Abstract
The current family mealtime literature shows that assessments of the mealtime environment are typically self-report, yet few studies discuss validation techniques or report using validated scales. As such, the current analysis was conducted to validate one of the only published measures to assess the mealtime environment from the adolescent perspective. Specifically, the Childhood Family Mealtime Questionnaire (CFMQ) was evaluated in a sample of 280 overweight and obese Hispanic adolescents to address the need for a validated measure of the family mealtime environment in a demographic that is disproportionately affected by the current obesity epidemic. Results of an exploratory and confirmatory factor analysis to evaluate the optimal factor structure, reliability, and validity for a revised, abbreviated CFMQ are presented here. The concurrent validity of the CFMQ was evaluated using correlations between the factor structures and the previously used, culturally appropriate comparable measure of family functioning. Correlations were also computed between factor scores and obesogenic outcomes (fruit and vegetable intake, added sugar intake, and physical activity). Analyses produced a revised, abbreviated version that includes 22 items (reduced from a total of 69 items) and consists of the following 4 factors: family mealtime communication (5 items), family mealtime stress (7 items), appearance weight control (5 items), and mealtime structure (6 items). Cronbach’s alphas are reported for reliability. When examining CFMQ concurrent validity with the family functioning latent variable, results showed the family mealtime communication subscale ranked highest. Additionally, the family mealtime communication subscale was associated with all three obesogenic outcomes. This abbreviated CFMQ may be a useful tool for those studying family mealtime environments and their influence on obesity and its associated lifestyle behaviors.
INTRODUCTION
Recent national prevalence estimates show that dietary intake and physical activity behaviors among the United States (US) adolescent population are not conducive to healthy weight development and are likely to promote adiposity (Kann et al., 2016). As such, pediatric obesity rates remain unacceptably high, particularly among Hispanic children and adolescents whose prevalence rates are higher than non-Hispanic whites and Asians, (38.2% compared to 19.1%, 12.1%, respectively) and about the same as non-Hispanic black adolescents (35.0%) (Skinner, Ravanbakht, Skelton, Perrin, & Armstrong, 2018). This disproportion among ethnic minority youth indicates the need for culturally competent strategies to target healthful eating and physical activity practices.
Studies have highlighted the important influence that parents and the family home environment have on youth dietary choices and other health-related behaviors (Burns, Parker, & Birch, 2011; Larsen et al., 2015; Lloyd, Lubans, Plotnikoff, Collins, & Morgan, 2014; Niemeier, Hektner, & Enger, 2012; Vaughn et al., 2015; Yee, Lwin, & Ho, 2017). The family meal has been shown to be influential in the consumption of a healthy diet and may be an important avenue for obesity treatment and prevention. Meta-analysis of 17 studies (15 reported cross-sectional findings and 5 reported longitudinal findings) with children and adolescents ages 2.8 to 17.3 years (N=182,836) found that youth from families who shared meals together three or more times per week were 12% less likely to be overweight, 20% less likely to consume unhealthy foods, and 24% more likely to consume healthy foods (Hammons & Fiese, 2011). No study to our knowledge has been conducted to examine how family mealtime is associated with physical activity. Yet studies have demonstrated the impact family functioning has on adolescent physical activity (Berge, Wall, Larson, Loth, & Neumark-Sztainer, 2013; Lebron et al., 2018). For example, in one study discrepancies between parent and adolescent report of family functioning resulted in less reported adolescent physical activity (Lebron et al., 2018). If family functioning constructs like communication and positive parenting influence are given the opportunity to play out during mealtime, it follows that mealtime behaviors would also have an impact on physical activity. Few studies have examined the relationship between mealtime frequency and obesity in diverse racial/ethnic groups. While some have reported that the association was not significant for Hispanic children (Rollins, Belue, & Francis, 2010) and adolescents (Fulkerson, Neumark/ Sztainer, Hannan, & Story, 2008; Sen, 2006), others have found that family meal frequency and family support of healthful eating was associated with outcomes like consuming more fiber and fruits and vegetables in both Hispanic children and adolescents (Andaya, Arredondo, Alcaraz, Lindsay, & Elder, 2011; Ayala et al., 2007). Inconsistent results have been attributed to differences in gender, level of education, and types of foods and portions consumed at family meals.
Although the literature supports family meal frequency as a protective factor for several adverse adolescent health outcomes, much less is known about how the family mealtime environment directly or indirectly contributes to weight status, and especially among Hispanic families. Parents who encourage shared meals may have better relationships with their adolescents (Goldfarb, Tarver, Locher, Preskitt, & Sen, 2015). Similarly, older adolescents may be given the choice by their parents to eat dinner together, and those that choose to may place different meaning or value on shared mealtime than those who chose to opt out (Goldfarb et al., 2015). One study conducted with children ages 5–12 years showed that families of healthy weight children considered mealtime important and meaningful for gathering and conversing (Fiese, Hammons, & Grigsby-Toussaint, 2012). The benefits of sharing family meals may be diminished, however, if the family consumes fast food, sits around the television, or if it creates an argumentative, stressful environment (Martin-Biggers et al., 2014). Therefore, questions have been raised about the protective nature of mealtimes and specifically if findings are due to the frequency of family meals or if there are other systematic differences between families who eat together and those who do not (D. Neumark-Sztainer, Larson, Fulkerson, Eisenberg, & Story, 2010).
To arrive at the meaning of the questions, validated measures are needed to evaluate multiple domains of adolescent mealtime experiences. Previous empirical studies of the familial mealtime atmosphere have typically collected data via parent-report of their children’s behaviors (Anderson, Must, Curtin, & Bandini, 2012; Burnier, Dubois, & Girard, 2011; McCurdy & Gorman, 2010), parent report of their own behavior (Hendy, Williams, Camise, Eckman, & Hedemann, 2009), or observation (Fiese et al., 2012). Other instruments have focused on family or child eating habits or behaviors (Boquin, Smith-Simpson, Donovan, & Lee, 2014; Golan & Weizman, 1998). For example, one widely validated scale is the Behavioral Pediatric Feeding Assessment Scale, which includes items like “Gets up from table during meal”, “Comes readily to mealtime”, and “Tantrums at mealtimes” (Crist & Napier-Phillips, 2001; Davis, Canter, Stough, Gillette, & Patton, 2013; Patton, Dolan, & Powers, 2006). The body of literature around family mealtimes and its impact on adolescents has been greatly influenced by Project EAT which has shown how family mealtime frequencies, food choices, and activities affect adolescent health outcomes (Arcan et al., 2007; D. Neumark-Sztainer, Eisenberg, Fulkerson, Story, & Larson, 2008; D. Neumark-Sztainer et al., 2010; D. Neumark-Sztainer, Wall, Perry, & Story, 2003; D. Neumark-Sztainer, Wall, Story, & Standish, 2012; Neumark/Sztainer, Wall, Story, & Sherwood, 2009; Watts, Berge, Loth, Larson, & Neumark-Sztainer, 2018). However, one of the foremost limitations of all of the studies discussed is the limited evidence of discussion of development and psychometrics (Martin-Biggers et al., 2014).
The current analysis was conducted to validate one of the only published measures to assess the mealtime environment from the adolescent perspective, the Childhood Family Mealtime Questionnaire (CFMQ) (Miller, McCluskey-Fawcett, & Irving, 1993). The CFMQ is a 69-item scale developed to assess childhood mealtime experiences and was inspired by the literature correlating various eating problems and disorders with early food experiences (Bruch, 1969; Frank, 1991; Marcus & Wiener, 1989; Miller et al., 1993). In a validation study of the CFMQ, Miller et al. (1993) reported that a 35-item subset of the questions could successfully predict respondent as being bulimic, repeat dieters, or non-bulimic. In one study, the CMFQ subscales were used to investigate the disturbed eating behaviors and related-psychographic characteristics of young adults (ages 18 to 26 years). Findings demonstrated that participants with diet-related chronic health conditions recalled more emphasis on mother’s weight and less mealtime structure (V. M. Quick, McWilliams, & Byrd-Bredbenner, 2012). This study seeks to extend the use of the CFMQ to include mealtime experiences in the context of overweight/obesity. Childhood overweight has been associated with an increased risk of disordered eating symptoms including body dissatisfaction, dieting, and other unhealthy weight control, and binge eating (Haines & Neumark-Sztainer, 2006; D. R. Neumark-Sztainer et al., 2007). The shared symptomology of overweight and disordered eating suggests that each condition may perpetuate the other (Goldschmidt, Aspen, Sinton, Tanofsky-Kraff, & Wilfley, 2008), and therefore, deem the CFMQ appropriate for use in overweight/obesity.
This study has three aims conducted sequentially. Aim 1 was to identify the optimal factor structure of the CFMQ scales as applied to a sample of Hispanic overweight/obese youth (mean age= 13.01) using an exploratory factor analysis (EFA) with items from the CFMQ. Aim 2 was to use confirmatory factor analysis (CFA) to evaluate the construct validity and reliability of the CFMQ factor structure results in Aim 1. Aim 3 was to evaluate the subscales produced and confirmed in Aims 1 and 2 by testing concurrent validity with a family functioning subscale and by analyzing the associations between the subscales and three obesogenic outcomes (fruit and vegetable intake, added sugar intake, and physical activity).
METHODS
Data for this analysis were derived from the baseline assessment of Familias Unidas for Health and Wellness, an ongoing randomized clinical trial evaluating the relative efficacy of a family-based intervention on obesity-related lifestyle behaviors among overweight and obese Hispanic adolescents (St. George, 2018). Study staff recruited participants from 18 middle schools in Miami-Dade County distributing letters with the study description to 7th and 8th graders. If parents were interested, they were instructed to provide their contact information. Students who returned a signed letter were visually screened by study staff who identified those who might have a BMI ≥ 85th percentile for their age and sex based on body silhouette images (Stunkard, Sorensen, & Schlusinger, 2006). This procedure was used to reduce the stigma associated with obesity (i.e., letters did not mention the BMI criterion and described the intervention broadly as one designed to “promote healthy choices and prevent risky behaviors in Hispanic youth”). To be eligible for this study families had to have a Hispanic adolescent who (1) was in the 7th or 8th grade, (2) had a BMI ≥ 85th percentile for their age and sex, (3) lived with an adult primary caregiver willing to participate in the two-year study, (4) have plans to remain a resident of South Florida during the two-year study period. If parent responses on a physical activity readiness questionnaire indicated a serious health issue (e.g., chest pain) for parents and/or adolescents, they were required to acquire physician approval to participate. Details of the intervention are described elsewhere (St George et al., 2018). This study was approved by both the University of Miami and Miami Dade County Public School System (MDCPS-S) Institutional Review Board.
Measures
Family functioning was used to evaluate concurrent validity because interaction patterns during a routine mealtime are thought to be consistent with healthy family functioning (Dickstein, 2002; Fiese, Foley, & Spagnola, 2006). Furthermore, positive family functioning has been associated with lower body mass index z score, more frequent family meals, and less sedentary behavior in adolescents (Berge et al., 2013). Adolescent self-report of measures were used as adolescent and parent reports on variables such as family functioning have been found to be incongruent (Ohannessian, Lerner, Lerner, & von Eye, 1995; Schwartz, Mason, Pantin, & Szapocznik, 2008; Stuart & Jose, 2012) and impactful in the relationship of obesogenic behaviors (Lebron et al., 2018). All measures were translated and back-translated and were offered to participants in English or Spanish.
Childhood Family Mealtime Questionnaire (CFMQ)
Although originally the CFMQ had 69-items, Miller et al (1993) conducted a factor analysis conducted on all items resulted in a subset of 35-items forming seven different factors. Those seven factors, in turn, were categorized as subscales of the CFMQ and labeled: 1) Mealtime Communication Based Stress, 2) Mealtime Structure, and 3) Appearance Weight Control, 4) Parental Mealtime Control, 5) Emphasis on Mother’s Weight, 6) Present Parental Meal Influence, 7) and Traditional Family (Miller et al., 1993). Other studies have used the original subscales of the CFMQ to analyze how family mealtimes influence disturbed eating patterns and eating attitudes in general (Meno, Hannum, Espelage, & Low, 2008; V Quick & Byrd/Bredbenner, 2013; V. M. Quick et al., 2012; Worobey, 2002a, 2002b). The original CFMQ has inter-item reliability of 0.91, with items scored on a scale ranging from 1 = “never” to 5 = “always” (Miller et al., 1993).
To examine factor structures of CFMQ in Hispanic youth population, the current study used the reduced scales (35 items)(Miller et al., 1993). Examples of each scale include: Mealtime Communication Based Stress (11 items) “In my family, everyone could speak their views at dinner time; ” Mealtime Structure (7 items) “During meals, I was told not to waste food; ” Appearance Weight Control (6 items) “I remember worrying about my weight when I was young;” Parental Mealtime Control (3 items) “We ate foods my father liked;” Emphasis on Mother’s Weight (3 items) “My mother dieted when I was young; ” Present Parental Meal Influences (2 items) “Presently, when I am at home, my parents influence what I eat; ” and Traditional Family (3 items) “I saw one of my mother’s main roles as that of a cook.”
Family Functioning
Family functioning was assessed using adolescent and parent reports of five indicators, including positive parenting, parental involvement, family communication, parental monitoring of peers, and parent-adolescent communication. Subscales from the Parenting Practices Scale (Gorman-Smith, Tolan, Zelli, & Huesmann, 1996) were used to assess positive parenting (9 items; adolescent report α = .79, parent report α =.68) and parental involvement (16 items; adolescent report α = .84, parent report α = .73). Alpha coefficients were previously reported as ranging from .68 to .81 (Gorman-Smith et al., 1996). The positive parenting subscale measures parent behaviors characterized by rewarding and acknowledging adolescent positive behaviors. Sample items for the adolescent and parent, respectively include “When you have done something that your parents like or approve of, how often does your mother say something nice about it.?”, and “ When your child has done something that you like or approve of, do you say something nice about it; praise or give approval.” The response options ranged from “0 = never” to “4 = always.” The parental involvement subscale included adolescent questions such as “How often do you and your mom do things together at home?”, and for the parent, “Do you and your child do things together at home?”, with a response range of “0 = never to “4 = always.” The Parent Relationship with Peer Group Scale (Pantin, 1996) was used to assess parental monitoring of peers (5 items; adolescent report α = .84, parent report α = .80); this measure asks parents to indicate the extent to which they supervise adolescents’ friends, activities, and whereabouts. A five-point Likert-type scale, ranging from “1 = not at all” to “5 = extremely well (often),” was used to record responses. Sample adolescent items included “How well do you personally know your child’s best friends?”, and for parents, “How well do your parents know your best friends?” Parent-adolescent communication (20 items; adolescent report α = .86, parent report α = .84) was assessed using the two subscales, open communication, and problems in family communication, of Parent-Adolescent Communication Scale (Barnes & Olson, 1985). Alpha reliabilities were previously reported for each subscale as .87 and .78 (Barnes & Olson, 1985). A sample adolescent question included “When I ask questions, I get honest answers from my mother/father” and for parents, “When I ask questions I get honest answers from my child.” Response choices ranged from “1 = strongly disagree” to “5 = strongly agree.”
Dietary Intake and Physical Activity
Dietary intake (i.e., fruit and vegetable intake, added sugar intake) was assessed using the Dietary Screener Questionnaire of the National Health and Nutrition Examination Survey (NHANES, 2008). The questionnaire asks participants how much of 22 specific foods or beverages they have had in the past month. There are eight responses choices: Never, 1 time last month, 2–3 times last month, 1 time per week, 2 times per week, 3–4 times per week, 5–6 times per week, 1 time per day, 2 or more times per day. The fruit and vegetable dietary factor consists of the following food items: fruit, fruit juice, salad, fried potatoes, other potatoes, dried beans, other vegetables, tomato sauce, salsa, and pizza. The added sugars dietary factor consists of the following food items: soda, fruit drinks, cookies, cake and pie, doughnuts, ice cream, sugar/honey in coffee/tea, candy, and cereal and cereal type. For the current analyses, we used algorithms developed by the National Cancer Institute (NCI) for use with the DSQ (available at https://epi.grants.cancer.gov/nhanes/dietscreen/scoring/current/#scoring) to calculate daily fruit and vegetable consumption (unit: a cup; Mean [SD] = 3.38 [2.53]; skewness = 1.67) and daily added sugar consumption (unit: tsp; Mean [SD] = 17.80 [17.00]; skewness = 2.78). Following George and Mallery (2010), daily sugar intake was positively skewed and was log-transformed for analyses. Development and evaluation of the DSQ have been described elsewhere (Thompson, Midthune, Kahle, & Dodd, 2017).
Physical activity was assessed by asking adolescents “During the past 7 days, on how many days were you physically active for a total of at least 60 minutes per day? Add up all the time you spend in any kind of physical activity that increases your heart rate and make you breathe hard some of the time” as is asked in the NHANES Physical Activity and Physical Fitness Questionnaire (NHANES, 2012).
Statistical Analysis
The analyses were conducted in three sequential steps. First, to identify the optimal factor structure of CFMQ scales, an exploratory factor analysis (EFA) with 35 CFMQ items was conducted using a principle component analysis (PCA) with geomin rotation (Sass & Schmitt, 2010). Principal Components’ Analysis (PCA) has been widely used as a multivariate technique for data reduction and identifying latent factor structures (Westfall, Arias, & Fulton, 2017).
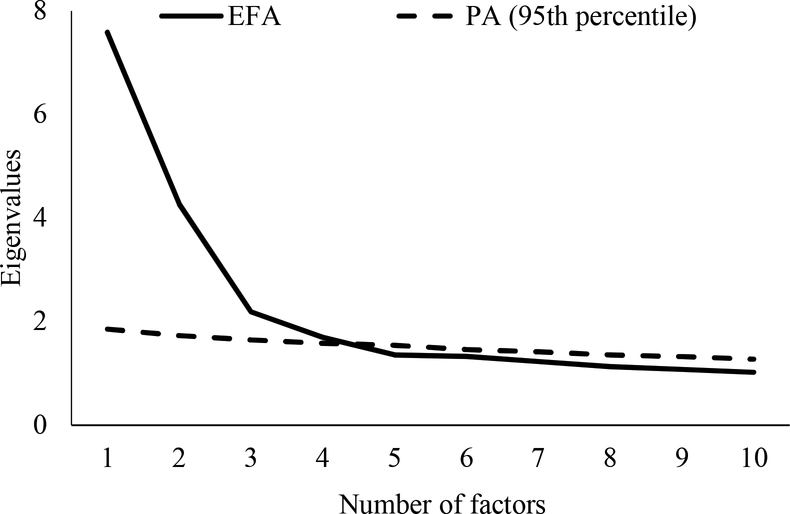
To determine the number of factors, a scree plot was used to show eigenvalues across all extracted factors. Though the criterion suggests retaining all factors that are above the eigenvalue of 1 (Yong & Pearce, 2013), this could potentially overestimate the number of true factors (Franklin, Gibson, Robertson, Pohlmann, & Fralish, 1995). To eliminate any overestimated factors, the current study used the scree plot criterion from both EFA and parallel analysis (PA). Parallel analysis is a method for creating eigenvalues from random data sets that have the same sample size and number of variables as the actual data set (Fabrigar, Wegener, MacCallum, & Strahan, 1999). Factors are retained when the eigenvalues estimated from a principal component analysis set exceeds the 95th percentile of the random data eigenvalue estimated from parallel analysis (O’Connor, 2000) because it suggests that the amount of variance explained by these factors is greater than that by chance (Lahey et al., 2004). In other words, if factor eigenvalues were lower in EFA compared to those in PA, those factors were considered unreliable and thus excluded from subsequent analyses. We derived eigenvalues from random data sets by running 100 simulations.
We investigated the communality of each item, reflecting the variance of an item in common with all other items together (Yong & Pearce, 2013). Previous studies suggest that items that obtain low commonality (< .30) have less contribution to the explanation of the variances of extracted factors (Yong & Pearce, 2013). When communality values are close to zero, the associated items are more likely to be outliers and thus distract from the model. Communality values between .30 and 1.0 indicate that these variables should be retained, as much of their common variance can be explained by the extracted factors (Pett et al., 2003). Consistent with other reports, the current study excluded items that obtained low commonality (< .30) from subsequent analyses (Morales, Yubero, & Larranaga, 2016). For the EFA model evaluation, two fit indices were used: the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (> .80 is an acceptable fit; (Kaiser, 1970)) and Bartlett’s test of sphericity (significant p-value indicates the EFA fits to the data).
Next, we evaluated construct validity and reliability of the optimal factor structure that was estimated in step 1. Construct validity was evaluated by using confirmatory factor analysis (CFA) with a structural equation modeling (SEM) approach (Brown, 2006). Construct validity was tested by investigating correlations between items and corresponding factors and among extracted factors (Brown, 2006). Standardized coefficients were used as effect sizes. In addition, the scale reliabilities of factors in CFMQ were evaluated by using internal reliability (i.e., Cronbach’s alphas were tested here). Concurrent validity was analyzed by measuring the correlations of family functioning with the final factors.
Finally, we evaluated the correlations between the factor structures and health behavior outcomes (self-reported fruit and vegetable intake, added sugar intake, and levels of physical activity). To estimate unique effects, the current study specified four demographic variables as controls: family annual income (continuous), marital status (married vs. non-married), parental education (continuous), and years in the US (more than 10 years vs. less than 10 years). Standardized path coefficients that assess the direct effect can be used as correlation coefficients (r) in structural equation modeling. Indirect effects can be also be calculated with standardized estimates corresponding to effect-size estimates (Kline, 2011). As such, effect sizes were interpreted based on small (r = .10), medium (r = .30), and large effects (r = .50)(Cohen, 1988).
For the model evaluation, we used several fit indices including the comparative fit index (CFI; acceptable fit >.90; Little, 2013) and the root mean square error of approximation (RMSEA; acceptable fit < .08; Little, 2013). We used the same sample (n = 280) to use EFA and CFA. The average missing percent for all 35 items in CFMQ was 3.2% out of total sample size (n=280). Using Little’s (1988) missing completely at random (MCAR) test, missing data patterns were analyzed to see whether any significant missing case patterns across 35 items of CFMQ. Chi-square tests showed no statistically reliable missing patterns for 35 items (χ2[df] = 1432.563 [1550], p = .984). To handle missing cases, we used a full-information maximum likelihood (FIML) estimator with robust standard errors (Enders & Bandalos, 2001), implemented as MLR in Mplus (version 8.00; (Muthen & Muthen, 1987–2017). The final analytic sample was 280.
RESULTS
Participants
The study sample consisted of 280 Hispanic overweight (≥ 85th percentile for age and sex) and obese (> 95th percentile for age and sex; (Barlow & Dietz, 1998)) 7th and 8th-grade youth and their primary caregivers recruited from middle schools in the MDCPS-S (Table 1). Forty-eight percent of the adolescents were male and 52% were female, and the mean age was 13.01 (range: 11–15; SD=0.83). Adolescents were mostly born in the U.S. (64%), Cuba (19.3%), Honduras (4.3%), and Venezuela (3.6%). The majority of adolescents not being born in the U.S. (66.1%) reported living in the USA for more than 10 years (n=185). Table 1 includes demographic data on parents as well as adolescents.
Table 1.
Sociodemographic Characteristics of Parent & Adolescent Participants
| Variable | Mean (SD) or % |
|---|---|
| Adolescent | |
| Female | 52% |
| Age | 13.01 (11–15; 0.83) |
| Country of Origin | |
| United States | 64.29% |
| Cuba | 19.29% |
| Honduras | 4.29% |
| Venezuela | 3.47% |
| BMI | 28.06 (6.07) |
| Obesity (> 30 BMI) | 23.92% |
| Percentile* | 94.63 (4.08) |
| Parent | |
| Female | 88.21% |
| Age | 41.88 (25–59; 6.0) |
| Country of Origin | |
| United States | 8.93% |
| Cuba | 34.29% |
| Nicaragua | 15.00% |
| Honduras | 11.43% |
| Marital Status | |
| Married | 57.86% |
| Divorced | 12.9% |
| Living with someone | 10.00% |
| Separated | 10.00% |
| Never married, not living with someone | 8.47% |
| Widowed | 0.71% |
| Full- time employment | 50.71% |
| Annual Income | |
| Less than $30,000 | 65.41% |
| Greater than $30,000 | 20.68% |
| Greater than $50,000 | 13.91% |
| BMI | |
| Obesity (> 30 BMI) | 47.14% |
adjusted for age and sex
CFMQ Factor Structure
To examine the factor structure of CFMQ in our study sample, an exploratory factor analysis (EFA) was conducted with the reduced scale (35 items). The value of the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy was .82. In addition, Bartlett’s test of sphericity yielded statistically significant results, χ2 (595) = 3224.85, p < .001. Taken together, these results indicate that the fit of the data to the factor model was acceptable. Next, to select the optimal factor structure, we conducted an exploratory factor analysis (EFA) with the 35 items of CFMQ. In Figure 1, the scree plot indicates that the eigenvalues for the first four factors of the exploratory factor analysis were larger than the corresponding parallel analysis (eigenvalues of EFA = 7.58, 4.27., 2.19., and 1.69.; eigenvalues of EFA = 1.86, 1.72., 1.64., and 1.58.), suggesting that the four extracted factors were reliable. However, within the four-factor structure, we found that 13 items contained low communality (< .30) (see corresponding items in Table 3). Therefore, after removing the 13 items that contained low communality, an additional EFA was conducted. The scree plot also suggests the same four factor model by showing the eigenvalues for the first four factors of the exploratory factor analysis were larger than the corresponding parallel analysis (eigenvalues of EFA = 5.34, 3.72, 1.73, and 1.54, respectively; eigenvalues of EFA = 1.55, 1.45, 1.38, and 1.32, respectively). Therefore, a four-factor structure reduced to 22 CFMQ items was selected as the optimal factor structure and was used for subsequent analyses.
Figure 1. Scree plot of CFMQ exploratory factor analysis.
Note. CFMQ = Childhood Family Mealtime Questionnaire. EFA = Exploratory Factor Analysis. PA = Parallel Analysis.
Table 3.
Structure coefficients, means, and standard deviations of reduced CFMQ 23 items in the extracted four factor model in a sample of 280 overweight/obese Hispanic adolescents,
| Structural coefficients | ||||||
|---|---|---|---|---|---|---|
| Reduced 23 items | F1 | F2 | F3 | F4 | h2 | M (SD) |
| I felt mealtimes were a warm and sharing time in my family. | .59 | .37 | 3.86 (1.18) | |||
| My family talked during dinner. | .54 | .31 | 3.91 (1.17) | |||
| I liked to eat dinner with my family. | .71 | .52 | 4.21 (1.06) | |||
| In my family, everyone could speak their views at dinner time. | .86 | .75 | 3.89 (1.26) | |||
| I remember feeling nervous during dinner. | .74 | .56 | 1.71 (1.10) | |||
| Dinner times were silent in my family. | .59 | .41 | 2.06 (1.20) | |||
| I felt able to speak my mind during mealtimes. | .70 | .50 | 3.50 (1.25) | |||
| Because of stress during meals, I liked or wished to eat alone. | .57 | .37 | 2.32 (1.37) | |||
| There was yelling during dinner. | .77 | .63 | 1.72 (1.07) | |||
| It was a relief when my father was not at dinner. | .58 | .35 | 1.70 (1.17) | |||
| During meals, I was told not to waste food. | .53 | .31 | 3.61 (1.26) | |||
| If I did not like what we were having for dinner, I had to eat it anyway. | .45 | .35 | 2.67 (1.29) | |||
| Table manners were important to my parents. | .71 | .56 | 3.89 (1.24) | |||
| Table manners were brought up at dinner. | .55 | .33 | 2.94 (1.43) | |||
| I remember thinking about my weight when I was young. | .86 | .75 | 3.01 (1.36) | |||
| I remember worrying about my weight when I was young. | .87 | .77 | 3.04 (1.41) | |||
| When I was young, I was encouraged to diet. | .62 | .41 | 2.71 (1.39) | |||
| In my family, we talked about our own or each other’s weight. | .41 | .35 | 2.41 (1.29) | |||
| In my family, we thought of beauty as depending a lot on weight. | .48 | .33 | 2.40 (1.29) | |||
| My father commented about my mother’s weight when I was young. | .75 | .57 | 1.76 (1.15) | |||
| Presently, when I am at home, my parents influence what I eat. | .73 | .54 | 3.43 (1.26) | |||
| Presently, when I am at home, my parents influence the way I eat. | .56 | .36 | 3.01 (1.30) | |||
| In my family, mealtimes were set by my father’s schedule. | .45 | .30 | 2.04 (1.21) | |||
| Eigenvalues | 5.54 | 3.73 | 1.78 | 1.56 | ||
| % of explained variance | 25.15 | 16.04 | 7.82 | 6.63 | ||
| Cronbach’s alpha | .81 | .82 | .81 | .76 | ||
Note. F = Factor. h2 = Communality. M = Mean. SD = Standard Deviation. Structural coefficients are standardized. Only standardized loadings over .40 are listed.
Table 3 shows the standardized loadings of items (only those items greater than .40 are reported). The total explained variance of these four factors was 56.61% (not shown in Table 2). The first factor included five items (> standardized loading .40) referring to family mealtime communication and explained 25.03% of the variance. The second factor comprised seven items (>.40 standardized loading) and for the most part, referred to family mealtime stress and explained 16.75% of the variance. The third factor consisted of five items (>.40 standardized loading) related to appearance weight control (i.e. the importance of weight management) and explained 8.03% of the variance. Finally, the fourth factor consisted of six items (>.40 standardized loading) and mostly referred to mealtime structure and explained 6.81% of the variance.
Table 2.
Communality (h2) of full 35 items from initial EFA model
| Items | h2 |
|---|---|
| I felt mealtimes were a warm and sharing time in my family. | .40 |
| My family talked during dinner. | .31 |
| I looked forward to mealtimes. | .26 |
| I liked to eat dinner with my family. | .51 |
| In my family, everyone could speak their views at dinner time. | .72 |
| I remember feeling nervous during dinner. | .54 |
| Dinner times were silent in my family. | .36 |
| I felt able to speak my mind during mealtimes. | .50 |
| Because of stress during meals, I liked or wished to eat alone. | .36 |
| There was yelling during dinner. | .63 |
| It was a relief when my father was not at dinner. | .34 |
| My family was conscious of wasting food. | .15 |
| During meals, I was told not to waste food. | .33 |
| If I did not like what we were having for dinner, I had to eat it anyway. | .42 |
| At home, I had to clean my plate (i.e. eat all the food on it). | .21 |
| My parents made me eat foods I did not like. | .27 |
| Table manners were important to my parents. | .48 |
| Table manners were brought up at dinner. | .29 |
| I remember thinking about my weight when I was young. | .71 |
| I remember worrying about my weight when I was young. | .77 |
| When I was young, I was encouraged to diet. | .45 |
| In my family, we thought and/or talked about physical appearance. | .29 |
| In my family, we talked about our own or each other’s weight. | .32 |
| In my family, we thought of beauty as depending a lot on weight. | .37 |
| We ate foods my father liked. | .14 |
| During meals, you could tell who was in control in my family | .20 |
| When my family wanted to celebrate, food was a part of the celebration. | .14 |
| My mother worried about her weight when I was young. | .28 |
| My mother dieted when I was young. | .23 |
| My father commented about my mother’s weight when I was young. | .51 |
| Presently, when I am at home, my parents influence what I eat. | .47 |
| Presently, when I am at home, my parents influence the way I eat. | .36 |
| I saw my mother’s main role as that of a homemaker. | .23 |
| I saw one of my mother’s main roles as that of a cook. | .19 |
| In my family, mealtimes were set by my father’s schedule. | .33 |
Note. h2 = Communality, reflecting the amount of variance in each variable explained by the extracted factors. Grayed and italic items (total 6 items) were low communality items (< .30), which we excluded from subsequent analyses.
Construct Validity and Reliability of Factor Structure in CFMQ
Using a four-factor structure reduced to 22 CFMQ items, we again conducted a CFA to confirm the construct validity of the extracted four factors. The model had an acceptable fit (χ2(df) = 387.91 (186), p < .001; CFI / TLI= .91 /.90, RMSEA [90% CI] = .06 [.05, .07]). Similar to the findings from the EFA, standardized factor loadings between the reduced 22 items and their respective factors ranged from .45 to .82 (p < .001), indicating moderate-to-large correlation (r) effects. This suggested evidence of good construct validity for all four constructs in CFMQ. Among the four latent factors, most correlations have relatively small-to-medium effect sizes (ranged from −.28 between childhood mealtime communication and stress, p < .001 to .39, and between childhood mealtime communication and appearance weight control, p < .001). The correlation between appearance weight control and mealtime structures was moderate-to-high (r = .48, p < .001). In addition, we also evaluated scale reliability of each construct using Cronbach’s alphas, which have acceptable ranges (alphas ranged from .73 to .82; see alphas in Table 3).
Concurrent Validity of CFMQ
Before investigating concurrent validity of CFMQ’s four factors, we first conducted CFA to assess the construct validity of the family functioning variables (one latent variable capturing family communication, parent-adolescent communication, positive parenting, parental monitoring of peer, and parental involvement) (Lebron et al., 2018; Malcolm et al., 2013; Schwartz, Pantin, Prado, Sullivan, & Szapocznik, 2005). The model fit indices were acceptable (χ2 (df) = 15.24 (5), p=1.13; CFI / TLI =.97 / .94; RMSEA [90% CI] = .06 [.04, .08]). All standardized factor loadings ranged from .55 to .88 indicating good construct validity of the indicators.
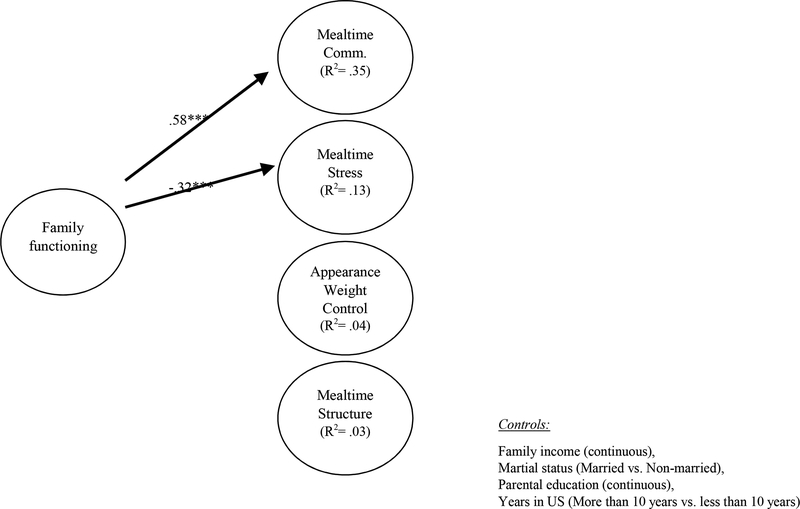
The results of concurrent validity are shown in Figure 2. The model fit indices were acceptable (CFI = .90 / RMSEA [90% CI] =.05 [.04, .06]). After adjusting for the demographic characteristics (i.e. family income, marital status, parental education, years living in the US ) , two significant associations were found. That is, results showed that family functioning was positively associated with childhood mealtime communication (β= .58, 95% CI = .47, .69, p < .001), but negatively associated with childhood mealtime stress (β= −.32, 95% CI = −.46, −.19, p < .001).
Figure 2. Concurrent validity of four factors in CFMQ.
Notes. Standardized coefficients were shown. Only significant standardized coefficients were shown in the figure.
Comm = Communication. Non-significant coefficients were not shown in figure. CFI = .90. RMSEA=.05.
**p < .01. ***p < .001.
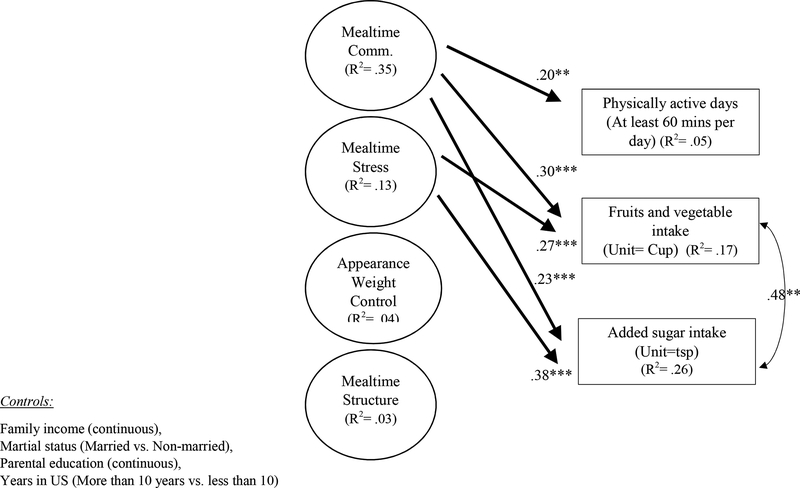
Correlations with Variables of Interest
The results of correlations between the newly identified factors and select obesogenic variables are shown in Figure 3. The model fit indices were acceptable (CFI = .90 / RMSEA [90% CI] =.05 [.04, .06]). Results show that childhood mealtime communication is positively associated with two healthy weight behaviors (physically active days: β= .20, 95% CI = .07, .32, p < .01; fruits and vegetable intake: β= .29, 95% CI = .15, .45, p < .001) but also an unhealthy weight behavior (added sugar intake: β= .23 (Lebron et al., 2018), 95% CI = .09, .37, p < .001). Interestingly, childhood mealtime stress was also positively associated with fruits and vegetable intake (β= .26, 95% CI = .08, .45, p < .01) and added sugar intake (β= .38, 95% CI = .21, .57, p < .001). There were no significant control variable effects in the estimated model. The revised version of the validated subscales are presented in the Appendix 1 & 2.
Figure 3. Predictive validity of four factors in CFMQ.
Notes. Standardized coefficients were shown. Only significant standardized coefficients were shown in the figure.
Comm = Communication. Non-significant coefficients were not shown in figure. CFI = .90. RMSEA=.05.
**p < .01. ***p < .001.
DISCUSSION
We identified the optimal factor structure of the CFMQ scales as applied to our sample of Hispanic overweight/obese youth using EFA with a subset of 35 CFMQ items and evaluated the construct validity and reliability of the CFMQ factor structure that are estimated in step 1 using CFA. Factor analyses produced a CFMQ four factor model, generating a measure with 22 items that assessed four domains within the family mealtime environment: family mealtime communication (5 items), family mealtime stress (7 items), appearance weight control (5 items), and mealtime structure (6 items). We also investigated the concurrent validity between the factor structures and the family functioning measure. Results showed that family functioning was positively associated with childhood mealtime communication, but negatively associated with childhood mealtime stress. Finally, we evaluated the correlations between the factor structures and obesogenic outcomes (self-reported fruit and vegetable intake, added sugar intake, and level of physical activity) and found that the family mealtime communication subscale was associated with all three obesogenic outcomes.
Factor Structure in CFMQ
Contrary to the 35 items (7 factors) result of the original CFMQ, our EFA and CFA produced a revised, abbreviated version that concluded with 23 items and consisted of the aforementioned four factors (family mealtime communication, family mealtime stress, appearance weight control, and mealtime structure). This version of the CFMQ does not support the inclusion of the subscales ‘Emphasis on Mother’s Weight’, ‘Present Parental Meal Influence’, and ‘Traditional Family.’ This may be attributed to the fact that the CFMQ was originally developed to assess how early mealtime experiences correlated with disturbed eating practices and was tested among bulimic women (Miller et al., 1993). However, the inclusion of 4 comparable factors highlights the similarities there are among the risk and protective factors of obesity and disordered eating, such as dieting and binge-eating, among adolescents and how family mealtime can influence weight-related conditions (Fagundo et al., 2012; Goldschmidt et al., 2008; Neumark-Sztainer et al., 2009; Thompson & Smolak, 2001). Previous studies have consistently documented disordered eating predicting further weight gain (Marcus & Wiener, 1989; Neumark-Sztainer et al., 2012; Tanofsky-Kraff et al., 2009) and a substantial portion of adolescents seeking treatment for eating disorders have a history of overweight/obesity (Lebow, Sim, & Kransdorf, 2015). In fact, researchers in the fields of obesity and eating disorders have proposed an integrated approach to the co-occurrence of these health conditions and the shared risk factors for different eating- and weight-related problems (Irving & Neumark-Sztainer, 2002; Sanchez-Carracedo, Neumark-Sztainer, & Lopez-Guimera, 2012). Furthermore, several organizations including the American Academy of Pediatricians, the American Dietetic Association, and the Society for Adolescent Health and Medicine have pointed out the potential overlap of overweight/obesity and eating disorders and have encouraged physicians to conduct early screening of eating disorders regardless of weight status (Daniels & Hassink, 2015; Golden, Katzman, Sawyer, & Ornstein, 2015; Golden, Schneider, & Wood, 2016; Ozier & Henry, 2011).
The CFMQ was not originally developed for Hispanics or to identify obesogenic behaviors, but we chose it because the items specified around the general atmosphere and attitudes were applicable to our population. This analysis is an initial step to quantify and learn about these intricate relationships especially among our target population who demonstrate very high rates of unhealthy weight compared to other racial/ethnic groups. A better understanding of how family mealtime behaviors affect Hispanic adolescents can contribute to the established literature about culture and eating (Counihan & Van Esterik, 2012). For example, Kumanyika (2008) describes various ethnic and cultural influences of childhood obesity like how cultural acceptability of overeating has been conditioned to avoid hunger. Cultural wisdom dictates that one should “feast” when food is available. Note that a recent report administered by the USDA states that 1 in 4 Latino children live in a food insecure household (Coleman-Jensen, Rabbit, Gregory, & Singh, 2017).
Concurrent Validity of CFMQ
Conducting concurrent validity analysis of the CFMQ and family functioning highlights similarities in terms of (1) family mealtime communication and (2) mealtime stress. This might be explained by the fact that family functioning is treated here as a latent variable that captures, among multi-domain family factors, family communication, and parent-adolescent communication. Furthermore, others have reported an association between positive family mealtime communication and lower stress (Offer, 2013). Interestingly, no significant associations were found between family functioning and the subscales of appearance weight control or mealtime structure.
Correlations with Variables of Interest
Increased mealtime communication was correlated with three weight-related behavioral outcomes: physical activity, fruit and vegetable intake, and added sugar intake. Similarly, Fiese et al. (2012) found that families with children of healthy weight engaged in more positive interpersonal communication at mealtime than those with overweight children. Although the association to added sugar may seem to be an anomaly, this may be explained by the cultural relationship there is between family and food in Hispanics (Kaufman & Karpati, 2007; Kumanyika, 2008; Perez-Escamilla, 2009). For example, family celebrations are often and common in the Hispanic culture and these gatherings revolve around an abundance of foods of all types. This places social pressure to participate in eating; nonattendance or food refusal is seen as rude and disrespectful (Castro, Shaibi, & Boehm-Smith, 2009; Weiler & Crist, 2009).
Interestingly, mealtime stress was also associated with fruit and vegetable intake and added sugar intake, suggesting that poor family functioning associated with higher stress during the mealtime results in higher dietary consumption of all foods regardless of their nutritional quality. Similarly, in a study among racially/ethnically diverse adolescents, 25% of the sample was using food as a coping mechanism for stress related to parents and self and romantic interests (MartynD Nemeth, Penckofer, Gulanick, Velsor-Friedrich, & Bryant, 2009). Furthermore, using food to cope was associated with higher body weight. In another study, the CFMQ was administered to college-aged women (Worobey, 2002a) and found that mealtime communication-based stress was actually highest among underweight woman compared to their overweight and normal weight counterparts. Conversely, another consideration is that better mealtime communication and lower mealtime stress may make mealtime more enjoyable for families and may be linked to higher consumption of all food types, simply given that families are eating together on a regular basis. Similarly, it has been demonstrated that eating fast food at family mealtime diminishes or negates the nutritional benefits associated with family mealtime (Martin-Biggers et al., 2014). Although these findings show a relationship between stress, family, and disordered eating, further research could determine how the specific subscales of the CFMQ can be used to predict how the family mealtime environment influences dietary outcomes over time.
Strengths and Limitations
This revised, abbreviated CFMQ was developed for researchers interested in understanding the mealtime environment in families with adolescents. However, it is important to recognize the limitations of the questionnaire. It does not include the question of mealtime frequency that has been cited in the literature (Hammons & Fiese, 2011). Additionally, it was not originally intended for obesogenic populations, but, as has been demonstrated in the literature, obesity and eating disorders share many of the same risk and protective factors (Haines & Neumark-Sztainer, 2006; D. R. Neumark-Sztainer et al., 2007). A further limitation of the questionnaire is that it is subject to social desirability bias and it is not known whether participants differed in their interpretation or understanding of the questions. The entire study sample consisted of overweight/obese adolescents which is likely to skew the measurement of obesogenic behaviors. Lastly, although concurrent validity was assessed with all four subscales, family functioning may not be the best measure to use as a comparison measure with appearance weight control or mealtime structure. However, this study has several methodological strengths. First, participants were recruited from a large range of Hispanic origins increasing the diversity and representativeness of the sample. Second, we employed rigorous exploratory and confirmatory factor analytical approaches to ascertain the inclusion of every individual item. Lastly, the validation of the CFMQ has been shown to be good, resulting in a valid measure that is suitable for use in future research.
CONCLUSION
In sum, the findings of this analysis provide a validated, abbreviated CFMQ as an adolescent measure for the report of family mealtime environment in overweight/obese Hispanics. Further use and evaluation of the questionnaire is needed, but these promising findings of reliability and validity suggest that researchers interested in understanding the adolescent perspective of the family mealtime environment, especially among Hispanics, may find this version of the CFMQ useful. Indeed, the literature focused on mealtime frequency may be overlooking these types of relationships, especially among adolescents of unhealthy weight who have adopted poor relationships with food. Our study supports a role for further research to understand individuals’ and families’ environments, beliefs, and sociocultural influences mealtime in order to foster the development of relevant interventions across diverse populations.
Appendix 1: Mealtime Communication from CFMQ (English & Spanish)
Instructions: Think back to family mealtimes during your childhood (up to the age of 13). Please select the answer to each question according to how you felt at that time.
| Mealtime Communication | |||||
|---|---|---|---|---|---|
| Never | Rarely | Sometimes | Usually | Always | |
| I felt mealtimes were a warm and sharing time in my family. | |||||
| My family talked during dinner. | |||||
| I liked to eat dinner with my family. | |||||
| In my family, everyone could speak their views at dinner time. | |||||
| I felt able to speak my mind during mealtimes. | |||||
Instrucciones: Trate de recordar sus cenas familiares (de niñez hasta los 13 años) y por favor escoge la respuesta de acuerdo a como se sintiό en esos momentos.
| Comunicación a la hora de comer | |||||
|---|---|---|---|---|---|
| Nunca | Raramente | A veces | En general | Siempre | |
| Sentía que las cenas familiares eran | |||||
| placenteras y eran un momento agradable para compartir con la familia. | |||||
| Durante la hora de la cena, mi familia conversaba. | |||||
| Me gustaba cenar con mi familia. | |||||
| A la hora de la cena, todos podiamos compartir nuestros puntos de vista. | |||||
| Durante la hora de la cena me sentia suficientemente comódo(a) de compartir mis puntos de vista. | |||||
Appendix 2: Mealtime Stress from CFMQ (English & Spanish)
Instructions: Think back to family mealtimes during your childhood (up to the age of 13). Please select the answer to each question according to how you felt at that time.
| Mealtime Stress | |||||
|---|---|---|---|---|---|
| Never | Rarely | Sometimes | Usually | Always | |
| I remember feeling nervous during dinner. | |||||
| Dinner times were silent in my family. | |||||
| Because of stress during meals, I liked or wished to eat alone. | |||||
| There was yelling during dinner. | |||||
| It was a relief when my father was not at dinner. | |||||
| My father commented about my mother’s weight when I was young. | |||||
| In my family, mealtimes were set by my father’s schedule. | |||||
Instrucciones: Trate de recordar sus cenas familiares (de niñez hasta los 13 años) y por favor escoge la respuesta de acuerdo a como se sintiό en esos momentos.
| Estrés a la hora de comer | |||||
|---|---|---|---|---|---|
| Nunca | Raramente | A veces | En general | Siempre | |
| Recuerdo sentirme nervioso(a) durante la hora de la cena | |||||
| En mi familia, la hora de la cena se pasaba en silencio. | |||||
| Prefería comer solo(a) para evitar el estrés de cenar en familia. | |||||
| Durante la hora de la cena, se gritaba. | |||||
| Era un alivio cuando mi padre no estaba presente en la hora de la cena. | |||||
| De joven, mi padre hacia comentarios sobre el peso de mi madre. | |||||
| El horario de mi padre establecía la hora de la cena para mi familia. | |||||
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andaya AA, Arredondo EM, Alcaraz JE, Lindsay SP, & Elder JP (2011). The association between family meals, TV viewing during meals, and fruit, vegetables, soda, and chips intake among Latino children. Journal of nutrition education and behavior, 43(5), 308–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson SE, Must A, Curtin C, & Bandini LG (2012). Meals in Our Household: reliability and initial validation of a questionnaire to assess child mealtime behaviors and family mealtime environments. Journal of the Academy of Nutrition and Dietetics, 112(2), 276–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcan C, Neumark-Sztainer D, Hannan P, Van Den Berg P, Story M, & Larson N (2007). Parental eating behaviours, home food environment and adolescent intakes of fruits, vegetables and dairy foods: longitudinal findings from Project EAT. Public health nutrition, 10(11), 1257–1265. [DOI] [PubMed] [Google Scholar]
- Ayala GX, Baquero B, Arredondo EM, Campbell N, Larios S, & Elder JP (2007). Association between family variables and Mexican American children’s dietary behaviors. Journal of nutrition education and behavior, 39(2), 62–69. [DOI] [PubMed] [Google Scholar]
- Barlow SE, & Dietz WH (1998). Obesity evaluation and treatment: expert committee recommendations. Pediatrics, 102(3), e29–e29. [DOI] [PubMed] [Google Scholar]
- Barnes HL, & Olson DH (1985). Parent-adolescent communication and the circumplex model. Child development, 438–447. [Google Scholar]
- Berge JM, Wall M, Larson N, Loth KA, & Neumark-Sztainer D (2013). Family functioning: associations with weight status, eating behaviors, and physical activity in adolescents. Journal of adolescent health, 52(3), 351–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boquin M, Smith-Simpson S, Donovan SM, & Lee SY (2014). Mealtime behaviors and food consumption of perceived picky and nonpicky eaters through home use test. Journal of food science, 79(12), S2523–S2532. [DOI] [PubMed] [Google Scholar]
- Brown T (2006). Confirmatory factor analysis for applied research. New York, NY: Guilford; Browne, MW, & Cudeck, R.(1993). Alternative ways of assessing model t. KA Bollen & JS Long. [Google Scholar]
- Bruch H (1969). Hunger and instinct. Journal of Nervous and Mental Disease. [DOI] [PubMed] [Google Scholar]
- Burnier D, Dubois L, & Girard M (2011). Arguments at mealtime and child energy intake. Journal of nutrition education and behavior, 43(6), 473–481. [DOI] [PubMed] [Google Scholar]
- Burns A, Parker L, & Birch LL (2011). Early childhood obesity prevention policies: National Academies Press. [Google Scholar]
- Castro FG, Shaibi GQ, & Boehm-Smith E (2009). Ecodevelopmental contexts for preventing type 2 diabetes in Latino and other racial/ethnic minority populations. Journal of behavioral medicine, 32(1), 89–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. 2nd: Hillsdale, NJ: erlbaum. [Google Scholar]
- Coleman-Jensen A, Rabbit MP, Gregory CA, & Singh A (2017). Statistical Supplement to Household Food Security in the United States in 2016. Economic Research Service, AP-077. [Google Scholar]
- Counihan C, & Van Esterik P (2012). Food and culture: A reader: Routledge. [Google Scholar]
- Crist W, & Napier-Phillips A (2001). Mealtime behaviors of young children: A comparison of normative and clinical data. Journal of Developmental & Behavioral Pediatrics, 22(5), 279–286. [DOI] [PubMed] [Google Scholar]
- Daniels SR, & Hassink SG (2015). The role of the pediatrician in primary prevention of obesity. Pediatrics, peds 2015–1558. [DOI] [PubMed] [Google Scholar]
- Davis AM, Canter KS, Stough CO, Gillette MD, & Patton S (2013). Measurement of mealtime behaviors in rural overweight children: An exploratory factor analysis of the behavioral pediatrics feeding assessment scale. Journal of Pediatric Psychology, 39(3), 332–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickstein S (2002). Family routines and rituals--The importance of family functioning: Comment on the special section. [PubMed]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural equation modeling, 8(3), 430–457. [PubMed] [Google Scholar]
- Fabrigar LR, Wegener DT, MacCallum RC, & Strahan EJ (1999). Evaluating the use of exploratory factor analysis in psychological research. Psychological methods, 4(3), 272. [Google Scholar]
- Fagundo AB, De la Torre R, Jimenez-Murcia S, Aguera Z, Granero R, Tarrega S, … Rodriguez R (2012). Executive functions profile in extreme eating/weight conditions: from anorexia nervosa to obesity. PloS one, 7(8), e43382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiese BH, Foley KP, & Spagnola M (2006). Routine and ritual elements in family mealtimes: Contexts for child well-being and family identity. New directions for child and adolescent development, 2006(111), 67–89. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Hammons A, & Grigsby-Toussaint D (2012). Family mealtimes: a contextual approach to understanding childhood obesity. Economics & Human Biology, 10(4), 365–374. [DOI] [PubMed] [Google Scholar]
- Frank ES (1991). Shame and guilt in eating disorders. American Journal of Orthopsychiatry, 61(2), 303–306. [DOI] [PubMed] [Google Scholar]
- Franklin SB, Gibson DJ, Robertson PA, Pohlmann JT, & Fralish JS (1995). Parallel analysis: a method for determining significant principal components. Journal of Vegetation Science, 6(1), 99–106. [Google Scholar]
- Fulkerson JA, Neumark-Sztainer D, Hannan PJ, & Story M (2008). Family meal frequency and weight status among adolescents: cross-sectional and 5-year longitudinal associations. Obesity, 16(11), 2529–2534. [DOI] [PubMed] [Google Scholar]
- Golan M, & Weizman A (1998). Reliability and validity of the family eating and activity habits questionnaire. European Journal of Clinical Nutrition, 52(10), 771. [DOI] [PubMed] [Google Scholar]
- Golden NH, Katzman DK, Sawyer SM, & Ornstein RM (2015). Position paper of the society for adolescent health and medicine: medical management of restrictive eating disorders in adolescents and young adults references. Journal of adolescent health, 56(1), 121–125. [DOI] [PubMed] [Google Scholar]
- Golden NH, Schneider M, & Wood C (2016). Preventing obesity and eating disorders in adolescents. Pediatrics, 138(3), e20161649. [DOI] [PubMed] [Google Scholar]
- Goldfarb SS, Tarver WL, Locher JL, Preskitt J, & Sen B (2015). A systematic review of the association between family meals and adolescent risk outcomes. Journal of adolescence, 44, 134–149. [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Aspen VP, Sinton MM, Tanofsky-Kraff M, & Wilfley DE (2008). Disordered eating attitudes and behaviors in overweight youth. Obesity, 16(2), 257–264. [DOI] [PubMed] [Google Scholar]
- Gorman-Smith D, Tolan PH, Zelli A, & Huesmann LR (1996). The relation of family functioning to violence among inner-city minority youths. Journal of family psychology, 10(2), 115. [Google Scholar]
- Haines J, & Neumark-Sztainer D (2006). Prevention of obesity and eating disorders: a consideration of shared risk factors. Health education research, 21(6), 770–782. [DOI] [PubMed] [Google Scholar]
- Hammons AJ, & Fiese BH (2011). Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics, 127(6), e1565–e1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendy HM, Williams KE, Camise TS, Eckman N, & Hedemann A (2009). The Parent Mealtime Action Scale (PMAS). Development and association with children’s diet and weight. Appetite, 52(2), 328–339. [DOI] [PubMed] [Google Scholar]
- Irving LM, & Neumark-Sztainer D (2002). Integrating the prevention of eating disorders and obesity: feasible or futile? Preventive medicine, 34(3), 299–309. [DOI] [PubMed] [Google Scholar]
- Kaiser HF (1970). A second generation little jiffy. Psychometrika, 35(4), 401–415. [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Hawkins J, … Zaza S (2016). Youth risk behavior surveillance—United States, 2015. Morbidity and Mortality Weekly Report: Surveillance Summaries, 65(6), 1–174. [DOI] [PubMed] [Google Scholar]
- Kaufman L, & Karpati A (2007). Understanding the sociocultural roots of childhood obesity: food practices among Latino families of Bushwick, Brooklyn. Social science & medicine, 64(11), 2177–2188. [DOI] [PubMed] [Google Scholar]
- Kline R (2011). Principles and Practice of Structural Equation Modeling, 3rd edn Guilford Press; New York. [Google Scholar]
- Kumanyika SK (2008). Environmental influences on childhood obesity: ethnic and cultural influences in context. Physiology & behavior, 94(1), 61–70. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, & Rick J (2004). The structure of child and adolescent psychopathology: generating new hypotheses. Journal of abnormal psychology, 113(3), 358. [DOI] [PubMed] [Google Scholar]
- Larsen JK, Hermans RC, Sleddens EF, Engels RC, Fisher JO, & Kremers SP (2015). How parental dietary behavior and food parenting practices affect children’s dietary behavior. Interacting sources of influence? Appetite, 89, 246–257. [DOI] [PubMed] [Google Scholar]
- Lebow J, Sim LA, & Kransdorf LN (2015). Prevalence of a history of overweight and obesity in adolescents with restrictive eating disorders. Journal of adolescent health, 56(1), 19–24. [DOI] [PubMed] [Google Scholar]
- Lebron CN, Lee TK, Park SE, St George SM, Messiah SE, & Prado G (2018). Effects of parent-adolescent reported family functioning discrepancy on physical activity and diet among Hispanic youth. Journal of family psychology, 32(3), 333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJ (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American statistical Association, 83(404), 1198–1202. [Google Scholar]
- Little TD (2013). Longitudinal structural equation modeling: Guilford Press. [Google Scholar]
- Lloyd AB, Lubans DR, Plotnikoff RC, Collins CE, & Morgan PJ (2014). Maternal and paternal parenting practices and their influence on children’s adiposity, screen-time, diet and physical activity. Appetite, 79, 149–157. [DOI] [PubMed] [Google Scholar]
- Malcolm S, Huang S, Cordova D, Freitas D, Arzon M, Jimenez GL, … Prado G (2013). Predicting condom use attitudes, norms, and control beliefs in Hispanic problem behavior youth: The effects of family functioning and parent-adolescent communication about sex on condom use. Health Education & Behavior, 40(4), 384–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus D, & Wiener M (1989). Anorexia nervosa reconceptualized from a psychosocial transactional perspective. American Journal of Orthopsychiatry, 59(3), 346–354. [DOI] [PubMed] [Google Scholar]
- Martin-Biggers J, Spaccarotella K, Berhaupt-Glickstein A, Hongu N, Worobey J, & Byrd-Bredbenner C (2014). Come and Get It! A Discussion of Family Mealtime Literature and Factors Affecting Obesity Risk-. Advances in nutrition, 5(3), 235–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martyn-Nemeth P, Penckofer S, Gulanick M, Velsor-Friedrich B, & Bryant FB (2009). The relationships among self-esteem, stress, coping, eating behavior, and depressive mood in adolescents. Research in nursing & health, 32(1), 96–109. [DOI] [PubMed] [Google Scholar]
- McCurdy K, & Gorman KS (2010). Measuring family food environments in diverse families with young children. Appetite, 54(3), 615–618. [DOI] [PubMed] [Google Scholar]
- Meno CA, Hannum JW, Espelage DE, & Low KD (2008). Familial and individual variables as predictors of dieting concerns and binge eating in college females. Eating behaviors, 9(1), 91–101. [DOI] [PubMed] [Google Scholar]
- Miller DA, McCluskey-Fawcett K, & Irving LM (1993). Correlates of bulimia nervosa: Early family mealtime experiences. Adolescence, 28(111), 621. [PubMed] [Google Scholar]
- Morales JF, Yubero S, & Larranaga E (2016). Gender and bullying: Application of a three-factor model of gender stereotyping. Sex Roles, 74(3–4), 169–180. [Google Scholar]
- Muthen L, & Muthen B (1987–2017). Mplus user: T s Guide. Seventh Edition Los Angeles, CA: Muthen & Muthén. [Google Scholar]
- Neumark-Sztainer D, Eisenberg ME, Fulkerson JA, Story M, & Larson NI (2008). Family meals and disordered eating in adolescents: longitudinal findings from project EAT. Archives of pediatrics & adolescent medicine, 162(1), 17–22. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Larson NI, Fulkerson JA, Eisenberg ME, & Story M (2010). Family meals and adolescents: what have we learned from Project EAT (Eating Among Teens)? Public health nutrition, 13(7), 1113–1121. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Perry C, & Story M (2003). Correlates of fruit and vegetable intake among adolescents: Findings from Project EAT. Preventive medicine, 37(3), 198–208. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Story M, & Standish AR (2012). Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. Journal of adolescent health, 50(1), 80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer DR, Wall MM, Haines JI, Story MT, Sherwood NE, & van den Berg PA (2007). Shared risk and protective factors for overweight and disordered eating in adolescents. American journal of preventive medicine, 33(5), 359–369. e353. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Story M, & Sherwood NE (2009). Five-year longitudinal predictive factors for disordered eating in a population-based sample of overweight adolescents: Implications for prevention and treatment. International Journal of Eating Disorders, 42(7), 664–672. [DOI] [PubMed] [Google Scholar]
- Niemeier BS, Hektner JM, & Enger KB (2012). Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis. Preventive medicine, 55(1), 3–13. [DOI] [PubMed] [Google Scholar]
- O’connor BP (2000). SPSS and SAS programs for determining the number of components using parallel analysis and Velicer’s MAP test. Behavior research methods, instruments, & computers, 32(3), 396–402. [DOI] [PubMed] [Google Scholar]
- Offer S (2013). Assessing the relationship between family mealtime communication and adolescent emotional well-being using the experience sampling method. Journal of adolescence, 36(3), 577–585. [DOI] [PubMed] [Google Scholar]
- Ohannessian CM, Lerner RM, Lerner JV, & von Eye A (1995). Discrepancies in adolescents’ and parents’ perceptions of family functioning and adolescent emotional adjustment. The Journal of Early Adolescence, 15(4), 490–516. [Google Scholar]
- Ozier AD, & Henry BW (2011). Position of the American Dietetic Association: nutrition intervention in the treatment of eating disorders. Journal of the American Dietetic Association, 111(8), 1236–1241. [DOI] [PubMed] [Google Scholar]
- Pantin H (1996). Ecodevelopmental measures of support and conflict for Hispanic youth and families. Miami, FL: University of Miami School of Medicine. [Google Scholar]
- Patton SR, Dolan LM, & Powers SW (2006). Parent report of mealtime behaviors in young children with type 1 diabetes mellitus: Implications for better assessment of dietary adherence problems in the clinic. Journal of Developmental & Behavioral Pediatrics, 27(3), 202–208. [DOI] [PubMed] [Google Scholar]
- Perez-Escamilla R (2009). Dietary quality among Latinos: is acculturation making us sick? Journal of the American Dietetic Association, 109(6), 988–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quick V, & Byrd-Bredbenner C (2013). Disturbed eating behaviours and associated psychographic characteristics of college students. Journal of Human Nutrition and Dietetics, 26(s1), 53–63. [DOI] [PubMed] [Google Scholar]
- Quick VM, McWilliams R, & Byrd-Bredbenner C (2012). Case-control study of disturbed eating behaviors and related psychographic characteristics in young adults with and without diet-related chronic health conditions. Eating behaviors, 13(3), 207–213. [DOI] [PubMed] [Google Scholar]
- Rollins BY, Belue RZ, & Francis LA (2010). The beneficial effect of family meals on obesity differs by race, sex, and household education: the national survey of children’s health, 2003–2004. Journal of the American Dietetic Association, 110(9), 1335–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Carracedo D, Neumark-Sztainer D, & Lopez-Guimera G (2012). Integrated prevention of obesity and eating disorders: barriers, developments and opportunities. Public health nutrition, 15(12), 2295–2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sass DA, & Schmitt TA (2010). A comparative investigation of rotation criteria within exploratory factor analysis. Multivariate Behavioral Research, 45(1), 73–103. [DOI] [PubMed] [Google Scholar]
- Schwartz SJ, Mason CA, Pantin H, & Szapocznik J (2008). Effects of family functioning and identity confusion on substance use and sexual behavior in Hispanic immigrant early adolescents. Identity: An International Journal of Theory and Research, 8(2), 107–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ, Pantin H, Prado G, Sullivan S, & Szapocznik J (2005). Family functioning, identity, and problem behavior in Hispanic immigrant early adolescents. The Journal of Early Adolescence, 25(4), 392–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen B (2006). Frequency of family dinner and adolescent body weight status: evidence from the national longitudinal survey of youth, 1997. Obesity, 14(12), 2266–2276. [DOI] [PubMed] [Google Scholar]
- Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, & Armstrong SC (2018). Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics, e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St George S, Petrova M, Kyoung Lee T, Sardinas K, Kobayashi M, Messiah S, & Prado G (2018). Predictors of Participant Attendance Patterns in a Family-Based Intervention for Overweight and Obese Hispanic Adolescents. International journal of environmental research and public health, 15(7), 1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St. George SM, Messiah SE, Sardinas KM, Poma S, Lebron C Tapia M, Velazquez MR, Pantin H, & Prado G (2018). Familias Unidas for health & wellness: Adapting an evidence-based substance use and sexual risk behavior intervention for obesity prevention in Hispanic adolescents. The Journal of Primary Prevention. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart J, & Jose PE (2012). The influence of discrepancies between adolescent and parent ratings of family dynamics on the well-being of adolescents. Journal of family psychology, 26(6), 858. [DOI] [PubMed] [Google Scholar]
- Stunkard A, Sorensen T, & Schlusinger F (2006). Use of Danish adoption register for the study of obesity and thinness. 1983. Scagliusi FB et al. [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, & Yanovski JA (2009). A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. International Journal of Eating Disorders, 42(1), 26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson FE, Midthune D, Kahle L, & Dodd KW (2017). Development and evaluation of the National Cancer Institute’s dietary screener questionnaire scoring algorithms. The Journal of nutrition, 147(6), 1226–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JK, & Smolak L (2001). Body image, eating disorders, and obesity in youth: Assessment, prevention, and treatment: Taylor & Francis. [Google Scholar]
- Vaughn AE, Ward DS, Fisher JO, Faith MS, Hughes SO, Kremers SP, … Power TG (2015). Fundamental constructs in food parenting practices: a content map to guide future research. Nutrition reviews, 74(2), 98–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts A, Berge JM, Loth K, Larson N, & Neumark-Sztainer D (2018). The transmission of family food and mealtime practices from adolescence to adulthood: longitudinal findings from project EAT-IV. Journal of nutrition education and behavior, 50(2), 141–147. e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiler DM, & Crist JD (2009). Diabetes self-management in a Latino social environment. The Diabetes Educator, 35(2), 285–292. [DOI] [PubMed] [Google Scholar]
- Westfall PH, Arias AL, & Fulton LV (2017). Teaching Principal Components Using Correlations. Multivariate Behavioral Research, 52(5), 648–660. [DOI] [PubMed] [Google Scholar]
- Worobey J (2002a). Early family mealtime experiences and eating attitudes in normal weight, underweight and overweight females. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 7(1), 39–44. [DOI] [PubMed] [Google Scholar]
- Worobey J (2002b). Interpersonal versus intrafamilial predictors of maladaptive eating attitudes in young women. Social Behavior and Personality, 30(5), 423–434. [Google Scholar]
- Yee AZ, Lwin MO, & Ho SS (2017). The influence of parental practices on child promotive and preventive food consumption behaviors: A systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yong AG, & Pearce S (2013). A beginner’s guide to factor analysis: Focusing on exploratory factor analysis. Tutorials in quantitative methods for psychology, 9(2), 79–94. [Google Scholar]