzi E, Dimitriou G, Dimitropoulos K, Vantarakis A. Pre-pregnancy obesity: maternal, neonatal and childhood outcomes. J Neonatal Perinatal Med 2013;6:203–16. [DOI] [PubMed] [Google Scholar]
- 14. Han Z, Mulla S, Beyene J, Liao G, McDonald SD. Maternal underweight and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. Int J Epidemiol 2011;40:65–101. [DOI] [PubMed] [Google Scholar]
- 15. Yu Z, Han S, Zhu J, Sun X, Ji C, Guo X. Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS ONE 2013;8:e61627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Block SR, Watkins SM, Salemi JL, Rutkowski R, Tanner JP, Correia JA, Kirby RS. Maternal pre-pregnancy body mass index and risk of selected birth defects: evidence of a dose-response relationship. Paediatr Perinat Epidemiol 2013;27:521–31. [DOI] [PubMed] [Google Scholar]
- 17. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Finucane MM. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 2011;377:557–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stevens GA, Singh GM, Lu Y, Danaei G, Lin JK, Finucane MM, Bahalim AN, McIntire RK, Gutierrez HR, Cowan M, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr 2012;10:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barquera S, Campos I, Rivera JA. Mexico attempts to tackle obesity: the process, results, push backs and future challenges. Obes Rev 2013;14:69–78. [DOI] [PubMed] [Google Scholar]
- 21. Gordon-Larsen P, Wang H, Popkin BM. Overweight dynamics in Chinese children and adults. Obes Rev 2014;15:37–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Popkin BM, Slining MM. New dynamics in global obesity facing low- and middle-income countries. Obes Rev 2013;14:11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. United States Agency for International Development (USAID), Demographic and Health Surveys (DHS) Program Available Datasets [cited 2014 Feb 25]. Available from: http://www.measuredhs.com/data/available-datasets.cfm.
- 24. Corsi DJ, Neuman M, Finlay JE, Subramanian S. Demographic and Health Surveys: a profile. Int J Epidemiol 2012;41:1602–13. [DOI] [PubMed] [Google Scholar]
- 25. The Indonesia Family Life Survey (IFLS)2014 [cited 2014 Feb 25]. Available from: http://www.rand.org/labor/FLS/IFLS.html.
- 26. Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: the China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol 2010;39:1435–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Instituto Brasileiro de Geografia e Estatística (IBGE) Pesquisa de orçamentos familiares, 2008–2009: análise do consumo alimentar pessoal no Brasil. Rio de Janeiro, Brazil: Instituto Brasileiro de Geografia e Estatística; 2011. [Google Scholar]
- 28. Romero-Martínez M, Shamah-Levy T, Franco-Núñez A, Villalpando S, Cuevas-Nasu L, Gutiérrez JP, Rivera-Dommarco JA. Encuesta Nacional de Salud y Nutrición 2012: diseño y cobertura. Salud Publica Mex 2013;55:S332–40. [PubMed] [Google Scholar]
- 29. Gutiérrez J, Rivera-Dommarco J, Shamah-Levy T. Villalpando- Hernández S, Franco A, Cuevas-Nasu L, Romero-Martinez M, Hernandez-Avila M. Encuesta Nacional de Salud y Nutrición 2012: Resultados Nacionales. Cuernavaca, Mexico: Instituto Nacional de Salud Pública; 2012. [Google Scholar]
- 30. Olaiz G, Rivera J, Shamah T, Rojas R, Villalpando S, Hernández M, Sepúlveda J. Encuesta Nacional de Salud y Nutrición 2006. Cuernavaca, Mexico: Instituto Nacional de Salud Pública; 2006. [Google Scholar]
- 31. United States Agency of International Development (USAID), Demographic and Health Surveys (DHS) Program DHS Methodology: Biomarker Field Manual. Calverton (MD): United States Agency of International Development (USAID); 2012. [Google Scholar]
- 32. World Health Organization and Food and Agriculture Organization Diet, nutrition and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 33. ICF International. Demographic and health survey sampling and household listing manual. Calverton, MD: ICF International; 2012. [Google Scholar]
- 34. World Development Indicators (WDI) 2014 [cited 2014 Feb 25]. Available from: http://data.worldbank.org/indicator.
- 35. United Nations, Department of Economic and Social Affairs, Population Division World population prospects: The 2012 revision, DVD edition. 2013 [cited 2014 Nov 3]. Available from: http://esa.un.org/wpp/Excel-Data/EXCEL_FILES/1_Population/WPP2012_POP_F07_1_POPULATION_BY_AGE_BOTH_SEXES.XLS.
- 36. Popkin BM. Nutrition, agriculture and the global food system in low and middle income countries. Food Policy 2014;47:91–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Food and Agriculture Organization of the United Nations Crop prospects and food situation. Rome, Italy: Food and Agriculture Organization of the United Nations; 2008. [Google Scholar]
- 38. Goryakin Y, Suhrcke M. Economic development, urbanization, technological change and overweight: what do we learn from 244 Demographic and Health Surveys? Econ Hum Biol 2014;14:109–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. United Nations Standing Committee on Nutrition Global recession increases malnutrition for the most vulnerable people in developing countries. New York: United Nations; 2009. [Google Scholar]
- 40. Demeke M, Pangrazio G, Maetz M. Country responses to the food security crisis: Nature and preliminary implications of the policies pursued. Rome, Italy: Food and Agriculture Organization of the United Nations; 2008. [Google Scholar]
- 41. The World Factbook Benin. 2014 [cited 2014 Apr 25]. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/bn.html.
- 42. Delisle H, Ntandou-Bouzitou G, Agueh V, Sodjinou R, Fayomi B. Urbanisation, nutrition transition and cardiometabolic risk: the Benin study. Br J Nutr 2012;107:1534–44. [DOI] [PubMed] [Google Scholar]
- 43. Sodjinou R, Agueh V, Fayomi B, Delisle H. Obesity and cardio-metabolic risk factors in urban adults of Benin: relationship with socio-economic status, urbanisation, and lifestyle patterns. BMC Public Health 2008;8:84,2458–8-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ntandou G, Delisle H, Agueh V, Fayomi B. Abdominal obesity explains the positive rural-urban gradient in the prevalence of the metabolic syndrome in Benin, West Africa. Nutr Res 2009;29:180–9. [DOI] [PubMed] [Google Scholar]
- 45. United Nations Population Division World urbanization prospects: the 2011 revision. New York: United Nations; 2012. [Google Scholar]
- 46. Dorélien A, Balk D, Todd M. What Is urban? Comparing a satellite view with the Demographic and Health Surveys. Popul Dev Rev 2013;39:413–39. [Google Scholar]
- 47. Hugo G, Champion A, Lattes A. Toward a new conceptualization of settlements for demography. Popul Dev Rev 2003;29:277–97. [Google Scholar]
- 48. Thompson LA, Zhang S, Black E, Das R, Ryngaert M, Sullivan S, Roth J. The association of maternal pre-pregnancy body mass index with breastfeeding initiation. Matern Child Health J 2013;17:1842–51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.