Abstract
OBJECTIVES:
To evaluate the effect of emergency department (ED) interventions on clinical, utilization, and care experience outcomes for older adults.
DESIGN:
A conceptual model informed, protocol-based systematic review.
SETTING:
Emergency Department (ED).
PARTICIPANTS:
Older adults 65 years of age and older.
METHODS AND MEASUREMENT:
Medline, Embase, CINAHL, and PsycINFO were searched for English-language studies published through December 2017. Studies evaluating the use of one or more eligible intervention strategies (discharge planning, case management, medication safety or management, and geriatric EDs including those that cited the 2014 Geriatric ED Guidelines) with adults 65 years of age and older were included. Studies were classified by the number of intervention strategies used (ie, single strategy or multi-strategy) and key intervention components present (ie, assessment, referral plus follow-up, and contact both before and after ED discharge [“bridge”]). The effect of ED interventions on clinical (functional status, quality of life [QOL]), patient experience, and utilization (hospitalization, ED return visit) outcomes was evaluated.
RESULTS:
A total of 2000 citations were identified; 17 articles describing 15 unique studies (9 randomized and 6 nonrandomized) met eligibility criteria and were included in analyses. ED interventions showed a mixed pattern of effects. Overall, there was a small positive effect of ED interventions on functional status but no effects on QOL, patient experience, hospitalization at or after the initial ED index visit, or ED return visit.
CONCLUSION:
Studies using two or more intervention strategies may be associated with the greatest effects on clinical and utilization outcomes. More comprehensive interventions, defined as those with all three key intervention components present, may be associated with some positive outcomes.
Keywords: geriatric emergency medicine, emergency department, interventions
Older adults have some of the highest rates of emergency department (ED) visits. In the United States, older adults make 64 ED visits per 100 persons annually, nearly twice the frequency of their younger counterparts.1 Challenges that impact ED care for this patient population include multiple morbidities, atypical symptoms or disease states, polypharmacy and adverse drug-drug interactions, and misunderstandings or misuse of prescription and over- the-counter medications.2,3 Additionally, older adults may be challenged by functional disabilities, impaired cognition, communication problems, and reduced social support.4,5 Together, these challenges can negatively impact the care received while in the ED, transitions to home or other settings, and postdischarge health outcomes and utilization patterns including hospitalization and ED return visits.6,7
A broad range of interventions have been designed to improve clinical and utilization outcomes in older adults who visit the ED. Broadly speaking, these interventions can be grouped into several categories including staffing, physical infrastructure, care delivery (including functional and geriatric assessments, and risk prediction tools), case management, and transitional care or discharge planning.8–12 Existing reviews have classified interventions globally rather than identifying details of the intervention structure and its components. This global approach may potentially obscure relationships between components of the intervention structure and outcomes. Further, most prior studies of geriatric ED practices have focused on utilization outcomes; few prior studies have included clinical outcomes such as functional status.
The past decade has seen growing attention on geriatric emergency medicine, as evident by an increasing number of special interest groups within professional organizations, initiatives sponsored by the Centers for Medicare & Medicaid such as GEDI WISE,13 and the publication of research priorities advocating for additional work focusing on the structure of ED services and the impact of ED care on function and other patient-prioritized outcomes.14,15 Perhaps the most recognized initiative was the publication of Geriatric Emergency Department Guidelines in 2014.16–19 These guidelines offer a “template” of recommendations in developing a “geriatric-friendly ED.” Recommendations focus on staffing, administration, physical environment, and leadership, yet they do not provide recommendations on specific interventions or programs for older adults seeking care in the ED. Many of these initiatives just described and research priorities have focused on specific subgroups of older adults, making it difficult to determine which strategies might be most effective for the heterogeneous population typically seen in the ED.
In the absence of suggested interventions and facing a growing number of older adults using Veterans Affairs (VA) EDs, this review was performed in collaboration with clinical and operations leaders of the Veterans Health Administration (VHA) with the primary goal of identifying effective intervention strategies that could be implemented in more than 100 EDs across the VHA system. The key question of this review was “How effective are emergency department (ED) interventions in improving clinical, patient experience, and utilization outcomes in older adults (age ≥65)?” Additionally, our review included both single- and multi-strategy interventions, and carefully classified individual intervention components used within these strategies.
METHODS
This review is part of a larger report for the US VHA’s Evidence- based Synthesis Program conducted in collaboration with VA operational partners and a technical expert panel (TEP). Members of TEP were chosen for their clinical or research expertise in geriatric EDs and were consulted throughout the course of the review, specifically in finalizing research questions, reviewing the final list of included and excluded studies, contextualization of results, and peer review of the final report.
Our review was informed by a conceptual model (Figure S1) that drew on previously published models.20,21 We followed a standard protocol for all steps of this review (PROSPERO: CRD42018087660). Our full report, referenced earlier, is available at https://www.hsrd.research.va.gov/publications/esp.
Search Strategy
Our study protocol, including search strategy and detailed identification of intervention strategies and components, was developed a priori in collaboration with the partners, TEP, and project team previously described. Intervention strategies and components were identified based on prior literature22,23 and Effective Practice and Organization of Care (EPOC) guidelines,24 and finalized through a series of collaborative iterative discussions. We conducted searches of Medline (via PubMed), Embase, CINAHL, and PsyclNFO for English- language studies published through December 2017 evaluating interventions for older adults using the ED (Table S1). We also reviewed bibliographies of relevant review articles. In an effort to identify research currently in progress, including studies that cited the 2014 Geriatric ED Guidelines, we also searched ClinicalTrials.gov and performed a targeted search of Scopus for relevant conference abstracts.
Study Selection
Using prespecified eligibility criteria (Table S2), titles and abstracts identified through our initial search were reviewed by two reviewers. To be included, studies had to (1) enroll older adults aged 65 or older presenting to the ED, (2) evaluate an eligible intervention strategy (described later and in Table S3), (3) use a randomized or quasi-experimental design (nonrandomized trial, case-matched controlled prospective before-and-after cohort study, interrupted time series),24 (4) be conducted in an Organization for Economic Cooperation and Development (OECD) country,25 and (5) report one or more clinical or utilization outcomes of interest. Articles included by either reviewer underwent full-text screening.
Data Abstraction and Analyses
Data from published reports were abstracted into a customized DistillerSR database by one reviewer; a second investigator reviewed these data for accuracy, and disagreements were resolved by consensus or a third reviewer. Key characteristics abstracted included patient descriptors, intervention characteristics, comparator, and outcomes.
For this review, ED interventions included four major strategies: discharge planning, case management, medication safety or management, and geriatric EDs including those that cited the 2014 Geriatric ED Guidelines.16 Table S3 has an in-depth description of intervention strategies and components. Reviewers classified each study by its primary intervention strategy; studies utilizing two or more intervention strategies were classified as “multi-strategy.” Detailed information about the intervention structure and individual intervention components was also abstracted. This included the timing and setting (ie, before or after ED discharge, or both [“bridge”]); target of intervention (eg, patient, caregiver/family member, provider); mode of delivery (eg, telephone, in person); number and type of providers; number of planned contacts; and number of actual contacts. Additional details were abstracted regarding patient-focused intervention components (eg, assessment/ screening, patient and/or caregiver education, or support) and provider- or service-driven components (eg, referral to provider and/or community resources, follow-up call or visit, continuity of care/care coordination, environmental or procedural changes in response to 2014 Geriatric ED guidelines). In consultation with our stakeholders and TEP, we evaluated the presence of three key intervention components: assessment, referral plus follow-up, and contact both before and after ED discharge (“bridge” design).
Two reviewers independently assessed study risk of bias (ROB) using the criteria described by the Cochrane EPOC.24 Summary ROB ratings were assigned to each study: low bias (unlikely to alter the results seriously), unclear bias (raises some doubts about the results), or high bias (may alter the results seriously).
Data Synthesis and Analysis
Primary outcomes were organized into clinical and utilization outcomes. We developed summary tables to describe the key study and intervention characteristics (Tables S4–S7). All analyses were stratified by study design (randomized or nonrandomized).
We aggregated outcomes when there were at least three studies with the same outcome, reported at similar time points; for nonrandomized studies, we required adequately adjusted analyses to be reported for inclusion in quantitative syntheses. When quantitative synthesis was possible, we used random effects models (DerSimonian-Laird estimator with Knapp-Hartung SE adjustment26,27) to synthesize dichotomous outcomes (ie, hospitalization at or after the ED index visit, ED return visit) using risk ratios, and the mean difference (MD) for continuous outcomes (ie, quality of life [QOL]). We evaluated statistical heterogeneity using visual inspection and Cochran’s Q and I2 statistics. There were too few studies to assess publication bias with test statistics. We planned formal subgroup analyses of moderator variables (eg, intervention strategy, individual intervention components), but there were too few studies to conduct these analyses.
Strength of the Body of Evidence
The strength of evidence (SOE) was assessed using the Grading of Recommendations Assessment, Development and Evaluation working group (GRADE) approach.28 In brief, this approach requires assessment of four domains: ROB, consistency, directness, and precision. We considered these domains qualitatively for the primary outcomes and assigned a summary rating of high, moderate, low, or very low SOE after evaluating using the GRADEpro software29 and discussion by two reviewers. SOE was assessed only for outcomes considered critical to clinical or administrative decision making: functional status, ED return visit, hospital admission, and patient experience.
RESULTS
Literature Flow and Included Studies
A total of 2000 citations were identified from a combined search of databases, reviewing bibliographies of relevant review articles, and targeted searches of ClinicalTrials.gov and Scopus. After applying eligibility criteria, 17 articles describing 15 studies, nine randomized30–38 and six nonrandomized39–44 were included (Figure 1).
Figure 1.
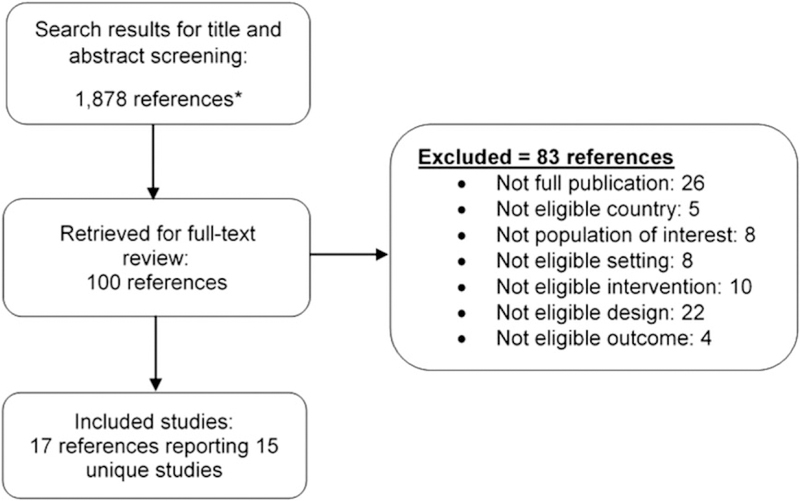
Literature flow diagram. Asterisk indicates unique citations after combining all searches and manual bibliography review.
The literature evaluated three of the four a priori intervention strategies including case management (n = 12), discharge planning (n = 7), and medication management/medication safety (n = 3). We found no studies that evaluated geriatric EDs, including those that cited the 2014 Guidelines.16 Roughly one-half of studies (n = 7) evaluated two or more intervention strategies and were classified as multi-strategy. Studies were also evaluated for three key patient-focused intervention components including assessment (n = 12, 8 of which specified use of a comprehensive geriatric assessment), referral plus follow- up (n = 6), and contact both before and after ED discharge, defined as a bridge design (n = 5). Studies that included all three key intervention components were classified as having a more comprehensive structure (n = 4).33,34,36,37 Additional details of the 15 included studies, including characteristics of study participants, is shown in Table 1. Additional details of the included intervention components are included in Tables S6 and S7.
Table 1.
Evidence Profile for Emergency Department Interventions for Older Adults
| Randomized (n = 9) | Nonrandomized (n = 6) | |||
|---|---|---|---|---|
| Study designs | 8 randomized studies | 5 nonrandomized studies | ||
| 1 cluster-randomized study | 1 controlled before-after study | |||
| No. of patients | 4561 | 11 580 | ||
| Patient eligibilitya | 4 high-risk patients only | 4 high-risk patients only | ||
| 5 unselected older adults | 2 unselected older adults | |||
| Exclusion criteria | 3 need for immediate treatment | 3 need for immediate treatment | ||
| 6 long-term care facility | 0 long-term care facility | |||
| 5 cognitive impairment | 1 cognitive impairment | |||
| Median patient age (range) | 79 (74–82) (1 study NR) | 78.5 (75–86) | ||
| Patient sex, % | 59% women | 59% women | ||
| Race, % | 64% white (6 studies NR) | 67% white (5 studies NR) | ||
| 25% black | 32% black | |||
| Patients with cognitive impairmentb | 27.3% (5 studies NR) | 8.5% (5 studies NR) | ||
| Patients’ living status (%) | 789/4688 (16.8%) living alone | 3072/11 580 (26.5%) living alone | ||
| (5 studies NR) | (2 studies NR) | |||
| Patient has primary carec | 88% (8 studies NR) | NR | ||
| Intervention strategyd | 3 discharge planning | 4 discharge planning | ||
| 9 case management | 3 care management | |||
| 2 medication safety | 1 medication management | |||
| 0 geriatric EDs | 0 geriatric EDs | |||
| Multi-strategy interventions | 5 studies | 2 studies | ||
| Key intervention componentsd | 7 assessment | 5 assessment | ||
| 5 referral plus follow-up | 1 referral plus follow-up | |||
| 4 bridge designe | 1 bridge designe | |||
| Outcomes reported | 7 ED readmission | 5 ED readmission | ||
| 6 functional status | 1 functional status | |||
| 5 hospitalization after ED discharge | 3 hospitalization after ED discharge | |||
| 4 patient experience | 1 patient experience | |||
| 2 quality of life | 1 quality of life | |||
| 2 hospitalization at ED index | 2 hospitalization at ED index | |||
| Risk of bias for objective and patient-reported | Objective: | Patient-reported: | Objective: | Patient-reported: |
| outcomes | 2 high risk | 4 high risk | 5 high risk | 2 high risk |
| 3 unclear risk | 3 unclear risk | 1 low risk | 4 NA | |
| 3 low risk | 2 low risk | |||
| 1 NA | ||||
Abbreviation: ED = emergency department; NA = not applicable; NR = not reported.
High-risk is defined by the study authors based on risk assessment tool and/or specific criteria or condition(s).
Definitions of impairment varied from abnormal cognitive screen to dementia to delirium/confusion.
Six randomized and five nonrandomized studies were conducted in countries with National Health Service.
Numbers sum to more than 15 because studies used more than one intervention type.
Design refers to interventions that include contact both within the ED and after discharge.
Effects on Clinical Outcomes
Functional Status
Six studies, five randomized, evaluated the effect of ED interventions on functional status, assessed from 1 to 18 months after the ED visit.33–36,38,42 Three studies evaluated multi-strategy interventions, all using discharge planning plus case management,34,36,42 two of which included all three intervention components of interest.34,36 Positive intervention effects were observed in four of the five randomized studies.33,34,36,38
Functional status was assessed differently across the studies. Three randomized studies defined functional status as changes in dependence in activities of daily living (ADLs) or instrumental activities of daily living (IADLs).34,36,38 One multi-strategy study, using discharge planning plus case management and one key intervention component, found a statistically significant lower odds of clinically important functional dependency (odds ratio [OR] = .53; 95% CI = .31-.91) at 3 and 4 months, respectively.36 A second multi-strategy study, also utilizing discharge planning plus case management and one key intervention component, found a significantly greater odds of functional improvement, as defined by improvement in ADL performance measured at 3 months (OR = 2.37; 95% CI = 1.20–4.68) and 12 months (OR = 2.04; 95% CI = 1.03–4.06).34 A third single-strategy study of case management involving one key intervention component found that intervention participants reported higher levels of functional independence in IADLs compared with the control group (P = .027), but there were no significant differences in ADL independence (P = .47).38 One nonrandomized multi-strategy study of discharge planning plus case management included only one key intervention component and examined the number of older adults reporting basic and intermediate dependency in ADLs based on the Katz scale.42 Although no statistical tests were presented, the number of participants reporting each level of dependency at 3 months was similar for the intervention and control groups.
Two randomized studies of case management interventions evaluated change in functional status as a continuous outcome.33,35 The first study included one key intervention component and recruited a high-risk population of older adults who had been admitted to the hospital in the prior 12 months.35 There were no differences in ADL or IADL mean scores between groups. A second study included all three key intervention components and found that intervention participants reported less functional decline at 6 months compared with control (‒.25 intervention vs ‒.75 control; P < .001),33 although there were no significant differences between groups at 18 months.
Quality of Life
Two randomized studies evaluated multi-strategy interventions of discharge planning plus case management on QOL.35,37 Both studies reported physical and mental health-related QOL using the Short Form-36 physical function and mental health component scores at 3037 and 120 days.35 There were no statistically significant effects of the ED interventions on either physical or mental health–related QOL at any time point. There were not sufficient data reported in one nonrandomized study42 to conduct an analysis. However, scores were similar for intervention and control participants.
Effects on Patient Experience Outcomes
Four randomized studies evaluated the effect of ED interventions on patient experience using a range of outcome measures; effects were mixed.35–38 Two studies evaluated multi-strategy interventions of discharge planning plus case management, and they included all three intervention components of interest.36,37 Overall, these studies show a mixed pattern, with one single-strategy and one multi-strategy study reporting higher satisfaction with care or greater patient knowledge of community resources.37,38
Two studies, one using case management and the second discharge planning plus case management, evaluated patient satisfaction with care using continuous outcome measures, the Client Satisfaction Questionnaire and Satisfaction with Care Scale.35,36 Assessment time points occurred at 1 and 10 months. There were no statistically significant effects on patient experience in either study. A third study37 found higher satisfaction among intervention participants regarding information received in the ED on postdischarge support services (3.42 vs 3.03; MD = .37; 95% CI = .13‒.62). A fourth study evaluating case management utilized an unnamed instrument and found that 40% of intervention participants recalled helpful information, and 28% reported benefits of improved confidence and self-esteem.38
Effects on Utilization Outcomes
Hospitalization at the ED Index Visit
Four studies, two randomized, examined the effect of ED interventions on hospitalization at the index ED visit.30,36,39,41 Overall, there was no pattern of interventions on hospitalization at the index visit. Only one study included all three intervention components, with very few patients admitted at the index visit because one of the inclusion criteria was an expectation that the patient would be discharged from the ED.36 One single-strategy intervention that utilized only one of the key intervention components found that a subset of patients who received the discharge planning intervention had a lower rate of admission.39 This was a large nonrandomized study that was judged high ROB.
Hospitalization after the ED Index Visit
Nine studies, five randomized, reported effects of ED interventions on hospitalization after the index ED visit.31–33,35,37,38,40–42 Five evaluated multi-strategy interventions,31,32,37,41,42 two of which included all three intervention components.33,37
Six studies, three randomized, reported hospitalization as a dichotomous outcome.32,33,37 Overall, there was no intervention effect for the randomized studies (relative risk [RR] = .96; 95% CI = .51–1.83; Figure 2), but the CI was wide, and intervention effects varied significantly (Q = 5.4; P = .07; I2 = 63%). Two studies had prolonged follow-up periods of 120 days and 18 months,33,37 with one finding a decreased risk of hospitalization at each of the follow-up time points.33 This study was a single-strategy case management intervention with all three key intervention components.33 Another study evaluated case management and included all three intervention components.44 This study found a lower likelihood of hospitalization at 30 days (RR = .55; 95% CI = .36-.82). A high ROB study that evaluated discharge planning and included only one intervention component, assessment, found that intervention participants had a higher risk of hospitalization at 1 year.40 The matching used for this study involved matching a high-risk intervention participant with a low-risk control participant.
Figure 2.
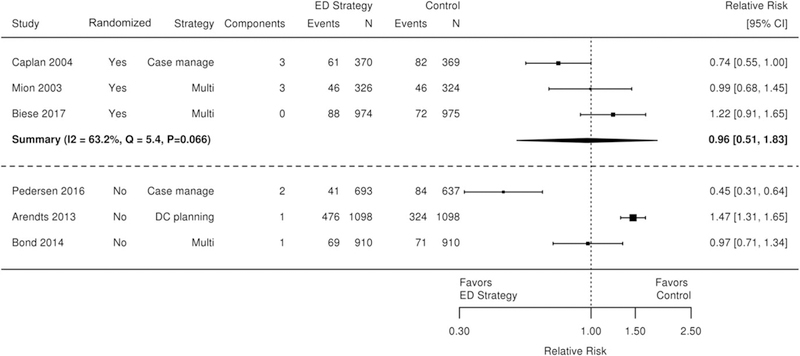
Forest plot for effect of emergency department interventions on hospitalization after the index visit. CI = confidence interval; DC = discharge; ED = emergency department.
Three randomized studies reported hospitalization after the ED index visit using a variety of continuous outcome measures.33,35,37 Only one study, which used all three intervention components, found a significant effect of the intervention on hospitalization after the ED index, with a reported number needed to treat of 18 to prevent one hospitalization at 30 days, and a number needed to treat of 10 to prevent one hospital admission at 18 months.33
Emergency Department Return Visit
Twelve studies, seven randomized, reported on return visits to the ED after the initial index ED visit.31–33,35–38,40–44 Six studies evaluated multi-strategy interventions.31,32,36,37,41,42 All three intervention components were present in three randomized studies33,36,37 and one nonrandomized study.42
When considered together, the randomized studies reporting ED return visit(s) as a dichotomous outcome found no effect on ED return visit(s) (RR = 1.13; 95% CI = .94‒1.36; Figure 3).31–33,37,38 A single low ROB study (n = 345) found that a multi-strategy intervention that used all three key components led to an increased risk of ED return visit(s) at 30 days.36 In a post hoc stratified analysis, this effect was seen only in patients who had not visited their primary care physician in the month before the ED index visit. There was also no effect of interventions on ED return visit(s) when measured as a continuous variable including both number of hospitalizations and mean length of stay at 10-month follow-up.35
Figure 3.
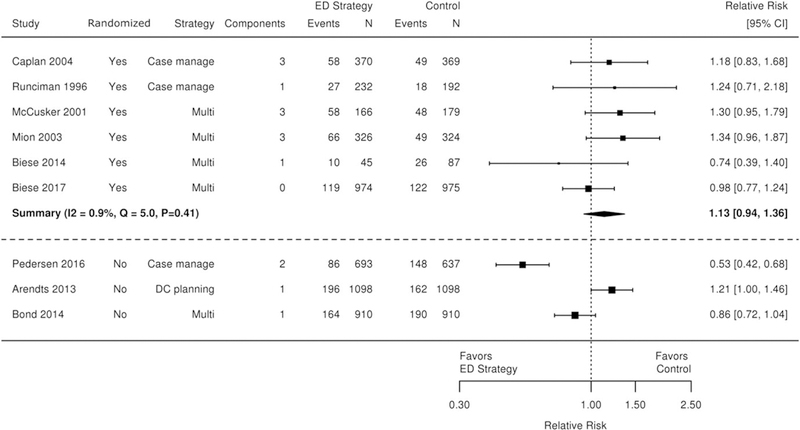
Forest plot for effect of emergency department interventions on emergency department return visit. CI = confidence interval; DC = discharge; ED = emergency department.
Four nonrandomized studies reported ED return visit(s) as a dichotomous variable,40,41,43,44 one of which evaluated a multi-strategy intervention.41 One study that used a case management strategy, with two of the three key intervention components, found that risk of ED return visit(s) following an intervention was decreased (hazard ratio = .49; 95% CI = .33-.72).44 In this study, a higher percentage of participants in the intervention group were discharged to home at the index ED visit and had more prompt follow-up and/or a longer length of sustained contact with the geriatric team. Another study evaluating a discharge planning intervention, with only assessment as a key component, found the risk of ED return visit(s) to be increased (risk difference 3%; P = .05) following receipt of the intervention.40 In this study, control case matches were low-risk participants while those in the intervention group were deemed to be high risk. A fifth nonrandomized study reported the number of ED visits within a 3-month follow-up period but found no difference between groups.42
Quality of Evidence
ROB is described for the nine randomized studies in Figure S2. We separately evaluated objective outcomes (eg, ED return visit or visits) and patient-reported, or subjective, outcomes (eg, QOL). For objective outcomes, we judged six of the nine studies as low or unclear ROB. For patient- reported outcomes, five of nine studies were judged low or unclear ROB. Factors that led to higher ROB judgments included unclear randomization and allocation concealment, detection bias (patient-reported outcomes), and differences in baseline patient characteristics.
We judged five of the six nonrandomized studies (Figure S3) as high ROB for objective outcomes and one as low ROB.44 Because the EPOC quality criteria consider random sequence generation even for nonrandomized designs, this was a major factor in the high ROB ratings. Other concerns were lack of proof that baseline provider characteristics (eg, experience) were similar, and lack of proof that baseline outcome measurements were similar. Also, many studies had fundamental differences in baseline patient characteristics that may affect outcomes.
We rated SOE for outcomes judged critical to decision making on the basis of study design, ROB, consistency, directness, and precision (Table 2). The SOE was rated high for effects on ED return visit(s). SOE was low or very low for all other outcomes. Concerns that contributed to the lower SOE were high ROB, inconsistent effects, and imprecision that was attributed to the 95% Cl not excluding a small or small to moderate effect.
Table 2.
Strength of Evidence for Effects of Interventions to Improve Outcomes for Older Adults in Emergency Departments
| Outcome | Studies (patients) | Findings | Strength of evidence (rationale by domain) |
|---|---|---|---|
| Physical function | Randomized: 5 (2233) | 3 of 5 showed benefit; beneficial interventions were multi-strategy | Very low SOE (Serious ROB, inconsistent, imprecise) |
| Nonrandomized: 1 (687) | No effect | ||
| ED readmission | Randomized: 7 (4629) | Relative risk 1.13 (.94–1.36) (9 fewer to 53 more per 1000) | High SOE (No serious ROB, consistent, precise) |
| Nonrandomized: 5 (6432) | 2 of 5 showed lower readmission; beneficial interventions were multi-strategy or case management | ||
| Hospital admission after index | Randomized: 3 (3338) | Relative risk .96 (.51–1.83) (59 fewer to 100 more per 1000) | Low SOE (No serious ROB, inconsistent, imprecise) |
| Nonrandomized: 3 (5346) | No consistent effects on readmission | ||
| Patient experience | Randomized: 4 (1889) | 2 of 4 showed benefit for satisfaction, helpfulness or self-esteem; beneficial interventions were multi-strategy or case management | Low SOE (No serious ROB, consistent, indirect, imprecise) |
| Nonrandomized: 1 (199) | No usable data | ||
Abbreviation: ED = emergency department; ROB = risk of bias; SOE = strength of evidence.
DISCUSSION
This review evaluated the effect of ED intervention strategies for older adults on a range of outcomes. Our review is unique in the approach to classifying intervention strategies and individual intervention components, careful ROB assessment, and the inclusion of randomized and more rigorous quasi-experimental designs. When considering the interventions collectively, we found a small benefit on functional status but no overall effect on ED return visit(s) or subsequent hospitalization. Although there was no overall effect on healthcare utilization, two studies with a more comprehensive intervention (ie, all three intervention components present) and longer duration of follow-up were associated with decreased ED return visits and hospitalization after the index ED visit.33,44 Other outcomes were reported less frequently, and intervention effects could not be determined definitively. Overall, the small number of included studies, the heterogeneity of study designs, and the incomplete details provided around individual intervention components prevented us from drawing definitive conclusions about the effectiveness of any one specific intervention strategy. Key takeaway messages are listed in Table 3. Some of the review’s strengths and limitations are described next.
Table 3.
Key Implications of Review
| Clinical implications | • Conducting a comprehensive geriatric assessment may be useful in identifying patients’ needs and areas for intervention |
| • Interventions that bridge care occurring before and after ED discharge may be associated with better outcomes | |
| Research implications | • Additional research is needed to identify appropriate outcome measures that are sensitive to change and can be utilized across different studies |
| • Quality improvement initiatives may represent an important aspect of research, revealing important findings within real-world settings | |
| Policy implications | • Further specificity around the 2014 Geriatric ED Guidelines, including consistent terminology, may be beneficial |
| • Patients, caregivers, providers, and other key stakeholders should be involved in guiding future research agendas |
Rather than focusing narrowly on condition-specific interventions (eg, geriatric falls, heart failure), we evaluated interventions applicable to a broad range of older adults. We were particularly interested in determining if specific strategies or intervention components were associated with greater benefit to older adults. Two strategies were evaluated infrequently (medication management) or not at all (geriatric EDs). Interventions evaluated were relatively low intensity (ie, short duration and limited number of planned patient contacts), and thus our findings are applicable only to low-intensity geriatric management interventions in the ED. Although the use of more than one strategy or a more comprehensive intervention structure (ie, a higher number of patient-centered intervention components) may be associated with better outcomes, the relative benefit of individual intervention strategies and components is unclear and requires further research.
In contrast to prior reviews that focused on single strategies,2,9,10,12 our review included studies with multiple intervention strategies. Only one of the prior systematic reviews was published in the past 5 years (search date 2013; number of studies = 9) and evaluated discharge planning; the findings of this good-quality review were consistent with our results.12 Also similar to findings from our review, another review of case management found that these interventions did not impact QOL, although the amount of evidence for this outcome was sparse.2 Across these reviews, general themes are that more comprehensive interventions and those using multiple strategies are associated with greater effects but that interventions tested to date do not show a consistent effect on utilization outcomes. Similar to previous reviews45 and the 2014 Geriatric Emergency Department Guidelines,16 our finding that bridge designs may be associated with positive outcomes suggests that ED visits should not be considered in isolation but rather as an integral part of the older patient’s continuum of care, bridging inpatient and outpatient services.
Limitations
Our protocol-driven review has several strengths, specifically the use of rigorous methods including input from an expert panel, use of a conceptual model, and a structured approach to describing the key strategies and components of the tested interventions. Despite these strengths, we note several limitations. We limited our review to English-language publications that may have excluded potentially informative evidence. In an effort to identify ED strategies conducted in similar healthcare environments and/or systems as the United States, we elected to include only those studies conducted in an OECD country. However, this may have prevented inclusion of rigorous studies published in other countries.
Variations in basic study design and the lack of analyses that adjust for potential confounders were common problems. Diversity across study designs and intervention characteristics (ie, strategies, components, delivery, and intensity) made coherent synthesis and identification of themes difficult. We were often limited in our ability to fully abstract details of individual intervention components because few studies provided in-depth descriptions of the interventions. Also, the studies identified did not apply a consistent conceptual model hypothesizing the relationship between intervention strategies and outcomes; nor did studies follow a set of clinical recommendations or guidelines, such as the 2014 Geriatric ED Guidelines,16 to inform intervention structure.
We acknowledge that the lack of studies that reference the 2014 Guidelines likely has to do with the short time frame from the publication and the length of time required to obtain funding, execute a study, conduct analyses, and publish results. Overall, we were limited by the quality of and consistency in the existing literature. Of the nine randomized studies, only three were evaluated as low ROB for objective outcomes. The most common limitation was lack of blinded outcomes assessment. Almost all nonrandomized studies were judged high ROB for both objective and patient-reported outcomes. Finally, we were unable to rule out publication bias; given the small number of studies, statistical methods to detect publication bias are not useful.
Future Directions
As the number of older adults continues to rise, and as EDs continue to provide frequent care for this population’s complex needs, it is critical that future research be conducted to identify best practices including intervention strategies. We believe future research may benefit from the following considerations. First, the use of a conceptual model may encourage researchers to consider the multilevel factors that influence ED use (eg, sociodemographic factors, clinical and individual characteristics, access to services), complex intervention strategies, and outcomes of interest, plus the relationship among these factors. Second, the use of innovative intervention designs, such as adaptive trials (eg, stepped care), and sophisticated study designs, such as pragmatic trials, may enable researchers to accommodate the heterogeneity of older adult patients while isolating and evaluating the effects of individual intervention components within real-world settings. Third, careful selection of measures that are both appropriate for a heterogeneous population and responsive to change is critical. Developing common measures to be used across studies may also help advance the field, as has been done within other geriatric research areas.46
The field of geriatric emergency medicine continues to evolve rapidly. For instance, between the conclusion of our search and the peer review process of this article, an array of studies were published including a review of self-defined geriatric EDs,47 a nurse transition intervention,48 and a pragmatic trial of an Australian-based geriatric ED.49 Ongoing research is likely to result in additional articles in the near future, as evidenced by scientific abstracts presented at recent scientific meetings. Additionally, in a targeted search of ClinicalTrials.gov, we found eight active studies focused on older adults in the ED. Of note, none of these studies evaluated intervention strategies to be used with a general older adult population.
The 2014 Guidelines offer recommendations across a number of domains (eg, staffing, administration, clinical procedures) and may, in combination with a theory-informed conceptual model, inform future studies. It is our experience that health systems often implement changes and measure their effects on an internal basis for quality improvement purposes. We would encourage health systems to design their evaluation of implemented change in such a way that it can be published for wider distribution and affect change on a large scale. Finally, future research may benefit from working across settings and disciplines, and from incorporating feedback from patients, care partners, and key stakeholders representing both ED and post-ED settings.
In conclusion, our results indicate mixed effects of ED intervention strategies on select clinical and utilization outcomes for older adults. In contrast to the growing number of older adults visiting the ED, we found a surprisingly small number of studies evaluating geriatric ED interventions. The limited number of studies using any single intervention strategy makes it difficult to draw definitive conclusions because of imprecise estimates of effect and variability in study populations, intervention strategies, and intervention components. However, we found evidence that individual studies evaluating multi-strategy interventions and those with a more comprehensive structure, as indicated by the presence of three key intervention components, may be associated with a small benefit in functional status, decreased hospitalization after the ED index visit, and a lower likelihood of ED return visit(s).
Supplementary Material
ACKNOWLEDGMENTS
This article is based on research conducted by the Evidence-based Synthesis Program (ESP) Center located at the Durham VA Medical Center, Durham, NC, funded by the Department of Veterans Affairs, Veterans Health Administration, and Office of Research and Development, Quality Enhancement Research Initiative. This work was also supported by the Center of Innovation for Health Services Research in Primary Care (CIN 13–410) at the Durham VA Health Care System. We would like to thank Liz Wing, MA; Avishek Nagi, MS; Jennifer McDuffie, PhD; and Megan Van Noord, MSIS, for their assistance with this project.
Financial Disclosure: US Department of Veterans Affairs (PROSPERO: CRD42018087660).
Sponsor’s Role: This project and the Durham VA ESP are funded by the US Department of Veterans Affairs that had no involvement in data collection, analysis, interpretation of the results, or the decision to submit this manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, the US government, or Duke University.
Footnotes
Conflict of Interest: The authors have declared no conflicts of interest for this article.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
REFERENCES
- 1.Rui P, Kang K. National hospital ambulatory medical care survey: 2014 emergency department summary tables. https://www.cdc.gov/nchs/ahcd/web_tables.htm. Accessed June 21, 2018.
- 2.Sinha SK, Bessman ES, Flomenbaum N, Leff B. A systematic review and qualitative analysis to inform the development of a new emergency department-based geriatric case management model. Ann Emerg Med. 2011; 57:672–682. [DOI] [PubMed] [Google Scholar]
- 3.Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39:238–247. [DOI] [PubMed] [Google Scholar]
- 4.Keim S, Sanders A. Geriatric emergency department use and care In: Meldon S, Ma OJ, Woolard R, eds. Geriatric Emergency Medicine. New York, NY: McGraw-Hill; 2004:1–3. [Google Scholar]
- 5.Sanders AB, Morley JE. The older person and the emergency department. J Am Geriatr Soc. 1993;41:880–882. [DOI] [PubMed] [Google Scholar]
- 6.Baum SA, Rubenstein LZ. Old people in the emergency room: age-related differences in emergency department use and care. J Am Geriatr Soc. 1987; 35:398–404. [DOI] [PubMed] [Google Scholar]
- 7.Grief CL. Patterns of ED use and perceptions of the elderly regarding their emergency care: a synthesis of recent research. J Emerg Nurs. 2003;29: 122–126. [DOI] [PubMed] [Google Scholar]
- 8.Preston LR, Chambers D, Campbell F, Cantrell A, Turner J, Goyder E. What evidence is there for the identification and management of frail older people in the emergency department? A systematic mapping review. National Institute for Health Research; Southampton, UK: Queen’s Printer and Controller of HMSO; April 2018. [PubMed] [Google Scholar]
- 9.Conroy SP, Stevens T, Parker SG, Gladman JR. A systematic review of comprehensive geriatric assessment to improve outcomes for frail older people being rapidly discharged from acute hospital: “interface geriatrics”. Age Ageing. 2011;40:436–443. [DOI] [PubMed] [Google Scholar]
- 10.Fealy G, McCarron M, O’Neill D, et al. Effectiveness of gerontologically informed nursing assessment and referral interventions for older persons attending the emergency department: systematic review. J Adv Nurs. 2009; 65:934–935. [DOI] [PubMed] [Google Scholar]
- 11.Jay S, Whittaker P, McIntosh J, Hadden N. Can consultant geriatrician led comprehensive geriatric assessment in the emergency department reduce hospital admission rates? A systematic review. Age Ageing. 2017;46:366–372. [DOI] [PubMed] [Google Scholar]
- 12.Lowthian JA, McGinnes RA, Brand CA, Barker AL, Cameron PA. Discharging older patients from the emergency department effectively: a systematic review and meta-analysis. Age Ageing. 2015;44:761–770. [DOI] [PubMed] [Google Scholar]
- 13.GEDI Wise Investigators, Adams J, Adinaro D, et al. GEDI WISE: geriatric emergency department innovations in care through workforce, informatics, and structural enhancements. Ann Emerg Med. 2013;62:S54–S55. [Google Scholar]
- 14.Carpenter CR, Heard K, Wilber S, et al. Research priorities for high-quality geriatric emergency care: medication management, screening, and prevention and functional assessment. Acad Emerg Med. 2011;18:644–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carpenter CR, Shah MN, Hustey FM, Heard K, Gerson LW, Miller DK. High yield research opportunities in geriatric emergency medicine: prehospital care, delirium, adverse drug events, and falls. J Gerontol A Biol Sci Med Sci. 2011;66A:775–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, Society for Academic Emergency Medicine, Geriatric Emergency Department Guidelines Task Force. Geriatric emergency department guidelines. Ann Emerg Med. 2014;63:e7–e25. [DOI] [PubMed] [Google Scholar]
- 17.Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: introducing multidisciplinary geriatric emergency department guidelines from the American College of Emergency Physicians, American Geriatrics Society, emergency nurses association, and Society for Academic Emergency Medicine. Acad Emerg Med. 2014;21:806–809. [DOI] [PubMed] [Google Scholar]
- 18.Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: introducing multidisciplinary geriatric emergency department guidelines from the American College of Emergency Physicians, American Geriatrics Society, emergency nurses association, and Society for Academic Emergency Medicine. J Am Geriatr Soc. 2014;62:1360–1363. [DOI] [PubMed] [Google Scholar]
- 19.Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: introducing multidisciplinary geriatric emergency department guidelines from the American College of Emergency Physicians, American Geriatrics Society, emergency nurses association, and Society for Academic Emergency Medicine. Ann Emerg Med. 2014;63:e1–e3. [DOI] [PubMed] [Google Scholar]
- 20.Pines JM, Lotrecchiano GR, Zocchi MS, et al. A conceptual model for episodes of acute, unscheduled care. Ann Emerg Med. 2016;68:484–491. e3. [DOI] [PubMed] [Google Scholar]
- 21.Gruneir A, Silver MJ, Rochon PA. Emergency department use by older adults: a literature review on trends, appropriateness, and consequences of unmet health care needs. Med Care Res Rev. 2011;68:131–155. [DOI] [PubMed] [Google Scholar]
- 22.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174:1095–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day hospitalization: a systematic review. Ann Intern Med. 2011; 155:520–528. [DOI] [PubMed] [Google Scholar]
- 24.Effective Practice and Organisation of Care (EPOC). EPOC Resources for Review Authors. Oslo, Norway: Norwegian Knowledge Centre for the Health Services; 2015. http://epoc.cochrane.org/resources/epoc-resourcesreview-authors. Accessed November 3, 2017. [Google Scholar]
- 25.List of OECD member countries—ratification of the convention on the OECD. http://www.oecd.org/about/membersandpartners/list-oecd-membercountries.htm. Accessed November 3, 2017.
- 26.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 27.Knapp G, Hartung J. Improved tests for a random effects meta-regression with a single covariate. Stat Med. 2003;22:2693–2710. [DOI] [PubMed] [Google Scholar]
- 28.Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406. [DOI] [PubMed] [Google Scholar]
- 29.GRADEpro GDT. GRADEpro Guideline Development Tool [software]. McMaster University, 2015. (developed by Evidence Prime, Inc.). gradepro.org. [Google Scholar]
- 30.Basic D, Conforti DA. A prospective, randomised controlled trial of an aged care nurse intervention within the emergency department. Aust Health Rev. 2005;29:51–59. [DOI] [PubMed] [Google Scholar]
- 31.Biese K, Lamantia M, Shofer F, et al. A randomized trial exploring the effect of a telephone call follow-up on care plan compliance among older adults discharged home from the emergency department. Acad Emerg Med. 2014; 21:188–195. [DOI] [PubMed] [Google Scholar]
- 32.Biese KJ, Busby-Whitehead J, Cai J, et al. Telephone follow-up for older adults discharged to home from the emergency department: a pragmatic randomized controlled trial. J Am Geriatr Soc. 2018;66:452–458. [DOI] [PubMed] [Google Scholar]
- 33.Caplan GA, Williams AJ, Daly B, Abraham K. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department—the DEED II study. J Am Geriatr Soc. 2004;52:1417–1423. [DOI] [PubMed] [Google Scholar]
- 34.Eklund K, Wilhelmson K, Gustafsson H, Landahl S, Dahlin-Ivanoff S. One-year outcome of frailty indicators and activities of daily living following the randomised controlled trial: “continuum of care for frail older people”. BMC Geriatr. 2013;13:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gagnon AJ, Schein C, McVey L, Bergman H. Randomized controlled trial of nurse case management of frail older people. J Am Geriatr Soc. 1999;47:1118–1124. [DOI] [PubMed] [Google Scholar]
- 36.McCusker J, Verdon J, Tousignant P, de Courval LP, Dendukuri N, Belzile E. Rapid emergency department intervention for older people reduces risk of functional decline: results of a multicenter randomized trial. J Am Geriatr Soc. 2001;49:1272–1281. [DOI] [PubMed] [Google Scholar]
- 37.Mion LC, Palmer RM, Meldon SW, et al. Case finding and referral model for emergency department elders: a randomized clinical trial. Ann Emerg Med. 2003;41:57–68. [DOI] [PubMed] [Google Scholar]
- 38.Runciman P, Currie CT, Nicol M, Green L, McKay V. Discharge of elderly people from an accident and emergency department: evaluation of health visitor follow-up. J Adv Nurs. 1996;24:711–718. [DOI] [PubMed] [Google Scholar]
- 39.Arendts G, Fitzhardinge S, Pronk K, Donaldson M, Hutton M, Nagree Y. The impact of early emergency department allied health intervention on admission rates in older people: a non-randomized clinical study. BMC Geriatr. 2012;12:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arendts G, Fitzhardinge S, Pronk K, Hutton M. Outcomes in older patients requiring comprehensive allied health care prior to discharge from the emergency department. Emerg Med Australas. 2013;25:127–131. [DOI] [PubMed] [Google Scholar]
- 41.Bond CM, Freiheit EA, Podruzny L, et al. The emergency to home project: impact of an emergency department care coordinator on hospital admission and emergency department utilization among seniors. Int J Emerg Med. 2014;7:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Miller DK, Lewis LM, Nork MJ, Morley JE. Controlled trial of a geriatric case-finding and liaison service in an emergency department. J Am Geriatr Soc. 1996;44:513–520. [DOI] [PubMed] [Google Scholar]
- 43.Mortimer C, Emmerton L, Lum E. The impact of an aged care pharmacist in a department of emergency medicine. J Eval Clin Pract. 2011;17:478–485. [DOI] [PubMed] [Google Scholar]
- 44.Pedersen LH, Gregersen M, Barat I, Damsgaard EM. Early geriatric follow-up after discharge reduces readmissions—a quasi-randomised controlled trial. Eur Geriatr Med. 2016;7:443–448. [DOI] [PubMed] [Google Scholar]
- 45.Karam G, Radden Z, Berall LE, Cheng C, Gruneir A. Efficacy of emergency department-based interventions designed to reduce repeat visits and other adverse outcomes for older patients after discharge: a systematic review. Geriatr Gerontol Int. 2015;15:1107–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Working Group on Health Outcomes for Older Persons with Multiple Chronic Conditions. Universal health outcome measures for older persons with multiple chronic conditions. J Am Geriatr Soc. 2012;60:2333–2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schumacher JG, Hirshon JM, Magidson P, Chrisman M, Hogan T. Tracking the rise of geriatric emergency departments in the United States. J Appl Gerontol. 2018; 0733464818813030. 10.1177/0733464818813030 [DOI] [PubMed] [Google Scholar]
- 48.Hwang U, Dresden SM, Rosenberg MS, et al. Geriatric emergency department innovations: transitional care nurses and hospital use. J Am Geriatr Soc. 2018;66:459–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wallis M, Marsden E, Taylor A, et al. The geriatric emergency department intervention model of care: a pragmatic trial. BMC Geriatr. 2018;18:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


